Moments of Discovery - UT Southwestern
Moments of Discovery - UT Southwestern
Moments of Discovery - UT Southwestern
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Moments</strong> <strong>of</strong> <strong>Discovery</strong>A Journey to the 2011 Nobel Prize
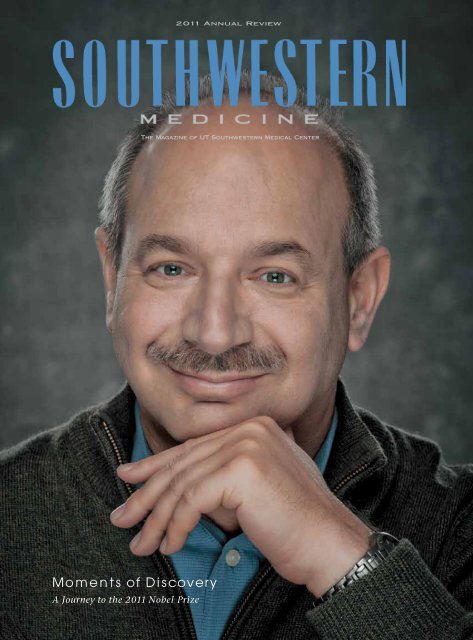
C O N T E N T SLUNG CANCER IN THE CROSSHAIRS 2Physicians and researchers are taking aim on several fronts to target America’s biggest cancer killer.THE NATION’S NO. 1 KILLER SENDS SILENT SIGNALS 10Cardiologists are uncovering new risk factors and predictors that can indicate heart disease before it strikes.BRAVE NEW WORLD: HIGH TECH MEDICINE 18Merging medicine and technology can advance scientific discovery and enhance patient care.MOMENTS OF DISCOVERY 26Dr. Bruce A. Beutler describes the long journey that led not only to pr<strong>of</strong>ound discoveries<strong>of</strong> how the immune system works, but also a Nobel Prize.THE HOSPITAL OF THE F<strong>UT</strong>URE 34Designed around the needs <strong>of</strong> patients and their families, the new <strong>UT</strong> <strong>Southwestern</strong> University Hospitalwill be as innovative as the scientific discoveries for which the medical center is known.CAN FOODBORNE ILLNESSES BE STOPPED? 42Researchers are at the forefront <strong>of</strong> understanding and preventing the spread <strong>of</strong> dangerous bacteria in food.VOLUME 21 / NUMBER 1 VOLUME / FEBRUARY 21 / 2012 NUMBER 1 / FEBRUARY 2012<strong>Southwestern</strong> Medicine is <strong>Southwestern</strong> a publication Medicine <strong>of</strong> the University is a publication <strong>of</strong> the UniversityNews Bureau at The University News Bureau <strong>of</strong> Texas at The <strong>Southwestern</strong> University <strong>of</strong> Texas <strong>Southwestern</strong>Medical Center, a component Medical <strong>of</strong> Center, The University a component <strong>of</strong> <strong>of</strong> The University <strong>of</strong>Texas System. Copyright, Texas 2012, System. <strong>UT</strong> <strong>Southwestern</strong> Copyright, 2012, Medical <strong>UT</strong> <strong>Southwestern</strong> MedicalCenter. For permission Center. to quote For permission reprint any to material quote or reprint any materialwritten herein, for permission written to herein, reproduce for permission art, or to to reproduce art, or torequest additional copies, request please additional contact the copies, University please contact the UniversityNews Bureau, 5323 Harry News Hines Bureau, Blvd., 5323 Dallas, Harry Texas Hines Blvd., Dallas, Texas75390-9060. <strong>UT</strong> <strong>Southwestern</strong> 75390-9060. is an equal <strong>UT</strong> <strong>Southwestern</strong> opportunity is an equal opportunityinstitution.institution.WHAT IT TAKES TO BECOME A WORLD-CLASS PHYSICIAN 50<strong>UT</strong> <strong>Southwestern</strong> prepares the next generation <strong>of</strong> physicians to process and retain vast amounts <strong>of</strong> medicalknowledge, which, by 2020, is expected to double approximately every four months.THE CLINICAL FRONTIER 60CLINIC TREATS SLEEP AND BREATHING DISORDERS 60TARGETED THERAPY FOR ADVANCED GYNECOLOGIC CANCERS 61PRESIDENTDANIEL K. PODOLSKY, PRESIDENT M.D. DANIEL K. PODOLSKY, M.D.MAKING HEADWAY ON HEADACHES 62COMMUNICATIONS, VICE PRESIDENT MARKETING FOR COMMUNICATIONS, AND PUBLIC AFFAIRS MARKETING TIM DOKE AND PUBLIC AFFAIRS TIM DOKEDIRECTOR OF UNIVERSITY NEWS DIRECTOR BUREAUOF MICHAEL UNIVERSITY BERMAN NEWS BUREAU MICHAEL BERMANASSISTANT EDITORSR<strong>UT</strong>H EYRE ASSISTANT EDITORS R<strong>UT</strong>H EYREDONNA STEPH HANSARDONNA STEPH HANSARDROBIN LOVEMAN ROBIN LOVEMANPATRICK WASCOVICH PATRICK WASCOVICH2011 ANNUAL REVIEW 65highlights <strong>of</strong> the year 66financial statement 76gift report 79WRITERS DEBBIE BOLLESWRITERSDEBBIE BOLLESJEFF CARLTON JEFF CARLTONLAKISHA LADSON LAKISHA LADSONALEX LYDAALEX LYDARUSSELL RIAN RUSSELL RIANROBIN RUSSELL ROBIN RUSSELLERIN PRATHER STAFFORDERIN PRATHER STAFFORDPHOTOGRAPHERSBRIAN COATS PHOTOGRAPHERSDAVID GRESHAMBRIAN COATSDAVID GRESHAMDIRECTOR OF CREATIVE SERVICES DIRECTOR SHAYNE OF CREATIVE WASHBURN SERVICESSHAYNE WASHBURNDESIGNERS KEVIN BAILEYDESIGNERSJAY CALDWELLANGELA CHARLTONSHANE DENNEHEYYOLANDA FUENTESWALTER HORTONKEVIN BAILEYJAY CALDWELLANGELA CHARLTONSHANE DENNEHEYYOLANDA FUENTESWALTER HORTONPRODUCTIONCHERYL SUDOL PRODUCTIONKATHY WATSONCHERYL SUDOLKATHY WATSONOn the cover: 2011 Nobel On the Laureate cover: Dr. 2011 Bruce Nobel A. Beutler Laureate Dr. Bruce A. BeutlerArticles from <strong>Southwestern</strong> Medicine and other news and information from <strong>UT</strong> <strong>Southwestern</strong> are available online at www.utsouthwestern.edu.
Lung Cancer in theCrosshairsTargeting America's Biggest Cancer KillerAfter undergoing a routine hernia operation, Anita Vasquez returned to her Fort Worthhome only to come down with a fever and cough. A simple chest X-ray revealed a nightmarishscenario: Mrs. Vasquez learned she was facing a tumor that threatened to burstout <strong>of</strong> her lung and invade other organs. Never having touched a cigarette, she and herhusband were shocked. “The doctor <strong>of</strong>fered to show me a picture <strong>of</strong> my left lung on thecomputer,” the 68-year-old former unit secretary at Harris Methodist Hospital recalledrecently. “And there it was: a round shadow.” The couple immediately started pollingfriends and family about where to go for treatment. A dietitian at work quietly saidshe should go to Dallas, specifically to <strong>UT</strong> <strong>Southwestern</strong> Medical Center’s Harold C.Simmons Cancer Center, which has an excellent lung cancer program. She prayed.But it wasn’t until standing in a checkout line the next day that she heard anothercustomer speaking highly <strong>of</strong> the Simmons Cancer Center.B Y A L E X L Y D A1 2
“It was more than a coincidence that I wasin line with this man,” Mrs. Vasquez said onerecent afternoon. “That’s when God intervenedand made my decision for me.”She would go to Dallas.Patients are bringing their cancer fight tothe Simmons Cancer Center daily. For somewho are emotionally prepared and intellectuallycurious enough to see cancer up close, thecenter allows patients to get smart about thedisease, in ways that other cancer centerswithout equally strong research underpinningscannot. In order to effectively fight an enemy,one must see it to treat it. This is where doctorsand scientists at <strong>UT</strong> <strong>Southwestern</strong> are makingheadway every day.Seeing the enemyDr. Adi Gazdar and other Simmons CancerCenter specialists believe that seeing the canceron a molecular level is important, and not justfor the diagnostician. Dr. Gazdar, pr<strong>of</strong>essor<strong>of</strong> pathology, holds the W. Ray WallaceDistinguished Chair in Molecular OncologyResearch at <strong>UT</strong> <strong>Southwestern</strong>.To most patients, the cancers growing inthe flasks and petri dishes that fill Dr. Gazdar’slaboratory will remain an invisible enemy.Yet the clumps <strong>of</strong> non-small cell lung cancers,giant-cell carcinomas and tumors are visibleto the naked eye. Hold the flask up to anyfluorescent light and they make cancer very realand very alive.Cynthia Gonzalez was in her early 50swhen diagnosed with advanced lung cancer,only after developing a persistent cough thatwas first thought by doctors to be bronchitisor pneumonia. After multiple visits at anotherfacility and an ineffective course <strong>of</strong> antibiotics,doctors discovered the truth. A biopsy done at<strong>UT</strong> MD Anderson Cancer Center in Houstonrevealed Stage 4 lung cancer.“By this time I had zero trust in doctors,”Mrs. Gonzalez said. “They did give me a videoand a brochure and that told me what to expect,but I didn’t feel like I was getting the personalattention that I needed.”After asking some friends in the medicalcommunity where she could go for thetrust and individualized treatment she wasseeking, she contacted Dr. Joan Schiller, chief<strong>of</strong> the Hematology/Oncology Division at<strong>UT</strong> <strong>Southwestern</strong> and holder <strong>of</strong> the AndreaL. Simmons Distinguished Chair in CancerResearch.Mrs. Gonzalez remembers the day vividly.It was Dec. 27, 2010.“Dr. Schiller called me back that day fromher family vacation in Colorado,” Mrs. Gonzalezsaid. “My experience is that most doctors careabout their own time, so I was so surprised andencouraged that she would be so selfless.”Mrs. Gonzalez’s experience at the SimmonsCancer Center is typical <strong>of</strong> many patients.The process usually starts with lab tests. Tumortissue is analyzed every way possible underthe microscope and through a series <strong>of</strong> highlysophisticated molecular assays. Then, usingthe state-<strong>of</strong>-the-art information collected ata cellular level, cancer specialists select thebest therapy for that patient – what types <strong>of</strong>chemotherapy drugs and, if indicated, the mosteffective uses <strong>of</strong> radiation, what doctors call a“combined modality” treatment.Understanding the enemyIn scientific terms, cancer is a disease <strong>of</strong>pathological hyperplasia – uncontrolled growth<strong>of</strong> the body’s own cells. And some patients’interest in the disease – ultimately a fightagainst their own body – can be comprehensivein itself: Doctors say the informed patient triesto absorb as much information as possibleabout the latest clinical advances and themost cutting-edge research in cancer biology,applying what they learn to fight their cancerin ways that make sense for them.At the Simmons Cancer Center, cancerpatients can visit the labs to understand moreabout the enemy, said Dr. John Minna, director<strong>of</strong> the Nancy B. and Jake L. Hamon Centerfor Therapeutic Oncology Research and theW.A. “Tex” and Deborah Moncrief Jr. Centerfor Cancer Genetics. A cancer patient beingtreated can not only see cancer cells, but has thechance to watch them swarm and multiply inDr. Gazdar’s lab.“We do have patients who want to considerthe totality <strong>of</strong> their disease and attack it fromall angles,” said Dr. Minna, a pr<strong>of</strong>essor <strong>of</strong>internal medicine, who holds the Sarah M. andCharles E. Seay Distinguished Chair in CancerResearch and the Max L. Thomas DistinguishedChair in Molecular Pulmonary Oncology. “Tothese patients, visualizing the ‘enemy’ andunderstanding it on a fundamental level canincrease their interest in shaping a treatmentthat ultimately improves the outcome.”Call it a personalized, team-based approachthat puts the patient on par with theoncologists, researchers, nurses and supportivecare personnel who are all dedicated to the fight.An Invisible enemyThe Simmons Cancer Center is the onlycancer center in North Texas to have received adesignation from the National Cancer Institute(NCI). While the center is on the cutting edge<strong>of</strong> detecting and imaging cancer, the problem<strong>of</strong> adequately seeing cancer on a cellular leveldates to when leukemia was known simply as“white blood.”Until the middle <strong>of</strong> the last century,observing the behavior <strong>of</strong> cancer cells didnot significantly advance until the renownedpediatric pathologist Dr. Sidney Farber firsttrained his microscope in Boston on theblood <strong>of</strong> very sick children suffering from anexplosion in their white blood cell counts. Theblood looked milky under the microscope; hewas seeing leukemia. It was 1947, around thetime when <strong>UT</strong> <strong>Southwestern</strong> as it is knownnow was just getting <strong>of</strong>f the ground, thanks tothe inimitable leadership <strong>of</strong> Drs. Edward Cary,Donald Seldin and others.Fast-forward to 2012.The landscape for detecting, studying andtreating cancer has changed radically. Many <strong>of</strong>the advances are on full display at the SimmonsCancer Center, particularly in the fight againstlung cancer, the nation’s top cancer killer. Morethan 173,000 new cases <strong>of</strong> lung cancer areDr. Adi Gazdar scrutinizes a flask forclumps <strong>of</strong> cancer cells visible withthe naked eye. Dr. Gazdar’s laboratoryhas cataloged and analyzedover 2,200 human cancer specimens,with an emphasis on lung cancerand lymphomas.diagnosed each year in the U.S., accounting for13 percent <strong>of</strong> new cancer cases, according to theAmerican Cancer Society. That is equal to theentire city <strong>of</strong> Dayton, Ohio, getting a diagnosis– when 88 percent <strong>of</strong> the people living there donot even smoke.Peter Jennings, the late and pioneering ABCNews anchor, smoked. While he passed awayquietly in the palliative care unit <strong>of</strong> MemorialSloan-Kettering Cancer Center in 2005, noamount <strong>of</strong> money or expert care could save him.A number <strong>of</strong> other celebrities and notablepersonalities have succumbed to lung cancer,smokers and non-smokers alike: Dana Reeve,the wife <strong>of</strong> actor Christopher Reeve; actorsSteve McQueen and Vincent Price; and singerLou Rawls.Dr. Gazdar is among a select group <strong>of</strong> cancerscientists searching for lung cancer biomarkersin people who have never smoked. In 2009,the National Cancer Institute’s Early DetectionResearch Network and the Canary Foundation,a nonpr<strong>of</strong>it organization that funds research inearly cancer detection, provided initial funding<strong>of</strong> $1 million to <strong>UT</strong> <strong>Southwestern</strong> for thefirst year <strong>of</strong> a biomarker project that is beingconducted at five sites across the country.The clinical problem is that lung cancer<strong>of</strong>ten cannot be detected until its advancedstages, and the average life expectancy <strong>of</strong>4SO<strong>UT</strong>HWESTERN MEDICINE 5
Lung cancer biology: getting down to the DNAsomeone receiving a lung cancer diagnosis isless than five years. It is a swift and stealthykiller, <strong>of</strong>ten with no early symptoms. Andunlike mammography for breast cancer,colonoscopy for colon cancer or PSA tests forprostate cancer, there is no routine screeningtest for early lung cancer.Mrs. Vasquez’s physician, Dr. Schiller, istrying to fix that.“The need for a comprehensive andprescribed way <strong>of</strong> detecting lung cancer earlyis crucial,” Dr. Schiller, pr<strong>of</strong>essor <strong>of</strong> internalmedicine said. “Older ways <strong>of</strong> screening justaren’t effective at catching lung cancer beforeit’s too late.”A study published Oct. 26, 2011, in theJournal <strong>of</strong> the American Medical Association foundthat routine chest X-rays do not reduce therisk <strong>of</strong> death from lung cancer in smokers orformer smokers. The NCI study involved morethan 150,000 older Americans. The finding wasstartling: Those who had annual chest X-rayscreenings over four years were just as likely todie <strong>of</strong> lung cancer as study volunteers who didnot get screened. In other words, chest X-raysare not useful in preventing lung cancer orseeing it early enough.Dr. Joan Schiller andher colleagues haveestablished a chestCT scanning programat <strong>UT</strong> <strong>Southwestern</strong>aimed at current andprior smokers ages 55years and older. Thescreening helps identifycancers beforethey become a seriousproblem.The findings suggest the best strategy fordiscovering lung tumors in an early, moretreatable stage is screening with computedtomography (CT) scans, which were shownin a separate recent study to lower the deathrate by 20 percent.To detect lung cancer earlier, the team ledby Dr. Schiller, Dr. Kemp Kernstine, Chair <strong>of</strong> theDivision <strong>of</strong> Thoracic Surgery and holder <strong>of</strong>Robert Tucker Hayes Foundation DistinguishedChair in Cardiothoracic Surgery, and Dr. HakChoy, chair <strong>of</strong> the Department <strong>of</strong> RadiationOncology and holder <strong>of</strong> the Nancy B. and JakeL. Hamon Distinguished Chair in TherapeuticOncology Research, have started a chest CTscreening program that allows qualified peoplewho are at risk to elect to have a spiral CT scandone. Team members Dr. Muhanned Abu-Hijleh, associate pr<strong>of</strong>essor <strong>of</strong> internal medicine,and Dr. Cecelia Brewington, pr<strong>of</strong>essor <strong>of</strong>radiology, designed the program, which also hasa research component to identify other meansfor detecting cancer earlier, in the breath, saliva,mouth cells and blood.While preventative CT scans are not yetcovered by insurance, they are recommendedfor current and prior smokers ages 55 and older.The test consists <strong>of</strong> one low-dose CT scan peryear for three years. Lung cancer is not the onlypotentially life-threatening disease the scan isable to detect. While scanning for lung cancer,CT scans also can reveal the presence <strong>of</strong> otherdiseases, such as heart disease, emphysema andother cancers that may originate in or havespread to the chest.“There are some caveats, but this representsan opportunity to catch lung cancer and otherdiseases very early, well before they become aserious problem,” Dr. Schiller said.Nearly a quarter <strong>of</strong> the patients will be foundto have suspicious findings, most <strong>of</strong> them notcancer. While patients are exposed to low doses<strong>of</strong> radiation, each scan’s radiation dose is lessthan a fifth <strong>of</strong> the dose <strong>of</strong> regular CT scans.The key is to see the cancer while there isstill time to do something about it, Dr. Schillersaid. In Mrs. Vasquez’s case, there was still timebut the window was rapidly closing.Attacking the enemy<strong>UT</strong> <strong>Southwestern</strong> leads a SPORE (SpecializedPrograms <strong>of</strong> Research Excellence) grant thatis shared with MD Anderson. Such grants arethe cornerstone <strong>of</strong> the NCI’s effort to promotecollaborative, interdisciplinary cancer researchand treatment. These grants involve both basicscientists and clinicians working on new waysRadiation therapy is a powerful tool in treating cancer, but asmany patients can attest, being treated with radiation is notwithout side effects.“Radiation is a double-edged sword that affects bothtumors and healthy tissues,” says Dr. Hak Choy, chairman<strong>of</strong> radiation oncology and holder <strong>of</strong> the Nancy B. and Jake L.Hamon Distinguished Chair in Therapeutic Oncology Research.“Therefore, it is imperative that we administer radiation ascarefully and as precisely as possible. If we didn’t have to worryabout the side effects <strong>of</strong> radiation, we could curealmost any cancer.”In order to deliver the most preciseand least harmful doses <strong>of</strong> radiation, theuniversity’s Department <strong>of</strong> Radiation Oncologyhas invested in leading-edge devices capable<strong>of</strong> treating cancers anywhere in the body (see“Brave New World: High Tech Medicine” onp. 18), while ensuring minimal damageto surrounding healthy tissue. The resultis fewer side effects for treatments that 10years ago would have been associated withextreme fatigue, skin changes, hair loss, mouththe division <strong>of</strong> molecular radiation biology and holder <strong>of</strong> theDavid A. Pistenmaa, M.D., Ph.D., Distinguished Pr<strong>of</strong>essorshipin Radiation Oncology, leads the five-year project to identify themolecular events that underlie the choice between pathwaysfor repairing DNA double-strand breaks (DSBs).Although normal human cells are exposed to multiple DNAlesions every day, the type <strong>of</strong> damage inflicted by radiation –double-strand breaks – is the most harmful. In this instance,both pairs <strong>of</strong> genes are broken, increasing the likelihoodthat the cell will either be unable torepair itself or that the genetic code willpass on damaged information during cellreplication.Human cells have two distinct methods torepair DSBs, and one <strong>of</strong> the major unresolvedquestions in the field <strong>of</strong> DNA research is whatmechanism determines the choice betweenthe two. The importance <strong>of</strong> these repairpathways is supported by the observationthat an increase in cancer incidence isassociated with impaired DSB repair.“The increased level <strong>of</strong> DNA damage inproblems and more.But these are only the visible effects <strong>of</strong>radiation. Radiation therapy works bydeliberately damaging the cellular DNA, whichultimately induces tumor cell death. WhileDr. David Chen and his team arestudying how DNA is repaired by thebody, with an eye toward mitigatingthe side effects <strong>of</strong> radiation and moreeffectively targeting tumors.cancer cells and the use <strong>of</strong> DNA-damagingagents in cancer treatment underlie theimportance <strong>of</strong> DSB repair in cancerbiology,” Dr. Chen says. “Basic mechanisticinsights into DSB repair mechanisms andDNA damage to the tumor is desirable, healthy tissue may alsobe subjected to DNA damage, which may result in side effectsranging from temporary irritation, to scarring, necrosis and even (inthe long term) giving rise to new cancers.Understanding how tumor and healthy tissue repair DNAdamage is an area that may significantly impact the future ability<strong>of</strong> physicians to mitigate such side effects while more effectivelytargeting tumors.In March, the Cancer Prevention and Research Institute <strong>of</strong> Texas(CPRIT) awarded $6.4 million to a multi-institutional groupled by a <strong>UT</strong> <strong>Southwestern</strong> researcher who has made historiccontributions to the field <strong>of</strong> DNA repair. Dr. David Chen, chief <strong>of</strong>the regulation <strong>of</strong> pathway choice for the repair <strong>of</strong> DSBs arelikely to translate into new opportunities for cancer treatment.”With the CPRIT money awarded to <strong>UT</strong> <strong>Southwestern</strong>, Dr.Benjamin Chen, assistant pr<strong>of</strong>essor <strong>of</strong> radiation oncologytogether with Dr. David Chen, will investigate whether activityat a specific amino acid cluster (the T2609 cluster) plays a rolein determining pathway choice. Another university researcher,Dr. Hongtao Yu, pr<strong>of</strong>essor <strong>of</strong> pharmacology, a Howard HughesMedical Institute investigator and a Michael L. RosenbergScholar in Medical Research, will study regulation <strong>of</strong> the DNArepair pathway choice by two other protein complexes that areinvolved in cell replication. Their individual projects are fundedat $1.3 million each.6continued page 86 SO<strong>UT</strong>HWESTERN MEDICINE 7
Dr. John Minnabelieves that<strong>UT</strong> <strong>Southwestern</strong>’sedge in personalizedcare comesfrom tailoringtreatment optionsto a molecularanalysis <strong>of</strong> eachpatient’s tumor.to prevent, detect and diagnose cancers, as wellas to treat them. The Simmons Cancer Centeris now headlong into an effort to identify themolecular hallmarks <strong>of</strong> lung cancer, with an eyetoward developing better drugs.The goal is to further personalize thetherapeutic options available to individualcancer patients who may be facing commoncancers with a unique set <strong>of</strong> characteristics.When combined with state-<strong>of</strong>-the-art methodsto test compounds against hundreds <strong>of</strong> differentcombinations <strong>of</strong> genetic mutations, a curefor certain cancers, such as lung, may bewithin reach.Dr. Michael White, pr<strong>of</strong>essor <strong>of</strong> cell biology,who is focused on uncovering the mechanisms bywhich cells can adversely react to their ownenvironment, said this represents a departurefrom the “guess-and-test” approach that hascharacterized a lot <strong>of</strong> the cancer biology thateventually moved into the clinical realm.Rather than “throwing spaghetti at the wallsto see what sticks,” Dr. White, who holds theSherry Wigley Crow Cancer Research EndowedChair, in Honor <strong>of</strong> Robert Lewis Kirby, M.D.and the Grant A. Dove Chair for Research inOncology, said <strong>UT</strong> <strong>Southwestern</strong> researchers aswell as colleagues elsewhere are tapping intoan array <strong>of</strong> genetics assays, cell lines and tumormodels that have exclusively been built at<strong>UT</strong> <strong>Southwestern</strong> over the years.Collaborating with leaders in biochemistryand pharmacology, Dr. White and hiscolleagues, Dr. Michael Roth, the interimdean <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong> Graduate School<strong>of</strong> Biomedical Sciences and vice chairman <strong>of</strong>biochemistry who holds the Diane and HalBrierley Distinguished Chair in BiomedicalResearch; Dr. Bruce Posner, associate pr<strong>of</strong>essor<strong>of</strong> biochemistry; and Dr. Minna are supportedby large grants from the National CancerInstitute and the Cancer Preventionand Research Institute <strong>of</strong> Texas (CPRIT).CPRIT has allowed these researchers tocross-test thousands <strong>of</strong> different compoundsand biological agents against different cancersranging from the ordinary to the exotic.As Dr. White points out, “combining ourhigh-throughput screening results with all <strong>of</strong>the molecular information we have assembledon lung cancers allows us to determine manynew therapeutic targets, which will change howwe approach lung cancer. This will also allow usto ‘personalize’ the use <strong>of</strong> these new therapiesby finding the right molecular match for eachpatient’s tumor – something we refer to as‘enrollment biomarkers.’”Researchers here and elsewhere believe thatthis is the most promising way in which socalled“translational” research is poised to crackthe cancer code and “catch up” with biology.“The doctors at <strong>UT</strong> <strong>Southwestern</strong> used acombination <strong>of</strong> drugs that was specificallytailored for my particular cancer,” Mrs.Gonzalez said. “I think the drugs that my otherdoctors would have put me on would not havebeen as effective.”Outwitting the enemySince feelings can be hard to see, theemotional component <strong>of</strong> a positive diagnosisis <strong>of</strong>ten the most difficult aspect <strong>of</strong> cancer t<strong>of</strong>ully appreciate. The marshaling <strong>of</strong> spiritualresources needed to take on a war againstcancer is a battle with which Mrs. Vasquezand Mrs. Gonzalez are intimately familiar.“Patients <strong>of</strong>ten are looking for things thatgive them hope and a sense <strong>of</strong> control,” said Dr.Simon Craddock Lee, a medical anthropologistwho focuses on cancer disparities andpatient decision-making, and a member <strong>of</strong>the Population Sciences and Cancer ControlProgram within the Simmons Cancer Center.“Oncologists do their best to communicatethe options for patients while supportingthem in their right to decide the best course<strong>of</strong> treatment. In comprehensive cancer care, acadre <strong>of</strong> experts works with oncologists to try toaddress all the different needs <strong>of</strong> a patient.”To this end, the Simmons Cancer Centerhas a growing, multifaceted support programdesigned to work in concert with oncologistsand their patients from the very moment <strong>of</strong>diagnosis.“This is where our program is distinct fromother cancer care support programs,” said Dr.Jeff Kendall, associate pr<strong>of</strong>essor <strong>of</strong> psychiatryand the clinical leader <strong>of</strong> the supportive servicesprogram at the center. “Rather than beingmentioned as an afterthought to treatment, webring support services to the fore right away, asa seamless complement to treating the wholepatient, perhaps before he or she even realizes itis necessary.”The new direction in cancer care todayis treating the “whole patient,” Dr. Kendallnotes. This treatment model means recognizingthe importance <strong>of</strong> the emotional, social andspiritual changes that <strong>of</strong>ten accompany adevastating diagnosis <strong>of</strong> cancer and the effectthe illness can have on an entire family.However, recognition is not enough. It is justas important to intervene once certain needshave been identified, he said.Efforts by Dr. Kendall and his staff havesought to raise awareness and identifyemotional issues in cancer care through“psychosocial distress screening” interviewswith patients. In a sense, Dr. Kendall isattempting to see any signs <strong>of</strong> distress in hispatients while there is time to intervene.The stress associated with a cancer diagnosishas been shown to cause considerablepsychological morbidity, with 25 percent to50 percent <strong>of</strong> all cancer patients indicatingsignificant levels <strong>of</strong> distress.“While our advances in cancer research andtreatment continue at a steady pace, patientsnow face more complex treatment decisionsand follow-up options,” said Dr. James K.V.Willson, director <strong>of</strong> the Simmons CancerCenter and holder <strong>of</strong> the Lisa K. SimmonsThe Harold C. Simmons CancerCenter is one <strong>of</strong> only seven in thenation to obtain a prestigiousSpecialized Program <strong>of</strong> ResearchExcellence (SPORE) grant from theNational Cancer Institute.Distinguished Chair in ComprehensiveOncology. “<strong>UT</strong> <strong>Southwestern</strong> has a caring staff<strong>of</strong> medical pr<strong>of</strong>essionals who are committedto enhancing patients’ quality <strong>of</strong> life, as wellas meeting the needs <strong>of</strong> patients’ families. Akey component <strong>of</strong> our mandate as an NCIdesignatedcancer facility is that we meet allaspects <strong>of</strong> a patient’s total care. Support servicesare a key element in that.”After undergoing a lobectomy to remove thepart <strong>of</strong> her lung that was cancerous, followed bya chemotherapy and radiation regimen at theSimmons Cancer Center, Mrs. Vasquez still seesher doctors regularly.“When I was diagnosed and decided tostart going to <strong>UT</strong> <strong>Southwestern</strong>, people said,‘Why do you keep going there? It’s too far!’” sherecently recounted. “The fact that I bonded sowell with Dr. Schiller and that they still checkon me is why. Of course, having cancer hasmade me more religious. I thank God for thecare I get there.”8SO<strong>UT</strong>HWESTERN MEDICINE 9
BY LAKISHA LADSONDespite the notion that heart disease occurs withoutwarning, <strong>UT</strong> <strong>Southwestern</strong> Medical Center cardiologistsare discovering that the nation’s No. 1 killer doesindeed send silent signals <strong>of</strong> impending cardiovasculardisease decades before seemingly healthy people realizetheir lives are under assault.The murderer’s many weapons, which includeatherosclerosis, heart attack, stroke and congestiveheart failure, may be noted through silent cues fromblood-based tests, advanced imaging scans and possiblyeven a person’s capacity to exercise.“We’re discovering risk factors that are clear andcompletely silent,” said Dr. Darren McGuire, associatepr<strong>of</strong>essor <strong>of</strong> internal medicine at <strong>UT</strong> <strong>Southwestern</strong>.“People feel fine even when the classic risk factors forcardiac disease are diagnosed, such as increasedblood pressure, abnormal cholesterol or diabetes.Uncovering these silent signals that become abnormallong before disease is evident gives us opportunitiesto create therapies to intervene before heart diseasedisables or ends a person’s life.”The Nation’sNo.1 KillerSends SilentSignalsSO<strong>UT</strong>HWESTERN MEDICINE 11
Drs. Jarett Berry,Sachin Gupta<strong>of</strong> cardiology, said the multiyear investigationmirrors the populations <strong>of</strong> most U.S. cities.“One <strong>of</strong> the many strengths <strong>of</strong> the Dallas HeartStudy is that important findings can be used atthe community level.”While the study’s findings will be a source <strong>of</strong>scientific information for many years to come,<strong>UT</strong> <strong>Southwestern</strong> cardiologists also are exploringother avenues to reduce health risks. One <strong>of</strong> themore intriguing is the interplay between exerciseand heart disease.Most people have heard and accept that ifthey exercise they might be able to stave <strong>of</strong>fdiabetes, obesity and heart disease for a while.Moving beyond these general benefits, <strong>UT</strong> <strong>Southwestern</strong>researchers, in conjunction with theCooper Institute <strong>of</strong> Dallas, have found that thelevel and intensity <strong>of</strong> exercise a person can doon a treadmill may actually tell how likely theyare to die decades later from heart disease.Researchers analyzed the heart disease risk <strong>of</strong>45-, 55- and 65-year-old men based on theirfitness level and traditional risk factors – age,systolic blood pressure, diabetes, total cholesteroland smoking habits – and found that low levels <strong>of</strong>midlife fitness, measured by how fast and longsomeone could exercise, are associated withmarked differences in lifetime risk for cardiovasculardisease. Higher fitness levels lowered thelifetime risk <strong>of</strong> heart disease even in people withother risk factors.Researchers also found the same treadmilltest predicts how likely a person is to die <strong>of</strong>heart disease or stroke more accurately thanassessing the risk using only traditionalprediction tools.For this work, the American HeartAssociation (AHA) gave the Elizabeth Barrett-Connor Research Award in Epidemiology to Dr.Sachin Gupta, postdoctoral trainee in internalmedicine. The award is one <strong>of</strong> the AHA’s mostprestigious awards, recognizing excellence inresearch by an early-career investigator.“Our study shows that fitness level measuredin middle age can significantly improverisk prediction algorithms and help to identifyindividuals at risk for cardiovascular deathboth in the short term and in the long term,”Dr. Gupta said.This trial has great potential for everyone butspecial significance for youth and women, whohave fewer prediction tools to assess long-termcardiovascular risk.“Nearly all women in the U.S. less than 50years <strong>of</strong> age are at low risk for heart disease,”said Dr. Berry, a Dedman Family Scholar inClinical Care. “As women get older, however,their risk increases dramatically. In our study,we found that low levels <strong>of</strong> fitness were particularlyhelpful in identifying women at riskfor heart disease over the long term.”<strong>UT</strong> <strong>Southwestern</strong>, Cooper partnerThese studies were done in conjunctionwith the Cooper Institute, which has compileddata on exercise and fitness from healthyvolunteers for 40 years. <strong>UT</strong> <strong>Southwestern</strong> hasa partnership with the institute, the preventivemedicine research and educational nonpr<strong>of</strong>itlocated at the Cooper Aerobics Center, todevelop a joint scientific medical researchprogram aimed at improving health andpreventing a wide range <strong>of</strong> chronic diseases.The hallmark study from the institute – theCooper Center Longitudinal Study – includesdetailed information from more than 250,000clinic visits that has been collected since Dr.Kenneth Cooper founded the institute andclinic in 1970.Large population studies like Dallas Heartand Cooper Center Longitudinal allowresearchers to examine not only factorscontributing to disease but, more importantly,factors that promote cardiovascular health.“We’re as interested in the protective factorsas the harmful ones,” Dr. de Lemos said. “Forexample, we are going to learn a huge amountfrom people who live their whole lives overweightor obese yet never develop cardiovascularcomplications – we’ve found a lot <strong>of</strong> peoplelike that in our study.”Doctors now are bringing these tests forsilent signals <strong>of</strong> heart disease to fruition and seeinghow they work in the real world. For example,<strong>UT</strong> <strong>Southwestern</strong> researchers have founddifferences in blood levels <strong>of</strong> C-reactive protein(CRP) according to race or sex. CRP is a marker<strong>of</strong> inflammation and has been heavily toutedas a test to improve prediction <strong>of</strong> heart attacks.“White woman have higher levels <strong>of</strong> CRPthan both black and white men,” Dr. Kherasaid. “Since white women have lower rates <strong>of</strong>cardiovascular disease, this study raises somequestion about how to best use CRP in thereal world.”Dr. Khera said some tests may call fordifferent thresholds between men and womento determine more accurately the risk <strong>of</strong> heartdisease, and that overreliance on CRP for riskassessment in African-American patients mayoverestimate risk for cardiac and vascularevents, since more than one-half <strong>of</strong> thesepatients had elevated levels.Some <strong>of</strong> these signals are stronger for certaintypes <strong>of</strong> heart disease: calcium scanning forincreased risk <strong>of</strong> heart attack, fitness level andcardiac troponin T detection for heart failure.“We believe that combining imaging testswith protein tests is going to help identifypeople who feel perfectly well but who willhave notably increased risk <strong>of</strong> heart complicationsdown the line,” Dr. de Lemos said.The findings about fitness are now availableand can be accessed at www.lifetimerisk.org.On this website, an individual can help determinehis or her lifetime risk for cardiovasculardisease by entering their age, sex, fitness leveland other risk information.“Fitness has the potential to have a largeimpact because everybody can do it,” Dr. Kherasaid. “Fitness is relatively easy to measure,costs very little to improve, and people wantalternatives to medicines.”Cardio health balance delicateEven though heart disease is the leadingcause <strong>of</strong> death in the U.S., its incidence isdeclining in large segments <strong>of</strong> the generalpopulation due to decreases in cigarettesmoking and improved cholesterol levels.The nation’s aging population and its risingobesity epidemic, however, run counter tohealth-conscious gains.“Every adult in America is potentially atrisk for heart disease in some form or fashion.Once you have a heart attack, the risk foradditional heart problems down the road ismuch higher,” said Dr. Khera, co-chair <strong>of</strong> theAmerican Heart Association’s state advocacycommittee. “We’re proud that we’re doing thework on the front end to make sure the horsenever leaves the barn.”Increased screening is one solution, buteven then, approved implementation will bechallenging.“Without clear guidance and acceptedalgorithms for test interpretation, there ispotential for both inappropriate under-treatmentand over-treatment <strong>of</strong> individuals basedon test results,” Dr. Khera said. “Still, we thinkcritically and carefully about how to helpidentify those people who seem healthy, butare at increased risk <strong>of</strong> heart disease later on.”As long as heart disease remains rampant,<strong>UT</strong> <strong>Southwestern</strong> researchers will work toprevent it, tweaking traditional predictiontools and creating new ones as a preemptivestrike against heart disease to eliminatesneak attacks in people without obvioussymptoms <strong>of</strong> disease.“We’ve learned a lot already about discoveringthe silent signals <strong>of</strong> the heart,” Dr. deLemos said, “and have great hope that biggerthings will come.”Dr. Amit KheraSO<strong>UT</strong>HWESTERN MEDICINE17
Brave New World:High TechMedicine<strong>UT</strong> <strong>Southwestern</strong> innovateswith many different technologiesto advance medical discoveryand revolutionize patient careBy Debbie Bolles
Using advancedtechnology, such asthis recently installedpositron emissionmammography (PEM)device used for breastcancer detection,Dr. Robert Lenkinskiplans to test newimaging agents that willprovide more detaileddisease information.By modifying the settings <strong>of</strong> the magnetduring an MRI scan, Dr. Changho Choi, associatepr<strong>of</strong>essor <strong>of</strong> radiology in the AdvancedImaging Research Center (AIRC), enhanced themagnetic resonance spectroscopy and identifieda protein that accumulates in the tumor cells<strong>of</strong> patients such as Mr. Smith with a specificgenetic mutation. When Mr. Smith’s symptomsworsened, his doctors noted huge spikes <strong>of</strong> thisprotein showing up on a research study scan.They have since treated the tumor and the levels<strong>of</strong> this protein have fallen. Mr. Smith now walkswithout difficulty and his seizures are gone.“This marks the first time a mutational biomarkerhas been identified through imaging,”said Dr. Elizabeth Maher, associate pr<strong>of</strong>essor <strong>of</strong>internal medicine and neurology and neurotherapeutics,and the lead investigator in thisclinical trial. “It is a major breakthrough inour ability to treat patients.” Dr. Maherholds the Theodore H. Strauss Pr<strong>of</strong>essorshipin Neuro-Oncology.<strong>UT</strong> <strong>Southwestern</strong> researchers and cliniciansdaily are using new imaging technology toimprove diagnosis and treatment, <strong>of</strong>ten probingdisease processes at the molecular level. Otherimaging innovations at the medical centerinclude more precise and less invasive imagingtools, development <strong>of</strong> contrast agents thatliterally “light up” disease processes never beforeseen and application <strong>of</strong> imaging devices fornonsurgical treatments.Dr. Neil R<strong>of</strong>sky, chairman <strong>of</strong> radiology,expects imaging technologies to become morepervasive in medical procedures and diagnostictests as advancements continue.“We’ll be able to visualize processes at alevel previously impossible and be able to usethat information in real time to make decisionsabout therapies that may optimize efficaciesfor patients,” said Dr. R<strong>of</strong>sky, who holds theEffie and W<strong>of</strong>ford Cain Distinguished Chair inDiagnostic Imaging.One example <strong>of</strong> this type <strong>of</strong> microscopicdetail involves how researchers at the AIRC aredeveloping hyperpolarized solutions for usein MRIs. Pyruvate, a naturally occurring metabolite,or small molecule, can be manipulated toincrease its sensitivity to MR signals, includingwhen it metabolizes into lactate. Lactate isproduced during cellular respiration as glucosebreaks down.“It’s a complicated method for increasingthe MR signal <strong>of</strong> specific molecules in metabolicpathways. You inject those, and you can see asignal you otherwise would not see,” said Dr.Robert Lenkinski, pr<strong>of</strong>essor and vice chairman<strong>of</strong> research in radiology, who is testing hyperpolarizedagents, along with Dr. Dean Sherry,pr<strong>of</strong>essor <strong>of</strong> radiology and director <strong>of</strong> the AIRC,and Dr. Craig Malloy, pr<strong>of</strong>essor <strong>of</strong> internalmedicine and radiology in the AIRC and holder<strong>of</strong> the Richard A. Lange Chair in Cardiology.After injecting hyperpolarized pyruvate intothe body intravenously, doctors can potentiallysee how much <strong>of</strong> a person’s heart muscle ismetabolizing well, based on the MR image <strong>of</strong>pyruvate’s changes.“You can tell which part <strong>of</strong> the heart isdoing well and which is not. That will help indesigning an intervention or drug, or assessingif a treatment is working,” said Dr. Lenkinski.In similar research but using differenttechnology, Dr. Sumer, the robotic surgery expertfor head and neck cancer removal, is workingwith Dr. Jinming Gao, pr<strong>of</strong>essor <strong>of</strong> pharmacologyin the Harold C. Simmons ComprehensiveCancer Center, to develop nanotechnologybasedfluorescent contrast agents for MR cancerimaging. Using imaging agents, the researchershave developed injectable pH-sensitivenanoparticles that light up with fluorescence inthe low-pH tumor environment. Because mostsolid cancers are slightly acidic, this <strong>of</strong>f-to-onmechanism fluorescently identifies the tumor’sborders, allowing the surgeon to remove thecancer more accurately.The research team also is creating nanoparticleswith targeting proteins on their surfacethat will direct the nanoprobes to bloodvessels feeding a tumor, stromal cells aroundthe tumor, and the cancer cells themselves.Still to come, another research team willdevelop tracers for positron emission tomography(PET) used in cancer diagnosis andtreatment. Dr. Xiankai Sun, assistant pr<strong>of</strong>essor<strong>of</strong> radiology, plans to use funds from a CancerPrevention and Research Institute <strong>of</strong> Texasgrant to purchase a biomedical cyclotron, amachine that produces radioisotopes for production<strong>of</strong> PET tracers. Medical institutions orresearch centers that have their own cyclotronscan produce a variety <strong>of</strong> PET tracers on-site forimmediate use.Taking advantage <strong>of</strong> new imaging technologyremains a priority at <strong>UT</strong> <strong>Southwestern</strong>.In October 2011, the first positron emission“ This marks the first time a mutational biomarkerhas been identified through imaging.”mammography (PEM) unit was installed atthe Mary Nell and Ralph B. Rogers MagneticResonance Imaging Center on the NorthCampus. This technology helps pinpoint cancerin women with dense breast tissue and showstumor characteristic detail.Imaging technology also has expanded tonovel treatment methods. A new type <strong>of</strong>ultrasound uses the heat <strong>of</strong> high-intensityfocused ultrasound (HIFU) waves for noninvasivesurgery, such as uterine fibroid removal.<strong>UT</strong> <strong>Southwestern</strong> researchers also plan to testMR-guided HIFU for prostate cancer treatment.“A tremendous amount <strong>of</strong> energy isdeposited in a very tiny spot. We irradiatewith ultrasound,” Dr. R<strong>of</strong>sky said.Revolutionizing radiation therapyAs associate pr<strong>of</strong>essor <strong>of</strong> health studies at TexasWoman’s University, Dr. Kristin Wiginton isquite knowledgeable regarding the latest medicaltechnology. She never imagined, however,becoming a pioneer in testing a new radiationtreatment for breast cancer.After being diagnosed, Dr. Wiginton faced adifficult decision. Because heart disease runs inher family, she knew that traditional radiation—Dr. Elizabeth Maher2223
therapy potentially could damage her heart. Soshe took a risk, becoming the first woman toparticipate in a clinical trial at <strong>UT</strong> <strong>Southwestern</strong>using precisely focused high-beam radiation totreat breast cancer. After five radiation treatmentsin 2011, the results are encouraging. Thestudy still is under way.“I feel I made the right decision volunteeringfor this clinical trial,” said Dr. Wiginton. “Allin all, I think my recovery and comfort levelshave been much better than if I had gonethrough traditional whole-breast radiation.”This first trial in the region using the AccurayCyberKnife System not only cut treatment timeby 83 percent for Dr. Wiginton and other trial“ We are the pioneers in advancedtechnology We are the pioneers in radiation in advanced oncology, buttechnology there is a fine radiation line between oncology, curing butthere cancer is and a fine preserving line between quality curing <strong>of</strong> life.”cancer and preserving quality <strong>of</strong> life.”—Dr. Hak Choyparticipants, it also illustrates the real results<strong>of</strong> cutting-edge research into new radiationtherapies and technologies embraced by<strong>UT</strong> <strong>Southwestern</strong>.“We are the pioneers in advanced technologyin radiation oncology, but there is a fine linebetween curing cancer and preserving quality<strong>of</strong> life,” said Dr. Hak Choy, chairman <strong>of</strong>radiation oncology and holder <strong>of</strong> the NancyB. and Jake L. Hamon Distinguished Chair inTherapeutic Oncology Research.The balancing act means killing as muchcancer as possible with radiation while minimizingharm to healthy tissue. It’s a challengethat <strong>UT</strong> <strong>Southwestern</strong> radiation oncologistsface and make advancements in constantly.The stars in <strong>UT</strong> <strong>Southwestern</strong>’s radiationoncology arsenal include the Gamma KnifePerfexion system, which effectively treatsmultiple tumors in the brain, the CyberKnifehigh-beam radiation system and the Vero, amachine that directs radiation precisely whereneeded through stereotactic body radiationtherapy, or SBRT.Without the human element, however, suchmachinery would be useless. Some <strong>of</strong> themost renowned radiation oncology experts inthe country conduct breakthrough research at<strong>UT</strong> <strong>Southwestern</strong>, including Dr. Robert Timmerman,vice chairman <strong>of</strong> radiation oncologyand pr<strong>of</strong>essor <strong>of</strong> neurological surgery.Dr. Timmerman, one <strong>of</strong> the nation’s top expertson SBRT, led the CyberKnife breast cancertrial and currently is co-leading a multi-institutionalstudy comparing the effectiveness <strong>of</strong>minimally invasive surgery versus SBRT in 400non-small cell lung cancer patients.“In the past, patients have been <strong>of</strong>feredlimited treatment options for this highly deadlydisease,” said Dr. Timmerman, holder <strong>of</strong> theEffie Marie Cain Distinguished Chair in CancerTherapy Research. “This trial will show us howbest to deploy both therapies and optimizethem for a given patient.”In a related study, Dr. Timmerman also istesting hyp<strong>of</strong>ractionated image-guided radiotherapyon non-small cell lung cancer patients.This type <strong>of</strong> treatment uses advanced imaging,motion control and dosimetry principlesto deliver treatments at higher doses, andwith more precision. These methods includemonitoring movement <strong>of</strong> lung cancer tumorsthrough imaging techniques as a patientbreathes and then adjusting radiation beamsaccordingly.Since most tumors are closely situatedwithin normal tissues, potent radiation can bea double-edged sword. With these and otheradvances, however, radiation therapy is becomingfaster, safer and more precise, as well as lessrecovery-intensive for patients.A picture in Dr. Choy’s <strong>of</strong>fice <strong>of</strong> a radiationtherapy machine used to treat a boy for ringwormat an Italian hospital in 1903 is a starkreminder <strong>of</strong> just how far this technology hasevolved. In his 20-plus years as a radiationoncologist, Dr. Choy has seen significant advancements– such as radiation treatments evolvingfrom inpatient to outpatient procedures.“We are truly the most sophisticated centerfor radiation therapy. Our patients come fromall over the world seeking the best technologyand the experts in the field,” Dr. Choy said.For his part, Mr. Perdue says he’s an idealexample and an avid proponent <strong>of</strong> the benefits<strong>of</strong> such high tech medical delivery.“There are so many new and better waysto do things. We, as patients, need to be opento those new findings and techniques,” he said.“If we’re not, I think we’re missing the boatand making a grave mistake.”Researchers develop effective radiation protocolwith fewer treatments | by Robin RussellYour doctor diagnoses you with prostate cancer, and your mind reels. You are scared, worry about loss <strong>of</strong>sexual function and maybe don’t even want to discuss it.Men diagnosed with low-risk prostate cancer currently must consider several treatment options – activesurveillance, radiation therapy, surgical removal <strong>of</strong> the gland – for this typically slow-growing disease.For those who choose radiation therapy, treatments for localized prostate cancer typically take 42 to 45days, spanning eight to nine weeks.Thanks to <strong>UT</strong> <strong>Southwestern</strong> Medical Center researchers using the latest technologies in a series <strong>of</strong> clinicaltrials, however, new protocols are being discovered.In a recent multicenter trial, researcherstweaked increasingly higher doses <strong>of</strong> ultra-preciseradiation known as stereotactic body radiationtherapy (SBRT), and found it safe and effective forpatients with low- to intermediate-risk prostatecancer, with fewer treatments needed.The linchpin <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>’s SBRTprogram is the Vero. Installed in 2011, it is theonly one in North America. The system – whichinitially is being used to treat patients withprostate and lung cancer – combines threedifferent imaging technologies with a gimbaledX-ray delivery head, allowing physicians to followand treat a moving target safely.“The Vero gives us the most precise linearaccelerator that can spare normal tissuewhile taking care <strong>of</strong> cancer,” said Dr. Hak Choy,chairman <strong>of</strong> radiation oncology.Trial researchers used SBRT to treat patientswith localized prostate cancer in just five 30-minute sessions every other day, over the course <strong>of</strong> two weeks.“We were trying to develop a fast, convenient, outpatient, non-invasive treatment without injuringthe urethra, the bladder or the rectum,” said Dr. Robert Timmerman, vice chairman <strong>of</strong> radiation oncologyand pr<strong>of</strong>essor <strong>of</strong> neurological surgery.Prostate cancer is the most common cancer in men, with some 230,000 cases diagnosed annually in theU.S. About half <strong>of</strong> those who are treated undergo radiation therapy. Not everyone is cured, however, becausesome tumors are resistant to radiation.SBRT has been used effectively for patients with lung, liver and brain cancers. The <strong>UT</strong> <strong>Southwestern</strong>study tested whether high-potency treatments could work in a moving target like the prostate, which shiftsconsiderably due to normal bladder and bowel functioning.To avoid injuring healthy tissue, researchers used beams <strong>of</strong> radiation that were only millimeters largerthan the target itself. That narrow scope helped avert consequences such as rectal injury, impotence anddifficulty urinating.The second phase <strong>of</strong> the clinical trial, completed in fall 2010, increased the dosage in participants by10 percent. More than 90 percent <strong>of</strong> the 50 patients involved tolerated the therapy well.Following clinical trials, <strong>UT</strong> <strong>Southwestern</strong> researchers will work with a multicenter consortium to developa next-step protocol to further improve the therapy.Dr. Robert Timmermantalks with radiationtherapist Lindsay Henryabout the Vero, the latestimaging technologyin <strong>UT</strong> <strong>Southwestern</strong>’sarsenal <strong>of</strong> stereotacticbody radiation therapyequipment.24SO<strong>UT</strong>HWESTERN MEDICINE25
MOMENTSDISCOVERYOFBy Dr. Bruce A. Beutler, as told to Deborah WormserIn 1993, Dr. Bruce Beutler – one <strong>of</strong><strong>UT</strong> <strong>Southwestern</strong> Medical Center’sfirst Howard Hughes MedicalInstitute (HHMI) investigators –embarked on a five-year journeythat led to his discovery <strong>of</strong> howthe innate immune system recognizesand responds to infectionin mammals, an achievement thatearned him the 2011 Nobel Prize inPhysiology or Medicine. Dr. Beutlerrecently returned to <strong>UT</strong> <strong>Southwestern</strong>as director <strong>of</strong> the newCenter for the Genetics <strong>of</strong> HostDefense and holder <strong>of</strong> theRaymond and Ellen Willie DistinguishedChair in CancerResearch, in Honor <strong>of</strong> Laverneand Raymond Willie Sr. Here, hedescribes the painstaking workthat led to his discovery and thepressures bearing down uponhim in the summer <strong>of</strong> 1998.
Dr. Beutler’s father transformshis son’s fascinationwith nature into a quest forknowledge“My father encouraged me to go to medical school.And I am glad that he did.”My interest in science was sparked at an earlyage. When I was quite young I was interested innature, especially animals, and kept lists <strong>of</strong>birds I had seen. I still go birding when I have achance. I think the first spark <strong>of</strong> interest inscience had to do with the aesthetic pleasure <strong>of</strong>nature. One day, my father (scientist Dr. ErnestBeutler) suggested that what I was doing wasobservation rather than science. He explainedthat science meant asking specific questionsand addressing them through experimentationin order to gain insight into how things work.My father was a distinguished biomedicalresearcher, a member <strong>of</strong> the National Academy<strong>of</strong> Sciences and winner <strong>of</strong> many awards. WhenI was about 14, I began working in his laboratoryat the City <strong>of</strong> Hope Medical Center in Duarte,Calif. There I learned a great deal about how topurify proteins and analyze them, and also afair amount about genetics. I loved lab workand devoted myself to it as much as I could.I graduated early from high school and hada lot <strong>of</strong> advanced placement credit when, at 16,I went to college at the University <strong>of</strong> California,San Diego (UCSD), so I finished in two years.I certainly learned a lot about basic science, includinggenetics, at UCSD. But I was in a greathurry and actually looked on college, with itsmany humanities requirements, as an impedimentto becoming an independent researcher.I first learned about endotoxin, also knownas lipopolysaccharide (LPS), from UCSD pr<strong>of</strong>essorDr. Abraham Braude [associate pr<strong>of</strong>essor <strong>of</strong>internal medicine from 1953 to 1957 at whatwas then <strong>Southwestern</strong> Medical School <strong>of</strong>the University <strong>of</strong> Texas]. Later, understandingLPS formed the core <strong>of</strong> myresearch, but at that time it wasjust a casual introduction. Ididn’t see it in its full contextin those days. I saw itmore as a laboratoryAt the age <strong>of</strong> 14,Bruce Beutler beginsworking in his father’slaboratory at theCity <strong>of</strong> Hope MedicalCenter in Duarte,Calif.curiosity and didn’tknow how importantit was in immunity andin disease.My father encouragedme to go tomedical school, and Iam glad that he did.At the University <strong>of</strong>Chicago School <strong>of</strong>Medicine, I learnedabout the principalchallenges in biomedicine, which tend to changequite slowly over time. I was one <strong>of</strong> thosepeople who went to medical school to learnabout the pathogenesis <strong>of</strong> disease and to understandwhat the big questions were.I first came to <strong>UT</strong> <strong>Southwestern</strong> in 1981when I was matched to the house staff trainingprogram (internship). <strong>UT</strong> <strong>Southwestern</strong> wasmy first choice because I knew that I would getoutstanding training here. And I did.Dr. Donald Seldin was one <strong>of</strong> my teachers,along with Dr. Daniel Foster, Dr. Jean Wilsonand other greats <strong>of</strong> medicine and biomedicalscience. I spent a year as an internal medicineintern, and then a year as a neurology resident.The neurology program was run byDr. Roger Rosenberg, who had made a strongpitch to recruit me.Infection connectionDuring my clinical training, I saw what aproblem infection could be. Remember, I hadlearned something about LPS – endotoxin –from Dr. Braude and I began to think about itquite a lot in clinical terms, and to take note<strong>of</strong> the damage it could do. LPS is released fromGram-negative bacteria, sometimes evenmore after antibiotic therapy has begun thanbeforehand, and it causes fever, shock, abnormalities<strong>of</strong> blood coagulation and organ injury.This process is usually what kills, not theinfection. I began to wonder why that was.Did the bacteria utilize LPS as a virulencefactor? Or was it simply a structural element,and in that case, was it the host reaction thatwas excessive? And why would excessivereactivity be retained in the course <strong>of</strong> evolution?At that point, it hadn’t really occurred to meto address the question.After two years <strong>of</strong> residency, I went toRockefeller University, where my work demonstratedthat tumor necrosis factor (TNF), aninflammatory protein the body produces inresponse to pathogens, is an extremely importanteffector protein <strong>of</strong> the innate immunesystem. It plays a part both in inflammationand in resisting infection. And it turned out tobe an excellent therapeutic target: TNF blockadeis now a standard way <strong>of</strong> treating manyinflammatory diseases.I returned to <strong>UT</strong> <strong>Southwestern</strong> in 1986 asan assistant pr<strong>of</strong>essor.With the passage <strong>of</strong> time, I realized that thekey question about innate immune responses,especially where infection was concerned butperhaps more generally too, was “how iseverything started?”How is it that LPS activates the macrophage,which then makes TNF? What’s the receptorfor LPS? And how do we become aware <strong>of</strong> aninfection during the first minutes or hoursafter we encounter microbes? In reality, theseare all variants <strong>of</strong> the same question.Our work was fairly fruitless from 1988 to1992 because <strong>of</strong> the way we went about it.We tried to use classical immunological methodsto find the difference between certain micethat couldn’t respond to LPS and other micethat could. We also used analytical biochemistryand we used expression cDNA cloning.None <strong>of</strong> these methods led anywhere.Applying geneticsThe real epiphany for me was embracing classicalgenetics, starting in 1993, to try to solvethe problem. And that was not accidental. Idon’t think I would have done it just anywhere.Genetics was so much a part <strong>of</strong> life here at<strong>UT</strong> <strong>Southwestern</strong>, and it was also a place whereone could quickly learn about what everyoneelse was doing. The students in my lab wouldtalk to students in other labs; there were reallyno barriers. And they would come back andchat with me about the latest innovations andabout how to get things done.First learns aboutendotoxin, also known aslipopolysaccharide (LPS)Graduates from UCSDwith bachelor’s <strong>of</strong> arts,biology, at the age <strong>of</strong> 18Enrolls in the University <strong>of</strong> California,San Diego, at the age <strong>of</strong> 1619641972197419762829
First comes to<strong>UT</strong> <strong>Southwestern</strong> asan internThere were three somewhatoverlapping phasesto our work: genetic mapping,physical mappingand gene identification.In the first phase, wehad to localize the mutationto a point betweentwo markers on the chromosome.This involveda lot <strong>of</strong> breeding <strong>of</strong> mice,and analysis <strong>of</strong> whetherthey would respond to LPS.In the second phase,we had to clone all theDNA between those twomarkers – about 2.6 millionbase pairs as weoriginally estimated. This involved isolatinghuge pieces <strong>of</strong> DNA in bacterial artificialchromosomes (BACs) and yeast artificial chromosomes(YACs).And in the third phase, we had to discoverthe gene content <strong>of</strong> those BACs and YACs,then search for a mutation in each <strong>of</strong> the geneswe found to find the change in the genomethat caused resistance to LPS in the C3H/HeJstrain <strong>of</strong> mouse. One must remember thatin those days, the entire genome <strong>of</strong> the mousewas terra incognita; there was not even anaccurate estimate <strong>of</strong> the number <strong>of</strong> genes, letalone what they might be.Each phase was tough but each in a differentway. I think the last two phases were thehardest. We mostly identified genes by sequencingthe DNA, and sequencing 2.6 millionbase pairs <strong>of</strong> DNA – about 0.1 percent <strong>of</strong> thegenome – was a real grind in an academiclab. Not only that, but today we know thesize was really about twice what we thought;about 5.2 million base pairs <strong>of</strong> DNA. It wasan assembly line. Someone would isolateBAC clones using markers within thecritical region. Someone else wouldshear BACs with ultrasound andmake libraries <strong>of</strong> the DNAfragments, cloning theminto Escherichia coliFinishes an internship in internal medicine andstarted a residency in neurology (1982-1983)(E. coli), and plating the libraries on agar. Yetanother would pick colonies and inoculatebroth to grow each colony in liquid culture,then prepare DNA for sequencing from culturesthat had grown the day before. Someone elsewould sequence the purified DNA.I myself spent much <strong>of</strong> my time analyzingthe sequence, and writing computer scriptsto facilitate this. I should mention that Drs.Alexander Poltorak and Irina Smirnova, mypostdoctoral researchers at that time and nowindependent scientists at Tufts University,were the tireless heroes <strong>of</strong> this effort, andwithout them, we surely would not have foundthe mutation.Sequencing in the earliest days was donewith radioactive nucleotides. You’d get a ladder<strong>of</strong> bands on a gel and you’d expose it overnightto X-ray film and read <strong>of</strong>f the base pairsthe next day. Betsy Layton, my administrativeassistant, would read and I would type or viceversa. We would read about 4,000 to 5,000bases <strong>of</strong> DNA in a morning, and that wouldbe about the limit a person could toleratereading in one day. Your eyes wouldget tired. Today’s methods can“There were three somewhat overlapping phases toour work: genetic mapping, physical mapping andgene identification.”deliver about 1 million base pairs per second,and certainly nothing <strong>of</strong> the kind we attemptedwill ever be done again.We were reading sequence in this manner in1993 and 1994. Then, using my own funds, Ibought a used ABI 373XL sequencer. That allowedus to sequence about 40,000 base pairsper day if we ran the machine around the clock.And we decentralized our sequencing also,farming it out to numerous core laboratories.Working around the clockWe worked most weekends, and we’d also workuntil late at night. We would look at theresults <strong>of</strong> the Basic Local Alignment Search Tool(BLAST) searches from sequencing that hadbeen done during the day. We would see if ourgenomic sequences had matches in an expressedsequence tag (EST) database. We used bothdbEST (database <strong>of</strong> Expressed Sequence Tags),which was public, and we used the TIGR (TheInstitute for Genomic Research) database,which was proprietary.Both <strong>of</strong> those were databases <strong>of</strong> complementaryDNA (cDNA) sequences, meaning theyrepresented the parts <strong>of</strong> the genome that wereknown to be expressed as messenger RNA.The idea was to look for genes that way. If youBLAST a genomic DNA sequence and it hasan EST match, that part <strong>of</strong> the genome is expressedand is part <strong>of</strong> a gene (with certain caveats;nothing is absolutely certain).Starts research career at RockefellerUniversity where he is lead author <strong>of</strong>the first study to demonstrate theinflammatory activity <strong>of</strong> tumor necrosisfactor (TNF)We cloned that immense span <strong>of</strong> DNAbecause we thought our mutation <strong>of</strong> interestmust be somewhere within it. We refer to sucha span <strong>of</strong> DNA as the “critical region.” Thearray <strong>of</strong> YACs and BACs that contain that part<strong>of</strong> the genome is called the “contig.” Alexander,Irina and I spent most <strong>of</strong> two years analyzingthe contig. Betsy worked in administration forthe lab but also physically organized massiveamounts <strong>of</strong> data, inoculated colonies, helpedread the sequence files and helped with theBLAST searches.We’d open 50 or 60 BLAST searches and havethem going at the same time – all open onthe toolbar <strong>of</strong> the computer. Sometimes we’dhave a memory problem and everythingwould shut down, which was most frustrating.Once, out <strong>of</strong> the blue, I received a telephonecall from someone at the National Centerfor Biotechnology Information, where theBLAST servers were housed, and the caller toldme, “You’ve been doing too many BLASTsearches and you can’t do that many anymore.”So for a time I cut back, mainly by stoppingthe recursive searches <strong>of</strong> old sequences asfrequently as I had been doing them. I alsobought a Linux computer <strong>of</strong> my own to BLASTlocally after a while. They don’t complainabout things like that these days.By the summer <strong>of</strong> 1998, we had finished sequencingalmost the entire contig and I knewwe were running out <strong>of</strong> anything to sequence.It was as though you’ve explored 90 percent<strong>of</strong> a room looking for a lost cufflink and thoroughlycovered the room and looked undereverything and you’ve looked at practicallyeverything except one s<strong>of</strong>a. And you know ithas to be under there, or else it’s going to benowhere in the room at all. It was that kind <strong>of</strong>Returns to <strong>UT</strong> <strong>Southwestern</strong>as anassistant pr<strong>of</strong>essorand assistantinvestigator at theHoward HughesMedical Institute19811982198319863031
Has an epiphany—began embracingclassical genetics“We knew we had opened a new windowin immunology.”feeling: that we were running out <strong>of</strong> anythingto sequence and the probability <strong>of</strong> finding themutation was increasing with every BAC thatwe’d explore. Either that or we’d made a terriblemistake <strong>of</strong> some kind, and the mutationwasn’t in the critical region at all.And we had learned only in May 1998 thatour HHMI funding was going to end in August2000. This was very disappointing because we’dreally worked so hard on this difficult projectand that was what they had encouraged us todo, but they had run out <strong>of</strong> patience.A powerful matchOn Sept. 5, 1998, I was in my study at home atabout 9:30 p.m. We were doing BLAST analysis<strong>of</strong> the BAC I17, and I suddenly saw a powerfulmatch between one <strong>of</strong> our genomic sequencesand an EST. Then I saw another match. Eachwas nearly perfect, and I was confident that thiswas not a pseudogene. Looking further, I sawthat the target gene was known as Toll-likereceptor 4 (Tlr4), named for its similarity to theDrosophila Toll gene. And I also saw stronghomology to the interleukin-1 (IL-1) receptor,which I knew produced a strongly inflammatorysignal. I knew, too, that the Toll family hadleucine-rich repeats, as did CD14 – the oneprotein that was known to be involved in LPSsignaling, though it was not the product <strong>of</strong>the LPS locus. All these facts were exciting. But<strong>of</strong> course, they didn’t yet prove that Tlr4 wasthe gene we were after.I remember telephoning Alexander immediately,and later telephoning my father totell him about it, too, because I felt almostsure that this was the gene, based onthe fact that we had been nearly exhaustivein covering the criticalregion if nothing else. Thatvery night, I designedprimers to amplify the cDNA for Tlr4, andthe next morning Alexander and I had themsynthesized.By evening, he had begun to amplify usingpreparations <strong>of</strong> cDNA from the mutant C3H/HeJ strain and the control C3H/HeN strains <strong>of</strong>mice. It was a very long cDNA – more than4,000 base pairs. We were very skilled at shotguncloning, using ultrasound to break up apiece <strong>of</strong> DNA, by that time. We’d shatter theDNA with ultrasound and then we’d cloneall the pieces into a sequencing vector that hadprimer sites so we could sequence in both directions.We decided to fragment the band andsequence it in depth; then align the reads withPhrap, an assembly program. We saw the sequenceabout a week later, but couldn’t view itwith consed, the definitive program for visualizingaligned sequence, until Sept. 15. That wasthe day we were certain we saw the mutationin C3H/HeJ mice for the very first time, andthat was the second moment <strong>of</strong> excitement.I think it was the most thrilling moment <strong>of</strong>my career. It occurred over in the Y building[Green Research Building]: the critical moment<strong>of</strong> finding the mutation that distinguishedendotoxin unresponsive mice from the controlmice. I remember going to the computer inthe corner <strong>of</strong> our lab to look at it and then I’dwalk away and do some work and then goback and look at it again and again. After fiveyears <strong>of</strong> searching, you can hardly believe itwhen you’ve really found what you’ve beenlooking for, given the many frustrations andfalse starts. But, indeed, it was real. Still, therewas one final piece <strong>of</strong> pro<strong>of</strong> missing.We knew <strong>of</strong> another strain <strong>of</strong> mice –C57BL/10ScCr – that also couldn’t respond toLPS. And we were confident on genetic groundsthat they had a defect in the same gene. Welooked at this second strain <strong>of</strong> mouse and wefound we couldn’t amplify the cDNA at all,nor any part <strong>of</strong> the gene. We did a Southernblot (a test to determine if a DNAsample contains a specific geneticsequence) to see if we coulddetect the gene by probingit on a nylon membrane,and we couldn’t detectthe gene that way either.It seemed that in thecontrol strain, knownas C57BL/10ScSn, thegene was there, but inthe C57BL/10ScCrstrain, the gene was gone.Eventually, by sequencing,we found that74,000 base pairs <strong>of</strong> DNAwere missing from thegenome <strong>of</strong> this mouse. OnlyTlr4 was excised; no other geneswere harmed.That was really incontrovertibleevidence. Here we had two different alleles:One was a point mutation, one was a largedeletion. The first was likely to destroy Tlr4,and the second certainly did so. Both <strong>of</strong> themcaused endotoxin resistance. We concludedthat Tlr4 must be necessary for the responseto endotoxin.Finding the C57BL/10ScCr mutationmight have occurred perhaps a week later, nomore than that, because we were quite confidentthat we had really found the relevant locus.By Sept. 30, 1998, we had submitted ourpaper to Science.The paper was reviewed quite promptly,and there were only minor revisions to bemade. It was published in December 1998. Weknew we had opened a new window inimmunology, discovering how the innate immunesystem “sees” microbes. And we hadfound the very molecule that initiates Gramnegativeseptic shock.Returns to <strong>UT</strong> <strong>Southwestern</strong>as Director <strong>of</strong>the new Center forthe Genetics <strong>of</strong> HostDefenseWins Shaw Prize in LifeScience and MedicineIs awarded the 2011Nobel Prize in Physiologyor MedicineA powerful match is found, leading to confirmatoryexperiments, and the writing <strong>of</strong> a landmark paperpublished in Science that December1993199820082011Is elected to the National Academy <strong>of</strong>Sciences and the Institute <strong>of</strong> Medicine3233
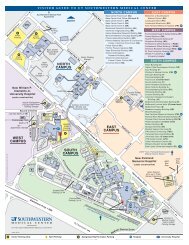
The Hospital <strong>of</strong> the FutureDesigned around the needs <strong>of</strong> patients and their families, the new<strong>UT</strong> <strong>Southwestern</strong> University Hospital will be as innovative as the scientificdiscoveries for which the medical center is knownby Russell RianU.S. News & World Report has ranked <strong>UT</strong> <strong>Southwestern</strong> Medical Center as the top hospital in theDallas-Fort Worth region, with six nationally recognized specialties.University Hospital - Zale Lipshy was one <strong>of</strong> just three hospitals in the nation to earn thePatient Voice Award for Academic Medical Centers from Press Ganey, an independent firm that trackspatient safety and satisfaction.University Hospital - St. Paul ranks No. 1 in Texas for survival rates for heart transplants and in thetop 5 percent <strong>of</strong> programs in the country.University Hospitals & Clinics were named to the “Most Wired” list by Hospitals & Health Networks.So, what’s next?Envisioning – and building – the hospital <strong>of</strong> the future.1SO<strong>UT</strong>HWESTERN MEDICINE 35
Dr. Daniel K. PodolskyDr. Daniel K. Podolsky, president <strong>of</strong><strong>UT</strong> <strong>Southwestern</strong>, laid out the challenge.“After a careful assessment it became clearthe aging University Hospital - St. Paul couldnot be economically upgraded to fully achieveour aspirations: to provide world-class patientcare in a comprehensive, state-<strong>of</strong>-the-artacademic medical center,” said Dr. Podolsky,who holds the Philip O’Bryan MontgomeryJr., M.D., Distinguished Presidential Chair inAcademic Administration and the Doris andBryan Wildenthal Distinguished Chair inMedical Science.This facility needed to be more than justa rebuild, he emphasized, and had to deliverbeyond being just a showcase for <strong>UT</strong> <strong>Southwestern</strong>’sexpertise in clinical services likethose recognized by U.S. News & World Report:urology, cardiology/heart surgery, diabetes/endocrinology, gynecology, nephrology andneurology/neurosurgery.The call also went out to the medical centerand the broader community for ideas and input.More than 800 people responded. Civic leaders.Patients. Doctors. Nurses. Technicians. Staffers.Students. Community members.As work groups took up the challenge <strong>of</strong>what would be needed and how to arrangeall the pieces cohesively and coherently, theprocess distilled to a single, rather simplequestion: How do we improve patient outcomeswhile integrating our other missions <strong>of</strong> researchand education into a single new hospital?To find the right answers, teams examinedwhat worked and what didn’t, then traveledaround the nation to see whether the ideasbeing considered worked elsewhere.“We really tried to test our own ideas,” saidDr. John Warner, chief executive <strong>of</strong>ficer for<strong>UT</strong> <strong>Southwestern</strong> Hospitals. “We tried to figureout how to borrow from other places that havedone things really well and we tried to go to awide variety <strong>of</strong> hospitals, not just the top 10academic medical centers.” Dr. Warner holdsthe Jim and Norma Smith Distinguished Chairfor Interventional Cardiology and the Audreand Bernard Rapoport Chair in CardiovascularResearch.“We went to places that had the fastestturnaround for emergency patients, communityhospitals that did it really well, to determinewhat they did, the way they organizedthemselves and the way they planned theirspace,” Dr. Warner said.In the end, the answer was rather simple:perspective.“We want to take care <strong>of</strong> the person whohas a disease, not just the disease itself,”summarized Dr. Bruce Meyer, executive vicepresident for health system affairs and pr<strong>of</strong>essor<strong>of</strong> obstetrics and gynecology.The challenge: to turn competitiveenvironments into complementary ones; toseamlessly blend practicality into practice; todeliver patient-room convenience by embracingtomorrow’s technology; to transform visionsinto something visionary.A patient-centered approach“At every step along the way, we askedourselves a key question: How can we make thisbetter for patients?” explained Dr. Podolsky.“And it shows. This will be a different kind <strong>of</strong>hospital and you will see that from the momentyou enter the lobby.”Four simple themes emerged from that initialquestion <strong>of</strong> how to make patients well, andthey are woven into every aspect <strong>of</strong> the newbuilding: safety, privacy, communication andflexibility.Each harmonizes with the other. Safetydepends on good communication and privacy.Privacy factors significantly into effectivecommunication and safety. Flexibility is essentialto good communication, privacy and safety.While the scope <strong>of</strong> the project remainedconstant, the shape <strong>of</strong> the building evolved.What started as a traditional four-corneredbuilding became a unique “W” shaped designso that nurses could be closer to patients, havea more direct view <strong>of</strong> beds and not have todisturb patients just to monitor them.Every patient room in the new hospital isprivate. There’s an obvious comfort factor innot having to listen to the person next to youcough or wheeze and in not being disturbedwhen someone else is being attended to. Privacyobviously averts the awkward moments at thehospital – bathing, asking your neighbor to turndown the television’s volume or listening toothers sharing their struggles with familyand friends.Each <strong>of</strong> the 460 patient rooms in the hospital will be private with accommodations forfamily to stay overnight or virtually visit by video-conference (pictured above). Patientrooms will feature comfortable seating areas for visitors, bedside and dimmer controlsfor lighting, multimedia options and Internet access.Family comfort and privacy figure prominently into the design <strong>of</strong> two waiting areaslocated on each patient floor (pictured above). A frosted glass wall will shield the waitingroom from elevators and a secluded cell phone area will provide a quiet space for privatecalls. The hospital also will include 16 labor and delivery suites (pictured below).In addition to the personal benefits, privacyserves practical purposes, as an effective tool forreducing the spread <strong>of</strong> infections, both into andout <strong>of</strong> the room.“We want everyone to have their own roomsince infection risks are much lower whenpatients have privacy,” said Dr. Gary Reed,chief quality <strong>of</strong>ficer and pr<strong>of</strong>essor <strong>of</strong> internalmedicine. Dr. Reed holds the Sinor/Pritchard(Katy Sinor and Kay Pritchard) Pr<strong>of</strong>essorship inMedical Education Honoring Donald W. Seldin,M.D.; the S.T. Harris Family Distinguished Chairin Internal Medicine; and the Eva A. RosenthalPr<strong>of</strong>essorship in Internal Medicine.The one patient/one room model also meansthat when caregivers are assembled, they areonly focused on that patient’s needs so there’sless confusion, less bustle and less chance <strong>of</strong>error. It means only equipment needed for thatpatient’s care needs to be in the room, so there'smore space for family and friends. It means thesometimes embarrassing moments don’t have tobe shared, nor the sometimes painful ones. Andit all happens in an environment where there isa better opportunity to communicate what bothpatients and their caregivers need to know toachieve positive outcomes.A healing environmentBeyond merely embracing the medicaladvantages inherent in a new hospital, designteams also thought about home comforts.One essential element <strong>of</strong> feeling better ishaving some control <strong>of</strong> your surroundingsand environment, so designers incorporatedbedside and dimmer controls for lighting andtemperature, multimedia options at patients’fingertips and Internet access for laptops,phones and other devices that they wouldotherwise be enjoying at home.Another well-established critical comfortfactor for patients is having friends and familythere, so each room will feature a dedicatedseating area for visitors, as well as a pull-outs<strong>of</strong>a bed so a spouse or other loved one can stayovernight. As is the case with home visitations,family and friends who come to visit patients atthe new University Hospital will feel welcomeand will be treated well. So each patient floorwill include two family waiting areas thatprovide comfortable and private spaces forpatients’ visitors to gather. Each floor also willinclude family conference rooms for privateconsultations with physicians.36SO<strong>UT</strong>HWESTERN MEDICINE 37
By The Numbers:<strong>UT</strong> <strong>Southwestern</strong>’s new University Hospital, scheduled to open in 2015, will have:• 12 floors• Approximately 1.3 million square feet <strong>of</strong> space• 460 private patient rooms• 72 private adult ICU rooms• 30 private neonatal ICU rooms• 16 labor and delivery suites• 40 rooms in the emergency department complex• 27 surgical suites• 12 cardiac catheterization, electrophysiology,and interventional radiology procedure rooms• 6 endoscopy rooms• 4 CT scanning rooms• 2 MRI rooms• 4 X-ray suites“My late wife spent a long time in varioushospitals throughout the country,” said RogerHorchow, founder <strong>of</strong> The Horchow Collection,Broadway producer, philanthropist and amember <strong>of</strong> the Building the Future <strong>of</strong> MedicineCampaign Steering Committee. “I know howdifficult it can be to have a family memberin the hospital, so it’s critical that a hospitalbe designed to lessen a potentially stressfulsituation by providing a healing environmentfor patients and their families. The patientrooms will provide many <strong>of</strong> the comforts<strong>of</strong> home, which you don’t <strong>of</strong>ten find in ahospital.”“The design is absolutely wonderful,”said Gay Solomon, an interior designer whohelped spearhead the public reviews for thenew facility and whose husband, Bill Solomon,chairs the Campaign Steering Committee andserves as chairman <strong>of</strong> <strong>Southwestern</strong> MedicalFoundation. “They’ve gone to elaboratemeasures to ensure plenty <strong>of</strong> communityand patient-friendly input, as well as inputfrom nurses and doctors, about what actuallyworks. It’s going to be an incredibly pleasantenvironment, very user friendly and relaxing,given the fact that people are going to bestressed when they are here.”The daily practicality <strong>of</strong> moving supplies– from sheets and towels to medicationsand monitors – is no small function at amajor hospital and can add to that stressfulenvironment. Recognizing this, designers tooksome lessons from production companies likeDisney and four-star hotels to learn how to shiftsupport operations backstage.Pushing the operational side <strong>of</strong> things tothe backstage by using separate elevators forpatients, supplies and visitors or providingconference rooms for staff meetings andbriefings, addresses all the fundamentals– flexibility and privacy, safety and bettercommunications – for both patients andemployees.The operational design focuses on frontlinepatient care, reducing distractions andfacilitating better communications. Quieter,safer hallways translate to more privacyand a less crowded feel. Such operationalconsiderations in the new UniversityHospital’s design will ensure the patientcenteredapproach will continue, even whenconstruction is complete.Technology for family and careWith state-<strong>of</strong>-the-art medical technology, thenew University Hospital will be as innovative asthe health care at <strong>UT</strong> <strong>Southwestern</strong>. Each roomwill feature a monitor that allows patients andtheir caregivers to review charts and images,such as X-rays, CT scans and MRIs, facilitatingbetter communication and privacy.Notably, the monitor will also allow inroomvideo-conferencing, enabling patients tocommunicate virtually with members <strong>of</strong> theircare team, out-<strong>of</strong>-<strong>of</strong>fice physicians, <strong>of</strong>f-siteprimary care physicians, or family and friends.Such technology can help alleviate the solitude<strong>of</strong> treatment and recovery when a patient'sloved ones are unable to visit in person.The new <strong>UT</strong> <strong>Southwestern</strong> University Hospital has been meticulously designed based on input from a dedicatedplanning team <strong>of</strong> physicians, nurses, institutional leaders and community supporters. Always mindful <strong>of</strong> the needs<strong>of</strong> patients and their families, the team envisioned a facility that will <strong>of</strong>fer state-<strong>of</strong>-the-art, specialized care in apatient-centric environment.38SO<strong>UT</strong>HWESTERN MEDICINE 39
The new University Hospital also willinclude an on-site education center, wherepatients or family members can find outmore about diseases or treatments and geteducational materials, including informationabout relevant research being done by <strong>UT</strong><strong>Southwestern</strong> faculty.Along those lines, the hospital will houseand support clinical researchers who willwork to translate scientific discoveries intotreatments for patients. Yet another advantage<strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>’s care is research – itsmission to move laboratory findings to bedsidepracticality and improve clinical outcomes withtrials <strong>of</strong> new drugs and other therapies. Fundingfrom federal agencies, foundations, companiesand private donors provides more than $417million per year to support about 3,500 researchprojects.Enabling patients to take advantage <strong>of</strong> aclinical trial requires greater flexibility than isfound at a typical hospital environment. Soeach floor <strong>of</strong> the new University Hospital willinclude dedicated research space for clinicaland translational research activities, which canrange from analyzing blood or tissue samples toentering data about the progression <strong>of</strong> a diseaseor illness and the progress in treating it.Being able to handle research duties on-sitemeans physicians can spend less time awayfrom the hospital, making them more accessibleto patients or other health care pr<strong>of</strong>essionals.A rendering <strong>of</strong> one <strong>of</strong> the hospital’s three adult intensive care units (ICUs) is shown above.Team-based care<strong>UT</strong> <strong>Southwestern</strong> leadership takes pride inits team approach to health care – cardiologistswork with cardiothoracic surgeons andanesthesiologists, specially trained teams<strong>of</strong> cardiac nurses join with technicians andimaging specialists, along with pathologists,case managers, social workers and therapists.The medical center was among the first inthe nation to use electronic health records.These records, used across the ambulatoryand hospital environments, facilitate easiercommunication and help ensure patient safetyby providing a seamless transfer <strong>of</strong> informationamong all members <strong>of</strong> a patient’s care team.Every caregiver has the same informationavailable when and where it’s needed. Theelectronic system reduces the risk for errorby requiring specific information, noting if aform hasn’t been completed, informing careproviders if there are problems with medicationinteractions, and other patient care safeguards.“A lot <strong>of</strong> people talk about multidisciplinarycare and team-based care, while in reality theyare taking a team and moving it around thehospital,” said Dr. Warner, associate pr<strong>of</strong>essor <strong>of</strong>internal medicine who is also medical director<strong>of</strong> the Doris and Harry W. Bass Jr. ClinicalCenter for Heart, Lung and Vascular Disease.“This hospital will be built around team-basedcare. We thought about a process or a diseaseor a service and designed it so people who needto be working together will always be in closeproximity to one another.“In most hospitals, for example, acardiac catheterization laboratory and thecardiovascular operating rooms are on differentfloors. Ours will be right next to each other.They’re across the hall from each other, soeverybody that has anything to do with theheart is on one floor.”A culture <strong>of</strong> communicationThe team also may need to communicateimmediately, so each <strong>of</strong> the hospital’s surgicalsuites will be connected by live video to thepathology lab. This will enable surgeonsand pathologists to view and discuss tissuespecimens in real time while a procedure is stillunder way. The hospital plan includes on-callrooms and facilities for physicians, so they canaccess computers between surgeries or clinicvisits without having to trek across campus.As part <strong>of</strong> the bigger picture, the newAn on-site education center (above) will provide patients and family membersaccess to educational materials about diseases or treatments.University Hospital will feature conferencefacilities as well, key to helping <strong>UT</strong> <strong>Southwestern</strong>’sphysicians stay atop the latest medicalfindings while meeting continuing educationrequirements and helping pass along the latestfindings to other physicians in the community.“This facility will be one <strong>of</strong> the mostadaptable hospitals in the country,” saidDr. Warner. “We really tried to design flexibilityinto the hospital so that at every single step weadded the ability to expand or renovate withminimal disruption to the building.”Viewed from the perspective <strong>of</strong> Harry HinesBoulevard, the new University Hospital is animpressive construction site <strong>of</strong> an $800 millionfacility. Institutionally, however, the project isbeing realized and fulfilled with each individualpatient in mind, a perspective that is provingpriceless.“As an academic medical center, chief amongour missions is to translate whatever lessonswe learn, from wherever we learn them, intosomething applicable to the bedside,” Dr.Podolsky noted. “Our mission was to design thehospital <strong>of</strong> the future that would harmonize ourclinical, educational and research missions atthe bedside. It turned out to be quite a symphony.”40All artist's renderings provided by architectural firm RTKL Associates.SO<strong>UT</strong>HWESTERN MEDICINE 41
Can FoodborneIllnessesbe Stopped?<strong>UT</strong> <strong>Southwestern</strong> researchers are at the forefront <strong>of</strong> understandingand preventing the spread <strong>of</strong> dangerous bacteria in foodYou’re looking for fresh produce at the grocery when a text comes acrossyour smartphone. Holding the device away from your 3-year-old, you read afrantic message from your mother: “CANTALOUPES DANGEROUS!!!DO NOT BUY CANTALOUPES!!!” n Turns out the media are reportinga Listeria outbreak. In addition to her text message, your mother calledfive times. She’s panicking because her grandchild, your toddler, happensto love cantaloupe. n The Centers for Disease Control and Prevention(CDC) estimates that each year foodborne illnesses sicken roughly one insix Americans, kill 3,000 and cause 128,000 to be hospitalized. The mostcommonly recognized bacterial pathogens are Campylobacter jejuni (C. jejuni),Salmonella and Escherichia coli (E. coli). n After contaminated food is consumed,the bacterium incubates in the host before revealing itself throughillness symptoms. During incubation the bacterium passes through the stomachinto the intestine, attaching itself to the cells lining the intestinal walls.B y E r i n P r a t h E r S t a f f o r dSO<strong>UT</strong>HWESTERN MEDICINE43
“Disease caused by foodborne pathogens can beanything from mild diarrhea in some individuals to moreserious hemorrhagic diarrhea, kidney failure and strokelikesymptoms. The bacteria can even be fatal, especiallyfor young children, the elderly and those with compromisedimmune systems.”—Dr. Vanessa SperandioThe pathogen then multiplies, killing cellsby stealing their nutrients. Some <strong>of</strong> the bacteriastay in the intestine, while others producetoxins that then are absorbed into thehost’s bloodstream or even body tissues.Many pathogens responsible for foodborneillness cause similar symptoms such asdiarrhea, abdominal cramps and nausea. Thereis so much overlap that it can be difficult toidentify what specific bacterium is causingillness without laboratory tests to identify thepathogen unless there is a recognized outbreak.Most cases are mild and can be treated byincreasing fluid intake. But not all reactions areminor, and death is a tragic possibility.“These bacteria are very potent; it onlytakes a few to get someone severely sick,” saidDr. Vanessa Sperandio, pr<strong>of</strong>essor <strong>of</strong> microbiologyand biochemistry at <strong>UT</strong> <strong>Southwestern</strong> MedicalCenter. “Disease caused by foodborne pathogenscan be anything from mild diarrhea in someindividuals to more serious hemorrhagic diarrhea,kidney failure and stroke-like symptoms.The bacteria can even be fatal, especially foryoung children, the elderly and those withcompromised immune systems.”Many antibiotics have become ineffectiveagainst foodborne pathogens and can potentiallycause more harm by increasing the amount<strong>of</strong> released toxins. Instead <strong>of</strong> focusing on thebugs after they cause illness, <strong>UT</strong> <strong>Southwestern</strong>researchers are investigating how to neutralizethe pathogens so they never have a chance towreak havoc on the human body.Exploiting cell-to-cell signalingDr. Sperandio always has been fascinated withbacteria/host interactions. Much <strong>of</strong> her researchhas focused on E. coli, specifically the lethalenterohemorrhagic E. coli (EHEC) strain. Thebacterium is primarily transmitted to humansthrough consumption <strong>of</strong> beef. However, fecalcontamination <strong>of</strong> water and other foods, aswell as cross contamination during food preparation,also can cause disease. Recent E. colioutbreaks have been linked to beef, cheese,cookie dough, poultry, Romaine lettuce, spinachand sprouts.Dr. Sperandio and her team are investigatingtwo tactics to fight the pathogen. The firstinvolves exploiting its cell-to-cell signaling tostop EHEC from colonizing in the intestines.Her lab has successfully identified two receptorsrequired by the bacteria for infection <strong>of</strong> the host.In 2006 she found the receptor QseC, aprotein in the EHEC’s membrane. After aperson ingests the bacterium, it travels peacefullythrough the digestive tract until reachingthe intestine. Once there, the QseC receptorcommunicates with the human stress hormonesepinephrine and norepinephrine, asignaling cascade begins and EHEC colonizesthe intestine and causes disease.Searching <strong>UT</strong> <strong>Southwestern</strong>’s library <strong>of</strong>150,000 small molecules, Dr. Sperandiouncovered LED209. Nontoxic to mammalcells, LED209 has proven successful in preventingQseC from initiating the virulencecascade and allowing EHEC to colonize.She and research colleagues also aretargeting EHEC in live cattle. An estimated70 percent to 80 percent <strong>of</strong> herds in the U.S.carry the bacteria. Although deadly to humans,EHEC is a natural part <strong>of</strong> cattle’s normalgastrointestinal flora. It harbors a gene calledSdiA, which makes the SdiA protein. The SdiAprotein senses a chemical made by microbesin the animal’s rumen, the first <strong>of</strong> a cow’s fourstomachs, which serves as a large fermentationchamber. Detecting this signal allows EHEC topass through the rumen and colonize the rectoanaljunction.Dr. Sperandio’s lab injected two types <strong>of</strong>EHEC into the rumens <strong>of</strong> eight grain-fedadult cows. One mutant version lacked SdiAand could not detect the signal in the rumen.Another strain produced an enzyme thatdestroyed the chemicals in the rumen sensedby SdiA.“If there’s no signal, then there’s no acidresistance, a requirement for the pathogen tomake it to the recto-anal junction,”Dr. Sperandio said. “Everybody had thoughtthat this type <strong>of</strong> signaling occurred naturallyin the gastrointestinal tract <strong>of</strong> mammals. Ourfindings suggest we might be able to target thissystem to prevent food contamination fromcattle. We can render EHEC harmless before itreaches humans.”Dr. Sperandio also found that colonizationdiminished significantly when EHEC wasunable to sense the rumen chemicals. Theprocess prevented the bacteria from movingon through the stomach and colonizing. Hernext step is to assess what happens to cows feda grass-based, rather than grain-based, diet.E coli, shown forming lesions on host cells, is primarily transmitted to people by eating beef.44SO<strong>UT</strong>HWESTERN MEDICINE45
Stopping attachmentBacterial pathogens face a number <strong>of</strong> challengeswhen trying to connect with human cells.Evading immune recognition, invading celltissue and modulating cellular signaling arejust a few tasks they must accomplish to ensuresurvival. Dr. Kim Orth, pr<strong>of</strong>essor <strong>of</strong> molecularbiology and biochemistry, is investigatingwhether cell damage caused by pathogenscan be prevented by disrupting their initialattachment to host cells.She and her team looked to the pathogenVibrio parahaemolyticus (V. para) for answers.The bacterium, found in every ocean, can causefood poisoning through consumption <strong>of</strong> rawor undercooked shellfish, particularly oysters.Previous work by Dr. Orth had found thatV. para kills its host’s cells by causing them toburst, providing the bacteria with food used t<strong>of</strong>uel proliferation. To accomplish this nutrientrobbery, the bacteria must successfully attach tothe membranes <strong>of</strong> host cells.“Bacteria are dependent on that union,”said Dr. Orth, a W.W. Caruth Jr. Scholar inMedical Research. “We suspect many bacterial“Bacteria have been evolving for a very long time. If we canfigure out how they work, it could have an incredible impacton everyone in the world.”—Dr. Kim Orthpathogens actually use a common mechanismto establish that first contact. Our goals areto understand this mechanism and thenexploit it to develop therapeutic tools thatcompletely shut down the pathogens’ abilityto colonize cells.”In investigating V. para, Dr. Orth’s laboratoryfound that the protein MAM7 enables a widerange <strong>of</strong> pathogens (including E. coli, Salmonellaand Cholera) to bind to host cells during theearly stages <strong>of</strong> infection. When researchersdeleted MAM7, V. para had difficulty binding tohost cells and efficiently killing them.They also engineered a harmless strain <strong>of</strong>E. coli to express MAM7. Exposing human cellsto this harmless form <strong>of</strong> the bacteria causedhuman cells to become more resilient toV. para and other types <strong>of</strong> pathogenic bacteria.Dr. Orth is optimistic that the protein eventuallycould help prevent foodborne illness.“It would be amazing to give susceptiblechildren in pathogen-plagued areas a bit<strong>of</strong> yogurt containing some form <strong>of</strong> MAM7and have it decrease their risk for seriouscomplications,” she said. “Bacteria have beenevolving for a very long time. If we can figureout how they work, it could have an incredibleimpact on everyone in the world.”“It’s known that as people get older theybecome more susceptible to infectiousdiseases and also that autophagydecreases.”—Dr. Beth LevineAutophagy fights backSometimes the answers to stopping bacterialpathogens are found in the cell’s own naturalprocess. Autophagy is the way cells eliminatetheir own unwanted or damaged parts. It isa highly regulated and completely normalprocess by which they remain healthy byperforming “routine housekeeping” and“garbage disposal.”Dr. Beth Levine, director <strong>of</strong> the Center forAutophagy Research and pr<strong>of</strong>essor <strong>of</strong> internalmedicine and microbiology, has determinedthat autophagy prevents Salmonella bacteriafrom becoming successful intracellular pathogens.She and her team studied the effects <strong>of</strong>Salmonella infections in two organisms theyhad genetically engineered to lack activeautophagy genes.In both cases, the animals with inactiveautophagy genes fared far worse than thosewith active ones. Rather than being targeted forelimination, the bacterium was able to invadethe host cells, where it started replicating.Dr. Levine’s findings also suggest thatdecreases in autophagy – such as those thatoccur in the elderly and in certain patientswith Crohn’s disease – may lead to abnormalitiesin the way the intestinal tract dealswith bacterial infections.“It’s known that as people get older theybecome more susceptible to infectious diseasesand also that autophagy decreases,” saidDr. Levine, who holds the Charles CameronSprague Distinguished Chair in BiomedicalScience. “We’ve found that signaling pathwaysthat extend life and protect against bacterialinvaders do so by triggering autophagy. Thissuggests that therapeutic strategies to increaseautophagy may be effective in defeatingharmful bacteria that can enter inside cells.”It’s unclear why older people becomemore susceptible to infections, but researchhas shown that autophagy declines with age.Dr. Levine, a Howard Hughes Medical InstituteInvestigator at <strong>UT</strong> <strong>Southwestern</strong>, suggeststhat by reversing or regulating this process,researchers could make the elderly and otherswith weakened immune systems more resistantto infections.Her lab is now looking into the efficacy <strong>of</strong> anew autophagy-inducing molecule for treatinga number <strong>of</strong> intracellular bacterial infectionsincluding Salmonellosis, tuberculosis, tularemiaand Listeriosis.46SO<strong>UT</strong>HWESTERN MEDICINE47
“Unlike in humans, C. jejuni doesnot invade chicken intestinalepithelial cells and damage thesecells. Also, the immune systems<strong>of</strong> chickens likely deal with thebacterium differently. Chickens area great model for investigating howdisease by C. jejuni is prevented.”—Dr. David Hendrixson“Scientists are still unsure how C. jejuni,or similar bacteria, know to create an exactnumber <strong>of</strong> flagella and at specific locations,”said Dr. Hendrixson. “We want to understandthese spacial and numerical parameters, becauseif we know how C. jejuni builds its flagellum,we may be able to disrupt the process andimmobilize the pathogen.”Protecting the kitchenThe global incidence <strong>of</strong> foodborne disease isdifficult to estimate. As international shippingin the food industry continues to expand, sodoes the possibility <strong>of</strong> bacterial pathogenscrossing borders.There are steps consumers can take to tryto keep a market trip from leading to a stay inthe hospital. The CDC reports that raw meatand poultry, raw eggs, unpasteurized milk andraw shellfish are the foods most likely to becontaminated. Lona Sandon, assistant pr<strong>of</strong>essor<strong>of</strong> clinical nutrition and a spokeswomanfor the American Dietetic Association, stressesthat all meat, poultry and eggs should becooked thoroughly. She recommends using athermometer to measure the internal temperature<strong>of</strong> meat to ensure it is cooked sufficientlyto kill bacteria. Most meats should be cookedto 165 degrees and leftovers also need to beheated to this temperature.“It’s also important to avoid cross-contamination<strong>of</strong> one food with another,” said Ms.Sandon. “Wash hands, utensils and cuttingboards after they have been in contact with rawmeat or poultry and before you touch anotherfood. Place the cooked meat on a separate dish,rather than one that has held raw meat. And besure to refrigerate leftovers promptly. Bacteriacan grow quickly at room temperature.”Regarding vegetables and fruits, Ms. Sandonsays washing these foods with running water isthe best way to remove unwanted pathogens.She warns that the cut surface on fruits andvegetables is a prime environment for bacteriagrowth. It also is important for consumersto be mindful <strong>of</strong> slicing the foods on cleancutting surfaces.Yet despite such precautionary measureseveryone, no matter their location in the world,is susceptible to illness caused by foodbornebugs. And the clock is ticking as more and more<strong>of</strong> these bacteria are becoming immune to theeffects <strong>of</strong> antibiotics. Over time bacteria haveadapted to make human cells work to theiradvantage. <strong>UT</strong> <strong>Southwestern</strong> researchers aredetermined to turn the tables on them.Immobilizing colonization and mobilityDr. David Hendrixson, associate pr<strong>of</strong>essor <strong>of</strong>microbiology, is conducting research aimedat ridding the world <strong>of</strong> one <strong>of</strong> the mostcommon and severe forms <strong>of</strong> diarrheal diseasein humans. Campylobacter jejuni (C. jejuni)is a bacterial pathogen that colonizes thegastrointestinal tracts <strong>of</strong> humans andanimals, particularly chickens and othertypes <strong>of</strong> poultry.It <strong>of</strong>ten is spread among flocks in feces andinfects humans through their consumption<strong>of</strong> contaminated poultry. C. jejuni has alsosickened consumers <strong>of</strong> other meats andunpasteurized milk. The bacterium is harmlessin livestock but it can cause mild to severediarrhea when passed to humans.“The chicken gastrointestinal tract hasadapted to the presence <strong>of</strong> C. jejuni,” Dr.Hendrixson said. “Unlike in humans, C. jejunidoes not invade chicken intestinal epithelialcells and damage these cells. Also, the immunesystems <strong>of</strong> chickens likely deal with thebacterium differently. Both <strong>of</strong> these factorscontribute to the reasons why chickens don’tbecome ill due to C. jejuni infections. Chickensare a great model for investigating how diseaseby C. jejuni is prevented.”Dr. Hendrixson’s lab is studying the genesthe bacterium needs to live within an avianhost in hopes that this understanding may leadto strategies to eradicate it from chickens andthus decrease the amount <strong>of</strong> the bacterium inhuman food.He and his <strong>UT</strong> <strong>Southwestern</strong> colleagues haveidentified many factors C. jejuni requires for thecolonization <strong>of</strong> poultry and are analyzing howthese factors benefit bacteria growth and mightbe targets for future vaccines.Dr. Hendrixson also is focusing on the genesinvolved in the function and regulation <strong>of</strong>the flagellum C. jejuni produces, which allowsthe bug to propel itself throughout a host’sgastrointestinal tract. Flagellum is a tail-likeprojection that protrudes from the pathogenand can move it toward various nutrients forgrowth. Bacteria create only a certain number<strong>of</strong> flagella and at very specific locations.“Wash hands, utensilsand cutting boards afterthey have been in contactwith raw meat or poultryand before you touchanother food. Place thecooked meat on a separatedish, rather than onethat has held raw meat.And be sure to refrigerateleftovers promptly. Bacteriacan grow quickly atroom temperature.”—Lona Sandon48SO<strong>UT</strong>HWESTERN MEDICINE49
What it takes to becomea world-class physicianBy Russell RianKnowledge, skill and years and years <strong>of</strong> practice—from basic anatomy classes as a first-year medicalstudent to training as an intern to subspecialtyexpertise as a fellow and beyondIt’s one <strong>of</strong> life’s most vulnerable moments –wondering exactly what’s wrong as you waitfor the doctor to enter the room. Was it a heartattack? A stroke? Is it cancer, or a brain tumor?Your mind reels ... How bad is it? Is there atreatment? Is surgery needed?Eventually, we all look into the face <strong>of</strong> ourphysician – searching for answers to some<strong>of</strong> the most personal, complex and <strong>of</strong>ten frighteningproblems we will ever face.Each year, <strong>UT</strong> <strong>Southwestern</strong> Medical Center’steams <strong>of</strong> physicians look into the eyes <strong>of</strong> about100,000 hospitalized patients – and even moreindividuals during nearly 2 million visits atoutpatient clinics – to provide answers to howtheir illnesses might be diagnosed, treated orsurgically addressed.When they arrive at <strong>UT</strong> <strong>Southwestern</strong>, thesepatients tap into a unique brain trust. Itincludes five Nobel laureates, 12 Howard HughesMedical Institute investigators, 19 members<strong>of</strong> the National Academy <strong>of</strong> Sciences, 20members <strong>of</strong> the Institute <strong>of</strong> Medicine and 15members <strong>of</strong> the American Academy <strong>of</strong> Artsand Sciences. It’s a brain trust forged <strong>of</strong> boardcertifiedsurgeons, specialists, sub-specialistsand internists, past and present presidents <strong>of</strong>national medical societies, investigators forNational Institutes <strong>of</strong> Health studies, and chairs<strong>of</strong> national committees in fields from pediatricsto plastic surgery, from breast care toneurology. It’s a trust clinically recognized nationallyin six specialties by U.S. News &World Report and delivered in the top-rankedhospital in the Dallas-Fort Worth region.Many members <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>’sfaculty have written the textbooks used toteach others or have served as editors on prestigiouspeer-reviewed journals such as theJournal <strong>of</strong> the American Medical Association andthe New England Journal <strong>of</strong> Medicine, publicationsthe medical pr<strong>of</strong>ession relies on to staycurrent regarding cutting-edge treatmentsand procedures.Yet underlying that cavalcade <strong>of</strong> expertiseand excellence are the humble beginnings– the first steps every doctor takes tobecome a physician.Founded in 1943, <strong>UT</strong> <strong>Southwestern</strong> MedicalSchool has graduated nearly 10,000 physicians.This academic year, the medical school willtrain nearly 1,000 medical students and almost1,500 clinical residents. <strong>UT</strong> <strong>Southwestern</strong><strong>of</strong>fers more than 30 residency programs andmore than 60 clinical subspecialties fellowshipsin the Dallas area. More than 60 percent<strong>of</strong> physicians in the Dallas area earned theirdegrees from <strong>UT</strong> <strong>Southwestern</strong>, and more remainaffiliated with the university.Preparing those doctors is more than justpart <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>’s mission for academicmedicine practitioners; it is a duty, a sacredone taken as seriously as the physician’s oath.While we, as patients and consumers, maycatch a glimpse <strong>of</strong> the medical world when weare ill or injured, our doctors – even theyoungest among them – have been immersed inmedicine for at least the better part <strong>of</strong> a decade,most far longer. And the amount <strong>of</strong>knowledge they acquire, and the multitude moreat their disposal, is simply astounding.51
U.S. News & World Report ranks <strong>UT</strong> <strong>Southwestern</strong> in the Top 25 in the nation for both research and primary care in its listing <strong>of</strong> BestMedical Schools for 2012. These accolades, as well as a decades-long reputation for superior education and training, drive a selectstudent body. Virtually all <strong>of</strong> these students are among the smartest in their undergraduate class.SO JUST HOW MUCH DOESYOUR DOCTOR KNOW?Consider:• They’ve learned an encompassinglexicon – from diseasesto medicines to procedures – an exactingvocabulary all its own. They have masteredmyriad instruments, how to use them andhow not to use them.• They have dedicated years <strong>of</strong> observing, learningand appreciating cellular reactions; whereand how muscles connect; how glands delivervarious enzymes and why; how organswork in concert and the signs that they aren’tfunctioning properly; which test can pinpointtroubles and which can rule them out.• They are able to tell patients what that rashis; whether their limb is really broken; andwhen they need to do something about ourever-declining capabilities to see and hear.• They’ve learned to give injections, todetermine which drugs fight infections andto perform surgery.• They have learned to handle the human factor,such as how to share with someone thatthey are facing cancer, need bypass surgeryor have a complicated pregnancy. They havelearned not to panic when the diagnosis isnot easy, how to search medical literature fora similar case or situation, and how to determinetheir patients’ best treatment options.• From years <strong>of</strong> classroom and clinical training,they have learned statistical analysis so theycan filter cause-and-effect from mere association.They have learned the proper handling<strong>of</strong> hazardous, toxic and medical wastes, andhave memorized billing codes and masteredelectronic medical records to ensure completeand correct paperwork and charts.They have learned all this for dozens <strong>of</strong>types <strong>of</strong> cancers, hundreds <strong>of</strong> cardiology problemsand thousands <strong>of</strong> other diseases andconditions.BECOMING AN M.D.Becoming a doctor is not reallya moment; it is at best an evolutionaryprocess.“What a student really has todo is learn how to be a student for life,”noted Dr. J. Gregory Fitz, executive vice presidentfor academic affairs, provost and dean<strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong> Medical School.Becoming a doctor involves a gauntlet <strong>of</strong>years spent, knowledge learned and experiencegained. Those who make the decision to shouldersuch challenges, responsibilities, oathsand heartaches do so because their hearts andheads told them to do so.MEDICAL SCHOOL<strong>UT</strong> <strong>Southwestern</strong> MedicalSchool – the 68th established inthe country and the second <strong>of</strong>four established in the University<strong>of</strong> Texas system – <strong>of</strong>fers six medical degrees,from Doctor <strong>of</strong> Medicine to combinations thatinclude master and Ph.D. degrees.U.S. News & World Report ranks <strong>UT</strong> <strong>Southwestern</strong>in the Top 25 in the nation for bothresearch and primary care in its listing <strong>of</strong> BestMedical Schools for 2012. And for three <strong>of</strong>the past four years, <strong>UT</strong> <strong>Southwestern</strong> has beenranked as the nation’s top medical schoolfor Hispanics by Hispanic Business magazine,which takes into account academic excellence,enrollment, faculty, student services andretention rates.These accolades, as well as a decades-longreputation for superior education and training,drive a select student body. Only about 230<strong>of</strong> the roughly 3,500 students applying annuallyto <strong>UT</strong> <strong>Southwestern</strong> Medical School areaccepted. That’s a 6.5 percent acceptance rate.“Virtually all <strong>of</strong> these students were amongthe smartest in their undergraduate class. Manywere valedictorians. They are all very bright,”said Wes Norred, vice president for student andalumni affairs. “But then you arrive at medicalschool, you’re not the smartest kid in the classanymore. It’s filled with the smartest kids inthe class. That’s an adjustment for some.“Another immediate adjustment is that thevolume <strong>of</strong> material to be learned is huge. A lot <strong>of</strong>people say it’s like drinking from a fire hose.”YEAR ONEThe first-year curriculum at<strong>UT</strong> <strong>Southwestern</strong> is nine monthslong. It begins with a study <strong>of</strong>the typical human body and itsprocesses at the molecular and cellular levels.Biochemistry, genetics, anatomy and embryologyare presented concurrently for the first portion<strong>of</strong> the year, melding the concepts <strong>of</strong> macromolecularand cellular interactions within tissues.Students take introductory courses in clinicalethics in medicine and critical thinking; byspring they are taking interdisciplinary coursesin physiology and neuroscience, as well ascourses in cell biology and human behavior andpsychopathology. An 11-week summer breakat the end <strong>of</strong> the first year <strong>of</strong>ten is filled withclinical training or basic science and clinicalresearch opportunities, providing simultaneousexposures to the practice world.During the first year, students learn how totake a patient’s history and to perform a detailedphysical exam on “standardized patients,”receiving careful instruction from their mentorsand detailed feedback on their clinical skills.“Standardized patients” are people trainedand scripted for various diseases to provide aconsistent, reproducible presentation <strong>of</strong> aclinical case. This exercise is digitally recordedfor later review by the student and mentors,and the trained “patients” also provide theirown feedback.YEAR TWOIn the second year, the instructionalperspective shifts to organsystems: clinical medicine,microbiology, pathology andpharmacology laid out in 12 specialized blocksspread over another nine-month period.Certification in advanced cardiac life support,a requirement for graduation, is usually completedafter the second year, and students typicallytake Step 1 <strong>of</strong> the three-part United StatesMedical Licensure Exam (USMLE). All portionsmust be completed before being permittedto practice medicine domestically. Step 1 is aneight-hour, computer-based exam consisting<strong>of</strong> 322 multiple-choice questions.Simultaneous exposure to the clinical worldalso awaits students the second year. Amongthose opportunities is The Monday Clinic, a freeweekly clinic for adult patients operatedunder the supervision <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>physicians by volunteer medical students whoreceive special training before participating.“Hypothetical scenarios in class are one thing,but being able to use the knowledge I gainedin my first-year medical education at The MondayClinic was a refreshing reminder <strong>of</strong> how importantour studies truly are,” said Sandeep Mehta,a second-year medical student.5253
A typical day on hospital wards consists <strong>of</strong> morning rounds, a noon conference and afternoon rounds, in addition to a daily fare <strong>of</strong>reading journal articles and attending conferences, grand rounds and case presentations.YEAR THREEIn the third year, the curriculumlengthens to 11 months, andthe focus shifts to the first <strong>of</strong>two years <strong>of</strong> intense clinicaltraining and experiences involving direct patientcare. Though some medical schools havemoved to more <strong>of</strong> an observer-type role for theirstudents with no on-call time, medicalstudents at <strong>UT</strong> <strong>Southwestern</strong> are integral topatient-care teams. They take overnight callsand have real responsibilities and exposure tothe care process.“This is a school that values learning by doing,”said Dr. Fitz, pr<strong>of</strong>essor <strong>of</strong> internal medicinewho holds the Nadine and Tom CraddickDistinguished Chair in Medical Science andthe Atticus James Gill, M.D., Chair in MedicalScience.A typical day on hospital wards consists <strong>of</strong>morning rounds, a noon conference and afternoonrounds, in addition to a daily fare <strong>of</strong>reading journal articles and attending conferences,grand rounds and case presentations.Departmental rotations include family medicine,internal medicine, neurology and neurotherapeutics,obstetrics and gynecology, pediatrics,psychiatry, and surgery in hospital and outpatientclinics as well as public and private practices.A typical schedule includes: 12 weeks <strong>of</strong>internal medicine, eight weeks <strong>of</strong> pediatric andsurgery rounds, six weeks <strong>of</strong> psychiatry and OB/GYN, and four weeks <strong>of</strong> family medicine andneurology and neurotherapeutics.Third-year students take initial patient histories,perform initial physical exams, writedaily progress notes on their assigned patientsand present them on daily rounds. Duringthe OB/GYN rotation and under supervision,students assist in delivering babies in uncomplicatedpregnancies, assist in managing complicatedpregnancies during the labor anddelivery process, and follow patients postpartum.In the surgical rotation, emphasis is onthe underlying pathophysiology rather thantechnical aspects, but students are fully involvedin the daily care <strong>of</strong> surgical patients andparticipate in diagnostic and therapeuticdecision-making.“Students <strong>of</strong>ten tell me that they areamazed by the fact that even on their first day<strong>of</strong> their clinical rotations, when they <strong>of</strong>ten feelinsecure and unprepared, patients commonlywelcome their participation in their care andput a lot <strong>of</strong> faith and confidence in them,” saidDr. Angela Mihalic, associate dean for studentaffairs and associate pr<strong>of</strong>essor <strong>of</strong> pediatrics.“Students are truly humbled by the sacred trustplaced in them as patients reveal their mostintimate thoughts, fears and concerns associatedwith their health. This faith and confidenceprovides students with a mission and a directiveto do everything in their power to developtheir knowledge and clinical skills to be able tolive up to the expectations placed in themand be worthy <strong>of</strong> this trust.”In addition, a number <strong>of</strong> simulated environmentsprovide an opportunity for students tolearn, practice and hone those clinical skills. TheSimCenter <strong>of</strong>fers a small group teaching centerwhere students can learn and practice skillson high-fidelity simulators that are close replicas<strong>of</strong> human patients. Students in surgical rotationscan practice skills in the Center for MinimallyInvasive Surgery, a hands-on localecontinued page 56PHYSICIAN ASSISTANT PROGRAMCELEBRATES 40 YEARSWhile well known and respected for itsmedical school, <strong>UT</strong> <strong>Southwestern</strong> MedicalCenter also is known in health carecircles for its top physician assistanttraining program.In 2012, <strong>UT</strong> <strong>Southwestern</strong> School <strong>of</strong>Health Pr<strong>of</strong>essions celebrates 40 yearsgraduating physician assistants as one <strong>of</strong>the first, and now among the top, programsin the nation. <strong>UT</strong> <strong>Southwestern</strong>’s Master<strong>of</strong> Physician Assistant Studies Program,ranked eighth in the nation by U.S. News &World Report in “America’s Best GraduateSchools 2012,” admits only a small fraction<strong>of</strong> those who apply for the 31-monthdegree program. For the class commencing in2011, the school accepted just 36 <strong>of</strong> nearly1,100 applicants.“It’s enormously gratifying to see thesekinds <strong>of</strong> accolades for our program as oursand other programs have matured over thedecades,” said Dr. P. Eugene Jones, chairand program director for the Department<strong>of</strong> Physician Assistant Studies. “But the realbenefit is to the thousands <strong>of</strong> patients whoincreasingly depend on highly qualifiedphysician assistants to help provide care.”Physician assistants practice under doctorsupervision. They take medical histories,conduct physical exams, diagnose and treatillnesses, order and interpret tests, providecounseling on preventive health care, developtreatment plans, assist in surgery andprescribe medications. More than 81,000certified PAs practice in primary care andmost medical specialties, according to theAmerican Academy <strong>of</strong> Physician Assistants.PAs are one <strong>of</strong> the nation’s fastestgrowingsegments <strong>of</strong> health care, accordingto the academy. The U.S. Bureau <strong>of</strong>Labor Statistics projected that the number<strong>of</strong> PA jobs would increase by 27 percentbetween 2006 and 2016.Wanting to deliver hands-on health care<strong>of</strong>ten is the driving factor for students. Thatwas the case for Dr. Tina Kaufman about 15years ago when she began <strong>UT</strong> <strong>Southwestern</strong>’sphysician assistant program, allowingher to combine interests in research, teachingand indigent care.“It’s enormously gratifying to see these kinds <strong>of</strong> accolades for our program as oursand other programs have matured over the decades.” — Dr. P. Eugene Jones“When I went into PA school, I knew mostly Navy corpsmen with medical skillsI wanted to do primary care and I knew I developed during their service, and itwanted to do indigent care. That was really was viewed as an opportunity to helpmy focus,” said Dr. Kaufman, who became tackle a shortage <strong>of</strong> primary care doctorsthe first physician assistant in the Internal at the time. The initial training was basedMedicine Clinic at Parkland Memorial Hospital,on the expedited training developed forwhere she had trained. She went on military doctors during World War II. Byto establish training clinics for residents to 1968, the American Association <strong>of</strong> Phylearnabout exercise prescription and counseling,sician Assistants was created, and in 1971chronic pain, smoking cessation and Congress apportioned $4 million to launchinjections.physician assistant programs through theDr. Kaufman, who majored in exercise Comprehensive Health Manpower Trainingscience in college, already had earned a Act. That same year, a number <strong>of</strong> pr<strong>of</strong>essionalPh.D. in physiology and completed twoorganizations, including the Ameri-postdoctoral fellowships at <strong>UT</strong> <strong>Southwestern</strong>can Medical Association, the American– in pediatric cardiology and in surgery College <strong>of</strong> Physicians and the American– before joining the PA program in 1996. Academy <strong>of</strong> Pediatrics, agreed to minimumShe recently joined the faculty at Oregonstandards. <strong>UT</strong> <strong>Southwestern</strong> launchedHealth and Science University as assistant its physician assistant degree programpr<strong>of</strong>essor in preventive cardiology and cardiacthrough the graduate school in 1972.rehabilitation in the Division <strong>of</strong> Cardio-The curriculum for physician assistantsvascular Medicine.emphasizes both academic learning andWhen recounting her <strong>UT</strong> <strong>Southwestern</strong>hands-on clinical training. Students beginexperience, Dr. Kaufman said, “I can’t with four semesters <strong>of</strong> lecture and bedsidethink <strong>of</strong> anywhere else I could have gotten demonstration in medical and behavioralthe training and fulfillment that I’ve gotten sciences as the foundation. Four additionalfrom my patients.”semesters <strong>of</strong> clinical rotations in a wideAfter graduation and certification, range <strong>of</strong> disciplines and settings follow,today’s physician assistants have a host <strong>of</strong> mainly at Parkland Memorial Hospital, butareas to consider for additional study and also through rotations in other affiliatedspecialization. These include cardiothoracic hospitals, clinics, private physician practices,surgery, dermatology, emergency medicine,and long-term care facilities. At the endneonatology, neurology, neurological surgery, <strong>of</strong> 30 months, successful students receiveobstetrics/gynecology, oncology, orthopaedica Master <strong>of</strong> Physician Assistant Studiessurgery, pediatrics, psychiatry, rheuma-degree and are eligible for the Physiciantology, surgery and urology.Assistant National Certifying ExaminationThe concept <strong>of</strong> physician assistants was required to practice. In the past five years,first introduced in the 1960s, with the first 99 percent <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong> graduatesclass graduating in 1967 from a program have passed the exam on the first try.established at Duke University MedicalCenter. The program included54655
designed for learning and practicing surgicalskills, such as knot tying, suturing and videoendoscopictechniques.Third-year students also generally take thetwo-part Step 2 USMLE. The two parts coverclinical knowledge and clinical skills. Passingeach is a requirement for graduation.YEAR FOURFourth-year students completerotations that prepare themfor internships and to apply forresidency positions. Duringthis 10-month period, students select four,four-week electives from Acute Care Clerkship,Ambulatory Care Clerkship, Sub-internship –all completed at <strong>UT</strong> <strong>Southwestern</strong> – andother electives that can be completed at<strong>UT</strong> <strong>Southwestern</strong> or elsewhere.The Acute Care Clerkship <strong>of</strong>fers instructionin the diagnosis and management <strong>of</strong> an acutelyill or injured patient, with rotations from avariety <strong>of</strong> clinical settings, including intensivecare units, critical care services and emergencydepartments. The selection sites for thisclerkship include Parkland Memorial Hospital’sburn ICU, critical care unit, emergency department,neonatal ICU, surgical ICU and traumaservice; Dallas Veterans Affairs Medical Center’scardiovascular anesthesia and surgical ICU;and Children’s Medical Center Dallas’ emergencydepartment, pediatric ICU and pediatriccardiac critical care unit.“The hospitals are wonderful places totrain because <strong>of</strong> their size and the volume <strong>of</strong>patients. The entire staff is all about gettingstudents involved in patient care and havingthem be part <strong>of</strong> the team,” said Dr. RachelJamison, Class <strong>of</strong> 2010.In the Ambulatory Care Clerkship, studentsspend one month in outpatient clinics or privatephysicians’ <strong>of</strong>fices for internal medicine,family medicine, women’s health, urologyor ophthalmology.In the Medicine Sub-Internship, studentsspend four weeks on an inpatient service in internalmedicine, pediatrics, obstetrics andgynecology, or surgery.By this point, students are an integrated part<strong>of</strong> the care team. They interview patients, obtainvital information for patient care, interpretdata, discuss the treatment plan with the patientand family, promote general health maintenanceand disease prevention, and consultwith specialty services and teams to coordinatecare. While closely supervised, fourth-yearstudents are able to provide a diagnosis and<strong>of</strong>fer treatment plans, and demonstrate theycan effectively communicate with the healthcare teams, patients and patients’ families.Four months <strong>of</strong> the fourth year <strong>of</strong> medicalschool are available for electives selected frommore than 100 courses <strong>of</strong>fered by departmentsand divisions. The electives are designed toprovide specific, extended experience in areas<strong>of</strong> particular interest to the student.“I’ve seen them ecstatic with their acceptanceinto medical school. I’ve seen them consumedby the overwhelming volume <strong>of</strong> knowledgethey must master. I’ve seen them evolve intophysicians,” said Dr. James Wagner, associatedean for student affairs and associate pr<strong>of</strong>essor<strong>of</strong> internal medicine, who has witnessed morethan 15 years <strong>of</strong> graduating classes.INTERNS AND RESIDENTSWith their medical degree inhand, quite an accomplishment,they still stand at the bottomrung <strong>of</strong> the next ladder to beclimbed. Interns are M.D.s in their first yearafter graduating medical school. The internshipcan be part <strong>of</strong> a multi-year residency, makingthe intern the equivalent <strong>of</strong> a first-year resident;or the internship may be a stand-alone programpreceding a residency. A residency lasts at leastthree years and can extend up to six or sevenyears for surgical specialties.A requirement for practicing independentlyis passing Step 3 <strong>of</strong> the USMLE. Step 3 is thefinal exam <strong>of</strong> the three-part licensing exam andis <strong>of</strong>ten taken after the first year <strong>of</strong> residencyor internship. Step 3 is a two-day exam thatcovers several hundred multiple-choice items.Residency involves clinical training targetedto a specific specialty such as internal medicine,pediatrics or surgery, as opposed to the moregeneralized teachings in medical school. Whilestudents experience a meteoric rise in knowledgeand skills during medical school, it is duringresidency where those skills are hammered,hardened and honed so that each doctor is preparedto practice medicine independently.Training for emergency medicine residentsat <strong>UT</strong> <strong>Southwestern</strong> serves as an ideal example.Emergency medicine residency trainingincludes the emergency departments <strong>of</strong> ParklandMemorial Hospital and Children’s MedicalCenter Dallas, both recognized elite Level ITrauma Centers and among the busiest in thenation in their respective categories. As anintegrated system, the departments triage morethan 200,000 adults and children annually.Emergency medicine residents performresuscitations on every shift. EM residents participatein rotations in pediatric EM, adult EM,toxicology and disaster medicine, as well asreceive training in ground and air transport.They have opportunities to practice event medicine– caring for emergencies at large eventssuch as football and baseball games – andpractice in other countries. Emergency medicineresidents also participate in disaster responseefforts locally. During Hurricane Katrina in2005, for example, <strong>UT</strong> <strong>Southwestern</strong>residents helped treat the more than 8,000patients seen in the supervised EM unit at theDallas Convention Center, operated by<strong>UT</strong> <strong>Southwestern</strong> physicians.An <strong>of</strong>ten perpetuated misconception is thatresidents should have an over-the-shoulderview in the care <strong>of</strong> a patient in a passive,watch-and-learn capacity. In reality, residencyis the time in which the new M.D. steps forwardand the attending supervising physicianmust begin to gradually step back.It is hardly an all-or-nothing proposition.Each step – forward for the resident and backingaway for the attending – is a graduated,carefully synchronized transition. Called pr<strong>of</strong>iciency-basedtraining, the process allowsthe resident to step forward only after successfullydemonstrating prior pr<strong>of</strong>iciency <strong>of</strong> theskill needed to the attending, who takes a stepback to supervise and observe.“If you look at that scenario, it is similar tohow they do things in such sports as gymnastics,”said Dr. Robert Rege, chairman <strong>of</strong> surgeryand a noted pioneer in educating surgical residents.“You are on a low beam first, and whenyou can perform certain tasks, then you areallowed to go to a higher beam. That would beBy the time <strong>UT</strong> <strong>Southwestern</strong> students and trainees exit, years <strong>of</strong> education and training have provided a rock-solid foundationto handle those most vulnerable moments <strong>of</strong> life they will experience with their patients.5657
What has changed in the past century is the amount <strong>of</strong> information the physician must process and retain. It is estimated that by2020, medical knowledge will double approximately every four months.pr<strong>of</strong>iciency-based training. You have to showcompetency at certain skills before you can gointo training for the next level <strong>of</strong> skills.”It is critical to allow residents to perform examinations,order tests, diagnose illnesses, crafttreatment plans and perform surgical procedureswith graduated independence – with moreexperienced physicians still on hand. Thisassures that when residency training is completed,the resident doctors are well-prepared tohandle the patients they will see independently.“If someone wants to say it’s immoral, becausethey’re letting doctors practice on patients,my answer to that is no, it is immoral to letsomebody into the community who is notqualified to take care <strong>of</strong> you,” said Dr. Rege,who holds the Hall and Mary Lucile ShannonDistinguished Chair in Surgery. “Within someboundary that keeps it as safe as possible, wedo need to allow that responsibility to be taken.“This is a school that values learning by doing.” — Dr. Gregory Fitz“It is how every major teaching hospital inthe country works. You’re never going tobe able to do something independently if younever have a chance first.”It is also why institutions like <strong>UT</strong> <strong>Southwestern</strong>,where students are immersed in someaspect <strong>of</strong> clinical care from year one, findspecial favor among those training to becomedoctors and those recruiting for theirresidency programs.“The quality <strong>of</strong> the scientific curriculum at<strong>UT</strong> <strong>Southwestern</strong> is unquestionable, and theclinical training, one finds out upon startingresidency, is second to none. You learn howto be a self-sufficient physician years before youever start internship,” said Dr. Scott Paulson,Class <strong>of</strong> 2008.FELLOWSHIPS ANDBEYONDWhile the conclusion <strong>of</strong> residencyprograms allows physicianswho have passed therequisite licensing tests to practice independently,many choose to continue to an evenhigher plane – becoming a fellow. Fellowshipsare <strong>of</strong>fered for expertise in subspecialties likecardiology, gastroenterology and orthopaedics,and typically involve a balance <strong>of</strong> researchand clinical care in the specified subspecialty.In emergency medicine, for example, fellowshipopportunities include toxicology, governmentemergency medical services and security,practice management and health care policy,and pediatric emergency medicine. <strong>UT</strong> <strong>Southwestern</strong>’sDepartment <strong>of</strong> Pediatrics has morethan 90 postdoctoral trainees in the sub-specialtytraining programs overseen by its divisions.To retain a medical license, physicians alsomust attend and complete continuing medicaleducation courses and accumulate creditsannually. Last year, <strong>UT</strong> <strong>Southwestern</strong> facultymembers provided continuing medical educationtraining to nearly 38,600 participants atalmost 260 activities.“To be a great physician, Dr. William Osler said in a famous speech to residents, you have to have a clear head and a kind heart.I’m not sure that’s changed in the 100 years since that statement was made.” — Dr. David Johnson (right)THE F<strong>UT</strong>URE OF MEDICALDOCTORSMore than 100 years ago, manymedical schools <strong>of</strong>fered nothingmore than lectures. This inadequacyled to a foundational critique in 1908called The Flexner Report, which laid out thefundamentals <strong>of</strong> what a medical educationshould be required to provide – and it remainsthe standard today: a robust balance <strong>of</strong> biologicaland anatomical understanding, coupledwith hands-on practice <strong>of</strong> medicine so doctorshave the knowledge and experience neededwhen they leave medical school.Dr. William Osler, still considered the father<strong>of</strong> modern medicine, created the first residencyprogram to train specialists, emphasizing theneed for students to go beyond lecture halls tolearn hands-on, bedside care.“To be a great physician, he said in a famousspeech to residents, you have to have a clearhead and a kind heart. I’m not sure that’schanged in the 100 years since that statementwas made,” said Dr. David Johnson, chairman<strong>of</strong> internal medicine at <strong>UT</strong> <strong>Southwestern</strong>.What has changed in the past century is theamount <strong>of</strong> information the physician mustprocess and retain. It is estimated that by 2020,medical knowledge will double approximatelyevery four months.While that may require changes in how doctorsaccess information – spending more timeat a computer, for instance – it shouldn’t meanphysicians simply become providers. As Dr. Fitznoted, they have to become lifelong students.“Texans actually believe there is nothingthey can’t do. They believe they can do everything.I like that attitude,” said Dr. Johnson,holder <strong>of</strong> the Donald W. Seldin DistinguishedChair in Internal Medicine, adding that theopportunity to help define the future <strong>of</strong> medicaleducation was among the reasons he decidedto come to <strong>UT</strong> <strong>Southwestern</strong>. “It’s not arrogance.It’s sort <strong>of</strong> a roll-up-your-sleeves mentality.You get that precise feeling when you walkthrough the doors here.”By the time <strong>UT</strong> <strong>Southwestern</strong> students andtrainees exit, years <strong>of</strong> education and traininghave provided a rock-solid foundation tohandle those most vulnerable moments <strong>of</strong> lifethey will experience with their patients.“By the end, idealism turns into seasonedwisdom,” Dr. Wagner said. “They learn their ownlimits, the limits <strong>of</strong> our knowledge, and thepower <strong>of</strong> a kind word, gentle touch and simplybeing there. They become accustomed to themiracle <strong>of</strong> birth, the inevitability <strong>of</strong> death, theexhilaration <strong>of</strong> cure and the devastation <strong>of</strong>failure. The magnetic pole for their moral compasschanges from within themselves to withinthe well-being <strong>of</strong> their patients.”5859
THE CLINICAL FRONTIER(special section)" What makes usunique is that wetake care <strong>of</strong> thesetwo big populations– sleep disorders andbreathing disorders."—Dr. Won LeeClinic treats sleep andbreathing disordersBy Jeff CarltonIf anyone knows the importance <strong>of</strong> a goodnight’s sleep, it’s Roland Dickey.The owner <strong>of</strong> the Dallas-based chain <strong>of</strong>barbecue restaurants that bears his name, Mr.Dickey said he’d wake up exhausted, fight <strong>of</strong>fsleep throughout the day and sometimes findhimself nodding <strong>of</strong>f while driving.He sought treatment at <strong>UT</strong> <strong>Southwestern</strong>Medical Center’s Clinical Center for Sleepand Breathing Disorders, where new medicationsand treatments are dawning in theworld <strong>of</strong> sleep medicine. One night at thecenter brought an end to Mr. Dickey’s sleepdeprivedlife.“I felt the difference immediately,”Mr. Dickey said. “I was jumping out <strong>of</strong> bedwith a lot more energy and it lasted all day.”Dr. Won Lee, medical director <strong>of</strong> the sleepcenter, located at University Hospital - St. Paul,understands that the right amount <strong>of</strong> shut-eyetranslates into a restful peace <strong>of</strong> mind and,more importantly, improved health.Unlike many sleep centers, <strong>UT</strong> <strong>Southwestern</strong>focuses not only on caring for patients withprimary sleep disorders but also those withsecondary breathing disorders resulting fromprogressive neuromuscular diseases.“What makes us unique is that we take care<strong>of</strong> these two big populations – sleep disordersand breathing disorders,” said Dr. Lee, assistantpr<strong>of</strong>essor <strong>of</strong> internal medicine.Patients with chronic sleep loss are atincreased risk for hypertension, diabetes,obesity, depression, heart attack and stroke,according to the Institute <strong>of</strong> Medicine, whichhas identified sleeping disorders as an unmetpublic health problem.In addition, researchers have linked sleeploss and sleeping disorders to more than$63 billion in lost productivity in the U.S.annually and to 20 percent <strong>of</strong> all seriousautomobile crashes.At its 6,000-square-foot facility on the secondfloor <strong>of</strong> Pr<strong>of</strong>essional Office Building 2 on<strong>UT</strong> <strong>Southwestern</strong>’s West Campus, the Centerfor Sleep and Breathing Disorders addressesthese issues head on. The center is among thenation’s most advanced and is accredited bythe American Academy <strong>of</strong> Sleep Medicine,“which guarantees that the quality <strong>of</strong> our sleeplab testing is exceptional,” Dr. Lee said.The busy clinical center, which conductsabout 120 sleep studies a month, has a six-bedsleep laboratory with private bathrooms ineach patient room, and spaces for physicianand staff member <strong>of</strong>fices, patient counselingareas and more. Patient treatment starts with acomprehensive questionnaire that leads to anindividualized plan based on each person’s specificneeds and therapy goals.Treating such a broad base <strong>of</strong> patientsrequires a multidisciplinary approach that anacademic medical center such as <strong>UT</strong> <strong>Southwestern</strong>is best equipped to provide. Thecenter’s team <strong>of</strong> pulmonologists and neurologistsare all certified or board eligible in sleepmedicine. The collaborative effort between pulmonologyand neurology is further bolsteredby a strong relationship with <strong>UT</strong> <strong>Southwestern</strong>physicians who specialize in otolaryngologyand oral maxill<strong>of</strong>acial surgery, as well as anurse practitioner and a full staff <strong>of</strong> sleep technologistswho are dually trained in both sleepmedicine and respiratory therapy.This team approach ensures that the centercan meet the respiratory and neurologicalneeds <strong>of</strong> all its patients.Those needs can be vast and varied. Thecenter sees patients suffering from some <strong>of</strong>the more common sleep problems, includingsleep apnea, insomnia, restless leg syndrome,narcolepsy and circadian rhythm disorders.The breathing disorders program, led by Dr.Joseph Viroslav, pr<strong>of</strong>essor <strong>of</strong> internal medicine,focuses on the assessment and management<strong>of</strong> respiratory problems in patients with neuromusculardiseases, including amyotrophiclateral sclerosis, muscular dystrophy, spinalcord injuries and scoliosis.The center features state-<strong>of</strong>-the-art diagnosticand treatment equipment, includingadvanced monitoring s<strong>of</strong>tware that collectsdata on sleep parameters; sophisticatedpolysomnogram usage and subsequent interpretations;and use and education <strong>of</strong> patientson continuous and bilevel positive airwaypressure devices (better known as CPAP andBPAP machines).Open since 2007, the center already hasestablished itself as the region’s premier facilityfor sleeping and breathing disorders.“There is not always a lot we can do inmedicine that can make an immediate impacton someone’s quality <strong>of</strong> life,” Dr. Lee said.“But when we effectively treat sleeping disorders,people immediately feel better. And theopportunity to see that day in and day out isvery satisfying.”uFor more information about sleep therapy, pleasecall 214-645-5337.Targeted therapy foradvanced gynecologiccancersBy Robin RussellAdvanced endometrial cancer patients aretypically treated with both surgery and chemotherapy,but long-term prognosis remains poor.The five-year survival rate for Stage 3 patientsis just 50 percent; for Stage 4, it drops to 20percent. Optimizing additional therapy foradvanced endometrial cancers remains an area<strong>of</strong> significant research interest.Now, <strong>UT</strong> <strong>Southwestern</strong> researchers areworking with the Gynecologic OncologyGroup (GOG), a nonpr<strong>of</strong>it organization dedicatedto research in gynecologic cancer, andsupported by the National Cancer Institute<strong>of</strong> the National Institutes <strong>of</strong> Health. Theyare seeking to improve outcomes by <strong>of</strong>feringa national clinical trial in hopes that oneor more <strong>of</strong> three biologic targeted agents, incombination with chemotherapy, will be moreeffective than the standard care for endometrialcancer, or cancer <strong>of</strong> the uterine lining.For advanced endometrial cancer, chemotherapytypically consists <strong>of</strong> carboplatin andpaclitaxel, given every three weeks for a total<strong>of</strong> six treatments. In the current trial, GOG86 P, patients are randomly assigned to alsoreceive one <strong>of</strong> three therapeutic agents shownto be effective in other types <strong>of</strong> cancer.“This is useful for patients with advanced orrecurrent endometrial cancer because it <strong>of</strong>fersthem the opportunity to receive a targetedagent that would not be available otherwise.These types <strong>of</strong> trials will hopefully providegreater benefit for endometrial cancerpatients,” said Dr. Jayanthi Lea, an assistantpr<strong>of</strong>essor in the division <strong>of</strong> gynecologic oncology.“The design <strong>of</strong> this trial is enticing –exploring three novel agents, using a randomizedthree-armed study pattern.”Endometrial cancers arethe most common gynecologiccancers in the U.S.,with over 35,000 womendiagnosed each year, andthe third-most commoncause <strong>of</strong> gynecologic cancerdeath, behind ovarian andcervical cancer.Symptoms includepostmenopausal vaginalbleeding, irregular vaginalbleeding in premenopausalwomen, pelvic pain andpelvic mass. The cornerstone<strong>of</strong> treatment is surgicalremoval <strong>of</strong> the uterus,tubes, ovaries and lymphnodes to remove the bulk <strong>of</strong>the disease and to assess thestatus <strong>of</strong> the lymph nodes,the size and histology <strong>of</strong> thetumor, the depth <strong>of</strong> invasion,and the stage <strong>of</strong> the disease.Advanced stage patients alsoreceive chemotherapy.Patients in the GOG 86 P trial randomlyreceive either an mTOR inhibitor, whichinhibits some <strong>of</strong> the enzymes needed for cellgrowth; bevacizumab, which is an angiogeneticactivator and can block enzymes neededfor cell growth; or a novel antimitotic agent,which inhibits cancer growth by stoppingcell division in combination with bevacizumab.Each is given in combination withthe one or two standard chemotherapy drugs.Maintenance treatment will be given followinga planned course <strong>of</strong> chemotherapy.Researchers participating in the GOG 86P clinical trial hope to test 330 patients in a23-month period at multiple medical centersacross the U.S. Several gynecologic oncologistsin the Dallas-Fort Worth area already havereferred patients to <strong>UT</strong> <strong>Southwestern</strong> for thistrial, Dr. Lea said.About 45 GOG clinical trials are active atany one time for patients with a variety <strong>of</strong>gynecologic malignancies. <strong>UT</strong> <strong>Southwestern</strong>currently has 19 GOG trials open.uFor more information about GOG clinical trials,please call 214-645-4673." The design <strong>of</strong> thistrial is enticing– exploring threenovel agents, usinga randomizedthree-armed studypattern."—Dr. Jayanthi Lea60SO<strong>UT</strong>HWESTERN MEDICINE61
THE CLINICAL FRONTIER(special section)" There are probablymany genes involvedand several geneshave already beendiscovered."—Dr. Deborah FriedmanMaking headwayon headachesBy Russell RianOnly about half those suspected <strong>of</strong> havingit are ever diagnosed.There’s no cure.No known cause yet.Its triggers can seem little more than ajumble <strong>of</strong> endless possibilities.And effective treatments are sometimeselusive.Migraine pain has proven an exasperatingheadache not only for sufferers, but for thephysicians and researchers engaged in tracingthose triggers, targeting effective treatmentsand tracking down its genetic causes.More than 35 million Americans reportsuffering from the pain <strong>of</strong> migraines, whichhas become one <strong>of</strong> the most common reasonsfor missed work, second only to back pain.Migraines are about three times more commonin women than men and are thought to belinked to estrogen fluctuations.Half <strong>of</strong> all migraine sufferers have their firstattack before the age <strong>of</strong> 12. Roughly 7 percent<strong>of</strong> children experience migraine pain, and childrenare more likely to have migraines if theirparents also suffer them. Children sufferingfrom migraines are absent from school twice as<strong>of</strong>ten as children who don’t have them.“Migraine is not just a headache,” explainsDr. Deborah Friedman, pr<strong>of</strong>essor <strong>of</strong> neurologyand neurotherapeutics at <strong>UT</strong> <strong>Southwestern</strong>Medical Center and a national expert on headaches.”Many structures throughout the brainare involved in migraine to explain the pain,nausea, light and sound sensitivity, emotionalchanges, confusion and other symptoms<strong>of</strong> migraine. While there is still much to belearned, migraine research has flourished duringthe past 10 years.”People with recurrent migraines likelyhave a genetic predisposition to them, saidDr. Friedman, also a pr<strong>of</strong>essor <strong>of</strong> ophthalmology.About 80 percent <strong>of</strong> sufferers report afamily history <strong>of</strong> migraines, and a child has a50 percent chance <strong>of</strong> having migraines if oneparent suffers them and a 75 percent chance ifboth parents experience migraines, accordingto recent studies. People with other types <strong>of</strong>neurological disease such as epilepsy, as wellas those with asthma and some psychiatricdiseases such as depression or anxiety, also aremore likely to experience migraines.“There are probably many genes involvedand several genes have already been discovered,”Dr. Friedman said.Research has shown that patients withfrequent or severe migraines are best managedat a headache center like the Headache andFacial Pain Program being established at<strong>UT</strong> <strong>Southwestern</strong> under Dr. Friedman’s direction.The migraine brain is more “sensitive” tovarious trigger factors and to a process calledcortical spreading depression (CSD), which isa wave <strong>of</strong> increased excitability <strong>of</strong> nerve cells,followed by decreased excitability and changesin blood flow. Researchers also have identifiedchanges in and around the blood vessels thatsupply the lining <strong>of</strong> the brain and release <strong>of</strong>various chemicals in the brain that create painand inflammation.About 15 percent to 20 percent <strong>of</strong> peoplewith migraines get an “aura,” neurologicalsymptoms that signal the onset <strong>of</strong> a migraine.An aura can last anywhere from five minutesto nearly an hour before fading as the migrainetakes over. These can include visual cues –wavy or jagged lines, flashing light or dots,blind spots and tunnel vision. Sufferers alsomay experience strange smells and sounds,tingling or numbness.A proactive first step if you suspectmigraines is to seek out migraine experts whocan start ruling out other causes, such as tensionor other types <strong>of</strong> headaches. Commonindicators include a lack <strong>of</strong> relief from overthe-countermedications and severe headachesthat occur on a routine or cyclical basis.The program at <strong>UT</strong> <strong>Southwestern</strong> can <strong>of</strong>ferthe expertise <strong>of</strong> neurologists specializing inheadache medicine, anesthesiologists who arepain management specialists, plastic surgeonswith nerve decompression expertise, oromaxill<strong>of</strong>acialsurgeons, physical therapists, psychologists,acupuncturists, nutritionists and speciallytrained support staff attuned to the sensitivitiesexperienced by headache suffers. The programwill include state-<strong>of</strong>-the-art outpatient andinpatient therapy.In addition, <strong>UT</strong> <strong>Southwestern</strong>’s plasticsurgery faculty has surgical treatments formigraines if more traditional therapies don’tprovide relief. Dr. Jeffrey Janis, associate pr<strong>of</strong>essor<strong>of</strong> plastic surgery, helped champion atechnique that uses Botox – typically knownfor cosmetic uses – to help potential peripheralnerve trigger points that may be contributingto migraine pain. He also was involved in thedevelopment <strong>of</strong> surgical techniques based onanatomical studies to decompress these nervesin order to provide more long-lasting symptomaticrelief.In a recently published study, Dr. Janiscorroborated the effectiveness <strong>of</strong> using Botoxand surgery to treat migraine headaches,with participants reporting an averageimprovement <strong>of</strong> 85.5 percent over theiroriginal symptoms.“This represents the type <strong>of</strong> clinicalresearch into the effectiveness <strong>of</strong> new treatmentswe need,” said Dr. Janis, chief <strong>of</strong> plasticsurgery at Parkland Memorial Hospital.The new headache program has similarresearch plans.“We will conduct clinical research in headachedisorders so our patients will have theopportunity to help determine the effectiveness<strong>of</strong> new treatments as they are in the developmentstage,” Dr. Friedman noted.Current research is targeting specific aspects<strong>of</strong> the migraine process, such as chemicalsinvolved in the generation <strong>of</strong> inflammation,changes in blood vessels, and mediators <strong>of</strong> thepain process (CGRP, substance P, nitric oxide,serotonin receptors and others). In addition,Dr. Janis plans further research into possiblecompression points <strong>of</strong> peripheral nerves, proteomics<strong>of</strong> nerves and quality <strong>of</strong> life studies.Drug prevention therapy generallyinvolves anti-seizure medications, antidepressantsor medications used for high blood pressure,such as calcium channel blockers andbeta blockers. Drug therapy for pain relief maycome in the form <strong>of</strong> pills, injections or even anasal spray. Many migraine sufferers find relieffrom triptans, which help control pain andother symptoms such as nausea and sensitivityto light and noise.Nerves supplying muscles in the neck areconnected to the circuits in the brain stem thatare involved in migraines, so physical therapyand treatments directed at the neck are sometimesbeneficial. Medical procedures, such asoccipital nerve stimulation and transcranialmagnetic stimulation, also may help patientswho have severe migraines that cannot be controlledwith conventional medications.Unfortunately, the solutions can haveside effects, such as gastrointestinal disruptionor increased likelihood <strong>of</strong> kidney stones.Dr. Friedman said staying hydrated can sometimeshelp avoid kidney stones, which stillremain relatively rare. Previous research at<strong>UT</strong> <strong>Southwestern</strong> showed that long-term use<strong>of</strong> the popular migraine drug topiramate maymake patients more likely to develop stones.People who took the drug for more than ayear had chemical changes in their bloodand urine that are associated with increasedrisk for kidney stone formation, according toresearch by Dr. Khashayar Sakhaee, chief <strong>of</strong>mineral metabolism and holder <strong>of</strong> the LauraKim Pak Pr<strong>of</strong>essorship in Mineral MetabolismResearch and the BeautiControl CosmeticsInc. Pr<strong>of</strong>essorship in Mineral Metabolismand Osteoporosis.From specialists in neurology to plasticsurgeons, from physical therapists to nutritionists,from inpatient stays to outpatient therapy,<strong>UT</strong> <strong>Southwestern</strong>’s Headache and FacialPain Program will apply a multidisciplinaryapproach in matching each migraine patientwith the most effective treatment options. u" We will conductclinical research inheadache disordersso our patients willhave the opportunityto help determinethe effectiveness<strong>of</strong> new treatmentsas they are in thedevelopment stage."—Dr. Deborah Friedman62SO<strong>UT</strong>HWESTERN MEDICINE63
A20 1 1N N U A LR E V I E W66HIGHLIGHTS OF THE YEAR42 76FINANCIAL STATEMENT44 79GIFT REPORT5355S O U T H W E S T E R N M E D I C I N E 65
H I G H L I G H T SH I G H L I G H T S<strong>of</strong> the yearF A L L 2 0 1 0MEDICAL CENTERESTABLISHES GLOBALHEALTH OFFICE<strong>UT</strong> <strong>Southwestern</strong> establishedan Office for Global Health todirect and develop training andresearch initiatives with partnersaround the world. Headed byDr. Fiemu Nwariaku, the new<strong>of</strong>fice expands the institutionalmission by integrating existinginternational activities,establishing new programs andtraining courses, and serving asa resource for faculty andstudents who wish to workabroad.A task forcefor globalhealth andcare for theunderservedwas estab -lished in 2009as part <strong>of</strong> themedicalDR. FIEMU NWARIAKUcenter’sstrategic priorities.By fall 2011, <strong>UT</strong> South -western’s farsighted initiative insupport <strong>of</strong> its missions <strong>of</strong>education, research and patientcare had resulted in three newinstitutional partnerships. Themedical center’s academic andscientific alliances are with SunYat-sen University and its FirstAffiliated Hospital inGuangzhou, China; with RabinMedical Center in Israel; andwith the University <strong>of</strong> CapeTown in South Africa.<strong>UT</strong> <strong>Southwestern</strong> also has anagreement with the University<strong>of</strong> Paris for an internationalmedical student exchangeprogram.SCIENTISTS CREATEEXPERIMENTALALZHEIMER’S VACCINEAfter seven years <strong>of</strong> laboratorywork, researchers at <strong>UT</strong> South -western have created anexperimental vaccine againstbeta-amyloid, the small proteinthat forms plaques in the brainand is believed to contribute tothe development <strong>of</strong> Alzheimer’sdisease.The new experimentalvaccine stimulated more than10 times as many antibodiesthat bind to and eliminate betaamyloidcompared with similarso-called DNA vaccines that thescientists tested in an animalstudy, said Dr. Roger Rosenberg,director <strong>of</strong> the Alzheimer’sDisease Center at <strong>UT</strong> South -western.A traditional vaccine – aninjection <strong>of</strong> beta-amyloidprotein itself into the arm – hasbeen shown in other research totrigger an immune response,including the production <strong>of</strong>antibodies and other bodilydefenses against beta-amyloid.However, the immune responseto this type <strong>of</strong> vaccinesometimes caused significantbrain swelling, so Dr. Rosenbergand his colleagues focused ondeveloping a nontraditionalDNA vaccine.The new DNA vaccine doesnot contain beta-amyloid itselfbut instead a piece <strong>of</strong> the betaamyloidgene that codes for theprotein. Once in the body, theDNA stimulated an immuneresponse, including antibodiesto beta-amyloid.OBESITY-RELATEDINFLAMMATIONSPURS RESEARCHSpecialists at <strong>UT</strong> <strong>Southwestern</strong>are investigating how fat tissue“talks” to the brain and the liverto promoteinflammationrelateddisorders suchas diabetes,heart diseaseand obesity.A five-year,$8 millionDR. PHILIPP SCHERERgrant from theNational Institutes <strong>of</strong> Healthtakes advantage <strong>of</strong> expertiseacross the <strong>UT</strong> <strong>Southwestern</strong>campus, including faculty in theTouchstone Center for DiabetesResearch, the division <strong>of</strong>hypothalamic research, and thedepartments <strong>of</strong> moleculargenetics, internal medicine, andpharmacology.Dr. Philipp Scherer, director<strong>of</strong> the Touchstone Center, saidthe work will tackle thecomplexity <strong>of</strong> how adipose [fat]tissue, the brain and the livertalk to each other and how thiscross talk affects metabolismand inflammation.In 2007, the Task Force forObesity Research at <strong>UT</strong> South -western (TORS) received a$22 million NIH grant toenhance the institution’sgroundbreaking obesityresearch. Dr. Scherer said thatwhile there is clearly synergywith the TORS grant, this neweffort is unique because it isspecifically focused onphenomena related toinflammation, considered anunderlying cause <strong>of</strong> metabolicdisorders in humans.The five laboratories involvedin the project will workindividually on two commonareas: identifying the criticalsites for lipid-relatedinflammation in the periphery<strong>of</strong> the body as well as the brain,and identifying the biochemicalsignals that take place in thebody after exposure to high-fat,lipid-rich foods.W I N T E R 2 0 1 0 - 2 0 1 1POTENTIAL NOVELTREATMENT FOR TYPE 1DIABETES IS UNCOVEREDType 1 diabetes could beconverted to a non-insulindependentdisorder byeliminating the actions <strong>of</strong> aspecific hormone, <strong>UT</strong> South -western research suggests.The findings, in mice, showthat insulin becomes completelysuperfluous and its absence doesnot cause diabetes or any otherabnormality when the actions <strong>of</strong>glucagon are suppressed.Glucagon, a hormone producedby the pancreas, prevents lowblood sugar levels in healthyindividuals. It causes high bloodsugar in people with type 1diabetes.Insulin treatment has beenthe gold standard for type 1diabetes (insulin-dependentdiabetes) in humans since itsdiscovery in 1922. But evenoptimal regulation <strong>of</strong> type 1diabetes with insulin alonecannot restore normal glucosetolerance. The new findingsdemonstrate that theelimination <strong>of</strong> glucagon actionrestores glucose tolerance tonormal.In type 1 diabetes, whichaffects about 1 million people inthe U.S., the pancreatic isletcells that produce insulin aredestroyed. As a countermeasureto this destruction, type 1diabetics currently must takeinsulin multiple times a day.In this study, <strong>UT</strong> South -western scientists led by Dr.Roger Unger, pr<strong>of</strong>essor <strong>of</strong>internal medicine, tested howmice genetically altered to lackworking glucagon receptorsresponded to an oral glucosetolerance test. The test measuresthe body’s ability to metabolize,or clear, glucose from thebloodstream. The researchersfound that the mice withnormal insulin production butwithout functioning glucagonreceptors responded normally tothe test.BUSY TRANSPLANTTEAM RECORDS 400THHEART PROCEDURESandra Childers became the400th adult patient to receive aheart transplant at UniversityHospital – St. Paul.When Mrs. Childers hearsher heartbeat, she still isamazed. She was without a pulseduring the six-month span shewore a left ventricular assistdevice (LVAD) that helped herheart pump blood throughouther body. “Now I can actuallyhear and feel a heart. And itfeels wonderful,” she said.Through summer 2011,<strong>UT</strong> <strong>Southwestern</strong> hearttransplant surgeons hadperformed 428 procedures at St.Paul alone, as well as additionaltransplants at the medicalcenter’s affiliated hospitals.LVADs allow patients to leavethe hospital while they arewaiting for a transplant.Reaching the milestone was atestament to the commitment<strong>of</strong> many, including the surgicalteam <strong>of</strong> Dr. Mark Drazner,medical director <strong>of</strong> the HeartFailure and CardiacTransplantation Program; Dr.Dan Meyer, pr<strong>of</strong>essor <strong>of</strong>cardiovascular and thoracicsurgery, whose group isinstrumental in implanting theLVADs; and clinical nursespecialist Patricia Kaiser, whohas been with the program sinceits beginning.NANOTECHNOLOGYSUPPORT HELPSLAB MOVE FORWARDAlmost $5 million in fundingis moving the manufacturingand delivery <strong>of</strong> nanotechnologybasedmaterials toward reality.Nanotechnology has shownpromise for both diagnosingand treating a range <strong>of</strong> medicalconditions including cancer,autoimmune disease and humanimmunodeficiency virus, butdeveloping a reliable way tomanufacture those potentiallylifesaving particles in largequantities for use in humans hasremained a challenge.Sen. Kay Bailey Hutchisonwas instrumental in securingresources from the Department<strong>of</strong> Defense to build a laboratoryto research and produce carbonbasednanoparticles and toprepare biological materials thatcan then be delivered topatients. She also providedcritical federal support for theconstruction <strong>of</strong> the GoodManufacturing Process (GMP)Nanoparticle and CellProcessing Lab on the<strong>UT</strong> <strong>Southwestern</strong> campus, incollaboration with <strong>UT</strong> Dallas.DRS. ROGER UNGER AND YOUNG LEE66S O U T H W E S T E R N M E D I C I N E 67
H I G H L I G H T SH I G H L I G H T SDr. James K.V. Willson,director <strong>of</strong> the Harold C.Simmons Cancer Center, theonly National Cancer Institutedesignatedcenter in NorthTexas, said that having this GMPfacility will provide a uniqueopportunity for researchers toprepare cell materials – such asthe hematopoietic stem cellsroutinely used to treat leukemia– for use in humans. Theexisting GMP laboratory in theCancer Immunobiology Centeris Food and Drug Admini -stration-approved to produceantibodies and vaccines but notcells treated with these agents.GMP facilities are regulatedby the FDA and must be built toexacting federal specifications.These facilities remain understrict environmental control inorder to assure the manufacture<strong>of</strong> sterile, potent anduncontaminated products forhuman therapies.NEWBORN HEARTMUSCLE HAS ABILITYTO REGENERATEResearchers at <strong>UT</strong> South -western have discovered in micethat the mammalian newbornheart can heal itself completely.The scientists found that aportion <strong>of</strong> the heart removedduring the first week after birthgrew back wholly and correctly– as if nothing had happened.Dr. Hesham Sadek, assistantpr<strong>of</strong>essor <strong>of</strong> internal medicine,was co-senior author with Dr.Eric Olson, chairman <strong>of</strong>molecular biology and director <strong>of</strong>the Nancy B.and Jake L.Hamon Centerfor BasicResearch inCancer. Dr.Sadek said theheart <strong>of</strong>newbornDR. ERIC OLSONmammals can fix itself; it justforgets how as it gets older. Thechallenge now is to find a way toremind the adult heart how to fixitself, an important step in thesearch for a cure for heart disease,the No. 1 killer in the developedworld.The researchers found thatwithin three weeks <strong>of</strong> removing15 percent <strong>of</strong> the newbornmouse heart, it was able to growback the lost tissue completely,and as a result looked andfunctioned just like a normalheart. The researchers believethat uninjured beating heartcells, called cardiomyocytes, are amajor source <strong>of</strong> the new cells.Dr. Olson, who holds theAnnie and Willie NelsonPr<strong>of</strong>essorship in Stem CellResearch and the PogueDistinguished Chair in Researchon Cardiac Birth Defects, said theinability <strong>of</strong> the adult heart toregenerate following injuryrepresents a major barrier incardiovascular medicine. “Thiswork demonstrates that cardiacregeneration is possible in themammalian heart during awindow <strong>of</strong> time after birth. Withthis knowledge, we can nextwork to discover methods toreawaken cardiac regeneration inadulthood,” he said.S P R I N G 2 0 1 1CPRIT AWARDS$36.7 MILLION FORCANCER STUDIESThe Cancer Prevention andResearch Institute <strong>of</strong> Texas(CPRIT) awarded more than$36.7 million in new grants to<strong>UT</strong> <strong>Southwestern</strong> investigatorsto support cancer-relatedprojects and recruit pre-eminentcancer investigators.These awards, made after arigorous peer-review process,resulted in <strong>UT</strong> <strong>Southwestern</strong>receivingmore fundingthan anyotherindividualTexasinstitution inthis round <strong>of</strong>grants. AwardsDR. JAMES K.V.to <strong>UT</strong> South -WILLSONwesternresearchers were part <strong>of</strong>$116 million allocated for 22projects at 16 Texas-basedacademic institutions andprivate firms by CPRIT,established in 2007 after Texasvoters approved a constitutionalamendment that authorized thestate to fund cancer researchand prevention programs.<strong>UT</strong> <strong>Southwestern</strong> leaders saidsupport from CPRIT – now at$115 million for more than 70projects over the past two years– will accelerate dramatically theimpact <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>research on cancer care andillustrate the importance <strong>of</strong>teams <strong>of</strong> physicians andinvestigators working togetherto defeat the disease.Dr. James K.V. Willson,director <strong>of</strong> the Harold C.Simmons Cancer Center, saidthe awards fund projectshighlighting the forefront <strong>of</strong>translating basic science andlaboratory findings intopractical treatments andtechnologies.NEW HOSPITALPROJECT SURGESWITH SUPPORTThe north end <strong>of</strong> campusbegan a four-yeartransformation, as the medicalcenter swung into action for thenew University Hospital, an$800 million state-<strong>of</strong>-the-artfacility slated to open in 2015.Several clinical service lines,<strong>of</strong>fices and departments wererelocated prior to siteCONSTRUCTION CREWS OPERATING HEAVY EQUIPMENT WORK ON THE FOUNDATION OF THE NEWUNIVERSITY HOSPITAL. <strong>UT</strong> SO<strong>UT</strong>HWESTERN LEADERS, COMMUNITY DIGNITARIES AND MEDICALCENTER SUPPORTERS GATHERED AT THE SITE EARLIER IN CELEBRATION OF THE PROJECT’SSTART.preparation and buildingdemolition, which began in thespring.The 12-floor, 460-bedhospital – which will be thekeystone facility on a 32-acretract on the southwest side <strong>of</strong>Harry Hines Boulevard betweenMockingbird Lane and InwoodRoad – is an essential step in<strong>UT</strong> <strong>Southwestern</strong>’s plan tobecome one <strong>of</strong> the nation’s verytop comprehensive academicmedical centers.The $800 million hospital –designed by architectural firmRTKL Associates and being builtby the Hunt ConstructionGroup – will replace UniversityHospital - St. Paul, which cannotbe expanded to handle growingcapacity needs or economicallyrenovated to incorporate thetechnology required to practicethe medicine <strong>of</strong> the future.University Hospital - St. Paulwill remain fully operationaluntil the new 1.31-million-square-foot facility opens.The goal <strong>of</strong> <strong>UT</strong> South -western’s Building the Future <strong>of</strong>Medicine capital campaign is toraise $200 million in privatesupport for the new UniversityHospital. When first announced,the campaign had alreadysecured commitments <strong>of</strong> nearly$62 million from communitysupporters. In addition,<strong>UT</strong> <strong>Southwestern</strong> physicianshave committed $200 million <strong>of</strong>their clinical earnings to supportthe project.Dr. Daniel K. Podolsky,president <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>,said the facility represents theforefront <strong>of</strong> design for patientcentrichospitals <strong>of</strong> the future,integrating best practicesgathered from the nation’s topmedical facilities with theinnovation and high standards<strong>of</strong> research and education thatthe medical center is known foraround the world.[See story ….. Page 34]PEDIATRICIANSUNDERTAKEUNPRECEDENTEDLONGITUDINALCHILDREN’S STUDY<strong>UT</strong> <strong>Southwestern</strong> pediatriciansare helping lead the largest longtermstudy <strong>of</strong> children’s health inthe U.S.The multicenter study willeventually follow 100,000children nationwide from birthuntil age 21 to determine howvarious factors, includingenvironmental and geneticones, affect a child’s health,development and quality <strong>of</strong> life.The findings may help form thebasis <strong>of</strong> child health guidance,interventions and policy forfuture generations.Dr. George Lister, formerchairman <strong>of</strong> pediatrics, isprincipal investigator for theNorth Texas Children’s StudyCoalition, a collaboration <strong>of</strong>three <strong>UT</strong> System campuses andBattelle Memorial ResearchInstitute in Columbus, Ohio. Hesaid the significance <strong>of</strong> thestudy can’t be overstated. Thelocal core will be in LamarCounty, about 100 milesnortheast <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>,along the Texas-Oklahomaborder.Now associate dean foreducation for <strong>UT</strong> <strong>Southwestern</strong>Medical School, Dr. Lister iscollaborating on the study withDr. Debra Cherry, principalinvestigator for the LamarCounty location andoccupational medicinephysician at the <strong>UT</strong> HealthScience Center at Tyler.Dr. Lister said the team hopesto enroll and follow 1,000Lamar County children. Theundertaking is an observationalresearch study rather than aclinical trial, so participants willnot be asked to change theirday-to-day routines or take anymedicines or drugs. Staff68S O U T H W E S T E R N M E D I C I N E 69
H I G H L I G H T SH I G H L I G H T Sinitially will collect data onpregnancies, such as theparticipant’s diet, chemicalexposure and emotional stress.Once new children are born, theresearchers will begin collectingbiological samples as well asenvironmental samples.NATIONAL ACADEMY OFSCIENCES ELECTSPARADA TO MEMBERSHIPThe NationalAcademy <strong>of</strong>Scienceselected Dr. LuisF. Parada,chairman <strong>of</strong>developmentalbiology, tomembership,DR. LUIS F. PARADArepresentingone <strong>of</strong> the highest honorsattainable by an Americanscientist.With Dr. Parada’s election,<strong>UT</strong> <strong>Southwestern</strong> now has 19members <strong>of</strong> this prestigioussociety among its faculty, morethan all others in Texascombined.Dr. Parada directs the KentWaldrep Center for BasicResearch on Nerve Growth andRegeneration and holds the<strong>Southwestern</strong> Ball DistinguishedChair in Nerve RegenerationResearch and the Diana K. andRichard C. Strauss DistinguishedChair in Developmental Biology.His research integrates thefields <strong>of</strong> molecular genetics,embryonic development andsignal transduction. His studieshave provided critical insightsinto brain development,associated disorders and cancerbiology, and have led to theidentification <strong>of</strong> molecules thatinhibit nerve regeneration afterinjury.His laboratory focuses on theregulatory pathways thatcontrol the complex process <strong>of</strong>nervous system developmentand the consequences <strong>of</strong>inappropriate development,which can include behavioraland mood disorders, as well ascancer.S U M M E R 2 0 1 1BE<strong>UT</strong>LER RETURNS;BECOMES <strong>UT</strong>SW’S5TH NOBEL LAUREATEDr. Bruce Beutler, aninternationally recognizedleader in immunology andmember <strong>of</strong> the NationalAcademy <strong>of</strong> Sciences, wasselected as the founding director<strong>of</strong> a new Center for the Genetics<strong>of</strong> Host Defense at <strong>UT</strong> South -western.His anticipated arrival wasquickly followed by news <strong>of</strong> hiswinning the Shaw Prize,sometimes referred to as the“Nobel Prize <strong>of</strong> the East.” Thatrecognition was followed by theultimate honor for Dr. Beutler –the 2011 Nobel Prize inPhysiology or Medicine.Dr. Beutler and Dr. Jules A.H<strong>of</strong>fmann <strong>of</strong> StrasbourgUniversity’s Institut de BiologieMoléculaire et Cellulaire inFrance shared half the NobelPrize for their discovery <strong>of</strong>receptor proteins that recognizedisease-causing agents andactivate innate immunity, thefirst step in the body’s immuneresponse. The other half went tothe late Dr. Ralph M. Steinman<strong>of</strong> Rockefeller University in NewYork.Dr. Beutler, who started hisscientific career at <strong>UT</strong> South -western as an internal medicineintern and neurology resident,served as a faculty member from1986 to 2000. Dr. Beutler madehis seminal discoveries at<strong>UT</strong> <strong>Southwestern</strong> whilesearching for a receptor able tobind the bacterial productlipopolysaccharide, which cancause life-threatening septicshock, a condition that involvesoverstimulation <strong>of</strong> the immunesystem.Recruited from ScrippsResearch Institute in La Jolla,Calif., where he has developedone <strong>of</strong> the most robust genediscovery programs in theworld, Dr. Beutler has focusedon the genetics <strong>of</strong> innateimmunity. The implications <strong>of</strong>his findings are broadly relevantto host responses to viralinfection, cancer developmentand autoimmunity.<strong>UT</strong> <strong>Southwestern</strong> facultymembers now have won fiveNobel Prizes since 1985. Dr.Michael Brown and Dr. JosephGoldstein (1985), Dr. JohannDeisenh<strong>of</strong>er (1988), Dr. AlfredGilman (1994) and Dr. Beutler(2011) have been honored bythe Nobel Assembly atKarolinska Institutet in Sweden.[See story ….. Page 26]PRESIDENT’S RESEARCHCOUNCIL HONORSSCIENTISTS WITHDISTINGUISHED YOUNGRESEARCHER AWARDSThe President’s ResearchCouncil presented its 2011Distinguished Young ResearcherAward to a pair <strong>of</strong> outstanding<strong>UT</strong> <strong>Southwestern</strong> investigators.The recipients – Dr. Kevin Choe,assistant pr<strong>of</strong>essor <strong>of</strong> radiationDR. KEVINCHOEDR. SHUSHENGWANGoncology, and Dr. ShushengWang, assistant pr<strong>of</strong>essor <strong>of</strong>ophthalmology andpharmacology – each received a$65,000 award.Dr. Choe said PRC supportwill enable him to makemeaningful contributions to theunderstanding <strong>of</strong> glioma biologyas he seeks to identify potentialtherapeutic targets formalignant gliomas, the mostcommon type <strong>of</strong> brain cancer inadults. Malignant gliomas arenotoriously resistant to conven -tional therapy, Dr. Choe said.Dr. Choe earned a doctoratein cell biology and a medicaldegree from the Albert EinsteinCollege <strong>of</strong> Medicine in 2005after receiving a degree inbiology from the MassachusettsInstitute <strong>of</strong> Technology in 1997.He completed an internship atYale University and residency atthe University <strong>of</strong> Chicago beforejoining the <strong>UT</strong> <strong>Southwestern</strong>faculty in 2010.Dr. Wang is investigating therole <strong>of</strong> microRNAs in retinalvascular development anddisease, focusing on how theyregulate multiple pathways inage-related maculardegeneration (AMD). Hisresearch has therapeuticimplications for neovascularAMD, the leading cause <strong>of</strong>blindness in the elderly. AMDaffects about 2 million people inthe U.S.Dr. Wang received hisdoctoral degree in develop -mental biology from TulaneUniversity after earning amaster’s degree in cell biologyfrom Peking University inBeijing. He went on to dopostdoctoral work in molecularbiology at <strong>UT</strong> <strong>Southwestern</strong>before joining the faculty in2009.The Distinguished YoungResearcher Award is presentedannually by the PRC, which ismade up <strong>of</strong> community leaderswho are interested in learningabout and advancing medicalresearch at <strong>UT</strong> <strong>Southwestern</strong>.365 EARN DEGREESFROM THREE SCHOOLSDiplomas were received by 207<strong>UT</strong> <strong>Southwestern</strong> MedicalSchool students and 42<strong>UT</strong> <strong>Southwestern</strong> GraduateSchool <strong>of</strong> Biomedical Sciencesstudents in Junecommencement ceremonies.In mid-December 2010, 116students graduated from the<strong>UT</strong> <strong>Southwestern</strong> School <strong>of</strong>Health Pr<strong>of</strong>essions. Thecommence ment ceremony, overwhich dean Dr. Raul Caetanopresided, took place in the Tomand Lula Gooch Auditorium.Dr. Francisco G. Cigarroa,chancellor <strong>of</strong> the <strong>UT</strong> System and1983 graduate <strong>of</strong> <strong>UT</strong> South -western Medical School,addressed the medical schoolgraduates and guests. Thegraduate school’s address wasdelivered by Dr. Melanie Cobb,pr<strong>of</strong>essor <strong>of</strong> pharmacology andformer dean <strong>of</strong> the school.<strong>Southwestern</strong> MedicalFoundation’s Ho Din Award, thetop graduating medical studentaward, was presented to Dr.George “Ge<strong>of</strong>” LeBus. Ying Liureceived the Nominata Award,given to the outstandinggraduate school student.Dr. Daniel K. Podolsky,president <strong>of</strong> the medical center,conferred the degrees, diplomasand certificates to all <strong>of</strong> themedical, graduate and healthpr<strong>of</strong>essions students.U.S. NEWS AGAINCITES CARE AREASIN ‘BEST HOSPITALS’For the second year in a row,<strong>UT</strong> <strong>Southwestern</strong> is the toprankedhospital in the Dallas-Fort Worth region, according toU.S. News & World Report’sannual ranking <strong>of</strong> the nation’sbest hospitals.<strong>UT</strong> <strong>Southwestern</strong> earned itsNo. 1 ranking by beingDR. GEORGE “GEOF” LEBUS (RIGHT) RECEIVES THE HO DIN AWARD FROM W. PLACK CARR JR.,EXEC<strong>UT</strong>IVE VICE PRESIDENT OF SO<strong>UT</strong>HWESTERN MEDICAL FOUNDATION.70S O U T H W E S T E R N M E D I C I N E 71
H I G H L I G H T SH I G H L I G H T Snationally recognized in sixspecialties: urology,cardiology/heart surgery,diabetes/endocrinology,gynecology, nephrology andneurology/neurosurgery. Themagazine also rated <strong>UT</strong> South -western as high-performing insix specialties: cancer,ear/nose/throat,gastroenterology, geriatrics,orthopaedics and pulmonology.Dr. Daniel K. Podolsky,president <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>,said the ratings acknowledge<strong>UT</strong> <strong>Southwestern</strong>’s UniversityHospitals & Clinics’ placeamong the nation’s leadingmedical institutions inproviding exceptional care topatients while remainingcommitted to groundbreakingresearch and academicallypreparing the next generation <strong>of</strong>caregivers and scientists.Since 1990, U.S. News &World Report has identified thenation’s elite medical centerswith its annual “America’s BestHospitals” edition. Themagazine produces rankings in16 specialties. In 12 <strong>of</strong> the 16specialties, the magazinefactored in reputation, mortalityindex, patient safety index andother elements, such as nursestaffing ratios and trauma centerdesignations. In the other fourspecialties the magazine went byreputation alone, determined bya nationwide survey <strong>of</strong>physicians.A P P O I N T M E N T SF O R 2 0 1 0 - 2 0 1 1The following individuals wereappointed to endowed positionsor to major leadership positionsat <strong>UT</strong> <strong>Southwestern</strong> during thepast fiscal year.■ Peggy Bailey, assistant vicepresident/accreditation andclinical support services forUniversity Hospitals.■ Dr. Bruce Beutler, director<strong>of</strong> the Center for the Genetics <strong>of</strong>Host Defense and to theRaymond and Ellen WillieDistinguished Chair in CancerResearch, in Honor <strong>of</strong> Laverneand Raymond Willie Sr.■ Dr. Ilya Bezprozvanny, tothe Carl J. and Hortense M.Thomsen Chair in Alzheimer’sDisease Research.■ John A. Brandecker, chiefoperating <strong>of</strong>ficer for UniversityHospitals.■ Dr. Elizabeth “Beth”Brickner, to the Charles B.Mullins, M.D., Pr<strong>of</strong>essorship inClinical Practice and Teachingin Cardiology.■ Dr. Brian Casey, to theGillette Pr<strong>of</strong>essorship inObstetrics and Gynecology.■ Dr. Zhijian “James” Chen,to the George L. MacGregorDistinguished Chair inBiomedical Science.■ Dr. Susan M. Cox, regionaldean – Austin programs.■ Dr. Ponciano Cruz, to thePaul R. Bergstresser, M.D., Chairin Dermatology.■ Dr. Byron Cryer, associatedean for faculty diversity anddevelopment.■ Dr. Jef De Brabander, to theJulie and Louis Beecherl Jr. Chairin Medical Science.■ Dr. Joel Elmquist, to theCarl H. Westcott DistinguishedChair in Medical Research.■ Lynn Fischer, associate vicepresident/cardiovascularservices, and surgical services forUniversity Hospitals.■ Dr. Abhimanyu Garg, tothe Distinguished Chair inHuman Nutrition Research.■ Dr. Elizabeth Goldsmith, tothe Patti Bell BrownPr<strong>of</strong>essorship in Biochemistry.■ Dr. Yu-Guang He, to theJosephine Long Biddle Chair inAge-Related MacularDegeneration Research.■ Dr. Lora Hooper, to the J.Wayne Streilein, M.D.,Pr<strong>of</strong>essorship in Immunology.■ Dr. Mustafa Husain, to theLydia Bryant Test DistinguishedPr<strong>of</strong>essorship in PsychiatricResearch.■ Dr. Michael Jessen,chairman <strong>of</strong> cardiovascular andthoracic surgery and to theFrank M. Ryburn Jr.Distinguished Chair inCardiothoracic Surgery andTransplantation.■ Rashard Johnson, assistantvice president/non-clinicalsupport services for UniversityHospitals.■ Dr. Ege Kavalali, to theRosewood Corporation Chair inBiomedical Science.■ Dr. Kemp Kernstine, to theRobert Tucker Hayes FoundationDistinguished Chair inCardiothoracic Surgery.■ Dr. George Lister, associatedean for education.■ Dr. James Malter, to theSenator Betty and Dr. AndyAndujar DistinguishedChairmanship <strong>of</strong> Pathology.■ Dr. David Mangelsdorf, tothe Raymond and Ellen WillieDistinguished Chair inMolecular Neuropharmacology,in Honor <strong>of</strong> Harold B.Crasilneck, Ph.D.■ Dr. Bradley F. Marple,assistant dean, graduate medicaleducation.■ Becky McCulley, associatevice president for clinicalprogram development.■ Mike Medina, associatevice president for UniversityHospitals clinical supportservices.■ Dr. Ronald Mitchell, to theWilliam Beckner, M.D.,Distinguished Chair inOtolaryngology.■ Dr. Sean Morrison, director<strong>of</strong> the Children’s ResearchInstitute at <strong>UT</strong> <strong>Southwestern</strong>and to the Mary McDermottCook Chair in PediatricGenetics.■ Dr. Shawna Nesbitt,associate dean <strong>of</strong> minoritystudent affairs.■ Dr. Jerry Niederkorn, to theRoyal C. Miller Chair in Age-Related Macular DegenerationResearch.■ Dr. Orhan Oz, to theWechun Pak Pr<strong>of</strong>essorship <strong>of</strong>Bone Biophysics.■ Dr. Amit Pandya, to the Dr.J.B. Shelmire Pr<strong>of</strong>essorship inDermatology.■ Donna Richardson,associate vice president andchief nursing <strong>of</strong>ficer forUniversity Hospitals.■ Dr. Claus Roehrborn, to theS.T. Harris Family Chair inMedical Science, in Honor <strong>of</strong>John D. McConnell, M.D.■ Dr. Peter Roland, to theBeth and Marvin C. (Cub)Culbertson Pr<strong>of</strong>essorship inPediatric Otolaryngology.■ Dr. Michael Roth, interimdean <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>Graduate School <strong>of</strong> BiomedicalSciences.■ Dr. David Russell, viceprovost and dean <strong>of</strong> basicresearch.■ Dr. Arthur Sagalowsky,master <strong>of</strong> Cary College.■ Michael Serber, vicepresident for financial affairs.■ Dr. Philip Shaul, to theAssociates First CapitalCorporation DistinguishedChair in Pediatrics.■ Dr. Stephen Skapek, to theChildren’s Cancer FundDistinguished Pr<strong>of</strong>essorship inPediatric Oncology Research.■ Dr. John Sweeney, to theTownsend Distinguished Chairin Research on Autism SpectrumDisorders.■ Dr. Dwain Thiele, seniorassociate dean for strategicdevelopment.■ Dr. Robert Toto, director <strong>of</strong>the Houston J. and Florence A.Doswell Center for theDevelopment <strong>of</strong> NewApproaches for the Treatment <strong>of</strong>Hypertension and associatedean, translational science.■ Dr. Kosaku Uyeda, to theBonnie Bell HardingPr<strong>of</strong>essorship in Biochemistry.■ Dr. James “Jim” Valentine,chairman <strong>of</strong> the Division <strong>of</strong>Vascular Surgery in theDepartment <strong>of</strong> Surgery.■ Dr. John Warner, assistantvice president for UniversityHospitals planning.■ Dr. George Wendel, to theNorman F. Gant Jr., M.D., Chairin Obstetrics and Gynecology.■ Dr. Michael White, to theGrant A. Dove Chair forResearch in Oncology.■ Dr. Charles Whitten, to theMargaret Milam McDermottDistinguished Chair inAnesthesiology and PainManagement.■ Dr. Charles Preston WilesJr., to the Drs. Anne and GeorgeRace Pr<strong>of</strong>essorship <strong>of</strong> StudentPsychiatry.■ Dr. DuWayne Willett, chiefmedical informatics <strong>of</strong>ficer,health system.■ Angela Wishon, vicepresident for researchadministration.■ Dr. Richard Wu, to theL. David Hillis, M.D.,Pr<strong>of</strong>essorship in ClinicalResearch in Cardiology.M A J O R G I F T SI N 2 0 1 0 - 2 0 1 1Philanthropists continued todemonstrate their commitmentto <strong>UT</strong> <strong>Southwestern</strong> in 2010-2011, providing support for avariety <strong>of</strong> research, clinical andeducational programs.Major new pledges and giftsreceived in the fiscal year 2010-2011 included:■ $13,413,530 from ananonymous donor to supportresearch and patient careprograms at <strong>UT</strong> <strong>Southwestern</strong>.■ $10,261,000 from Mrs.Eugene McDermott, including$10,161,000 to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital and $100,000 to<strong>UT</strong> <strong>Southwestern</strong> to furtherresearch on Fragile X Syndromeunder the direction <strong>of</strong> Dr.Kimberly Huber.■ $5,000,000 from ananonymous donor to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> Southwest -ern’s new University Hospital.■ $5,000,000 from Robertand Terry Rowling to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> Southwest -ern’s new University Hospital.■ $3,000,000 from theHarlan R. Crow family,Trammell S. Crow family andStuart M. Crow family tosupport the construction <strong>of</strong><strong>UT</strong> Southwest ern’s newUniversity Hospital.■ $2,000,000 from ananonymous donor to supportresearch into the causes,prevention and treatment <strong>of</strong>heart failure.■ $2,000,000 from theHoblitzelle Foundation to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> Southwest -ern’s new University Hospital.■ $1,617,984 from proceeds<strong>of</strong> the 2010 Sweetheart Ball to<strong>Southwestern</strong> MedicalFoundation in support <strong>of</strong> heartresearch at <strong>UT</strong> <strong>Southwestern</strong>.■ $1,233,000 from the DavidM. Crowley Foundation,including $1,000,000 to<strong>Southwestern</strong> Medical72S O U T H W E S T E R N M E D I C I N E 73
H I G H L I G H T SH I G H L I G H T SFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> Southwest -ern’s new University Hospitaland $233,000 to <strong>UT</strong> South -western to support research inthe areas <strong>of</strong> breast cancer, spinalcord injury, Parkinson’s disease,and peripheral nerve and painmanagement.■ $1,125,000 from Sam Y.Dorfman, Jr., M.D., and LouisDorfman, Sr., including$1,000,000 to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital and $125,000 to<strong>UT</strong> <strong>Southwestern</strong> to supportclinical research programs.■ $1,025,000 from the A.L.Chilton Foundation to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital, establish the Patti BellBrown Pr<strong>of</strong>essorship inBiochemistry, establish theBonnie Bell HardingPr<strong>of</strong>essorship in Biochemistry,provide five post-doctoralresearch fellowships inbiochemistry and continuesupport for the Chilton VisitingLectureship.■ $1,000,000 from ananonymous donor to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from theKenneth C. English FamilyFoundation to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from UteSchwarz and Rolf R. Haberechtto <strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from Sandi andRon W. Haddock to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from Nancy B.Hamon, through a bequest to<strong>Southwestern</strong> MedicalFoundation, to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from Linda W.and Mitch Hart to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from the HawnFoundation, Inc., to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from the HirschFamily Foundation to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from theEugene McDermott Foundationto <strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from OnceUpon a Time… to support theLow Birth Weight Clinic andprograms in pediatricneurodevelopment.■ $1,000,000 from the RalphB. Rogers Foundation to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from Mr. andMrs. Edward W. Rose III to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from William T.and Gay F. Solomon to<strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $1,000,000 from Jean andTom Walter to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $900,000 from The LupeMurchison Foundation tosupport Alzheimer’s diseaseresearch.■ $600,000 from the MaryKay Family Foundation andMary Kay, Inc., including$500,000 to <strong>Southwestern</strong>Medical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital and $100,000 to<strong>UT</strong> <strong>Southwestern</strong> to supportbreast cancer research.■ $515,392 from the Rose S.Van Wert Trust to <strong>Southwestern</strong>Medical Foundation to provideunrestricted support for<strong>UT</strong> <strong>Southwestern</strong>.■ $510,535 from the Mary R.Saner Charitable RemainderAnnuity Trust to support patientassistance programs at<strong>UT</strong> <strong>Southwestern</strong> UniversityHospital – St. Paul.■ $500,000 from ananonymous donor to<strong>Southwestern</strong> MedicalFoundation to provideunrestricted support for<strong>UT</strong> <strong>Southwestern</strong>.■ $500,000 from St. PaulMedical Foundation to supportthe construction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $425,000 from theHartwell Foundation to provideindividual and collaborativebiomedical research fellowshipsfor promising early-careerinvestigators at <strong>UT</strong> South -western.■ $417,925 from MaryFrances King, through a bequestto <strong>Southwestern</strong> MedicalFoundation, to advance cancerresearch at <strong>UT</strong> <strong>Southwestern</strong>.■ $400,000 from the DorisDuke Charitable Foundation to<strong>Southwestern</strong> MedicalFoundation to support the DorisDuke Clinical ResearchFellowship Program for MedicalStudents at <strong>UT</strong> <strong>Southwestern</strong>.■ $350,000 from ananonymous donor to supportmultiple sclerosis research underthe direction <strong>of</strong> Dr. ElliotFrohman.■ $344,000 from the NIWAInstitute for Pharmacology tosupport research <strong>of</strong> rheumaticdiseases under the direction <strong>of</strong>Dr. Joel D. Taurog.■ $300,000 from theNational Multiple SclerosisSociety to support the MultipleSclerosis Program and ClinicalCenter at <strong>UT</strong> <strong>Southwestern</strong>.■ $274,132 from Loyse J.Quinlan, through a bequest toSt. Paul Medical Foundation, insupport <strong>of</strong> clinical programs at<strong>UT</strong> <strong>Southwestern</strong> UniversityHospital – St. Paul.■ $250,000 from the WilliamDavidson Foundation to supportthe Jonathan W. Uhr, M.D.,Distinguished Chair inImmunology.■ $250,000 from Mrs. S. T.Harris to support a fund tohonor Kern Wildenthal, M.D.,Ph.D.■ $250,000 from Rollin W.King to <strong>Southwestern</strong> MedicalFoundation to support theconstruction <strong>of</strong> <strong>UT</strong> South -western’s new UniversityHospital.■ $250,000 from Dr. GerardNoteboom, through a bequest to<strong>Southwestern</strong> MedicalFoundation, to establish theElizabeth Haaland, M.D., andGerard Noteboom, M.D.,Endowed Medical ScientistTraining Program ScholarshipFund; the Elizabeth Haaland,M.D., Endowed Fund forClinical Care in Dermatology;the Gerard Noteboom, M.D.,Endowed Fund for Clinical Carein Pathology; and the GerardNoteboom, M.D., EndowedFund for Stem Cell Research.Generous contributions andpledges <strong>of</strong> $100,000 to $249,999were received from a number <strong>of</strong>additional donors, including thefollowing new commitmentsfrom:■ Mr. and Mrs. Edward M.Ackerman to <strong>Southwestern</strong>Medical Foundation to support avariety <strong>of</strong> programs at <strong>UT</strong> South -western.■ An anonymous donor tosupport <strong>UT</strong> <strong>Southwestern</strong>’sPatient Navigator Program, aswell as lung cancer research andpatient care programs in honor<strong>of</strong> Drs. Hak Choy, J. MichaelDiMaio, Jonathan E. Dowell andDavid A. Pistenmaa.■ The Kent & JoAnn FosterFamily Foundation to supportresearch aimed at definingbetter treatment <strong>of</strong> Type 1diabetes.■ Gayden Family Foundationto <strong>Southwestern</strong> MedicalFoundation to provideunrestricted support for<strong>UT</strong> <strong>Southwestern</strong>.■ Mr. and Mrs. Mark D.Gibson to <strong>Southwestern</strong> MedicalFoundation to provideunrestricted support for<strong>UT</strong> <strong>Southwestern</strong>.■ Felix B. and Josephine I.Goldman, through atestamentary gift to<strong>Southwestern</strong> MedicalFoundation, to supportscholarships for medicalstudents attending <strong>UT</strong> South -western Medical School.■ Harry and RosemaryHolcomb Living Trust to supportAlzheimer’s disease research.■ David M. Marshall,through a bequest, to supportprograms in medical research,education and clinical care.■ Catherine & JamesMcCormick Foundation toestablish the Catherine & JamesMcCormick CharitableFoundation Fund in Aging.■ Wm A & Elizabeth BMoncrief Foundation to supportactivities in <strong>UT</strong> <strong>Southwestern</strong>’sDepartment <strong>of</strong> Plastic Surgery.■ The Muscular DystrophyAssociation to support ALSresearch.■ The Ted Nash Long LifeFoundation to advanceAlzheimer’s disease research.■ The Charles Y.C. PakFoundation to support researchconducted by the NeillWalsdorf, Sr. BiotechnologyCenter in Mineral Metabolismand the Charles and Jane PakCenter for Mineral Metabolismand Clinical Research.■ Rudman Securities toprovide support for theJosephine Rudman Laboratoryfor Alzheimer’s DiseaseResearch.■ Dr. Donald C. Schenk to<strong>Southwestern</strong> MedicalFoundation to supporteducation, research and clinicalcare programs at <strong>UT</strong> South -western.■ The Tom ThumbFoundation to support clinicaltrials for the treatment <strong>of</strong> breastcancer.■ The West Endowment tosupport bone marrowtransplantation and follicularlymphoma research.■ Womack Machine SupplyCompany to support theactivities <strong>of</strong> <strong>UT</strong> <strong>Southwestern</strong>’sPatient and Guest Services.74S O U T H W E S T E R N M E D I C I N E 75