Outpatient Competency Restoration - Hogg Foundation for Mental ...
Outpatient Competency Restoration - Hogg Foundation for Mental ...
Outpatient Competency Restoration - Hogg Foundation for Mental ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
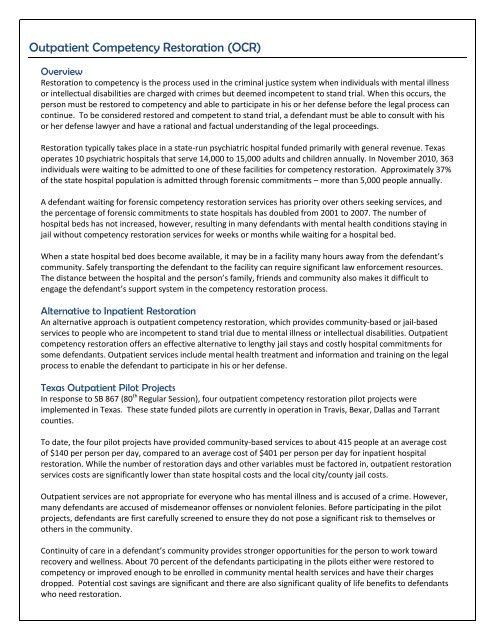
<strong>Outpatient</strong> <strong>Competency</strong> <strong>Restoration</strong> (OCR)Overview<strong>Restoration</strong> to competency is the process used in the criminal justice system when individuals with mental illnessor intellectual disabilities are charged with crimes but deemed incompetent to stand trial. When this occurs, theperson must be restored to competency and able to participate in his or her defense be<strong>for</strong>e the legal process cancontinue. To be considered restored and competent to stand trial, a defendant must be able to consult with hisor her defense lawyer and have a rational and factual understanding of the legal proceedings.<strong>Restoration</strong> typically takes place in a state-run psychiatric hospital funded primarily with general revenue. Texasoperates 10 psychiatric hospitals that serve 14,000 to 15,000 adults and children annually. In November 2010, 363individuals were waiting to be admitted to one of these facilities <strong>for</strong> competency restoration. Approximately 37%of the state hospital population is admitted through <strong>for</strong>ensic commitments – more than 5,000 people annually.A defendant waiting <strong>for</strong> <strong>for</strong>ensic competency restoration services has priority over others seeking services, andthe percentage of <strong>for</strong>ensic commitments to state hospitals has doubled from 2001 to 2007. The number ofhospital beds has not increased, however, resulting in many defendants with mental health conditions staying injail without competency restoration services <strong>for</strong> weeks or months while waiting <strong>for</strong> a hospital bed.When a state hospital bed does become available, it may be in a facility many hours away from the defendant’scommunity. Safely transporting the defendant to the facility can require significant law en<strong>for</strong>cement resources.The distance between the hospital and the person’s family, friends and community also makes it difficult toengage the defendant’s support system in the competency restoration process.Alternative to Inpatient <strong>Restoration</strong>An alternative approach is outpatient competency restoration, which provides community-based or jail-basedservices to people who are incompetent to stand trial due to mental illness or intellectual disabilities. <strong>Outpatient</strong>competency restoration offers an effective alternative to lengthy jail stays and costly hospital commitments <strong>for</strong>some defendants. <strong>Outpatient</strong> services include mental health treatment and in<strong>for</strong>mation and training on the legalprocess to enable the defendant to participate in his or her defense.Texas <strong>Outpatient</strong> Pilot ProjectsIn response to SB 867 (80 th Regular Session), four outpatient competency restoration pilot projects wereimplemented in Texas. These state funded pilots are currently in operation in Travis, Bexar, Dallas and Tarrantcounties.To date, the four pilot projects have provided community-based services to about 415 people at an average costof $140 per person per day, compared to an average cost of $401 per person per day <strong>for</strong> inpatient hospitalrestoration. While the number of restoration days and other variables must be factored in, outpatient restorationservices costs are significantly lower than state hospital costs and the local city/county jail costs.<strong>Outpatient</strong> services are not appropriate <strong>for</strong> everyone who has mental illness and is accused of a crime. However,many defendants are accused of misdemeanor offenses or nonviolent felonies. Be<strong>for</strong>e participating in the pilotprojects, defendants are first carefully screened to ensure they do not pose a significant risk to themselves orothers in the community.Continuity of care in a defendant’s community provides stronger opportunities <strong>for</strong> the person to work towardrecovery and wellness. About 70 percent of the defendants participating in the pilots either were restored tocompetency or improved enough to be enrolled in community mental health services and have their chargesdropped. Potential cost savings are significant and there are also significant quality of life benefits to defendantswho need restoration.
FY 2009-2010 Statistics: SB 867 <strong>Outpatient</strong> <strong>Competency</strong> <strong>Restoration</strong> Pilot Projects(Bexar, Travis, Dallas, and Tarrant Counties)Average Cost of <strong>Restoration</strong>Average CostType of <strong>Restoration</strong> Per Person, Per DayAverage Lengthof StayAverage Total Cost of <strong>Restoration</strong>Per PersonState Psychiatric Facility $401 1 89 days 2 $35,689 3OCR Pilots $140 4 102 Days 5 $14,280Return on Investment (ROI)ROI Formula: ROI = (Return / Investment) x 100ROI Definitions: Return = Costs Avoided; Investment = Dollars AppropriatedFour OCR pilot projects funded by an investment of $3 million in FY 2009 – 2010 (18 months) have served 415individuals through FY 2010 at a cost of $500,000 per site annually. (Sixty percent of these individuals werecharged with misdemeanors, 40% were charged with non-violent felonies.) Approximate cost of restoration of 415 individuals in state hospitals: $14,810,935(415 x $35,689 = $14,810,935) Approximate cost of restoration of 415 individuals using OCR: $5,926,200(415 x $14,280 = $5,926,200) Total costs averted <strong>for</strong> restoration of 415 individuals using OCR: $8,884,735($14,810,935 - $5,926,200 = $8,884,735) ROI <strong>for</strong> OCR Pilots = (8,884,735 / 3,000,000) x 100 = 296%Every dollar spent <strong>for</strong> OCR averted approximately $2.96 in state hospital costs.Using this ROI <strong>for</strong>mula, a $10 million investment in four existing and six additional OCR pilot sites could producean estimated $29.6 million in costs averted, generating savings of more than $19.6 million <strong>for</strong> the biennium. 6For More In<strong>for</strong>mation Contact:Colleen Horton, Policy Program Officer Sarah Kidder, Policy Fellow Dennis Borel, Executive Director<strong>Hogg</strong> <strong>Foundation</strong> <strong>for</strong> <strong>Mental</strong> Health <strong>Hogg</strong> <strong>Foundation</strong> <strong>for</strong> <strong>Mental</strong> Health Coalition of Texans with Disabilitiescolleen.horton@austin.utexas.edu sarah.kidder@austin.utexas.edu dborel@cotwd.org(512) 471-2988 (512) 471-7627 (512) 478-3361 Health and Human Services Commission, Department of State Health Services, State Hospitals Section, 2010 Management Plan StatewidePer<strong>for</strong>mance Indicators, 4th Quarter FY 2010, Measure 1A - Average Cost Per Patient Served.2 Health and Human Services Commission, Department of State Health Services, Continuity of Care Task Force, PowerPoint presentation onMarch 26, 2010.3 Note: These costs do not include the cost of time spent in a local jail waiting <strong>for</strong> a hospital bed. The length of wait in jails <strong>for</strong> a <strong>for</strong>ensichospital bed varies from 72 days to 6 months, according to the Texas Public Policy <strong>Foundation</strong>. <strong>Outpatient</strong> community restoration also wouldreduce local jail costs.4 Texas Department of State Health Services, December 8, 2010. In<strong>for</strong>mation provided to the <strong>Hogg</strong> <strong>Foundation</strong> <strong>for</strong> <strong>Mental</strong> Health.5 Ibid.6 Note: Actual savings likely are higher because the data available to date is <strong>for</strong> less than the full 2009/2010 biennium due to start-up time.January 15 th , 2011