New KY MMIS 837P Companion Guide - Kymmis.com
New KY MMIS 837P Companion Guide - Kymmis.com
New KY MMIS 837P Companion Guide - Kymmis.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
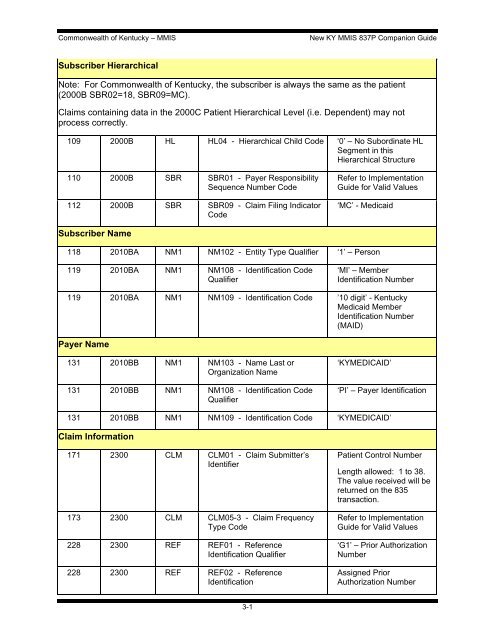
Commonwealth of Kentucky – <strong>MMIS</strong><strong>New</strong> <strong>KY</strong> <strong>MMIS</strong> <strong>837P</strong> <strong>Companion</strong> <strong>Guide</strong>Subscriber HierarchicalNote: For Commonwealth of Kentucky, the subscriber is always the same as the patient(2000B SBR02=18, SBR09=MC).Claims containing data in the 2000C Patient Hierarchical Level (i.e. Dependent) may notprocess correctly.109 2000B HL HL04 - Hierarchical Child Code ‘0’ – No Subordinate HLSegment in thisHierarchical Structure110 2000B SBR SBR01 - Payer ResponsibilitySequence Number Code112 2000B SBR SBR09 - Claim Filing IndicatorCodeRefer to Implementation<strong>Guide</strong> for Valid Values‘MC’ - MedicaidSubscriber Name118 2010BA NM1 NM102 - Entity Type Qualifier ‘1’ – Person119 2010BA NM1 NM108 - Identification CodeQualifier‘MI’ – MemberIdentification Number119 2010BA NM1 NM109 - Identification Code ’10 digit’ - KentuckyMedicaid MemberIdentification Number(MAID)Payer Name131 2010BB NM1 NM103 - Name Last orOrganization Name131 2010BB NM1 NM108 - Identification CodeQualifier‘<strong>KY</strong>MEDICAID’‘PI’ – Payer Identification131 2010BB NM1 NM109 - Identification Code ‘<strong>KY</strong>MEDICAID’Claim Information171 2300 CLM CLM01 - Claim Submitter’sIdentifier173 2300 CLM CLM05-3 - Claim FrequencyType Code228 2300 REF REF01 - ReferenceIdentification Qualifier228 2300 REF REF02 - ReferenceIdentificationPatient Control NumberLength allowed: 1 to 38.The value received will bereturned on the 835transaction.Refer to Implementation<strong>Guide</strong> for Valid Values‘G1’ – Prior AuthorizationNumberAssigned PriorAuthorization Number3-1