Medco Version D.0 Payers Secondary to Medicare ... - Express Scripts
Medco Version D.0 Payers Secondary to Medicare ... - Express Scripts
Medco Version D.0 Payers Secondary to Medicare ... - Express Scripts
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
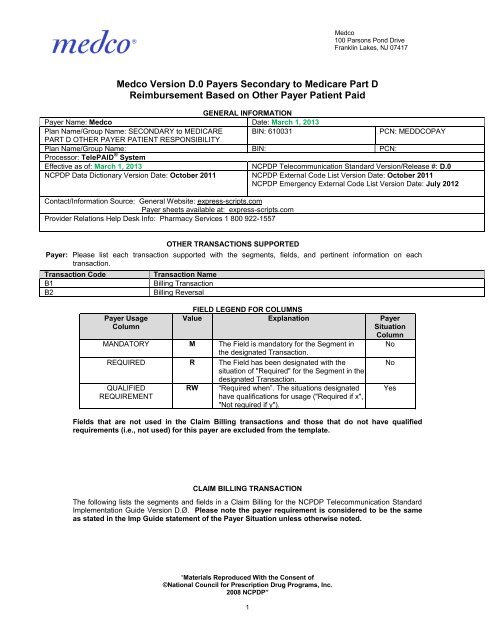
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417<strong>Medco</strong> <strong>Version</strong> <strong>D.0</strong> <strong>Payers</strong> <strong>Secondary</strong> <strong>to</strong> <strong>Medicare</strong> Part DReimbursement Based on Other Payer Patient PaidGENERAL INFORMATIONPayer Name: <strong>Medco</strong> Date: March 1, 2013Plan Name/Group Name: SECONDARY <strong>to</strong> MEDICARE BIN: 610031PCN: MEDDCOPAYPART D OTHER PAYER PATIENT RESPONSIBILITYPlan Name/Group Name: BIN: PCN:Processor: TelePAID ® SystemEffective as of: March 1, 2013 NCPDP Telecommunication Standard <strong>Version</strong>/Release #: <strong>D.0</strong>NCPDP Data Dictionary <strong>Version</strong> Date: Oc<strong>to</strong>ber 2011 NCPDP External Code List <strong>Version</strong> Date: Oc<strong>to</strong>ber 2011NCPDP Emergency External Code List <strong>Version</strong> Date: July 2012Contact/Information Source: General Website: express-scripts.comPayer sheets available at: express-scripts.comProvider Relations Help Desk Info: Pharmacy Services 1 800 922-1557OTHER TRANSACTIONS SUPPORTEDPayer: Please list each transaction supported with the segments, fields, and pertinent information on eachtransaction.Transaction CodeB1B2Transaction NameBilling TransactionBilling ReversalFIELD LEGEND FOR COLUMNSPayer UsageColumnValue Explanation PayerSituationColumnMANDATORY M The Field is manda<strong>to</strong>ry for the Segment in Nothe designated Transaction.REQUIRED R The Field has been designated with theNosituation of "Required" for the Segment in thedesignated Transaction.QUALIFIEDREQUIREMENTRW “Required when”. The situations designatedhave qualifications for usage ("Required if x","Not required if y").YesFields that are not used in the Claim Billing transactions and those that do not have qualifiedrequirements (i.e., not used) for this payer are excluded from the template.CLAIM BILLING TRANSACTIONThe following lists the segments and fields in a Claim Billing for the NCPDP Telecommunication StandardImplementation Guide <strong>Version</strong> D.Ø. Please note the payer requirement is considered <strong>to</strong> be the sameas stated in the Imp Guide statement of the Payer Situation unless otherwise noted.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”1
Transaction Header Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXSource of certification IDs required in SoftwareXVendor/Certification ID (11Ø-AK) is Payer IssuedSource of certification IDs required in SoftwareVendor/Certification ID (11Ø-AK) is Switch/VANissuedSource of certification IDs required in SoftwareVendor/Certification ID (11Ø-AK) is Not used<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Transaction Header SegmentClaim BillingField # NCPDP Field Name Value Payer Payer SituationUsage1Ø1-A1 BIN NUMBER See Values above in the Mgeneral information1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø4-A4 PROCESSOR CONTROL NUMBER See PCNS under General MInformation1Ø9-A9 TRANSACTION COUNT 1 M2Ø2-B2 SERVICE PROVIDER ID QUALIFIER 01 M BIN 610031 only allows for ServiceProvider Qualifier = 01 NPI2Ø1-B1 SERVICE PROVIDER ID Pharmacy or Dispensing MPhysician NPI4Ø1-D1 DATE OF SERVICE M11Ø-AK SOFTWAREVENDOR/CERTIFICATION IDAssigned when certifiedby TelePAID®MInsurance Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXInsurance SegmentClaim BillingSegment Identification (111-AM) =“Ø4”Field # NCPDP Field Name Value Payer Payer SituationUsage3Ø2-C2 CARDHOLDER ID M3Ø1-C1 GROUP ID M Imp Guide: Required if necessary forstate/federal/regula<strong>to</strong>ry agency programs.Required if needed for pharmacy claimprocessing and payment.3Ø9-C9 ELIGIBILITY CLARIFICATION CODE R Imp Guide: Required if needed forreceiver inquiry validation and/ordetermination, when eligibility is notmaintained at the dependent level.3Ø3-C3 PERSON CODE RW Imp Guide: Required if needed <strong>to</strong>uniquely identify the family memberswithin the Cardholder ID.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”2Payer Requirement: Required WhenPerson Number is provided on the IDcard.3Ø6-C6 PATIENT RELATIONSHIP CODE R Imp Guide: Required if needed <strong>to</strong>
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Insurance SegmentSegment Identification (111-AM) =“Ø4”Field # NCPDP Field Name Value PayerUsageClaim BillingPayer Situationuniquely identify the relationship of thePatient <strong>to</strong> the Cardholder.997-G2 CMS PART D DEFINED QUALIFIEDFACILITYRWImp Guide: Required if specified intrading partner agreement.Payer Requirement: May be submitted byLong Term Care PharmaciesPatient Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXThis Segment is situationalPatient SegmentClaim BillingSegment Identification (111-AM) =“Ø1”Field NCPDP Field Name Value Payer Payer SituationUsage3Ø4-C4 DATE OF BIRTH R3Ø5-C5 PATIENT GENDER CODE R31Ø-CA PATIENT FIRST NAME R Imp Guide: Required when the patienthas a first name.311-CB PATIENT LAST NAME R325-CP PATIENT ZIP/POSTAL ZONE RW Imp Guide: Optional.Payer RequirementEmergency/Disaster Situations;include current ZIP code of displacedpatient3Ø7-C7 PLACE OF SERVICE 01(Pharmacy) RW Imp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.Payer Requirement: Valid valuesrequired for Patient Residence andPharmacy Type. Values enteredshould be consistent with yourcontract384-4X PATIENT RESIDENCE RW Imp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.Payer Requirement: Valid valuesrequired for Patient Residence andPharmacy Type. Values enteredshould be consistent with yourcontract.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”3
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXThis payer does support partial fillsThis payer does not support partial fillsXClaim SegmentSegment Identification (111-AM) =“Ø7”Field # NCPDP Field Name Value PayerUsage455-EMPRESCRIPTION/SERVICEREFERENCE NUMBER QUALIFIERClaim BillingPayer Situation1(Rx Billing) M Imp Guide: For Transaction Code of“B1”, in the Claim Segment, thePrescription/Service ReferenceNumber Qualifier (455-EM) is “1” (RxBilling).M4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBER436-E1 PRODUCT/SERVICE ID QUALIFIER 00 (Not Specified)M Use 00 for Multi- ingredient compound03(NDC)claim.4Ø7-D7 PRODUCT/SERVICE ID M Use 0 for Multi- ingredient compoundclaim.442-E7 QUANTITY DISPENSED R4Ø3-D3 FILL NUMBER R4Ø5-D5 DAYS SUPPLY R4Ø6-D6 COMPOUND CODE 1(Not a Compound)2 (Compound)RSee Compound Segment for support ofmulti-ingredient compounds whencompound = 2.4Ø8-D8 DISPENSE AS WRITTENR(DAW)/PRODUCT SELECTIONCODE414-DE DATE PRESCRIPTION WRITTEN R419-DJ PRESCRIPTION ORIGIN CODE R Imp Guide: Required if necessary forplan benefit administration.354-NXSUBMISSION CLARIFICATIONCODE COUNTMaximum count of 3. RW Imp Guide: Required if SubmissionClarification Code (42Ø-DK) is used.42Ø-DKSUBMISSION CLARIFICATIONCODERWImp Guide: Required if clarification isneeded and value submitted is greaterthan zero (Ø).Payer Requirement: The value of 2 isused <strong>to</strong> respond <strong>to</strong> a Max DailyDose/High Dose Reject.3Ø8-C8 OTHER COVERAGE CODE 3 (Other Coverage Billed –claim not covered)8(Claim is billing for patientfinancial responsibility only)RWImp Guide: Required if needed byreceiver, <strong>to</strong> communicate a summationof other coverage information that hasbeen collected from other payers.Required for Coordination of Benefits.454-EK SCHEDULED PRESCRIPTION ID RW Imp Guide: Required if necessary for“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”4
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim SegmentSegment Identification (111-AM) =“Ø7”Field # NCPDP Field Name Value PayerUsageNUMBERClaim BillingPayer Situationstate/federal/regula<strong>to</strong>ry agencyprograms.Payer Requirement: Must be providedwhen State Medicaid Regulationsrequire this information.418-DI LEVEL OF SERVICE RW Imp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.461-EUPRIOR AUTHORIZATION TYPECODE1 (Prior Authorization)2(Medical Certification)8(Payer Defined Exemption)9(Emergency Preparedness)RWImp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.Payer Requirement:When value 1, 8, or 9 is used inconjunction with the Prior AuthorizationNumber Submitted field. Based onbenefit set up, a client may allow forTCO (Temporary Coverage Overrides,Transaction Supplies or EmergencyFills).When value “2” for Medical Certificationthen the Prior Authorization Number isnot required.462-EVPRIOR AUTHORIZATION NUMBERSUBMITTEDRWImp Guide: Required if this field couldresult in different coverage, pricing, orpatient financial responsibility.Payer Requirement:When “1” in field 461-EU, then 1111populated.When “8” in field 461-EU, then 9999populated.When “2” in field 461-EU, then this fieldis not required.When “9” in field 461-EU, then one ofthe 911-0 thru 5 populated or whenapplicable from the appropriate rejectclaim response use the value returnedfrom field 498-PY PRIORAUTHORIZATION NUMBER–ASSIGNED.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”5
Claim SegmentSegment Identification (111-AM) =“Ø7”Field # NCPDP Field Name Value PayerUsage357-NV DELAY REASON CODE 1=Proof of eligibility unknown RWor unavailable2=Litigation7=Third party processingdelay8=Delay in eligibilitydetermination9=Original claims rejected ordenied due <strong>to</strong> a reasonunrelated <strong>to</strong> the billinglimitation rules10=Administration delay inthe prior approval process<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingPayer SituationImp Guide: Required when needed <strong>to</strong>specify the reason that submission ofthe transaction has been delayedbeyond 90 days from the date of service.Payer Requirement: Processor acceptsvalues indicated <strong>to</strong> override a claimreject '81'.995-E2 ROUTE OF ADMINISTRATION RW Imp Guide: Required if specified intrading partner agreement.147-U7 PHARMACY SERVICE TYPE 1 (Community/RetailPharmacy Services)3( Home Infusion TherapyServices)5( Long Term Care PharmacyServices)RWPayer Requirement: Required whenCompound Code (4Ø6-D6) = 2(compound).Imp Guide: Required when the submittermust clarify the type of services beingperformed as a condition for properreimbursement by the payer.Payer Requirement:Valid values are required for PatientResidence and Pharmacy Service Type.Values entered should be consistentwith your contract.Pricing Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXPricing SegmentClaim BillingSegment Identification (111-AM) =“11”Field # NCPDP Field Name Value Payer Payer SituationUsage4Ø9-D9 INGREDIENT COST SUBMITTED R438-E3 INCENTIVE AMOUNT SUBMITTED RW Imp Guide: Required if its value has aneffect on the Gross Amount Due (43Ø-DU) calculation.Payer Requirement: Required whensubmitting a claim for a vaccine drugand administrative fee.481-HAFLAT SALES TAX AMOUNTSUBMITTEDRWImp Guide: Required if its value has aneffect on the Gross Amount Due (43Ø-DU) calculation.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”6
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417482-GE483-HEPERCENTAGE SALES TAX AMOUNTSUBMITTEDPERCENTAGE SALES TAX RATESUBMITTEDRWRWImp Guide: Required if its value has aneffect on the Gross Amount Due (43Ø-DU) calculation.Imp Guide: Required if PercentageSales Tax Amount Submitted (482-GE)and Percentage Sales Tax BasisSubmitted (484-JE) are used.Required if this field could result indifferent pricing.484-JEPERCENTAGE SALES TAX BASISSUBMITTEDRWRequired if needed <strong>to</strong> calculatePercentage Sales Tax Amount Paid(559-AX).Imp Guide: Required if PercentageSales Tax Amount Submitted (482-GE)and Percentage Sales Tax RateSubmitted (483-HE) are used.Required if this field could result indifferent pricing.Required if needed <strong>to</strong> calculatePercentage Sales Tax Amount Paid(559-AX).426-DQ USUAL AND CUSTOMARY CHARGE R Imp Guide: Required if needed pertrading partner agreement43Ø-DU GROSS AMOUNT DUE R423-DN BASIS OF COST DETERMINATION R Imp Guide: Required if needed forreceiver claim/encounter adjudication.Payer Requirement: Basis of CostDetermination not required for MultiIngredient Compound claims.Prescriber Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentXThis Segment is situationalPrescriber SegmentSegment Identification (111-AM) =“Ø3”Field # NCPDP Field Name Value PayerUsage466-EZ PRESCRIBER ID QUALIFIER 01(NPI)R08(State License)12(DEA)411-DB PRESCRIBER ID NPI , State License or DEA RNumberClaim BillingPayer SituationImp Guide: Required if Prescriber ID(411-DB) is used.Imp Guide: Required if this field couldresult in different coverage or patientfinancial responsibility.Required if necessary forstate/federal/regula<strong>to</strong>ry agencyprograms.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”Payer Requirement: NPI, State Licenseor DEA Number. For vaccines, anindividual NPI is required. It may be the7
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Prescriber SegmentClaim BillingSegment Identification (111-AM) =“Ø3”Field # NCPDP Field Name Value PayerUsagePayer Situationprescriber who wrote the prescription oralternate care provider (pharmacist,nurse practitioner, etc.) whoadministered the vaccine.427-DR PRESCRIBER LAST NAME RW Imp Guide: Required when thePrescriber ID (411-DB) is not known.Required if needed for Prescriber ID(411-DB) validation/clarification.Payer Requirement: Required whenPrescriber Id Qualifier = 08 (StateLicense) is submitted.367-2N PRESCRIBER STATE/PROVINCEADDRESSRWImp Guide: Required if needed <strong>to</strong> assistin identifying the prescriber.Required if necessary forstate/federal/regula<strong>to</strong>ry agencyprograms.Payer Requirement: PayerRequirement: Required whensubmitting Prescriber Id Qualifier = 08(State License) or Prescriber Id Qualifier= 12 (DEA) is submitted.Coordination of Benefits/Other Payments Segment Check Claim BillingQuestionsIf Situational, Payer SituationThis Segment is situational X Required only for secondary, tertiary, etc claims.Scenario 1 - Other Payer Amount Paid Repetitions OnlyScenario 2 - Other Payer-Patient Responsibility AmountRepetitions and Benefit Stage Repetitions OnlyXScenario 3 - Other Payer Amount Paid, Other Payer-Patient Responsibility Amount, and Benefit StageRepetitions Present (Government Programs)Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) =“Ø5”“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”8Claim BillingScenario 2 - Other Payer-PatientResponsibility Amount Repetitions andBenefit Stage Repetitions OnlyPayer SituationField # NCPDP Field Name Value PayerUsage337-4C COORDINATION OFMaximum count of 9. MBENEFITS/OTHER PAYMENTSCOUNT338-5C OTHER PAYER COVERAGE TYPE M339-6C OTHER PAYER ID QUALIFIER 03(BIN) R Imp Guide: Required if Other Payer ID(34Ø-7C) is used.
Coordination of Benefits/OtherPayments SegmentSegment Identification (111-AM) =“Ø5”Field # NCPDP Field Name Value PayerUsage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingScenario 2 - Other Payer-PatientResponsibility Amount Repetitions andBenefit Stage Repetitions OnlyPayer SituationPayer Requirement:BIN 610031 allows value 03 only34Ø-7C OTHER PAYER ID R Imp Guide: Required if identification of theOther Payer is necessary forclaim/encounter adjudication.443-E8 OTHER PAYER DATE R Imp Guide: Required if identification of theOther Payer Date is necessary forclaim/encounter adjudication.471-5E OTHER PAYER REJECT COUNT Maximum count of 5. RW Imp Guide: Required if Other PayerReject Code (472-6E) is used.472-6E OTHER PAYER REJECT CODE RW Imp Guide: Required when the otherpayer has denied the payment for thebilling.353-NR351-NP352-NQOTHER PAYER-PATIENTRESPONSIBILITY AMOUNT COUNTOTHER PAYER-PATIENTRESPONSIBILITY AMOUNTQUALIFIEROTHER PAYER-PATIENTRESPONSIBILITY AMOUNTRWRWRWImp Guide: Required if Other Payer-Patient Responsibility Amount Qualifier(351-NP) is used.Imp Guide: Required if Other Payer-Patient Responsibility Amount (352-NQ)is used.Imp Guide: Required if necessary forpatient financial responsibility only billing.392-MU BENEFIT STAGE COUNT Maximum count of 4. RW Imp Guide: Required if Benefit StageAmount (394-MW) is used.Payer Requirement: Only allowed for BIN610031.393-MV BENEFIT STAGE QUALIFIER RW Imp Guide: Required if Benefit StageAmount (394-MW) is used.Payer Requirement: Only allowed for BIN610031.394-MW BENEFIT STAGE AMOUNT RW Imp Guide: Required if the previous payerhas financial amounts that apply <strong>to</strong><strong>Medicare</strong> Part D beneficiary benefitstages. This field is required when theplan is a participant in a <strong>Medicare</strong> Part Dprogram that requires reporting of benefitstage specific financial amounts.DUR/PPS Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentThis Segment is situational X Based on pharmacy determination for clinical or vaccineprocessing. When submitting a claim for a vaccine andadministration fee, only the 440-E5 (Professional Service Code)field is required in this segment.When submitting a compound claim, field 474-8E (DUR/PPS Levelof Effort) is required; using the values consistent with your contract.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”9
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Compound SegmentSegment Identification (111-AM) = “1Ø”Field # NCPDP Field Name Value PayerUsage45Ø-EF COMPOUND DOSAGE FORMMDESCRIPTION CODE451-EG COMPOUND DISPENSING UNITMFORM INDICATOR447-EC COMPOUND INGREDIENTMaximum 25 MCOMPONENT COUNTingredients488-RE COMPOUND PRODUCT IDMQUALIFIER489-TE COMPOUND PRODUCT ID M448-ED COMPOUND INGREDIENTMQUANTITY449-EE COMPOUND INGREDIENT DRUGRCOSTClaim BillingPayer SituationImp Guide: Required if needed for receiver claimdetermination when multiple products are billed.49Ø-UECOMPOUND INGREDIENT BASISOF COST DETERMINATIONRImp Guide: Required if needed for receiver claimdetermination when multiple products are billed.Clinical Segment Questions Check Claim BillingIf Situational, Payer SituationThis Segment is always sentThis Segment is situational X This segment may be required as determined by benefit design.When the segment is submitted then the fields defined below aremanda<strong>to</strong>ry.Clinical SegmentSegment Identification (111-AM) =“13”Field # NCPDP Field Name Value PayerUsageClaim BillingPayer Situation491-VE DIAGNOSIS CODE COUNT Maximum count of 5. M Imp Guide: Required if Diagnosis CodeQualifier (492-WE) and Diagnosis Code(424-DO) are used.492-WE DIAGNOSIS CODE QUALIFIER 01 = ICD-902=ICD-10MImp Guide: Required if Diagnosis Code(424-DO) is used.424-DO DIAGNOSIS CODE M Imp Guide: Required if this field couldresult in different coverage, pricing, patientfinancial responsibility, and/or drugutilization review outcome.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”11Required if this field affects payment forprofessional pharmacy service.Required if this information can be used inplace of prior authorization.Required if necessary forstate/federal/regula<strong>to</strong>ry agency programs.
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417CLAIM BILLING RESPONSEGENERAL INFORMATIONPayer Name: <strong>Medco</strong> Date: March 1, 2013Plan Name/Group Name: SECONDARY <strong>to</strong> MEDICARE BIN: 610031PART D OTHER PAYER PATIENT RESPONSIBILITYPCN: MEDDCOPAYCLAIM BILLING PAID (OR DUPLICATE OF PAID) RESPONSEThe following lists the segments and fields in a Claim Billing response (Paid or Duplicate of Paid) Transaction for theNCPDP Telecommunication Standard Implementation Guide <strong>Version</strong> D.Ø. Please note the payer requirement isconsidered <strong>to</strong> be the same as stated in the Imp Guide statement of the Payer Situation unless otherwisenoted.Response Transaction Header SegmentQuestionsThis Segment is always sentCheckXClaim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationResponse Transaction HeaderSegmentField # NCPDP Field Name Value PayerUsage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS A M2Ø2-B2 SERVICE PROVIDER ID QUALIFIER Same value as in request M2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MClaim BillingAccepted/Paid (or Duplicate of Paid)Payer SituationResponse Message Header Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentThis Segment is situational X Provided when additional message text is necessaryResponse Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value PayerUsageClaim BillingAccepted/Paid (or Duplicate of Paid)Payer Situation5Ø4-F4 MESSAGE RW Imp Guide: Required if text is neededfor clarification or detail.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”12
Response Insurance Header SegmentQuestionsThis Segment is always sentResponse Insurance SegmentSegment Identification (111-AM) =“25”CheckX<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationClaim BillingAccepted/Paid (or Duplicate of Paid)Field # NCPDP Field Name Value Payer Payer SituationUsage3Ø1-C1 GROUP ID R Imp Guide: Required if needed <strong>to</strong>identify the actual cardholder oremployer group, <strong>to</strong> identify appropriategroup number, when available.Required <strong>to</strong> identify the actual groupthat was used when multiple groupcoverage exists.545-2F NETWORK REIMBURSEMENT ID R Imp Guide: Required if needed <strong>to</strong>identify the network for the coveredmember.Required if needed <strong>to</strong> identify the actualNetwork Reimbursement ID, whenapplicable and/or available.Required <strong>to</strong> identify the actual NetworkReimbursement ID that was used whenmultiple Network Reimbursement IDsexist.3Ø2-C2 CARDHOLDER ID RW Imp Guide: Required if the identification<strong>to</strong> be used in future transactions isdifferent than what was submitted onthe request.Response Status Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentXResponse Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value PayerUsage112-AN TRANSACTION RESPONSEP, D MSTATUSClaim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation5Ø3-F3 AUTHORIZATION NUMBER R Imp Guide: Required if needed <strong>to</strong>identify the transaction.547-5F APPROVED MESSAGE CODECOUNTMaximum count of 5. RW Imp Guide: Required if ApprovedMessage Code (548-6F) is used.548-6F APPROVED MESSAGE CODE RW Imp Guide: Required if ApprovedMessage Code Count (547-5F) isused and the sender needs <strong>to</strong>communicate additional follow up fora potential opportunity.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”13
Response Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value PayerUsage13Ø-UF132-UH526-FQ131-UGADDITIONAL MESSAGEINFORMATION COUNTADDITIONAL MESSAGEINFORMATION QUALIFIERADDITIONAL MESSAGEINFORMATIONADDITIONAL MESSAGEINFORMATION CONTINUITY549-7F HELP DESK PHONE NUMBERQUALIFIER<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)Payer SituationMaximum count of 9. RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.RWRWRWRWImp Guide: Required if AdditionalMessage Information (526-FQ) isused.Imp Guide: Required when additionaltext is needed for clarification ordetail.Imp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetition ofAdditional Message Information (526-FQ) follows it, and the text of thefollowing message is a continuation ofthe current.Imp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed <strong>to</strong>provide a support telephone number<strong>to</strong> the receiver.Response Claim Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentXResponse Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value PayerUsage455-EM PRESCRIPTION/SERVICEMREFERENCE NUMBER QUALIFIERClaim BillingAccepted/Paid (or Duplicate ofPaid)Payer SituationImp Guide: For Transaction Code of“B1”, in the Response ClaimSegment, the Prescription/ServiceReference Number Qualifier (455-EM)is “1” (Rx Billing).4Ø2-D2 PRESCRIPTION/SERVICEMREFERENCE NUMBER551-9F PREFERRED PRODUCT COUNT Maximum count of 6. RW Imp Guide: Required if PreferredProduct ID (553-AR) is used.552-APPREFERRED PRODUCT IDQUALIFIERRWPayer Requirement: Based on benefitand when preferred alternative areavailable for the submitted productservice ID.Imp Guide: Required if PreferredProduct ID (553-AR) is used.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”14
Response Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value PayerUsage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation553-AR PREFERRED PRODUCT ID RW Imp Guide: Required if a productpreference exists that needs <strong>to</strong> becommunicated <strong>to</strong> the receiver via anID.556-AUPREFERRED PRODUCTDESCRIPTIONResponse Pricing Segment Questions Check Claim BillingAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentXResponse Pricing SegmentSegment Identification (111-AM) =“23”Field # NCPDP Field Name Value PayerUsageRWImp Guide: Required if a productpreference exists that either cannotbe communicated by the PreferredProduct ID (553-AR) or <strong>to</strong> clarify thePreferred Product ID (553-AR).Claim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation5Ø5-F5 PATIENT PAY AMOUNT R5Ø6-F6 INGREDIENT COST PAID R5Ø7-F7 DISPENSING FEE PAID R Imp Guide: Required if this value isused <strong>to</strong> arrive at the finalreimbursement.557-AV TAX EXEMPT INDICATOR R Imp Guide: Required if the sender(health plan) and/or patient is taxexempt and exemption applies <strong>to</strong>this billing.558-AW FLAT SALES TAX AMOUNT PAID RW Imp Guide: Required if Flat SalesTax Amount Submitted (481-HA) isgreater than zero (Ø) or if Flat SalesTax Amount Paid (558-AW) is used<strong>to</strong> arrive at the final reimbursement.559-AXPERCENTAGE SALES TAXAMOUNT PAIDRWImp Guide: Required if this value isused <strong>to</strong> arrive at the finalreimbursement.Required if Percentage Sales TaxAmount Submitted (482-GE) isgreater than zero (Ø).56Ø-AY561-AZPERCENTAGE SALES TAX RATEPAIDPERCENTAGE SALES TAX BASISPAIDRWRWRequired if Percentage Sales TaxRate Paid (56Ø-AY) and PercentageSales Tax Basis Paid (561-AZ) areused.Imp Guide: Required if PercentageSales Tax Amount Paid (559-AX) isgreater than zero (Ø).Imp Guide: Required if PercentageSales Tax Amount Paid (559-AX) isgreater than zero (Ø).“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”15
Response Pricing SegmentSegment Identification (111-AM) =“23”Field # NCPDP Field Name Value PayerUsage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation521-FL INCENTIVE AMOUNT PAID RW Imp Guide: Required if this value isused <strong>to</strong> arrive at the finalreimbursement.5Ø9-F9 TOTAL AMOUNT PAID R522-FM BASIS OF REIMBURSEMENTRDETERMINATIONRequired if Incentive AmountSubmitted (438-E3) is greater thanzero (Ø).Imp Guide: Required if IngredientCost Paid (5Ø6-F6) is greater thanzero (Ø).523-FNAMOUNT ATTRIBUTED TO SALESTAX16RWRequired if Basis of CostDetermination (432-DN) is submittedon billing.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes sales taxthat is the financial responsibility ofthe member but is not also includedin any of the other fields that add up<strong>to</strong> Patient Pay Amount.Imp Guide: Provided forinformational purposes only.Imp Guide: Provided forinformational purposes only.512-FC ACCUMULATED DEDUCTIBLEAMOUNTRW513-FD REMAINING DEDUCTIBLERWAMOUNT514-FE REMAINING BENEFIT AMOUNT RW Imp Guide: Provided forinformational purposes only.517-FH AMOUNT APPLIED TO PERIODICRWDEDUCTIBLEImp Guide: Required if Patient PayAmount (5Ø5-F5) includesdeductible.518-FI AMOUNT OF CO-PAY RW Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes co-payas patient financial responsibility.52Ø-FK571-NZAMOUNT EXCEEDING PERIODICBENEFIT MAXIMUMAMOUNT ATTRIBUTED TOPROCESSOR FEERWRWImp Guide: Required if Patient PayAmount (5Ø5-F5) includes amountexceeding periodic benefitmaximum.Imp Guide: Required if the cus<strong>to</strong>meris responsible for 1ØØ% of theprescription payment and when theprovider net sale is less than theamount the cus<strong>to</strong>mer is expected <strong>to</strong>pay.575-EQ PATIENT SALES TAX AMOUNT RW Imp Guide: Used when necessary <strong>to</strong>identify the Patient’s portion of theSales Tax.574-2Y PLAN SALES TAX AMOUNT RW Imp Guide: Used when necessary <strong>to</strong>identify the Plan’s portion of theSales Tax.572-4U AMOUNT OF COINSURANCE RW Imp Guide: Required if Patient PayAmount (5Ø5-F5) includescoinsurance as patient financialresponsibility.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”
Response Pricing SegmentSegment Identification (111-AM) =“23”Field # NCPDP Field Name Value PayerUsage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation577-G3 ESTIMATED GENERIC SAVINGS RW Imp Guide: This information shouldbe provided when a patient selectedthe brand drug and a generic form ofthe drug was available. It willcontain an estimate of the differencebetween the cost of the brand drugand the generic drug, when thebrand drug is more expensive thanthe generic.128-UC129-UD133-UJ134-UK135-UM136-UNSPENDING ACCOUNT AMOUNTREMAININGHEALTH PLAN-FUNDEDASSISTANCE AMOUNTAMOUNT ATTRIBUTED TOPROVIDER NETWORK SELECTIONAMOUNT ATTRIBUTED TOPRODUCT SELECTION/BRANDDRUGAMOUNT ATTRIBUTED TOPRODUCT SELECTION/NON-PREFERRED FORMULARYSELECTIONAMOUNT ATTRIBUTED TOPRODUCT SELECTION/BRANDNON-PREFERRED FORMULARYSELECTION566-J5 OTHER PAYER AMOUNTRECOGNIZEDRWRWRWRWRWRWImp Guide: This dollar amount willbe provided, if known, <strong>to</strong> thereceiver when the transaction hadspending account dollars reportedas part of the patient pay amount.Imp Guide: Required when thepatient meets the plan-fundedassistance criteria, <strong>to</strong> reduce PatientPay Amount (5Ø5-F5). The resultingPatient Pay Amount (5Ø5-F5) mustbe greater than or equal <strong>to</strong> zero.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable <strong>to</strong> a costshare differential due <strong>to</strong> theselection of one pharmacy overanother.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable <strong>to</strong> apatient’s selection of a Brand drug.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable <strong>to</strong> apatient’s selection of a non-preferredformulary product.Imp Guide: Required if Patient PayAmount (5Ø5-F5) includes anamount that is attributable <strong>to</strong> apatient’s selection of a Brand nonpreferredformulary product.Imp Guide: Required if this value isused <strong>to</strong> arrive at the finalreimbursement.Required if Other Payer AmountPaid (431-DV) is greater than zero(Ø) and Coordination ofBenefits/Other Payments Segmentis supported.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”17
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Check Claim BillingResponse DUR/PPS Segment QuestionsAccepted/Paid (or Duplicate of Paid)If Situational, Payer SituationThis Segment is always sentThis Segment is situational X When DUR Information <strong>to</strong> be providedResponse DUR/PPS SegmentSegment Identification (111-AM) =“24”Field # NCPDP Field Name Value PayerUsage567-J6 DUR/PPS RESPONSE CODECOUNTERMaximum 9 occurrencessupported.RWClaim BillingAccepted/Paid (or Duplicate ofPaid)Payer SituationImp Guide: Required if ReasonFor Service Code (439-E4) isused.439-E4 REASON FOR SERVICE CODE RW Imp Guide: Required if utilizationconflict is detected.528-FS CLINICAL SIGNIFICANCE CODE RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.529-FT OTHER PHARMACY INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.53Ø-FU PREVIOUS DATE OF FILL RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.Required if Quantity of PreviousFill (531-FV) is used.531-FV QUANTITY OF PREVIOUS FILL RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.Required if Previous Date of Fill(53Ø-FU) is used.532-FW DATABASE INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.533-FX OTHER PRESCRIBER INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.544-FY DUR FREE TEXT MESSAGE RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.57Ø-NS DUR ADDITIONAL TEXT RW Imp Guide: Required if needed <strong>to</strong>supply additional information forthe utilization conflict.CLAIM BILLING/ACCEPTED/REJECTED RESPONSEResponse Transaction Header SegmentQuestionsThis Segment is always sentResponse Transaction HeaderSegmentCheckXClaim Billing Accepted/RejectedIf Situational, Payer SituationClaim BillingAccepted/Rejected“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”18
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Field # NCPDP Field Name Value PayerUsage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS A M2Ø2-B2 SERVICE PROVIDER ID QUALIFIER Same value as in request M2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MPayer SituationResponse Message Segment Questions Check Claim Billing Accepted/RejectedIf Situational, Payer SituationThis Segment is always sentThis Segment is situational X Provided when additional message textResponse Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value PayerUsageClaim BillingAccepted/RejectedPayer Situation5Ø4-F4 MESSAGE Imp Guide: Required if text isneeded for clarification or detail.Response Insurance Segment Questions Check Claim Billing/Claim Rebill Accepted/RejectedIf Situational, Payer SituationThis Segment is always sentXThis Segment is situationalResponse Insurance SegmentSegment Identification (111-AM) =“25”Field # NCPDP Field Name Value PayerUsageClaim BillingAccepted/RejectedPayer Situation3Ø1-C1 GROUP ID RW Imp Guide: Required if needed <strong>to</strong>identify the actual cardholder oremployer group, <strong>to</strong> identifyappropriate group number, whenavailable.Required <strong>to</strong> identify the actual groupthat was used when multiple groupcoverage exists.545-2F NETWORK REIMBURSEMENT ID RW Imp Guide: Required if needed <strong>to</strong>identify the network for the coveredmember.Required if needed <strong>to</strong> identify theactual Network Reimbursement ID,when applicable and/or available.Required <strong>to</strong> identify the actualNetwork Reimbursement ID thatwas used when multiple NetworkReimbursement IDs exist.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”19
Response Insurance SegmentSegment Identification (111-AM) =“25”Field # NCPDP Field Name Value PayerUsage<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingAccepted/RejectedPayer Situation3Ø2-C2 CARDHOLDER ID RW Imp Guide: Required if theidentification <strong>to</strong> be used in futuretransactions is different than whatwas submitted on the request.Response Status Segment Questions Check Claim BillingAccepted/RejectedIf Situational, Payer SituationThis Segment is always sentXResponse Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value PayerUsage112-AN TRANSACTION RESPONSERMSTATUS51Ø-FA REJECT COUNT Maximum count of 5. R511-FB REJECT CODE R546-4F REJECT FIELD OCCURRENCERWINDICATOR13Ø-UF132-UH526-FQ131-UGADDITIONAL MESSAGEINFORMATION COUNTADDITIONAL MESSAGEINFORMATION QUALIFIERADDITIONAL MESSAGEINFORMATIONADDITIONAL MESSAGEINFORMATION CONTINUITY549-7F HELP DESK PHONE NUMBERQUALIFIERClaim Billing Accepted/RejectedPayer SituationImp Guide: Required if a repeatingfield is in error, <strong>to</strong> identify repeatingfield occurrence.Maximum count of 9. RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.Ø1- Ø9 = Free-Form Text1Ø = Next Available FillDate (CCYYMMDD)RWRWRWRWImp Guide: Required if AdditionalMessage Information (526-FQ) isused.Imp Guide: Required whenadditional text is needed forclarification or detail.Imp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetitionof Additional Message Information(526-FQ) follows it, and the text ofthe following message is acontinuation of the current.Imp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed <strong>to</strong>provide a support telephonenumber.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”20
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Response Status SegmentClaim Billing Accepted/RejectedSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value Payer Payer SituationUsage987-MA URL RW Imp Guide: Provided forinformational purposes only <strong>to</strong> relayhealthcare communications via theInternet.Payer Requirement: Will returnhttp://www.expressscripts.com/services/pharmacistsResponse Claim Segment Questions Check Claim Billing Accepted/RejectedIf Situational, Payer SituationThis Segment is always sentXResponse Claim SegmentSegment Identification (111-AM) =“22”Field # NCPDP Field Name Value PayerUsage455-EMPRESCRIPTION/SERVICEREFERENCE NUMBER QUALIFIERClaim BillingAccepted/Paid (or Duplicate ofPaid)Payer Situation1 (Rx Billing) M Imp Guide: For Transaction Code of“B1”, in the Response ClaimSegment, the Prescription/ServiceReference Number Qualifier (455-EM)is “1” (Rx Billing).M4Ø2-D2 PRESCRIPTION/SERVICEREFERENCE NUMBER551-9F PREFERRED PRODUCT COUNT Maximum count of 6. RW Imp Guide: Required if PreferredProduct ID (553-AR) is used.552-APPREFERRED PRODUCT IDQUALIFIERRWImp Guide: Required if PreferredProduct ID (553-AR) is used.553-AR PREFERRED PRODUCT ID RW Imp Guide: Required if a productpreference exists that needs <strong>to</strong> becommunicated <strong>to</strong> the receiver via anID.556-AUPREFERRED PRODUCTDESCRIPTIONRWImp Guide: Required if a productpreference exists that either cannotbe communicated by the PreferredProduct ID (553-AR) or <strong>to</strong> clarify thePreferred Product ID (553-AR).Response DUR/PPS Segment Questions Check Claim Billing Accepted/RejectedIf Situational, Payer SituationThis Segment is always sentThis Segment is situational X When DUR has additional information <strong>to</strong> be returnedResponse DUR/PPS SegmentSegment Identification (111-AM) =“24”Claim Billing/Accepted/Rejected“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”21
Response DUR/PPS SegmentSegment Identification (111-AM) =“24”Field # NCPDP Field Name Value PayerUsage567-J6 DUR/PPS RESPONSE CODECOUNTERMaximum 9 occurrencessupported.RW<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim Billing/Accepted/RejectedPayer SituationImp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetitionof Additional Message Information(526-FQ) follows it, and the text ofthe following message is acontinuation of the current.439-E4 REASON FOR SERVICE CODE RW Imp Guide: Required if utilizationconflict is detected.528-FS CLINICAL SIGNIFICANCE CODE RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.529-FT OTHER PHARMACY INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.53Ø-FU PREVIOUS DATE OF FILL RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.Required if Quantity of Previous Fill(531-FV) is used.531-FV QUANTITY OF PREVIOUS FILL RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.Required if Previous Date of Fill(53Ø-FU) is used.532-FW DATABASE INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.533-FX OTHER PRESCRIBER INDICATOR RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.544-FY DUR FREE TEXT MESSAGE RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.57Ø-NS DUR ADDITIONAL TEXT RW Imp Guide: Required if needed <strong>to</strong>supply additional information for theutilization conflict.Response Prior Authorization SegmentQuestionsCheck Claim Billing Accepted/RejectedIf Situational, Payer SituationThis Segment is always sentThis Segment is situational X Provided when the receiver has the opportunity <strong>to</strong> reprocessthe claim with using a Prior Authorization Number.Response Prior AuthorizationSegmentSegment Identification (111-AM) =“26”Claim BillingAccepted/Rejected“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”22
<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Field # NCPDP Field Name Value PayerUsage498-PY PRIOR AUTHORIZATIONRWNUMBER–ASSIGNEDPayer SituationImp Guide: Required whenthe receiver must submit this PriorAuthorization Number in order <strong>to</strong>receive payment for the claim.Payer Requirement: The valuereturned in this field will provide thevalue that may be submitted in PriorAuthorization Number Submitted, field462-EV. This value must be submittedwith appropriate corresponding PriorAuthorization Type Code, field 461-EU.CLAIM BILLING REJECTED/REJECTED RESPONSEResponse Transaction Header SegmentQuestionsThis Segment is always sentCheckXClaim BillingRejected/RejectedIf Situational, Payer SituationResponse Transaction HeaderSegmentField # NCPDP Field Name Value PayerUsage1Ø2-A2 VERSION/RELEASE NUMBER DØ M1Ø3-A3 TRANSACTION CODE B1 M1Ø9-A9 TRANSACTION COUNT Same value as in request M5Ø1-F1 HEADER RESPONSE STATUS R M2Ø2-B2 SERVICE PROVIDER IDSame value as in request MQUALIFIER2Ø1-B1 SERVICE PROVIDER ID Same value as in request M4Ø1-D1 DATE OF SERVICE Same value as in request MClaim BillingRejected/RejectedPayer SituationResponse Message Segment Questions Check Claim Billing/Claim Rebill Rejected/RejectedIf Situational, Payer SituationThis Segment is always sentThis Segment is situationalProvided X When additional message text is necessaryResponse Message SegmentSegment Identification (111-AM) =“2Ø”Field # NCPDP Field Name Value PayerUsageClaim BillingRejected/RejectedPayer Situation5Ø4-F4 MESSAGE Imp Guide: Required if text is neededfor clarification or detail.Response Status Segment Questions Check Claim Billing/Rejected/RejectedIf Situational, Payer SituationThis Segment is always sentX“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”23
Response Status SegmentSegment Identification (111-AM) =“21”Field # NCPDP Field Name Value PayerUsage112-AN TRANSACTION RESPONSERM<strong>Medco</strong>100 Parsons Pond DriveFranklin Lakes, NJ 07417Claim BillingRejected/RejectedPayer SituationSTATUS5Ø3-F3 AUTHORIZATION NUMBER RW Imp Guide: Required if needed <strong>to</strong>identify the transaction.51Ø-FA REJECT COUNT Maximum count of 5 R511-FB REJECT CODE R546-4F REJECT FIELD OCCURRENCEINDICATORRW13Ø-UF132-UH526-FQ131-UGADDITIONAL MESSAGEINFORMATION COUNTADDITIONAL MESSAGEINFORMATION QUALIFIERADDITIONAL MESSAGEINFORMATIONADDITIONAL MESSAGEINFORMATION CONTINUITY549-7F HELP DESK PHONE NUMBERQUALIFIERImp Guide: Required if a repeatingfield is in error, <strong>to</strong> identify repeatingfield occurrence.Maximum count of 9 RW Imp Guide: Required if AdditionalMessage Information (526-FQ) isused.RWRWRWRWImp Guide: Required if AdditionalMessage Information (526-FQ) isused.Imp Guide: Required when additionaltext is needed for clarification ordetail.Imp Guide: Required if and only ifcurrent repetition of AdditionalMessage Information (526-FQ) isused, another populated repetition ofAdditional Message Information (526-FQ) follows it, and the text of thefollowing message is a continuation ofthe current.Imp Guide: Required if Help DeskPhone Number (55Ø-8F) is used.55Ø-8F HELP DESK PHONE NUMBER RW Imp Guide: Required if needed <strong>to</strong>provide a support telephone number<strong>to</strong> the receiver.“Materials Reproduced With the Consent of©National Council for Prescription Drug Programs, Inc.2008 NCPDP”24