Tuberculosis - UT Southwestern
Tuberculosis - UT Southwestern
Tuberculosis - UT Southwestern
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
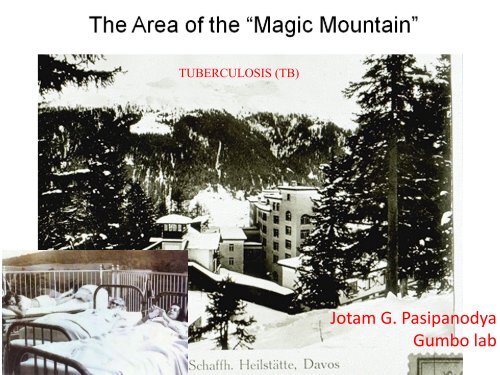
TUBERCULOSIS (TB)Jotam G. PasipanodyaGumbo lab
History of TB
History of TB• Historically known bya variety of names,including:– Consumption– Wasting disease– White plague– Sanatorium was partof treatment– Those who could notafford died at home• TB was a deathsentence for many
TB History Timeline1865:Jean-AntoineVilleminproved TB iscontagious1884:First TBsanatoriumestablishedin U.S.1943:Streptomycin(SM) a drug usedto treat TB isdiscovered1993: TB cases decline due toincreased funding and enhancedTB control effortsMid-1970s: MostTB sanatoriums inU.S. closed1840 1860 1880 1900 1920 1940 1960 1980 20001882:Robert Koch discoversM. tuberculosis1943-1952:Two more drugs arediscovered to treatTB: INH and PASMid-1980s:Unexpected rise inTB cases
“It seems likely that the tubercle is surroundedWith a special wall of unusual properties, andThat the penetration of a dye through this wallCan occur when alkali, aniline, or similarSubstance is present”Mycobacterium TB (scanning EM)Robert KochNobel Prize-Medicine (1905)Mycobacterium TB on Lowenstein-Jensen medium
Epidemiology of TB
Significance for Global Health: TB• TB is a disease of poverty; affecting mostly youngadults in their most productive years. The vastmajority of TB deaths are in the developing world,with more than half of all deaths occurring in Asia• More than 2 billion people, equal to 1/3 of the worldpopulation, are latently infected with TB (LTBI)– 1 in 10 people with LTBI bacilli will become sick with activeTB in their lifetime; those with HIV are at much greater risk– Africa accounted for 85% of estimated global HIV positiveTB cases in 2006.• 1.7 million people died from TB in 2006 including231,000 people with HIV. This is equal to 4,500deaths a day
The global population structure and geographical distribution of M. tuberculosisGagneux S. et.al. PNAS 2006;103:2869-2873©2006 by National Academy of Sciences
U.S. TB Resurgence1986 - 199220% increaseNo. of Cases28,00026,00024,00022,00020,00018,00016,00014,00012,00010,0001982 1986 1990 1994 1998 2002 2008YearReported TB Cases, U.S., 1982-2008
16000Reported <strong>Tuberculosis</strong> Cases Among Blacksand Whites, United States, 1980 - 1992Number of notified cases(log scale)13000100008000BlackWhite80 82 84 86 88 90 92Year of reportUS Centers for Disease Control and Prevention<strong>Tuberculosis</strong> Statistics in the United States, 1992
TB TransmissionTypes of Mycobacteria• M. tuberculosis causesmost TB cases in U.S.• Mycobacteria that causeTB:– M. tuberculosis– M. bovis– M. africanum– M. microti– M. canetti• Mycobacteria that do notcause TB– e.g., M. avium complexM. tuberculosis13
• TB is spread person toperson through the air viadroplet nuclei• M. tuberculosis may beexpelled when aninfectious person:– Coughs– Sneezes– Speaks– Sings• Transmission occurswhen another personinhales droplet nucleiTB Transmission
TB TransmissionDots in air represent droplet nuclei containingM. tuberculosis
TB Transmission• Probability that TB will be transmitted dependson:– Infectiousness of person with TB disease– Environment in which exposure occurred– Length of exposure– Virulence (strength) of the tubercle bacilli• The best way to stop transmission is to:– Isolate infectious persons– Provide effective treatment to infectious persons assoon as possible16
Percentage of Secondary Cases Among Tuberculin-PositiveContacts, by Type of Source Case, Canada, 1966 - 1971Per cent cases among reactors76543210sm+/cul+sm-/cul+Intimatecontactsm-/cul-sm+/cul+sm-/cul+Casualcontactsm-/cul-Grzybowski S, et al. Bull Int Union Tuberc 1975;50:90-106Rieder HL, et al. Epidemiol Rev 1989;11:79-98
Drug-Resistant TB• Caused byM. tuberculosisorganisms resistant toat least one TBtreatment drug– Isoniazid (INH)– Rifampin (RIF)– Pyrazinamide (PZA)– Ethambutol (EMB)• Resistant means drugscan no longer kill thebacteriaModule 1 – Transmission and Pathogenesis of <strong>Tuberculosis</strong> 19
Drug-Resistant TBMono-resistant Resistant to any one TB treatmentdrugPoly-resistantMultidrugresistant(MDR TB)Extensivelydrug resistant(XDR TB)Resistant to at least any 2 TB drugs(but not both isoniazid and rifampin)Resistant to at least isoniazid andrifampin, the 2 best first-line TBtreatment drugsResistant to isoniazid and rifampin,PLUS resistant to any fluoroquinoloneAND at least 1 of the 3 injectablesecond-line drugs (e.g., amikacin,kanamycin, or capreomycin)Module 1 – Transmission and Pathogenesis of <strong>Tuberculosis</strong> 20
TB PathogenesisPathogenesis is defined as how an infection ordisease develops in the body.
Sites of TB DiseaseBacilli may reach any part of the body, butcommon sites include:BrainLarynxBoneKidneyLymph nodePleuraLungSpine
Sites of TB Disease (2)LocationFrequencyPulmonary TB Lungs Most TB cases arepulmonaryExtrapulmonary TB Places other thanlungs such as:• Larynx• Lymph nodes• Pleura• Brain• Kidneys• Bones and jointsFound more often in:• HIV-infected orotherimmunosuppressedpersons• Young childrenMiliary TBCarried to all partsof body, throughbloodstreamRareModule 1 – Transmission and Pathogenesis of <strong>Tuberculosis</strong> 23
TB PathogenesisTB Disease• Develops when immune system cannot keeptubercle bacilli under control– May develop very soon after infection ormany years after infection• About 10% of all people with normal immunesystems who have LTBI will develop TBdisease at some point in their lives• People with TB disease are often infectious
TB Pathogenesis (2)Latent TB Infection (LTBI)• Occurs when tubercle bacilli are in the body,but the immune system is keeping them undercontrol• Detected by the Mantoux tuberculin skin test(TST) or by blood tests such as interferongammarelease assays (IGRAs) which include:– QuantiFERON ® -TB Gold test (QFT-G)– QuantiFERON ® -TB Gold In-Tube (QFT-GIT)– T-Spot ® .TB test (T-SPOT)• People with LTBI are NOT infectiousModule 1 – Transmission and Pathogenesis of <strong>Tuberculosis</strong> 25
LTBI vs. TB DiseaseLatent TB Infection (LTBI)Inactive, contained tubercle bacilliin the bodyTST or blood test results usuallypositiveChest x-ray usually normalSputum smears and culturesnegativeNo symptomsNot infectiousNot a case of TBTB Disease (in the lungs)Active, multiplying tubercle bacilliin the bodyTST or blood test results usuallypositiveChest x-ray usually abnormalSputum smears and cultures maybe positiveSymptoms such as cough, fever,weight lossOften infectious before treatmentA case of TB
From Infection to Disease• • • • • • 5%2-5 years• 5%rest of lifetime
Referent: Infection >7 yr pastInfection
Clinical Presentation29
Treatment and PublicHealth Control Strategies35
A Model for the Epidemiology of <strong>Tuberculosis</strong>RiskfactorsRiskfactorsRiskfactorsRiskfactorsExposureSubclinicalinfectionInfectioustuberculosisDeathNon-infectioustuberculosisRieder HL. Infection 1995;23:1-4
500Correlation Between Extent of HIV-Induced Immuno-Suppression and Clinical Manifestation of <strong>Tuberculosis</strong>Pulmonary tuberculosisMedian CD4 cell count / mm 3400300200100Lymphatic, serous tuberculosisTuberculous meningitisDisseminated tuberculosis0Duration of HIV infectionDe Cock KM, et al. J Am Med Assoc 1992;268:1581-7
Diagnostic tools• • • • ® • ®
STOP TB Strategy• GLOBAL (DOTS)– MDG Targets: halt and reverse TB incidence by 2015• Strategy: Directly Observed Treatments Short-course (DOTS)has 5 elements: i) political commitment with increased andsustained financing ii) case detection through quality-assuredbacteriology iii) standardized treatment with supervision andpatient support iv) an effective drug supply and managementsystem v) monitoring and evaluation system• US (Targeted testing and treating LTBI)– Target TB Elimination by 2010: 1 case per million pop.• 5 areas of decisive action: 1) maintain TB control, 2) acceleratedecline, 3) develop new tools, 4) increase global efforts, 5)mobilize and sustain public support– Hopefully target can be achieved by 2035 or 2107 at the most
Albert CalmetteBacillus Calmette-Guérin = BCG!Camille Guérin• An “attenuated” strain ofMycobacteria that does not causedisease but can stimulate theimmune response• Newer attenuated strain vaccinesand recombinant versions of BCGare now in Phase II and Phase IIIclinical trials