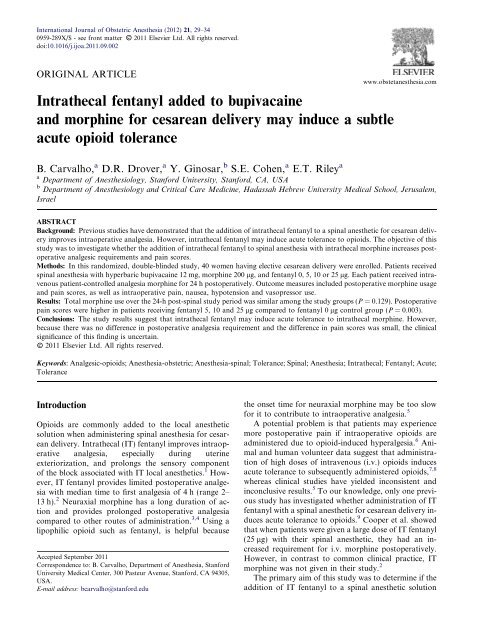
Intrathecal fentanyl added to bupivacaine and ... - Thblack.com
Intrathecal fentanyl added to bupivacaine and ... - Thblack.com
Intrathecal fentanyl added to bupivacaine and ... - Thblack.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
30 <strong>Intrathecal</strong> <strong>fentanyl</strong> <strong>and</strong> acute <strong>to</strong>lerancecontaining IT morphine induces acute opioid <strong>to</strong>lerance,quantified by increased pos<strong>to</strong>perative morphine requirements<strong>and</strong> pain scores. The secondary aim was <strong>to</strong> determineif there is a dose–response associated with thisphenomenon. Our null hypothesis was that the additionof IT <strong>fentanyl</strong> would not change pos<strong>to</strong>perative analgesicuse or pain scores.MethodsA <strong>to</strong>tal of 40 patients were enrolled (10 per group) inthis r<strong>and</strong>omized, double-blinded, controlled, dose-rangingstudy after obtaining Institutional Review Board approval<strong>and</strong> written informed consent. We enrolledhealthy women (American Society of Anesthesiologistsphysical status 1 or 2) with term single<strong>to</strong>n pregnancies(>37 weeks of gestation) undergoing elective cesare<strong>and</strong>elivery under spinal anesthesia before noon. Patientswere excluded from study participation if they met anyof the following criteria: morbid obesity (body mass index>40 kg/m 2 ), planned postpartum tubal ligation, previousadverse reaction <strong>to</strong> opioid medications or his<strong>to</strong>ryof chronic opioid use.The spinal anesthetic was administered with a 25-gauge Whitacre needle (B. Braun Medical, Bethlehem,PA, USA) at the L2–3 or L3–4 intervertebral space withthe patient in the sitting position. Each participant receivedIT hyperbaric <strong>bupivacaine</strong> 12 mg <strong>and</strong> preservative-freemorphine sulfate 200 lg (Astramorph PF,APP Pharmaceuticals LLC, Schaumburg, IL, USA)with an <strong>added</strong> r<strong>and</strong>omized dose of 0, 5, 10 or 25 lg IT<strong>fentanyl</strong> (Baxter Healthcare Corporation, Deerfield,IL, USA). R<strong>and</strong>omization was by <strong>com</strong>puter-generatedr<strong>and</strong>om-number allocation. The mixture was diluted <strong>to</strong>a <strong>to</strong>tal of 2.5 mL with sterile saline. The investiga<strong>to</strong>r,patient, anesthesiologist treating the patient, <strong>and</strong> allstudy staff remained blinded <strong>to</strong> the assigned treatment.An anesthesiologist not involved in the study or patientcare prepared the <strong>fentanyl</strong> doses.Patients were immediately placed supine with leftuterine displacement after the spinal anesthetic wasadministered. The height of the spinal block was assessedby pinprick <strong>and</strong> <strong>to</strong>uch every 2 min until the blockreached the T4 derma<strong>to</strong>me bilaterally. Intraoperative vital-signmeasurements included: mean arterial pressuremeasured with a non-invasive blood pressure moni<strong>to</strong>r,heart rate, respira<strong>to</strong>ry rate <strong>and</strong> oxygen saturation.Ephedrine was given in 5-mg increments <strong>to</strong> treat sys<strong>to</strong>licarterial pressure
B. Carvalho et al. 31after 12 h. Two patients dropped out because of pos<strong>to</strong>perativepain: one in the <strong>fentanyl</strong> 5 lg group who had<strong>com</strong>plete data until 8 h, <strong>and</strong> another in the <strong>fentanyl</strong>25 lg group who had <strong>com</strong>plete data until 12 h. Therefore,partial data for three patients <strong>and</strong> <strong>com</strong>plete datafor 37 patients were analyzed. There were no statisticallysignificant differences in the demographics amonggroups with respect <strong>to</strong> age, height, weight, gestationalage <strong>and</strong> parity (Table 1).Total pos<strong>to</strong>perative PCA morphine consumption didnot differ among the groups (Fig. 1). Pos<strong>to</strong>perative painscores during the study period are outlined in Fig. 2.There was a significant difference between the pos<strong>to</strong>perativepain AUC with increasing <strong>fentanyl</strong> doses (Tau0.38, P = 0.003, Kendal correlation test). The median[interquartile range] pain AUC in the <strong>fentanyl</strong> 0 lg controlgroup was 267 [120–360] mm.h, <strong>com</strong>pared with 487[367–760] mm.h in the <strong>fentanyl</strong> 5 lg group (P = 0.018),520 [381–647] mm.h in the <strong>fentanyl</strong> 10 lg group(P = 0.007), <strong>and</strong> 608 [483–757] mm.h in the <strong>fentanyl</strong>25 lg group (P = 0.023). There was a poor correlationbetween pain, AUC <strong>and</strong> <strong>to</strong>tal morphine consumption(q = 0.194; P = 0.265).There were no significant differences in pos<strong>to</strong>perativeoxygen saturation or respira<strong>to</strong>ry rate between thegroups. At no time did any patient have an oxygen saturation
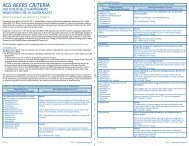
32 <strong>Intrathecal</strong> <strong>fentanyl</strong> <strong>and</strong> acute <strong>to</strong>leranceTable 2Incidence of intraoperative pain <strong>and</strong> nausea requiring treatment0 lg(n = 10)5 lg(n = 10)Fentanyl dose10 lg(n = 10)Patients requiring treatment for pain 2 0 0 1Patients requiring treatment for nausea 4 * 0 2 0Data are number of patients per group. * There was a significant difference <strong>com</strong>pared <strong>to</strong> the <strong>fentanyl</strong> groups <strong>com</strong>bined (P = 0.031).25 lg(n = 10)Table 3Intraoperative hemodynamic data0 lg(n = 10)5 lg(n = 10)Fentanyl dose10 lg(n = 10)25 lg(n = 10)Mean BP (mmHg) 70 ± 5 71 ± 7 77 ± 26 70 ± 15Minimum BP (mmHg) 59 ± 7 57 ± 11 55 ± 9 56 ± 20Ephedrine dose (mg) 17 ± 10 13 ± 11 19 ± 10 19 ± 15Data are mean ± SD. There were no significant differences among the groups. BP: blood pressure.DiscussionOur primary objective was <strong>to</strong> investigate if clinically significantacute <strong>to</strong>lerance <strong>to</strong> opioids developed with theaddition of IT <strong>fentanyl</strong> <strong>to</strong> a <strong>bupivacaine</strong> spinal anestheticsolution containing IT morphine. This was assessed bymeasuring the pos<strong>to</strong>perative i.v. morphine requirement<strong>and</strong> pos<strong>to</strong>perative pain for patients who had received IT<strong>fentanyl</strong> in doses 5, 10, <strong>and</strong> 25 lg <strong>com</strong>pared <strong>to</strong> a no-<strong>fentanyl</strong>group. We expected that if acute <strong>to</strong>lerance occurred,the amount of morphine consumed <strong>and</strong> pos<strong>to</strong>perativepain experienced would be greater for the patients whowere given <strong>fentanyl</strong> versus no <strong>fentanyl</strong>, assuming subjectsin each group used the PCA <strong>to</strong> treat their pain <strong>to</strong> the samelevel. In addition, morphine usage <strong>and</strong> pain would likelyincrease successively with increasing doses of IT <strong>fentanyl</strong>if there was a dose response associated with IT <strong>fentanyl</strong>dose <strong>and</strong> acute <strong>to</strong>lerance.Our study did not find any significant difference inpos<strong>to</strong>perative morphine usage with increasing <strong>fentanyl</strong>dosages. However, pain scores over the first 24 h aftersurgery, as measured by AUC, were increased in thegroups receiving IT <strong>fentanyl</strong>. Our assumption that patientswould self-administer the PCA <strong>to</strong> keep their painlevels the same across groups was incorrect, whichmakes interpretation of the data difficult. Patients whoreceived IT <strong>fentanyl</strong>, on average, did not treat themselves<strong>to</strong> the same pain level as the patients not receivingIT <strong>fentanyl</strong>. A number of fac<strong>to</strong>rs may influence morphineuse including side effects such as nausea, patientpreferences for analgesics <strong>and</strong> concerns for exposure ofmedication <strong>to</strong> breast-feeding infants. 10 However, wedid not measure or control for these fac<strong>to</strong>rs <strong>and</strong> potentialconfounders. In addition, large inter-patient variabilityin PCA use (24-h morphine doses ranged from3 <strong>to</strong> 68 mg) made opioid consumption data difficult <strong>to</strong>interpret. A post-hoc power calculation based on meanPCA use, showed that we would require 170 patients(control group 42: <strong>fentanyl</strong> group 128) <strong>to</strong> have enoughpower <strong>to</strong> have shown a difference in analgesic use (SD10.75 mg, power 0.8, alpha 0.05). Although the higherpos<strong>to</strong>perative pain scores in patients receiving <strong>fentanyl</strong>did not result in increased analgesic use, we believe thatthe differences in pain scores suggests that intrathecal<strong>fentanyl</strong> may induce acute opioid <strong>to</strong>lerance when ITmorphine is included in the spinal anesthesia solution.One limitation with our study design is that it doesnot allow us <strong>to</strong> definitively differentiate if IT <strong>fentanyl</strong> resultsin <strong>to</strong>lerance <strong>to</strong> the IT morphine administered in thespinal solution or the i.v. PCA morphine used <strong>to</strong> treatpos<strong>to</strong>perative pain. Differentiation between IT <strong>and</strong> i.v.morphine <strong>to</strong>lerance could have occurred if only non-opioidswere administered for pos<strong>to</strong>perative analgesia,however, we felt that non-opioids (non-steroidal antiinflamma<strong>to</strong>rydrugs, acetaminophen) would provideinadequate post-cesarean analgesia <strong>and</strong> could not beethically justified at our institution.Four patients in the control group versus two patientsin all the <strong>fentanyl</strong> groups <strong>com</strong>bined required treatmentfor intraoperative nausea (P = 0.031). A numberof other studies have shown less intraoperative pain<strong>and</strong> nausea when <strong>fentanyl</strong> is <strong>added</strong> <strong>to</strong> the local anestheticfor spinal anesthesia. 2,11–15 <strong>Intrathecal</strong> <strong>fentanyl</strong>blunts the noxious input from visceral afferents thatare stimulated by pulling on the peri<strong>to</strong>neal structures<strong>and</strong> exteriorization or manipulation of the uterus. 16These visceral afferent stimuli can manifest clinicallyas nausea, vomiting or cramping <strong>and</strong> do not appear <strong>to</strong>be blocked <strong>com</strong>pletely with the local anesthetic blockalone. Even when IT morphine 200 lg was <strong>added</strong>, asin this study, visceral stimuli appeared <strong>to</strong> be inadequatelyblocked in the absence of IT <strong>fentanyl</strong>. Althoughhypotension can cause nausea <strong>and</strong> be a potential confounder,there was no evidence in our study that patients
B. Carvalho et al. 33treated for nausea had more hypotension than the otherpatients. The intraoperative benefit of using IT <strong>fentanyl</strong>suggested in this study <strong>and</strong> a number of previous studiesappears <strong>to</strong> outweigh the potential for inducing acutepos<strong>to</strong>perative <strong>to</strong>lerance.An important message from the data in this study,<strong>and</strong> other studies of post-cesarean delivery pain 4,17–19is the variability in the pos<strong>to</strong>perative analgesic use <strong>and</strong>pain scores across all groups. The phenomenon of acute<strong>to</strong>lerance that we were studying accounted for very littleof the variation in the amount of pain or analgesia required.For example, the range of morphine doses usedby any group was three times the median dose in thegroups. Large inter-patient variability in opioid use isnot unique <strong>to</strong> this study. 20Although this study was underpowered <strong>to</strong> show smalldifferences among groups, we found no apparent benefitwith larger IT <strong>fentanyl</strong> doses. These findings are consistentwith those of Hunt et al., who studied IT <strong>fentanyl</strong>doses, ranging from 2.5 <strong>to</strong> 50 lg in <strong>com</strong>bination withIT <strong>bupivacaine</strong> for cesarean delivery. 21 They found improvedintraoperative analgesia <strong>com</strong>pared <strong>to</strong> <strong>bupivacaine</strong>alone, but minimal additional benefit beyond IT<strong>fentanyl</strong> doses of 6.25 lg <strong>and</strong> interestingly also no differencein pos<strong>to</strong>perative morphine use amongst the groups.Side effects from IT opioids are dose-dependent <strong>and</strong> largerdoses of <strong>fentanyl</strong> may increase the risk of respira<strong>to</strong>rydepression. 11 We did not observe any significant respira<strong>to</strong>rydepression in the study groups. One patient who received<strong>fentanyl</strong> 25 lg had a decreased respira<strong>to</strong>ry rateintraoperatively for 20 min. Although the patient’srespira<strong>to</strong>ry rate fell below 10 breaths/min, the oxygensaturation remained above 96% <strong>and</strong> the episode resolvedspontaneously.A potential limitation of this study is the multiplesmall-group <strong>com</strong>parisons, which were a function of thedose–response design. The strength of this design is thatwe obtain information over a wide range of doses. However,the multi-group design reduces the statisticalpower <strong>to</strong> show small differences between the groups.Due <strong>to</strong> the variability in pos<strong>to</strong>perative morphine use,<strong>com</strong>bined with the small sample size <strong>and</strong> multiplegroups, we lacked power <strong>to</strong> show a small difference inmorphine use. Although there was a statistically significantdifference in pos<strong>to</strong>perative pain in the <strong>fentanyl</strong>groups, the clinical effect size was small <strong>and</strong> did not lead<strong>to</strong> increased analgesic use despite a five-fold increase in<strong>fentanyl</strong> dose. However, we acknowledge that subtle differencesamong study groups would not have been detecteddue <strong>to</strong> study design limitations acknowledgedabove.In conclusion, our findings suggest that IT <strong>fentanyl</strong> indoses from 5 <strong>to</strong> 25 lg co-administered with IT <strong>bupivacaine</strong><strong>and</strong> morphine for cesarean delivery under spinalanesthesia may induce subtle acute opioid <strong>to</strong>lerance asevidenced by higher overall pain scores in patientswho received <strong>fentanyl</strong> <strong>com</strong>pared with the control group.However, this did not result in increased analgesic usepost-cesarean delivery. Therefore the clinical importanceof our findings is uncertain. Future studies with largersample sizes are required <strong>to</strong> fully elucidate this phenomenon<strong>and</strong> determine its clinical significance before cliniciansconsider avoid using IT <strong>fentanyl</strong> for fear ofinducing acute <strong>to</strong>lerance pos<strong>to</strong>peratively, especially within light of previous studies showing that IT <strong>fentanyl</strong> resultsin less intraoperative pain <strong>and</strong> nausea during cesare<strong>and</strong>elivery.DisclosureThe authors involved in this study <strong>and</strong> the preparationof the manuscript received no external funding. Thisstudy was financially supported by the Department ofAnesthesia, Stanford University School of Medicine,Stanford, California. We thank Karen Giarrusso, MDfor her valuable help with patient enrollment <strong>and</strong> datacollection. We would also like <strong>to</strong> thank Alex McMillan,Human Health <strong>and</strong> Policy Biostatistics, Stanford University.For his expertise <strong>and</strong> advice on this analysis.References1. Liu S, Chiu AA, Carpenter RL, et al. Fentanyl prolongs lidocainespinal anesthesia without prolonging recovery. Anesth Analg1995;80:730–4.2. Dahl JB, Jeppesen IS, Jorgensen H, Wetterslev J, Moiniche S.Intraoperative <strong>and</strong> pos<strong>to</strong>perative analgesic efficacy <strong>and</strong> adverseeffects of intrathecal opioids in patients undergoing cesareansection with spinal anesthesia: a qualitative <strong>and</strong> quantitativesystematic review of r<strong>and</strong>omized controlled trials. Anesthesiology1999;91:1919–27.3. Cohen SE, Subak LL, Brose WG, Halpern J. Analgesia aftercesarean delivery: patient evaluations <strong>and</strong> costs of five opioidtechniques. Reg Anesth 1991;16:141–9.4. Palmer CM, Emerson S, Volgoropolous D, Alves D. Doseresponserelationship of intrathecal morphine for postcesareananalgesia. Anesthesiology 1999;90:437–44.5. Fournier R, Van Gessel E, Macksay M, Gamulin Z. Onset <strong>and</strong>offset of intrathecal morphine versus nalbuphine for pos<strong>to</strong>perativepain relief after <strong>to</strong>tal hip replacement. Acta Anaesthesiol Sc<strong>and</strong>2000;44:940–5.6. Fishbain DA, Cole B, Lewis JE, Gao J, Rosomoff RS. Do opioidsinduce hyperalgesia in humans? An evidence-based structuredreview. Pain Med 2009;10:829–39.7. Gus<strong>to</strong>rff B, Hoechtl K, Sycha T, Felouzis E, Lehr S, Kress HG.The effects of remifentanil <strong>and</strong> gabapentin on hyperalgesia in anew extended inflamma<strong>to</strong>ry skin pain model in healthy volunteers.Anesth Analg 2004;98:401–7.8. Angst MS, Koppert W, Pahl I, Clark DJ, Schmelz M. Short-terminfusion of the mu-opioid agonist remifentanil in humans causeshyperalgesia during withdrawal. Pain 2003;106:49–57.9. Cooper DW, Lindsay SL, Ryall DM, Kokri MS, Eldabe SS, LearG. A. Does intrathecal <strong>fentanyl</strong> produce acute cross-<strong>to</strong>lerance <strong>to</strong>i.v. morphine? Br J Anaesth 1997;78:311–3.10. Carvalho B, Cohen SE, Lipman SS, Fuller A, Mathusamy AD,Macario A. Patient preferences for anesthesia out<strong>com</strong>es associatedwith cesarean delivery. Anesth Analg 2005;101:1182–7.
34 <strong>Intrathecal</strong> <strong>fentanyl</strong> <strong>and</strong> acute <strong>to</strong>lerance11. Dahlgren G, Hultstr<strong>and</strong> C, Jakobsson J, Norman M, ErikssonH, Martin H. <strong>Intrathecal</strong> sufentanil, <strong>fentanyl</strong>, or placebo <strong>added</strong> <strong>to</strong><strong>bupivacaine</strong> for cesarean section. Anesth Analg 1997;85:1288–93.12. Manullang TR, Vis<strong>com</strong>i CM, Pace NL. <strong>Intrathecal</strong> <strong>fentanyl</strong> issuperior <strong>to</strong> intravenous ondansetron for the prevention ofperioperative nausea during cesarean delivery with spinal anesthesia.Anesth Analg 2000;90:1162–6.13. Ben-David B, Miller G, Gavriel R, Gurevitch A. Low-dose<strong>bupivacaine</strong>-<strong>fentanyl</strong> spinal anesthesia for cesarean delivery. RegAnesth Pain Med 2000;25:235–9.14. Palmer CM, Voulgaropoulos D, Alves D. Subarachnoid <strong>fentanyl</strong>augments lidocaine spinal anesthesia for cesarean delivery. RegAnesth 1995;20:389–94.15. Connelly NR, Dunn SM, Ingold V, Villa EA. The use of <strong>fentanyl</strong><strong>added</strong> <strong>to</strong> morphine-lidocaine-epinephrine spinal solution inpatients undergoing cesarean section. Anesth Analg1994;78:918–20.16. Wang C, Chakrabarti MK, Whitwam JG. Specific enhancementby <strong>fentanyl</strong> of the effects of intrathecal <strong>bupivacaine</strong> on nociceptiveafferent but not on sympathetic efferent pathways in dogs.Anesthesiology 1993;79:766–73.17. Girgin NK, Gurbet A, Turker G, Aksu H, Gulhan N. <strong>Intrathecal</strong>morphine in anesthesia for cesarean delivery: dose-responserelationship for <strong>com</strong>binations of low-dose intrathecal morphine<strong>and</strong> spinal <strong>bupivacaine</strong>. J Clin Anesth 2008;20:180–5.18. Carvalho B, Riley E, Cohen SE, et al. Single-dose, sustainedreleaseepidural morphine in the management of pos<strong>to</strong>perativepain after elective cesarean delivery: results of a multicenterr<strong>and</strong>omized controlled study. Anesth Analg 2005;100:1150–8.19. Carvalho B, Rol<strong>and</strong> LM, Chu LF, Campitelli 3rd VA, Riley ET.Single-dose, extended-release epidural morphine (DepoDur) <strong>com</strong>pared<strong>to</strong> conventional epidural morphine for post-cesarean pain.Anesth Analg 2007;105:176–83.20. Sia AT, Lim Y, Lim EC, et al. A118G single nucleotidepolymorphism of human mu-opioid recep<strong>to</strong>r gene influences painperception <strong>and</strong> patient-controlled intravenous morphine consumptionafter intrathecal morphine for postcesarean analgesia. Anesthesiology2008;109:520–6.21. Hunt CO, Naulty JS, Bader AM, et al. Perioperative analgesiawith subarachnoid <strong>fentanyl</strong>-<strong>bupivacaine</strong> for cesarean delivery.Anesthesiology 1989;71:535–40.