In This Issue2 3 4 5 6 7 8 - Catholic Health System
In This Issue2 3 4 5 6 7 8 - Catholic Health System
In This Issue2 3 4 5 6 7 8 - Catholic Health System
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
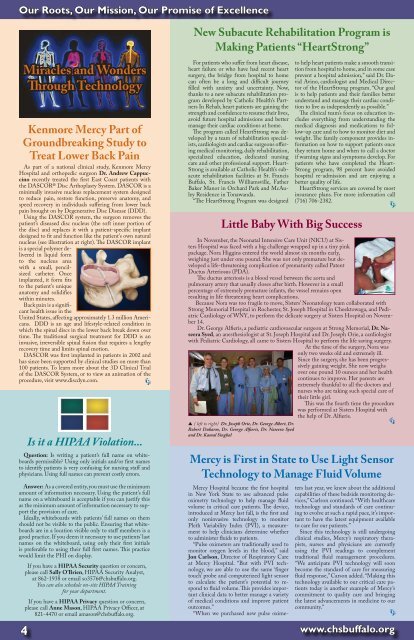
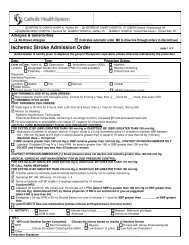
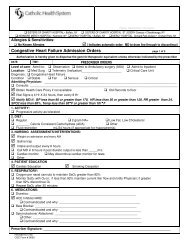
Our Roots, Our Mission, Our Promise of ExcellenceMiracles and WondersThrough TechnologyKenmore Mercy Part ofGroundbreaking Study toTreat Lower Back PainAs part of a national clinical study, Kenmore MercyHospital and orthopedic surgeon Dr. Andrew Cappuccinorecently treated the first East Coast patients withthe DASCOR® Disc Arthoplasty <strong>System</strong>. DASCOR is aminimally invasive nucleus replacement system designedto reduce pain, restore function, preserve anatomy, andspeed recovery in individuals suffering from lower backpain brought on by Degenerative Disc Disease (DDD).Using the DASCOR system, the surgeon removes thepatient’s diseased disc nucleus (the soft inner portion ofthe disc) and replaces it with a patient-specific implantdesigned to fit and function like the patient’s own naturalnucleus (see illustration at right). The DASCOR implantis a special polymer deliveredin liquid formto the nucleus areawith a small, pencilsizedcatheter. Onceimplanted, it form fitsto the patient’s uniqueanatomy and solidifieswithin minutes.Back pain is a significanthealth issue in theUnited States, affecting approximately 1.3 million Americans.DDD is an age and lifestyle-related condition inwhich the spinal discs in the lower back break down overtime. The traditional surgical treatment for DDD is aninvasive, irreversible spinal fusion that requires a lengthyrecovery time and limits spinal motion.DASCOR was first implanted in patients in 2002 andhas since been supported by clinical studies on more than100 patients. To learn more about the 3D Clinical Trialof the DASCOR <strong>System</strong>, or to view an animation of theprocedure, visit www.discdyn.com.4Is it a HIPAA Violation...Question: Is writing a patient’s full name on whiteboardspermissible? Using only initials and/or first namesto identify patients is very confusing for nursing staff andphysicians. Using full names can prevent costly errors.Answer: As a covered entity, you must use the minimumamount of information necessary. Using the patient’s fullname on a whiteboard is acceptable if you can justify thisas the minimum amount of information necessary to supportthe provision of care.Ideally, whiteboards with patients’ full names on themshould not be visible to the public. Ensuring that whiteboardsare in a location visible only to staff members is agood practice. If you deem it necessary to use patients’ lastnames on the whiteboard, using only their first initialsis preferable to using their full first names. <strong>This</strong> practicewould limit the PHI on display.If you have a HIPAA Security question or concern,please call Sally O’Brien, HIPAA Security Analyst,at 862-1938 or email so3576@chsbuffalo.org.You can also schedule on-site HIPAA Trainingfor your department.If you have a HIPAA Privacy question or concern,please call Anne Mason, HIPAA Privacy Officer, at821-4470 or email amason@chsbuffalo.org.New Subacute Rehabilitation Program isMaking Patients “HeartStrong”For patients who suffer from heart disease,heart failure or who have had recent heartsurgery, the bridge from hospital to homecan often be a long and difficult journeyfilled with anxiety and uncertainty. Now,thanks to a new subacute rehabilitation programdeveloped by <strong>Catholic</strong> <strong>Health</strong>’s Partners<strong>In</strong> Rehab, heart patients are gaining thestrength and confidence to resume their lives,avoid future hospital admissions and bettermanage their cardiac conditions at home.The program called HeartStrong was developedby a team of rehabilitation specialists,cardiologists and cardiac surgeons offeringmedical monitoring, daily rehabilitation,specialized education, dedicated nursingcare and other professional support. Heart-Strong is available at <strong>Catholic</strong> <strong>Health</strong>’s subacuterehabilitation facilities at St. FrancisBuffalo, St. Francis Williamsville, FatherBaker Manor in Orchard Park and McAuleyResidence in Tonawanda.“The HeartStrong Program was designedto help heart patients make a smooth transitionfrom hospital to home, and in some caseprevent a hospital admission,” said Dr. DavidAvino, cardiologist and Medical Directorof the HeartStrong program. “Our goalis to help patients and their families betterunderstand and manage their cardiac conditionto live as independently as possible.”The clinical team’s focus on education includeseverything from understanding themedical diagnosis and medications to follow-upcare and to how to monitor diet andweight. The family component provides informationon how to support patients oncethey return home and when to call a doctorif warning signs and symptoms develop. Forpatients who have completed the Heart-Strong program, 98 percent have avoidedhospital re-admission and are enjoying abetter quality of life.HeartStrong services are covered by mostinsurance plans. For more information call(716) 706-2382.Little Baby With Big Success<strong>In</strong> November, the Neonatal <strong>In</strong>tensive Care Unit (NICU) at SistersHospital was faced with a big challenge wrapped up in a tiny pinkpackage. Nora Higgins entered the world almost six months early,weighing just under one pound. She was not only premature but developeda life-threatening complication of prematurity called PatentDuctus Arteriosus (PDA).The ductus arteriosis is a blood vessel between the aorta andpulmonary artery that usually closes after birth. However in a smallpercentage of extremely premature infants, the vessel remains openresulting in life threatening heart complications.Because Nora was too fragile to move, Sisters’ Neonatology team collaborated withStrong Memorial Hospital in Rochester, St. Joseph Hospital in Cheektowaga, and PediatricCardiology of WNY, to perform the delicate surgery at Sisters Hospital on November14.Dr. George Alfieris, a pediatric cardiovascular surgeon at Strong Memorial, Dr. NaseeraSyed, an anesthesiologist at St. Joseph Hospital and Dr. Joseph Orie, a cardiologistwith Pediatric Cardiology, all came to Sisters Hospital to perform the life saving surgery.At the time of the surgery, Nora wasonly two weeks old and extremely ill.Since the surgery, she has been progressivelygaining weight. She now weighsover one pound 10 ounces and her healthcontinues to improve. Her parents areextremely thankful to all the doctors andnurses who are taking such special care oftheir little girl.<strong>This</strong> was the fourth time the procedurewas performed at Sisters Hospital withthe help of Dr. Alfieris.▲ ( left to right) Dr. Joseph Orie, Dr. George Albert, Dr.Robert Dukarm, Dr. George Alfieris, Dr. Naseera Syedand Dr. Kamal SinghalMercy is First in State to Use Light SensorTechnology to Manage Fluid VolumeMercy Hospital became the first hospitalin New York State to use advanced pulseoximetry technology to help manage fluidvolume in critical care patients. The device,introduced at Mercy last fall, is the first andonly noninvasive technology to monitorPleth Variability <strong>In</strong>dex (PVI), a measurementto help clinicians determine whetherto administer fluids to patients.“Pulse oximeters are traditionally used tomonitor oxygen levels in the blood,” saidJon Carlson, Director of Respiratory Careat Mercy Hospital. “But with PVI technology,we are able to use the same ‘fingertouch’ probe and computerized light sensorto calculate the patient’s potential to respondto fluid volume. <strong>This</strong> provides importantclinical data to better manage a varietyof medical conditions and improve patientoutcomes.”“When we purchased new pulse oximeterslast year, we knew about the additionalcapabilities of these bedside monitoring devices,”Carlson continued. “With healthcaretechnology and standards of care continuingto evolve at such a rapid pace, it’s importantto have the latest equipment availableto care for our patients.”Since this technology is still undergoingclinical studies, Mercy’s respiratory therapists,nurses and physicians are currentlyusing the PVI readings to complementtraditional fluid management procedures.“We anticipate PVI technology will soonbecome the standard of care for measuringfluid response,” Carson added. “Making thistechnology available to our critical care patientstoday is another example of Mercy’scommitment to quality care and bringingthe latest advancements in medicine to ourcommunity.”www.chsbuffalo.org