Management of acute myocardial infarction in patients presenting ...
Management of acute myocardial infarction in patients presenting ...
Management of acute myocardial infarction in patients presenting ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ESC Guidel<strong>in</strong>es 2915<br />
The hypotension and bradycardia will usually respond to atrop<strong>in</strong>e<br />
(0.5–1 mg i.v., up to a total dose <strong>of</strong> 2 mg), and respiratory<br />
depression may require ventilatory support. Oxygen (2–4 L/m<strong>in</strong><br />
by mask or nasal prongs) should be adm<strong>in</strong>istered to those who<br />
are breathless or who have any features <strong>of</strong> heart failure or shock<br />
(see also Table 15). Non-<strong>in</strong>vasive monitor<strong>in</strong>g <strong>of</strong> blood oxygen<br />
saturation greatly helps <strong>in</strong> decid<strong>in</strong>g on the need for oxygen adm<strong>in</strong>istration<br />
or, <strong>in</strong> severe cases, ventilatory support. Non-steroidal<br />
anti-<strong>in</strong>flammatory drugs (NSAIDs) should not be given for pa<strong>in</strong><br />
relief because <strong>of</strong> possible prothrombotic effects.<br />
Anxiety is a natural response to the pa<strong>in</strong> and to the circumstances<br />
surround<strong>in</strong>g a heart attack. Reassurance <strong>of</strong> <strong>patients</strong> and<br />
those closely associated with them is <strong>of</strong> great importance. If the<br />
patient becomes excessively disturbed, it may be appropriate to<br />
adm<strong>in</strong>ister a tranquillizer, but opioids are all that is required <strong>in</strong><br />
many cases.<br />
3. Cardiac arrest<br />
Many deaths occur <strong>in</strong> the very first hours after STEMI due to<br />
ventricular fibrillation (VF). The implementation <strong>of</strong> an organization<br />
to cope with out-<strong>of</strong>-hospital cardiac arrest is pivotal to provide<br />
prompt cardiopulmonary resuscitation, early defibrillation if<br />
needed, and effective advanced cardiac life support. Availability<br />
<strong>of</strong> automated external defibrillators is a key factor <strong>in</strong> <strong>in</strong>creas<strong>in</strong>g<br />
survival. Readers are referred to the latest guidel<strong>in</strong>es on cardiopulmonary<br />
resuscitation provided by the European Resuscitation<br />
Council. 22<br />
D. Pre-hospital or early<br />
<strong>in</strong>-hospital care<br />
1. Restor<strong>in</strong>g coronary flow and<br />
<strong>myocardial</strong> tissue reperfusion<br />
For <strong>patients</strong> with the cl<strong>in</strong>ical presentation <strong>of</strong> STEMI with<strong>in</strong> 12 h<br />
after symptom onset and with persistent ST-segment elevation<br />
or new or presumed new left bundle-branch block, early mechanical<br />
(PCI) or pharmacological reperfusion should be performed.<br />
There is general agreement that reperfusion therapy (primary<br />
PCI) should be considered if there is cl<strong>in</strong>ical and/or electrocardiographic<br />
evidence <strong>of</strong> ongo<strong>in</strong>g ischaemia, even if, accord<strong>in</strong>g to the<br />
patient, symptoms started .12 h before as the exact onset <strong>of</strong><br />
symptoms is <strong>of</strong>ten unclear. However, there is no consensus as to<br />
whether PCI is also beneficial <strong>in</strong> <strong>patients</strong> present<strong>in</strong>g .12 h from<br />
symptom onset <strong>in</strong> the absence <strong>of</strong> cl<strong>in</strong>ical and/or electrocardiographic<br />
evidence <strong>of</strong> ongo<strong>in</strong>g ischaemia. In a randomized study <strong>in</strong><br />
STEMI <strong>patients</strong> present<strong>in</strong>g without persist<strong>in</strong>g symptoms between<br />
12 and 48 h after symptom onset (n ¼ 347), PCI was associated<br />
with significant <strong>myocardial</strong> salvage, lend<strong>in</strong>g some support to an<br />
<strong>in</strong>vasive strategy <strong>in</strong> these <strong>patients</strong>, but cl<strong>in</strong>ical outcomes were not<br />
better. 23 In the OAT trial <strong>in</strong>clud<strong>in</strong>g 2166 stable <strong>patients</strong> with an<br />
occluded <strong>in</strong>farct-related vessel 3 to 28 calendar days after<br />
symptom onset, PCI did not improve cl<strong>in</strong>ical outcome, 24 <strong>in</strong>clud<strong>in</strong>g<br />
<strong>in</strong> the subgroup <strong>of</strong> 331 <strong>patients</strong> randomized between 24 and 72 h<br />
after onset <strong>of</strong> <strong><strong>in</strong>farction</strong>. 25 No firm recommendations can be<br />
made given the limited data currently available (Table 5).<br />
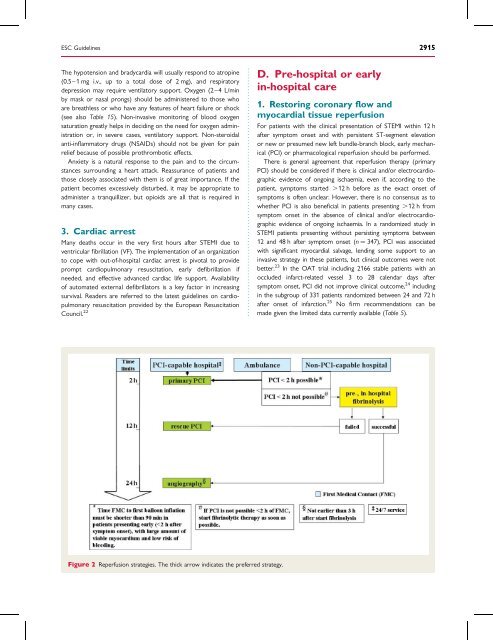
Figure 2 Reperfusion strategies. The thick arrow <strong>in</strong>dicates the preferred strategy.