Hallux Varus - The Podiatry Institute
Hallux Varus - The Podiatry Institute
Hallux Varus - The Podiatry Institute
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
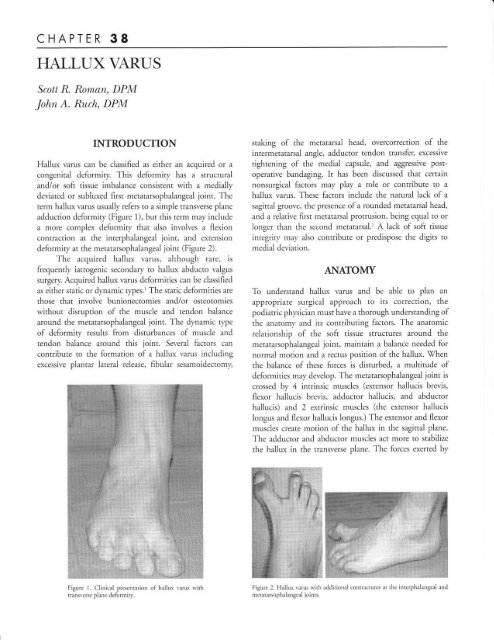
CHAPTER 38FIALLUX VARI]SScott R. Roman, DPM.lolrn A. Ruclt, DPMINTRODUCTION<strong>Hallux</strong> varus can be classified as either an acquired or acongenital deformity. This deformity has a structuraland/or solt tissue imbalance consistent with a mediallydeviated or subluxed first metatarsophaiangeal joint. <strong>The</strong>term hallux varus usually refers to a simple transverse planeadduction deformity (Figure 1), but this term may includea more complex deformity that aiso involves a flexioncontraction at the interphalangeal joint, and extensiondeformity at the metatarsophalangeal joint (Figure 2).<strong>The</strong> acquired hallux varus, although rare, isfrequently iatrogenic secondary to hallux abducto valgussurgery. Acquired hallux varus deformities can be classifiedas either static or dynamic types.'<strong>The</strong> static deformities arethose that involve bunionectomies and/or osteotomieswithout disruption of the muscle and tendon balancearound the metatarsophalangeal joint. <strong>The</strong> dynamic rypeof deformity results from disturbances of muscle andtendon balance around this joint. Several factors cancontribute to the formation of a hallux varus includingexcessive plantar lateral release, fibular sesamoidectomy,staking of the metatarsal head, overcorrection of theintermetatarsal angle, adductor tendon transfer, excessivetightening of the medial capsule, and aggressive postoperativebandaging. It has been discussed that certainnonsurgical factors may play a role or contribute to ahallux varus. <strong>The</strong>se factors include the natural lack of asagittal groove, the presence of a rounded metatarsal head,and a relative first metatarsal protrusion, being equal to orlonger than the second metatarsal.' A lack of soft tissueintegriry may also contribute or predispose the digits tomedial deviation.ANAIOMYTo understand hallux varus and be able to plan anappropriate surgical approach to its correction, thepodiatric physician must have a thorough understanding ofthe anatomy and its contributing factors. <strong>The</strong> anatomicrelationship of the soft tissue structures around themetatarsophalangeal joint, maintain a balance needed fornormal motion and a rectus position of the hallux. 'i7henthe balance of these forces is disturbed, a muititude ofdeformities may develop. <strong>The</strong> metatarsophalangeal joint iscrossed by 4 intrinsic muscles (extensor hallucis brevis,flexor hallucis brevis, adductor hallucis, and abductorhallucis) and 2 extrinsic muscles (the extensor hallucislongus and flexor haliucis longus.) <strong>The</strong> extensor and flexormuscles create motion of the hallux in the sagittal plane.<strong>The</strong> adductor and abductor muscles act more to stabilizethe hallux in the transverse plane. <strong>The</strong> forces exerted byFigure 1. Clinical presentarion oF hallux varus rvithtransverse plane deformitl..Figure 2. <strong>Hallux</strong> varus u,ithmcratarsophalangeal joints.;rdditional contracrures at the interphalanqeirl and
CHAPTE,R 38 237these muscles are baianced by their anatomic position,preventing the hallux from deviating. <strong>The</strong> metatarsopha-Iangeal joint is further stabilized by a strong capsule andcollaterai ligaments. <strong>The</strong>se ligaments form a fan-shapedband that originates from the medial and lateralepicondyles. <strong>The</strong>y run distal and plantar to the base of theproximal phalanx and blend inferior with the ligamentsof the medial and lateral sesamoid. <strong>The</strong> sesamoids areincorporated into the medial and lateral heads of the flexorhallucis brevis tendon and articulate with the plantarsurface of the metatarsal. <strong>The</strong>y provide the muscle withincreased force and leverage in plantarflexing the hallu-x.ETIOLOGYAn approach to hallux varus repair can only beaccomplished by following a thorough evaluation andunderstanding its cause. Although fibular sesamoidectomyhas historically been attributed as a primary cause,3 severalfactors must be present before the first metatarsophaiangealjoint will assume a varus position.a't <strong>The</strong>se factors arediscussed individually but it is a combination of thesefactors that usually lead to this deformity.Plantar Lateral ReleaseOne approach to the restoration of joint balance in halluxabducto valgus surgery is based on a sequential release oflateral joint contractures. This systematic approach beginswith the release of the adductor tendon, transaction of thefibular sesamoidal ligament, transaction of the lateral headof the flexor hallucis brevis, fibular sesamoidectomy, andfinally lateral capsulotomy. This is a step-wise processicareful consideration must be taken into account thatwith each step, the medial structures gain an enhancedmuscular advantage.Medial ExostectomyExcessive resection of the medial eminence or staking thefirst metatarsal head acts to destabilize this portion of thejoint (Figure 3). <strong>The</strong> sagittal groove stabilizes the medialrim of the base of the proximal phalanx. <strong>The</strong> plantarmedial condyle serves as a buttress for the tibial sesamoid.Excessive resection of these 2 areas may result in medialdisplacement of the proximai phalanx and tibialsesamoid. This displacement will further accentuate themedially deforming pull to hold the hallux in varus. <strong>The</strong>appropriate resection of the medial eminence would be anangle that is oriented dorsal lateral to plantar medial(Figure 4). This would preserve the sagittal and tibialsesamoidal grooyes, and allow for medial stability of themerararsophala ngeal joi n r.Overcorrection of Intermetatarsal AngleFollowing metatarsal osteotomy, an aggressive lateraltranslocation of the capital fragment may lead to a negativeintermetatarsal angle. As the intermetatarsal angledecreases, the medial vector of pull from the soft tissuesincreases. This is only compounded when accompanied byFigure 3. Hailux varus resulting from excessiveresection of the medial eminence.Figure 4. Appropriate angle for resection ofthe medialeminence. Note the preservation of the sagittal andtibial sesamoidal grooves.
238 CHAPTER 38weak lateral soft tissue structures andlor loss of medialosseous stabiliq.. An aggressive lateral shift may also bevisualized by an increased proximal space between the firstand second metatarsal on the dorso-plantar radiograph(Figure 5).Adductor Tendon ThansferLateral deviation of the sesamoid apparatus is commonlyencountered in hallux valgus surgery. Restoration of thisapparatus beneath the head of the first metatarsal can beaccomplished in several ways. <strong>The</strong> release of lateral softtissue contractures and lateral translocation of themetatarsal head have already been discussed. <strong>The</strong> adductortendon may be transferred beneath the extensor hallucisIongus and attached to the medial capsule. 'W4ren appliedwith adequate tension, this transfer can help repositionthe laterally deviated sesamoids below the meratarsal(Figure 6). An overly aggressive transfer may create medialsubluxation of the sesamoid apparatus and subsequentmedial joint imbalance.6Excessive Medial CapsulorrhaphyJoint balance may also be altered if one excises too muchcapsular tissue or plicates the capsule too tightly in orderto obtain greater correction. This alone may not create ahallux varus, but in conjunction with other previouslydiscussed factors, will predispose toward medialsubluxation. An aggressive postoperative dressing mayhave a similar effect, to hold the hallux malpositioned andallow for fibrosis in an adducted position.CLINICAL FINDINGS<strong>The</strong> clinical evaluation attempts to identifi, all componentsof the deformity. <strong>The</strong> patient should be observed in both anonweightbearing and full-weightbearing attitude. Thisexamination should be compared to the contra lateralextremiq,. An exaggeration of the deformity with weightbearing suggests an increased role of muscle tendonimbalance. This applies not only to the transverse planeadduction deformity, but also to the sagittal planecontracture and loss of purchase with supporting surface.-Figure 5. <strong>Hallux</strong> varus resulting from an aggressive lateral shift. Note theincreased space berween the proximal first and second metatarsals.Figure 6. Adductor tendon transfer to reposition the lateralll' deviatedrerlrtto'dr belou rlre n eiarJr)rlFigure 7. <strong>Hallux</strong> r.arus follorving fibuJar sesamoidectomy.Figure 8. Intermetatarsal angle reduced to zero degrees.
CHAPTER 38 239Other finding may include a positive metatarsal protrusionangle and/or a rounded metatarsal head, <strong>The</strong>se findingsshould confirm clinical observations.PAIIENTS AND METHODSFigure 9. <strong>Hallux</strong> varus with associated metatarsus adductus.A great toe that purchases the suppordng surftcewith weightbearing indicates that the intrinsicmusculature integrity has been preserved. A floating to ormalleus deformity suggests partial or complete loss of thosemuscles responsible for stabilization of the proximalphalanx. A thorough examination of flexion and extensionat both the interphalangeal and metatarsophalangeal jointswill assess integrity and function of the surroundingmusculature. Manipulation in the transverse plane willprovide an appreciation of the amount of contractureassociated with the abductor hallucis muscle and integrityof the lateral capsular structures. <strong>The</strong> quality and range ofmotion, as well as the ability to reduce the deformiry areimportant factors in determining corrective procedures.This assessment will help to determine whether muscletendon balancing or osseous procedures are needed foradequate reduction of the deformity.RADIOGRAPHIC FINDINGS<strong>The</strong> dorsoplantar radiograph provides informationregarding the severity of the deformity in the transverseplane, status and alignment of the joints, and presence orabsence of the sesamoid bones (Figure 7). <strong>The</strong> degree ofdeformity can be measured by determining the halluxabductus angle. <strong>The</strong> normal values are between 5 and 15degrees, but with a varus deformity this angle may be zeroor even negative, as the phalanx subluxes medially on themetatarsal head. <strong>The</strong> intermetatarsal angle may also havean angle close to zero or negative (Figure 8). <strong>The</strong>metatarsus adductus angle can be increased (Figure 9).Medial transposition of the tibial sesamoid on themetatarsal is often seen following staking of the head.<strong>The</strong> authors reviewed the possible cause(s) for halluxvarus in 1 1 patients that presented with this postoperativedeformity. <strong>The</strong> corresponding radiographs of these feetwere reviewed: the hallux abductus and intermetatarsaiangles, the shape of the first metatarsal head, the presenceof metatarsus adductus, the relative iengths of the firstand second metatarsals, and tibial/fibular sesamoidpositioned were noted on these films. A review of thecorresponding operative reports noted possible soft tissuecontributions to the varus deformiry such as lateral headrelease ofthe flexor hallucis brevis, Iateral capsular release,adductor tendon transfer, and medial capsulorrhaphy.OBSERVATIONS<strong>The</strong> patient population in this hallux varus reviewconsisted of 11 adult females. <strong>The</strong> deformity presentedpostoperatively to hallux abducto valgus surgery. <strong>The</strong>rewere 10 distal Austin osteotomies and 1 closing base wedgeperformed. All procedures inciuded a lateral release of someform. Adductor tendons were released in all 11 cases withtransfer of the tendon in 6 cases. <strong>The</strong> lateral head of theflexor hallucis brevis was resected in 7 cases and the fibularsesamoid was removed in 6 cases. <strong>The</strong> lateral capsule of themetatarsophalangeal joint remained intact in all cases.Resection of the medial eminence was accomplished withhand instrumentation in an angle oriented dorsal lateral toplantar medial as previously described. <strong>The</strong> sagittal grooveand plantar medial condyle remained intact in all cases.In an analysis of this data no consistent finding couldbe attributed to the formation of the postoperative haliuxvarus. <strong>The</strong> combinations of multiple factors wereexamined; fibular sesamoidectomy with or withoutadductor tendon transfer, and flexor hallucis brevis tendonrelease without sesamoidectomy and/or tendon transfer. Amedial capsulorrhaphy was performed in just over half thecases, in combinations with the other factors. Only onecase of hallux varus had a metatarsus adductus component.A varus was also reported with none of the abovecontributing factors. <strong>The</strong> presence of a positive metatarsalprotrusion angle, rounded metatarsal head, or congenitalabsence ofa sagittal groove, was not reported.
240 CHAPTER 38CONCLUSION<strong>Hallux</strong> varus as a complication of surgery for halluxvalgus is complex and often has a multi factorial cause. Athorough understanding of the possible contributingfactors will help the podiatric physician to avoid orminimize its occurrence. Although this complication isunlikely to be caused by any one contribution factor, theexact combination in unknown. Our evaluation of a smallvarus popuiation failed to conclude a consistent factor inits development. Unique and individual characteristics toeach patient may play a role in this complication. Tominimize the overall risks, several key areas need to beaddressed. <strong>The</strong> plantar lateral release is a sequential releaseof deforming forces. Care must be taken to avoid beingtoo aggressive and disturb muscle balance at the joint.<strong>The</strong> medial sagittal and tibial sesamoidal groove needs tobe preserved to maintain the osseous balance berween thebase of the proximal phalanx, the sesamoids, and themetatarsal head. And finally, avoid the overcorrection ofthe intermetatarsal angle with an overly aggressive lateraltranslocation of the capital fragment and adductortendon transfer. Although surgical correction of thisdeformity was not discussed, careful evaluation of thepotential causes will aid in the decision of availableprocedures to correct its deformity.REFERENCES1. Hawkins FB. Acquired hallux varus: cause, prevention, and prevention.C lin. Orthop 197 1 :7 6:L69 -7 6.2. Janis LR, Donic II. <strong>The</strong> etiology of hallu varus: a review. J Am <strong>Podiatry</strong>,4ssoc 1975:65:233-7.3. Sanders M. Complications of hallux valgus surgery. Foot Ankle Clin1998;3.4. Edelman RD. Iatrogenically induced hallux varus. Clin Podia* MedSurg. 199l;8:367-82.5. Banks AS, Ruch lA, Kalish SR. Surgical repair of halllx varu. J Am PodMed. Asoc 1988:7 8:339-47.6. Taylor GC, Jimenez Al. Hallu varus. Reconstructive Surgery of theFoot and Leg, Update '92. Tucker (GA) <strong>Podiatry</strong> <strong>Institute</strong>Publishing; 1992. p. 367 -77.7. Yu GV, Sellers CS, Shook JE, Karlock LG. <strong>The</strong> firsr ray: iarrogenlcdeformities of the first ray. Clin Pod Med 1996;13:367-422.