Evidence-based Medicine: Time for a change? - Journal of Medical ...
Evidence-based Medicine: Time for a change? - Journal of Medical ...
Evidence-based Medicine: Time for a change? - Journal of Medical ...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
EDITORIAL<br />
<strong>Evidence</strong>-<strong>based</strong> <strong>Medicine</strong>: <strong>Time</strong> <strong>for</strong> a <strong>change</strong>?<br />
1<br />
Sudheeranjan Thingbaijam, 2 A Devadutta Sharma<br />
The <strong>Evidence</strong>-<strong>based</strong> <strong>Medicine</strong> (EBM)<br />
movement emerged due to research-practice<br />
gap, poor quality <strong>of</strong> much research,<br />
in<strong>for</strong>mation overload and clinical medicine<br />
which is not evidence-<strong>based</strong>, in the context<br />
<strong>of</strong> post-modern “risk society”, “managerialism”<br />
and “audit society” 1 . This movement<br />
also coincided with the rise <strong>of</strong> pr<strong>of</strong>essionalism,<br />
empowerment and consumerism and has<br />
been aided by the in<strong>for</strong>mation technology<br />
movement. Sackett and colleagues 2 describe<br />
EBM as the “conscientious, explicit, and<br />
judicious use <strong>of</strong> current best evidence in<br />
making decisions about the care <strong>of</strong> individual<br />
patients,…..integrating individual clinical<br />
expertise with the best available external<br />
clinical evidence from systematic research”.<br />
The traditional EBM tools are randomized<br />
controlled trial and systematic review,<br />
championed by the Cochrane Collaborations.<br />
While some critics define EBM as one which<br />
is purely guided by evidence from clinical<br />
research and some even brand it as “cookbook<br />
medicine” 3 , most subscribe to the<br />
definition <strong>of</strong> ‘the use <strong>of</strong> best external research<br />
evidence in the context <strong>of</strong> clinical experience,<br />
clinical situation, and patient values and<br />
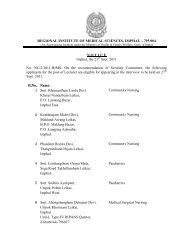
1. Associate Pr<strong>of</strong>essor <strong>of</strong> ENT,2. Associate<br />
Pr<strong>of</strong>essor <strong>of</strong> GI Surgery, Regional Institute <strong>of</strong><br />
<strong>Medical</strong> Sciences, Imphal<br />
Address <strong>for</strong> Correspondence:<br />
Dr A Devadutta Sharma, Associate Pr<strong>of</strong>essor <strong>of</strong> GI<br />
Surgery, Department <strong>of</strong> Surgery, Regional Institute<br />
<strong>of</strong> <strong>Medical</strong> Sciences, Imphal<br />
e-mail: aribam.sharma@jipmer.net<br />
preferences <strong>for</strong> making clinical decisions’ 4 .<br />
Though the EBM movement has gained<br />
tremendous momentum in the last two<br />
decades, the gold-standard status <strong>of</strong> RCT,<br />
meta-analysis and systematic review remains<br />
less than certain. <strong>Evidence</strong> synthesis, a term<br />
expounded by Pr<strong>of</strong> Thanos and Pr<strong>of</strong> Ara<br />
Darzi 5 , applies to a group <strong>of</strong> assessment<br />
techniques that integrate the data from<br />
variable evidence sources, and is applicable<br />
to both clinicians and policy-makers. The<br />
ultimate maturation <strong>of</strong> EBM would be when<br />
genomics, proteomics and in<strong>for</strong>matics lead<br />
us to “personalized medicine”.<br />
The prerequisites <strong>for</strong> a viable evidence-<strong>based</strong><br />
practice (EBP) include clinicians educated<br />
and skilled in the fundamentals <strong>of</strong> EBM and<br />
ready to <strong>change</strong>; the system or organization<br />
whose board-level members and leadership<br />
are committed and geared toward rendering<br />
the best evidenced health care; a workable IT<br />
infrastructure; an in<strong>for</strong>med and involving public<br />
and a sound EBM education module at hand.<br />
The decision making process <strong>of</strong> EBM<br />
essentially comprises <strong>of</strong> 1) designing an<br />
answerable clinical question directly relevant<br />
to one’s patient 2) searching the literature(<br />
including and mainly electronic) skill-fully <strong>for</strong><br />
the right evidence from the right sources 3)<br />
critically analysing the identified evidence 4)<br />
examining if the evidence is closely similar to<br />
one’s patient or should be ignored and make<br />
the final presumptive decision 5) to evaluate<br />
the patient outcome and other audit<br />
parameters which will in<strong>for</strong>m future EBM<br />
initiatives 2 .<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
1
EDITORIAL<br />
The main short-coming <strong>of</strong> EBM is that there<br />
is more diseases and clinical questions<br />
without evidence-base than those with a<br />
robust external evidence. While critics point<br />
out the statistical nature <strong>of</strong> most research<br />
evidence thereby making extrapolation to a<br />
particular patient rather difficult, this<br />
translational gap could be bridged by filtering<br />
all evidence through “clinical relevance”. Most<br />
important and worrying is the fact that these<br />
‘gold-standards’ are not without errors and<br />
thus are fallible. One <strong>of</strong> the main arguments<br />
on what constitutes “clinical judgement”<br />
arises from the fact that while critics seem to<br />
equate it with “ clinical experience” which is<br />
afflicted with psychological biases 6 , the EBM<br />
enthusiasts point out that best evidence is an<br />
important part <strong>of</strong> the decision-making process<br />
or “clinical judgement” <strong>for</strong> the patient. Clinical<br />
freedom and innovation are other potential<br />
collateral victims <strong>of</strong> EBM movement according<br />
to the critiques and some suspect it to be a<br />
“management Trojan-horse”.<br />
As pointed out by the Institute <strong>of</strong> <strong>Medicine</strong><br />
(IOM) Roundtable conference on “ Learning<br />
health care system”, convened in 2006, the<br />
success <strong>of</strong> the EBM movement mandates<br />
involvement <strong>of</strong> all the stake-holders <strong>of</strong><br />
healthcare delivery system. They include<br />
pr<strong>of</strong>essionals, managers, leaders, policymakers,<br />
industry representatives and the<br />
public. Incidentally, evidence synthesis would<br />
help put the evidence into perspectives <strong>for</strong><br />
different stake-holders, thereby preventing<br />
EBM policies and initiatives from getting out<br />
<strong>of</strong> context.<br />
Sadly, despite more than two decades <strong>of</strong> the<br />
movement, much headway has not been<br />
made in turning the fundamentals and the<br />
philosophy into practice so as to lift up patient<br />
outcomes. Some <strong>of</strong> the tested interventions<br />
include “feedback”, “ ownership”, “<br />
administrative “, “detailing” which is a part <strong>of</strong><br />
“social influence”, “ involvement <strong>of</strong> opinionleader”,<br />
“computerized decision-support<br />
systems” and “consumerism”. “Ownership” <strong>of</strong><br />
which examples include pr<strong>of</strong>essional<br />
guidelines means making the pr<strong>of</strong>essional<br />
members feel they are part <strong>of</strong> ‘it’ and have<br />
contributed materially, resonates with the<br />
current managerial advances. Total quality<br />
management leads us to health care<br />
equivalent -continuous quality improvement<br />
(CQI). In short, it requires a system overhaul.<br />
In the USA <strong>for</strong> example, managed-care<br />
hospitals are put under the umbrella <strong>of</strong> pay<strong>for</strong>-per<strong>for</strong>mance(P4P)<br />
guidelines, which is<br />
basically a “financial penalties” intervention.<br />
The pr<strong>of</strong>essionals are looking toward the IT<br />
revolution and beyond <strong>for</strong> solutions, and use<br />
<strong>of</strong> hand-held PDA and e-book reader <strong>for</strong> point<strong>of</strong>-care<br />
evidence needs is a recent such<br />
example which seems to be working at least<br />
in the developed countries. But perhaps even<br />
more important <strong>for</strong> developing country is EBM<br />
“training the trainers” programs 7 . Globally<br />
present research is directed towards<br />
developing an adequate assessment tool after<br />
interventions to ensure positive patient<br />
outcomes. The “Fresno Test” is one such<br />
promising tool which has been validated in<br />
Spain 8 and is being tested in Australia starting<br />
this year 9 . The Spanish study found that<br />
framing a clinical question according to<br />
PICOTT guidelines is the most difficult<br />
outcome to achieve. The authors<br />
hypothesized that it could be due to the fact<br />
that during the rather short EBM course the<br />
participants were constrained by the<br />
multitudes <strong>of</strong> tasks. The Australian study is<br />
looking at institution <strong>of</strong> EBM skills as early as<br />
the 3rd clinical year.<br />
The situation back home is wanting especially<br />
in the peripheral and rural areas. The third<br />
world countries including India with its northeastern<br />
states are a fry cry from seeing a<br />
general acceptance <strong>of</strong> EBP sooner, probably<br />
because <strong>of</strong> lack <strong>of</strong> locally relevant evidence<br />
base; corrupted infrastructure and processes;<br />
heavy influence <strong>of</strong> the industry; lack <strong>of</strong><br />
adequate IT solutions customized to the local<br />
needs; lack <strong>of</strong> a critical mass <strong>of</strong> concerned<br />
citizens, and resistance <strong>of</strong> the private sector<br />
to follow EBM principles <strong>for</strong> obvious reasons.<br />
Paradoxically we are actually in need <strong>of</strong><br />
controlling the distribution <strong>of</strong> healthcare<br />
delivery demography-wise as well as<br />
geography-wise while doing away with the<br />
unnecessary cost <strong>of</strong> ineffective interventions.<br />
And mostly in this part <strong>of</strong> the world clinicians<br />
2 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
EDITORIAL<br />
are depraved <strong>of</strong> the much-needed evidencebase<br />
as well as the access to it, partly due to<br />
utter lack <strong>of</strong> IT infrastructure and partly<br />
because EBM has not gained a firm foothold<br />
yet. Possibly the Department <strong>of</strong> <strong>Medical</strong><br />
Education in each institute can take a more<br />
pro-active role in EBM skills courses and CME<br />
and take up research on integration <strong>of</strong> EBM<br />
principles into medical curriculum and clinical<br />
rounds while the local or regional pr<strong>of</strong>essional<br />
bodies or societies can take up leadership roles<br />
in EBP guidelines and awareness campaigns.<br />
We, both academicians and practitioners,<br />
cannot depend on wishful thinking but on being<br />
prepared <strong>for</strong> the inevitable health re<strong>for</strong>ms and<br />
realities sweeping across the globe.<br />
References:<br />
1. Trinder L. Introduction: the Context <strong>of</strong><br />
<strong>Evidence</strong>-Based Practice: In Trinder L,<br />
Reynolds S.eds. evidence-Based<br />
Practice: A Critical Appraisal.<br />
Ox<strong>for</strong>d:Blackwell Science 2000. p.1-16<br />
2. Sackett DL, Rosenberg WMC, Gray<br />
JAM, Haynes RB, Richardson WS.<br />
<strong>Evidence</strong> <strong>based</strong> medicine: what it is and<br />
what it isn’t. BMJ. 1996;312:71–2.<br />
3. Straus SE, McAlister FA. <strong>Evidence</strong><strong>based</strong><br />
medicine: a commentary on<br />
common criticisms. CMAJ.<br />
2000;163:837–41.<br />
4. Charlton BG. Restoring the Balance:<br />
<strong>Evidence</strong>-<strong>based</strong> medicine put in its<br />
place. J Eval Clin Pract 1997;3:87-98<br />
5. Ashrafian H, Darzi A, Athanasiou TH.<br />
<strong>Evidence</strong> Synthesis: Evolving<br />
Methodologies to Optimise Patient Care<br />
and Enhance Policy Decisions. In:<br />
Athanasiou TH, Darzi A (Editors).<br />
<strong>Evidence</strong> Synthesis in Healthcare : A<br />
Practical Handbook <strong>for</strong> Clinicians.<br />
London: Springer 2011.p.1-46<br />
6. Tversky A, Kahneman D. Judgment<br />
under uncertainty: Heuristics and biases.<br />
Science. 1974;185:1124–31<br />
7. Walczak J, Kaleta A, Gabryœ E, et al.<br />
How are “teaching the teachers” courses<br />
in evidence <strong>based</strong> medicine evaluated?<br />
A systematic review BMC <strong>Medical</strong><br />
Education 2010, 10:64<br />
8. Argimon-Pallàs JM, Flores-Mateo G,<br />
Jimenez-Villa J et al. Effectiveness <strong>of</strong> a<br />
short-course in improving knowledge<br />
and skills on evidence-<strong>based</strong> practice<br />
BMC Family Practice 2011, 12:64<br />
9. Ilic D, Tepper K, Misso M. Teaching<br />
evidence <strong>based</strong> medicine literature<br />
searching skills to medical students<br />
during the clinical years – a protocol <strong>for</strong><br />
a randomised controlled trial BMC<br />
<strong>Medical</strong> Education 2011, 11:49<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
3
ORIGINAL ARTICLE<br />
Comparison <strong>of</strong> laparoscopic pyeloplasty and open pyeloplasty <strong>for</strong> the treatment<br />
<strong>of</strong> primary uretero pelvic junction obstruction<br />
1<br />
Ak. Kaku Singh, 2 N.P.Gupta,<br />
Abstract<br />
Objectives: To compare the complications ,<br />
hospital stay , and functional results <strong>of</strong><br />
laparoscopic and open pyeloplasty <strong>for</strong> primary<br />
uretero pelvic junction (UPJ) obstruction.<br />
Methods: From July 2004 to Dec. 2006, 56<br />
consecutive non randomized patients <strong>of</strong><br />
primary UPJ obstruction who underwent open<br />
and laparoscopic pyeloplasty in All India<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences were included<br />
in the study.There were 31 cases <strong>of</strong><br />
laparoscopic pyeloplasty and 25 cases <strong>of</strong><br />
open pyeloplasty .The decision between the<br />
two techniques depended on patient‘s<br />
preference and surgeon‘s experience .The<br />
preoperative evaluation included history <strong>of</strong><br />
clinical symptoms, ultrasound, X-ray IVP and<br />
renal dynamic scan . The patients were<br />
followed up at 3 months and 1 year after the<br />
surgery by evaluation <strong>of</strong> clinical symptom and<br />
renal dynamic scan. Success was<br />
considered if there was improvement <strong>of</strong><br />
symptom and absence <strong>of</strong> an obstructive<br />
pattern during the washout phase <strong>of</strong> a renal<br />
scan. Result: The mean operating time was<br />
less in the open than in the laparoscopy group<br />
( 98 mins and 145 mins respectively). The<br />
mean blood loss was 85ml in the laparoscopy<br />
and 101 ml in the open pyeloplasty group. The<br />
mean analgesic requirement was less in the<br />
1. Associate Pr<strong>of</strong>essor, Department <strong>of</strong> Urology,<br />
RIMS, Imphal, 2. Ex. Pr<strong>of</strong>essor and Head<br />
Department <strong>of</strong> Urology AIIMS , New Delhi<br />
Address <strong>for</strong> correspondence<br />
Dr.Ak.Kaku Singh, Associate Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Urology RIMS , Imphal<br />
Pin : 795004 e-mail : kakuakoijam@yahoo.com<br />
laparoscopy group than in the open group<br />
(75mg vs 127 mg <strong>of</strong> pethidine). No<br />
intraoperative complications occurred in either<br />
group. Post operative complications occurred<br />
in 2/31 cases in laparoscopic group and none<br />
in the open group.The mean hospital stay was<br />
5.8 days <strong>for</strong> laparoscopic pyeloplasty and 6.7<br />
days <strong>for</strong> open pyeloplasty. Of the 27 cases in<br />
the laparoscopy group, 25 cases were free <strong>of</strong><br />
symptoms and all the 22 patients in the open<br />
group were free <strong>of</strong> symptoms. Renal scan<br />
shows good clearance in 23 cases, slow<br />
clearance in 3 cases and obstructed drainage<br />
in 1 in the laparoscopy group, and good<br />
clearance in19 cases and slow clearance in<br />
3 cases in the open group. At 1 year follow<br />
up, 14 cases were available in group I, all were<br />
free <strong>of</strong> symptoms and 12 showed good<br />
clearance and 2 showed slow clearance .And<br />
in group II, 10 cases were available <strong>for</strong> follow<br />
up , all were free <strong>of</strong> symptoms and 8 cases<br />
showed good clearance and 2 cases showed<br />
slow clearance on diuretic renogram.<br />
Conclusion: Laparoscopic pyeloplasty is<br />
associated with decreased hospital stay and<br />
early recovery from pain but takes longer<br />
operating time and has comparable functional<br />
results as open pyeloplasty.<br />
Key words: Laparoscopic pyeloplasty, open<br />
pyeloplasty.<br />
Introduction: Open Anderson Hyne’s<br />
dismembered pyeloplasty is the gold standard<br />
<strong>for</strong> the treatment <strong>of</strong> UPJ obstruction with the<br />
highest long term success rate with which<br />
other techniques should be compared 1.<br />
Laparoscopic pyeloplasty which was first<br />
4 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
described by Schuessler et al in 1993 has<br />
emerged as an alternative technique with<br />
comparable results to open pyeloplasty.<br />
Laparoscopic pyeloplasty producing<br />
comparable functional result with the open<br />
pyeloplasty and having the advantages <strong>of</strong> a<br />
minimally invasive procedure is gradually<br />
replacing open surgery as the gold standard<br />
in the treatment <strong>of</strong> UPJ obstruction , but the<br />
laparoscopic procedure requires significant<br />
laparoscopic surgical training and<br />
experience 2-6 .<br />
We report our results <strong>of</strong> a prospective nonrandomized<br />
study conducted to compare the<br />
clinical and functional result <strong>of</strong> laparoscopic<br />
and open pyeloplasty <strong>for</strong> primary UPJ<br />
obstruction.<br />
Materials and Methods: Between July 2004<br />
to December 2006, 56 patients underwent<br />
laparoscopic or open pyeloplasty <strong>for</strong> primary<br />
UPJ obstruction in our department. In the<br />
laparoscopic group (Group I) , there were 31<br />
and in the open group (Group II), there were<br />
25 patients. Symptomatic patients with<br />
primary UPJ obstruction proven with X-Ray<br />
IVP and diuretic renogram who has normal<br />
renal function and normal contralateral kidney<br />
unit were included in the study.<br />
Secondary UPJ obstruction, UPJ obstruction<br />
associated with other pathology or congenital<br />
anomaly were excluded. The operative time,<br />
estimated blood loss, type <strong>of</strong> pyeloplasty and<br />
the presence <strong>of</strong> crossing vessel were<br />
recorded . In the laparoscopy group, the route<br />
<strong>of</strong> approach was either Retroperitoneoscopic<br />
or Transperitoneal, the method <strong>of</strong> stenting<br />
either antigrade or retrograde and conversion<br />
to open with the reason were also recorded.<br />
In post operative period , mean analgesic<br />
requirement , period <strong>of</strong> hospital stay , start <strong>of</strong><br />
normal daily activity, resumption <strong>of</strong> normal diet<br />
and postoperative complications were<br />
recorded. The DJ stent was removed 4-6<br />
weeks after the operation. In the follow up<br />
diuretic renogram was per<strong>for</strong>med at 3 months<br />
and 1 year after the surgery and compared<br />
with the pre operative finding , the relieve or<br />
presence <strong>of</strong> symptoms because <strong>of</strong> the UPJ<br />
obstruction was also recorded.<br />
Result: Anderson Hyne’s dismembered<br />
pyeloplasty was per<strong>for</strong>med in 26/31<br />
procedures in Group I and 21/25procedures<br />
in Group II . The age <strong>of</strong> the patients range<br />
from 12 -70 years in the laparoscopy group<br />
and 2 – 68 in the open group showing a<br />
tendency <strong>for</strong> open pyeloplasty in children. The<br />
mean operating time was less in the open than<br />
in the laparoscopy group , 98 mins and 145<br />
mins respectively.The mean blood loss was<br />
85 ml in the laparoscopy group and 101 ml in<br />
the open group .The average analgesic<br />
requirement was less in the laparoscopy<br />
group than in the open group . Crossing vessel<br />
was encountered in 7/31 cases in Group I and<br />
2/25 cases in Group II (Table I) . No<br />
intraoperative complications occurred in either<br />
group . One case in the laparoscopy group<br />
was converted to open pyeloplasty because<br />
<strong>of</strong> anastomotic tension . Post operative<br />
complications occurred in 2/31 cases in<br />
laparoscopic group and none in the open<br />
group.The patient who was converted to open<br />
surgery because <strong>of</strong> tension while<br />
anastomosing had wound infection and post<br />
operative fever . The other patient had<br />
misplaced DJ stent , coiled in the pelvis had<br />
post operative prolong drainage , ileus ,fever<br />
and jaundice .The mean hospital stay was 5.8<br />
days <strong>for</strong> laparoscopic pyeloplasty and 6.7 days<br />
<strong>for</strong> open pyeloplasty (Table I ). At 3 months <strong>of</strong><br />
follow up 25/27 and 22/22 patients in group I<br />
and group II respectively are free <strong>of</strong> symptom.<br />
Renal scan shows good clearance in 23/27,<br />
slow clearance in 3/27 and obstructed<br />
drainage in 1 /27 in group I, and good clearance<br />
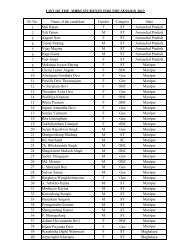
Table 1. Operative and Post operative parameters<br />
Laparoscopic Open pyeloplasty<br />
pyeloplasty<br />
Mean operating time<br />
in minutes (range) 145.32±26.83 97.80±18.15<br />
Mean blood loss in<br />
ml (range) 84.84 ±34.53 100.8±43.84<br />
Mean analgesic<br />
requirement<br />
(pethidine in mg) 75±15.81 127±53.97<br />
Mean length <strong>of</strong><br />
hospital stay in<br />
days (range) 5.8±3.0 6.7 ±1.7<br />
Mean duration <strong>of</strong><br />
recovery to routine<br />
activity in days (range) 15.0±7.4 20.2±5.8<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
5
ORIGINAL ARTICLE<br />
Table 2. Follow up at 3 months<br />
Lap Open<br />
pyeloplasty pyeloplasty<br />
` N=27/31 N=22/25<br />
Renal Dynamic Scan<br />
Good clearance 23 19<br />
Slow clearance 3 3<br />
Obstruction 1<br />
Symptom (Pain)<br />
Absent 26 22<br />
Present 1 0<br />
Table 3. Follow up at 1 years<br />
Lap Open<br />
pyeloplasty pyeloplasty<br />
` N=14/31 N=10/25<br />
Renal Dynamic Scan<br />
Good clearance 12 8<br />
Slow clearance 2 2<br />
Obstruction<br />
Symptom (Pain)<br />
Absent 14 10<br />
Present - -<br />
in19/22 and slow clearance in 3/22 in group II<br />
(Table 2). The one patient in Group I, who had<br />
obstructed drainage and was symptomatic<br />
underwent nephrectomy as it was found to<br />
be pyonephrotic when explored <strong>for</strong> redo<br />
pyeloplasty. At 1 year follow up 12/14 and 2/<br />
14 patients show good and slow clearance<br />
respectively in group I and all the patients are<br />
free <strong>of</strong> symptom in this group and in group II<br />
,8/10 patients show good clearance and 2/10<br />
patients show slow clearance and all the<br />
patients are free <strong>of</strong> symptom (Table 3).<br />
Discussion: Open dismembered pyeloplasty<br />
is the gold standard <strong>for</strong> the treatment <strong>of</strong> UPJ<br />
obstruction with a success rate exceeding<br />
90%. Minimally invasive procedure like<br />
antegrade percutaneous endopyelotomy,<br />
endop-yeloplasty, retrograde endopyelotmy<br />
and balloon dilatation are associated with<br />
lower success rates and outcome is not<br />
favourable in the presence <strong>of</strong> a crossing<br />
vessel, severe hydronephrosis, poor renal<br />
function, long UPJ stricture or complete<br />
obliteration and severe periureteral fibrosis.<br />
These procedures are also associated with<br />
significant risk <strong>of</strong> hemorrhage, many cases<br />
requiring blood transfusion and sometimes<br />
postoperative embolization or nephrectomy<br />
7,8,9 .<br />
Laparoscopic pyeloplasty which was first<br />
reported by Schuessler et al became a<br />
minimally invasive technique having equal<br />
success rate as that <strong>of</strong> open surgery .<br />
Laparoscopic pyeloplasty can be per<strong>for</strong>med<br />
by transperitoneal or retroperitoneal approach.<br />
We have per<strong>for</strong>med laparoscopic pyeloplasty<br />
by both transperitoneal and retroperitoneal<br />
approaches. Both approaches has pros and<br />
cons but we preferred transperitoneal<br />
approach as it allows more working space<br />
which favour easy dissection and suturing .<br />
However , others recommend extraperitoneal<br />
approach as they do not find the smaller<br />
operating space hindering the dissection and<br />
anastomosis and also decreased risk <strong>of</strong><br />
intraperitoneal organ damage, decreased post<br />
operative ileus and absence <strong>of</strong> contaminating<br />
the peritoneal cavity with blood, urine or<br />
carbonic acid 3,10 . Laparoscopic pyeloplasty<br />
has all the good quality <strong>of</strong> minimally invasive<br />
procedure like decreased length <strong>of</strong> hospital<br />
stay, decreased post operative pain, less<br />
analgesic requirement and faster recovery<br />
while it has comparable funtional results with<br />
open pyeloplasty. However , laparoscopic<br />
pyeloplasty require greater laparoscopic skills<br />
<strong>for</strong> reconstructive surgery involving<br />
intracorporeal suturing techniques with a<br />
steep learning curve which limited this<br />
procedure to become widely practiced 11,12,13 .<br />
With the advent <strong>of</strong> robot, which provides ease<br />
<strong>of</strong> intracorporeal suturing and shorter learning<br />
curve, robotic assisted laparoscopic<br />
pyeloplasty is becoming another minimally<br />
invasive technique <strong>for</strong> the treatment <strong>of</strong> UPJ<br />
obstruction.<br />
Anderson Hyne’s dismembered pyeloplasty<br />
was the commonest procedure per<strong>for</strong>med<br />
and was preferred <strong>for</strong> patients with crossing<br />
vessel, bulky pelvis requiring subtraction<br />
pyeloplasty and in patients with poor renal<br />
function. Fenger pyeloplasty was per<strong>for</strong>med<br />
if there was only a short stenotic ureteropelvic<br />
segment and the renal pelvis was not baggy.<br />
Foley Y-V pyeloplasty was done if the renal<br />
pelvis did not require reduction and ureter was<br />
inserted high into the renal pelvis .Scardino<br />
prince vertical flap pyeloplasty was per<strong>for</strong>med<br />
6 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
in two cases <strong>of</strong> open pyeloplasty ,both cases<br />
having long obstructed UPJ segment .<br />
The mean operation time <strong>of</strong> 145 minutes in<br />
laparoscopic pyeloplasty was very much<br />
longer than in the open pyeloplasty group but<br />
is comparable to other series <strong>of</strong> laparoscopic<br />
pyeloplasty. The mean blood loss were<br />
comparable in both the groups and the mean<br />
blood loss in the laparoscopy group is<br />
comparable to other studies . In our study ,<br />
there was not much difference in the mean<br />
length <strong>of</strong> hospital stay though it was less in<br />
the laparoscopy pyeloplasty group .The mean<br />
hospital stay <strong>of</strong> approximately 5. 8 days in the<br />
laparoscopy group is also longer in<br />
comparison with other series <strong>of</strong> laparoscopic<br />
pyeloplasty, this is because <strong>of</strong> two patients in<br />
this group , one patient who was converted to<br />
open surgery and got wound infection in the<br />
post operative period with a hospital stay <strong>of</strong><br />
10 days. Another patient who got misplaced<br />
DJ stent , complicated with post operative<br />
fever, prolong drainage ,jaundice and<br />
abdominal pain with post operative hospital<br />
References:<br />
1. O’Reilly P H , Brooman P J , Mak S et al.<br />
The long-term results <strong>of</strong> Anderson-Hynes<br />
pyeloplasty . BJU Int 2001;87: 287- 289 .<br />
2. Schuessler W W, Grune MT, Tecuanhuey<br />
L V and Preminger G M. Laparoscopic<br />
dismembered pyeloplasty. J Urol<br />
1993;150: 1795-1799.<br />
3. Moon DA, El-Shazly MA, Chang CM,<br />
Gianduzzo TR, Eden CG. Laparoscopic<br />
pyeloplasty: evolution <strong>of</strong> a new gold<br />
standard. Urology 2006;67: 932-6.<br />
4. Klinger HC,Remzi M, Janetschek G et al.<br />
Comparison <strong>of</strong> open versus laparoscopic<br />
pyeloplasty technique in treatment <strong>of</strong><br />
uretero-pelvic junction obstruction . Eur<br />
Urol 2003; 44: 340-345<br />
5. Brooks JD, Kavoussi LR, Preminger GM<br />
et al. Comparison <strong>of</strong> open and<br />
endourologic approaches to the<br />
obstructed uretero pelvic junction.<br />
Urology 1995; 45: 791-795.<br />
6. Motola JA, Badlani GH and Smith AD.<br />
Results <strong>of</strong> 212 consecutive<br />
endopyelotomies : an 8-year follow up. J<br />
Urol 1993;149: 453-456.<br />
7. Nadler B, Rao GS, Pearl MS et al.<br />
stay <strong>of</strong> 20 days.Moreover our patients prefer<br />
to get discharged from the hospital when they<br />
have recuperated fully and perurethral catheter<br />
and drain is removed .The mean analgesic<br />
requirement was less in the laparoscopic<br />
pyeloplasty group which is in consistence with<br />
other studies 4,5 .We are not per<strong>for</strong>ming<br />
statistical analysis <strong>of</strong> our results because <strong>of</strong><br />
the small size <strong>of</strong> the study groups , multiple<br />
number <strong>of</strong> surgeons have per<strong>for</strong>med the<br />
operations in both the groups and majority <strong>of</strong><br />
the patients were lost to follow up at 1 year .<br />
Conclusion: Laparoscopic pyelpoplasty<br />
requires skilled intracorporeal suturing and it<br />
takes longer time to per<strong>for</strong>m. But laparoscopic<br />
pyeloplasty has the advantage <strong>of</strong> minimally<br />
invasive procedure havingadvantages <strong>of</strong> less<br />
pain, less amount <strong>of</strong> analgesic required,<br />
shorter period <strong>of</strong> hospital stay, faster recovery<br />
and better cosmesis over open pyeloplasty.<br />
Short term functional results also shows that<br />
laparoscopic pyeloplasty is equally efficacious<br />
as open pyeloplasty.<br />
Acucise endopyelotomy: assessment <strong>of</strong><br />
long-term durability. J Urol 1996;156:<br />
1094-1098.<br />
8. Van Cangh PJ. Wilmart JF, Opsomer RJ<br />
et al. Long-term results and late<br />
recurrence after endouretero pyelotomy:<br />
a critical analysis <strong>of</strong> prognostic factors.<br />
J Urol 1994;151: 934-937.<br />
9. Van Cangh PJ, Nesa S. Endopyelotomy.<br />
prognostic factors and patient selection.<br />
Urol Clin N Am 1998; 25 : 281<br />
10. Ben Slama M R, Salomon L, Hoznek A,<br />
et al. Extraperitoneal laparoscopic repair<br />
<strong>of</strong> uretero pelvic junction obstruction:<br />
initial experience in 15 Cases. Urology<br />
2000;56: 45-48.<br />
11. Eden CG, Cahill D, Allen JD. Laparoscopic<br />
dismembered pyeloplasty: 50<br />
consecutive cases. BJU Int 2001; 88:<br />
526-81.<br />
12. Jarett TW, Chan DY, Charambura TC,<br />
Fugita O, Kavoussi LR. Laparoscopic<br />
pyeloplasty the first 100 cases. J Urol<br />
2002;167: 1253-6.<br />
13. Inagaki T, Rha K H, Ong AM et al.<br />
Laparoscopy pyeloplasty : current status.<br />
BJU Int 2005;95: 102-105.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
7
ORIGINAL ARTICLE<br />
Acute kidney injury in HIV-positive patients<br />
1<br />
Devi PS, 2 Singh Lk S, 2 Dhanaraj Ch, 3 Shreeniwas S, 4 Singh S<br />
Abstract<br />
Objective : To study the incidence, spectrum,<br />
prognosis and outcome <strong>of</strong> clinical renal<br />
disease with special emphasis on acute<br />
kidney injury in patients with HIV infection.<br />
Methods: A protocol <strong>of</strong> study was prepared.<br />
All HIV patients <strong>of</strong> both genders regardless <strong>of</strong><br />
age attending Antiretroviral treatment (ART)<br />
Centre and those admitted in the wards <strong>of</strong> the<br />
hospital (Sir Sunderlal Hospital, Varanasi, Uttar<br />
Pradesh, India) were subjected <strong>for</strong> screening<br />
<strong>of</strong> clinical renal disease. HIV-seropositive<br />
patients with clinical renal diseases were<br />
included and divided into two groups: (A)<br />
Asymptomatic patients without manifestations<br />
<strong>of</strong> renal diseases but found to have a<br />
significant renal involvement on screening<br />
and (B) Patients with symptomatic renal<br />
diseases. HIV-associated renal disease were<br />
diagnosed using the following criteria: 1)<br />
Positive HIV Serology, 2) CD4 T-Lymphocyte<br />
count, 3) Proteinuria / Haematuria, 4) Elevated<br />
serum creatinine and 5)Quantitative<br />
proteinuria (24 hours urinary protein or spot<br />
urine Protein/creatinine ratio). National AIDS<br />
Control Organisation (NACO) Guidelines <strong>of</strong><br />
India, 2007 were followed <strong>for</strong> the diagnosis <strong>of</strong><br />
1<br />
Assistant Pr<strong>of</strong>essor 2 Associate pr<strong>of</strong>essor, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal; 3 Consultant<br />
Nephrologist, ARTEMIS Hospital, Gurgaon; 4 Lecturer,<br />
Department <strong>of</strong> Nephrology, Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Banaras Hindu University, Varanasi (India).<br />
Address <strong>for</strong> Correspondence:<br />
Dr Loukrakpam Sharatchandra Singh, Associate<br />
Pr<strong>of</strong>essor (<strong>Medicine</strong>), Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal – 795004 (India).<br />
e-mail: lkbhu@sify.com<br />
HIV-seropositivity. Results: 47 HIVseropositive<br />
patients were found to have<br />
clinical renal disease during the study period<br />
<strong>of</strong> August 2007 and July 2009. During the two<br />
years study period, there were 3545 patients<br />
<strong>of</strong> HIV-seropositive patients and only 1725<br />
patients (611 females and 1114 males) were<br />
enrolled <strong>for</strong> ART as they fulfilled NACO<br />
guidelines. 47 (1.33%) patients (44 males and<br />
3 females) were found to have clinical renal<br />
disease. Most <strong>of</strong> the patients (45/47) had AKI<br />
(pre-renal-15, acute tubular necrosis-27,<br />
interstitial nephritis-3). Proteinuria, serum<br />
creatinine and serum albumin were 0.935±<br />
0.985 gm/day, 5.28± 5.64 mg% and 2.92± 0.58<br />
respectively. Renal biopsy were done on 2<br />
indicated patients who showed<br />
granulomatous glomerulonephritis, and<br />
Tubulointerstitial nephritis in one patient each.<br />
CD4 count was in the range <strong>of</strong> 43-<br />
842(170.36± 157.75) cells/µL. 9 patients<br />
(1.7%) having HIV-related clinical renal disease<br />
died due to sepsis (5), tubercular meningitis<br />
(3) and hypovolemia (2). Peritoneal dialysis<br />
could be done in 6 patients. Conclusion: AKI<br />
mostly related to acute tubular necrosis was<br />
the most common HIV-related clinical renal<br />
disease. <strong>Evidence</strong> <strong>of</strong> non-specific glomerular<br />
disease with or without interstitial nephritis<br />
was observed in 2 patients. HIV-associated<br />
nephropathy well documented in western /<br />
African-American literatures was not observed<br />
in our study<br />
Key words: HIV Infection, Acute Kidney injury,<br />
Mortality, CD4.<br />
8 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Introduction : As early as 1984, physicians<br />
in New York and Miami recognized kidney<br />
disease as rare but devastating complication<br />
<strong>of</strong> the acquired immunodeficiency syndrome<br />
(AIDS) 1 . The association between HIV-1<br />
infection and kidney disease was made in<br />
1984 and much has been learnt over the last<br />
25 years. Renal disorders are encountered at<br />
all stages <strong>of</strong> HIV infection, and range from fluid<br />
and electrolyte imbalances commonly seen<br />
in hospitalised HIV infected patients to HIVassociated<br />
nephropathy (HIVAN), which<br />
progresses to end stage renal disease 2 . Acute<br />
kidney injury is also common among patients<br />
with HIV/AIDS. The exact pathogenesis <strong>of</strong><br />
renal disease in HIV-associated nephropathy<br />
is not known in spite <strong>of</strong> intense research in<br />
the field. However, it is proposed that HIVassociated<br />
kidney disease is due to direct<br />
kidney infection with HIV or from medications<br />
used to treat HIV and their resulting adverse<br />
effects 3 . There are a few Indian studies on<br />
HIV-associated renal disease 4 . Most <strong>of</strong> the<br />
studies are from African population 5 .<br />
The aim <strong>of</strong> our proposed work is to study the<br />
incidence, spectrum, prognosis and outcome<br />
<strong>of</strong> clinical renal disease with special emphasis<br />
on acute kidney injury in patients with HIV<br />
infection in the Indian setting.<br />
Material and Methods: All HIV- seropositive<br />
patients <strong>of</strong> both genders regardless <strong>of</strong> age<br />
attending ART Centre <strong>of</strong> Sir Sunderlal<br />
Hospital, Institute <strong>of</strong> <strong>Medical</strong> Sciences,<br />
Banaras Hindu University, Varanasi, India and<br />
those admitted in the wards <strong>of</strong> the hospital<br />
were subjected to screening <strong>for</strong> clinical renal<br />
disease. HIV positive patients with clinical<br />
renal disease during August 2007 and July<br />
2009 were included in this prospective study.<br />
HIV-infected patients were divided into two<br />
groups:<br />
(1) Asymptomatic patients without<br />
manifestations <strong>of</strong> renal disease but found to<br />
have a significant renal involvement on<br />
screening and<br />
(2) Patients with symptomatic renal<br />
disease. The following procedures or<br />
methods were utilized:<br />
A. In<strong>for</strong>med consent from all patients<br />
B. Ethical clearance from the ethical<br />
committee <strong>of</strong> the institute<br />
C. Criteria <strong>for</strong> HIV-positivity <strong>based</strong> on National<br />
AIDS Control Organisation (NACO)<br />
Guidelines <strong>of</strong> India.<br />
D. Criteria <strong>for</strong> HIV-associated clinical renal<br />
Disease:<br />
1) Asymptomatic group: Mild proteinuria,<br />
elevated serum creatinine, normal or<br />
decreased CD4 count<br />
2) Symptomatic group: Hypertension,<br />
proteinuria, haematuria, elevated serum<br />
creatinine, decreased CD4 count d
ORIGINAL ARTICLE<br />
Results: The two years prospective study<br />
included 3545 HIV-seropositive patients who<br />
were referred to the ART centre <strong>for</strong> further<br />
evaluation. Of 3545 HIV-seropositive patients,<br />
1725 (1114 males, 611 females) patients were<br />
enrolled or ART drugs as they fulfilled the<br />
NACO guidelines <strong>of</strong> India <strong>for</strong> the treatment <strong>of</strong><br />
AIDS. The clinical renal disease was noted in<br />
47/3545 (1.33%) patients. The majority <strong>of</strong> HIVseropositive<br />
patients with clinical renal<br />
disease were males (93.61%) (Table 1).<br />
Maximum number <strong>of</strong> patients were in the age<br />
LEGENDS<br />
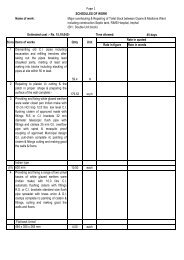
Table 1 : Demography <strong>of</strong> patients (n=47).<br />
Parameter Number %<br />
Sex Male<br />
Female 44 93.61<br />
3 6.38<br />
Age 15-20 2 4.25<br />
21-30 12 25.53<br />
31-40 23 48.93<br />
41-50 8 17.02<br />
>50 2 4.25<br />
Table 5 : 24 hours Urinary Protein, CD4 count<br />
and Mortality (n=47).<br />
Table 6 :Serum creatinine, CD4 count and<br />
Mortality (n=47).<br />
Table 2 : Spectrum <strong>of</strong> clinical renal disease in<br />
HIV-serpositive patients (n=47).<br />
Parameter Number %<br />
AKI<br />
Pre-renal 15 31.91<br />
ATN 27 57.45<br />
AIN 3 6.38<br />
CKD stage IV 2 4.26<br />
Proteinuria > 0.5 gm/day 32 68.06<br />
Nephrotic syndrome 2 4.25<br />
Table 3 : Causes <strong>of</strong> AKI (45/47).<br />
Cause Number %<br />
Hypovolemia 2 4.44<br />
Sepsis 4 8.89<br />
Urosepsis 3 6.67<br />
Drug induced 3 6.67<br />
*Mixed causes 33 82.23<br />
*Dehydration, drug induced, bleeding, etc.<br />
Table 4 : Outcome <strong>of</strong> AKI (n=45).<br />
Cause<br />
No. <strong>of</strong> patient (s) Percentage Status<br />
AKI <strong>of</strong> various causes 36 80 Alive<br />
Sepsis 4 8.89 Expired<br />
Tubercular meningitis 3 6.67 Expired<br />
Hypovolemia 2 4.44 Expired<br />
group <strong>of</strong> 31 to 40 years (48.9%) and the age<br />
<strong>of</strong> patients ranged between 16 and 58<br />
(36.34±9.33) years. 28/47(59.57%) were<br />
sexually active males having the occupation<br />
<strong>of</strong> driver. 44 patients were married and 3 were<br />
unmarried. Most <strong>of</strong> the patients were addicted<br />
to alcohol (31), smoking (29) and ganja/<br />
bhang (16).<br />
Anemia (100%), weight loss (100%), oral<br />
candidiasis (61.70%), fever (68.08%),<br />
respiratory problems mostly due to pulmonary<br />
tuberculosis (23.79%) and decreased Urine<br />
output (27.65%) were the common<br />
manifestations in HIV-seropositive patients<br />
with clinical renal disease (Table not shown).<br />
Acute kidney injury (AKI) was the most<br />
common renal manifestation <strong>of</strong> HIVseropositive<br />
patients. Acute tubular necrosis<br />
(57.45%) was the prominent intrinsic renal<br />
lesion <strong>of</strong> AKI in these patients (Table 2). AKI in<br />
HIV-serpositive patients had mixed causes<br />
(82.23%) like dehydration, drugs, and bleeding.<br />
Sepsis (15.56%) was the common factor<br />
10 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
associated with HIV-related AKI (Table 3 &4).<br />
Of 47 HIV-serpositive patients, all patients<br />
were anemic with the hemoglobin level <strong>of</strong><br />
7.87±2.62 gm/dl. Proteinuria, serum creatinine<br />
and serum albumin in these patients were<br />
0.935 ± 0.985 gm/day, 5.28± 5.64 mg /dl and<br />
2.92± 0.58 gm/dl respectively.<br />
Proteinuria more than 0.5 gm/day was found<br />
in 68.08% <strong>of</strong> HIV-serpositive patients (n=47).<br />
24 hour urinary protein excretion in HIVseropositive<br />
patients was in the range <strong>of</strong> 500<br />
mg/day – 1 gm/day in 24 (51.1%) patients.<br />
Urinary protein excretion was in the range <strong>of</strong><br />
300-500 mg/day in 11 (23.4%) <strong>of</strong> cases. 9<br />
patients (19.14%) <strong>of</strong> AKI died due to sepsis<br />
(4), tubercular meningitis (3) and hypovolemia<br />
(2). Thus 80% <strong>of</strong> HIV-seropositive patients with<br />
AKI showed full recovery <strong>of</strong> renal function<br />
(Table 4). 6 symptomatic patients with AKI<br />
were subjected to peritoneal dialysis due to<br />
severe acute renal failure. Low CD4 count<br />
ORIGINAL ARTICLE<br />
hyperuricosuria from tumor lysis syndrome,<br />
and extrarenal obstruction, including<br />
retroperitoneal fibrosis, pelvic<br />
lymphadenopathy, bladder dysfunction,<br />
fungus balls, and nephrolithiasis which have<br />
been observed by various groups. 14 Despite<br />
an observed association between ART<br />
exposure and AKI, individual antiretroviral<br />
agents rarely are implicated. 15<br />
Age, baseline serum creatinine level, and<br />
history <strong>of</strong> hypertension or diabetes were not<br />
associated independently with AKI in 2 recent<br />
studies including a large number <strong>of</strong><br />
ambulatory patients. 15 Prognosis in AKI varies<br />
with severity and etiology. Studies have shown<br />
higher mortality in patients with AKI secondary<br />
to ATN and hemodynamic instability, 9-10 with<br />
similar overall mortality rates in AIDS versus<br />
non-AIDS patients. 10 Nevertheless, AKI<br />
remains a strong predictor <strong>of</strong> mortality in the<br />
ART era. Among hospitalized patients in New<br />
York State, a documented diagnosis <strong>of</strong> AKI<br />
was independently associated with a nearly<br />
6-fold increase in mortality among HIV-infected<br />
patients. 11 Rao et al reported a high incidence<br />
<strong>of</strong> mortality (60%) in HIV-associated clinical<br />
renal disease 2 . However we have observed<br />
only 20% mortality in HIV-associated AKI in<br />
the study. Further studies are needed to<br />
determine if AKI is an independent predictor<br />
<strong>of</strong> mortality or rather a marker <strong>for</strong> greater<br />
systemic illness. The acute and chronic<br />
impact <strong>of</strong> various medications used in the HIVinfected<br />
patient, including ART and antibiotic<br />
medications, also should be investigated<br />
further to decrease toxicity. Future studies <strong>of</strong><br />
AKI in HIV-infected patients should attempt to<br />
use standard definitions to allow <strong>for</strong><br />
comparison across studies.<br />
Poor prognostic markers in patients <strong>of</strong> HIVassociated<br />
AKI are related to a low CD4 count<br />
< 200 cells/µl, low serum albumin, systolic<br />
blood pressure, HIV-RNA level < 10000 copies/<br />
ml and higher serum creatinine level. 2 Lower<br />
CD4 nadir < 200 cells/µl was associated with<br />
AKI, whereas hepatitis C virus (HCV) coinfection<br />
and intravenous drug use were<br />
associated with the development <strong>of</strong> AKI after<br />
the first 3 months <strong>of</strong> HIV care. 15<br />
We have observed most <strong>of</strong> the mortality<br />
related to sepsis and lower CD4 count as also<br />
observed by others. Hypertension, which is<br />
estimated to be present in 12% to 21% <strong>of</strong> the<br />
HIV-infected population, is an independent risk<br />
factor <strong>for</strong> mortality in women beginning ART. 16<br />
Mortality rates <strong>for</strong> HIV-positive patients on<br />
dialysis were initially quite high, approaching<br />
nearly 70% in 1991 and subsequently<br />
decreasing to 24% by 2002. 17 In the CDC<br />
sponsored HIV Epidemiology Research Study<br />
(HERS), the presence <strong>of</strong> proteinuria and / or<br />
elevated serum creatinine levels was<br />
positively associated with an increased rate<br />
<strong>of</strong> death (adjusted hazard ratio, 2.5) as well<br />
as having renal causes <strong>of</strong> death recorded on<br />
death certificates (26% <strong>of</strong> the total deaths).<br />
We have observed all deaths (19.14%) due<br />
to HIV-associated AKI with or without AIDS<br />
defining illnesses.<br />
Proteinuria in HIV-infected patients is defined<br />
as spot urinary protein/ creatinine ratio level<br />
more than 200 mg/g as per Kidney Disease<br />
Outcome Quality Initiative (KDOQI)<br />
guidelines 1,2 . Even in patients with normal<br />
renal function, the presence <strong>of</strong> proteinuria<br />
mainly indicates early kidney disease. And the<br />
presence <strong>of</strong> hypertension in such patients is<br />
12-21%.We have also observed 91.5% <strong>of</strong> the<br />
patients having proteinuria more than 0.3 g/<br />
day. However all the nine deaths related to<br />
HIV-related clinical renal disease had<br />
proteinuria in the range <strong>of</strong> 0.3 – 1.0 g/day. It<br />
indicates the acuity <strong>of</strong> the disease. In the<br />
western and African counterparts heavy<br />
proteinuria (nephrotic range proteinuria) were<br />
found to be associated with CKD or<br />
ESRD. 5,8,9,18<br />
High serum creatinine is an independent risk<br />
factor <strong>for</strong> advancement <strong>of</strong> renal disease and /<br />
or mortality in HIV-associated renal<br />
disease. 10,12 We have got the mean serum<br />
creatinine <strong>of</strong> 5. 28 mg/dl (range, 2.1-37.4 mg/<br />
dl) and all the deaths were related to patients<br />
with serum creatinine level <strong>of</strong> more than 5 mg/<br />
dl. In one study, the mean serum creatinine<br />
level at presentation was 4.2 mg/dL (range, 2<br />
- 15 mg/dL), and proteinuria levels were<br />
variable with a median level <strong>of</strong> 1.76 g/24h<br />
(range, 0-4.5 g/24 h). 19<br />
Renal biopsy in the HIV-infected patient is<br />
required to establish a diagnosis <strong>of</strong> intrinsic<br />
12 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
renal disease, including a variety <strong>of</strong> HIV-related<br />
glomerular diseases, non–HIV-related renal<br />
diseases, and medication nephrotoxicity. We<br />
have come across only 2 patients <strong>of</strong> biopsy<br />
proven granumatous glomerulonephritis (1)<br />
and Intersitial nephritis (1). Our patients<br />
(95.74%) predominantly had AKI. We also had<br />
not found cases <strong>of</strong> HIVAN and HIV-associated<br />
immune complex disease (HIVICK)<br />
which was reported by the western<br />
counterparts 18,20<br />
Hepatitis co-infection and other <strong>for</strong>ms <strong>of</strong> liver<br />
disease also have been associated with AKI<br />
in hospitalized and ambulatory patients with<br />
HIV infection. 21 We have come across only<br />
one case <strong>of</strong> HBV infection in the HIVseropositive<br />
case. Hepatitis C virus (HCV) coinfection<br />
is common among HIV-infected<br />
patients. In our study, there was no HCV coinfection<br />
<strong>of</strong> patients with HIV-associated<br />
clinical renal disease.<br />
Conclusion: Acute kidney injury mostly related<br />
to intrinsic renal injury was the most common<br />
renal disease in our HIV-seropositive patients.<br />
<strong>Evidence</strong> <strong>of</strong> non-specific glomerular disease<br />
with or without interstitial nephritis was<br />
observed in 2 patients.<br />
References<br />
1. Wyatt CM. Kidney Disease in HIV<br />
Infection: Introduction. Seminars in<br />
Nephrology. 2008; 28(6):511-12.<br />
2. Ahuja TS, Borucki M, Funtanilla M,<br />
Shahinian V, Hollander M, Rajaraman S.<br />
Is the prevalence <strong>of</strong> HIV-associated<br />
nephropathy decreasing? Am J<br />
Nephrol.1999;19(6):655-9.<br />
3. Salifu MO. e<strong>Medicine</strong> – HIV Nephropathy.<br />
2007. Available from :<br />
http://www.emedicine.com/med/topic<br />
3203.<br />
4. Anuradha S, Chatterjee A, Bajaj J, Singh<br />
NP, Agarwal SK, Kaur R. Trichosporon<br />
beigelli peritonitis in a HIV-positive patient<br />
on continuous ambulatory peritoneal<br />
dialysis. J Assoc Physicians<br />
India.2000;48(10):1022-4.<br />
5. Wools-Kaloustian K, Gupta SK, Muloma<br />
E, Willis O or, Sidle J, Aubrey RW,et al.<br />
Renal disease in an antiretroviral-naïve<br />
HIV infected outpatient population in<br />
Western Kenya. Nephrol Dialysis<br />
Transplantation. 2007;22(8):2208-12.<br />
6. Hilton R. Acute renal failure. BMJ.<br />
2006;333:786-90.<br />
7. Franceschini N, Napravnik S, Eron JJJ,<br />
Szczech LA, Finn WF. Incidence and<br />
etiology <strong>of</strong> acute renal failure among<br />
ambulatory HIV-infected patients. Kidney<br />
Int.2005;67:1526-31.<br />
8. Nochy D, Glotz D, Dosquet P, et al. Renal<br />
disease associated with HIV infection: a<br />
multicentric study <strong>of</strong> 60 patients from<br />
Paris hospitals. Nephrol Dial Transplant.<br />
1993;8:11-9.<br />
9. Valeri A, Neusy AJ. Acute and chronic<br />
renal disease in hospitalized AIDS<br />
patients. Clin Nephrol.1991; 35:110-18.<br />
10. Peraldi MN, Maslo C, Akposso K,<br />
Mougenot B, RondeauE, Sraer JD. Acute<br />
renal failure in the course <strong>of</strong> HIV infection:<br />
a single-institution retrospective study <strong>of</strong><br />
ninety-two patients and sixty renal<br />
biopsies. Nephrol Dial Transplant.<br />
1999;14:1578-85.<br />
11. Wyatt CM, Arons RR, Klotman PE,<br />
Klotman ME. Acute renal failure in<br />
hospitalized patients with HIV: risk factors<br />
and impact on in-hospital mortality.<br />
AIDS.2006;20:561-5.<br />
12. Rao TK, Friedman EA. Outcome <strong>of</strong><br />
severe acute renal failure in patients with<br />
acquired immunodeficiency syndrome.<br />
Am J Kidney Dis. 1995;25:390-8.<br />
13. Rastegar D, Claiborne C, Fleisher A,<br />
Matsumoto A. A patient with primary<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
13
ORIGINAL ARTICLE<br />
human immunodeficiency virus infection<br />
who presented with acute<br />
rhabdomyolysis. Clin Infect Dis.<br />
2001;32:502-4.<br />
14. Kalim S, Szczech LA., Wyatt CM. Acute<br />
Kidney Injury in HIV-Infected Patients.<br />
Seminars in Nephrology.2008;28(6) :<br />
556-62.<br />
15. Roe J, Campbell LJ, Ibrahim F, Hendry<br />
BM, Post FA. HIV care and the incidence<br />
<strong>of</strong> acute renal failure. Clin Infect Dis.<br />
2008;47:242-9.<br />
16. U.S. Renal Data System. USRDS 2007<br />
Annual data report: atlas <strong>of</strong> chronic kidney<br />
disease and end-stage renal disease in<br />
the United States. 2007. Available from:<br />
http://www.usrds.org/<br />
17. Carter JT, Melcher ML, Carlson LL,<br />
Roland ME, Stock PG. Thymoglobulinassociated<br />
Cd4 T-cell depletion and<br />
infection risk in HIV-infected renal<br />
transplant recipients. Am J Transplant.<br />
2006;6:753-60.<br />
18. Agati VD, Suh JI, Carbone L, Cheng JT,<br />
Appel G. Pathology <strong>of</strong> HIV-associated<br />
nephropathy: A detailed morphologic and<br />
comparative study. Kidney Int<br />
1989;35:1358-70.<br />
19. Briggs WA, Tanawattanacharoen S, Choi<br />
MJ, et al. Clinicopathologic correlates <strong>of</strong><br />
prednisone treatment <strong>of</strong> human<br />
immunodeficiency virus-associated<br />
nephropathy. Am J Kidney Dis.<br />
1996;28:618-21.<br />
20. Szczech LA, Anderson A, Ramers C, et<br />
al. The uncertain significance <strong>of</strong> antiglomerular<br />
basement membrane antibody<br />
among HIV-infected persons with kidney<br />
disease. Am J Kidney Dis. 2006;48:E55-<br />
9.<br />
21. Boccia RV, Gelmann EP, Baker CC, Marti<br />
G, Longo DL. A hemolytic-uremic<br />
syndrome with the acquired<br />
immunodeficiency syndrome. Ann Intern<br />
Med. 1984; 101:716-7.<br />
14 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Clinical pr<strong>of</strong>ile <strong>of</strong> chronic liver disease with reference to hepatocellular<br />
carcinoma in RIMS<br />
1<br />
N. Biplap, 2 Th. Bhimo, 1 Th. Suraj, 3 Th. Brojendro, 4 Lalbiakdiki<br />
Abstract:<br />
Objective: To study the clinical pr<strong>of</strong>ile <strong>of</strong><br />
chronic liver disease (CLD) with reference to<br />
hepatocellular carcinoma (HCC). Methods:<br />
The study was conducted on one hundred and<br />
thirty-two (132) CLD cases at Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences (RIMS), Imphal.<br />
Routine investigations including hepatitis B<br />
surface antigen (HBsAg), hepatitis C antibody<br />
(HCV), and Ultrasound (USG) upper abdomen<br />
were done. Aspiration cytology was done <strong>for</strong><br />
confirmation <strong>of</strong> HCC localized by USG, CT or<br />
MRI. Results: 20 (15.16%) CLD cases had<br />
HCC. Male to female ratio was 3:1. The<br />
maximum number <strong>of</strong> patients with CLD was<br />
found in the age group <strong>of</strong> 45-54 years and<br />
most <strong>of</strong> them were from Imphal west. The<br />
commonest risk factors associated with CLD<br />
are alcohol 67(50.75%), chronic HCV 61<br />
(46.21%) and HIV 31 (23.41%). There were<br />
20 cases <strong>of</strong> HCC (15.15%) including 9(45%)<br />
HCV associated HCC. These nine HCC<br />
cases had HIV-HCV (2 cases), HIV-HBV-HCV<br />
(1 case) as co-infection and chronic HCV with<br />
alcoholism (6 cases). Conclusion: The<br />
commonest risk factors <strong>for</strong> CLD associated<br />
with HCC are alcohol, HCV and co-infection<br />
with HBV, HIV. Routine screening <strong>of</strong> HCV, HBV<br />
and HIV must be done in CLD cases.<br />
Keywords: Chronic liver disease,<br />
Hepatocellular Carcinoma (HCC).<br />
1. Assoc. Pr<strong>of</strong>. 2. Pr<strong>of</strong>. 3. Asst. Pr<strong>of</strong>. 4. PGT, Dept. <strong>of</strong><br />
<strong>Medicine</strong>, RIMS Imphal<br />
Address <strong>for</strong> Correspondence:<br />
Dr. N. Biplap, Assoc. Pr<strong>of</strong>., Dept. <strong>of</strong> <strong>Medicine</strong>, RIMS<br />
Introduction: Hepatocellular Carcinoma<br />
(HCC) is among the commonest malignancies<br />
in the world, ranking the third most frequent<br />
cause <strong>of</strong> cancer mortality. It is up to 4 times<br />
more common in males than in women and<br />
usually arises in a cirrhotic liver. 1 The most<br />
clearly established risk factors <strong>for</strong> HCC are<br />
liver cirrhosis, chronic infection with hepatitis<br />
B and/or C virus, aflatoxin exposure, male<br />
sex, alcohol drinking, and cigarette smoking. 2<br />
A typical interval between HCV-associated<br />
transfusion and subsequent HCC is ~30<br />
years. HCV-associated HCC patients tend to<br />
have more frequent and advanced cirrhosis,<br />
but in HBV-associated HCC, only half the<br />
patients have cirrhosis; the remainders have<br />
chronic active hepatitis. 3 There are about 170<br />
million Hepatitis C Virus (HCV) infected and<br />
about 350 million hepatitis B virus (HBV)<br />
infected persons in the world, both <strong>of</strong> which<br />
are transmitted through parenteral route. 4,5<br />
There are about 33.2 million Human<br />
immunodeficiency virus (HIV) infected<br />
persons in the world, transmission <strong>of</strong> which<br />
is the same as HBV and HCV. 6<br />
HCC have been reported as one <strong>of</strong> the fatal<br />
complications <strong>of</strong> both hepatitis B and C. There<br />
are variations in the proportion and prevalence<br />
<strong>of</strong> these factors in association with and<br />
causation <strong>of</strong> HCC in different regions. There<br />
is so far no study in this part <strong>of</strong> the country<br />
about HCC and the associated risk factors.<br />
There<strong>for</strong>e the present study was taken up to<br />
establish the clinical pr<strong>of</strong>ile <strong>of</strong> HCC in chronic<br />
liver disease and its association with risk<br />
factors like alcohol, HBV, HCV and<br />
co-infection <strong>of</strong> both HBV and HCV.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
15
ORIGINAL ARTICLE<br />
Materials and Methods: The study was<br />
carried out in 132 patients <strong>of</strong> CLD with or<br />
without HCC attending <strong>Medicine</strong> OPD in<br />
collaboration with Departments <strong>of</strong><br />
Radiotherapy and Radiodiagnosis, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal during<br />
September 2008 to August 2010. It is a cross<br />
sectional study. Patients <strong>of</strong> known underlying<br />
malignancy, un-cooperative and unwilling<br />
subjects were excluded.<br />
In<strong>for</strong>med written consent was taken <strong>for</strong> each<br />
case. Detail clinical examination was carried<br />
out <strong>for</strong> each case. Routine investigations<br />
including complete haemogram, urine routine<br />
examination, kidney function test, liver function<br />
test, prothrombin time, random blood sugar,<br />
hepatitis B surface antigen (HBsAg),<br />
HBeAntigen and HCV antibody were done.<br />
HBV and HCV were confirmed by PCR at<br />
Roche Lab, Mumbai. Computed Tomography<br />
(CT) or Magnetic resonance Imaging (MRI)<br />
was done when USG report and serum AFP<br />
level are suggestive <strong>of</strong> HCC. Ultrasound/CT<br />
guided aspiration cytology was done <strong>for</strong><br />
confirmation <strong>of</strong> HCC.<br />
RESULTS AND OBSERVATIONS<br />
A total <strong>of</strong> 132 CLD were enrolled in the study,<br />
out <strong>of</strong> which 20 (15.16%) have HCC and 112<br />
(84.84%) were without HCC (p = 0.24). Of the<br />
112 CLD without HCC 83 (74.1%) were males<br />
and 29(25.9%) were females; <strong>of</strong> the 20<br />
subjects with HCC, 17 (85%) were males and<br />
3(15%) females (p = 0.43) as shown<br />
in Table 1.<br />
Table1.Pr<strong>of</strong>ile <strong>of</strong> chronic liver disease<br />
Pr<strong>of</strong>ile Male Female Total<br />
(N=100) (N=32) (N=132)<br />
CLD without HCC 83(83%) 29 (90.62%) 112 (84.84%)<br />
CLD with HCC 17(17%) 3 (9.38%) 20 (15.16%)<br />
The age-wise distribution <strong>of</strong> CLD with and<br />
without HCC is shown in table 2 and was<br />
found to be maximum in the age group 45-54<br />
years. The ages <strong>of</strong> the 20 HCC (15.15%) were<br />
all above 35 years. The maximum cases were<br />
from Imphal west which is also most thickly<br />
populated.<br />
Table 2. Age distribution:<br />
Age Group CLD without HCC CLD with HCC Total CLD<br />
64 yrs 7 (6.25%) 5 (25%) 12<br />
Total 112 (100%) 20 (100%) 132<br />
Of the 132 chronic liver disease subjects,<br />
69(52 presented with abdominal distension,<br />
49 with fever and 43 with jaundice. 21 had<br />
generalised weakness, 12 pain abdomen, 10<br />
upper GI bleeding, 4 hepatic encephalopathy<br />
and 2 with pulmonary tuberculosis. 18 had<br />
palpable hepatomegaly.<br />
The associated risk factors among the 132<br />
CLD were alcoholism (67 cases ie 50.75%),<br />
HCV (61 cases ie 46.21%) and HBV (11 ie<br />
8.33%). Twenty-six <strong>of</strong> the 67 chronic ALD were<br />
associated with HIV, chronic HCV, chronic<br />
HBV or combination <strong>of</strong> these. Of the 61 chronic<br />
HCV, 37(60.65%) were HCV mono-infection<br />
and the other 24 (39.35%) chronic HCV were<br />
associated with other risk factors like ALD (7<br />
cases), HIV (13 cases), HBV (3 cases) and<br />
HIV-ALD (1case).<br />
There were 20 cases <strong>of</strong> HCC (15.15%)<br />
amongst the 132 CLD cases. 9 <strong>of</strong> 61(14.75%)<br />
Graph showing risk factors <strong>of</strong> chronic liver<br />
disease and HCC<br />
chronic HCV and 3 <strong>of</strong> 11 (27.27%) chronic<br />
HBV were found to have HCC. 9 HCV<br />
associated HCC were associated with risk<br />
16 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
factors HIV (2 cases), HBV-HIV (1 case) and<br />
chronic alcoholism (6 cases). ALD is the<br />
predominant risk factor in all cases <strong>of</strong> CLD<br />
and HCV is the predominant risk factor<br />
amongst HCC (p = 0.04). Four (4) <strong>of</strong> 67<br />
chronic alcoholic cases (5.97%) were<br />
associated with HCC. The other associated<br />
risk factors with chronic alcoholism were<br />
chronic smoking (46%), multiple sexual<br />
partner (36%), and occasional sexual<br />
exposure (20%).<br />
Discussion: The present study was carried<br />
out in 132 patients with chronic liver disease<br />
who were admitted in medicine ward and those<br />
attending <strong>Medicine</strong> outpatient Department<br />
(OPD) and Radiotherapy OPD <strong>of</strong> Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Lamphelpat<br />
from September 2008 to August 2010.<br />
Out <strong>of</strong> the total 132 patients, 100 (75.75%)<br />
were males and 32 (24.25%) were females,<br />
male to female ratio being 3:1. Khan et al<br />
found similar male:female ratio <strong>of</strong> hepatitis B<br />
and hepatitis C (73:27) in Hazara, Pakistan. 7,8<br />
In a study on precipitating factors <strong>of</strong><br />
encephalopathy in chronic liver disease, Malik<br />
et al found that males comprises 64% cases<br />
<strong>of</strong> CLD. 9 In the analysis <strong>of</strong> patients who died<br />
with cirrhosis by Johnson et.al, 24% patients<br />
had developed hepatocellular carcinoma.<br />
Those patients with HCC showed a striking<br />
male preponderance (11:1). 10 Male dominance<br />
<strong>of</strong> chronic liver disease may be attributable to<br />
more common practice <strong>of</strong> alcohol drinking and<br />
substance abuse among males.<br />
The maximum numbers <strong>of</strong> patients with CLD<br />
with and without HCC were found in the age<br />
group <strong>of</strong> 45-54 years comprising <strong>of</strong> 38<br />
(33.93%) and 6(30%) patients each. This is<br />
more or less in accordance with the findings<br />
<strong>of</strong> Malik SH et al where chronic liver disease<br />
is most common among the age group 40-49<br />
followed by 50-59 years. 9 Bell et al also<br />
reported that age group <strong>of</strong> 45-54 years<br />
comprises maximum patients in their study<br />
<strong>of</strong> epidemiology <strong>of</strong> chronic liver disease in US<br />
population. 11<br />
The most commonly associated risk factor<br />
<strong>for</strong> CLD were ALD (67 cases i.e. 50.75%),<br />
Chronic HCV (61 cases i.e. 46.21%) and HIV<br />
(31 cases i.e. 23.48%). Twenty-six (26) <strong>of</strong> the<br />
67 chronic ALD cases were found to be<br />
associated with HIV, chronic HCV, chronic<br />
HBV or combination <strong>of</strong> these infections thereby<br />
showing that alcohol is one <strong>of</strong> the most<br />
common risk behaviors in the transmission<br />
<strong>of</strong> these infections. The findings <strong>of</strong> the present<br />
study are almost similar to those <strong>of</strong> others<br />
found in the literature. Garcia et al conducted<br />
a retrospective study among veterans in<br />
Puerto Rico and concluded that Alcoholic liver<br />
disease is the principal underlying liver<br />
disease, closely followed by HCV infection<br />
among 114 patients with biopsy proven HCC. 12<br />
Similarly, In France, ethanol is still the leading<br />
cause <strong>of</strong> cirrhosis and was responsible <strong>for</strong><br />
60% <strong>of</strong> all HCC causes during the last<br />
decade. 13<br />
Chronic HCV is the second commonest factor<br />
(46.21%) associated with CLD. Of the 61<br />
chronic HCV, 37(60.65%) were only HCV<br />
infection with various features <strong>of</strong> chronic liver<br />
diseases like cirrhosis and portal hypertension.<br />
The other 24 (39.35%) cases <strong>of</strong> chronic HCV<br />
were associated with other risk factors like<br />
ALD (7 cases), HIV (13 cases) HBV-HIV (3<br />
cases) and HIV-ALD (1case). In a study<br />
conducted on 2,353 newly diagnosed CLD by<br />
Bell et al, Hepatitis C, either alone or in<br />
combination with ALD, accounted <strong>for</strong> twothirds<br />
<strong>of</strong> the cases. Other etiologies included<br />
nonalcoholic fatty liver disease (NAFLD), ALD,<br />
and hepatitis B. 11 In a study conducted by<br />
Laraba et al HCV infection was present in<br />
5.6% <strong>of</strong> patients with Chronic hepatitis and<br />
12.1% <strong>of</strong> patients with Liver cirrhosis. 14 A study<br />
by Lesi et al in Lagos, South-Western Nigeria<br />
found a HCV infection rate <strong>of</strong> 12.2% in patients<br />
with CLD. 15 Furthermore, Shehu in his study<br />
in Jos, North-Central Nigeria found that 11.8%<br />
<strong>of</strong> their patients with CLD had evidence <strong>of</strong><br />
HCV infection. 16 The findings <strong>of</strong> these studies<br />
are much lower than that <strong>of</strong> the present study.<br />
In some countries, more than 10% <strong>of</strong> HCC<br />
cases were coinfected with both HBV and<br />
HCV viruses, thus hampering the attribution<br />
<strong>of</strong> a fraction <strong>of</strong> HCC cases to HBV or HCV. 17<br />
Coinfection with HIV is a frequent occurrence<br />
because <strong>of</strong> shared routes <strong>of</strong> transmission. A<br />
recent study <strong>of</strong> HCC in HIV-HCV coinfected<br />
patients indicated rapid development <strong>of</strong> HCC<br />
in these patients. 18 The combination <strong>of</strong><br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
17
ORIGINAL ARTICLE<br />
associated risk factors like HIV-HCV and HIV-<br />
HBV-HCV over and above alcoholic liver<br />
disease is an unique finding <strong>of</strong> this Northeastern<br />
state <strong>of</strong> India.<br />
There were 20 cases <strong>of</strong> HCC (15.15%)<br />
amongst the 132 CLD cases and 9 <strong>of</strong><br />
61(14.75%) chronic HCV. Out <strong>of</strong> the 20 HCC<br />
cases, 9 were associated with HCV (45%).<br />
Other associated risk factors found in these<br />
9 HCC cases were HIV-HCV (2 cases), HCV-<br />
HBV-HIV (1 case) and HCV cirrhosis with<br />
chronic alcoholic (6 cases). Other studies by<br />
Olubuyide et al in Ibadan, Kirk et al in West<br />
Africa and Kew in his study among blacks in<br />
Southern Africa found HCV infection in<br />
18.7%,19%, 13.2% and 19.5% <strong>of</strong> their<br />
patients with HCC respectively. 19,20,21 These<br />
studies show lower percentage <strong>of</strong> HCV<br />
associated HCC cases than the present<br />
study. However, Chen in his study among<br />
natives in Taiwan, found that 70-80% <strong>of</strong> his<br />
patients with HCC had evidence <strong>of</strong> HCV<br />
infection. 22 Similarly, Tanaka et al found that<br />
78% <strong>of</strong> Japanese patients with HCC had<br />
evidence <strong>of</strong> HCV infection. 23 The higher<br />
prevalence <strong>of</strong> HCV associated HCC (45%) in<br />
the present study may be because <strong>of</strong> high<br />
prevalence <strong>of</strong> IDU and sexually transmitted<br />
HIV which shares similar route <strong>of</strong><br />
transmission.<br />
Three (3) <strong>of</strong> the 11 cases (27.27%) <strong>of</strong> chronic<br />
HBV was found to be associated with HCC.<br />
In a prospective study conducted by Yang HI<br />
et al, the relative risk <strong>of</strong> HCC was 9.6 among<br />
men who were positive <strong>for</strong> HBsAg alone and<br />
60.2 among those who were positive <strong>for</strong> both<br />
HBsAg and HBeAg, as compared with men<br />
who were negative <strong>for</strong> both. 24 In the present<br />
study, 15% <strong>of</strong> the total HCC cases were<br />
associated with chronic HBV which include<br />
both HBeAg positive as well as negative<br />
cases. In Manipur AIDS Control Organisation<br />
report also, HBV coinfection with HIV is much<br />
lower than that <strong>of</strong> HCV though the real cause<br />
is not known so far.<br />
Four (4) <strong>of</strong> 67 chronic alcoholic cases (5.97%)<br />
were associated with HCC. Associated risk<br />
factors with chronic alcoholism were chronic<br />
smoking (46%), multiple sexual partner (36%),<br />
and occasional sexual relational relationship<br />
(20%)<br />
Presence <strong>of</strong> 31(23.48%) cases <strong>of</strong> HIV, HIV-<br />
HCV, HIV-HBV-HCV among 132 cases <strong>of</strong> CLD<br />
shows that there are multiple infections<br />
among CLD with or without HCC which can<br />
be an eye opener <strong>for</strong> the health care workers<br />
and the importance <strong>of</strong> prevention <strong>of</strong> these viral<br />
infections. Thus routine screening <strong>of</strong> HIV, HBV<br />
and HCV are important while managing CLD<br />
cases. The high prevalence <strong>of</strong> HCC amongst<br />
chronic HCV calls <strong>for</strong> the need <strong>of</strong> HCC<br />
screening among chronic HCV patients with<br />
nodular liver.<br />
Conclusion: The present study shows that<br />
the commonest risk factors <strong>for</strong> CLD are<br />
chronic alcoholism, (50.75%) and chronic<br />
HCV (46.21%). There were 20 (15.16%) cases<br />
<strong>of</strong> HCC. The most commonly associated risk<br />
factors <strong>for</strong> HCC are Chronic HCV (45%) with<br />
or without co-infection, chronic alcoholism<br />
(30%), etc.<br />
The limitations <strong>of</strong> the present study are small<br />
sample size, unvailability <strong>of</strong> facilities <strong>for</strong> HBV/<br />
HCV genotyping and viral load and liver biopsy.<br />
A larger study with adequate sample size is<br />
needed to give us more insight about the<br />
clinical pr<strong>of</strong>ile <strong>of</strong> Chronic liver disease with<br />
reference to hepatocellular Carcinoma in<br />
Manipur.<br />
Reference:<br />
1. Yu MH, Chang HC, Liaw YF, Lin SM, Lee<br />
SD, Liu CJ. Familial Risk <strong>of</strong><br />
Hepatocellular Carcinoma among<br />
Chronic Hepatitis B Carriers and Their<br />
Relatives. J natl cancer Inst 2000 Jul 19;<br />
92(14):1159.<br />
2. Sherlock S, Dooley J. Hepatic<br />
transplantation. In: Sherlock S, Dooley<br />
J, editors. Diseases <strong>of</strong> the liver and biliary<br />
system. 11 th ed. London: Blackwell<br />
Science; 2002. p. 657-76.<br />
3. Carr BI. Tumors <strong>of</strong> the biliary tree. In:<br />
Fauci AS, Kasper DL, Longo DL,<br />
Braunwald E, Hauser SL, Jameson JL,<br />
editors. Harrison’s principles <strong>of</strong> internal<br />
medicine. 17 th ed. New York: McGraw<br />
Hill; 2008. p. 581-82.<br />
18 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
4. WHO media centre. Fact sheet N o 164.<br />
WHO Hepatitis C [online]. Revised 2000<br />
Oct [cited 2008]. Available from:<br />
URL:http://www.WHO .int /W HO<br />
Hepatitis C.html.<br />
5. Custer B, Sullivan SD, Hazlet TK, Iloeje<br />
U, Veenstra DL, Kowdley KV. Chronic<br />
hepatitis B from a Global perspective:<br />
Epidemiology and costs <strong>of</strong> illness. J clin<br />
Gastroenterol 2004 Nov/ Dec; 38(10)<br />
supplement 3:158-68.<br />
6. Knott SB. WHO media centre. Global HIV<br />
prevalence has leveled <strong>of</strong>f [Online]. 2007<br />
[cited 2008 Apr]. Available from:<br />
URL:http://www.unaids.org/.<br />
7. Khan TS, Rizvi FJ: Hepatitis B<br />
seropositivity among chronic liver<br />
disease patients in Hazara division<br />
Pakistan. J Ayub Med Coll Abbottabad<br />
2003 , 15:54-55.<br />
8. Khan T, Rizvi F, Rashid A. Hepatitis C<br />
seroposivity among chronic liver disease<br />
patients in hazera, Pakistan. J Ayub Med<br />
Coll Abbottabad 2003; 15 (2): 53-5.<br />
9. Malik SH, Suliman MI. Chronic liver<br />
disease: precipitating factors <strong>for</strong><br />
encephalopathy. The pr<strong>of</strong>essional 2004<br />
Oct-Dec; 2(4):446-50.<br />
10. Johnson PJ, Krasner N, Portmann B,<br />
Eddleston ALWF, Williams R.<br />
Hepatocellular carcinoma in Great<br />
Britain: influence <strong>of</strong> age, sex, HBsAg<br />
status, and aetiology <strong>of</strong> underlying<br />
cirrhosis. Gut 1978 Jun; 19:1022-26.<br />
11. Bell BP, Manos MM, Zaman A, Terrault N,<br />
Thomas A, Navarro VJ et al. The<br />
epidemiology <strong>of</strong> newly diagnosed<br />
chronic liver disease in gastroenterology<br />
practices in the United States: results<br />
from population-<strong>based</strong> surveillance. Am<br />
J Gastroenterol. 2008 Nov;103(11):2727-<br />
36.<br />
12. Garcia LLJ, Toro DH, Mayol H, Souss MJ,<br />
Dueno MI, Perez RP. Hepatocellular<br />
carcinoma: ten years experience among<br />
veterans in Puerti Rico. P R Health Sci J<br />
2007 Jun; 26(2):103-07.<br />
13. Michielson PP, Francque SM and<br />
Dongen JLV. Viral hepatitis and<br />
hepatocellular carcinoma. World J Surg<br />
Oncology 2005; 3:27<br />
14. Laraba A, Wadzali G, Sunday B,<br />
Abdulfatai O, Fatai S. Hepatitis C Virus<br />
Infection In Nigerians With Chronic Liver<br />
Disease. The Internet <strong>Journal</strong> <strong>of</strong><br />
Gastroenterology 2010; 9(1).<br />
15. Lesi OA, Kehinde MO, Anomneze EE,<br />
Wali SS. Hepatitis C infection and risk <strong>of</strong><br />
chronic liver disease in Lagos. Nig Q J<br />
Hosp Med 2002;12(1):1-4.<br />
16. Shehu MY. Prevalence <strong>of</strong> hepatitis C virus<br />
antibodies among patients with chronic<br />
liver disease at the Jos University<br />
Teaching Hospital. A dissertation<br />
submitted to the West African College<br />
<strong>of</strong> Physicians in partial fulfillment <strong>of</strong> the<br />
requirements <strong>for</strong> the award <strong>of</strong> Fellowship<br />
<strong>of</strong> the college, 2002.<br />
17. Raza SA, Clif<strong>for</strong>d GM, Francesch S.<br />
Worldwide variation in the relative<br />
importance <strong>of</strong> hepatitis B and hepatitis<br />
C viruses in hepatocellular carcinoma:<br />
a systematic review. Br J Cancer (2007)<br />
96, 1127–34.<br />
18. Michielsen PP, Francque SM and<br />
Dongen JLV. Viral hepatitis and<br />
hepatocellular carcinoma. World J Surg<br />
Oncology 2005; 3:27.<br />
19. Olubuyide IO, Aliyu B, Olaleye OA, Ola<br />
SO, Olawuyi F, Malabu UH et al. Hepatitis<br />
B and C virus and Hepatocellular<br />
carcinoma. Trans R Soc Trop Med Hyg<br />
1997;91(1): 38-41.<br />
20. Kirk GD, Lesi OA, Mendy M, Akano AO,<br />
Sam O, Geodert JJ et al. The Gambia<br />
Liver Cancer Study: infection with<br />
hepatitis B and C and the risk <strong>of</strong><br />
Hepatocellular carcinoma in West Africa.<br />
Hepatology 2004;39(1):211-219.<br />
21. Kew MC. Hepatitis C virus infection in<br />
black patients with Hepatocellular<br />
carcinoma in Southern Africa. Princess<br />
Takamatsu Symp 1995;25:33-40.<br />
22. Chen DS. Hepatitis C virus infection in<br />
chronic liver disease and Hepatocellular<br />
carcinoma in Taiwan. Princess<br />
Takamatsu Symp 1995; 25:27-32.<br />
23. Tanaka K, Ikematsu H, Hirohata T,<br />
Kashiwagi S. Hepatitis C virus infection<br />
and risk <strong>of</strong> Hepatocelluar carcinoma<br />
among Japanese: possible role <strong>of</strong> type<br />
1b(II) infection. J Natl Cancer Inst 1996;<br />
88(11): 742-746.<br />
24. Yang HI, Lu SN, Liaw YF, et al. Hepatitis<br />
B e antigen and the risk <strong>of</strong> hepatocellular<br />
carcinoma. N Engl J Med 2002; 347:168.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
19
ORIGINAL ARTICLE<br />
An insight on HIV-1 discordant couples-A RIMS study<br />
1<br />
K. Felix Jebasingh, 2 Robinson Ningshen, 3 Th. Shanti Devi, 2 N. Biplab Singh , 4 S. Bhagyabati Devi,<br />
Abstract:<br />
Objective: To discuss the characteristics <strong>of</strong><br />
the patients with Human Immunodeficiency<br />
Virus-1(HIV-1) infection, who has discordant<br />
partners and the postulated mechanism <strong>for</strong><br />
their persistent HIV seronegativity from various<br />
literatures. Methods: We retrospectively<br />
analyzed HIV-1 discordant infected partners<br />
who were admitted in <strong>Medicine</strong> ward, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences (RIMS), Imphal,<br />
Manipur from 2005 to 2010. Results: Out <strong>of</strong><br />
the 25 infected patients with negative partners<br />
22 were male and 3 were female. 3 patients<br />
were <strong>of</strong> HIV WHO stage III and others were <strong>of</strong><br />
stage IV. The mean CD4 count <strong>of</strong> our patients<br />
is 119. 84% <strong>of</strong> the patients had infection<br />
through IDU. Only 4 patients had infection<br />
through heterosexual behavior. Conclusion:<br />
This retrospective study is to highlight that<br />
discordant partners do exist in our population.<br />
Through proper counseling and by advising<br />
safe sex, we can prevent HIV transmission to<br />
the non infected partners.<br />
Keywords: HIV; IDU-Intravenous Drug User;<br />
Discordant couples; CD4 count.<br />
Introduction: India is one <strong>of</strong> the hubs <strong>of</strong> HIV<br />
infection in this modernized world. HIV<br />
1. P.G. Student , 2. Associate Pr<strong>of</strong>essor, 3. Senior<br />
Resident, 4. Pr<strong>of</strong>essor, RIMS, Imphal, Manipur.<br />
Corresponding author:<br />
Dr.Robinson Ningshen, MBBS., MD (General<br />
<strong>Medicine</strong>), Associate Pr<strong>of</strong>essor, Department <strong>of</strong><br />
<strong>Medicine</strong>, Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences,<br />
Imphal, Manipur. Phone No: 9612159017. E-Mail:<br />
dr.ningshen@yahoo.co.in<br />
infection is predominantly a sexually<br />
transmitted disease worldwide .The most<br />
common mode <strong>of</strong> infection, particularly in<br />
developing countries, is heterosexual<br />
transmission 1 . According to NACO, in 2008<br />
there are about 2.27 million people between<br />
15 and 49 years <strong>of</strong> age, affected by HIV<br />
infection in India. Compared to the African<br />
countries the number <strong>of</strong> HIV infected is less.<br />
The major route <strong>of</strong> transmission is different in<br />
different parts <strong>of</strong> India. In India states like<br />
Andhra Pradesh, Karnataka, Maharashtra,<br />
Manipur, Nagaland and Tamil Nadu have high<br />
HIV prevalence than the National prevalence.<br />
Manipur has the highest prevalence <strong>of</strong> HIV<br />
infection in the country. In 2008, the adult<br />
prevalence <strong>of</strong> HIV infection in India is 0.29%<br />
.This figure is much less, as compared to<br />
2002 which was 0.45%. Manipur with a<br />
population <strong>of</strong> 0.2 percentage <strong>of</strong> total Indian<br />
population has 8 percent <strong>of</strong> the total HIV<br />
infected people in India. As per the 2008 report<br />
the overall HIV prevalence among different<br />
High Risk Groups were Intravenous Drug<br />
Users- IDU (9.2%), Male having Sex with Male<br />
-MSM (7.3%), Female Sex workers-FSW<br />
(4.9%) and STD clinic attendees (2.5%) .Low<br />
prevalence is seen among ANC clinic<br />
attendees (0.49%). Heterosexual behavior is<br />
the main route <strong>of</strong> transmission (87.1%) as per<br />
NACO 2008. But IDU is the main mode <strong>of</strong><br />
transmission in North Eastern parts <strong>of</strong> India 2 .<br />
The prevalence <strong>of</strong> HIV infection among the IDU<br />
was 17.9%, FSW was 13% and MSM in<br />
Manipur was 16.4% in 2007 3 . We<br />
retrospectively studied the case files <strong>of</strong> HIV<br />
20 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
discordant couples, admitted in the <strong>Medicine</strong><br />
Department, Regional Institute <strong>of</strong> <strong>Medical</strong><br />
sciences (RIMS), Imphal. Our aim is to<br />
discuss the characteristic features and the<br />
possible postulated mechanism behind the<br />
discordance from the available literatures.<br />
Materials and Methods: This is a<br />
retrospective study <strong>of</strong> HIV-1 infected patients<br />
who have discordant partners, who were<br />
admitted under <strong>Medicine</strong> Department,<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences (RIMS),<br />
Imphal from 2005 to 2010. HIV patients were<br />
diagnosed as per the NACO guidelines. The<br />
patients were all legally married and living<br />
together <strong>for</strong> not less than 2 years and the HIV-<br />
1 seropositive status was known be<strong>for</strong>e the<br />
marriage and were practicing unsafe sex and<br />
had multiple issues. Seronegative partners<br />
were repeatedly negative <strong>for</strong> HIV antibody,<br />
tested every 3 months.<br />
Results: 25 HIV-1 infected patients, who had<br />
discordant partners, were admitted in<br />
<strong>Medicine</strong> Department, RIMS, Imphal. Out <strong>of</strong><br />
25 patients, 22 were male and 3 were female.<br />
The infected male: infected female ratio was<br />
7.3:1. The mean CD4 count was 119. The<br />
mean age <strong>of</strong> our patients was 39.9 years. At<br />
presentation all the patients had at least one<br />
Acquired Immune Deficiency Syndrome<br />
(AIDS) defining opportunistic infection.84 %<br />
were IDU’s and remaining 16 % were<br />
heterosexuals. Of the 22 males, only one<br />
patient was a heterosexual and the remaining<br />
were IDU’s. The patients with IDU habits were<br />
addicted to illicit drugs <strong>for</strong> a period <strong>of</strong> more<br />
than 15-16 years. All the 3 females who had<br />
discordant husbands got infected through<br />
heterosexual behavior. Their children were<br />
negative <strong>for</strong> HIV infection. Out <strong>of</strong> 25 patients<br />
one patient had Hepatitis and other had<br />
Hepatitis C co-infection. Of the 25 patients 14<br />
had Koch’s infection, 3 had pneumocystis<br />
carinii pneumonia (PCP) or pneumocystis<br />
jiroveci pneumonia, 3 had cryptococcal<br />
meningitis, 2 had cerebral toxoplasmosis, 1<br />
had disseminated candidiasis, 1 had chronic<br />
intestinal isosporiasis, as opportunistic<br />
infections and 1 had Progressive multifocal<br />
leukoencephalopathy (PML) (Table-1).3<br />
patients were <strong>of</strong> stage 3 HIV WHO staging<br />
and remaining were <strong>of</strong> stage 4 4 . Because <strong>of</strong><br />
the non-availability <strong>of</strong> the viral load estimation<br />
<strong>for</strong> HIV -1, none <strong>of</strong> our patients had viral load<br />
estimation done. It is well defined that low<br />
CD4+ counts are associated with high levels<br />
<strong>of</strong> plasma viremia 1 . Since the CD4 count <strong>of</strong><br />
all our patients was low and <strong>of</strong> WHO stage III/<br />
IV infection at presentation, their viral loads<br />
were presumed to be high. All the patients<br />
were on antiretroviral therapy (ART) and were<br />
advised to practice safe sex.<br />
Table: 1. Characteristics <strong>of</strong> the HIV Infected Partners<br />
PCP-Pneumocystis carinii, IDU-Intravenous Drug User.<br />
PML- Progressive multifocal leukoencephalopathy.<br />
Discussion: Humans demonstrate significant<br />
variability in their susceptibility to Human<br />
Immunodeficiency Virus type 1 (HIV-1)<br />
infection. There are three groups <strong>of</strong> people,<br />
one with infection and disease manifestation,<br />
second who are persistently seronegative<br />
even after unprotected sexual behavior and<br />
third , though HIV infected but without the<br />
disease progression. Such variable HIV<br />
infective patterns have indicated that natural<br />
resistance to HIV-1 infection might be the<br />
reason behind 5 .<br />
In Pune, a prospective study was conducted<br />
to study the pr<strong>of</strong>ile <strong>of</strong> HIV discordant couples<br />
and the secondary transmission rate. The<br />
study conducted from September 2002 <strong>for</strong> a<br />
period <strong>of</strong> 26 months found 457 discordant<br />
couples 6 .Kumarasamy et al did a cross<br />
sectional study to compare the clinical and<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
21
ORIGINAL ARTICLE<br />
behavioral characteristics <strong>of</strong> HIV-infected<br />
South Indian patients in concordant and<br />
discordant heterosexual relationships. 839<br />
concordant patients were compared with 996<br />
discordant patients in his study. Concordant<br />
patients had significantly higher CD4 cell<br />
counts than discordant patients at the time <strong>of</strong><br />
enrolling to care. Their study concluded that<br />
couple-<strong>based</strong> interventions in addition to<br />
proper provision <strong>for</strong> HAART will decrease the<br />
HIV transmission among discordant South<br />
Indian married couples. 7<br />
A study from Canada has postulated that a<br />
cumulative effect due to cellular immunity, viral<br />
characteristics, and co receptor integrity could<br />
be the reason behind the seronegativity results<br />
after studying 11 discordant couples. There<br />
is no single reason behind the resistance to<br />
HIV infection 8 . Immunoglobulin A (IgA)<br />
responses found in the cervico-vaginal fluids<br />
<strong>of</strong> sex workers in Thailand as well as in other<br />
discordant groups, suggests that local<br />
mucosal immune responses might be the<br />
reason behind the persistent seronegativity . It<br />
has been studied that purified IgA from HIV<br />
resistant sex workers have a neutralizing effect<br />
towards HIV isolates from different clades and<br />
inhibit HIV infection <strong>of</strong> susceptible cells in vitro.<br />
This provides further evidence that IgA may<br />
be an important part <strong>of</strong> the immune defense<br />
against HIV 9, 10 . In literature there is evidence<br />
<strong>of</strong> elevated levels <strong>of</strong> IgA, IgG and IgM which<br />
are believed to suppress HIV, in the<br />
cervicovaginal secretions <strong>of</strong> a cohort <strong>of</strong> HIVseronegative<br />
African sex workers, suggesting<br />
that the immune response may not be limited<br />
to just IgA (Belec et al.) 11 .<br />
It is postulated that cytotoxic T-lymphocytes<br />
(CTLs) might have a role in resistance to HIV<br />
infection although the resistance is believed<br />
to be dependent on persistent exposure to<br />
HIV. 12 This type <strong>of</strong> responses have been<br />
found in babies born to infected mothers,<br />
regular sexual partners <strong>of</strong> HIV-infected<br />
individuals, and sex workers with high levels<br />
<strong>of</strong> exposure to HIV. 13 Rowland-Jones et al in<br />
their work on sex workers in Nairobi who were<br />
HIV seronegative had discovered CTL<br />
responses targeting epitopes defined by HIV<br />
clade B. 14 A study in HIV seronegative Kenyan<br />
sex workers, found that HIV-specific CD8+ T<br />
cells in the genital mucosa <strong>of</strong> the sex workers,<br />
suggesting that CTL responses were<br />
protective against heterosexual transmission<br />
<strong>of</strong> HIV infection (Kaul et al). 15 Another study<br />
by the same author among a cohort <strong>of</strong><br />
exposed-uninfected Kenyan sex workers, a<br />
subset who seroconvert <strong>for</strong> HIV infection were<br />
found to have had lapses in sex work. This<br />
apparent interruption in HIV exposure might<br />
have lead to loss <strong>of</strong> HIV-specific CD8+<br />
responses, suggesting that constant or<br />
frequent exposure to HIV is needed to<br />
maintain a protective CTL response. 16<br />
A study among the Chinese males had shown<br />
that 30% <strong>of</strong> the persistently negative<br />
individuals have HIV-1 specific T cell immune<br />
responses. 17 Though various studies explains<br />
the evidence <strong>for</strong> CTL involvement in resistance<br />
to HIV infection there is no conclusive<br />
evidence, leaving the possibility that CTLs are<br />
surrogate markers <strong>of</strong> some other<br />
mechanism. Thomas et al in their study have<br />
confirmed the reduced expression <strong>of</strong> CCR5<br />
in HIV-1 resistance. This reduced expression<br />
<strong>of</strong> CCR5 could be the reason <strong>for</strong> the<br />
seronegativity. 18 A study among high risk<br />
individuals <strong>of</strong> Indian origin had concluded that<br />
single nucleotide polymorphism (SNP) in<br />
Stromal Derived factor (SDF-1); a ligand <strong>for</strong><br />
CXCR4 could be a protective factor towards<br />
HIV infection. 19, 20 Another study by Sangok et<br />
al showed a high expression <strong>of</strong> CD26/DPPIV<br />
enzymes in exposed seronegative individuals.<br />
This opens a new dimension <strong>of</strong> CD26/DPPIV<br />
in protection against HIV infection in vivo. 21<br />
DPPIV enzymes are the enzymes which are<br />
implicated in the carbohydrate metabolism.<br />
Stan<strong>for</strong>d et al in their study had observed a<br />
strong non-cytotoxic CD81-cell anti-HIV<br />
response in discordant persons suggesting<br />
that this might be a contributing factor <strong>for</strong> the<br />
reason towards the persistent negativity<br />
Though various postulates have been given<br />
<strong>for</strong> the persistent seronegativity or HIV<br />
resistance /susceptibility, we could not<br />
evaluate the reason <strong>for</strong> the discordance in our<br />
patients due to lack <strong>of</strong> resources. An insight<br />
towards the resistance or susceptibility to HIV-<br />
1 infection is important in the context <strong>of</strong> future<br />
treatment modalities and research towards<br />
22 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
the HIV vaccine. Counseling regarding the<br />
safe sex is a challenge <strong>for</strong> the treating<br />
physician in discordant couples.<br />
Conclusion: Through our study we would like<br />
to highlight that HIV discordance among<br />
couples is prevalent in our population. Though<br />
research had been done in high risk Indian<br />
population who are seronegative, we could<br />
not find any study <strong>for</strong> the discordant or<br />
persistent negativity <strong>for</strong> HIV-1 infection in the<br />
discordant partners in India. Though we have<br />
25 discordant couples the reason could not<br />
be evaluated due to non-availability <strong>of</strong><br />
resources. Such couples should be advised<br />
to practice safe sex and should be given<br />
proper counseling. This kind <strong>of</strong> study will be a<br />
boost <strong>for</strong> HIV vaccine research in future.<br />
References:<br />
1) Fauci AS, Lane C.Human<br />
Immunodeficiency Virus Disease: AIDS and<br />
related Disorders. In: Fauci AS, Kasper<br />
DL, Longo DL, et al, eds. Harrison’s<br />
Principles <strong>of</strong> Internal <strong>Medicine</strong>. 17th ed.<br />
New York: McGraw-Hill, 2008: 1137-1204.<br />
2) NACO (2008) UNGASS Country Progress<br />
Report 2008 India.<br />
3) Annual Report NACO India 2008-09.<br />
4) NACO 2008 .Guidelines <strong>for</strong> prevention and<br />
management <strong>of</strong> common opportunistic<br />
inf ections/malignancies among HIVinfected<br />
adult and adolescent.India.<br />
5) Marmor M, Hertzmark K, Thomas SM, et<br />
al. Resistance to HIV infection. J Urban<br />
Health. 2006 Jan;83(1):5-17.<br />
6) Mehendale SM, Ghate MV, Kishore Kumar<br />
B, et al. Low HIV-1 incidence among<br />
married serodiscordant couples in Pune,<br />
India. J Acquir Immune Defic Syndr. 2006<br />
Mar;41(3):371-3.<br />
7) Kumarasamy N, Venkatesh KK, Srikrishnan<br />
AK, et al .Risk factors <strong>for</strong> HIV transmission<br />
among heterosexual discordant couples in<br />
South India. HIV Med. 2010 Mar;11(3):178-<br />
86. Epub 2009 Sep 24.<br />
8) Bienzle D, MacDonald KS, Smaill FM, et al<br />
.Factors contributing to the lack <strong>of</strong> human<br />
immunodeficiency virus type 1 (HIV-1)<br />
transmission in HIV-1-discordant partners.<br />
J Infect Dis. 2000 Jul;182(1):123-32. Epub<br />
2000 Jun 29.<br />
9) Beyrer C, Artenstein AW, Rugpao S, et al.<br />
Epidemiologiv and biologic<br />
characterization <strong>of</strong> a cohort <strong>of</strong> human<br />
immunodeficiency virus type 1 highly<br />
exposed persistently seronegative female<br />
sex workers in Northern Thailand. J Infect<br />
Dis. 1999;179:59–67.<br />
10) Broliden K, Hinkula J, Devito C, et al.<br />
Functional HIV-1 specific IgA antibodies in<br />
HIV-1exposed, persistently IgG<br />
seronegative female sex workers. Immunol<br />
Lett. 2001;79:29–36.<br />
11) Belec L, Ghys PD, Hocini H, et al.<br />
Cervicovaginal secretory antibodies to<br />
human immunodeficiency virus type 1 (HIV-<br />
1) that block viral transcytosis through tight<br />
epithelial barriers in highly exposed HIV-<br />
1-seronegative African women. J Infect<br />
Dis.2001;184(11):1412–1422.<br />
12) Kaul R, Rowland-Jones SL, Kimani J, et<br />
al. New insights into HIV-1 specific cytotoxic<br />
T lymphocyte responses in exposed,<br />
persistently seronegative Kenyan sex<br />
workers. Immunol Lett. 2001;79(1–2):3–13.<br />
13) Rowland-Jones SL, Pinheiro S, Kaul R, et<br />
al. How important is the Fquality_ <strong>of</strong> the<br />
cytotoxic T lymphocyte (CTL) response in<br />
protection against HIV infection? Immunol<br />
Lett. 2001;79:15–20.<br />
14) Rowland-Jones S, Dong T, Fowke KR, et<br />
al. Cytotoxic T cell responses to multiple<br />
conserved HIV epitopes in HIV-resistant<br />
prostitutes in Nairobi. J Clin<br />
Invest.1998;102(9):1758–1765.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
23
ORIGINAL ARTICLE<br />
15) Kaul R, Plummer FA, Kimani J, et al. HIV-<br />
1-specif ic mucosal CD8+ lymphocyte<br />
responses in the cervix <strong>of</strong> HIV-1-resistant<br />
prostitutes in Nairobi. J<br />
Immunol.2000;164(3):1602–1611.<br />
16) Kaul R, Rowland-Jones SL, Kimani J, et<br />
al. Late seroconversion in HIV-resistant<br />
Nairobi prostitutes despite pre-existing<br />
HIV-specific CD8+ responses.[comment].<br />
J Clin Invest.2001;107(3):341–349.<br />
17) Liu HW, Hong KX, Ma J, et al. Identification<br />
<strong>of</strong> HIV-1 specific T lymphocyte responses<br />
in highly exposed persistently<br />
seronegative Chinese. Chin Med J (Engl).<br />
2006 Oct 5;119(19):1616-21.<br />
18) Thomas SM, Tse DB, Ketner DS, et al.<br />
CCR5 expression and duration <strong>of</strong> high risk<br />
sexual activity among HIV-seronegative<br />
men who have sex with men. AIDS. 2006<br />
Sep 11;20(14):1879-83.<br />
19) Chaudhary O, Rajsekar K, Ahmed I,et<br />
al.Polymorphic variants in DC-SIGN, DC-<br />
SIGNR and SDF-1 in high risk seronegative<br />
and HIV-1 patients in Northern Asian<br />
Indians. J Clin Virol. 2008 Oct;43(2):196-<br />
201.<br />
20) Michael NL.Genetic Restriction <strong>of</strong> AIDS<br />
Pathogenesis by an SDF-1 Chemokine<br />
Gene Variant. JAMA 1998:279;389-393.<br />
21) Songok EM, Osero B, McKinnon L, et al<br />
.CD26/dipeptidyl peptidase IV (CD26/<br />
DPPIV) is highly expressed in peripheral<br />
blood <strong>of</strong> HIV-1 exposed uninfected female<br />
sex workers. Virol J. 2010 Nov 25;7:343.<br />
24 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Preloading versus prophylactic intravenous ephedrine in the prevention <strong>of</strong> hypotension<br />
following subarachnoid block in patients undergoing caesarean section<br />
1<br />
N. Anita Devi 2 L. Chaoba Singh 3 Pr<strong>of</strong>. L. Kameshwar Singh, 1 Th. Rupendra, 2 L. Eshori<br />
Abstract<br />
Objective: The primary objective <strong>of</strong> this study<br />
was to compare the efficacy <strong>of</strong> preloading with<br />
ringer lactate and prophylactic intravenous<br />
ephedrine in prevention <strong>of</strong> hypotension<br />
following subarachnoid block in patients<br />
undergoing caesarean section. Methods:<br />
One hundred parturient <strong>of</strong> ASA I &II undergoing<br />
caesarean section in RIMS hospital during the<br />
period <strong>of</strong> 2006- 2008 were enrolled <strong>for</strong> the<br />
study. They were randomly divided into two<br />
groups <strong>of</strong> fifty each.<br />
Group I (preloading) – patients were preloaded<br />
with ringer lactate at the dose <strong>of</strong> 20ml/kg, 30<br />
mins be<strong>for</strong>e the spinal anaesthesia<br />
Group II (ephedrine) – patients were given inj<br />
ephedrine 10 mg intravenously just be<strong>for</strong>e the<br />
induction <strong>of</strong> spinal anaesthesia .<br />
Heart rate, systolic blood pressure , peripheral<br />
oxygen saturation were recorded at baseline<br />
and thereafter every 2min interval <strong>for</strong> the first<br />
10min and than at every 5min till the end <strong>of</strong><br />
the study. Results: Preloading with ringer<br />
lactate did not absolutely prevent hypotension<br />
and the incidence <strong>of</strong> hypotension was 44% in<br />
the preloading group and 32% in the<br />
ephedrine group. This finding was not<br />
significant statistically between the groups.<br />
Conclusion: Preloading with crystalloid<br />
administration was a safe procedure, its<br />
1. Assistant Pr<strong>of</strong>essor 2. Registar. 3. Pr<strong>of</strong>. and<br />
Head. Dept. <strong>of</strong> Anaesthesia RIMS<br />
Address <strong>for</strong> correspondence<br />
Pr<strong>of</strong>. L. Kameshwar Singh, Pr<strong>of</strong>. & Head, Dept. <strong>of</strong><br />
Anaesthesiology RIMS Imphal.<br />
effectiveness in preventing hypotension in<br />
parturient undergoing caesarean section<br />
under spinal anaesthesia was questionable.<br />
And at the same time prophylactic ephedrine<br />
had limited efficiency <strong>for</strong> the prevention <strong>of</strong><br />
hypotension.<br />
Key words: Hypotension, preloading,<br />
ephedrine, spinal anaesthesia<br />
Introduction: Spinal anesthesia is commonly<br />
used <strong>for</strong> caeserian section as it has got rapid<br />
onset, pr<strong>of</strong>ound sensory and motor blockade<br />
and avoidance <strong>of</strong> side effects <strong>of</strong> general<br />
anaesthesia. But hypotesion complicates<br />
spinal anaesthesia in about 80% <strong>of</strong> the<br />
parturient and if left untreated it produces<br />
foetal acidosis and a poor neonatal outcome.<br />
Hypotension is universally treated with<br />
preloading with either crystalloid like ringer<br />
lactated at a dose <strong>of</strong> 10-30ml/kg body weight<br />
be<strong>for</strong>e induction <strong>of</strong> spinal anaesthesia or with<br />
colloids like gelatine and starch. However rapid<br />
infusion <strong>of</strong> fluid causes pulmonary oedema in<br />
patients with heart diseases, hypothermia or<br />
dilutional coagulopathy 1, 2 . There is increase<br />
used <strong>of</strong> vasopressors 3,4 like ephedrine,<br />
phenylephrine with no preloading or minimal<br />
loading. Of the available vasopressors,<br />
ephedrine is most commonly used. IM<br />
ephedrine has been described, but its efficacy<br />
has been inconsistent 5,6 , and its use may be<br />
associated with unacceptable hypertension,<br />
particularly if spinal anesthesia is<br />
unsuccessful 7 . As an alternative, IV ephedrine<br />
given immediately after the induction <strong>of</strong> spinal<br />
anesthesia has been described 8,9 .The present<br />
study was conducted to compare the<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
25
ORIGINAL ARTICLE<br />
effectiveness <strong>of</strong> preloading with ringer lactate<br />
to the vasopressor ephedrine in the<br />
management <strong>of</strong> parturient undergoing<br />
caesarean section under spinal anaesthesia.<br />
Material and method: After obtaining written<br />
in<strong>for</strong>med consent and approval <strong>of</strong> the institute<br />
ethical committee, one hundred (100)<br />
parturient <strong>of</strong> ASA I and II undergoing caesarean<br />
section under spinal anaesthesia were<br />
enrolled <strong>for</strong> the study. Patients with<br />
cardiovascular or respiratory disorders,<br />
abnormal cardiac anatomy, hypertension, preeclampsia,<br />
diabetes, electrolyte imbalance,<br />
patients with haemoglobin concentration less<br />
than 10 gm%, weight more than 80 kg, fasting<br />
<strong>for</strong> less than 6 hours and those on medication<br />
which have direct cardiac effects such as beta<br />
blockers were excluded from the study. All the<br />
patients were premedicated with inj ranitidine<br />
50mg and ondensetron 4mg intravenously 45<br />
min be<strong>for</strong>e induction <strong>of</strong> spinal anaesthesia .<br />
Patients were randomly divided into two<br />
groups<br />
Group A- patients were preloaded with ringer<br />
lactate at the dose <strong>of</strong> 20ml/kg body weight 30<br />
min be<strong>for</strong>e spinal anaesthesia<br />
Group B– patients were given inj ephedrine<br />
10mg intravenously just be<strong>for</strong>e the induction<br />
<strong>of</strong> spinal anaesthesia<br />
Spinal anaesthesia was given in L34 space<br />
with 25G spinal needle with 2.2 ml <strong>of</strong> 0.5% inj<br />
bupivacaine in left lateral position. A wedge<br />
was placed under the right hip <strong>for</strong> left uterine<br />
displacement in patients undergoing<br />
caesarean section. Supplemental oxygen 2<br />
Lmin-1 was given through face mask. The<br />
level <strong>of</strong> loss to pinprick sensation was<br />
assessed and surgery was started when<br />
sensory loss <strong>of</strong> T6 was achieved. Heart rate,<br />
mean arterial pressure, peripheral oxygen<br />
saturation were recorded just be<strong>for</strong>e induction<br />
<strong>of</strong> spinal anaesthesia and thereafter every 2<br />
mins interval <strong>for</strong> the first 10 mins and than at<br />
every 5mins till the end <strong>of</strong> surgery.<br />
Hypotension was defined as a decrease <strong>of</strong><br />
systolic blood pressure more than 30% <strong>of</strong> the<br />
baseline or less than 90 mmHg. During an<br />
episode <strong>of</strong> hypotension Inj ephedrine 5mg iv<br />
was given. The data were collected and<br />
analyzed.<br />
Results and observations<br />
Patient Characteristics : Mean age in years<br />
<strong>of</strong> the patients in ephedrine group and<br />
preloading group were 28.50± 2.72 and 28.76<br />
± 2.52 respectively. The weight ranges from<br />
66.50 ± 30 kg in ephedrine group to 66.40 ±<br />
3.20 kg in preloading group. The variation in<br />
age and weight between the two groups were<br />
statistically not significant.<br />
Figure I: The mean systolic blood pressure<br />
The mean systolic blood pressure between<br />
the groups was shown in figure I. There was<br />
a significant fall in the mean systolic blood<br />
pressure throughout the study period in both<br />
the groups, compared to the baseline values.<br />
In preloading group significant decrease was<br />
seen during 10 and 15 minutes <strong>of</strong> the study.<br />
Table 1: The incidence <strong>of</strong> hypotension<br />
Groups No <strong>of</strong> patients X 2 Df P- value<br />
with hypotension<br />
Ephedrine 16 (32%) 1.528 1 0.216<br />
Preloading 22 (44%)<br />
Table I showed the incidence <strong>of</strong> hypotension<br />
in the two groups. Hypotension was observed<br />
in 16 (32%) patients in ephedrine group and<br />
22 (44%) patients in preloading group. These<br />
finding was statistically insignificant with p<br />
value <strong>of</strong> 0.216.<br />
26 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Figure 2: The mean heart rate<br />
The mean heart rate was more in the preloading<br />
group than the ephidrine group in every stage<br />
<strong>of</strong> the time period <strong>of</strong> the study as shown in Fig.<br />
2. This difference was statistically significant<br />
with p value <strong>of</strong> less than 0.5.<br />
Discussion: Rapid administration <strong>of</strong><br />
crystalloid solutions to correct hypotension<br />
was first advocated by Greiss and Crandell in<br />
1965 but they showed that intravenous fluid<br />
only partly restored uterine blood flow in gravid<br />
uterus rendered hypotension by spinal<br />
anaesthesia and at the same time Jackson R<br />
et al 1 also concluded that volume preloading<br />
was not essential to prevent spinal induced<br />
hypotension in caesarean section. Large<br />
volume <strong>of</strong> fluid also decrease decreses<br />
oxygen carrying capacity and also increase<br />
the risk <strong>of</strong> pulmonary oedema in susceptible<br />
patients.<br />
Vasopressors such as ephedrine maintains<br />
the systemic vascular resistance. They<br />
reduces the need <strong>for</strong> an increase in cardiac<br />
output and directly reverses the physiological<br />
<strong>change</strong>s produced by the block.<br />
In the present study incidence <strong>of</strong> hypotension<br />
in the preloading group was 44% and 32%<strong>of</strong><br />
the patients in the ephedrine group . The<br />
decrease in blood pressure was rapid in the<br />
first 10 min and thereafter it was gradual in<br />
the prealoding group whereas it was more<br />
gradual in the ephedrine group. Our findings<br />
were in aggrement with Rout CC et al 10 where<br />
they found hypotension in 43% <strong>of</strong> the patients<br />
in preloading group and 44% <strong>of</strong> the patients in<br />
the nonloading group. In our study, patients<br />
were given “rescue” ephedrine as soon as<br />
hypotension occurred, and the total dose <strong>of</strong><br />
ephedrine given was similar among groups.<br />
Because this caused the blood pressure in<br />
hypotensive patients to return toward baseline,<br />
it is a confounding factor in the repeated<br />
measures analysis, with the tendency to<br />
reduce the likelihood <strong>of</strong> finding a difference<br />
between doses. This explains the<br />
convergence <strong>of</strong> systolic blood pressure<br />
measurements in the latter part <strong>of</strong> the<br />
recording period.<br />
Our finding <strong>of</strong> hypotension in 32% <strong>of</strong> the<br />
patients in ephedrine group was different from<br />
Marcel PV et al 11 where they found<br />
hypotension in 25%<strong>of</strong> the patients. These<br />
difference might be because <strong>of</strong> prehydration<br />
with 1000ml <strong>of</strong> crystalloids in all their cases<br />
and used <strong>of</strong> small-dose (bupivacaine 6.6mg)<br />
spinal anesthesia <strong>for</strong> cesarean delivery in their<br />
study.<br />
In our study we did not encounter any case <strong>of</strong><br />
reactive hypertension which was different<br />
from Ngan Kee WD 12 . We used 10mg<br />
intravenous ephedrine .They found that<br />
incidence <strong>of</strong> hypotension was reduced to 35%<br />
in the patients who received ephedrine 30 mg<br />
compared with the control rate <strong>of</strong> 95%, this<br />
was at the expense <strong>of</strong> an increased incidence<br />
<strong>of</strong> hypertension, which occurred in 45% <strong>of</strong> the<br />
patients. They suggested that 30-mg<br />
intravenous ephedrine may not be suitable in<br />
some patients such as those with<br />
cardiovascular or cerebrovascular<br />
disease.<br />
Conclusion : Although preloading with<br />
crystalloid administration is a safe procedure,<br />
its effectiveness in preventing hypotension in<br />
parturient undergoing caesarean section<br />
under spinal anaesthesia is questionable. And<br />
at the same time prophylactic ephedrine has<br />
limited efficiency <strong>for</strong> the prevention <strong>of</strong><br />
hypotension. Further study are required to<br />
determine the optimal doses/technique <strong>of</strong><br />
prophylactic ephedrine administration and<br />
trials <strong>of</strong> other prophylactic vasopressors are<br />
warranted.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
27
ORIGINAL ARTICLE<br />
References<br />
1. Jackson R, Reid JA, Thorburn J. Volume<br />
preloading is notessential to prevent<br />
spinalinduced hypotension at caesarean<br />
section. Br J Anaesth 1995; 75: 262-5.<br />
2. Turner RJ ,Gatt SP, Ramzan I , Daley M<br />
. Administration <strong>of</strong> crystalloid fluid preload<br />
does not prevent the decrease inarterial<br />
blood pressure after induction <strong>of</strong><br />
anaesthesia with prop<strong>of</strong>ol and fentanyl.<br />
Br J Anaesth 1988;8 : 737-41.<br />
3. Lee A, Ngan Kee WD, Gin T. Prophylactic<br />
ephedrine prevents hypotension during<br />
spinal anesthesia <strong>for</strong> cesarean delivery<br />
but does not improve neonatal outcome:<br />
a quantitative systematic review. Can J<br />
Anaesth. 2002;49:588–59<br />
4. Bhattacharya D, Chowdhury M, Biswas<br />
B, Nitish G, Rudra A, Banarjee A.<br />
Comparison <strong>of</strong> an ephedrine infusion with<br />
crystalloid administration <strong>for</strong> prevention<br />
<strong>of</strong> hypotension during spinal anaesthesia<br />
<strong>for</strong> elective caesarean section. Indian J<br />
Anaesth 2001; 45(4): 290-3.<br />
5. Gutsche BB. Prophylactic ephedrine<br />
preceding spinal analgesia <strong>for</strong> cesarean<br />
section. Anesthesiology 1976;45:462–5.<br />
6. Webb AA, Shipton EA. Re-evaluation <strong>of</strong><br />
im ephedrine as prophylaxis against<br />
hypotension associated with spinal<br />
anaesthesia <strong>for</strong> Caesarean section. Can<br />
J Anaesth 1998;45:367–9.<br />
7. Rout CC, Rocke DA, Brijball R,<br />
Koovarjee RV. Prophylactic intramuscular<br />
ephedrine prior to caesarean section.<br />
Anaesth Intensive Care 1992;20:448–52<br />
8. Chan WS, Irwin MG, Tong WN, Lam YH.<br />
Prevention <strong>of</strong> hypotension during spinal<br />
anaesthesia <strong>for</strong> Caesarean section:<br />
ephedrine infusion versus fluid preload.<br />
Anaesthesia 1997;52:896–913.<br />
9. King SW, Rosen MA. Prophylactic<br />
ephedrine and hypotension associated<br />
with spinal anesthesia <strong>for</strong> cesarean<br />
delivery. Int J Obstet Anesth 1998;7:18–<br />
22.<br />
10. Rout CC, Rocke DA, Levin J. A reevaluation<br />
<strong>of</strong> the role <strong>of</strong> crystalloid<br />
preload in the prevention <strong>of</strong> hypotension<br />
associated with spinal anesthesia <strong>for</strong><br />
elective cesarean section.<br />
Anesthesiology 1993;79:262–9.<br />
11. Marcel PV, Hilde CC, Vincent HH,<br />
Mertens E, Hugo AA. Prevention <strong>of</strong><br />
hypotension by a single 5-mg dose <strong>of</strong><br />
ephedrine during small-dose spinal<br />
anesthesia in prehydrated caesarean<br />
delivery patients. Anesth Analg<br />
1999;90(2):241-2.<br />
12. Ngan Kee WD, Khaw KS, Lee BB, Lau<br />
TK, Gin T. A dose-response study <strong>of</strong><br />
prophylactic intravenous ephedrine <strong>for</strong><br />
the prevention <strong>of</strong> hypotension during<br />
spinal anesthesia <strong>for</strong> cesarean delivery.<br />
Anesth Analg. 2000;90:1390–5.<br />
28 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
The effect <strong>of</strong> intrathecal clonidine on hyperbaric bupivacaine <strong>for</strong> postoperative<br />
analgesia<br />
1<br />
L. Chaoba Singh, 2 N. Anita Devi, 2 N. Ratan Singh, 3 Laithangbam PKS, 4 Kh. Maniram Singh<br />
Abstract<br />
Objective: To evaluate the postoperative<br />
analgesic effect and associated complication<br />
<strong>of</strong> intrathecal clonidine as an adjuvant to inj<br />
0.5% hyperbaric bupivacaine in patients<br />
undergoing lower abdominal surgeries.<br />
Methods: 60 (sixty) patients <strong>of</strong> ASA I and II<br />
Grades, age between 20–60 years,<br />
undergoing lower abdominal surgery were<br />
included in the study. Patients with<br />
neurological deficits or diseases, bleeding<br />
disorders, psychiatric disorders, chronic pain,<br />
obvious skeletal de<strong>for</strong>mities and those<br />
patients on antihypertensive medication were<br />
excluded. The patients were randomly divided<br />
into two groups <strong>of</strong> 30 (thirty) each.<br />
a. Group I patients received 0.5% hyperbaric<br />
bupivacaine 0.3mg/kg.<br />
b. Group II patients received 0.5% hyperbaric<br />
bupivacaine 0.3mg/kg and 1 µg/ kg body<br />
weight <strong>of</strong> preservative free inj.clonidine<br />
hydrochloride.<br />
The hemodynamic parameters such as heart<br />
rate, NIBP, ECG and SpO2 were monitored<br />
periodically. Patients were observed <strong>for</strong> the<br />
presence <strong>of</strong> side effects (dry mouth,<br />
dizziness, anxiety, restlessness pruritus,<br />
sedation, nausea, etc)<br />
Duration <strong>of</strong> analgesia was taken as the pain<br />
free post operative interval between the end<br />
1. Registrar 2. Asst Pr<strong>of</strong>essor 3. Assoc Pr<strong>of</strong>essor<br />
4. Pr<strong>of</strong>essor, Dept <strong>of</strong> Anaesthesia, RIMS, Imphal<br />
Address <strong>of</strong> correspondence:-<br />
Pr<strong>of</strong>. Kh. Maniram Singh, Dept. <strong>of</strong> Anaesthesiology,<br />
RIMS Imphal<br />
<strong>of</strong> injection and patient’s first analgesic<br />
request and rescue analgesia was provided<br />
by inj tramadol hydrochloride 100mg<br />
intravenously. Results: Duration <strong>of</strong> postoperative<br />
analgesia in the clonidine group<br />
(360.83 ± 50.489 min) was significantly longer<br />
than control group(190.43 ± 23.942 min).<br />
There was no significant complication <strong>of</strong><br />
intrathecal clonidine during the study.<br />
Conclusion: It may be concluded that<br />
intrathecal clonidine at the dose <strong>of</strong> 1µg/kg<br />
significantly prolongs the post-operative pain<br />
free period without significant cardiovascular<br />
<strong>change</strong>s and side effects.<br />
Key words: Bupivacaine, clonidine, spinal<br />
anaesthesia, postoperative analgesia<br />
Introduction: Spinal anaesthesia with<br />
hyperbaric bupivacaine is commonly used <strong>for</strong><br />
lower abdominal and lower limb surgeries.<br />
Search is on <strong>for</strong> the ideal adjuvant drugs which<br />
may be added to local anaesthetic agents to<br />
prolong the duration <strong>of</strong> the block and also to<br />
provide post operative analgesia. Even though<br />
opioids administered intrathecally can provide<br />
pr<strong>of</strong>ound postoperative analgesia, there are<br />
disadvantages like nausea, vomiting, pruritus,<br />
urinary retention, respiratory depression, etc.<br />
The use <strong>of</strong> clonidine - an alpha 2 adrenergic<br />
receptor agonist, has been <strong>of</strong> considerable<br />
and sustained interest <strong>for</strong> the last two<br />
decades. It has been shown that clonidine<br />
administered in the epidural space or<br />
intrathecally has a substantial antinociceptive<br />
effect by its action on the α 2-receptor in the<br />
dorsal horn <strong>of</strong> the spinal cord 1 . Several authors<br />
had used high doses <strong>of</strong> intrathecal clonidine<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
29
ORIGINAL ARTICLE<br />
in the range <strong>of</strong> 75µg-450 µg but they were<br />
usually associated with bradycardia 2 ,<br />
hypotension 2,3,4 , sedation 4 , dry mouth 4,5 , etc.<br />
The present study was conducted in the<br />
Department <strong>of</strong> Anaesthesiology, RIMS, Imphal,<br />
to evaluate the postoperative analgesic effect<br />
and associated complication <strong>of</strong> intrathecal<br />
clonidine as an adjuvant to hyperbaric<br />
bupivacaine in patients undergoing lower<br />
abdominal surgeries.<br />
Materials and methods: After obtaining<br />
approval by Institutional Ethical Committee and<br />
in<strong>for</strong>med written consent, 60(sixty) patients<br />
<strong>of</strong> ASA I and II Grades 6 , age between 20 – 60<br />
years, undergoing lower abdominal surgery<br />
at RIMS, Imphal, were included in the study.<br />
Patients with neurological deficits or diseases,<br />
bleeding disorders, psychiatric disorders,<br />
chronic pain, obvious skeletal de<strong>for</strong>mities and<br />
those patients on antihypertensive medication<br />
were excluded. All patients were advised to<br />
fast after 2200 hrs and administered diazepam<br />
orally (10 mg) and tab ranitidine 150mg the<br />
night be<strong>for</strong>e surgery. Baseline pulse rate and<br />
blood pressure were recorded. Preloading<br />
was done with inj Ringer’s lactate 15 ml per<br />
kg body weight about 15 minutes be<strong>for</strong>e the<br />
intended time <strong>of</strong> intrathecal drug<br />
administration. Patients were given spinal<br />
anaesthesia with one <strong>of</strong> the drugs prepared.<br />
The study solution was prepared by a person<br />
not involved in the study<br />
The patients were randomly divided into two<br />
groups <strong>of</strong> 30 (thirty) each.<br />
a. Group I (control group) patients received<br />
0.5% bupivacaine (heavy) 0.3mg/kg.<br />
b. Group II (clonidine group) patients received<br />
0.5% bupivacaine (heavy) 0.3mg/kg and<br />
1 µg/ kg body weight 7,8 <strong>of</strong> preservative<br />
free inj.clonidine hydrochloride.<br />
The hemodynamic parameters such as Heart<br />
rate, NIBP, ECG and SpO2 were monitored<br />
periodically and recorded at 2 minutes interval<br />
<strong>for</strong> the first 10 min and thereafter at 5min<br />
intervals until the end <strong>of</strong> surgery. Patients were<br />
observed <strong>for</strong> the presence <strong>of</strong> side effects (dry<br />
mouth, dizziness, anxiety, restlessness<br />
pruritus, sedation, nausea, etc)<br />
Intravenous fluid was administered in the <strong>for</strong>m<br />
<strong>of</strong> Ringer’s lactate (RL) at the rate <strong>of</strong> 10ml<br />
per kg body weight per hour. A decrease in<br />
mean arterial pressure (MAP) <strong>of</strong> >20% from<br />
baseline was treated with rapid infusion <strong>of</strong> 500<br />
ml <strong>of</strong> RL and 3mg <strong>of</strong> injection mephentermine<br />
intravenously if there was no response to fluid<br />
administration. Bradycardia (heart rate< 60/<br />
minute) was treated with intravenous atropine<br />
sulphate 0.3mg.<br />
All the patients were observed in the post<br />
anaesthesia recovery room and then in the<br />
ward <strong>for</strong> 24 hours. Duration <strong>of</strong> analgesia was<br />
taken as the pain free post operative interval<br />
between the end <strong>of</strong> injection and patient’s first<br />
analgesic request and rescue analgesia was<br />
provided by inj tramadol hydrochloride 100mg<br />
intravenously.<br />
Results and observation<br />
Table 1. Comparison <strong>of</strong> patient characteristics<br />
(Age and Weight) between groups<br />
Table 2. Comparison <strong>of</strong> patient characteristic<br />
(gender) between groups<br />
Sex Clonidine Group Control group Total<br />
Female 24 25 49<br />
Male 6 5 11<br />
Total 30 30 60<br />
2 = 0.111; d.f. =1; P = 0.739<br />
Table-1 shows the comparison <strong>of</strong> mean age<br />
and weight <strong>of</strong> patients between clonidine group<br />
and control group. It was observed from the<br />
table that those persons who belong to<br />
clonidine group had older age (35.20±12.947<br />
vs 34.40±10.981) as well as heavier<br />
(57.00±8.052 vs 56.47±7.655 ) than those <strong>of</strong><br />
the control group. But it was statistically<br />
insignificant even at 5% probability level.<br />
As shown in Table -2 gender distribution <strong>of</strong><br />
the study subjects between the two groups<br />
were almost similar (p=0.739). However, both<br />
the groups had higher number <strong>of</strong> female<br />
patients.<br />
30 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Table 3. Comparison <strong>of</strong> Mean±SD <strong>of</strong> Duration<br />
<strong>of</strong> Surgery & Analgesia between groups<br />
Fig. 1: Shows comparison <strong>of</strong> Mean Heart Rate<br />
Fig. 1 highlights the difference <strong>of</strong> average HR<br />
between the groups. On an average the heart<br />
rate in clonidine group was lesser than that <strong>of</strong><br />
its counterpart control group which was true<br />
in all the stages except at 2 nd minute but was<br />
not statistically significant (P>0.01).<br />
Fig.- 2: Shows comparison <strong>of</strong> mean SpO2<br />
There was a much fluctuated trend <strong>of</strong> mean<br />
peripheral oxygen saturation (SpO2) was<br />
witnessed when comparison was made<br />
between clonidine and control groups <strong>for</strong> each<br />
stage. However, insignificant value <strong>of</strong> ‘t’ <strong>for</strong><br />
every stage confirmed that SpO2 <strong>for</strong> clonidine<br />
group was almost alike with the control group.<br />
Fig.-3: Shows comparison <strong>of</strong> Mean Arterial Pressure<br />
The mean arterial pressure was higher in the<br />
control group, in all the stages considered<br />
except at 6 th and 30 th minutes, than the<br />
corresponding value <strong>for</strong> clonidine group but<br />
statistically it was insignificant as shown in<br />
Figure 3.<br />
Parameter Clonidine group Control group t-<br />
value d.f. P-<br />
No. Mean± No. Mean±<br />
value<br />
cases SD (min) cases SD (min)<br />
Duration <strong>of</strong><br />
Surgery<br />
(min)<br />
Duration <strong>of</strong><br />
analgesia<br />
(min)<br />
30 44.83±<br />
13.55<br />
30 306.83±<br />
50.48<br />
30 43.67±<br />
10.822<br />
30 190.43±<br />
23.942<br />
0.368 58 0.714<br />
11.410 58 0.000<br />
Duration <strong>of</strong> post-operative analgesia in the<br />
clonidine group (306.83 ± 50.489 min) was<br />
significantly longer than control group(190.43<br />
± 23.942 min) even though duration <strong>of</strong> surgery<br />
(44.83 ± 13.55 vs 43.67± 10.82 min) was<br />
statistically not significant. The maximum<br />
dose <strong>of</strong> clonidine used was 65 µg. There was<br />
no significant complication <strong>of</strong> intrathecal<br />
clonidine during the study (Table 3).<br />
Discussion: Clonidine is a selective partial<br />
agonist <strong>for</strong> α2 adrenoreceptors. It is known<br />
to increase both sensory and motor block <strong>of</strong><br />
local anaesthetics. The analgesic effect<br />
following its intrathecal administration is<br />
mediated spinally through activation <strong>of</strong> post<br />
synaptic α2 receptors in substantia<br />
gelatinosa <strong>of</strong> spinal cord 1 . The rationale behind<br />
intrathecal administration <strong>of</strong> clonidine is to<br />
achieve a high drug concentration in the<br />
vicinity <strong>of</strong> α2 adrenoreceptors in the spinal<br />
cord and it works by blocking the conduction<br />
<strong>of</strong> C and A delta fibres.<br />
In the present study, duration <strong>of</strong> analgesia in<br />
the clonidine group (306 ± 50 min) was<br />
significantly longer than the control group (190<br />
± 23 min). This finding was in agreement with<br />
the study by Kaabachi O et al 7 wherein 1 µg/<br />
kg <strong>of</strong> clonidine was added to 15mg <strong>of</strong> 0.5%<br />
bupivacaine intrathecally in patients<br />
undergoing orthopedic surgery. They<br />
observed that clonidine prolonged the duration<br />
<strong>of</strong> both the sensory and motor block, and time<br />
to first rescue analgesia was longer (461+/-<br />
147 min) in clonidine group.<br />
Interestingly, Sethi BS et al 8 had also<br />
demonstrated that addition <strong>of</strong> clonidine to<br />
bupivacaine in the dose <strong>of</strong> 1 µg/kg significantly<br />
increases the duration <strong>of</strong> analgesia (614 min)<br />
following its placement in subarachnoid space<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
31
ORIGINAL ARTICLE<br />
as compared to bupivacaine alone, which is<br />
comparatively longer than that <strong>of</strong> the present<br />
study finding. However more sedation,<br />
<strong>change</strong> in the heart rate and mean arterial<br />
pressure were observed in their study than<br />
ours.<br />
When the analgesic effects <strong>of</strong> 150µg <strong>of</strong><br />
intrathecal clonidine were compared with<br />
placebo (saline) in cesarean section under<br />
general anesthesia, Filos KS and co-workers 3<br />
observed that clonidine provided pain relief <strong>for</strong><br />
7 +/- 2.2 hr vs. 3+/- 2.8 hr <strong>of</strong> saline. They also<br />
investigated response to 150µg, 300µg, and<br />
450µg doses <strong>of</strong> intrathecal clonidine in a<br />
similar design and patient population and<br />
observed that clonidine produced dosedependent<br />
and long-lasting analgesia (7 +/-<br />
1.3, 10 +/- 1.3, and 14 +/-1.3 hr respectively).<br />
In both the studies, they found sedation was<br />
dose dependent and more pronounced after<br />
450 µg <strong>of</strong> intrathecal clonidine. The maximum<br />
dose used in our study was 65 ìg and this low<br />
dose <strong>of</strong> clonidine (1 µg/kg) might be cause<br />
<strong>for</strong> single incidence <strong>of</strong> sedation in this series.<br />
Our study also shows that moderate<br />
prolongation <strong>of</strong> duration <strong>of</strong> analgesia is<br />
possible with low dose clonidine without<br />
sedation.<br />
Many previous studies had used intrathecal<br />
clonidine combined with opioids and local<br />
anaesthetics <strong>for</strong> labour analgesia and<br />
orthopaedic surgery. However, the<br />
combination with opioids would seem less<br />
attractive <strong>for</strong> obvious reasons. Using<br />
intrathecal clonidine in place <strong>of</strong> opioids avoids<br />
problems <strong>of</strong> respiratory depression, pruritus,<br />
urinary retention and abuse liability.<br />
The works <strong>of</strong> Dobrydnjov I et al 1 , Filos KS et<br />
al 5 , Kock DM et al 9 , where clonidine was used<br />
more than 75 ìg, found prolongation <strong>of</strong><br />
analgesia but at the expense <strong>of</strong> sedation. Even<br />
though sedation is a well known side effect <strong>of</strong><br />
clonidine we had encountered only one case<br />
in our study <strong>of</strong> intrathecal clonidine (1 µg/kg).<br />
This might be because <strong>of</strong> low dose as<br />
suggested by Eisenach et al 10 which stated<br />
that clonidine produces dose dependent<br />
sedation <strong>of</strong> rapid onset at the range 50-900<br />
ìg, regardless <strong>of</strong> route <strong>of</strong> administration. Our<br />
findings were in agreement with Kaabachi O<br />
et al 7 which again underlines the safety <strong>of</strong> low<br />
dose intrathecal clonidine.<br />
Conclusion: It might be concluded that<br />
intrathecal clonidine at the dose <strong>of</strong> 1µg/kg<br />
significantly prolongs the post-operative pain<br />
free period without significant cardiovascular<br />
<strong>change</strong>s and side effects.<br />
Reference<br />
1. Dobrydnjov I, Axelsson K, Samartel J,<br />
Holmstrom B. Postoperative pain relief<br />
following intrathecal bupivacaine<br />
combined with intrathecal or oral clonidine.<br />
Acta Anaesthesiol Scand 2002; 46:806-<br />
14.<br />
2. Chiari A, Lober C, Eisenach JC, Wildling<br />
E, Krenn C, Zavrsky A et al. Analgesic and<br />
hemodynamic effects <strong>of</strong> intrathecal<br />
clonidine as the sole analgesic agent<br />
during first stage <strong>of</strong> labor:A doseresponse<br />
study. Anesthesiology1999;<br />
9:388-96.<br />
3. Filos KS, Goudas LC, Patroni O, Polyzou<br />
V. Intrathecal clonidine as a sole analgesic<br />
<strong>for</strong> pain relief after cesarean section.<br />
Anesthesiology 1992; 77:267-74.<br />
4. Benhamou D, Thorin D, Brichant JF,<br />
Dailland P, Milon D, Schneider M.<br />
Intrathecal clonidine and fentanyl with<br />
hyperbaric bupivacaine improve analgesia<br />
during cesarean section . Anesth Analg<br />
1998; 87: 609–13.<br />
5. Filos KS, Goudas LC, Patroni O, Polyzou<br />
V. Hemodynamic and analgesic pr<strong>of</strong>ile<br />
after intrathecal clonidine in humans. A<br />
dose-response study. Anesthesiology<br />
1994; 81:591-601.<br />
6. Owens WD, Felts JA, Spitznagel EL Jr.<br />
ASA physical Status classification: a study<br />
<strong>of</strong> consistency <strong>of</strong> ratings. Anesthesiology<br />
1978; 49:239-43.<br />
7. Kaabachi O, Zarghouni A, Ouezini R,<br />
Abdelaziz AB, Chattaoui O,Kokki H.<br />
Clonidine 1 µg/kg is a safe and effective<br />
32 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
adjuvant to plain bupivacaine in spinal<br />
anesthesia in adolescents. Anesth Analg<br />
2007; 105:516-9.<br />
8. Sethi BS, Mary S, Deepak S. Efficacy <strong>of</strong><br />
analgesic effects <strong>of</strong> low dose intrathecal<br />
clonidine as adjuvant to bupivacaine. In J<br />
Anesth 2007; 51: 415-9.<br />
9. Kock DM, Gautier P, Fanard L, Luc HJ,<br />
Lavandhomme P. Intrathecal ropivacaine<br />
and clonidine <strong>for</strong> ambulatory knee<br />
arthroscopy: a dose-response study.<br />
Anesthesiology 2001; 94:574-8.<br />
10. Eisenach JC, Kock MD, KlimschaW.<br />
Alpha sub 2- adrenergic agonists <strong>for</strong><br />
regional anesthesia: a clinical review <strong>of</strong><br />
clonidine (1984-1995). Anesthesiology<br />
1996; 85(3):655-74.<br />
11. Fogarty DJ, Carabine UA, Milligan KR.<br />
Comparision <strong>of</strong> the analgesic effects <strong>of</strong><br />
intrathecal clonidine and intrathecal<br />
morphine after spinal anaesthesia in<br />
patients undergoing total hip replacement.<br />
Br J Anaesth 1993; 71:661-4.<br />
12. Bonnet F, Brun-Buisson V, Saada M,<br />
Boico O, Rostaing S, Touboul C. Doserelated<br />
prolongation <strong>of</strong> hyperbaric<br />
tetracaine spinal anesthesia by clonidine<br />
in humans. Anesth Analg 1989; 68:619-<br />
22.<br />
13. Racle JP, Benkhadra A, Poy JY, Gleizal B.<br />
Prolongation <strong>of</strong> isobaric bupivacaine<br />
spinal anesthesia with epinephrine and<br />
clonidine <strong>for</strong> hip surgery in the elderly.<br />
Anaesth Analg 1987; 66:442-6.<br />
14. Grace D, Bunting H, Milligan KR, Fee JPH.<br />
Postoperative Analgesia after coadministration<br />
<strong>of</strong> clonidine and morphine<br />
by the intrathecal route in patients<br />
undergoing hip replacement. Anesth Analg<br />
1995; 80:86-91.<br />
15. Heo GJ, Kim YH, Hyun Oh J, and Chul<br />
Joo J. Effect <strong>of</strong> intrathecal clonidine in<br />
hyperbaric bupivacaine spinal anesthesia.<br />
Korean J Anesthesiol 1997; 33:304-8.<br />
16. Alex THS. Optimal dose <strong>of</strong> intrathecal<br />
clonidine added to sufentanil plus<br />
bupivacaine <strong>for</strong> labour analgesia. Can J<br />
Anesth 2000; 47:875-80<br />
17. Maria DC, Juliao C, Gabriela RL. Lowdose<br />
intrathecal clonidine combined with<br />
sufentanil as analgesic drugs in abdominal<br />
gynecological surgery. J Cl Anesth 2000<br />
;12: 357-62<br />
18. Dobrydnjov I, Axelsson K, Thorn SE,<br />
Matthiesen P, Klockh<strong>of</strong>f H, Holmstrom B,et<br />
al. Clonidine combined with small-dose<br />
bupivacaine during spinal anesthesia <strong>for</strong><br />
inguinal herniorrhaphy: a randomized<br />
double-blinded study. Anesth Analg<br />
2003;96:1496-503<br />
19. Brain DS, Micheal B, Russel B, Rohan C.<br />
Intrathecal clonidine added to a<br />
bupivacaine-morphine spinal anesthetic<br />
improves postoperative analgesia <strong>for</strong> total<br />
knee arthroplasty. Anesth Analg<br />
2003;96:1083–8<br />
20. Strebel S, Gurzeler JA, Schneider MC,<br />
Aeschbach A, Kindler CH. Small dose<br />
intrathecal clonidine and isobaric<br />
bupivacaine <strong>for</strong> orthopedic surgery: a<br />
dose-response study. Anesth Analg 2004;<br />
99:1231-8.<br />
21. Van IT, Klei VWA, Werff VD, Kalkman CJ.<br />
The effect <strong>of</strong> addition <strong>of</strong> intrathecal<br />
clonidine to hyperbaric bupivacaine on<br />
postoperative pain and morphine<br />
requirements after caesarean section: a<br />
randomized controlled trial. Br J Anaesth<br />
2006; 97:365–70<br />
22. Ogun CO, Kirgiz EN, Duman A, Kara I,<br />
Okesli S. The comparison <strong>of</strong> intrathecal<br />
isobaric ropivacaine and isobaric<br />
ropivacaine-clonidine <strong>for</strong> caesarean<br />
delivery. Internet J Anesthesiol 2007;15:(1).<br />
Available from: http://www.ispub .com /<br />
ostia / index. php ? xml File Path =<br />
journals/ija vol 15n1/intrathecal.xml.<br />
Accessed on June 15, 2008.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
33
ORIGINAL ARTICLE<br />
Pretreatment with lidocaine and metoclopramide <strong>for</strong> the prevention <strong>of</strong> pain<br />
associated with prop<strong>of</strong>ol injection<br />
1<br />
Cherry JB Kharbudnah , 2 N. Ratan Singh, 3 Laithangbam PKS, 4 L. Deban Singh, 5 L.Kameshwar Singh<br />
6<br />
A. Jack Meitei<br />
Objective: To study the effectiveness <strong>of</strong><br />
Pretreatment with lidocaine and metoclopramide<br />
<strong>for</strong> the prevention <strong>of</strong> pain associated<br />
with prop<strong>of</strong>ol injection Methods: Following<br />
ethics committee approval, 105 adult patients<br />
<strong>of</strong> either sex (ASA I & II, Aged 18 – 60 yrs)<br />
undergoing major elective surgery under<br />
general anaesthesia were randomly divided<br />
into three groups (n = 35) to receive injection<br />
20 mg <strong>of</strong> injection lignocaine 2% plus<br />
metoclopromide 10 mg (Group A), injection<br />
lignocaine 2% 20 mg alone (Group B) or saline<br />
(Group C) given over 10 seconds into a large<br />
antecubital vein after applying a rubber<br />
tourniquet (pressure <strong>of</strong> 50 mm Hg). After one<br />
minute, the tourniquet was released and 25%<br />
<strong>of</strong> the calculated dose <strong>of</strong> prop<strong>of</strong>ol (2 mg/kg)<br />
was given, and patient’s pain response was<br />
graded into four point scale (0 = no pain, 1 =<br />
mild pain/pain reported only on questioning<br />
without any behavioural sign; 2 = moderate<br />
pain/pain reported spontaneously/pain<br />
reported on questioning accompanied by<br />
behavioural signs; 3 = severe pain/strong<br />
vocal response/pain accompanied by facial<br />
grimacing, withdrawal or tears. Results: It<br />
was found that 12 (34.29%) patients in the<br />
control group had pain compared to 7 (20%)<br />
patients in the lignocaine group and 8 (22.86%)<br />
patients in the lignocaine - metoclopromide<br />
1. PGT, 2. Asst. Pr<strong>of</strong>., 3. Assoc. Pr<strong>of</strong>.,<br />
4. Pr<strong>of</strong>essor, 5. Pr<strong>of</strong>essor & Head, 6. Registrar<br />
Deptt. <strong>of</strong> Anaesthesiology, RIMS, Imphal, Manipur.<br />
Corresponding author:<br />
Dr L. Deban Singh, Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Anaesthesiology; RIMS, Imphal, Manipur<br />
combination group (p < 0.05). Conclusion:<br />
We could not appreciate lignocaine and<br />
metoclopromide combination to be superior<br />
to lignocaine or placebo in reducing prop<strong>of</strong>ol<br />
injection pain.<br />
Key words: Injection pain, pre-treatment, pain<br />
attenuation<br />
Introduction: Prop<strong>of</strong>ol is a potent intravenous<br />
hypnotic agent widely used <strong>for</strong> induction and<br />
maintenance <strong>of</strong> general anaesthesia, <strong>for</strong><br />
sedation in ICU, and also to provide sedation<br />
during surgery. However, pain on its injection<br />
remains a problem. Various strategies have<br />
been tried to reduce the incidence <strong>of</strong> prop<strong>of</strong>ol<br />
injection pain, which include injecting prop<strong>of</strong>ol<br />
into a large antecubital vein 1 ,cooling 2 , adding<br />
local anaesthetics 3 , diluting prop<strong>of</strong>ol solution 4 ,<br />
or by administering opioids 5 ,metoclopramide 6 ,<br />
non steroidal anti-inflammatory drugs<br />
(NSAIDS) 7 , etc. Interestingly, out <strong>of</strong> all these<br />
methods cited, several workers have<br />
advocated the use <strong>of</strong> lidocaine and<br />
metoclopramide <strong>for</strong> ameliorating the prop<strong>of</strong>ol<br />
injection pain, and some studies have shown<br />
that lidocaine & metoclopramide are equally<br />
effective in the reduction <strong>of</strong> prop<strong>of</strong>ol injection<br />
pain 8 . The present study was designed to<br />
investigate if lidocaine & metoclopramide<br />
combination is superior to lidocaine alone or<br />
a placebo (saline).<br />
Methods: This Study was conducted in the<br />
department <strong>of</strong> Anaesthesiology, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal. After<br />
obtaining permission from the institutional<br />
ethics committee and written in<strong>for</strong>med<br />
34 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
consent, 105 adult patients <strong>of</strong> ASA grade I &<br />
II, between 18 and 60 years <strong>of</strong> age <strong>of</strong> either<br />
sex who were scheduled to undergo major<br />
elective surgery under general anesthesia<br />
were included in this study.<br />
105 (One hundred and five) patients were<br />
randomly allocated into three groups (n=35)<br />
viz. Group A=Lidocaine + metoclopramide<br />
group received 20 mg lidocaine 2% along with<br />
10 mg <strong>of</strong> metoclopramide, Group B =<br />
Lidocaine group received 20 <strong>of</strong> lidocaine 2%<br />
and Group C = Saline group received 0.9%<br />
saline intravenously.<br />
On the morning <strong>of</strong> surgery, 20gauze IV<br />
cannula was inserted on the <strong>for</strong>earm vein <strong>for</strong><br />
administering the study drugs. Premedication<br />
was provided with injection glycopyrrolate 0.2<br />
mg IM and inj. Ranitidine 50 mg IV, 1 hour<br />
be<strong>for</strong>e the induction <strong>of</strong> anesthesia. On arrival<br />
at the operation theatre, non invasive<br />
monitoring <strong>for</strong> blood pressure (BP),<br />
electrocardiogram (ECG), and pulse oximetry<br />
were started. A rubber tourniquet was applied<br />
to the arm <strong>for</strong> venous occlusion. The study<br />
drugs were administered over 10 seconds<br />
through the cannula (pretreatment). After 1<br />
minute, the tourniquet was released and 25%<br />
<strong>of</strong> the induction dose <strong>of</strong> the drug (2mg/kg) was<br />
injected, and the during this injection, the<br />
patients were asked standard questions<br />
regarding the com<strong>for</strong>t <strong>of</strong> injection, and were<br />
continuously observed <strong>for</strong> vocal responses,<br />
facial grimacing , arm withdrawal or tears<br />
suggesting severe pain. Pain was graded<br />
using a four point scale 9 : 0= no pain, 1= mild<br />
pain or pain reported only in response to<br />
questioning without any behavioral signs, 2=<br />
moderate pain or pain reported in response<br />
to questioning and accompanied by a<br />
behavioral sign or pain reported spontaneously<br />
without questioning and 3= severe pain with<br />
strong vocal response or response<br />
accompanied by facial grimacing, arm<br />
withdrawal or tears.<br />
Once the assessment <strong>of</strong> the injection pain had<br />
been made, induction <strong>of</strong> anesthesia was<br />
completed with the remaining dose <strong>of</strong> prop<strong>of</strong>ol<br />
and tracheal intubation was facilitated with<br />
vecuronium. Anaesthesia was maintained with<br />
halothane, nitrous oxide (66%) in oxygen and<br />
tramadol hydrochloride with controlled<br />
ventilation.<br />
Results: Table I shows the distribution <strong>of</strong><br />
patients in relation to their age, weight, sex<br />
and ASA (American Society <strong>of</strong> Anesthesiologist)<br />
classification in Group A, Group B<br />
and Group C. The mean (± SD) age <strong>of</strong> group<br />
A was 40.26 ± 12.96, group B was 42.07 ±<br />
12.86 and group C was 39.75 ± 13.56; while<br />
the mean weight <strong>for</strong> Group A, B & C were<br />
53.54±8.26, 54.97±9.81 and 51.97±8.25<br />
respectively. So, statistically there are no<br />
significant differences between the three<br />
groups with respect to age and weight with<br />
an ‘F’-value <strong>of</strong> 1.00and P value <strong>of</strong> 0.37.<br />
Similarly, there was no statistically significant<br />
difference in the sex and ASA distribution in<br />
the three study groups as shown in the said<br />
table 1.<br />
Table 1. Demographic pr<strong>of</strong>ile<br />
Group A Group B Group C<br />
(n=35) (n=35) (n=35) Test Level P value<br />
Age(yrs)<br />
Mean ±SD 40.26± 42.07± 39.75± F=1.00 0.37<br />
12.96 12.86 13.56<br />
Weight(kg)<br />
Mean ±SD 53.54± 54.97± 51.97± F=1.01 0.37<br />
8.26 9.81 8.25<br />
Sex(M:F) 11:24 14:21 9:26 × 2 = 0.82 0.4<br />
ASA(I:II) 35:0 34:1 32:3 × 2 = 1.83 0.15<br />
Table 2. Distribution <strong>of</strong> Pain during<br />
prop<strong>of</strong>ol injection<br />
Table 2 shows the distribution <strong>of</strong> the pain in<br />
the three groups during the injection <strong>of</strong><br />
prop<strong>of</strong>ol. The number <strong>of</strong> patients with no pain<br />
were 27(77.14%) in group A, 28(80.00%) in<br />
group B and 23(65.71%) in group C. Mild pain<br />
was experienced by 8(22.86%), 5(14.29%)<br />
and 8(22.86%) <strong>of</strong> the patients in group A, group<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
35
ORIGINAL ARTICLE<br />
B and group C respectively. Severe pain was<br />
experienced by a few patients in all the groups.<br />
This distribution <strong>of</strong> pain grades is not<br />
statistically significant with a chi-square value<br />
<strong>of</strong> 5.40 and a P value <strong>of</strong> 0.49.<br />
Discussion: The mechanism <strong>of</strong> prop<strong>of</strong>ol<br />
injection pain is attributed to the activation <strong>of</strong><br />
kallikren & kinin system and the release <strong>of</strong><br />
bradykinin 10 . Prop<strong>of</strong>ol injection pain depends<br />
on the site <strong>of</strong> injection, size <strong>of</strong> the vein, age <strong>of</strong><br />
the patient, temperature and concentration <strong>of</strong><br />
prop<strong>of</strong>ol or the use <strong>of</strong> tourniquet inflation 11 . The<br />
idea <strong>of</strong> the use <strong>of</strong> tourniquet is to allow the<br />
exertion <strong>of</strong> local anesthetic effect <strong>of</strong> lidocaine<br />
or metoclopramide by allowing more direct<br />
contact with the free nerve endings after<br />
tourniquet inflation 12 . However, local<br />
anesthetic effect is not the only mechanism<br />
as some studies have shown that lidocaine<br />
causes inhibition <strong>of</strong> bradykinin 10 . This may<br />
explain why some investigators found<br />
lidocaine mixed with prop<strong>of</strong>ol is superior to<br />
pretreatment in attenuating pain 13 . In our study<br />
we could not demonstrate significant<br />
difference among the three groups. This is in<br />
sharp contrast to the findings <strong>of</strong> Fujii Y and<br />
Nakayama M 6 who found significant pain<br />
reduction (p
ORIGINAL ARTICLE<br />
8. Liaw WJ, Pang WW, Chang DP, Hwang<br />
MH. Pain on injection <strong>of</strong> prop<strong>of</strong>ol: the<br />
mitigating influence <strong>of</strong> metoclopramide<br />
using different techniques. Acta<br />
Anaesthesiol Scand 1999 Jan; 43(1):<br />
24- 7.<br />
9. Memis D, Turan A, Karamanlioglu B, Sut<br />
N, Pamukcu Z. The use <strong>of</strong> magnesium<br />
sulfate to prevent pain on injection <strong>of</strong><br />
prop<strong>of</strong>ol. Anesth Analg 2002; 95:<br />
606–8.<br />
10. Nakane M, Iwama H. A potential<br />
mechanism <strong>of</strong> prop<strong>of</strong>ol – induced pain<br />
on injection <strong>based</strong> on studies using<br />
nafamostat mesilate. British <strong>Journal</strong> <strong>of</strong><br />
Anaesthesia 1999; 83(3): 397-<br />
404.<br />
11. Gupta M, Mishra S, Gupta D, Gujjar M,<br />
Bhatnagar S. Prevention <strong>of</strong> pain on<br />
prop<strong>of</strong>ol injection. A comparative<br />
randomized double blind study between<br />
lignocaine, pethidine, dexamethasone<br />
and placebo. The Internet <strong>Journal</strong> <strong>of</strong><br />
Anesthesiology 2007; 11(2). Accessed<br />
on 25August 2010.<br />
12. Mangar D, Holak EJ. Torniquet at 50<br />
mmhg followed by intravenous lidocaine<br />
diminishes hand pain associated with<br />
prop<strong>of</strong>ol injection. Anesth Analg 1992<br />
Feb; 74(2): 250-2.<br />
13. Overbaugh R, Jones P, Nguyen A, Swaney<br />
G. Effect <strong>of</strong> mixed versus unmixed<br />
lidocaine with prop<strong>of</strong>ol. The Internet<br />
<strong>Journal</strong> <strong>of</strong> Anesthesiology 2003; 7 (2).<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
37
ORIGINAL ARTICLE<br />
Histological pattern <strong>of</strong> thyroid diseases in RIMS Hospital, Imphal: A report <strong>of</strong><br />
ten years study.<br />
1<br />
Rajesh Singh Laishram, 1 O. Okendrajit Singh, 2 Janet Zoremnghaki, 3 Durlav Chandra Sharma, 4 S Thingbaijam<br />
Abstract<br />
Objective: The study was conducted to<br />
observe the different types <strong>of</strong> thyroid lesions<br />
in specimens received in Pathology<br />
department, RIMS, Imphal. Methods: This<br />
retrospective study was carried out on<br />
surgically resected thyroid specimens in<br />
RIMS Hospital, Imphal, during the period<br />
between January 2001 and December 2010.<br />
One hundred and eighty four<br />
histopathologically diagnosed thyroid lesions<br />
were reviewed and analysed in respect <strong>of</strong> age,<br />
gender and histological types. Cases with<br />
metastatic lesions in thyroid were excluded<br />
from the study. Results: In the study, <strong>of</strong> the184<br />
histologically diagnosed thyroid diseases,<br />
20(10.87%) cases were males and<br />
164(89.13%) were females and male to<br />
female ratio was 1:8.2. Age range was from 8<br />
to 88 years. Colloid goitre was the<br />
commonest thyroid lesion (45.11%) followed<br />
by follicular adenoma (8.70%).There were 13<br />
cases <strong>of</strong> thyroiditis, eight <strong>of</strong> whom were<br />
lymphocytic thyroiditis and five were<br />
Hashimoto’s thyroiditis. The overall<br />
malignancy was seen in 19.02%, papillary<br />
carcinoma was the commonest comprising<br />
1. Assistant Pr<strong>of</strong>essor. 2. PGT. 3. Pr<strong>of</strong>essor & Head,<br />
Deptt. <strong>of</strong> Pathology RIMS, IMphal. 4. Associate<br />
Pr<strong>of</strong>essor Deptt. <strong>of</strong> ENT, RIMS, Lamphelpat, Imphal.<br />
Corresponding author:<br />
Dr. O. Okendrajit Singh<br />
Assistant Pr<strong>of</strong>essor, Department <strong>of</strong> Pathology,<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences, Lamphelpat,<br />
Imphal- 795004, Manipur, India.<br />
Mobile: +919436025356 e-mail: okendradr@yahoo.com<br />
<strong>of</strong> 29(82.85%) cases followed by medullary<br />
carcinoma in 3(8.57%) cases and there were<br />
2.86% each <strong>of</strong> follicular carcinoma, anaplastic<br />
carcinoma and insular carcinoma.<br />
Conclusion: Thyroid diseases are more<br />
common in females than males. Colloid goitre<br />
is the most common lesion. Papillary thyroid<br />
carcinoma is the commonest malignant<br />
tumour and among the benign tumour,<br />
follicular adenoma is the commonest.<br />
Keywords: Thyroid diseases, Colloid goitre,<br />
Papillary carcinoma, Follicular adenoma<br />
Introduction: Thyroid diseases are<br />
progressively becoming one <strong>of</strong> the most<br />
frequent reasons <strong>for</strong> seeking medical advice.<br />
The worldwide prevalence <strong>of</strong> goitre in the<br />
general population is estimated to be 4-7%<br />
and most <strong>of</strong> them are colloid goitre with few<br />
malignancies mainly in solitary nodules. 1<br />
Thyroid cancer is the most common<br />
endocrine tumour and its annual incidence<br />
estimated worldwide from 0.5-10 per<br />
100,000. 2 It is more common in females than<br />
in males. There is a well-recognised spectrum<br />
<strong>of</strong> variable prognosis with different histological<br />
variants.Papillary carcinoma is the most<br />
common histological type <strong>of</strong> malignancy in<br />
most parts <strong>of</strong> the world. 3-5<br />
This study was carried out to observe the<br />
pattern <strong>of</strong> various histological types <strong>of</strong> thyroid<br />
lesions from the specimens received in<br />
Pathology department, Regional Institute <strong>of</strong><br />
<strong>Medical</strong> Sciences(RIMS), Imphal, Manipur.<br />
Materials and Methods: This retrospective<br />
study was done in the cases treated surgically<br />
38 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
<strong>for</strong> thyroid lesions in RIMS hospital, Imphal,<br />
Manipur. Histologically diagnosed thyroid<br />
lesions during the period between January<br />
2001 and December 2010 were reviewed and<br />
analysed according to age, sex and<br />
histological types with the approval <strong>of</strong> the<br />
Institutional Ethics Committee. Cases with<br />
metastatic lesions in the thyroid were excluded<br />
from the study. All the slides had been stained<br />
with Hematoxylin and Eosin and special stains<br />
like Congo red were used when and where<br />
necessary.<br />
Result: In the present study, 184 histologically<br />
diagnosed thyroid diseases were reviewed.<br />
Table 1: Age and sex distribution <strong>of</strong> the cases<br />
Age Male Female Total Percentage(%)<br />
groups(yrs)<br />
0-10 2 1 3 1.63<br />
11-20 1 7 8 4.35<br />
21-30 5 41 46 25<br />
31-40 4 42 46 25<br />
41-50 4 35 39 21.20<br />
51-60 1 30 31 16.85<br />
61-70 3 7 10 5.43<br />
71-80 0 0 0 0<br />
81-90 0 1 1 0.54<br />
Total 20 164 184 100<br />
Table 2: Histopathological types <strong>of</strong> lesions<br />
Histopathological diagnosis Number Percentage<br />
Nodular goitre 11 5.98 %<br />
Multinodular goitre 12 6.52 %<br />
Adenomatous goitre 12 6.52 %<br />
Colloid goitre 83 45.11 %<br />
Toxic goitre 1 0.54 %<br />
Hashimoto’s thyroiditis 5 2.72 %<br />
Lymphocytic thyroiditis 8 4.35 %<br />
Follicular adenoma 16 8.70 %<br />
Hyalinising trabecular adenoma 1 0.54 %<br />
Thyroid malignancy 35 19.02 %<br />
Total 184 100<br />
Table 3: Histological types <strong>of</strong> thyroid malignancies<br />
Histopathological diagnosis Nos. %<br />
Papillary thyroid carcinoma 29 82.85<br />
Medullary carcinoma 3 2.86<br />
Follicular carcinoma 1 2.86<br />
Anaplastic carcinoma 1 8.57<br />
Insular carcinoma 1 2.86<br />
Total 35 100<br />
Table 4: Distribution <strong>of</strong> benign lesions in relation to<br />
age (years)<br />
Histopa- 0-10 11-20 21-30 31-40 41-50 51-60 61-70 71-80 81-90<br />
thological<br />
lesions<br />
Nodular 0 0 2 7 1 1 0 0 0<br />
goitre<br />
Multinodu- 1 1 0 3 4 3 0 0 0<br />
lar goitre<br />
Adenoma- 0 0 5 0 2 5 0 0 0<br />
tous goitre<br />
Colloid 0 3 19 19 23 15 4 0 0<br />
goitre<br />
Toxic 0 0 0 0 0 1 0 0 0<br />
goitre<br />
Hashim- 0 0 1 0 2 1 0 0 1<br />
oto’s<br />
thyroiditis<br />
Lympho- 0 0 0 0 0 0 1 0 0<br />
cytic<br />
thyroiditis<br />
Follicular 2 0 4 8 0 0 2 0 0<br />
adenoma<br />
Hyalini- 0 0 0 1 0 0 0 0 0<br />
sing<br />
trabecular<br />
adenoma<br />
Total 3 4 31 41 36 26 7 0 1<br />
% 2.01 2.68 20.81 27.52 24.16 17.45 4.70 0 0.67<br />
Out <strong>of</strong> which 20(10.87%) cases were males<br />
and 164(89.3%) were females, with a male to<br />
female ratio <strong>of</strong> 1:8.2. The ages ranged from 8<br />
to88 years. Table 1. shows the age and sex<br />
distribution <strong>of</strong> the cases. Thyroid diseases<br />
were rare below the age <strong>of</strong> 20 years and only<br />
11 cases were seen. The most common<br />
incidence was seen in the age group <strong>of</strong> 21-40<br />
years with 92(50%) cases followed by age<br />
group <strong>of</strong> 41-50 years in 39 (21.2%) cases.<br />
Among females, the highest incidence <strong>of</strong><br />
thyroid disease was found in the age group <strong>of</strong><br />
31-40 years and whereas in males it was 21-<br />
30 years.<br />
The histopathological types <strong>of</strong> thyroid lesions<br />
are shown in Table 2. Colloid goitre was the<br />
commonest thyroid lesion (45.11%), followed<br />
by follicular adenoma in 16(8.70%).Thyroiditis<br />
was found in 13 cases, eight <strong>of</strong> which had<br />
lymphocytic thyroiditis and the remaining five<br />
had Hashimoto’s thyroiditis. Hyalinising<br />
trabecular adenoma and toxic goitre were<br />
found in one case (0.54%) each. Among the<br />
184 patients, 35(19.02%) had thyroid<br />
malignancies,32 <strong>of</strong> these were in females with<br />
a male to female ratio <strong>of</strong> 1:10.67. Papillary<br />
thyroid carcinoma was the commonest<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
39
ORIGINAL ARTICLE<br />
Table 5: Distribution <strong>of</strong> malignant lesions in relation to<br />
age (years). Figures within the parenthesis indicate<br />
percentage & ca indicate carcinoma.<br />
Histolo- 0-10 11-20 21-30 31-40 41-50 51-60 61-70 >70 Total<br />
gical<br />
lesions<br />
Papillary 0 2 13 8 3 3 0 0 29<br />
ca (6.8) (44.8) (27.5) (10.3) (10.3)<br />
Medullary 0 1 1 0 0 0 1 0 3<br />
ca (33.3) (33.3) (33.3)<br />
Follicular 0 1 0 0 0 0 0 0 1<br />
ca (100)<br />
Anaplastic 0 0 0 0 0 1 0 0 1<br />
ca (100)<br />
Insular ca 0 0 0 0 0 0 1 0 1<br />
(100)<br />
Total 0 4 14 8 3 4 2 0 35<br />
% 0 11.43 40 22.86 8.57 11.43 5.71 0 100<br />
(82.85%) followed by medullary carcinoma<br />
(8.57%). One case each (2.86%) <strong>of</strong> anaplastic<br />
carcinoma, follicular carcinoma and insular<br />
carcinoma were also found as shown in<br />
Table 3.<br />
The age distributions <strong>of</strong> various thyroid lesions<br />
are shown in Table 4 and 5. Colloid goitre was<br />
commonest in the age group <strong>of</strong> 41-50 years,<br />
as also in cases <strong>of</strong> thyroiditis. Papillary<br />
carcinoma was commonest (44.8%) in ages<br />
between 21 and 30 years whereas in other<br />
types <strong>of</strong> carcinomas there were no specific<br />
age group.<br />
Discussion: Thyroid nodules which are<br />
surgically treated may be benign or malignant<br />
and their incidences varies widely. 3-6 From<br />
the 184 cases <strong>of</strong> thyroid lesions reviewed, we<br />
observed that there was higher incidence in<br />
females (89.13%) than in males (10.87%) with<br />
a male to female ratio <strong>of</strong> 1:8.2. This is<br />
compatible to studies done by Htwe et al and<br />
other workers who found that there is female<br />
preponderance <strong>for</strong> thyroid lesions. 1,3,7,8,9<br />
In our study, age ranged from 8 to 88 years<br />
and high incidence <strong>of</strong> thyroid lesion were in<br />
ages between 11 and 70 years and among<br />
the females, thyroid disease occur mostly in<br />
the age group between 31 and 40 years. Our<br />
observations are well comparable with many<br />
<strong>of</strong> the published figures. 1,4-8,10,11<br />
The present study showed colloid goitre as<br />
the commonest cause <strong>of</strong> thyroid nodule<br />
comprising <strong>of</strong> 45.11% whereas in the studies<br />
<strong>of</strong>Memon W et al, Gandolfi PP et al and others<br />
reported the most common cause as<br />
multinodular goitre. 4-6,10<br />
The overall malignancy in this study was<br />
19.02% which was slightly higher than<br />
findings in Italy (13.7%), Yemen (17.7%) and<br />
Nigeria (15%). However, much lower<br />
incidence were reported in Malaysia (6.7%)<br />
and Pakistan (2.92%). 5,8,9,12<br />
Papillary carcinoma (82.85%) was the<br />
commonest malignant tumour and more<br />
common in the age group <strong>of</strong> 21-30 years<br />
which is similar to the findings <strong>of</strong> many<br />
workers. 1,3-6,8,10-15 In contrast to our finding,<br />
Mulandzi et al and Edino ST et al reported that<br />
follicular carcinoma was the commonest<br />
thyroid malignancy in the African countries. 7,9<br />
Medullary carcinoma(8.57%) was the second<br />
most common tumour in our study whereas<br />
it was follicular carcinoma as observed by<br />
some other workers. 1,7,10,14 Anaplastic<br />
carcinoma and insular carcinoma(2.86%<br />
each) had low incidence as also reported in<br />
various studies. 8,16,17 It was observed that all<br />
types <strong>of</strong> thyroid carcinomas are more<br />
common in females(91.4%). Similar findings<br />
have been reported in many studies done in<br />
different parts <strong>of</strong> the world. 4-7,10<br />
Conclusion: Thyroid disease is more<br />
common in females than males. Colloid goitre<br />
is the commonest finding in thyroid nodules.<br />
Papillary carcinoma is the most common<br />
thyroid malignancy and usually occurs in the<br />
second and third decade.<br />
40 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
References :<br />
1. Htwe TT, Hamdi MM, Swethadri GK,<br />
Wong JOL, Soe MM, Abdullah MS.<br />
Incidence <strong>of</strong> thyroid malignancy among<br />
thyroid lesions from the Sarawak General<br />
Hospital 2000-2004. Singapore Med J<br />
2009; 50(7):724-8.<br />
2. Chan JKC. The Thyroid Gland. In:<br />
Fletcher CDM. Diagnostic Histopathology<br />
<strong>of</strong> Tumors. 3 rd ed.Philadelphia: Elsevier;<br />
2007.p.997.<br />
3. Haq RN, Khan BA, Chaudhry IA.<br />
Prevalence <strong>of</strong> malignancy in goitre- A<br />
review <strong>of</strong> 718 thyroidectomies. J Ayub<br />
Med CollAbbotabad 2009; 21(4):134-6.<br />
4. Memon W, Khanzada TW, Samad A,<br />
Kumar B. Incidence <strong>of</strong> thyroid carcinoma<br />
in multinodulargoiters. Rawal <strong>Medical</strong><br />
<strong>Journal</strong> 2010 Jan-Jun; 35(1)65-7.<br />
5. Gandolfi PP, Frisina A, Raffa M, Renda F,<br />
Rochetti O, Ruggeri C et al. The incidence<br />
<strong>of</strong> multinodular goitre: retrospective<br />
analysis. Acta Bio Medica Ateneo<br />
Parmense 2004; 75:114-7.<br />
6. Marjani A and Kabir MJ. Incidence <strong>of</strong><br />
thyroid cancer in Golestan Province <strong>of</strong><br />
Iran: some initial observations. Pak J Med<br />
Sci 2008; 24(6):887-90.<br />
7. Mulandzi TV, Ramdial PK, Madiba TE,<br />
Callaghan RA. Thyroid carcinoma at King<br />
Edward VIII hospital, Durban, South Africa.<br />
East African <strong>Medical</strong> <strong>Journal</strong> 2001 May;<br />
78(5):242-5.<br />
8. Hussain M, Anwar M, Nadia N, Ali Z.<br />
Pattern <strong>of</strong> Surgically treated thyroid<br />
disease in Karachi. Biomedica Jan-Jun<br />
2005; 21:18-20.<br />
9. Edino ST, Mohammed AZ, Ochicha O,<br />
Malami SA, yakubu AA. Thyroid cancers<br />
in nodular goitres in Kano, Nigeria. Niger<br />
J ClinPract 2010 Sep; 13(3):298-300.<br />
10. Larijani B, Aghakhani S, Kajeh-Dini H,<br />
BaradarJalili R. Clinicopahological<br />
features <strong>of</strong> thyroid cancer as observed in<br />
five referral hospitals in Iran.<br />
ActaOncologica 2003; 42(4):334-7.<br />
11. Arora R and Dias A. Iodine and thyroid<br />
cancer in Goa. Online J Health Allied Scs<br />
2006;4:3.<br />
12. Abdulmughni YA, Al-Hureibi MA, Al-Hureibi<br />
KA, Ghafoor MA, Al Wadan AH, Al-Hureibi.<br />
Thyroid cancer in Yemen.Saudi med J<br />
2004 Jan; 25(1):55-9.<br />
13. Ito Y and Miyauchi A. Thyroidectomy and<br />
lymph node dissection in papillary thyroid<br />
carcinoma. <strong>Journal</strong> <strong>of</strong> thyroid research<br />
2011.<br />
14. Tanton R and Gupta S. Pattern <strong>of</strong><br />
malignant thyroid neoplasms in Ajmer. J<br />
Indian MA 1988 Aug; 86(8):212-3.<br />
15. Ahmed M, Alsaihati B,GreerW, Al-Nuaim<br />
A, Bakheet S, Abdulkareem AM et al. A<br />
study <strong>of</strong> 875 cases <strong>of</strong> thyroid cancer<br />
observed over a fifteen year period (1975-<br />
1987) at the King Faisal Specialist<br />
Hospital and Research Centre. Ann Saudi<br />
Med 1995 Nov; 15(6):579-84.<br />
16. Dorairajan N, Saravanakumar P,<br />
karthikayan S, Siddarth D, Kanna S. Review<br />
Analysis <strong>of</strong> Medullary carcinoma thyroid–a<br />
15 year Indian experience. J Indian Med<br />
Assoc 2005 Aug; 103(8):415-7.<br />
17. Jain R, Chaturvedi KU, Khurana N,<br />
Aggarwal AK. Insular Carcinoma <strong>of</strong><br />
Thyroid-a case report. IndJ<br />
PatholMicrobiol 2004; 47(3):420-2.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
41
ORIGINAL ARTICLE<br />
Bacterial pr<strong>of</strong>ile <strong>of</strong> osteomyelitis cases at RIMS hospital, Imphal<br />
1<br />
Ksh. Mamta Devi, 2 Lyngdoh CJ, 3 Kh. Sulochana Devi, 4 Ch. Arunkumar Singh,<br />
Abstract<br />
Objective: To isolate and identify bacteria<br />
responsible <strong>for</strong> osteomyelitis, to study the<br />
changing pattern <strong>of</strong> bacterial flora and drug<br />
sensitivity <strong>of</strong> the bacterial isolates to the<br />
commonly used antibiotics. Methods: A<br />
cross-sectional study was undertaken from<br />
cases <strong>of</strong> orthopaedic wound infections in<br />
patients attending RIMS hospital <strong>for</strong> a period<br />
<strong>of</strong> two years from August 2006 to July 2008.<br />
Two samples were collected, one <strong>for</strong> aerobic<br />
culture and another <strong>for</strong> anaerobic culture.<br />
Anaerobic culture was done in a Gas Pak<br />
anaerobic chamber. Any growth was identified<br />
using standard biochemical tests.<br />
Antimicrobial susceptibility <strong>of</strong> the isolates was<br />
done by Kirby Bauer disc diffusion method in<br />
accordance with Clinical Laboratory Standard<br />
Institute (CLSI) guidelines. Results: The study<br />
subjects were predominantly males (66.7%)<br />
in the age group <strong>of</strong> 0-15 years (51.6%). The<br />
maximum number <strong>of</strong> cases was seen in the<br />
summer months <strong>of</strong> April to July. Positive<br />
culture <strong>of</strong> 52% <strong>of</strong> cases was seen with a<br />
predominance <strong>of</strong> gram-positive organisms<br />
(89.4%). Among the gram-positive organisms,<br />
the predominant isolate was Staphylococcus<br />
aureus (68.3%). Among the gram-negative<br />
organisms (10.6%), the isolated organisms<br />
1. Assistant Pr<strong>of</strong>essor, 2. Post Graduate student;<br />
3. Pr<strong>of</strong>essor, Deptt. <strong>of</strong> Microbiology, RIMS, 4. Pr<strong>of</strong>essor<br />
& Head <strong>of</strong> Department, Department <strong>of</strong> Orthopaedics,<br />
RIMS Imphal, Manipur- 795004.<br />
Address <strong>for</strong> correspondence:<br />
Dr. Kh Sulochana Devi 3 Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Microbiology RIMS, Imphal-795004<br />
E mail: sulo_khu@rediffmail.com<br />
were Pseudomonas aeruginosa and<br />
Acinetobacter baumannii. Most <strong>of</strong> the grampositive<br />
isolates were sensitive to<br />
Erythromycin and Gentamicin. 100%<br />
sensitivity to vancomycin is maintained. 100%<br />
<strong>of</strong> the isolates were found to be Methicillin<br />
resistant. A lower sensitivity to the<br />
Cephalosporin group <strong>of</strong> antibiotics was<br />
observed. Conclusion: High occurrence <strong>of</strong><br />
resistance is seen in surgical and orthopaedic<br />
patients where antibiotic usage is the greatest.<br />
Hence therapy should be initiated following<br />
antimicrobial susceptibility testing to prevent<br />
the acquisition and spread <strong>of</strong> resistant strains<br />
<strong>of</strong> the organisms.<br />
Keywords: Osteomyelitis, Antimicrobial<br />
susceptibility, Staphylococcus aureus,<br />
Pseudomonas aeruginosa.<br />
Introduction: Florence Nightingale, more than<br />
100 years ago is believed to have said ‘No<br />
stronger condemnation <strong>of</strong> any hospital or ward<br />
could be pronounced than the single fact that<br />
infectious diseases has originated in it, or that<br />
such a disease has attacked other patients<br />
than those brought in with them.<br />
Bacteria and resultant infection have<br />
continued to inflict untold misery on humanity<br />
from time immemorial and even today, post<br />
operative infections have plagued us. 1 In spite<br />
<strong>of</strong> advances in medicine and surgery, wound<br />
sepsis is a dreadful complication that<br />
challenges every physician and surgeon.<br />
Moreover the patient suffers prolonged<br />
morbidity, economic loss, and <strong>of</strong>ten<br />
permanent disability. 2<br />
42 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Bone and joint infections remain a <strong>for</strong>midable<br />
challenge to the orthopaedic surgeon. The<br />
high success rate obtained with antibiotic<br />
therapy in most bacterial disease has not<br />
been obtained in bone and joint infections<br />
because <strong>of</strong> the physiological and anatomical<br />
characteristics <strong>of</strong> bone. 3<br />
The most common causative organism in<br />
orthopaedic wound infections is<br />
Staphylococcus aureus. 4,5 Others include S.<br />
epidermidis, Streptococci and enteric gramnegative<br />
bacteria such as Escherichia coli<br />
and Pseudomonas aeruginosa. Anaerobic<br />
bacteria are recognized increasingly as an<br />
important cause in orthopaedic wound<br />
infections, particularly in osteomyelitis <strong>of</strong><br />
bones <strong>of</strong> feet associated with diabetes and<br />
foot ulcers. 3, 4<br />
The Clinical Microbiology Laboratory is<br />
increasingly challenged by the spectrum <strong>of</strong><br />
orthopaedic infection. The ever-expanding list<br />
<strong>of</strong> organisms underscores the need <strong>for</strong> careful<br />
microbiological studies that identify the<br />
infecting agent precisely.<br />
Hence this study was carried out to isolate<br />
and identify bacteria responsible <strong>for</strong><br />
osteomyelitis, to study the changing pattern<br />
<strong>of</strong> bacterial flora and drug sensitivity <strong>of</strong> the<br />
bacterial isolates to the commonly used<br />
antibiotics.<br />
Methods : This study included 33 patients <strong>of</strong><br />
Osteomyelitis from amongst the patients<br />
attending Orthopaedic OPD and those<br />
admitted in RIMS Orthopaedic ward. Cases<br />
clinically suspected to be suffering from<br />
tubercular infections were excluded. The<br />
study was conducted in the Departments <strong>of</strong><br />
Microbiology and Orthopaedics, RIMS, Imphal<br />
from August 2006 to July 2008.<br />
Under strict aseptic and antiseptic<br />
precautions, pus or wound swabs were<br />
collected using sterile swabs or using a needle<br />
and syringe. Specimens <strong>for</strong> anaerobic culture<br />
were inoculated into Robertson’s cooked<br />
meat medium. The specimens were<br />
subjected to direct smear, gram staining and<br />
culture by inoculating on Nutrient agar, Blood<br />
agar and MacConkey agar media. The<br />
colonies were then subjected to a series <strong>of</strong><br />
tests <strong>for</strong> identification. Anaerobic culture was<br />
done on selective blood agar containing 20µg<br />
<strong>of</strong> gentamicin in a Gas Pak anaerobic jar<br />
(Dynamicro labs). 6<br />
Antibiotic susceptibility testing was carried out<br />
by Kirby Bauer disc diffusion method in<br />
accordance with Clinical Laboratory Standard<br />
Institute (CLSI) guidelines.<br />
Results: In this study it was observed that<br />
the maximum number <strong>of</strong> cases were seen<br />
during the summer months <strong>of</strong> April ’07 to July<br />
’07 (18.2%) and April’08 to July ’08 (42.3%)<br />
constituting more than half <strong>of</strong> the cases.<br />
Fewer cases occurred during the autumn and<br />
winter season. Most <strong>of</strong> the patients <strong>of</strong><br />
osteomyelitis were males (66.7%) especially<br />
<strong>of</strong> the age group <strong>of</strong> 0-15 years (51.6%) with a<br />
lower prevalence in females (33.3%). The<br />
percentage age and sex distribution among<br />
the different clinical groups was found to be<br />
insignificant (p> 0.05).<br />
Out <strong>of</strong> the total <strong>of</strong> 33 cases <strong>of</strong> osteomyelitis,<br />
positive culture was seen in 17 (52%) <strong>of</strong> the<br />
cases. Total number <strong>of</strong> organisms isolated<br />
was 19 as shown in Table 1. Two <strong>of</strong> the<br />
samples showed mixed infection<br />
(Staphylococcus aureus/ Coagulase negative<br />
Staphylococcus and Staphylococcus aureus<br />
/ Acinetobacter baumannii).<br />
Out <strong>of</strong> a total <strong>of</strong> 17 Gram-positive organisms<br />
which was isolated, the predominant organism<br />
was Staphylococcus aureus (68.3%) followed<br />
by Coagulase-negative Staphylococcus<br />
(21.1%). The gram-negative organisms<br />
isolated were Pseudomonas aeruginosa and<br />
Acinetobacter baumanii as shown in table 1.<br />
Table 2 shows that 100% sensitivity to<br />
vancomycin was seen in all the Gram-positive<br />
organisms. 76.9% <strong>of</strong> Staphylococcus aureus<br />
were sensitive to Erythromycin whereas<br />
61.5% and 69.2% <strong>of</strong> Staphylococcus aureus<br />
were sensitive to Gentamicin and<br />
Cipr<strong>of</strong>loxacin respectively. 53.8% <strong>of</strong> the<br />
isolates showed sensitivity to Piperacillintazobactam.<br />
Among the CONS, most <strong>of</strong> the<br />
isolates (75%) showed sensitivity to<br />
Erythromycin, Gentamicin and Piperacillintazobactam.<br />
All the Staphylococcal isolates<br />
were resistant to oxacillin.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
43
ORIGINAL ARTICLE<br />
Among the gram negative organisms, both the<br />
Pseudomonas aeruginosa and Acinetobacter<br />
baumannii isolates were sensitive to Amikacin,<br />
Table 1: Number and types <strong>of</strong> bacteria from positive<br />
cultures<br />
Bacteria Organism Osteomyelitis<br />
n=19<br />
Gram positive S.aureus 13<br />
(68.3)<br />
CONS 04<br />
(21.1)<br />
Total 17<br />
(89.4)<br />
Gram negative Pseudomonas aeruginosa 01<br />
(5.3)<br />
Acinetobacter baumanii 01<br />
(5.3)<br />
Total 02(10.6)<br />
*Figures in parentheses indicate the percentage<br />
Table 2: Antimicrobial susceptibility pattern <strong>of</strong> Grampositive<br />
bacteria<br />
Antibiotics Staphylococcus CONS<br />
aureus (n=13)<br />
(n=04)<br />
S I R S I R<br />
Erythromycin 10 00 3 3 00 1<br />
(76.9) (23.1) (75) (25)<br />
Gentamicin 8 00 5 3 00 1<br />
(61.5) (38.5) (75) (25)<br />
Cipr<strong>of</strong>loxacin 9 00 4 1 1 2<br />
(69.2) (30.8) (25) (25) (50)<br />
Piperacillin- 7 1 5 3 00 1<br />
tazobactam (53.8) (7.7) (38.5) (75) (25)<br />
Vancomycin 13 00 00 4 00 00<br />
(100) (100)<br />
Cefotaxime 6 03 4 1 1 2<br />
(46.1) (23.1) (30.8) (25) (25) (50)<br />
Oxacillin 00 00 13 00 00 04<br />
(100) (100)<br />
*Figures in parentheses indicate the percentage<br />
Gentamicin, Piperacillin-tazobactam.<br />
The isolates showed resistance to<br />
Ceftazidime, Ceftriaxone, Cipr<strong>of</strong>loxacin and<br />
Co-trimoxazole.<br />
Discussion: According to Resnick D 7 , the<br />
distribution <strong>of</strong> osteomyelitis is greatly<br />
influenced by the age <strong>of</strong> the patient, the<br />
specific causative organism and the presence<br />
or absence <strong>of</strong> any underlying disorder or<br />
situation. In this study, the maximum patients<br />
belong to the age group <strong>of</strong> 0-15 years. In all<br />
the age groups, males (66.7%) were<br />
predominant over the females (33.3%)<br />
comparable to a study by Waldvogel FA et al 8<br />
and Duthie and Nelson. 9<br />
The maximum number <strong>of</strong> cases <strong>of</strong><br />
osteomyelitis was seen in the summer<br />
months <strong>of</strong> April to July which constituted more<br />
than half the total number <strong>of</strong> cases. A similar<br />
finding was reported by Mukhopadhyay B 10<br />
wherein it was stated that osteomyelitis was<br />
more common in summer and rainy seasons.<br />
A culture positivity rate <strong>of</strong> 52% was observed<br />
in this study, consistent with findings <strong>of</strong><br />
Vishwakarma and Lal 11 and Kundsen and<br />
H<strong>of</strong>fman 12 . In this study, majority <strong>of</strong> the<br />
isolates were gram- positive organisms<br />
(89.4%). Gram-negative organisms<br />
constituted 10.6%. Mixed infection was seen<br />
in 2 cases.<br />
Staphylococcus aureus (68.3%) was the<br />
commonest isolate comparable to studies by<br />
Gupta U and Bhattacharya AN 13 Ng<br />
Brajachand et al 14 and Dhawan et al 15 .<br />
However the relative rates <strong>of</strong> Staphylococcus<br />
aureus vary from centre to centre. Classen<br />
et al 16 reported as low as 16.3%.<br />
Staphylococcus aureus and Staphylococcus<br />
epidermidis are the 2 major pathogens<br />
responsible <strong>for</strong> most cases <strong>of</strong> osteomyelitis<br />
in the present study.<br />
There was no isolation <strong>of</strong> anaerobes. It could<br />
probably due to the fact that anaerobic<br />
organisms require very stringent conditions<br />
<strong>for</strong> isolation and transportation which could<br />
not always be maintained.<br />
Consistent susceptibility (100%) to<br />
Vancomycin is retained in this study. Most <strong>of</strong><br />
the isolates <strong>of</strong> Staphylococcus were sensitive<br />
to Erythromycin. All the Staphylococcal<br />
isolates showed resistance to methicillin.<br />
Onche I and Adedeji O 17 also reported<br />
Staphylococcus aureus completely resistant<br />
to oxacillin in a hospital setting and inferred<br />
that this was not unconnected with abuse <strong>of</strong><br />
antibiotics by the populace related to over the<br />
counter selling <strong>of</strong> antibiotics.<br />
44 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Among the gram-negative bacteria,<br />
Acinetobacter showed resistance to<br />
Ceftazidime, Ceftrixone, Cipr<strong>of</strong>loxacin and<br />
Co-trimoxazole. Agarwal AC et al 18 however<br />
reported ceftriaxone to be most effective<br />
antibiotic against gram-negative bacteria in<br />
contrast to this study. Overuse <strong>of</strong> broadspectrum<br />
antibiotics may be an important<br />
factor in building resistant strains.<br />
The antimicrobial sensitivity pattern differs in<br />
different studies and at different times. Many<br />
studies implied a high level <strong>of</strong> resistance to<br />
the commonly used antibiotics due to MRSA<br />
and ESBL producers resulting from<br />
indiscriminate and inappropriate use <strong>of</strong><br />
antibiotics. High occurrence <strong>of</strong> resistance is<br />
seen in surgical and orthopaedic patients due<br />
to overcrowding, workload and understaffing<br />
and where antibiotic usage is the greatest.<br />
Hence therapy should be initiated following<br />
antimicrobial susceptibility testing keeping in<br />
mind the condition <strong>of</strong> the patient, the side<br />
effects and practical considerations to prevent<br />
the acquisition and spread <strong>of</strong> resistant strains<br />
<strong>of</strong> the organisms.<br />
References<br />
1. Lidwell Om, Lowberry EJL and Whyte W.<br />
Bacteria isolated from deep joint sepsis after<br />
operation <strong>for</strong> total hip or knee replacement and<br />
the sources <strong>of</strong> infection with Staphylococcus<br />
aureus. I Hosp Infect. 1983; 4: 111.<br />
2. Ramon B. Gustilo. Evolving concepts in<br />
treatment <strong>of</strong> musculoskeletal sepsis,<br />
Orthopaedic inf ection- Diagnosis and<br />
treatment. 1 st Edn. Philadelphia: WB<br />
Saunders Company; 1989. p.1-6.<br />
3. Cleveland KB.General Principles <strong>of</strong> Infection,<br />
Campbell’s Orthopaedics. 10 th Edn.<br />
Philadelphia: Mosby; 2003. P.643-686.<br />
4. Jawetz E, Melnick JL and Adelberg EA. Cases<br />
and clinical correlations, Jawetz, Melnick and<br />
Adelberg’s <strong>Medical</strong> Microbioloby. 20 th Edn.<br />
New York: McGraw Hill; 1995.p.638-639.<br />
5. Schonholtz GJ, Borgia CA and Blair JD. Wound<br />
sepsis in orthopaedic surgery. J Bone Joint<br />
Surg Am. 1962; 44: 1548.<br />
6. Bhattacharya AN and Gupta U. Changing<br />
bacterial pattern in orthopaedic infections.<br />
Indian <strong>Journal</strong> <strong>of</strong> Orthopaedics. 1974; 8: 34-<br />
38.<br />
7. Resnick D. Osteomyelitis, Septic arthritis and<br />
S<strong>of</strong>t tissue infection, Resnick Diagnosis <strong>of</strong><br />
Bone and Joint Disorders. 4 th Edn.<br />
Philadelphia: WB Saunders Company;<br />
2002.p.2375-2377.<br />
8. Waldvogel FA, Med<strong>of</strong>f G and Swartz MN.<br />
Osteomyelitis: A review <strong>of</strong> clinical features,<br />
therapeutic considerations and unusual<br />
aspects. N. Engl. J. Med. 1970; 282: 198-206.<br />
9. Duthie and Nelson. Inf ection <strong>of</strong> the<br />
musculoskeletal system, Mercer’s<br />
Orthopaedic Surgery. 9 th Edn. Great Britain:<br />
Arnold; 1996.p.549-645.<br />
10. Mukhopadhyay B. Pyogenic haematogenous<br />
osteomyelitis: Acute and chronic, Textbook<br />
<strong>of</strong> Orthopaedics and Trauma. 1 st Edn. New<br />
Delhi: Jaypee Brothers; 1999.p.161-196.<br />
11. Vishwakarma and Lal. Changing bacterial flora<br />
in osteomyelitis. Archives <strong>of</strong> Med. Sciences.<br />
1970; 1: 55.<br />
12. Kundsen CJM and H<strong>of</strong>fman EB. Neonatal<br />
osteomyelitis. J Bone Joint Surg (Br). 1990;<br />
72-B: 846-57.<br />
13. Gupta U and Bhattacharya AN. Anaerobic<br />
organisms in osteomyelitis, Indian J. Surgery.<br />
1980; 1: 143.<br />
14. Brajachand Ng, Lokhendro H and Ibotomba<br />
Y. Bacteriological study <strong>of</strong> post-operative<br />
wound infections and antimicrobial<br />
susceptibility <strong>of</strong> the wound pathogens. <strong>Journal</strong><br />
<strong>of</strong> <strong>Medical</strong> Science. 1988; 11: 19-22.<br />
15. Dhawan B, Mohanty S, Das BK and Kapil A.<br />
Bacteriology <strong>of</strong> orthopaedic wound infections<br />
in an Indian Tertiary Care Hospital. Indian J<br />
Med Res. 2005; 121: 784-785.<br />
16. Classen DC, Sott Evans R and Pestonik SL.<br />
The timing <strong>of</strong> prophylactic administration <strong>of</strong><br />
antibiotics and the risk <strong>of</strong> surgical wound<br />
infection. N Engl J Med. 1992; 326: 281-285.<br />
17. Onche I and Adedeji O. Microbiology <strong>of</strong> postoperative<br />
wound infection in implant surgery.<br />
Nigerian <strong>Journal</strong> <strong>of</strong> Surgical Research. 2004;<br />
6: 37-40<br />
18. Agrawal AC, Jain S, Jain RK and Aza HKT.<br />
Pathogenic bacteria in an orthopaedic hospital<br />
in India. J infect Developing Countries. 2008;<br />
2(2): 120-123.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
45
ORIGINAL ARTICLE<br />
Attention deficit hyperactivity disorder (ADHD) in a school sample in Manipur<br />
1<br />
R.K. Lenin Singh, 2 S. Gojendra Singh, 3 L. Roshan Singh, 4 N. Heramani singh, 5 M. Akshyakumar Singh<br />
Abstract<br />
Objective: To find out the prevalence <strong>of</strong><br />
ADHD among the school children in a city<br />
school, Imphal, Manipur. Methods: A total <strong>of</strong><br />
312 students within the age range <strong>of</strong> 5-12<br />
years were evaluated by using Vanderbilt<br />
ADHD Diagnostic Teacher Rating Scale and<br />
Vanderbilt ADHD Diagnostic Parents Rating<br />
Scale. Results: The prevalence <strong>of</strong> ADHD was<br />
estimated to be 4.17% and the rate was higher<br />
among boys than girls with a percentage <strong>of</strong><br />
2.9% and 1.8% respectively. Conclusion:<br />
ADHD is common among the school children<br />
in Manipur.<br />
Keywords: Prevalence, attention deficit<br />
hyperactivity disorder, school children<br />
Introduction: Attention-deficit/hyperactivity<br />
disorder (ADHD) has defining features <strong>of</strong><br />
inattention, over activity, and impulsivity 1 . It is<br />
the most frequently encountered childhoodonset<br />
neurodevelopment disorder in primary<br />
care settings.<br />
Symptoms frequently co-occur with other<br />
emotional, behavioral, and learning problems,<br />
including oppositional defiant disorder,<br />
conduct disorder, depression, anxiety, and<br />
learning disabilities.<br />
1. Associate pr<strong>of</strong>essor, 2. Registrar, Dept. <strong>of</strong><br />
psychiatry, 3. Assistant Pr<strong>of</strong>essor, Dept. <strong>of</strong> Clinical<br />
Psychology, 4. Pr<strong>of</strong>essor & Head, Dept. <strong>of</strong><br />
Psychiatry 5. Pr<strong>of</strong>essor, Dept. <strong>of</strong> Clinical<br />
Psychology<br />
Correspondence: Dr. R.K.Lenin Singh, Associate<br />
Pr<strong>of</strong>essor, Department <strong>of</strong> Psychiatry, RIMS, Imphal<br />
Email Address: leninrk@yahoo.com<br />
Introduction: Attention-deficit/hyperactivity<br />
disorder (ADHD) has defining features <strong>of</strong><br />
inattention, over activity, and impulsivity 1 . It is<br />
the most frequently encountered childhoodonset<br />
neurodevelopment disorder in primary<br />
care settings. Symptoms frequently co-occur<br />
with other emotional, behavioral, and learning<br />
problems, including oppositional defiant<br />
disorder, conduct disorder, depression,<br />
anxiety, and learning disabilities. The National<br />
Institute <strong>of</strong> Mental Health (NIMH), estimates<br />
that between 3% and 5% <strong>of</strong> preschool and<br />
school-age children have ADHD or<br />
approximately two million children in the<br />
United States. This means in a class <strong>of</strong> 25 to<br />
30 students, it is likely that at least one student<br />
will have this common condition 2 . The cause<br />
<strong>of</strong> ADHD is unknown, and multiple pathways<br />
may lead to the phenotypic expression <strong>of</strong> the<br />
disorder 3 . Some studies suggest that genes<br />
play a large role. Like many other illnesses,<br />
ADHD probably results from a combination<br />
<strong>of</strong> factors. In addition to genetics, researchers<br />
are looking at possible environmental factors,<br />
and are studying how brain injuries, nutrition,<br />
and the social environment might contribute<br />
to ADHD. Results from several international<br />
studies <strong>of</strong> twins show that ADHD <strong>of</strong>ten runs<br />
in families. Researchers are looking at several<br />
genes that may make people more likely to<br />
develop the disorder 4,5 . Children with ADHD<br />
who carry a particular version <strong>of</strong> a certain gene<br />
have thinner brain tissue in the areas <strong>of</strong> the<br />
brain associated with attention. This National<br />
Institute <strong>of</strong> Mental Health (NIMH) research<br />
showed that the difference was not<br />
46 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
permanent, however, and as children with this<br />
gene grew up, the brain developed to a normal<br />
level <strong>of</strong> thickness. Their ADHD symptoms also<br />
improved. 6 Other studies suggest a potential<br />
link between cigarette smoking and alcohol<br />
use during pregnancy and ADHD in children. 7,8<br />
In addition, preschoolers who are exposed to<br />
high levels <strong>of</strong> lead, which can sometimes be<br />
found in plumbing fixtures or paint in old<br />
buildings, may have a higher risk <strong>of</strong> developing<br />
ADHD. 9 Children who have suffered a brain<br />
injury may show some behaviors similar to<br />
those <strong>of</strong> ADHD. However, only a small<br />
percentage <strong>of</strong> children with ADHD have<br />
suffered a traumatic brain injury. Recent<br />
British research indicates a possible link<br />
between consumption <strong>of</strong> certain food<br />
additives like artificial colors or preservatives,<br />
and an increase in activity. 10 Research is under<br />
way to confirm the findings and to learn more<br />
about how food additives may affect<br />
hyperactivity.<br />
Treatments can relieve many <strong>of</strong> the disorder’s<br />
symptoms, but there is no cure. With<br />
treatment, most people with ADHD can be<br />
successful in school and lead productive lives.<br />
Researchers are developing more effective<br />
treatments and interventions, and using new<br />
tools such as brain imaging, to better<br />
understand ADHD and to find more effective<br />
ways to treat and prevent it.<br />
Methods: A cross-sectional study design was<br />
used. Primary data was collected through<br />
personal interview method from both the<br />
teachers <strong>of</strong> the City Montessori Higher<br />
Secondary School, Imphal and parents <strong>of</strong> the<br />
children studying in the school. The<br />
interviewer read out a prepared script that<br />
provided an overview <strong>of</strong> the study aims and<br />
objectives and also benefits <strong>for</strong> participation<br />
were explained. All the students belonging to<br />
classes between I to VII with an age range <strong>of</strong><br />
5-12 years who were studying in the school<br />
were recruited. Based on purposive sampling<br />
technique, a sample <strong>of</strong> 312 children was<br />
selected. All the children were screened <strong>for</strong><br />
ADHD by using Vanderbilt ADHD Diagnostic<br />
Teacher Rating Scale 11 and Vanderbilt ADHD<br />
Diagnostic Parents Rating Scale. 11<br />
Sociodemographic data were collected using<br />
a semi-structured pro<strong>for</strong>ma and the diagnosis<br />
<strong>of</strong> ADHD was made using DSM-IV-TR<br />
criteria.<br />
Procedure: To proceed with the study,<br />
necessary permission was sought from the<br />
school authority. The teachers <strong>of</strong> the school<br />
were educated and trained about ADHD. One<br />
day training programme <strong>for</strong> the teachers on<br />
ADHD screening tool were conducted by a<br />
specialist in the field. In the programme, all<br />
the 18 criteria <strong>for</strong> ADHD in Vanderbilt Teacher<br />
rating Scale was discussed and explained one<br />
by one. After the training, teachers were asked<br />
to screen the school children belonging to<br />
class I to VII using the particular scale.<br />
The parents <strong>of</strong> the students were also<br />
educated about ADHD by organizing one day<br />
awareness programme <strong>for</strong> parents at schools.<br />
Parents were explained about the Vanderbilt<br />
Parents Rating Scale. The scale is the<br />
parents’ version <strong>of</strong> teachers rating scale which<br />
has all the 18 DSM-IV criteria <strong>for</strong> ADHD. The<br />
scale was further simplified and translated into<br />
Manipuri and back translated, so that parents<br />
could understand at ease. After that, parents<br />
were also asked to screen and rate the severity<br />
<strong>of</strong> each behavior on a 4 point Scale.<br />
Result: The present study was <strong>based</strong> on a<br />
primary sample <strong>of</strong> study subjects. For the<br />
particular school 312 students, both boys and<br />
girls were screened.<br />
Table 1. Students screened <strong>for</strong> ADHD by Teachers<br />
Class students students with positive positive<br />
screened ADHD boys girls<br />
I 28 4 2 2<br />
II 55 11 6 5<br />
III 53 1 1 0<br />
IV 47 0 0 0<br />
V 47 0 0 0<br />
VI 43 0 0 0<br />
VII 39 1 1 0<br />
TOTAL 312 17 (5.45%) 10 (3.23%) 7 (2.22%)<br />
Table 2. Student screened <strong>for</strong> ADHD by Parents<br />
Class student No. <strong>of</strong> No. <strong>of</strong> Negative Miss out Total No. <strong>of</strong><br />
screened boys girls students<br />
positive by positive <strong>of</strong><br />
teachers ADHD<br />
I 4 1 2 1 0 3<br />
II 11 6 3 2 0 9<br />
III 1 1 0 0 0 1<br />
IV 0 0 0 0 0 0<br />
V 0 0 0 0 0 0<br />
VI 0 0 0 0 0 0<br />
VII 1 0 0 0 1 0<br />
TOTAL 17 8 5 3 1 13<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
47
ORIGINAL ARTICLE<br />
Table 3. Student found positive <strong>for</strong> ADHD in both the<br />
settings<br />
Class No. <strong>of</strong> No. <strong>of</strong> boys No. <strong>of</strong> girls No. <strong>of</strong> student<br />
student found found positive <strong>of</strong><br />
screened positive positive ADHD in<br />
two settings<br />
I 28 1 2 3<br />
II 55 6 3 9<br />
III 53 1 0 1<br />
IV 47 0 0 0<br />
V 47 0 0 0<br />
VI 43 0 0 0<br />
VII 39 0 0 0<br />
TOTAL 312 8 (2.9%) 5 (1.8%) 13 (4.17%)<br />
Out <strong>of</strong> the 312 students belonging to classes<br />
from I to VII who were recruited and screened<br />
<strong>for</strong> the study (as shown in table-1). The data<br />
collected from teachers shown that out <strong>of</strong> 312<br />
students screened, 17 students were<br />
screened positive <strong>of</strong> ADHD with a percentage<br />
<strong>of</strong> 5.45%. Out <strong>of</strong> which 10 were boys and 7<br />
were girls with a percentage <strong>of</strong> 3.23% and<br />
2.22% respectively.. From the data collected<br />
by parents it was found that out <strong>of</strong> the 17<br />
positive students, 13 <strong>of</strong> them were again<br />
screened positive – 8 boys and 5 girls,<br />
whereas 3 <strong>of</strong> them were found negative and<br />
1 <strong>of</strong> the student could not be traced as he had<br />
already dropped out <strong>of</strong> the school. Special<br />
focus was given on the above mentioned 17<br />
positive students (shown in table – 2,3).<br />
Putting the above two data together, it was<br />
found that out <strong>of</strong> the total <strong>of</strong> 312 students<br />
screened, 13 students were diagnosed<br />
positive <strong>of</strong> ADHD. So, it stands that 4.17 % <strong>of</strong><br />
the students were affected by ADHD.<br />
Discussion: Besides providing in<strong>for</strong>mation<br />
that can be compared with the child’s behavior<br />
at home, school setting can be used as an<br />
alternative setting <strong>for</strong> carrying out interventions<br />
and allows sampling <strong>of</strong> a broader spectrum<br />
and area <strong>of</strong> behavior. 12 Moreover, externalizing<br />
problems get reported more <strong>of</strong>ten by teachers<br />
and internalizing problems more <strong>of</strong>ten by the<br />
parents. 13 Keeping these views in mind, school<br />
was chosen as a plat<strong>for</strong>m to obtain samples<br />
<strong>for</strong> study. This has been done in several other<br />
studies. 14, 15. The sample consisting <strong>of</strong> 312<br />
children that were screened comprised <strong>of</strong> an<br />
almost equal proportion <strong>of</strong> girls and boys. This<br />
ensured proportional representation <strong>of</strong> both<br />
sexes. In the present study, in<strong>for</strong>mation from<br />
child, teacher and parents was used and the<br />
interviewer’s best judgment was applied to<br />
arrive at a final conclusion.<br />
The prevalence <strong>of</strong> ADHD in the current study<br />
was found to be 4.17 %. Though, the finding<br />
was agreed with several other studies. Studies<br />
by Kashani et al., 16 Cohen et al. 17 and<br />
Deivasigamani 14 have found higher rates while<br />
that by Esser et al 18 revealed lower rate <strong>of</strong><br />
prevalence. This difference could be attributed<br />
to variations in age group, in<strong>for</strong>mants,<br />
diagnostic system, diagnostic tools and<br />
sampling techniques. The higher rate <strong>of</strong> ADHD<br />
among boys than girls were similar to findings<br />
<strong>of</strong> Rutter et al., 19 and Of<strong>for</strong>d et al 20 .<br />
Conclusion: ADHD is not uncommon in<br />
school going children in Manipur. It is a barrier<br />
in the effective management <strong>of</strong> children at<br />
school and home. And yet many <strong>of</strong> the parents<br />
and teachers are not aware <strong>of</strong> the same.<br />
Present study could bring up awareness<br />
among the teachers and parents.<br />
Limitations: The present study had certain<br />
limitations. Inherent disadvantages <strong>of</strong><br />
sampling in schools remained. Subjects with<br />
severe ADHD, being probable school<br />
dropouts, were automatically left out. Certain<br />
socio-demographic and clinical variables<br />
such as peer adjustment, environment in<br />
neighborhood, parenting style and intelligence,<br />
which were not probed, kept room <strong>for</strong> future<br />
improvement.<br />
References<br />
1. American Psychiatric Association.<br />
Diagnostic and Statistical Manual <strong>of</strong> Mental<br />
Disorders. 4th ed. Washington, DC:<br />
American Psychiatric Association; 1994<br />
2. National Institute <strong>of</strong> Mental Health.<br />
“Attention Deficit Hyperactivity Disorder.”<br />
Department <strong>of</strong> Health and Human<br />
Services. National Institutes <strong>of</strong> Health.<br />
2006.<br />
48 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
3. National Institutes <strong>of</strong> Health. Diagnosis<br />
and Treatment <strong>of</strong> Attention-Deficit/<br />
Hyperactivity Disorder. Washington, DC:<br />
US Government Printing Office; 1998.<br />
4. Faraone SV, Perlis RH, Doyle AE, Smoller<br />
JW, Goralnick JJ, Holmgren MA, Sklar P.<br />
Molecular genetics <strong>of</strong> attention-deficit/<br />
hyperactivity disorder. Biological<br />
Psychiatry, 2005; 57:1313-1323.<br />
5. Khan SA, Faraone SV. The genetics <strong>of</strong><br />
attention-deficit/hyperactivity disorder: A<br />
literature review <strong>of</strong> 2005. Current<br />
Psychiatry Reports, 2006; 8:393-397.<br />
6. Shaw P, Gornick M, Lerch J, Addington A,<br />
Seal J, Greenstein D, Sharp W, Evans A,<br />
Giedd JN, Castellanos FX, Rapoport JL.<br />
Polymorphisms <strong>of</strong> the dopamine D4<br />
receptor, clinical outcome and cortical<br />
structure in attention-deficit/hyperactivity<br />
disorder. Archives <strong>of</strong> General Psychiatry,<br />
2007; 64(8):921-931.<br />
7. Linnet KM, Dalsgaard S, Obel C, Wisborg<br />
K, Henriksen TB, Rodriguez A, Kotimaa<br />
A, Moilanen I, Thomsen PH, Olsen J,<br />
Jarvelin MR. Maternal lifestyle factors in<br />
pregnancy risk <strong>of</strong> attention-deficit/<br />
hyperactivity disorder and associated<br />
behaviors: review <strong>of</strong> the current evidence.<br />
American <strong>Journal</strong> <strong>of</strong> Psychiatry, 2003;<br />
160(6):1028-1040.<br />
8. Mick E, Biederman J, Faraone SV, Sayer<br />
J, Kleinman S. Case-control study <strong>of</strong><br />
attention-deficit hyperactivity disorder and<br />
maternal smoking, alcohol use, and drug<br />
use during pregnancy. <strong>Journal</strong> <strong>of</strong> the<br />
American Academy <strong>of</strong> Child and<br />
Adolescent Psychiatry, 2002; 41(4):378-<br />
385.<br />
9. Braun J, Kahn RS, Froehlich T, Auinger<br />
P, Lanphear BP. Exposures to<br />
environmental toxicants and attentiondeficit/hyperactivity<br />
disorder in U.S.<br />
children. Environmental Health<br />
Perspectives, 2006; 114(12):1904-1909.<br />
10. McCann D, Barrett A, Cooper A, Crumpler<br />
D, Dalen L, Grimshaw K, Kitchin E, Lok<br />
E, Porteous L, Prince E, Sonuga-Barke<br />
E, Warner JO. Stevenson J. Food additives<br />
and hyperactive behaviour in 3-year-old<br />
and 8/9-year-old children in the<br />
community: a randomised, doubleblinded,<br />
placebo-controlled trial. Lancet,<br />
2007; 370 (9598):1560-1567.<br />
11. Wolraich ML, Feurer ID, Hannah JN.<br />
Obtaining systematic teacher reports <strong>of</strong><br />
disruptive behavior disorders utilizing<br />
DSM-IV. <strong>Journal</strong> <strong>of</strong>Abnormal Child<br />
Psychology, 1998; 26(2):141–152.<br />
12. Malhotra S. Child psychiatry in India: An<br />
approach to assessment and<br />
management <strong>of</strong> childhood psychiatric<br />
disorders. New Delhi: Macmillan India;<br />
2002.<br />
13. Banerjee T. Psychiatric morbidity among<br />
rural primary school children in West<br />
Bengal. Indian J Psychiatry, 1997; 39:<br />
1305.<br />
14. Deivasigamani TR. Psychiatric morbidity<br />
in primary school children: An<br />
epidemiological study. Indian J Psychiatry<br />
1990; 32:235-40.<br />
15. Of<strong>for</strong>d DR, Boyle MH, Szatmari P. Ontario<br />
Child Health Study-II. Six month<br />
prevalence <strong>of</strong> disorder and rates <strong>of</strong><br />
service utilization. Arch Gen Psychiatry<br />
1987; 44: 832-6.<br />
16. Kashani JH, Daniel AE, Sulzberger LA.<br />
Conduct disordered adolescents from a<br />
community sample. Can J Psychiatry<br />
1987; 32: 756-60.<br />
17. Cohen P, Cohen J, Kasen S. An<br />
epidemiological study <strong>of</strong> disorders in late<br />
childhood and adolescence-I: Age- and<br />
genderspecific prevalence. J Child<br />
Psychol Psychiatry, 1993; 34: 85167.<br />
18. Esser G, Schmidt MH, Woerner W.<br />
Epidemiology and course <strong>of</strong> psychiatric<br />
disorders in school-age children-results<br />
<strong>of</strong> a longitudinal study. J Child Psychol<br />
Psychiatry, 1990; 31: 243-63.<br />
19. Feehan M, McGee R, Raja SN, et al. DSM-<br />
III-R disorders in New Zealand 18-yearolds.<br />
Aust N Z J Psychiatry 1994;28: 87-<br />
99.<br />
20. Rutter M, Tizard J, Whitmore K.<br />
Education, health and behavior. London:<br />
Longmans; 1970.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
49
ORIGINAL ARTICLE<br />
Clinical and endoscopic studies <strong>of</strong> dysphagia<br />
1<br />
G.S. Moirangthem, 2 Ch. Arun Kumar Singh, 3 Dathiadiam Tongper, 3 Dacto Gara<br />
Abstract<br />
Objective: The aim and objective <strong>of</strong> the<br />
present study was to evaluate the nature and<br />
frequency <strong>of</strong> different upper gastrointestinal<br />
conditions leading to dysphagia and to study<br />
the diagnostic potential <strong>of</strong> upper<br />
gastrointestinal endoscopy in relation with<br />
clinical symptoms. Methods: The present<br />
study was conducted in Surgical<br />
Gastroenterology and Minimal Access Surgery<br />
Unit, Department <strong>of</strong> Surgery, RIMS, Imphal,<br />
Manipur over the period <strong>of</strong> twenty four month<br />
(September 2008 to September 2010). The<br />
study population consisted <strong>of</strong> 50 patients<br />
presenting with dysphagia at our OPD or<br />
referred to our unit from various departments<br />
<strong>for</strong> endoscopic evaluation <strong>for</strong> dysphagia<br />
irrespective <strong>of</strong> age, sex, marital status, social<br />
caste, religion. Results: There was male<br />
preponderance <strong>of</strong> 56% (28 pts) as against<br />
44% (22 pts) <strong>of</strong> his female counterpart. The<br />
average age <strong>of</strong> the patients in the sample (n<br />
= 50) was 53± years. Nineteen patients out <strong>of</strong><br />
50 patients were associated with a recent<br />
significant weight loss, rest 31 patients does<br />
not have any weight loss. Significant,<br />
1. Pr<strong>of</strong>essor & Head; 2. Associate Pr<strong>of</strong>essor;<br />
3. PGT, Surgical Gastroenterology & Minimal<br />
Access Surgery Unit, RIMS, Imphal-795004,<br />
Manipur (INDIA)<br />
Corresponding author:<br />
Dr. Ch. Arun Kumar Singh, Surgical<br />
Gastroenterology & Minimal Access Surgery Unit,<br />
RIMS, Imphal-795004, Manipur e-mail:<br />
drcharun@yahoo.com<br />
Lymphadenopathy was found in 7 patients<br />
only. Endoscopic Biopsy <strong>for</strong> HPE was down<br />
in 16 out <strong>of</strong> 50 patients who were suspected<br />
<strong>of</strong> having Carcinoma <strong>of</strong> esophagus and<br />
carcinoma <strong>of</strong> oropharynx.<br />
Out <strong>of</strong> the sample <strong>of</strong> 50 patients presenting<br />
with dysphagia and associated complaints,<br />
10 patients (20%) were diagnosed as<br />
superficial esophagitis on upper GI<br />
endoscopy, in 10 patients (20%) no obvious<br />
pathological findings were demonstrated<br />
(Normal findings) and fourteen cases <strong>of</strong><br />
carcinoma (6 Ca. esophagus, 5 Ca.<br />
oropharynx and 3 Ca. stomach), 5 cases <strong>of</strong><br />
benign esophageal stricture (corrosive<br />
stricture), 5 cases <strong>of</strong> Grade III & IV esophageal<br />
varices, 2 cases <strong>of</strong> GERD, 3 achalasia, 1 case<br />
<strong>of</strong> hiatus hernia were detected.<br />
Conclusion: The present study shows that<br />
Upper GI endoscopy in conjunction with HPE<br />
and barium X ray is a good diagnostic modality<br />
in evaluating a case <strong>of</strong> dysphagaia. Different<br />
cases <strong>of</strong> dysphagia in a limited number <strong>of</strong> 50<br />
patients were evaluated.<br />
Keywords: Dysphagia, Upper GI Endoscopy<br />
and dysphagia, Barium swallow and<br />
dysphagia<br />
Introduction: Dysphagia is a Greek word and<br />
means ‘disordered eating’. Dysphagia<br />
typically refers to difficulty in eating as a result<br />
<strong>of</strong> disruption in the swallowing process.<br />
Dysphagia may be caused by a variety <strong>of</strong><br />
upper GI conditions, it can be divided into high<br />
and low causes.<br />
50 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
High causes may be:<br />
Neurological<br />
• Stroke<br />
• Parkinsons disease<br />
• Cranial nerve palsy or bulbar palsy<br />
(such as multiple sclerosis, motor<br />
neurone disease)<br />
Anatomical or muscular<br />
• Myasthenia gravis<br />
• Oropharyngeal malignancy<br />
• Cricopharyngeal spasm<br />
• Pharyngeal pouch<br />
Low causes (oesophagial)<br />
• Carcinoma oesophagus<br />
• Reflux disease with or without stricture<br />
• Motility disturbance (such as<br />
achalasia, scleroderma, or<br />
oesophageal spasm)<br />
There are several diagnostic investigations<br />
available to evaluate dysphagia, including<br />
upper gastrointestinal radiography and<br />
endoscopy. OGD is an effective and an<br />
appropriate tool <strong>for</strong> the evaluation <strong>of</strong> patients<br />
presenting with dysphagia. Early OGD should<br />
be considered particularly in male patients ><br />
40 years old with dysphagia which <strong>of</strong>ten leads<br />
to the therapeutic intervention even in quite<br />
frail subjects.<br />
Materials and Methods: The study was<br />
conducted in the Surgical Gastroenterology<br />
and Minimal Access Surgery Unit, Department<br />
<strong>of</strong> Surgery, RIMS, Imphal, Manipur over a<br />
period <strong>of</strong> twenty four month (September 2008<br />
to September 2010) and included patients<br />
presenting with dysphagia. Be<strong>for</strong>e including<br />
the patients in the study group in<strong>for</strong>med written<br />
consent was taken. A detailed clinical history<br />
was taken <strong>for</strong> each and every case. A thorough<br />
general, physical and systematic examination<br />
was done using a predesigned pro<strong>for</strong>ma.<br />
Investigations like blood routine examination,<br />
X-ray chest, LFT etc. were also included.<br />
Patients presenting with dysphagia<br />
irrespective <strong>of</strong> age, sex, marital status, social<br />
caste, religion etc were also included.<br />
Patients presenting with dysphagia<br />
irrespective <strong>of</strong> age, sex, marital status, social<br />
caste, religion etc. were included in the study.<br />
The cases were subjected to esophagogastroscopy<br />
under local anaesthesia, findings<br />
were noted and endoscopic biopsy was taken<br />
from any suspicious lesions. Barium swallow<br />
and meal wear also advised if necessary and<br />
the final diagnosis were made after reviewing<br />
those HPE reports and barium series.<br />
Results: Average age <strong>of</strong> the patients <strong>of</strong><br />
sample (n=50) in the study was 53 years, with<br />
a minimum and maximum <strong>of</strong> 25 years and 78<br />
years and age range <strong>of</strong> 53 years. There was<br />
male preponderance <strong>of</strong> 56% as against 44%<br />
<strong>of</strong> his female counterpart in this study.<br />
Most <strong>of</strong> the patients had mean duration <strong>of</strong><br />
onset <strong>of</strong> symptoms <strong>of</strong> 2-3 months. Significant<br />
weight loss was associated in 19 patients and<br />
clinically apparent lymphadenopathy found in<br />
only 7 patients. (Table 1)<br />
Table 1: Clinical pr<strong>of</strong>iles<br />
Parameters Numbers (50)<br />
Duration <strong>of</strong> the symptoms 1 month 10<br />
2-3 months 29<br />
> 4 months 11<br />
Significant wt lossPresent 19<br />
Absent 31<br />
Lymphadenopathy Present 7<br />
Absent 43<br />
Esophagogastroduodenoscopy per<strong>for</strong>med,<br />
endoscopic biopsy <strong>for</strong> HPE were done in 16<br />
out <strong>of</strong> 50 patients who were suspected <strong>of</strong><br />
carcinoma <strong>of</strong> esophagus and carcinoma <strong>of</strong><br />
oropharynx and barium swallow studies <strong>for</strong><br />
16 patients. (Table 2)<br />
Table2: Endoscopy with associated interventions<br />
Parameter<br />
Numbers (n=50)<br />
Endoscopy per<strong>for</strong>med 50<br />
Endoscopy with biopsy 16<br />
Endoscopy with barium studies 16<br />
Superficial esophagitis and normal findings<br />
were the commonest findings demonstrated<br />
in Upper GI endoscopy 10 patients each in<br />
our study, commonly seen in 40 to 70 years.<br />
(Table 3)<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
51
ORIGINAL ARTICLE<br />
Table 3: Endoscopy findings and provisional<br />
diagnosis<br />
Diagnosis<br />
(Endoscopically)<br />
Total<br />
Carcinoma <strong>of</strong> esophagus 6<br />
Carcinoma <strong>of</strong> stomach 3<br />
(GE junction)<br />
Superficial esophagitis 10<br />
Corrosive stricture 5<br />
Esophageal varices Gr III & IV 5<br />
Carcinoma oropharynx 5<br />
GERD 2<br />
Achalasia 3<br />
Normal study 10<br />
Pharyngeal pouch/Hiatus Hernia 1<br />
Total 50<br />
Final diagnosis was made by collaborating the<br />
endoscopic findings with the barium study<br />
report and histophathodological reports.<br />
Table 4: Final diagnosis<br />
Final Diagnosis<br />
Total<br />
Carcinoma <strong>of</strong> stomach 3<br />
(GE junction)<br />
Carcinoma <strong>of</strong> esophagus 6<br />
Superficial esophagitis 10<br />
Corrosive stricture 5<br />
Esophageal varices Gr III & IV 5<br />
Carcinoma oropharynx 5<br />
GERD 2<br />
Achalasia 3<br />
Normal study 10<br />
Pharyngeal pouch/Hiatus Hernia 1<br />
Total 50<br />
Out <strong>of</strong> the sample <strong>of</strong> 50 patients presenting<br />
with dysphagia and associated complaints,<br />
10 patients (20%) were diagnosed as<br />
Superficial esophagitis on upper GI<br />
endoscopy, in 10 patients (20%) no obvious<br />
pathological findings were demonstrated<br />
(Normal findings), fourteen cases <strong>of</strong><br />
carcinoma (6 Ca. esophagus, 5 Ca.<br />
oropharynx and 3 Ca. stomach), 5 cases <strong>of</strong><br />
benign esophageal stricture (Corrosive<br />
stricture), 5 cases <strong>of</strong> grade III & IV esophageal<br />
varices, 2 cases <strong>of</strong> GERD, 3 achalasia and 1<br />
case <strong>of</strong> hiatus hernia. (Table 3)<br />
Discussion: Dysphagia, an important<br />
alarming symptom especially when<br />
associated with other upper gastrointestinal<br />
symptoms like dyspepsia, chronic<br />
gastrointestinal bleeding, progressive<br />
unintentional weight loss, persistent vomiting,<br />
iron deficiency anemia or epigastric mass.<br />
Dysphagia needs to be investigated on an<br />
urgent basis to establish a diagnosis early in<br />
the course <strong>of</strong> the patient’s management and<br />
to rule out any ongoing serious pathology such<br />
as a neoplastic process. A detailed medical<br />
history and clinical examination is the key to<br />
rule out various causes <strong>of</strong> dysphagia. Several<br />
diagnostic investigations are available to<br />
evaluate dysphagia, like upper gastrointestinal<br />
endoscopy, contrast imaging studies and<br />
manometeric studies.<br />
Several studies have been done to find the<br />
diagnostic potential <strong>of</strong> esophagogastroduodenscopy<br />
in evaluating dysphagia.<br />
Varadarajulu Shyam et al 1 conducted a study<br />
on a total <strong>of</strong> 1649 patients with dysphagia.<br />
(mean age 56.7 years, M:F=3:2). Abnormal<br />
findings at OGD were found in 70% (1150) <strong>of</strong><br />
the patients and a major pathology was seen<br />
in 54% (898). Cancer was found in 4% (70) <strong>of</strong><br />
the patients and was predicted by male<br />
gender, age and weight loss. The esophagus<br />
was normal in 29% (483) <strong>of</strong> patients.<br />
Nafees A Quereshi et al 2 also reported<br />
esophagus was abnormal in 678 cases<br />
(74%). Superficial esophagitis, Barrett’s<br />
esophagus, esophageal cancer and<br />
esophageal ulcer were main histological<br />
findings. Ahmed et al 3 reported in a survey <strong>of</strong><br />
120 consecutive endoscopies on elderly<br />
patients with suspected obstructive dysphagia.<br />
Seventy eight patients had positive findings.<br />
Benign structure <strong>of</strong> the esophagus was the<br />
commonest findings; fifteen patients had<br />
upper GI malignancy (12 esophagus and 3<br />
stomach). Six patients with negative<br />
endoscopies had established by other means<br />
and in 14 no cause was not identified. Thus<br />
they concluded that upper gastro intestinal<br />
endoscopy is a safe and valuable procedure<br />
in elderly patients with dysphagia and <strong>of</strong>ten<br />
52 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
leads to positive therapeutic interventions even<br />
in quite frail subjects.<br />
Stephen M wildi et al 4 in a study <strong>of</strong> total 175<br />
patients with worsening symptoms <strong>of</strong> ongoing<br />
reflux per<strong>for</strong>med upper GI endoscopy. Major<br />
esophageal finding were discovered in 95<br />
patients, in 10 patients major gastric or<br />
duodenal findings were detected as follows:<br />
erosive gastritis (n=8), gastric ulcer (n=2),<br />
duodenal ulcer (n=2), erosive duodenitis<br />
(n=2), and duodenal polyp (n=1).<br />
Gupta SD et al 5 conducted a study on<br />
endoscopic evaluation <strong>of</strong> dysphagia in the<br />
elderly. A survey <strong>of</strong> 100 consecutive<br />
endoscopies on elderly patients with<br />
suspected obstructive dysphagia is reported.<br />
Seventy eight patients had positive findings<br />
<strong>of</strong> 1 to 3 lesions. Benign structure <strong>of</strong> the<br />
esophagus was the commonest findings and<br />
15 patients had upper GI malignancy. Six<br />
patients with negative endoscopies had<br />
diagnosis established by other means and in<br />
14 patients, no cause could be identified. The<br />
study concluded that upper GI endoscopy is<br />
a safe and valuable procedure in elderly<br />
patients and <strong>of</strong>ten leads to positive therapeutic<br />
intervention even in quite frail subjects.<br />
In our series <strong>of</strong> 50 cases, superficial<br />
esophagitis, followed by carcinoma<br />
esophagus, corrosive stricture, esophageal<br />
varices Gr-III & IV and carcinoma oropharynx.<br />
In 10 patients (20%) no abnormality were<br />
detected, superficial esophagitis 10 patients<br />
(20%), Carcinoma <strong>of</strong> esophagus was found<br />
in 6 patients (12%), Corrosive stricture in 5<br />
patients (10%), Esophageal varices Gr-III &<br />
IV in 5 patients (10%), Carcinoma oropharynx<br />
in 5 patients (10%), carcinoma <strong>of</strong> stomach in<br />
3 patients (6%), GERD 2 patients (4%),<br />
Achalasia 3 patients (6%) and hiatus hernia<br />
in 1 patient (2 %).<br />
Conclusion: The study shows that Upper GU<br />
endoscopy is a good diagnostic modality in<br />
evaluating a case <strong>of</strong> dysphagia. It has the<br />
advantage <strong>of</strong> direct vision <strong>of</strong> the lesion and<br />
tissue biopsy if required <strong>for</strong> histopathological<br />
examination. The commonest cause <strong>of</strong><br />
dysphagia in patients presenting at RIMS<br />
surgical OPD was superficial esophagitis<br />
followed by carcinoma <strong>of</strong> esophagus and<br />
carcinoma <strong>of</strong> oropharynx respectively.<br />
Malignancy was associated with significant<br />
loss <strong>of</strong> weight and lymphadenopathy. The<br />
normal study on the UGI endoscopy in the 10%<br />
patients having dysphagia is also another<br />
notable and significant finding <strong>of</strong> the study.<br />
These groups <strong>of</strong> patients may require further<br />
psychiatric evaluation. There<strong>for</strong>e, while<br />
evaluating a case <strong>of</strong> dysphagia consideration<br />
<strong>for</strong> endoscopy should be correlated with<br />
clinical examination.<br />
References<br />
1. Shyam Varadarajulu, Mohamad A.<br />
Eloubeidi, Rig S. Patel, Hugh E.<br />
Mulcahy, Alan Barkun, Paul Jowell et<br />
al. The yield and the predictors <strong>of</strong><br />
esophageal pathology when upper<br />
endoscopy is used in the initial<br />
evaluation <strong>of</strong> dysphagia. American<br />
<strong>Journal</strong> <strong>of</strong> Surgery 2005; 61:804-808.<br />
2. Nafees A Qureshi, Micheal T Hallissey<br />
ad John W Fielding. Outcome <strong>of</strong> index<br />
upper gastrointestinal endoscopy in<br />
patients presenting with dysphagia in<br />
a tertiary care hospital. BMC<br />
Gastroenterology 2007; 7:43.<br />
3. Ahmed, Petrus FJ, Dellipiani AW.<br />
Endoscopic evaluation <strong>of</strong> dysphagia in<br />
elderly. BMC surgery 2001;16:159-<br />
164.<br />
4. Stephen M Weldi, Tammy F Glenn,<br />
Robert F Woolson, Wei Wang<br />
Roberts H Hawes, Micheal B Wallace.<br />
Is esophagoscopy alone sufficient <strong>for</strong><br />
patients with reflux symptoms?<br />
Gatrointestinal Endoscopy 2004<br />
March; 59:349-354.<br />
5. Gupta SD, LV Petrus, FJ Gibbins and<br />
AW Dellipiani. Endoscopic Evaluation<br />
<strong>of</strong> Dysphagia in the Elderly. Ox<strong>for</strong>d<br />
<strong>Journal</strong>s 1987; 16:159-164.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
53
ORIGINAL ARTICLE<br />
Effect <strong>of</strong> ethyl acetate extract <strong>of</strong> black catechu (Acacia catechu) on oral glucose<br />
tolerance and hydrocortisone induced hyperglycemia<br />
1<br />
Ng. Gunindro, 2 Lakshman Das, 3 Kh. Krishna Pramodini, 4 Th. Imoba Singh<br />
Abstract<br />
Objective: To evaluate effects <strong>of</strong> ethyl acetate<br />
extract <strong>of</strong> black catechu (Acacia catechu) on<br />
oral glucose tolerance and hydrocortisone<br />
induced hyperglycemia in an attempt to<br />
explore the possible mechanisms <strong>of</strong><br />
hypoglycemic activity <strong>of</strong> Acacia catechu, a<br />
plant reported to possess hypoglycemic<br />
property. Methods: Ethyl acetate extract <strong>of</strong><br />
black catechu (Acacia catechu) was orally<br />
tested at the doses <strong>of</strong> 250 and 500 mg/kg <strong>for</strong><br />
hypoglycemic activity in normal and alloxan<br />
induced hyperglycemic rats. Using the same<br />
doses, effects <strong>of</strong> the extract on oral glucose<br />
tolerance and hydrocortisone induced<br />
hyperglycemia were evaluated. In all the<br />
studies, the results <strong>of</strong> the extract treated<br />
groups were compared with those <strong>of</strong> the<br />
control and standard groups. The results were<br />
analysed <strong>for</strong> statistical significance. Results:<br />
The extract showed hypoglycemic activity. It<br />
reduced hydrocortisone induced hyperglycemia<br />
but not the hyperglycemia after oral<br />
glucose load. Conclusion: Reduction <strong>of</strong><br />
hydrocortisone induced hyperglycemia by the<br />
ethyl acetate extract <strong>of</strong> black catechu<br />
Affiliations:<br />
1. Asst. pr<strong>of</strong>., Dept. <strong>of</strong> Pharmacology, RIMS, Imphal,<br />
2. Asst. pr<strong>of</strong>., Dept. <strong>of</strong> Pharmacology, Tripura<br />
<strong>Medical</strong> College & Dr. B.R. Ambedkar Teaching<br />
Hospital, Hapania, Agartala, 3. Pr<strong>of</strong>essor Dept. <strong>of</strong><br />
Pharmacology RIMS, 4. Pr<strong>of</strong>. and Head, Dept. <strong>of</strong><br />
Pharmacology, JNIMS, Imphal<br />
Address <strong>for</strong> correspondence:<br />
Ngangom Gunindro, Asst. pr<strong>of</strong>essor, Dept. <strong>of</strong><br />
Pharmacology, RIMS, Imphal PIN – 795004<br />
Email: pharrims @yahoo.co.in<br />
(Acacia catechu) suggested the possibility <strong>of</strong><br />
inhibition <strong>of</strong> hepatic gluconeogenesis as one<br />
<strong>of</strong> the mechanisms contributing to its<br />
hypoglycemic activity.<br />
Key words: Black catechu, alloxan, oral<br />
glucose tolerance. hydrocortisone induced<br />
hyperglycemia<br />
Introduction: Black catechu (Kattha in Hindi)<br />
or cutch is an aqueous extract prepared from<br />
the heart wood <strong>of</strong> Acacia catechu Willd<br />
(Family – Leguminosae) and is mainly used<br />
as an ingredient <strong>of</strong> paan and paan masala. 1<br />
The plant Acacia catechu is a small thorny<br />
tree <strong>of</strong> up to 12 m in height, with crooked stem,<br />
straggling branches, compound, feathery<br />
leaves and pale yellow, fluffy flowers in dense<br />
heads. This tree is found in India, Burma,<br />
Thailand and China. In India, it is grown as a<br />
multipurpose tree in <strong>for</strong>estation schemes in<br />
dry parts <strong>of</strong> the country. The black catechu<br />
extract is used to a limited extent against<br />
diarrhoea, dysentery, chronic catarrh,<br />
haemorrhage and mouth inflammation. The<br />
diluted <strong>for</strong>m is employed as gargle <strong>for</strong> sore<br />
throat, mouth and gum infections. Externally,<br />
it is applied to boils and ulcers. 2 Black catechu<br />
is odourless, light brown to black, friable and<br />
porous cake. 3 It contains catechin isomers,<br />
acacatechin (2-12%), catechu tannic acid or<br />
phlobatannin (25-35%), gum (20-30%),<br />
quercitrin, quercetin, catechu red and water, 1<br />
and tastes first somewhat bitter and<br />
afterwards sweetish. 4<br />
Acacia catechu is reported to show activities<br />
like hepatoprotective, 5,6,7 antidiarrhoeal,<br />
antipyretic ,7 and hypoglycemic. 7,8 However,<br />
54 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
there is hardly any study where the<br />
hypoglycemic action has been explored<br />
further to establish the mechanism <strong>of</strong> action.<br />
The present study is undertaken using ethyl<br />
acetate extract <strong>of</strong> black catechu (EBC) to<br />
reassess the hypoglycemic activity both in<br />
normal and hyperglycemic albino rats. Studies<br />
have been taken up to evaluate effects on oral<br />
glucose tolerance (OGT) and on<br />
glucocorticoid induced hyperglycemia. The<br />
study protocol is approved by the Institutional<br />
Animal Ethics Committee, and the study is<br />
carried out in the Department <strong>of</strong><br />
Pharmacology, RIMS, Imphal.<br />
Materials and Methods: Animals: Healthy<br />
Wistar albino rats <strong>of</strong> either sex (110-150 g)<br />
were used in the present study. The animals<br />
were housed in standard rat cages and<br />
maintained on standard diet with free access<br />
to water. They were acclimatized at room<br />
temperature with natural light-dark cycle <strong>for</strong> 7<br />
days in the departmental animal house. The<br />
animals described as fasted, were deprived<br />
<strong>of</strong> food <strong>for</strong> 18 h with due care to prevent<br />
coprophagy, but with free access to water.<br />
Plant material and extract preparation:<br />
Black catechu (Kattha) was collected from the<br />
local market. It was identified and differentiated<br />
from pale catechu (Uncaria gambier), a<br />
closely alike preparation by Gambier fluorescin<br />
test. 3,4 Powdered catechu was defatted with<br />
petroleum ether (B.P 40 - 60 o C) in soxhlet<br />
apparatus and spread out to evaporate<br />
petroleum ether. The dried defatted product<br />
was repacked and extracted with 95% ethanol<br />
until the eluent was colourless. Dried ethanol<br />
extract was again extracted with ethyl<br />
acetate. 6 The ethyl acetate extract was spread<br />
on the drying tray and kept <strong>for</strong> use in the study.<br />
The yield at the end <strong>of</strong> the extraction was 4.5%.<br />
Dose <strong>of</strong> test drug: The LD 50<br />
<strong>of</strong> ethyl acetate<br />
extract <strong>of</strong> Acacia catechu in mice was<br />
reported to be 2500 mg/kg. 6 The LD 50<br />
<strong>of</strong> the<br />
extract in rats as calculated by extrapolation<br />
method 9 was 1750 mg/kg. Two doses <strong>of</strong> 250<br />
and 500 mg/kg <strong>of</strong> the extract were used as<br />
suspensions in 2% aqueous gum acacia and<br />
given per orally as single doses.<br />
Blood sample collection and glucose<br />
estimation: Blood samples were collected<br />
from orbital sinus puncture by using capillary<br />
tubes. 9 The samples were allowed to settle<br />
<strong>for</strong> 30 minutes, and then centrifuged at 2000<br />
rpm <strong>for</strong> 20 minutes. 6 The serum glucose<br />
estimation was done by enzymatic<br />
colorimetric test using commercial assay kit<br />
(Human, Germany).<br />
Induction <strong>of</strong> hyperglycemia: A single dose<br />
<strong>of</strong> 120 mg/kg s.c 10,11 <strong>of</strong> freshly prepared<br />
alloxan monohydrate (Sigma Ltd, USA)<br />
dissolved in normal saline was used <strong>for</strong><br />
induction <strong>of</strong> hyperglycemia in fasted healthy<br />
albino rats. The animals were fed on standard<br />
diet and water ad libitum. The induction <strong>of</strong><br />
hyperglycemia was confirmed 48 h after<br />
alloxan administration by blood glucose<br />
estimation, and rats showing blood glucose<br />
levels <strong>of</strong> 300-350 mg/dl were used <strong>for</strong><br />
evaluation <strong>of</strong> the effect the test substance on<br />
blood glucose in hyperglycemic rats.<br />
Effect <strong>of</strong> ethyl acetate extract <strong>of</strong> black<br />
catechu (EBC) on blood glucose in normal<br />
rats: To evaluate the effect <strong>of</strong> EBC on blood<br />
glucose, the method <strong>of</strong> Babu V et al. 12 was<br />
followed. The healthy albino rats <strong>of</strong> either sex<br />
weighing 110 – 150 g were divided into four<br />
groups – I (control) II, III and IV (standard) <strong>of</strong><br />
six rats in each group. After fasting <strong>for</strong> 18 h,<br />
the rats in group I received 2% aqueous gum<br />
acacia suspension at the dose <strong>of</strong> 10 ml/ kg.<br />
The group II and III rats were given the test<br />
substance i.e. EBC at the doses <strong>of</strong> 250 and<br />
500 mg/kg respectively. The group IV animals<br />
were administered glibeclamide at the dose<br />
<strong>of</strong> 0.5 mg/kg. 13 The test and standard drugs<br />
were prepared as suspensions in 2% aqueous<br />
gum acacia such that each ml <strong>of</strong> the<br />
suspension contained the required dose <strong>of</strong> the<br />
drug. Each treatment was given per orally as<br />
single dose. The glucose concentrations in<br />
the blood samples collected just prior to drug<br />
treatments, at 1 and 2 h after treatments were<br />
estimated.<br />
Effect <strong>of</strong> ethyl acetate extract <strong>of</strong> black<br />
catechu (EBC) on blood glucose in alloxan<br />
induced hyperglycemic rats: The selected<br />
hyperglycemic rats with blood glucose levels<br />
between 300 – 350 mg/dl were divided into<br />
four groups – I (control), II, III and IV (Standard)<br />
<strong>of</strong> six rats in each group. After collection <strong>of</strong><br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
55
ORIGINAL ARTICLE<br />
the fasting blood samples, the animals in the<br />
different groups were treated in the similar way<br />
as in the study in normal rats. The glucose<br />
concentrations were estimated in the fasting<br />
blood samples, and samples collected at 1<br />
and 2 h after the treatments.<br />
Effect <strong>of</strong> ethyl acetate extract <strong>of</strong> black<br />
catechu (EBC) on oral glucose tolerance:<br />
To study the effect <strong>of</strong> EBC on oral glucose<br />
tolerance (OGT), the principal adopted by Puri<br />
D and Baral N was followed. 14 Six healthy<br />
albino rats <strong>of</strong> either sex (110-150g) were kept<br />
fasted. After collecting fasting blood samples,<br />
each rat was administered 2% aqueous gum<br />
acacia at the dose <strong>of</strong> 10 ml/kg p.o, followed<br />
immediately by a glucose load <strong>of</strong> 3 g/kg p.o<br />
(30% D-glucose in D/W). The glucose<br />
concentrations were estimated in the fasting<br />
blood samples, and samples collected at 1<br />
and 2 h after glucose load.<br />
Using the same set <strong>of</strong> animals, the oral<br />
glucose tolerance (OGT) tests were repeated<br />
after single oral doses <strong>of</strong> 250 and 500 mg/kg<br />
<strong>of</strong> EBC, and 20 mg/kg <strong>of</strong> nateglinide. The drug<br />
wash out period <strong>of</strong> 10 days was maintained<br />
in between successive OGT tests. 15 The dose<br />
<strong>of</strong> nateglinide was obtained from human dose<br />
<strong>of</strong> 240 mg/day by extrapolation method. 9<br />
Effect <strong>of</strong> ethyl acetate extract <strong>of</strong> black<br />
catechu (EBC) on gluconeogenesis:<br />
Twenty four healthy albino rats <strong>of</strong> either sex<br />
(110 – 150g) were divided into four groups <strong>of</strong><br />
six rats in each – I (control) II, III and IV<br />
(standard) and given fasting. After collection<br />
<strong>of</strong> fasting blood samples, all the animals were<br />
injected hydrocortisone sodium succinate<br />
(240 mg/kg i.p) 16 and followed immediately<br />
by the treatments as follows:<br />
Group I: 2% aqueous gum acacia – 10 ml/ kg<br />
Group II: EBC - 250 mg/kg<br />
Group III: EBC - 500 mg/kg<br />
Group IV: Met<strong>for</strong>min -135 mg/kg<br />
The dose <strong>of</strong> met<strong>for</strong>min was extrapolated from<br />
human dose <strong>of</strong> 1.5 g/day. 9 The drugs were<br />
suspended in 2% aqueous gum acacia such<br />
that 1 ml <strong>of</strong> each preparation contained the<br />
required dose and given per orally as single<br />
doses. The blood samples were collected at<br />
1 and 2 h after the treatments. The glucose<br />
concentrations in the fasting and after<br />
treatment blood samples were estimated.<br />
Statistical analysis: All values were<br />
expressed as mean ± SD <strong>for</strong> each group. The<br />
data were analyzed using One - way ANOVA<br />
followed by Bonferroni test, and a P value less<br />
than 0.05 was considered statistically<br />
significant.<br />
Results: Effect <strong>of</strong> EBC on blood glucose<br />
in normal and alloxan induced<br />
hyperglycemic rats: In both the normal and<br />
hyperglycemic rats, the mean blood glucose<br />
<strong>change</strong>s (decrease) at 1 and 2 h after<br />
treatments from the fasting values in the<br />
different groups were compared. The glucose<br />
<strong>change</strong>s were increased in the EBC and<br />
glibenclamide treated groups, thereby,<br />
reflecting more reductions in glucose<br />
Table 1: Effect <strong>of</strong> EBC on blood glucose in normal albino rats<br />
Values are mean ± SD. n = 6 in each group. All preparations are suspended in 2% aqueous gum acacia and given per orally<br />
in single doses. *p
ORIGINAL ARTICLE<br />
Table 2: Effect <strong>of</strong> EBC on blood glucose in alloxan induced hyperglycemic albino rats<br />
Values are mean ± SD. n = 6 in each group. All preparations are suspended in 2% aqueous gum acacia and given per orally<br />
in single doses. *p
ORIGINAL ARTICLE<br />
concentrations from the fasting values. The<br />
EBC (500 mg/kg p.o) and glibenclamide (0.5<br />
mg/kg p.o) treated groups showed significantly<br />
different glucose <strong>change</strong>s (increase) when<br />
compared with the <strong>change</strong>s in the control<br />
groups (Table 1 and 2).<br />
Effect <strong>of</strong> EBC on hydrocortisone induced<br />
hyperglycemia: Following treatments with the<br />
different drugs just after hydrocortisone<br />
injection, the blood glucose concentrations<br />
increased in all the groups from the fasting<br />
values. The glucose <strong>change</strong>s (increase) at 1<br />
and 2 h from the fasting values in the different<br />
groups were compared. When compared with<br />
the glucose <strong>change</strong>s in the control group, the<br />
EBC treated groups showed significantly less<br />
(p
ORIGINAL ARTICLE<br />
glucose induced hyperglycemia at 1 and 2 h<br />
after nateglinide when compared with<br />
corresponding values in the control group<br />
supports the fact that the drug acts as an<br />
insulin secretagogue. The failure on the part<br />
<strong>of</strong> the test substance to produce significant<br />
fall <strong>of</strong> glucose induced hyperglycemia shows<br />
that it is unlikely to act as an insulin<br />
secretagogue.<br />
Conclusion<br />
From the present study, it is evident that ethyl<br />
acetate extract <strong>of</strong> black catechu (Acacia<br />
catechu) exhibits hypoglycemic property. The<br />
extract possibly does not enhance insulin<br />
secretion, but inhibition <strong>of</strong> hepatic<br />
gluconeogenesis is one <strong>of</strong> the mechanisms<br />
which have contributed to its hypoglycemic<br />
effect.<br />
References<br />
1. Ali M. Black catechu. Text book <strong>of</strong><br />
Pharmacognosy. 2 nd ed. New Delhi: CBS<br />
Publishers & Distributors; 1998.p142-43<br />
2. Wyk BE, Wink M. Acacia catechu<br />
Medicinal Plants <strong>of</strong> the World. 1 st ed<br />
(reprint). Portland: Timber Press;<br />
2005.p28.<br />
3. Kokate CK, Purohit AP, Gokhale SB. Pale<br />
catechu. Pharmacognosy. 43 rd ed.<br />
Mumbai: Nirali Prakashan; 2009.p9.16-<br />
9.17<br />
4. Evans WC. Phenols and Phenolic<br />
glycosides. Trease and Evans<br />
Pharmacognosy. 15 th ed (Indian reprint).<br />
New Delhi: Elsevier; 2006.p214-252.<br />
5. Subramoniam A and Pushpangadan P.<br />
Development <strong>of</strong> phytomedicines <strong>for</strong> liver<br />
diseases. Indian J Pharmacol 1999;<br />
31(3): 166-75.<br />
6. Jayasekhar P, Mohanan PV and<br />
Rathinam K. Hepatoprotective activity <strong>of</strong><br />
ethyl acetate extract <strong>of</strong> Acacia catechu.<br />
Indian J Pharmacol 1997; 29(6): 426 –<br />
28.<br />
7. Ray D, Sharatchandra K and Thokchom<br />
IS. Antipyretic, antidiarrhoeal,<br />
hypoglycaemic and hepatoprotective<br />
activities <strong>of</strong> ethyl acetate extract <strong>of</strong> Acacia<br />
catechu Willd in albino rats. Indian J<br />
Pharmacol 2006; 38(6): 408 – 13.<br />
8. Singh KN, Mittal RK and Barthwal KC.<br />
Hypoglycemic activity <strong>of</strong> Acacia catechu,<br />
Acacia suma, Albizzia odoratissima seed<br />
diets in normal albino rats. Indian J Med<br />
Res 1976; 64(5): 754 – 57.<br />
9. Ghosh MN. Fundamentals <strong>of</strong><br />
Experimental Pharmacology. 3rd ed.<br />
Kolkata: Hilton & Company; 2005.<br />
10. Shoka AAE. Effect <strong>of</strong> some oral<br />
antidiabetic drugs on glucose and mineral<br />
metabolism in alloxan diabetic rats<br />
pretreated with ethylene diamine tetra<br />
acetic acid disodium salt. Indian J<br />
Pharmacol 1992; 24(4): 201 – 6.<br />
11. Parmer NS, Prakash S. Screening<br />
methods in Pharmacology. New Delhi:<br />
Narosa Publishing House; 2006.<br />
12. Babu V, Devi TG, Subramoniam A.<br />
Antidiabetic activity <strong>of</strong> ethanol extract <strong>of</strong><br />
Cassia klenni leaf in glucose fed normal<br />
rats and alloxan induced diabetic rats.<br />
Indian J Pharmacol 2002; 34(6): 409 – 15.<br />
13. Ignacimuthu S, Amalraj T. Effect <strong>of</strong> leaf<br />
extract <strong>of</strong> Zizyphus jujuba on diabetic rats.<br />
Indian J Pharmacol 1998; 30(2): 107 – 8.<br />
14. Puri D, Baral N. Hypoglycemic effect <strong>of</strong><br />
Biophytum sensitivum in the alloxan<br />
diabetic rabbits. Indian J Physiol<br />
pharmacol 1998; 42(3): 401 - 6.<br />
15. Venkateswarlu V. Biopharmaceutics and<br />
Pharmacokinetics. Hyderabad: Pharma<br />
Book Syndicate; 2004.<br />
16. Marcus DF, Wales JK, Viktoria JK, Wolff<br />
FW. A comparative study <strong>of</strong> various<br />
hyperglycemic agents in potassium<br />
deficient rats. Proc Soc Exptl Biol Med<br />
1968; 127(2): 533 – 38.<br />
17. Brahmachari HD, Augusti KT. Isolation <strong>of</strong><br />
orally effective hypoglycemic compounds<br />
from Ficus bengalensis Linn. Indian J<br />
Physiol Pharmacol 1964; 8(11): 60 – 64.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
59
ORIGINAL ARTICLE<br />
18. Rerup CC. Drugs producing diabetes<br />
through damage <strong>of</strong> insulin secreting<br />
cells. Pharmacol Rev 1970; 22(4); 485 –<br />
81.<br />
19. Zastrow MV, Bourne HR. Drug receptors<br />
and pharmacodynamics. In: Katzung BG,<br />
Masters SB, Trevor AJ, editors. Basic<br />
and Clinical Pharmacology. 11 th ed. New<br />
Delhi: Tata McGraw-Hill education Pvt Ltd;<br />
2009. p 15 – 35.<br />
20. Schimmer BP, Parker KL.<br />
Adrenocorticotropic hormone;<br />
Adrenocortical steroids and their<br />
synthetic analogs; Inhibitors <strong>of</strong> synthesis<br />
and actions <strong>of</strong> adrenocortical hormones.<br />
In: Brunton LL, Lazo JS, Parker editors.<br />
Goodman & Gillman’s The<br />
Pharmacological basis <strong>of</strong> Therapeutics.<br />
11 th ed. New York: McGraw- Hill; 2006. p<br />
1587 – 1612.<br />
21. Gunindro N, Das L, Pramodini KK, Singh<br />
TI. Study <strong>of</strong> the ethyl acetate extract <strong>of</strong><br />
Cutch (Acacia catechu) on peripheral<br />
glucose uptake and its interaction with<br />
insulin by using isolated rat<br />
hemidiaphragm. Indian <strong>Medical</strong> Gazette<br />
2008; CXLII (8): 306 – 9.<br />
22. Puri D, Prabhu KM, Murthy PS.<br />
Mechanism <strong>of</strong> action <strong>of</strong> a hypoglycemic<br />
principle isolated from Fenugreek seeds.<br />
Indian J Physiol Pharmacol 2002; 46(4):<br />
457 – 462.<br />
23. DeFronzo RA. Pathogenesis <strong>of</strong> type 2<br />
Diabetes mellitus. Med Clin N Am 2004;<br />
88(4): 787 – 835.<br />
60 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Trends in blood component therapy – A RIMS experience.<br />
1<br />
A. Barindra Sharma, 2 O. Geetchandra Singh, 2 Pratima Khoyumthem, 2 K. Rachandra Singh, 3 Kh. Nando<br />
Singh, 4 Pr<strong>of</strong>. A. Meina Singh,<br />
Abstract<br />
Aim <strong>of</strong> study: To evaluate the use <strong>of</strong> different<br />
types <strong>of</strong> blood components. Methods: The<br />
present study is <strong>based</strong> on the different types<br />
<strong>of</strong> blood components prepared and issued<br />
from the department <strong>of</strong> Immunohaematology<br />
and Blood transfusion, RIMS, Imphal during<br />
the five year period from January 2006 to<br />
December 2010. Blood components were<br />
prepared from whole blood collected in multiunit<br />
bags containing CPD-A solution and<br />
centrifuged in refrigerated centrifuge as per<br />
standard operating procedures (SOPs). The<br />
components were packed red cells, liquid<br />
plasma, platelet rich plasma, platelet<br />
concentrate, fresh frozen plasma and<br />
cryoprecipitate. Results: The total number <strong>of</strong><br />
blood components issued were 11130 out <strong>of</strong><br />
total 69512 blood units issued making a<br />
percentage <strong>of</strong> 16.01%. Packed red cells were<br />
utilized most (72.98%) followed by platelets<br />
(24.57%). The least utilized was<br />
cryoprecipitate (5 units only). The maximum<br />
number<strong>of</strong> components were utilized in 2010<br />
(3701 units). Conclusion: The trend <strong>of</strong><br />
component therapy is encouraging. Use <strong>of</strong><br />
blood components has many advantages.<br />
Whole blood transfusion should be minimized<br />
as it has limited indications.<br />
1. Associate pr<strong>of</strong>., 2. P.G. Trainee 3. Chief <strong>Medical</strong><br />
Officer, 4. Pr<strong>of</strong>. and Head, Dept. <strong>of</strong> Immunohaematology<br />
and Blood transfusion<br />
Corresponding author:<br />
Dr. A. Barindra Sharma, Assoc. Pr<strong>of</strong>. <strong>of</strong> Immunohaematology<br />
& Blood Transfusion, RIMS, Imphal<br />
E-mail: abarindras @ yahoo.co.in<br />
Key words: Blood components, whole blood,<br />
transfusion transmissible infections.<br />
Introduction: Blood is always in short supply<br />
both in developing and developed countries.<br />
Be<strong>for</strong>e component separation was not known<br />
the shortage <strong>of</strong> any <strong>of</strong> the blood components<br />
was treated by transfusing whole blood. This<br />
means the patient received a host <strong>of</strong> unwanted<br />
cells and components from someone else<br />
which the patient may not need, besides<br />
volume overload. Since blood transfusion<br />
involves the transplant <strong>of</strong> tissue from the donor<br />
to the recipient, there are risks to the recipient<br />
<strong>of</strong> transfusing transmissible infections and <strong>of</strong><br />
immunological responses to the <strong>for</strong>eign cells<br />
and plasma proteins. 1<br />
These days blood transfusion therapy has<br />
been converted into component therapy<br />
because very few require transfusion <strong>of</strong> whole<br />
blood. This has become one <strong>of</strong> the effective<br />
methods <strong>of</strong> optimizing blood usage.<br />
Materials and methods: The study was<br />
conducted in the department <strong>of</strong> Immunohaematology<br />
and blood transfusion, RIMS,<br />
Imphal during the period from January 2006<br />
to December 2010. Data <strong>of</strong> whole blood<br />
collection, component separation and issued<br />
during the period were analysed and<br />
recorded. The components were prepared<br />
from whole blood collected in multi-unit bags<br />
containing CPD-A solution. The bags were<br />
centrifuged in the refrigerated centrifuge<br />
(Cry<strong>of</strong>uge 6000i, Heraeus, Germany) at<br />
different speeds and time as per standard<br />
operating procedures (SOPs) and the<br />
components prepared were packed red cells,<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
61
ORIGINAL ARTICLE<br />
liquid plasma, platelet rich plasma, platelet<br />
concentrate and fresh frozen plasma (FFP).<br />
Cryoprecipitate was further prepared from<br />
FFP by collecting the precipitate <strong>for</strong>med during<br />
controlled thawing and resuspending in 10-<br />
20ml plasma.<br />
Results: A total <strong>of</strong> 69512 blood units were<br />
issued during the five-year period, out <strong>of</strong> which<br />
11130 units were issued as components,<br />
making a percentage <strong>of</strong> 16.01 (Table 1).<br />
Packed red cells were the most utilized<br />
component (72.98%) followed by platelet<br />
component (24.57%), liquid plasma (1.46%)<br />
and FFP (0.93%) respectively and the least<br />
utilized was cryoprecipitate with only 5 units<br />
issued during the period (Table 2). The<br />
maximum number <strong>of</strong> components were<br />
utilized in 2010 (3701 units and a percentage<br />
<strong>of</strong> 26.89).<br />
Discussion: Blood component and derivative<br />
therapy began during the world war-II when<br />
Edwin J. Cohn and his collaborators<br />
developed the cold ethanol method <strong>of</strong> plasma<br />
fractationation 2 .<br />
Making components from whole blood not only<br />
serves more patients but also improves the<br />
storage <strong>of</strong> the individual blood elements. Red<br />
cells are best stored cold, platelets at room<br />
temperature with agitation and plasma<br />
frozen. 3,4 Whole blood when stored at 2-6 0 C<br />
has few viable platelets after 24 hours while<br />
after separation, platelets can be stored <strong>for</strong><br />
five days at 22 0 C. Where plasma is frozen at<br />
-25 0 C or colder, it can be stored <strong>for</strong> at least<br />
one year or longer and heat labile coagulation<br />
factors (Factor V and VIII) are preserved 1,5 .<br />
Liquid plasma is plasma separated from a<br />
whole blood unit and stored at 4 0 C and is<br />
devoid <strong>of</strong> any labile coagulation factors 1 .<br />
Moreover the specific components could be<br />
given as required in adequate dose without<br />
danger <strong>of</strong> overloading or complications due<br />
to other portion <strong>of</strong> blood 6 .<br />
In India, 80 percent <strong>of</strong> blood is used as whole<br />
blood and only 20 percent units are utilized<br />
as components 7 . WHO also recommends<br />
that the ratio <strong>of</strong> the use <strong>of</strong> blood components<br />
and whole blood should be 90:10. As a national<br />
action plan, NACO has advocated under<br />
NACP-III (2007-2012) that at least 50% <strong>of</strong> all<br />
blood collections should be separated into<br />
components 7 . In Maharastra, 40% <strong>of</strong> the total<br />
blood units are separated into components<br />
and in Gujarat, 38% are given as components 8 .<br />
It was also suggested that promoting blood<br />
component therapy would not only bring down<br />
the requirement <strong>of</strong> whole blood by 60-70%, it<br />
would also ensure the optimum use <strong>of</strong> all<br />
resources 7,8 . The overall percentage <strong>of</strong><br />
components in RIMS (16%) is still lower than<br />
the national average <strong>of</strong> 20%. Encouraging<br />
trends are emerging in RIMS Hospital since<br />
the availability <strong>of</strong> component separation facility<br />
since October 2002, and components issued<br />
reached 26% in 2010. Component therapy is<br />
now a better medicine and we should<br />
encourage this <strong>for</strong> better patient care services.<br />
Conclusion: Appropriate component therapy<br />
now provides more effective treatment and<br />
more complete use <strong>of</strong> blood products. By<br />
providing the right blood product, in the right<br />
quantity <strong>for</strong> the right patient, the gap between<br />
demand and supply can be bridged.<br />
AcknowleDgement: The authors sincerely<br />
express gratitude to Dr. Y. Bijoykumar Singh,<br />
Chief <strong>Medical</strong> Officer, Department <strong>of</strong><br />
Immunohaematology and Blood Transfusion,<br />
RIMS <strong>for</strong> his various inputs and technical<br />
support in completion <strong>of</strong> the work.<br />
62 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
References:<br />
1. The clinical use <strong>of</strong> blood. WHO, Blood<br />
Transfusion Safety, Geneva, 2002.<br />
2. Cohn EJ. The separation <strong>of</strong> blood into<br />
fraction <strong>of</strong> therapeutic value. Ann Intern<br />
Med 1947; 26: 341-52<br />
3. Solheim BG, Hess JR: Red cell<br />
metabolism and preservation. In: Simon<br />
TL, Synder EL, Solheim BG, Stowell CP,<br />
Stauss RG, Petrides M, editors. Rossi’s<br />
Principles <strong>of</strong> Transfusion <strong>Medicine</strong>, 4 th ed.<br />
U.K. Wiley-Blackwell, 2009: 54-66.<br />
4. Transfusion Guidelines <strong>for</strong> blood<br />
components. <strong>Medical</strong> advisory committee<br />
<strong>of</strong> the American Red Cross Blood<br />
Services, New England, USA, December<br />
2003.<br />
5. Practice parameters <strong>for</strong> the use <strong>of</strong> FFP,<br />
cryoprecipitate and platelets. Task Force<br />
<strong>of</strong> American College <strong>of</strong> Pathologists.<br />
JAMA 1994; 271: 777-781.<br />
6. Saran RK. Transfusion <strong>Medicine</strong><br />
Technical manual. 2 nd ed. Directorate<br />
General <strong>of</strong> Health Services, Ministry <strong>of</strong><br />
Health and Family Welfare, Government<br />
<strong>of</strong> India, New Delhi. 2003.<br />
7. An action plan <strong>for</strong> blood safety. NACO,<br />
Ministry <strong>of</strong> Health and Family welfare,<br />
Government <strong>of</strong> India, New Delhi, 2007.<br />
8. Romani KV, Mavalankar DV, Govil D.<br />
Study <strong>of</strong> Blood transfusion services in<br />
Maharastra and Gujarat states, India. J<br />
Health Popul Nutr 2009 April : 259-270.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
63
ORIGINAL ARTICLE<br />
Breast-feeding: patterns and correlates in Manipur<br />
1<br />
R.K. Narendra 2 N. Sharat Singh 3 N. Sanajaoba Singh<br />
Abstract<br />
Objective: To study the breastfeeding (BF)<br />
patterns and also to identify the determinants<br />
which may have pr<strong>of</strong>ound effects on the<br />
duration <strong>of</strong> BF.<br />
Methods: A cross sectional study <strong>of</strong> 1225<br />
ever-married women <strong>of</strong> reproductive age with<br />
at least one live birth was conducted in four<br />
valley districts <strong>of</strong> Manipur under cluster<br />
sampling scheme. Survival analysis technique<br />
has been adopted through SPSS vs 16.<br />
Results: The median duration <strong>of</strong> BF is found<br />
to be 20.37 months. Among the seven<br />
explanatory variables <strong>of</strong> interest, only two<br />
factors – place <strong>of</strong> residence (urban, relative<br />
risk (RR) =1.35) and employment status<br />
(employed, RR=1.88) have highly significant<br />
effect (P
ORIGINAL ARTICLE<br />
availability <strong>of</strong> supplementary foods, socioeconomic<br />
status etc. 10-13 So the study <strong>of</strong><br />
behaviour and differential <strong>of</strong> BF is very<br />
important in a society where the fertility,<br />
woman as well as child health are becoming<br />
a serious problem. There<strong>for</strong>e this study tries<br />
to touch these issues. The main objective <strong>of</strong><br />
this paper is to study the breastfeeding (BF)<br />
patterns and also to identify the determinants<br />
which may have pr<strong>of</strong>ound effects on the<br />
duration <strong>of</strong> BF by using survival analysis<br />
techniques.<br />
Materials and methods: A cross sectional<br />
study was conducted in four valley districts –<br />
Bishnupur, Thoubal, Imphal West and Imphal<br />
East – <strong>of</strong> Manipur during January1 to June 30,<br />
2009. Under cluster sampling scheme, house<br />
to house survey was carried out with pretested<br />
and semi-structural interview schedule<br />
on ever-married women <strong>of</strong> reproductive age<br />
with atleast one live birth. The clusters <strong>of</strong><br />
randomly selected villages in rural area and<br />
wards in urban were completely enumerated<br />
which entailed a sample <strong>of</strong> 1225 women from<br />
1013 households<br />
Here, the duration <strong>of</strong> BF is taken as the<br />
response variable and is defined as the child’s<br />
age (in months) at the time <strong>of</strong> complete<br />
weaning, regardless <strong>of</strong> when consumption <strong>of</strong><br />
other food began. For the children who have<br />
died or still being breastfed at the time <strong>of</strong><br />
survey, the duration is the child’s age at death<br />
or at the time <strong>of</strong> survey. Such cases are<br />
treated as censored ones.<br />
The explanatory variables or so termed as<br />
covariates are socio-economic and<br />
demographic characters. The categorical<br />
variables are quantified by binary dummy<br />
variable (0, 1). The socio-economic variables<br />
include place <strong>of</strong> residence (urban=1, rural=0),<br />
educational level, employment status<br />
(employed=1, unemployed=0) and family<br />
income. The demographic variables are age<br />
at marriage, sex <strong>of</strong> previous child (male=1,<br />
female=0) and parity.<br />
As the study is confined in censored data,<br />
statistical analysis is there<strong>for</strong>e carried out<br />
using survival analysis techniques. Firstly, the<br />
survival function <strong>of</strong> BF (the proportion <strong>of</strong><br />
women reported termination <strong>of</strong> BF within 6,<br />
12, 18 and 24 months) with respect to socioeconomic<br />
is estimated by life table technique<br />
14-15<br />
and log rank test 16 is employed to<br />
compare the survival experience between<br />
different groups under study. Secondly, the<br />
effects <strong>of</strong> various demographic and socioeconomic<br />
factors on the dynamics <strong>of</strong> duration<br />
<strong>of</strong> BF are investigated by utilizing Cox’s<br />
proportional hazard model. 17<br />
Results: Table 1 provides the overall median<br />
duration <strong>of</strong> BF <strong>of</strong> the study population which<br />
is 20.37 months. About 59 per cent, 35 per<br />
cent, 24 per cent, 16 per cent and 13 per cent<br />
<strong>of</strong> the mothers who have married during the<br />
age group <strong>of</strong> below 15 years, 15-20 years,<br />
20-25 years, 25-30 years, and 30 years and<br />
above respectively terminate BF within 12<br />
months. It also highlights that the median<br />
duration <strong>of</strong> BF increases with the increase in<br />
the age at marriage <strong>of</strong> mothers. By the Log<br />
rank test, the association between age at<br />
marriage and duration <strong>of</strong> BF is highly<br />
significant (x 2 = 26.181, P < 0.001). It could be<br />
examined that 59 per cent <strong>of</strong> mothers having<br />
parity zero terminate BF within 12 months.<br />
On contrary, 23 per cent <strong>of</strong> mothers having<br />
parity one, that <strong>of</strong> 22 per cent <strong>of</strong> parity two,<br />
20 per cent <strong>of</strong> parity three and 19 per cent <strong>of</strong><br />
parity four and above terminate BF within 12<br />
months. The median duration <strong>of</strong> BF increases<br />
with the increase in parity and this variation is<br />
highly significant in the study population<br />
irrespective <strong>of</strong> other covariates (P < 0.001).<br />
Mothers residing in rural areas have longer<br />
duration <strong>of</strong> BF (20.85 months) than residing<br />
in urban areas (18.48 months) and relationship<br />
is found to be statistically significant<br />
(P
ORIGINAL ARTICLE<br />
mothers (20.55 months) than employed<br />
mothers (15.40 months). About 22 per cent<br />
<strong>of</strong> unemployed mothers terminate BF within<br />
12 months while 41 per cent <strong>of</strong> employed<br />
mothers terminate BF within 12 months. Only<br />
15 per cent <strong>of</strong> mother having family income <strong>of</strong><br />
below Rs. 2000 terminate BF within 12<br />
months. But 19 per cent <strong>of</strong> the study subjects<br />
having family income <strong>of</strong> Rs. 2000-4000, 21 per<br />
cent in the income <strong>of</strong> Rs. 4000-6000, 25 per<br />
cent in Rs. 6000-8000, 29 per cent in Rs. 8000-<br />
10000 and 34 per cent in Rs. 10000 and above<br />
terminate BF within the same period. The<br />
variation in the median duration <strong>of</strong> BF with<br />
respect to family income is highly significant<br />
(P
ORIGINAL ARTICLE<br />
Table 2<br />
Cox’s regression analysis <strong>of</strong> covariates on the<br />
duration <strong>of</strong> BF<br />
Table 3<br />
Stepwise Cox’s regression analysis <strong>of</strong> covariates on<br />
the duration <strong>of</strong> BF<br />
0.090<br />
Discussion: The above result shows that the<br />
median duration <strong>of</strong> BF is 20.37 months, which<br />
is lower than the minimum <strong>of</strong> 24 months<br />
recommended by WHO <strong>for</strong> most children.<br />
The duration <strong>of</strong> about 20 months is also<br />
lacking behind the India’s national figure <strong>of</strong> 25<br />
months observed by National Family Health<br />
Survey-3 (NHFS-3). The findings arrived in the<br />
present study also highlight that different<br />
factors have different effects on duration BF.<br />
The duration <strong>of</strong> BF increases with the increase<br />
in parity. It might be due to the fact that mothers<br />
<strong>of</strong> high parity may be older and they produce<br />
less milk but they may be more traditional in<br />
orientation, and usually lower order births<br />
occur in quick succession than higher order<br />
births and hence the chance <strong>of</strong> voluntary<br />
termination <strong>of</strong> BF at an early age <strong>of</strong> child might<br />
be higher <strong>for</strong> the lower birth order babies than<br />
<strong>for</strong> the higher birth order. This view is<br />
consistent with the other findings observed<br />
by several researchers. 4,11,13,18 The<br />
educational level <strong>of</strong> mothers show an inverse<br />
relationship with the duration <strong>of</strong> BF, owing to<br />
the fact that educated mothers probably start<br />
giving food supplements to their children<br />
earlier and so a shorter period <strong>of</strong> lactation.<br />
Similar, findings have also been obtained by<br />
other researchers in developing countries . 1,<br />
8, 11<br />
Place <strong>of</strong> residence has a significant impact<br />
on the duration <strong>of</strong> BF. The risk <strong>of</strong> termination<br />
<strong>of</strong> BF <strong>of</strong> mothers residing in urban is higher<br />
than those in rural. The shorter duration <strong>of</strong> BF<br />
in urban areas is thought to be caused by<br />
higher educational level and higher income<br />
than that <strong>of</strong> rural. This view is incorporated<br />
with the past findings. 9, 13 Besides, employed<br />
mothers have shorter duration <strong>of</strong> BF than<br />
unemployed one. The reason may be that<br />
employed mothers do not get enough time to<br />
breastfeed their children as they work outside<br />
and thus tend to lactate <strong>for</strong> shorter period and<br />
probably also provide food supplements to the<br />
children much earlier. It is supported by the<br />
earlier findings too. 1, 12 Mothers <strong>of</strong> high income<br />
group have shorter duration <strong>of</strong> BF. It may<br />
perhaps be the fact that economically affluent<br />
families could af<strong>for</strong>d to buy powder milk, other<br />
baby <strong>for</strong>mulae, wet nurses etc. Similar views<br />
have also been reported by other researchers<br />
<strong>based</strong> on the data from developing countries. 12<br />
Conclusion: The present duration <strong>of</strong><br />
breastfeeding, that is about 20 months, is<br />
lower than the WHO recommended figure <strong>of</strong><br />
24 months and even lacking behind the all<br />
India’s figure <strong>of</strong> 25 months. This low status <strong>of</strong><br />
breastfeeding may cause hazardous problem<br />
in reproductive and child health. Thus, we<br />
have to promote the breastfeeding practice<br />
among the educated and employed women<br />
having high income and the women residing<br />
in urban areas too through vigorous<br />
implementation <strong>of</strong> inter-sectoral operational<br />
strategies. Over and above, prolong breastfed<br />
mothers have to lengthen the duration <strong>of</strong> inter<br />
live-birth interval <strong>for</strong> reducing current fertility<br />
and to improve economic status <strong>of</strong> general<br />
community resulting into better way <strong>of</strong> life.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
67
ORIGINAL ARTICLE<br />
References<br />
1. Huffman SL. Determinants <strong>of</strong><br />
breastfeeding in developing countries:<br />
overview and policy implications. Studies<br />
in Family Planning 1984; 15(4): 144-54.<br />
2. Thapa S, Williamson NE. Breast-feeding<br />
in Asia: an overview. Asia-Pacific<br />
Population <strong>Journal</strong> 1990; 5(1): 7-25.<br />
3. Lechtig JAD, Jelliffe E. The first workshop<br />
on national breast-feeding programmes<br />
in Latin America: a personal view. <strong>Journal</strong><br />
<strong>of</strong> Tropical Pediatrics; 1990.<br />
4. Mannan HR, Islam MN. Breastfeeding in<br />
Bangladesh: patterns and impact on<br />
fertility. Asia-Pacific Population <strong>Journal</strong><br />
1995; 10 (4): 23-38.<br />
5. Chhabra P, Grover VL, Aggarwal OP,<br />
Dubey KK. Breastfeeding patterns in an<br />
urban resettlement colony <strong>of</strong> Delhi. Indian<br />
<strong>Journal</strong> <strong>of</strong> Pediatrics 1998; 65: 867-72.<br />
6. Lawrence RA. Peer support: making a<br />
difference in breastfeeding duration. Can<br />
Med Assoc J 2002; 166: 42-43.<br />
7. Yngve A, Sjostrom M. Breastfeeding in<br />
countries <strong>of</strong> the European Union and<br />
EFTA: current and proposed<br />
recommendations, rationale, prevalence,<br />
duration and trends. Public Health Nutr<br />
2001; 4: 631-45.<br />
8. Koosha A, Hashemifesharaki R,<br />
Mousavinasab N. Breast-feeding patterns<br />
and factors determining exclusive breastfeeding.<br />
Singapore Med J 2008; 49 (12):<br />
1002.<br />
9. Agrawal DK, Agarwal KN, Tiwari IC,<br />
Yadava KNS. Breast-feeding practices in<br />
urban slum and rural areas <strong>of</strong> Varanasi.<br />
<strong>Journal</strong> <strong>of</strong> Tropical Pediatrics 1982; 28.<br />
10. Aaryal TR. Some techniques to estimate<br />
child mortality in Nepal. <strong>Journal</strong> <strong>of</strong> Institute<br />
<strong>of</strong> Science and Technology 2004; 13: 48-<br />
61.<br />
11. Aaryal TR. Differentials <strong>of</strong> breastfeeding<br />
among rural women <strong>of</strong> Western Nepal: a<br />
survival analysis. <strong>Journal</strong> <strong>of</strong> Nepal Health<br />
Research Council 2005; 3(2): 58-64.<br />
12. Giashuddin MS, Kabir M. Duration <strong>of</strong><br />
breastfeeding in Bangladesh. Indian J Med<br />
Res 2004; 119: 267-272.<br />
13. Islam S, Yadava KNS, Alam MA.<br />
Differentials and determinants <strong>of</strong> the<br />
duration <strong>of</strong> breastfeeding in Bangladesh:<br />
a multilevel analysis. Proc. Pakistan<br />
Acad. Sci. 2006; 43(1): 1-14.<br />
14. Berkson J, Gage RR. Calculation <strong>of</strong><br />
survival rates <strong>for</strong> Cancer. Proceedings <strong>of</strong><br />
staff meetings <strong>of</strong> the Mayo Clinic 1950;<br />
25: 250.<br />
15. Cutler SJ, Ederer F. Maximum utilization<br />
<strong>of</strong> the life table method in analyzing<br />
survival. <strong>Journal</strong> <strong>of</strong> Chronic Diseases<br />
1958; 8: 699-712.<br />
16. Peto R, Peto J. Asymptotically efficient<br />
rank invariant procedures. <strong>Journal</strong> <strong>of</strong> the<br />
Royal Statistical Society 1972; Series A,<br />
135: 185-207.<br />
17. Cox DR. Regression models and life<br />
tables. <strong>Journal</strong> <strong>of</strong> the Royal Statistical,<br />
Society 1972; Series B, 34(2): 187-220.<br />
18. Ahamed MM. Breastfeeding in<br />
Bangladesh. <strong>Journal</strong> <strong>of</strong> Biosocial Science<br />
1986; 18(4): 425-434.<br />
68 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
ORIGINAL ARTICLE<br />
Clinical pr<strong>of</strong>ile <strong>of</strong> nasopharyngeal Carcinoma with neurological complications<br />
1<br />
Lozinu J, 2 S. Thingbaijam, 1 Rino K, 3 Sobita P, 1 Das B, 4 W. Jatishwar<br />
Abstract:<br />
Objective: To study the clinical and<br />
radiological pr<strong>of</strong>ile <strong>of</strong> nasopharyngeal<br />
Carcinoma with neurological complications.<br />
Method: Discriptive study <strong>of</strong> twenty eight<br />
newly diagnosed patients <strong>of</strong> nasopharyngeal<br />
carcinoma (NPC) with neurological<br />
complications admitted in the department <strong>of</strong><br />
Otorhinolaryngology, Regional Institute <strong>of</strong><br />
<strong>Medical</strong> Sciences, Imphal, Manipur during a<br />
two years period between September 2008-<br />
July 2010 were evaluated <strong>for</strong> clinical pr<strong>of</strong>ile.<br />
Patients with histologically proven NPC with<br />
neurological complications <strong>of</strong> all age group<br />
were included in the study irrespective <strong>of</strong> age,<br />
sex, occupation, religion, race, socioeconomic<br />
status and address. Patients with<br />
recurrent or residual NPC or without<br />
neurological complications were excluded<br />
from the study. The diagnosis was made from<br />
the clinical findings, histopathological tests<br />
and radiological studies. Results: Cervical<br />
lymphadenopathy was the most common<br />
presenting complaint (75%). The most<br />
common neurological symptoms at diagnosis<br />
were facial pain/trigeminal neuralgia present<br />
in 19 patients (38.8%). The most commonly<br />
involved nerve was the trigeminal (V) nerve<br />
1. Post graduate trainee; 2. Associate Pr<strong>of</strong>essor;<br />
3. Assistant Pr<strong>of</strong>essor, Department <strong>of</strong><br />
Otorhinolaryngology, RIMS 4. Pr<strong>of</strong>. Dept. <strong>of</strong><br />
Radiodiagnosis, RIMS, Imphal<br />
Corresponding author:<br />
Dr. Thingbaijam S, Associate Pr<strong>of</strong>essor, Dept <strong>of</strong><br />
Otorhinolaryngology, RIMS, Imphal – 795004<br />
Email – dr_sthingbaijam@yahoo.in<br />
(67.9% <strong>of</strong> cases). The CT evaluation <strong>of</strong> NPC<br />
patients with cranial nerve involvement should<br />
include thin cuts <strong>of</strong> the skull base <strong>for</strong> detection<br />
<strong>of</strong> subtle bone erosion. Conclusion: NPC<br />
with neurological complications is not as<br />
uncommon as believed to be. There<strong>for</strong>e it is<br />
important to do a thorough neurological<br />
examination and radiological imaging to know<br />
the exact extent <strong>of</strong> the primary tumour in a<br />
case <strong>of</strong> NPC.<br />
Key words: Nasopharyngeal carcinoma,<br />
neurological symptoms, cranial nerve,<br />
computerized tomography (CT) and MRI<br />
(Magnetic resonance imaging)<br />
Introduction: Nasopharyngeal carcinoma<br />
malignancies (NPC) frequently escape early<br />
recognition. This can be attributed to the<br />
insidious manner <strong>of</strong> growth, the lack <strong>of</strong><br />
specificity <strong>of</strong> initial symptoms, and the relative<br />
inaccessibility <strong>of</strong> the nasopharynx to routine<br />
examination. Neurological manifestations may<br />
occur early or late in the course <strong>of</strong> the disease,<br />
and may at times be the earliest recognizable<br />
abnormalities. 1 This study on NPC presenting<br />
in advanced stage or with neurological<br />
complications was carried out with the<br />
purpose <strong>of</strong> calling attention to the disease as<br />
one cause <strong>of</strong> neurological symptoms and<br />
signs which may be puzzling at times.<br />
Materials and Methods: 28 cases <strong>of</strong><br />
histologically confirmed cases Of NPC with<br />
neurological manifestations were studied in<br />
the Department <strong>of</strong> Otorhinolaryngology,<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal,<br />
Manipur during a period between September<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
69
ORIGINAL ARTICLE<br />
2008 and July, 2010. Detailed history with<br />
clinical examination was done and recorded<br />
in a prescribed pro<strong>for</strong>ma. Endoscopic<br />
examination with 0 0 and 30 0 Karl Storz<br />
endoscope, biopsy <strong>for</strong> histopathological<br />
examination along with computer tomography<br />
(CT) and magnetic resonance imaging (MRI)<br />
<strong>of</strong> the nasopharynx, head and neck were done.<br />
Patients with recurrent or residual disease or<br />
without neurological involvement were<br />
excluded from the study. Statistical analysis<br />
was done with Chi-square test in SPSS 17<br />
version.<br />
Results: The results <strong>of</strong> the study done on 28<br />
cases <strong>of</strong> NPC with neurological manifestations<br />
are presented below:<br />
Neck swelling was the most common clinical<br />
feature among 21(75%) patients; followed by<br />
facial pain in 19 ( 67.9%) patients. Otological<br />
symptoms: hearing loss and ear fullness in<br />
18 (64.3%) patients as shown in table 1.<br />
Table I: Clinical features <strong>of</strong> Nasopharyngeal carcinoma patients<br />
with neurological involvement<br />
Symptoms<br />
No. <strong>of</strong> patients(%)<br />
Neck swelling 21(75)<br />
Sticky sensation back <strong>of</strong>nose/throat<br />
10(35.7)<br />
Epistaxis 9(32.1)<br />
Nasal obstruction 10(35.7)<br />
Tinnitus 10(35.7)<br />
Fullness <strong>of</strong> ears & Hearing loss 18(64.3)<br />
Otalgia 3(10.7)<br />
Otorrhea 3(10.7)<br />
Headache 16(57.1)<br />
Dysphagia 11(39.3)<br />
Nasal regurgitation 11(39.3)<br />
Diplopia 12(42.9)<br />
Diminished vision 7(25)<br />
Proptosis 1(3.6)<br />
Facial pain 19(67.9)<br />
Ptosis 7(25)<br />
Hoarseness 1(3.6)<br />
Loss <strong>of</strong> smell 1(3.6)<br />
Trismus 4(3.6)<br />
Facial asymmetry 2(7.1)<br />
Fig. 2 shows Cranial Nerve involvement<br />
among the Nasopharyngeal carcinoma<br />
patients with neurological complications.<br />
Trigeminal nerve (Cr. nerve V ) was found to<br />
be the most common cranial nerve involved<br />
in 19 (67.9%), followed by the Abducent nerve<br />
(Cr. nerve VI), which was since in 12 (43%).<br />
Figure 2: Bar chart representing the different<br />
types <strong>of</strong> cranial nerves involved<br />
Table-2: Histopathological report <strong>of</strong> the Nasopharyngeal<br />
carcinoma patients with intracranial complications<br />
Table-3: Computed Tomography nasopharynx findings among<br />
the Nasopharyngeal carcinoma patients with neurological<br />
involvement.<br />
Table-4: Magnetic Resonance Imaging study <strong>of</strong> nasopharynx<br />
findings <strong>of</strong> the nasopharynx carcinoma patients with intracranial<br />
complications.<br />
Non-keratinizing undifferentiated type was<br />
found to be the most common histopathological<br />
picture in Nasopharyngeal<br />
carcinoma patients with intracranial<br />
complications comprising <strong>of</strong> 23 (82.1%),<br />
70 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
Table 5: CT finding showing relation <strong>of</strong> skull base<br />
erosion, intracranial extension, and cranial nerve<br />
involvement (n=28)<br />
Table 6: MRI finding showing relation <strong>of</strong> skull base<br />
erosion, intracranial extension, and cranial nerve<br />
involvement (n= 23)<br />
follow by differentiated non-keratinising<br />
carcinoma 4 (14.3%) as shown in table 2.<br />
Skull base erosion was detected via CT in 14<br />
(50%) <strong>of</strong> the patients. Intracranial extension<br />
was detected in 14 (46.4%) <strong>of</strong> the patients<br />
as shown in table 3. MRI could detect 14<br />
(50%) <strong>of</strong> skull base erosion and 18 (64.3%)<br />
<strong>of</strong> intracranial extension <strong>of</strong> the nasopharyngeal<br />
carcinoma as shown in table 4.<br />
A significant correlation was found between<br />
skull base erosion and involvement <strong>of</strong> cranial<br />
nerves III-VI and either skull base erosion or<br />
intracrenial extension (p=0.000) as seen in<br />
both the CT and MRI findings (Table 5 & 6).<br />
The last four cranial nerves IX-XII are involve<br />
ORIGINAL ARTICLE<br />
significantly (P=006,P=000) when there is no<br />
skull base erosion or intracranial extension<br />
detected by CT or MRI scans.<br />
Discussion: Cervical lymphadenopathy was<br />
the most common presenting complaint in 21<br />
(75%) patients. A study in Taiwan, reported<br />
75.5% (729 out <strong>of</strong> 966) <strong>of</strong> patients presented<br />
with neck mass. 2,3 Neurological complications<br />
associated with malignant tumours <strong>of</strong><br />
nasopharynx range from 30 to 70% in large<br />
series 4 . In our study, the most common<br />
neurological symptoms at diagnosis was<br />
facial pain/trigeminal neuralgia present in<br />
19(67.9%) patients and the trigeminal was the<br />
most commonly involved nerve (67.9%). We<br />
have found that I and VIII nerves are rarely<br />
affected. These finding agrees with most <strong>of</strong><br />
the studies. 5,6,7,8 The cranial nerves traversing<br />
the middle fossa are the most susceptible to<br />
injury because Rosenmûller’s fossa, the<br />
classic site <strong>of</strong> origin <strong>of</strong> primary<br />
nasopharyngeal malignant tumors, lies<br />
directly beneath the <strong>for</strong>amen lacerum. This<br />
aperture and the nearby <strong>for</strong>amen ovale are<br />
the preferred routes <strong>of</strong> entry into the cranial<br />
cavity. The structures in immediate proximity<br />
to these <strong>for</strong>amina are the tip <strong>of</strong> the petrous<br />
pyramid that is crossed by the abducents<br />
nerve, the gasserian ganglion, and emerging<br />
trigeminal branches, and the cavernous sinus<br />
with its contents. Thus there is a high<br />
incidence <strong>of</strong> patients with fifth and sixth nerve<br />
lesions. Cranial nerves leaving the skull<br />
through the posterior fossa are also<br />
susceptible to damage from such a tumor.<br />
As a rule, these lesions are extracranial and<br />
are caused either by spread <strong>of</strong> the tumor into<br />
the retroparotidean space, or by pressure<br />
from metastasis in the retropharyngeal lymph<br />
nodes. I, III and IV nerves are usually<br />
compromised when the tumor reaches<br />
<strong>for</strong>ward to the anterior portion <strong>of</strong> the cavernous<br />
sinus and the superior orbital fissure. The VII<br />
nerve generally is involved in the neck after<br />
its emergence from the stylomastoid <strong>for</strong>amen,<br />
and the olfactory nerve is affected by<br />
expansion <strong>of</strong> the tumor into the nasal cavity<br />
or through the cribri<strong>for</strong>m plate. 1 The VII and<br />
VIII nerves are protected by the petrous bone<br />
and hence are rarely injured in all series 9 , as<br />
seen in our case. In the present study non-<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
71
ORIGINAL ARTICLE<br />
keratinizing undifferentiated carcinoma was<br />
found as the most common histopathological<br />
picture (82.1%). This is comparable to the<br />
study done by McGuire LJ et al (82.1%). 10<br />
There were 14 (28.6%) patients who had skull<br />
base erosion and the 13 (26.5%) patients who<br />
had intracranial extension on CT scan. This<br />
is comparable to a study in Hong Kong which<br />
observed erosion <strong>of</strong> skull base in 31.3% but<br />
reported a lower percentage <strong>of</strong> intracranial<br />
extension (12.2%). 11 In the present study, 14<br />
(50%) patients had skull base erosion and 18<br />
(78.2%) had intracranial extension on MRI<br />
study <strong>of</strong> the 23 patients. All skull base erosion<br />
were detected by CT scan but intracranial<br />
extension was seen better by MRI particularly<br />
parasellar and cavernous sinus region. It was<br />
observed that patients having skull base<br />
erosion or widening <strong>of</strong> <strong>for</strong>amina may not<br />
necessarily have intracranial extension. This<br />
finding agrees with Sham JST at al. 11 A Hong<br />
Kong study <strong>of</strong> 67 patients reported that MRI<br />
showed intracranial extension in 38(56.7%)<br />
versus 24(35.8%) on CT. 12 A significant<br />
involvement <strong>of</strong> cranial nerve III-VI (p=0.000) is<br />
seen in patients who had either skull base<br />
erosion or intracranial extension, a finding<br />
References:<br />
1. Thomas JE, Waltz AG. Neurological<br />
manifestations <strong>of</strong> nasopharyngeal tumors.<br />
JAMA 1965;192: 95-8.<br />
2. Garandawa HI, Ahmad BM, Ngadda HA.<br />
Nasopharyngeal carcinoma in Northeastern<br />
Nigeria: clinical trends. Niger J Clin<br />
Pract 2009; 12(4):379-82<br />
3. Wong BYK. Nasopharyngeal carcinoma in<br />
Hong Kong- clinical features and diagnosis.<br />
Hong Kong Med J 1987;39:243-5<br />
4. Turgman J, Braham J, Modan B,<br />
Goldhammer Y. Neurological<br />
complications in patients with malignant<br />
tumors <strong>of</strong> the nasopharynx. Eur Neurol<br />
1978; 17:149-54.<br />
5. Neel HB III. Nasopharyngeal carcinoma:<br />
clinical presentation, diagnosis, treatment,<br />
and prognosis. Otolaryngol Clin North Am<br />
1985; 18:479-90.<br />
6. Godtfredson E. Ophthalmologic and<br />
neurologic symptoms at malignant<br />
nasopharyngeal tumors: clinical study<br />
comprising 454 cases with special<br />
similar to Sham JST et al. 11 The last four<br />
cranial nerves IX-X are found to be affected<br />
significantly (p=0.00 & p=0.000) in patients<br />
without either skull base erosion or intracranial<br />
extension. These nerves might have been<br />
involved in the retroparotidian space or in the<br />
retropharyngeal space outside the skull by<br />
either extension <strong>of</strong> the tumor or metastatic<br />
node.<br />
Conclusion: NPC with neurological<br />
manifestations is common as found in our<br />
study. V is the most commonly involved cranial<br />
nerve. Most <strong>of</strong> the patients with III-VI cranial<br />
nerve involvement had skull base erosion.<br />
Non-keratinizing undifferentiated carcinoma<br />
was found as the most common<br />
histopathological picture. Skull base erosion<br />
and intracranial extension are demonstrated<br />
well in CT and MRI and they are thus,<br />
important tools <strong>for</strong> the diagnosis, staging and<br />
treatment planning <strong>of</strong> nasopharyngeal<br />
carcinoma. Neurological manifestations<br />
should be paid attention to, in a case <strong>of</strong> NPC<br />
and proper otoneurological examination with<br />
CT and MRI should be <strong>for</strong> early diagnosis and<br />
treatment which would improve the prognosis<br />
<strong>of</strong> the disease.<br />
reference to histopathology and possibility<br />
<strong>of</strong> earlier recognition. Acta Otolaryngol<br />
1944; 59 suppl:19-323.<br />
7. Hoppe RT, G<strong>of</strong>finet DR, Baghshaw MA.<br />
Carcinoma <strong>of</strong> the nasopharynx: eighteen<br />
years experience with megavoltage radiation<br />
therapy. Cancer 1976; 37:2605-12.<br />
8. Baker SR. Malignant tumours <strong>of</strong> the<br />
nasopharynx. J Surg Oncol 1981; 17:25-32.<br />
9. Brennan B nasopharyngeal carcinoma.<br />
Orphanet J Rare Dis 2006; 15:1765-77.<br />
10. McGuire LJ, Lee JC. The histopathologic<br />
diagnosis <strong>of</strong> nasopharyngeal. Ear Nose<br />
and Throat J 1990; 69:229-36.<br />
11. Sham JST, Cheung YK, Choy D, Chan FL,<br />
Leong L. Cranial nerve involvement and<br />
base <strong>of</strong> the skull erosion in<br />
nasopharyngeal carcinoma. Cancer<br />
1991;68:422-6.<br />
12. Ng SH, Chang TC, Ko SF, Yen PS, Wan<br />
YL, Tand LM et al. Nasopharyngeal<br />
carcinoma: MRI and CT assessment.<br />
Neuroradiology 1997;39:741-6.<br />
72 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASES SERIES<br />
A pr<strong>of</strong>ile <strong>of</strong> renal tubular acidosis<br />
1<br />
K. Felix Jebasingh, 2 Salam Ranabir, 3 Lallan Prasad, 4 M.Bijoy, 5 Th. Premchand Singh<br />
Abstract:<br />
Objective: To Study the characteristic and<br />
biochemical feature <strong>of</strong> Renal tubular acidosis<br />
(RTA). Methods: Retrospective analysis <strong>of</strong> 4<br />
cases <strong>of</strong> RTA from the Department <strong>of</strong><br />
<strong>Medicine</strong>, Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal. Results: Our case series<br />
comprised <strong>of</strong> 4 cases. The mean age <strong>of</strong> our<br />
series was 41+ 18 years. The male to female<br />
ratio was 1:1.Three patients had recurrent<br />
periodic paralysis and one had proximal<br />
muscle weakness. The mean arterial<br />
bicarbonate was 14.97+ 2.98.The mean<br />
potassium, chloride and fasting urine pH levels<br />
were 2.45+ 1.33, 117+ 1.41 and 7.07+1.22<br />
respectively. All the patients had distal RTA<br />
(d-RTA). Out <strong>of</strong> four patients, one had dRTA<br />
secondary to autoimmune disease.<br />
Conclusion: From our case series we would<br />
like to highlight that in the presence <strong>of</strong><br />
recurrent periodic paralysis or persistent<br />
hypokalemia, RTA is a possibility. As these<br />
patients need bicarbonate, in addition to<br />
potassium supplements a proper evaluation<br />
is needed.<br />
Keywords: RTA, Metabolic acidosis, Periodic<br />
paralysis.<br />
Introduction: Renal tubular acidosis is the<br />
syndromic disorder characteristic by defect<br />
1. P.G. student, 2. Assistant Pr<strong>of</strong>essor, 3. Associate<br />
Pr<strong>of</strong>essor, 4. Senior Registrar, 5. Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> <strong>Medicine</strong>, RIMS, Imphal, Manipur.<br />
Corresponding Author:<br />
Dr.Lallan Prasad, Associate Pr<strong>of</strong>essor, Department<br />
<strong>of</strong> <strong>Medicine</strong>, Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal, Manipur.<br />
in the urinary acidification, in the absence <strong>of</strong><br />
defect in the nephron leading to metabolic<br />
acidosis and its systemic complication 1 .<br />
Patients who presents with hyperchloremic<br />
hypokalemic metabolic acidosis in the setting<br />
<strong>of</strong> normal renal function without<br />
gastrointestinal potassium loss, diagnosis <strong>of</strong><br />
renal tubular acidosis (RTA) needs to be<br />
considered 2 . Unlike hypokalemia due to renal<br />
or gastrointestinal loss these patients need<br />
bicarbonate along with potassium<br />
supplements and calcium/vitamin D<br />
supplements depending upon the type <strong>of</strong><br />
RTA 3 .<br />
There are three major type <strong>of</strong> renal tubular<br />
acidosis.<br />
1) Type 1 or distal renal tubular acidosis<br />
(dRTA) where there is failure <strong>of</strong> the kidney to<br />
lower the PH less than 5.5 in the presence <strong>of</strong><br />
metabolic acidosis. Fractional excretion <strong>of</strong><br />
bicarbonate is low and the patients may have<br />
nephrocalcinosis and nephrolithiasis.<br />
2) Type 2 or proximal renal tubular acidosis<br />
(pRTA) is characterized by glucosuria in the<br />
presence <strong>of</strong> normal plasma sugars,<br />
aminoaciduria, phosphaturia, with high<br />
fractional excretion <strong>of</strong> bicarbonate. The<br />
generalized defect in the proximal tubule is<br />
called Fanconi syndrome.<br />
3) Third type which is termed as Type 4 RTA<br />
may be due to hyporeninaemic<br />
hypoaldosteronism or secondary to<br />
obstructive uropathy 4, 5 . The patients will have<br />
high or high normal serum potassium with<br />
metabolic acidosis. This type <strong>of</strong> RTA is usually<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
73
CASES SERIES<br />
seen in chronic renal failure, diabetes mellitus,<br />
hypoadrenalism, drugs such as ACE<br />
inhibitors, heparin, trimethoprim etc 6 .<br />
In this article we are presenting a series <strong>of</strong><br />
patients with RTA admitted or attended the<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal,<br />
Manipur. Though RTA have been reported from<br />
the other parts <strong>of</strong> Indian subcontinent ,to best<br />
<strong>of</strong> our knowledge this is the first kind <strong>of</strong> case<br />
series from north eastern part <strong>of</strong> India.<br />
Materials and methods: This is a<br />
retrospective analysis <strong>of</strong> patients with clinical<br />
and biochemical features <strong>of</strong> RTA admitted or<br />
attended the <strong>Medicine</strong> department, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal. All<br />
patients underwent serum sodium, potassium,<br />
chloride, calcium and phosphate analysis in<br />
biochemistry department. Arterial blood gas<br />
(ABG) was also done to look <strong>for</strong> metabolic<br />
acidosis. Anion gap was calculated using the<br />
<strong>for</strong>mula (Serum Sodium+ Serum potassium)<br />
– (Serum chloride+ Serum bicarbonate). The<br />
normal anion gap is taken as 8±2 meq/l.<br />
Fasting urine pH was examined after a<br />
overnight fasting <strong>of</strong> at least 8 hours. Thyroid<br />
hormones were done to rule out thyrotoxicosis/<br />
hyperthyroidism. Ophthalmology evaluation<br />
was undertaken to look <strong>for</strong> causes <strong>for</strong> RTA.<br />
Ultrasonography <strong>of</strong> the abdomen was done<br />
<strong>for</strong> nephrocalcinosis/ nephrolithiasis<br />
evaluation. All the biochemistry results were<br />
pronounced as mean+SD.<br />
Results: Four patients with clinical and<br />
biochemical features <strong>of</strong> RTA were analyzed<br />
in our case series. All our patients had<br />
hypokalemia with normal anion gap,<br />
hyperchloremic metabolic acidosis. The<br />
metabolic acidosis was diagnosed with<br />
arterial blood gas. The male to female ratio<br />
was 1:1.The mean age <strong>of</strong> our patients was<br />
41 ± 18 years. Three <strong>of</strong> our patients presented<br />
with history <strong>of</strong> recurrent periodic paralysis and<br />
one had proximal muscle weakness. The<br />
mean arterial bicarbonate was 14.97±<br />
2.98.The mean potassium, chloride and<br />
fasting urine PH levels were 2.45±1.33, 117±<br />
1.41 and 7.07±1.22 respectively. All patients<br />
had normal thyroid status. All patients had<br />
normal alkaline phosphatase levels<br />
suggesting no bony involvement. Our entire<br />
patient has type 1 RTA. Only One patient had<br />
nephrocalcinosis in the ultrasonography <strong>of</strong> the<br />
abdomen and hypercalciuria in 24 hour<br />
urinary calcium. One patient with the distal<br />
RTA is <strong>of</strong> secondary to autoimmune disease.<br />
The causes <strong>of</strong> RTA in other patients could not<br />
be found. All the patients were given oral<br />
potassium in addition to bicarbonate either<br />
made in-house or as potassium citrate. One<br />
<strong>of</strong> the patients had phosphaturia (Tubular<br />
Maximum <strong>of</strong> Phosphate Reabsoption per<br />
Glomerular Filtration Rate-TmPO4/GFR) less<br />
than 2.5 and she was advised to take<br />
phosphate solution. The details <strong>of</strong> our patients<br />
are shown in table 1.<br />
Table 1. Pr<strong>of</strong>ile <strong>of</strong> Patients with RTA<br />
Discussion: RTA is characterized by a triad<br />
<strong>of</strong> generalized weakness or periodic paralysis<br />
with hypokalemia and systemic metabolic<br />
acidosis. The main objective is differentiating<br />
the type <strong>of</strong> RTA and the correction <strong>of</strong> metabolic<br />
acidosis 3, 4 .<br />
The diagnostic criteria <strong>for</strong> the RTA are as<br />
follows.<br />
1) Type -1 or dRTA- Fasting urine pH more<br />
than 5.5 in the presence <strong>of</strong> metabolic<br />
acidosis with Fractional excretion <strong>of</strong><br />
Bicarbonate-FEHCO3 less than 15%<br />
2) Type -2 or pRTA- Fasting urine pH less<br />
than 5.5 in the presence <strong>of</strong> metabolic<br />
acidosis with FEHCO3 more than 15% 2<br />
FEHCO3= urine Bicarbonate × plasma<br />
creatinine Plasma Bicarbonate x urine<br />
creatinine<br />
When a diagnosis <strong>of</strong> d-RTA is made the<br />
diagnostic work-up should always include<br />
ultrasonography <strong>for</strong> nephrocalcinosis or renal<br />
calculi, and measurement <strong>of</strong> urinary calcium<br />
and citrate excretion. Hypercalciuria and<br />
hyperphosphaturia is due to calcium and<br />
phosphate release from the bones due to<br />
<strong>change</strong> in H + buffer and systemic acidosis 1-<br />
74 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASES SERIES<br />
5<br />
. Hypercalciuria with hypocitraturia and high<br />
urine pH contribute to occurrence <strong>of</strong> calcium<br />
phosphate renal stones. Hypercalciuria is<br />
suspected when the 24-hr calcium excretion<br />
exceeds 4 mg/Kg/day. Hypocitraturia is said<br />
to be present when the 24 hr urinary citrate is<br />
below 2 mg/Kg/day 1 .<br />
All patients with idiopathic dRTA should<br />
undergo a <strong>for</strong>mal hearing evaluation, as they<br />
are prone <strong>for</strong> sensorineural deafness;<br />
deafness may not be present in infancy and<br />
can develop later 7 . Since dRTA in adults may<br />
be associated with systemic lupus<br />
erythematosus(SLE), Sjogren syndrome or<br />
chronic hepatitis, appropriate evaluation has<br />
to be done 3, 8, 9 . A subtype <strong>of</strong> RTA, caused by<br />
deficiency <strong>of</strong> carbonic anhydrase type II<br />
isoenzyme, is associated with<br />
osteopetrosis 10 . In suspected patients with<br />
incomplete dRTA, ammonium chloride loading<br />
test is done to confirm the diagnosis <strong>of</strong> dRTA.<br />
But it is not needed in patients who had<br />
systemic acidosis 11 .<br />
For the diagnosis <strong>of</strong> pRTA all the functions <strong>of</strong><br />
the proximal tubules have to be studied. The<br />
proximal is a major site <strong>for</strong> the reabsorption<br />
<strong>of</strong> filtered bicarbonate and a decreased<br />
threshold <strong>of</strong> bicarbonate reabsorption results<br />
in bicarbonaturia. The proximal tubules <strong>of</strong> the<br />
kidney are also the site <strong>for</strong> the absorption <strong>of</strong><br />
the aminoacids, glucose, anions such as<br />
citrate and phosphate. So the assessment <strong>for</strong><br />
aminoaciduria, glucosuria (in the presence <strong>of</strong><br />
normal plasma sugars) and osteomalacia<br />
have to be done in addition to phosphate<br />
excretion calculated using the Bijvoet<br />
nomogram 1-5 . Fractional excretion <strong>of</strong><br />
phosphate (FePO4) is calculated first and<br />
using the slide-rule method recommended by<br />
Bijvoet, Tubular Maximum <strong>of</strong> Phosphate<br />
Reabsoption per Glomerular Filtration Rate-<br />
(TmPO4/GFR) is calculated. The normal<br />
value <strong>of</strong> TmPo4/GFR is 2.8-4.4 mg/dL. If the<br />
value is less than 2.5, it indicates phosphaturia.<br />
Such patients need oral phosphate<br />
supplementation 12 .<br />
Fepo4= urine phosphate × plasma creatinine<br />
Plasma phosphate x urine creatinine<br />
It is also important to determine whether the<br />
defect is isolated or complete/generalized<br />
which is defined as Fanconi syndrome.<br />
Patients with pRTA should undergo eye<br />
examination to rule out cystinosis and Wilsons<br />
disease. Congenital enzyme deficiency such<br />
as Fabry’s disease, Ehlers Darlos syndrome,<br />
galactosemia, etc should also be<br />
screened <strong>for</strong> 3 .<br />
There are various causes <strong>of</strong> both proximal<br />
and distal RTA’s. But in real practice it is<br />
difficult to come to conclusion on the etiology<br />
<strong>for</strong> RTA 3 . In our cases series too, further<br />
evaluation to find the etiology <strong>for</strong> RTA could<br />
not be done because <strong>of</strong> limited facility in the<br />
centre.<br />
The treatment aim in dRTA is providing<br />
adequate bicarbonate in order to balance the<br />
H+ production. Oral potassium has also has<br />
be supplemented <strong>for</strong> normalizing the<br />
extracellular potassium to prevent life<br />
threatening periodic paralysis. In patients with<br />
nephrolithiasis/nephrocalcinosis, oral<br />
potassium citrate/bicarbonate therapy<br />
reduces the urinary calcium excretion thereby<br />
preventing the progression <strong>of</strong><br />
nephrocalcinosis/nephrolithiasis. Monitoring <strong>of</strong><br />
24 urinary calcium and citrate should be done<br />
in the follow up.<br />
The treatment goal <strong>for</strong> pRTA is correction <strong>of</strong><br />
chronic metabolic acidosis. Alkali treatment<br />
with potassium supplement is cornerstone in<br />
the treatment <strong>of</strong> pRTA to prevent systemic<br />
effects <strong>of</strong> metabolic acidosis. Some patients<br />
need massive dose <strong>of</strong> bicarbonate to maintain<br />
the bicarbonate levels and compliance is the<br />
problem in these patients as bicarbonate is<br />
an unpalatable compound. In such patients<br />
concomitant administration <strong>of</strong> a thiazide<br />
diuretic may help in reducing the quantity <strong>of</strong><br />
alkali treatment required. Correction <strong>of</strong><br />
acidosis in children with pRTA is particularly<br />
important in achieving normal linear growth<br />
rates. Supplemental calcium and activated<br />
vitamin D have to be given <strong>for</strong> these patients.<br />
For type IV RTA, treatment and prognosis<br />
depends on the underlying cause. The<br />
treatment <strong>for</strong> includes dietary modification and<br />
cation ex<strong>change</strong> resins, to reduce serum<br />
potassium and alkali administration 1-6 .<br />
In a retrospective analysis from Hyderabad,<br />
India 96 patients with distal RTA were<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
75
CASES SERIES<br />
analyzed. Their series showed that majority<br />
<strong>of</strong> children with dRTA had urological problems<br />
in contrast to autoimmune disorders in<br />
adults 13 . In the hypokalemic case series<br />
published from CMC Vellore, India 42 % <strong>of</strong><br />
patients had RTA. Out <strong>of</strong> the 13 patients with<br />
RTA, 10 had pRTA and 3 had dRTA 14 . In a<br />
case series from Malaysia they studied 16<br />
cases <strong>of</strong> RTA and emphasized on the long<br />
term follow up <strong>for</strong> such patients to prevent<br />
future life threatening complications 15 .From<br />
Kolkata, India 2 case reports <strong>of</strong> Wilsons’<br />
disease presenting as periodic paralysis due<br />
to dRTA had been reported by two different<br />
authors 16, 17 .<br />
In children, RTA can present as short stature<br />
or with features <strong>of</strong> rickets/ osteomalacia.<br />
From CMC Vellore, a short Klinefelter’s<br />
syndrome with features <strong>of</strong> rickets was<br />
reported, where the short stature is due to<br />
pRTA .But Klinefelter’s syndrome patients are<br />
supposed to be tall. So RTA is a cause <strong>for</strong><br />
short staure in children 18 .<br />
The long term management and follow up is<br />
important as it not only prevents future life<br />
threatening periodic paralysis but also<br />
prevents further complications due to<br />
metabolic acidosis and preserves the renal<br />
functions. Once the nephrocalcinosis sets in,<br />
it cannot be reverted back, but treatment with<br />
bicarbonate will prevent <strong>for</strong>m further<br />
progression <strong>of</strong> nephrocalcinois 1-6 .<br />
Conclusion: In the presence <strong>of</strong> persistent or<br />
recurrent hypokalemia without any<br />
gastrointestinal loss <strong>of</strong> potassium the<br />
likelihood <strong>of</strong> RTA is high. Unlike the patients<br />
with isolated hypokalemia, patients with<br />
hypokalemia and RTA should be given<br />
potassium and bicarbonate supplementation.<br />
Proper evaluation <strong>for</strong> type and etiology <strong>of</strong> the<br />
RTA is important in these patients. Early<br />
diagnosis and adequate treatment prevents<br />
life threatening periodic paralysis and further<br />
deterioration <strong>of</strong> the renal functions.<br />
Reference:<br />
1) Bagga A, Sinha A. Evaluation <strong>of</strong> Renal<br />
Tubular Acidosis. Indian J Pediatr<br />
2007;74 (7):679-86.<br />
2) Kumar S, Vaswani M, Srivastava RN, et<br />
al.Urinary net charge in hyperchloremic<br />
metabolic acidosis.Indian Pediatr. 1998<br />
Jan;35(1):13-8.<br />
3) Penney MD, Oleesky DA. Renal tubular<br />
acidosis. Ann Clin Biochem 1999; 36:<br />
408-22.<br />
4) Booth BE. Renal tubular acidosis:<br />
pathogenesis, diagnosis and treatment.<br />
Indian J Pediatr 1988; 55:379-94<br />
5) Saborio P, Krieg RJ, Ahmad TM,et al.<br />
Renal tubular acidosis in children. Saudi<br />
J Kidney Dis Transpl. 1997 Jul-<br />
Sep;8(3):235-46.<br />
6) Reddy P. Clinical approach to renal<br />
tubular acidosis in adult patients. Int J<br />
Clin Pract. 2011 Mar;65(3):350-60<br />
7) Mythili A, Subrahmanyam KA, Kumar<br />
KD. Type 1 renal tubular acidosis with<br />
sensorineural deafness. J Assoc<br />
Physicians India. 2007 Apr;55:303-5.<br />
8) Comer DM, Droogan AG, Young IS, et al.<br />
Hypokalaemic paralysis precipitated by<br />
distal renal tubular acidosis secondary<br />
to Sjögren’s syndrome. Ann Clin<br />
Biochem. 2008 Mar;45(Pt 2):221-5.<br />
9) Gera C, Mohapatra D, Calton N.<br />
Hypokalaemic paralysis secondary to<br />
distal renal tubular acidosis as the<br />
presenting symptom <strong>of</strong> systemic lupus<br />
erythematosus. Singapore Med J. 2011<br />
Jan;52(1):e1-3.<br />
10) Soriano JR. Renal tubular acidosis, the<br />
clinical entity. J Am Soc Nephrol 2002;<br />
13: 2160-2170.<br />
11) Lash JP, Arruda JAL. Laboratory<br />
evaluation <strong>of</strong> renal tubular acidosis. Clin<br />
Lab Med 1993; 13: 117-29<br />
12) Walton RJ, Bijvoet OL. Nomogram <strong>for</strong><br />
derivation <strong>of</strong> renal threshold phosphate<br />
concentration. Lancet. 1975 Aug<br />
16;2(7929):309-10.<br />
13) Jha R, Muthukrishnan J, Shiradhonkar S,<br />
et al.Clinical pr<strong>of</strong>ile <strong>of</strong> distal renal tubular<br />
acidosis. Saudi J Kidney Dis Transpl.<br />
2011 Mar;22(2):261-7.<br />
76 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASES SERIES<br />
14) Rao N, John M, Thomas N, et al.<br />
Aetiological, clinical and metabolic pr<strong>of</strong>ile<br />
<strong>of</strong> hypokalaemic periodic paralysis in<br />
adults: a single-centre experience. Natl<br />
Med J India. 2006 Sep-Oct;19(5):<br />
246-9.<br />
15) Zainal D. Renal tubular acidosis in<br />
Kelantan, Malaysia—a case review.<br />
Singapore Med J. 1994 Jun;35(3):<br />
303-5.<br />
16) Thapa R, Biswas B, Mallick D.Recurrent<br />
limb weakness in a 17-year-old boy.Clin<br />
Pediatr (Phila). 2009 Jun;48(5):555-7.<br />
17) Chakraborty PP, Mandal SK,<br />
Bandyopadhyay D, et al. Recurrent limb<br />
weakness as initial presentation <strong>of</strong><br />
Wilson’s disease. Indian J Gastroenterol.<br />
2007 Jan-Feb;26(1):36-8<br />
18) Jebasingh F, Paul TV, Spurgeon R, et al.<br />
Klinefelter’s syndrome with renal tubular<br />
acidosis: impact on height. Singapore<br />
Med J. 2010 Feb;51(2):e24-6.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
77
CASES SERIES<br />
Head and neck malignancies in HIV infected persons-report <strong>of</strong> 9 cases<br />
1<br />
Rino K, 2 Thingbaijam S, 3 Sobita P, 1 Momin E, 1 Kalpana TH<br />
Abstract<br />
Objectives: To analyze the spectrum <strong>of</strong> head<br />
and neck malignancies in HIV infected cases<br />
registered at Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal. Methods: We have<br />
retrospectively reviewed records <strong>of</strong> head and<br />
neck malignancies in HIV infected persons<br />
registered at our hospital from Sept 2009 to<br />
October 2010 to analyze HIV associated head<br />
and neck malignancies. Results: Nine cases<br />
<strong>of</strong> HIV-associated head and neck<br />
malignancies were identified. All the patients<br />
were below 50 years (age range 18-43yrs).<br />
Five were males. There were three cases <strong>of</strong><br />
NHL, two cases <strong>of</strong> NPC, one carcinoma ex<br />
pleomorphic adenoma parotid, one Kaposi<br />
sarcoma, one maxillary carcinoma and one<br />
SCC. NHL was the most common overall<br />
malignancy while NPC happened to be the<br />
most common non AIDS defining malignancy.<br />
All patients were in advanced stage <strong>of</strong> AIDS<br />
and 75% were in the advanced stage <strong>of</strong><br />
malignancy (II&IV). One patient expired while<br />
the remaining patients are currently on followup.<br />
Conclusion: We believe that there is an<br />
urgent need to direct research ef<strong>for</strong>ts <strong>for</strong> timely<br />
prevention, screening and management <strong>of</strong> HIV<br />
1. Post graduate trainee; 2. Associate Pr<strong>of</strong>essor;<br />
3. Assistant Pr<strong>of</strong>essor; Department <strong>of</strong><br />
Otorhinolaryngology, Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences (RIMS), Imphal.<br />
Corresponding author:<br />
Dr. S. Thingbaijam, Associate Pr<strong>of</strong>essor, Dept <strong>of</strong><br />
Otorhinolaryngology, Regional Institute <strong>of</strong> <strong>Medical</strong><br />
Sciences, Imphal – 795004<br />
Email – dr_sthingbaijam@yahoo.in<br />
infected persons with Head and neck<br />
malignancies. Cancer screening in HIVinfected<br />
patients should be considered at an<br />
earlier age than in the general population.<br />
Key words: Head and neck malignancy in HIV<br />
infected persons, AIDS defining malignancy,<br />
Non AIDS defining malignancy.<br />
Introduction: According to NACO (2009) 33.4<br />
Million people are living with HIV and there were<br />
2 million HIV/AIDS deaths in 2008. India<br />
contributes 2.4 million whereas Manipur<br />
contributes 8%. Malignancies are the no 1<br />
cause <strong>of</strong> death in HIV+ persons. 1 AIDS<br />
associated carcinoma is clinically classified<br />
as AIDS defining carcinoma (ADC), non AIDS<br />
defining carcinoma (NADC) and other<br />
carcinoma in HIV-infected community like<br />
multiple myeloma, s<strong>of</strong>t tissue sarcoma, etc<br />
including head and neck carcinoma (HNCA).<br />
ADC includes Kaposi sarcoma, non Hodgkin’s<br />
lymphoma(NHL) and invasive cervical<br />
carcinoma while NADC include Hodgkin’s<br />
lymphoma, anal carcinoma, lung carcinoma,<br />
testicular germ tumors. 2 With the advent <strong>of</strong><br />
HAART ( highly active antiretroviral therapy),<br />
malignancies are increasing in importance as<br />
a cause <strong>of</strong> AIDS-Related morbidity and<br />
mortality. 3 HIV-Infected persons have higher<br />
incidence <strong>of</strong> developing NADC than among<br />
the general population. 4 NADC incidence have<br />
surpassed that <strong>of</strong> ADC in HIV infected persons<br />
and cancer prevalence ranges from 7-15 %<br />
as cause <strong>of</strong> mortality in HIV population. 5 ADC<br />
now cause 13% <strong>of</strong> deaths in HIV + persons 1<br />
whereas prevalence <strong>of</strong> HNCA is 27%. 6<br />
Although it remains unclear whether HIV-1<br />
78 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASES SERIES<br />
acts directly as an oncogenic agent, it may<br />
contribute to the development <strong>of</strong> malignancies<br />
through several mechanisms. Infection by<br />
oncogenic viruses (e.g., cytomegalovirus,<br />
Epstein-Barr virus, HHV-5, HHV-8, HPV-16 and<br />
HPV-18), impaired immune surveillance,<br />
dysregulation <strong>of</strong> cytokine pathways and growth<br />
factor production, chronic B cell stimulation,<br />
and imbalance between cellular proliferation<br />
and differentiation may all contribute to the<br />
development <strong>of</strong> HIV/AIDS-associated<br />
malignancies. 2<br />
Objectives: To review the number <strong>of</strong> HIV<br />
infected persons with Head and Neck<br />
malignancy admitted in Regional Institute <strong>of</strong><br />
<strong>Medical</strong> Sciences Hospital and to find out the<br />
different types <strong>of</strong> head and neck malignancies<br />
HIV infected persons.<br />
Materials and Methods: It is a Retrospective<br />
review record <strong>of</strong> HNCA patients from Sept<br />
2009 – Oct 2010 to identify and analyze types<br />
<strong>of</strong> HIV-associated Head and Neck carcinoma<br />
(HNCA) encountered in the Regional Institute<br />
<strong>of</strong> <strong>Medical</strong> Sciences, Imphal. HIV diagnosed<br />
during the work up. In<strong>for</strong>mation about<br />
Histology, CD4 counts and stage <strong>of</strong> HIV status<br />
(according to WHO clinical staging <strong>of</strong> HIV<br />
disease) as well as the malignancies were<br />
recorded.<br />
Results: The results <strong>of</strong> the study done on 9<br />
cases <strong>of</strong> HIV infection with head and neck<br />
malignancy are presented below:<br />
Out <strong>of</strong> 9 patients 3(33.3%) presented with<br />
NHL, 1(11.1%) with Kaposi sarcoma (KS) and<br />
the remaining 5(55.5%) presented with Non<br />
AIDS Defining Carcinoma(NADC) like<br />
Nasopharyngeal carcinoma (NPC), Ex<br />
pleomorphic carcinoma parotid (EPC),<br />
carcinoma maxilla (CM) and Squamous cell<br />
Table 1. Pr<strong>of</strong>il <strong>of</strong> HIV infected patients with head and<br />
neck malignancies<br />
carcinoma (SCC). NHL was the most<br />
common overall malignancy comprising <strong>of</strong> 3<br />
patients (33.3%) as shown in table 1. NPC<br />
happened to the most common NADC<br />
comprising <strong>of</strong> 2 cases (40%). The age range<br />
among the patients was found to be 18-43<br />
years (mean 36 years) and male; female<br />
ration is 1.0.8 as shown in table 2. The<br />
youngest patient was <strong>of</strong> 18 yrs. with NHL and<br />
the oldest patient was 43 yrs. old with KS. 7<br />
patients (75%) were in stage III/IV <strong>of</strong><br />
malignancy and all the patients were in stage<br />
III/IV <strong>of</strong> HIV disease as shown in table 3. 55.5%<br />
<strong>of</strong> the patients have NADC type <strong>of</strong> HNCA as<br />
seen in table 4.<br />
Table 2: Sex distribution <strong>of</strong> head and neck<br />
malignancies in HIV infected persons<br />
Table 3: WHO clinical staging <strong>of</strong> HIV among the HNCA<br />
patients<br />
Table 4: Types <strong>of</strong> head and neck malignancy among<br />
the cases<br />
ADC~ Aids defining cancer, NADC~ Non AIDS<br />
defining cancer<br />
Dicussion: In our review the age range was<br />
18-36 years and mean age 36 years. The<br />
patients here were <strong>of</strong> a younger age, this is in<br />
keeping with the findings <strong>of</strong> other studies. 6 We<br />
believe that HIV-infected individuals are at<br />
greater risk <strong>of</strong> acquiring HNCA at a younger<br />
age than their HIV-seronegative counterparts.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
79
CASES SERIES<br />
Male to female ratio is 1:0.8 and this<br />
complements the report in other studies 6 .<br />
Since the emergence <strong>of</strong> AIDS some ADC are<br />
said to be increasing even among females<br />
though no apparent reason has been found.<br />
75% <strong>of</strong> the patients were in Stage III/IV <strong>of</strong><br />
malignancy. This indicates that HNCA among<br />
the HIV infected persons are diagnosed late.<br />
Although Kaposi sarcoma is considered as<br />
the most common AIDS Defining Carcinoma<br />
(ADC), by other literatures 6 , the present study<br />
found Non Hodgkin’s Lumphoma as the most<br />
common AIDS defining casinima which is<br />
comparable to the report <strong>of</strong> Rabkin C 3 .<br />
According to recent studies, HAART use may<br />
prevent most excess risk <strong>of</strong> ADC, but not that<br />
<strong>of</strong> NADC. 3,7 In the present study we found more<br />
number <strong>of</strong> HIV infected patients with NADC<br />
and the ratio <strong>of</strong> NADC: ADC was 1.2:1. This<br />
may be attributed to the advent <strong>of</strong> HAART<br />
which as reported in other studies decreased<br />
the occurrence <strong>of</strong> ADC. 7 Infact, very recent<br />
studies have shown that the incidence <strong>of</strong><br />
many types <strong>of</strong> NADC is higher among HIV<br />
infected persons than among the general<br />
population from 1992 to 2003. 4<br />
Conclusion: From our review we conclude<br />
that NHL is the most common HIV associated<br />
Head and Neck malignancy encountered in<br />
our institute. NADCs in Head and neck are<br />
almost equally prevalent as ADC among the<br />
HIV patients. Head and neck NADC in HIV<br />
infected persons occurs in early age and are<br />
diagnosed late. We believe that there is an<br />
urgent need to improve collection <strong>of</strong><br />
epidemiological data and to direct research<br />
ef<strong>for</strong>ts <strong>for</strong> timely prevention, screening and<br />
management <strong>of</strong> HIV infected persons with<br />
Head and neck malignancies. Cancer<br />
screening in HIV-infected patients should be<br />
considered at an earlier age than in the general<br />
population, keeping in mind not to overlook the<br />
NADC.<br />
Reference:<br />
1. Bonnet F, Lewden C, May T, Heripret L,<br />
Jougla E, Bevilacqua S, Costagliola D,<br />
Salmon D, Chêne G, Morlat P<br />
Malignancy-related causes <strong>of</strong> death in<br />
human immunodeficiency virus-infected<br />
patients in the era <strong>of</strong> highly active<br />
antiretroviral therapy.CANCER 2004<br />
101:317-324<br />
2. Barbaro G, Barbarini G. HIV infection and<br />
cancer in the era <strong>of</strong> highly active<br />
antiretroviral therapy. oncology reports<br />
2007; 17: 1121-26<br />
3. Rabkin C. AIDS and cancer in the era <strong>of</strong><br />
highly active antiretroviral therapy<br />
(HAART). Eur j cancer 2001 July;<br />
37(10):1316-19.<br />
4. Patel P, Hanson DL, Sullivan PS, Novak<br />
AM, Moorman AC, Tong TC, et al.<br />
incidence <strong>of</strong> types <strong>of</strong> cancer among HIVinfected<br />
persons compared with the<br />
general population in the united states.<br />
Ann intern med 2008 May;148(10):728-<br />
36<br />
5. Ruiz M.Certain non-AIDS-defining<br />
cancers higher in HIV population. HIV<br />
clinicians winter 2009;21(4):13-16<br />
6. Butt F, Chindia M, F Rana, Machigo F.<br />
Pattern <strong>of</strong> head and neck malignant<br />
neoplasms in HIV-infected patients in<br />
Kenya. Int j oral maxill<strong>of</strong>ac surg 2008<br />
Sept;37(10):907-11<br />
7. Berretta M, Cinelli R, Martellotta F, Spina<br />
M, Vaccher E, Tirelli U. Therapeutic<br />
approaches to AIDS-related<br />
malignancies. Oncogene 2003: 22:<br />
6646–6659.<br />
80 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
REFLECTED ARTICLES OF PREVIOUS ISSUES<br />
1. Title : Oral <strong>change</strong>s in diabetics - a review<br />
Authors - Ng. Sanjeeta, W. Robindro, T. Nabachandra Singh<br />
Published in JMS Vol. 25 (1) January, 2001 on page 55-58 as review articles<br />
The above article has been retracted due to dispute regarding the contribution and Authorship<br />
<strong>of</strong> one <strong>of</strong> the Authors. The article may further be resubmitted <strong>for</strong> publications in subsequence<br />
issues <strong>of</strong> JMS when the dispute is settled.<br />
2. Title : Herpes zodter in a hrlthy adult: Report <strong>of</strong> a case with oro-cutaneous presentations<br />
Authors - Ng. Sanjeeta, W. Robindro Singh, O. Brajachand Singh<br />
Published in JMS Vol. 25 (2) May, 2011 on page 99-101 as a case report<br />
The above article has been retracted due to dispute regarding the contribution and Authorship<br />
<strong>of</strong> one <strong>of</strong> the Authors. The article may further be resubmitted <strong>for</strong> publications in subsequence<br />
issues <strong>of</strong> JMS when the dispute is settled.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
81
CASE REPORT<br />
“Deltoid paralysis following post herpetic axillary nerve neuropathy: Review<br />
<strong>of</strong> literatures”<br />
1<br />
N. Romi Singh, 2 C. Zonunsanga, 2 Hmingthanmawii , 3 S. Langlunthang Simte, 2 S. Kharlukhi<br />
Introduction: Herpes zoster infection<br />
causing motor neuropathy is rarely reported.<br />
Broadbent 1 in 1866 was the first to describe a<br />
“case <strong>of</strong> herpetic eruption in the course <strong>of</strong><br />
branches <strong>of</strong> the brachial plexus followed by<br />
partial paralysis in corresponding motor<br />
nerves.” Few cases have been reported about<br />
motor involvement 2-5 by this organism as it<br />
mainly causes sensory symptoms. Infection<br />
is usually limited to sensory ganglion and<br />
nerve roots but it may occasionally involve<br />
motor system leading to paresis <strong>of</strong> muscles<br />
supplied by the affected nerve segment 6 .<br />
Isolated axillary nerve involvement is rare in<br />
such infection and here, we report a case <strong>of</strong><br />
axillary nerve motor neuropathy following<br />
herpes zoster infection in view <strong>of</strong> the rarity <strong>of</strong><br />
such occurance and review <strong>of</strong> the<br />
contemporary literatures is be discussed.<br />
Case report: A 35 year old married male who<br />
is in active service by pr<strong>of</strong>ession reported with<br />
complaints <strong>of</strong> inability to lift his right arm <strong>for</strong><br />
two weeks <strong>of</strong> insidious onset. There was<br />
neither history <strong>of</strong> trauma nor fever. On<br />
examination, there was vesiculoerythematous<br />
rash / scar on right upper limb<br />
1. Associate Pr<strong>of</strong>essor, 2. Postgraduate student,<br />
3. House Officer, Physical <strong>Medicine</strong> & Rehabilitation<br />
Department, Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences,<br />
Imphal<br />
Corresponding author:<br />
Dr. N. Romi Singh<br />
Associate Pr<strong>of</strong>essor<br />
Department <strong>of</strong> Physical <strong>Medicine</strong> & Rehabilitation<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal – 795<br />
004 Manipur (India)<br />
E-mail:dr.romi.singh@gmail.com<br />
extending from the upper arm laterally to the<br />
dorsal aspect <strong>of</strong> <strong>for</strong>earm with a tattoo mark<br />
over the deltoid muscle (figures 1 a. ).<br />
Fig.1 (a)<br />
Fig.1 (b)<br />
Fig.1 (a) : Showing scar / rashes over shoulder<br />
Fig 1 (b): Showing inability to fully abduct the arm<br />
actively beyond 15 0 (Deltoid paresis)<br />
He had noticed the painful vesiculo- bullous<br />
rash two weeks back, which eventually dried<br />
up by the time he reported to us. Motor power<br />
<strong>of</strong> deltoid muscle was 1/5, other muscles<br />
around the shoulder were <strong>of</strong> good power.<br />
Range <strong>of</strong> movement (ROM) <strong>of</strong> shoulder<br />
(passive) was normal, but active abduction<br />
<strong>of</strong> shoulder ROM was limited to first 15 0 with<br />
the scapulo-thoracic participation (figure 1 b.).<br />
Sensory affection in <strong>for</strong>m <strong>of</strong> hypo-esthesia<br />
was present over badge area <strong>of</strong> the arm. We<br />
consented the patient <strong>for</strong> retroviral antibody<br />
<strong>for</strong> human immuno-deficiency virus in view <strong>of</strong><br />
his occu-pation and extensive tatoo mark, but<br />
was negative <strong>for</strong> retroviral antibody and no<br />
significant findings were observed <strong>for</strong> the<br />
routine investigations. No electro-physio-<br />
82 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASE REPORT<br />
logical test was per<strong>for</strong>med as the tale-tale<br />
features <strong>of</strong> herpes zoster infection was already<br />
evident. His past illness was insignificant but<br />
he had affection with varicella zoster virus<br />
(VSV) during childhood. He was treated with<br />
supportive treatment like neurotropic<br />
vitamines and gabapantin only. No antiretroviral<br />
treatment was administered as there<br />
was no active vesiculo-bullous eruptive stage<br />
at the time <strong>of</strong> presentation. He was advised<br />
to undergo regular shoulder ROM exercise<br />
and has been put on physical therapy modality<br />
viz. electrical stimulation <strong>for</strong> the paralysed<br />
deltoid muscle, besides advice to support the<br />
shoulder with a sling support to the arm to<br />
prevent any possible traction subluxation <strong>of</strong><br />
shoulder by weight <strong>of</strong> gravity. The patient is<br />
being followed up <strong>for</strong> motor recovery <strong>of</strong> the<br />
paralyzed deltoid.<br />
Discussion: The common affection <strong>of</strong> herpes<br />
zoster usually occurs in thoracic (53%),<br />
cervical roots viz. C , C , C ( 20%),<br />
2 3 1<br />
opthalmic division <strong>of</strong> trigeminal nerve (15%)<br />
and lumbo-sacral (11%) dermatomes <strong>of</strong><br />
body 7 . Moschella 8 found most common<br />
involvement <strong>of</strong> C & L dermatomes. Herpes<br />
2 2<br />
zoster or shingles infection is the reactivation<br />
<strong>of</strong> dormant VZV in the dorsal root ganglia 3,9 .<br />
Segmental motor paresis is rare and only few<br />
cases <strong>of</strong> brachial plexitis have been reported<br />
in the literature. Axillary nerve is <strong>for</strong>med from<br />
the posterior cord <strong>of</strong> brachial plexus and<br />
supplies the deltoid muscle. We report this<br />
case with axillary nerve affection causing<br />
paralysis <strong>of</strong> deltoid muscle folowing herpes<br />
zoster infection in a normal immune status<br />
adult. The patient had history <strong>of</strong> childhood VZV<br />
infection but not suffering from any immunocompromised<br />
status viz. human immunedefficiency<br />
virus infection, myeloproliferative<br />
disorders under chemotherpeutic treatment,<br />
etc. The reactivation occurs when immunity<br />
to VZV declines because <strong>of</strong> aging or<br />
immunosuppression. Hence, herpes zoster<br />
infection can occur at any age but most<br />
commonly affects the elderly population or<br />
immunocompromized patients 9 .<br />
Bhargava R et al 10 also reported a case <strong>of</strong><br />
isolated axillary nerve palsy following herpes<br />
zoster in a 52 year old man in a normal<br />
immune status patient with eruptive rashes<br />
completely healed by two weeks time. The<br />
deltoid paralysis with no improvement in<br />
motor power was persisting till three months<br />
post herpetic eruption. No significant post<br />
herpetic neuralgia was also reported. We also<br />
did not find any unbearable post herpetic<br />
neuralgia in the case reported herein except<br />
<strong>for</strong> the marked deltoid weakness. Probably the<br />
post herpetic neuralgia as normally<br />
encountered in the dorsal root involment is <strong>of</strong><br />
less magnitude in such cases when there is<br />
predominant motor / anterior horn pathway<br />
involment leading peripheral nerve motor<br />
neuropathy.<br />
Eban R 11 also described a case <strong>of</strong> deltoid<br />
muscle paresis after cervical herpes zoster<br />
and subsequent painful shoulder with marked<br />
subluxation <strong>of</strong> head <strong>of</strong> humerus. Bhargava R<br />
et al 10 also had observed dropping and<br />
flattening <strong>of</strong> shoulder after 3 months <strong>of</strong> follow<br />
up, probably due to disuse atrophy following<br />
the deltoid paralysis. The present case has<br />
been given due care <strong>for</strong> prevention <strong>of</strong> any<br />
possible shoulder subluxation due to weak<br />
deltoid action by prescribing a shoulder<br />
support sling during early phase <strong>of</strong> recovery.<br />
Hopefully with the return <strong>of</strong> deltoid power and<br />
proper biomechanical advice, he may be<br />
prevented from further complication <strong>of</strong><br />
shoulder subluxation as reported by the two<br />
authors 10,11 .<br />
The cause <strong>of</strong> motor neuropathy in case <strong>of</strong><br />
herpes zoster infection is not exactly clear.<br />
However, there are probably few possible<br />
factors which have been proposed <strong>for</strong> the<br />
motor neuropathy like, (i) gangliomuscular<br />
disease subsequent to infection <strong>of</strong><br />
propioceptive ganglion cells (ii) myositis 12 ,<br />
(iii) acquired demyelination <strong>of</strong> the peripheral<br />
nerve 13 etc. Schmidbauer M et al 12 have<br />
demonstrated varice1la zoster virus in<br />
myositic masseter muscle in a case <strong>of</strong><br />
trigeminal nerve affected by herpes zoster.<br />
Even if myositis occurs with herpes zoster, it<br />
is not clear, if myositis or some other factors<br />
were responsible <strong>for</strong> the muscle paralysis .<br />
Alshekhlee A et al 4 described three patients<br />
who exhibited classic symptoms <strong>of</strong> herpes<br />
zoster infection <strong>of</strong> the upper limb with various<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
83
CASE REPORT<br />
neuropathic findings, including multiple<br />
neuropathies, radiculopathy, and brachial<br />
plexopathy. As the distribution <strong>of</strong> weakness<br />
and electrodiagnostic findings involved not only<br />
the concerned dermatome, further<br />
electrodiagnostic studies per<strong>for</strong>med on one<br />
such patient showed evidence <strong>of</strong> acquired<br />
demyelination. Hence, spread <strong>of</strong> the infectious<br />
process to the axon and myelin sheath <strong>of</strong><br />
peripheral nerve may probably be responsible<br />
<strong>for</strong> the motor weakness in case <strong>of</strong> herpes<br />
zoster infection.<br />
Conclusion: We have reported the case <strong>for</strong><br />
the rare occurance <strong>of</strong> axillary nerve neuropathy<br />
causing deltoid palsy following post herpes<br />
zoster infection in a case <strong>of</strong> normal immune<br />
status adult individual. Early and prompt<br />
management with exercise therapy and<br />
biomechanical support intervention to prevent<br />
complications like subluxation <strong>of</strong> the shoulder<br />
will be the cornerstone <strong>for</strong> management <strong>for</strong><br />
axillary nerve neuropathy following herpes<br />
zoster, besides antiviral and supportive<br />
medications.<br />
References:<br />
1. Taterka JH, O’Sullivan ME. Motor<br />
complications <strong>of</strong> Herpes Zoster JAMA.<br />
1943;122(11):737-739. doi: 10.1001/<br />
jama.1943.02840280021006 [Pubmed]<br />
2. Aktas I, Akgun K, Gunduz OH. Axillary<br />
mononeuropathy after herpes zoster<br />
infection mimicking subacromial<br />
impingement syndrome. Am J Phys Med<br />
Rehabil. 2008 Oct;87(10):85961.<br />
3. Jeevarethinam A, Ihuoma A, Ahmad N.<br />
Herpes zoster brachial plexopathy with<br />
predominant radial nerve palsy. Clin<br />
Med. 2009;9(5):5001.<br />
4. Alshekhlee A, Tay E, Buczek M, Shakir<br />
ZA, Katirji B. Herpes zoster with motor<br />
involvement: discordance between the<br />
distribution <strong>of</strong> skin rash and localization<br />
<strong>of</strong> peripheral nervous system dysfunction.<br />
J Clin Neuromuscul Dis. 2011;12(3):<br />
153-7.<br />
5. Burkman KA, Gaines RW Jr, Kashani<br />
SR, Smith RD. Herpes zoster: a<br />
consideration in the differential diagnosis<br />
<strong>of</strong> radiculopathy. Arch Phys Med<br />
Rehabil. 1988;69(2):1324.<br />
6. Denny - Brown D, Adams R D,<br />
Fitzgerald,P J. Pathologic features <strong>of</strong><br />
herpes zoster : a note on geniculate<br />
herpes. Arch Neurol Psychiatr 1944; 51 :<br />
216-31.<br />
7. Nagington J, Rook A, Highest AS. Virus<br />
and related infection : Varicella and zoster.<br />
In : Text book <strong>of</strong> Dermatology (Rook A,<br />
Wilkinson DS, Ebling FJG, et al eds), 4th<br />
edn. Bombay Ox<strong>for</strong>d University Press,<br />
1987; 680-5.<br />
8. Burnett JW, Cruteher WA. Viral and<br />
Rickettsial infections: Herps zoster. In :<br />
Dermatology (Moschella SL, Hurley HJ,<br />
eds), 2nd edn. New Delhi: Jaypee<br />
brothers, 1985; 686-9.<br />
9. Sampathkumar P, Drage LA, Martin DP.<br />
Herpes zoster (shingles) and postherpetic<br />
neuralgia. Mayo Clin Proc. 2009<br />
Mar;84(3):274-80.<br />
10. Bhargava R, Agarwal US, Narayan R.<br />
Axillary nerve palsy following herpes<br />
zoster. Indian J Dermatol Venereol Leprol<br />
1994;60:97-8.<br />
11. Eban R. Cervical herpes zoster and<br />
shoulder Pain. Br Med J 1978; 177: 21.<br />
12. Schmidbauer M, Budka H, Pilz P, Kurata<br />
T, Hondo R. Presence, distribution and<br />
spread <strong>of</strong> productive varicella zoster virus<br />
infection in nervous tissue, Brain 1992;<br />
115 : 383-98.<br />
84 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASE REPORT<br />
Fibrocalculus pancreatic diabetes - a case report<br />
1<br />
Dhanaraj Singh Chongtham, 2 Sambhaji Raut, 3 Ranabir Salam, 4 S. Subhashchandra, 5 M. Kulachandra<br />
Case Report<br />
A twenty year unmarried, non-alcoholic<br />
female,from low socioeconomic status,<br />
Christian by religionfrom Khongsang, Manipur<br />
was admitted at <strong>Medicine</strong> ward <strong>of</strong> Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal with<br />
chief complaints <strong>of</strong> pain in abdomen since<br />
two years, significant weight loss and<br />
indigestion since last one year. Pain in<br />
abdomen was dull aching, present mainly in<br />
upper abdomen and aggravated after taking<br />
food. There was no history <strong>of</strong> cough, fever,<br />
night sweatsand previous history <strong>of</strong><br />
tuberculosis or bleeding per rectum. She did<br />
not give any history <strong>of</strong> diabetes mellitus and<br />
tuberculosis in the family. Her bowel habits<br />
are disturbed and appetite is decreased.On<br />
general physical examination she was found<br />
to be malnourished (Body Mass Index<br />
16.43kg/m 2 ) with mild pallor, sparse hairs on<br />
head. Per abdominal examination revealed flat<br />
abdomen with tenderness in umbilical,<br />
epigastric and left hypochondrium. There was<br />
no guarding, rigidity or any lump, other<br />
systems were within normal limits. On<br />
investigation, random blood sugar (RBS) was<br />
350 mg%,complete hemogram was normal,<br />
kidney function tests were within normal limits,<br />
1. Asso. 2. Pr<strong>of</strong>. P.G. Student, 3. Assist. Pr<strong>of</strong>.,<br />
Department <strong>of</strong> <strong>Medicine</strong> Assist 4. Pr<strong>of</strong>. Department<br />
<strong>of</strong> Radiodiagnosis, 5. Pr<strong>of</strong>essor and Head,<br />
Department <strong>of</strong> <strong>Medicine</strong>, Regional Institute <strong>of</strong><br />
<strong>Medical</strong> Sciences, Imphal.<br />
Address <strong>for</strong> correspondence:<br />
Dr Dhanaraj Singh Chongtham, Department <strong>of</strong><br />
<strong>Medicine</strong>, RIMS, Imphal 795004<br />
Email: dhanarajcardiology@yahoo.co.in<br />
alkaline phosphatase was364KAU, SGOT<br />
was 184Uand SGPT was 276U. Urinalysis<br />
showed glycosuria <strong>of</strong> 2%. Keeping in mind<br />
some chronic illness patient was started on<br />
symptomatic management followed by X-ray<br />
abdomen which showed multiple calcified<br />
lesions grouped together in linear fashion in<br />
upper abdomen centrally, in front <strong>of</strong> L1-L3<br />
lumbar vertebral level suggestive <strong>of</strong> pancreatic<br />
calcification (Fig. 1).<br />
Fig.1: Plain X-ray Abdomen showing pancreatic<br />
calcification<br />
Fig. 2: Contrast enhanced CT abdomen axial image<br />
showing ductal parenchymal and periductal<br />
calcification in head and uncinate process <strong>of</strong><br />
pancreas.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
85
CASE REPORT<br />
Fig. 3: Contrast enhanced CT abdomen axial image<br />
showing ductal and parenchymal calcification in<br />
body and tail region <strong>of</strong> pancreas.<br />
Ultrasonography (USG) whole abdomen<br />
showed outline <strong>of</strong> pancreas with extensive<br />
parenchymal and ductal calcifications with<br />
loss <strong>of</strong> normal parenchymal echotexture.<br />
Major pancreatic duct diameter was 4.4 mm.<br />
(Fig. 2). These features were suggestive <strong>of</strong><br />
chronic calcific pancreatitis. Fasting and post<br />
prandialblood sugar were 304 and 382mg%<br />
respectively. Montoux test was negative<br />
measuring 2×2mm. Fasting and post prandial<br />
blood sugar level and urine dipsticks charting<br />
were done <strong>for</strong> adjustment <strong>of</strong> Insulin doses.<br />
Contrast enhanced (CECT) abdomen<br />
showed pancreas measuring 16 mm at body<br />
with irregular margins (Fig. 3). There is<br />
multifocal extensive calcification in<br />
parenchyma and ducts causing irregular<br />
ductal dilatation. Main pancreatic duct<br />
measures 8mm in diameter these features<br />
suggestive <strong>of</strong> chronic calcific pancreatitis with<br />
parenchymal atrophy.<br />
Barium meal study was within normal limits,<br />
serum calcium was within normal limits,<br />
glycosylated Hb was 17.8%.Then patient was<br />
started on low dose mixed Insulin and<br />
pancreatic enzyme supplementation. Patient<br />
was receiving mixed insulin(50/50) 35/30 units<br />
with voglibose 0.3 mg and pancreatic<br />
enzymes at the time <strong>of</strong> discharge. Patient was<br />
symptomatically better and fasting post<br />
prandial blood sugar level was within normal<br />
limits at the time <strong>of</strong> discharge.<br />
Discussion: Tropical chronic pancreatitis<br />
(TCP) is a juvenile <strong>for</strong>m <strong>of</strong> chronic,<br />
calcific,non-alcoholic pancreatitis seen<br />
almost exclusively in developing countries <strong>of</strong><br />
the tropical world. The classical triad <strong>of</strong> tropical<br />
chronic pancreatitis is abdominal pain,<br />
steatorrhoea and diabetes. When diabetes is<br />
present the condition is calledFibrocalculus<br />
pancreatic diabetes (FCPD) which is thus a<br />
later stage <strong>of</strong> TCP. 1 Severalterms had been<br />
earlier proposed <strong>for</strong> this syndrome including<br />
tropicalcalcific pancreatitis, tropical chronic<br />
pancreatitis, tropical pancreatic diabetes,<br />
nutritional pancreatitis, endemic pancreatic<br />
syndrome, etc. As the term Fibrocalculus<br />
Pancreatic Diabetes was introduced by the<br />
World Health Organization Report this is the<br />
preferred term used by diabetologists, while<br />
the term Tropical Calcific Pancreatitis (TCP)<br />
is used by gastroenterologists. 2 The<br />
prevalence <strong>of</strong> FCPD very low, in one <strong>of</strong> study<br />
from southern urban areas <strong>of</strong> India was shown<br />
to be 0.36 % <strong>of</strong> total diabetic population. 3 The<br />
single largest series <strong>of</strong> cases <strong>of</strong> FCPD<br />
reported to date is from the southwestern state<br />
<strong>of</strong> Kerala in India, where Geevarghese and<br />
Pitchumoni observed this disease in endemic<br />
proportions in two major medical college<br />
hospitals. Indeed, Geevarghese collected one<br />
<strong>of</strong> the largest series in the world (over 1700<br />
patients) and two monogramson the subject<br />
were published by him and isthere<strong>for</strong>e<br />
<strong>of</strong>tenreferred to as “Father <strong>of</strong> Pancreatic<br />
Diabetes”. 2<br />
The cardinal manifestations <strong>of</strong> TCP are<br />
recurrent abdominal pain in childhood,<br />
followed by onset <strong>of</strong> diabetes mellitus a few<br />
years later. Early reports on TCP identified<br />
patients only in the late stages <strong>of</strong> the disease<br />
when extreme emaciation and other obvious<br />
clinical signs <strong>of</strong> protein malnutrition, such as<br />
bilateral parotid gland enlargement as well as<br />
skin and hair <strong>change</strong>s <strong>of</strong> kwashiorkor,<br />
dominated the clinical picture. 4<br />
Diagnostic criteria <strong>for</strong> fibro-calculuspancreatic<br />
diabetes (FCPD)<br />
1. Occurrence in a “tropical” country.<br />
2. Diabetes by WHO Study criteria.<br />
3. <strong>Evidence</strong> <strong>of</strong> chronic pancreatitis:<br />
pancreatic calculi on X-ray or at least three<br />
<strong>of</strong> the following:<br />
a) Abnormal pancreatic morphology by<br />
ultrasonography<br />
b) Chronic abdominal pain since<br />
childhood<br />
c) Steatorrhoea<br />
d) Abnormal pancreatic function test.<br />
86 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASE REPORT<br />
4. Absence <strong>of</strong> other causes <strong>of</strong> chronic<br />
pancreatitisi.e. alcoholism, hepatobiliarydisease<br />
or primary hyperparathyroidism<br />
etc. 5<br />
The etiopathogenetic mechanisms <strong>of</strong> FCPD<br />
still remain unclear. Thereis no satisfactory<br />
experimental model <strong>for</strong> FCPD. The following<br />
hypotheses have been proposed <strong>based</strong> on<br />
epidemiological data:<br />
1. Malnutrition theory<br />
2. The cassava hypothesis and other dietary<br />
toxins<br />
3. Oxidant stress hypothesis and trace<br />
element<br />
4. Familial and genetic factors 1<br />
One <strong>of</strong> the characteristicclinical features <strong>of</strong><br />
FCPD is that despite requiring insulin <strong>for</strong><br />
control,patients rarely becomeketotic on<br />
withdrawal <strong>of</strong> insulin. This is attributedto the<br />
following factors:<br />
1. Partial preservation <strong>of</strong> beta cell functions<br />
as shown by C-peptidestudies.<br />
2. Decreased glucagon reserve.<br />
3. Reduced supply <strong>of</strong> non-esterified fatty<br />
acid (NEFA), the fuelneeded <strong>for</strong><br />
ketogenesis, due to the loss <strong>of</strong><br />
subcutaneous tissue.<br />
4. Resistance <strong>of</strong> subcutaneous adipose<br />
tissue lipolysis to epinephrine.<br />
5. Carnitine deficiency, affecting transfer <strong>of</strong><br />
NEFA across mitochondrialmembrane. 2<br />
Complications due to chronic pancreatitis<br />
include pseudocysts, pancreaticabscesses,<br />
References<br />
1. Mohan V. Fibrocalculous pancreatic<br />
diabetes. In:Balakrishnan V, harishkumar,<br />
Sudhindran S, Unnikrishnan AG editors.<br />
Chronic Pancreatitis and Pancreatic<br />
Diabetes in India1 st ed. Bangalore: The<br />
Indian Pancreatitis Study Group;<br />
2006.p155-174<br />
2. Mohan V, Farooq S, Mohan D. Prevalence<br />
<strong>of</strong> Fibrocalculous Pancreatic Diabetes in<br />
Chennai in South India .J Pancreas 2008;<br />
9(4):489-92.<br />
3. Barman KK, Premalatha G, Mohan V.<br />
Tropical chronic pancreatitis. PostgradMed<br />
J 2003; 79: 606-15.<br />
4. Mahurkar S, Reddy DN, Rao GV, Chandak<br />
and ascites. Obstructive jaundice may also<br />
be occasionally seen, which can be due to<br />
common bile duct obstruction or associated<br />
carcinoma <strong>of</strong> the pancreas. 1 Microvascular<br />
complications like retinopathy and<br />
nephropathy was seen in FCPD patients.<br />
Renal failure due to diabetic nephropathy has<br />
also been reported in other <strong>for</strong>ms <strong>of</strong> pancreatic<br />
diabetes. Peripheral neuropathy and<br />
autonomic neuropathy have also been<br />
reported in those with FCPD. Macrovascular<br />
complications are however,rare in FCPD. This<br />
is believed to be due to three reasons: the<br />
patients are young, lean, and have low lipid<br />
levels. 2 It was previously believed that chronic<br />
complications do not occur in subjects with<br />
FCPD but both acute and chronic<br />
complications have been documented time<br />
and again 6 . Although the frequency is low,<br />
diagnosis <strong>of</strong> Fibrocalculus pancreatic<br />
diabetes must be kept in mind in treating<br />
diabetic subjects in developing countries as<br />
its management would include management<br />
<strong>of</strong> pain,pancreatic enzyme supplements and<br />
periodic surveillance <strong>for</strong> pancreatic<br />
malignancy. 3<br />
An overall association was observed between<br />
FCPD and HLA-DQB1 (P = 0.003), that was<br />
largely due to a positive association with HLA-<br />
DQB1*0302 and a negative association with<br />
HLA-DQB1*0202, a novel protective<br />
association was found with HLA-DQB1*0202<br />
in Bangladeshi FCPD subjects. The genetic<br />
susceptibility to FCPD has features both<br />
similar and dissimilar to T1DM. 7<br />
GR. Genetic mechanismsunderlying the<br />
pathogenesis <strong>of</strong> tropical calcific<br />
pancreatitis. World Gastroenterology J2009<br />
January 21; 15(3): 264-269.<br />
5. Mohan V. Fibrocalculous pancreatic<br />
diabetes in indiaInt J Diab Dev Countries<br />
1993; 13: 14-21.<br />
6. ZargarAH,Bhat MH,Laway BA,Masoodi SA.<br />
Clinical and aetiological pr<strong>of</strong>ile <strong>of</strong> early<br />
onset diabetes mellitus: data from a tertiary<br />
care centre in the Indian subcontinent.<br />
Postgrad Med J 2001; 47(1): 27-9.<br />
7. Chowdhury ZM, McDermott MF, Davey S,<br />
Hassan Z, Genetic susceptibility to<br />
fibrocalculous pancreaticdiabetes in<br />
Bangladeshi subjects: a family study.<br />
Genes and Immunity J (2002); 3:5-8.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
87
Colour Page<br />
CASE REPORT<br />
Jejunal GIST presenting as an exophytic mass with obscure lower gastrointestinal<br />
bleeding<br />
1<br />
D. Nilottpal, 2 Kh. Gojen Singh, 3 K. Lekhachandra Sharma, 2 L. Jaleshwar, 4 Th. Gojendra,<br />
Case report<br />
A 37 years old woman presented to us with<br />
complaints <strong>of</strong> a painless swelling in her left<br />
upper part <strong>of</strong> abdomen <strong>for</strong> the past three<br />
months followed by weight loss <strong>for</strong> the past<br />
one month (around 10kg). She also gave<br />
history <strong>of</strong> bleeding per rectum 6 years back<br />
<strong>for</strong> which she was hospitalised and two units<br />
<strong>of</strong> blood were transfused. There was no<br />
history <strong>of</strong> upper GI complaints like<br />
hematemesis,nausea,vomiting, alteration in<br />
bowel habits, or history <strong>of</strong> fever, upper<br />
abdominal discom<strong>for</strong>t or shortness <strong>of</strong> breath.<br />
Micturation habit was normal. On examination<br />
patient was pale but general examination<br />
including vital parameters were within normal<br />
limits. Systemic examination including<br />
abdominal examination, DRE and PV<br />
examinations were essentially normal. She<br />
had normocytic hypochromic anemia with Hb<br />
8.7mg%, TLC-6200/Cumm, SAKP-487U/L,<br />
S.bilirubin-1.2mg%, S. total protein - 6.4mg%,<br />
S. alb-3.1mg%, S.glb-3.3mg%, SGOT-134U/<br />
L,SGPT-92U/L, stool was positive <strong>for</strong> occult<br />
blood .In barium studies no lesion was<br />
found.CXR PAview was normal. USGabdomen<br />
suggested a colonic mass<br />
9.4cm×6.7 cm at around spleenic flexure with<br />
suspected target lesions at 7 th and 8 th hepatic<br />
segments with mild hepato spleenomegaly<br />
and right sided renal cortical cyst, but in Upper<br />
GI endoscopy it was reported as antral<br />
gastritis. After transfusing two units <strong>of</strong><br />
compatible blood ,she was subjected toFNAC<br />
which reported as Leiomyoma (benign<br />
spindle cells).In suspicion <strong>of</strong> Gastro intestinal<br />
stromal tumor, CECT abdomen was advised<br />
but the patient’s family could not af<strong>for</strong>t.Thus<br />
the patient was subjected to MRI where a<br />
large exophytic cavity <strong>of</strong> small bowel mass<br />
(9.85×8.29cm)with evidence <strong>of</strong> communication<br />
with jejunal loop and showing<br />
intermediate signal intensity <strong>change</strong>s in all the<br />
sequence and necrotic lesion at segment 7<br />
<strong>of</strong> liver with minimal pleural effusion (Fig. 1).<br />
Fig: 1 MRI showing<br />
exophytic mass.<br />
Fig: 2 Cut section<br />
showing hemorrhagic<br />
1 PGT. 2.Registrar. 3. Pr<strong>of</strong>essor. 4. Asst.<br />
Pr<strong>of</strong>essor. Department <strong>of</strong> Surgery, RIMS, Imphal<br />
Address <strong>for</strong> correspondence:<br />
Dr.Kh.Gojen Singh,<br />
Registrar, Department <strong>of</strong> Surgery,<br />
Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences,<br />
Imphal, Manipur -795004<br />
Fig: 3 Histopathology<br />
showing areas with<br />
cavitation spindle cells<br />
Fig : 4 Immuno<br />
histochemistry<br />
staining positive <strong>for</strong><br />
CD-117.<br />
88 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASE REPORT<br />
CECT-abdomen/ MRangiography were also<br />
suggested but due to the economic constrains<br />
all these investigations were abandoned and<br />
after explaining the nature <strong>of</strong> the disease ,likely<br />
course and outcome the patient was put up<br />
<strong>for</strong> exploratory laparotomy on the 4 th <strong>of</strong> Nov.<br />
2008.At operation, a hypervascular exophytic<br />
jejunal mass (15×10×6 cm) 5cm away from<br />
DJ junction was noted which was resected<br />
with grossly tumor free mergin followed by end<br />
to end jejuno-jejunal anastomosis. Liver was<br />
found to be normal in appearance , the<br />
peritoneum, mesentry and omentum were<br />
also normal with no suspicious lymph node<br />
enlargement. Cut section showed firm gray<br />
white with central area <strong>of</strong> cavitation and<br />
hemorrhage (Fig. 2). After histopathological<br />
and immunohistochemical analysis it was<br />
confirmed to be a jejunal GIST(borderline<br />
malignancy) with mitoic figure (‹5/50hpf),<br />
CD117 – positive (score 4+) (Fig. 3&4) .The<br />
patient had an uneventful recovery and is<br />
asymptomatic with no features suggestive <strong>of</strong><br />
recurrence in subsequent follow up clinically,<br />
till June 2011. Neither we could start imatinib<br />
mesylate therapy nor could investigate<br />
properly <strong>for</strong> recurrence as the cost <strong>of</strong> the<br />
investigation & therapy was beyond her<br />
af<strong>for</strong>dability.<br />
Discussion: GISTS are rare nonepithelial<br />
primitive digestive tract tumours, first identified<br />
by Mazur and Clark in 1983, arising from the<br />
connective tissue <strong>of</strong> the digestive tract with<br />
an incidence <strong>of</strong> 0.1–1%<strong>of</strong> gastrointestinal<br />
malignancies. 1 GIST and leiomyosarcomas<br />
(LMS) <strong>of</strong> the abdominal cavity and<br />
retroperitoneum are unusual malignancies<br />
that until recently were classified histologically<br />
together as leiomyosarcomas because <strong>of</strong> their<br />
similarities on light microscopy. 2<br />
Phenotypicaly mesenchymal tumors can be<br />
classified in three catagories (1) Tumours with<br />
differentiation towards smooth muscle cells<br />
[I.H.C. – (alpha) smooth muscle actin and<br />
desmin] (2) Tumours with neural<br />
differentiation (I.H.C. – S 100 protein) (3)<br />
Tumours with no differentiation – GIST [2].<br />
GISTS are believed to arise from the interstitial<br />
cells <strong>of</strong> Cajal (pacemaker cells <strong>of</strong> GIT) and<br />
hence were termed in the past as GANT<br />
(Gastrointestinal Autonomic Nerve Tumours). 3<br />
Age <strong>of</strong> onset is between 50–70 years without<br />
any sex predeliction, 25 % <strong>of</strong> GISTS are<br />
malignant. The clinical manifestations depend<br />
upon the site and size <strong>of</strong> the GIST. About 5 %<br />
are in oesophageal, 50–70 % are in the<br />
stomach, 25–40 % in the small intestine, 10–<br />
20 % in the duodenum, 27–37 % in jejunum,<br />
27–53 % in ileum and < 10 % are located at<br />
colorectal (50 % colonic 50 % rectal). 60 %<br />
are submucosal, 30 % are subserosal and<br />
some are intramural. 4 Small imtestinal GIST<br />
may remain silent till it become large enough<br />
to cause obstruction or causes GI bleeding<br />
due to ulceration <strong>of</strong> mucosa. Exophytic and<br />
extramural GISTS have been noted in 18–30<br />
% <strong>of</strong> cases. Small bowel GISTS have higher<br />
propensity to have malignant behaviour than<br />
gastric GIST. 5 It spreads mainly to adjacent<br />
organs, omentum, mesentery, retroperitoneum,<br />
liver, and to the lymph nodes, extra<br />
abdominally to lung and rarely to bone. 6 Upto<br />
30 % <strong>of</strong> GISTS are metastatic on presentation.<br />
Table 1<br />
Prognostic Criteria <strong>for</strong> GIST (Berman 2001;<br />
Fletcher et al 2002)<br />
Size in cm.<br />
Mitotic<br />
count/50 hpf<br />
Very low risk ‹2 ‹5<br />
Low risk 2-5 ‹5<br />
Intermediate risk ‹5 6-10<br />
High risk ›5 ›10<br />
Other proposed prognostic factors are<br />
mucosal and muscularis propria invasion,<br />
ploidy, proliferation markers (PCNA, Ki67),<br />
necrosis, hemorrhage, degeneration and<br />
calcification (which can be found in benign<br />
GISTS), cellularity, pleomorphism and<br />
immunophenotype. 7 No single factor is<br />
predictive enough to be used exclusively. CD<br />
117 positivity has become definitional in the<br />
diagnosis <strong>of</strong> GISTS. Metastasis may lose CD<br />
117 positivity. CD 34 positive GISTS have a<br />
more favourable prognosis. In 5% <strong>of</strong> the cases<br />
PDGFR-α may be positive with epitheloid<br />
histology picture. 8<br />
Preoperative diagnosis <strong>of</strong> GIST is difficult. CT<br />
and MR Angiography are helpful in clinching<br />
preoperative diagnosis. US endoscopy and<br />
FNA with subsequent immunohistochemical<br />
analysis along with c-kit gene mutation study<br />
<strong>of</strong>fers the best diagnostic accuracy .<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
89
CASE REPORT<br />
Resection <strong>of</strong>fers the best treatment option.<br />
Unresectable and/or metastatic GISTS (CD<br />
117 +ve) are treated with Imatinib mesylate<br />
(tyrosine kinase receptor inhibitor). 9 Our<br />
patient presented as an obscure lower GI<br />
bleed due to an exophytic jejunal GIST, CD<br />
117 positive score+4 , with mitotic figures <strong>of</strong><br />
‹5/50 hpfs, with suspected metastasis in the<br />
liver. In general gastric GISTS are spindle<br />
celled in 70 to 80 % <strong>of</strong> cases and epitheloid in<br />
20–30 %, while small intestinal GISTS are<br />
usually spindle celled, usually the benign ones.<br />
Esophageal and rectal GISTS are usually<br />
malignant and predominately spindle cells.<br />
Conclusion: GISTS are rare tumours <strong>of</strong> GIT,<br />
which are difficult to diagnose preoperatively.<br />
Surgery <strong>of</strong>fers definitive treatment and regular<br />
follow up is required lifelong post resection.<br />
Their unusual presentations must be borne<br />
in mind. An unusual exophytic jejunal<br />
malignant stromal tumor with obscure lower<br />
GI bleed is being presented.<br />
References<br />
1. Pappillon E, Rolachon A, Calender A, et al<br />
(2001) A malignant GIST in a patient with<br />
multiple endocrine neoplasia type I. Eur J<br />
Gastroenterol Hepatol 13(2):207–211.<br />
2. Miettinen M, Kopczynski J, Makhlouf HR,<br />
et al (2003) Gastrointestinal stromal<br />
tumours, Intramural leiomyomas, and<br />
leiomyosarcomas in the duodenum. Am<br />
J Surg Pathol 27(5): 625–641.<br />
3. Crowther KS, Wlyd L, Yamani Q, Jacob<br />
G (2002) Case report: gastroduodenal<br />
intussussception <strong>of</strong> a GIST. BJR<br />
75(900):987–988.<br />
4. Mukhopadyay S, Gupta SD (2002)<br />
Gastrointestinal Stromal Tumours: Benchto-bedside<br />
review. GI Surgery Annual 9:<br />
101–148.<br />
5. Dubenec SR, Dawes-Higgs RJ, Truskett<br />
PG (2001) Haemoperitoneum caused by<br />
spontaneous rupture <strong>of</strong> a GIST. ANZ J<br />
Surg 71(10):612–614.<br />
6. Rizzo S, Bonomo S, Moser A, et al (2001)<br />
Bilateral phaeochromocytoma associated<br />
with duodeno-jejunal GIST in patient with<br />
von Recklinghausen’s disease: report <strong>of</strong><br />
a clinical case. Chir Ital 53(2):243–46.<br />
7. Johnston AT, Khan AL, Beakney R, Keenan<br />
RA (2001) Stromal tumour within a<br />
Meckel’s Diverticulum: CT and ultrasound<br />
findings. BJR 74(888): 1142–1144.<br />
8. Miettinen M, Virolainen M, Sarlomo-Rikala<br />
M (1995) Gastrointestinal stromal tumours<br />
– Value <strong>of</strong> CD34 antigen in their identi.<br />
cation and separation from true<br />
leiomyomas and schwannomas. Am J<br />
Surg Pathol 19:207–16.<br />
9. Lattarulo S, Ugenti I, Ferrarese F, Fabiano<br />
G (2003) GIST : current issues. Chir Ital<br />
55(2):219–226.<br />
90 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011
CASE REPORT<br />
Hypokalemic periodic paralysis in Grave’s disease<br />
1 Arvind G, 2 Robinson Ningshen, 3 S. Bhagyabati Devi, 3 Th. Bhimo Singh, 4 Th. Shanti Devi,<br />
Case Report<br />
A 33 year old male presented to the<br />
Emergency Room with sudden onset<br />
paraparesis without any sensory, bladder or<br />
bowel symptoms. He denied having diarrhoea<br />
or vomiting, use <strong>of</strong> alcohol, diuretics, exertion,<br />
a high carbohydrate intake or fever preceding<br />
weakness. He had no past history <strong>of</strong> similar<br />
weakness and family history <strong>for</strong> periodic<br />
paralysis was negative. There was no history<br />
<strong>of</strong> diabetes or hypertension. However he gave<br />
history <strong>of</strong> palpitations, heat intolerance,<br />
increased bowel frequency, weight loss with<br />
increased appetite and increased sweating<br />
since 6 months. However he had no history<br />
<strong>of</strong> intake <strong>of</strong> antithyroid medication.<br />
His examination revealed a Pulse rate <strong>of</strong> 120/<br />
min, BP 130/80 and no dehydration. He was<br />
fully conscious with normal higher mental<br />
functions, no cranial nerve deficits, muscle<br />
power <strong>of</strong> 2/5 in both lower limbs with<br />
decreased reflexes, normal power and<br />
reflexes in both upper limbs, no sensory<br />
deficits. He had exophthalmos with lid lag, a<br />
firm enlarged thyroid gland with a bruit and<br />
his palms were moist and warm. His other<br />
system examination revealed nothing<br />
abnormal.<br />
1. PGT, 2. Associate Pr<strong>of</strong>essor, 3. Pr<strong>of</strong>essor,<br />
4. Registrar, Department <strong>of</strong> <strong>Medicine</strong>, Regional<br />
Institute <strong>of</strong> <strong>Medical</strong> Sciences, Imphal, Manipur.<br />
Corresponding Author:<br />
Dr.Robinson Ningshen, MBBS., MD (General<br />
<strong>Medicine</strong>), Associate Pr<strong>of</strong>essor, Department <strong>of</strong><br />
<strong>Medicine</strong>, Regional Institute <strong>of</strong> <strong>Medical</strong> Sciences,<br />
Imphal, Manipur. Phone No: 9612159017.<br />
E-Mail: dr.ningshen@yahoo.co.in<br />
On investigation serum electrolytes revealed<br />
K+ level <strong>of</strong> 1.9 mEq/l and normal serum<br />
sodium, chloride and bicarbonate. Serum<br />
calcium, magnesium, phosphate were within<br />
normal limits. Random blood sugar was<br />
148mg/dl.ECG revealed Sinus tachycardia<br />
with heart rate <strong>of</strong> 112/min and PR interval 0.20<br />
sec, presence <strong>of</strong> ST-T flattening with U wave.<br />
Urinary electrolyes were normal.<br />
Free T4 levels-270 nmol/L (66-181 nmol/L)<br />
Free T3 levels-3.0 (1.3-3.1 nmol/L)<br />
TSH level- 0-05 (0.3-6.0 microIU/ml)<br />
Patient was treated with intravenous<br />
potassium chloride at the rate <strong>of</strong> 10 mEq/hr<br />
in normal saline infusion with cardiac<br />
monitoring and was also given propranolol 40<br />
mg 8hrly orally. At the 8 th hour <strong>of</strong> KCl infusion<br />
patient’s paraparesis resolved completely and<br />
neurological examination was normal except<br />
<strong>for</strong> increased ankle jerks bilaterally. Repeat<br />
serum K+ was 5.3 mEq/L. KCl infusion was<br />
discontinued and K+ supplementation was<br />
given orally and propranolol continued.<br />
In view <strong>of</strong> the TPO antibody positivity patient<br />
was labelled to be suffering from Grave’s<br />
Disease and was treated with Carbimazole<br />
15mg 8 hourly with propranolol continued at<br />
40mg 8hrly.<br />
Patient had no recurrent episodes <strong>of</strong><br />
paraparesis on follow up and serum T4<br />
normalised at 6 weeks and was put on<br />
maintenance Carbimazole at 10mg daily.<br />
Patient continues do well after 6 months<br />
follow up.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
91
CASE REPORT<br />
Discussion: Diagnosis <strong>of</strong> Thyrotoxic periodic<br />
paralysis (TPP) is a challenge to clinicians,<br />
the reason being in most cases it can present<br />
with only mild elevations <strong>of</strong> thyroid hormone.<br />
Thorough history with emphasis on age,<br />
previous similar weakness, family history <strong>of</strong><br />
weakness, high carbohydrate intake,or acute<br />
gastroenteritis, drug and history <strong>of</strong> alcoholism<br />
needs to be elucidated.<br />
Hypokalemia in TPP results from an<br />
intracellular shift <strong>of</strong> potassium and not total<br />
body K+ depletion. It has been shown that the<br />
Na+/K+–ATPase activity in platelets and<br />
muscles is significantly higher in patients with<br />
TPP 1 . Hyperthyroidism may result in a<br />
hyperadrenergic state, which may lead to the<br />
activation <strong>of</strong> the Na+/K+–ATPase pump and<br />
result in cellular uptake <strong>of</strong> potassium.<br />
Thyroid hormones may also directly stimulate<br />
Na+/K+– ATPase activity and increase the<br />
number and sensitivity <strong>of</strong> beta receptors 2 .<br />
Patients with TPP have been found to have<br />
hyperinsulinemia during episodes <strong>of</strong> paralysis.<br />
This may explain the attacks after highcarbohydrate<br />
meals.<br />
The typical presentation <strong>of</strong> the disease is in<br />
Asian males 3 , generally in 2 nd -4 th decades<br />
occurring as sudden onset symmetrical lower<br />
limb weakness, affecting the proximal<br />
muscles more than the distal muscles.The<br />
weakness occurs at rest after exertion and a<br />
high carbohydrate meal. It may last <strong>for</strong> 3-96<br />
hours with resolution <strong>of</strong> weakness in an<br />
opposite direction to that <strong>of</strong> appearance. On<br />
rare occasions there may be respiratory<br />
muscle weakness needing ventilatory<br />
support 3 .<br />
Since TPP can be life threatening, prompt<br />
treatment with intravenous potassium should<br />
be initiated. Ahmed I et al recommend K+<br />
doses <strong>of</strong> < 10 mEq/hr with close monitoring 4 .<br />
Prompt treatment results in prompt resolution<br />
<strong>of</strong> weakness. Propranolol, a nonselective<br />
beta-blocker, prevents the intracellular shift <strong>of</strong><br />
potassium and phosphate by blunting the<br />
hyperadrenergic stimulation <strong>of</strong> Na+/ K+–<br />
ATPase 5 . Combination <strong>of</strong> low IV potassium<br />
and non selective B blockade appears to be<br />
the treatment <strong>of</strong> choice <strong>for</strong> recovery and<br />
reducing rebound hyperkalemia.<br />
Acetazolamide used in the the treatment <strong>of</strong><br />
HPP is contraindicated in TPP 6 .<br />
However definitive treatment lies in treating<br />
Hyperthyroidism per se.TPP is curable once<br />
a euthyroid state is achieved.<br />
Conclusion: In the setting <strong>of</strong> hypokalemic<br />
periodic paralysis one should look out <strong>for</strong><br />
secondary causes, particularly <strong>for</strong> a thyrotoxic<br />
cause in males <strong>of</strong> Asian origin 3 in 2-4 decades<br />
<strong>of</strong> life.TPP is a potentially treatable cause and<br />
further episodes can be prevented on<br />
achieving euthyroid status.<br />
Furthermore, low dose <strong>of</strong> IV potassium
CASE REPORT<br />
Giant condyloma acuminata: a case report<br />
1<br />
T.Y Babu Singh, 2 Ksh. Raju, 3 Manju Darang<br />
Case report<br />
A 40 years Hindu male from Lilong Chajing,<br />
mansion by occupation was admitted on 18-<br />
10-10 with chief complaint <strong>of</strong> swelling in the<br />
right scrotum <strong>for</strong> eight years. The swelling<br />
was gradual in onset and progressive in<br />
nature. It increased in size at a faster rate in<br />
the last 2 years. It was not associated with<br />
pain except some heavy/dragging sensation<br />
when not wearing undergarments. There were<br />
occasional oozing <strong>of</strong> blood when traumatized<br />
but there was no discharge as such.<br />
There was no discom<strong>for</strong>t during passing stool/<br />
urine or sexual relationship. He was an<br />
occasional smoker and drank alcohol<br />
occasionally. There was no other significant<br />
history like<br />
STD in both the<br />
partners but<br />
his wife was<br />
m a r r i e d<br />
previously to<br />
another man<br />
who expired,<br />
and history<br />
couldn’t be Fig. 1 Giant condyloma acuminata<br />
traced regarding any STD. The patient also<br />
denies any history <strong>of</strong> extra marital contact<br />
be<strong>for</strong>e or after marriage.<br />
1. Pr<strong>of</strong>. and Head <strong>of</strong> Department, Surgery,<br />
2. Asst. Pr<strong>of</strong>. 3. Jr. Resident, Department Of<br />
Surgery, RIMS, Imphal.<br />
Corresponding Author:<br />
Dr. Ksh. Raju Singh, Assistant Pr<strong>of</strong>essor,<br />
Department <strong>of</strong> Surgery, RIMS, Imphal.<br />
Local examination showed a pinkish grey<br />
white cauliflower like non pedunculated<br />
growth over the right scrotum, the surface<br />
was rough and showed papillations. Adjacent<br />
skin showed tortuous dilated veins radiating<br />
from the growth. The growth measured about<br />
14x7cm with no local rise in temperature and<br />
non tender. It was firm in consistency with well<br />
defined margin. The growth was fixed to the<br />
scrotal skin but free from the testes. There<br />
were bilateral inguinal lymphadenopathy which<br />
was slightly tender, firm, non matted and<br />
mobile .The left scrotum showed no <strong>change</strong><br />
and the penis was normal though it was<br />
slightly pushed to the left by the scrotal growth<br />
(fig.1). Routine investigations <strong>for</strong> blood were<br />
normal. Incisional biopsy was done and<br />
showed hyperplastic verrucous epithelial<br />
lesion. FNAC <strong>of</strong> inguinal lymph nodes showed<br />
non specific reactive lymphadenitis. Growth<br />
was excised with free margin <strong>of</strong> 1cm under<br />
spinal anesthesia, haemostasis secured and<br />
wound was closed primarily after putting a<br />
corrugated drain. Histopathological<br />
examination <strong>of</strong> excised tissue showed skin<br />
with epidermis displaying broad irregular<br />
acanthosis, papillomatosis and<br />
hyperkeratosis. The underlying dermis<br />
showed proliferating capillaries with moderate<br />
pericapillary lymphocytic infiltration. No<br />
evidence <strong>of</strong> malignancy was seen. Features<br />
were <strong>of</strong> Giant Condyloma Acuminata.<br />
Postoperative period was uneventful except<br />
<strong>for</strong> some wound gapping <strong>for</strong> which secondary<br />
stitching were done and patient was put on<br />
oral antibiotic, analgesic and multivitamins.<br />
JMS * Vol 25 * No. 13 * June, September, 2010 2011<br />
93
CASE REPORT<br />
Patient was discharged and advised to attend<br />
STD clinic with his wife after one week.<br />
Patient reported after one week and wound<br />
was found healthy and healing was<br />
satisfactory.<br />
Discussion: Giant condyloma acuminata also<br />
known as Buschke–Lowenstein Tumor or<br />
Verrucous lesion is a locally aggressive <strong>for</strong>m<br />
<strong>of</strong> Condyloma Acuminata. Although these<br />
lesions do not metastasize, they can cause<br />
an extensive local tissue destruction and may<br />
be grossly indistinguishable from epidermoid<br />
carcinoma. Giant Condyloma Buschke<br />
Lowenstein is mostly located in glans penis<br />
however it can be found on any anogenital<br />
mucosal surface, including the vulva, vagina,<br />
rectum, scrotum, and bladder. 1 Co-localization<br />
with human papillomavirus (HPV) types 6 and<br />
11 2 , occasionally HPV types 16 and 18, and,<br />
on one occasion, HPV 54 has been shown.<br />
Giant Condyloma Buschke-Lowenstein<br />
(GCBL) is rare type <strong>of</strong> Condyloma Acuminata.<br />
Estimates <strong>of</strong> incidence shows that GCBL<br />
accounts <strong>for</strong> 5-24% <strong>of</strong> penile cancers, which,<br />
in turn, are 0.3-0.5%<strong>of</strong> male malignancies.<br />
Another review assessed that Verrucous<br />
carcinoma accounted <strong>for</strong> approximately 50%<br />
<strong>of</strong> all low grades squamous cell carcinoma<br />
(SCC) <strong>of</strong> the penis. GCBL located outside the<br />
penis is more frequent. GCBL typically starts<br />
on the prepuce as a keratotic plaque and<br />
slowly expands into a cauliflowerlike mass,<br />
as large as 15 cm. The lesion may ulcerate<br />
or <strong>for</strong>m a penile horn and typically is<br />
associated with a foul odour. Expansion to the<br />
corpus cavernosum and urethra may occur,<br />
with subsequent fistulation. Regional<br />
lymphadenopathy is common, primarily due<br />
to secondary infection, not metastases.<br />
Biopsy is the diagnostic procedure necessary<br />
<strong>for</strong> evaluation. It must be sufficiently deep and<br />
generous to evaluate <strong>for</strong> possible foci <strong>of</strong><br />
squamous cell carcinoma (SCC). Although the<br />
rate <strong>of</strong> regional lymph node involvement is<br />
low, sentinel lymph node biopsy should be<br />
considered if clinical findings suggest the need<br />
<strong>for</strong> it. The treatment <strong>of</strong> choice <strong>for</strong> GCBL is wide<br />
surgical excision. Surgery alone has resulted<br />
in a disease-free status in 45.5% <strong>of</strong> patients. 5<br />
In addition, oral and topical chemotherapeutic<br />
modalities have been used with mixed<br />
success as adjuvant to surgery or as<br />
treatment <strong>for</strong> recurrences. Inadequately<br />
treated GCBL has a relentless progression<br />
and is fatal by direct spread to pelvic organs.<br />
By definition, adequately treated GCBL has a<br />
low recurrence rate and, there<strong>for</strong>e, an<br />
excellent prognosis.<br />
Conclusion: Giant Condyloma Acuminata is<br />
a rare type <strong>of</strong> condyloma acuminata. In our<br />
case there was no history <strong>of</strong> STD exposure<br />
and there was no evidence <strong>of</strong> malignancy.<br />
Surgical excision is the treatment <strong>of</strong> choice.<br />
References:<br />
1 Wiedemann A, Diekmann WP, Holtmann<br />
G, Kracht H. Report <strong>of</strong> a case with<br />
giant condyloma (Buschke-Lowenstein<br />
tumor) localized in the bladder. J<br />
Urol. Apr 1995;153(4):12224.<br />
2 Dianzani C, Bucci M, Pierangeli A,<br />
Calvieri S, Degener AM. Association <strong>of</strong><br />
human papillomavirus type 11 with<br />
carcinoma <strong>of</strong> the<br />
penis. Urology. Jun 1998;51(6):10468.<br />
3 Castren K, Vahakangas K, Heikkinen E,<br />
Ranki A. Absence <strong>of</strong> p53 mutations in<br />
benign and pre-malignant male genital<br />
lesions with over-expressed p53<br />
protein. Int J Cancer. Aug<br />
31 1998;77(5):6748.<br />
4 Crespo R, Puig F, Lanzon A, Borell<br />
A. Buschke Lowenstein tumor and<br />
pregnancy: a case report. Eur J<br />
Gynaecol Oncol. 2007;28(4):3289.<br />
5 Renzi A, Giordano P, Renzi G, Landolfi V,<br />
Del Genio A, Weiss EG. Buschke-<br />
Lowenstein tumor successful treatment<br />
by surgical excision alone: a case<br />
report. Surg Innov. Mar 2006;13(1):<br />
69-72.<br />
94 JMS * JMS Vol 25 * Vol * No. 25 3 * No. * September, 1 * June, 2010 2011