Continuing Education
Continuing Education
Continuing Education
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
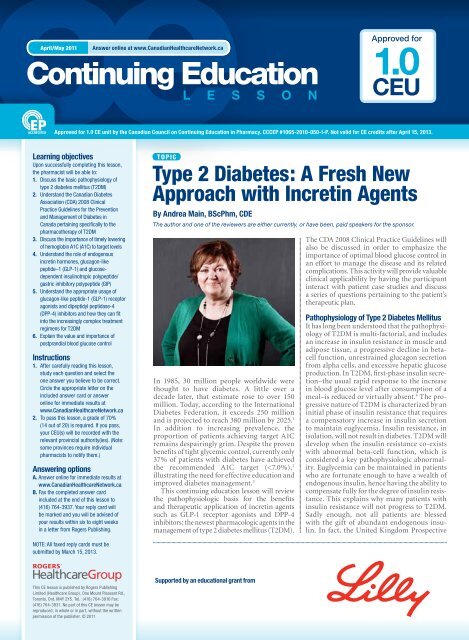
ce<strong>Continuing</strong> <strong>Education</strong>L e s s o n2Type 2 Diabetes: A Fresh New Approach with Incretin AgentsApril/May 2011Answer online at www.CanadianHealthcareNetwork.caFIGURE 1Increased glucose production↓ Metformin↓ ThiazolidinedionesFIGURE 2Pathogenesis of type 2 diabetes and traditional drug class targets 43LiverCarbohydrate loadDigestion of polysaccharides↓ a-Glucosidase inhibitorsHyperglycemiaPancreasImpaired insulin secretion↑ Sulfonylureas↑ MeglitinidesPhysiologic effects of GLP-1 44Diabetes Study (UKPDS) found that patientswith T2DM have lost approximately 50% oftheir pancreatic beta-cell function by the timethey are diagnosed and that decline will continue,despite therapy. 5In addition to well-known metabolicabnormalities, it is now evident that otherfactors, including defective actions of thegastrointestinal incretin hormones glucagonlikepeptide–1 (GLP-1) and glucose-dependentinsulinotropic polypeptide/gastric inhibitorypolypeptide (GIP), also play significantroles. Traditional pharmacotherapy developedfor the treatment of T2DM specificallytargets one or more pathophysiologic defects(Figure 1). It is quite exciting that one categoryof novel agents, “the incretins,” can addressmost of these abnormalities, and more.Role of Endogenous Incretin HormonesThe incretin hormones, GLP-1 and GIP, aregut-produced hormones that are importantcontributors to the maintenance of glucoseAdiposeIncreased FFA↓ ThiazolidinedionesSkeletal muscleDecreased glucose uptakeand utilization↑ Metformin↑ ThiazolidinedionesGLP-1 Effects in humans: understanding the glucoregulatory role of incretinsGLP-1 secreted uponthe ingestion of foodBeta cells: Enhancesglucose-dependentinsulin secretionPromotes satietyand reduces appetiteAlpha cells:↓ Postprandialglucagon secretionLiver:↓ Glucagon reduceshepatic glucose outputStomach:Slows gastricemptyingAdapted from Flint A, et al. J Clin Invest 1998;101:515-20; Adapted from Larsson H, et al. Acta Physiol Scand 1997;160:413-22;Adapted from Nauck MA, et al. Diabetologia 1996;39:1546-53; Adapted from Drucker DJ. Diabetes 1998;47:159-69.homeostasis, particularly the control of postprandialglucose. GLP-1 is secreted by L cells inthe ileum and colon, while GIP is secreted by Kcells in the duodenum. 6 These hormones werefirst discovered when it was noted that ingestedglucose elicits a larger insulin response thanwith intravenous (IV) glucose, suggestingthat a mechanism exists within the gut thatenhances insulin release in response to meals. 7This “incretin effect” is thought to be responsiblefor 50–70% of the total insulin secretedfollowing the ingestion of glucose. 8The physiologic actions of native GLP-1are depicted in Figure 2 and include thefollowing:• Glucose-dependent increase in insulinsecretion from the pancreatic beta-cell• Suppression of glucagon secretion in thealpha cells in a glucose-dependent mannerthereby reducing hepatic glucose productionAt higher concentrations of GLP-1, asachieved by GLP-1 receptor agonist pharmacotherapy,additional effects occur, such as:• A delay in gastric emptying which in turndelays absorption of ingested nutrients anddampens postprandial glucose excursion• An increase in satiety which in turn suppressesappetite, decreases food intake andeventually leads to weight lossUnfortunately, the biological actions ofGLP-1 and GIP are short-lived as they are rapidlyinactivated, within two to three minutes,by the enzyme dipeptidyl peptidase-4 (DPP-4). In T2DM, endogenous GLP-1 retains itsinsulinotropic effects, even though it is presentin diminished concentrations. GIP, however,is present in normal concentrations, butlacks insulinotropic effects, thereby restrictingthe possibilities of its clinical use. 9 Itappears that GLP-1 has a more dominant roleas a metabolic regulator than does GIP, andfor this reason, intense research and pharmaceuticalefforts directed at potentiation ofincretin actions for the treatment of T2DMhas focused on GLP-1 receptor agonists.Case 1You are conducting a “Diabetes Day” atyour retail pharmacy and have a number ofpatients scheduled for medication reviews.Your first patient presents as follows:Brian is a 48-year-old obese male who wasdiagnosed with T2DM five years ago. He alsohas hypertension and dyslipidemia. His sedentaryjob as a truck driver often takes him tothe southern United States on lengthy hauls.He complains of increasing weight gain secondaryto his inactive lifestyle in and outsideof work, and a lack of nutritious food choiceson the road. His current medications includemetformin 500 mg 2 tablets BID, rosuvastatin10 mg OD, ramipril 10 mg OD and atenolol50 mg OD. He brings in a copy of his currentlabwork (A1C 8.2%) and a record of his homeblood glucose monitoring.DateBefore bkfst*After bkfst*Before lunch*After lunch*Before supper*After supper*Before snack*Sun 7.5 11.2Mon 5.9 9.3Tues 7.3Wed 12.9Thurs 6.5 8.0Fri 9.1 11.3Sat 8.4* mmol/LQuestionIs Brian’s glycemic control optimal according to thecurrent Clinical Practice Guidelines?DiscussionBrian’s glycemic control is not optimal. TheCDA 2008 Clinical Practice Guidelines forthe Prevention and Management of Diabetesin Canada include a section dedicated to
Type 2 Diabetes: A Fresh New Approach with Incretin AgentsAnswer online at www.CanadianHealthcareNetwork.ca April/May 2011ce<strong>Continuing</strong> <strong>Education</strong>L e s s o n5TABL E 2 Comparison of various incretin agents 22,28,50-55Class ofmedicationIncretinreceptoragonistDPP-4inhibitorName ofmedicationExenatideUsual dosage Side effects Comments ↓A1C 5To minimize GI intolerance, start with 5 mcgs/c BID then increase to 10 mcg s/c BIDafter one month; exenatide can be administeredat any time within the 60-minute periodbefore the morning and evening meal(≥6 hours apart) and never after a mealNausea, vomiting, diarrheaNo dose adjustment required in mild renal insufficiency;caution when increasing dose from 5 mcgto 10 mcg in moderate renal insufficiency; notrecommended in severe renal insufficiency or endstagerenal diseaseWeight loss 1.6-2.6 kg at week 30 with 10 mcg BIDExenatide LAR* 0.8 or 2.0 mg s/c weekly Mild nausea Weight loss 4.1 kg at week 52 with 2.0 mg s/c weekly 2.0%Liraglutide To minimize GI intolerance, start with 0.6mg s/c once daily at any time, independentof meals. After one week, the dose shouldbe increased to 1.2 mg then up to 1.8 mgafter at least one week if required for acceptableglycemic controlNausea, vomiting, diarrheaSitagliptin 100 mg once daily URI, nasopharyngitis,possible immunogenicitySitagliptin/metformincombinationGradual escalations:50/500 mg daily to 100/2,000 mg dailyURI, nasopharyngitis,bloating, gas, diarrheaSaxagliptin 5 mg once daily Nasopharyngitis, bronchitiswith Met combo hypoglycemia,UTI with SU comboMet=metformin; SU=sulfonylurea; UTI=Urinary Tract Infection; URI=Upper Respiratory Infection*Exenatide LAR is not available in Canada.No dose adjustment required in mild renal insufficiency;liraglutide is not recommended for use inpatients with moderate or severe renal insufficiencyor end-stage renal diseaseWeight loss 2.6 kg at week 26 with dose 1.2 mgdailyNot recommended in moderate or severe renalinsufficiencyWeight neutralNot recommended in moderate or severe renalinsufficiencyWeight neutralNot recommended in moderate or severe renalinsufficiencyWeight neutral0.9%1.0%0.7%Notstudied0.7%is inappropriate due to contraindications orintolerance or in combination with metformin.32 In September 2009, a combinationproduct containing sitagliptin and metforminreceived approval and is also available. 33 Thesitagliptin/metformin combination productis indicated as an adjunct to diet and exercisein patients with T2DM inadequately controlledon metformin or in patients alreadybeing treated with the combination of sitagliptinand metformin. 34SaxagliptinIn November 2009, Health Canada approvedanother DPP-4 inhibitor, saxagliptin, which isindicated for patients with T2DM in combinationwith metformin or a sulfonylurea, whenthese agents used alone with diet and exercisedo not provide adequate glycemic control. 35Currently, many more DPP-4 inhibitors arebeing evaluated in clinical trials by differentpharmaceutical companies, including vildagliptin(approved in Europe), alogliptin, linagliptin,and denagliptan. 36 Please refer to Table2 for a comparison of various incretin agents.Adverse Events Associated withIncretin AgentsPancreatitisA safety concern is a possible increased riskof pancreatitis attributable to drugs that actthrough the GLP-1 pathway. This concernarose from postmarketing surveillance submittedto the FDA Adverse Event ReportingSystem regarding pancreatitis associated withthe use of exenatide and sitagliptin, both ofwhich act through this pathway. Interestingly,in at least 90% of subjects, there existed otherfactors that could predispose the individualsto pancreatitis. In addition, analysis of pancreatitisin subjects with T2DM suggests thattheir risk is increased threefold over subjectswithout diabetes. 37 This has made it difficultto determine whether the spontaneousreports indicate that use of these drugs wasthe cause of increased risk.Despite this uncertainty, the product monographfor exenatide contains a warning thatstates that patients must be carefully observedfor signs and symptoms of pancreatitis (persistent,severe abdominal pain, occasionallyradiating to the back, plus/minus vomiting).Exentatide is not recommended in patientswith a history of or risk factors for pancreatitis(gallstones, alcoholism, hypertriglyceridemia).22 Similarly, the product monographfor liraglutide specifies that it should be usedwith caution in patients with a history ofpancreatitis. 28Medullary Thyroid Carcinoma (MTC)In addition to pancreatic islets, GLP-1 receptorscan be found in several other cells of neuronaland neuroendocrine origin, includingparafollicular thyroid C-cells. Studies havesuggested that liraglutide stimulates calcitoninsecretion and can promote C-cell hyperplasiaand C-cell tumors at clinically relevant exposuresin rodents. In rodents, C-cell hyperplasiais considered a pre-neoplastic lesion leading tomedullary thyroid carcinoma (MTC). 39The Canadian product monograph forliraglutide includes a boxed warning statingthat liraglutide causes a dose-dependent andtreatment-duration dependent thyroid C-celltumours in rats and mice. Since it is unknownwhether liraglutide causes thyroid C-celltumours, including MTC, in humans, it is contraindicatedin patients with a personal or familyhistory of MTC and in patients with MultipleEndocrine Neoplasia syndrome type 2 (MEN2). Similarly, the Canadian exenatide productmonograph states that until further long-termdata in humans are available, the same contraindications(MTC, MEN 2) exist. 22 It is thereforeprudent to counsel patients regarding therisk for MTC and the symptoms of thyroidtumors (mass in the neck, dysphagia, dyspnea,or persistent hoarseness). 40Case 2The next patient scheduled for medicationreview on your Diabetes Day is Maria, a 53-yearoldPortuguese homemaker with a BMI of30 kg/m 2 . Her diet is high in carbohydrates, fat,and salt, and she gets little exercise. Her medicalhistory includes hypertension and dyslipidemia.When diagnosed with T2DM threemonths ago, her A1C was 8.7%, and her fastingplasma glucose range was 7.5–8.9 mmol/L. Herinitial therapy consisted of metformin 500 mgtitrated to 1,000 mg BID, plus a diet and exerciseplan. Today, after three months, her A1Cis 7.2% and her logbook is as follows:DateBefore bkfst*After bkfst*Before lunch*After lunch*Before supper*After supper*Sun 5.5 9.6Mon 6.7 12.4Tues 6.1Wed 7.0Thurs 6.8Fri 11.5* mmol/LBefore snack*
Type 2 Diabetes: A Fresh New Approach with Incretin AgentsAnswer online at www.CanadianHealthcareNetwork.ca April/May 2011ce<strong>Continuing</strong> <strong>Education</strong>L e s s o n7com/dpp-iv_inhibitors.htm (accessed January 7, 2011).37. Noel RA, Braun DK, Patterson RE, et al. Increased risk of acute pancreatitisand biliary disease observed in patients with type 2 diabetes:a retrospective cohort study. Diabetes Care 2009;32:834-8.38. Parks M, Rosebraugh C, Weighing risks and benefits of liraglutide—the FDA’s review of a new antidiabetic therapy, NEJM. www.nejm.org/doi/full/10.1056/NEJMp1001578 (accessed January 7, 2011).39. McConnell EE, Solleveld HA, Swenberg JA, et al. Guidelines forcombining neoplasms for evaluation of rodent carcinogenesis studies.J Natl Cancer Inst 1986;76:283-9.40. Novo Nordisk Canada. Victoza (liraglutide) product monograph,May 21, 2010.41. Glucose tolerance and mortality: comparison of WHO and AmericanDiabetes Association diagnostic criteria. The DECODE studygroup. European Diabetes Epidemiology Group. Diabetes Epidemiology:Collaborative analysis of diagnostic criteria in Europe.Lancet 1999;354:617-21.42. Monnier L, Lapinski H, Colette C. Contributions of fasting andpostprandial plasma glucose increments to the overall diurnalhyperglycemia of type 2 diabetic patients: variations with increasinglevels of HbA(1c). Diabetes Care 2003;26:881-5.43. Evans J, Rushakoff R. Oral pharmacological agents for type 2diabetes: sulfonylureas, meglitinides, metformin, thiazolidinediones,α-glucosidase inhibitors, and emerging approaches. www.endotext.org/diabetes/diabetes16/diabetes14.html (accessedJanuary 7, 2011).44. Munro N. Modern management of hyperglycemia EPCCS 2009www.epccs.eu/default.aspx?id=23&subId=24&presentationId=9 (accessed January 7, 2011).45. Reid T. The importance and treatment of postprandial hyperglycemia.J Fam Pract 2010;59(5):S9-S14.46. Canadian Diabetes Association Clinical Practice Guidelines ExpertCommittee. Canadian Diabetes Association. 2008 clinical practiceguidelines for the prevention and management of diabetes inCanada. Can J Diabetes 2008;32(Suppl 1):S1-S201.47. Freeman J, Unger J. Why and when to implement incretin therapy.J Fam Pract 2008;57. www.jfponline.com/pages.asp?id=6688(accessed January 7, 2011).48. Nathan B, Buse J, Davidson M, et al. Medical management of hyperglycemiain type 2 diabetes: a consensus algorithm for the initiationand adjustment of therapy. Clin Diabetes 2009;27:14-5.49. Eli Lilly. Byetta (exenatide) prescribing information. http://pi.lilly.com/us/byetta-pi.pdf (accessed January 7, 2011).50. Buse JB, Drucker DJ, Taylor KL, et al. DURATION-1: exenatide onceweekly produces sustained glycemic control and weight loss over52 weeks. Diabetes Care June 2010;33(6):1255-61.51. LEAD-6: Liraglutide superior to exenatide in improving glycemiccontrol. www.endocrinetoday.com/view.aspx?rid=40742 (accessedJanuary 7, 2011).52. Hindsberger C, Jacobsen L, Robson R, et al. Effect of renal impairmenton the pharmacokinetics of the GLP-1 analogue liraglutide.Br J Clin Pharmacol 2009;68(6):898-905(8).53. Merck Frosst Canada. Januvia (sitagliptin) product monograph.Kirkland QC. 2009.54. Merck Frosst Canada. Janumet (sitagliptin phosphate monohydrateand metformin hydrochloride) product monograph. Kirkland QC.September 23, 2009.55. Onglyza Prescribing Information. www.onglyza.com/hcp/hcp.aspx(accessed January 7, 2011).Questions Answer online at www.CanadianHealthcareNetwork.ca, CE section, Quick Search CCCEP #1065-2010-050-I-P1. The natural progression ofT2DM can best be described aswhich of the following?a) An initial phase of insulinresistance that requires acompensatory increase ininsulin secretion to maintainnormal blood glucose levels.b) An initial phase of decreasedinsulin secretion which resultsin insulin resistance.c) An initial phase of increasedinsulin secretion which resultsin insulin resistance.d) An initial phase of decreasedglycogen production whichrequires increased insulinsecretion to maintain normalblood glucose levels.2. Nutrition therapy can reduceA1C by:a) 0.1–0.5% c) 1.0–2.0%b) 0.5–1.0% d) 2.0–3.0%3. Which of the following statementsis true?a) Insulin resistance will alwayslead to T2DM.b) At diagnosis of T2DM, mostpatients have already lost 50%of their beta-cell function.c) Intense research is underwayto develop new agentsto mimic the actions of GIP(glucose-dependent insulinotropicpolypeptide).d) According to the CDA 2008CPGs, if glycemic targets arenot achieved within six to 12months of lifestyle management(nutrition therapy andexercise recommendations),antihyperglycemic pharmacotherapyshould be initiated.4. Which of the followingstatements is true?a) A1C reduction is durable withsulfonylurea therapy.b) Metformin is an insulin sensitizerthat is capable of inhibitinghepatic gluconeogenesis.c) Weight loss is a side effect ofDPP-4 inhibitors.d) Insulin is a desired add-ontherapy to TZDs.5. Which of the followingstatements is true?a) Insulin therapy can reduceA1C by 0.5–1.5%.b) Sulfonylurea therapy canreduce A1C by 0.5–0.8%.c) Alpha-glucosidase therapy canreduce A1C by 0.5–0.8%.d) TZD therapy can reduce A1Cby 1–2%.6. As A1C levels decreasetowards the target, the importanceof postprandial glucosefor A1C reduction:a) increasesb) decreasesc) stays the samed) increases first then decreasesas the A1C is closer to target7. Which of the followingstatements about incretinhormones is true?a) “GLP-1” is an acronym for“glycogen-like peptide-1.”b) “GIP” is an acronym for“glucagon-dependentinsulinotropic polypeptide.”c) “GLP-1” is an acronym for“glucose-like peptide-1.”d) “GIP” is an acronym for“glucose-dependent insulinotropicpolypeptide.”8. Which of the following statementsabout incretin hormonesis true?a) GIP level and insulinotropiceffects are significantlyreduced in T2DM.b) GLP-1 level is normal but itloses its insulinotropic effectsin T2DM.c) GLP-1 level is reduced butinsulinotropic effects areretained in T2DM.d) GIP level is reduced butinsulinotropic effects areretained in T2DM.9. Native GLP-1 has anapproximate half-life of:a) 10–15 minutesb) four to six hoursc) two to three minutesd) two to three seconds10. Which of the followingstatements is true?a) GLP-1 receptor agonist therapywill result in physiologicconcentrations of GLP-1.b) DPP-4 therapy will resultin supraphysiologicconcentrations of GLP-1.c) GLP-1 receptor agonisttherapy will result in supraphysiologicconcentrationsof GLP-1.d) DPP-4 therapy will resultin supraphysiologicconcentrations of GIP.11. Treatment with exenatide, aGLP-1 agonist, is associated withall but which of the following?a) diminished appetiteb) improved beta-cell functionin rat modelc) decreased postprandialblood glucosed) weight gain12. Which of the followingmechanisms contributes tothe glucose-lowering propertiesof GLP-1 receptor agonists?a) continuous pancreaticbeta-cell stimulationb) enhanced postprandialinsulin secretionc) increased gastric emptyingd) increased glucagon secretion13. Which of the following statementsis true?a) Sulfonylureas stimulate insulinsecretion in a glucose-dependentmanner.b) Meglitinides stimulates insulinsecretion in a glucose-dependentmanner.c) DPP-4 inhibitors stimulateinsulin secretion in a glucosedependentmanner.d) DPP-4 inhibitors stimulateinsulin secretion in a glucoseindependentmanner.14. Which of the following agentshas the potential to reduce A1Cby the greatest amount?a) sitagliptin c) metforminb) exenatide d) pioglitazoneQuestions 15-18 pertain to thefollowing case:Roger, a 45-year-old male witha BMI of 35 kg/m2 presentsto your pharmacy and asks youto review his logbook. He wasdiagnosed with T2DM three yearsago (with an A1C of 8.5%) andhas been taking metformin eversince. He tells you that his A1Cis 10.1% and his logbook revealsthat his fasting sugars have beenquite high recently. Exercise isdifficult due to chronic backpain. He denies any othermedical conditions.15. According to the CDA 2008Clinical Practice Guidelines, whatis an appropriate A1C goal forthis patient?a)
ce<strong>Continuing</strong> <strong>Education</strong>L e s s o n8Type 2 Diabetes: A Fresh New Approach with Incretin AgentsApril/May 2011Answer online at www.CanadianHealthcareNetwork.caQuestions Answer online at www.CanadianHealthcareNetwork.ca, CE section, Quick Search CCCEP #1065-2010-050-I-P16. Which of the following agentswould be most appropriate asadd-on therapy?a) acarbose c) glargineb) saxagliptin d) gliclazide17. If Roger’s A1C at diagnosiswas 10.1%, what would bethe most appropriate initialtherapeutic regime?a) lifestyle intervention andmetforminb) pioglitazone onlyc) detemir insulin onlyd) lifestyle intervention,metformin and glimepiride18. What is the most likelyreason why Roger’s A1C hasincreased from 8.5% to 10.1%in three years?a) Roger should have beenprescribed a sulfonylurea asinitial therapy as this class ofmedication has the greatestability to lower A1C.b) Roger didn’t exercise.c) This is the natural progressionof T2DM, despite therapy;Roger should have had his glycemiccontrol /pharmacotherapymonitored and adjustedevery three months.d) Roger should have been prescribeda TZD as initial therapyas this class of medicationhas the most durable glycemiceffects.19. Which of the followingstatements is true?a) An advantage of saxagliptinis that it could induceweight loss.b) An advantage of sitagliptin isthat it can be taken orally.c) An advantage of sitagliptinis that it can be safely givenin moderate or severe renalinsufficiency.d) An advantage of saxagliptinis that it can be safely givenin moderate or severe renalinsufficiency.20. Which of the followingstatements is true?a) GLP-1 is secreted by thepancreas in response to anIV glucose load.b) GLP-1 is secreted by thepancreas in response to anoral glucose load.c) Ingested glucose elicits alarger insulin responsecompared with IV glucose.d) IV glucose elicits a largerinsulin response comparedwith ingested glucose.FacultyType 2 Diabetes: A Fresh New Approach with Incretin AgentsAbout the authorAndrea Main has been a licensed,practicing pharmacist since 1987 anda Certified Diabetes Educator since2000. With her enthusiastic nature,she promotes and supports patientempowerment, offering guidance andencouragement to patients with diabetes.She has extensive experiencein both retail and clinical pharmacy.In addition, Andrea has worked as amedical author and consultant on avariety of projects involving pharmacotherapyand disease state management.She is currently employedas a clinical pharmacist within themulti-disciplinary Family Health Teamat the Grandview Medical Centre inCambridge, Ontario as well as anAdjunct Clinical Assistant Professorat the School of Pharmacy, Universityof Waterloo.ReviewersAll lessons are reviewed by pharmacistsfor accuracy, currency and relevanceto current pharmacy practice.This lesson is valid until April 15, 2013.Information about Type 2 Diabetesmay change over the course of thistime. Readers are responsible fordetermining the most current aspectsof this topic.<strong>Continuing</strong> <strong>Education</strong>Project ManagerSheila McGovern, Toronto, Ont.Client LiaisonBrandAide MedicalCommunications Inc.CE DesignerShawn Samson, TwoCreative.caFor information about CE marking,please contact Mayra Ramos at(416) 764-3879, fax (416) 764-3937or mayra.ramos@rci.rogers.com.No part of this CE lesson may bereproduced, in whole or in part,without the written permission ofthe publisher. © 2011Approved for1.0 CEU1.0 CEUNIT INQUEBECType 2 Diabetes:A Fresh New Approachwith Incretin Agents<strong>Continuing</strong> <strong>Education</strong>L e s s o n1. a b c d 5. a b c d 9. a b c d 13. a b c d 17. a b c d2. a b c d 6. a b c d 10. a b c d 14. a b c d 18. a b c d3. a b c d 7. a b c d 11. a b c d 15. a b c d 19. a b c d4. a b c d 8. a b c d 12. a b c d 16. a b c d 20. a b c dApril/May 2011CCCEP #1065-2010-050-I-PNot valid for CE Credits afterApril 15, 2013.PLEASE NOTE: All faxed replycards must be submitted byMarch 15, 2013.First NameLast NamePrimary Licensing Province Licence # Secondary Licensing Province Licence #Pharmacy NameHome Address City ProvincePostal Code Telephone FaxEmailYear graduatedType of practiceq Drug chain or franchiseq Bannerq Independentq Mass merchandiserq Grocery store pharmacyq Hospital pharmacyq Other (specify):______________________Supported by an educational grant fromANSWERINGOPTIONS:1. Answer ONLINE for immediate results at www.CanadianHealthcareNetwork.ca2. FAX this reply card to Mayra Ramos at (416) 764-3937 (Please allow 6-8 weeks for notification of score)Over 100 FREE CCCEP-approved CE lessons online.Click on <strong>Education</strong>, then CE online.