Treatment - The Journal of Clinical Endocrinology & Metabolism
Treatment - The Journal of Clinical Endocrinology & Metabolism
Treatment - The Journal of Clinical Endocrinology & Metabolism
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
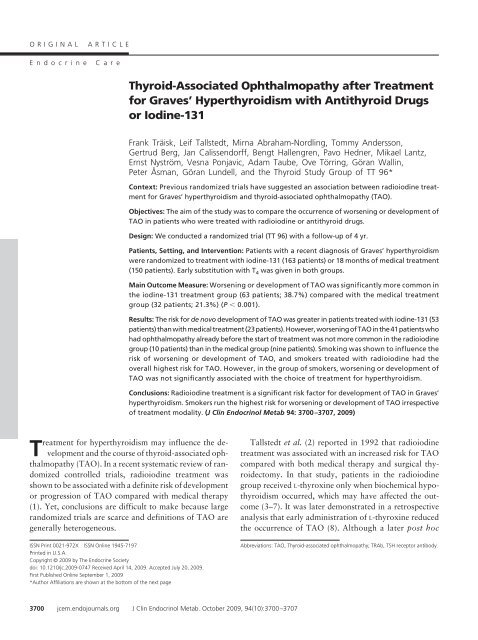
ORIGINAL ARTICLE<br />
Endocrine Care<br />
Thyroid-Associated Ophthalmopathy after <strong>Treatment</strong><br />
for Graves’ Hyperthyroidism with Antithyroid Drugs<br />
or Iodine-131<br />
Frank Träisk, Leif Tallstedt, Mirna Abraham-Nordling, Tommy Andersson,<br />
Gertrud Berg, Jan Calissendorff, Bengt Hallengren, Pavo Hedner, Mikael Lantz,<br />
Ernst Nyström, Vesna Ponjavic, Adam Taube, Ove Törring, Göran Wallin,<br />
Peter Åsman, Göran Lundell, and the Thyroid Study Group <strong>of</strong> TT 96*<br />
Context: Previous randomized trials have suggested an association between radioiodine treatment<br />
for Graves’ hyperthyroidism and thyroid-associated ophthalmopathy (TAO).<br />
Objectives: <strong>The</strong> aim <strong>of</strong> the study was to compare the occurrence <strong>of</strong> worsening or development <strong>of</strong><br />
TAO in patients who were treated with radioiodine or antithyroid drugs.<br />
Design: We conducted a randomized trial (TT 96) with a follow-up <strong>of</strong> 4 yr.<br />
Patients, Setting, and Intervention: Patients with a recent diagnosis <strong>of</strong> Graves’ hyperthyroidism<br />
were randomized to treatment with iodine-131 (163 patients) or 18 months <strong>of</strong> medical treatment<br />
(150 patients). Early substitution with T 4 was given in both groups.<br />
Main Outcome Measure: Worsening or development <strong>of</strong> TAO was significantly more common in<br />
the iodine-131 treatment group (63 patients; 38.7%) compared with the medical treatment<br />
group (32 patients; 21.3%) (P � 0.001).<br />
Results: <strong>The</strong> risk for de novo development <strong>of</strong> TAO was greater in patients treated with iodine-131 (53<br />
patients)thanwithmedicaltreatment(23patients).However,worsening<strong>of</strong>TAOinthe41patientswho<br />
had ophthalmopathy already before the start <strong>of</strong> treatment was not more common in the radioiodine<br />
group (10 patients) than in the medical group (nine patients). Smoking was shown to influence the<br />
risk <strong>of</strong> worsening or development <strong>of</strong> TAO, and smokers treated with radioiodine had the<br />
overall highest risk for TAO. However, in the group <strong>of</strong> smokers, worsening or development <strong>of</strong><br />
TAO was not significantly associated with the choice <strong>of</strong> treatment for hyperthyroidism.<br />
Conclusions: Radioiodine treatment is a significant risk factor for development <strong>of</strong> TAO in Graves’<br />
hyperthyroidism. Smokers run the highest risk for worsening or development <strong>of</strong> TAO irrespective<br />
<strong>of</strong> treatment modality. (J Clin Endocrinol Metab 94: 3700–3707, 2009)<br />
<strong>Treatment</strong> for hyperthyroidism may influence the development<br />
and the course <strong>of</strong> thyroid-associated ophthalmopathy<br />
(TAO). In a recent systematic review <strong>of</strong> randomized<br />
controlled trials, radioiodine treatment was<br />
shown to be associated with a definite risk <strong>of</strong> development<br />
or progression <strong>of</strong> TAO compared with medical therapy<br />
(1). Yet, conclusions are difficult to make because large<br />
randomized trials are scarce and definitions <strong>of</strong> TAO are<br />
generally heterogeneous.<br />
ISSN Print 0021-972X ISSN Online 1945-7197<br />
Printed in U.S.A.<br />
Copyright © 2009 by <strong>The</strong> Endocrine Society<br />
doi: 10.1210/jc.2009-0747 Received April 14, 2009. Accepted July 20, 2009.<br />
First Published Online September 1, 2009<br />
*Author Affiliations are shown at the bottom <strong>of</strong> the next page<br />
3700 jcem.endojournals.org J Clin Endocrinol Metab. October 2009, 94(10):3700–3707<br />
Tallstedt et al. (2) reported in 1992 that radioiodine<br />
treatment was associated with an increased risk for TAO<br />
compared with both medical therapy and surgical thyroidectomy.<br />
In that study, patients in the radioiodine<br />
group received L-thyroxine only when biochemical hypothyroidism<br />
occurred, which may have affected the outcome<br />
(3–7). It was later demonstrated in a retrospective<br />
analysis that early administration <strong>of</strong> L-thyroxine reduced<br />
the occurrence <strong>of</strong> TAO (8). Although a later post hoc<br />
Abbreviations: TAO, Thyroid-associated ophthalmopathy; TRAb, TSH receptor antibody.
J Clin Endocrinol Metab, October 2009, 94(10):3700–3707 jcem.endojournals.org 3701<br />
analysis did not show an association between TAO and<br />
posttherapy hypothyroidism (9), a new study in a similar<br />
population with early administration <strong>of</strong> L-thyroxine<br />
was strongly called for.<br />
<strong>The</strong> principal aim <strong>of</strong> this study was to compare radioiodine<br />
treatment and medical therapy for long-term worsening<br />
or development <strong>of</strong> TAO. Smoking and hypothyroidism<br />
as confounding risk factors were controlled for, and<br />
L-thyroxine supplementation was given early, i.e. at 2 wk<br />
after the initiation <strong>of</strong> treatment for hyperthyroidism in<br />
both arms.<br />
Patients and Methods<br />
Study design<br />
<strong>The</strong> study was designed as an open, randomized, prospective<br />
multicenter trial. Patients were randomized to radioiodine<br />
(group I) and medical treatment (group M) within each center<br />
(stratified randomization). Randomization was made in blocks<br />
over time and was performed by the Oncological Centre at the<br />
Karolinska University Hospital in Stockholm.<br />
<strong>The</strong> primary endpoint was the difference in the proportion <strong>of</strong><br />
patients with worsening or development <strong>of</strong> TAO during a 4-yr<br />
follow-up in the two groups (intention-to-treat analysis). A comparison<br />
(� � 0.05, two-tailed test) <strong>of</strong> the binomial proportions<br />
between two groups <strong>of</strong> 300 patients each would give more than<br />
90% probability (power) to detect a true difference <strong>of</strong> 10%.<br />
Power estimates were based on the results from the previous trial<br />
by Tallstedt et al. (2).<br />
Enrollment in the study (TT 96) started in May 1996. By<br />
the second half <strong>of</strong> 2002, it was obvious, however, that the<br />
inclusion rate was too slow to obtain the full number <strong>of</strong> patients<br />
within a reasonable period <strong>of</strong> time, and the study was<br />
closed in 2003. This meant that with the above specifications<br />
and the number <strong>of</strong> observations obtained so far (333 enrolled<br />
patients), the study had a power <strong>of</strong> about 70% at least. With<br />
the 4-yr clinical follow up, the study was terminated by the end<br />
<strong>of</strong> 2007.<br />
<strong>The</strong> study was approved by the ethics committee <strong>of</strong> the Karolinska<br />
Institute (Ref.: KI 96-096).<br />
Patients<br />
Inclusion criteria were as follows: age, 35–69 yr; symptomatic<br />
Graves’ hyperthyroidism; confirmation <strong>of</strong> the diagnosis by serum<br />
TSH (�0.1 mIU/liter) and T 3 and/or free T 4 (elevated), thyroid<br />
uptake <strong>of</strong> iodine-131, and radionuclide scans compatible with<br />
Graves’ disease, i.e. an even distribution <strong>of</strong> radionuclide. Furthermore,<br />
the activity <strong>of</strong> an orally administered dose <strong>of</strong> iodine-131<br />
(as calculated for the patient to give an absorbed radiation dose<br />
<strong>of</strong> 120 Gy) should not exceed 600 MBq, enabling the therapy to<br />
be given on an outpatient basis (see formula in Iodine-131<br />
section). Patients with a previous history <strong>of</strong> treatment with<br />
antithyroid drugs, iodine-131, or thyroid surgery were excluded<br />
as well as patients with severe TAO requiring treatment<br />
with corticosteroids at the time <strong>of</strong> inclusion. This was<br />
done because concomitant steroid treatment would limit the<br />
possibility to evaluate the effect <strong>of</strong> the treatment for Graves’<br />
disease on worsening or development <strong>of</strong> TAO. Additional<br />
exclusion criteria were: incipient toxic crisis, coronary heart<br />
disease, pregnancy, breast-feeding or pregnancy planned<br />
within the following 2 yr.<br />
<strong>The</strong> full number <strong>of</strong> patients that met the inclusion criteria is<br />
not known, but the reported cases were 482. A total <strong>of</strong> 333<br />
patients gave their informed consent to participate and were<br />
enrolled in the study. For ethical reasons, clinical data were not<br />
documented for the patients who did not wish to participate or<br />
did not meet the inclusion criteria.<br />
Of the 333 patients enrolled in the study, 313 were included<br />
in the study group: 150 in the medical therapy group, and 163<br />
in the radioiodine group (Table 1). <strong>The</strong> number <strong>of</strong> patients<br />
belonging to each center was: Gothenburg, 58; Lund, 40; Malmoe,<br />
73; and Stockholm, 142 patients, respectively. Twenty<br />
patients were excluded: one patient had an incorrect diagnosis<br />
(Hashimoto thyroiditis), 17 had no ophthalmological assessment<br />
at randomization, and two had no follow-up visits.<br />
<strong>The</strong>se excluded patients had an average age <strong>of</strong> 50.1 yr, the<br />
male/female ratio was 5/15, five <strong>of</strong> 18 were smokers, and two<br />
were missing data.<br />
<strong>The</strong> cumulative dropout (last observation carried forward)<br />
from the ophthalmological follow-up in group I and group M,<br />
respectively, was as follows: at 1 yr, 3 and 1%; at 2 yr, 6 and 3%;<br />
and at 3 yr, 10 and 9%, respectively. At 4 yr (i.e. after protocol<br />
for ophthalmological follow-up), 20% <strong>of</strong> the patients in both<br />
groups were still followed by ophthalmologists.<br />
<strong>Treatment</strong> for Graves’ hyperthyroidism<br />
Medical<br />
Methimazole was given 15 mg twice daily; at d 14, 50 �g <strong>of</strong><br />
L-thyroxine was added, and it was increased to 100 �g 2 wk later.<br />
At 6 wk, the dose <strong>of</strong> L-thyroxine was adjusted to normalize the<br />
levels <strong>of</strong> serum T 3 and free T 4 and to bring TSH to less than 0.4<br />
mIU/liter. A slightly elevated serum free T 4 was accepted up to<br />
20% above the upper normal limit.<br />
Beta-blockers were used for symptomatic treatment. Patients<br />
showing serious adverse reactions to methimazole received alternative<br />
treatment. Methimazole was replaced by 150 mg propylthiouracil<br />
three times daily in patients with minor adverse<br />
reactions.<br />
Antithyroid drug therapy was discontinued after 18 months<br />
with an additional month <strong>of</strong> L-thyroxine substitution <strong>of</strong> 100 �g<br />
daily, which thereafter was discontinued.<br />
Departments <strong>of</strong> <strong>Endocrinology</strong> (E.N.), Oncology (G.B.), and Ophthalmology (T.A.), Sahlgrenska University Hospital, SE-413 45 Gothenburg, Sweden; Departments <strong>of</strong> <strong>Endocrinology</strong> (P.H.)<br />
and Ophthalmology (V.P.), Lund University Hospital, SE-221 85 Lund, Sweden; Departments <strong>of</strong> <strong>Endocrinology</strong> (B.H., M.L.) and Ophthalmology (P.Å.), Malmoe University Hospital, SE-205<br />
02 Malmoe, Sweden; Department <strong>of</strong> Oncology, Radiumhemmet (G.L.), Department <strong>of</strong> Molecular Medicine and Surgery, Division <strong>of</strong> Surgery (G.W.), and Department <strong>of</strong> <strong>Endocrinology</strong><br />
(J.C.), Karolinska University Hospital, Karolinska Institute, SE-141 86 Stockholm, Sweden; Department <strong>of</strong> <strong>Clinical</strong> Neurosciences (L.T., F.T.), St. Erik Eye Hospital, Karolinska Institute, SE-112<br />
82 Stockholm, Sweden; Department <strong>of</strong> <strong>Clinical</strong> Research and Education, Karolinska Institute and Department <strong>of</strong> Internal Medicine, Division <strong>of</strong> <strong>Endocrinology</strong>, (O.T.), Södersjukhuset, SE-118<br />
83 77 Stockholm, Sweden; Department <strong>of</strong> <strong>Clinical</strong> Sciences, Division <strong>of</strong> Surgery (M.A.-N.), Danderyd Hospital, Karolinska Institute, SE-171 77 Stockholm, Sweden; and Department <strong>of</strong><br />
Information Science (A.T.), University <strong>of</strong> Uppsala, SE-751 20 Uppsala, Sweden
3702 Träisk et al. TAO after Antithyroid Drug or Iodine-131 <strong>Treatment</strong> J Clin Endocrinol Metab, October 2009, 94(10):3700–3707<br />
TABLE 1. Characteristics <strong>of</strong> patients randomized to<br />
treatment with iodine-131 or antithyroid drugs<br />
Characteristics <strong>of</strong><br />
patients before start <strong>of</strong><br />
treatment Group I Group M<br />
n 163 150<br />
Age (yr) 51 (SD, 8) 50(SD, 8)<br />
Age range (yr) 36–68 35–69<br />
Female gender (patients) 141 (87%) 137 (91%)<br />
Weight (kg) 65 (SD, 12)/160 a<br />
67 (SD, 13)/145 a<br />
Previous smoking (patients) 52 (32%) 39 (27%)/146 a<br />
Current smoking (patients) 59 (36%) 62 (42%)/148 a<br />
No. <strong>of</strong> cigarettes/day 13 (SD, 10) 12 (SD, 7)<br />
No TRAb (patients) 10 (6%) 11 (7%)<br />
Estimated pretreatment<br />
duration <strong>of</strong><br />
hyperthyroidism<br />
(months)<br />
Radioiodine uptake at<br />
24h(%)<br />
64 (SD, 11)/162 a<br />
Thyroid volume<br />
62 (SD, 11)<br />
�30 g (patients) 29 (18%) 35 (24%)<br />
30–39 g (patients) 69 (42%) 53 (36%)<br />
�40 g (patients) 65 (40%) 58 (39%)<br />
TAO—present (patients) 22 (13%) 19 (13%)<br />
Only eyelid<br />
retraction—present<br />
(patients)<br />
31 (19%) 28 (19%)<br />
TAO and retraction—absent<br />
(patients)<br />
110 (67%) 103 (69%)<br />
Proptosis right eye (mm) 16 (SD, 2) 16(SD, 2)<br />
Proptosis left eye (mm)<br />
Patients with TAO before<br />
start <strong>of</strong> treatment<br />
16 (SD, 2) 16(SD, 2)<br />
n 22 19<br />
Proptosis right eye (mm) 18 (SD, 2) 18(SD, 2)<br />
Proptosis left eye (mm) 17 (SD, 2) 17(SD, 3)<br />
TAO activity index (see<br />
Appendix I)<br />
2.3 (SD, 1.7) 2.0 (SD, 0.0)<br />
Impaired eye motility<br />
(patients)<br />
7 1<br />
Eyelid retraction (patients) 14 8<br />
Data includes age, sex, smoking habits, duration <strong>of</strong> hyperthyroidism<br />
(the patient’s own assessment before randomization), TRAb,<br />
radioiodine uptake at 24 h, thyroid volume, and TAO in the patients<br />
who were randomized to iodine-131 or medical treatment for Graves’<br />
hyperthyroidism. No patient in either group had optic neuropathy or<br />
corneal ulcer. Differences between the two groups were<br />
nonsignificant. Data on thyroid volume were missing in four patients in<br />
the medical treatment group.<br />
a<br />
Number <strong>of</strong> available recordings, if data were missing.<br />
5(SD, 4)/162 a<br />
6(SD, 5)/148 a<br />
Iodine-131<br />
Beta-blockers were used as pretreatment to radioiodine. <strong>The</strong><br />
intention was to give one dose <strong>of</strong> radioactive iodine, aiming for<br />
an estimated absorbed radiation dose in the thyroid gland <strong>of</strong> 120<br />
Gy. <strong>The</strong> administered activity was calculated using the following<br />
formula (10): Activity (MBq) � [23.4 � thyroid mass (grams) �<br />
120 (Gy)]/[estimated uptake (0 h; %) � effective half-life (days)].<br />
<strong>The</strong> thyroid mass was assessed by thyroid scintigraphy and by<br />
palpation. Reference models <strong>of</strong> a thyroid gland were used to aid<br />
the assessment (30, 40, 50, and 60 ml). <strong>The</strong> half-life <strong>of</strong> iodine-<br />
131 and the estimated thyroid uptake at zero hours were calculated<br />
from the initial 24-h thyroid iodine uptake and a new uptake<br />
test 4 to 9 d later, i.e. the same day the radioiodine therapy<br />
was given. L-Thyroxine substitution was administered with the<br />
same type <strong>of</strong> regimen as used in Group M.<br />
Follow-up by thyroidologist (endocrinologist or<br />
oncologist)<br />
<strong>Treatment</strong> for hyperthyroidism was monitored by clinical assessments<br />
and laboratory evaluations <strong>of</strong> the serum T 3, free T 4,<br />
and TSH levels as follows: at 6 and 10 wk and after 6, 9, 12, 15,<br />
18, 24, 36, and 48 months in both groups, and in group I also at<br />
4 months. Serum TSH receptor antibody (TRAb) and thyroid<br />
peroxidase antibody (optional) were analyzed at randomization,<br />
6, 12, 18, 24, 36, and 48 months in both groups. Smoking habits<br />
and body weight were also registered.<br />
At each visit, an ophthalmological assessment was done by<br />
the physician. If at any time TAO developed or deteriorated, the<br />
patients were referred to the ophthalmologist for additional eye<br />
examinations.<br />
Follow-up by ophthalmologist<br />
Within the first 2 wk after enrollment, all patients were seen<br />
by an ophthalmologist, and thereafter they were seen as part <strong>of</strong><br />
the study protocol at 3, 12, 24, and 36 months. After 36 months,<br />
additional assessments were performed at the eye clinic upon<br />
referral by the thyroidologists or if the patients were followed<br />
because <strong>of</strong> established TAO. Also, during the 4-yr follow-up,<br />
patients with active TAO had eye assessments by ophthalmologists<br />
every 6 wk until the condition had markedly improved. At<br />
each visit at the eye clinic, visual acuity, proptosis, eyelid retraction,<br />
eyelid swelling, chemosis, conjunctival redness, impairment<br />
<strong>of</strong> the eye movements, corneal ulceration, and optic nerve involvement<br />
were documented (Appendix I, published as supplemental<br />
data on <strong>The</strong> Endocrine Society’s <strong>Journal</strong>s Online web site<br />
at http://jcem.endojournals.org). Eyelid retraction alone was not<br />
classified as TAO. Within each center, the majority <strong>of</strong> patients<br />
were followed by the same ophthalmologist throughout the<br />
study.<br />
Change <strong>of</strong> TAO, with and without set criteria<br />
At each visit, the ophthalmologists determined whether TAO<br />
had worsened/developed, improved, or was unchanged. Here,<br />
both the observed changes in activity and severity <strong>of</strong> TAO and<br />
the reported eye symptoms were taken into account. However,<br />
because the observed changes in TAO were sometimes minor and<br />
transient, a post hoc validation was performed <strong>of</strong> the events<br />
defined as worsening or development, improvement, and no<br />
change <strong>of</strong> TAO. For this, modified criteria were chosen from a<br />
trial where similar outcomes had previously been compared (11).<br />
For the set criteria (worsening or development and improvement<br />
<strong>of</strong> TAO), two <strong>of</strong> the following four decisive factors were required<br />
(compared with baseline data): 1) change in exophthalmometry<br />
readings <strong>of</strong> 2 mm or more; 2) improvement or deterioration <strong>of</strong><br />
the patient’s eye movements between the four scoring levels (Appendix<br />
I: no impairment, clearly impaired, diplopia in the primary<br />
position, fixation <strong>of</strong> the globe); 3) changes <strong>of</strong> visual acuity<br />
caused by optic neuropathy; and 4) changes in two <strong>of</strong> the three<br />
TAO activity measures (chemosis, eyelid edema, and conjunctival<br />
redness). <strong>The</strong> patients who did not meet the criteria <strong>of</strong> improvement<br />
or worsening or development <strong>of</strong> TAO were referred<br />
to as having no change <strong>of</strong> TAO. <strong>The</strong> outcome for worsening or<br />
development <strong>of</strong> TAO according to set criteria are reported separately<br />
in Results.
J Clin Endocrinol Metab, October 2009, 94(10):3700–3707 jcem.endojournals.org 3703<br />
Laboratory analysis<br />
<strong>The</strong> laboratory analyses were performed at the different study<br />
centers. <strong>The</strong> reference intervals as well as the analysis methodology<br />
were consequently different. Also, the methods changed<br />
during the time <strong>of</strong> the study. <strong>The</strong> lower reference limit for free T 4<br />
at randomization was 8–11.7 pmol/liter, and the upper limit was<br />
18–28 pmol/liter. Disregarding the fact that different methods<br />
had been used, the levels <strong>of</strong> serum free T 4 at randomization were<br />
not different in the two groups [in group I, 56.8 (SD 18.0) pmol/<br />
liter; and in group M, 56.4 (SD 19.2) pmol/liter].<br />
Statistical analysis<br />
<strong>The</strong> primary endpoint hypothesis was tested by means <strong>of</strong> a � 2<br />
test. <strong>The</strong> influence <strong>of</strong> possible prognostic factors on the time to<br />
TAO was investigated with Cox regression analysis. <strong>The</strong> development<br />
within the various subgroups was illustrated by means <strong>of</strong><br />
Kaplan Meier technique. P values were two-sided, and P � 0.05<br />
was considered significant. <strong>The</strong> MEDLOG s<strong>of</strong>tware system (release<br />
2008-2; Information Analysis Corp., MEDLOG Systems,<br />
Crystal Bay, NV) was used for storage <strong>of</strong> data and statistical<br />
analysis.<br />
Results<br />
<strong>The</strong> two treatment groups were similar for the characteristics<br />
listed in Table 1. Among the patients randomized for<br />
iodine-131, two patients relapsed and had thyroid surgery<br />
and further radioiodine treatment, respectively. Among<br />
the patients randomized for and accounted for medical<br />
treatment, 12 patients experienced adverse events that led<br />
to change <strong>of</strong> therapy to radioiodine. Furthermore, 33<br />
(22%) <strong>of</strong> the patients randomized for medical treatment<br />
relapsed. Of those, five were treated with surgery, 25 with<br />
radioiodine, and three with further medical therapy.<br />
Among the patients in group M who received iodine-131<br />
as treatment for relapse, only one subsequently developed<br />
TAO (see Appendix II). Early administration <strong>of</strong> L-thyroxine<br />
after radioiodine treatment was not associated with<br />
arrhythmia or serious adverse effects.<br />
In patients randomized to treatment with radioiodine,<br />
a significantly higher cumulative incidence <strong>of</strong> worsening<br />
or development <strong>of</strong> TAO (63 patients; 38.7%) was observed<br />
compared with the group randomized to antithyroid<br />
drugs (32 patients; 21.3%; � 2 , P � 0.001). <strong>The</strong> log<br />
rank Mantel-Haenszel test for equality <strong>of</strong> the curves for<br />
worsening or development <strong>of</strong> TAO confirmed this difference<br />
(P � 0.001; see Fig. 2A).<br />
In the patients with TAO already at the first visit (13.1%),<br />
the overall course <strong>of</strong> the ophthalmopathy was not significantly<br />
affected by the choice <strong>of</strong> treatment, but de novo development<br />
<strong>of</strong> TAO was significantly more frequent in group<br />
I (Fig. 1; P � 0.001). Of the 41 patients with preexisting<br />
TAO, 10 patients in each group improved; one patient in<br />
group I and two patients in group M had initial improvement<br />
Number <strong>of</strong> patients<br />
60<br />
50<br />
40<br />
30<br />
20<br />
10<br />
0<br />
10<br />
9<br />
with a subsequent deterioration. Two patients in group I had<br />
no change; nine and seven patients deteriorated in groups I<br />
and M, respectively. If patients with only eyelid retraction<br />
were included in the group with preexisting TAO, a Mantel-<br />
Haenszel comparison between the treatment groups still<br />
yielded a nonsignificant difference for worsening (P �<br />
0.24) and an increased risk for de novo development <strong>of</strong><br />
TAO (P � 0.001).<br />
Independent <strong>of</strong> the choice <strong>of</strong> treatment, smoking increased<br />
the risk <strong>of</strong> worsening or development <strong>of</strong> TAO (P �<br />
0.001; Fig. 2B). However, in smokers the choice <strong>of</strong> treatment<br />
for Graves’ hyperthyroidism did not have a significant<br />
impact on the outcome (P � 0.38; Fig. 2D), in contrast to<br />
nonsmokers where iodine-131 treatment significantly increased<br />
the risk <strong>of</strong> worsening or development <strong>of</strong> TAO (P �<br />
0.001; Fig. 2C).<br />
In a Cox regression analysis, both the choice <strong>of</strong> therapy<br />
and smoking habits were shown to influence the risk <strong>of</strong><br />
worsening or development <strong>of</strong> TAO (Table 2). <strong>The</strong> effect <strong>of</strong><br />
therapy for hyperthyroidism on the time to worsening or<br />
development <strong>of</strong> TAO was significantly different in the<br />
group <strong>of</strong> smokers and nonsmokers (P � 0.01). In the Cox<br />
regression statistics, this was analyzed by using the interaction<br />
term iodine-131 therapy in smokers (Table 2). <strong>The</strong><br />
differences are demonstrated graphically in Fig. 2, C and D.<br />
<strong>The</strong> associations between TAO and pretreatment laboratory<br />
levels <strong>of</strong> thyroid hormone could merely be estimated,<br />
because the methods and reference intervals differed<br />
between the centers. However, taking these limitations into<br />
consideration, the Cox regression analysis suggested that<br />
higher free T 4 levels were associated with an increased risk<br />
for TAO (Table 2).<br />
In the post hoc analysis, using the set criteria for the<br />
change in TAO, worsening or development <strong>of</strong> TAO was<br />
also found to occur more <strong>of</strong>ten in group I (40 patients;<br />
25%) than in group M (16 patients; 11%; P � 0.002). <strong>The</strong><br />
Mantel-Haenszel comparisons between different groups<br />
as shown in Fig. 2, A–D, showed comparable results. <strong>The</strong><br />
53<br />
23<br />
worse pre-existing new development<br />
Iodine-131<br />
Medical<br />
FIG. 1. Number <strong>of</strong> patients with worsening <strong>of</strong> preexisting TAO [10 <strong>of</strong><br />
22 patients (45%) in group I; and nine <strong>of</strong> 19 patients (47%) in group<br />
M] and de novo development <strong>of</strong> TAO [53 <strong>of</strong> 141 patients (38%) in<br />
group I; and 23 <strong>of</strong> 131 patients (18%) in group M] at any time during<br />
follow-up.
3704 Träisk et al. TAO after Antithyroid Drug or Iodine-131 <strong>Treatment</strong> J Clin Endocrinol Metab, October 2009, 94(10):3700–3707<br />
A B<br />
Probability <strong>of</strong> W/D <strong>of</strong> TAO<br />
1.0<br />
0.9<br />
0.8<br />
0.7<br />
0.6<br />
0.5<br />
0.4<br />
0.3<br />
0.2<br />
0.1<br />
0<br />
0<br />
^ ^<br />
1<br />
^ 2<br />
Years after start <strong>of</strong> therapy<br />
^ 3<br />
corresponding significance level for the comparisons in<br />
Fig. 2A was P � 0.002; Fig. 2B, P � 0.009; Fig. 2C, P �<br />
0.001; and Fig. 2D, P � 0.44. <strong>The</strong> Cox regression results<br />
for four risk factors when using the set criteria for TAO for<br />
worsening or development <strong>of</strong> TAO are shown in Table 2.<br />
Patients with TAO at randomization had the following<br />
change during the time <strong>of</strong> follow-up according to the set<br />
criteria: worsening <strong>of</strong> TAO in five and four patients, improvement<br />
in seven and zero patients, and no change in 10<br />
and 15 patients in group I and group M, respectively.<br />
TABLE 2. Cox regression analysis for four possible risk<br />
factors regarding worsening or development <strong>of</strong> TAO<br />
with and without set criteria for worsening or<br />
development <strong>of</strong> TAO<br />
Covariate<br />
Odds ratio<br />
(95% CI) P value<br />
<strong>The</strong>rapy (iodine-131 vs.<br />
medical therapy)<br />
4.05 (1.95 to 8.43) �0.001<br />
Set criteria 7.72 (2.31 to 25.75) �0.001<br />
Current smoking (yes vs. no) 5.20 (2.35 to 11.53) �0.001<br />
Set criteria 9.80 (2.75 to 34.90) �0.001<br />
Iodine-131 therapy in<br />
smokers (smokers<br />
treated with iodine-131<br />
vs. all others)<br />
0.29 (0.11 to 0.74) 0.010<br />
Set criteria 0.14 (0.04 to 0.60) 0.007<br />
Serum free T4 (pmol/liter) 1.01 (1.00 to 1.03) 0.012<br />
Set criteria 1.03 (1.01 to 1.04) �0.001<br />
CI, Confidence interval.<br />
p
J Clin Endocrinol Metab, October 2009, 94(10):3700–3707 jcem.endojournals.org 3705<br />
the follow-up period, but one patient was subject to orbital<br />
decompression surgery (in group I). No significant<br />
differences were found between the different centers for<br />
worsening or development <strong>of</strong> TAO or the severity <strong>of</strong> hyperthyroidism<br />
using the Cox test (results not shown).<br />
During the first 12 months <strong>of</strong> follow-up, 87.7% <strong>of</strong> the<br />
patients in group I and 86.0% in group M had no recorded<br />
serum TSH above 4.5 mIU/liter. Worsening or development<br />
<strong>of</strong> TAO was in a Mantel-Haenszel analysis not found<br />
to be more frequent in the patients who at any occasion<br />
had serum TSH above 4.5 mIU/liter (P � 0.49).<br />
Discussion<br />
Radioiodine treatment was shown to be associated with a<br />
higher cumulative incidence <strong>of</strong> worsening or development<br />
<strong>of</strong> TAO compared with medical therapy. In this study,<br />
L-thyroxine therapy was introduced early in both treatment<br />
groups to avoid hypothyroidism, which was in contrast<br />
to the previous report by Tallstedt et al. (2). <strong>The</strong> time<br />
for active follow-up by ophthalmologists was longer in the<br />
present study compared with the two previous large prospective<br />
randomized trials where radioiodine and medical<br />
therapy were compared (2, 11). In the present study, the<br />
proportion <strong>of</strong> worsening or development <strong>of</strong> TAO after<br />
1-yr follow-up was 31% in the iodine-131 group and 16%<br />
in the medical treatment group. <strong>The</strong> corresponding figures<br />
were similar in Tallstedt et al. (2) (33 and 10%, respectively)<br />
but lower in Bartalena et al. (11) (15 and 3%,<br />
respectively).<br />
In contrast to the results in Bartalena et al. (11), the<br />
differences in the ophthalmological outcome between the<br />
treatment groups in the present study were explained by de<br />
novo development <strong>of</strong> TAO and not by worsening <strong>of</strong> preexisting<br />
TAO. This may partly be explained by differences<br />
in the study designs. In this study and that by Tallstedt et<br />
al. (2), only newly diagnosed patients with Graves’ disease<br />
were randomized, whereas in the study by Bartalena et al.<br />
(11), 70% <strong>of</strong> all patients had a previous history <strong>of</strong> treatment<br />
<strong>of</strong> Graves’ disease. Also, in the latter study a 3-month<br />
course <strong>of</strong> antithyroid drugs was part <strong>of</strong> the protocol for<br />
those treated with radioiodine. In the present study and in<br />
that by Tallstedt et al. (2), TAO was present at randomization<br />
in 13% <strong>of</strong> the patients, whereas this number was<br />
50% in the study by Bartalena et al. (11). <strong>The</strong> discrepancy<br />
in incidence data between this and previous studies may<br />
also be explained by patient characteristics, sample size,<br />
treatment practice, the assessment <strong>of</strong> TAO, and thresholds<br />
for introducing steroid treatment.<br />
It is well known that radioiodine treatment leads to a<br />
prolonged release <strong>of</strong> TRAb and thyroid peroxidase antibody,<br />
but the mechanism for this is not known. <strong>The</strong> rise in<br />
serum antibodies against thyroid antigens after radioiodine<br />
treatment mirrors an immune reaction in the thyroid<br />
that may be the triggering event for the orbital inflammation,<br />
assuming that the thyroid and orbital tissues share<br />
resembling antigens (9, 12–17).<br />
To the patients who were randomized to medical therapy,<br />
L-thyroxine was given early by routine to achieve a<br />
stable thyroid function and because previous studies have<br />
shown that a more severe and unstable Graves’ disease is<br />
a common denominator for the development <strong>of</strong> TAO (2,<br />
9). Furthermore, the potential benefits on the immune system<br />
by antithyroid drugs need to be pointed out (18–21).<br />
If applicable for the present, such influences on the immune<br />
system may have contributed to the lower frequency<br />
<strong>of</strong> worsening or development <strong>of</strong> TAO that was observed<br />
in the medically treated group.<br />
Smoking is an established risk factor for TAO, and this<br />
relationship was also confirmed in this study (22, 23).<br />
Interestingly, in the group <strong>of</strong> smokers, worsening or development<br />
<strong>of</strong> TAO was not significantly associated with<br />
the choice <strong>of</strong> treatment for hyperthyroidism. This infers<br />
that radioiodine may be an independent risk factor for<br />
TAO and that this treatment-related risk factor is not as<br />
strong in smokers as in nonsmokers. However, because<br />
smokers who received radioiodine had the overall highest<br />
risk <strong>of</strong> TAO, one might argue that radioiodine should be<br />
avoided in smokers or be given together with immunesuppressive<br />
prophylaxis.<br />
Prophylactic steroid treatment has been shown to significantly<br />
reduce the risk for TAO in radioiodine-treated<br />
patients (11, 24). However, there have been discussions<br />
about whether the eye changes observed after radioiodine<br />
treatment warrant the use <strong>of</strong> prophylactic steroid treatment<br />
as a rule (25–27). In this decision making, there is to<br />
date no solid agreement about what risk factors should be<br />
taken into account. Smoking habits and preexisting TAO<br />
should probably be regarded, but presumably other possible<br />
risk factors should also be considered, e.g. pretreatment<br />
serum T 3 and antithyroid antibodies (28, 29). <strong>The</strong><br />
high proportion <strong>of</strong> de novo development <strong>of</strong> TAO in the<br />
iodine-131 group implies that other factors besides clinically<br />
apparent preexisting TAO should be considered in<br />
the decision making regarding steroid prophylaxis in patients<br />
who are treated for newly diagnosed Graves’<br />
hyperthyroidism.<br />
This present trial has both strengths and limitations.<br />
<strong>The</strong> prospective randomized design, although open-label,<br />
and the extensive follow-up time by both thyroidologists<br />
and ophthalmologists strengthens the observations. Even<br />
if the final study group did not meet the requisite <strong>of</strong> the<br />
trial, the number <strong>of</strong> 313 patients makes this trial one <strong>of</strong> the<br />
largest on the issue. Surgery was not included as a third
3706 Träisk et al. TAO after Antithyroid Drug or Iodine-131 <strong>Treatment</strong> J Clin Endocrinol Metab, October 2009, 94(10):3700–3707<br />
treatment, which was reasonable because the ophthalmological<br />
outcome after surgery and medical therapy did not<br />
differ significantly in the earlier study by Tallstedt et al.<br />
(2). <strong>The</strong> inclusion <strong>of</strong> patients aged 35–69 yr may limit<br />
generalization <strong>of</strong> the results to other age groups. Changes<br />
<strong>of</strong> TAO (improvement, worsening, de novo development)<br />
were initially determined by clinical observations, as opposed<br />
to preset criteria. Validation <strong>of</strong> the event <strong>of</strong> worsening<br />
or development <strong>of</strong> TAO by the use <strong>of</strong> set criteria for<br />
change in s<strong>of</strong>t tissue signs, eye motility, vision, and exophthalmos<br />
confirmed the results and hence gives strength<br />
to our conclusions. Also, the data on TAO severity that by<br />
nature is less likely to be biased and the use <strong>of</strong> corticosteroids,<br />
which was more frequent in the iodine-131 group,<br />
provides evidence that the observations were clinically<br />
relevant.<br />
<strong>The</strong> proportion <strong>of</strong> patients with relapse <strong>of</strong> Graves’ disease<br />
after medical treatment was relatively low. This may<br />
partly be explained by the exclusion <strong>of</strong> patients younger<br />
than 35 yr and those with large goiters and TAO that<br />
required corticosteroid treatment already at the start <strong>of</strong><br />
the trial. In the current study, relapse after medical treatment<br />
that was treated with iodine-131 was not associated<br />
with worsening or development <strong>of</strong> TAO.<br />
In summary, this study confirms an association between<br />
radioiodine treatment and TAO and between<br />
smoking and TAO. A watchful follow-up for development<br />
<strong>of</strong> TAO after iodine-131 treatment is important,<br />
but clinically observed mild-moderate TAO at diagnosis<br />
<strong>of</strong> Graves’ disease might not be critical for the choice<br />
<strong>of</strong> treatment for hyperthyroidism. Smoking habits should<br />
be considered in the decision making for treatment. Smokers<br />
who were treated with radioiodine had the overall<br />
highest risk for TAO, but the risk for TAO associated with<br />
radioiodine treatment was not significant compared with<br />
medical treatment in the group <strong>of</strong> patients who smoked.<br />
More studies are called for to unveil additional risk factors<br />
for TAO.<br />
Acknowledgments<br />
We thank Elisabeth Bjurstedt at the Department <strong>of</strong> Oncology,<br />
Radiumhemmet, for secretarial help. We also thank the Karolinska<br />
Institute, the staff <strong>of</strong> the Oncology Center and the Karolinska University<br />
Hospital, and St. Erik Eye Research Foundation.<br />
<strong>The</strong> Thyroid Study Group <strong>of</strong> the TT 96 trial is represented<br />
by the authors listed above and the following collaborators:<br />
G. Lindstedt from the Department <strong>of</strong> <strong>Clinical</strong> Chemistry,<br />
Sahlgrenska University Hospital, Gothenburg; A. Michanek<br />
from the Department <strong>of</strong> Oncology, Sahlgrenska University<br />
Hospital, Gothenburg; K. Norrsell from the Department <strong>of</strong><br />
Ophthalmology, Sahlgrenska University Hospital, Gothenburg;<br />
S. Valdemarsson from the Department <strong>of</strong> <strong>Endocrinology</strong>, Lund<br />
University Hospital; M. Garkavij, J. Tennvall, and H. Widmark<br />
from the Department <strong>of</strong> Oncology, Lund University Hospital; G.<br />
Stigmar from the Department <strong>of</strong> Ophthalmology, Lund University<br />
Hospital; Å. Arwidi and G. Bjelkengren from the Department<br />
<strong>of</strong> Oncology, Malmoe University Hospital; B. Hemdahl<br />
and H. Jönsson from the Department <strong>of</strong> Radiophysics, Malmoe<br />
University Hospital; C. Becker from the Department <strong>of</strong> <strong>Clinical</strong><br />
Chemistry, Malmoe University Hospital; B. Freyschuss, J.<br />
H<strong>of</strong>fstedt, O. Tullgren, H. Wahrenberg, and A. Wennlund<br />
from the Department <strong>of</strong> <strong>Endocrinology</strong>, Karolinska University<br />
Hospital (Huddinge), Stockholm; S. Röjdmark, M. Sääf, and M.<br />
Thorén from the Department <strong>of</strong> <strong>Endocrinology</strong>, Karolinska<br />
University Hospital (Solna), Stockholm; B. Hamberger from<br />
the Department <strong>of</strong> Surgery, Karolinska University Hospital,<br />
Stockholm; and H. Blomgren, C. Hilding, and A.-L. Hjelm<br />
Skog from the Department <strong>of</strong> Oncology, Karolinska University<br />
Hospital, Stockholm.<br />
Address all correspondence and requests for reprints to: Frank<br />
Träisk, M.D., Ph.D., Department <strong>of</strong> <strong>Clinical</strong> Neurosciences, Karolinska<br />
Institute, St. Erik Eye Hospital, Polhemsg. 50, SE-11282,<br />
Stockholm, Sweden. E-mail: frank.traisk@sankterik.se.<br />
This trial was planned in association with the Medical Council<br />
for Research (Mediciska Forskningsrådet). Nycomed contributed<br />
with funding for secretarial assistance.<br />
Disclosure Summary: <strong>The</strong> authors have no conflicts <strong>of</strong> interest.<br />
References<br />
1. Acharya SH, Avenell A, Philip S, Burr J, Bevan JS, Abraham P 2008<br />
Radioiodine therapy for Graves’ disease and the effect on ophthalmopathy—a<br />
systematic review. Clin Endocrinol (Oxf) 69:943–950<br />
2. Tallstedt L, Lundell G, Tørring O, Wallin G, Ljunggren JG,<br />
Blomgren H, Taube A 1992 Occurrence <strong>of</strong> ophthalmopathy after<br />
treatment for Graves’ hyperthyroidism. <strong>The</strong> Thyroid Study Group.<br />
N Engl J Med 326:1733–1738<br />
3. Almqvist S, Algvere P 1972 Hypothyroidism in progressive ophthalmopathy<br />
<strong>of</strong> Graves’ disease. Acta Ophthalmol (Copenh) 50:<br />
761–770<br />
4. Sjöberg HE, Sääf M, Boström L, Lundell G, Tallstedt L 1989 Observations<br />
on progression periods in Graves’ ophthalmopathy. Acta<br />
Endocrinol (Copenh) 121(Suppl 2): 179–181<br />
5. Karlsson FA, Dahlberg PA, Jansson R, Westermark K, Enoksson<br />
P 1989 Importance <strong>of</strong> TSH receptor activation in the development<br />
<strong>of</strong> severe endocrine ophthalmopathy. Acta Endocrinol (Copenh)<br />
121(Suppl 2):132–141<br />
6. Kung AW, Yau CC, Cheng A 1994 <strong>The</strong> incidence <strong>of</strong> ophthalmopathy<br />
after radioiodine therapy for Graves’ disease: prognostic factors<br />
and the role <strong>of</strong> methimazole. J Clin Endocrinol Metab 79:542–<br />
546<br />
7. Gorman CA 1995 Radioiodine therapy does not aggravate Graves’<br />
ophthalmopathy. J Clin Endocrinol Metab 80:340–342<br />
8. Tallstedt L, Lundell G, Blomgren H, Bring J 1994 Does early administration<br />
<strong>of</strong> thyroxine reduce the development <strong>of</strong> Graves’ ophthalmopathy<br />
after radioiodine treatment? Eur J Endocrinol 130:<br />
494–497<br />
9. Törring O, Tallstedt L, Wallin G, Lundell G, Ljunggren JG, Taube<br />
A, Sääf M, Hamberger B 1996 Graves’ hyperthyroidism: treatment<br />
with antithyroid drugs, surgery, or radioiodine—a prospective, randomized<br />
study. Thyroid Study Group. J Clin Endocrinol Metab 81:<br />
2986–2993<br />
10. Berg GE, Michanek AM, Holmberg EC, Fink M 1996 Iodine-131
J Clin Endocrinol Metab, October 2009, 94(10):3700–3707 jcem.endojournals.org 3707<br />
treatment <strong>of</strong> hyperthyroidism: significance <strong>of</strong> effective half-life measurements.<br />
J Nucl Med 37:228–232<br />
11. Bartalena L, Marcocci C, Bogazzi F, Manetti L, Tanda ML,<br />
Dell’Unto E, Bruno-Bossio G, Nardi M, Bartolomei MP, Lepri A,<br />
Rossi G, Martino E, Pinchera A 1998 Relation between therapy for<br />
hyperthyroidism and the course <strong>of</strong> Graves’ ophthalmopathy. N Engl<br />
J Med 338:73–78<br />
12. Gamstedt A, Wadman B, Karlsson A 1986 Methimazole, but not<br />
Betamethasone, prevents iodine-131 treatment-induced rises in thyrotropin<br />
receptor autoantibodies in hyperthyroid Graves’ disease.<br />
J Clin Endocrinol Metab 62:773–777<br />
13. Laurberg P, Wallin G, Tallstedt L, Abraham-Nordling M, Lundell<br />
G, Tørring O 2008 TSH-receptor autoimmunity in Graves’ disease<br />
after therapy with anti-thyroid drugs, surgery, or radioiodine: a<br />
5-year prospective randomized study. Eur J Endocrinol 158:69–75<br />
14. Valyasevi RW, Erickson DZ, Harteneck DA, Dutton CM, Heufelder<br />
AE, Jyonouchi SC, Bahn RS 1999 Differentiation <strong>of</strong> human orbital<br />
preadipocyte fibroblasts induces expression <strong>of</strong> functional thyrotropin<br />
receptor. J Clin Endocrinol Metab 84:2557–2562<br />
15. Valyasevi RW, Harteneck DA, Dutton CM, Bahn RS 2002 Stimulation<br />
<strong>of</strong> adipogenesis, peroxisome proliferator-activated receptor-�<br />
(PPAR�), and thyrotropin receptor by PPAR� agonist in human<br />
orbital preadipocyte fibroblasts. J Clin Endocrinol Metab 87:2352–<br />
2358<br />
16. Pritchard J, Han R, Horst N, Cruikshank WW, Smith TJ 2003<br />
Immunoglobulin activation <strong>of</strong> T cell chemoattractant expression in<br />
fibroblasts from patients with Graves’ disease is mediated through<br />
the insulin-like growth factor I receptor pathway. J Immunol 170:<br />
6348–6354<br />
17. Smith TJ, Hoa N 2004 Immunoglobulins from patients with Graves’<br />
disease induce hyaluronan synthesis in their orbital fibroblasts<br />
through the self-antigen, insulin-like growth factor-I receptor. J Clin<br />
Endocrinol Metab 89:5076–5080<br />
18. Tötterman TH, Karlsson FA, Bengtsson M, Mendel-Hartvig I 1987<br />
Induction <strong>of</strong> circulating activated suppressor-like T cells by methimazole<br />
therapy for Graves’ disease. N Engl J Med 316:15–22<br />
19. Weetman AP, Holt ME, Campbell AK, Hall R, McGregor AM 1984<br />
Methimazole and generation <strong>of</strong> oxygen radicals by monocytes: potential<br />
role in immunosuppression. Br Med J (Clin Res Ed) 288:<br />
518–520<br />
20. Hallengren B, Forsgren A, Melander A 1980 Effects <strong>of</strong> antithyroid<br />
drugs on lymphocyte function in vitro. J Clin Endocrinol Metab<br />
51:298–301<br />
21. McGregor AM, Petersen MM, McLachlan SM, Rooke P, Smith BR,<br />
Hall R 1980 Carbimazole and the autoimmune response in Graves’<br />
disease. N Engl J Med 303:302–307<br />
22. Bartalena L, Baldeschi L, Dickinson AJ, Eckstein A, Kendall-Taylor<br />
P, Marcocci C, Mourits MP, Perros P, Boboridis K, Boschi A, Currò<br />
N, Daumerie C, Kahaly GJ, Krassas G, Lane CM, Lazarus JH,<br />
Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz<br />
S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM 2008<br />
Consensus Statement <strong>of</strong> the European Group on Graves’ Orbitopathy<br />
(EUGOGO) on Management <strong>of</strong> Graves’ Orbitopathy. Thyroid<br />
18:333–346<br />
23. Bartalena L, Baldeschi L, Dickinson A, Eckstein A, Kendall-Taylor<br />
P, Marcocci C, Mourits M, Perros P, Boboridis K, Boschi A, Currò<br />
N, Daumerie C, Kahaly GJ, Krassas GE, Lane CM, Lazarus JH,<br />
Marinò M, Nardi M, Neoh C, Orgiazzi J, Pearce S, Pinchera A, Pitz<br />
S, Salvi M, Sivelli P, Stahl M, von Arx G, Wiersinga WM; European<br />
Group on Graves’ Orbitopathy (EUGOGO) 2008 Consensus Statement<br />
<strong>of</strong> the European Group on Graves’ Orbitopathy (EUGOGO)<br />
on Management <strong>of</strong> Graves’ Orbitopathy. Eur J Endocrinol 158:<br />
273–285.<br />
24. Bartalena L, Marcocci C, Bogazzi F, Panicucci M, Lepri A, Pinchera<br />
A 1989 Use <strong>of</strong> corticosteroids to prevent progression <strong>of</strong> Graves’<br />
ophthalmopathy after radioiodine therapy for hyperthyroidism.<br />
N Engl J Med 321:1349–1352<br />
25. Dederichs B, Dietlein M, Jenniches-Kloth B, Schmidt M, <strong>The</strong>issen P,<br />
Moka D, Schicha H 2006 Radioiodine therapy <strong>of</strong> Graves’ hyperthyroidism<br />
in patients without pre-existing ophthalmopathy: can<br />
glucocorticoids prevent the development <strong>of</strong> new ophthalmopathy?<br />
Exp Clin Endocrinol Diabetes 114:366–370<br />
26. Perros P, Kendall-Taylor P, Neoh C, Frewin S, Dickinson J 2005 A<br />
prospective study <strong>of</strong> the effects <strong>of</strong> radioiodine therapy for hyperthyroidism<br />
in patients with minimally active graves’ ophthalmopathy.<br />
J Clin Endocrinol Metab 90:5321–5323<br />
27. Sisson JC, Schipper MJ, Nelson CC, Freitas JE, Frueh BR 2008<br />
Radioiodine therapy and Graves’ ophthalmopathy. J Nucl Med 49:<br />
923–930<br />
28. Eckstein AK, Plicht M, Lax H, Neuhäuser M, Mann K, Lederbogen<br />
S, Heckmann C, Esser J, Morgenthaler NG 2006 Thyrotropin receptor<br />
autoantibodies are independent risk factors for Graves’ ophthalmopathy<br />
and help to predict severity and outcome <strong>of</strong> the disease.<br />
J Clin Endocrinol Metab 91:3464–3470<br />
29. Wiersinga WM 2007 Management <strong>of</strong> Graves’ ophthalmopathy. Nat<br />
Clin Pract Endocrinol Metab 3:396–404