Journal Spring 2013.pdf - Spinal Research Foundation
Journal Spring 2013.pdf - Spinal Research Foundation
Journal Spring 2013.pdf - Spinal Research Foundation
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
JOURNAL OF THESPINALRESEARCHFOUNDATIONNew Horizons in Spine TreatmentVolume 8, Number 1SPRING 2013
SPINAL RESEARCH FOUNDATIONTHE JOURNAL OF THE SPINAL RESEARCH FOUNDATIONA multidisciplinary journal for patients and spine specialistsBrian R. Subach, M.D., F.A.C.S.Editor-in-ChiefMarcus M. Martin, Ph.D. and Anne G. Copay, Ph.D.Managing EditorsCarrie B. CalifanoAssociate EditorMelissa B. Luke, Marcia A. Phillips and Nancy J. GoldbransonEditorial StaffSPINAL RESEARCH FOUNDATION (SRF)BOARD OF DIRECTORSGuy E. BeattyChairmanMichael H. HowlandSecretaryBrian D. NaultMemberPaul J. Slosar, Jr., M.D.MemberThomas C. Schuler, M.D., F.A.C.S.PresidentAndrew T. GreeneTreasurerWilliam H. Evers, Jr., Ph.D.MemberBrian R. Subach, M.D., F.A.C.S.Director of <strong>Research</strong>Raymond F. PugsleyNational Race LiaisonKevin M. Burke, Jr.MemberNajeeb M. Thomas, M.D.MemberTHE JOURNAL OF THE SPINAL RESEARCH FOUNDATIONEDITORIAL BOARDJames P. Burke, M.D., Ph.D.Altoona, PAJ. Kenneth Burkus, M.D.Columbus, GAChristopher H. Comey, M.D.<strong>Spring</strong>field, MAAleksandar Curcin, M.D., M.B.A.Coos Bay, ORGeorge A. Frey, M.D.Englewood, COGerard J. Girasole, M.D.Trumbull, CTMatthew F. Gornet, M.D.Chesterfield, MORobert J. Hacker, M.D. &Andrea Halliday, M.D.<strong>Spring</strong>field, ORRegis W. Haid, Jr., M.D.Atlanta, GALarry T. Khoo, M.D.Los Angeles, CANoshir A. Langrana, Ph.D.Piscataway, NJMark R. McLaughlin, M.D., F.A.C.S.Langhorne, PAPatrick T. O’Leary, M.D.Peoria, ILDavid P. Rouben, M.D.Louisville, KYRick C. Sasso, M.D.Indianapolis, INThomas C. Schuler, M.D., F.A.C.S.Reston, VAJames D. Schwender, M.D.Minneapolis, MNNirav K. Shah, M.D., F.A.C.SLanghorne, PAPaul J. Slosar, Jr., M.D.Daly City, CANajeeb M. Thomas, M.D.Metairie, LAJim A. Youssef, M.D. &Douglas G. Orndorff, M.D.Durango, CO<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPINAL RESEARCH FOUNDATIONFrom the EditorBrian R. Subach, M.D., F.A.C.S.Iam excited to present to you this <strong>Journal</strong> of the<strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> which focuses on newhorizons in spinal surgery. In shaping this issue, webrought together experts from various fields to presenttheir thoughts and ideas about the future of spinalhealth care and to comment on the techniques that areshaping the future of spinal surgery.In referring to new horizons, I believe that thereare three aspects of spinal surgery which will continueto evolve. The first is the use of minimally invasivetechniques. Such approaches to decompression andfusion of the spine have made significant improvementssecondary to advances in imaging technology.Computer systems which combine CT scan, MRI data,or x-ray into three-dimensional images increase theaccuracy of identifying the critical structures, makingthe procedures both safer and less uncomfortable forthe patient. One such example is the Mazor robotictechnology. This computer platform allows CT scanimages to be mapped to the patient’s x-rays while thatpatient is on the table. This gives unparalleled accuracyand precision in identifying critical structures andplacing hardware in sensitive areas of the spine.The second advance which deserves comment isthe advent of motion-preservation approaches. Typicallyfor degenerative conditions, arthrodesis, or fusionprocedures, have been performed to stabilize segmentswhich were painful or unstable. Now using arthroplasty,or artificial disc techniques, there are real and provenalternatives to fusion technology. Although only FDAapproved for single-level cervical and single-levellumbar disease, surgeons across the globe have beenpushing the envelope and performing multiple arthroplastyprocedures in the same patient. In some cases,a hybrid technique using both arthrodesis and arthroplasty(fusion and motion preservation) in the same patientseems to work optimally.The third and final area which represents a newhorizon has to do with regenerative strategies for thespine. As we are all well aware, the aging processcauses discs to deteriorate, cartilage to wear away,and bone spurs to form. This progressive wear andtear is unavoidable as one ages. Many times, basedupon body weight or choice of exercise regimen,these degenerative changes can be accelerated. It ispossible to utilize injection therapy to stabilize unstableligaments. In a technique known as prolotherapy,using either salt water or sugar water to causean inflammatory response, ligaments will actuallyscar, tighten, and stabilize. Additionally, research isbeing done using bone marrow aspirate, autologousfat grafting, and cartilage-forming stem cells. Thesematerials can be taken from the patient and injecteddirectly into a degenerating disc. The hope is that theaging process, which causes the loss of the vital cellularelements of the disc, will reverse. By populatinga disc with new cellular elements, it is possibleto turn back the clock of aging and avoid an opensurgical procedure.I would also like to draw your attention to the upcoming<strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>’s, “We’ve GotYour Back” Race for <strong>Spinal</strong> Health, to be held May18, 2013 in Reston, Virginia. The website at www.SpineRF.org has a listing of all of the race sites anddates around the country.Finally, I would like to call special attention toour <strong>Spinal</strong> Hero, Dr. Thomas Schuler. Dr. Schuler isan expert in the non-operative and operative care ofspinal disorders who takes excellent care of his patients,but he is also an advocate for spinal health care,both on a national and local level. It is heroes likeDr. Schuler who make a difference in patients’ livesevery day.1 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013From the PresidentThomas C. Schuler, M.D., F.A.C.S.Monopolies in Health Care are Limiting Patients’ Options<strong>Spinal</strong> health care has advanced immensely, especiallyin the past twenty years. Through advancementsin knowledge and technology, we are able tohelp heal people rapidly with minimal down time andmaximum restoration of their normal activity levels.This is all accomplished through improved diagnosticsand therapeutic agents, improvements in surgery (bothopen and minimally invasive), and improved rehabilitation.We have disc arthroplasties, motion preservingdevices, biologics to accelerate fusions, improved spinalinstrumentation, minimally invasive surgery, andmore. This is all exciting and great news. The problemis that an individual American’s access to theselife-changing interventions is diminishing becauseof changes in health care reimbursements. Insurancecompanies are searching for ways to deny treatmentsin order to save their dollars and improve their profits.The government is doing the same. The problem isthat we are on a rapid course to a single-payer system,in function if not in form. There has been extreme consolidationin the health care market, and the public isnot aware of it.When I founded The Virginia Spine Institute overtwenty years ago, there were greater than twenty insurancecompanies willing to offer up to thirty differenttypes of insurance policies for the employees of myorganization. In 2012, while we were negotiating ourinsurance renewal, there were only four companies,each offering a maximum of three different policies.This consolidation has been fueled by market forces,as well as legislation.Wall Street and government policy led to thehousing crash of 2007. Wall Street created significant,bad investments by combining toxic assets with reasonableassets. Once the housing bubble burst, WallStreet could no longer make money in that sector.Since that time, Wall Street has moved on to othersectors to pillage. One significant focus in the pastfive years has been the health care sector. During thistime, a significant increase in mergers and acquisitionshas occurred amongst hospitals, insurance companies,and various provider organizations. The resultof these monopolies is a decrease in the number ofoptions available for consumers. As the number of insuranceproviders dwindles, it is easier for the remaininginsurers to deny coverage for a service for whichthey, unilaterally, choose to not pay. This problem isexacerbated by the fact that the government and theseprivate insurers are cross-sharing their denial information,all leading to decreased access to life-improvinginterventions. This is what we have been living withat an accelerating rate during 2012, and it will onlygreatly worsen over the next several years as the newhealth legislation is further implemented, resulting inone large monopoly.The difficulty in surgical fields is to meet whatsome of these rationing forces interpret as scientificproof that a treatment works. The insurance companieshave hired for-profit companies to create policiesto determine which care will be reimbursed. Thesehired guns are requiring human experimentation tovalidate surgical procedures, thereby enabling insurersto use unobtainable standards to create policieswhich deny care.It is very difficult in surgical procedures to effectivelyand ethically perform randomized, blinded trials.Herein lies the catch-22 that exists in modern healthcare. Although we know with great certainty and greatoutcomes data that certain procedures work, insurancecompanies and the government choose to disregardthis data since they claim it has not been validated in arandomized, blinded prospective fashion. In addition,if any corporate funding has been involved in the research,which meets their arbitrary requirements, thenany data that meets these strict criteria is disregardedbecause, again, it is unilaterally viewed as biased. Theproblem only worsens because, where is the fundingfor these costly research projects supposed to comeSPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 2
SPINAL RESEARCH FOUNDATIONfrom, if not from the companies invested in sellingtheir advances?Denial of service is the easiest cost-saving maneuverfor insurers and the government. Failure to provideaccess to appropriate interventions, surgeries, and therapieswill greatly decrease the quality of life for millionsof Americans, as well as prevent their ability tobe gainfully employed and be active members of theirfamilies and society. It is critical as we move forwardthat we continue to understand the miracles of modernmedicine that are possible when competent spinal specialistsare allowed to perform their technical abilitiesas determined by their educated assessments of eachindividual’s situation. <strong>Spinal</strong> surgery is the most complexarea of health care, and there is great variability inthe individualized treatment that is required to resolveeach person’s specific pathology, anatomy, and socialsituation. No prospective, randomized studies will giveus the answer to all of the situations or even to mostof the situations in spinal health care. Large outcomestudies can show us trends and ideas, but individualdecisions will need to be made. Because of the rapidconsolidation of the health care market, we will end upwith one government insurer, through CMS, coveringthe government insured and one to three private insurerscovering the rest of the country. Decision making willbecome centralized, thus removing it from the hands ofthe physicians and patients. Bureaucrats and “professorsof evidence-based medicine” will dictate standard careor one-size-fits-all care. This will cause loss of access tocare for Americans who require these life-changing and,more specifically, life-improving interventions.We must restore the sanity of evidence-basedmedicine (comparative effectiveness) back to the trueintent: that a physician integrates individual clinicalexpertise with the best available external clinical evidencefrom systematic research to determine what isin the best interest of an individual patient.3 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Neck and Back Pain Affects MillionsThe <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> is anon-profitorganization dedicated to improvingspinal health care through research,education, and patient advocacy. Located inReston, Virginia, the <strong>Foundation</strong> collaborateswith spinal research partners acrossthe country to prove the success of traditionalapproaches, as well as develop newtechniques and technologies. These resultsare shared with both the medical professionand the general public to improve the overallquality and understanding of optimal spinalhealth care.The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> has made remarkable progress inscientific research associated with neck and back pain. The <strong>Foundation</strong>collects data relative to patients’ treatments and outcomes and hasembarked on projects designed to better understand the biochemistryof neuropathic pain and develop new drug and surgical regimens toaddress it. The <strong>Foundation</strong> continues to expand its research efforts,partnering with other research institutions to further the advancementof spine related research. The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>has been involved in numerous studies:• The use of novel perioperative drug therapy to improvesurgical outcomes.• The evaluation of medical devices for relief of back pain.More than 85% of the population will sufferfrom severe neck and/or low back painduring their lifetime. Eight percent of thesepeople develop chronic pain, which meansthat at any given time, around 25 million peoplein the United States are directly affectedby this condition and many more indirectly.Techniques to cure, manage, and preventthis limiting and disabling condition need tobe developed. Educating the public, healthcare providers, and insurance providers isthe firststep in advancing spinal health care.You can help!The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> isAmerica’s leading non-profit healthorganization dedicated to spinal health.Friends like you have made it possiblefor us to make huge strides andgroundbreaking research discoveries.Join us in our mission to improve spinalhealth care. Support cutting edgeresearch by making a donation to the<strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>.• The evaluation of analgesic drug regimens.• The development of non-operative techniques to resolvedisabling neck and back pain.• Investigating the use of BMP (Bone MorphogeneticProtein) in minimally invasive spinal surgery to minimizepost-operative pain and dysfunction.• The development of cervical and lumbar discreplacement technologies.• The development of disc regeneration technologythrough the use of stem cells derived from bone marrow.• The investigation of lactic acid polymers to preventfibroblast in-growth in surgical wounds.• A nation-wide multi-center prospective spinetreatment outcomes study.Support Cutting-edge <strong>Research</strong>• Visit www.SpineRF.org to make a secure online donation.• Call (703)766-5404 to make a donation over the phone.• The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> is a non-profit 501(c)(3)organization. Donations are tax deductible.Stay Informed• Visit our website often to keep up-to-date on the <strong>Foundation</strong>’sactivities and research breakthroughs.www.SpineRF.orgSPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 4
SPINAL RESEARCH FOUNDATIONOverviewMarcus M. Martin, Ph.D. and Anne G. Copay, Ph.D.1WHO The burden of musculoskeletal conditions at the start of the newmillennium. World Health Organ Tech Rep Ser. 2003;919:1–218.Every day, scientists make advancements that bringus closer to overcoming the diseases which plaguehumanity. Through research efforts in academia and inphilanthropic and private enterprises, we are steadilymoving closer to a time when many of the diseaseswhich now afflict mankind will be mere fodder for ourhistorical archives.<strong>Spinal</strong> disease affects millions in the United Statesand across the globe. Consequences range from milddiscomfort to extreme pain and physical disability. Thelifetime incidence of spinal pain has been reported to be80% to 85% of all adults. 1 Around the world, researchersand spinal care practitioners are relentlessly workingto develop new treatments for spinal ailments. The currentissue of the <strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>aims to highlight some of these advances andupcoming developments in the field of spinal diseasetreatment. We have tapped into the experts from variousspecializations to provide the reader with an update onsome of the major advances in the field of spinal care.Robotic technology is expanding in scope and applicability.This technology is rapidly and dramaticallyrevolutionizing modern life. It is now also being utilizedin spinal surgery. The Mazor robot, for example,is a guidance system for surgeons performing spinalprocedures. Its precise mapping of human anatomyenables it to act as a surgeon’s extra sense during surgicalprocedures. Dr. Good, a spine surgeon who utilizesrobotic technology, provides an expert overviewof the workings of the device.The use of biologics to enhance spine treatment ishighlighted in an article by Dr. Coric. He explains theutility of cell therapy in the treatment of degenerativedisc disease, a condition that affects all aging humans.For many who have been confined to wheelchairs,regaining the ability to walk upright has longbeen considered an implausible dream. However, thisdream is now becoming a reality through technologicaladvances. The ReWalk system does just that. In aninformative article about this system, Dr. Esquenaziexplains how this walking assistance device has literallychanged the lives of those crippled as a result ofspinal cord injury.Advances in the realm of conservative spinal therapyare reflected in both physical therapy and painmanagement. Dr. Nguyen provides an overview ofcurrent pain management approaches, while JessicaStepien, DPT, presents a review of dry needling, atherapeutic approach that is rapidly gaining popularityas a means of treating myofascial trigger points.The sacroiliac (SI) joint is considered by manytherapists as an under-recognized pain generator. Dysfunctionof this joint is often addressed by immobilizationthrough joint fusion. The traditional approach to SIfusion requires a large incision and the use of musclesplittingtechniques. New approaches to SI joint fusionand their significant benefits, compared to the traditionalapproach, are highlighted by Dr. Hasz.The article ‘Advances in Bone Grafts and FusionAugmentation’ examines an assortment of bone growthadjuvants. It covers the use of specifically engineeredanchor proteins (P-15) to induce cell anchoring and boneformation. This relatively new product is explained andcontrasted to the traditional bone morphogenetic proteinswhich are also designed to enhance bone fusion.Harnessing the fundamental principles of physics,the 4WEB technology combines stronger structuralsupport with more space for bone ingrowth and osteoinductivesurfacing to create a revolutionary newapproach to interbody spinal cages. The material andthe structural characteristics of this novel approach tospinal implants are underscored by Dr. Gainey in hisinformative review.The current issue highlights advances in minimallyinvasive approaches to surgery which allow for smallerincisions, less tissue injury, shorter hospital stays, andoften faster recovery times. In an insightful article byDr. Orndorff et al., readers are exposed to the processand benefits of minimally invasive spine surgery.5 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013The future of spinal therapy is bright. The advancesoutlined in this issue give emphasis to some of themajor frontiers in the field of spinal research. As youread this current issue, know that, at this very moment,thousands of scientists and physicians and millions ofsupport staff are working tirelessly toward the goal offreeing patients from the debilitating condition that isspinal disease.Marcus M. Martin, Ph.D.Dr. Martin’s research interests includeneuroimmunology, virology, and immunology.He is engaged in collaborativeresearch through The <strong>Spinal</strong> <strong>Research</strong><strong>Foundation</strong> with the Medical Universityof South Carolina Children’s Hospital,geared toward the development ofneuro protective and neuroregenerativecompounds for the treatment of nerve pathology. Dr. Martin’scurrent research collaborations include research initiatives toapply stem cell therapy for tissue preservation, the developmentof regenerative therapies for intervertebral discs, andthe development of novel methods of enhancing bone fusion.Anne G. Copay, Ph.D.Dr. Copay studies the outcomes of surgicaland non-surgical spine treatments. Shepublished several articles on the outcomesof spine fusion. She has ongoing researchprojects concerning the effectiveness ofnew spine technologies and the long-termoutcomes of surgical treatments.Past Issues of the<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>The Crisis of OsteoporosisFall 2008The Genetics of <strong>Spinal</strong> Disease<strong>Spring</strong> 2009Obesity and <strong>Spinal</strong> DiseaseFall 2009The Evolution of <strong>Spinal</strong> Health Care<strong>Spring</strong> 2010The Success of <strong>Spinal</strong> Health CareFall 2010Spine Support:Muscles, Tendons, and Ligaments<strong>Spring</strong> 2011Trauma and Tumors of the SpineFall 2011Spines of Service<strong>Spring</strong> 2012Spines in Motion: Biomechanics of the SpineFall 2012Please follow this link to access previous journal issues:http://www.spinerf.org/education/journal.phpSPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 6
SPINAL RESEARCH FOUNDATIONAsk the ExpertJonathan R. Slotkin, M.D.How are stem cells used inspine treatment?There are three sources of stem cells: from the patient(autologous), from cadavers (allograft), and from livingdonors (allograft). Without doubt, the most successfulstem cell product is cadaveric derived stemcells within a bone matrix. Seven years ago, the firstcadaveric-based stem cell products came to market.Given that no adverse events have been reportedso far, these allograft-based stem cell products areincreasingly considered to be safe and reliable sourcesof growth factors.Stem cells may be used to promote bone formationand, hence, improve the fusion of bones in thespine. Stem cells may also be used to generate newcells inside an intervertebral disc and allow us to heala degenerated disc. Autologous and allograft biologicstrategies are increasingly attractive avenuesof innovation. Between 30–40% of all spine andneurosurgeons are now incorporating stem cell treatmentsin their practice.What are the benefits ofminimally invasive spine surgeryversus traditional approachesto spine surgery?The term “minimally invasive” has been used in a lessthan genuine manner. Some procedures are called minimallyinvasive because they are performed through asmaller incision. However, these procedures may stillbe very invasive if they involve cutting through musclesand removing bone.In a traditional approach, the removal of a discherniation relies on cutting through muscles andremoving pieces of bones to access the disc. In a trulyminimally invasive surgery, it is now possible to avoidmuscle dissection and bone removal. A small nanoprobe is inserted through the skin with an incision assmall as a freckle. This incision does not require anystitches and is covered by a Band-Aid after the surgery.The probe is guided between the vertebrae tothe herniated disc. Nano tools are then used throughthe hollow center of the probe. The nano tools can beused to remove disc fragments and small bone spurs.A traditional surgery cuts through skin, muscles, andbones; this creates scar tissue and potentially lingeringpain. It also requires longer recovery time and longerhospital stay. A truly minimally invasive surgeryavoids damage to surrounding tissue and decreasesthe recovery time.Do you foresee thedevelopment of apreventative treatment forspinal degeneration?The new frontier in biologics involves both trying toregenerate the disc and preventing degenerative discdisease. Currently, numerous companies and basicscience labs are working on these issues. Many thingsare being tried, including growth factors, differentgenes, and injecting stem cells into the disc. Thereare on-going studies where OP-1 (BMP-7) is injectedinto the degenerated disc. I think that the OP-1 growthfactor injection is probably not going to be the finaltreatment. It is a great first step, but growth factorswon’t survive long enough inside the disc to continueto prevent disc arthritis; repeated injections would beneeded. The environment in the disc itself is harsh.The pH level is low and there is no blood supply, sothe injected cells are short-lived. This harsh environmentmakes it hard to grow new cells and regeneratethe disc. As degeneration progresses, the biomechan-7 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013ics of the disc change, the disc space collapses, andthere is more instability. Once we identify the propergrowth factor, we may be able to inject the gene forthe growth factor in the disc. Theoretically, the genefor the growth factor will remain active for a longerperiod of time inside the disc. It is widely believedthat in the future, success will mean a combinationof the right genes, growth factors, and stem cells, andeven using biomechanical devices for later stages ofdisc degeneration when the disc biomechanics arealtered.Have you used robotics inyour treatment? How hasthis enhanced your surgicalpractice?Yes, I started to use robotics for my more complexsurgeries. It allows me to both plan and execute thecomplex surgery cases with more precision. The robot3D software creates a blueprint of the procedure thatI intend to perform. This blueprint is specific to thepatient’s anatomy and condition.In the operating room, I use the guidance of therobot, that is, the robot guides my tools according tothe blueprint to place the implants safely and accuratelyin the exact pre-planned locations. The averageaccuracy of implant placement by spine surgeons isabout 90%. With the help of the robot, the accuracyincreases to 98.3%. While in surgery, I also rely onthe robot to check the position of the pedicle screwsthat I implant. The robot creates a 3D axial view of thespine showing the exact location of each pedicle screwand its relationship to the spinal canal. I can immediatelyevaluate the positions of the screws and, if needbe, correct them. This takes no more than five to tenminutes of additional OR time. Without the robot,surgeons have to wait for a post-operative CT scan toverify the placement of the screws. Significant misplacementsof the instrumentation would have to berevised with a second surgery.Jonathan R. Slotkin, M.D.Jonathan Slotkin, MD is director of spinalsurgery at Geisinger NeuroscienceInstitute and the director of spinal cordinjury research. He has clinical interestsin brain tumor surgery and complexspinal surgery, including degenerativeconditions, spinal oncology, spine trauma,surgical back pain, adult deformity, minimally invasiveapproaches, and artificial disc replacement technologies. Healso has an interest in sports-related spine and neurologicalinjuries. Dr. Slotkin is an active researcher and is currently focusingon spinal cord injuries, neural regeneration, and nanotechnology.He has been published in peer-reviewed publicationsand co-edited a two volume publication on spine surgery.Dr. Slotkin is also a member of the scientific advisory board ofIn Vivo Therapeutics Corporation.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8
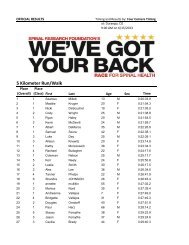
SPINAL RESEARCH FOUNDATION“We’ve Got Your Back” Race for <strong>Spinal</strong> HealthLaura A. Bologna, <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> National Program CoordinatorSan Francisco, CASeptember 15, 2012San Francisco’s famous fog burned off in time tokick off the third annual “We’ve Got Your Back”Race for <strong>Spinal</strong> Health at scenic Lake Merced.As this event continues to grow, wewelcomed more participants, more volunteers,and most excitingly, more <strong>Spinal</strong>Champions at this year’s event. Almost200 participants, 30 volunteers, and manyfriends and family were in attendance torun, walk, and provide support.The Daly City Police SWAT teammade a big impression on the event, returningafter their participation in lastyear’s race to support their colleagueMike P. The presence of the officialSWAT truck was an exciting addition tothe event.Dr. Paul Slosar gave a heartfelt thanksto all of the patients who were able toparticipate in the run or the walk and acknowledgedour generous sponsors.The host for this event was theSpineCare Medical Group, whose staff made up thecore group of volunteers. Thanks again to all of ournational sponsors and local donors for their generosity,which ensured the success of this 3rd annual event.And a very special thanks to Dr. Slosar and his wifewho make this entire event possible.9 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Orleans, LAJanuary 6, 2013The first annual New Orleans “We’ve Got Your Back”Race for <strong>Spinal</strong> Health was held this past January. Theinaugural event was a great success and attracted overtwo hundred New Orleans area residents who bravedthe pouring rain to support this event. Our goal was toto increase community awareness about the devastatingeffects of back and/or neck pain and to get peopleinvolved in our efforts to battle its effects. This wasthe first event of its kind in New Orleans.Dr. Thomas addressed the crowd and got them excitedto take part in this event. He spoke of the importanceof research and development in spinal surgery,emphasizing how each attendee’s support allows forprogress to be made every day.SPRING 2013 VOL. 8 No. 1The event’s primary purpose was to celebrate theachievements of patients who have overcome debilitatingback or neck pain to regain their lives and sharetheir successes with the community. We celebratedseveral <strong>Spinal</strong> Champions and their successes at thisevent.The host for this event was Southern Brain andSpine. Thanks again to all our national and local sponsorsfor their generosity, and to our race volunteersfor their willingness to be involved in our first event.A special thanks to Denise Crawford and MichelleJacob for making this event a success.Upcoming RacesWe are excited to announce seven upcoming racesin 2013. Five of these races are being hosted by newlocations this year as our event continues to grow andgain national presence. The upcoming races are: 1stannual race in Freehold, New Jersey, hosted by PrincetonBrain and Spine Care on April 6th; 1st annual racein Carmel, Indiana, hosted by Indiana Spine Group onApril 27th; 1st annual race in Coos Bay, OR, hostedby South Coast Orthopaedic and Bay Area Hospitalon May 4th; 6th annual race at our flagship race sitein Reston, VA, hosted by The Virginia Spine Instituteon May 18th; 1st annual race in Durango, CO hostedby Spine Colorado on June 15th; 3rd annual race inSan Francisco, CA on September 14th; and 1st annualrace in Peoria, IL hosted by Midwest Orthopaedicin October. Show your support and join us at one ofour upcoming events. For registration and volunteeropportunities, please visit www.spineRF.org/race.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 10
SPINAL RESEARCH FOUNDATIONSpine TaleSilvana MasoodBrian R. Subach, M.D., F.A.C.S.On initial evaluation, Silvana had tremendous lowback pain and tenderness overlying multiple jointsof her lumbar spine. There was muscle spasm andnumbness in her entire right leg. She was prescribedphysical therapy and anti-inflammatory medicationsfor the pain and numbness while considering her optionsfor her lumbar degenerative disc disease. TheMRI scan that she had in 2008 demonstrated one discshowing signs of moderate degeneration without anycompression of the sciatic nerves. She continued tomaintain her core strength and took anti-inflammatories,dealing with the pain fairly well until she had herdaughter. Both the pregnancy and the child care significantlyworsened her pain. She found that not onlyher life, but also her career and her family were beingaffected by the pain. In discussions with her husband,she decided to undergo spinal fusion. An updatedMRI scan demonstrated worsening of the disease atL5/S1, with progressive loss of height and bone spurformation. She had clearly done everything possibleto avoid surgery.Silvana Masood had known about spinal diseasefor years having watched her husband go throughphysical therapy, spinal injections, and pain medicationswith little benefit. When he eventually underwentspinal fusion surgery with excellent results, shebecame a believer.Silvana first came to The Virginia Spine Institutein 2008. She was experiencing disabling low back painwith both pain and numbness in her entire right leg.The pain had been bothering her intermittently for thepast ten years, but she had never really sought medicalattention until years later when her pain progressivelyworsened.Figure 1. Lateral view of the pre-operative MRI: the red arrow indicatesa herniated disc at the L5-S1 level.11 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 2. Lateral view of the pre-operative x-ray: the arrowidentifies the L5/S1 disc with loss of disc height and bone spurformation.In April 2012, she underwent anterior lumbar interbodyfusion at L5/S1. Two large LT cages wereplaced through a small abdominal incision into herL5/S1 disc space. (Figure 3) Those cages restored theheight and posture of the disc space and gave it immediatestability. There had been such collapse at the discspace that the cages wedged firmly in place, obviatingthe need for any further surgery. (Figure 2)At her follow-up visit two weeks after surgery, herpain level was down to a two (on a scale from oneto ten), and she had noticed an immediate difference.Figure 3. Lateral view of the post-operative x-ray shows restoreddisc height and posture at L5/S1 following a minimally invasiveanterior lumbar interbody fusion using two LT cages.She felt that her spine was stronger, her leg symptomshad resolved, and she was ready to begin physicaltherapy.Silvana is presented as a Spine Tale in this issue ofthe <strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> becauseshe had lived with degenerative lumbar disc diseasefor a decade. When things finally worsened despitenonoperative care, she decided to do something aboutit. With a minimally invasive intervention, instead ofbeing disabled by pain, she now has her career, herlife, and her family back.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 12
SPINAL RESEARCH FOUNDATIONSpine TaleDaisy CherBrian R. Subach, M.D., F.A.C.S.Figure 1. Lateral view of the pre-operativex-ray: the arrow points to the collapse of theC7 screws into the vertebral body of C7 (belowthe prior fusion) causing a kyphotic posture andspondylolisthesis of C7 on T1.Daisy Cher is a 43-year-old woman with a historyof neck pain and right upper extremity weakness.She had previously been operated on in 2011, undergoinganterior cervical fusion from C4 through C7.Her x-rays from February 2011 demonstrated excellentposture, alignment, and healing; however, repeatx-rays done in August 2012 demonstrated evidenceof subsidence or collapse of the C7 screws into thevertebral body, causing a kyphotic (leaning forward)posture. She had also developed spondylolisthesis, orforward slippage, of bone C7 on bone T1. Her EMGstudy done in September 2012 demonstrated an acuteC7 radiculopathy (ongoing nerve damage).Daisy was suffering from severe pain as well asprogressive weakness in her upperextremities. Subsequent x-raysdemonstrated evidence of kyphosisand progression of collapse atC7. Daisy returned to the operatingroom for a combined anterior andposterior reconstruction of her cervicalspine. (Figure 1)The primary goal of the reconstructionwas to bring her postureback to normal. Her posture wasforward flexed, causing her tohunch or lean forward. By enteringthe front of the spine first, it waspossible to remove the previousplate and to redo the anterior cervicalfusion, restoring her postureto normal. Given the kyphosis, orforward flexed posture, which wasoccurring at the junction of the cervicaland thoracic spine, she needed a posterior decompressionand fusion extending from the cervicalspine through the upper thoracic spine.She underwent the revision anterior cervical fusionin October 2012. The previously placed plate wasremoved, as well as most of the fractured C7 bone, andthen additional fusion was performed at both the C6/7and C7/T1 disc spaces. A new anterior cervical platewas placed in Daisy’s neck with excellent posture andalignment. (Figure 1)The day following the surgery, she underwent afine-cut CT scan to evaluate her alignment as well asthe room available for the spinal cord. That CT scanand the Mazor robot were used to plan and perform theposterior screw fixation from C3 through T3. The robotictechnology enhanced the surgeon’s accuracy andprecision as well as the safety of the operation. Daisyunderwent an uncomplicated second stage operation,placing Vertex lateral mass screws in the upper cervicalspine and Solera screws into the upper thoracicspine. The use of Vertex technology in combinationwith Solera, as well as robotic guidance, represents atrue new horizon in spinal surgery.Figure 2. Lateral view of the post-operativex-ray: revised fusion from C4 through C7 andadditional fusion at C6/C7 and C7/T1.13 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Spine TaleSean O’NeilBrian R. Subach, M.D., F.A.C.S.Sean O’Neil isa 52-year-oldtennis professionalwho initiallypresented tohis neurologist in2011 complainingof numbness inboth of his hands.He felt that hewas losing somegrip strength andslowly but progressivelyworsening. According to his neurologist,he had a normal neurologic examination of both arms,including strength and reflexes. This was followed byan EMG study (nerve test) of his arms, which onlyshowed mild carpal tunnel syndrome in both hands.When he arrived at The Virginia Spine Institute in December2012, he was still complaining of numbnessin both hands. He felt that there was no obvious positionalcomponent, but that the numbness was worseif he used his hands. He noted decreased fine motorcontrol, but he was still active in his profession.The x-rays of Sean’s cervical spine demonstratedevidence of mild degenerative changes involving thediscs. There were some bone spurs that were formingacross the front of the spine, consistent with someonein his early 50s. However, the reflexes in both hisarms and legs were extremely hyperactive or jumpy.He had a positive Hoffmann’s sign in his thumb andevidence of clonus in both ankles, both consistentwith someone who has pressure on his cervical spinalcord.An urgent MRI scan of the cervical spine was ordered.The radiologist called from the MRI scanner tocomment about the severity of Sean’s disease. Seanessentially had three discs which were bulging and hadsignificant arthritic changes, but more importantly, hisspinal cord was being compressed to approximatelyhalf of its normal diameter. There was some signalchange seen within the cord itself, indicative of swellingor bruising of the spinal cord.The most common operation carried out for cervicaldegenerative disease and bone spur formation isan anterior cervical fusion. In the setting of an eliteathlete, such a cervical fusion can irreparably alter hisability to use his neck, meaning he would lose significantrange of motion in flexion, extension, and lateralbending. Such motions are generally necessaryfor a tennis professional. A second option, much lessfrequently performed, is a cervical laminoplasty. Theoperation essentially cuts the bone in the back of theneck and then repositions it so the spinal cord is nolonger compressed. It does not change the arthriticdisease in the spine, meaning it will not alter his rangeof motion, nor would it alter any pain that he mayhave from the arthritis. Sean considered his optionsand chose to undergo a posterior cervical laminoplastyprocedure designed to give his spinal cord thenormal amount of room.On January 7, 2013 he underwent the laminoplastyprocedure in which small titanium plates were placedin the back of his neck, securing the cut bone to theadjacent spine. This was not a fusion operation, butrather a surgery designed to give him the room necessaryfor his spinal cord to avoid further injury and alsostabilize his spine using its own intrinsic ligamentsand muscular support. (Figure 2)When Sean returned approximately two weeksafter surgery, he was complaining of soreness in theback of the neck. However, his range of motion wasexcellent. He stated that he had already noticed improvementin the numbness in his hands. He still hascarpal tunnel syndrome which will become obviouswith repetitive use of his hands; however, his spinalstenosis has been completely cured.Although his hyperreflexia will remain, furthersurgery may not be necessary. By doing the laminoplastyprocedure, his range of motion was spared andSean is able to maintain the high level of function necessaryin his sport.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 14
SPINAL RESEARCH FOUNDATIONFigure 1. Lateral view of the pre-operative x-ray.Figure 2. Lateral view of the post-operative x-ray shows the smalltitanium plates placed in Sean’s neck during the laminoplastyprocedure.Brian R. Subach, M.D., F.A.C.S.Dr. Subach is a spine surgeon and thePresident of The Virginia Spine Institute.He is a nationally recognized expert in thetreatment of spinal disorders and an activemember of the American Associationof Neurological Surgery, the Congressof Neurological Surgeons, and the NorthAmerican Spine Society. He is an invited member of the internationalLumbar Spine Study Group and a Fellow in the AmericanCollege of Surgeons. He lectures extensively regarding themanagement of complex spinal disorders in both national andinternational forums. He is the Director of <strong>Research</strong> and BoardMember for the non-profit <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> (SRF)and Editor-in-Chief of the <strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>(JSRF). He has written 15 book chapters and more than50 published articles regarding treatment of the spine.15 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Robot-Guided Spine SurgeryChristopher R. Good, M.D., F.A.C.S. and Blair K. Snyder, P.A.-C.The goals of modern spinal surgery are to maximizepatient function and accelerate a return to a fulllife. As spinal surgery has evolved, more focus hasbeen placed on minimizing trauma to the body duringsurgery and expediting a return to function through theuse of minimally invasive techniques. The era of modernspinal surgery has blossomed over the past 15 to20 years as a result of scientific advancements includingminimally invasive surgery, genetic testing, nextgeneration spinal implants, stem cell research, and theuse of biologic agents to promote spinal healing.Robot-guided spinal surgery offers many potentialadvantages to patients and surgeons including improvingthe safety of both minimally invasive and complexsurgical procedures, improving the accuracy of spinalinstrumentation placement, and minimizing the use ofradiation during surgery. Robot-guided spine surgeryutilizes highly accurate, state-of-the-art technology forthe treatment of many spinal conditions including degenerativespinal conditions, spine tumors, and spinaldeformities.Figure 1. CT scan images of the spine are taken prior to surgery, and the exact location ofspinal implants is blueprinted with 3D software. The orange and purple lines represent screwsthat are to be placed into the bones of the spine.Figure 2. The Mazor Robot is attached to the spine of the patient.The robot arm helps guide the surgeon’s hand during a minimallyinvasive surgery. Image courtesy of Mazor Robotics.How It WorksThe Mazor Robotics’ Renaissance system is one ofthe only robotic guidance products in the UnitedStates used for implanting devices during spine surgery.The Mazor Robotics system allows the surgeonto use the images from a computerized tomographyscan (CT scan) that is taken before surgery to createa blueprint for each surgical case. The CT scan informationis loaded into a computerized 3D planningsystem which allows the surgeon to plan the surgicalprocedure with a high degree of precision before everentering the operating room (Figure 1).In the operating room, the surgeondoes all of the physical work ofthe surgery. The robot-guidance systemis a tool that helps to guide thesurgeon’s instruments based on thehighly accurate pre-operative planningof spinal implant placement.During the surgery, the robot is placednear the patient either by attaching itto the bed or directly anchoring it tothe spine of the patient. The robot isapproximately the size of a 12 oz.beverage can with a small arm attached.The robot has the ability tobend and rotate in order to place itsarm on the spine in a very specific locationand trajectory (Figure 2). Thisultra-precise guidance can improveSPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 16
SPINAL RESEARCH FOUNDATIONC.R. Good and B.K. Snyder/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 16–21the surgeon’s ability to safely place implants, particularlywhen working through very small incisions (minimallyinvasive surgery) or when dealing with complexanatomy (spinal deformity or previous spine surgery).Minimally Invasive Spine FusionOne common technique presently used by spine surgeonsto correct spinal conditions is spine fusion. The purposeof a spinal fusion is to create a rigid union betweentwo separate segments of the spine to correct malalignmentor instability. Spine fusion has traditionally beenperformed using “open surgery” with an incision thatis big enough to expose the entire area being treated.Open surgical techniques are beneficial and necessaryfor many conditions; however, in some cases minimallyinvasive surgery (MIS) can be utilized to safely obtain asimilar result. MIS uses smaller incisions which usuallyresult in less damage to surrounding healthy tissue, lesspost-operative pain, and faster recovery.In many situations, MIS requires an increase in theuse of intraoperative x-rays in order to compensate fora surgeon’s inability to directly visualize the spine. Insome cases, this lack of visualization could decreasethe surgeon’s accuracy when compared to open surgery.In addition, the increased radiation exposure duringsurgery is a concern for the patient as well as thehealth care team, as previous studies have shown anincreased rate of cancer among spine surgeons, comparedto the general population. 1Robot-guided surgery technology allows the surgeonto perform MIS in a very precise fashion whileminimizing the need for radiation during the surgicalprocedure. Robot-guidance technology guides the surgeon’stools during MIS to ensure accuracy while alsodecreasing tissue trauma, resulting in less bleeding,smaller scars, less pain, and faster recovery (Figure 3).A recent study reviewed 635 surgeries involvingthe placement of 3,271 spinal implants and found aFigure 3. X-rays of a patient before and after minimally invasive correction of spondylolisthesis of the lumbar spine. Progressive disc collapseand slippage of the bone (red arrow) has been corrected using minimally invasive techniques. Using robot-guidance, the screws wereplaced in the back through an incision one inch in length.17 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 4. Left: x-ray of patient with thoracolumbar scoliosis. Center: pre-operative blueprint showing the location where screws will be placedduring scoliosis correction surgery. Right: final location of the implants after surgical correction.98.3% accuracy rate for implants placed with robotguidance.In this study, 49% were defined as minimallyinvasive surgeries. Neurologic issues werenoted in 4 cases, but following revision surgery, nopermanent nerve damage was encountered. The studyreported an improvement in accuracy of instrumentationplacement and lower risk for neurologic issuescompared to previous studies. 2 Robot-guidance hasbeen directly compared to open surgical techniques,and in one retrospective study demonstrated an improvementin implant accuracy by 70%, reduction inradiation dose by 56%, and decrease in hospital stayby 27%. 3SPRING 2013 VOL. 8 No. 1Scoliosis Correction SurgeryScoliosis is an abnormal curvature of the spine thataffects approximately seven million people in the UnitedStates. Adolescent idiopathic scoliosis is most commonlydiagnosed between the ages of 10 to 12 years oldand may be discovered by parents, during school screenings,or at pediatric visits. When scoliosis is suspected,patients are referred to orthopedic scoliosis specialistswho evaluate the patient to determine the severity of thepatient’s curvature. Symptoms of scoliosis may includeback pain, uneven shoulders or hips, abnormal gait,breathing issues, and neurologic problems.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 18
SPINAL RESEARCH FOUNDATIONC.R. Good and B.K. Snyder/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 16–21Treatment options for idiopathic scoliosis includeobservation, bracing, and surgery. In general, bracingis recommended for curves between 25–30 degrees inpatients with significant growth remaining, and correctivesurgery is generally reserved for progressivescoliosis curves greater than 45° or curves that do notrespond to bracing treatment. The goals of scoliosiscorrection surgery are to amend the spinal curvatureand to prevent the curve from progressing further duringthe patient’s life (Figures 4 and 5).Surgery for scoliosis involves the use of spinal instrumentationsuch as screws, rods, hooks, and wireswhich are placed along the spine. Surgery treats butdoes not cure scoliosis; it corrects the abnormal curvatureand prevents further progression of the disease.Surgical treatment of scoliosis requires a high degreeof planning and precision. Each specific curve patternis unique, and many patients with scoliosis haveatypically shaped vertebrae, making the surgery morechallenging.Robot-guided scoliosis correction offers increasedprecision of instrumentation placement and therefore,an increase in the safety of the surgical procedure. Itoffers the surgeon the ability to carefully plan aheadbefore entering the operating room and design theideal procedure for each patient. Studies have validatedsuperior clinical results for adolescent scoliosisreconstruction with robotic technology based on improvedaccuracy of implant placement and safety. Ina recent study of 120 teenagers with scoliosis, robotguidedsurgery was found to achieve 99.7% accuracyof 1,815 implants placed. 3VertebroplastyVertebroplasty is an outpatient procedure commonlyperformed for the treatment of osteoporotic compres-Figure 5. Left: x-ray of patient with large thoracic and lumbar scoliosis which is affecting heart and lung function. Center: pre-operative blueprint,showing the location where screws will be placed during scoliosis correction surgery. Right: final location of the implants after surgicalcorrection.19 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentsion fractures. During the procedure, synthetic bonecement is injected into a broken spine vertebra througha needle. This cement hardens a few minutes afterit is injected which stabilizes the fractured vertebra,thereby decreasing pain and the potential for the boneto break further. (Figure 6)Vertebroplasty requires a high level of precisionbecause a needle is guided through the vertebra nearthe spinal cord or nerves. Additionally, the accuracyof the needle location is important to prevent the bonecement from flowing into the area around the nervesin the spine. Robot-guidance allows the surgeon to positionthe needle precisely to minimize the risks surroundingvertebroplasty procedures. In a recent studyof osteoporotic compression fractures, robot-guidancewas shown to yield improved accuracy over traditionalmethods, which reduced the total time needed for theprocedure and in some cases, allowed the procedure tobe performed on patient’s who would not have beenable to be treated conventionally. 4 The use of the robothas also been reported to decrease radiation exposureto the patient and operating room staff by 50–70% invertebroplasty procedures 5 (Figure 7).Spine BiopsiesIn some cases, it is necessary to obtain a small piece oftissue from the spine in order to perform microscopicstudies to understand a patient’s disease or make a specificdiagnosis. This is particularly true in cases of spinaltumors when it is imperative to determine if a lesionis benign, malignant, or infected. Biopsies are usuallytaken with a needle through a small incision withoutdirect surgeon visualization of the tumor. In many cases,surgeons use CT or x-ray images to guide the needle intothe correct location. This process involved additionalradiation and in some cases, it can be difficult to findthe right spot for the biopsy. Robot-guidance allows thesurgeon to pinpoint the exact location the biopsy is tobe performed and can decrease the time needed for theprocedure and the duration of radiation (Figure 8).ConclusionRobot-guided spine surgery is a promising new technologythat has many advantages and may allow sur-SPRING 2013 VOL. 8 No. 1Figure 6. Example of a balloon Kyphoplasty. Image courtesy ofMedtronic.Figure 7. X-ray taken during vertebroplasty with robot-guidance.The compressed bone has been accessed by a needle (red arrow)and filled with synthetic bone cement for stabilization.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 20
SPINAL RESEARCH FOUNDATIONC.R. Good and B.K. Snyder/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 16–214. Silberstein B, Bruskin, A, Alexandrovskii, V. Robot guidedsurgery in treatment of osteoporotic fractures. Presented at:European Federation of National Associations of Orthopaedicsand Traumatology (EFORT) 2011 Annual Congress; June 1–4,2011:abs 1097.5. Kaplan, et al. Robotic assisted vertebral cement augmentation: amajor radiation reduction tool. Aging Spine Symposium, March2011. Jerusalem, Israel.Christopher R. Good, M.D.,F.A.C.S.Figure 8. Pre-operative blueprint showing the trajectory of biopsyneedle accessing a lesion in the bone.geons to perform less invasive surgical procedureswith smaller incisions, less bleeding, faster recovery,and shorter hospital stays. Robot-guidance also canincrease the accuracy and safety of surgical proceduresand allow these procedures to be performed withless intra-operative radiation exposure to patients andhealth care providers.Dr. Good is a spine surgeon and Directorof <strong>Research</strong> at The Virginia SpineInstitute. He has extensive training andexperience in the treatment of complexspinal disorders with special expertise innon-operative and operative treatmentof adult and pediatric spinal deformitiesincluding scoliosis, kyphosis, flatback, and spondylolisthesis.Dr. Good has co-authored numerous articles and has beeninvited to lecture nationally and internationally at the Scoliosis<strong>Research</strong> Society, the International Meeting on Advanced<strong>Spinal</strong> Techniques, the American Academy of OrthopaedicSurgeons, and the North American Spine Society.Blair K. Snyder, P.A.-C.References1. Singer G. Occupational radiation exposure to the surgeon. J AmAcad Orthop Surg. 2005;13(1):69–76.2. Devito DP, Kaplan L, Dietl R, et al. Clinical acceptance andaccuracy assessment of spinal implants guided with SpineAssistsurgical robot: retrospective study. Spine (Phila Pa 1976). 2010;35(24):2109–2115.3. Kantelhardt SR, Martinez R, Baerwinkel S, et al. Perioperativecourse and accuracy of screw positioning in conventional, openrobotic-guided and percutaneous robotic-guided, pedicle screwplacement. Eur Spine J. 2011;20(6):860–868.Blair is a physician assistant at TheVirginia Spine Institute. She obtaineda Bachelor of Science in Physician AssistantStudies from Long Island University-Brooklyn,NY and a Bachelor ofScience in Biology from Loyola College,MD. Her residency and fellowship focusedspecifically on medical and surgicalmanagement of spinal disorders, and she holds licensesfrom both the Virginia and Maryland Boards of Medicine.21 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Cell Therapy in Intervertebral Disc RepairDomagoj Coric, M.D.Low back pain (LBP) is a common condition affectingtens of millions of Americans yearly. Fortunately,the vast majority of LBP cases respond wellto non-surgical management. A small, but still sizablepercentage of patients are plagued by recurring, severediscogenic LBP triggered by simple activities such assitting, standing, or walking. These patients are notoriouslydifficult to diagnose, as well as treat, and canbecome debilitated by their symptoms. Ultimately, asignificant number of these patients turn to chronic,long-acting narcotic therapy, repeated invasive procedures,such as epidural steroid injections or facetrhizotomy, and major surgical procedures, such as fusionor total disc replacement. 4,6,8 (Figure 1)The intervertebral disc is a fibro-cartilaginousstructure that consists of two parts: (1) an outer annulusfibrosus which consists of fibroblast cells and typeI collagen, and provides tensile strength and (2) an innernucleus pulposus with disc or chondrocytic cellsand type II collagen which resists compressive forces.Therefore, the predominant native disc cell type is acartilage-like disc cell that produces extracellularmatrix (ECM). ECM consists primarily of proteoglycans,such as aggrecan and versican. These proteoglycansare hydrophilic molecules consisting of proteinstems surrounded by highly negatively chargedglycosaminoglycan (GAG) side chains. The two mostabundant GAGs in ECM are chondroitin sulfate andkeratin sulfate which serve to attract and hold waterLumbarspineNeedleFacet jointNerveFigure 1. Facet rhizotomy: heat is conducted through a needleto destroy the medial nerve branches of the spine in order to interruptthe pain signal transmission. Image courtesy of Twin CitiesPain Clinic.molecules. Degenerative disc disease (DDD) compromisesthe native disc cell’s ability to produce andmaintain ECM. The subsequent loss of proteoglycansand GAG side chains causes disc desiccation and lossof disc height with increased mechanical loads on surroundingvertebral bodies. These increased stressesultimately manifest themselves radiographically asannular tears, endplate sclerosis (or Modic changes),and disc dehydration (or ‘black disc disease’). Thesestructural changes to the disc can be manifested clinicallyas mechanical LBP. In this somewhat simplifiedview, DDD and mechanical LBP can be viewed as theresult of the disc cell’s inability to produce and maintainECM. 4,6 (Figure 2)Surgery for patients with chronic, severe LBP isgenerally viewed as a treatment of last recourse andhas traditionally involved removal of the majority ofthe intervertebral disc followed by instrumented fusionof the adjacent vertebral bodies. Currently, themost common fusion techniques involve instrumentedinterbody fusion via various approaches, such as anterior(ALIF), posterior (PLIF or TLIF), or lateral(LLIF) approaches. Minimally invasive techniquesmay decrease operative morbidity, but still involveloss of segmental motion and increased adjacent levelstresses. Total disc replacement (TDR) was developedto maintain motion, but still represents a majorsurgical procedure with removal of the majority of thedisc, including the annulus and nucleus. 6,8 (Figure 3)Recently, novel technologies have focused on lessinvasive procedures seeking to maintain or enhancethe structure and function of the disc. These disc repairprocedures can be broadly categorized as: (A)nucleus augmentation and (B) nucleus repair. Thereare currently no FDA-approved devices/drugs fordisc repair, but there has been extensive preclinicaland some clinical research into these areas. Nucleusrepair involves introducing biologically active materialinto the disc to replenish cells or increase productionof ECM. Nucleus augmentation involvesadding a synthetic or biologic material to the disc.Nucor, an injectable silk/elastic polymer, and BiostatBiologix, an injectable form of fibrin sealant, are examplesof nucleus augmentation that have been studiedclinically. 3,5,6,15SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 22
SPINAL RESEARCH FOUNDATIOND. Coric/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 22–25Figure 2. T1 & T2 MRI showing Modic changes. (A&B) Type 1 modicchanges: the endplates are black in T1 and white in T2 (edema).(C&D) Type 2 modic changes: the endplates are white in both T1and T2 (fat). (E&F) Type 3 modic changes: the endplates are blackin both T1 and T2 (sclerotic). Images A and B courtesy of MedicalHypotheses, retrieved from Albert, H.B., et al. Modic changes, possiblecauses and relation to low back pain. Medical Hypotheses2008; 70(2):361–368.Nucleus repair procedures can be subdivided intothree categories: (1) growth factor therapy, (2) genetherapy and (3) cellular therapy. 6,7 Growth factors aresmall peptide cytokines with cell regulatory functionthat can increase the existing disc cell’s ECM production.Bone morphogenetic proteins (BMPs) are exam-ples of growth factors,and BMP-7 (OP-1)and BMP-14 (GDF-5)have been used inclinical trials. 7,10 Genetherapy involves thetransfer of geneticmaterial to enhancethe disc cell’s nativeproduction of ECM.Gene therapy requiresvectors, either viral ornonviral, to transfergenetic material intohost cells. There havebeen no clinical trialsFigure 3. Lateral x-ray of a two levelanterior lumbar interbody fusion.of gene therapy for disc repair to date. 16 Tissue engineeredcell therapy actually introduces new cells intothe disc to produce more ECM. Cellular therapy fordisc repair has focused on chondrocyte and stem cellreplacement therapy. 6,13 (Figure 4)Some anatomic factors favorably predispose thedisc to cellular therapy. The nucleus is contained bythe annulus and has a limited blood supply, limitingcell migration and providing a relatively immunologicallyprivileged environment. 13,14 There has been extensivebasic research and animal studies investigatingnucleus repair, but there have been few clinicalstudies. 1,2,9 Both Yoshikawa et al. (2010), 17 two patients,and Orozco et al. (2011), 12 ten patients, publishedsmall series on patients with LBP treated withexpanded iliac crest derived mesenchymal stem cells.Meisel and associates (2006) reported on 12 patientswho underwent discectomy with harvest of autologousdisc chondrocytes which were subsequently expandedin culture and re-injected into the disc space aftertwelve weeks (Eurodisc Study). 11 The preliminary resultswere promising with post-discectomy patientstreated with autologous chondrocytes showing greaterpain reduction at two year follow-up. 6,11Clinical study into these disc repair procedureshave been classified by the FDA as InvestigationalNew Drug (IND) studies, as opposed to the InvestigationalDevice Exemption (IDE) studies of spinaldevice implants. Recently, two different IND studies23 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 4. Proposed mechanism for cell therapy using mesenchymal stem cells (MSC) to preserveintervertebral discs. Image courtesy of Arthritis <strong>Research</strong> and Therapy, retrieved fromMiyamoto, T., et al., Intradiscal transplantation of synovial mesenchymal stem cells preventsintervertebral disc degeneration through suppression of matrix metalloproteinase-related genesin nucleus pulposus cells in rabbits. Arthritis & <strong>Research</strong> Therapy 2010;12(6):R206.have completed enrollment evaluating chondrocyteand stem cell procedures for disc repair, respectively:(1) 15 patients were treated prospectively at two siteswith NuQu juvenile cartilage cells in ‘An Open LabelI/II Pilot Study to Evaluate the Treatment of DegenerativeLumbar Discs with Allogenic CulturedChondrocytes’ and (2) 100 patients were enrolled in aprospective, randomized study comparing Mesoblaststem cells to placebo in ‘A Prospective, Multicenter,Double-Blind, Controlled Study Evaluating Safetyand Preliminary Efficacy of a Single Injection of AdultAllogeneic Mesenchymal Precursor Cells Combinedwith Hyaluronan in Subjects with Chronic DiscogenicLumbar Back Pain.’ A second multicenter trial utilizingNuQu juvenile chondrocyte cells is currently activelyenrolling: ‘A Phase II, Randomized, Double Blind,Placebo Controlled Study Evaluating the Treatment ofDegenerative Lumbar Discs with Allogeneic CulturedChondrocytes.’ The research department at CarolinaNeurosurgery and Spine Associates (CNSA) has beeninvolved in all three studies, serving as the lead investigativesite for both the NuQu studies. 6 (Figure 5)Both NuQu (allogeneic juvenilechondrocyte cells) and Mesoblast(allogeneic mesenchymal stemcells) are investigational cellulartherapies that involve harvest of cadavericcells that are subsequentlyexpanded in cell culture and frozen.Prior to use, the cells are thawedand combined with a carrier (commercialfibrinogen and thrombin,for the chondrocyte cells, and hyaluronicacid, for the stem cells).Finally, 5–10 million viable cells/cc are injected into the center of thedisc space under fluoroscopic guidanceduring an outpatient procedureusing 22-gauge needle. Generally,1–2cc are injected into the disc overa period of 5–45 seconds. 6The results of the Phase I NuQustudy have been published. 6 Fifteenpatients (6 female, 9 male)were treated at 2 investigationalsites with a single delivery of NuQu juvenile chondrocytes(levels: L3-4 = 2, L4-5 = 1, L5-S1 = 12, Pfirrmanngrade III = 12; grade IV = 3). Mean age was40 years (range 19–47). Fourteen of the 15 patientsFigure 5. Examples of cell therapy using cadaveric chondrocytes asan allograft for regenerative intervertebral disc cell therapy and cartilagetissue transplant. Image courtesy of ISTO Technologies, Inc.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 24
SPINAL RESEARCH FOUNDATIOND. Coric/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 22–25(93%) completed a minimum of 1 year follow-up. Thepre-procedure morbidity of this patient population isreflected by the relatively high baseline disability (ODI= 53.3) and pain (NRS = 5.7) scores comparable to thebaseline disability and pain scores of patients in theCharite and ProDisc-L IDE surgical trials. The clinicalresults showed statistically significant improvementsfrom baseline on all clinical scales (ODI-disabilityscale, NRS-pain scale, and SF-36). The majority ofradiographic parameters were unchanged; however,there was improvement in 10 of 13 patients imaged at6 months and 8 of 13 patients imaged at 12 months.Improvements were primarily seen in posterior annulartears. Safety was also demonstrated; no patients experiencedneurological deterioration, there were no discinfections, and there were no serious and unexpectedadverse events. Lab studies indicated that there was noimmunological response to the chondrocyte treatment. 6Biologic disc repair represents a minimally invasiveand motion-preserving treatment to address LBP dueto early lumbar DDD. Early results have been promising,but remain preliminary. Further investigation withprospective, randomized, blinded, placebo-controlledstudy design is necessary, warranted, and ongoing.References1. Acosta FL, Metz L, Adkisson HD, Liu J, Liebenberg EC, MillimanC, et al. Porcine Intervertebral disc repair using allogeneicjuvenile articular chondrocytes or mesenchymal stem cells. TissEng Part 2011;A17:3045–3055.2. Adkisson HD, Milliman C, Zhang X, Mauch K, Maziarz RT,Streeter PR. Immune evasion by neocartilage-derived chondrocytes:implications for biologic repair of joint articular cartilage.Stem Cell Res 2010;4:57–68.3. Berlemann U, Schwarzenbach. An injectable nucleus replacementas an adjunct to microdiscectomy: 2 year follow-up in apilot clinical study. Eur Spine J 2009;18:1706–1712.4. Chou R, Qaseem A, Snow V, Casey D, Cross T, Shekelle P, et al.Diagnosis and treatment of low back pain: a joint clinical practiceguideline from the American College of Physicians and theAmerican Pain Society. Ann Int Med 2007;147:478–491.5. Coric D and Mummanemi PV. Nucleus replacement technologies.J Neurosurg-Spine 2008;8:115–120.6. Coric D, Pettine K, Sumich A, Boltes MO. Prospective Study ofDisc Repair with NuQu ® Injectable Allogeneic Chondrocytes.J Neurosurg-Spine 2013;18:36–42.7. Evans C. Potential biologic therapies for the intervertebral disc.JBJS-A 2006;88:95–98.8. Fritzell P, Hagg O,Wessberg P, Nordwell A. 2001 Volvo AwardWinner in Clinical Studies: lumbar fusion versus nonsurgicaltreatment for chronic low back pain: a multicenter randomizedcontrolled trial from the Swedish Lumbar Spine Study Group.Spine 2001;26:2521–2532.9. Kim AJ, Adkisson HD, Wendland M, Seyedin M, Berven S,Lotz JC. Juvenile chondrocytes may facilitate disc repair. OpenTiss Engin Regen Med J 2010;3:18–27.10. Masuda K, Imai Y, Okuma M, Muehleman C, Nakagawa K,Akeda K, et al. Osteogenic protein-1 injection into a degenerateddisc induces the restoration of disc height and structuralchanges in the rabbit annular puncture model. Spine 2006;31:743–754.11. Meisel H, Sioldla V, Ganey T, Minkus Y, Hutton W, Alasevic.Clinical experience in cell-based therapeutics: disc chondrocytetransplantation a treatment for degenerated or damaged intervertebraldisc. Bio Eng 2007;24:5–21.12. Orozco L, Soler R, Morera C, Alberca M, Sanchez A, Garcia-Sancho J. Intervertebral disc repair by autologous mesenchymalbone marrow cells: a pilot study. Transplant 2011;92:822–828.13. Sakai D: Future perspectives of cell-based therapy for intervertebraldisc disease. Eur Spine J 2008;17(S):S452–S458.14. Urban JP, Smith S, Fairbank JC: Nutrition of the intervertebraldisc. Spine 2004;29:2700.15. Yin W, Pauza K, Olan W, Doerzbacher J. Long-term outcomesfrom a prospective, multicenter investigational device exemption(IDE) pilot study of intradiscal fibrin sealant for the treatmentof discogenic pain. Pain Medicine 2009;10:488–493.16. Yoon ST. Commentary. A promising gene therapy approach totreat disc degeneration. Spine J 2012;12:21.17. Yoshikawa T, Ueda Y, Miyazaki K, Koizumi M, Takakura Y.Disc regeneration therapy using marrow mesenchymal celltransplantation: a report of two cases. Spine 2010;35:E475–80.Domagoj Coric, M.D.Dr. Coric practices neurosurgery atCarolina Neurosurgery and Spine Associatesin Charlotte, North Carolina. Hegraduated with an MD from Wake ForestUniversity. He did his residency andinternship at Wake Forest UniversityBaptist Medical Center. He is affiliatedat the Carolinas Medical Center as Chief of Neurosurgery. Heserves on the Scientific Committee of Joint Section on Disordersof the Spine & Peripheral Nerves of the AANS and CNS,Executive Council of the Southern Neurosurgical Society andpast-President of North Carolina Spine Society. Dr. Coric isBoard Certified in Neurosurgery. His expertise and specialinterests are Artificial Disc Replacement, <strong>Spinal</strong> Trauma and<strong>Spinal</strong> Cord Injuries, <strong>Spinal</strong> Tumors, Degenerative Diseasesof the Spine and Minimally Invasive Surgery.25 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Bipedal Locomotion Option for Individuals withThoracic Level Motor Complete <strong>Spinal</strong> Cord InjuryAlberto Esquenazi, M.D.Until now, wheelchair propulsion has been themost common mode of locomotion for individualswith a motor complete thoracic level spinal cordinjury (SCI). 1 Using a wheelchair, individuals are oftenable to navigate around a properly modified homeand workplace environment, perform many activitiesof daily living, and engage in some social and recreationalactivities. However, wheelchair seating posturereduces the opportunity for eye to eye social interactionwith able bodied adults, does not load the legsin a normal manner, can promote joint contractures,lead to pressure sores, and increase the risk of shoulderoveruse.Other modes of locomotion such as knee-anklefootorthoses (KAFOs) have come up far short of eventhe standard set by the wheelchair. Difficulty donning/doffing, high energy consumption and potential forincreased upper limb overuse can all be identified ascauses for KAFOs’ limited use only as a therapeuticintervention.Functional Electric Stimulation (FES) systems mayenable patients to ambulate for very limited distances.This technique also has many limitations including requiringfunctioning lower motor neurons (LMNs) forneuromuscular excitability and complete sensory lossto tolerate the significant electrical stimulus needed toachieve muscular contraction. In addition, electricalstimulation differs greatly from the physiological nerveimpulse because in FES all motor units in a musclegroup are stimulated simultaneously. This rapidly inducesmuscle fatigue and results in high-energy consumption.The functional performances of all thesemethods remain quite modest in comparison to normalgait due to very low walking speed and high-energyutilization.An alternative here described is the use of an externallypowered orthosis that facilitates independentwalking and in some cases stair climbing.lower level motor complete SCI to walk independently.ReWalk contains independently computer-controlledbilateral hip and knee joint motors, rechargeable batteries,and a computerized control system carried ina backpack. ReWalk users fully control their walkingthrough subtle trunk motion and changes in center ofgravity positions. A sensor registers these changes,determines the angle of the torso, and generates a presethip and knee displacement (angle and time) thatresults in stepping. The ankles are supported usingsimple double action orthotic joints that have limitedmotion and spring assisted dorsiflexion, adjustablethrough screw tension. ReWalk currently existsin two versions, ReWalk I for use in institutional setup and ReWalk P for use at home and in the community.ReWalk I is easily adjustable in height andwidth, has padded interfaces for calves and thighs,and a rigid pelvic frame linking the limbs. PaddedDescription of the ReWalk TMExoskeleton Suit 2,3The ReWalk is a lower extremity, battery poweredexoskeleton that allows individuals with thoracic orSPRING 2013 VOL. 8 No. 1The ReWalk suit enables ambulation for those with thoracic levelmotor complete spinal cord injury. Image courtesy of Argo MedicalTechnologies.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 26
SPINAL RESEARCH FOUNDATIONA. Esquenazi/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 26–28Velcro closures, shoes, and a waist belt are used tosecure the user in the exoskeleton. ReWalk P is availablein 4 sizes and multiple colors and is fitted by themanufacturer to match the patient anatomy. The samesystem, as previously described for ReWalk I, is alsoused to secure the user in the ReWalk P exoskeleton.Crutches provide standing stability, and the subject caninteract remotely with the computer system handlinga user-operated wrist pad controller that can commandsit to stand, stand to sit, and walk activation.Currently, there are two other commercial systemsfollowing on the tracks of ReWalk, but theunique manner in which the user is actively involvedin controlling walking is only available inthe ReWalk system. The specially designed softwarealgorithm interprets a signal from the torsoplaced sensor and generates alternating limb coordinatedmotion to produce bipedal walking. As asafety feature, the system prevents two sequentialsteps of the same leg. During training, joint angledisplacements for the knee and hip can be adjustedusing an external computer to optimize the walkingcharacteristics of the user. A manual training modecan be used to trigger steps bypassing the tilt sensor.The same mode of operation can be used to triggersit-stand-sit transfers.ReWalk is suitable for adults who have preservedbilateral upper extremity function after sustaining aSCI. Because the system is battery powered, completelyuntethered, and individuals are fully in controlof when they step, ReWalk offers a real optionto improve upon the current ambulation standard forindividuals with thoracic level motor complete SCI.Moreover, because walking in ReWalk emulatesupright bipedal walking, it may offer the potentialto overcome some of the physical and psychosocialproblems caused by the loss of natural walking.(Figure 1)Figure 1. Components of Argo’s ReWalk system. Image courtesy ofArgo Medical Technologies.Impact of the Loss of Walking for theSCI PopulationLack of standing, ambulation, muscle activity, weightbearing, and neuro-endocrine changes, all contributeto rapid and marked alteration in body composition.Individuals with SCI experience declines inmuscle mass and bone density, as well as increasesin adipose tissue. Additional complications, such asmuscle atrophy, joint contractures, pressure sores,osteoporosis, increased spasticity, pain, edema, urinaryand intestinal stasis, and carbohydrate, lipidand protein metabolism abnormalities may also bepresent. 4,527 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentNon-recreational walking accounts for a significantfraction of activity for the average non-disabledadult. Lower physical activity levels have been observedafter SCI resulting from lost motor function,lack of training during acute rehabilitation, decreasedaccess to exercise facilities with adequate adaptivefitness equipment, limited time, and psychologicalfactors. The physical de-conditioning resulting fromlargely sedentary lives of individuals with thoracic orhigher level SCI is well documented. 5,6 Exercise hasbeen shown to be an effective contributor to overallhealth maintenance, bone density, a proper level ofmuscle tone, cardiovascular fitness, regular boweland bladder function, reduced risk for obesity, heartdisease, and reduction of Type II diabetes for patientswith SCI. Therapeutic exercise for individuals withSCI have several limitations. For example, they mayhave difficulty in exercise execution, insufficient cardiovascularstimulus, greater potential for injury, andthey need specialized equipment. Individuals with thoraciclevel SCI who rely on wheelchair propulsion forlocomotion and their arms for transfers may increasethe likelihood of overuse of already taxed upper limbjoints when performing upper body exercises includinghand ergometry or weight lifting. Reduced workand leisure time after a SCI has been reported to reduceadherence to an exercise routine that is separatefrom, rather than a part of, the activities of daily living.Functional walking is an excellent means to accomplishexercise without requiring extra time commitments,but this is a difficult option—particularlyfor those with motor complete SCI at the thoracic orhigher levels. ReWalk facilitates functional independentwalking and may have a positive impact on manyof the detrimental effects of spinal cord injury. In tworecent publications, we have demonstrated the safetyand tolerability of the device and some of the effectsof training. Additional trials needed to demonstrate itsimpact on other physiological parameters are in thedevelopment stage.References1. Kirshblum S, Priebe M, Ho C, et al. <strong>Spinal</strong> cord injury medicine.3. Rehabilitation phase after acute spinal cord injury. Arch PhysMed Rehabil. 2007;88((3 Suppl 1)):S62–70.2. Esquenazi A, Talaty M, Packel A, et al. The ReWalk powered exoskeletonto restore ambulatory function to individuals with thoracic-levelmotor-complete spinal cord injury. American <strong>Journal</strong>of Physical Medicine & Rehabilitation. 2012;91(11):911–921.3. Zeilig G, Weingarden H, Zwecker M, et al. Safety and toleranceof the ReWalk exoskeleton suit for ambulation by people withcomplete spinal cord injury: a pilot study. The <strong>Journal</strong> of <strong>Spinal</strong>Cord Medicine. 2012;35(2):96–101.4. Elder C, Apple D, Bickel C, et al. Intramuscular fat and glucosetolerance after spinal cord injury—a cross-sectional study. <strong>Spinal</strong>Cord. 2004;42(12):711–716.5. Brenes G, Dearwater S, Shapera R, et al. High density lipoproteincholesterol concentrations in physically active and sedentaryspinal cord injured patients. Arch Phys Med Rehabil. 1986;67(7):445–450.6. Jacobs P, Nash M. Exercise recommendations for individualswith spinal cord injury. Sports Med. 2004;34(11):727–751.Alberto Esquenazi, M.D.Alberto Esquenazi, MD is board-certifiedin physical medicine and rehabilitation.His areas of interest are amputation, gaitand balance disorders, and post-poliosyndrome. Dr. Esquenazi is a member ofAmerican Academy of Physical Medicineand Rehabilitation (AAPM&R), AmericanSociety of Biomechanics, Gait and ClinicalMovement Analysis Society, and International Society forProsthetics and Orthotics. He is a professor of rehabilitationat Temple University School of Medicine, Thomas JeffersonUniversity—Jefferson Medical College and Drexel UniversityCollege of Medicine. He serves as director of the Annual Inter-City Gait and Orthotics course sponsored by the Temple/Moss-Rehab physical medicine and rehabilitation residency trainingprogram. He was a member of the Task Force on Medical Rehabilitation<strong>Research</strong> for the U.S. Department of Health andHuman Services. He is a fellow of the American Academy ofCerebral Palsy and Developmental Medicine and AAPM&R.He has published many original papers, book chapters andhas presented nationally and internationally on amputation, rehabilitation,orthosis, gait analysis and spasticity management.He’s an active researcher in technology and rehabilitation.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 28
SPRING 2013New Horizons in Spine TreatmentNSAIDsWhen treating pain, physicians will typically start withoral nonsteroidal anti-inflammatory drugs that willaddress the pain from acute or chronic inflammation incases of arthritis, bursitis, tendonitis and some cancerpain. Traditional NSAIDs are numerous and can haveassociated side effects of gastrointestinal discomfortespecially with long term use. Newer, more selectiveNSAIDs known as COX-II inhibitors (e.g., Celebrex),increase tolerability by decreasing the chance of GIirritation. Other new medications (Arthrotec, Vimovo)come in a combination of a NSAID and a GI “protective”medication to negate the common adverseeffects on the stomach. Albeit helpful, these newerNSAIDs still have potential to cause harm if not carefullymonitored.AntidepressantsFor a long time, low doses of common antidepressantswere being prescribed for many chronic pain problems.These drugs adjust levels of neurochemicals,which is thought to be their mechanisms for helpingto control pain. Antidepressants are often used asanalgesic adjuvants when patients don’t get completechronic pain relief from other treatments. They relievepain regardless of whether the person is depressed ornot. The doses needed to treat pain are usually lowerthan doses used for depression treatment. Tricyclicantidepressants (TCA) like amitriptyline (Elavil) andnortriptyline (Pamelor) have long been the mainstayantidepressants prescribed to help treat neuropathicpain like cancer pain, diabetic peripheral neuropathy,and postherpetic neuralgia (PHN) pain from shingles.They affect the brain concentrations of norepinephrineand serotonin. Their main disadvantage, which limitedtheir use, was their strong side effects including, butnot limited to, sedation, dry mouth, and orthostasis(low blood pressure upon standing).More recently, new antidepressants have been developedwith better side effect profiles and specificindications for certain chronic pain syndromes. Duloxetine(Cymbalta) and Milnacipran HCL (Savella)are in a class of antidepressants called serotonin andnorephinephrine reuptake inhibitors (SNRI), whichSPRING 2013 VOL. 8 No. 1increases the availability of these chemicals in thebrain. Cymbalta is FDA-approved for the treatmentof diabetic neuropathy, fibromyalgia, and musculoskeletalpain like that of osteoporosis and chronic lowback pain. Savella is FDA-approved for the treatmentof fibromyalgia.Topical MedicationsPain relief creams are increasingly becoming morepopular to treat certain types of pain. Topical pain killerslike Zostrix contain capsaicin, an ingredient foundin peppers, which works by reducing transmission of apain-relaying chemical called Substance P to the brain.Other products like Aspercreme and Bengay haveingredients like salicylate which decreases inflammationand relieves pain as well as counter-irritants likecamphor, eucalyptus oil, and menthol, which relievepain by causing either coolness or heat at the painfulregion. Topical NSAIDs are now available in gel(Voltaren Gel) and liquid (Pennsaid) form to addressarthritic conditions.There are also new types of transdermal patchesthat act to relieve pain. The Lidoderm patch containslidocaine to offer local anesthesia. These patches areFDA-approved for chronic nerve pain from shingles,a condition known as postherpetic neuralgia. Qutenzais another pain patch that contains capsaicin to helprelieve neuropathic pain. It is usually applied byyour doctor and can be used every three months. Afinal type of pain patch is a transdermal NSAID patch(Flector) indicated for acute musculoskeletal strainsand sprains.Opiate AnalgesicsWhen pain is severe, pain specialists may opt to trystronger pain medications. Opiate pain medicationshave been used since the beginning of human history.Narcotic pain medications like codeine, fentanyl,morphine, and oxycodone bind to central pain receptorsand are very effective in controlling severe pain.Oxymorphone (Opana) is a newer synthetic opiatethat is unique in its lack of CYP enzyme interactionwith other drug metabolism (avoiding adverse druginteraction). Advances in opiate medication include<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 30
SPINAL RESEARCH FOUNDATIONT. Nguyen/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 29–35extended release preparations that are longer induration, ranging from a twenty-four hour extendedrelease morphine pill (Avinza) to a seven day extendedrelease transdermal buprenorphine patch (Butrans).Innovation in immediate release preparations includetransmucosal fentanyl lozenges (Actiq), sublingualfentanyl sprays (Subsys) and sublingual fentanyl tablets(Fentora, Abstral); all of which are indicated forbreakthrough cancer pain.Recent advances have also come in the area of injectiontechnique. First came fluoroscopic imaging to assistwith needle placement, which was previously done“blinded” or by “feel”. Now, in an attempt to limit exposureto radiation, needle guidance and identification ofstructures is done with ultrasound. (Figures 2 and 3)Procedures and InjectionsInjections of medications to decrease pain and inflammationhave long been used in pain medicine as additional,adjunctive treatment to medications. Traditionally,it has always been a combination of a steroid anda local anesthetic agent. The steroid acts to interruptthe inflammatory cascade that leads to pain and swelling.The local anesthetic provides immediate painrelief to provide diagnostic confirmation of the paingenerator as well as to break the pain cycle in certainchronic pain syndromes like Complex Regional PainSyndrome (CRPS) and trigger points.Platelet Rich Plasma (PRP) TherapyThis is a revolutionary new treatment that relievespain by promoting long lasting healing of musculoskeletalconditions. The body’s first response to softtissue injury is to deliver platelet cells. Packed withgrowth and healing factors, platelets initiate repairand attract the critical assistance of stem cells. PRPtherapy channels the body’s natural healing processto an injured region by delivering a higher concentrationof platelets. To create PRP therapy, a smallsample of blood is drawn (similar to a lab test sample)from the patient and placed in a centrifuge thatspins the blood at high speeds, separating the plateletsfrom the other components. The concentratedplatelet rich plasma (PRP) is then injected into andaround the point of injury, jump-starting and significantlystrengthening the body’s natural healing signal.Because the patient’s own blood is used, thereis no risk of a transmissible infection and a very lowrisk of allergic reaction.Figure 2. Fluoroscopic-guided procedure helps physicians visualizeneedle placement during injections.Figure 3. Ultrasound machines guide needle injections withoutharmful radiation exposure. Image courtesy of the Mayo Clinic.31 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentRadiofrequency AblationA radiofrequency ablation (RFA) interrupts the sensorynerve pain signal to the involved facet or sacroiliacjoint through the use of thermal denervation. Afterthe skin is adequately anesthetized, the physician usesfluoroscopy (x-ray) guidance to place special radiofrequencyneedles alongside the nerves that supply theinflamed joint. After testing to ensure that the needleis in the correct position, thermal energy is applied,and the nerve is deadened. The goal of the RFA procedureis to provide more prolonged duration of relieffor many months to years that is not achieved throughstandard steroid injections. This procedure is done asan outpatient. (Figures 4 and 5)Interventional Therapies<strong>Spinal</strong> Cord Stimulation<strong>Spinal</strong> cord stimulation (SCS) is an innovative technologythat addresses some of the most difficultpain problems experienced. Proven 1–3 as an effectivetreatment option for many chronic sufferers, SCSFigure 5. Facet radiofrequency ablation. Thermal energy is conductedthrough needles to destroy nerves surrounding the irritatedfacets in order to interrupt the painful stimulus. Image courtesy ofthe Mayo Clinic.Figure 4. Fluoroscopic image of lumbar facet radiofrequency ablationprocedure.SPRING 2013 VOL. 8 No. 1is most often used for neuropathic pain, includingspinal radiculopathies, diabetic peripheral neuropathies,post-laminectomy syndrome (residual painafter back surgery), and Complex Regional PainSyndrome (CRPS). 4 Neuropathic pain occurs whenthere is an injury, disease, or trauma to the centralnervous system (spinal cord) or peripheral nervoussystem (any nerves outside the spinal column). Neuropathicpain symptoms can cause sharp, pricking,and/or stabbing pain. You may experience intensepain from a non-painful stimulus such as a lighttouch or a brush against the skin. You may also feelan exaggerated response to a painful stimulus. <strong>Spinal</strong>cord stimulation is an implanted device that transmitsmild electrical impulses to the pain transmittingtracts on the spinal cord. The stimulation interruptsthe message of feeling pain and substitutes it with amore pleasing sensation called paresthesia or “pleasanttingling”. <strong>Spinal</strong> cord stimulation is often used<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 32
SPINAL RESEARCH FOUNDATIONT. Nguyen/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 29–35when other treatments havefailed. Recent new technologyis focused on rechargeable,multi-programmable generatorsand various electrical leadarrays and configurations toprovide maximal stimulationcoverage. (Figure 6)Intrathecal PumpsAn intrathecal pain pump is amethod of delivering pain medicationdirectly to a patient’sspinal cord. The system usesa small, programmable pumpthat is surgically placed underthe skin of the abdomen anddelivers medication through acatheter into the area aroundthe spinal cord (similar to anepidural that women may haveduring childbirth). A pain pumpmay be a treatment option if allother traditional methods havefailed to relieve long-term symptoms of chronic pain.Because the medication is delivered directly to thespinal cord, symptoms can be controlled with a muchsmaller dose than is needed with oral medication. Thegoal of an intrathecal pain pump is to better controla patient’s symptoms while drastically reducing theside effects noted with oral medications. An intrathecalpain pump works much more efficiently than oralpain medication because it delivers medicine directlyinto the cerebrospinal fluid, bypassing the path thatoral medication takes through the body. In fact, thepotency of the medication is about 100–300x morewith the pump than when taken orally. (Figure 7)Figure 6. An implanted spinal cord stimulator device treats neuropathies by interrupting the painfulnerve signal and replacing it with a more pleasant sensation called paresthesia. Image courtesy ofSt. Jude Medical, Inc.implanted electrodes. DBS was developed in the 1980sprincipally to treat movement disorders associatedwith essential tremor (ET) and Parkinson’s disease(PD). Today, its applications include other types ofNew Therapies on the HorizonDeep Brain Stimulation (DBS)The goal of deep brain stimulation and motor cortexstimulation is to restore function or relieve painby stimulating neural activity through surgicallyFigure 7. This intrathecal pain pump is implanted under the skin ofthe abdomen and delivers pain medication directly to the spinalcord.33 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentmovement disorders and certain non-motor syndromesand pain conditions. Currently, deep brain stimulationis being studied to treat central neuropathic pain syndromeslike trigeminal autonomic cephalgia and clusterheadaches. 5Transcranial Magnetic Stimulation (TMS)Transcranial magnetic stimulation is a tool that hasbeen used in a wide variety of neurological disorders,including experimental, diagnostic, and therapeuticpurposes. The TMS procedure produces a magneticfield that traverses the skull relatively unimpeded andinduces an electrical field that yields actual brain stimulation.(Because TMS is noninvasive and painless, itcan be easily performed in awake patients. RepetitiveTMS has been investigated as a potential therapy inpatients with medically intractable neuropathic painand migraine headaches. 6 (Figure 8)Fentanyl HCL Iontophoretic Transdermal System(Fentanyl ITS)The use of patient-controlled analgesia (PCA) over thelast few decades has resulted in vast improvement inmanagement of postoperative pain control and patientFigure 8. Transcranial Magnetic Stimulation (TMS) uses a magneticcoil to induce a magnetic field across the brain, yielding brain activitystimulation. Image courtesy of the Laboratory for Cognitionand Neural Stimulation, Neurology Department, School of Medicine,University of Pennsylvania.satisfaction. PCA allows patients to self-administerpain medications according to their own personalrequirements for pain relief. The common routes ofFigures 9 and 10. Iontophoresis. The patient controls drug delivery through the skin with low-intensity electric current. Image courtesy ofJanssen Pharmaceutica NV, Beerse, Belgium.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 34
SPINAL RESEARCH FOUNDATIONT. Nguyen/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 29–35administration for the PCA have been through theintravenous line or epidural catheter. Iontophoresisuses a low-intensity electric current to transport ionizeddrug molecules actively across the skin and intothe systemic circulation. Iontophoretic drug delivery ismore advantageous over passive transdermal administrationas the drug delivery is strictly controlled bythe application of electric current which offers precisecontrol over the frequency of analgesic dosing with anon-invasive approach. 7 (Figures 9 and 10)ConclusionAs the field of pain management evolves, scientistsand clinicians from various specialties and medicalfields work towards ever improving our understandingof the mechanism of pain and how to counteractit to provide excellent pain control. We look for newinnovative medications, devices, delivery systems andsurgeries. We aim to achieve satisfactory analgesiawhile limiting adverse effects from medications. Wehave only reached the tip of the iceberg.References1. Cameron T. Safety and efficacy of spinal cord stimulation for thetreatment of chronic pain: a 20-year literature review. J Neurosurg.2004;100(3 Suppl Spine):254–267.2. Mailis-Gagnon A, Furlan AD, Sandoval JA, et al. <strong>Spinal</strong> cordstimulation for chronic pain. Cochrane database of systematicreviews (Online). 2004(3):CD003783.3. Ubbink DT, and Vermeulen H. <strong>Spinal</strong> cord stimulation for nonreconstructablechronic critical leg ischaemia. Cochrane databaseof systematic reviews (Online). 2005(3):CD004001.4. Kemler MA, Barendse GA, van Kleef M, et al. <strong>Spinal</strong> cord stimulationin patients with chronic reflex sympathetic dystrophy. NEngl J Med. 2000;343(9):618–624.5. Bittar RG, Kar-Purkayastha I, Owen SL, et al. Deep brain stimulationfor pain relief: a meta-analysis. <strong>Journal</strong> of Clinical Neuroscience.2005;12(5):515–519.6. Leo RJ, and Latif T. Repetitive transcranial magnetic stimulation(rTMS) in experimentally induced and chronic neuropathic pain:a review. J Pain. 2007;8(6):453–459.7. Power I. Fentanyl HCl iontophoretic transdermal system (ITS):clinical application of iontophoretic technology in the managementof acute postoperative pain. British <strong>Journal</strong> of Anaesthesia.2007;98(1):4–11.Thomas T. Nguyen, M.D.,D.A.B.P.M.Dr. Nguyen specializes in advanced,minimally invasive diagnostic andtreatment modalities for acute andchronic pain syndromes. Dr. Nguyenhas practiced pain medicine since finishinghis pain fellowship at the MayoClinic in 1999. He was the founder andmedical director of the Comprehensive Pain ManagementCenter in Newport News, VA from 1999–2002. He is an activemember of the American Academy of Pain Medicine, theInternational Spine Intervention Society, and the AmericanAcademy of Family Practice. Dr. Nguyen is involved in severalnational multicenter studies for the treatment of chronicback pain.35 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Sacroiliac Joint StabilizationMichael W. Hasz, M.D., F.A.C.S.Within the past few years, there has been a resurgencein the recognition of the sacroiliac (SI)joint as a potential source of low back pain. For instance,up to 25% of patients presenting to a spineclinic have been found to have significant pain contributionfrom the hip or SI joint. 1 Much of this resurgenceis due to recent advances in the treatmentoptions of sacroiliac joint dysfunction. The majorityof patients can be treated non-operatively throughanti-inflammatory medications, physical therapy, or SIjoint injections. However, some patients will requiresurgical treatment. This review discusses two recententries into the lateral approach for the stabilizationand fusion of the sacroiliac joint.Numerous techniques have been described for thesurgical treatment of sacroiliac joint dysfunction withlittle agreement as to their relative advantages. OneFigure 1. SI-Bone’s iFuse implant. Image courtesy of SI-BONE, Inc.SPRING 2013 VOL. 8 No. 1Figure 2. The iFuse implant inserted across the sacroiliac joint to reducepain and give stability to the joint. Image courtesy of SI-BONE, Inc.type of surgical technique involves the removal of arectangular window of bone from the ilium immediatelyover the sacroiliac joint, allowing exposure ofthe articular surface of the joint. The articular cartilageis curetted from the sacrum and the ilium, thenthe bone block is reinserted. The joint is stabilizedwith the use of a T- or L-plate and screws. Patientshave to remain non-weightbearing on the affectedside for 3 months or until evidence of solid fusion isseen. 2Another approach to the stabilization of the sacroiliacjoint uses the percutaneous placement of cannulatedscrews across the joint. This procedure stabilizesthe joint but does not fuse it. In my experience, reviewingpatients who have had this procedure, the initialstabilization can afford some pain relief. However,often the continued micromotion across the sacroiliacjoint lends toward eventual loosening of the stabilization,and the patient’s symptoms often return.Two recent techniques have been proposed toaddress the issue of late loosening. One is the iFuseimplant system from SI-Bone (San Jose, CA). Theother is the SImmetry system from Zyga Technologies(Minneapolis, MN). Both of these technologies affordlateral access to and offer stabilization of the sacroiliacjoint. The initial stabilization is provided by theinstrumentation.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 36
SPINAL RESEARCH FOUNDATIONM.W. Hasz/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 36–37In the case of the iFuse system, two to four, butusually three, triangular shaped titanium rods areplaced across the sacroiliac joint, with the rod extendingfrom within the ilium to within the sacrum (Figure1). These rods afford initial stabilization and canprovide significant initial improvement in the pain,postoperatively. The iFuse procedure also relies upona surface technology on the implants (porous plasmaspray) to encourage and/or allow bone in-growth intothese devices. Both the triangular shape and the coatingof the implant are designed to prevent rotation andmotion of the SI joint, with the intention to give longtermstability to the joint (Figure 2).The Zyga SImmetry system also affords initial stabilizationacross the SI joint via two large compressionscrews (Figure 3). Zyga’s technology differs fromthat of SI-Bone in that it actually addresses a goal ofobtaining a fusion of the SI joint. A device is placed directlyinto the SI joint to remove soft tissue and preparethe bony edges for actual fusion. Once the SI joint hasbeen prepared, bone graft can then be placed withinthe joint. Two screws are placed across the joint forinitial stability andthe long-term goal ofactual fusion of theSI joint (Figure 4).Both technologies,from SI-Boneand Zyga, are musclesplitting, smallincision approaches.They require fluoroscopicimaging orother image guidancefor the procedure.They are a lateralapproach to andacross the sacroiliacjoint, and both canallow the patient tobe up and mobilizedvery rapidly.Figure 4. SImmetry screws implanted tofuse the sacroiliac joint. Image courtesyof Zyga Technology.References1. Sembrano, JN, and DW Polly, Jr. How often is low back pain notcoming from the back Spine. 2009;34(1):E27–32.2. Buchowski, JM, et al. Functional and radiographic outcome ofsacroiliac arthrodesis for the disorders of the sacroiliac joint. Thespine journal. 2005;5(5):520–528.Michael W. Hasz, M.D.,F.A.C.S.Figure 3. Zyga Technology’s SImmetry compression screws. Imagecourtesy of Zyga Technology.Dr. Hasz is a spine surgeon at The VirginiaSpine Institute. He is board certifiedby The American Board of Spine Surgery,a Fellow in the American Academyof Orthopaedic Surgeons and a memberof both the American Association ofOrthopaedic Surgeons and the North American Spine Society.He was Chairman of the Department of Orthopaedic Surgeryand Director of <strong>Spinal</strong> Surgery at the Andrews Air Force Base/Malcolm Grow Medical Center in Maryland. He currently holdsan appointment as Clinical Instructor of Orthopaedic Surgeryand Assistant Professor of Surgery at the Uniformed ServicesHealth Science University in Bethesda, Maryland.37 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013Trigger Point Dry NeedlingJessica Stepien, P.T., D.P.T.Trigger point dry needling, also known as intramuscularstimulation, is a technique using asolid filament needle to treat hyperirritable spots ofthe skeletal muscle. These hyperirritable spots arecalled trigger points and are typically associated withpalpable nodules in taut bands of tissue. (Figure 1)Physical therapists insert a dry needle, without medicationor injection, in trigger points to treat myofascialpain. 1As far back as the 16th century, myofascial painsyndromes have been recognized by medical practitionersas causing sensory, motor, and autonomic symptomsand dysfunctions. Myofascial pain syndromesare associated with the palpable nodules or taut bandsknown as myofascial trigger points. Dr. Janet Travellis recognized for bringing attention to myofascial triggerpoints in the mid 1900’s. Dr. Travell started hermedical career in cardiology and later shifted to musculoskeletalconditions due to her interest in musclepain and the impact of referred pain on patient’s dysfunction.Myofascial origin of pain was discoveredthrough an injection of hypertonic saline into triggerpoints which produced referred pain patterns. Initially,injection of an analgesic medication into the triggerpoints produced a decrease in a patient’s symptoms,pain, and the sensitivity to touch of the trigger points. 2After further research, it was discovered that the actualinsertion and stimulation of the muscle with a dryneedle produced pain relief without the need for medication.Thus, the development of trigger point dry needlingbegan. (Figure 2)Figure 1. Trigger point complex. Image courtesy of Medscape.com,2011, available at http://emedicine.com/article/89095-overview. Figure 2. Trigger point needling.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 38
SPINAL RESEARCH FOUNDATIONJ. Stepien/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 38–40The perpetuating factors of myofascial pain syndromesare low level musculature contraction, unaccustomedeccentric contraction, muscle overloads, andmuscle fatigue. These factors can be caused by, but notlimited to, mechanical dysfunctions such as forwardhead postures, joint hypermobilities, ergonomic stressors,poor body mechanics, and scoliosis.Dry needling techniques are developed on variousmodels, which are implemented in physical therapypractices on a daily basis. Dr. Chan Gunn contributedto the development of dry needling and introduced theterm intramuscular stimulation (IMS), in which he describedthat myofascial pain syndromes are a result ofradiculopathy or peripheral neuropathy, causing a disorderedfunction of the peripheral nerve. This conceptis referred to as the radiculopathy model and is basedon the Cannon and Rosenblueth’s law of denervation,which states that free flow of nerve impulses maintainsinnervated function and integrity of structures. Whenany neural flow is disrupted, all the structures thatare innervated by that nerve, such as skeletal muscle,smooth muscle, spinal neurons, sympathetic ganglia,and sweat glands, are affected and can become atrophic,highly irritable, and hypersensitive. The triggerpoint model describes myofascial trigger points consistingof taut musculature bands due to the excessiverelease of acetylcholine. Myofascial trigger points areclassified as active or latent. Active myofascial triggerpoints can cause local and referred pain, or otherparasthesias, whereas latent myofascial trigger pointsmay not produce pain without being stimulated. Activemyofascial trigger points typically refer pain toa particular site, and these sites are not restricted toa single segmental or peripheral nerve distribution.Clinically, myofascial trigger points can cause motordysfunction or muscle weakness as a result of motorinhibition, restricted motion, and muscular stiffness.Furthermore, sensory dysfunctions may be notedthrough localized tenderness, referral of pain to specificareas, hyperalgesia (extreme pain reaction to apainful stimulus), and/or allodynia (pain reaction to anon-painful stimulus).The goal of the insertion of a fine filament needleinto a trigger point is to produce a twitch response(short contraction) of the muscle being needled. Thetwitch of the muscle is the desired response; however,benefits can occur even without a twitch of themuscle. The simple insertion of the needle into thetaut bands can interrupt the pathogenic process andproduce mechanical changes in the tissue. (Figure 3)The insertion of a needle into the trigger point canproduce a deep ache or cramping pressure that lastsonly briefly. Reproduction of pain and referral ofsymptoms may also occur, and soreness may last upto 24–48 hours. Improvements in functional range ofmotion, decrease in complaints of pain, and ease ofmobility may be seen after treatment.Dry needling allows access to deep musculaturethat may never have been reached without the useof a needle. By releasing the myofascial restrictionsthrough trigger point dry needling, a physical therapistis able to further enhance a patients care and returnto function. Trigger point dry needling can disrupt theFigure 3. Identification of trigger by low-twitch response to palpation.Image courtesy of Medscape.com, 2011, available at http://emedicine.com/article/89095-overview.39 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentneurological feedback loop eliciting pain in the musculoskeletalsystem.Myofascial trigger point dry needling has no similaritieswith traditional acupuncture except for the toolbeing used during the process. 3 Traditionally, acupunctureis based upon Chinese medicine that seeksto regulate flow and stability of energy through subcutaneousplacements of needles. Acupuncture pointsare points mainly along the paths of energy flow (ormeridians). In contrast, trigger point dry needles areinserted into specific musculature, targeting tight muscles,and based on neuromuscular and biomechanicalprinciples.Trigger point dry needling is a novel technique inphysical therapy. 4 Internationally, Australia, Belgium,Canada, Chile, Denmark, Ireland, The Netherlands,New Zealand, Norway, South Africa, Spain, Sweden,and Switzerland have recognized trigger point dryneedling to be within the scope of practice for a physicaltherapist. In the United States, each state licensureboard determines the appropriateness of dry needlingwithin the state’s scope of practice for physical therapy.In 1984, Maryland was the first state to approvedry needling as a technique within the scope of physicaltherapy practice. The acceptance of dry needling israpidly spreading. As of 2012, approximately 30 stateshave approved dry needling as a procedure within thescope of the physical therapy practice.References1. Dommerholt J, Mayoral del Moral O, Grobil C. Trigger PointDry Needling. J. Man. Manip. Ther. 2006;14(4):E70–E87.2. Dommerholt J, Bron C, and Franssen J. Myofascial TriggerPoints: An Evidence-Informed Review. J. Man. Manip. Ther.2006;14(4):203–221.3. Itoh K, Katsumi Y, Kitakoji H. Trigger Point Acupuncture Treatmentof Chronic Low Back Pain in Elderly Patients—a blindedRCT. Acupunct. Med. 2004;22(4):170–177.4. American Physical Therapy Association. Physical Therapist &the Performance of Dry Needling—An Educational ResourcePaper. 2012;2–5.Jessica Stepien, P.T., D.P.T.Dr. Stepien is a physical therapist at TheVirginia Therapy and Fitness Center.Her certifications and training includes:North American Institute of OrthopaedicManual Training, Level I & II; TherabandAcademy, Beyond Ball, Institute ofAdvanced Musculoskeletal Treatments,Trigger Point Dry Needling. Jessica’s commitment to quality inpatient care returns her patients back to physical excellencewhile achieving their goals and maximizing their quality of life.During her graduate studies, Jessica was awarded the K. MadisonSmith Award for Clinical Excellence as voted on by herclinical internship instructors, the 2012 Outstanding GraduateAward as voted on by her Shenandoah University professors,and received the Best Performance on Physical Therapy ComprehensiveExam for her graduation class.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 40
SPINAL RESEARCH FOUNDATIONAdvances in Bone Grafts and Fusion AugmentationMarcus M. Martin, Ph.D., and Anne G. Copay, Ph.D.One of the main sources of back pain is clinical spinalinstability. 1 This pain often originates at themotion segments of the spine or intervertebral discs.The resultant back pain is often treated with the surgicalstabilization of a painful spine segment. Instrumentationprovides an immediate stabilization of thespine segment, while bone grafts facilitate a biologicresponse to promote the formation of new bone. Theformation of new bone permanently fuses the spinesegments. Once fusion occurs, mechanical loads aretransferred from the instrumentation to the fused spinesegment. If fusion does not occur, the instrumentationwill remain subject to mechanical loads and mayeventually fail due to metal fatigue. 2 Furthermore,continued motion in a painful spine segment is likelyto remain a source of pain.Bone grafts are utilized as either scaffolding forosteogenesis (bone formation) or stimulation of bonegrowth in a desired area. Recently, there has been anincreased emphasis on incorporating biologic therapiesin bone-forming grafts.The mechanisms of actions of bone grafts fallinto three general types:• Osteogenesis: The bone graft contains boneformingcells (osteoblasts). Bone harvestedfrom a person’s iliac crest is typically used andcontains osteoblasts. Local bone removed atthe surgical site is a convenient source of graft,but generally contains cortical bone with muchfewer osteoblasts.• Osteoconduction: The graft material acts as ascaffold onto which bone cells can attach, grow,divide, and migrate. Osteoblasts work muchbetter when they have a scaffold or matrix forattachment.• Osteoinduction: The bone graft contains chemicalsthat attract primitive stem cells and immaturebone cells, then promote the proliferation anddifferentiation of these cells into bone-formingcells.Grafts may be classified according to their compositionand mechanism of actions.• Bone: Grafts made of bone are osteoconductiveand may be osteogenic if they contain boneformingcells.○○Autografts: patients’s own bone (iliac crest orlocal bone)○○Allografts: donor bone (cadavers or tissuebank)■■Demineralized bone matrix (DBM):human-derived bone powder is demineralized,leaving only the organic bone matrix■■Mineralized allograft: cortical/cancellousbone chips are chopped-up pieces of bone♦♦Xenograft: mineralized cortical granulesof bone derived from another species(most commonly cows and pigs).• Ceramics: Ceramics are synthetic materialsmanufactured so that each ceramic granulemimics human cancellous bone. Ceramics areprimarily osteoconductive. Common ceramicmaterials are:○○Hydroxyapatite (HA)○○Tricalcium Phosphate (TCP)○○Biphasic Calcium Phosphate (HA:TCP)○○Calcium Sulfate• Cell-signaling materials: Cell-signaling materialsare osteoinductive.○○Bone Morphogenetic Proteins (BMPs) areproteins present in small quantities withinbone. It would require hundreds of kilogramsof bone to extract milligram quantities ofBMP. <strong>Research</strong>ers were able to produce theseproteins in large quantities through the useof recombinant DNA technology. BMPs promotethe migration of primitive stem cells andimmature bone cells, their proliferation, andtheir differentiation into bone-forming cells.○○i-FACTOR Biologic Bone Graft combines aunique anorganic bone mineral (ABM) andsmall peptide (P-15) that acts as an attachmentfactor for specific integrins on osteogenic cells.Historically, bone harvested from the iliac crest hasbeen the graft of choice in spine surgery. However, itseffectiveness depends on the patient’s bone quality.41 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 1. BMPs are osteoinductive proteins that promote cell migration of bone-forming cells such as osteoblasts (shown in green), osteoprogenitorcells, and undifferentiated mesenchymal stem. Image courtesy of Medtronic, Inc.Furthermore, the added surgical procedure required toharvest bone from the iliac crest may lead to increasedmorbidity, blood loss, injury to local nerves, damageto blood and lymphatic vessels, infection, disturbancesin gait, prolonged hospitalization, and protracted recuperativetime. 3In 2006, the FDA approved the use of bone morphogeneticproteins (BMPs) in spinal fusion. BMPsare members of the TGF β superfamily of biologicalmolecules. BMP molecules share a similar structureand amino acid sequence at the carboxyl terminalregion. Different BMPs are not interchangeable,though some such as BMP-2 and BMP-4 show significanthomology. Through signaltransduction, BMP receptors effectthe mobilization of members of theSMAD family of proteins which areassociated with bone development. 4BMPs interact with bone morphogeneticprotein receptors (BMPRs)on the cell surface. This initiates acascade of events that can facilitatebone formation. BMPs may be activeat multiple points throughoutthis cascade. First, BMPs induce cellmigration to the site of administration.Osteoprogenitor cells, osteoblasts,and mesenchymal stem cellsrespond to the chemotaxic signal.Mesenchymal stem cells are undifferentiatedand can produce severalconnective tissue cells includingcartilage-producing chondrocytesand bone-producing osteoblasts.The proliferative response may beenhanced by molecular signals released by cells at theinjury site. BMPs affect undifferentiated cells but donot appear to have a cell-specific effect on mature differentiatedcells. 5 (Figure 1)Currently, a clinical trial has been launched investigatingthe use of P-15, an amino acid peptide, in cervicalfusion. i-FACTOR (Cerapedics, Broomfield,CO) is a peptide-enhanced bone graft that utilizes aunique small peptide (P-15) intended to stimulatethe natural bone healing process. It combines anorganicbone mineral (ABM) and P-15 to act togetheras an attachment factor for specific integrins on osteogeniccells. (Figure 2)Figure 2. iFACTOR Bone Graft is injected during spinal fusion surgeries. Image courtesy ofCerapedics, Inc.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 42
SPINAL RESEARCH FOUNDATIONM.M. Martin and A.G. Copay/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 41–44The first step in the bone formation process is cellattachment. Osteogenic precursor cells bind to P-15via their α2β1 integrins, which are signaling receptors.i-FACTOR bone graft is placed in a bony defectin the presence of bleeding bone, an environment richwith osteogenic cells. It is intended to increase the opportunityfor cell binding in the fusion site by makingan abundance of P-15 available to osteogenic precursorcells, potentially resulting in enhanced cell attachment.Osteogenic cells contain α2β1 integrins that actas signaling receptors, allowing cells to attach to P-15.Cell binding between P-15 and α2β1 integrins is intendedto initiate natural signaling of mechanical andchemical information within the cell and the extracellularmatrix, contributing to the production of specificgrowth factors, cytokines, and bone morphogeneticproteins (BMPs) and ultimately, leading to new boneformation. i-FACTOR is designed to stimulate a healingresponse only in the presence of bone-formingcells. This novel mechanism of action is intended toenhance the body’s natural bone healing process.P-15 Small Peptide- i-FACTOR technology isbased on the biological activity resulting from asynthetically derived form of a 15-amino acid peptidefound in type I human collagen. Type I humancollagen is the primary organic component foundin autograft bone. This 15-amino acid peptide isresponsible for the attachment and proliferation ofosteogenic cells. These cells attach to the syntheticP-15 part of i-FACTOR in a similar way they wouldattach to type I collagen.• Anorganic Bone Mineral (ABM) provides theoptimal surface for irreversible electrostaticbinding of P-15. ABM is a naturally porous bonescaffold with a physiological rate of resorption,resulting in a substrate favorable to osteogeniccell growth and formation.Figure 3. P-15: A synthetic fifteen amino acid polypeptide that mimics the cell-binding of Type 1 human collagen and is responsible forosteogenic cell attachment via α2-β1 integrins which activates the body’s production of BMPs and growth factors. Image courtesy ofCerapedics, Inc.43 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatment• Hydrogel Carrier- i-FACTOR Putty uses carboxymethylcellulose(CMC), an inert and biocompatiblehydrogel, to aid in the handling andplacement of the ABM/P-15 particles at thegraft site.i-FACTOR bone graft received the CE Mark, aregulatory conformity marking for products on theEuropean market, in late 2008. It has been utilizedclinically in over 10,000 spine, trauma, and orthopedicsurgeries worldwide. Currently, i-FACTOR bone graftis commercially available in both a Putty and Flex(flexible strip) form in more than 20 countries outsidethe United States. i-FACTOR bone graft is currentlybeing evaluated in the United States (FDA) as part ofan Investigational Device Exemption (IDE) clinicalstudy in the cervical spine and is not available for salein the US.A study of the early fusion rates and the rate ofgraft-related complications during an ALIF was performedcomparing autograft, i-FACTOR (P-15) andInfuse (rhBMP). Over 24 months, data was collectedfrom 95 consecutive ALIF implants in 75 patients (57single level, 16 double level and 2 three level surgeries).Of these, 10 were Infuse (rh-BMP), 10 wereautograft (iliac crest bone) and 75 were i-FACTOR(P-15). Outcomes were assessed based on standardcut coronal CT scans and graft-associated complications.Based upon 3 month data, all groups demonstratedexcellent early fusion rates with bony bridgingoccurring faster in Infuse and i-FACTOR patients. Atthe 3 month point, 3 out of 10 autograft patients sufferedfrom significant graft site pain; 1 out of 10 BMPpatients had a clinical complication; none of the 45iFACTOR patients had a clinical complication, thoughgraft migration was noted. The study data will have tobe analyzed after longer term follow-up to draw clinicallyrelevant conclusions from the study; however,the three month data is very promising.References1. Nachemson, AL. Advances in low-back pain, Clin Orthop 2001985;266–278.2. Slone RM, MacMillan M, Montgomery WJ. <strong>Spinal</strong> fixation. Part3. Complications of spinal instrumentation. Radiographics 1993Jul;13(4):797–816.3. Carreon LY, Glassman SD, Djurasovic M, Campbell MJ, PunoRM, Johnson JR, Dimar JR 2nd. RhBMP-2 versus iliac crest bonegraft for lumbar spine fusion in patients over 60 years ofage:a cost-utility study. Spine (Phila Pa 1976). 2009 Feb 1;34(3):238-43. doi: 10.1097/BRS.0b013e31818ffabe.4. Nohe A, Keating E, Knaus P, Petersen NO. Signal transductionof bone morphogenetic protein receptors. Cell Signal 2004Mar;16(3):291–9.5. Bishop GB, Einhorn TA. Current and future clinical applicationsof bone morphogenetic proteins in orthopaedic trauma surgery.Int Orthop. Dec 2007;31(6):721–727.Marcus M. Martin, Ph.D.Dr. Martin’s research interests include neuroimmunology,virology and immunology. Heis engaged in collaborative research throughSRF, with the Medical University of SouthCarolina Children’s Hospital, geared towardthe development of neuroprotective and neuroregenerativecompounds for the treatmentof nerve pathology. Dr. Martin’s current research collaborationsinclude research initiatives to apply stem cell therapy for tissuepreservation, the development of regenerative therapiesfor intervertebral discs, and the development of novel methodsof enhancing bone fusion.Anne G. Copay, Ph.D.Dr. Copay studies the outcomes of surgicaland non-surgical spine treatments. Shepublished several articles on the outcomesof spine fusion. She has ongoing researchprojects concerning the effectiveness of newspine technologies and the long-term outcomesof surgical treatments.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 44
SPINAL RESEARCH FOUNDATION4WEB <strong>Spinal</strong> Truss SystemTimothy Gainey, Ph.D.The Annual Meeting of the North American SpineSociety has always provided the perfect backdropfor original ideas and novel products, and supported aforum for creative exchange. This past year’s NASSmeeting in Dallas, TX did not disappoint those lookingfor innovation. One product in particular that garnereda lot of attention was the 4WEB <strong>Spinal</strong> TrussSystem. The cage was conceived by Jessee Hunt andinitially developed as a device that would providestructural support for interbody fusion. Its open configurationwas designed to sustain strength withoutimpeding or restricting the potential for bone to growinto and through the implant. It is believed that bydoing so, this new device would enable greater boneformation and fusion without compromising initialhealing or mechanical support (Figure 1). Modeledfrom a truss structure, the inherent design goal wasto extend the strain to the margins of the constructand reduce the concentration of forces at the surfaceof the implant in contact with the bony endplates—,essentially dissipating load broadly across the entiresurface (Figure 2).It has been known for some time that distributionand dissipation of stress are the hallmarks of bone remodeling.In that light, this device represents a uniqueforay into applied design that integrates the strengthinherent to truss geometry, the architecture of staticdistribution force, and the dynamics of bone remodelingas a fresh therapeutic approach to spine surgery.Recent advances in engineering technology (additivefabrication in particular) have aligned, and a new potentialfor complex and intricate designs and structurespreviously unavailable to medical manufacturing hasemerged. The 4WEB Truss Implant Technology representsa first opportunity to view that technology in aclinical application. A final design was evaluated andoptimized by Lisa Ferrara, Ph.D. (OrthoKinetic Technologies,LLC, Southport, NC) that would effectivelyminimize the material and maximize the distributionof strain—her guidance defining lateralization of forceand reduction of subsidence risk as an integrated facetof the process. The 4WEB truss was fabricated frommedical grade titanium alloy using Electron BeamWelding, conferring a rigid truss structure that wassubsequently validated for strength, stress, and straindistribution.The 4WEB <strong>Spinal</strong> Truss System was subjectedto a number of rigorous tests including finite elementanalysis, subsidence and mechanical performanceevaluation, as well as a 12-month large animal study.Even with the greatest confidence in product design,sometimes it is not possible to anticipate the serendip-Figure 1. The 4WEB <strong>Spinal</strong> Truss System was designed to promotegreater bone formation and fusion. Image courtesy of 4WEB Inc.Figure 2. The 4WEB design is based upon truss geometry in orderto disperse the load force across the structure’s surface. Imagecourtesy of 4WEB, Inc.45 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentity of biologic translation. Working with Peggy Lalor,Ph.D. (Histion, Inc., Everett, WA), a respected authorityof bone pathology, Jessee was on pins and needleswaiting for the histology results. Her remark of neverhaving seen such profuse filling of an interbody spinefusion device filled with autograft at 3-months increasedthe excitement surrounding this technology.Several additional independent reviews and positiveclinical reception from all physicians who have hadthe chance to interpret the histology, and an expeditedreview and clearance by FDA of the devices for clinicaluse as an ALIF for lumbar spine fusion, and morerecently as a cervical fusion device validate the animalstudy results.Assessments of the bone histology from the preclinicalmodel offered insight into bone remodelingthat under-anticipated the implications of the design.In an effort to lessen stress shielding, the 4WEB<strong>Spinal</strong> Truss System accentuated load sharing whilehastening structural bone constructs that interfacedand accepted the truss load. Unprecedented amountsof bone were deposited throughout the cage that resultedin an integrated fusion mass throughout thecage.increases, the bone will remodel over time to resiststrain associated with loading and translate the forcein tension.Recent advances in applied bone biomechanicsdefine optimal structural cues that encourage or escortbone remodeling. Insight emerging from thisfield addresses the eventuality of material evolutionand the appearance of structural synergy with loadbearing, strain energy density, and resultant boneformation. The innovation of the 4WEB geometricdesign incorporates unique engineering conceptsthat integrate truss resolution from global loadingpotentials resulting in augmented bone formationwith unique reciprocity and reliance on trajectorydriven loading (Figure 3). Impressive about boneformation around the construct is that bone thatformed both inside and outside the 4WEB <strong>Spinal</strong>Truss System is matched (Figures 4a and 4b). Thebone image inside the cage has been rendered athigher magnification to demonstrate the lamellarbone structure on both sides of the truss.The 4WEB <strong>Spinal</strong>Truss System—Load Transfer DesignThe open web design increasesvolume for bone deposition,and at the same time, providestensile struts that facilitate apposition.These effects were collaterallyefficient, assuring biomechanicalsupport analogousto rebar in cement and stimulatingan osteogenic responsevia a load transfer mechanism.Wolf’s Law describes the naturein which bone remodels, statingthat bone in a healthy person oranimal will adapt to the loads itis placed under to reduce strain.If loading on a particular boneFigure 3. Bone formation utilizing the 4WEB <strong>Spinal</strong> Truss System. Image courtesy of 4WEB, Inc.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 46
SPINAL RESEARCH FOUNDATIONT. Gainey/<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 45–48Figure 4. Left: bone formation outside of the 4WEB cage. Right: bone formation inside the 4WEB cage. Images courtesy of 4WEB, Inc.The 4WEB <strong>Spinal</strong> Truss System—Surface TopologyThe additive fabrication process used to manufacturethe intricate 4WEB design results in a fullyfused solid that has a micro texture surface topology/energy that has been shown to guide mesenchymalstem cells toward an osteogenic lineage. Presentedat the AAOS, and later published in The Spine <strong>Journal</strong>,an evaluation of acid-etched titanium alloy surfaceswas reported to guide stem cell osteogenic differentiation.1 While the concept of surface topologytriggering cell recognition and tissue differentiationis not a new concept, the 4WEB design maximizesthis mechanical asset by providing the microstructureto all of the struts that run throughout the boneimplant construct rather than restricting the surfacetopology to select contact surfaces seen in predicatedevices.SummaryThe 4WEB <strong>Spinal</strong> Truss System utilizes the geometricdistribution provided in a truss design to redistributeaxial loading vectors and exploit the generation ofshear forces that accentuate bone formation. This boneformation is highly organized, stabile, and hastens thedeposition of structural lamellar bone in a very shorttime. Histopatholological assessment did not revealany evidence of hypertrophic cartilage formation, suggestinstability, or provide any evidence of inflammatorychanges in the marrow that might resonate withchronic reactive bone.Finite element analysis shored up a basis forstress distribution that would minimize the likelihoodof subsidence while accentuating the openstructure that would allow bone to pass throughoutthe construct and integrate with the two adjacent cranialand caudal vertebral bodies. Topologic surfacefeatures of titanium struts mirrored roughness assessmentsthat have been shown to actively promoteosteoblast phenotype and reduce surface proliferation.The added enhancement of the additive fabricationtechnology contributed and correlated with theimpressive quality and substantial quantity of bonethat was seen within the devices tested in the largeanimal model.Although the 4WEB <strong>Spinal</strong> Truss System hasonly recently received FDA clearance for ALIF andACDF procedures, available clinical data suggeststhat reduced pain, accelerated return to function, anddemonstrated bone production are hallmarks of thesuccess of the device. The robust response demonstratedradiographically at 4 months provides confidencethat fusion is accelerated and that the openstructure of the system does not hamper clinicalevaluation (Figure 5). Given the accelerated forma-47 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 5. Radiographic evidence of fusion at 4 months after the cage was implanted. Images courtesy of 4WEB, Inc.tion of bone and reduction of pain attendant to use ofthe 4Web geometry, perhaps the next considerationis then furthered by optimization of intent to achievebetter clinical outcome, lessened patient morbidity,and demonstrated improvement in quality of life. Offeringrelief of pain, enhanced bone formation, andreturn to function, the 4WEB <strong>Spinal</strong> Truss Systemrepresents a tool affording a unique strategy for securinga stable fusion in treating degenerative discdisease.Reference1. Olivares-Navarrete R, Gittens RA, Schneider JM, Hyzy SL,Haithcock DA, Ullrich PF, Schwartz Z, and Boyan BD. Osteoblastsexhibit a more differentiated phenotype and increasedbone morphogenetic protein production on titanium alloy substratesthan on poly-ether-ether-ketone. The Spine <strong>Journal</strong> 2012;12:265–272 .Timothy Gainey, Ph.D.Tim Gainey is Director of Orthopaedic<strong>Research</strong> and Technology Developmentat the Atlanta Medical Center. He is alsothe recent President of co.don Tissue Engineering,a subsidiary of co.don AG. Hehas been published extensively in peer reviewjournals and a lecturer at a variety ofscientific meetings both domestically and overseas. Tim holds aB.S./B.A. degree at the University of Illinois and a Ph.D. degreeat the University of South Florida. He is a member of elevenprofessional societies including the Orthopaedic <strong>Research</strong> Societyand the American Association for the Advancement of theSciences. He has also been honored by various professionaland business organizations, most recently as the 2000 winnerof the Outstanding <strong>Research</strong> Award, Sofamor-Danek Award,Australian Spine Society. Further, Tim is an Editorial Reviewerfor industry publications including BioDrugs, <strong>Journal</strong> of PediatricOrthopaedics, Tissue Engineering, <strong>Journal</strong> of Shoulder andElbow Surgery.SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 48
SPINAL RESEARCH FOUNDATIONMinimally Invasive Approaches for Spine SurgeryDouglas G. Orndorff, M.D., Jim A. Youssef, M.D., Morgan A. Scott, M.S.,Florence C. Paillard, Ph.D., and Casey C. RobertsHistory and Rationale of MinimallyInvasive Spine SurgeryIt is estimated that 80% of the US population willexperience some form of back pain in their lifetimes. 1In many instances these symptoms are secondarydegenerative spinal conditions broadly referred to asdegenerative disc disease. Diagnoses include spinalstenosis, disc herniations, spondylolisthesis, and otherdegenerative conditions. The first attempt at care formost spinal conditions includes nonsurgical care suchas physical therapy and corticosteroid injections in thespine. When those nonsurgical procedures fail, surgerymay be considered.Traditional open surgery techniques for posteriorlumbar fusion procedures are widely acceptedas the basis of surgery in patients with prolonged orsevere pain, loss of function, and/or instability. However,these open procedures, which involve large5- to 6-inch incisions, are associated with lengthyhospital stays, long-term use of narcotic pain medication,and sizeable direct (hospital bills) and indirect(loss of patient productivity) costs. 2,3,4 Additionally,complications related to open surgical procedureshave become a concern. All of these open procedurescan be associated with incision-related pain and increasedpost-operative infections. 3,5 There are alsospecific complications associated with particular surgeries.For instance, posterior lumbar interbody fusion(PLIF), the fusion of vertebrae accessed throughan incision in the back, involves significant dissectionof the spine muscles. This potentially leads topermanent muscle denervation and loss of functionof the erector spinae, a large back muscle that runsup on each side of the spine and helps support thetorso. 6,7 Anterior lumbar interbody fusion (ALIF), thefusion of vertebrae accessed through the abdomen,may result in injury to the ureters, which carry urinefrom the kidneys to the bladder, large blood vessels,and the sympathetic plexus, a nerve complex whichresides in the abdomen and are all in close proximityto the surgical site. 8 In an open ALIF, the large incisionthrough the abdominal muscles may also resultin delayed recovery of abdominal muscle strengthand function.In the last two decades, spine surgery has greatlybenefited from innovations in surgical techniqueswhich have made it possible to use less invasive surgicalapproaches. These minimally invasive techniquesallow the surgeon to access the spine via smaller incisions(typically 1–2 inches instead of 5–6 inches),resulting in less dissection and less tissue trauma thanclassic open surgeries. Reducing tissue trauma duringsurgery has an important impact on patient outcomesbecause it decreases blood loss and scarring. This reducesthe incidence of complications, such as infections,shortens the length of hospital stay, and speedsrecovery. 3,5 Minimally invasive procedures can be performedas an outpatient surgery, where the patient canreturn home that same day. Patients also tend to beambulatory right away.Although many benefits can be obtained by usinga minimally invasive surgical technique, some of thedisadvantages must be considered; in some cases, thedisadvantages of the minimally invasive approach maynegate its advantages. The minimally invasive techniquehas a steep learning curve, and in the hands of aninexperienced surgeon, operative times may be prolonged,decreasing the advantages of the technique. 9Moreover, during minimally invasive surgeries, x-rays(fluoroscopy) are used to visualize the anatomy andguide the surgeon; thus, the exposure of the patientand the surgeon to increased radiation doses must alsobe considered. The issue of reduced visibility has beenone of the greatest barriers to the widespread adoptionof minimally invasive spine surgery. 10 To be competentin minimally invasive techniques, the surgeonmust have an exact knowledge of the spinal anatomyand all associated anatomical structures since the traditionalvisual and tactile landmarks may or may notbe present to guide the surgeon during the surgery.Without these visual and tactile cues, there is risk formisplacing spinal instrumentation or causing inadvertentneurological damage. 11,12Techniques Used in Minimally InvasiveSpine SurgeryAdvances in minimally invasive surgical technologiesin the last several decades were first made for joint49 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentsurgeries (such as knee and shoulder) by introducingarthroscopic surgery and gynecologic surgeries withthe advent of laparoscopy. In these techniques, the jointspace or abdominal cavity is expanded, and a camerais inserted to visualize the tissues. However, thesetechniques are rarely used in spine surgery becausethere is no joint space or cavity to expand, renderingthe introduction of a camera impossible. Thus, thefield of spine surgery had to develop specific tools toenable spine surgeons to perform minimally invasivesurgeries. Herein we describe some of the innovativetechniques that have made minimally invasive spinesurgery possible.Retractors and DilatorsTypically when a physician performs a traditionalopen spine surgery, a large incision (5 to 6 inches) ismade, and large retractors are used to hold the skinand muscles back to provide visualization of the levelsof the spine under operation. When a physicianperforms a less invasive surgery, a 1-inch incision ismade, and small tubular dilators (about ½ inch) areused to reach the area of the spine to be operated on.The dilator splits the muscles of the back creating achannel to the surgical site. This is often accomplishedthrough native avascular muscle planes, thus reducingthe amount of bleeding, tissue retraction, and traumato the spine musculature. This method is less damagingthan an open surgery where back muscles are dissectedto access the spine. The dilators progressivelyget larger until the physician feels that he or she has abig enough window to perform the procedure. A smallretractor is then placed over the dilator to hold theviewing space open. A light source can then be placedwithin the retractor for better visualization. Thesesmall, minimally invasive retractor systems allow forthe same direct visualization of the spine as open surgery,but do so with a much smaller footprint.DevicesSpine fusion surgeries sometimes require placementof hardware such as cages, screws, plates, and rods.Cages are hardware that acts like a spacer and may bemade of metal, carbon fiber, ceramic, bone, or otherSPRING 2013 VOL. 8 No. 1materials. These devices, some of which were typicallylarge, have been redesigned by manufacturers tobe smaller so they would fit through small incisions,allowing fusion surgeries to be performed in a minimallyinvasive fashion.Intraoperative X-ray (Fluoroscopy)A minimally invasive spine surgery significantlyreduces tissue trauma, but in doing so, the ability tovisualize the spine is also greatly diminished. For this,the physician must heavily rely on specialized imageguidance during surgery. Radiographic imaging forthese surgeries is usually achieved with a C-arm x-raymachine, which gives the surgeon a 360 degree viewof the spine while performing different parts of theprocedure (Figure 1).Intraoperative NeuromonitoringWhen performing a minimally invasive spine surgery,the spine surgeon may not be able to see the specificFigure 1. Fluoroscopic (x-ray) image taken during a procedure. Thisimaging technique allows the surgeon to visualize the structures ona screen to accurately perform the minimally invasive surgery procedures.Here, the hardware seen on the right side of the imageare the retractors.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 50
SPINAL RESEARCH FOUNDATIOND.G. Orndorff et al./<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 49–55nerve anatomy below the surface of the skin. To protectthe nerves from damage during the surgery, thesurgeon uses a technique called neuromonitoring,which records the activity of the nerves that activatethe spine muscles. One of these techniques, calledelectromyogram (EMG) monitoring, assesses nerveroot function by recording muscle activity during thesurgical procedure. This gives the physician the abilityto track the nerve function and ensure the nerves areintact and protected.Bone Graft SubstituteAn important technological advance that has reducedthe invasiveness of spine surgery is the developmentof bone graft substitutes. Examples of these graftsinclude recombinant human bone morphogenic protein(BMP), which is loaded onto a sponge; demineralizedbone matrix; synthetic bone graft, often madeof ceramic; and allograft, bone from donors or cadavers.13 The bone graft substitute is placed into the discspace, generally with a cage, to promote vertebralfusion. The use of bone graft substitute avoids harvestingbone from the patient’s hip to use as a bone graftduring the spine fusion procedure. Harvesting bonefrom the patient’s hip requires an additional incisionin the hip and removal of a piece of the hip bone. Ultimately,this leads to complications and often leavespatients with persistent pain lasting at least 2 years. 14By eliminating the need to harvest bone from thepatient’s hip, bone graft substitutes have reduced theoverall invasiveness of the spine fusion surgeries.Various Minimally Invasive Spine SurgeryProceduresLumbar MicrodiscectomyThis surgery is performed on patients with herniations(bulging) of the intervertebral discs of the spine(see Figure 2 for anatomy). The chief complaint fromthese patients is usually pain (called sciatic pain orsciatica) that originates in the spine and may radiateinto the buttock(s) and down the leg(s) (see Figure 2for anatomy). Physical examinations performed byphysicians provide information that links the causeof the pain to a specific level of the spine. Imagingof the lumbar spine using fluoroscopy usuallyreveals a nerve root compression (pinched nerve) bya herniated disc (Figure 3, left panel). NonsurgicalFigure 2. Nerve root compression. Left: axial view of an intervertebral disc without nerve (shown in yellow) compression. Right: nerve root compressiondue to a herniated/damaged disk.51 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine TreatmentFigure 3. Spine fusion. This shows how two vertebrae are fused. A cage plus a bone graft substitute (BGS) is inserted in the disc space afterremoval of the disc. In this case, the two vertebrae have been secured with 2 pedicle screws linked by a rod. Left: Fluoroscopic image of thecompleted surgery (side view); the 2 screws and rod are easily spotted; note the cage in the disc space (faint vertical lines). Center: Backview of completed surgery. Right: Explanatory diagram of what is shown in the left panel. Image modified and adapted from MummaneniPV, Rodts GE Jr. The mini-open transforaminal lumbar interbody fusion. Neurosurgery. 2005;57:256–61.approaches are almost always prescribed for patientswith disc herniations; these treatments include physicaltherapy, pharmacological pain management, andspinal injections with corticosteroids. If the patient’ssymptoms do not resolve through nonsurgical care, amicrodiscectomy (also called microdecompression) isperformed microscopically to relieve pressure on thespinal nerves. During microdiscectomy, the surgeonperforms a 1-inch incision posteriorly at the level ofthe herniated disc and uses a microscope to access thespine. First, the surgeon removes a small piece of bonefrom the lamina (the bones in the back of the spine)(Figure 3, center panel); this reduces pressure on thesciatic nerve and provides access to the damageddisc below. The surgeon then removes the herniated/damaged part of the disc to relieve pressure on thenerve root (Figure 3, right panel).SPRING 2013 VOL. 8 No. 1Lumbar FusionLumbar fusion surgeries are indicated when thereis radiographic evidence of instability or deformity.Fusion procedures are necessary when nonsurgicalapproaches have failed and patients are in significantpain from conditions such as degenerative disc diseaseor recurrent disc herniations. The goal of lumbarfusion surgery is to create solid bone betweentwo adjoining vertebrae by removing the disc andfusing the two vertebrae; this eliminates any movementbetween the bones and reduces pain and nerveirritation. Generally, the damaged disc is eliminated,and the bone surfaces of adjacent vertebrae areprepared for fusion. Bone graft substitute, such asautograft, and usually a cage is inserted into the discspace. The cage acts like a spacer, and the bone graftsubstitute enhances fusion between the two adjacentvertebrae. Rods and screws are often placed betweenthe two vertebrae to provide additional support whilethe two vertebrae are becoming fused, a process thatusually takes 6 to 12 months. All these proceduresare performed using x-ray (fluoroscopic) imaging tovisualize the procedure.There are a number of minimally invasive spine surgeryprocedures that can be used to achieve the fusionof the spinal vertebrae. These techniques, describedbelow, mainly differ in the way the spine is accessedby the surgeon: through the front (lower abdomen), theback, or from the side. Consequently, these approachesmainly differ by the types of tissues or structures thatare being penetrated, resected (cut), or retracted by thesurgeon to access the spine. The characteristics of thesetechniques are summarized in Table 1.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 52
SPINAL RESEARCH FOUNDATIOND.G. Orndorff et al./<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 49–55Table 1. Characteristics of the different minimally invasive surgeries for spine fusion.Type of FusionSurgeryAccessDuration of Surgery(hours) Potential Complications Comments and ContraindicationsALIFFront (lowerabdomen)3.5 Damage to large vessels,organs, and nerves in theabdomenOnly option for patients with highiliac crestsPLIFBack(midline)3 to 6 Damage to spine musclesand their nerves; damageto duraTLIFBack (to theside of themidline)2.5 Damage to dura • May not be possible in patientswith high iliac crests;• Not indicated to fuse >3vertebraeXLIFSide (abovehip)1 to 1.5 Transient leg pain due toretraction of the psoas• Offers only limited accessto spine (L5-S1 cannot beaccessed);• Cannot be done in patientswith high iliac crestsMini-open ALIF (Anterior Lumbar InterbodyFusion). Because the intervertebral discs are on thefront side of the spine (Figure 2, left panel for anatomy),spinal fusions can be obviously achieved viaan anterior (front) approach. Anterior fusions requiremaking an incision in the lower abdomen, often cuttingthrough or splitting the abdominal muscles, anddissecting behind the abdomen to gain access to thelumbar spine. This procedure is best used when targetingthe L4-L5 or L5-S1 level. The XLIF technique(describe below) is usually recommended for fusionof the levels above L5-S1. The advantage of this procedureis that it spares the patient’s back muscles.However, the ALIF approach can result in damageto abdominal organs and structures because the surgeonhas to dissect through the abdomen and retractthese abdominal structures to reach the spine. Thesecomplications may include damage to the large bloodvessels, leading to excessive blood loss); injury tothe sympathetic plexus, causing retrograde ejaculationin men; injury to the ureters, the canals that bringurine from the kidneys to the bladder; or damage tothe intestines.Mini-open PLIF (Posterior Lumbar InterbodyFusion). In the PLIF, the surgeon accesses the spineposteriorly. A small incision is made in the middleof the back at the indicated level, and the backmuscles are split or retracted to access the spine.The lamina, which blocks access from the back,needs to be removed on both sides to allow accessto the disc, and the facet joints on both sides mayalso need to be trimmed (See Figure 2 for anatomy).The thecal sac is then retracted. The surgeonremoves the damaged disc and inserts a cage withbone graft substitute into the disc space. Rods andscrews are usually placed to further stabilize thespine. The main disadvantages of the PLIF is that itmay result in damage to back muscles and/or theirnerves, and create tears in the dura (the materialthat protects the spinal nerves), which is forcefullyretracted. The advantage of PLIF over ALIF isthat it does not damage the abdominal organs andstructures.Minimally Invasive TLIF (Transforaminal LumbarInterbody Fusion). The TLIF is a modification ofthe PLIF that has become popular. In the TLIF, the53 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013New Horizons in Spine Treatmentsurgeon approaches the spine from the back, but a littlemore to the side (about 2 inches right or left of themidline), through a small incision. The back musclesare split using a series of dilators, and the facet jointon one side only is removed. 16 The rest of the procedureis similar to the PLIF; in comparison, the lateral(side) entry used in the TLIF minimizes the retractionof the nerve root and the dura, reducing the risk ofnerve injury. The TLIF also reduces the amount oftrauma to the back muscles. However, there is still arisk for damaging the dura.XLIF (Extreme Lateral Interbody Fusion). Thisrelatively new procedure uses a lateral (side) approachto access the lumbar spine above the L5-S1level. 18 A small incision is made on the flank of thepatient (just above the hip), and sometimes anothersmall incision (1-inch long) is made just behind thefirst incision. The dilators are passed behind the abdominalcontents (retroperitoneal) and through thehip flexor muscle (psoas) to gain access of the spine.The rest of the procedure is typical of a fusion surgery.The lateral approach avoids the vascular, visceral,and sexual dysfunction complications thatmay be associated with anterior approaches (ALIF),as well as the possible nerve damage and dural tearthat may occur with posterior approaches (PLIF). 7One potential, yet minor complication of the XLIFis transient leg pain or weakness due to retraction ofthe psoas muscle to access the spine. 7 Nevertheless,the lateral approach has an important limitation: theL5-S1 disc, a very common level of surgery, is situatedtoo low to be safely accessed using the lateralapproach due to the obstruction of the pelvis and thevasculature.The reasons for performing one approach versusanother include particular patient anatomy and surgeonexpertise and preference. Regarding patient anatomy,the lateral approach may not be possible in patientswith a “low riding” L4-L5 level and is contraindicatedat L5-S1. The XLIF, and sometimes TLIF, may not begood options in patients whose iliac crest is high andblocks the passage from a lateral approach; in thosepatients the only method for accessing the spine isfrom the front (ALIF).SPRING 2013 VOL. 8 No. 1ConclusionMinimally invasive techniques for spine surgery wereinitiated in the 1980’s and have evolved and improvedin the past 3 decades thanks to technical innovations.Such advances include better imaging techniques (suchas fluoroscopy), dilators, smaller retractors, neuromonitoring,and bone graft substitutes. Today, minimallyinvasive surgery techniques are considered as effectiveas open surgery techniques to repair the spine. Themain reason for using minimally invasive techniques isto minimize the trauma to tissues during surgery, whichtypically results in fewer complications, less pain, lesstime spent in the hospital, and faster recovery, all ofwhich are very important outcomes for patients. Therefore,minimally invasive techniques have become thestate of the art in back surgery and have replaced opensurgeries, whenever it is feasible.Now, virtually all levels of the spine can be accessedthrough minimally invasive approaches, makingit amenable for use in an increasing number ofpatients and an increasing number of back problems.Skilled surgeons are now able to use minimally invasiveapproaches to treat complex disorders, includingtumors, deformity, infection, and trauma. 11 Nevertheless,not all types of surgeries can be performed throughminimally invasive techniques, and some patients maynot be good candidates for minimally invasive spinesurgery. Moreover, in some cases, the disadvantagesof the minimally invasive approach may counteract itsadvantages, making open surgery a better option.Several types of minimally invasive approachesare available for spinal fusion surgery. These variousapproaches mainly differ by the way the surgeon accessesthe spine to perform the surgery. The choice ofthe appropriate approach for surgery mainly dependson the patient’s anatomy and the surgeon’s expertiseand preference. Regardless of the approach chosen tomanage a patient with a spine injury or disorder, thegoal of the treatment is always to prevent the developmentof a neurologic deficit, enhance neurologicrecovery, achieve a stable spine that will allow for appropriaterehabilitation, and prevent post-surgical deformityand pain.<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 54
SPINAL RESEARCH FOUNDATIOND.G. Orndorff et al./<strong>Journal</strong> of the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 8 (2013) 49–55REFERENCES1. Deyo RA, Mirza SK, Martin BI. Back pain prevalence andvisit rates: estimates from U.S. national surveys, 2002. Spine2006;31:2724–7.2. Adogwa O, Parker SL, Bydon A, et al. Comparative effectivenessof minimally invasive versus open transforaminal lumbarinterbody fusion: 2-year assessment of narcotic use, return towork, disability and quality of life. J <strong>Spinal</strong> Disord Tech 2011;24:479–84.3. Parker SL, Lerner J, McGirt MJ. Effect of minimally invasivetechnique on return to work and narcotic use following transforaminallumbar inter-body fusion: a review. Prof Case Manag2012;17:229–35.4. Lucio JC, Vanconia RB, Deluzio KJ, et al. Economics of lessinvasive spinal surgery: an analysis of hospital cost differencesbetween open and minimally invasive instrumented spinalfusion procedures during the perioperative period. Risk ManagHealthc Policy 2012;5:65–74.5. McGirt MJ, Parker SL, Lerner J, et al. Comparative analysisof perioperative surgical site infection after minimally invasiveversus open posterior/ transforaminal lumbar interbodyfusion: analysis of hospital billing and discharge data from 5170patients. J Neurosurg Spine 2011;14:771–8.6. Kawaguchi Y, Matsui H, Tsuji H. Back muscle injury after posteriorlumbar spine surgery. Part 2: histologic and histochemicalanalyses in humans. Spine 1994;19:2598–602.7. Youssef JA, McAfee PC, Patty CA, et al. Minimally invasivesurgery: lateral approach interbody fusion: results and review.Spine 2010;35:S302–11.8. Whitecloud TS 3rd, Castro FP Jr, Brinker MR, et al. Degenerativeconditions of the lumbar spine treated with intervertebraltitanium cages and posterior instrumentation for circumferentialfusion. J <strong>Spinal</strong> Disord 1998;11:479–86.9. Mannion RJ, Guilfoyle MR, Efendy J, et al. Minimally InvasiveLumbar Decompression Long-term outcome, morbidity andthe learning curve from the first 50 cases. J <strong>Spinal</strong> Disord Tech2012;25:47–51.10. Slosar PJ. Minimally invasive spine surgery: An evolution inprogress. J Spine Res Found 2010;5:26–31.11. Gomez JA, Ludwig SC. Minimally invasive techniques for thoracolumbarspine trauma. Contemp Spine Surg 2012;131:7.12. Mikhael MM, Celestre PC, Wolf CF, et al. Minimally invasivecervical spine foraminotomy and lateral mass screw placement.Spine 2012;37 E318–E22.13. Grabowski G, Cornett CA. Bone graft and bone graft substitutesin spine surgery: current concepts and controversies. J Am AcadOrthop Surg 2013 Jan;21:51–60.14. Sasso RC, LeHuec JC, Shaffrey C; Spine Interbody <strong>Research</strong>Group. Iliac crest bone graft donor site pain after anterior lumbarinterbody fusion: a prospective patient satisfaction outcomeassessment. J <strong>Spinal</strong> Disord Tech 2005;18:S77–81.15. Lee SH, Choi WG, Lim SR, et al. Minimally invasive anteriorlumbar interbody fusion followed by percutaneous pediclescrew fixation for isthmic spondylolisthesis. Spine J 2004;4:644–9.16. Mummaneni PV, Rodts GE Jr. The mini-open transforaminallumbar interbody fusion. Neurosurgery 2005;57:256–61.17. Habib A, Smith ZA, Lawton CD, et al. Minimally invasivetransforaminal lumbar interbody fusion: a perspective on currentevidence and clinical knowledge. Minim Invasive Surg2012;2012:657342.18. Ozgur BM, Aryan HE, Pimenta L, et al. Extreme Lateral InterbodyFusion (XLIF): a novel surgical technique for anteriorlumbar interbody fusion. Spine J 2006;6:435–43.Douglas G. Orndorff, M.D.Dr. Orndorff is a board-certified orthopedicsurgeon with Spine Colorado. Hisspecial interests include motion preservationsurgery, cervical and lumbar degenerativeand trauma conditions, spinaldeformity, and the treatment of spinaltumors. Dr. Orndorff completed his undergraduatestudies at the University of Denver. He earnedhis medical degree at the University of Colorado School ofMedicine. He completed his internship in General Surgeryand his residency in Orthopaedic Surgery at the Universityof Virginia. He completed a fellowship in spine surgery at theUniversity of Wisconsin. Dr. Orndorff’s professional objectivesare to practice comprehensive orthopaedic and spinalsurgery within the Four Corners community and to be activelyinvolved in academic research and education. Dr. Orndorffis a member of the North American Spine Society, the AO/ASIF International Spine Society and a Member of the AmericanAcademy of Orthopaedic Surgery. Dr. Orndorff is a passionategolfer and an avid outdoorsman who enjoys skiing,mountain biking, cycling and fly-fishing. He and his wife havethree children.55 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
SPRING 2013<strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> <strong>Research</strong> PartnersThe <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> has named 25 <strong>Research</strong> Partners across the countrythat share one core mission: improving spinal health care through research, education,and patient advocacy. These centers offer the best quality spinal health care whilefocusing on research programs designed to advance spinal treatments and techniques.★★★★Allegheny Brain and Spine SurgeonJames P. Burke, MD, PhD201 Howard Ave, Building E-1Altoona, PA 16601814-946-9150centralpabrainandspinesurgeons.comAtlanta Brain and Spine CareRegis W. Haid, Jr., MD2001 Peachtree Rd, NE, Ste 575Atlanta, GA 30309404-350-0106atlantabrainandspine.comColorado ComprehensiveSpine InstituteGeorge A. Frey, MD3277 South Lincoln StEnglewood, CO 80113303-762-0808coloradospineinstitute.comThe Hughston ClinicJ. Kenneth Burkus, MD6262 Veterans ParkwayColumbus, GA 31909706-324-6661hughston.comIndiana Spine GroupRick C. Sasso, MD13225 N. Meridian StCarmel, IN 46032317-228-7000indianaspinegroup.comInova <strong>Research</strong> CenterZobair M. Younossi, MD, MPH3300 Gallows RdFalls Church, VA 22042703-776-2580Menlo Medical ClinicAllan Mishra, MD1300 Crane StMenlo Park, CA 94025650-498-6500MUSC Darby Children’s<strong>Research</strong> InstituteInderjit Singh, PhD59 Bee St, MSC 201Charleston, SC 294251-800-424-MUSCNew England NeurosurgicalAssociates, LLCChristopher H. Comey, MD300 Carew St, Ste One<strong>Spring</strong>field, MA 01104413-781-2211SPRING 2013 VOL. 8 No. 1<strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 56
SPINAL RESEARCH FOUNDATIONOregon Neurosurgery SpecialistsRobert J. Hacker, MDAndrea Halliday, MD3355 RiverBend Dr, Ste 400<strong>Spring</strong>field, OR 97477541-686-8353oregonneurosurgery.comThe Orthopaedic and SportsMedicine CenterGerard J. Girasole, MD888 White Plains RdTrumbull, CT 06611203-268-2882osmcenter.comMidwest Orthopaedic CenterPatrick T. O’Leary, MDDaniel S. Mulconrey, MD6000 North Allen RoadPeoria, IL 61614(309) 691-1400midwest-ortho.comPrinceton Brain and Spine CareMark R. McLaughlin, MD, FACS1203 Langhorne-Newtown Rd, Ste 138Langhorne, PA 19047215-741-3141princetonbrainandspine.comRiver City Orthopaedic SurgeonsDavid P. Rouben, MD9300 Stonestreet Rd, Ste 200Louisville, KY 40272502-935-8061rivercityortho.comThe Orthopedic Center of St. LouisMatthew F. Gornet, MD14825 N. Outer Forty Rd, Ste 200Chesterfield, MO 63017314-336-2555toc-stl.comSouth Coast Orthopaedic AssociatesAleksandar Curcin, MD, MBA2699 N. 17th StCoos Bay, OR 97420541-266-3600scoastortho.comThe Spine Clinic of Los AngelesLarry T. Khoo, MD1245 Wilshire Blvd, Ste 717Los Angeles, CA 90017213-481-8500spineclinicla.comSouthern Brain and SpineNajeeb M. Thomas, MD4228 Houma Blvd, Ste 510Metairie, LA 70006504-889-7200sbsdocs.netSpineCare Medical GroupPaul J. Slosar, Jr., MDSan Francisco Spine Institute1850 Sullivan AveDaly City, CA 94015650-985-7500spinecare.comRutgers UniversityDepartment of Biomedical EngineeringNoshir A. Langrana, PhD, PE599 Taylor RdPiscataway, NJ 08854732-445-4500Spine ColoradoJim A. Youssef, MDDouglas G. Orndorff, MD1 Mercado St, Ste 100Durango, CO 81301970-375-3697spinecolorado.comTwin Cities Spine CenterJames D. Schwender, MD913 East 26th St, Ste 600Minneapolis, MN 55404612-775-6200tcspine.comUniversity of Minnesota MedicalCenter, FairviewDavid W. Polly, Jr., MD2450 Riverside Ave, SouthMinneapolis, MN 55454612-672-7575The Virginia Spine InstituteThomas C. Schuler, MD, FACSBrian R. Subach, MD, FACS1831 Wiehle AveReston, VA 20190703-709-1114spinemd.comVirginia Therapy & Fitness CenterRichard A. Banton, PT, DPT, ATCE. Larry Grine, PT, MSPT, ATC, CSCS1831 Wiehle AveReston, VA 20190703-709-1116vtfc.com57 <strong>Journal</strong> of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> SPRING 2013 VOL. 8 No. 1
“It is our dedication to continuousimprovement, innovation, and leadershipthat has led to many significant advanceswhich have helped to revolutionize spinalhealth care. The knowledge gained fromthis research empowers us to better serveour patients. Improving lives is ourmost important purpose!”SPINALHEROThomas C. Schuler, M.D., F.A.C.S.CEO/Founder, The Virginia Spine InstitutePresident, The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> recognizes ouroutstanding clinicians and researchers in thefield of spine research and profiles them as <strong>Spinal</strong> Heroes. Thesededicated spine care professionals embrace excellence in bothresearch and education, contributing significantly to improvementsin the diagnosis and treatment of spinal disorders. Werecognize Thomas C. Schuler, M.D., F.A.C.S., as a <strong>Spinal</strong> Hero.
Thank You!The Board of Directors of The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>is grateful for the continued investment of our donors andextends its appreciation to all who have contributed.<strong>Research</strong>Through the generous support of our donors, The <strong>Spinal</strong><strong>Research</strong> <strong>Foundation</strong> has been able to signifi cantly expandthe scope of our scientifi c research and educational programs.These gifts have been utilized to embark on projects gearedtoward understanding the mechanism of spinal diseases anddeveloping new treatments for these conditions. This workwould not be possible without the support of our donors.EducationPatient AdvocacyTo make a donation in order to improve the quality of spinalhealth care in America, please visit:www.SpineRF.orgor contact us at:<strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong>1831 Wiehle Ave, Ste 100Reston, VA 20190Phone: 703-766-5405Fax: 703-709-1397Innovation