Semi-direct application of a prefabricated composite veneering ...
Semi-direct application of a prefabricated composite veneering ...
Semi-direct application of a prefabricated composite veneering ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
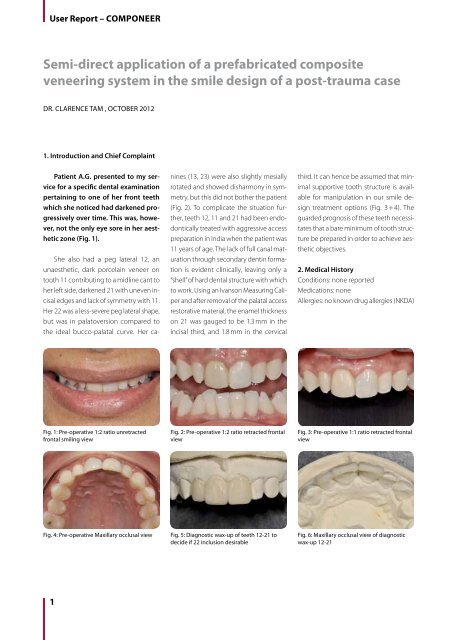
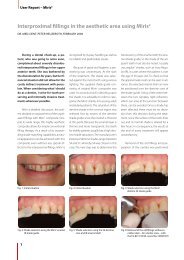
User Report – COMPONEER3. Treatment Plan for Limited Treatment <strong>of</strong> Maxillary Anterior Sextant (12-22)• Diagnostic wax-up to be fabricated to determine amount <strong>of</strong> buccal reduction required (Fig. 5 + 6) as well as for accurategauging <strong>of</strong> projected COMPONEER size using the provided COMPONEER Contour guide (Fig. 8 + 9).• Internal bleaching to be completed first on 21, then on 11 as required post-procedure depending on blockout ability <strong>of</strong> theA1/B1 SYNERGY D6 dentin shade (Fig. 7).• Minimal preparations to be completed under rubber dam isolation (split dam technique).• Mylar strip or similar isolation from adjacent teeth, micro-air abrasion (50 µm aluminum oxide) (Fig. 10) to be completed from12-22 buccal and proximal surfaces and incisal aspects followed by etching with 33 % orthophosphoric acid (Fig. 11) and<strong>application</strong> <strong>of</strong> One Coat Bond (Fig. 12 + 13)• Confirm COMPONEER desired size and pre-contour to fit (Fig. 14).• COMPONEER pre-treated with One Coat Bond left wet, and A1/B1 SYNERGY D6 dentin shade applied to intaglio surface <strong>of</strong>COMPONEER and spread evenly including marginal areas. COMPONEER placed in light-safe <strong>composite</strong> box during holdingphase (Fig. 16).• Etch, bond, palatal wall on peg lateral incisors to be placed with matrix support using Enamel Universal Shade (SYNERGY D6)and cured.• Creative Color Pink Opaquer placed on 11 to block out dark colour (Cosmedent) (Fig. 15).• Body dentin to be built up and pre-contoured to receive the COMPONEER but not cured.• COMPONEER placed on surface <strong>of</strong> tooth 11 (Fig. 17) and adapted using the COMPONEER Placer (Fig. 18). Excess removedusing COMPONEER Modelling Instrument MBS.• Procedure repeated for contralateral central incisor without curing the first. Midline and axial inclination confirmation beforetack-curing (10 seconds) each tooth. Excess removal before proceeding with lateral incisors (Fig. 19).• Procedure repeated individually for 12 and 22 having first built up the palatal wall using Enamel Universal.• Final curing to start on palatal aspect for 40 seconds per tooth before progressing to buccal aspects to control <strong>direct</strong>ion <strong>of</strong><strong>composite</strong> shrinkage.• Finishing, contouring and polishing to be completed (COLTENE Comprepol Plus, Composhine Plus) (Fig. 20 – 22).• Final buffing with Enamelize aluminum oxide paste (Cosmedent).Fig. 7: Componeer-specific shade tabsFig. 8: Componeer Contour Guide - Preoperativeevaluation tooth 11Fig. 9: Componeer Contour Guide -Pre-operative evaluation tooth 12Fig. 10: Post micro-air-abrasion and Mylarmatrix placementFig. 11: Application <strong>of</strong> 33 % orthophosphoricacid to enamel surfaceFig. 12: Application <strong>of</strong> 7th generationOne Coat Bond2
User Report – COMPONEER4. Description <strong>of</strong> Treatment IncludingRationale for Choice <strong>of</strong> RestorativeMaterialPatient A.G. Is -a 22-year-old femalewith a compromised dentition in her estheticzone. Features that are planned forimprovement would be increased incisaledge symmetry between the central andlateral incisors, correction <strong>of</strong> the peg lateralshape, correction <strong>of</strong> inconsistent shade valuesbetween teeth 12-22 and midline cantto the patient’s left side cervicoincisally.4.1. Considerations for RestorativeMaterialThe restorative modality called uponwould need to fulfil the criteria <strong>of</strong> minimaltooth preparation due to severely-compromisedcoronal strength <strong>of</strong> teeth 12, 11and 21, yet have surface gloss and texturesimilar to natural teeth. The feature <strong>of</strong> predictablereparability due to financial constraintsis attractive. Minimal preparationporcelain veneers would have resultedin a colour difference between the previously-veneeredtooth 11 and the 21 dueto thickness <strong>of</strong> ceramic material. If internalbleaching were not an option, tooth21 would need to be prepared aggressivelyto provide enough space to opaqueout the underlying colour. This would resultin an even-more compromised tooth.4.2. Treatment DescriptionFollowing successful internal bleaching<strong>of</strong> tooth 21 (35 % H 2O 2(aq) [OpalescenceEndo, Ultradent], the upper anterior sextantwas isolated with a split dam technique,comprised <strong>of</strong> #2A Hu-Friedy rubberdam clamps on teeth 24 and 14, anda Roeko non-latex rubber dam. Minimalveneer preparations were completedon teeth 12-22 and the projected size <strong>of</strong>COMPONEER confirmed using the contourguide. Interdental contact regionswere roughened and opened slightlyusing interdental abrasive strips. Surfacemicro-air abrasion (50 micron aluminumoxide) was completed before interdentalMylar matrices were fitted to isolateeach tooth. Each tooth was then etchedwith 33 % H3PO4 (aq) before <strong>application</strong><strong>of</strong> One Coat Bond (COLTENE) and lightcured.The peg laterals required separateconstruction <strong>of</strong> the palatal wall withSYNERGY D6 Enamel Universal before thenext stage.The COMPONEER is now secured usingthe COMPONEER Holder and trimmedto best fit the preparation before OneCoat Bond is applied to the intaglio surface.The bond is not cured at this point,and the body dentin shade chosen (A1/B1 SYNERGY D6) in this case is appliedevenly over the intaglio surface, coveringthe margins. This prepared COMPONEERis then shielded in a light-safe box untiluse. Tooth 11 was treated first withCreative Color Pink Opaquer (Cosmedent,Inc.) as there was an obvious valuedifference between 11 and 21. A1/B1SYNERGY D6 was then contoured <strong>direct</strong>lyon the tooth but not cured. The preparedCOMPONEER was pressed gently into positionusing the Placer instrument. Axialinclination can be easily-controlled usingthis instrument. Before tack-curing thisveneer, the same process was appliedto tooth 21, with the exception <strong>of</strong> pinkopaque <strong>application</strong>. The patient is thenFig. 13: Curing <strong>of</strong> One Coat Bond on eachtoothFig. 14: Contouring <strong>of</strong> Componeer usingabrasive discsFig. 15: Application <strong>of</strong> pink opaquer againstdarker value 11 prepFig. 16: Application <strong>of</strong> A1/B1 Synergy D6Dentin after wetting <strong>of</strong> Componeer intagliosurface with One Coat BondFig. 17: Application <strong>of</strong> Componeer to 11 and21 simultaneously surface withOne Coat BondFig. 18: Pressure seating <strong>of</strong> Componeer withPlacer instrument3
User Report – COMPONEERseated upright and the midline and arrangementjudged for the last time. TheCOMPONEER were tack cured for 10 secondswith an SDI Radii LED light sourcebefore fine debris removal. COMPONEERwere trimmed, fitted and prepared aspreviously described for teeth 12 and 22before seating with SYNERGY D6 A1/B1dentin <strong>composite</strong>, excess removal andtack-curing. The matrices were removed,and the patent contacts confirmed. Thegingivoproximal aspects were refined andtrimmed using a 12b scalpel blade. Followingfinal curing <strong>of</strong> the material andconfirming patent contacts, pencil markingswere placed over the facial surfaces<strong>of</strong> teeth 12, 11, 21 and 22, defining theline angles to be preserved. Incisal shapingwas completed using the provideddual-sided abrasive disks, and line anglesrefined. Primary and secondary anatomywas defined using needle-pointfine diamond burs (Mani Dia-burs) andlarge, coarse COMPONEER shaper discs(COLTENE), both without water irrigation.Final polishing was completed using thehigh-shine ultrapolishers that are specificto COMPONEER (Coltene DiatechPolishers), along with an Occlubrush(Kerr). Final buffing was achieved usingEnamelize (Cosmedent) aluminum oxidepolishing paste. The final result is a veryesthetically-pleasing, biomimetic, minimally-invasivesolution to the patient’s initialissues (Fig. 23 + 24). Note that postoperativeinternal bleaching <strong>of</strong> tooth 11for two days was required to just touchup the value to match acceptably withtooth 21. Taking virtually no tooth structureaway, the COMPONEER solution <strong>of</strong>fersa highly-refined solution for a dentalsituation many would just solve with fullcoverage porcelain restorations.4.3. Rationale for Choice <strong>of</strong> RestorativeMaterialFor patient A.G., factors <strong>of</strong> considerationin deciding the type <strong>of</strong> restoration involvedthe age <strong>of</strong> the patient, preservation<strong>of</strong> residual healthy tooth structure andenamel for bonding, coronal restrengtheningand esthetic predictability. In thiscase, the patient did not have an adequate“quorum” <strong>of</strong> residual tooth structure,obviating the bonded porcelainrestorative solution that would be idealgiven enough freedom to prepare toothstructure. The beauty <strong>of</strong> resin bonding ismaximum conservation <strong>of</strong> tooth structurewith maximum esthetic outcome ifthe restorative technique is correct, not tomention low-cost <strong>of</strong> maintainability overtime. Bonded porcelain restorations canbe justified only when the risk <strong>of</strong> biologicalreduction is outweighed by benefits,such as restoration <strong>of</strong> coronal stiffness. Inthis case, the risk <strong>of</strong> needed biological reductionmeant almost a terminal prognosisfor the teeth. In this case, the enamelshell has not been significantly compromised,merely added to.The rationale for using pure-nanohybrid-layeredresin restorations was basedon the studies <strong>of</strong> Periera et al 1) in 2003.They utilized a three-point bending device(ISO4049) and demonstrated that thehighest flexural strength was noted forthe pure hybrid <strong>composite</strong> veneer comparedto the micr<strong>of</strong>ill-veneered-hybrid resinveneer. To nobody’s surprise, the pureFig. 19: Rough finishing <strong>of</strong> Componeermargins after placement <strong>of</strong> 11 and 21 andflash-curingFig. 20: Formation <strong>of</strong> labial lobes with finetapered diamond burFig. 21: Contour refinement with CompPrePolPlus Diatech finishing rubber cupFig. 22: Initiation <strong>of</strong> high-polishing withCompo- Shine Plus Diatech finishing rubbercupFig. 23: Post-operative 1:2 ratio unretractedfrontal smiling viewFig. 24: Post-operative 1:2 ratio retractedfrontal view4
User Report – COMPONEERmicr<strong>of</strong>ill veneer exhibited the lowest flexuralstrength.COMPONEER is fabricated from pureSYNERGY D6 nanohybrid <strong>composite</strong>(COLTENE), and is “cemented” using pureSYNERGY D6 <strong>composite</strong>, creating a monoblockrestoration that is both very highin fracture toughness, but simultaneouslyreparable. Its physical properties are remarkablysimilar to the tooth layers weare replacing. The compressive strength<strong>of</strong> enamel is 384 MPa. The compressivestrength <strong>of</strong> COMPONEER is 392 MPa. Theflexural strength <strong>of</strong> dentin is 165.6 MPa.The flexural strength <strong>of</strong> COMPONEER is127 MPa. This is irrelevant as the residualdentin in the tooth has not been removedat all during this procedure. COMPONEERin this minimal-preparation case acted asmainly an additive restorative material.Bonding strength is one feature that is affectedpr<strong>of</strong>oundly by preparation technique,particularly with ceramic veneerbonding. Despite this, adhesive strength<strong>of</strong> the ceramic to the <strong>composite</strong> cementlayer remains low, and this is the regionwhere most failures are observed. Thechemistry <strong>of</strong> bonding <strong>composite</strong> resin totooth structure is well-documented. Byusing a pure-<strong>composite</strong> veneer solution,the adhesive strength value <strong>of</strong> the restorationis significantly greater comparedto a porcelain veneer cement sandwichsituation, minimizing retention failures.Surface hardness is ensured by applyingthe COMPONEER material through a dualcycle,500 kg mechanical press that ensuresmaximal homogeneity and lack <strong>of</strong> porositybefore light curing under pressure.As a result, Vickers hardness is rated at73 kg/mm 2 or 716 MPa. Dimensional stabilityis ensured by a low water absorptionrating <strong>of</strong> 16 µg/mm3, and a water solubility<strong>of</strong> less than 1 µg/mm3.COMPONEER represents an innovativeopportunity to provide a high-quality,long-lasting esthetic restoration that isboth tissue-conservative and cost-effective.There is no difference in modifiabilitycompared to a <strong>direct</strong>, layered <strong>composite</strong>veneer and yet its ease <strong>of</strong> <strong>application</strong>makes it extraordinarily time-efficient. Thesurface can be contoured, reduced or addedto as required, but what is comfortingis knowing that underneath the brilliantesthetic result lies a virtually flawless <strong>composite</strong>surface that not only strengthensthe tooth but will provide it and the patientwith a lustrous, confident face formany years to come.Fig. 25: Post-operative 1:1 ratio retractedfrontal viewFig. 26: Periapical X-ray 23011/23012 suffix:Post-operative view <strong>of</strong> teeth 12 and 11/21and 225
User Report – COMPONEER4.4. Treatment List (FDI classification)• Tooth 12 MIBD: Direct COMPONEER restoration with supporting acid-etched resin• Tooth 11 MIBD: Direct COMPONEER restoration with supporting acid-etched resin• Tooth 11: non-vital bleaching × 2 days• Tooth 21 MIBD: Direct COMPONEER restoration with supporting acid-etched resin• Tooth 21: non-vital bleaching × 2 days• Tooth 22 MIBD: Direct COMPONEER restoration with supporting acid-etched resin4.5. Restorative Material• Lingual shelf formation on peg laterals: Enamel Universal SYNERGY D6• Body dentin formation: A1/B1 SYNERGY D6 dentin shade• Universal enamel shade chameleon effect demonstration (COMPONEER Enamel Universal shade)4.6. Adhesive System• Teeth 12, 11, 21, 22: micro-air abrasion (50 micron aluminum oxide) followed by acid-etched 5th generation(One Coat Bond, COLTENE) preparation5. References1)Pereira, C.L., Demarco, F.F., Cenci, M.S., Osinago, W.R. and Piovesan, E.M. Flexural Strength <strong>of</strong> Composites:Influences <strong>of</strong> Polyethylene Fiber Reinforcement and type <strong>of</strong> <strong>composite</strong>. Clinical Oral Investigations 2003; 7(2): 116-119CONTACTDr. Clarence Tam, HBSc, DDSCosmetic and General Dentistry18 Morrow StreetNewmarket, Auckland 1023www.clarencetam.co.nzDr. Clarence TamChairperson and DirectorNew Zealand Academy <strong>of</strong> CosmeticDentistrywww.nzacd.co.nz0013886