Annual Report 2009-2010 - Merseyside & Cheshire Cancer Network
Annual Report 2009-2010 - Merseyside & Cheshire Cancer Network
Annual Report 2009-2010 - Merseyside & Cheshire Cancer Network
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>-<strong>2010</strong>
Contents<br />
Foreword 3<br />
About the <strong>Merseyside</strong> and <strong>Cheshire</strong> <strong>Cancer</strong> <strong>Network</strong> 4<br />
Director’s report 5<br />
Key achievements: <strong>2009</strong>/<strong>2010</strong> 6<br />
Focus for <strong>2010</strong>/2011 7<br />
<strong>Cancer</strong> intelligence 8<br />
<strong>Cancer</strong> peer review programme 12<br />
<strong>Network</strong> groups: Service improvement 13<br />
<strong>Network</strong> groups: Development of clinical practice, pathways and guidelines 17<br />
<strong>Network</strong> groups: Excellence in clinical audit 20<br />
<strong>Network</strong> groups: Education, training and workforce development 22<br />
Medical Director’s report 24<br />
Nursing 25<br />
Research 26<br />
Patient and public involvement 28<br />
iVan 30<br />
Cover image: gates at Warrington town hall<br />
2 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Foreword<br />
<strong>Network</strong> chair: Kathy Doran<br />
I am delighted to<br />
welcome you to the<br />
eighth annual report<br />
of the <strong>Merseyside</strong><br />
and <strong>Cheshire</strong> <strong>Cancer</strong><br />
<strong>Network</strong> (MCCN). This<br />
report highlights the<br />
main achievements and<br />
collaborations that have helped to develop cancer<br />
services for local people and their carers during<br />
<strong>2009</strong>/<strong>2010</strong>.<br />
The network continued to deliver against an<br />
ambitious programme of work during <strong>2009</strong>/<strong>2010</strong><br />
with the overarching aims to reduce cancer<br />
incidence, to reduce the effects of cancer and<br />
to reduce mortality across the population. In<br />
particular work was focused on:<br />
• ensuring delivery of the recommendations<br />
from the <strong>Cancer</strong> Reform Strategy and further<br />
developed through the North West <strong>Cancer</strong> Plan<br />
• ensuring compliance with the national cancer<br />
peer review programme<br />
• developing services collaboratively, based on<br />
evidence, recognised good practice, and clinical<br />
pathways, for the benefit of all patients in<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong><br />
• highlighting where services can become more<br />
efficient without compromising quality and<br />
standards<br />
• continuing to focus on further developing<br />
services to support patients at the end of<br />
their life, with partners in other conditions,<br />
including dementia, heart failure, respiratory<br />
and renal disease<br />
• reducing health inequalities in the population,<br />
by focusing on access to services and reducing<br />
variations in care<br />
• informing the commissioning and delivery of<br />
world class cancer services for local people<br />
Committed patients, carers, volunteers and staff<br />
continue to make a significant contribution<br />
to the collective work of the network and to<br />
invest time and energy in mature collaboration<br />
across organisations. The strength of these local<br />
commitments and relationships forms an excellent<br />
basis for continued work into <strong>2010</strong>/11, when we<br />
will be collectively challenged to transform care to<br />
ensure even better outcomes for patients, to take<br />
further steps to improve quality and productivity<br />
and to demonstrate that we collectively<br />
commission and deliver services which represent a<br />
good investment of resource.<br />
I would like to formally thank all of our partners,<br />
in particular all of our clinicians, patient and carers,<br />
for their continued commitment, time and energy.<br />
I look forward to continuing collaboration into<br />
<strong>2010</strong>/11.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 3
About the <strong>Merseyside</strong> and <strong>Cheshire</strong> <strong>Cancer</strong><br />
<strong>Network</strong><br />
The <strong>Merseyside</strong> & <strong>Cheshire</strong><br />
<strong>Cancer</strong> <strong>Network</strong> was formed<br />
in 2000 and links together the<br />
organisations that provide care<br />
for people with cancer across<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong>.<br />
We work closely with patients,<br />
carers, health professionals and<br />
managers to help implement<br />
the NHS <strong>Cancer</strong> Reform Strategy<br />
and North West <strong>Cancer</strong><br />
Plan for the people<br />
of <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong>.<br />
The network covers<br />
a population of 2.3<br />
million people and<br />
encompasses one strategic<br />
health authority, seven primary<br />
care trusts, twelve hospital trusts,<br />
ten hospices and a number of<br />
voluntary organisations.<br />
The purpose of the network is<br />
broadly to organise and oversee<br />
the local implementation of the<br />
NHS <strong>Cancer</strong> Reform Strategy,<br />
which sets out a programme<br />
of investment and reform. The<br />
plan also includes a number<br />
of ambitious targets, with the<br />
overall aim to save more lives<br />
and to improve the patient’s<br />
experience by ensuring that<br />
people with cancer have access<br />
to the right professional support<br />
and access to the best treatment<br />
throughout their period<br />
of care.<br />
The network is managed by<br />
the <strong>Cancer</strong> Taskforce who are<br />
accountable for ensuring that<br />
the network meets its key<br />
responsibilities and objectives as<br />
defined within the Manual of<br />
<strong>Cancer</strong> Services Standards. The<br />
<strong>Cancer</strong> Taskforce meets quarterly;<br />
its membership is drawn from<br />
chief executives of trusts and<br />
PCTs across the network.<br />
Clinical network groups (CNGs)<br />
are the prime focus of the<br />
network’s activity and work<br />
alongside the cancer research<br />
network.<br />
The CNGs are the source of<br />
‘expert’ clinical opinion from<br />
which the Taskforce draws its<br />
advice on a wide range of<br />
service issues including<br />
clinical guidelines and<br />
treatment options.<br />
They adopt an evidencebased<br />
approach,<br />
adopting the National<br />
Institute for Health and<br />
Clinical Excellence (NICE)<br />
guidance as their reference for<br />
determining common standards<br />
and pathways for cancer<br />
patients. Patients and carers are<br />
increasingly playing an important<br />
role in the work of these groups;<br />
we welcome patient and carer<br />
members on all CNGs.<br />
For more information, please see<br />
our website at www.mccn.nhs.uk.<br />
4 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Director’s report<br />
<strong>Network</strong> director: Pat Higgins<br />
The <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong> <strong>Cancer</strong> <strong>Network</strong><br />
works with partners to<br />
help prevent and tackle<br />
cancer, and ensure that<br />
local people can access<br />
high quality services,<br />
including end of life<br />
care. The network supports commissioners to be world<br />
class, works alongside providers to help translate<br />
developments and evidence into clinical services and<br />
engages with patients and their carers to ensure<br />
that their views influence decisions and inform the<br />
continued developments and improvements. <strong>Cancer</strong><br />
remains a strategic health priority for <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong>, because of high rates of cancer and high<br />
rates of death from cancer. The network continues<br />
to encourage collective work to keep a spotlight on<br />
the impact that cancer has on the population and to<br />
promote the continual improvement of services.<br />
care teams on a range of initiatives to promote learning<br />
around early detection of cancer and have continued to<br />
promote cancer screening programmes.<br />
Increasingly, the network is focusing on the quality<br />
of services: leading the peer review process, ensuring<br />
that the experience of patients and carers is reflected<br />
in strategy and using data to identify priorities for<br />
improvement and to recognise where services are<br />
delivering a high quality of care. We have been<br />
promoting clinical trials and the development of<br />
research, while developing new models of care in<br />
order to improve clinical outcomes for patients and to<br />
develop the cancer workforce to respond to changes<br />
in clinical practice. We are also developing approaches<br />
to ensure support for people living with and beyond<br />
cancer. Over the next few years, this drive to improve<br />
quality will continue in an increasingly constrained<br />
financial environment and we will continue to promote<br />
consistency in care.<br />
We are particularly proud of the work that has<br />
developed during <strong>2009</strong>/10 to reach out to communities<br />
and local people to support campaigns to help prevent<br />
cancer, as well as to raise awareness of the signs and<br />
symptoms to promote early detection. Through this<br />
work with local partners, volunteers and communities,<br />
we have helped people with undiagnosed cancer to<br />
seek professional help. We have lobbied successfully<br />
and worked on raising awareness on the dangers<br />
of sunbeds and exposure to sun, with parliament<br />
approving legislation in early <strong>2010</strong> on the use of<br />
sunbeds by children. We have worked with primary<br />
I would like to thank everybody who made a<br />
contribution to the network during <strong>2009</strong>/<strong>2010</strong>. The<br />
network functions well because of the active and<br />
committed participation of our partners. This report<br />
acknowledges the collective achievements, work and<br />
input of patients, carers, staff and clinicians as well<br />
as the efforts of our partner organisations in shared<br />
efforts and focus to prevent cancer and minimise its<br />
impact. I look forward to working with you to address<br />
the challenges we will face over the forthcoming year,<br />
to ensure that we continue to serve the interests of our<br />
population to the very best of our collective ability.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 5
Key achievements: <strong>2009</strong>/<strong>2010</strong><br />
Preventing cancer and diagnosing cancer earlier<br />
• The network continued to lead lobbying to<br />
introduce legislation on sun bed usage, and<br />
supported the further development of smoking<br />
cessation strategies.<br />
• The bowel cancer screening programme<br />
completed its first cycle; we are working with<br />
communities with lower screening uptake.<br />
• Work was started to modernise cervical cytology<br />
laboratory configuration and move towards a two<br />
week turnaround time for results reporting.<br />
• Breast units started to plan for the extension of<br />
the breast screening programme.<br />
• Education, audit and review of cancer diagnosis<br />
trends started in all PCTs, with primary care and<br />
public health active partners in this work.<br />
• iVan (page 30) engaged with over 14,000 people<br />
and helped with early diagnosis of cancers.<br />
Better treatment in the most appropriate settings<br />
• The network and its partner trusts got to grips<br />
with the new challenging peer review schedule.<br />
• Significant service developments during <strong>2009</strong>/10<br />
include the development of the network wide<br />
sarcoma service.<br />
• The acute oncology model was developed,<br />
resulting in the recruitment of an additional five<br />
clinical oncologists and nursing roles in support<br />
of the actute oncology model which is now in the<br />
process of being implemented.<br />
• A significant programme of work continued to<br />
promote the use of end of life tools to improve<br />
choice for people towards the end of their lives.<br />
• <strong>2009</strong>/10 saw the opening of the Liverpool <strong>Cancer</strong><br />
Trials Unit, a partnership with the University of<br />
Liverpool, <strong>Cancer</strong> Research UK and <strong>Merseyside</strong><br />
and <strong>Cheshire</strong> <strong>Cancer</strong> Research <strong>Network</strong> to improve<br />
access to trials and support the development of<br />
new clinical trials.<br />
• Sustained and further improvement of cancer<br />
waiting times targets across the network (page 8).<br />
• The Anticipatory Care calendar Project received a<br />
prestigious nomination and commendation at the<br />
<strong>2009</strong> Trustech North West NHS Innovation Awards.<br />
Living with and beyond cancer<br />
• The guideline for the key worker role was agreed<br />
for roll-out across the network.<br />
• The network continued to ensure that patient<br />
and carer views influenced the development of<br />
pathways during and following treatment.<br />
• Macmillan support was secured to pilot health and<br />
wellbeing clinics in two hospitals.<br />
Stronger commissioning<br />
• An exercise to assess the network against the<br />
11 world class commissioning competencies<br />
was undertaken. MCCN was noted to be well<br />
placed to support PCTs in commissioning quality<br />
cancer services and was recognised for its work in<br />
supporting the collection of meaningful clinical<br />
data real time to help inform strategic planning.<br />
6 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Focus for <strong>2010</strong>/2011<br />
The network will continue to lead the delivery of the <strong>Cancer</strong> Reform Strategy and North West <strong>Cancer</strong><br />
Plan across <strong>Merseyside</strong> and <strong>Cheshire</strong>. In accordance with our objectives, we aim to:<br />
1<br />
Continue to focus on reducing health<br />
inequalities, working particularly with learning<br />
disabilities, mental health and prison groups.<br />
2<br />
Further embed the network strategy for<br />
early detection and prevention to improve<br />
population awareness of the signs and<br />
symptoms of cancer and to promote earlier<br />
presentation.<br />
3<br />
Work in partnership with the University of<br />
Liverpool to develop a world class academic<br />
oncology unit to further increase research<br />
activity within the network.<br />
4<br />
Continue to work with providers and<br />
commissioners to expand radiotherapy facilities<br />
to improve access for all patients, reducing<br />
travel times and developing purpose-built state<br />
of the art facilities.<br />
5<br />
Work with providers and commissioners to<br />
expand the oncology workforce, to include<br />
establishing acute oncology teams in all<br />
hospitals with A&E departments, so that<br />
patients are cared for where and when is most<br />
appropriate.<br />
6<br />
Implement remedial action arising from peer<br />
review in conjunction with clinical network<br />
groups and partner organisations.<br />
7<br />
Continue to improve the quality of clinical<br />
information, building on the successes within<br />
the staging project in each MDT and adding<br />
to intelligence regarding cancer presentation,<br />
treatment and outcomes.<br />
8<br />
Support improved access to laparoscopic<br />
surgery across the network by increasing<br />
capacity and developing the workforce,<br />
enabling patients to make an informed choice<br />
regarding types of treatment.<br />
9<br />
Continue the implementation of action plans<br />
for Improving Outcomes Guidance (IOG) to<br />
10<br />
11<br />
12<br />
ensure all patients have access to services that<br />
are delivered to nationally recommended<br />
standards.<br />
Continue to develop pathways that meet new<br />
and extended waiting time targets to further<br />
reduce referral to treatment times.<br />
Lead an inpatient improvement programme<br />
that supports innovative practice and improves<br />
the quality and efficiency of inpatient services.<br />
Work with commissioners and providers to<br />
improve the quality and productivity of cancer<br />
services to ensure optimal use of resources in<br />
the delivery of services.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 7
<strong>Cancer</strong> intelligence<br />
The challenge of incidence (new<br />
cases) and mortality (death rates)<br />
150<br />
Figure 1.1: National and network incidence rates (2005-2007)<br />
is ubiquitous within the whole of<br />
the North West. <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong>, Lancashire and South<br />
Cumbria and Greater Manchester<br />
and <strong>Cheshire</strong> all experience rates<br />
that are higher than the national<br />
average.<br />
Age-standardised rate (per 100,000 applicable population)<br />
120<br />
90<br />
60<br />
30<br />
0<br />
Urological<br />
(all persons)<br />
Breast<br />
(female)<br />
Lung<br />
(all persons)<br />
Colorectal<br />
(all persons)<br />
Upper GI<br />
(all persons)<br />
MCCN<br />
GMCCN<br />
LSCCN<br />
England<br />
New cases diagnosed within<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong><br />
numbered 11,146 in 2007, which<br />
represented a 3% increase<br />
compared to 2006. In contrast,<br />
the Lancashire and South<br />
Cumbria, Greater Manchester<br />
and <strong>Cheshire</strong> and England<br />
experienced a decrease in new<br />
cases. Like the other networks<br />
in the North West, the most<br />
common tumour types in<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong> were<br />
urological, breast, lung, lower<br />
gastrointestinal and upper<br />
gastrointestinal respectively.<br />
Both nationally and within<br />
the North West, <strong>Merseyside</strong><br />
and <strong>Cheshire</strong> has the highest<br />
incidence rate for all cancers<br />
(2005-2007). Within the most<br />
common tumour types, the<br />
network also has the highest<br />
incidence rates for breast,<br />
lung, colorectal and upper<br />
gastrointestinal for the region,<br />
all of which exceed the national<br />
rate as well (Figure 1.1).<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong> has<br />
the highest mortality rates in<br />
the region and nationally for<br />
all cancers (2006-2008). Of the<br />
most common tumour types,<br />
urological, lung, colorectal<br />
and upper gastrointestinal all<br />
demonstrate mortality rates<br />
higher than the national level.<br />
In addition to this, urological,<br />
lung, colorectal and upper<br />
gastrointestinal cancers have the<br />
highest mortality rates in the<br />
region. In contrast, however, the<br />
mortality rate for breast cancer<br />
is below the national rate (figure<br />
1.2).<br />
With regards to cancer survival,<br />
one-year survival is used as a<br />
measurement of early diagnosis,<br />
as the patients who die within a<br />
year of diagnosis are more likely<br />
to have been diagnosed at an<br />
advanced stage of disease. The<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong> network<br />
has the lowest one-year survival<br />
rates (2003-2007) in the North<br />
West for all cancer types.<br />
When considered individually,<br />
urological, colorectal and lung<br />
cancer one-year survival rates<br />
exceed the national rate and<br />
are the highest regionally. In<br />
contrast, breast and upper<br />
gastrointestinal cancer one-year<br />
survival is below the national<br />
rate, with the latter being the<br />
8 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Cancer</strong> intelligence (continued)<br />
Age-standardised rate (per 100,000 applicable population)<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
Urological<br />
(all persons)<br />
Figure 1.2: National and network mortality rates (2006-2008)<br />
Breast<br />
(female)<br />
lowest in the region (figure 1.3).<br />
Five-year survival rates provide a<br />
measure of the effectiveness of<br />
treatments received by patients.<br />
The latest information (1998-<br />
2002) has highlighted that<br />
Lung<br />
(all persons)<br />
the <strong>Merseyside</strong> and <strong>Cheshire</strong><br />
network has the highest fiveyear<br />
survival in the North West<br />
for all cancer types, although<br />
this is lower than the national<br />
rate. Individual consideration<br />
of tumour types has shown that<br />
urological, lung and upper gastro<br />
intestinal cancer five-year survival<br />
is the highest in the region and<br />
higher than the national level.<br />
Once again, in contrast to this,<br />
breast and colorectal cancer fiveyear<br />
survival rates are both lower<br />
than the national figure, with<br />
the latter being the lowest in the<br />
Colorectal<br />
(all persons)<br />
region (figure 1.4 overleaf).<br />
Programme budgeting<br />
Programme budgeting not only<br />
enables the network to outline<br />
spend on cancer services within<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong>, but<br />
also allows a comparison with the<br />
other networks within the North<br />
West and nationally. Intelligence<br />
surrounding programme<br />
budgeting enables organisations<br />
Relative survival (%)<br />
100<br />
80<br />
60<br />
40<br />
20<br />
0<br />
Upper GI<br />
(all persons)<br />
All cancers<br />
MCCN<br />
GMCCN<br />
LSCCN<br />
England<br />
to understand current patterns<br />
of service provision and where<br />
improvements can be made.<br />
<strong>Cancer</strong> spend in <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong> improved dramatically<br />
from 2004/05 to 2008/09, with<br />
network expenditure increasing<br />
from £6 million to £9.7 million<br />
per 100 000 of the population.<br />
This expenditure now exceeds<br />
the national rate and means the<br />
network is equivalent to other<br />
cancer network within the North<br />
West (figure 1.5).<br />
It is important to note that<br />
this programme budgeting<br />
category only covers diseasespecific<br />
costs and expenditure<br />
on early detection, prevention,<br />
screening and cancer awareness<br />
are addressed within the ‘healthy<br />
Figure 1.3: National and regional one year survival (2002-2006)<br />
Urological<br />
Breast<br />
Lung<br />
Colorectal Upper gastrointestinal<br />
MCCN<br />
GMCCN<br />
LSCCN<br />
England<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 9
<strong>Cancer</strong> intelligence (continued)<br />
individuals’ category (Figure<br />
1.5). Figure 1.5 illustrates a 68%<br />
100<br />
Figure 1.4: National and regional five year survival (1998-2002)<br />
increases in expenditure with<br />
regards to this category since<br />
the <strong>Cancer</strong> Reform Strategy<br />
(2007) and the announcement<br />
of National Awareness and Early<br />
Detection initiative (NAEDI).<br />
Relative survival (%)<br />
80<br />
60<br />
40<br />
20<br />
MCCN<br />
GMCCN<br />
LSCCN<br />
England<br />
<strong>Cancer</strong> waiting times<br />
0<br />
All cancers<br />
Urinary tract<br />
Breast<br />
Lung<br />
Colorectal<br />
Upper GI<br />
Reducing the time that a<br />
patient waits for the beginning<br />
of treatment from an urgent<br />
referral plays a fundamental<br />
role in the efficient and timely<br />
delivery of services. Intelligence<br />
surrounding this data enables<br />
local trusts to assess whether<br />
delays in waiting times are a<br />
result of the system of care<br />
rather than diagnosis or a<br />
patient’s personal choice.<br />
Two week wait referrals<br />
target<br />
In total, 40829 urgent referrals<br />
took place from April <strong>2009</strong> to<br />
March <strong>2010</strong>, which, on average,<br />
meant 3402 patients with<br />
suspected cancer were seen<br />
across <strong>Merseyside</strong> and <strong>Cheshire</strong><br />
per month. The network<br />
achieved the national standard<br />
for 11 months out of this period.<br />
31 day first treatment target<br />
Expenditure (£million/100,000 population)<br />
Figure 1.5: <strong>Network</strong> and national expenditure for Healthy Individuals Programme<br />
12<br />
10<br />
GMCCN Ca<br />
LSCCN Ca<br />
8<br />
6<br />
MCCN Ca<br />
National Ca<br />
GMCCN HI<br />
4<br />
2<br />
LSCCN HI<br />
MCCN HI<br />
National HI<br />
0<br />
2006/2007 2007/2008 2008/<strong>2009</strong><br />
The network exceeded this target<br />
from March to December <strong>2009</strong><br />
by ensuring that 98% patients<br />
began their first treatment<br />
within 31 days.<br />
31 day subsequent treatment<br />
target<br />
Following the expansion of<br />
national standards with regards<br />
10 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Cancer</strong> intelligence (continued)<br />
Figure 1.6: 62 day wait for first treatment - urgent GP referral to treatment<br />
<strong>Merseyside</strong> and <strong>Cheshire</strong><br />
Performance threshold<br />
even now, these issues are being<br />
addressed.<br />
% Performance<br />
100<br />
95<br />
90<br />
85<br />
80<br />
75<br />
70<br />
65<br />
60<br />
March April May June July<br />
to cancer waiting times, the<br />
network has closely monitored<br />
the progress for this target.<br />
Surgery<br />
The network achieved the<br />
standard required for subsequent<br />
surgical treatment by achieving<br />
97% for the ten month period.<br />
This involved the surgical<br />
treatment of 4661 patients<br />
within 31 days.<br />
Drugs<br />
The <strong>Merseyside</strong> and <strong>Cheshire</strong><br />
network has performed very<br />
well with regards to this type of<br />
treatment. Of 1933 patients that<br />
were treated, only six had to wait<br />
longer than the required 31 days.<br />
August September October November December<br />
62 day treatment target<br />
As well as the expansion of the<br />
<strong>Cancer</strong> Waiting Times data set,<br />
there are now much stricter<br />
constraints with regards to<br />
patient pathways. As a result of<br />
this, there has been an increase<br />
in performance variability<br />
compared with 2008 (Figure<br />
1.6). The network achieved the<br />
new national standards for five<br />
months. Constant monitoring of<br />
the <strong>Cancer</strong> Waiting Times and<br />
patient pathways means that,<br />
The North West Staging<br />
Project<br />
The North West Staging Project<br />
has now come to an end.<br />
Achieving the aims of the project<br />
brief, all trusts in the <strong>Merseyside</strong><br />
and <strong>Cheshire</strong> <strong>Cancer</strong> <strong>Network</strong> are<br />
now submitting PAS, Pathology<br />
and MDT data to NWCIS.<br />
Seven trusts have successfully<br />
implemented our recommended<br />
solution comprising a<br />
comprehensive review of process<br />
and data collection methodology<br />
and a fully-supported<br />
deployment of the Somerset<br />
<strong>Cancer</strong> Register. A further six<br />
Trusts and a PCT are due to<br />
implement the Somerset <strong>Cancer</strong><br />
Register by Christmas <strong>2010</strong>.<br />
The median waiting time from urgent<br />
GP referral to first treatment in <strong>2009</strong><br />
was 44 days<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 11
<strong>Cancer</strong> peer review programme<br />
The National <strong>Cancer</strong> Peer Review Programme aims<br />
to improve care for people with cancer and their<br />
families by:<br />
• ensuring services are as safe as possible<br />
• improving the quality and effectiveness of care<br />
• improving the patient and carer experience<br />
• undertaking independent, fair reviews of<br />
services<br />
• providing development and learning for all<br />
involved<br />
• encouraging the dissemination of good practice<br />
<strong>Cancer</strong> networks have delegated responsibility<br />
from SHAs and PCTs to ensure that services are<br />
appropriately commissioned and have robust clinical<br />
governance processes. The process of cancer peer<br />
review is concerned not only with the review of an<br />
organisation’s compliance against measures, but<br />
also with the qualitative assessment of a broad<br />
set of objectives for the delivery of services. These<br />
objectives encompass the whole system of quality<br />
and safety in relation to patient care and patient<br />
and carer experience.<br />
<strong>2009</strong>/10 was the first year of implementing the<br />
new approach to cancer peer review with the<br />
introduction of annual self assessment, internal<br />
validation, external verification & target visits.<br />
Across the network a number of teams were<br />
reviewed including:<br />
• breast<br />
• lung<br />
• skin<br />
• urology<br />
• gynaecology<br />
• pancreas<br />
• oesophago-gastric<br />
Reviews have now concluded and while the process<br />
has identified discrete areas of non-compliance<br />
across the network, overall the results have been<br />
positive. In particular, the zonal team has applauded<br />
the robustness of local internal validation processes.<br />
Following the outcomes from the different stages<br />
in the peer review process, the cancer network and<br />
its constituent organisations<br />
have now agreed<br />
the actions that<br />
need to be taken<br />
within agreed<br />
timescales,<br />
building on<br />
the strengths<br />
identified<br />
and addressing<br />
any aspects in need of<br />
improvement.<br />
The schedule of self assessments and targeted visits<br />
for <strong>2010</strong>/11 has been issued and work is already<br />
underway to prepare for this next round.<br />
12 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Service improvement<br />
There are 24 clinical network groups (CNGs) across<br />
the cancer network; all are multi-disciplinary in<br />
nature. They reflect a focus of local expertise in<br />
specific cancer types (e.g. lung cancer or breast<br />
cancer) or a group of experts who work in crosscutting<br />
services which support care of people<br />
with cancer (such as chemotherapy, or allied<br />
health professionals). This is how we engage with<br />
clinicians across the patch - a key competency<br />
for PCTs to demonstrate in World Class<br />
Commissioning. Some of the CNGs’ highlights and<br />
achievements in <strong>2009</strong>/<strong>2010</strong> are detailed below.<br />
Service improvement<br />
The Allied Health Professionals CNG began<br />
preparatory work to agree criteria for the four<br />
level model, undertook a survey of current service<br />
provision, agreed cancer rehabilitation guidelines<br />
and started to develop a service specification,<br />
needs assessment, and training and education<br />
strategy. Work commenced on developing a<br />
rehabilitation section for each locality’s cancer<br />
services directory. This work will continue and be<br />
subject to peer review assessment in January 2011.<br />
The Breast CNG helped to prepare units for the<br />
two week wait for all breast referrals from January<br />
<strong>2010</strong>, with the exception of referrals for family<br />
history services and for reconstructive procedures.<br />
The Breast CNG acknowledged the excellent<br />
Professor Emiel Rutgers presents the “People’s Prize”, won by A Farooq, S<br />
Azmi and M Chandrashekar at the breast Tri-network event in Nov. <strong>2009</strong><br />
comments about local breast services from<br />
the <strong>2009</strong> patient survey. The group secured<br />
100% compliance against the CNG peer review<br />
measures and the panel noted the enthusiasm and<br />
commitment of regular group attendees.<br />
Via the Children and Young Peoples CNG, an<br />
MDT co-ordinator was appointed at Alder Hey to<br />
support the Paediatric Oncology MDT and ensure<br />
that robust arrangements are in place between the<br />
treatment centre and referring teams. The Teenage<br />
and Young Adult MDT is now well established and<br />
is led by Dr Nasim Ali, medical oncologist. During<br />
its first 12 months the MDT has discussed 95 cases,<br />
offering supportive care packages to patients in<br />
<strong>Merseyside</strong>, <strong>Cheshire</strong> and North Wales. A peer<br />
support group for young people aged 16 to 24<br />
years was established during the year to which all<br />
patients discussed at the MDT are invited to join.<br />
The Colorectal CNG continued to monitor and<br />
support laparoscopic colorectal surgery in line with<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 13
<strong>Network</strong> groups: Service improvement<br />
the national guidance; this method of surgery<br />
is now available in each trust in the network. A<br />
national baseline assessment was undertaken by<br />
each colorectal MDT and highlighted an increase<br />
in the proportion of patients having a laparoscopic<br />
resection in line with national trends. The group<br />
also embraced the enhanced recovery programme,<br />
which improves elective inpatient management by<br />
ensuring that patients are supported appropriately<br />
at each stage of treatment. Aintree University<br />
Hospital Trust was confirmed as an innovation site<br />
as part of the national programme.<br />
The End of Life and Palliative Care CNG has<br />
taken a coordinating role in progressing the<br />
implementation of the NHS North West End of Life<br />
Care Clinical Pathway Group recommendations,<br />
producing and regularly updating a performance<br />
report on the uptake of end of life care tools<br />
across the network.<br />
Dying Matters: “Lets talk about it” is a national<br />
campaign to raise public awareness on planning<br />
for end of life. There was a week of events across<br />
the country, locally led by the End of Life and<br />
Palliative Care CNG in March <strong>2010</strong> with colleagues<br />
at local level joining forces for a very successful<br />
event. The cancer information bus iVan (see page<br />
30) was dressed in different clothing for the week<br />
and travelled across the network manned by<br />
professionals and patient volunteers to deliver<br />
information around end of life issues.<br />
Professor Sir Mike Richards with MCCN’s Sandra Rowlands and Gloria<br />
Payne from the iVan team<br />
During <strong>2009</strong>/<strong>2010</strong> the Haematology CNG and<br />
Pathology CNG continued to work towards a<br />
solution to the outstanding IOG requirement for<br />
the Haematological Malignancy Diagnostic Service<br />
(HMDS).<br />
The Head and Neck CNG and network team started<br />
work with Professor Simon Rogers, consultant<br />
in maxillofacial surgery, to develop a DVD and<br />
supporting material to raise awareness of the signs<br />
and symptoms of mouth cancer. Jointly funded by<br />
the Mersey Deanery and cancer network, this will<br />
be positioned in dentists and GPs’ practices to be<br />
launched as part of Mouth <strong>Cancer</strong> Action Month.<br />
The Health Inequalities CNG saw good progress on<br />
most objectives; considerable external investment<br />
was secured for <strong>Merseyside</strong> and <strong>Cheshire</strong> and the<br />
Early Detection Strategy has been mainstreamed<br />
into the cancer network’s (and some PCTs’)<br />
business plans, resulting in good engagement of<br />
general practice and acute trusts. Relations with<br />
14 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Service improvement<br />
external partners such as <strong>Cancer</strong> Research UK and<br />
Clatterbridge <strong>Cancer</strong> Research have developed.<br />
Paul Mackenzie, health inequalities manager for<br />
the network, continues to be a member of the<br />
national awareness early detection and national<br />
equalities committees.<br />
The Health Inequalities CNG developed a quality<br />
performance framework/cancer dashboard,<br />
an information-based tool that enables PCT<br />
teams to self-assess their effectiveness on cancer<br />
inequalities. It has three parts: a baseline report<br />
from the cancer network, a self-assessment group<br />
exercise lasting a maximum of two hours and a<br />
round of action and review. Work commenced<br />
with Liverpool PCT to develop this process, to<br />
ensure robust evidence for inspections from<br />
the Care Quality Commission, World Class<br />
Commissioning panels etc.<br />
The Health Inequalities CNG continued to<br />
coordinate activity to improve screening uptake.<br />
The group identified good practice in report<br />
formats for GPs and modelling outcomes,<br />
collaborated work with the National Screening<br />
Committee to include sentenced prisoners in the<br />
bowel cancer screening programme, provided<br />
leadership for change in cervical cytology labs<br />
and developed a breast screening DVD aimed at<br />
women with learning disabilities.<br />
Several social marketing initiatives have been<br />
developed and implemented across MCCN via the<br />
Health Inequalities CNG, for example prostate<br />
cancer insights and awareness raising in two<br />
deprived wards in Wirral, three wards in an<br />
affluent area in <strong>Cheshire</strong> and the Afro-Caribbean<br />
centre. In April to July <strong>2010</strong> MCCN is rolling out the<br />
successful malignant melanoma initiative in each<br />
PCT. This project raises awareness of skin cancer for<br />
men over 50 years of age. Social marketing insights<br />
were developed for cancer of the breast, lung,<br />
bowel, bladder, cervix and skin.<br />
The Liverpool Heart and Chest Hospital established<br />
a transbronchial needle aspiration service for the<br />
network, working alongside the Lung CNG to do<br />
this.<br />
The Neuro-oncology CNG and Radiology CNG<br />
started work across partner trusts in <strong>Merseyside</strong><br />
and <strong>Cheshire</strong> to develop a network-wide approach<br />
to the management of metastatic spinal cord<br />
compression, to ensure delivery of NICE CG 75.<br />
The Pathology CNG oversaw a number of networkfunded<br />
trust-based projects which will enable them<br />
to implement new pathology reporting systems.<br />
This will subsequently improve data collection<br />
and assist with various local and national data<br />
requirements. Work continued on implementation<br />
of the cervical cytology sector arrangements; the<br />
laboratories made good progress towards the<br />
planned consolidation of services.<br />
During <strong>2009</strong>/<strong>2010</strong>, the Primary Care CNG refocused<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 15
<strong>Network</strong> groups: Service improvement<br />
its efforts on engaging with the primary care<br />
community across <strong>Merseyside</strong> and <strong>Cheshire</strong><br />
via a regular e-bulletin titled ‘<strong>Cancer</strong> Matters<br />
in Primary Care’. The bulletin and associated<br />
work have enabled engagement with a wider<br />
group of colleagues, including practice-based<br />
commissioners, PCT cancer leads and practices with<br />
an interest in cancer.<br />
The Sarcoma CNG received confirmation from the<br />
North West Specialist Commissioning Group that<br />
the CNG proposal to offer one of the North West<br />
treatment centres for soft tissue sarcoma at the<br />
Royal Liverpool University Hospital was accepted.<br />
The CNG supported the specialist MDT through a<br />
successful internal peer review.<br />
The Radiology CNG reviewed and further<br />
developed the standardised protocols for cancer<br />
imaging to be applied across the network. The use<br />
of the protocols maximises imaging capacity whilst<br />
promoting patient safety by minimising exposure<br />
to radiation. The CNG has resurrected the PET CT<br />
operational group with co-opted colleagues to<br />
plan for a static service beyond 2012 when the<br />
current national contract concludes. Plans include<br />
building reporting capability and capacity within<br />
radiology.<br />
The Radiology CNG has also been liaising closely<br />
with the <strong>Cheshire</strong> and <strong>Merseyside</strong> PACS managers<br />
group to resolve some of the issues around the<br />
transfer of images in a timely manner to support<br />
MDT discussion. A network audit has revealed that<br />
there are now no delays in patients being discussed<br />
at MDT and that the use of CDs to transfer images<br />
has ceased. The Cardiac and Stroke Clinical<br />
<strong>Network</strong> is looking to revise the imaging strategy<br />
for both disease groups; through collaboration<br />
between both networks the Radiology CNG has<br />
representation identified for this work.<br />
As the Skin CNG prepared for the first peer review<br />
assessments, a substantial amount of work went<br />
into the implementation of a number of clinical<br />
pathways and protocols. The Specialist Skin <strong>Cancer</strong><br />
MDT was formally established at Whiston Hospital<br />
and the Supranetwork MDT for cutaneous T-Cell<br />
lymphoma patients was formally established<br />
at the Royal Liverpool University Hospital. In<br />
addition, the network Mohs service (a microscopic<br />
surgical technique for the treatment of some skin<br />
cancers) became operational at Wirral University<br />
Hospital. The CNG produced and launched a<br />
comprehensive melanoma leaflet for local patients<br />
and also contributed to the development of a<br />
BBC documentary relating to sunbed use and skin<br />
cancer.<br />
The Supportive and Palliative Care CNG<br />
completed a full stocktake against the IOG in<br />
May <strong>2009</strong> and March <strong>2010</strong>. While there were<br />
many areas requiring progress earlier in the year,<br />
significant progress had been made by March.<br />
Notwithstanding, there remain areas of noncompliance,<br />
for example rehabilitation, psychology<br />
16 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Development of clinical<br />
practice, pathways and guidelines<br />
and 24/7 provision of specialist palliative care,<br />
which will require intensive performance<br />
management supported by the SHA.<br />
The Urology CNG was externally reviewed in<br />
January and achieved 100% compliance against<br />
the national measures. Reviewers acknowledged<br />
strong leadership, improvements in communication<br />
between the local and specialist MDTs and active<br />
patient involvement. The report identified a<br />
number of areas which will need to be reviewed.<br />
These include a review of the two centre service<br />
for penile cancer (supra-network MDT), South<br />
sector renal MDT arrangements and the need<br />
to ensure consistency in the provision of services<br />
across the network, for example oncology input<br />
and joint clinics for patients.<br />
Development of clinical<br />
practice, pathways and<br />
guidelines<br />
The Allied Health Professionals CNG participated in<br />
the development of national pathways, to develop<br />
an evidence base relating to the effectiveness of<br />
rehabilitation interventions relating to cancer<br />
in brain and central nervous system, breast,<br />
colorectal, gynaecology, head and neck, lung,<br />
upper GI and urology.<br />
The Chemotherapy CNG received the long-awaited<br />
final report from the National Chemotherapy<br />
Advisory Group (NCAG), “Chemotherapy services<br />
in England, ensuring quality and safety”. The<br />
group has started to effect fundamental changes<br />
in the way chemotherapy services operate as<br />
a consequence of the recommendations. The<br />
group has completed work on incident reporting<br />
and off protocol chemotherapy use and has<br />
planned with partners in the chemotherapy and<br />
pharmacy groups to deliver end of treatment<br />
records, standardised network protocols and<br />
multidisciplinary competencies for prescribing,<br />
checking, and administering chemotherapy.<br />
The Children and Young People’s CNG continued<br />
to develop guidelines and policies with a particular<br />
focus on clinical and communication arrangements<br />
between Alder Hey and the shared care units.<br />
Children’s cancer measures were published in<br />
<strong>2009</strong> and the group has been actively engaged<br />
in developing the evidence necessary at network,<br />
principal treatment centre and shared care level<br />
to ensure consistency across children’s cancer<br />
services. This work has included the development<br />
of a key worker policy for children, guidelines for<br />
psychosocial assessment and clinical management<br />
protocols.<br />
The Colorectal CNG reviewed pathways for early<br />
rectal and anal cancer to ensure that access<br />
is available to colorectal patients requiring<br />
specialist input. This work has included a review<br />
of support available to patients at every stage and<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 17
<strong>Network</strong> groups: Development of clinical<br />
practice, pathways and guidelines<br />
communication between local and specialist teams.<br />
The work has also contributed to the development<br />
of network-wide guidelines for governance and<br />
communication.<br />
Referral guidelines across the Colorectal CNG<br />
and Hepato-pancreato-biliary CNG were finalised<br />
during the year in light of the NICE guidance<br />
for Cetuximab for patients with colorectal liver<br />
metastases. Arrangements for the commissioning<br />
of specialist pathology (KRAS testing) to test<br />
patients’ eligibility for this treatment were also<br />
confirmed. Further work developed to cement the<br />
links between the associated CNGs, with Mr Hassan<br />
Malik, liver surgeon, now an active member of<br />
both groups.<br />
The Gynaecology CNG undertook a full review of<br />
all clinical protocols and pathways as preparation<br />
for the peer review assessments which commenced<br />
during <strong>2009</strong>.<br />
The Haematology CNG had a productive year, with<br />
a particular focus on confirming network clinical<br />
guidelines. Many colleagues actively contributed<br />
to this work and the resulting guidelines reflect<br />
this combined effort. The group also regularly<br />
reviewed access to trials with a view to improving<br />
uptake and started to develop the network’s<br />
website to hold up-to-date information about<br />
open clinical trials.<br />
The Head and Neck CNG reviewed a number<br />
Professor Emiel Rutgers presents the prize for best abstract to Dr Joanna<br />
Coote at the breast Tri-network event in November <strong>2009</strong><br />
of guidelines and pathways, including imaging<br />
guidelines for head & neck and thyroid cancer<br />
and management of neck lumps. Clinical support<br />
services were also being reviewed within localities<br />
to ensure that arrangements for aftercare and<br />
rehabilitation are in place.<br />
The Hepato-pancreato-biliary CNG wrote<br />
new guidelines during the course of the year.<br />
These include guidelines on liver adhesions<br />
and liver cysts. The network-wide guidance on<br />
communications and governance between local<br />
and specialist MDTs has been discussed in depth.<br />
The liver team has visited referring trusts once<br />
again this year to strengthen the links across the<br />
care pathway.<br />
In anticipation of the publication of IOG measures<br />
in <strong>2010</strong>, the Neuro-oncology CNG continued to<br />
work on the development of clinical pathways<br />
and guidelines, with particular focus on a patient<br />
referral pathway for patients with a newly<br />
18 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Development of clinical<br />
practice, pathways and guidelines<br />
diagnosed brain tumour and the rehabilitation<br />
pathways/roles of allied health professionals. The<br />
group also started to review cancer registry data<br />
and cancer waiting times data to inform the work<br />
of the group.<br />
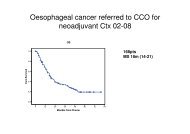
The Oesophago-gastric CNG wrote new guidelines<br />
for the management of dysplasia; several other<br />
guidelines and imaging protocols were updated<br />
to reflect new practices such as the use of PET-CT.<br />
In January <strong>2010</strong> the CNG underwent peer review.<br />
The visiting review team confirmed that the CNG<br />
had complied with 100% of the national measures<br />
and praised the input of the group’s patient<br />
representative, Sue Kernaghan, in particular. The<br />
peer review team noted that a small number of<br />
surgical procedures had been performed outside<br />
the designated centres. This matter was raised<br />
immediately with the trusts concerned and<br />
appropriate assurance was received. The reviewers<br />
also stated that a structured plan to decrease the<br />
number of surgeons performing oesophago-gastric<br />
cancer resections should be developed. This will<br />
form a major part of the CNG’s workplan during<br />
<strong>2010</strong>.<br />
A system of formally managing tertiary referrals to<br />
the Royal Liverpool Hospital laboratory (for MDT<br />
reporting/second opinions) was established via the<br />
Pathology CNG so that the financial and workload<br />
implications can be monitored. In anticipation of<br />
the NICE appraisal for Iressa for non small cell lung<br />
cancer patients, an estimated glomerular filtration<br />
rate (EGFR) testing service has been developed<br />
at the Royal Liverpool Hospital to enable better<br />
targeted prescribing of the drug.<br />
The Pharmacy CNG implemented the first networkwide<br />
online intervention monitoring tool.<br />
Results from the first four months of operation<br />
were presented at the network chemotherapy<br />
conference poster exhibition.<br />
Pharmacists routinely make interventions,<br />
correcting errors on chemotherapy prescriptions.<br />
Recording and collating these errors provides<br />
important safety related data and allows<br />
chemotherapy regimens which cause problems<br />
to be identified before an actual clinical incident<br />
occurs. For example, half of all the interventions<br />
reported concerned regimens containing<br />
fludarabine or rituximab and fludarabine. The<br />
interventions included wrong doses and the wrong<br />
interval between cycles and were judged to have<br />
prevented serious harm in all cases. Findings have<br />
been reported back through CNGs with the advice<br />
to refer to protocols and take extra care in the<br />
prescribing, dispensing and administering of these<br />
chemotherapy regimens.<br />
The Sarcoma CNG developed a policy for genetic<br />
testing in diagnostic sarcoma referrals, in<br />
collaboration with the <strong>Merseyside</strong> and <strong>Cheshire</strong><br />
regional genetics laboratories. Work also started to<br />
develop referral pathways and cross-MDT working<br />
across <strong>Merseyside</strong> & <strong>Cheshire</strong> and Lancashire &<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 19
<strong>Network</strong> groups: Excellence in clinical<br />
audit<br />
South Cumbria<br />
The Supportive and Palliative Care CNG developed<br />
network guidance for bereavement support during<br />
<strong>2009</strong>/11 - this was approved by the End Of Life<br />
and Palliative Care CNG in March <strong>2010</strong>. A directory<br />
of bereavement support services within each<br />
locality is underway and will be concluded in the<br />
forthcoming months.<br />
The Psychological Support Working Group<br />
continues to meet regularly and has made<br />
significant inroads in developing a network<br />
model for holistic needs assessment, which<br />
incorporates a psychological screening tool. A<br />
final draft of the guidance was circulated March<br />
<strong>2010</strong>. Work continues to develop a training<br />
programme to support the process. In addition,<br />
the group has continued to work on a network<br />
service specification for psychology. This work will<br />
continue into <strong>2010</strong>.<br />
During the year, the Urology CNG finalised clinical<br />
and referral guidelines for bladder, prostate,<br />
renal and testicular cancer and worked with the<br />
team at The Christie to develop the penile cancer<br />
guidelines. As part of its work programme, the<br />
CNG has started to review follow up practice<br />
and opportunities to explore different models<br />
of follow up. Dr Steve Connolly, GP, is working<br />
with the group to look at the interface between<br />
primary and secondary care supported by clinical<br />
guidelines.<br />
Excellence in clinical audit<br />
The Colorectal CNG reviewed emergency colorectal<br />
cancer activity in each trust as part of its audit<br />
programme. Further work is underway to audit<br />
stenting services as part of the CNG’s review of its<br />
policy for management of emergencies.<br />
The <strong>Merseyside</strong> and <strong>Cheshire</strong> Palliative care<br />
<strong>Network</strong> Audit Group has produced the fourth<br />
edition of standards and guidelines in palliative<br />
care.<br />
In November <strong>2009</strong> the Gynaecology CNG hosted<br />
a successful audit day with a number of clinical<br />
and educational presentations relating to local<br />
projects and areas of current interest. This included<br />
continuation of the local ovarian cancer audit,<br />
and an endometrial hyperplasia audit. In addition,<br />
the development of a local clinical database has<br />
enabled improved gynaecological data collection<br />
while trusts prepare for full implementation of the<br />
Somerset <strong>Cancer</strong> Register.<br />
The Head and Neck CNG audited head and neck<br />
patient pathways to identify any variation against<br />
the agreed clinical pathway and to address clinical<br />
and non-clinical delays. Head and neck patients<br />
often experience complex diagnostic pathways<br />
involving a number of different trusts and the<br />
audit highlighted a number of areas for action.<br />
Submissions to the national clinical dataset for<br />
20 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Excellence in clinical<br />
audit<br />
head and neck - DAHNO - have improved and all<br />
trusts were given a ‘green’ status. Data quality<br />
is now being addressed. Overall the network<br />
achieved 74% in staging, a notable increase on the<br />
last report.<br />
In addition, an audit of gastrostomy services was<br />
carried out in order to gather information on the<br />
availability of local services. The audit highlighted<br />
some gaps in service leading to increased travel<br />
for patients and the outcome of the audit is being<br />
discussed with appropriate localities.<br />
Survival data for the most common cancers at one<br />
and five years is now available by PCT or tumour<br />
type and has been shared in the cancer dashboard,<br />
led by the Health Inequalities CNG. In addition,<br />
survival modelling will soon be possible for bowel<br />
cancers identified through screening.<br />
Via the Health Inequalities CNG, the PCTs have<br />
collectively participated in the nationally validated<br />
<strong>Cancer</strong> Awareness Measure. This tool is being used<br />
across the network using appropriate sampling<br />
methods and is being led by the University of<br />
Liverpool and Clatterbridge Center for Oncology<br />
research team. The results will be available in late<br />
spring <strong>2010</strong>.<br />
The hepato-pancreato-biliary minimum data sets<br />
for primary liver cancer, metestatic liver cancer,<br />
pancreas cancer and neuroendocrine tumours have<br />
been revised so that the majority of data items are<br />
The cancer dashboard enables PCT teams to self-assess their effectiveness<br />
on cancer inequalities<br />
now common across the tumour types. It is hoped<br />
that this will ensure that better, more consistent<br />
and relevant data are collected in the future.<br />
With this in mind, the Hepatobiliary (HPB) CNG<br />
has decided to hold an annual HPB audit day. In<br />
January <strong>2010</strong>, the CNG was visited by a peer review<br />
team. The visiting team concluded that the CNG<br />
was 100% compliant with the national measures<br />
and singled out the approach taken by Wirral<br />
Hospitals to track HPB patients for praise.<br />
The Lung CNG hosted a wide-ranging audit and<br />
education event in December <strong>2009</strong>, which allowed<br />
a number of colleagues to discuss statistical and<br />
epidemiological data as well as developments in<br />
lung cancer care across <strong>Merseyside</strong> and <strong>Cheshire</strong>. A<br />
comprehensive report was presented to the group<br />
detailing performance against an agreed clinical<br />
performance indicator (CPI) programme as well<br />
as the LUCADA dataset. A system for collecting<br />
data relating to mesothelioma diagnoses was<br />
implemented to enable a thorough assessment of<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 21
<strong>Network</strong> groups: Education, training and<br />
workforce development<br />
the workload and treatment pathways.<br />
All trusts contributed data to the national<br />
oesophago-gastric cancer audit. The<br />
recommendations from the audit have been<br />
discussed at length and have been incorporated<br />
into the Oesophago-gastric CNG’s workplan. In<br />
July <strong>2009</strong>, the CNG held a very successful audit day.<br />
Twenty five members of the CNG were joined by<br />
a further 20 colleagues from their MDTs to hear<br />
audits of patient outcomes and presentations<br />
on innovative techniques including HALO<br />
radiofrequency ablation.<br />
The Primary Care CNG led some local work on the<br />
national audit of cancer diagnosis in primary care;<br />
33 practices from seven PCTs submitted full returns<br />
for this project and analysis was undertaken on the<br />
main findings. This work generated a significant<br />
level of interest and engagement from primary<br />
care and the CNG is considering how to maintain<br />
momentum and interest. Professor Greg Rubin,<br />
national lead for this work, visited the network<br />
in February and led a workshop with over 20<br />
participants to discuss the audit of cancer diagnosis<br />
in primary care and learning from the rest of the<br />
country.<br />
Skin Electron Beam radiotherapy service (TSEB).<br />
The Urology CNG Audit Event was held on<br />
23rd September and was well attended by CNG<br />
members and wider members of local MDTs.<br />
Presentations included peer review, organ based<br />
tumour data and clinical trials. The main focus<br />
of the meeting related to communication and<br />
referral arrangements between local and specialist<br />
MDTs and the information provided to patients at<br />
different stages of their care. As a result, the CNG<br />
made a significant contribution to the network<br />
guidelines for governance and communication<br />
between local and specialist MDTs.<br />
Education, training and<br />
workforce development<br />
The Allied Health Professionals CNG undertook<br />
a further local review to quantify rehabilitation<br />
workforce provision for cancer and palliative care<br />
patients. This has been a valuable exercise as the<br />
data will support the development of a network<br />
specification for cancer rehabilitation. The group<br />
collaborated with the lead nurses group to focus<br />
on survivorship.<br />
The Skin CNG oversaw data collection against<br />
agreed clinical performance indicators; this<br />
culminated in an annual report, supporting local<br />
MDT performance evidence for peer review. A<br />
successful education event was held in May <strong>2009</strong><br />
covering a number of topics including the Total<br />
The Breast CNG organised the annual tri-network<br />
breast conference in partnership with the<br />
North West Breast Screening Quality Assurance<br />
Reference Centre, for the <strong>Merseyside</strong> and<br />
<strong>Cheshire</strong>, Lancashire and South Cumbria and<br />
Greater Manchester cancer networks. The event<br />
22 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
<strong>Network</strong> groups: Education, training and<br />
workforce development<br />
attracted international speakers and over 150<br />
local delegates. The clinical debate was lively,<br />
local research projects were presented and the<br />
evaluation of the learning from the event was<br />
extremely positive.<br />
The Chemotherapy Nurse CNG planned,<br />
organised and hosted the third annual network<br />
Chemotherapy Conference, covering a broad<br />
agenda with topics ranging from acute oncology,<br />
survivorship and NCAG (National Chemotherapy<br />
Advisory Group) to cytogenetics, lung and<br />
haematological clinical updates for the more<br />
clinically minded in the audience.<br />
The Education <strong>Network</strong> Group oversaw the<br />
sixth <strong>Network</strong> Development Programme (NDP),<br />
to enable individuals to be better equipped<br />
to develop their personal leadership and<br />
networking skills in relation to their cancer<br />
role. This has now concluded and the seventh<br />
programme commenced in March <strong>2010</strong>. Work<br />
also continued on the e-learning programme and<br />
all three packages (intravenous access care and<br />
maintenance, chemotherapy and spiritual care)<br />
are now near completion. The final draft of the<br />
<strong>Network</strong> Education Strategy was circulated in<br />
March <strong>2010</strong> for consultation. Feedback has been<br />
positive; the strategy recognises the key role of<br />
training and education in the development of a<br />
competent cancer workforce.<br />
annual conference with the National Council<br />
for Palliative Care, which was well attended and<br />
successfully evaluated. The next event is scheduled<br />
for July <strong>2010</strong>.<br />
The Supportive and Palliative Care CNG continued<br />
to roll out the Advanced Communication Skills<br />
Training (ACST) programme for senior healthcare<br />
professionals. A total of 18 ACST courses were<br />
held in <strong>2009</strong>, including three end of life courses.<br />
So far in <strong>2010</strong>, five courses have been held with<br />
another three dates confirmed and further dates<br />
to be confirmed for the rest of the year. To date a<br />
total of 187 MDT core professionals have attended<br />
for training; a total of 67 have applied but are<br />
still awaiting a date. In addition there will be<br />
additional core professionals who need to attend<br />
training but have not yet applied. Three of our<br />
trainees were successfully accredited this year:<br />
Margaret Kendal, Debbie Wyatt and Jan Vickers.<br />
The group also held a very well attended<br />
conference in June <strong>2009</strong> titled “Psychological<br />
Problems: Psychological solutions across the<br />
lifespan”.<br />
The End of Life and Palliative Care CNG held its<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 23
Medical director’s report<br />
Medical director: Ged Corcoran<br />
Having held this position for almost ten years,<br />
welcome to my first ever annual report.<br />
During the last year I was able to increase my<br />
sessions to the network in order to lead on several<br />
important strategies:<br />
• Non-surgical oncology<br />
• PET-CT<br />
• Cervical cytology reconfiguration<br />
• Links with the university<br />
• Clinical governance<br />
• Clinical engagement<br />
• Peer review<br />
We have made great progress in all of these areas<br />
and are likely to be among the first networks<br />
to have acute oncology teams in place. By early<br />
summer <strong>2010</strong> we will have five out of the seven<br />
teams in place, having successfully recruited five<br />
additional medical oncologists.<br />
With colleagues and the Lung and Radiology<br />
CNG chairs, we have been working to improve<br />
the current PET-CT access and are developing a<br />
strategy for the future. Similarly we are working<br />
closely with the University of Liverpool to develop<br />
academic radiology. With the acquisition of a<br />
Research PET-CT scanner at the Royal, the prospect<br />
for both these strategies has been significantly<br />
enhanced.<br />
ensure that good<br />
clinical governance is<br />
in place across patient<br />
pathways developing in<br />
the CNGs. I am pleased<br />
to say that there have<br />
been no significant<br />
or serious untoward<br />
incidents during the<br />
year.<br />
Another major focus in my role is maintaining the<br />
momentum for clinicians to engage with us and<br />
with each other through our many and varied<br />
CNGs. Supporting CNG chairs, including chairing<br />
one CNG (Oesophago-Gastric), has occupied a<br />
good deal of my time. I know how difficult it<br />
is to juggle clinical demands with non-clinical<br />
commitments and am grateful to all of those who<br />
give generously and freely of their time to ensure<br />
that we have strong engagement at network level.<br />
This was formally recognised in the recent peer<br />
review round.<br />
I look forward to working with you over the next<br />
year to further strengthen and develop services for<br />
all our patients.<br />
As Medical Director, it is my responsibility to<br />
24 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Nurse director’s report<br />
Nurse director: Anita Corrigan<br />
Having taken up post in March <strong>2009</strong>, welcome to my<br />
first annual report. This has been a busy 12 months,<br />
both in terms of reviewing the nursing contribution<br />
to cancer care and in progressing the supportive care<br />
agenda. I have led on several important work areas,<br />
including:<br />
• Nursing Strategy finalised<br />
• <strong>Network</strong> Key Worker Guideline finalised<br />
• <strong>Network</strong> Bereavement Support Guideline finalised<br />
• <strong>Network</strong> Holistic Needs Assessment Guideline<br />
developed<br />
• Secured Macmillan funding for an <strong>Network</strong> AHP<br />
Lead<br />
• <strong>Network</strong> service specifications for psychology and<br />
rehabilitation commenced<br />
• E-learning developments<br />
The network nursing strategy - ‘The pursuit of<br />
excellence in cancer nursing <strong>2009</strong>-2012’ - was<br />
approved by Taskforce in October <strong>2009</strong>. This latest<br />
strategy aims to set out a vision for cancer nursing to<br />
respond to the new challenges set out in Modernising<br />
Nursing Careers (2006), the <strong>Cancer</strong> Reform Strategy<br />
(2007), the NHS Next Stage Review (2008) and the<br />
End of Life Care Strategy (2008) which clearly focus<br />
on improving the quality of care across the whole<br />
NHS. Our strategy responds to this challenge, putting<br />
patients at the heart of our business and our services,<br />
with the central aim of improving the patient<br />
experience and outcome.<br />
The latest network patient experience survey was<br />
rolled out in July <strong>2009</strong>. This was coordinated by lead<br />
nurses within each organisation. <strong>2010</strong> will focus on<br />
implementation of remedial action plans.<br />
A joint-led nurse and AHP meeting was held in<br />
November <strong>2009</strong> – this was the first joint open meeting<br />
of lead nurses and allied health professionals; the<br />
focus of the meeting was ‘survivorship’. The meeting<br />
was supported by a number of patient and carer<br />
representatives, whose contribution to the group<br />
work was greatly appreciated.<br />
The network key worker guideline was approved in<br />
October <strong>2009</strong>. The guideline specifies the standard<br />
of care coordination that should be achieved by any<br />
organisation involved in delivering cancer services and<br />
the role of the ‘key worker’. It applies to the delivery<br />
of both supportive and palliative care, covering the<br />
needs of patients who are expected to be discharged<br />
from treatment and those requiring end of life care.<br />
I have also participated in two national work streams:<br />
modernising cancer nursing careers and nurse sensitive<br />
outcomes in ambulatory chemotherapy. These will<br />
continue to inform the work of the group over the<br />
forthcoming year.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 25
Research<br />
Research network<br />
The aim of the <strong>Merseyside</strong> and <strong>Cheshire</strong> <strong>Cancer</strong><br />
Research <strong>Network</strong> (MCCRN) is to provide the<br />
cancer network with an infrastructure to support<br />
randomised prospective trials of cancer treatment.<br />
These include surgery, radiotherapy, chemotherapy,<br />
palliative care, newer treatment modalities and<br />
other well-designed studies that form part of<br />
the National Institute for Health Research (NIHR)<br />
portfolio.<br />
The purpose of the MCCRN is to benefit patients<br />
by improving the integration, quality and speed<br />
of cancer research. The MCCRN has developed<br />
a broad portfolio of approximately 130 studies,<br />
including 10 NIHR adopted commercial studies.<br />
The team is working hard to ensure that each<br />
trust’s portfolio is robust, suitable for the needs<br />
of the local population and integrated into the<br />
delivery of cancer services. This means working<br />
to our own strengths and investing the necessary<br />
time and resources to develop research in more<br />
challenging cancer areas, as well as maximising<br />
patient choice<br />
Despite a number of workforce challenges<br />
encountered by the network in <strong>2009</strong>/10,<br />
recruitment to RCTs has been excellent enabling<br />
us to achieve the 7.5% RCT target. In <strong>2009</strong>/10 the<br />
MCCRN appointed a new clinical lead for research:<br />
Dr Ernie Marshall, Macmillan consultant in medical<br />
oncology takes up his new role on 1st June <strong>2010</strong>.<br />
During <strong>2010</strong>/11 the MCCRN key priorities are:<br />
• Performance management of the team and<br />
their respective portfolios to ensure we meet<br />
our recruitment targets and provide patients<br />
with access to a comprehensive portfolio of<br />
studies<br />
26 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Research (continued)<br />
• Identifying new and more cost effective<br />
ways of working in response to the economic<br />
downturn and associated financial challenges<br />
• Continually evaluating skill mix to maximise<br />
the use of resource<br />
• To work with our Clinical <strong>Network</strong> Groups and<br />
Multidisciplinary Teams to overcome obstacles<br />
to recruitment into studies and critically<br />
examine areas where there are poor levels of<br />
recruitment<br />
• Continue to provide high quality education<br />
and training through regional groups<br />
Research group<br />
There are currently three research work streams<br />
addressing diverse topics related to cancer<br />
experience and awareness:<br />
1) A study to explore the impact of<br />
prostate cancer on the daily lives of men.<br />
This study will explore men’s experiences<br />
before and following treatment for prostate<br />
cancer.<br />
2) A study to explore how language<br />
impacts on people affected by cancer in<br />
the period following treatment<br />
The aims of the Research Group are:<br />
• To achieve the objectives set within the <strong>Cancer</strong><br />
Nursing Strategy 2008-2012<br />
• To promote a multi-disciplinary team approach<br />
to the development and dissemination of<br />
research findings<br />
• To develop and sustain partnerships with<br />
academic staff, lay partners and professional<br />
bodies<br />
• To develop and undertake research as defined<br />
through the priorities and needs of patients,<br />
carers, professionals and the broader NHS<br />
• To apply for external funding for research<br />
proposals<br />
This study will explore how the language<br />
that health professionals and members of the<br />
public use to talk to people affected by cancer<br />
influences their well-being in the difficult<br />
period following the completion of a course of<br />
cancer treatment.<br />
3) The <strong>Cancer</strong> Awareness Study<br />
As part of the MCCN strategy (2008-<strong>2010</strong>) for<br />
reducing health inequalities through the early<br />
detection and prevention of cancer, a study is<br />
currently underway which has been designed<br />
to identify the levels of awareness about<br />
cancer in the seven PCTs within the network.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 27
Patient and public involvement<br />
The <strong>Cancer</strong> <strong>Network</strong> Partnership<br />
Group (CNPG) continues to work<br />
on the priorities set in their 2008-<br />
2012 strategy:<br />
• Raising awareness<br />
• Information<br />
• <strong>Network</strong> research<br />
• Getting involved<br />
• Support and survivorship<br />
Raising awareness<br />
Group members have been<br />
involved in raising awareness<br />
of cancer in the community by<br />
working on iVan, the network’s<br />
mobile vehicle.<br />
Doris MacGlashan and Kate<br />
Jones - both members of locality<br />
partnership groups - have<br />
qualified as volunteers on iVan,<br />
while other members have helped<br />
in an ad hoc way such as raising<br />
awareness of prostate cancer with<br />
the help of the Wirral Prostate<br />
<strong>Cancer</strong> Support Group.<br />
Gloria Payne, patient and public<br />
involvement lead has also been<br />
raising awareness of men’s<br />
cancers in Risley Prison and Thorn<br />
Cross Youth Offenders Institute,<br />
Warrington as well as joining the<br />
Army for a day to raise awareness<br />
at the Dale Barracks, Chester.<br />
Information<br />
Good information is very<br />
important for people affected<br />
by cancer and group members<br />
have been involved in helping<br />
professionals to devise leaflets<br />
and booklets for cancer patients.<br />
Gloria Payne and Ray Murphy,<br />
chair of the CNPG, have attended<br />
conferences and workshops<br />
discussing patient information<br />
pathways and prescriptions at<br />
national and regional levels.<br />
The network’s website continues<br />
to develop with input and<br />
comment from group members.<br />
Yvonne Potter is the patient<br />
representative on the information<br />
steering group and inputs at<br />
network level.<br />
St Helens and Knowsley Hospitals<br />
Trust opened an information<br />
centre; the centre’s manager has<br />
also joined the partnership locality<br />
group.<br />
<strong>Network</strong> research<br />
A patient experience survey was<br />
undertaken in July <strong>2009</strong>, involving<br />
data from nine of the network’s<br />
hospital trusts. Over 800 surveys<br />
were returned overall; a report<br />
on the findings was compiled by<br />
Gloria Payne and Ian Connolly,<br />
the network’s performance<br />
28 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
Patient and public involvement (continued)<br />
improvement manager. This<br />
report can be found on the<br />
network website at www.mccn.<br />
nhs.uk.<br />
The <strong>Network</strong> Research Group’s<br />
developments can be found in the<br />
‘Research’ section of this report.<br />
Getting involved<br />
Gloria Payne has been visiting<br />
local cancer support groups to<br />
encourage their members to get<br />
involved with the work of the<br />
CNPG, resulting in many new<br />
people attending events and<br />
workshops and the recruitment<br />
of a patient representative to the<br />
Haematology Clinical <strong>Network</strong><br />
Group.<br />
In September <strong>2009</strong> the North West<br />
cancer networks held their annual<br />
patient partnership conference in<br />
Wigan, which was well attended<br />
by all three networks. The keynote<br />
speaker was Joanne Rule, national<br />
lead for user involvement in<br />
commissioning. The event was<br />
chaired by Derek Stewart.<br />
by Macmillan <strong>Cancer</strong> Support was<br />
held in February <strong>2010</strong>. A report on<br />
the findings of this can be found<br />
on the MCCN website at www.<br />
mccn.nhs.uk.<br />
Support and survivorship<br />
The fifth course of ‘Living Life<br />
after Treatment’ (LLaFT) sessions<br />
started in April <strong>2010</strong>. The course<br />
is for cancer patients who have<br />
finished their treatment at the<br />
Countess of Chester hospital. The<br />
course covers a variety of topics<br />
such as diet, exercise, information<br />
and support, physiotherapy and<br />
anxiety.<br />
Sue Kernaghan, the patient<br />
representative on the network’s<br />
psychological working group,<br />
became a radio personality when<br />
she appeared on BBC Woman’s<br />
Hour with Cieran Devane, chief<br />
executive of Macmillan <strong>Cancer</strong><br />
Support, where they discussed<br />
cancer survivorship.<br />
National <strong>Cancer</strong> Partnership<br />
Forum (NCPF)<br />
representative from Sussex and<br />
chair of the forum for a number<br />
of years, tendered his resignation<br />
at the March event and named<br />
Ray Murphy as his successor. This<br />
now means that Ray will chair the<br />
forum for the next couple of years<br />
and join Gloria Payne as a member<br />
of the NCPF planning group.<br />
<strong>Cancer</strong> <strong>Network</strong> Partnership<br />
Group<br />
A more detailed report of the<br />
activities of the CNPG can be<br />
found in the <strong>Cancer</strong> <strong>Network</strong><br />
Partnership Group annual report,<br />
which can be found at www.mccn.<br />
nhs.uk. The network would like<br />
to thank Barbara Burkey, who<br />
is standing down from her role<br />
as chair of the Liverpool, North<br />
<strong>Cheshire</strong> and Wirral Locality<br />
Group, for her outstanding<br />
contribution to patient<br />
involvement. We are pleased<br />
that she is able to continue as the<br />
representative for palliative care<br />
and end of life activities.<br />
A ‘Rarer <strong>Cancer</strong>s’ event funded<br />
Mike Vincent, a patient<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 29
iVan<br />
Following successful visits with the Macmillan cancer<br />
information and support vehicle in the network, a<br />
proposal was put together to have a similar vehicle<br />
with a greater focus on awareness raising and early<br />
detection. This led to successful bids to the National<br />
<strong>Cancer</strong> Action Team and the cancer network for a<br />
mobile cancer awareness vehicle. We took delivery of<br />
the vehicle in June <strong>2009</strong>.<br />
The vehicle was intended to support a particular<br />
emphasis on skin cancer awareness and sun safety,<br />
due to the rising skin cancer incidence rates within<br />
England. The vehicle is informally know as iVan,<br />
which stands for information van.<br />
iVan’s objectives are detailed below:<br />
Awareness<br />
• Utilise a cancer risk assessment tool to increase<br />
cancer symptom awareness and initiate referral to<br />
appropriate service if required/ desired.<br />
• Be responsive to local and national health<br />
initiatives and campaigns.<br />
• Raise skin cancer awareness and highlight the<br />
dangers of sun bed use.<br />
• Promote cancer screening and self awareness<br />
programmes.<br />
• Highlight cancer risk factors such as excessive<br />
UV exposure, smoking, obesity, frequent alcohol<br />
consumption and genetic predisposition.<br />
• Use network and national data intelligence.<br />
Engaging communities<br />
• Encourage people to take an active role in the<br />
maintenance of their health at a preventative<br />
stage.<br />
• Promote self awareness checks, such as regularly<br />
checking skin for significant changes.<br />
• Provide specific information and support to<br />
targeted populations.<br />
• Enable, facilitate and signpost to appropriate<br />
services.<br />
• Assess the feasibility and justification for the<br />
development of a mobile rapid assessment skin<br />
cancer clinic.<br />
Since going on the road, iVan has had contact<br />
with over 14,200 people in 6 months (July <strong>2009</strong> –<br />
30 - MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong>
iVan (continued)<br />
December <strong>2009</strong>) with 190 clients being referred to a<br />
GP because of concerns about symptoms.<br />
Total figures from July <strong>2009</strong> to end of December <strong>2009</strong><br />
Level of No. of Description<br />
intervention contacts<br />
0 11,160 Leaflet taker, no<br />
intervention<br />
1 2,173 Brief intervention<br />
e.g. brief advice/<br />
intervention<br />
2 433 More in depth,<br />
specific targeted<br />
information<br />
3 245 Psychological<br />
support, signposting<br />
4 190 In depth support<br />
or referral with<br />
significant symptoms<br />
Total 14,201<br />
Follow up of the most complex cases has revealed<br />
that GPs have fast tracked 16 clients under the urgent<br />
suspected cancer route. Eight cancers have been<br />
diagnosed, nine pre cancerous conditions have been<br />
discovered and there were 43 referrals to services for<br />
reasons other than cancer.<br />
Pre cancerous diagnosis<br />
(n)<br />
Actinic Keratosis 5<br />
Bowen’s disease 2<br />
Bowel polyp 1<br />
Cervix CIN 3 loop dissection 1<br />
Total 9<br />
For those clients referred to a GP from iVan staff,<br />
nearly 1 in 2 (42%) have resulted in a positive<br />
intervention, either by treatment by their GP or by<br />
referral to secondary care.<br />
Working collaboratively with others<br />
The iVan team has worked collaboratively with many<br />
organisations and individuals in order to highlight<br />
the early detection and prevention of cancer. We<br />
have actively engaged with the Healthy Communities<br />
Collaborative projects in Liverpool and Halton & St<br />
Helens. We have also engaged with groups such<br />
as the <strong>Merseyside</strong> Deaf Society, local colleges and<br />
schools and Liverpool’s Chinese community. We have<br />
also been working with the Wirral Prostate <strong>Cancer</strong><br />
Support Group.<br />
Future plans and targets<br />
Number of cancers diagnosed<br />
Malignancy diagnosis<br />
(n)<br />
Basal cell carcinoma 5<br />
Squamous cell carcinoma wide excision 1<br />
Malignant Melanoma wide excision 2<br />
Total 8<br />
The iVan project will continue to focus on raising<br />
awareness of cancer prevention and early detection<br />
of all cancers, with a particular focus on skin cancer<br />
during the summer months. We will continue to work<br />
collaboratively and engage with as many different<br />
groups as possible.<br />
MCCN <strong>Annual</strong> <strong>Report</strong> <strong>2009</strong>/<strong>2010</strong> - 31
<strong>Merseyside</strong> & <strong>Cheshire</strong> <strong>Cancer</strong> <strong>Network</strong><br />
Suite 4<br />
Woodcourt<br />
Riverside Park<br />
Southwood Road<br />
Bromborough<br />
Wirral<br />
CH62 3QX<br />
Tel: 0151 201 4150 ext. 6200<br />
Fax: 0151 201 4151<br />
Web: www.mccn.nhs.uk