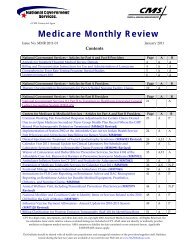
- Page 1 and 2: SUPPLIERDME MAC JURISDICTION CMANUA
- Page 3: Chapter One √Introduction
- Page 7: Introduction Chapter 1A Medicare ca
- Page 10 and 11: Introduction Chapter 1Freedom of In
- Page 12 and 13: Supplier Enrollment Chapter 2Overvi
- Page 14 and 15: Supplier Enrollment Chapter 2Each D
- Page 16 and 17: Supplier Enrollment Chapter 2those
- Page 18 and 19: Supplier Enrollment Chapter 2Do Not
- Page 20: Supplier Enrollment Chapter 2answer
- Page 23 and 24: Supplier Enrollment Chapter 2Suppli
- Page 25 and 26: Supplier Documentation Chapter 3Gen
- Page 27 and 28: Supplier Documentation Chapter 3des
- Page 29 and 30: Supplier Documentation Chapter 3K08
- Page 31 and 32: Supplier Documentation Chapter 3E26
- Page 33 and 34: Supplier Documentation Chapter 3Sup
- Page 35 and 36: Supplier Documentation Chapter 3Med
- Page 37: Supplier Documentation Chapter 3Mis
- Page 41 and 42: Supplier Documentation Chapter 3per
- Page 43 and 44: Supplier Documentation Chapter 3Exa
- Page 45 and 46: Chapter Four √Certificates of Med
- Page 49 and 50: CMNs Chapter 4Suppliers and physici
- Page 51 and 52: CMNs Chapter 4Evidence of Medical N
- Page 53 and 54: CMNs Chapter 4blood gas study on th
- Page 55 and 56: CMNs Chapter 4The request for recer
- Page 57 and 58: CMNs Chapter 4Not all requirements
- Page 59 and 60: CMNs Chapter 4Plan, or hospice and
- Page 61 and 62: DMEPOS Fee Schedule Chapter 5DMEPOS
- Page 63 and 64: DMEPOS Fee Schedule Chapter 5Artifi
- Page 65 and 66: DMEPOS Fee Schedule Chapter 5A new
- Page 67 and 68: DMEPOS Fee Schedule Chapter 5items
- Page 69 and 70: DMEPOS Fee Schedule Chapter 5QE Use
- Page 71 and 72: DMEPOS Fee Schedule Chapter 54. Own
- Page 73 and 74: DMEPOS Fee Schedule Chapter 5lifeti
- Page 75 and 76: DMEPOS Fee Schedule Chapter 5For ca
- Page 77 and 78: DMEPOS Fee Schedule Chapter 58. The
- Page 79 and 80: Claim Submission Chapter 6Mandatory
- Page 81 and 82: Claim Submission Chapter 6Suppliers
- Page 83 and 84: Claim Submission Chapter 6addition
- Page 85 and 86: Claim Submission Chapter 6upgrade.
- Page 87 and 88: Claim Submission Chapter 654 Interm
- Page 89 and 90:
Claim Submission Chapter 6to defaul
- Page 91 and 92:
Claim Submission Chapter 6in the NA
- Page 93 and 94:
Claim Submission Chapter 6NOTE: Thi
- Page 95 and 96:
Claim Submission Chapter 6Item 17b
- Page 97 and 98:
Claim Submission Chapter 6When a ph
- Page 99 and 100:
Claim Submission Chapter 6• Simpl
- Page 101 and 102:
Claim Submission Chapter 6Beneficia
- Page 103 and 104:
Claim Submission Chapter 6The diffe
- Page 105 and 106:
Chapter Seven √Crossover Claims
- Page 107 and 108:
Crossover Claims Chapter 7• The w
- Page 109 and 110:
Chapter Eight √Electronic Data In
- Page 111 and 112:
Electronic Data Interchange (EDI) C
- Page 113 and 114:
Electronic Data Interchange (EDI) C
- Page 115 and 116:
Coverage and Medical Policy Chapter
- Page 117 and 118:
Coverage and Medical Policy Chapter
- Page 119 and 120:
Coverage and Medical Policy Chapter
- Page 121 and 122:
Coverage and Medical Policy Chapter
- Page 123 and 124:
Coverage and Medical Policy Chapter
- Page 125 and 126:
Pricing Chapter 10PricingThe Medica
- Page 127 and 128:
Pricing Chapter 102006, is arrayed
- Page 129 and 130:
Pricing Chapter 10equipment that we
- Page 131 and 132:
Coordination of Benefits Chapter 11
- Page 133 and 134:
Coordination of Benefits Chapter 11
- Page 135 and 136:
Coordination of Benefits Chapter 11
- Page 137 and 138:
Coordination of Benefits Chapter 11
- Page 139 and 140:
Coordination of Benefits Chapter 11
- Page 141 and 142:
Coordination of Benefits Chapter 11
- Page 143 and 144:
Chapter Twelve √Overpayments
- Page 145 and 146:
Overpayments and Refunds Chapter 12
- Page 147 and 148:
Overpayments and Refunds Chapter 12
- Page 149 and 150:
Inquiries and Appeals Chapter 13Tel
- Page 151 and 152:
Inquiries and Appeals Chapter 13In
- Page 153 and 154:
Inquiries and Appeals Chapter 13(Ju
- Page 155 and 156:
Inquiries and Appeals Chapter 13Add
- Page 157 and 158:
Inquiries and Appeals Chapter 13Cle
- Page 159 and 160:
Chapter Fourteen √Fraud and Abuse
- Page 161 and 162:
Fraud and Abuse Chapter 14pre- and
- Page 163 and 164:
Fraud and Abuse Chapter 14Abuse tak
- Page 165 and 166:
Fraud and Abuse Chapter 14Protect Y
- Page 167 and 168:
Resources Chapter 15ResourcesThe fo
- Page 169 and 170:
Resources Chapter 15Advance Determi
- Page 171 and 172:
Resources Chapter 15The supplier en
- Page 173 and 174:
Resources Chapter 15Medicare Covera
- Page 175 and 176:
Coding Chapter 16The Statistical An
- Page 177 and 178:
Coding Chapter 161/1/2003)BO Orally
- Page 179 and 180:
Coding Chapter 16KNKOKPKQKRKSKTRepl
- Page 181 and 182:
Chapter Seventeen √Symptoms Outpu
- Page 183 and 184:
System Outputs Chapter 17the remit.
- Page 185 and 186:
System Outputs Chapter 171003 INV P
- Page 187 and 188:
Chapter Eighteen √Acronyms and Ab
- Page 189 and 190:
Acronyms and Abbreviations Chapter
- Page 191 and 192:
HCPCSAppendix ALevel II HCPCS Codes
- Page 193 and 194:
HCPCSAppendix AA4236 Replacement ba
- Page 195 and 196:
HCPCSAppendix AA4332 Lubricant, ind
- Page 197 and 198:
HCPCSAppendix A(Eff. Date 1/1/2000)
- Page 199 and 200:
HCPCSAppendix AA4423 Ostomy pouch,
- Page 201 and 202:
HCPCSAppendix A1/1/2003) (Deleted e
- Page 203 and 204:
HCPCSAppendix A11/1/1996)A4631 Repl
- Page 205 and 206:
HCPCSAppendix Adialysis (Eff. Date
- Page 207 and 208:
HCPCSAppendix AA4930 Gloves, steril
- Page 209 and 210:
HCPCSAppendix Ashoe (Eff. Date 1/1/
- Page 211 and 212:
HCPCSAppendix AdressingA6218 Gauze,
- Page 213 and 214:
HCPCSAppendix AA6257 Transparent fi
- Page 215 and 216:
HCPCSAppendix AA6445 Conforming ban
- Page 217 and 218:
HCPCSAppendix A(Eff. Date 1/1/2006)
- Page 219 and 220:
HCPCSAppendix AA7037 Tubing used wi
- Page 221 and 222:
HCPCSAppendix A(Deleted eff. 12/31/
- Page 223 and 224:
HCPCSAppendix AB4104 Additive for e
- Page 225 and 226:
HCPCSAppendix AB4199 Parenteral nut
- Page 227 and 228:
HCPCSAppendix ADate 1/1/2004)E0141
- Page 229 and 230:
HCPCSAppendix AE0197 Air pressure p
- Page 231 and 232:
HCPCSAppendix AE0292 Hospital bed,
- Page 233 and 234:
HCPCSAppendix AE0443 Portable oxyge
- Page 235 and 236:
HCPCSAppendix AE0575 Nebulizer; ult
- Page 237 and 238:
HCPCSAppendix AE0668 Segmental pneu
- Page 239 and 240:
HCPCSAppendix AE0783 Infusion pump
- Page 241 and 242:
HCPCSAppendix A1/1/2003)E0972 Wheel
- Page 243 and 244:
HCPCSAppendix AE1038 Transport chai
- Page 245 and 246:
HCPCSAppendix AE1550 Bath conductiv
- Page 247 and 248:
HCPCSAppendix AALL COMPONENTS AND A
- Page 249 and 250:
HCPCSAppendix Aattaching hardware (
- Page 251 and 252:
HCPCSAppendix A1/1/2004)E2367 Power
- Page 253 and 254:
HCPCSAppendix AE2506 Speech generat
- Page 255 and 256:
HCPCSAppendix AHCPCS GPayment Categ
- Page 257 and 258:
HCPCSAppendix AJ0215 Injection, ale
- Page 259 and 260:
HCPCSAppendix AJ0630 Injection, cal
- Page 261 and 262:
HCPCSAppendix AJ1055 Injection, med
- Page 263 and 264:
HCPCSAppendix AJ1510 Injection, gam
- Page 265 and 266:
HCPCSAppendix AJ1750 Injection, iro
- Page 267 and 268:
HCPCSAppendix AJ2300 Injection, nal
- Page 269 and 270:
HCPCSAppendix AJ2730 Injection, pra
- Page 271 and 272:
HCPCSAppendix AJ3246 Injection, Tir
- Page 273 and 274:
HCPCSAppendix AJ7110 Infusion, dext
- Page 275 and 276:
HCPCSAppendix ABioengineered or pro
- Page 277 and 278:
HCPCSAppendix A(Terminated on 6/30/
- Page 279 and 280:
HCPCSAppendix AJ7644 Ipratropium br
- Page 281 and 282:
HCPCSAppendix AJ8498 Antiemetic dru
- Page 283 and 284:
HCPCSAppendix AJ9182 Etoposide, 100
- Page 285 and 286:
HCPCSAppendix AHCPCS KPayment Categ
- Page 287 and 288:
HCPCSAppendix AK0040 Adjustable ang
- Page 289 and 290:
HCPCSAppendix AK0088 Battery charge
- Page 291 and 292:
HCPCSAppendix AK0132 Male external
- Page 293 and 294:
HCPCSAppendix AK0182 Water, distill
- Page 295 and 296:
HCPCSAppendix AK0222 Gauze, impregn
- Page 297 and 298:
HCPCSAppendix A12/31/1996)K0260 Wou
- Page 299 and 300:
HCPCSAppendix AK0412 Mycophenolate
- Page 301 and 302:
HCPCSAppendix AK0450 Adhesive, liqu
- Page 303 and 304:
HCPCSAppendix AK0530 Nebulizer, dur
- Page 305 and 306:
HCPCSAppendix AK0559 Addition to lo
- Page 307 and 308:
HCPCSAppendix AK0595 Ostomy pouch,
- Page 309 and 310:
HCPCSAppendix AK0627 Traction equip
- Page 311 and 312:
HCPCSAppendix AK0643 Lumbar-sacral
- Page 313 and 314:
HCPCSAppendix AK0664 Positioning wh
- Page 315 and 316:
HCPCSAppendix AK0827 Power wheelcha
- Page 317 and 318:
HCPCSAppendix AK0868 Power wheelcha
- Page 319 and 320:
HCPCSAppendix AL0200 Cervical, mult
- Page 321 and 322:
HCPCSAppendix AL0462 TLSO, triplana
- Page 323 and 324:
HCPCSAppendix AL0490 TLSO, sagittal
- Page 325 and 326:
HCPCSAppendix AL0627 Lumbar orthosi
- Page 327 and 328:
HCPCSAppendix AT-9 vertebra, latera
- Page 329 and 330:
HCPCSAppendix AL1040 Addition to CT
- Page 331 and 332:
HCPCSAppendix AL1815 Knee orthosis,
- Page 333 and 334:
HCPCSAppendix AL1970 Ankle-foot ort
- Page 335 and 336:
HCPCSAppendix AL2136 Knee-ankle-foo
- Page 337 and 338:
HCPCSAppendix AL2520 Addition to lo
- Page 339 and 340:
HCPCSAppendix AL3031 Foot, insert/p
- Page 341 and 342:
HCPCSAppendix AL3360 Sole wedge, ou
- Page 343 and 344:
HCPCSAppendix A(e.g., neoprene, lyc
- Page 345 and 346:
HCPCSAppendix AL3906 Wrist hand ort
- Page 347 and 348:
HCPCSAppendix AL3938 Wrist hand fin
- Page 349 and 350:
HCPCSAppendix AL3978 Shoulder elbow
- Page 351 and 352:
HCPCSAppendix AL5100 Below knee, mo
- Page 353 and 354:
HCPCSAppendix AL5580 Preparatory, a
- Page 355 and 356:
HCPCSAppendix AL5660 Addition to lo
- Page 357 and 358:
HCPCSAppendix AL5702 Replacement, s
- Page 359 and 360:
HCPCSAppendix AL5855 Addition, endo
- Page 361 and 362:
HCPCSAppendix AL6025 Transcarpal/me
- Page 363 and 364:
HCPCSAppendix AL6615 Upper extremit
- Page 365 and 366:
HCPCSAppendix A(Eff. Date 1/1/2005)
- Page 367 and 368:
HCPCSAppendix AL6860 Terminal devic
- Page 369 and 370:
HCPCSAppendix AL7007 Electric hand,
- Page 371 and 372:
HCPCSAppendix AL7611 TERMINAL DEVIC
- Page 373 and 374:
HCPCSAppendix A12/31/2005)L8230 Gra
- Page 375 and 376:
HCPCSAppendix AL8640 Patella implan
- Page 377 and 378:
HCPCSAppendix AQ0168 Dronabinol, 5
- Page 379 and 380:
HCPCSAppendix AQ4075 Injection, acy
- Page 381 and 382:
HCPCSAppendix AHCPCS VPayment Categ
- Page 383 and 384:
HCPCSAppendix AV2211 Spherocylinder
- Page 385 and 386:
HCPCSAppendix AV2531 Contact lens,
- Page 387:
HCPCSAppendix AV5070 Glasses, air c