Evidence-based Medicine: Time for a change? - Journal of Medical ...
Evidence-based Medicine: Time for a change? - Journal of Medical ...
Evidence-based Medicine: Time for a change? - Journal of Medical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ORIGINAL ARTICLE<br />
Acute kidney injury in HIV-positive patients<br />
1<br />
Devi PS, 2 Singh Lk S, 2 Dhanaraj Ch, 3 Shreeniwas S, 4 Singh S<br />
Abstract<br />
Objective : To study the incidence, spectrum,<br />
prognosis and outcome <strong>of</strong> clinical renal<br />
disease with special emphasis on acute<br />
kidney injury in patients with HIV infection.<br />
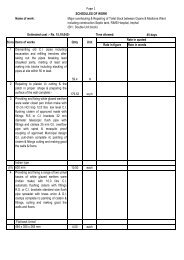
Methods: A protocol <strong>of</strong> study was prepared.<br />
All HIV patients <strong>of</strong> both genders regardless <strong>of</strong><br />
age attending Antiretroviral treatment (ART)<br />
Centre and those admitted in the wards <strong>of</strong> the<br />
hospital (Sir Sunderlal Hospital, Varanasi, Uttar<br />
Pradesh, India) were subjected <strong>for</strong> screening<br />
<strong>of</strong> clinical renal disease. HIV-seropositive<br />
patients with clinical renal diseases were<br />
included and divided into two groups: (A)<br />
Asymptomatic patients without manifestations<br />
<strong>of</strong> renal diseases but found to have a<br />
significant renal involvement on screening<br />
and (B) Patients with symptomatic renal<br />
diseases. HIV-associated renal disease were<br />
diagnosed using the following criteria: 1)<br />
Positive HIV Serology, 2) CD4 T-Lymphocyte<br />
count, 3) Proteinuria / Haematuria, 4) Elevated<br />
serum creatinine and 5)Quantitative<br />
proteinuria (24 hours urinary protein or spot<br />
urine Protein/creatinine ratio). National AIDS<br />
Control Organisation (NACO) Guidelines <strong>of</strong><br />
India, 2007 were followed <strong>for</strong> the diagnosis <strong>of</strong><br />
1<br />
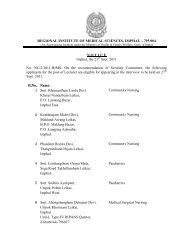
Assistant Pr<strong>of</strong>essor 2 Associate pr<strong>of</strong>essor, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal; 3 Consultant<br />
Nephrologist, ARTEMIS Hospital, Gurgaon; 4 Lecturer,<br />
Department <strong>of</strong> Nephrology, Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Banaras Hindu University, Varanasi (India).<br />
Address <strong>for</strong> Correspondence:<br />
Dr Loukrakpam Sharatchandra Singh, Associate<br />
Pr<strong>of</strong>essor (<strong>Medicine</strong>), Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal – 795004 (India).<br />
e-mail: lkbhu@sify.com<br />
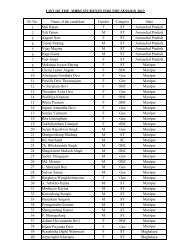
HIV-seropositivity. Results: 47 HIVseropositive<br />
patients were found to have<br />
clinical renal disease during the study period<br />
<strong>of</strong> August 2007 and July 2009. During the two<br />
years study period, there were 3545 patients<br />
<strong>of</strong> HIV-seropositive patients and only 1725<br />
patients (611 females and 1114 males) were<br />
enrolled <strong>for</strong> ART as they fulfilled NACO<br />
guidelines. 47 (1.33%) patients (44 males and<br />
3 females) were found to have clinical renal<br />
disease. Most <strong>of</strong> the patients (45/47) had AKI<br />
(pre-renal-15, acute tubular necrosis-27,<br />
interstitial nephritis-3). Proteinuria, serum<br />
creatinine and serum albumin were 0.935±<br />
0.985 gm/day, 5.28± 5.64 mg% and 2.92± 0.58<br />
respectively. Renal biopsy were done on 2<br />
indicated patients who showed<br />
granulomatous glomerulonephritis, and<br />
Tubulointerstitial nephritis in one patient each.<br />
CD4 count was in the range <strong>of</strong> 43-<br />
842(170.36± 157.75) cells/µL. 9 patients<br />
(1.7%) having HIV-related clinical renal disease<br />
died due to sepsis (5), tubercular meningitis<br />
(3) and hypovolemia (2). Peritoneal dialysis<br />
could be done in 6 patients. Conclusion: AKI<br />
mostly related to acute tubular necrosis was<br />
the most common HIV-related clinical renal<br />
disease. <strong>Evidence</strong> <strong>of</strong> non-specific glomerular<br />
disease with or without interstitial nephritis<br />
was observed in 2 patients. HIV-associated<br />
nephropathy well documented in western /<br />
African-American literatures was not observed<br />
in our study<br />
Key words: HIV Infection, Acute Kidney injury,<br />
Mortality, CD4.<br />
8 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011