CHURCHWIDE HEALTHCARE - Pension Fund
CHURCHWIDE HEALTHCARE - Pension Fund
CHURCHWIDE HEALTHCARE - Pension Fund
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
HURCHWIDE<strong>HEALTHCARE</strong><br />
Freedom<br />
to choose<br />
your<br />
provider<br />
Self -<br />
insured<br />
savings<br />
Prompt<br />
answers to<br />
questions<br />
HEALTH AND WELL-BEING<br />
MADE SIMPLE<br />
Coverage<br />
wherever<br />
you travel<br />
Over<br />
720,000<br />
providers<br />
Chat with<br />
a nurse<br />
24/7
CONTENT<br />
P.02<br />
P.03<br />
P.04<br />
P.05<br />
P.06<br />
P.07<br />
P.08<br />
P.10<br />
P.12<br />
P.14<br />
P.15<br />
P.17<br />
Welcome/Our Partners<br />
Membership Guidelines<br />
Highmark BCBS Program<br />
Summary of Medical Benefits<br />
Prescription Drug Overview<br />
Prescription Drug Details<br />
Flexible Spending Accounts (FSA) Overview<br />
Voluntary Dental Program<br />
Employer Paid Dental Program<br />
Vision Benefits<br />
Legal Updates<br />
Medicare Part D Notice<br />
The benefit information included in this guide is summary information. It is not intended<br />
to be a complete description of the benefit plans. That description, which contains coverage<br />
and exclusion information, is contained in the Summary Plan Descriptions (SPD). If a<br />
discrepancy exists, the SPD will prevail.<br />
PAGE 1
Benefits Guide 2011<br />
Thank you for your interest in the Churchwide Healthcare.<br />
The Christian Church Health Care Benefit Trust (CCHCBT) and the <strong>Pension</strong> <strong>Fund</strong> have been offering health<br />
coverage (Churchwide Healthcare) since 1972 to clergy and employees of the ministries of the Stone-Campbell<br />
Tradition, including the Christian Church (Disciples of Christ), Church of Christ, and North American Christian<br />
Convention. We offer three medical plan options (covering prescription drugs and vision); two fully – insured<br />
dental plans, and flexible spending account administration.<br />
The Christian Church Health Care Benefit Trust, with the <strong>Pension</strong> <strong>Fund</strong> of the Christian Church as Trustee,<br />
manages these programs on behalf of the General Assembly of the Christian Church (Disciples of Christ).<br />
Together with our partner vendors, the Christian Church Health Care Benefit Trust strives to offer<br />
comprehensive, affordable, and portable coverage to clergy and employees of the Stone-Campbell Tradition.<br />
Our partner vendors are:<br />
Medical & Flexible Spending<br />
Accounts Benefit Plans<br />
Highmark Blue Cross Blue Shield<br />
1.800.648.4078<br />
www.highmarkbcbs.com<br />
Preferred Provider Network<br />
Blue Card PPO Network<br />
1.800.648.4078<br />
www.highmarkbcbs.com<br />
Pharmacy Benefit Manager<br />
Medco Health Solutions<br />
1.800.818.0093<br />
www.medcohealth.com<br />
Vision Benefits<br />
VSP<br />
1.800.877.7195<br />
www.vsp.com<br />
Dental Benefit<br />
Delta Dental of Indiana, Inc.<br />
1.800.524.0149<br />
www.deltadentalin.com<br />
PAGE 2
Membership Guidelines<br />
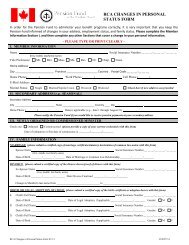
Who is eligible for coverage?<br />
In order to particpate in the Churchwide Healthcare program, you must be a compensated staff member of an eligible<br />
organization. Eligible organizations include Christian Church (Disciples of Christ), affiliated non-profit organizations<br />
and other churches that share a heritage from the Stone-Campbell movement. Eligible staff includes: ministers, church<br />
support staff, missionaries, K-12 Christian school personnel, and non-profit Christian college and university employees.<br />
Specific eligibility rules are determined by each individual entity/organization.<br />
If you qualify as an eligible staff member, you can also cover your eligible dependents. Eligible dependents include:<br />
Spouse/Domestic Partner<br />
Children under 26 years of age, including:<br />
Newborn Children<br />
Stepchildren<br />
Children legally placed for adoption<br />
Legally adopted children or children for whom the employee’s spouse is the child’s<br />
legal guardian<br />
Children awarded coverage pursuant to an order of court<br />
Children over age 26 who are not able to support themselves due to mental retardation, physical<br />
disability, mental illness or developmental disability.<br />
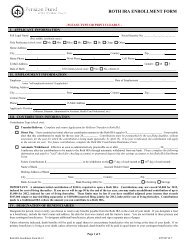
Making enrollment changes during the year<br />
In most cases, your benefit elections remain in effect for the entire plan year. During each annual enrollment period, you<br />
will have the opportunity to review your benefit elections and make changes for the coming year.<br />
Certain coverages allow limited changes to elections during the year. These benefits include the medical, dental and<br />
vision plans. Under these benefits, you may only make changes to your elections during the year if you have a change in<br />
family status. Family status changes include:<br />
Marriage, divorce or legal seperation<br />
Gain or loss of an eligible dependent for reasons such as birth, adoption, court order, disability,<br />
death, marriage, or reaching the dependent child age limit<br />
Changes in your spouse’s employment affecting benefit eligibility<br />
Changes in your spouse’s benefit coverage with another employer that affects benefit eligibility<br />
The change to your benefit elections must be consistent with the change in family status. For example, if you gain a new<br />
dependent due to birth, you may only change your benefit elections to add that dependent. In this case, coverage for<br />
other dependents cannot be changed.<br />
You have 30 days from the date of a change in family status to complete an enrollment change form and return it to<br />
Michael Porter, Director of Health Services. Otherwise, you must wait until the next annual enrollment period to make a<br />
change to your elections. Your elections will become effective the first of the following month, with the exception of a<br />
change due to birth or adoption.<br />
PAGE 3
Highmark BCBS Medical Program<br />
About your Churchwide Healthcare<br />
coverage<br />
Welcome to Churchwide Healthcare (CWHC) coverage<br />
through Christian Church Healthcare Benefit Trust<br />
(CCHCBT). CCHCBT has contracted with Highmark BCBS<br />
to act as Third-Party Administrator of the benefits program,<br />
which gives you access to the BCBS system, one<br />
of the most widely recognized and accepted throughout<br />
the United States. For decades, the nationwide<br />
BCBS family of independent plan providers has offered<br />
members innovative health coverage designed to meet<br />
their needs. You will be covered through the CWHC PPO<br />
plan administered by Highmark BCBS. No matter where<br />
you live in the United States, you may take advantage<br />
of the expansive provider networks and discounts<br />
arranged by the PPO plans around the country. In most<br />
cases, you should not have to file claim forms or pay<br />
anything except your co-payments, deductibles, etc.,<br />
in advance. This guide explains your coverage through<br />
CWHC and the PPO program. For more information,<br />
such as details about how we cover a particular service<br />
or prescription drug, please read your contract or use<br />
one of the sources located in the front of this guide.<br />
How does my medical plan work?<br />
You pay less out-of-pocket if you use the physicians,<br />
hospitals, and other health care providers that participate<br />
in the BCBS PPO network. While you don’t need<br />
referrals to visit specialists, you receive the highest<br />
level of benefits when you use Preferred Providers. In<br />
some instances, such as hospital admissions and home<br />
healthcare services, Highmark BCBS can require prior<br />
approval. In other words, Highmark BCBS must approve<br />
the need for the care before you seek it, or they may<br />
choose not to pay for such care.<br />
To find preferred providers<br />
(in-network):<br />
Visit the www.highmarkbcbs.com web site<br />
and click on “Find a Physician or Facility.”<br />
Call 1-800-648-4078 to find out if the<br />
provider you select is Preferred.<br />
(Remember, you will reach your out-of-pocket maximum<br />
quicker when you use Out-of-Network Providers.<br />
Further, there are separate deductibles and out of pocket<br />
limits for Out-of-Network medical services.) The medical<br />
summary of benefits in the booklet shows a comparison<br />
between benefits when you use In-Network<br />
Providers and benefits when you use Out-of-Network<br />
Providers. Also, keep in mind that your health plan pays<br />
the Allowed Price for services and supplies. In-Network<br />
Providers agree to accept the Allowed Price as payment<br />
in full. When you use Out-of-Network Providers, you<br />
must pay the difference between the Allowed Price and<br />
the provider’s charge. Benefits for most services require<br />
that you pay a deductible each year for In-Network<br />
Providers’ services and Out-of-Network Providers’ services.<br />
Once you have met your deductible, you share<br />
the cost of your care through coinsurance. Deductible<br />
and out-of-pocket amounts do not cross apply. Once<br />
again, your coinsurance percentage amount for Out-of-<br />
Network Providers is higher than the one for In-Network<br />
Providers. You need only pay the deductible and coinsurance<br />
until you meet your out-of-pocket maximum<br />
for the year.<br />
PAGE 4
Summary of Medical Benefits<br />
Benefit Category<br />
PPO Medical Plan Benefit Summaries<br />
In-Network<br />
PPO1 PPO2 PPO HDHP<br />
Benefit Period Calendar Year Calendar Year Calendar Year<br />
Deductible: Individual $500 $1,000 $2,500<br />
Deductible: Family $1,500 $3,000 $5,000<br />
Payment Level/Coinsurance 80% after deductible until out-of-pocket is met, then 100%<br />
Out-of-Pocket (OOP) Maximums: Individual $3,000 $4,500 $6,050<br />
Out-of-Pocket (OOP) Maximums: Family $6,000 $9,000 $12,100<br />
Deductible included in OOP Maximum No No No<br />
Lifetime Maximum<br />
Unlimited<br />
Physician & Specialist Office Visits<br />
80% after deductible<br />
Adult Preventive Care - Routine physical exams<br />
100%; deductible does not apply<br />
Adult Preventive Care - Routine gynecological exams including<br />
a Pap Test<br />
Adult Preventive Care - Mammograms, as required<br />
Pediatric Preventive Care - Routine physical exams<br />
Pediatric Preventive Care - Immunizations<br />
Emergency Room Services<br />
Ambulance<br />
Hospital Expenses - Inpatient<br />
Hospital Expenses - Outpatient<br />
Hospital Expenses - Maternity<br />
Infertility Counseling, Testing & Treatment<br />
Medical/Surgical Expenses (Except Office Visits)<br />
Spinal Manipulations<br />
Diagnostic Services (Lab, X-Ray & other tests)<br />
Physical Medicine (Acupuncture included)<br />
Occupational/Speech Therapy<br />
Durable Medical Equipment, Orthotics and Prosthetics<br />
Skilled Nursing Facility Care<br />
Home Healthcare<br />
Private Duty Nursing<br />
Hospice<br />
Mental Health/Substance Abuse - Impatient<br />
Mental Health/Substance Abuse - Outpatient<br />
Precertification Requirements<br />
100%; deductible does not apply<br />
100%; deductible does not apply<br />
100%; deductible does not apply<br />
100%; deductible does not apply<br />
80% after $100 copayment & deductible; 80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
80% after deductible<br />
Combined Limit: 20 visits per calendar year<br />
80% after deductible<br />
80% after deductible<br />
Combined Limit: 20 visits per calendar year<br />
80% after deductible<br />
Combined Limit: 20 visits per calendar year<br />
80% after deductible<br />
80% after deductible<br />
Combined Limit: 120 visits per calendar year<br />
80% after deductible<br />
Combined Limit: 40 visits per calendar year<br />
80% after deductible<br />
80% after deductible<br />
Combined Limit: 180 days per lifetime<br />
80% after deductible<br />
Combined Limit: 30 days/calendar year<br />
80% after deductible<br />
Combined Limit: 30 visits/calendar year<br />
Performed by member*<br />
PAGE 5
Prescription Drug Program Overview<br />
Prescription Drug Program<br />
The CCHCBT, through its partnership with Medco, a<br />
Pharmaceutical Benefit Manager, has a tiered prescription<br />
drug program. That means that you pay the lowest<br />
co-payments when you use tier 1 (generic) drugs.<br />
Below is the co-payment structure at retail pharmacies<br />
for a 30-day supply:<br />
Annual Deductible: $50 Individual; $100 Family<br />
Tier 1 (Generic): $10<br />
Tier 2 (Brand Formulary): 20%<br />
(min. $25-max. $75)<br />
Tier 3 (Brand Non-Formulary): 50%<br />
(min. $4O-max. $120)<br />
When you go to in-network pharmacies, you will be<br />
responsible for paying the copay or coinsurance - nothing<br />
more. The pharmacy will bill Medco for the left-over<br />
amount. As you can see, you will pay the lowest copay<br />
if you use a generic drug. Make sure to ask your pharmacist<br />
if a generic alternative is available for the brandname<br />
drug you are prescribed.<br />
You must use pharmacies that are in Medco’s network<br />
to receive the benefit levels above. Over 90% of pharmacies<br />
nationwide currently belong to this network.<br />
Should you use an out-of-network pharmacy, you will<br />
be responsible for the co-pay listed above plus 20% of<br />
the remaining cost of the drug.<br />
The plan provides for 3 refills of medication at a retail<br />
pharmacy. After this, the plan will require you to pay an<br />
additional cost, unless you have this medication filled<br />
using Medco Mail Pharmacy.<br />
Wouldn’t you rather pay $4 for<br />
your prescription?<br />
Did you know that Wal-Mart offers over 300 different<br />
drugs at only $4 per prescription fill or refill (up to a<br />
30-day supply or 60 pill maximum). The program is<br />
available at all Wal-Mart, Sam’s Club and Neighborhood<br />
Market pharmacies. A similar program is also offered<br />
through Target stores.<br />
Brand Formulary-Name Drugs<br />
What is a brand-name drug?<br />
A brand-name druge is a prescription drug that is marketed<br />
under a proprietary, trademark-protected name.<br />
What is a Tier 2 Drug?<br />
A Tier 2 Drug is a “preferred” brand-name drug. The<br />
list of these preferred drugs is created by Medco, your<br />
pharmacy vendor. Many factors are taken into account<br />
when deriving the list, such as the utilization of the<br />
drugs, the cost, and the therapeutic class to name a few.<br />
What is important to know is that Tier 2 Prescription<br />
Drugs are less expensive than Tier 3 Prescription Drugs.<br />
Tier 3 are non-preferred and have the highest coinsurance<br />
level attached to them.<br />
Where can I find the Formulary Drug List?<br />
The Formulary Drug list is updated quarterly to ensure<br />
that newer, more effective drugs are on it. Drugs automatically<br />
come off the list when generic alternatives<br />
become available. To get the most updated formulary<br />
list, register at www.medco.com. Once there, you can<br />
download the formulary listing or search for a medication<br />
by name.<br />
You may want to print off the formulary list and take<br />
it with you to your next doctor’s appointment. If your<br />
doctor has the list, he or she can be sure to prescribe<br />
you a preferred drug. Make sure you take the most<br />
updated list as it is updated quarterly.<br />
PAGE 6
Prescription Drug Program Details<br />
Mandated Generics<br />
For Non-Preferred drugs, including non-sedating antihistamines<br />
(Allegra®, Clarinex®, Zyrtec®, etc.) or if you<br />
purchase a brand medication when a generic is available,<br />
you will pay your copay plus the difference in cost<br />
between the brand and the generic.<br />
Medco By Mail Pharmacies<br />
Over 6 million members enjoy the convenience and<br />
savings of having their long-term medications (maintenance<br />
medications, those taken for three months or<br />
more) delivered to their home or office. Medco by Mail<br />
advantages include:<br />
Get up to a 90 day supply (compared with a typical<br />
30 day supply at retail) of each covered medication<br />
for just one mail order payment.<br />
Tier 1 (Generic): $20<br />
Tier 2 (Brand Formulary): 20%<br />
(min. $60-max. $180)<br />
Tier 3 (Brand Non-Formulary): 50%<br />
(min. $100-max. $300)<br />
Specialty Medications<br />
Specialty medications are drugs that are used to treat<br />
complex conditions, such as cancer, growth hormone<br />
deficiency, hemophilia, hepatitis C, immune deficiency,<br />
multiple sclerosis and rheumatoid arthritis. Medco’s<br />
specialty pharmacy, Accredo Health Group, Inc. is<br />
composed of therapy-specific teams that provide an<br />
enhanced level of personalized service to patients with<br />
special therapy needs. By ordering your specialty medications<br />
through Accredo, you can receive:<br />
Personalized counseling from our dedicated team<br />
of registered nurses and pharmacists.<br />
Expedited, scheduled delivery of your medications<br />
at no extra charge.<br />
Complimentary supplies, such as needles and<br />
syringes.<br />
Refill reminder calls.<br />
Safety checks to help prevent potential drug interactions.<br />
Order refills online, by mail or by phone-anytime<br />
day or night. To order online, register at www.<br />
medco.com. Refills are usually delivered within three<br />
to five days after Medco receives your order. You can<br />
also have your doctor fax your prescriptions. Ask<br />
your doctor to call 1-888-327-9791.<br />
Choose a convenient payment option-Medco<br />
offers two safe, automatic options for prescription<br />
orders. You can use e-check to have payments automatically<br />
deducted from your checking account, or<br />
you can use AutoCharge to have payments automatically<br />
charged to the credit card of your choice.<br />
For more information, visit www.medco.com or call<br />
member services at 1-800-418-9925.<br />
PAGE 7
Flexible Spending Accounts Overview<br />
What is a healthcare Flexibile<br />
Spending Account (FSA)?<br />
A healthcare flexible spending account provides you<br />
the opportunity to benefit from the tax savings available<br />
by setting aside money to pay for future health<br />
care expenses on a pre-tax basis. Healthcare flexible<br />
spending account contributions are not subject to federal<br />
income tax, Social Security taxes, and most state<br />
and local income taxes. Check with your local tax advisor<br />
regarding your state and local income tax laws.<br />
How does the FSA work?<br />
The Christian Church (Disciples of Christ) Flexible<br />
Spending Accounts for Healthcare (“Healthcare FSA”)<br />
allows you to prefund out-of-pocket medical and dental<br />
costs and other qualified medical costs not otherwise<br />
covered through the Churchwide Healthcare.<br />
Qualified expenses may include:<br />
Deductibles<br />
Well Baby Care<br />
Co-payments<br />
Organized Weight Loss Programs<br />
Vision Care (including RK and LASIK)<br />
Dental Care<br />
Hearing Aids and other related expenses<br />
Prescription Drugs<br />
Transportation to receive care<br />
Certain non-covered procedures such<br />
as experimental surgeries<br />
Annual Physicals<br />
Body scanning and Heart scoring<br />
How do I get reimbursed?<br />
You do not need to submit a copy of a cancelled check<br />
or a receipt for a bill that is already paid as proof of<br />
expense. An invoice or copy of an unpaid bill is acceptable<br />
since the program operates on an incurred date.<br />
We will look at the date the service was received to<br />
determine if it is eligible for the program year.<br />
Dependent Care Spending<br />
Account<br />
Day care expenses are covered for the following dependents<br />
while you work (and if married, while your spouse<br />
is at work, is a full-time student or is disabled):<br />
Your children under 13;<br />
Your dependent who is physically or mentally disabled<br />
and incapable of self-care, including your<br />
spouse or child of any age;<br />
Claimed as dependents for income tax purposes, and;<br />
Your dependent parent or other dependent who<br />
spends at least eight hours a day in your home.<br />
Eligible dependent care expenses include those for care<br />
in your home, in a babysitter’s home, or at a licensed<br />
day care<br />
Minimum: $520.00<br />
Maximum: $ 5,000.00 (or $2,500.00 if you are married<br />
and file separate income tax returns)<br />
PAGE 8
Flexible Spending Account Overview<br />
Use it or lose it<br />
It is important to accurately estimate your expenses<br />
and only elect an annual contribution to cover expected<br />
claims, because IRS rules require that any money left<br />
in your Health Care FSA account be forfeited. However,<br />
as long you are a participant you do have until March<br />
31 to submit any eligible expenses you incur between<br />
January 1 and March 15 of the next year.<br />
How do I submit a claim?<br />
When you have an eligible expense to be reimbursed<br />
from your Health Care FSA, you can file a claim by completing<br />
a Flexible Spending Account Claim Form and<br />
submitting it, and proof of expense, to Highmark BCBS:<br />
Account Service Center<br />
P.O. Box 22130<br />
Pittsburgh, PA 15222-0130<br />
Fax: 866-309-8906<br />
This form is also available on the Disciples Health website:<br />
www.discipleshealth.org<br />
Can medical and dental premiums<br />
be reimbursed?<br />
No, the IRS does not allow reimbursement of monthly<br />
insurance premiums through a flexible spending<br />
account.<br />
When may I enroll?<br />
You must enroll within 31 days of your hire date or<br />
along with enrollment in the Churchwide Health Care<br />
Program. If you do, your contributions take effect as<br />
of the date you enroll. If you don’t enroll within the<br />
prescribed time frames, you must wait until the next<br />
annual enrollment to enroll.<br />
Annual enrollment takes place each year. During this<br />
time, you can start, stop, or change the amounts you are<br />
contributing to the flexible spending account(s). Any<br />
elections you make, however, take effect on January<br />
1 and remain in effect through December 31 of that<br />
calendar year.<br />
The before-tax advantage<br />
By contributing to a Healthcare FSA, you authorize a<br />
congregation or church-related organization to set<br />
aside a certain amount from your pay before taxes are<br />
withheld. Since you are taxed only on the cash salary<br />
amount remaining in your paycheck, this reduces your<br />
taxable wages. Lower taxable income means that you<br />
pay less in taxes.<br />
Your Health Care FSA contributions are not subject to:<br />
Federal Income Taxes;<br />
Social Security (FICA or SECA) taxes, and;<br />
Most state and local (including county) income<br />
taxes. (Rules vary, and state and local taxes are subject<br />
to frequent changes.)<br />
PAGE 9
Voluntary Dental Program<br />
Dental PPO Plan - Delta Dental (voluntary)<br />
Delta Dental has one of largest networks of dentists in<br />
the country through DeltaPremier USA. With the PPO<br />
dental plan, you may see any dentist that you choose.<br />
However, you have access to discounted charges by<br />
utilizing network providers.<br />
You will receive your Dental ID card in the mail within<br />
three weeks of your enrollment.<br />
To locate participating dentists, go to www.deltadental.<br />
com or call1-800-524-0149.<br />
PPO Dentist Premier Dentist Non-Participating<br />
Dentist<br />
Plan Pays Plan Pays Plan Pays*<br />
Diagonstic & Preventive<br />
Diagnostic & Preventive Services:<br />
includes exams, cleanings and flouride<br />
100% 100% 100%<br />
Brush Biopsy: to dectect oral cancer 100% 100% 100%<br />
Bitewing Radiographs: bitewing X-rays 100% 100% 100%<br />
Basic Services<br />
Space Maintainers: appliances to prevent<br />
tooth movement<br />
50% 50% 50%<br />
Emergency Palliative Treatment:<br />
to temporarily relieve pain<br />
50% 50% 50%<br />
Sealants: to prevent decay of permanent<br />
teeth<br />
50% 50% 50%<br />
All Other Radiographs: other x-rays 50% 50% 50%<br />
Minor Restorative Services: fillings &<br />
crown repair<br />
50% 50% 50%<br />
Endodontic Services: root canals 50% 50% 50%<br />
Periodontic Services: to treat gum disease 50% 50% 50%<br />
Oral Surgery Services: extractions & dental<br />
surgery<br />
50% 50% 50%<br />
Other Basic Services: misc. services 50% 50% 50%<br />
Relines & Repairs: bridges & dentures 50% 50% 50%<br />
Major Services<br />
Major Restorative Services: crowns 25% 25% 25%<br />
Prosthodontic Services: includes bridges,<br />
implants & dentures<br />
25% 25% 25%<br />
Orthodontic Services<br />
Orthodontic Services: includes braces 50% 50% 50%<br />
Orthodontic Age Limit up to age 19 up to age 19 up to age 19<br />
*When you receive services from a Nonparticipating Dentist, the percentages in this column indicate the portion of Delta Dental’s<br />
Nonparticipating Dentist Fee that will be paid for those services. This Nonparticipating Dentist Fee may be less than what your dentist<br />
charges, which means that you will be responsible for the difference.<br />
PAGE 10
Voluntary Dental Program<br />
Covered Services<br />
Oral exams (including evaluations by a specialist) are<br />
payable twice per calendar year.<br />
Prophylaxes (cleanings) are payable twice per calendar<br />
year.<br />
Fluoride treatments are payable once per calendar<br />
year for people up to age 14.<br />
Bitewing X-rays are payable once per calendar year<br />
and full mouth X-rays (which include bitewing<br />
X-rays) are payable once in any five-year period.<br />
Sealants are only payable once per tooth per lifetime<br />
for the occlusal surface of first permanent molars<br />
up to age nine and second permanent molars up<br />
to age 14. The surface must be free from decay and<br />
restorations.<br />
Crowns, inlays, and substructures are payable once<br />
per tooth in any seven-year period.<br />
Deductible<br />
$50 deductible per person total per benefit year. The<br />
deductible does not apply to diagnostic services, prophylaxes<br />
(cleanings), fluoride, brush biopsy, bitewing<br />
x-rays, and orthodontic services.<br />
Dental Care Around the World<br />
Having Delta Dental coverage makes it easy for our<br />
enrollees to get dental care almost everywhere in the<br />
world! You can receive expert dental care when you<br />
are outside of the United States through our Passport<br />
Dental program. This program gives you access to<br />
a worldwide network of dentists and dental clinics.<br />
English-speaking operators are available around the<br />
clock to answer questions and help you schedule care.<br />
For more information, check our web site or contact<br />
your benefits representative to get a copy of our<br />
Passport Dental information sheet.<br />
Composite resin (white) restorations are Covered<br />
Services on posterior teeth.<br />
Porcelain crowns are optional treatment on posterior<br />
teeth.<br />
Full and partial dentures are payable once in any<br />
seven-year period.<br />
Bridges and substructures are payable once in any<br />
seven-year period.<br />
Implants and implant related services are payable<br />
once per tooth in any seven-year period.<br />
People with certain high-risk medical conditions<br />
may be eligible for additional prophylaxes (cleanings)<br />
or fluoride treatment. The patient should talk<br />
with his or her dentist about treatment.<br />
Maximum Payment<br />
$1,000 per person total per benefit year on all services<br />
except orthodontics. $500 per person total per lifetime<br />
on orthodontic services.<br />
PAGE 11
Employer Paid Dental Program<br />
Dental PPO Plan - Delta Dental (employer paid)<br />
What is DeltaPremier USA?<br />
DeltaPremier USA is a carefully managed fee-for-service<br />
program administered by Delta Dental. “Fee-for-service”<br />
means that the dentist charges a fee for each service<br />
performed, then sends a claim to Delta Dental. Delta<br />
Dental then pays a certain percentage for each covered<br />
service. With DeltaPremier USA, you are likely to lower<br />
your out-of-pocket costs by going to a DeltaPremier<br />
participating dentist. That is because participating dentists<br />
agree to accept their fee or Delta Dental’s UCR fee,<br />
whichever is less, as full payment for covered services.<br />
More than 108,000 dentists throughout the United<br />
States and its territories participate in DeltaPremier<br />
USA.<br />
PPO Dentist Premier Dentist Non-Participating<br />
Dentist<br />
Plan Pays Plan Pays Plan Pays*<br />
Diagonstic & Preventive<br />
Diagnostic & Preventive Services:<br />
includes exams, cleanings, flouride &<br />
100% 100% 100%<br />
space maintainers<br />
Emergency Palliative Treatment:<br />
to temporarily relieve pain<br />
100% 100% 100%<br />
Sealants: to prevent decay of permanent<br />
teeth<br />
100% 100% 100%<br />
Radiographs: x-rays 100% 100% 100%<br />
Basic Services<br />
Minor Restorative Services: fillings &<br />
crown repair<br />
80% 80% 80%<br />
Endodontic Services: root canals 80% 80% 80%<br />
Periodontic Services: to treat gum disease 80% 80% 80%<br />
Oral Surgery Services: extractions & dental<br />
surgery<br />
80% 80% 80%<br />
Other Basic Services: misc. services 80% 80% 80%<br />
Major Services<br />
Major Restorative Services: crowns 50% 50% 50%<br />
Relines & Repairs: bridges & dentures 50% 50% 50%<br />
Prosthodontic Services: includes bridges,<br />
implants & dentures<br />
50% 50% 50%<br />
Orthodontic Services<br />
Orthodontic Services: includes braces 50% 50% 50%<br />
Orthodontic Age Limit up to age 19 up to age 19 up to age 19<br />
*When you receive services from a Nonparticipating Dentist, the percentages in this column indicate the portion of Delta Dental’s<br />
Nonparticipating Dentist Fee that will be paid for those services. This Nonparticipating Dentist Fee may be less than what your dentist<br />
charges, which means that you will be responsible for the difference.<br />
PAGE 12
Employer Paid Dental Program<br />
Covered Services<br />
Oral exams (including evaluations by a specialist) are<br />
payable twice per calendar year.<br />
Prophylaxes (cleanings) are payable twice per calendar<br />
year.<br />
Fluoride treatments are payable twice per calendar<br />
year for people up to age 19.<br />
Bitewing X-rays are payable once per calendar year<br />
and full mouth X-rays (which include bitewing<br />
X-rays) are payable once in any five-year period.<br />
Sealants are only payable once per tooth per lifetime<br />
for the occlusal surface of first permanent molars<br />
up to age nine and second permanent molars up<br />
to age 14. The surface must be free from decay and<br />
restorations.<br />
Composite resin (white) restorations are Covered<br />
Services on posterior teeth.<br />
Porcelain crowns are optional treatment on posterior<br />
teeth.<br />
Deductible<br />
$50 deductible per person total per benefit year limited<br />
to a maximum deductible of $150 per family per benefit<br />
year. The deductible does not apply to diagnostic and<br />
preventive services, emergency palliative treatment,<br />
x-rays, sealants and orthodontic services.<br />
Dental Care Around the World<br />
Having Delta Dental coverage makes it easy for our<br />
enrollees to get dental care almost everywhere in the<br />
world! You can receive expert dental care when you<br />
are outside of the United States through our Passport<br />
Dental program. This program gives you access to<br />
a worldwide network of dentists and dental clinics.<br />
English-speaking operators are available around the<br />
clock to answer questions and help you schedule care.<br />
For more information, check our Web site or contact<br />
your benefits representative to get a copy of our<br />
Passport Dental information sheet.<br />
Implants and implant related services are payable<br />
once per tooth in any seven-year period.<br />
People with certain high-risk medical conditions<br />
may be eligible for additional prophylaxes (cleanings)<br />
or fluoride treatment. The patient should talk<br />
with his or her dentist about treatment.<br />
Maximum Payment<br />
$1,200 per person total per benefit year on all services<br />
except orthodontics. $1,000 per person total per lifetime<br />
on orthodontic services.<br />
PAGE 13
Vision Benefits<br />
Vision - Vision Service Plan (VSP)<br />
Your vision coverage will be provided by Vision Service<br />
Plan (VSP) with national and local network access. With<br />
VSP doctors, you’ll enjoy quality, personalized care. Your<br />
VSP doctors will get to know you and your eyes, helping<br />
you keep them healthy year after year. Besides helping<br />
you see better, routine eye exams can detect symptoms<br />
of serious conditions such as glaucoma, cataracts, diabetes,<br />
and even tumors.<br />
Effortless Benefits<br />
Choose a VSP doctor at www.vsp.com or call 1-800-877-<br />
7195.<br />
Make an appointment and tell the doctor you are a VSP<br />
member.<br />
That’s it! No ID cards or filling out claim forms.<br />
Your Coverage from a VSP Doctor<br />
Exam covered in full<br />
Every plan year<br />
Prescription Eyewear Discounts<br />
Lens<br />
Frame<br />
Contact Lens Care<br />
20% discount when complete pair of glasses are purchased.<br />
20% discount when complete pair of glasses are purchased.<br />
15% discount off the contact lens fitting and evaluation exam.<br />
This exam is in addition to your vision exam to ensure proper fit<br />
of contacts.<br />
Extra Discounts and Savings<br />
Vision Correction Discounts<br />
Prescription Glasses<br />
Contacts<br />
20% off additional complete pairs of prescription glasses.<br />
15% off cost of contact lens exam (fitting & evaluation).<br />
20% off additional complete pairs of prescription glasses.<br />
Prescription Glasses*<br />
*Available from the same VSP doctor who provided your eye exam<br />
within the last 12 months<br />
15% off cost of contact lens exam (fitting & evaluation)<br />
Contacts*<br />
*Available from the same VSP doctor who provided your eye exam<br />
within the last 12 months<br />
Your Copays Exam $20<br />
PAGE 14
Legal Updates<br />
The Women’s Health and Cancer<br />
Rights Act<br />
The Women’s Health and Cancer Rights Act requires<br />
group health plans that provide coverage for mastectomy<br />
and certain reconstructive services. This law also<br />
requires that written notice of the availability of the<br />
coverage be delivered to all plan participants upon<br />
enrollment and annually thereafter. This language<br />
serves to fulfill that requirement for this year. These<br />
services include:<br />
Reconstruction of the breast(s) upon which the<br />
mastectomy has been performed;<br />
Surgery/reconstruction of the other breast to<br />
produce a symmetrical appearance;<br />
Prostheses; and<br />
Treatment for physical complications during all<br />
stages of mastectomy, including Iymphedemas.<br />
In addition, the plan may not:<br />
Interfere with a participant’s rights under the plan to<br />
avoid these requirements; or<br />
Offer inducements to the health care provider, or<br />
assess penalties against the provider, in an attempt<br />
to interfere with the requirements of the law.<br />
HIPAA Special Enrollment Rights<br />
If you are declining or have declined enrollment for<br />
yourself or your dependents (including your spouse)<br />
because of other health insurance coverage, you may<br />
in the future be able to enroll yourself or your dependents<br />
in this plan, provided that you request enrollment<br />
within 30 days after your other coverage ends.<br />
You may also be able to enroll yourself or your dependents<br />
in the future if you or your dependents lose health<br />
coverage under Medicaid or your state’s Children’s<br />
Health Insurance Program, or become eligible for state<br />
premium assistance for purchasing coverage under a<br />
group health plan, provided that you request enrollment<br />
within 60 days after that coverage ends or after<br />
you become eligible for premium assistance.<br />
In addition, if you have a new dependent as a result of<br />
marriage, birth, adoption, or placement for adoption,<br />
you may be able to enroll yourself and your dependents,<br />
provided that you request enrollment within 30<br />
days after the marriage, birth, adoption, or placement<br />
for adoption.<br />
HIPPA Privacy Notice<br />
Contact Michael Porter, Director of Health Services, for<br />
further details or questions. Churchwide Healthcare<br />
follows all legal requirements with regard to protecting<br />
your Protected Health Information (PHI).<br />
However, the plan may apply deductibles, coinsurance,<br />
and copays consistent with other coverage provided by<br />
the Plan.<br />
PAGE 15
Legal Updates<br />
Newborns & Mothers Health<br />
Protection Act<br />
Federal Law (Newborn’s and Mother’s Health Protection<br />
Act of 1996) prohibits the plan from limiting a mother’s<br />
or newborn’s length of hospital stay to less than 48<br />
hours for a normal delivery or 96 hours for a cesarean<br />
delivery or from requiring the provider to obtain<br />
pre-authorization for a stay of 48 hours or 96 hours,<br />
as appropriate. However, Federal Law generally does<br />
not prohibit the attending provider, after consultation<br />
with the mother, from discharging the mother or her<br />
newborn earlier than 48 hours for normal delivery or 96<br />
hours for cesarean delivery.<br />
Mental Health Parity Act<br />
According to the Mental Health Parity Act of 1996, the<br />
lifetime maximum and annual maximum dollar limits<br />
for mental health benefits under the CCHCBT Group<br />
Medical Plan are equal to the lifetime maximum and<br />
annual maximum dollar limits for medical and surgical<br />
benefits under this plan. However, mental health benefits<br />
may be limited to a maximum number of treatment<br />
days per year or series per lifetime.<br />
Children’s Health Insurance<br />
Program (CHIP) Coverage<br />
Under the Churchwide Healthcare group health plans,<br />
employees and their eligible dependents may enroll<br />
for coverage when they first become eligible for coverage<br />
and annually during Open Enrollment. In addition,<br />
employees and/or their eligible dependents are<br />
allowed to enroll in the group health plan if they experience<br />
a special enrollment event under the Health<br />
Insurance Portability and Accountability Act (HIPAA).<br />
Effective April 1, 2009, the plan rules have changed to<br />
allow you and/or your eligible dependents to enroll for<br />
coverage under a new HIPAA special enrollment opportunity.<br />
If you have any questions or want more information,<br />
please contact Michael Porter, Director of Health<br />
Services at 866-495-7322.<br />
Continuation Required by Federal<br />
Law for You and Your Dependents<br />
Federal law enables You or Your Dependent to continue<br />
health insurance if coverage would cease due<br />
to a reduction of your work hours or your termination<br />
of employment (other than for gross misconduct).<br />
Federal law also enables Your Dependent(s) to continue<br />
health insurance if their coverage ceases due to your<br />
death, divorce, legal separation, or with respect to a<br />
Dependent Child (ren), failure to continue to qualify as<br />
a Dependent. Continuation must be elected in accordance<br />
with the rules of Your Employer’s group health<br />
plan(s) and is subject to Federal law, regulations and<br />
interpretations.<br />
PAGE 16
Medicare Part D Notice<br />
Important Notice about your prescription drug coverage and Medicare<br />
Please read this notice carefully and keep it where<br />
you can find it. This notice has information about your<br />
current prescription drug coverage with Churchwide<br />
Healthcare and about your options under Medicare’s<br />
prescription drug coverage. This information can help<br />
you decide whether or not you want to join a Medicare<br />
drug plan. If you are considering joining, you should<br />
compare your current coverage, including which drugs<br />
are covered at what cost, with the coverage and costs of<br />
the plans offering Medicare prescription drug coverage<br />
in your area. Information about where you can get help<br />
to make decisions about your prescription drug coverage<br />
is at the end of this notice.<br />
There are two important things you need to know about<br />
your current coverage and Medicare’s prescription drug<br />
coverage: Medicare prescription drug coverage became<br />
available in 2006 to everyone with Medicare. You can<br />
get this coverage if you join a Medicare Prescription<br />
Drug Plan or join a Medicare Advantage Plan (like an<br />
HMO or PPO) that offers prescription drug coverage. All<br />
Medicare drug plans provide at least a standard level of<br />
coverage set by Medicare. Some plans may also offer<br />
more coverage for a higher monthly premium.<br />
When can you join a Medicare drug plan?<br />
You can join a Medicare drug plan when you first<br />
become eligible for Medicare and each year from<br />
November through December.<br />
However, if you lose your current creditable prescription<br />
drug coverage, through no fault of your own,<br />
you will also be eligible for a two (2) month Special<br />
Enrollment Period (SEP) to join a Medicare drug plan.<br />
What happens to your current coverage if you<br />
decide to join a Medicare drug plan?<br />
If you decide to join a Medicare drug plan, your current<br />
CCHCBT coverage will not be affected. Your current<br />
coverage pays for other expenses in addition to prescription<br />
drugs. If you enroll in a Medicare prescription<br />
drug plan, you and your eligible dependents will still<br />
be eligible to receive all of your current health and prescription<br />
drug benefits. If you drop your current coverage<br />
and enroll in Medicare prescription drug coverage,<br />
you may enroll back into Churchwide Healthcare’s benefit<br />
plan during the annual enrollment period under<br />
Churchwide Healthcare’s Benefit Plan.<br />
CCHCBT has determined that the prescription drug<br />
coverage offered by the Churchwide Healthcare Health<br />
Plan is, on average for all plan participants, expected<br />
to pay out as much as standard Medicare prescription<br />
drug coverage pays and is therefore considered<br />
Creditable Coverage. Because your existing coverage<br />
is Creditable Coverage, you can keep this coverage and<br />
not pay a higher premium (a penalty) if you later decide<br />
to join a Medicare drug plan.<br />
PAGE 17
Medicare Part D Notice<br />
When will you pay a higher premium (penalty) to join a Medicare Drug Plan?<br />
You should also know that if you drop or lose your current<br />
coverage with CCHCBT and don’t join a Medicare<br />
drug plan within 63 continuous days after your current<br />
coverage ends, you may pay a higher premium (a penalty)<br />
to join a Medicare drug plan later.<br />
If you go 63 continuous days or longer without creditable<br />
prescription drug coverage, your monthly premium<br />
may go up by at least 1% of the Medicare base<br />
beneficiary premium per month for every month that<br />
you did not have that coverage. For example, if you go<br />
nineteen months without creditable coverage, your<br />
premium may consistently be at least 19% higher than<br />
the Medicare base beneficiary premium. You may have<br />
to pay this higher premium (a penalty) as long as you<br />
have Medicare prescription drug coverage. In addition,<br />
you may have to wait until the following November to<br />
join.<br />
For more information about this notice or your current<br />
prescription drug coverage ...<br />
Contact Michael Porter, Director of Health Services, at<br />
866-495-7322. NOTE: You’ll get this notice each year.<br />
You will also get it before the next period you can join<br />
a Medicare drug plan, and if this coverage through<br />
CCHCBT changes. You also may request a copy of this<br />
notice at any time.<br />
For more information about your options under medicare<br />
prescription drug coverage ...<br />
More detailed information about Medicare plans that<br />
offer prescription drug coverage is in the “Medicare &<br />
You” handbook. You will get a copy of the handbook<br />
in the mail every year from Medicare. You may also be<br />
contacted directly by Medicare drug plans.<br />
For more information about Medicare prescription<br />
drug coverage:<br />
Visit www.medicare.gov<br />
Call your State Health Insurance Assistance Program<br />
(see the inside back cover of your copy of the “Medicare<br />
& You” handbook for their telephone number) for personalized<br />
help;<br />
Call 1-800-MEDICARE (1-800-633-4227). TTY users<br />
should call 1-877-486-2048.<br />
If you have limited income and resources, extra help<br />
paying for Medicare prescription drug coverage is available.<br />
For information about this extra help, visit Social<br />
Security on the web at www.socialsecurity.gov, or call<br />
them at 1-800-772-1213 (TTY 1-800-325-0778).<br />
Name of Entity/Sender<br />
Christian Church Health Care Benefit Trust<br />
Contact<br />
Michael Porter; Director of Health Services<br />
Address<br />
130 East Washington Street, Indianapolis, IN 46204<br />
Phone Number<br />
866-495-7322<br />
Remember: Keep this Creditable Coverage notice. If you decide to join one of the Medicare drug plans, you may be<br />
required to provide a copy of this notice when you join to show whether or not you have maintained creditable coverage<br />
and, therefore, whether or not you are required to pay a higher premium (a penalty).<br />
PAGE 18
Terms You Should Know<br />
Coinsurance<br />
The percentage of eligible expenses you and the plan<br />
share. The exact coinsurance depends on the plan your<br />
employer offers.<br />
Co-payment<br />
The fixed, up-front dollar amount you pay for certain<br />
covered expenses. Co-payment amounts do not apply<br />
toward your deductible or coinsurance, and they do not<br />
accumulate toward the out-of-pocket maximum.<br />
Deductible<br />
Intial amount you must pay each benefit year for<br />
covered services before the plan begins to provide<br />
benefits.<br />
Flexible Savings Account (FSA)<br />
An account allowed under Section 125 of the tax code<br />
to allow employees to set aside funds on a pre-tax basis<br />
to reimburse the member for IRS approved medical,<br />
dental and vision expenses not covered by Churchwide<br />
Healthcare. The catch is the “use it or lose it” clause,<br />
which means if you do not exhaust your account<br />
in the calendar year, then remaining funds remit to<br />
Churchwide Healthcare.<br />
High Deductible Health Plan (HDHP)<br />
A High Deductible Health Plan is defined as a health<br />
plan that does not have deductible less than $1200<br />
for individual/$2400 for family (not to exceed $6050<br />
individual/$12,100 for family). May be used with either<br />
a Health Reimbursement Account or Health Savings<br />
Account for approved non-covered medical expenses.<br />
Health Insurance Portability and<br />
Accessibility Act (HIPAA)<br />
This law has two affects on Churchwide Healthcare. On<br />
the one hand, it mandates the issuance of Certificates of<br />
Credible Coverage to help offset pre-existing condition<br />
time periods. More recently, it has been updated to<br />
protect personal health information (PHI) from being<br />
distributed to disinterested parties and to insure the<br />
privacy of our members.<br />
Health Reimbursement Account (HRA)<br />
Health Reimbursement Accounts are set up by<br />
employers to reimburse employees for IRS approved<br />
medical, dental and vision expenses not covered by<br />
Churchwide Healthcare, usually paired with the High<br />
Deductible Health Plan.<br />
Health Savings Account (HSA)<br />
Health Savings Accounts are money market like<br />
accounts that can be set up with contributions from<br />
either the employer, employee or both. <strong>Fund</strong>s go<br />
into these accounts tax-free and as long as the funds<br />
are used for IRS approved medical, dental and vision<br />
expenses not covered by Churchwide Healthcare<br />
High Deductible Health Plans, are withdrawn tax free.<br />
<strong>Fund</strong>s are owned by the employee, regardless of the<br />
contributor, and can be carried over year to year.<br />
In-Network Care<br />
Care you receive from in-network physicians, specialists,<br />
hospitals. rehabilitation centers, labs and other<br />
healthcare providers that have signed an agreement<br />
with their local Blue Cross and Blue Shield plan. Innetwork<br />
providers accept the allowable charge as<br />
payment in full. They also file claims for you. In-network<br />
care is paid at the higher level of benefits.<br />
Out-of-Network Care<br />
Care you receive from healthcare providers who are not<br />
in the network. This care is covered at the lower,. outof-network<br />
level when it is determined to be medically<br />
necessary and appropriate.<br />
Out-of-Pocket Maximum<br />
The amount you pay out of your pocket for eligbile<br />
healthcare expenses before the plan begins to pay 100%<br />
for additional eligible expenses. The out-of-pocket limit<br />
does not include co-payments, deductibles, mental<br />
health/substance abuse expenses, prescription drug<br />
expenses or amounts over the allowable plan charge.<br />
Preferred Provider Organization Program<br />
(PPO)<br />
A program that does not require the selection of a<br />
primary care physician, but is based on a provider<br />
network made up of physicians, specialists, hospitals<br />
and other healthcare facilities. Using this provider<br />
network helps assure members receive coverage for<br />
eligible services.<br />
Patient Protection and Afforadable Care<br />
Act of 2010 (PPACA)<br />
Commonly known as the Health Care Reform Law, this<br />
law is the guiding force of health coverage starting<br />
2011 going forward. Some of the changes already in<br />
place include covering dependents to age 26, no preexisting<br />
condition clauses for children under age 19,<br />
and codifying preventive care services to be covered at<br />
100%.<br />
PAGE 19
Christian Church (Disciples of Christ)<br />
Health Care Benefit Trust<br />
130 E. Washington Street<br />
Indianapolis, IN 46204-3659<br />
Toll-free: 866.495.7322<br />
Phone: 317-634-4504<br />
Fax: 317.634.4071<br />
www.discipleshealth.org