Implementation of Safe Surgery Saves Lives initiative in Ahmed ...
Implementation of Safe Surgery Saves Lives initiative in Ahmed ...
Implementation of Safe Surgery Saves Lives initiative in Ahmed ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Royal College <strong>of</strong> Surgeons <strong>in</strong> Irelande-publications@RCSIMasters theses/dissertations - taught coursesTheses and Dissertations1-1-2011<strong>Implementation</strong> <strong>of</strong> <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong><strong><strong>in</strong>itiative</strong> <strong>in</strong> <strong>Ahmed</strong>-Gasim’s Cardiac Center<strong>Ahmed</strong> AbdallahRoyal College <strong>of</strong> Surgeons <strong>in</strong> Ireland, ahmedkhier@hotmail.comCitationAbdallah A. <strong>Implementation</strong> <strong>of</strong> <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong> <strong><strong>in</strong>itiative</strong> <strong>in</strong> <strong>Ahmed</strong>-Gasim’s Cardiac Center. [Masters dissertation]. Dubl<strong>in</strong>:Royal College <strong>of</strong> Surgeons <strong>in</strong> Ireland; 2011.This Dissertation is brought to you for free and open access by the Thesesand Dissertations at e-publications@RCSI. It has been accepted for<strong>in</strong>clusion <strong>in</strong> Masters theses/dissertations - taught courses by an authorizedadm<strong>in</strong>istrator <strong>of</strong> e-publications@RCSI. For more <strong>in</strong>formation, pleasecontact epubs@rcsi.ie.
— Use Licence —Creative Commons LicenceThis work is licensed under a Creative Commons Attribution-Noncommercial-Share Alike 3.0 License.This dissertation is available at e-publications@RCSI: http://epubs.rcsi.ie/mscttheses/4
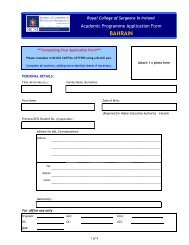
<strong>Implementation</strong> <strong>of</strong> <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong> <strong><strong>in</strong>itiative</strong> <strong>in</strong><strong>Ahmed</strong>-Gasim’s Cardiac CenterStudent ID: 9112723This Change Project report is a dissertation submitted <strong>in</strong> part fulfilment<strong>of</strong> the degree <strong>of</strong> MSc <strong>in</strong> Quality & <strong>Safe</strong>ty <strong>in</strong> Healthcare Management,Institute <strong>of</strong> Leadership,Royal College <strong>of</strong> Surgeons <strong>in</strong> Ireland, Dubl<strong>in</strong>Year 2, Bahra<strong>in</strong>- 2010-20111
Date: 27-06-2011Word Count: 11517Facilitator‟s Name: Dr. Jonathan Drennan2
3.3.4 Ma<strong>in</strong>stream<strong>in</strong>g ........................................................................................................................... 40Chapter 4 Evaluation .............................................................................................................................. 424.1 Introduction ....................................................................................................................................... 424.2 Evaluation Tools ............................................................................................................................... 424.3 Outcomes <strong>of</strong> Change ......................................................................................................................... 434.5. Summary .......................................................................................................................................... 46Chapter 5 Discussion and Conclusion ................................................................................................... 475.1 Introduction ....................................................................................................................................... 475.2 Strengths and limitations <strong>of</strong> the project ............................................................................................ 475.3 Implications <strong>of</strong> the Change for Management .................................................................................... 485.5 Recommendations for Future Improvements .................................................................................... 485.6. Reflections on the Project ................................................................................................................ 495.6 Conclusion ............................................................................................................................................ 514
Table <strong>of</strong> FiguresFigure 1: Map <strong>of</strong> Piloted Cities ..................................................................................................... 10Figure 2: The conceptual framework for the International Classification for Patient <strong>Safe</strong>ty ....... 14Figure 3: WHO Surgical <strong>Safe</strong>ty Checklist .................................................................................... 15Figure 4: Modified Surgical <strong>Safe</strong>ty Checklist .............................................................................. 25Figure 5: HSE Change Model ....................................................................................................... 28Figure 6: Staff Op<strong>in</strong>ion about checklist ........................................................................................ 45Figure 7: The Checklist implementation impact ........................................................................... 455
AbstractAim: This paper reports on the implementation <strong>of</strong> a <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>, <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center <strong>in</strong> 2011 us<strong>in</strong>g a change management framework.Background: Medical errors and <strong>in</strong>cidence <strong>of</strong> traumatic <strong>in</strong>juries <strong>in</strong> surgical care services wererecognized as a proportion <strong>of</strong> the total global burden <strong>of</strong> disease. Surgical care and procedures canpotentially affect the lives <strong>of</strong> millions <strong>of</strong> people worldwide. Studies done by WHO found thatwrong person, wrong procedure, and wrong site surgery is a preventable adverse event, anddef<strong>in</strong>ed a core set <strong>of</strong> m<strong>in</strong>imum standards that can be applied universally across borders andsett<strong>in</strong>gs, and developed a Surgical <strong>Safe</strong>ty Checklist as a tool to ensure safety culture, teamwork,communications, <strong>in</strong>formation hand<strong>of</strong>f, patient <strong>in</strong>volvement, and systematic check <strong>of</strong> processes.Methods: A Users‟ Guide to Manag<strong>in</strong>g Change <strong>in</strong> the Health Service Executive, HSE changemodel with major four phases; <strong>in</strong>itiation, plann<strong>in</strong>g, implementation, and ma<strong>in</strong>stream<strong>in</strong>g, wasused to guide the implementation <strong>of</strong> the <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> Live Initiative through us<strong>in</strong>g theWHO Surgical <strong>Safe</strong>ty Checklist <strong>in</strong> <strong>Ahmed</strong>-Gasim‟ Cardiac Center (AGCC).Results:<strong>Implementation</strong> <strong>of</strong> a surgery checklist improved safety culture, memory recall,communication, team work, systematic check process, and decrease medical errors, such aswrong patient, wrong site, and wrong procedure. <strong>Implementation</strong> <strong>of</strong> a surgery checklist did notdelay cases or <strong>in</strong>crease load <strong>of</strong> work.6
AcknowledgementsI am heartily thankful to my supervisors, Dr. Jonathan Drennan and other supervisors,whose encouragement, guidance and support from the <strong>in</strong>itial to the f<strong>in</strong>al level enabled meto develop an understand<strong>in</strong>g <strong>of</strong> the change project.It is a pleasure to thank those who made this project possible; the leaders, manager, andstaff <strong>of</strong> M<strong>in</strong>istry <strong>of</strong> Health, <strong>Ahmed</strong>-Gasim‟s Cardiac Center, and to change project team.Lastly, I <strong>of</strong>fer my regards and bless<strong>in</strong>gs to all <strong>of</strong> those who supported me <strong>in</strong> any respectdur<strong>in</strong>g the completion <strong>of</strong> the project.7
Chapter 1Introduction1.1 IntroductionThe <strong>in</strong>creas<strong>in</strong>g <strong>of</strong> healthcare services complexity over the past decade and <strong>in</strong>creas<strong>in</strong>g <strong>of</strong> coveragehas led to a correspond<strong>in</strong>g rise <strong>in</strong> the number <strong>of</strong> reported adverse events, def<strong>in</strong>ed as un<strong>in</strong>tended<strong>in</strong>juries caused by medical error rather than the disease process itself (Michel, Quenon, deSarasqueta, & Scemama, 2004). Good documentation and report<strong>in</strong>g systems also helped <strong>in</strong>identify<strong>in</strong>g the size <strong>of</strong> problem, such as <strong>in</strong> the famous report <strong>of</strong> the US Institute <strong>of</strong> Medic<strong>in</strong>enamed „„To Err is Human: Build<strong>in</strong>g a <strong>Safe</strong>r Health System,‟‟ (IOM, 2000). The huge size <strong>of</strong>reported medical errors led to establishment <strong>of</strong> patient safety <strong><strong>in</strong>itiative</strong>, and formation <strong>of</strong> WorldAlliance for Patient <strong>Safe</strong>ty. It was identified as a one <strong>of</strong> the key tasks fac<strong>in</strong>g healthcare at thestart <strong>of</strong> the 21st century. This <strong>Safe</strong>ty concept implementation has succeeded <strong>in</strong> ensur<strong>in</strong>g safety <strong>in</strong>aviation <strong>in</strong>dustry a long before (Donaldson, L J, 2007). By focus<strong>in</strong>g attention on this as a publichealth issue, World Alliance for Patient <strong>Safe</strong>ty was recognized the importance <strong>of</strong> improv<strong>in</strong>g thesafety <strong>of</strong> surgery as the second global patient safety challenge (WHO, 2008).1.2 Rationale for carry<strong>in</strong>g out the changeMedical errors and <strong>in</strong>cidence <strong>of</strong> traumatic <strong>in</strong>juries <strong>in</strong> surgical care services were recognized as aproportion <strong>of</strong> the total global burden <strong>of</strong> disease. Surgical care and procedures can potentiallyaffect the lives <strong>of</strong> millions <strong>of</strong> people worldwide. Studies done by WHO found that wrong person,wrong procedure, and wrong site surgery is a preventable adverse event, and def<strong>in</strong>ed a core set <strong>of</strong>m<strong>in</strong>imum standards that can be applied universally across borders and sett<strong>in</strong>gs, and developed aSurgical <strong>Safe</strong>ty Checklist as a tool to ensure safety culture, teamwork, communications,<strong>in</strong>formation hand<strong>of</strong>f, patient <strong>in</strong>volvement, and check <strong>of</strong> processes. WHO Alliance for Patient<strong>Safe</strong>ty promote apply<strong>in</strong>g those standards through the ““<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>”” program8
(WHO, 2008), hopes to create an environment for improv<strong>in</strong>g both access to and safety <strong>of</strong>surgical care.<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong> program, aims to improve the safety <strong>of</strong> surgical care. Nevertheless thesurgery nowadays is advanced, complicated, and widely practiced <strong>in</strong> almost all healthcarefacilities around the world, and even the advanced <strong>in</strong>vasive procedures such as cardiac surgeryhave been came <strong>in</strong> practice <strong>in</strong> develop<strong>in</strong>g countries.The f<strong>in</strong>al goal <strong>of</strong> the “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” <strong><strong>in</strong>itiative</strong> is to improve surgical outcomes forpatients regardless <strong>of</strong> circumstance or environment. By improv<strong>in</strong>g processes already <strong>in</strong> place <strong>in</strong>operat<strong>in</strong>g theatres safety will be enhanced and quality <strong>in</strong>creased without demand<strong>in</strong>g substantialf<strong>in</strong>ancial <strong>in</strong>vestments <strong>in</strong> health <strong>in</strong>frastructure (WHO, 2008). The WHO Alliance for Patient<strong>Safe</strong>ty designed the <strong><strong>in</strong>itiative</strong> to be simple, widely applicable, and measurable regardless <strong>of</strong> theoperative sett<strong>in</strong>g to ensure adherence to proven standards <strong>of</strong> care <strong>in</strong> all countries. This <strong><strong>in</strong>itiative</strong>piloted <strong>in</strong> eight countries from different WHO regions, economic circumstances and diversepopulations <strong>of</strong> patients, (Hayned, et al., 2009). Hospitals <strong>in</strong> eight cities around the globe havesuccessfully demonstrated that the use <strong>of</strong> a simple surgical checklist, developed by WHO, dur<strong>in</strong>gmajor operations can lower the <strong>in</strong>cidence <strong>of</strong> surgery-related deaths and complications by onethird. Analysis shows that the rate <strong>of</strong> major complications follow<strong>in</strong>g surgery fell from 11% <strong>in</strong> thebasel<strong>in</strong>e period to 7% after <strong>in</strong>troduction <strong>of</strong> the checklist, a reduction <strong>of</strong> one third. Inpatientdeaths follow<strong>in</strong>g major operations fell by more than 40% (from 1.5% to 0.8%). It provedapplicability, efficiency and effectiveness and It reduced mortality and morbidity <strong>in</strong> all eightcenters (Figure 1), from the high-perform<strong>in</strong>g ones to the develop<strong>in</strong>g ones (Hayned, et al., 2009).At least half a million deaths per year would be preventable with worldwide effectiveimplementation <strong>of</strong> the checklist.9
Figure 1: Map <strong>of</strong> Piloted CitiesDerived by this <strong>in</strong>ternational safety issue, <strong>Ahmed</strong>-Gasim‟s Cardiac Center (AGCC) was selectedfor implement<strong>in</strong>g the “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” <strong><strong>in</strong>itiative</strong>. AGCC provides specialized, highrisk and complicated surgical procedures and <strong>in</strong>terventions, where more 400 cardiac operationsdone annually with 5% mortality rate, and not well documented or analyzed morbidity rate.AGCC managers and staff are look<strong>in</strong>g for excellence and safety <strong>of</strong> services. They arechalleng<strong>in</strong>g to be the pioneers <strong>in</strong> implement<strong>in</strong>g this <strong><strong>in</strong>itiative</strong> as a pilot for Khartoum Statehospitals. They feel the need to ensure the safety <strong>of</strong> surgical and <strong>in</strong>vasive procedures. There ismore the 35 major cardiac operations performed <strong>in</strong> AGCC monthly, with 5 % mortality rate andunmeasured poor documented morbidity rate (AGCC , 2011).1.3 Summary<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> live <strong><strong>in</strong>itiative</strong> is a part <strong>of</strong> global patient safety program developed, pilotedand evaluated by the WHO 2007 – 2008. The ma<strong>in</strong> tool used was the “WHO Surgical <strong>Safe</strong>ty10
Checklist”. The aim <strong>of</strong> this program is to ensure surgical safety, and prevent wrong patient,wrong site and wrong procedure. <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> live <strong><strong>in</strong>itiative</strong> as a change project wasimplemented <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center <strong>in</strong> 2011. I was assigned by health authorities <strong>in</strong>the M<strong>in</strong>istry <strong>of</strong> Health (MOH) as change leader. The quality team was selected to assist thechange leader and form the “change project team” responsible for the implementation <strong>of</strong> “<strong>Safe</strong><strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” project. Project team followed the „Users‟ Guide to Manag<strong>in</strong>g Change <strong>in</strong>Health Service Executive‟ (HSE) change model (HSE, 2008) <strong>in</strong> the change process. The changeproject team secured the commitment and participation <strong>of</strong> the policy makers <strong>in</strong> the M<strong>in</strong>istry <strong>of</strong>Health together with managers <strong>of</strong> AGCC <strong>in</strong> the <strong>in</strong>itiation stage, the managers and staff <strong>of</strong> theAGCC were <strong>in</strong>volved by the change project team and comprehensively participated <strong>in</strong> plann<strong>in</strong>g,implement<strong>in</strong>g and ma<strong>in</strong>stream<strong>in</strong>g stages. The use <strong>of</strong> checklist is aim<strong>in</strong>g to improve the teamwork, safety culture, documentation, recall, and safeguard systematic approach <strong>in</strong> processes andsurgical procedures. The direct and immediate goal <strong>of</strong> this change project is to improvecompliance with m<strong>in</strong>imal set <strong>of</strong> evidence based standards and decrease medical errors related tohuman factors.This paper is composed <strong>of</strong> five chapters; <strong>in</strong>troduction, literature review, methods, evaluation, andlast chapter about discussion and conclusion <strong>of</strong> this project.11
Chapter 2Literature Review2.1 IntroductionSearch was done <strong>in</strong> the directories websites <strong>of</strong> World Health Organization (WHO), patient safetyand “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” published document and guidel<strong>in</strong>es, also other healthorganizations such national patient <strong>Safe</strong>ty Agency, and Jo<strong>in</strong>t Commission International (JCI) toget the overview <strong>of</strong> the literature. Which lead to search <strong>of</strong> the <strong><strong>in</strong>itiative</strong> component such as safetyculture, checklist, teamwork, communication and other human factors, at last came up to search<strong>of</strong> implementation <strong>of</strong> WHO Surgical <strong>Safe</strong>ty Checklist.2.2 Patient safety and safe surgeryPatient safety is a relatively new health care discipl<strong>in</strong>e that emphasizes the report<strong>in</strong>g, analysis,and prevention <strong>of</strong> medical errors, which <strong>of</strong>ten lead to patient harm or adverse health care events.Patient safety as def<strong>in</strong>ed by the WHO Alliance is the reduction <strong>of</strong> risk <strong>of</strong> unnecessary harmassociated with healthcare to an acceptable m<strong>in</strong>imum, which <strong>in</strong> turn refers to the collectivenotions <strong>of</strong> given current knowledge, resources available and the context <strong>in</strong> which care wasdelivered weighed aga<strong>in</strong>st the risk <strong>of</strong> non-treatment or other treatment (WHO, 2009). And so it isabout cont<strong>in</strong>uous improvement through build<strong>in</strong>g systems and procedures, on evidence learnedfrom medical errors, it is about risk and change management especially cultural change. Theproblem is well addressed by the landmark Institute <strong>of</strong> Medic<strong>in</strong>e Report To Err is Human (IOM,2000), which explore the size <strong>of</strong> medical errors and questioned the safety <strong>of</strong> healthcare servicesand <strong>in</strong>stitutes <strong>in</strong> USA. The size and magnitude <strong>of</strong> avoidable deaths, <strong>in</strong>juries and other adversepatient events was not well known until the 1990s, when multiple countries reported shock<strong>in</strong>gnumbers <strong>of</strong> patients harmed and killed by medical errors, classify<strong>in</strong>g that healthcare errors affectten percent (10 %) <strong>of</strong> the patients around the world, the World Health Organization calls patient12
safety an endemic concern <strong>in</strong> 2002, WHO Member States agreed on a World Health Assemblyresolution on patient safety and launched the World Alliance for Patient <strong>Safe</strong>ty <strong>in</strong> October 2004.The goal was to develop standards for patient safety and assist the countries to improve thesafety <strong>of</strong> health care. The Alliance raises awareness and political commitment to improve thesafety <strong>of</strong> care and facilitates the development <strong>of</strong> patient safety policy and practice <strong>in</strong> all WHOMember States. Each year, the Alliance for Patient <strong>Safe</strong>ty delivers a number <strong>of</strong> programscover<strong>in</strong>g systemic and technical aspects to improve patient safety around the world (WHO,2008).The result<strong>in</strong>g patient safety knowledge cont<strong>in</strong>ually <strong>in</strong>forms improvement efforts such as:apply<strong>in</strong>g lessons learned from bus<strong>in</strong>ess and <strong>in</strong>dustry, adopt<strong>in</strong>g <strong>in</strong>novative technologies,educat<strong>in</strong>g providers and consumers, enhanc<strong>in</strong>g error report<strong>in</strong>g systems, and develop<strong>in</strong>g neweconomic <strong>in</strong>centives. The safety is basic goal <strong>of</strong> health care services to accomplish this; healthcare providers must <strong>in</strong>corporate safety and quality <strong>in</strong>to their organization to assure appropriatecl<strong>in</strong>ical and adm<strong>in</strong>istrative activities. Over the last decade there has been a grow<strong>in</strong>g <strong>in</strong>ternationalrecognition that health care facilities are dangerous places and constitute significant threats to thesafety <strong>of</strong> patients (War<strong>in</strong>g & harrison, 2006).The shift<strong>in</strong>g away from blam<strong>in</strong>g the <strong>in</strong>dividual to build<strong>in</strong>g safety <strong>in</strong>to reeng<strong>in</strong>eer<strong>in</strong>g <strong>of</strong> processesand systems is a common practice to reduce medical errors. Near misses management proves thevulnerabilities and complexities <strong>of</strong> health care delivery and the need for a safety systems andstandards. Although, to err is human, elim<strong>in</strong>at<strong>in</strong>g “never events” is atta<strong>in</strong>able (Lum & Schachat,2009).The WHO Alliance for patient safety published the conceptual framework aims to provide acomprehensive understand<strong>in</strong>g <strong>of</strong> the area <strong>of</strong> patient safety def<strong>in</strong>ition and program (WHO, 2009).13
The framework aims to represent a cont<strong>in</strong>uous learn<strong>in</strong>g and improvement cycle emphasiz<strong>in</strong>gidentification <strong>of</strong> risk, prevention, detection, reduction <strong>of</strong> risk, <strong>in</strong>cident recovery and systemresilience; all <strong>of</strong> which occur throughout and at any po<strong>in</strong>t with<strong>in</strong> the conceptual framework.Figure 2: The conceptual framework for the International Classification for Patient <strong>Safe</strong>ty<strong>Safe</strong>ty Alliance published ten facts on safe surgery summarized that surgical care and its safedelivery affect the lives <strong>of</strong> about 7 million patient postoperatively out about 234 million majoroperations are performed worldwide every year (WHO, 2008). And accord<strong>in</strong>g to the analysis <strong>of</strong>14
these facts they selected “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” Challenge to be the second goal <strong>of</strong> <strong>Safe</strong>tyAlliance. The aim this <strong><strong>in</strong>itiative</strong> is to improve the safety <strong>of</strong> surgical care around the world byensur<strong>in</strong>g adherence to proven standards <strong>of</strong> care <strong>in</strong> all countries. The expertise developed getbenefit <strong>of</strong> safety approaches <strong>in</strong> aviation and other high risk <strong>in</strong>dustries and developed a checklist(figure 2) as tool to ensure the safety <strong>of</strong> surgery. They estimate this tool will prevent at least halfa million deaths per year with effective implementation <strong>of</strong> the WHO Surgical <strong>Safe</strong>ty Checklistworldwide. These results obta<strong>in</strong>ed <strong>in</strong> the World Health Organization's 2007-2008 pilot study; <strong>of</strong>its Surgical <strong>Safe</strong>ty Checklist and published the <strong><strong>in</strong>itiative</strong> <strong>of</strong> save surgery save lives <strong>in</strong> 2008(WHO, 2008).Figure 3: WHO Surgical <strong>Safe</strong>ty Checklist15
2.3 The checklistHealthcare relies greatly on healthcare specialists‟ ability to recall detailed critical <strong>in</strong>formationdur<strong>in</strong>g medical practice. However, memory is likely to be error prone, result<strong>in</strong>g <strong>in</strong> medical errorsand harm to patients. Many <strong>in</strong>dustries, <strong>in</strong>clud<strong>in</strong>g aviation, factories, operation and ma<strong>in</strong>tenancecompanies and nuclear power, attempted to overcome this particular recall limitation bymandat<strong>in</strong>g checklists. After exam<strong>in</strong><strong>in</strong>g flight deck checklists, Degani and Wiener <strong>in</strong>1993identified several advantages regard<strong>in</strong>g effective checklists.Emerton et al. discussed that the teamwork is def<strong>in</strong>able and measurable and can be improvedthrough formal structured communication, such as checklists. They suggested that theirpr<strong>in</strong>ciples could effectively be applied to other high-risk <strong>in</strong>dustries, such as healthcare, andsurgery <strong>in</strong> particular (Emerton, Panesar, & Forrest, 2009).A checklist is a tool widely used nowadays, to ensure documentation. It provides a valuabletechnique <strong>in</strong> error management. And checklist is compulsive part <strong>of</strong> aviation <strong>in</strong>dustry andproduction processes management <strong>of</strong> factories such as pharmaceutical <strong>in</strong>dustries. A checklist canhave several objectives, <strong>in</strong>clud<strong>in</strong>g memory recall, standardization and regulation <strong>of</strong> processes,procedures or methodologies. Also it provides a framework for supervision <strong>of</strong> work andevaluations, and a diagnostic tool. Though, <strong>in</strong> all uses <strong>of</strong> checklists the central goal is errorreduction or best practice adherence (Vijayasekar & Steele, 2009). The orig<strong>in</strong>s <strong>of</strong> the checklistdate back to 1935 when a long-range bomber designed by Boe<strong>in</strong>g crashed dur<strong>in</strong>g a competition.This accident resulted <strong>in</strong> the death <strong>of</strong> the most technically gifted pilot on board (Gawande ,2007). A few pilots believed that this catastrophe was a result <strong>of</strong> a s<strong>in</strong>gle pilot be<strong>in</strong>g forced toremember countless steps before take-<strong>of</strong>f. Consequently, they designed a set <strong>of</strong> simple step-bystepchecks for take-<strong>of</strong>f, flight, land<strong>in</strong>g and taxi<strong>in</strong>g. This resulted <strong>in</strong> an accumulation <strong>of</strong> 1.816
<strong>Safe</strong>ty culture need a blame free environment where people are able to report errors or nearmisses without fear, but the high cost <strong>of</strong> medical errors which may affect lives and healthgenerates <strong>in</strong>dividual blame culture <strong>in</strong> health care, which def<strong>in</strong>itely impairs the progress <strong>of</strong> asafety culture. One issue is that, while "no blame" is the appropriate for many errors, but certa<strong>in</strong>errors mandate accountability. In an effort to settle the tw<strong>in</strong> needs for no-blame and appropriateaccountability, the concept <strong>of</strong> "just culture" is be<strong>in</strong>g <strong>in</strong>troduced (We<strong>in</strong>er & Lewis). A just culturefocuses on identify<strong>in</strong>g and address<strong>in</strong>g systems issues that lead <strong>in</strong>dividuals to engage <strong>in</strong> unsafebehaviors, while ma<strong>in</strong>ta<strong>in</strong><strong>in</strong>g <strong>in</strong>dividual accountability by establish<strong>in</strong>g zero tolerance forirresponsible behavior. It dist<strong>in</strong>guishes between human error and irresponsible behavior, <strong>in</strong>contrast to an overarch<strong>in</strong>g "no-blame" approach still favored by some. In a just culture, theresponse to an error or near miss is predicated on the type <strong>of</strong> behavior associated with the error,and not the severity <strong>of</strong> the event. For example, irresponsible behavior such as refus<strong>in</strong>g to performa "time-out" prior to surgery would lead to punitive action, even if patients were not harmed.Although the term just culture can be construed broadly, the term is <strong>of</strong>ten more narrowly used torefer to the beliefs, assumptions, and expectations that govern accountability and discipl<strong>in</strong>e forunsafe acts (e.g., near misses, medical errors, and adverse events).Nevertheless safety problem causes and solutions may be outside <strong>of</strong> the powers <strong>of</strong> manypersonnel due to complex systems or procedures which <strong>in</strong>teract <strong>in</strong> difficult to predict wayslead<strong>in</strong>g to a cha<strong>in</strong> <strong>of</strong> events which results <strong>in</strong> an <strong>in</strong>jury, and because many are cross-organization(Øvretveit, 2009).Although illustrat<strong>in</strong>g the extent <strong>of</strong> the shift required <strong>in</strong> terms <strong>of</strong> creat<strong>in</strong>g a safety culture is adifficult task, but the National Patient <strong>Safe</strong>ty Agency – NHS <strong>in</strong> UK has given advice to18
healthcare staff by produc<strong>in</strong>g the Seven Steps to Patient <strong>Safe</strong>ty guide (NPSA, 2004). The sevensteps described are:• Build a safety culture.• Lead and support your staff.• Integrate your risk management activity.• Promote report<strong>in</strong>g.• Involve and communicate with patients and the public.• Learn and share safety lessons.• Implement solutions to prevent harm.To help <strong>in</strong> safety build<strong>in</strong>g WHO published Patient safety curriculum guide for medical schools <strong>in</strong>2009. Where the safety problems classified to: (i) the wrong patient <strong>in</strong> the operat<strong>in</strong>g room (OR);(ii) surgery performed on the wrong side or site; (iii) wrong procedure performed; (iv) failure tocommunicate changes <strong>in</strong> the patient‟s condition; (v) disagreements about stopp<strong>in</strong>g procedures;and (vi) failure to report errors (WHO, 2009).Team work, communication and empowerment <strong>of</strong> staff will help junior doctors or nurses whorarely speak up when they see a senior cl<strong>in</strong>ician about to make an error; this is universal andapplies to all cultures to vary<strong>in</strong>g degrees. However, patient safety pr<strong>in</strong>ciples require thateveryone is responsible for patient safety and should speak up even when they are lower <strong>in</strong> themedical and health-care hierarchy (WHO, 2009).2.5 Nontechnical skills and human factorsThere is grow<strong>in</strong>g evidence that poor non-technical skills can be a major cause <strong>of</strong> error <strong>in</strong>healthcare. Non-technical skills, or human factors, play an important role <strong>in</strong> improv<strong>in</strong>g teamfunction and improv<strong>in</strong>g these skills can drive improvements <strong>in</strong> patient safety and outcome. This19
editorial challenges traditional role stereo-types, and argues that fundamental changes <strong>in</strong> thebehavior <strong>of</strong> pr<strong>of</strong>essionals need to be made, and susta<strong>in</strong>ed, <strong>in</strong> order that the whole team can makea valuable contribution to the patient safety agenda (Odell, 2011). He classified human factors <strong>in</strong>to seven ma<strong>in</strong> categories <strong>of</strong> non-technical skills: 1. Situation awareness. 2. Decision mak<strong>in</strong>g. 3.Communication. 4. Team work<strong>in</strong>g. 5. Leadership. 6. Manag<strong>in</strong>g stress. 7. Cop<strong>in</strong>g with fatigue.Communication is considered an <strong>in</strong>tegral part <strong>of</strong> safety (Hohenfellner, 2009), and Milligandiscussed the role <strong>of</strong> education <strong>in</strong> establish<strong>in</strong>g a culture for patient safety (Milligan, 2007)through study<strong>in</strong>g the too common problem <strong>of</strong> drug adm<strong>in</strong>istration errors is used to illustrate therelevance <strong>of</strong> human factors theory to healthcare education with specific mention made <strong>of</strong> theHuman Factors Analysis and Classification System (HFACS). In this error analysis modelpreconditions <strong>in</strong>clude Environmental Factors, Condition <strong>of</strong> the Individuals and Personnel Factors(USCG, 2005). Personnel Factors classified to1- Self-Imposed Stress such as; (physical fitness, alcohol, drugs/supplements/selfmedication,nutrition, <strong>in</strong>adequate rest and unreported disqualify<strong>in</strong>g medical condition)2- Coord<strong>in</strong>ation/ Communication/Plann<strong>in</strong>g Factors; such as crew/team leadership, crossmonitor<strong>in</strong>gperformance, task delegation, rank/position authority gradient, assertiveness,communicat<strong>in</strong>g critical <strong>in</strong>formation, standard/proper term<strong>in</strong>ology, challenge and reply,mission plann<strong>in</strong>g, mission brief<strong>in</strong>g, task/mission-<strong>in</strong>-progress re-plann<strong>in</strong>g andmiscommunication (USCG, 2005).Poor <strong>in</strong>traoperative communication may compromise patient safety, and so Igor Belyanskyf<strong>in</strong>d<strong>in</strong>gs highlighted the importance <strong>of</strong> communication with<strong>in</strong> the surgical team <strong>in</strong> the prevention<strong>of</strong> untoward patient outcomes (Igor Belyansky, 2011). Also Wiegmann et al. highlighted the20
nature <strong>of</strong> many <strong>of</strong> these work system factors that affect surgical performance <strong>in</strong>clud<strong>in</strong>g theoperat<strong>in</strong>g room environment, teamwork and communication, technology and equipment, tasksand workload factors, and organizational variables (Wiegmann, ElBardissi, Parker, & Sundt,2008).Braaf et al. <strong>in</strong> review found documentation performed by healthcare pr<strong>of</strong>essionals <strong>in</strong> theperioperative environment, such as surgeons‟ operation notes, anesthetists‟ records and nurses‟perioperative notes, has the potential to result <strong>in</strong> communication failure and the delivery <strong>of</strong>suboptimal patient care. Documents such as preoperative checklists have the capacity to be used<strong>in</strong> coord<strong>in</strong>at<strong>in</strong>g verbal communication <strong>of</strong> multidiscipl<strong>in</strong>ary surgical team members with<strong>in</strong> theperioperative environment, thereby improv<strong>in</strong>g patient care (Braaf, Manias, & Riley, 2010)2.6 <strong>Implementation</strong> <strong>of</strong> <strong>Safe</strong> <strong>Surgery</strong> <strong><strong>in</strong>itiative</strong>Although it is a few years s<strong>in</strong>ce the program is published <strong>in</strong> 2008, the implementation widelyachieved <strong>in</strong> many hospitals and surgical centers worldwide. WHO Patient <strong>Safe</strong>ty Alliancecont<strong>in</strong>ues to support the implementation through publish<strong>in</strong>g tra<strong>in</strong><strong>in</strong>g and educational curriculum,brochures, and encourage research <strong>in</strong> this field (WHO, 2009). Also accreditation bodiesproduced and updated their standards, and <strong>in</strong>cluded the safe <strong>Surgery</strong> goal such Jo<strong>in</strong>t CommissionInternational (JCI). They stated <strong>in</strong> the fourth edition JCI Accreditation Standards for Hospitals;<strong>in</strong> the <strong>in</strong>ternational patient goals (IPSG) section (JCI, 2010);IPSG.1 Identify Patients CorrectlyIPSG.2 Improve Effective CommunicationIPSG.3 Improve the <strong>Safe</strong>ty <strong>of</strong> High-Alert MedicationsIPSG.4 Ensure Correct-Site, Correct-Procedure, Correct-Patient <strong>Surgery</strong>IPSG.5 Reduce the Risk <strong>of</strong> Health Care–Associated Infections.21
IPSG.6 Reduce the Risk <strong>of</strong> Patient Harm Result<strong>in</strong>g from Falls.The <strong>Implementation</strong> <strong>of</strong> use <strong>of</strong> the checklist <strong>in</strong> England & Wales commenced <strong>in</strong> February 2009and mandated February 2010. The form was designed for surgery <strong>of</strong> all types, but it was notappropriate for obstetrics and would not be used effectively. Therefore, modified the perioperativesafety checklist to represent the needs <strong>of</strong> an obstetric patient more appropriately wasdesigned (Rao, 2010).The WHO Surgical <strong>Safe</strong>ty Checklist provides a systematic approach towards improv<strong>in</strong>g teamwork and reduc<strong>in</strong>g the perioperative risk <strong>of</strong> harm to the patients.The checklist should be adapted to meet the specific challenges <strong>of</strong> obstetrics and gynecology”(Burbos & Morris, 2011), also <strong>in</strong> urology the Surgical <strong>Safe</strong>ty Checklist was used successfully <strong>in</strong>non-cardiac general surgery for patients at least 16 year <strong>of</strong> age. This success may prompt theEuropean Association <strong>of</strong> Urology to develop a committee <strong>of</strong> experts to extend and modify thechecklist for urologic surgery (Hohenfellner, 2009).In survey conducted for all maxill<strong>of</strong>acial units <strong>in</strong> the Yorkshire region to determ<strong>in</strong>e the use <strong>of</strong> theWHO checklist, the author found all respondents were aware <strong>of</strong> the checklist. Only 45% <strong>of</strong>surgeons were us<strong>in</strong>g the checklist. Those not currently us<strong>in</strong>g the WHO checklist stated that theywere us<strong>in</strong>g an alternative form <strong>of</strong> patient check and most (72%) were us<strong>in</strong>g pre- and postoperativeteam brief<strong>in</strong>gs. (Abdel-Galil, 2010).An <strong>in</strong>teractive analysis identified contextual factors and supportive activities that <strong>in</strong>creaseimplementation effectiveness. Factors <strong>in</strong>clude alignment with <strong>in</strong>stitutional and team values,senior leadership, multidiscipl<strong>in</strong>ary leadership, <strong>in</strong>ternal motivation, physician employment,organizational culture and prior history <strong>of</strong> quality improvement. Activities <strong>in</strong>clude educat<strong>in</strong>g andtra<strong>in</strong><strong>in</strong>g, facilitat<strong>in</strong>g ease <strong>of</strong> use, valu<strong>in</strong>g staff <strong>in</strong>put, modify<strong>in</strong>g the Checklist for local use,22
pilot<strong>in</strong>g, fram<strong>in</strong>g to promote Checklist use, monitor<strong>in</strong>g and provid<strong>in</strong>g feedback (Dante,Gawande, Sara, & Berry, 2010).Qualitative analysis suggested that effectiveness h<strong>in</strong>ges on the ability <strong>of</strong> implementation leadersto persuasively expla<strong>in</strong> why and adaptively show how to use the checklist. Coord<strong>in</strong>ated efforts toexpla<strong>in</strong> why the checklist is be<strong>in</strong>g implemented and extensive education regard<strong>in</strong>g its useresulted <strong>in</strong> buy-<strong>in</strong> among surgical staff and thorough checklist use. When implementation leadersdid not expla<strong>in</strong> why or show how the checklist should be used, staff neither understood therationale beh<strong>in</strong>d implementation nor were they adequately prepared to use the checklist (Dante ,Sara , Lizabeth , William , & Atul , 2011).“Potential problems on the way to successful implementation <strong>of</strong> the checklists may beobstructed by difficulties <strong>in</strong> engag<strong>in</strong>g those <strong>in</strong>dividuals who are reluctant to change. Such<strong>in</strong>dividuals should be encouraged to participate and shown the benefits to the safety <strong>of</strong> patientsand work<strong>in</strong>g practice. The role and responsibility <strong>of</strong> each member <strong>of</strong> the surgical team for thecompletion <strong>of</strong> the checklist should be clarified. Provid<strong>in</strong>g feedback and effective educationdur<strong>in</strong>g the implementation period will help with any unfamiliarity encountered. Regular auditson the implementation <strong>of</strong> the checklist should be part <strong>of</strong> the local practice, the results <strong>of</strong> whichshould be presented to the staff at regular <strong>in</strong>tervals. (Burbos & Morris, 2011)But de-Vries found <strong>in</strong> an observation <strong>of</strong> 170 surgical procedures, more than 50% <strong>of</strong> alldeviations <strong>in</strong> surgical processes occurred before or after surgery. Many <strong>of</strong> these omissions and<strong>in</strong>cidents can and should be corrected at an earlier stage than just before start<strong>in</strong>g surgery, when itcould be too late (De-Vries, 2008). So he suggested a checklist that covers the entire surgicalpathway from admission to discharge, <strong>in</strong>stead <strong>of</strong> just the perioperative phase.23
Barriers to implementation <strong>of</strong> the checklist listed by Mahajan Anxiety <strong>of</strong> unfamiliarity,Hierarchy <strong>of</strong> staff, Logistics and tim<strong>in</strong>g, Duplication, Relevance <strong>of</strong> checklist, Misuse <strong>of</strong> thechecklist (Mahajan R. P., 2011).2.7 SummaryThe medical errors problem is a real challenge fac<strong>in</strong>g the healthcare services. The WHOestablished the WHO Alliance for Patient <strong>Safe</strong>ty to deal with challenge, and f<strong>in</strong>d solutions forsafety problems. The alliance through The “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” <strong><strong>in</strong>itiative</strong> aimed toidentify m<strong>in</strong>imum standards <strong>of</strong> surgical care that can be universally applied across countries andsett<strong>in</strong>gs. A core set <strong>of</strong> safety checks was identified <strong>in</strong> the form <strong>of</strong> a “WHO Surgical <strong>Safe</strong>tyChecklist” that could be used <strong>in</strong> any operat<strong>in</strong>g theatre environment. Each step on the checklist issimple, widely applicable, and measurable, and it has already been demonstrated that its usereduced death and major complications regardless <strong>of</strong> the healthcare economies it was applied to.The checklist was succeeded to improve safety <strong>in</strong> many other high risk <strong>in</strong>dustries, it ensuressystematic check processes, helps recall, enhance communication, encourage teamwork, andpatient <strong>in</strong>volvement.24
Chapter 3Methods3.1 IntroductionThe health care services are subject to cont<strong>in</strong>uous change leaded with the best practice,<strong>in</strong>ternational standards, and grow<strong>in</strong>g needs and expectations <strong>of</strong> customers. This change projectaim to implement the “<strong>Safe</strong> <strong>Surgery</strong> saves lives” through us<strong>in</strong>g the modified <strong>Safe</strong>ty Surgicalchecklist (Figure 3) <strong>in</strong> AGCC, the change process followed the HSE change model.Figure 4: Modified Surgical <strong>Safe</strong>ty Checklist25
3.2 Change processThe implementation <strong>of</strong> modified WHO safety surgical <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center(AGCC) change process is follow<strong>in</strong>g the recommendation <strong>of</strong> WHO Alliance for Patient safety.The “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” challenge is guided by three pr<strong>in</strong>ciples <strong>of</strong> simplicity, wideapplicability and measurability. In addition, WHO alliance confirms that the use <strong>of</strong> this checklistshould not take more than two to three m<strong>in</strong>utes. The modified checklist is consisted <strong>of</strong> fourphases; the first phase is <strong>in</strong>cluded by as adaptation <strong>of</strong> the “WHO surgical safety checklist” tocover the preparation <strong>of</strong> the patient from the outpatient cl<strong>in</strong>ic and ward, the second phase <strong>of</strong> thechecklist can be done by the anesthetic assistant <strong>in</strong> the anesthetic room. The third phase or the„time out‟ can be done by the operat<strong>in</strong>g surgeon before the start <strong>of</strong> the procedure and the f<strong>in</strong>al„sign<strong>in</strong>g out‟ can be done by the surgeon or the anesthetic assistant.The change process is ma<strong>in</strong>ly about check<strong>in</strong>g the risk areas and orally confirm<strong>in</strong>g the processesguidedand documented by checklist execution <strong>of</strong> the follow<strong>in</strong>g steps <strong>in</strong> the mentioned fourphases (WHO, 2009):Preoperative phase: it is start with see<strong>in</strong>g patient <strong>in</strong> outpatient cl<strong>in</strong>ic, the checklist confirm theidentification and <strong>of</strong> correct person, site and procedure by surgeons, anesthetists and nurses,confirm the cl<strong>in</strong>ical notes is complete, the consent is filled and permanent marker <strong>in</strong> performed<strong>in</strong> the operation site.Sign <strong>in</strong> phase: Before <strong>in</strong>duction <strong>of</strong> anesthesia, members <strong>of</strong> the team (at least the nurse and ananesthesia pr<strong>of</strong>essional) orally confirm that: The patient has verified his or her identity, thesurgical site and procedure, and consent. This will <strong>in</strong>sure the participation <strong>of</strong> patient and help <strong>in</strong>prevention <strong>of</strong> wrong person, wrong site, and wrong procedure; the goal four <strong>in</strong> JCI standards(JCI, 2010) also confirm orally systematic check and risk assessment.26
Time out phase:Before sk<strong>in</strong> <strong>in</strong>cision, the entire team confirms orally all team members have been <strong>in</strong>troduced byname and role, patient‟s identity, surgical site, and procedure and systematic review to needed<strong>in</strong>puts and procedures is done.Sign out phaseBefore the patient leaves the operat<strong>in</strong>g room nurse reviews items aloud with the team, name <strong>of</strong>the procedure as recorded, that the needle, sponge, and <strong>in</strong>strument counts are complete , That thespecimen (if any) is correctly labeled and the surgeon, nurse, and anesthesia pr<strong>of</strong>essional reviewaloud the key concerns for the recovery and care <strong>of</strong> the patient.The change process also <strong>in</strong>clude strengthen <strong>of</strong> monitor<strong>in</strong>g and evaluation system, so thecollection <strong>of</strong> the checklist and analysis <strong>of</strong> them is cont<strong>in</strong>uous process, to assess thedocumentation rate, quality, and to measure the compliance <strong>of</strong> staff with safety practice andattitude. Moreover, these data then have to be correlated with the morbidity and mortality rates<strong>of</strong> these patients <strong>in</strong> the hospital, which currently is an entirely separate process to evaluate theimpact <strong>in</strong> long term period.As a change leader, I chose to use and follow the HSE change model throughout the changeprocess because is developed by medical <strong>in</strong>stitute, modern and updated. Also because the HSEchange adopted is an organisation development approach which places a strong focus on thepeople aspects <strong>of</strong> change such as teamwork, communication, participation and cultural change. Itis comb<strong>in</strong>ed with project management which br<strong>in</strong>gs structure and discipl<strong>in</strong>e to the process (HSE,2008).27
3.3 Change modelHSE change model (Figure 5) developed by Organisation Development and Design Unit, as ausers‟ guide to manag<strong>in</strong>g change, it consists <strong>of</strong> four ma<strong>in</strong> <strong>in</strong>teracted phases; <strong>in</strong>itiation, plann<strong>in</strong>g,implementation and ma<strong>in</strong>stream<strong>in</strong>g and has been developed to improve the experience <strong>of</strong>patients and service users, help staff and teams play a mean<strong>in</strong>gful role <strong>in</strong> work<strong>in</strong>g together toimprove services, promote a consistent approach to change across the system (HSE, 2008). Italso fulfill<strong>in</strong>g the effective activities contribut<strong>in</strong>g for effective change is motivat<strong>in</strong>g change,creat<strong>in</strong>g vision for change, develop<strong>in</strong>g political support, manag<strong>in</strong>g the transition <strong>of</strong> change andsusta<strong>in</strong><strong>in</strong>g momentum (Cumm<strong>in</strong>gs & Worley, 2008).The HSE change model was a result <strong>of</strong>adaptation <strong>of</strong> many change models to help change implementation healthcare services (HSE,2008).Figure 5: HSE Change Model28
3.3.1 InitiationThe purpose <strong>of</strong> this early preparation and scop<strong>in</strong>g stage is to create read<strong>in</strong>ess and a consideredcase for change, to establish a sense <strong>of</strong> shared responsibility, and to scope out a solid foundationfor successful change. It builds upon core leadership and management responsibilities (HSE,2008). It is about gett<strong>in</strong>g approval from leaders, and some consultation from experts regard<strong>in</strong>gthe applicability and importance <strong>of</strong> change <strong>in</strong> the selected area.In prepar<strong>in</strong>g to lead the change I started to communicate the idea <strong>of</strong> this change the qualitymanagers <strong>in</strong> the m<strong>in</strong>istry <strong>of</strong> health <strong>in</strong> Khartoum state – Sudan, dur<strong>in</strong>g a tra<strong>in</strong><strong>in</strong>g sessions <strong>of</strong>patient safety where the importance and the need <strong>of</strong> safe surgery discussed, then I approached theleaders <strong>of</strong> the m<strong>in</strong>istry, I expla<strong>in</strong>ed the ma<strong>in</strong> objectives, the rationale, and expected results <strong>of</strong> theproject. I found immediate support, and great appreciation, they assigned me as a project leaderassisted with the quality team <strong>in</strong> the m<strong>in</strong>istry <strong>of</strong> health to start immediately the project. Thechange project team composed <strong>of</strong> five members, the team role was to prepare the policydocuments to policy makers <strong>in</strong> the health authorities, and communicate with and AGCCmanagers and staff, <strong>in</strong>volve them, and ensue their participation and contribution <strong>in</strong> plann<strong>in</strong>g andimplementation <strong>of</strong> the safe surgery <strong><strong>in</strong>itiative</strong> change project. The health authority leaders securethe technical support from the WHO <strong>of</strong>fice.Together with quality team we formed the change project team.In the <strong>in</strong>itiation <strong>of</strong> the project, the change team performed a meet<strong>in</strong>g, where agreed on criteria <strong>of</strong>the piloted area, accord<strong>in</strong>g to that, and out <strong>of</strong> some alternatives the team agreed to select <strong>Ahmed</strong>-Gasim‟s Cardiac Center (AGCC) as a pilot area for implement<strong>in</strong>g the safe surgery saves liveproject. We consulted the managers <strong>of</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center (AGCC) about theapplicability <strong>of</strong> change, and read<strong>in</strong>ess <strong>of</strong> the AGCC. I met the director general <strong>of</strong> AGCC and29
discussed the project, and get the approval and commitment. Then, I commenced the proposalstage, and I started with the change project team members to perform many formal and <strong>in</strong>formalmeet<strong>in</strong>gs, and we performed <strong>in</strong>dividual contacts <strong>in</strong> regular meet<strong>in</strong>g with managers and someexpertise about approaches and needs for change. The AGCC managers had no resistant but they<strong>in</strong>sisted to have approved policy, detailed plan for implementation, and more resources for theirCenter. The team prepared the draft policy, and then I performed a meet<strong>in</strong>g with M<strong>in</strong>istry <strong>of</strong>Health leaders and get approval <strong>of</strong> the f<strong>in</strong>al policy.In plann<strong>in</strong>g stage the change project team prepared and used power po<strong>in</strong>t presentation,brochures, questionnaire, and meet<strong>in</strong>g notes as tools for shar<strong>in</strong>g data, rais<strong>in</strong>g awareness,discussion and mak<strong>in</strong>g decisions. Then, the team executed formal three meet<strong>in</strong>gs with AGCCmanagers and, staff. The team members performed direct contacts and ga<strong>in</strong>ed consultation foradaption <strong>of</strong> checklist and collected the basel<strong>in</strong>e data.The change project clarified leadership roles and identified the key <strong>in</strong>fluencers and stakeholders,and this summarized as followed, the acceptance <strong>of</strong> the leaders <strong>of</strong> health authorities <strong>in</strong> Khartoumwas ga<strong>in</strong>ed, and change project leader and team identified, the policy statement for safe surgeryprepared, discussed and approved. Then the change project team to start to communicate thechange aims with the partners <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center; managers and surgicalservices team‟s leaders. We agreed to Involved them <strong>in</strong> revis<strong>in</strong>g and adapt<strong>in</strong>g the tools anddeterm<strong>in</strong><strong>in</strong>g the preparation needed for the change.The project team performed two meet<strong>in</strong>g to prepare the needed roles and the skills to enable thechange to be successful. The team communicate these rules with the leaders <strong>in</strong> AGCC and getapproval <strong>of</strong> them, also communicate the skills needed with the AGCC staff <strong>in</strong> three differentgroups; the first meet<strong>in</strong>g performed with medical staff <strong>in</strong> the their weekly cl<strong>in</strong>ical morn<strong>in</strong>g30
meet<strong>in</strong>g, where a surpris<strong>in</strong>g event happened, one <strong>of</strong> five cardiac surgeon was participated <strong>in</strong> pilotstudy, when he was <strong>in</strong> Canada <strong>in</strong> 2008, the second meet<strong>in</strong>g with nurs<strong>in</strong>g staff, and the last onewith AGCC quality, <strong>in</strong>fection control, surgical operation managers. Senior managers <strong>of</strong> theAGCC carried the responsibility for the delivery <strong>of</strong> improved the safety <strong>of</strong> services for thecardiac patients, and to be the key change leaders <strong>in</strong> the system. The AGCC formed a local teamresponsible for implementation, to work with change project team composed <strong>of</strong> quality, <strong>in</strong>fectioncontrol, surgical operation and nurs<strong>in</strong>g managers, and support the management and cl<strong>in</strong>icalleaders <strong>in</strong> the change process. The team members was selected accord<strong>in</strong>g to their specialty andresponsibility,The change project team identified the stakeholders <strong>of</strong> this change project <strong>in</strong> groups because thecardiac health service is a complex, multi-sectorial and multi-pr<strong>of</strong>essional environment, andassessed the change impacts on them, there was fears <strong>in</strong>creas<strong>in</strong>g the load <strong>of</strong> work and maydocument the medical errors <strong>of</strong> services providers. But on other hands there is def<strong>in</strong>itely positiveimpact <strong>of</strong> good reputation <strong>of</strong> services providers, and good outcomes for patients. For that thesupport <strong>of</strong> senior cardiac surgeons, quality coord<strong>in</strong>ator and senior nurses was the most importantthe change process. Some resistance was expected from some people <strong>in</strong> the different groups duethe lack <strong>of</strong> knowledge and fears <strong>of</strong> unknown.Despite that the health authorities <strong>in</strong>clud<strong>in</strong>g quality department and <strong>Ahmed</strong>-Gasim‟s cardiaccenter managers have a vested <strong>in</strong>terest <strong>in</strong> the project success, the voice the senior surgeons has tobe heard as the change process is be<strong>in</strong>g planned. So <strong>in</strong>teract<strong>in</strong>g with them and their assistant staffis a must for atta<strong>in</strong><strong>in</strong>g their commitment.31
This <strong>in</strong>teraction must give great care for traditional hierarchy <strong>of</strong> position <strong>of</strong> seniors <strong>of</strong> surgeons,anesthesia, and nurs<strong>in</strong>g groups. The most appropriate way to communicate and <strong>in</strong>volve them isto direct contact and formal and <strong>in</strong>formal meet<strong>in</strong>gs, and consult them <strong>in</strong> every step.Although I am implement<strong>in</strong>g this change project <strong>in</strong> develop<strong>in</strong>g country, but fortunately, AGCCis a high class organization with well-educated staff and good resources. Although, it seems thateveryth<strong>in</strong>g is ready, some build<strong>in</strong>g capacity, teamwork and communications are badly needed tosupport people through the change. The <strong>in</strong>ternal and external factors support the change, somesystems need to improved and developed. Generally, the AGCC culture and the nature <strong>of</strong>relationships between staff <strong>of</strong> teams, and the cardiac surgery services support any improvement.Some efforts, motivation and support needed to from leaders to ma<strong>in</strong>ta<strong>in</strong> the read<strong>in</strong>ess, and thisOn other hands be<strong>in</strong>g a center for heart surgery this help <strong>in</strong> accept<strong>in</strong>g best practices and adopt<strong>in</strong>ghigh standards, also deal<strong>in</strong>g with selected well tra<strong>in</strong>ed staff facilitate the accept<strong>in</strong>g andimplement<strong>in</strong>g the change. The perceived risk is allocation <strong>of</strong> resources<strong>Safe</strong> surgery saves live expected to prevent wrong patient, wrong site and surgical procedurethrough achiev<strong>in</strong>g the follow<strong>in</strong>g objectives and outcomesEnhanc<strong>in</strong>g safety culture and team work to m<strong>in</strong>imize medical errorsPatient <strong>in</strong>volvement <strong>in</strong> safety practiceDocumentation and checklist to elim<strong>in</strong>ate the recall and memoriz<strong>in</strong>g limitationsImprove communicationsUnify<strong>in</strong>g standards and proceduresThere is some weaknesses <strong>in</strong> the quality systems such as poor documentation, us<strong>in</strong>g localstandards, lack <strong>of</strong> well tra<strong>in</strong>ed staff <strong>in</strong> quality and safety system, health <strong>in</strong>formation system,32
The change project team designed <strong>in</strong>itial assessment tool adopted from the surgical checklist, allsurgical units <strong>in</strong> AGCC should be <strong>in</strong>volved through their direct participation <strong>in</strong> meet<strong>in</strong>g and fieldvisits.Systematic approach <strong>of</strong> full process will be documented, checked through <strong>in</strong>volv<strong>in</strong>g the serviceproviders‟ team and patient <strong>in</strong>volvement this will expected to improve the safety <strong>of</strong> service andmake a good reputation for the center and specialty and the whole countryThe services provision strategy and policy, structure and process, people and culture will besubject for change and improvement. The safety culture, and no blame culture should beimproved through team work and learn<strong>in</strong>g process from medical errors.3.3.2 Plann<strong>in</strong>gThe purpose <strong>of</strong> plann<strong>in</strong>g phase is to determ<strong>in</strong>e the specific detail <strong>of</strong> the change and to createsupport for the change process. To communicate the change project with all stakeholders, andbuild organisation-wide commitment because the broader the support, the easier the process willbe. Creat<strong>in</strong>g this support ensures that people are jo<strong>in</strong><strong>in</strong>g <strong>in</strong> a team work, with a clear purpose,<strong>in</strong>tended results and resolve, to create a new future for the organisation (HSE, 2008).I started advocacy along with change team to the health authorities and AGCC leaders andmanagers to build commitment and secure the participation <strong>of</strong> policy makers. And with AGCCsenior staff to a sure their participation <strong>in</strong> adapt<strong>in</strong>g the WHO surgical checklist and develop<strong>in</strong>gimplementation plans, and monitor<strong>in</strong>g and evaluation system. We share the vision <strong>of</strong> the<strong><strong>in</strong>itiative</strong> “<strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>”, with safe culture, safety first concepts and learn<strong>in</strong>g fromerrors with all stakeholders. It is widely communicated and discussed with leaders, managers andservices providers through formal and <strong>in</strong>formal meet<strong>in</strong>gs, posters and tra<strong>in</strong><strong>in</strong>gs sessions. Also thespirit <strong>of</strong> team work was communicated, discussed and agreed on with services providers.33
I reviewed the structure needed for the safe surgery program with change team. We classifiedneeds to; materials such as sk<strong>in</strong> markers, patient identifiers and posters, safety checklists, <strong>in</strong>addition to short tra<strong>in</strong><strong>in</strong>g courses to the staff.The change leader with quality team performed field visit and conducted <strong>in</strong>terviews withmanagers and staff and assessed the current situation, SWOT analysis and force field was used(Tague, 2005).The WHO surgical checklist was compared to practice and gab identified, changeagents were agreed to be the surgeons, anesthetists, nurses and other assistants, they participated<strong>in</strong> modification <strong>of</strong> the checklist by add<strong>in</strong>g the preoperative phase. The results <strong>of</strong> situationanalysis and resources needed reported to the AGCC managers, and tra<strong>in</strong><strong>in</strong>g needed reported toquality department, follow up was done, through two formal meet<strong>in</strong>g with each department,ended by approval <strong>of</strong> required resources and tra<strong>in</strong><strong>in</strong>g. The situation analysis revealed that thereno checklist used <strong>in</strong> surgery. And so there are different practices, and no tool to ensure safety <strong>of</strong>surgery, or enhance teamwork, communication, risk management and systematic check. Thisidentified as gap for improvement.The WHO Surgical <strong>Safe</strong>ty checklist was designed to ensure the m<strong>in</strong>imal required standards forsafety <strong>of</strong> practic<strong>in</strong>g surgery, the WHO checklist was developed to <strong>in</strong>sure teamwork, enhancecommunication between staff, enforce systematic check<strong>in</strong>g, and secur<strong>in</strong>g patient <strong>in</strong>volvement tom<strong>in</strong>imize the human factor <strong>in</strong> medical errors.Then the change project team with the participation <strong>of</strong> AGCC managers and staff developed thedetailed implementation plan. And designed the detail <strong>of</strong> the future state that safety <strong>of</strong> surgerywill be enhanced, though, spread<strong>in</strong>g <strong>of</strong> safety culture concept, effective communication, teamwork, patient <strong>in</strong>volvement, and systematic risk assessment. Also processes and procedure <strong>of</strong>34
perform<strong>in</strong>g the surgery will cont<strong>in</strong>uously adheres to safety rules. The applications <strong>of</strong> all thisstandards will surely have positive impact <strong>in</strong> the f<strong>in</strong>al result <strong>of</strong> the patient management results. Inthe aspects <strong>of</strong> decreas<strong>in</strong>g patient harm, morbidity and mortality rates, on the side <strong>in</strong>creases thepatient satisfactions and services outcome. This will give the AGCC and its staff an excellencereputation.All stakeholders agreed on a detailed plan for implementation, consist <strong>of</strong> adapt<strong>in</strong>g the checklist,avail<strong>in</strong>g the needed materials, tra<strong>in</strong><strong>in</strong>g <strong>of</strong> staff, and plann<strong>in</strong>g the participation and attendance <strong>of</strong>partners to beg<strong>in</strong>n<strong>in</strong>g <strong>of</strong> implementation, also monitor<strong>in</strong>g and evaluation system was designedand approved.3.3.3 <strong>Implementation</strong>The purpose <strong>of</strong> implementation stage focuses on implement<strong>in</strong>g and monitor<strong>in</strong>g the changeproject implementation plan to ensure that it is meet<strong>in</strong>g its purpose. It is vital to signal that thenew ways <strong>of</strong> work<strong>in</strong>g are agreed and be<strong>in</strong>g implemented, and that <strong>in</strong>appropriate model <strong>of</strong>work<strong>in</strong>g are discont<strong>in</strong>ued. Leaders must actively attend to what is actually happen<strong>in</strong>g <strong>in</strong> theorganisation as it is chang<strong>in</strong>g (HSE, 2008).Step 5: Implement<strong>in</strong>g changeThis stage focuses on implement<strong>in</strong>g and monitor<strong>in</strong>g the implementation <strong>of</strong> safe surgery plan toensure that it is meet<strong>in</strong>g its purpose. It is vital to signal that the new ways <strong>of</strong> work<strong>in</strong>g are agreedand be<strong>in</strong>g implemented, and that <strong>in</strong>appropriate model <strong>of</strong> work<strong>in</strong>g are discont<strong>in</strong>ued. Leadersactively attended to what is actually happen<strong>in</strong>g <strong>in</strong> the organisation as it is chang<strong>in</strong>g (HSE, 2008).The change implementation started after the policy and implementation plan approved, I startedas change leader to communicate with <strong>Ahmed</strong>-Gasim‟s cardiac center managers and staff. We35
get the approval from director general <strong>of</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center. <strong>Implementation</strong> teamwas formed <strong>in</strong> the AGCC <strong>in</strong>volved <strong>of</strong> quality, safety and surgical operations coord<strong>in</strong>ators. Directand close contact with the staff was cont<strong>in</strong>ued to raise their awareness.The start<strong>in</strong>g date has been specified accord<strong>in</strong>g to plan discussed and approved with the cardiacsurgeons and the senior staff, and <strong>in</strong> coord<strong>in</strong>ation with AGCC leaders. It has been marked as thedate at which the first patient undergo<strong>in</strong>g surgical <strong>in</strong>tervention is be<strong>in</strong>g subjected to the check<strong>in</strong>gand cross check<strong>in</strong>g procedures.It has been emphasized on <strong>in</strong>sur<strong>in</strong>g that the <strong>in</strong>tended check<strong>in</strong>g and cross check<strong>in</strong>g steps will notcreate any sort <strong>of</strong> disturbance or confusion among the staff, and to avoid patient discomfort aspossible. The personal attendance <strong>of</strong> the change project team was mandated. with theimplementation <strong>of</strong> the program on first group <strong>of</strong> patient was important as all the proceed<strong>in</strong>gefforts practicality is to be judged be how “smooth” is the steps flow ,as well as to providesome sort <strong>of</strong> support with the team ,never the less is to detect any obstacle which may arise <strong>in</strong>order to elim<strong>in</strong>ate it as early as possible .At the preoperative stage <strong>in</strong> the cl<strong>in</strong>ic it was clearly that the new measures taken complies withprevious formerly used ,only that they have been systemized and organized <strong>in</strong> a manner thatfavors the issue <strong>of</strong> the guidel<strong>in</strong>e which is the prevention <strong>of</strong> wrong site ,wrong side ,wrongprocedure and wrong person surgery .At the outpatient department the patient correct name verification along with its match abilitywith the hospital number were carried out as planned by both the adm<strong>in</strong>istrative and cl<strong>in</strong>icalstaff. Some efforts were needed to write the detailed cl<strong>in</strong>ical notes as required by the guidel<strong>in</strong>eas it was stated that certa<strong>in</strong> standards is to followed, this is the same case for the operation36
consent ,as the one previously used did not <strong>in</strong>volve the needed details as required by theguidel<strong>in</strong>e. In this aspect cont<strong>in</strong>uous communication as well as close work<strong>in</strong>g with the staff andpatient and their relatives was needed to overcome this obstacle and to bridge the gap creat<strong>in</strong>gthe needed trust and confidence. This has occurred ma<strong>in</strong>ly due the medico-legal responsibilitiesburden on the staff as the implemented consent required more detailed <strong>in</strong>terventionaldocumentations, a matter which was partially thought to create more constra<strong>in</strong>s on the medicalstaff. This has been dealt with by more communication, so as to make clear that it is certa<strong>in</strong>lynot the aim <strong>of</strong> the program to create any constra<strong>in</strong> nor to crim<strong>in</strong>alize health service providers aswell as not to un<strong>in</strong>tentionally over protect them at the expense <strong>of</strong> the patient.On the other hand the patients were more satisfied with their “empowerment” and <strong>in</strong>volvement<strong>in</strong> the process <strong>of</strong> health care giv<strong>in</strong>g and never the less by the orientation and enlightment.Surgical site mark<strong>in</strong>g was another challenge to face, and with our culture <strong>in</strong> which bodyexposure lies under the strike umbrella <strong>of</strong> culture and tradition, sk<strong>in</strong> mark<strong>in</strong>g had a wide range<strong>of</strong> reaction from both; staff ( medical and adm<strong>in</strong>istrative) and patients themselves ( along withtheir relatives ). This reaction ranged from complete co-operation to hesitancy and uncerta<strong>in</strong>tyfrom patient and to a lesser extent staff. The medical staff was quite co-operative as the medicalbackground assisted to implement procedure. However, patient and their relatives neededadditional efforts as it is always, a new experimentfor the patient to undergo surgical<strong>in</strong>tervention. Some patients quite understood and it was easy to do the mark<strong>in</strong>g, however, for am<strong>in</strong>ority <strong>of</strong> them an extra-effort was needed so as to overcome this matter. Most <strong>of</strong> the hesitatedpatients had the fear <strong>of</strong> possible medical impact to the sk<strong>in</strong> mark<strong>in</strong>g, and <strong>in</strong>quired whether itis similar to traditional tattoo<strong>in</strong>g or not !, a few were quite reluctant <strong>in</strong> the acceptance <strong>of</strong> sk<strong>in</strong>37
mark<strong>in</strong>g, however there was no absolute refusal by the patient nor by their relatives to theprocedure.For the anesthetic preoperative steps it was somehow challeng<strong>in</strong>g as the common practicesregard<strong>in</strong>g the preoperative check is done on table, and <strong>in</strong> most cases a few laboratorial<strong>in</strong>vestigations and blood preparation stand for the preoperative anesthetic check!However, the exist<strong>in</strong>g <strong>in</strong>traoperative check<strong>in</strong>g and documentation system helped much toestablish the preoperative practice required by the guidel<strong>in</strong>e and the checklist. One <strong>of</strong> the<strong>in</strong>terest<strong>in</strong>g remarks <strong>in</strong> this program was that the check<strong>in</strong>g and cross check<strong>in</strong>g helped to create apractice <strong>of</strong> a non –hierarchy supervision, <strong>in</strong> which all those <strong>in</strong>volved <strong>in</strong> the process <strong>of</strong> surgicalpatient care giv<strong>in</strong>g had the means not only to observe other team member documentedperformance, but also had an <strong>in</strong>direct <strong>in</strong>fluence to clam to perform any missed procedure by asenior staff through the mandatory cascade <strong>of</strong> steps and procedure required <strong>in</strong> the program.The presence <strong>of</strong> all supportive documents like X-rays, CT scan, and MRI scan reportsconfirmation by the surgeon and outpatient staff before transferr<strong>in</strong>g the patient to the ward hasbeen carried out by the a delegated medical personnel rather by the surgeons or the anesthetiststhemselves. In the ward the flow <strong>of</strong> procedure was <strong>in</strong> general as required as it matches thepreviously practiced ones.In the operation reception area although the required procedure flue well , some efforts wereneeded to specify the responsible medical personnel to do what was needed and how to beresponsible for the documentation as the operation reception area consists <strong>of</strong> multiple staff .Thenew required procedure for the surgeon to do a preoperative check <strong>in</strong> theoperation reception38
area was yet to encouraged as the culture <strong>of</strong> see<strong>in</strong>g the operated patient on table at theoperation date is still dom<strong>in</strong>at<strong>in</strong>g .An important matter was vital to be considered, which lies <strong>in</strong> the fact that the surgeon is theleader <strong>of</strong> the <strong>in</strong>terven<strong>in</strong>g team, as he is responsible for the essential decision <strong>of</strong> the surgical<strong>in</strong>tervention <strong>in</strong> the first place, and he is the one perform<strong>in</strong>g the ma<strong>in</strong> task <strong>of</strong> it never the less, heis the one to be performed responsible for any degree <strong>of</strong> failure “if th<strong>in</strong>gs went wrong”. For thatfact it was essential at this stage <strong>of</strong> implantation were the peak <strong>of</strong> tension occurs to <strong>in</strong>tervenewith the m<strong>in</strong>imum disturb<strong>in</strong>g way and with as much as diplomacy as possible , i.e. ; to susta<strong>in</strong>the program ma<strong>in</strong>stream keep<strong>in</strong>g the hierarchy <strong>of</strong> the classical surgical team <strong>in</strong> m<strong>in</strong>d .In the operation theater the circulat<strong>in</strong>g nurse was the key personnel to assure the guidel<strong>in</strong>e andcheck list procedures flow are accomplished , as he is only free handed team member with theability to communicate efficiently with all concern<strong>in</strong>g team members , however the presence<strong>of</strong> the guidel<strong>in</strong>e implantation team member was important to guarantee the proper implantationefforts .Many issues emerged dur<strong>in</strong>g the early stages <strong>of</strong> the guidel<strong>in</strong>e and check list implementationwhich was dealt with accord<strong>in</strong>gly, this was expected phases <strong>of</strong> transition <strong>in</strong> any change fromdenial, resistance to exploration to acceptance. As well as the established poor documentationculture and practice. Staff <strong>in</strong>stability yet represent another dragg<strong>in</strong>g factor as the cont<strong>in</strong>uouslyrotat<strong>in</strong>g staff members and their turn over around the hospital units as well as around differenthospitals established the need for cont<strong>in</strong>uous efforts <strong>in</strong>tra<strong>in</strong><strong>in</strong>g , coach<strong>in</strong>g and mentor<strong>in</strong>g.However <strong>in</strong> contrast to the apparently negative impression <strong>of</strong> the staff turn over the success<strong>of</strong> the whole program, it represent a positive factor when extend<strong>in</strong>g the implementation <strong>of</strong> this39
program to other hospitals as staff familiarity to the program will def<strong>in</strong>itely compensate thetime and efforts consumed to overcome the turnover.The tendency to go back to the old practices was dealt with cont<strong>in</strong>uous communication andclose work<strong>in</strong>g with concerned medical personnel emphasiz<strong>in</strong>g on the importance <strong>of</strong> the newprogram and its valuable benefits which to all health care stakeholders.The short term impact <strong>of</strong> the program was monitored be rout<strong>in</strong>e feedbacks ; either personallydur<strong>in</strong>g the <strong>Implementation</strong> or through health provider satisfaction forms which the majority <strong>of</strong>which was <strong>in</strong> favor <strong>of</strong> the program , elicit<strong>in</strong>g the need to extended it to cover other aspects <strong>of</strong><strong>in</strong>terventions.3.3.4 Ma<strong>in</strong>stream<strong>in</strong>gThe purpose <strong>of</strong> ma<strong>in</strong>stream<strong>in</strong>g is to focus attention on the success <strong>of</strong> the change effort and on<strong>in</strong>tegrat<strong>in</strong>g and susta<strong>in</strong><strong>in</strong>g the new ways <strong>of</strong> work<strong>in</strong>g and behav<strong>in</strong>g. This stage also focuses onmechanisms for evaluation and cont<strong>in</strong>uous improvement. It is known that the environment <strong>in</strong>which healthcare operates is constantly chang<strong>in</strong>g. The <strong>in</strong>ternal dynamics <strong>of</strong> the organisation willalso cont<strong>in</strong>ue to change. The new reality for people may never feel as if it has arrived (HSE,2008).In order to susta<strong>in</strong> the change and to preserve the momentum generated by this change project,keep<strong>in</strong>g <strong>in</strong> m<strong>in</strong>d the general behavior, mode <strong>of</strong> th<strong>in</strong>k<strong>in</strong>g and our national health staff a strategy<strong>of</strong> short term bullets was adopted as long term projects applicability faces the common obstacle<strong>of</strong> decrease enthusiasm over time prolongation , An example <strong>of</strong> these bullets was the<strong>in</strong>volvement <strong>of</strong> senior managerial, executive and pr<strong>of</strong>essionals <strong>in</strong> an orient<strong>in</strong>g ceremonialmeet<strong>in</strong>g, other means <strong>of</strong> <strong>in</strong>centives were also used as a reward<strong>in</strong>g act to those tak<strong>in</strong>g the burden40
<strong>of</strong> the project. These <strong>in</strong>centives do not necessary take the form <strong>of</strong> „physical once „but rathermoral and technical means (tra<strong>in</strong><strong>in</strong>g for example) which well have positives impact on the staffcareer.Leadership <strong>in</strong>volvement was essential to guarantee the overall commitment to the project, and <strong>in</strong>order to achieve this it was made clear that the guidel<strong>in</strong>e along with the check list provide asolution for a major scope <strong>of</strong> repeated problem that may drag down his organization andjeopardize his efforts to improve the overall organizational performance and obstruct his / her<strong>in</strong>novative <strong><strong>in</strong>itiative</strong>sLearn<strong>in</strong>g from errors and mistakes was considered as a mean to improve the performance thewhole program at both levels <strong>of</strong> staff and patients and was accomplished by variety <strong>of</strong> means<strong>in</strong>clud<strong>in</strong>g; <strong>in</strong>cidence report<strong>in</strong>g system, focal group discussions, and periodical meet<strong>in</strong>gs withprompt implementation <strong>of</strong> three outputs .Performance review appeared to be mandatory to susta<strong>in</strong> the program momentum as it allows usto estimate the qualitative and quantitative outputs as well as to predict the near and far future <strong>of</strong>the program. Systematic collection the safety surgical checklists, and analysis <strong>of</strong> them is requiredfor assessment, it can be done by the quality coord<strong>in</strong>ator, and periodic discussions <strong>of</strong> results <strong>of</strong>checklist. The <strong>in</strong>tegration <strong>of</strong> the checklist results with the statistical data <strong>of</strong> mortality andmorbidity is highly mandated to evaluate the effectiveness <strong>of</strong> implementation. On the other hand<strong>in</strong>tegrated the tra<strong>in</strong><strong>in</strong>g on safe surgery program with the tra<strong>in</strong><strong>in</strong>g and capacity build<strong>in</strong>g isessential particularly, <strong>in</strong> nurses and jo<strong>in</strong>er doctors because <strong>of</strong> their high turnover.41
Chapter 4Evaluation4.1 IntroductionThe plan will <strong>in</strong>clude identification <strong>of</strong> appropriate metrics for both usage and outcome, andensure report<strong>in</strong>g to quality and safety department. The usage is cont<strong>in</strong>uously monitored andmeasured, it also short term evaluation to measure the implementation <strong>of</strong> the safety surgicalcheck list and the degree <strong>of</strong> compliance <strong>of</strong> the surgical, anesthesia and nurs<strong>in</strong>g staff.The quality and completeness <strong>of</strong> checklists also evaluated to measure the knowledge and attitudeOn other hand the impact <strong>of</strong> implementation <strong>of</strong> the WHO safety surgical checklist on the safety<strong>of</strong> surgical procedures, <strong>in</strong> team <strong>of</strong> m<strong>in</strong>imiz<strong>in</strong>g patient harm and decreas<strong>in</strong>g medical errors, needlong term evaluation through analyz<strong>in</strong>g the checklist and correlate the result with morbidity andmortality <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center, also correlated to improvement <strong>of</strong> safety culture,team work, communication and learn<strong>in</strong>g process.Also the ability <strong>of</strong> AGCC implement<strong>in</strong>g team assessed to carry on the responsibility for ongo<strong>in</strong>gimplementation and monitor<strong>in</strong>g <strong>of</strong> change is an <strong>in</strong>herent part <strong>of</strong> the role <strong>of</strong> all leaders andmanagers <strong>in</strong> the system. It is important, however, the nature <strong>of</strong> this responsibility to build it <strong>in</strong>tothe performance management system with<strong>in</strong> the organisation is not only the role <strong>of</strong> the leaders.4.2 Evaluation ToolsFor short term objectives evaluation <strong>of</strong> correct implementation <strong>in</strong> this change project teamapproves and used the through participation <strong>of</strong> the work<strong>in</strong>g staff the follow<strong>in</strong>g for evaluat<strong>in</strong>gtools; first, focus group discussion with surgeons and their medical staff, anesthesia and theirassistant, nurs<strong>in</strong>g staff, and AGCC managers. Second tool was the direct observations fromoperat<strong>in</strong>g room, wards, and outpatient cl<strong>in</strong>ics. Third tool was the short two questionnaires for all42
medical and nurs<strong>in</strong>g staff before and after implementation, and fourth tool was WHO Surgical<strong>Safe</strong>ty Checklist review.For long term impact <strong>of</strong> the safe surgery program, the change project team recommendedresearches to cover the areas <strong>of</strong> expected morbidity, mortality, medical errors, and near misses.Moreover, other researches to cover the changes and improvements expected happened <strong>in</strong> safetyculture, communication, and team work.4.3 Outcomes <strong>of</strong> ChangeThe WHO safety surgical checklist have been implemented <strong>in</strong> all heart surgical operation roomsand for all types <strong>of</strong> cardiac surgery operations, the implementation process was <strong>in</strong>stitutionalizedand <strong>in</strong>tegrated to the established systems such as quality and safety, audit<strong>in</strong>g, documentation,supply cha<strong>in</strong>, monitor<strong>in</strong>g and evaluation, capacity build<strong>in</strong>g and tra<strong>in</strong><strong>in</strong>g systems.By observation, it was clear that all staff adhere to the new unified standards. One <strong>of</strong> the worthobservation f<strong>in</strong>d<strong>in</strong>gs is that the team work created <strong>in</strong> this program helped to deviate the formerculture and practices <strong>of</strong> handl<strong>in</strong>g patients partially and as separated “ units” , this is to say thatthe communication attitude <strong>in</strong> the new practice <strong>in</strong> addition to patient empowerment tendencyhad shifted the fore mentionedpatients handl<strong>in</strong>g practice to a more humanitarian and<strong>in</strong>tegrated one ; this is to say that as an example ; an on table patient used and is be<strong>in</strong>g handledby two poorly communicated teams ; surgical and anesthetic teams , result<strong>in</strong>g <strong>in</strong> two teamsdeal<strong>in</strong>g with two parts <strong>of</strong> one patient with a quite poor communication , a matter which willobviously <strong>in</strong>crease the risk <strong>of</strong> the undesired adverse events.I performed the first focus discussion with AGCC staff, they agreed that the 19-item checklistagreed <strong>of</strong> simplicity and applicability <strong>of</strong> the checklist, but they mentioned that it needs to be43
adopted so as to the cover the needed practices <strong>in</strong> cardiac surgery <strong>in</strong> AGCC, particularly thepreoperative preparation care that occur <strong>in</strong> the cl<strong>in</strong>ic and wards. Some <strong>of</strong> them particularly two<strong>of</strong> the surgeons questioned the third criterion <strong>of</strong> measurability and raised some doubt. In practicalapplication they commented about the importance <strong>of</strong> quality management system improvement,data management and analysis, tra<strong>in</strong><strong>in</strong>g and capacity build<strong>in</strong>g, <strong>in</strong>creas<strong>in</strong>g the awareness <strong>of</strong>patients and avail<strong>in</strong>g more resources to support the change.Us<strong>in</strong>g simple and short questionnaire, I conducted a survey about the checklist; most <strong>of</strong> the staffagreed as shown <strong>in</strong> figure 6 that the checklist is simple, applicable and takes less than threem<strong>in</strong>utes. Around two third <strong>of</strong> them agreed that the checklist is measurable. Most <strong>of</strong> the staffdecided that the checklist needs adaptation.Figure 7 shown most <strong>of</strong> the staff agreed that the checklist encourage communication, enhancedthe teamwork, helped recall, supported the systematic check and enhanced safety.Almost all staff agreed about the effectiveness <strong>of</strong> the checklist <strong>in</strong> creat<strong>in</strong>g safety culture andsafety practices. This approach <strong>of</strong> risk assessment <strong>in</strong> multidiscipl<strong>in</strong>ary team was provedeffectiveness <strong>in</strong> other high risk <strong>in</strong>dustries such as aviation, factories, and nuclear <strong>in</strong>dustries.In traditional hierarchy the senior <strong>in</strong>hibit the juniors, and doctors give no chance to other teammembers.This leadership skills, management tools, risk management best practice, was brought from other<strong>in</strong>dustries to healthcare services such as <strong>in</strong> the <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> lives.44
Staff Op<strong>in</strong>ion about Checklist87%98%85%95%67%take < 3 m<strong>in</strong>utesneed adaptationmeasurableapplicablesimpleFigure 6: Staff Op<strong>in</strong>ion about checklistChecklist Impact75%92%88%91%97%enhance safetysupportsystematicprocesseshelps recallenhanceteamworkencouragecommunicationsFigure 7: The Checklist implementation impact45
4.5. SummaryDespite that AGCC is not accredited hospital by any national or <strong>in</strong>ternational organization; thereare valued local efforts to improve the quality <strong>of</strong> the services. There is a lot <strong>of</strong> improvementprocesses go<strong>in</strong>g on. Nevertheless, still there was no previous experience with a well-documentedchange project or improvement <strong>in</strong> AGCC.Generally, the project through extensive uses <strong>of</strong> quality tools create a new sense, <strong>in</strong>creased thecommunications, and teamwork culture between the managers and cl<strong>in</strong>ical staff. Due to thenature <strong>of</strong> project itself, the project is <strong>in</strong>troduc<strong>in</strong>g new cultures like leadership, management tools,and management practices to the surgery team such as communications, teamwork, riskmanagement, and systematic check with oral confirmation to the rest <strong>of</strong> team s<strong>in</strong>ce everyth<strong>in</strong>g isdocumented by the checklist. The evaluation <strong>of</strong> the long term impact such as mortality andmorbidity is out <strong>of</strong> the scope <strong>of</strong> this paper, but it is recommended to be done later.The ma<strong>in</strong> aim <strong>of</strong> the project which was implement<strong>in</strong>g the WHO surgical safety checklist wassuccessfully achieved. With regard to the services delivery, the five cardiac surgeons and theirstaff unified work standards, and stick to the safe surgery saves lives guidel<strong>in</strong>es.The all participated <strong>in</strong> design<strong>in</strong>g the change and modify<strong>in</strong>g the checklist. The efforts done <strong>in</strong>communication with them and other staff elim<strong>in</strong>ated the resistance, reduced the fear fromunknown and kept the personal powers as it is. This approach has led to the full <strong>in</strong>volvement <strong>of</strong>all staff, moreover, the belief that this change is their own work, and has led to appreciat<strong>in</strong>g ourefforts <strong>in</strong> <strong>in</strong>itiat<strong>in</strong>g and facilitat<strong>in</strong>g the change process.On the management side, the extensive work done <strong>in</strong> the situation analysis and communicationwith cl<strong>in</strong>ical staff created many improvement projects, and clear the pathways for development.46
Chapter 5Discussion and Conclusion5.1 IntroductionThe HSE change model is enabl<strong>in</strong>g cont<strong>in</strong>uous and ongo<strong>in</strong>g discussion, evaluation, and<strong>in</strong>teract<strong>in</strong>g phases, throughout the <strong>in</strong>itiation, plann<strong>in</strong>g, and implementation and ma<strong>in</strong>stream<strong>in</strong>g.The results <strong>in</strong> short term evaluation confirm and support the <strong>in</strong>ternational experiences with safesurgery <strong><strong>in</strong>itiative</strong> implementation.5.2 Strengths and limitations <strong>of</strong> the projectThe strengths <strong>of</strong> the project embodied <strong>in</strong> the nature <strong>of</strong> it, as it address<strong>in</strong>g safety <strong>in</strong> healthcaresett<strong>in</strong>g provid<strong>in</strong>g a very high risk cases. The attractive vision, global implementation, withevidence based designed tool by WHO expertise, and evaluated outcomes <strong>in</strong> piloted cities andproved effectiveness. On the side the AGCC as highly specialized center, with the best possiblestandards <strong>in</strong> the country, also the highly committed leaders <strong>of</strong> health authorities <strong>in</strong> the m<strong>in</strong>istry <strong>of</strong>Health, and AGCC leaders and managers on all level, this <strong>in</strong> addition, to cooperative welleducatedstaff, and fortunately, one <strong>of</strong> the surgeons participated <strong>in</strong> the WHO pilot study when hewas <strong>in</strong> Canada 2008.The major limit <strong>of</strong> this change project was the time period, where it is not possible to evaluatethe long term impact <strong>of</strong> the Checklist on cardiac surgery <strong>in</strong> AGCC such as reduction <strong>of</strong> mortalityand morbidity rates, <strong>in</strong> spite <strong>of</strong> that the evaluation <strong>of</strong> the impact is not one <strong>of</strong> aims <strong>of</strong> the projectto validate the tool because it is already evaluated by WHO pilot study <strong>in</strong> 2008. Also, limitations<strong>of</strong> AGCC work systems <strong>of</strong> quality, cha<strong>in</strong> supply, and tra<strong>in</strong><strong>in</strong>g. No function<strong>in</strong>g report<strong>in</strong>g system<strong>of</strong> <strong>in</strong>cidence and near misses, limited used <strong>of</strong> available technology and paper based medical47
ecords, <strong>in</strong>stability <strong>of</strong> staff and managers, due to lack <strong>of</strong> f<strong>in</strong>ancial motivation and attractionmigration, specially nurses and junior doctors.Also be<strong>in</strong>g carried <strong>in</strong> develop<strong>in</strong>g country the resources is to extent represent one <strong>of</strong> the basiclimitation specially <strong>in</strong> ma<strong>in</strong>stream<strong>in</strong>g phase, because the tra<strong>in</strong>ed staff is not motivated andreta<strong>in</strong>ed used to migrate, on other hand the quality and safety systems need to be improvedspecially the report<strong>in</strong>g system <strong>of</strong> <strong>in</strong>cidence and near misses which need more resources.5.3 Implications <strong>of</strong> the Change for ManagementThis change project with this great contribution <strong>of</strong> leaders, managers, and senior staff represent adifferent experience and create new spirit toward safety and quality applications. Extensive use<strong>of</strong> quality tool, capacity build<strong>in</strong>gs, communication and teamwork establish new culture to thepr<strong>of</strong>essionals such as cardiac surgeons. The f<strong>in</strong>d<strong>in</strong>g <strong>of</strong> the evaluation confirms the <strong>in</strong>ternationalexperiences <strong>in</strong> the impact <strong>of</strong> the checklist implementation <strong>in</strong> creat<strong>in</strong>g teamwork, communication,and recall, through systematic check and orally team confirmation.On the side <strong>of</strong> service delivery implications, it improved the patient <strong>in</strong>volvement, to ensure thecorrect person, correct site, and correct procedure. All cardiac surgical units applied the” <strong>Safe</strong><strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>” <strong><strong>in</strong>itiative</strong> <strong>in</strong> all heart operations. This resulted <strong>in</strong> new safety culture,unify<strong>in</strong>g the practice; to best practice, documentation systems strengthen<strong>in</strong>g, and report<strong>in</strong>gsystem for surgical errors established as a part <strong>of</strong> patient safety, enforce systemic check for riskarea and orally confirmation <strong>of</strong> ma<strong>in</strong> procedures.5.5 Recommendations for Future ImprovementsThis project data “the checklist data” should be computerized and connected with the patientmedical records and statistical departments. Quality management systems should be strengthened48
y improv<strong>in</strong>g the report<strong>in</strong>g system develop<strong>in</strong>g such as <strong>in</strong>cidence, near miss events report<strong>in</strong>gsystem. Also <strong>in</strong>fection controls program need some improvement. More studies, researches arerequired to measure the impact <strong>of</strong> the implementation on the patient morbidity and mortality.Human resources tra<strong>in</strong><strong>in</strong>g and reta<strong>in</strong><strong>in</strong>g should be strengthen.5.6. Reflections on the ProjectLeaded with my beliefs <strong>in</strong> Jack Welch‟s quote "If the rate <strong>of</strong> change on the outside exceeds therate <strong>of</strong> change on the <strong>in</strong>side, then the end is <strong>in</strong>side”. Dur<strong>in</strong>g the implementation <strong>of</strong> this project Iwas confident with the idea <strong>of</strong> the project s<strong>in</strong>ce it is a best practice developed and evaluated byWorld Health Organization (WHO). This confidence <strong>in</strong>creased with the nice deal<strong>in</strong>g and respect<strong>of</strong>fered to me by the leaders, manager and staff, and deal<strong>in</strong>g with I as expert and change leader.This greatly helped me to overcome obstacles and expected resistance. Despite all that, I wasalways th<strong>in</strong>k<strong>in</strong>g about how to fix a change <strong>in</strong> a chang<strong>in</strong>g environment s<strong>in</strong>ce people, ideas, tools,and resources are always chang<strong>in</strong>g.Second th<strong>in</strong>g that made me worried <strong>in</strong> the beg<strong>in</strong>n<strong>in</strong>g <strong>of</strong> this project was the fact <strong>of</strong> implement<strong>in</strong>gthis best practice <strong>in</strong> a develop<strong>in</strong>g country, suffer<strong>in</strong>g a week management system and poorresources. But my feel<strong>in</strong>g was completely overturned.I really surprised with the effect <strong>of</strong> team work, communication, <strong>in</strong>volvement and participation <strong>in</strong>elim<strong>in</strong>at<strong>in</strong>g the resistance, and enabl<strong>in</strong>g the change to happen. All partners who participated <strong>in</strong>this change feel the ownership <strong>of</strong> it. I th<strong>in</strong>k this is one <strong>of</strong>49
Day by day, I really rediscovered my country, my people who have a great capacity and goodmanagement <strong>of</strong> resources.It was the happiest event to f<strong>in</strong>d that one <strong>of</strong> five cardiac surgeons <strong>in</strong> AGCC had participated <strong>in</strong>the pilot study <strong>in</strong> Toronto <strong>in</strong> Canada. Now he is lead<strong>in</strong>g the implementation change among theAGCC staff and act<strong>in</strong>g as a technical advisor for them. He is one <strong>of</strong> ma<strong>in</strong> factors to susta<strong>in</strong> thechange.Stage 3: EvaluationDespite that AGCC is not accredited hospital by any national or <strong>in</strong>ternational organization; thereare valued local efforts to improve the quality <strong>of</strong> the services. There is a lot <strong>of</strong> improvementprocesses go<strong>in</strong>g on. Nevertheless, still there was no previous experience with a well-documentedchange project or improvement <strong>in</strong> AGCC.Generally, the project through extensive uses <strong>of</strong> quality tools create a new sense, <strong>in</strong>creased thecommunications, and teamwork culture between the managers and cl<strong>in</strong>ical staff. Due to thenature <strong>of</strong> project itself, the project is <strong>in</strong>troduc<strong>in</strong>g new cultures like leadership, management tools,and management practices to the surgery team such as communications, teamwork, riskmanagement, and systematic check with oral confirmation to the rest <strong>of</strong> team s<strong>in</strong>ce everyth<strong>in</strong>g isdocumented by the checklist.The evaluation <strong>of</strong> the long term impact such as mortality and morbidity is out <strong>of</strong> the scope <strong>of</strong> thispaper, but it is recommended to be done later.The ma<strong>in</strong> aim <strong>of</strong> the project which was implement<strong>in</strong>g the WHO surgical safety checklist wassuccessfully achieved.50
5.6 ConclusionThe implementation <strong>of</strong> safe <strong>Surgery</strong> program <strong>in</strong> <strong>Ahmed</strong>-Gasim‟s Cardiac Center, was succeededto prove applicability and simplicity. And improved the safe culture <strong>in</strong> surgery, and put vision toother required improvement In AGCC, and create a function<strong>in</strong>g team with confidence to applythe future changes, all staff have a positive experience with change management. The expansion<strong>of</strong> implementation <strong>of</strong> this project to other hospital and surgical specialties is now <strong>in</strong> plann<strong>in</strong>gstage. The HSE change model is very powerful framework, putt<strong>in</strong>g great effort on the <strong>in</strong>itiationphase which lead to the <strong>in</strong>volvement <strong>of</strong> other partners <strong>in</strong> plann<strong>in</strong>g phase and secure theircommitment to the implementation, and ma<strong>in</strong>stream<strong>in</strong>g phases. It is very suitable for thehealthcare services improvement projects.51
ReferencesAbdel-Galil, K. (2010). The WHO Surgical <strong>Safe</strong>ty Checklist: are we measur<strong>in</strong>g up? British Journal <strong>of</strong> Oraland Maxill<strong>of</strong>acial <strong>Surgery</strong>, 48(5), 397-398.AGCC . (2011, June 15). <strong>Ahmed</strong>-Gasim Cardiac Center monthly Reports. Khartoum, Sudan.Braaf, S., Manias, E., & Riley, R. (2010). The role <strong>of</strong> documents and documentation <strong>in</strong> communicationfailure across the perioperative pathway. A literature review. International Journal <strong>of</strong> Nurs<strong>in</strong>gStudies.Burbos, N., & Morris, E. (2011). Apply<strong>in</strong>g the World Health Organization Surgical <strong>Safe</strong>ty Checklist toobstetrics and gynaecology. Obstetrics, Gynaecology & Reproductive Medic<strong>in</strong>e, 21(1), 24-26.Cox, S. (1991). The structure <strong>of</strong> employee attitudes to safety a European example Work and Stress. (6),93 - 106.Cumm<strong>in</strong>gs, T. G., & Worley, C. G. (2008). Organization developement change (9 ed.). South Western,Canada.Dante , M. C., Sara , J. S., Lizabeth , E., William , R. B., & Atul , A. G. (2011). Effective Surgical <strong>Safe</strong>tyChecklist <strong>Implementation</strong>. Journal <strong>of</strong> the American College <strong>of</strong> Surgeons, 212(5), 873-879.Dante, M. F., Gawande, A., Sara, S., & Berry, W. (2010). Factors associated with effectiveimplementation <strong>of</strong> a surgical safety checklist. Journal <strong>of</strong> the American College <strong>of</strong> Surgeons,211(3), S108.De-Vries. (2008). WHO’s checklist for surgery: don’t conf<strong>in</strong>e it to the operat<strong>in</strong>g room. Lancet, 1148-1149.Donaldson, L J. (2007). The quest for safer surgery. The Surgeon, 5(6), 324-326.Emerton, M., Panesar, S. S., & Forrest, K. (2009). <strong>Safe</strong>r surgery: how a checklist can make orthopaedicsurgery safer. ORTHOPAEDICS AND TRAUMA, 35(3).Gawande , A. (2007). The checklist. Retrieved 06 17, 2011, from The New Yorker:http://www.newyorker.com/report<strong>in</strong>g/2007/12/10/071210fa_fact_gawande?Hayned, B. A., Weiser, R. T., Berry, R. W., Lipsitz, R. S., Abdel-Hadi, S. B., Dell<strong>in</strong>ger, P. E., et al. (2009). ASurgical <strong>Safe</strong>ty Checklist to Reduce Morbidity and Mortality <strong>in</strong> a Global Population. the NewEngland Journal <strong>of</strong> Medic<strong>in</strong>e, 491-499.Haynes AB, W. T. (2009). <strong>Safe</strong> surgery saves lives Study Group. A surgical safety checklist to reducemorbidity and mortality <strong>in</strong> a global population. New England journal .Hohenfellner, R. (2009). Re: A Surgical <strong>Safe</strong>ty Checklist to Reduce Morbidity and Mortality <strong>in</strong> a Globalpopulation. European Urology, 65(2), 395.52
HSE. (2008, July). Improv<strong>in</strong>g ourservices- A Users’ Guide to Manag<strong>in</strong>g Change <strong>in</strong> the Health ServiceExecutive. (O. D. Unit, Ed.) Dubl<strong>in</strong>: Health Services Executive.Igor Belyansky, T. R. (2011). Poor Resident-Attend<strong>in</strong>g Intraoperative Communication May CompromisePatient <strong>Safe</strong>ty. Journal <strong>of</strong> Surgical Research.IOM. (2000). To Err is Human: Build<strong>in</strong>g a <strong>Safe</strong>r Health System. Institute <strong>of</strong> Medic<strong>in</strong>e, Committee onQuality <strong>of</strong> Health Care <strong>in</strong> America. Wash<strong>in</strong>gton, DC: National Academy Press.JCI. (2010). Jo<strong>in</strong>t Commission InternationalI Accreditation Standards for Hospitals. Ill<strong>in</strong>ois.Lum, F., & Schachat, P. A. (2009). The Quest to Elim<strong>in</strong>ate “Never Events”. Ophthalmology, 116(6), 1021-1022.Mahajan, P. R. (2011). The WHO surgical checklist. Best Practice & Research Cl<strong>in</strong>ical Anaesthesiology,161-168.Mahajan, R. P. (2011). The WHO surgical checklist. Best Practice & resaearch Cl<strong>in</strong>ical Anaesthesiologoy,161-168.Michel, P., Quenon, J., de Sarasqueta, A., & Scemama, O. (2004). Comparison <strong>of</strong> three methods forestimat<strong>in</strong>g rates <strong>of</strong> adverse events and rates <strong>of</strong> preventable adverse events <strong>in</strong> acute carehospitals. BMJ, 328, 199.Milligan, J. F. (2007). Establish<strong>in</strong>g a culture for patient safety – The role <strong>of</strong> education. Nurse EducationToday, 95–102.NPSA. (2004). Seven Steps to Patient <strong>Safe</strong>ty: An Overview Guide for Staff, second pr<strong>in</strong>t. Retrieved 6 12,2011, from national patient safety Agency - NHS: www.npsa.nhs.ukOdell, M. (2011). Human factors and patient safety: Chang<strong>in</strong>g roles <strong>in</strong> critical care. Australian CriticalCare.Øvretveit, J. (2009). Understand<strong>in</strong>g and improv<strong>in</strong>g patient safety: the psychological, social and culturaldimensions. Journal <strong>of</strong> Health Organization and Management, 23(6).Rao, K. (2010). Surgical safety checklists <strong>in</strong> obstetrics. International Journal <strong>of</strong> Obstetric Anesthesia, 19,235–240.Sukhmeet S. Panesar, A. C.-S. (2010). The WHO Surgical <strong>Safe</strong>ty Checklist – Junior doctors as agents forchange. International Journal <strong>of</strong> <strong>Surgery</strong>, 8, 414- 416.Sukhmeet, S., Carson-Stevens, A., Fitzgerald, J. E., & Emerton, M. (2010). The WHO Surgical <strong>Safe</strong>tyChecklist – Junior doctors as agents for change. International Journal <strong>of</strong> <strong>Surgery</strong>, 8(6), 414-416.Tague, R. N. (2005). The Quality Toolbox. Mliwaukee, USA: Amerca<strong>in</strong> Society for Quality "ASQ ".53
The Lancet. (2008). WHO's patient-safety checklist for surgery. The Lancet, 372(9632).USCG. (2005). Department <strong>of</strong> Defense Human Factors Analysis and Classification System A mishap<strong>in</strong>vestigation and data analysis tool. Retrieved June 15, 2011, from Un<strong>in</strong>ted states Coast Gaurd:http://www.uscg.mil/safety/docs/ergo_hfacs/hfacs.pdfVijayasekar, c., & Steele, R. J. (2009). The World Health Organization's surgical safety checklist. TheSurgeon, 7(5), 260-262.War<strong>in</strong>g, j., & harrison, S. (2006). <strong>Safe</strong>ty and complexity: Inter-departmental relationships as a threat topatient safety <strong>in</strong> the operat<strong>in</strong>g department. Journal <strong>of</strong> Health Organization and Management,20(3).We<strong>in</strong>er, B. J., & Lewis, M. A. (n.d.). The mean<strong>in</strong>g <strong>of</strong> justice <strong>in</strong> safety <strong>in</strong>cident report<strong>in</strong>g. Social Science &Medic<strong>in</strong>e, 6(2), 403-413.WHO. (2008, June 24). 10 facts on safe surgery. Retrieved Jun1 20, 2011, from www.who.<strong>in</strong>t:http://www.who.<strong>in</strong>t/features/factfiles/safe_surgery/en/<strong>in</strong>dex.htmlWHO. (2008). Patient safety <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>. Retrieved 06 09, 2011, from www.who.<strong>in</strong>t:http://www.who.<strong>in</strong>t/patientsafety/safesurgery/en/WHO. (2008). patient safety <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong> The Second Global Patient <strong>Safe</strong>ty Challenge.Retrieved 5 4, 2011, from World Health organization:http://www.who.<strong>in</strong>t/patientsafety/safesurgery/en/<strong>in</strong>dex.htmlWHO. (2009). More Than Words: Conceptual Framework for the International Classification for patientsafety. World health organization, Alliance for Patient safety. Geneva: WHO.WHO. (2009). WHO Guidel<strong>in</strong>es for <strong>Safe</strong> <strong>Surgery</strong> 2009 <strong>Safe</strong> <strong>Surgery</strong> <strong>Saves</strong> <strong>Lives</strong>.WHO. (2009). WHO Patient <strong>Safe</strong>ty Curriculum Guide for Medical Schools. Geneva: World HealthOrganization. II.World Alliance for Patient safety.Wiegmann, A. D., ElBardissi, W. A., Parker, H. S., & Sundt, M. T. (2008). Improv<strong>in</strong>g cardiac surgical care: Awork systems approach. Applied Ergonomics, 701-712.54