Overview of Pediatric Physical Assessment Overview of Pediatric ...
Overview of Pediatric Physical Assessment Overview of Pediatric ...
Overview of Pediatric Physical Assessment Overview of Pediatric ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
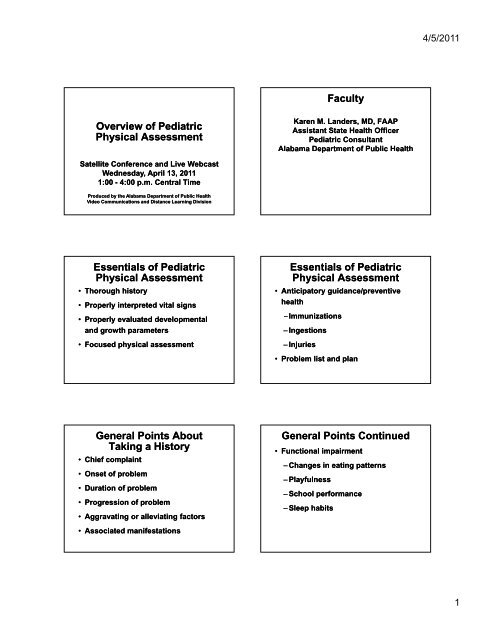
4/5/2011Faculty<strong>Overview</strong> <strong>of</strong> <strong>Pediatric</strong><strong>Physical</strong> <strong>Assessment</strong>Karen M. Landers, MD, FAAPAssistant State Health Officer<strong>Pediatric</strong> ConsultantAlabama a Department e t <strong>of</strong> Public HealthSatellite Conference and Live WebcastWednesday, April 13, 20111:00 - 4:00 p.m. Central TimeProduced by the Alabama Department <strong>of</strong> Public HealthVideo Communications and Distance Learning DivisionEssentials <strong>of</strong> <strong>Pediatric</strong><strong>Physical</strong> <strong>Assessment</strong>• Thorough history• Properly interpreted vital signs• Properly evaluated developmentaland growth parameters• Focused physical assessmentEssentials <strong>of</strong> <strong>Pediatric</strong><strong>Physical</strong> <strong>Assessment</strong>• Anticipatory guidance/preventivehealth– Immunizations– Ingestions– Injuries• Problem list and planGeneral Points AboutTaking a History• Chief complaint• Onset <strong>of</strong> problem• Duration <strong>of</strong> problem• Progression <strong>of</strong> problem• Aggravating or alleviating factors• Associated manifestationsGeneral Points Continued• Functional impairment– Changes in eating patterns– Playfulness– School performance– Sleep habits1
4/5/2011• Allergic historyGeneral Points• Medication history• Immunization history• Hospitalization and/or accidents• Birth history• Developmental milestones• Family history• Social historyGeneral Appearance <strong>of</strong>Infant or Child• Activity or movement• Facial features• Behavior when examiner enters room– Developmentally appropriate• Nutritional status• HygieneApproach to the<strong>Pediatric</strong> Patient• Age appropriate interaction– Gentle and engaging– Nonthreatening– Take the path <strong>of</strong> least resistance– Quiet and soothingApproach to the<strong>Pediatric</strong> Patient– Use observation liberally whiletaking the history– Always inform the patient <strong>of</strong> whatyou are about to do and never lieto the patient– Minimize the use <strong>of</strong> the exam tablein infants and younger childrenGrowth andDevelopment Parameters• Use current growth charts plottingBMI• Weigh appropriately– Dry diaper• Check height by placing infant onmeasuring table with head at the end<strong>of</strong> the board– Have older children take <strong>of</strong>f shoesGrowth andDevelopment Parameters• Measure head circumference up totwo years old placing measuring tapeabove eyebrows and measuringaround to occipital prominence2
4/5/2011Growth Parameters andAreas <strong>of</strong> Concern• Know normal weight gains for age• Usual expected height velocity forage• Family information specifically aboutparental stature• Consider children born in othercountriesGrowth Parameters andAreas <strong>of</strong> Concern• Be concerned about headcircumferences at extremes andheight/weight crossing percentilesDevelopmental <strong>Assessment</strong>for Age General Information• Use standardized developmentalscreening tools assessing grossmotor, fine motor, language,sensory, and social development• Be “open-ended” with questions• Use observation during the history t<strong>of</strong>ill-in developmental informationDevelopmental <strong>Assessment</strong>for Age General Information• Ask about hearing concerns evenwith newborns• Be alert to normal acquisition <strong>of</strong>language milestones• Screen at every well infant and childvisitMeasure Vital Signs andKnow How to Interpret AgeAppropriate Variations• Temperature– Can use tympanic thermometers toavoid invasive techniques such asrectal thermometers past thenewborn and early infant agesMeasure Vital Signs andKnow How to Interpret AgeAppropriate Variations• Pulse– Apical less than 2 years old/countfor one minute3
4/5/2011AgeHeart RateRange <strong>of</strong> RateBirth 70-1900-6 months 1306-12 months 1151-2 years 1102-6 years 80-1306-10 years 75-11510-14 years 70-11014 and above 65-100Focus Points for theNeonatal Examination• Fontanels• Skin color• Facies• Tone• Symmetry– Movement, respiratory effort,abdomen• ReflexesNeonatal Reflexes andWhen They Disappear• Stepping: 2 months• Moro: 3 months• Rooting: 3-4 months• Palmar grasp: 3-4 monthsNeonatal Reflexes andWhen They Disappear• Tonic neck: 4-6 months• Plantar grasp: 8-10• Sucking: 10-12 12 months• Babinski: 2 yearsSome Information on Weight• Newborns may lose up to 10% <strong>of</strong>their birth weight in the first 3-4 days• Newborns gain ½ to 1 ounce per dayafter that time• Excessive or poor weight gain needsto be addressedSome Information on Weight• Infants generally double their birthweight by 5 months and triple it byone year5
4/5/2011Be Alert forCongenital AnomaliesSome Specifics in Neonates• Anterior and posterior fontanels– Anterior closes between 12 - 18months– Posterior closes by 2-5 months• Red reflex• Sacral dimples• Mongolian spotsSacral DimpleMongolian SpotMongolianblue spotsCongenital NevusSystem by System<strong>Physical</strong> Examination• Integument• HEENT• Neck• Cardiovascular• Pulmonary6
4/5/2011System by System<strong>Physical</strong> Examination• Gastrointestinal• Genitourinary• Musculoskeletal• Neurologic• Inflammatory• Viral• Bacterial• Congenital• Allergic• OtherIntegumentaryGeneral Principles <strong>of</strong>Examination <strong>of</strong> the Skin• Color– Pallor– Jaundice• Normal after 24 hours innewborn up to 7-10 days butabnormal afterwards– Variations in skin pigmentationGeneral Principles <strong>of</strong>Examination <strong>of</strong> the Skin• Texture, turgor• Rashes• Lesions• Hair and nailsSome DescriptiveTerms <strong>of</strong> Rashes• Macular• Papular• Blanch with pressure• Excoriated• Hemorrhagic• Blistering• CysticSome DescriptiveTerms <strong>of</strong> Lesions• Hives or wheals• Scaling7
4/5/2011Some DescriptiveTerms <strong>of</strong> Lesions• Crusting/scab forming• Scars• Other– Congenital, neoplasticCandidiasisChicken PoxHerpes SimplexEczemaHemangioma8
4/5/2011MiliaUrticariaImpetigoContact DermatitisRingwormScabies9
4/5/2011SeborrheaCafé au LaitLymph Nodes• Small, nontender, English pea size,s<strong>of</strong>t, and freely moveable lymphnodes are common primarily in thecervical regionEnlarged Lymph Node• Check cervical, axillary, inguinalregion for lymph nodesHead and Neck• Check for symmetry, head control ininfants, posture to one side (anindicator <strong>of</strong> torticollis), range <strong>of</strong>motion• Feel the anterior and posteriorfontanels• Older infantHead and Neck– Flexion, extension, rigidity– Thyroid enlargement, branchialcleft cysts10
4/5/2011Eyes• Check for shape and symmetry• Note the color <strong>of</strong> the conjunctiva• Evaluate extra ocular movements• Check pupillary reflexes• Fundiscopic for red reflex• Appropriate vision testing in theclinical settingStrabismusConjunctivitisReflex PathologyEars• Evaluate shape, position• View internal structures• Newborn hearing screening andongoing assessment <strong>of</strong> hearingincluding language developmentNormal and AbnormalTympanic Membrane11
4/5/2011Nose• Structure, position• Evidence <strong>of</strong> grunting or flaring• Color <strong>of</strong> any drainage, foul odor,color <strong>of</strong> mucosa, location <strong>of</strong> septumThroat• Color <strong>of</strong> lips, presence <strong>of</strong> fissures• Teeth– Number and condition• Gums– Color and condition• Tongue– Midline, color, graphic patternsThroat• Integrity <strong>of</strong> palate and location <strong>of</strong>uvulaEnlarged Tonsils• Tonsillar sizeGeographic TongueChest and Back• Inspect size, shape, symmetry alongwith movement• Note any distress including use <strong>of</strong>accessory muscles• Note symmetry <strong>of</strong> nipples and anybreast development• Check for spinal curvature12
4/5/2011Pectus ExcavatumPectus ExcavatumDepressionin sternumNormal heart positionPectus ExcavatumPectus CarinatumDepression pushesheart to the sideHeart• Palpate over the valvular areas• Determine the PMI• Rate– Higher than adults• Rhythm noting that infants andchildren will have variation withrespiration• MurmursHeart– Systolic murmurs can be normal– Diastolic murmurs are alwaysabnormal• S1 and S213
4/5/2011Murmurs• Classic description– Grade I-VI– Descriptive terms• Crescendo, decrescendo, harsh,blowing, s<strong>of</strong>t• AuscultationLungs– Do not confuse upper airwaysounds with lung sounds– Equal breath sounds– Rales, ronchi, wheezingAbdomen• Inspect the shapeUmbilical Hernia• Auscult for bowel sounds– Normal should be heard every10 - 30 seconds• Palpate for masses, tenderness• MalesGenitaliaGenitalia– Location <strong>of</strong> urethral meatus– Presence or absence <strong>of</strong>circumcision– Penis– Tanner staging– Anal structure– Testes• Descended, undescended, orretractile14
4/5/2011AHerniasBHypospadiusGlanularSubcoronalAnterior(50%)Anterior(50%)CDEDistalpenileMidshaftProximalpenileMiddle(30%)Middle(30%)PenoscrotalScrotalPosterior(20%)Posterior(20%)Perineal• FemalesGenitalia– Labia majora and minora notingany labial fusion in young infantsor young girls– Urethral orificeGenitalia– Vaginal orifice along with anyevidence <strong>of</strong> imperforate hymen orother abnormalities– Tanner stage– AnusNormal and Abnormal HymensExtremities• Range <strong>of</strong> motion with specificconcerns for hip movement in infants• Femoral pulses• Joint warmth, stability, swelling,tenderness, clubbing <strong>of</strong> fingers• Gait• Genu valgum or varum15
4/5/2011Evaluation <strong>of</strong> Hip Mobilityin InfantsGenu VarumGenu ValgumNeurologic <strong>Assessment</strong> for Age• Considerable information can begained by watching the child duringthe history gathering portion <strong>of</strong> theexam• Reflexes-biceps, triceps, patellar,achillesNeurologic <strong>Assessment</strong> for Age• Assess cranial nerves• For older infants and children,cerebellar functionSources for Photographsand Images• Photographic images obtained forthis presentation are used withpermission and solely for medicaleducational purposes16
4/5/2011Sources for Photographsand Images• Sources– www.rainbowpediatrics.net– www.slideworld.orgorg– Kinsburg, K., M.D.17