Management of acute myocardial infarction in patients presenting ...
Management of acute myocardial infarction in patients presenting ...
Management of acute myocardial infarction in patients presenting ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
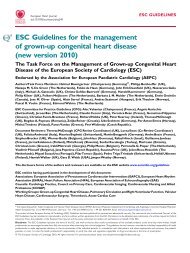
ESC Guidel<strong>in</strong>es 2933<br />
Table 22 Long-term management <strong>of</strong> specific coronary risk factors and LV dysfunction<br />
Recommendations Class a Level b<br />
.............................................................................................................................................................................<br />
Smok<strong>in</strong>g cessation<br />
Assess smok<strong>in</strong>g status and advise to quit and to avoid passive smok<strong>in</strong>g at each visit I B<br />
Bupropione and nicot<strong>in</strong>e treatment <strong>in</strong> <strong>patients</strong> who keep smok<strong>in</strong>g at follow-up I B<br />
Antidepressants IIa C<br />
.............................................................................................................................................................................<br />
Physical activity<br />
Exercise test-guided moderate <strong>in</strong>tensity aerobic exercise at least five times per week I B<br />
Medically supervised rehabilitation programmes for high-risk <strong>patients</strong> I B<br />
.............................................................................................................................................................................<br />
Diabetes management<br />
Lifestyle changes and pharmacotherapy to achieve HbA1c ,6.5% I B<br />
Intensive modification <strong>of</strong> other risk factors (hypertension, obesity, dyslipidaemia) I B<br />
Coord<strong>in</strong>ation with a physician specialized <strong>in</strong> diabetes I C<br />
.............................................................................................................................................................................<br />
Diet and weight reduction<br />
Weight reduction is recommended when BMI is 30 kg/m 2 and when waist circumference is .102/88 cm (men/women) I B<br />
Diet based on low <strong>in</strong>take <strong>of</strong> salt and saturated fats, and regular <strong>in</strong>take <strong>of</strong> fruit, vegetables, and fish I B<br />
Increased consumption <strong>of</strong> omega-3 fatty acid (oily fish) IIb B<br />
Supplementation with 1 g <strong>of</strong> fish oil <strong>in</strong> <strong>patients</strong> with a low <strong>in</strong>take <strong>of</strong> oily fish IIa B<br />
Moderate alcohol consumption should not be discouraged I B<br />
.............................................................................................................................................................................<br />
Blood pressure control<br />
Lifestyle changes and pharmacotherapy to achieve BP ,130/80 mmHg I A<br />
.............................................................................................................................................................................<br />
Lipid management<br />
Stat<strong>in</strong>s <strong>in</strong> all <strong>patients</strong>, <strong>in</strong> the absence <strong>of</strong> contra<strong>in</strong>dications, irrespective <strong>of</strong> cholesterol levels, <strong>in</strong>itiated as soon as possible to achieve I A<br />
LDL cholesterol ,100 mg/dL (2.5 mmol/L)<br />
Further reduction <strong>of</strong> LDL cholesterol to achieve ,80 mg/dL (2.0 mmol/L) should be considered <strong>in</strong> high-risk <strong>patients</strong> IIa A<br />
Lifestyle change emphasized if TG .150 mg/dL (1.7 mmol/L) and/or HDL cholesterol ,40 mg/dL (1.0 mmol/L) I B<br />
Fibrates and omega-3 supplements should be considered <strong>in</strong> <strong>patients</strong> who do not tolerate stat<strong>in</strong>s, especially if TG .150 mg/dL IIa B<br />
(1.7 mmol/L) and/or HDL cholesterol ,40 mg/ dL (1.0 mmol/L)<br />
.............................................................................................................................................................................<br />
<strong>Management</strong> <strong>of</strong> heart failure or LV dysfunction<br />
Oral b-blockers <strong>in</strong> all <strong>patients</strong> without contra<strong>in</strong>dications I A<br />
ACE-<strong>in</strong>hibitors <strong>in</strong> all <strong>patients</strong> without contra<strong>in</strong>dications I A<br />
ARB (valsartan) <strong>in</strong> all <strong>patients</strong> without contra<strong>in</strong>dications who do not tolerate ACE-<strong>in</strong>hibitors I B<br />
Aldosterone antagonists if EF 40% and signs <strong>of</strong> heart failure or diabetes if creat<strong>in</strong><strong>in</strong>e is ,2.5 mg/dL <strong>in</strong> men and ,2.0 mg/dL I B<br />
<strong>in</strong> women and potassium is ,5.0 mmol/L<br />
CRT <strong>in</strong> <strong>patients</strong> with EF 35% and QRS duration <strong>of</strong> 120ms who rema<strong>in</strong> <strong>in</strong> NYHA class III–VI <strong>in</strong> spite <strong>of</strong> optimal medical I A<br />
therapy if stunn<strong>in</strong>g can be excluded<br />
.............................................................................................................................................................................<br />
Prevention <strong>of</strong> sudden death<br />
ICD if EF 30–40% and NYHA II or III at least 40 days after STEMI I A<br />
ICD if EF 30–35% and NYHA I at least 40 days after STEMI IIa B<br />
a Class <strong>of</strong> recommendation.<br />
b Level <strong>of</strong> evidence.<br />
TG ¼ triglyceride.<br />
is raised. Many processed and prepared foods are high <strong>in</strong> salt, and<br />
<strong>in</strong> fat <strong>of</strong> doubtful quality.<br />
There is no evidence for the use <strong>of</strong> antioxidant supplements<br />
<strong>of</strong> antioxidants, low glycaemic <strong>in</strong>dex diets, or homocyste<strong>in</strong>elower<strong>in</strong>g<br />
therapies post-STEMI. The role <strong>of</strong> omega-3 fatty acid<br />
supplements for secondary prevention is unclear. 183 In the only<br />
(open-label) randomized study <strong>in</strong> <strong>patients</strong> post-<strong>myocardial</strong> <strong><strong>in</strong>farction</strong>,<br />
the GISSI prevenzione trial, 1 g daily <strong>of</strong> fish oil on top <strong>of</strong> a<br />
Mediterranean diet significantly reduced total and cardiovascular<br />
mortality. 197 However a meta-analysis, <strong>in</strong>clud<strong>in</strong>g GISSI prevenzione,<br />
showed no effect on mortality or cardiovascular events 198<br />
and no evidence that the source or dose affect outcome.<br />
Obesity is an <strong>in</strong>creas<strong>in</strong>g problem <strong>in</strong> <strong>patients</strong> with STEMI. At least<br />
one-third <strong>of</strong> European women and one <strong>in</strong> four men with <strong>acute</strong><br />
coronary syndromes below the age <strong>of</strong> 65 have a body mass<br />
<strong>in</strong>dex (BMI) <strong>of</strong> 30 kg/m 2 . 199 Current ESC Guidel<strong>in</strong>es 183 def<strong>in</strong>e a