Treatment of a, dermal fungal infection, complicated by a ... - Cutimed
Treatment of a, dermal fungal infection, complicated by a ... - Cutimed
Treatment of a, dermal fungal infection, complicated by a ... - Cutimed
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
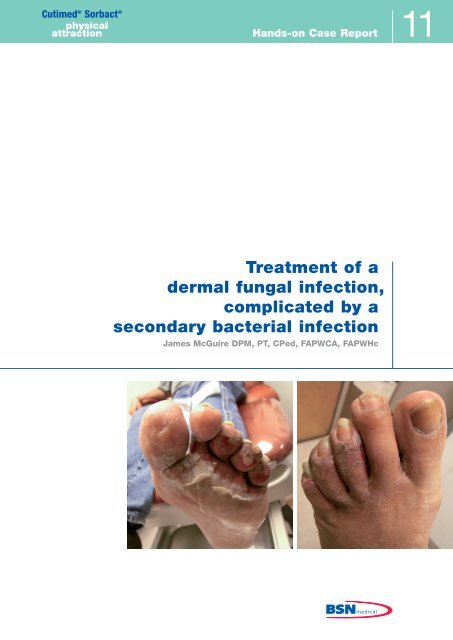
<strong>Cutimed</strong> ® Sorbact ®physicalattraction Hands-on Case Report 11<strong>Treatment</strong> <strong>of</strong> a,<strong>dermal</strong> <strong>fungal</strong> <strong>infection</strong>,<strong>complicated</strong> <strong>by</strong> a,secondary bacterial <strong>infection</strong>,James McGuire DPM, PT, CPed, FAPWCA, FAPWHc
2<strong>Treatment</strong> <strong>of</strong> a <strong>dermal</strong> <strong>fungal</strong> <strong>infection</strong>,<strong>complicated</strong> <strong>by</strong> a secondary bacterial<strong>infection</strong> using a novel hydrophobicdressingJAMES MCGUIREDPM, PT, CPED, FAPWCA, FAPWHCIntroductionPedal <strong>dermal</strong> <strong>fungal</strong> <strong>infection</strong>s are traditionallytreated using a combination <strong>of</strong> drying agents, anti<strong>fungal</strong>powders, creams or gels and if necessary anoral anti<strong>fungal</strong> agent. Frequently these <strong>infection</strong>sare <strong>complicated</strong> <strong>by</strong> local tissue inflammation fromthe destruction <strong>of</strong> <strong>fungal</strong> and bacterial cells andsecondary invasion <strong>of</strong> bacteria from resident skinflora in the intertrigenous spaces. The resulting cellulitisnecessitates the addition <strong>of</strong> an antibiotic toaddress the invasion <strong>of</strong> bacteria from the denudedinterspaces. In order to promote drying <strong>of</strong> the skinand resolution <strong>of</strong> the <strong>infection</strong>, interdigital spacers<strong>of</strong> foam, gauze or lamb’s wool are used to promoteairflow between the toes.<strong>Cutimed</strong> ® Sorbact ® , a unique hydrophobic dressingmaterial, has been demonstrated in a number <strong>of</strong>cases to help in the treatment <strong>of</strong> surface <strong>fungal</strong><strong>infection</strong>s <strong>by</strong> reducing the number <strong>of</strong> propagatingmicrobes on the surface <strong>of</strong> the skin there<strong>by</strong> allowingthe body’s own defenses to gain the upper handin suppressing the spread <strong>of</strong> the fungus in thetissues.¹Microbes, including fungi, are irreversibly boundthrough hydrophobic interaction to the DACC(dialkylcarbamoylchloride) fatty acid coating on thedressing surface, allowing them to be disposed <strong>of</strong>at dressing changes. This unique wound dressing,without a chemically active agent but with a uniquemode <strong>of</strong> action, can contribute to the healing <strong>of</strong>mycotic <strong>infection</strong>s <strong>of</strong> the feet.Patient history55 year old Hispanic male with Type I Diabetes presentedto the wound center with a severely ulceratedforefoot. He was initially seen <strong>by</strong> his PCP who placedhim on Econazole nitrate cream and daily warm saltsoaks for one week for what was diagnosed as atinea pedis <strong>infection</strong> <strong>of</strong> the 2nd and 3rd interspaces<strong>of</strong> the left foot. The cream was applied manually andoccluded with a DSD twice daily with once dailysoaks with Epsom salts and warm water. This resultedin a spread <strong>of</strong> the <strong>infection</strong> to all the interspacesduring the course <strong>of</strong> the next week with bullae formationand a marked loss <strong>of</strong> skin, increase in edema,ascending cellulitis, and pain.He eventually went to the ER where he was diagnosedas having an allergic reaction to the Econazole.The Econazole cream was discontinued and he wasplaced on Silvadene cream and plain dry dressingswhile he worked during the day, and Epsom saltsoaks at night, leaving the toes open while he slept.He failed to progress and sought the advice <strong>of</strong> alocal podiatric physician who felt he had developeda secondary bacterial cellulitis. He took cultures <strong>of</strong>the open areas and started him on Bactrim DS witha continuation <strong>of</strong> the Silvadene cream and drysterile dressings. He referred him to the woundcenter at his institution for follow up and managementone week later.<strong>Cutimed</strong> ® Sorbact ® , which is available in severalvariants (e.g., ribbon gauze, swabs, wound contactlayer, etc.), appears to present a genuine alternativeto conventional antimycotic therapies in the treatment<strong>of</strong> <strong>fungal</strong> <strong>infection</strong>s. In addition to neutralizingthe effect <strong>of</strong> the microbes, the <strong>fungal</strong> and bacterialpathogens present in the interspaces are notexpected to develop resistance to the dressings’mode <strong>of</strong> action.
3<strong>Treatment</strong> historyWhen he presented to the wound center he wasstill inflamed, painful, and draining with only a slightreduction in the advance <strong>of</strong> the cellulitis from theBactrim DS and a strong odor emanating from thefoot (Fig 1,2). The culture and sensitivity performedat the initial visit came back positive for StaphylococcusAureus sensitive to Bactrim and Pseudomonasaeruginosa sensitive to Cipr<strong>of</strong>loxacin with<strong>fungal</strong> elements noted. X-rays were taken to ruleout osteomyelitits. He was diagnosed as having asevere tinea pedis with a secondary cellulitis frombacterial invasion into the denuded areas in theinterspaces <strong>complicated</strong> <strong>by</strong> continuous occlusionwith creams and repeated soaking.Fig. 1The Bactrim was continued and he was started onCipr<strong>of</strong>loxacin and the use <strong>of</strong> <strong>Cutimed</strong> ® Sorbact ®ribbon gauze to all the interspaces changed daily.He was also placed in a surgical shoe and told tostay <strong>of</strong>f his feet. The following week Trychophytonrubrum was identified as the <strong>fungal</strong> agent. After oneweek using the <strong>Cutimed</strong> ® Sorbact ® ribbon gauze hispain and the odor had almost completely resolved(1/10) and he had little or no drainage from the interspaces(Figure 3).There was only a small open area that remained inthe 3rd interspace, with almost complete resolution<strong>of</strong> the active scaling and discoloration dorsally.<strong>Treatment</strong> with <strong>Cutimed</strong> ® Sorbact ® ribbon gauzewas continued for the next week with completehealing <strong>of</strong> the open areas. In time, resolution <strong>of</strong> thehemosiderosis and exfoliation <strong>of</strong> the peeling skinwould complete the healing process (Figure 4).ConclusionMaceration and occlusion <strong>of</strong> bacteria and fungi inbetween skin folds and in the interdigital areas onthe foot provides the perfect environment for rapidproliferation <strong>of</strong> the organisms. Seclusion <strong>of</strong> the footin a closed toe shoe during much <strong>of</strong> the day makesmatters worse and further exacerbates developing<strong>infection</strong>s <strong>of</strong> the foot. The dressing material <strong>of</strong> <strong>Cutimed</strong> ®Sorbact ® ribbon gauze, <strong>by</strong> virtue <strong>of</strong> its DACC (dialkylcarbamoyl-chloride)coating, is able to irreversiblybind microbes with cell-surface hydrophobicity (CSH)and remove them from active interaction with the hosttissues. Physically binding actively dividing bacteriawithout killing the microbes not only reduces thesheer numbers <strong>of</strong> microbes but also decreases theamount <strong>of</strong> inflammatory bacterial and <strong>fungal</strong> debristhat accumulates from cell death created <strong>by</strong> antibioticand anti<strong>fungal</strong> topical or oral medications.Fig. 2Fig. 3By providing a dry environment, eliminating intenseinflammation created <strong>by</strong> antigenic cellular debrisas well as decreasing cell numbers, the dressing isable to decrease pain and odor while allowing thetissues to heal without topical antiinfective agents.References1. Claesson M, Bulgakow B, Blomqvist P,Andersson K (Sweden). A promising alternative inthe treatment <strong>of</strong> <strong>dermal</strong> <strong>fungal</strong> <strong>infection</strong>s. Firstpublished in "Medizin & Praxis". 2006, Germany.Fig. 4
4AuthorJames McGuire DPM, PT, CPed, FAPWCA, FAPWHcTemple University, Leonard S. Abrams Center for Advanced Wound Healing, Foot and Ankle Institute at theSchool <strong>of</strong> Podiatric Medicine, 1801 N. Broad Street, Philadelphia, PA 19122, U.S.A.Temple University, Department <strong>of</strong> Podiatric Medicine and Orthopedics at the Temple University School <strong>of</strong>Podiatric Medicine, 1801 N. Broad Street, Philadelphia, PA 19122, U.S.A.70550-00545-01 08/2012