Chloracne, a Misnomer and Its Implications - ResearchGate
Chloracne, a Misnomer and Its Implications - ResearchGate
Chloracne, a Misnomer and Its Implications - ResearchGate
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
EditorialD e r m a t o l o g y 2010 ; 2 21: 2 3 –26DOI: 10.1159/000290672Published online: April 30, 2010Chlorac ne, a M isnome r <strong>and</strong> I t s<strong>Implications</strong>J. H . S aur at O. S orgS C A H T – D e r m a t o t o x i co l o g i e , Ce n t r e M é d i c a l U n i ve r s i t a i r e , G e n e v a , Sw i t z e r l a n dIn this issue, Passarini et al. [1] report on an outbreakof so-called chloracne in Italy. This article importantlyreminds us of the many issues that relate to human dermatotoxicologyin general <strong>and</strong> dioxin exposure in particular.The skin is a key organ for the recognition of exposureto several poisons, <strong>and</strong> more specifically those related tothe dioxin group. Such a ‘sentinel’ role for the skin is mostprobably related to the fact that many poisons, introducedeither through the skin or systemically, are metabolizedin the skin <strong>and</strong> therein induce symptoms thatmay be specific for that poison. It was through thethoughtful clinical <strong>and</strong> histological analysis of the Italiangroup from the dermatology department of Bologna thata diagnosis of ‘chloracne’ was made in several patientshaving been intoxicated in a holiday resort. For such adiagnosis, high clinical suspicion <strong>and</strong> specific laboratorymarkers are necessary, since important ecotoxicology issuesmay be involved.So how robust is the diagnosis of ‘chloracne’ in thiscase series from Passarini et al. [1] , a nd w he re a re t heguidelines for the minimum m<strong>and</strong>atory criteria for sucha diagnosis?T h e C l i n i c a l A s p e c t I s N o t D i a g n o s t i cFor the trained clinician, ‘chloracne’ is one of the differentialdiagnoses when an acneiform rash develops in apreviously non-acneic patient. Yet there has been so farno clinical sign specific for ‘chloracne’ that would not bepresent in some patients with either ‘spontaneous’ or exogenousacne. Most of the descriptions in the literatureeither on sporadic or epidemic cases do not provide uswith a robust red light that would trigger the specificecotoxicology diagnostic process.The current knowledge rather focuses on histology,which appears to provide a key robust, reproducible <strong>and</strong>specific sign, i.e. the disappearance of sebaceous gl<strong>and</strong>s.S k i n H i s t o l o g y I s M a n d a t o r y a n d P r ov i d e s St r o n gArguments for DiagnosisThere are two major signs that had been well describedbut perhaps not assigned their proper diagnosis weight. Itis our view that new unique constellation signs, both astructure addition <strong>and</strong> a structure loss, with the respectFax +41 61 306 12 34E-Mail karger@karger.chwww.karger.com© 2010 S. Karger AG, Basel1018–8665/10/2211–0023$26.00/0Accessible online at:www.karger.com/drmProf. Jean-Hilaire SauratSCAHT – Dermatotoxicologie, Centre Médical Universitaire1 rue Michel-ServetCH–1211 Genève 4 (Switzerl<strong>and</strong>)E-Mail Jean.Saurat@unige.ch
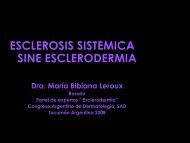
CICIOOCICICICIOCICICICICICICICI2,3,7,8-TCDD2,3,4,7,8-PeCDF3,3’,4,4’,5-PeCBOHNCICICIHOOFig. 1. Structure of known AhR agonists.FICZ = 6-formylindolo[3,2-b]carbazole;HCN = hexachloronaphthalene; PeCB =pentachlorobiphenyl; PeCDF = pentachlorodibenzofuran;TCDD = tetrachlorodibenzo-p -dioxin.NHFICZCICICI1,2,3,4,6,7-HCNOH OChrysin<strong>and</strong> conservation of most other features, are the specifichallmark of dioxin toxicity in the skin.The structure loss is of key importance. It is the disappearanceof the sebaceous gl<strong>and</strong>s. This has been repeatedlyindicated [2, 3] but perh aps not su f f ic ient ly emph a-sized as a key, almost diagnostic, feature. In human pathologythere is no other example where sebaceous gl<strong>and</strong>sdo vanish, which gives quite a weight to this observation.The term ‘chloracne’ is therefore a misleading misnomer:these lesions are not ‘acne’ because there is no sebaceousgl<strong>and</strong> hypertrophy, but rather the disappearance ofsebaceous gl<strong>and</strong>s [2, 3] .The structure addition is the presence of epidermalcysts, either superficial, with an open comedo-like aspect,or deeper in the dermis. The ontogeny, histologicallyspecific characters, focal expression of dioxin-metabolizingcytochrome P450 enzymes <strong>and</strong> dioxin storagepotential of these cysts are described elsewhere [Saurat etal., in preparation]. Based on the observations made in acase of massive dioxin poisoning [4] , we have proposed tocall these dioxin-induced cysts ‘metabolizing acquireddioxin-induced skin hamartomas’ (MADISH).The newly identified phenotypic attributes of theseMADISH [Saurat et al., in preparation], when confirmedin more than one paradigm case, may become a key diagnosticitem of dioxin exposure in humans.From this we can confirm that the case series fromPassarini et al. fulfills the currently accepted clinicopathologicalcriteria that should trigger – as the authorswrote – ‘environmental inquiry to detect potential contaminationby dioxins <strong>and</strong> polychlorinated biphenyls’.Unfortunately, despite all their efforts, they could notdemonstrate such a contamination. This is likely relatedto the complexity of the problem <strong>and</strong> the inappropriatenessof the current diagnostic procedures aiming at demonstratingharmful exposure of humans to dioxins.Where are the problems?D e m o n s t r a t i o n o f t h e Po i s o n : D i r e c t D o s i n g a n dBiological Signs of ExposureFacing a suspicion of ‘chloracne’ (better say MADISH)in a patient, the so-called chloracnegens can be assessedin serum <strong>and</strong> various tissues by direct chemical analysisor a biological assay [5] . The chemical analysis is performedby gas chromatography with high-resolutionmass spectrometry <strong>and</strong> gives the precise value for eachchloracnegen analyzed, usually 7 polychlorinated dibenzodioxins(PCDD) <strong>and</strong> 10 polychlorinated dibenzofurans(PCDF), then the global amount of chloracnegens isgiven as 2,3,7,8-tetrachlorodibenzo- p -dioxin equivalent(TEQ), using the 2,3,7,8-tetrachlorodibenzo- p -dioxinequivalent factor (TEF) for each analyte [4] :TEQ PCDD TEF PCDF TEFii i j jjSince these compounds are very lipophilic, the value isusually expressed as lipid weight, rather than as wetweight. This method requires a sophisticated equipment,a complex methodology, is very expensive <strong>and</strong>gives only the results for the particular chemicals thatwere ana lysed, i.e. it is possible to miss a chloracnegen24Dermatology 2010;221:23–26S au r at /S or g
AhRXAP2hsp90hsp90hsp90ArntAhRXAP2hsp90AhRArntFig. 2. Diagram illustrating the mode ofaction of dioxin-like compounds. Arnt =AhR nuclear translocator; hsp90 = 90-kDaheat shock protein; XAP2 = hepatitis B virusX-associated protein; XRE = xenobioticresponse element.CytoplasmNucleusAhRXREArntPhase I <strong>and</strong> II enzymesthat does not belong to the list of the chemicals analysed.However, the advantage of this method is the knowledgeof the nature of the chemicals participating in thesyndrome. The alternative method, dioxin-responsivechemically activated luciferase expression, is based onthe hypothesis that chloracnegens act via their bindingto the intracellular aryl hydrocarbon receptor (AhR)<strong>and</strong> the activation of DNA sequences called xenobioticresponse elements found in the promoter region of induciblegenes [6] ( f i g . 1 , 2 ). A s p e c i a l c e l lu l a r c on s t r uctionusing Photinus pyralis luciferase as the reportergene allows to assess the global activation of AhR lig<strong>and</strong>sapplied to the cells. This method has the advantageto give the global activation of the AhR pathway,expressed as TEQ, whatever the nature of all AhR lig<strong>and</strong>sinvolved in the syndrome. Thus, gas chromatography/high-resolutionmass spectrometry <strong>and</strong> dioxinresponsivechemically activated luciferase expressionare complementary.Once we get the results of chemical analysis <strong>and</strong>/orbiological assay for dioxin-like compounds in the serum,how to integrate them into the diagnosis? In other words,is there a minimum threshold value beyond which thecutaneous syndrome can be diagnosed? According toan IARC monograph on the evaluation of carcinogenicrisks to humans, where data on chloracne were gathered,no sign of chloracne was observed for serum TEQ valuesbelow 1,000 pg TEQ/g lipid weight, which correspondsto 50 times the level of that of the general population [7] ,whereas signs of chloracne were always found beyond10,000 pg TEQ/g lipid weight [8] . Thus, due to interindividualvariability of sensitivity to dioxin-like compounds,<strong>and</strong> maybe the fact that specialized structuresconcentrate these compounds, it is difficult to diagnosechloracne on the sole basis of serum TEQ values. Thisproblem is well illustrated by the report of Passarini et al.[1] , in which several cases of chloracne syndrome diagnosedon acceptable clinical <strong>and</strong> histological criteria hadserum TEQ values in the normal range, i.e. 5.39 pg TEQ/glipid weight. This highlights the need for other biomarkersof the cutaneous syndrome promoted by dioxin-likecompounds. A recent case of severe dioxin exposure [4]has provided important information on how modernmethods of analysing system biology markers in the organmay help solve this question [Saurat et al., in preparation].Analyses of sporadic cases such as those reported byPassarini et al. with such techniques are m<strong>and</strong>atory inorder to revisit the threshold of pathological dioxin-likeexposure in humans <strong>and</strong>, more precisely, better definethe ‘no-effect level’.<strong>Chloracne</strong>, a <strong>Misnomer</strong> Dermatology 2010;221:23–26 25
References1 Passarini B, Infusino SD, Kasapi E: <strong>Chloracne</strong>:still cause for concern. DermatologyDOI: 10.1159/000290694.2 Panteleyev AA, Thiel R, Wanner R, Zhang J,Roumak VS, Paus R, Neubert D, Henz BM,Rosenbach T: 2,3,7,8-Tetrachlorodibenzo- p -dioxin (TCCD) affects keratin 1 <strong>and</strong> keratin17 gene expression <strong>and</strong> differentially induceskeratinization in hairless mouse skin. J InvestDermatol 1997; 108: 330–335.3 Suskind RR: <strong>Chloracne</strong>, ‘the hallmark of dioxinintoxication’. Sc<strong>and</strong> J Work EnvironHealth 1985; 11: 165–171.4 Sorg O, Zennegg M, Schmid P, FedosyukR, Valikhnovskyi R, Gaide O, KniazevychV, Saurat JH: 2,3,7,8-Tetrachlorodibenzop-dioxin (TCCD) poisoning in Victor Yushchenko:identification <strong>and</strong> measurementof TCCD metabolites. Lancet 2009; 374:1179–1185.5 Taylor JS: Environmental chloracne: update<strong>and</strong> overview. Ann NY Acad Sci 1979; 320:295–307.6 Windal I, Denison MS, Birnbaum LS, VanWouwe N, Baeyens W, Goeyens L: Chemicallyactivated luciferase gene expression(CALUX) cell bioassay analysis for the estimationof dioxin-like activity: critical parametersof the CALUX procedure that impactassay results. Environ Sci Technol 2005;39 : 7357–7364.7 Fromme H, Albrecht M, Boehmer S, BuchnerK, Mayer R, Liebl B, Wittsiepe J, Bolte G:Intake <strong>and</strong> body burden of dioxin-like compoundsin Germany: the INES study. Chemosphere2009; 76: 1457–1463.8 IARC Monograph on the Evaluation of CarcinogenicRisks to Humans: PolychlorinatedDibenzo-Para-Dioxins <strong>and</strong> PolychlorinatedDibenzofurans. Lyon, IARC, 1997, p 69.26Dermatology 2010;221:23–26S au r at /S or g