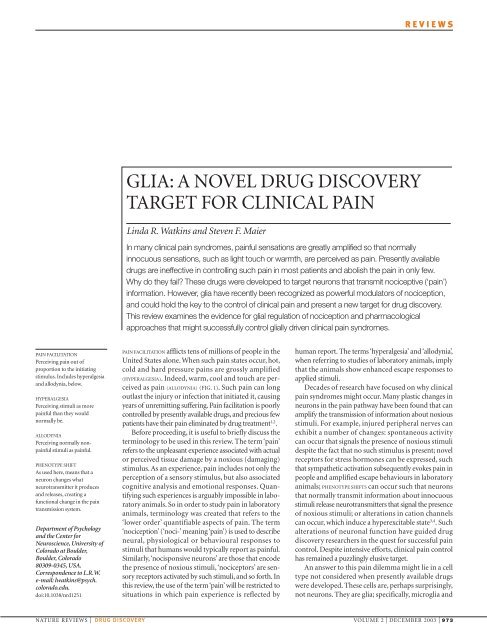
GLIA: A NOVEL DRUG DISCOVERY TARGET FOR CLINICAL PAIN
GLIA: A NOVEL DRUG DISCOVERY TARGET FOR CLINICAL PAIN
GLIA: A NOVEL DRUG DISCOVERY TARGET FOR CLINICAL PAIN
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
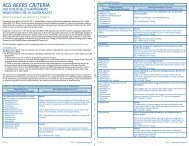
REVIEWSabIncomingA-δ/C fibre'pain' signalsNormalsubstance Prelease,EAA releaseQuiescent gliaPain messageto brain via PTNsNK-1receptorAMPAreceptorNMDAreceptorPain stimulusPTNcIncomingA-δ/C fibre'pain' signalsdViruses and bacteriaNonexistentgliaNK-1receptorEnhancedsubstance Prelease,EAA releaseAMPAreceptorCa 2+NMDAreceptorPTN: NO, PGs,fractal kineActivatedgliaPrimary afferent:Substance P, EAAs, ATP,fractal kinecNOSNOIL-1, TNF, IL-6, ROS, NO,PGs, EAAs, ATPL-argininePTNEnhance PTNexcitabilityEnhance primaryafferent substance Pand EAA releaseFigure 1 | Schematic of pain and pain modulation. a | Classical pain transmission pathway. When a noxious stimulus isencountered (such as stepping on a tack, as shown), peripheral nocisponsive nerves (A-δ and C fibres) are excited. These axonstransmit action potentials to their presynaptic terminals in the spinal cord dorsal horn. Neurotransmitters released here bind to andactivate postsynaptic receptors on pain transmission neurons (PTNs). In turn, the axons of PTNs ascend, predominantlycontralaterally, to the brain and carry information about the noxious stimulus to higher centres. The region of the sensory presynapticterminal and post-synaptic region of the PTN are shown in detail in (b–d). b | Normal pain. In normal, everyday situations in which painis experienced, glia are present but quiescent. Information about noxious stimuli arrives from the periphery along A-δ and C fibres,causing the release of substance P and excitatory amino acids (EAAs) in amounts appropriate to the intensity and duration of theinitiating noxious stimulus. Activation of neurokinin-1 (NK-1) receptors by substance P and activation of α-amino-3-hydroxy-5-methyl-4-isoxazole propionic acid (AMPA) receptors by EAAs cause transient depolarization of the PTNs, thereby generating action potentialsthat are relayed to higher brain areas. N-methyl-D-aspartate (NMDA)-linked channels are inoperative as they are chronically ‘plugged’by magnesium ions. c | Pathological pain: classic view. In reponse to intense and/or prolonged barrages of incoming nociceptiveinformation, the PTNs become sensitized and over-respond to subsequent incoming nociceptive signals. The intense and/orprolonged barrage depolarizes the PTNs such that the magnesium ions exit the NMDA-linked channel. The resultant influx of calciumions activates constitutively expressed nitric oxide synthase (cNOS), causing conversion of L-arginine to nitric oxide (NO). Because it isa gas, NO rapidly diffuses out of the PTNs. This NO acts presynaptically to cause exaggerated release of substance P and EAAs.Postsynaptically, NO causes the PTNs to become hyperexcitable. Glia have not been considered to have a role in creating painfacilitation by this neuronally driven model. d | Pathological pain: new view. Here, glial activation is conceptualized as a driving forcefor creating and maintaining pathological pain states. The role of glia is superimposed on the NMDA—NO-driven neuronal changesdetailed in c, so only the aspects added by including glia in the model are described here. Glia are activated (shown as hypertrophiedrelative to b, as this reflects the remarkable anatomical changes that these cells undergo on activation) by three sources: bacteria andviruses which bind specific activation receptors expressed by microglia and astrocytes; substance P, EAAs, fractalkine and ATPreleased by either A-δ or C fibre presynaptic terminals (shown) or by brain-to-spinal cord pain enhancement pathways (not shown);and NO, prostaglandins (PGs) and fractalkine released from PTNs. Following activation, microglia and astrocytes cause PTNhyperexcitability and the exaggerated release of substance P and EAAs from presynaptic terminals. These changes are created bythe glial release of NO, EAAs, reactive oxygen species (ROS), PGs, pro-inflammatory cytokines (for example, interleukin-1 (IL-1), IL-6,tumour-necrosis factor (TNF)), and nerve growth factor. Modified, with permission, from REF. 12 © Elsevier Science Ltd (2001).974 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWS<strong>GLIA</strong>L FIBRILLARY ACIDICPROTEIN(GFAP). An astrocyte-specificprotein. Increases in GFAP arefrequently used as a marker ofastrocyte activation.p38 MAP KINASEAn intracellular signallingcascade, activated in responseto pro-inflammatory cytokinereceptor binding. Activation ofthis cascade leads to productionof pro-inflammatorycytokines.astrocytes within the spinal cord. This review will firstexamine the evidence that activated glia drive the creationand maintenance of allodynia and hyperalgesia. Thisliterature review will demonstrate that astrocytes andmicroglia in the spinal cord must now be recognized asactive participants in the creation and maintenance ofpain facilitation induced by inflammation and damageto peripheral tissues, peripheral nerves, spinal nervesand the spinal cord. On activation, these glia release avariety of neuroexcitatory substances that potentiatepain transmission by neurons. Of these glial products,pro-inflammatory cytokines will be shown to be commonspinal mediators of allodynia and hyperalgesia.Given the failure of presently available drugs to provideadequate clinical pain management, this newly recognizedrole of glia in general, and pro-inflammatorycytokines in particular, is exciting because it predictsnovel approaches for effective pain control by targetingglial activation.A number of drugs will be introduced in the courseof this discussion that are effective in controlling gliallydriven exaggerated nociceptive states in laboratoryanimals. Each of these drugs will be discussed in thefinal section of this review, with regard to their potentialclinical application.What does it mean that glia are ‘activated’?In the following discussion, frequent reference will bemade to ‘activated’ glia. Activation is a fundamentallydifferent phenomenon in neurons compared with thatin glia. The term ‘activation’ refers to an enhanced abilityof a cell to perform a function beyond that present in abasal state. For neurons, activation is unidimensional, asit mainly relates to the production of action potentials.By contrast, activation of glia is multi-dimensionalbecause glia perform numerous functions (see below).So there are many different activational states, with variouscomponents expressed with different time-coursesand intensities that are dependent on the stimulus thattriggers activation.Astrocytes are basally active in carrying out a numberof functions, but unless there is an external stimulusthey do not become activated. Astrocytes serve severalfunctions in the normal central nervous system (CNS),including the regulation of: extracellular ion and neurotransmitterconcentrations; the availability of neurotransmitter/neuromodulatorprecursors to nearbyneurons; and extracellular pH. No evidence is apparentin the literature that these functions are regulated bystimuli that activate astrocytes or by substances releasedby activated glia. As such, they do not seem likely to beaffected by drugs that target these aspects of activatedastrocyte function.Astrocyte activation occurs in response to CNStrauma, ischaemia, tumours, neurodegeneration, andthe presence of immunogenic components of virusesand bacteria 5 .Activation is morphologically characterizedby hypertrophy and increased production of intermediatefilaments (<strong>GLIA</strong>L FIBRILLARY ACIDIC PROTEIN (GFAP),vimentin and/or nestin) 5 , and functionally by increasedproduction of a variety of pro-inflammatory substances 6 .Notably, functional changes and morphologicalchanges are not time-locked, so functional changescan be detected in the absence of increased intermediatefilaments, and vice versa.In contrast to astrocytes, microglia in the normalCNS are quiescent cells with no recognized function 7 .In this state, they exhibit a ramified morphology, noactivation of p38 MITOGEN-ACTIVATED PROTEIN (MAP) KINASE,and little or no expression of the receptors, cellsurfacemarkers or functional activities characteristicof activated microglia 7 .Microglial activation occurs in response to the samerange of stimuli that activate astrocytes. It is a gradedphenomenon, characterized by a specific morphology(retracted processes and hypertrophy; amoeboid morphologyunder strongly pathological circumstances),proliferation, increased expression of one or more cellsurfacemarkers or receptors (such as the complement 3receptor associated with adhesion, migration andphagocytosis and scavenger receptors associated withphagocytosis), and/or changes in functional activities(migration to areas of damage, phagocytosis, production/releaseof pro-inflammatory substances) 7 .Notably,the changes in receptors, cell-surface markers and/or theproduction of pro-inflammatory substances can occurin the absence of morphological changes, proliferationor phagocytosis 7,8 .So, as is the the case for astrocyteactivation, microglial activation is a multi-dimensionalprocess. The manner in which activation is expressed isdependent on the type and intensity of the inductivestimulus, and different patterns and time-courses ofresponses can occur.Spinal cord glia as powerful modulators of painUntil recently, glia were thought of simply as housekeepersfor neurons, regulating the extracellular ionicenvironment and removing debris. However, in recentyears it has become recognized that glia dynamicallymodulate the function of neurons under both physiologicaland pathological conditions 9 .In the discussion to follow, the term ‘glia’ will be usedto refer to both microglia and astrocytes. As will bereviewed below, both cell types are activated in thespinal cord in response to experimental manipulationsthat induce pain facilitation. Both cell types, on activation,can produce and release a variety of nociceptionenhancingsubstances. In addition, each stimulates thefurther activation of the other, perhaps forming afunctional unit. The use of the term ‘glia’ in the presentcontext reflects the fact that most presently availabledata support the notion that both microglia andastrocytes are involved in allodynia and hyperalgesia,but that these data cannot yet allow us to determine therelative contributions of each.Glia first came to the attention of pain researchersin the early 1990s when Garrison et al. reported thatperipheral nerve damage that created exaggerated nociceptiveresponses (neuropathic ‘pain’ behaviours) alsoactivated spinal cord glia (FIG. 2).Furthermore, theN-methyl-D-aspartate (NMDA) antagonist MK801,which blocks neuropathy induced allodynia andNATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 975
REVIEWSa Intact sidec Intact sidehyperalgesia, also blocked glial activation 10,11 .Thesestudies established that glial activation, at minimum,closely tracked neuropathy induced allodynia and hyperalgesiaas well as their pharmacological resolution.The potential implications of the data collected byGarrison et al. were breathtaking. If glial activation wasindeed a causal factor in the development of allodyniaand hyperalgesia, rather than simply being correlatedwith these conditions, it would be a dramatic departureb Nerve-damaged sided Nerve-damaged sideFigure 2 | A historical look at glial involvement in pain. The first evidence that glia wereinvolved in pain modulation came from the work of Garrison et al. who showed that astrocytes inspinal cord were activated (as reflected by immunohistochemistry for the astrocyte-specificactivation marker, glial fibrillary acidic protein) in response to sciatic nerve damage. They examinedthe effect of chronic constriction injury (CCI), as it is one of the best-validated animal models ofpartial nerve injury leading to chronic pain. Although previous studies had identified central nervoussystem glial activation as a rapid response to peripheral nerve injury, the work of Garrison et al. wasthe first to link such glial activation to a functional outcome, namely, enhanced nociception. In theupper panels (a and b), the spinal cord ipsilateral of sciatic CCI is compared with the spinal cord onthe healthy sciatic side. Clearly, these two sides look different. To more clearly see what thisdifference is due to, the lower panels (c and d) provide a higher-power image of dorsal hornastrocytes. Compared with astrocytes on the healthy spinal cord side (c), astrocytes on the nervedamagedside (d; same magnification as c) are hypertrophied and more darkly stained, which is asign of astrocyte activation. Modified, with permission, from REF. 10 © Elsevier Science Ltd (1991).from the classical view that exaggerated pain states arecreated and maintained solely by neurons. In practicalterms, if glia were key players, it would open up wholenew approaches for clinical pain control, as drugs thatalter glial function were likely to be unique from drugstargeting neurons.So, how could one test whether glia are necessary orsufficient for allodynia and hyperalgesia? Neitherquestion proved easy to address, given the limitedpharmacological tools available, and the even morelimited knowledge of how glia might alter nociception.What became clear, however, was that every modeltested that induced allodynia and/or hyperalgesia wasassociated with the activation of both astrocytes andmicroglia 12 (FIG. 3). So, finding ways to test glialinvolvement became essential.The question of whether glia are necessary for allodyniaand hyperalgesia addresses whether exaggeratednociceptive responses will occur if neurons, but not glia,are present. In practice, this translates to pharmacologically‘removing’ glia by disrupting their function. Twodrugs have been employed for this purpose: fluorocitrate,which selectively disrupts the Krebs energy cycle ofglia by inhibiting the glia-specific enzyme aconitase 13,14 ;and minocycline, which selectively disrupts the activationof microglia without directly affecting neurons or astrocytes15 .Both agents have been found to be effective inblocking diverse models of allodynia/hyperalgesia 16–21 .Two intriguing, and interrelated, findings are worth noting.First, fluorocitrate, which disrupts astrocyte as well asmicroglia function, seems to exert more profound blockadeof exaggerated nociceptive states than does minocycline,which targets only microglia. Second, minocyclineis far more effective in blocking, than reversing, exaggeratednociceptive responses 20,21 .The most importantrole of microglia might be involvement in the initialinduction of exaggerated responses to noxious stimuli.Microglial activation leads, in turn, to astrocyte activationthat maintains the facilitation of nociception 20 .Developing an effective strategy for testing whetherglial activation is sufficient to induce allodynia/hyperalgesiais dependent on identifying ways to selectivelyactivate these cells. Although studies of glial cultureshave identified neurotransmitters that can activate glia 9 ,that information is of little use here for two reasons.First, virtually all data on glial responses to neurotransmittershave been derived from glia isolated from thebrain. Given the marked heterogeneity in both receptorexpression and response properties of glia isolatedfrom various CNS regions 22,23 ,extrapolating results frombrain to spinal cord glia is problematic. Indeed, there areeven heterogeneities between glia in nocisponsive layersof the superficial dorsal horn (laminae I–III) versusother spinal regions 24–26 . Little information is availableas to what neurotransmitters excite dorsal spinal cord gliato produce and release neuroactive substances 27,28 .Giventhat dorsal horn glial activation occurs in response toperipheral injury and inflammation 12 , it would seemreasonable to predict that neurotransmitters are releasedin spinal cord in response to peripheral injury, and thatinflammation will be found to activate these cells.976 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWSaFigure 3 | Microglia, as well as astrocytes, are activated by manipulations that createenhanced nociception in animal models. Although the earliest studies focused on theactivation of astroctyes, microglia are also activated. These photomicrographs provide oneexample of microglial activation in response to a manipulation (intrathecal HIV-1 glycoprotein120) that produces robust mechanical allodynia and thermal hyperalgesia. Microglia are stainedfor expression of complement-3 receptor, which is upregulated when microglia are activated.a | Normal microglia in the dorsal horn of the spinal cord after peri-spinal injection of vehicle(control). b | Same magnification view of dorsal horn microglia after peri-spinal injection of a viralprotein (HIV-1 glycoprotein 120), which induces exaggerated pain responses. Modified, withpermission, from REF. 12 © Elsevier Science Ltd (2001).IMMUNOCOMPETENTFunctioning similar to immunecells; that is, expressingreceptors for bacteria/virusesand releasing pro-inflammatorycytokines and other immunecell products on activation.NEUROPATHIC <strong>PAIN</strong>Allodynia/hyperalgesia causedby inflammation of and/ortrauma to peripheral nerves.IL-6-NEUTRALIZINGANTIBODIESAntibodies that bind to IL-6and so prevent IL-6 frombinding to its receptor.bHowever, studying the effects of such neurotransmitterson glia in vivo is confounded by the fact that thesesubstances would also activate spinal neurons.The first approach that has been used to examinewhether glial activation is sufficient to create enhancednociception rests on the fact that both astrocytes andmicroglia are IMMUNOCOMPETENT cell types. That is,whereas microglia are of haematopoietic (immune) celllineage 29,30 (although this is not without controversy 31 ),astrocytes can also behave, in many regards, likeimmune cells, despite their neural-tube origins 32 .Ofdirect relevance here is that they express receptors for,and are activated by, viruses and bacteria 33 .So studieshave examined the effect of injecting the immunogenicportions of bacteria and viruses over spinal cord. Glialactivation and exaggerated pain responses occur as aresult 16,18,34 .Glial activation is causal to the allodynia andhyperalgesia observed in these studies, as the painchanges are blocked by disruption of glial function 16,18,34 .A second and very recent approach for examiningthis issue has tested the role of fractalkine (also knownas chemokine (C-X3-C motif) ligand-1) in pain facilitation.Fractalkine is a protein that is tethered to the extracellularsurface of neurons 35 .In spinal cord, no cell typesother than neurons express fractalkine 36,37 .In responseto strong neuronal activation, fractalkine can be releasedand diffuse away 38 .In spinal cord, only microglia expressreceptors for fractalkine (FIG. 4).So, fractalkine is aputative neuron-to-glia signal. The administration ofexogenous fractalkine produces allodynia and hyperalgesiathrough binding to CX3CR1, the only knownreceptor for fractalkine 36,37 .Furthermore, the blockadeof endogenous fractalkine attenuates allodynia andhyperalgesia induced in animal models of NEUROPATHIC<strong>PAIN</strong>, indicating that peripheral-nerve inflammation andinjury lead to the release of fractalkine from neurons indorsal spinal cord 36,37 .So neuron-to-glia signalling, hereevoked by fractalkine activation of microglia, againseems to be sufficient to create pain facilitation.Mechanisms of glial pain enhancementThe mechanisms by which glial activation enhancesneuronal transmission of nociceptive information areonly partially understood. Ultimately, activated spinalcord glia must lead to hyperalgesia and allodynia byreleasing substances that act on neurons in the painpathway(s). These substances could have a variety ofactions: they could direct excitation, sensitization, orpotentiation of action potentials; direct the upregulationof neuronal receptors; and promote the inductionof the release of other transmitters/modulators that canact on nocisponsive neurons.To date, most evidence has supported a putative rolefor the glial pro-inflammatory cytokines tumournecrosisfactor (TNF), interleukin-1 (IL-1) and IL-6.Pro-inflammatory cytokines are classically known as afamily of proteins released by activated immune cells.There is no amino-acid sequence motif or three-dimensionalstructure that links them; rather, they aregrouped on the basis of their biological activities 39 . TNF,IL-1 and IL-6 came to be classified as pro-inflammatorybecause they orchestrate the early immune responseto infection and injury by communicating with whiteblood cells, thereby attracting them to the site ofinfection/injury, and causing them to become activatedand respond 39 .Peripherally, and in the CNS, these proinflammatorycytokines are often sequentially formedin a cascade in which TNF is typically made first, causingthe induction of IL-1, which in turn causes the inductionof IL-6. It is an important feature that the effects of proinflammatorycytokines synergize (especially TNFand IL-1), such that far more powerful effects areobserved when more than one cytokine is present 39 .TNF and IL-1, in particular, are very potent biologicalmolecules, producing large effects when administeredin the CNS in the femptogram to picogram range 33 .Indeed it has been estimated that as few as four moleculesof IL-1 need bind to a cell to induce a physiologicalresponse 39 .Appropriately, given this potency, the productionand release of pro-inflammatory cytokines istightly regulated, and numerous negative-feedbackcontrol systems exist (such as the production of antiinflammatorycytokines, ‘decoy’ receptors and antagonistsof receptors for pro-inflammatory cytokines)which can help suppress the production and functionof pro-inflammatory cytokines 33 .Both astrocytes and microglia can release proinflammatorycytokines on activation 33 (FIG. 5), and gliaand neurons express receptors for them. In the brain,pro-inflammatory cytokines have a wide array ofeffects on the regulation of core body temperature, sleep,learning and memory, and hypothalamo–pituitary hormones40 .The injection of exogenous pro-inflammatorycytokines over the spinal cord enhances nociception 41–44 ,and electrophysiological studies document rapidenhancement of neuronal excitability in response tonoxious stimuli following the injection of proinflammatorycytokines to the region 43,45 .Conversely,the blockade of pro-inflammatory cytokine function,using either an IL-1-receptor antagonist, soluble TNFreceptors or anti-IL-6-NEUTRALIZING ANTIBODIES,preventsNATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 977
REVIEWSa b cFigure 4 | Neuron-to-glia communication. When pain processing is enhanced by inflammationor damage to peripheral tissues or peripheral nerves, signals must be relayed from sensorynerves to spinal cord glial cells to cause glial activation. There are at least two possible routes ofneuron-to-glia communication that could lead to glial activation and consequent enhancement ofnociception. First, neurotransmitters that relay information of the presence of peripheral noxiousstimuli could bind to and activate glia. Although probable, this has not yet been proven for spinalcord. Second, neurons could release a selective neuron-to-glia signal that binds to and activatesglia. This avenue of neuron-to-glia signalling has only very recently begun to be productivelyexplored. One candidate signal is fractalkine, a protein expressed on the extracellular surface ofneurons that, on strong neuronal activation, can be released into the extracellular fluid. In spinalcord, only microglia express receptors for fractalkine, making it a putative neuron-to-glia signal.Fractalkine, either injected exogenously or released endogenously in response to peripheral nervedamage, enhances nociception in animal models. The photomicrographs are of astrocyte andmicroglia mixed cultures. These photomicrographs demonstrate that microglia, but notastrocytes express fractalkine-binding sites. Green fluorescence (a and c) reveals glial fibrillaryacidic protein (GFAP), an astrocyte-specific marker. Red fluorescence (b and c) reveals bindingof fluorescent fractalkine. The lack of yellow (co-localization of green and red) indicates thatastrocytes do not express binding sites for fractalkine. By contrast, all microglia in the field bindthis putative neuron-to-glia signal. Panel c shows the mixed glial culture with superimposedfluorescence images. Modified with permission from REF. 133 © Springer-Verlag (2003).PERI-SPINAL INJECTIONAdministering a drug into thecerebrospinal fluid surroundingthe spinal cord; also called‘intrathecal’.their effects in brain 40 . Likewise, PERI-SPINAL INJECTION ofantagonists of pro-inflammatory cytokine functionprevents and/or reverses allodynia and hyperalgesia invirtually every animal model tested 17,19,34,36,46 .Suchmodels include inflammation and/or injury to peripheraltissues, peripheral nerves, spinal nerves and spinalcord.The fact that established allodynia and hyperalgesiacan be reversed by pro-inflammatory cytokineantagonists supports the conclusion that these glialproteins are involved in the maintenance, as well asthe initial induction, of these enhanced nociceptivestates. That is an important point when one is attemptingto identify drug targets for controlling pre-existingclinical pain syndromes.Recognition of the importance of pro-inflammatorycytokines in the induction and maintenance of allodyniaand hyperalgesia has led to the testing of variouscytokine-suppressive drugs in animal models. Oneapproach to control pro-inflammatory cytokines is toblock intracellular pathways that lead to their production.Another approach is to block intracellular pathwaysthat are activated by the binding of pro-inflammatorycytokines to their receptors. Although multiple intracellularsignalling cascades have been implicated in proinflammatorycytokine signalling and production, p38MAP kinase is crucially involved in both 33,47 .Indeed,p38 MAP kinase inhibitors were originally referred to ascytokine-suppressive anti-inflammatory drugs, reflectingthe importance of this signalling pathway. These compoundsinhibit allodynia and hyperalgesia induced byperipheral tissue inflammation, peripheral nerve injury,spinal nerve injury, spinal cord inflammation, andperi-spinal substance P and NMDA administration inanimal models 18,21,48–52 .At least some of these compoundscross the blood–brain barrier 51,52 , and so are effectivesystemically as well as after peri-spinal administration.An alternative approach to suppressing cytokines isto use xanthine derivatives, such as propentofylline.Propentofylline controls enhanced nociception inducedby spinal nerve transection 53 .Notably, it is equally effectivein reversing and preventing these changes, after bothsystemic and peri-spinal delivery 53 . Furthermore,propentofylline decreases both microglial and astrocyticactivation in spinal cord 53 .Other compounds that have been tested in animalmodels include the disease-modifying anti-rheumaticdrug leflunomide, the immunosuppressive drugmethotrexate and the immunomodulatory drug thalidomide.Systemic leflunomide was more effective inattenuating enhanced nociception induced by peripheralnerve injury than nociception caused by damage tospinal roots 54 .Methotrexate, delivered systemically aswell as at the site of spinal root injury, both preventedand reversed neuropathic pain behaviours in rats 55 ,anexciting outcome from a clinical perspective. Thalidomide,to date, has only been tested systemically. It hasproven effective in delaying enhanced nociceptiveresponses in rats induced by peripheral nerve damage 56 .However, its ability to reverse neuropathic pain behavioursin rats has been questioned 56 .Peripherally, thalidomideattenuated nerve-damage-induced TNF, but hadno effect on either IL-1 or IL-6 expression in the damagednerve 57 .Given that the focus of these investigators wasthalidomide-regulation of peripheral nerve changes,rather than spinal cord glia, they did not assess the effectof systemic thalidomide on central glial activation orpro-inflammatory cytokines. Because thalidomidecrosses the blood–brain barrier 58,59 ,changes in spinalcord glial function would be expected.The newest approach to controlling glially enhancednociception is upregulation of the expression of acytokine not yet discussed in this review, IL-10. Ratherthan being a pro-inflammatory cytokine, IL-10 is ananti-inflammatory cytokine. Like pro-inflammatorycytokines, anti-inflammatory cytokines are a family ofproteins that can be released by immune cells andimmunocompetent cells, such as glia 60,61 . Endogenously,anti-inflammatory cytokines serve as negative-feedbackregulators that keep potentially pathological activation ofimmune and immune-like cells under control 60,61 .Withinthis family, IL-10 is by far the most powerful member.IL-10 is attractive as a suppressor of glial pathologicalexcitation for a number of reasons: it can inhibit proinflammatorycytokine production at multiple levels,including transcription, translation and release; it candownregulate the expression of receptors for proinflammatorycytokines, so that even if pro-inflammatory978 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWSabTACETNF-αOthercellsCXCR4TNFRICa 2+ ERK1/2Glial cellFigure 5 | Pro-inflammatory cytokines are constitutively expressed in an inactive precursor form, allowing rapid release.Constitutive expression and rapid release of tumour-necrosis factor (TNF) is illustrated. a | Constitutive extracellular surfaceexpression of TNF on astrocytes. Exposure of living rat astrocytes (glial fibrillary acidic protein-positive, red) to an anti-TNF antibodyselectively reveals TNF sequences exposed on the extracellular surface (green) of about 50% of astrocytes. b | Molecular eventscoupling receptor activation of astrocytes (CX3CR4 shown in example) to TNF release. TNF is released in response to stimulationof various astrocyte receptors. Illustrated is TNF action on a G-protein-coupled receptor (CXCR4) by its endogenous ligand(SDF-1-α). The resultant intracellular signalling activates extracellular signal-regulated kinase (ERK1/2), which activatesTNF-α-converting enzyme (TACE). TACE is a specific enzyme required to cleave the extracellular domain of membrane-boundpro-TNF (a 26-kDa protein) to generate the released mature TNF (18-kDa protein) through a process known as ectodomainshedding. Once cleaved, the mature (active) TNF both exerts auto-stimulation of the same cell and diffuses away to exert paracrineactions on surrounding glia and neurons. Adapted with permission from REF. 134 © Oxford University Press (2002).SYNOVIAL TISSUESTissues encapsulating joints.cytokines are released they are less effective due todecreased availability of receptors; it can upregulateendogenous antagonists to pro-inflammatory cytokines,thereby limiting their effectiveness; and evidence to dateindicates that neurons in the spinal cord do not expressreceptors for IL-10, so normal neuronal functions wouldbe unaffected by the presence of IL-10 (REFS 60–62).Takentogether, this is a powerful profile of effects. Behaviourally,studies of IL-10 in rats demonstrate that it prevents orreverses every enhanced nociceptive state examined todate. These models include pain induced by spinalinflammation, inflammatory neuropathy, traumatic neuropathy,spinal trauma and peri-spinal dynorphin 19,36,63–65 .Drug discovery outlookThe potential efficacy of a drug is dependent on manyfactors. What follows is a summary of clinically relevantaspects of the various drugs that target glia and whichhave successfully controlled enhanced nociceptive statesin animal models. No drug presently available for use inhumans was developed to target glia. Rather, they weredeveloped to suppress the function of the peripheralimmune system. Indeed, their efficacy in suppressingpain in humans and enhanced nociceptive behavioursin rats following systemic administration supports theargument that suppressing pro-inflammatory cytokineproduction by SYNOVIAL TISSUES,Schwann cells and otherimmunocompetent cell types in peripheral tissues,peripheral nerves and/or dorsal root ganglia 3 candecrease transmission of nociceptive information to thespinal cord. In the present context, the discussion ofthese compounds will be focused on their potential foralso suppressing the pain-enhancing effects of spinalcord glial activation. There is a great need for new drugsto reach clinical trials for controlling the pathologicalside of spinal cord glial activation.Disrupting glial activation. The two drugs that havebeen examined in animal models for their ability todisrupt glial activation, to date, are fluorocitrate andminocycline. Fluorocitrate is a reversible glial poisonnot appropriate for human use. Although fluorocitrateis a selective glial inhibitor at low doses and short postdrugtime intervals 13,14 , higher doses and longerpost-drug times can indirectly affect neuronal functions.This indirect effect on neurons can result fromelevated extracellular concentrations of excitatoryamino acids due to the inhibition of glial transport 13,14 .Seizures have also been reported in response to glia-toxicdoses of this compound 66 .On the other hand, minocycline exhibits selectivityfor microglia. It is a tetracycline derivative that hasanti-inflammatory effects which are independent of itsantimicrobial actions. In rats, it can inhibit microglialactivation, p38-MAP-kinase activation, IL-1-convertingenzyme(caspase-1) activation, IL-1 release and theproduction of nitric oxide 28,67 .Although the animalliterature largely supports the conclusion that minocyclineinhibits activation of microglia independent ofdirect effects on astrocytes and neurons, neuroprotectiveeffects of minocycline on neuronal culturesexposed to toxic levels of nitric oxide have beenreported 68 .Although all of these indices are positivewith regards to minocycline’s potential for controllingglially driven allodynia and hyperalgesia, concern israised by the fact that minocycline fails to reverse, oris far less effective at reversing, established enhancednociceptive states in animal models, relative to agentsthat inhibit astrocyte as well as microglial activity 20,21 .These initial studies indicate that microglia mighthave a more important role in the initial creation ofenhanced nociceptive states in animals, whereas astrocytesmight become the key glial cell type as allodynia/NATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 979
REVIEWSNUCLEAR FACTOR-κB(NF-κB). A transcription factorthat is constitutively expressed.Its activation leads (amongother effects) to the productionof pro-inflammatory cytokines.Although constitutivelyexpressed, its ability to move tothe nucleus to bind to DNA istonically inhibited by bindingof IκB.INHIBITOR OF κB(IκB). An inhibitor of NF-κBactivation. It is binding to NF-κBthat keeps this transcriptionfactor from being able to moveto the nucleus to activatemessenger RNA transcription.hyperalgesia persists 20 .Iffurther animal studies supportthis conclusion, this is an important concept forguiding drug development. It would indicate thatminocycline is unlikely to be an effective drug for clinicalpain control.Pro-inflammatory cytokine antagonists. A variety ofbiological modifiers have been developed to target IL-1and TNF. Anakinra (Kineret; Amgen) is a recombinanthuman IL-1-receptor antagonist approved foruse in rheumatoid arthritis 69 .Infliximab (Remicade;Centocor) is a chimeric immunoglobulin G1 antibodyspecific for human TNF-α, approved for use inrheumatoid arthritis and Crohn’s disease 70 .Etanercept(Enbrel; Amgen/Wyeth) is a human TNF receptor/Fcfusion protein approved for use for the treatment ofpsoriatic arthritis 70 .Although anakinra and etanercepthave been successfully used in animal studies to bothprevent and reverse glially driven allodynia and hyperalgesia19,34,46 ,peri-spinal administration was required, asthis family of compounds does not cross the intactblood–brain barrier to any significant degree. Animalstudies support the idea that disruption of pro-inflammatorycytokine action is an excellent target for drugdiscovery,but that the potential of these compounds islimited by the need for a chronic indwelling subduralcatheter to allow daily peri-spinal administration.Pro-inflammatory cytokine synthesis inhibitors. Thisfamily of compounds includes propentofylline (Kronos;Aventis) and thalidomide (Thalomid; Celgene). Othercompounds (leflunomide, methotrexate, p38-MAPkinaseinhibitors and IL-10) also act as inhibitors ofpro-inflammatory cytokine synthesis but, in addition,disrupt pro-inflammatory cytokine signalling. Thesewill therefore be discussed separately later.Propentofylline is an orally active xanthine derivativewhich crosses the blood–brain barrier and is prescribedfor Alzheimer’s disease and vascular dementia 71,72 .Ithas a complex mechanism of action, but its profile ofactions strongly predicts its ability to resolve gliallydriven allodynia and hyperalgesia. Propentofylline hasbeen reported to reduce ischaemia-induced glial activationand proliferation, lipid peroxidation, and IL-1and TNF production 73–75 .In addition, it increases theuptake of extracellular glutamate 76 and increases extracellularadenosine 72 , an endogenous anti-inflammatory 77and pain suppressor 78 .In glial cultures, propentofyllineinhibits release of TNF, IL-1 and superoxide;IL-6 and nitric oxide release are unaffected 79 .Giventhat it is approved for other uses, crosses theblood–brain barrier, suppresses glial activation andreverses (as well as blocks) neuropathic pain behavioursin animals 53 ,propentofylline would seem to bean intriguing candidate for clinical trials that targetglially enhanced pain. However, Aventis is not pursuingfurther drug development on this compound dueto an unfavourable patent situation, inconsistent outcomesof studies as to its efficacy in Alzheimer’s andvascular dementia, and problems with oral delivery ofthe drug 71 .By contrast, thalidomide ([+]-α-phthalimidoglutarimide)and potentially safer analogues are beingactively developed by Celgene for clinical use 80 .Afterbeing banned from the market in 1963 due to the productionof severe birth defects 81 , thalidomide has beenapproved for treatment of erythema nodosum leprosum80 .Thalidomide is orally active and readily crossesthe blood–brain barrier 58,82 .It has a number of actionsthat are consonant with its potential use in controllingglially driven exaggerated pain. In vitro, thalidomideand its analogues can inhibit TNF, IL-1 and IL-6, aswell as increase IL-10 production 83–86 . Systemicadministration decreases TNF production by immunecells, either decreases or has no effect on IL-6 (REFS 87,88),and has no effect on IL-1. Thalidomide also inhibitsTNF- and IL1-induced NUCLEAR FACTOR-κB (NF-κB) transcriptionalactivation, probably as a result of inhibitingthe degradation of INHIBITOR OF κB (IκB) 82,89 . Last, thalidomideand its analogues can increase the concentrationof IL-10, an anti-inflammatory cytokine discussedbelow 57,90 .Animal models of neuropathy have documentedthat systemically administered thalidomidedelays the development of allodynia/hyperalgesia, andis correlated with reduced TNF, unaltered IL-1 or IL-6,and increased IL-10 at the site of nerve injury 56,57 .Given the high blood–brain barrier permeability of thiscompound, thalidomide might be capable of inhibitingpro-inflammatory cytokine production by spinal cordglia, but this potential has yet to be investigated.Although thalidomide failed to reverse neuropathyinduced enhanced nociception in rats 56 , it is notable thatrecent human studies report success in relieving longstanding,intense pain due to complex regional painsyndrome 91,92 .This pain syndrome is not controlled bydrugs developed to target neurons, and recently thehypothesis that spinal cord glia contribute to this enigmaticpain syndrome has been proposed 3 .So thalidomideis a compound worthy of further consideration.How to reconcile these data with reports of thalidomide-inducedneuropathy 58,59,80 is being examined.Disrupting pro-inflammatory cytokine signalling andsynthesis. This group of compounds includes leflunomide(Arava; Aventis), methotrexate (Rheumatrex;Wyeth-Ayerst), inhibitors of p38 MAP kinase, and IL-10.Leflunomide is an orally active malononitrilamide,a disease-modifying anti-rheumatic drug. It isapproved for the treatment of rheumatoid arthritis inhumans 93 .It is metabolized by the liver to form theactive metabolite A771726 (REF. 94). Leflunomideinhibits several pain-relevant substances. For example,it decreases rheumatoid arthritis synovial tissueexpression of IL-1, TNF, nitric oxide and cyclooxygenase-2(REFS 95–97).Also, it disrupts TNF-inducedNF-κB activation, cytotoxicity, production of reactiveoxygen species and lipid peroxidation 98 .Although thisprofile indicates that leflunomide would suppress allodyniaand hyperalgesia resulting from glial activation,concern is raised by the fact that leflunomide hasbroad-ranging immunosuppressive effects. Thisresults from its inhibition of the mitochondrial980 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWSBindingReceptor-mediatedendocytosisAdenovirusCAREndosomeLysosomeH +NucleusFigure 6 | One of the newest approaches to the treatment of pathological pain by the control of glial activation. Veryrecently, a number of laboratories have begun exploring the possibility that interleukin-10 (IL-10) might prove to be a powerfulweapon in the battle to control clinical pain states. IL-10 is an anti-inflammatory cytokine, meaning that it naturally serves the role ofa powerful negative feedback signal on pro-inflammatory cytokine expression and function. Although intrathecal administration ofexogenous IL-10 protein reverses enhanced nociception, the effects last less than one day. So gene therapy, to induce prolongedproduction and release of IL-10 protein, is being explored. Early data indicate that IL-10 can powerfully suppress every animalmodel of chronic pain examined to date. Several versions of gene therapy have been demonstrated to work following intrathecaladministration, including adenovirus. This figure illustrates the basics of gene therapy, using adenovirus as the example. Adenovirusvirons bind to the coxsackie adenovirus receptor (CAR) and integrins on the plasma membrane, and enter the cell by receptormediatedendocytosis. As the endosome acidifies (H + ), the capsid is broken down and released from the endosome. Double-strandedviral DNA is released from the degraded capsid and enters the nucleus through the nuclear pore. Modified, with permission, fromREF. 131 © Macmillan Magazines Ltd (2003).enzyme dihydro-orotate dehydrogenase, an enzymerequired for the synthesis of DNA and RNA, cell proliferationand differentiation, phospholipid synthesis andprotein glycosylation 99,100 .So although leflunomide hasshown promise in an animal model of neuropathy 54 ,enthusiasm for using this compound to control clinicalpain syndromes is dampened by its severe immunosuppressiveeffects. In addition, no studies have yetexamined whether leflunomide can reverse establishedexaggerated pain states, beyond inhibiting their initialdevelopment 54 .Additionally, no information is availableregarding the potential blood–brain barrier permeabilityof the active metabolite A771726, nor is much knownabout its actions on glia. All that is known at present isthat A771726 inhibits induced release of nitric oxidefrom rat astrocytes 101 .IfA771726 does indeed accessthe spinal cord following systemic administration, itmight, in part, explain its success in controllinginflammatory pain states such as rheumatoid arthritis,which activate spinal cord glia 102 as well as synovialimmune cells.In contrast to leflunomide, methotrexate is knownto cross the blood–brain barrier 103,104 .This makes itssystemic administration for controlling spinal cordglial activation potentially feasible. Methotrexate is aderivative of glutamic acid that was first marketed totreat neoplastic diseases 105 .It is orally active, althoughvariably absorbed. Low-dose methotrexate has beenNATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 981
REVIEWSused in humans to treat autoimmune diseases, includingrheumatoid arthritis 105 .Its mechanism of actioninvolves elevating the concentration of extracellularadenosine, a potent endogenous anti-inflammatory 106,107 .Low-dose methotrexate also decreases production ofpro-inflammatory cytokines 95,108,109 ,hydrogen peroxide 110and prostaglandin E 2(REF. 110).In addition, methotrexatecan increase IL-10 production 111 .Furthermore, methotrexatehas been proposed to be a competitive inhibitorof IL-1 binding to its receptor 112 , as methotrexate disruptsIL-1-induced effects 113,114 .This profile indicatesthat systemic methotrexate would be able to suppressallodynia and hyperalgesia resulting from spinal cordglial activation. As noted previously, methotrexate bothprevented and reversed established enhanced nociceptiveresponses in rats and reduced some anatomicalindices of spinal cord glial activation 55 .However,thereare concerns about the use of this drug as an inhibitorof spinal cord glial activation. For example, the dosageneeds to be carefully considered. Methotrexate canactivate astrocytes (as reflected by GFAP expression),induce astrocyte proliferation, as well as cause degenerativechanges in these cells 103,104 .Indeed, astrocytesare the primary targets for methotrexate neurotoxicity103,115 .So dosage would need to be adjusted toavoid potential glia-activating and glia-toxic effectswhile maintaining beneficial suppression of glial proinflammatorycytokines.Although glia-toxic side effects are a concern formethotrexate, no such concerns arise for inhibitors ofp38 MAP kinase. This group of compounds are beingdeveloped for clinical targets including Crohn’s disease,pancreatitis and rheumatoid arthritis 116 .These compoundsvary in their bioavailability, with some beingorally active (for example, SCIO-469 and SCIO-323;Scios) and others requiring injections (for example,CNI-1493; Cytokine Pharmasciences). Some, suchas CNI-1493 and NPC037282 (Scios) are active inspinal cord after systemic administration 51,52 .Theyvary in their cross-reactivity with other intracellularsignalling cascades 116,117 .Highly selective p38 MAPkinase inhibitors are in development 49 .This group of drugs is intriguing with respect totheir potential for controlling glially driven exaggeratedpain, for a number of reasons: pro-inflammatorycytokines activate (that is, phosphorylate) p38 MAPkinase 118 ; p38 MAP kinase activation is one of themajor intracellular signalling cascades leading to denovo production of pro-inflammatory cytokines 47,119 ;and (as noted above), at least some of these compoundscross the blood–brain barrier, making systemic administrationof the drugs plausible 51,52 .In rat spinal cord,microglial p38 MAP kinase activation has beendetected immunohistochemically in response to nociception-enhancingperipheral inflammation, peripheralnerve injury, spinal nerve ligation and peri-spinal substanceP 48,49,120,121 . p38 MAP kinase inhibitors do notaffect basal nociception. Rather, they block exaggeratednociception induced by tissue inflammation 17,48 ,peripheral nerve inflammation 19 , spinal nerve ligation50,120 , spinal cord inflammation 18 ,and peri-spinalNMDA and substance P 48,49 .Although CNI-1493reverses established allodynia induced by sciatic nerveinflammation 19 , SB203580 (Calbiochem) and SD-282(Scios) failed to reverse established spinal sensitizationinduced by spinal nerve ligation 50 or peripheralinflammation 48 .Whether these different outcomesreflect different nociceptive potencies of the models,different durations of phospho-p38 MAP kinaseinvolvement in pain maintenance across differentmodels, the inhibition of Jun N-terminal kinase aswell as p38 MAP kinase by CNI-1493 (REFS 116,117) orother factors is not yet clear.One potential issue for this class of drugs is thatp38 MAP kinase is expressed by neurons as well as byglia. Peripheral inflammation, chronic constrictioninjury and spinal nerve ligation increase activated p38MAP kinase in small-diameter neurons in the dorsalroot ganglia, as well as activating p38 MAP kinase indorsal horn microglia 50,120,121 .Activation of p38 MAPkinase in dorsal horn neurons, as well as in microglia,occurs in response to topical capsaicin and peri-spinalNMDA 49,51 .It will be important to identify the downstreameffects of p38 MAP kinase activation in neurons,so as to understand the impact of inhibitors onthe pain pathway.The last compound to be discussed is the antiinflammatorycytokine IL-10. The use of IL-10 is anintriguing approach to glially driven allodynia andhyperalgesia, as IL-10 can suppress the productionand activity of TNF, IL-1 and IL-6. IL-10 can exert thiseffect by inhibiting: p38 MAP kinase 47,60 ;NF-κB activation,translocation and DNA binding 60 ;pro-inflammatorycytokine messenger RNA transcription, stabilityand translation 47,122–124 ; and pro-inflammatorycytokine release 61 .In addition, IL-10 stabilizes mRNAsof suppressors of cytokine signalling, thereby increasingthe production of a family of proteins that furtherinhibits pro-inflammatory cytokine production 60 .IL-10can also interrupt pro-inflammatory cytokine signallingby downregulating the expresion of receptorsfor pro-inflammatory cytokines 125 . Last, it can upregulateendogenous antagonists of pro-inflammatorycytokines, including IL-1-receptor antagonist and solubleTNF receptors 126,127 .The known effects of IL-10 arerestricted to the suppression of pro-inflammatoryfunctions of activated immune and glial cells, leavingnon-inflammatory aspects of cellular functions unaffected61 .Although some neurons express IL-10 receptors,the only known action of IL-10 on neurons isinhibition of cell death (apoptosis) 128 .Although speculative,this profile of IL-10 actions indicates that IL-10might be able to suppress the pathological responsesof glia, while not markedly altering basal functions ofeither glia or neurons.Although there are at present no drugs that specificallytarget IL-10, Avigen is developing gene therapymethods (FIG. 6) to overexpress this anti-inflammatorycytokine for use in exaggerated pain states 129 , as well asother applications. IL-10 does not cross theblood–brain barrier 130 , so systemic administration isnot an option. Constant infusion into the spinal cord982 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWScerebrospinal fluid (CSF) space through an indwellingcatheter would not only be extraordinarily expensivegiven the short half-life of this protein and the cost ofproducing recombinant human IL-10, but also raisesconcerns of infection along the chronic catheter track.Given that IL-10 is an endogenous protein, gene therapycan be employed to drive cells surrounding the CSFspace to produce IL-10 for pain control and obviatethe need for indwelling spinal catheters. Gene therapytechnology is rapidly advancing and new methodologiesindicate that prolonged (many months to years)release of gene-therapy-induced protein can beattained after a single injection of the vector into thespinal CSF space 131 .Importantly, methodologies nowexist which allow the gene therapy to be controlled.That is, vectors can be engineered such that IL-10 productioncan be either activated or deactivated inresponse to systemically administered drugs thatinduce or suppress IL-10 mRNA transcription 132 .Soalthough this IL-10 gene therapy is not yet available forhuman use, this is a potentially exciting new approachfor clinical pain control.SummaryAstrocytes and microglia in the spinal cord are now recognizedas active participants in the creation and maintenanceof pain facilitation induced by inflammationand damage to peripheral tissues, peripheral nerves,spinal nerves and spinal cord. On activation, these gliarelease a variety of neuroexcitatory substances thatpotentiate pain transmission by neurons. Of these glialproducts, pro-inflammatory cytokines seem to be commonspinal mediators of allodynia and hyperalgesia.Given the failure of presently available drugs to provideadequate clinical pain management, this newly recognizedrole of glia is exciting as it predicts novelapproaches for effective pain control by targeting glialactivation. As summarized in this review, several compoundsseem worthy of further development and testingin the hope of reaching clinical trials for this application.Even more importantly, perhaps, is the message topharmaceutical and biotechnology companies thatspinal cord glia are key players in hyperalgesia and allodynia,and are prime targets for new drug developmentaimed at the as-yet-elusive outcome: clinical pain control.1. McQuay, H., Carroll, D., Jadad, A. R., Wiffen, P. & Moore, A.Anticonvulsant drugs for management of pain: a systematicreview. Brit. Med. J. 311, 1047–1052 (1995).2. McQuay, H. J. et al. A systematic review of antidepressantsin neuropathic pain. Pain 68, 217–227 (1996).3. Watkins, L. R. & Maier, S. F. Beyond neurons: Evidence thatimmune and glial cells contribute to pathological pain states.Physiol. Rev. 82, 981–1011 (2002).This article reviews the immunology of peripheralnerves, dorsal root ganglia and spinal nerves; theevidence from animal models of immuneinvolvement in pathological pain; and the evidencethat diverse human clinical pain syndromes involvean immune component.4. Woolf, C. J. & Salter, M. W. Neuronal plasticity: increasingthe gain in pain. Science 288, 1765–1769 (2000).An excellent review of neuronal changes implicated increation and maintenance of exaggerated pain states.5. Pekny, M. in Progress in Brain Research: Glial Cell Funtion(eds Castellano-Lopez, B. & Nieto-Sampedro, M.) 23–30(Elsevier, Amsterdam, 2001).6. Benveniste, E. N. in Neuroglia (eds Kettenmann, H. &Ransom, B. R.) 700–716 (Oxford, New York, 1995).7. Perry, V. H. Macrophages and the Nervous System(Landes, Austin, 1994).8. Gehrmann, J. & Kreutzberg, G. W. in Neuroglia(eds Kettenmann, H. & Ransom, B. R.) 883–904 (Oxford,New York, 1995).9. Araque, A., Parpura, V., Sanzgiri, R. P. & Haydon, P. G.Tripartite synapses: glia, the unacknowledged partner.Trends Neurosci. 22, 208–215 (1999).Synapses can no longer be considered as simply apresynaptic neuron and a postsynaptic neuron.Rather, three entities are involved, the third beingastrocytes. A review of the evidence that astrocytes‘listen’ to neuronal communication and ‘talk back’to the neurons is provided.10. Garrison, C. J., Dougherty, P. M., Kajander, K. C. &Carlton, S. M. Staining of glial fibrillary acidic protein (GFAP)in lumbar spinal cord increases following a sciatic nerveconstriction injury. Brain Res. 565, 1–7 (1991).This research article is historically important as itprovides the first evidence that nerve damage,which creates neuropathic pain, also activatesspinal cord glial11. Garrison, C. J., Dougherty, P. M. & Carlton, S. M. GFAPexpression in lumbar spinal cord of naive and neuropathicrats treated with MK-801. Exp. Neurol. 129, 237–243 (1994).Historically important, this article provides the firstevidence that drugs that inhibit neuropathic pain alsoinhibit glial activation. It provided the first evidencethat, at minimum, neuropathic pain and glial activationare strongly correlated.12. Watkins, L. R., Milligan, E. D. & Maier, S. F. Glial activation:a driving force for pathological pain. Trends Neurosci. 24,450–455 (2001).Evidence is reviewed that spinal cord glia are keymediators in the creation and maintenance ofexaggerated pain states.13. Berg-Johnsen, J., Paulsen, R. E., Fonnum, F. &Langmoen, I. A. Changes in evoked potentials and aminoacid content during fluorocitrate action studied in rathippocampal cortex. Exp. Brain Res. 96, 241–246 (1993).14. Hassel, B., Paulsen, R. E., Johnson, A. & Fonnum, F.Selective inhibition of glial cell metabolism by fluorocitrate.Brain Res. 249, 120–124 (1992).15. Tikka, T. M. & Koistinaho, J. E. Minocycline providesneuroprotection against N-methyl-D-aspartateneurotoxicity by inhibiting microglia. J. Immunol. 166,7527–7533 (2001).16. Meller, S. T., Dykstra, C., Grzbycki, D., Murphy, S. &Gebhart, G. F. The possible role of glia in nociceptiveprocessing and hyperalgesia in the spinal cord of the rat.Neuropharmacology 33, 1471–1478 (1994).Provides the first evidence that disrupting glialactivation blocks exaggerated pain responses. Inaddition, it is the first evidence that activation of glia,in their role as immune cells, is sufficient to induceexaggerated pain responses.17. Watkins, L. R., Martin, D., Ulrich, P., Tracey, K. J. &Maier, S. F. Evidence for the involvement of spinal cord gliain subcutaneous formalin induced hyperalgesia in the rat.Pain 71, 225–235 (1997).18. Milligan, E. D. et al. Thermal hyperalgesia and mechanicalallodynia produced by intrathecal administration of thehuman immunodeficiency virus-1 (HIV-1) envelopeglycoprotein, gp120. Brain Res. 861, 105–116 (2000).19. Milligan, E. D. et al. Spinal glia and proinflammatorycytokines mediate mirror-image neuropathic pain.J. Neurosci. 23, 1026–1040 (2003).20. Raghavendra, V., Tanga, F. & DeLeo, J. A. Inhibition ofmicroglial activation attenuates the development but notexisting hypersensitivity in a rat model of neuropathy.J. Pharmacol. Exp. Ther. 306, 624–630 (2003).Anatomical and pharmacological evidence supportsthe intriguing hypothesis that microglia are key in theinitiation of exaggerated pain states, but thatastrocytes (and not microglia) are crucial for themaintenance of enhanced pain.21. Ledeboer, A. et al. Selective inhibition of spinal cord microglialactivation attenuates mechanical allodynia in rat models ofpathological pain. Proc. Soc. Neurosci. (in the press).22. Cholewinski, A. J., Hanley, M. R. & Wilkin, G. P. Aphosphoinositide-linked peptide response in astrocytes:evidence for regional heterogeneity. Neurochem. Res. 13,389–394 (1988).23. Beaujouan, J. C. et al. Marked regional heterogeneity of125I-Bolton Hunter substance P binding and substanceP-induced activation of phospholipase C in astrocytecultures from the embryonic or newborn rat. J. Neurochem.54, 669–675 (1990).24. Sung, B., Lim, G. & Mao, J. Altered expression and uptakeactivity of spinal glutamate transporters after nerve injurycontribute to the pathogenesis of neuropathic pain in rats.J. Neurosci. 23, 2899–2910 (2003).25. Ochalski, P. A., Frankenstein, U. N., Hertzberg, E. L. &Nagy, J. I. Connexin-43 in rat spinal cord: localization inastrocytes and identification of heterotypic astro-oligodendrocyticgap junctions. Neurosci. 76, 931–945 (1997).26. Li, W. E. & Nagy, I. Activation of fibres in rat sciatic nervealters phosphorylation state of connexin-43 at astrocyticgap junctions in spinal cord: evidence for junction regulationby neuronal–glial interactions. Neurosci. 97, 113–123(2000).27. Palma, C. et al. Functional characterization of substance Preceptors on cultured human spinal cord astrocytes:synergism of substance P with cytokines in inducinginterleukin-6 and prostaglandin E2 production. Glia 21,183–193 (1997).28. Tikka, T., Fiebich, B. L., Goldsteins, G., Keinanen, R. &Koistinaho, J. Minocycline, a tetracycline derivative, isneuroprotective against excitotoxicity by inhibiting activationand proliferation of microglia. J. Neurosci. 21, 2580–2588(2001).29. Bartlett, P. F. Pluripotential hemopoietic stem cells in adultmouse brain. Proc. Natl Acad. Sci. USA 79, 2722–2725(1982).30. Carson, M. J., Reilly, C. R., Sutcliffe, J. G. & Lo, D. Maturemicroglia resemble immature antigen-presenting cells. Glia22, 72–85 (1998).31. Fedoroff, S. in Neuroglia (eds Kettenmann, H. &Ransom, B. R.) 162–184 (Oxford, New York, 1995).32. Lee, J. C., Mayer-Proschel, M. & Rao, M. S. Gliogenesis inthe central nervous system. Glia 30, 105–121 (2000).33. Watkins, L. R., Hansen, M. K., Nguyen, K. T., Lee, J. E. &Maier, S. F. Dynamic regulation of the proinflammatorycytokine, interleukin-1β: molecular biology for non-molecularbiologists. Life Sci. 65, 449–481 (1999).34. Milligan, E. D. et al. Intrathecal HIV-1 envelope glycoproteingp120 induces enhanced pain states mediated by spinalcord proinflammatory cytokines. J. Neurosci. 21,2808–2819 (2001).The first demonstration that activation of spinal cordglia, in their role as immune cells; (i) is sufficient toinduce thermal hyperalgesia and mechanicalallodynia, (ii) induces the production and release ofpro-inflammatory cytokines, and (iii) this proinflammatorycytokine release is causal to theresultant pain enhancement.NATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 983
REVIEWS35. Harrison, J. K. et al. Role for neuronally derived fractalkinein mediating interactions between neurons andCX3CR1-expressing microglia. Proc. Natl Acad. Sci. USA95, 10896–10901 (1998).36. Watkins, L. R., Milligan, E. D. & Maier, S. F. in Advances inPain Research and Therapy (eds Dostrovsky, J. O., Carr, D. B.& Koltzenberg, M.) 369–385 (IASP, Seattle, 2003).37. Verge, G. et al. Mapping fractalkine and its receptor(CX3CR1) in a rat model of sciatic inflammatory neuropathy(SIN). Proc. Soc. Neurosci. 28, 455.3 (2002).38. Chapman, G. A. et al. Fractalkine cleavage from neuronalmembranes represents an acute event in the inflammatoryresponse to excitotoxic brain damage. J. Neurosci. 20,RC87 (1–5) (2000).39. Dinarello, C. A. in Cytokines and Pain (eds Watkins, L. R. &Maier, S. F.) 1–19 (Birkhauser, Basel, 1999).An excellent review of pro-inflammatory cytokinemolecular biology and cellular signalling, with a focuson their role in pain facilitation.40. Maier, S. F. & Watkins, L. R. Cytokines for psychologists:implications of bi-directional immune-to-braincommunication for understanding behavior, mood, andcognition. Psychol. Rev. 105, 83-107 (1998).This review article examines the role ofpro-inflammatory cytokines in a wide array ofperipheral, brain and spinal cord processes.It is aimed at non-specialists to introduce themto this research area41. DeLeo, J. A., Colburn, R. W., Nochols, M. & Malhotra, A.Interleukin-6-mediated hyperalgesia/allodynia and increasedspinal IL-6 expression in a rat mononeuropathy model.J. Interferon Cytokine Res. 16, 695–700 (1996).42. Falchi, M., Ferrara, G., Gharib, C. & Dib, B. Hyperalgesiceffect of intrathecally administered interleukin-1 in rats.Drugs Exp. Clin. Res. 27, 97–101 (2001).43. Reeve, A. J., Patel, S., Fox, A., Walker, K. & Urban, L.Intrathecally administered endotoxin or cytokines produceallodynia, hyperalgesia and changes in spinal cord neuronalresponses to nociceptive stimuli in the rat. Eur. J. Pain 4,247–257 (2000).44. Tadano, T. et al. Induction of nociceptive responses byintrathecal injection of interleukin-1 in mice. Life Sci. 65,255–261 (1999).45. Oka, T. & Hori, T. in Cytokines and Pain (eds Watkins, L. R.& Maier, S. F.) 183–204 (Birkhauser, Basel, 1999).46. Sweitzer, S. M., Martin, D. & DeLeo, J. A. Intrathecalinterleukin-1 receptor antagonist in combination with solubletumor necrosis factor receptor exhibits an anti-allodynicaction in a rat model of neuropathic pain. Neurosci. 103,529–539 (2001).47. Clark, A. R., Dean, J. L. E. & Saklatvala, J. Posttranscriptionalregulation of gene expression by mitogenactivatedprotein kinase p38. FEBS Lett. 546, 37–44(2003).48. Svensson, C. I. et al. Activation of p38 MAP kinase in spinalmicroglia is a critical link in inflammation induced spinal painprocessing. J. Neurochem. (in the press).49. Svensson, C. I., Hua, X. Y., Protter, A. A., Powell, H. C. &Yaksh, T. L. Spinal p38 MAP kinase is necessary for NMDAinduced spinal PGE 2release and thermal hyperalgesia.Neuroreport 14, 1153–1157 (2003).50. Schafers, M., Svensson, C. I., Sommer, C. & Sorkin, L. S.Tumor necrosis factor induces mechanical allodynia afterspinal nerve ligation by activation of p38 MAPK in primarysensory neurons. J. Neurosci. 23, 2517–2521 (2003).51. Jones, T. L. et al. Involvement of p38α MAPK incapsaicin-induced hyperalgesia. Proc. Soc. Neurosci.28, 56.5 (2002).52. Milligan, E. D. et al. Systemic administration of CNI-1493, ap38 MAP kinase inhibitor, blocks HIV-1 gp120-inducedenhanced pain states in rats. J. Pain 2, 326–333 (2001).53. Sweitzer, S. M., Schubert, P. & DeLeo, J. A. Propentofylline,a glial modulating agent, exhibits antiallodynic properties in arat model of neuropathic pain. J. Pharmacol. Exp. Ther. 297,1210–1217 (2001).54. Winkelstein, B. A., Rutkowski, M. D., Sweitzer, S. M.,Pahl, J. L. & DeLeo, J. A. Nerve injury proximal or distal tothe DRG induces similar spinal glial activation and selectivecytokine expression but differential behavioral responses topharmacologic treatment. J. Comp. Neurol. 2, 127–139(2001).55. Hashizume, H., Rutkowski, M. D., Weinstein, J. N. &DeLeo, J. A. Central administration of methotrexate reducesmechanical allodynia in an animal model ofradiculopathy/sciatica. Pain 87, 159–169 (2000).56. Sommer, C., Marziniak, M. & Myers, R. R. The effect ofthalidomide treatment on vascular pathology andhyperalgesia caused by chronic constriction injury of ratnerve. Pain 74, 83–91 (1998).57. George, A., Marziniak, M., Schafers, M., Toyka, K. V. &Sommer, C. Thalidomide treatment in chronic constrictiveneuropathy decreases endoneurial tumor necrosis factor-α,increases interleukin-10 and has long-term effects on spinalcord dorsal horn met-enkephalin. Pain 88, 267–275 (2000).58. Eriksson, T., Bjorkman, S. & Hoglund, P. Clinicalpharmacology of thalidomide. Eur. J. Clin. Pharmacol. 5,365–376 (2001).59. Clemmensen, O. J., Olsen, P. Z. & Andersen, K. E.Thalidomide neurotoxicity. Arch. Dermatol. 120, 338–341(1984).60. Strle, K. et al. Interleukin-10 in the brain. Crit. Rev. Immunol.21, 427–449 (2001).61. Moore, K. W., deWaal Malefyt, R., Coffman, R. L. &O’Garra, A. Interleukin-10 and the interleukin-10 receptor.Annu. Rev. Immunol. 19, 683–765 (2001).62. Ledeboer, A. et al. Regional and temporal expressionpatterns of interleukin-10, interleukin-10 receptor andadhesion molecules in the rat spinal cord during chronicrelapsing EAE. J. Neuroimmunol. 136, 94–103 (2003).63. Yu, C.-G., Fairbanks, C. A., Wilcox, G. L. & Yezierski, R. P.Effects of agmatine, interleukin-10 and cyclosporin onspontaneous pain behavior following excitotoxic spinal cordinjury in rats. J. Pain (in the press).64. Laughlin, T. M., Bethea, J. R., Yezierski, R. P. & Wilcox, G. L.Cytokine involvement in dynorphin-induced allodynia. Pain84, 159–167 (2000).65. Plunkett, J. A., Yu, C.-G., Easton, J. M., Bethea, J. R. &Yezierski, R. P. Effects of interelukin-10 (IL-10) on painbehavior and gene expression following excitotoxic spinalcord injury in the rat. Exper. Neurol. 168, 144–154 (2001).66. Hornfeldt, C. S. & Larson, A. A. Seizures induced byfluoroacetic acid and fluorocitric acid may involve chelationof divalent cations in the spinal cord. Eur. J. Pharmacol. 179,307–313 (1990).67. Yrjanheikki, J., Keinanen, R., Pellikka, M., Hokfelt, T. &Korstinaho, J. Tetracyclines inhibit microglial activation andare neuroprotective in global brain ischemia. Neurobiology95, 15769–15774 (1998).68. Lin, S. et al. Minocycline blocks nitric oxide-inducedneurotoxicity by inhibition of p38 MAP kinase in rat cerebellargranule neurons. Neurosci. Lett. 315, 61–64 (2001).69. Kary, S. & Burmester, G. R. Anakinra: the first interleukin-1inhibitor in the treatment of rheumatoid arthritis. Int. J. Clin.Pract. 57 (2003).70. Calabrese, L. H. Molecular differences in anticytokinetherapies. Clin. Exp. Rheumatol. 21, 241–248 (2003).71. Mielke, R. et al. Propentofylline in the treatment of vasculardementia and Alzheimer-type dementia: overview of phase Iand phase II clinical trials. Alzheimer Dis. Assoc. Disord. 12,S29–35 (1998).72. Rother, M. et al. Propentofylline in the treatment ofAlzheimer’s disease and vascular dementia: a review ofphase III trials. Dement. Geriatr. Cogn. Disord. 9, 36–43(1998).73. Plaschke, K. et al. Neuromodulatory effect ofpropentofylline on rat brain under acute and long-termhypoperfusion. Br. J. Pharmacol. 133, 107–116 (2001).74. Wu, Y. P., McRae, A., Rudolphi, K. & Ling, E. A.Propentofylline attenuates microglial reaction in the rat spinalcord induced by middle cerebral artery occlusion. Neurosci.Lett. 260, 17–20 (1999).75. Numagami, Y., Marro, P. J., Mishra, O. P. & Delivoria-Papadopoulos, M. Effect of propentofylline on free radicalgeneration during cerebral hypoxia in the newborn piglet.Neuroscience 84, 1127–1133 (1998).76. Schubert, P. et al. Cascading glia reactions: a commonpathomechanism and its differentiated control by cyclicnucleotide signaling. Ann. NY Acad. Sci. 903, 24–33(2000).77. Schubert, P., Ogata, T., Marchini, C., Ferroni, S. &Rudolphi, K. Protective mechanisms of adenosine inneurons and glial cells. Ann. NY Acad. Sci. 825, 1–10 (1997).78. Sawynok, J. & Liu, X. J. Adenosine in the spinal cord andperiphery: release and regulation of pain. Prog. Neurobiol.69, 313–340 (2003).79. Si, Q., Nakamura, Y., Ogata, T., Kataoka, K. & Schubert, P.Differential regulation of microglial activation by propentofyllinevia cAMP signaling. Brain Res. 812, 97–104 (1998).80. Matthews, S. J. & McCoy, C. Thalidomide: a review ofapproved and investigational uses. Clin. Ther. 25, 342–395(2003).81. Mujagic, H., Chabner, B. A. & Mujagic, Z. Mechanisms ofaction and potential therapeutic uses of thalidomide. Croat.Med. J. 43, 274–285 (2002).82. Majumdar, S., Lamothe, B. & Aggarwal, B. B. Thalidomidesuppresses NF-κB activation induced by TNF and H 2O 2,but not that activated by ceramide, lipopolysaccharides, orphorbol ester. J. Immunol. 168, 2644–2651 (2002).83. Gallily, R., Kipper-Galperin, M. & Brenner, T. Mycoplasmafermentans-induced inflammatory response of astrocytes:selective modulation by aminoguanidine, thalidomide,pentoxifylline and IL-10. Inflammation 23, 495–505 (1999).84. Peterson, P. K. et al. Thalidomide inhibits tumor necrosisfactor-α production by lipopolysaccharide- andlipoarabinomannan-stimulated human microglial cells.J. Infect. Dis. 172, 1137–1140 (1995).85. Moreira, A. L. et al. Thalidomide exerts its inhibitory actionon tumor necrosis factor-α by enhancing mRNAdegradation. J. Exp. Med. 177, 1675–1680 (1993).86. Corral, L. G. et al. Differential cytokine modulation and T cellactivation by two distinct classes of thalidomide analoguesthat are potent inhibitors of TNF-α. J. Immunol. 163,380–386 (1999).87. Li, J., Luo, S., Hong, W., Zhou, Z. & Zou, W. Influence ofthalidomide on interleukin-6 and its transmission in multiplemyeloma patients. Zhonghua Zhong Liu Za Zhi 24,254–256 (2002).88. Bauditz, J., Wedel, S. & Lochs, H. Thalidomide reducestumour necrosis factor-α and interleukin-12 production inpatients with chronic active Crohn’s disease. Gut 50,196–200 (2002).89. Jin, S. H., Kim, T. I., Han, D. S., Shin, S. K. & Kim, W. H.Thalidomide suppresses the interleukin 1β-induced NF-κBsignaling pathway in colon cancer cells. Ann. NY Acad. Sci.973, 414–418 (2002).90. Thiele, A. et al. Cytokine modulation and suppression of liverinjury by a novel analogue of thalidomide. Eur. J. Pharmacol.453, 325–334 (2002).91. Rajkumar, S. V., Fonseca, R. & Witzig, T. E. Completeresolution of reflex sympathetic dystrophy with thalidomidetreatment. Arch. Intern. Med. 161, 2502–2503 (2001).92. Prager, J., Fleischman, J. & Lingua, G. Open label clinicalexperience of thalidomide in the treatment of complexregional pain syndrome Type 1. J. Pain 4, S68 (2003).93. Sanders, S. & Harisdangkul, V. Leflunomide for thetreatment of rheumatoid arthritis and autoimmunity.Am. J. Med. Sci. 323, 190–193 (2002).94. Furst, D. E. Innovative treatment approaches for rheumatoidarthritis. Cyclosporin, leflunomide and nitrogen mustard.Baillieres Clin. Rheumatol. 9, 711–729 (1995).95. Kraan, M. C. et al. Modulation of inflammation andmetalloproteinase expression in synovial tissue byleflunomide and methotrexate in patients with activerheumatoid arthritis. Findings in a prospective,randomized, double-blind, parallel-design clinical trial inthirty-nine patients at two centers. Arthritis Rheum. 43,1820–1830 (2000).96. Elkayam, O. et al. Active leflunomide metabolite inhibitsinterleukin-1β, tumour necrosis factor-α, nitric oxide, andmetalloproteinase-3 production in activated humansynovial tissue cultures. Ann. Rheum. Dis. 62, 440–443(2003).97. Cutolo, M. et al. Anti-inflammatory effects of leflunomide oncultured synovial macrophages from patients withrheumatoid arthritis. Ann. Rheum. Dis. 62, 297–302 (2003).98. Manna, S. K., Mukhopadhyay, A. & Aggarwal, B. B.Leflunomide suppresses TNF-induced cellular responses:effects on NF-κB, activator protein-1, c-Jun N-terminalprotein kinase, and apoptosis. J. Immunol. 165, 5962–5969(2000).99. Fox, R. I. et al. Mechanism of action for leflunomide inrheumatoid arthritis. Clin. Immunol. 93, 198–208 (1999).100. Herrmann, M. L., Schleyerbach, R. & Kirschbaum, B. J.Leflunomide: an immunomodulatory drug for the treatmentof rheumatoid arthritis and other autoimmune diseases.Immunopharmacology 47, 273–289 (2000).101. Miljkovic, D. et al. Leflunomide inhibits activation of induciblenitric oxide synthase in rat astrocytes. Brain Res. 889,331–338 (2001).102. Bao, L. et al. Adjuvant-induced arthritis: IL-1β, IL-6 andTNF-α are up-regulated in the spinal cord. Neuroreport 12,3905–3908 (2001).103. Bruce-Gregorios, J. H., Soucy, D. M., Chen, M. G. &Norenberg, M. D. Effect of methotrexate on glial fibrillaryacidic protein content of astrocytes in primary culture.J. Neuropathol. Exp. Neurol. 50, 118–125 (1991).104. el-Badawi, M. G., Fatani, J. A., Bahakim, H. & Abdalla, M. A.Light and electron microscopic observations on thecerebellum of guinea pigs following low-dose methotrexate.Exp. Mol. Pathol. 53, 211–222 (1990).105. Longo-Sorbello, G. S. & Bertino, J. R. Currentunderstanding of metrotrexate pharmacology and efficacyin acute leukemias. Use of newer antifolates in clinical trials.Haematologica 86, 121–127 (2001).106. Chan, E. S. & Cronstein, B. N. Molecular action ofmethotrexate in inflammatory diseases. Arthritis Res. 4,266–273 (2002).984 | DECEMBER 2003 | VOLUME 2 www.nature.com/reviews/drugdisc
REVIEWS107. Cronstein, B. N., Naime, D. & Ostad, E. The antiinflammatoryeffects of methotrexate are mediated byadenosine. Adv. Exp. Med. Biol. 370, 411–416 (1994).108. Montesinos, M. C. et al. Reversal of the antiinflammatoryeffects of methotrexate by the nonselective adenosinereceptor antagonists theophylline and caffeine: evidencethat the antiinflammatory effects of methotrexate aremediated via multiple adenosine receptors in rat adjuvantarthritis. Arthritis Rheum. 43, 656–663 (2000).109. Neurath, M. F. et al. Methotrexate specifically modulatescytokine production by T cells and macrophages in murinecollagen-induced arthritis (CIA): a mechanism formethotrexate-mediated immunosuppression. Clin. Exp.Immunol. 115, 42–55 (1999).110. Hayem, G., Domarle, O., Thuong-Guyot, M., Pocidalo, J. J.& Meyer, O. Effects of methotrexate on the oxidativemetabolism of cultured rabbit articular chondrocytes.J. Rheumatol. 27, 1117–1120 (2000).111. Rudwaleit, M. et al. Response to methotrexate in earlyrheumatoid arthritis is associated with a decrease of T cellderived tumour necrosis factor-α, increase of interleukin-10,and predicted by the initial concentration of interleukin-4.Ann. Rheum. Dis. 59, 311–314 (2000).112. Brody, M., Bohm, I. & Bauer, R. Mechanism of action ofmethotrexate: experimental evidence that methotrexateblocks the binding of interleukin-1β to the interleukin-1receptor on target cells. Eur. J. Clin. Chem. Clin. Biochem.31, 667–674 (1993).113. Segal, R., Mozes, E., Yaron, M. & Tartakovsky, B. The effectsof methotrexate on the production and activity of interleukin-1.Arthritis Rheum. 32, 370–377 (1989).114. Segal, R., Yaron, M. & Tartakovsky, B. Rescue ofinterleukin-1 activity by leucovorin following inhibition bymethotrexate in a murine in vitro system. Arthritis Rheum.33, 1745–1748 (1990).115. Gregorios, J. B. et al. Morphologic alterations in rat brainfollowing systemic and intraventricular methotrexateinjection: light and electron microscopic studies.J. Neuropathol. Exp. Neurol. 48, 33–47 (1989).116. Hommes, D. et al. Inhibition of stress-activated MAP kinasesinduces clinical improvement in moderate to severe Crohn’sdisease. Gastroenterology 122, 7–14 (2002).117. Lali, F. V., Hunt, A. E., Turner, S. J. & Foxwell, B. M. Thepyridinyl imidazole inhibitor SF203580 blocksphosphoinositide-dependent protein kinase activity, proteinkinase B phosphorylation, and retinoblastomahyperphosphorylation in interleukin-2-stimulated T cellsindependently of p38 mitogen-activated protein kinase.J. Biol. Chem. 275, 7395–7402 (2000).118. Dunn, S. L., Young, E. A., Hall, M. D. & McNulty, S. Activationof astrocyte intracellular signaling pathways by interleukin-1 inrat primary striatal cultures. Glia 37, 31–42 (2002).119. Jeohn, G. H. et al. Go6976 inhibits LPS-induced microglialTNF-α release by suppressing p38 MAP kinase activation.Neuroscience 114, 689–697 (2002).120. Jin, S. X., Zhaung, Z. Y., Woolf, C. J. & Ji, R. R. p38 MAPK isactivated after a spinal nerve ligation first in spinal cordmicroglia and then in DRG neurons and contributes to thegeneration of neuropathic pain. J. Neurosci. 23, 4017–4022(2003).121. Kim, S. Y. et al. Activation of p38 MAP kinase in the rat dorsalroot ganglia and spinal cord following peripheral inflammationand nerve injury. Neuroreport 13, 2483–2486 (2002).122. Hamilton, T. A., Ohmori, Y., Tebo, J. M. & Kishore, R.Regulation of macropahge gene expression by pro- and antiinflammatorycytokines. Pathobiology 67, 241–244 (1999).123. Kontoyiannis, D. et al. Interleukin-10 targets p38 MAPK tomodulate ARE-dependent TNF mRNA translation and limitintestinal pathology. EMBO J. 20, 3760–3770 (2001).124. Donnelly, R. P., Dickensheets, H. & Finbloom, D. S. Theinterleukin-10 signal transduction pathway and regulation ofgene expression in mononuclear phagocytes. J. InterferonCytokine Res. 19, 563–573 (1999).125. Sawada, M., Suzumura, A., Hosoya, H., Marunouchi, T. &Nagatsu, T. Interleukin-10 inhibits both production ofcytokines and expression of cytokine receptors in microglia.J. Neurochem. 72, 1466–1471 (1999).126. Foey, A. D. et al. Regulation of monocyte IL-10 synthesis byendogenous IL-1 and TNF-α: role of the p38 and p42/44mitogen-activated protein kinases. J. Immunol. 160,920–928 (1998).127. Huber, T. S. et al. Anticytokine therapies for acuteinflammation and the systemic inflammatory responsesyndrome: IL-10 and ischemia/reperfusion injury. Shock13, 425–434 (2000).128. Bachis, A. et al. Interleukin-10 prevents glutamate-mediatedcerebellar granule cell death by blocking caspase-3-likeactivity. J. Neurosci. 21, 3104–3112 (2001).129. Milligan, E. D. et al. Inflammatory and chronic constrictioninjury-induced pain states are controlled by spinal deliveryof viral and non-viral vectors encoding the antiinflammatorygene, interleukin-10 (IL10). Proc. Soc.Neurosci. 29 (in the press).130. Kastin, A. J., Akerstrom, V. & Pan, W. Interleukin-10 as aCNS therapeutic: the obstacle of theblood–brain/blood–spinal cord barrier. Brain Res. Mol.Brain Res. 114, 168–171 (2003).131. Davidson, B. L. & Breakefield, X. O. Viral vectors for genedelivery to the nervous system. Nature Rev. Neurosci. 4,353–364 (2003).This review article focuses on the promise of genetherapy for the resolution of a variety of clinical targets.132. Xu, Z. L., Mizuguchi, H., Mayumi, T. & Hayakawa, T.Regulated gene expression from adenovirus vectors: asystematic comparison of various inducible systems.Gene 309, 145–151 (2003).133. Wiesler-Frank, J., Milligan, E. D., Maier, S. F. & Watkins, L. R.in Encyclopedic Reference of Pam (eds Schmidt, R. &Willis, W. D.) (Springer, Berlin, in the press).134. Volterra, A. & Bezzi, P. in The Tripartite Synapse (edsVolterra, A., Magistretti, P. J. & Hayden, P. G.) 164–182(Oxford Univ. Press, Oxford, 2002).AcknowledgementsOur laboratory is supported by grants from the National Institute onDrug Abuse, National Institute of Neurological Diseases and Stroke,and National Institute of Mental Health.Competing interest statementThe authors declare competing financial interests: see Web versionfor details.Online linksDATABASESThe following terms in this article are linked online to:LocusLink: http://www.ncbi.nlm.nih.gov/LocusLink/CX3CR1 | fractalkineOnline Mendelian Inheritance in Man:http://www.ncbi.nlm.nih.gov/Omim/Alzheimer’s disease | Crohn’s disease | rheumatoid arthritisAccess to this interactive links box is free online.NATURE REVIEWS | <strong>DRUG</strong> <strong>DISCOVERY</strong> VOLUME 2 | DECEMBER 2003 | 985