Differential reinforcement of high rate behavior to increase the pace ...
Differential reinforcement of high rate behavior to increase the pace ...
Differential reinforcement of high rate behavior to increase the pace ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Behavioral InterventionsBehav. Intervent. 24: 17–22 (2009)Published online 16 December 2008 in Wiley InterScience(www.interscience.wiley.com) DOI: 10.1002/bin.273DIFFERENTIAL REINFORCEMENT OF HIGH RATEBEHAVIOR TO INCREASE THE PACE OF SELF-FEEDINGKelli M. Girolami 1 , SungWoo Kahng 2 *, Kellie A. Hilker 3 and Peter A. Girolami 31 Kennedy Krieger Institute, <strong>the</strong> University <strong>of</strong> Maryland, Baltimore County, USA2 Kennedy Krieger Institute, <strong>the</strong> Johns Hopkins University School <strong>of</strong> Medicine, USA3 Kennedy Krieger Institute, Baltimore USAAlthough numerous studies have examined treatments for increasing food consumption among childrenwith pediatric feeding disorders, very few have examined treatment <strong>of</strong> o<strong>the</strong>r mealtime-related difficulties.One such problem is a slow <strong>pace</strong> <strong>of</strong> self-feeding, which can lead <strong>to</strong> caregivers failure <strong>to</strong> adhere <strong>to</strong>treatments or be disruptive <strong>to</strong> o<strong>the</strong>rs. We examined <strong>the</strong> effects <strong>of</strong> a differential <strong>reinforcement</strong> <strong>of</strong> <strong>high</strong> <strong>rate</strong>(DRH) intervention <strong>to</strong> <strong>increase</strong> a 9-year-old boy’s <strong>pace</strong> <strong>of</strong> self-feeding. During treatment, <strong>the</strong> childreceived <strong>reinforcement</strong> contingent on consuming his meal within 30 min. Results showed an <strong>increase</strong> in<strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding and a concomitant decrease in meal duration as compared <strong>to</strong> baseline. Copyright# 2008 John Wiley & Sons, Ltd.INTRODUCTIONMealtime <strong>behavior</strong> problems (e.g., food refusal, food selectivity, and disruptive<strong>behavior</strong>) are relatively common in <strong>the</strong> pediatric population and are exhibited bychildren with and without developmental disabilities. Research suggests that 25–35%<strong>of</strong> typically developing children has some form <strong>of</strong> feeding problem, and <strong>the</strong>prevalence <strong>of</strong> feeding disorders is <strong>high</strong>er among individuals with disabilities and canreach as <strong>high</strong> as 80% among individuals with severe and pr<strong>of</strong>ound mental retardation(Linscheid, 1992; Palmer, Thompson, & Linscheid, 1975). Mealtime <strong>behavior</strong>problems are associated with an insufficient intake <strong>of</strong> nutrients and weight loss, whichcan have a harmful impact on children’s physical, social, and educationaldevelopment (Linscheid, Budd, & Rasnake, 1995).Although <strong>the</strong>re is a growing body <strong>of</strong> research demonstrating <strong>the</strong> efficacy <strong>of</strong><strong>behavior</strong>al interventions in increasing food acceptance/consumption (Iwata, Riordan,Wohl, & Finney, 1982; Kerwin, 1999), very few studies have examined o<strong>the</strong>r*Correspondence <strong>to</strong>: SungWoo Kahng, Department <strong>of</strong> Behavioral Psychology, Kennedy Krieger Institute, 707 N.Broadway, Baltimore, MD 21205, USA. E-mail: Kahng@kennedykrieger.orgCopyright # 2008 John Wiley & Sons, Ltd.
18 K. M. Girolami et al.mealtime-related difficulties such as staying seated, using appropriate utensils, and<strong>pace</strong> <strong>of</strong> self-feeding. The latter <strong>behavior</strong>, <strong>pace</strong> <strong>of</strong> self-feeding (i.e., <strong>the</strong> individualaccepts food but eats at an excessively rapid or slow <strong>pace</strong>), has been <strong>the</strong> focus <strong>of</strong> alimited amount <strong>of</strong> research. Although studies have evaluated methods <strong>of</strong> decreasingrapid self-feeding (Lennox, Miltenberger, & Donnelly, 1987; Wright & Vollmer,2002), eating <strong>to</strong>o slowly (i.e., dawdling) has very rarely been examined.Eating <strong>to</strong>o slowly during meals may result in lengthy meals, which is <strong>of</strong>tentimesdifficult and impractical for caregivers. This may in turn, lead some caregivers <strong>to</strong> relyupon less acceptable methods such as feeding <strong>the</strong> child. Dawdling during meals mayalso be problematic if <strong>the</strong> child is school-aged and has a limited amount <strong>of</strong> time <strong>to</strong> eat.In this instance, meals may be terminated early or <strong>the</strong> class schedule may be disruptedif <strong>the</strong> o<strong>the</strong>r students are required <strong>to</strong> wait.Luiselli (1988) used a prompting procedure <strong>to</strong> <strong>increase</strong> <strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding in achild with developmental disabilities. The participant was physically prompted <strong>to</strong>take a bite <strong>of</strong> food if she had not taken a bite within a certain period <strong>of</strong> time. Althougheffective in increasing <strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding, <strong>the</strong> prompting procedure may bedifficult <strong>to</strong> implement given <strong>the</strong> need for constant moni<strong>to</strong>ring. The purpose <strong>of</strong> <strong>the</strong>present study was <strong>to</strong> use a <strong>reinforcement</strong>-based procedure <strong>to</strong> <strong>increase</strong> <strong>the</strong> <strong>pace</strong> <strong>of</strong> selffeeding.Ideally, this intervention would require minimal prompting allowing for ease<strong>of</strong> implementation.METHODParticipantJude, a 9-year-old boy, was referred <strong>to</strong> <strong>the</strong> day treatment program for evaluation andtreatment for food refusal. Jude was diagnosed with failure <strong>to</strong> thrive, gastroesophagealreflux, attention deficit hyperactivity disorder (ADHD), and gastros<strong>to</strong>my tubedependence. He <strong>to</strong>ok a constant dose <strong>of</strong> methylphenidate (MPH) throughout thisevaluation. Jude received approximately 60% <strong>of</strong> his nutritional needs through hisgastros<strong>to</strong>my tube, due <strong>to</strong> his lack <strong>of</strong> solid and liquid intake by mouth. Although Judewould eat on occasion, he would not consume enough <strong>to</strong> sustain his needs, especially ina reasonable amount <strong>of</strong> time. A typical meal at home was terminated at about 35–45 min. If his parents tried <strong>to</strong> <strong>increase</strong> his food consumption, it <strong>to</strong>ok up <strong>to</strong> 1 hr. Despitelengthy meal times, he typically only consumed a few pieces <strong>of</strong> food.Dependent Variables, Data Collection, and Interobserver AgreementThe target <strong>behavior</strong>s were (a) number <strong>of</strong> independent bites consumed (i.e., howmany bites Jude consumed without a verbal prompt), which were converted <strong>to</strong> a <strong>rate</strong>Copyright # 2008 John Wiley & Sons, Ltd. Behav. Intervent. 24: 17–22 (2009)DOI: 10.1002/bin
Increasing self-feeding 19measure (bites per min) and (b) duration <strong>of</strong> <strong>the</strong> meal (min). The main goal was <strong>to</strong><strong>increase</strong> bites per min and decrease <strong>the</strong> amount <strong>of</strong> time it <strong>to</strong>ok him <strong>to</strong> eat an ageappropriate meal portion.All sessions were conducted in a <strong>the</strong>rapy room (3 m by 3 m). Observers were in <strong>the</strong>room collecting data on lap<strong>to</strong>p computers. A second observer independently collecteddata during 50 and 42% <strong>of</strong> <strong>the</strong> sessions in baseline and treatment, respectively.Interobserver agreement was calculated by dividing <strong>the</strong> <strong>to</strong>tal number <strong>of</strong> agreementsby <strong>the</strong> <strong>to</strong>tal number <strong>of</strong> agreements and disagreements. An agreement was defined aseach 10-s interval in which both observers scored <strong>the</strong> occurrence or <strong>the</strong> nonoccurrence<strong>of</strong> <strong>the</strong> <strong>behavior</strong>. Interobserver agreement was 95% (range, 88–98%) and92% (range, 67–98%) during baseline and treatment, respectively.ProceduresBaselineDuring baseline, Jude was instructed <strong>to</strong> eat 170 g <strong>of</strong> solid food and drink 118 ml <strong>of</strong>liquid (<strong>the</strong> liquid was eventually <strong>increase</strong>d <strong>to</strong> 177 ml) within 30 min (based on aparental interview). A timer set at 30 min was placed on a table nearby and was visible<strong>to</strong> Jude. There were no social consequences for consumption during <strong>the</strong> meal;however, Jude was given a verbal prompt <strong>to</strong> ‘take a bite’ or ‘take a drink’ if 2 min hadelapsed between bites <strong>of</strong> food or sips <strong>of</strong> drink. Therapists interacted with Jude byreciprocating conversation. Meals were terminated at 45 min.TreatmentTreatment consisted <strong>of</strong> differential <strong>reinforcement</strong> <strong>of</strong> <strong>high</strong> <strong>rate</strong> (DRH) <strong>behavior</strong>.This condition was similar <strong>to</strong> baseline except that if he consumed all <strong>of</strong> his food anddrink in 30 min or less, he received 10-min access <strong>to</strong> a video, which was identified ashis most <strong>high</strong>ly preferred stimulus through a preference assessment (Fisher, Piazza,Bowman, Hagopian, Owens, & Slevin, 1992). During treatment, Jude was againinstructed that <strong>the</strong> goal was <strong>to</strong> finish his meal in 30 min or less. Additionally, he wasinformed that if he met this goal, he would receive 10-min access <strong>to</strong> a Scooby Doo 1video. During treatment sessions, Jude was verbally prompted <strong>to</strong> ‘take a bite’ or ‘takea drink’ every 2 min, as in <strong>the</strong> baseline condition. Meals were terminated at 45 min.After 30 min elapsed, <strong>the</strong> timer beeped. If Jude consumed all his food and drink hewas provided access <strong>the</strong> Scooby Doo 1 video. If Jude did not finish his food and drinkwithin <strong>the</strong> 30-min time limit, he was <strong>to</strong>ld that he did not meet his goal but still had15 min <strong>to</strong> finish his meal.Copyright # 2008 John Wiley & Sons, Ltd. Behav. Intervent. 24: 17–22 (2009)DOI: 10.1002/bin
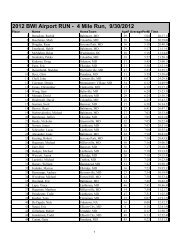
20 K. M. Girolami et al.Experimental DesignA multi-element design was used <strong>to</strong> demonst<strong>rate</strong> experimental control. In order <strong>to</strong>enhance discrimination across conditions, different colored tablecloths were used(baseline—yellow and DRH—green). The two conditions were randomly assigned<strong>to</strong> each meal and counterbalanced across meals (breakfast, lunch, and dinner). Datawere collected over a 3-week period starting when <strong>the</strong> participant was first admitted <strong>to</strong><strong>the</strong> hospital.RESULTS AND DISCUSSIONFollowing <strong>the</strong> initial introduction <strong>of</strong> treatment, <strong>the</strong>re was minimal differentiation inresponding between <strong>the</strong> two conditions (baseline and treatment). However, astreatment continued, <strong>the</strong> DRH intervention resulted in a significant <strong>increase</strong> in <strong>the</strong> <strong>rate</strong><strong>of</strong> self-feeding (Figure 1, Top Panel). During baseline, <strong>the</strong> <strong>rate</strong> <strong>of</strong> self-feeding was1.6 per min. During treatment, <strong>the</strong> self-feeding <strong>increase</strong>d <strong>to</strong> 2.0 per min. This <strong>increase</strong> in<strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding led <strong>to</strong> a decrease in meal duration. During baseline, <strong>the</strong> averageduration <strong>of</strong> meals was 35.5 min (Figure 1, Bot<strong>to</strong>m Panel). During treatment, <strong>the</strong> averageduration <strong>of</strong> meals decreased <strong>to</strong> 25.3 min, which amounted <strong>to</strong> a nearly 30% reduction in<strong>the</strong> duration <strong>of</strong> meals. Fur<strong>the</strong>rmore, Jude was completely weaned from <strong>the</strong> gastros<strong>to</strong>mytube over <strong>the</strong> course <strong>of</strong> <strong>the</strong> 8-week admission and no longer needed supplementalfeedings, as he was able <strong>to</strong> gain sufficient weight and maintain his needs from oral feeds.At <strong>the</strong> time <strong>of</strong> discharge, he was consistently eating 170 g <strong>of</strong> solid food and drinking177 ml <strong>of</strong> liquid in 30 min or less with his primary caregiver.We evaluated a DRH procedure <strong>to</strong> <strong>increase</strong> <strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding. DRH resultedin an <strong>increase</strong>d <strong>pace</strong> <strong>of</strong> self-feeding and a shorter meal duration. This studydemonst<strong>rate</strong>d that a simple differential <strong>reinforcement</strong> procedure could <strong>increase</strong> selffeedingwith minimal prompting. This, in turn, may have led <strong>to</strong> ease <strong>of</strong>implementation for <strong>the</strong> caregiver, which may ultimately improve treatment integrity.It is interesting <strong>to</strong> note that Jude <strong>to</strong>ok a constant dose <strong>of</strong> MPH throughout this study.Given that one <strong>of</strong> <strong>the</strong> primary adverse side effects <strong>of</strong> MPH is loss <strong>of</strong> appetite, this maypartially account for his slow <strong>pace</strong> <strong>of</strong> self-feeding. Despite this potential side effect,our DRH intervention was successful in increasing Jude’s <strong>pace</strong> <strong>of</strong> self-feeding.In this study, Jude had <strong>to</strong> wait up <strong>to</strong> 30 min <strong>to</strong> receive <strong>reinforcement</strong> during treatment.For children with more severe disabilities and/or more severe feeding problems,30 min may be <strong>to</strong>o long <strong>of</strong> a delay <strong>to</strong> <strong>reinforcement</strong>. Future studies should examinealternative methods <strong>of</strong> providing more immediate <strong>reinforcement</strong> (e.g., <strong>to</strong>kens).Given that initially <strong>the</strong>re was minimal differentiation between <strong>the</strong> two conditions(i.e., baseline and treatment); it may be <strong>the</strong> case that Jude had difficulty discriminatingCopyright # 2008 John Wiley & Sons, Ltd. Behav. Intervent. 24: 17–22 (2009)DOI: 10.1002/bin
Increasing self-feeding 214Baseline(5.1)TreatmentIndependent Bites Per Min3210Increase <strong>to</strong> 177mls liquidJude0 2 4 6 8 10 12 14 16 18MealsBaselineDRA50BaselineTreatment40Increase <strong>to</strong> 177mls liquidMeal Duration (Min)30201000 2 4 6 8 10 12 14 16 18MealsFigure 1. Independent bites per minute (Top Panel) and meal duration (Bot<strong>to</strong>m Panel) during baselineand treatment for Jude.Judebetween <strong>the</strong> two conditions or that <strong>the</strong>re was carryover between <strong>the</strong> conditions. Inorder <strong>to</strong> minimize this problem, we used salient discriminative stimuli (differentcolored tablecloths) <strong>to</strong> enhance discrimination between <strong>the</strong> two conditions.Eventually, <strong>the</strong>re was clear differentiation in responding between <strong>the</strong> two conditions,with bite <strong>rate</strong> <strong>high</strong>er during treatment. Never<strong>the</strong>less, future studies should examineusing alternative single-case experimental designs such as a reversal design <strong>to</strong> avoidthis potential problem. This lack <strong>of</strong> immediate differentiation in responding betweenbaseline and treatment may also bring in<strong>to</strong> question whe<strong>the</strong>r or not experimentalcontrol was demonst<strong>rate</strong>d. However, as <strong>the</strong> treatment evaluation continued, weCopyright # 2008 John Wiley & Sons, Ltd. Behav. Intervent. 24: 17–22 (2009)DOI: 10.1002/bin
22 K. M. Girolami et al.observed a modest level <strong>of</strong> differentiation across <strong>the</strong> two treatment conditions in terms<strong>of</strong> <strong>the</strong> independent bites per min and <strong>the</strong> duration <strong>of</strong> <strong>the</strong> meals.Follow-up data were not available as <strong>the</strong> family was from out <strong>of</strong> state and unable <strong>to</strong>attend follow-up appointments. However, during phone contacts over a 3-monthperiod after discharge, <strong>the</strong> primary caregiver reported that Jude was not receiving tubefeedings and meeting his goals <strong>the</strong> majority <strong>of</strong> time.Finally, <strong>the</strong> generality <strong>of</strong> <strong>the</strong>se findings are limited in <strong>the</strong> sense that this study onlyincluded one participant. Therefore, future studies should continue <strong>to</strong> evaluate <strong>the</strong> use<strong>of</strong> DRH as a means <strong>of</strong> increasing <strong>the</strong> <strong>pace</strong> <strong>of</strong> self-feeding. Despite this limitation, thisstudy provides support for <strong>the</strong> use <strong>of</strong> differential <strong>reinforcement</strong> <strong>to</strong> <strong>increase</strong>appropriate mealtime <strong>behavior</strong>s.ACKNOWLEDGEMENTSThis research is based on a project submitted in partial fulfillment <strong>of</strong> requirementsfor <strong>the</strong> MA degree by <strong>the</strong> first author. We thank David Richman for comments onearlier versions <strong>of</strong> this paper and Annie Stipicevic for her assistance in this project.REFERENCESFisher, W., Piazza, C. C., Bowman, L. G., Hagopian, L. P., Owens, J. C. & Slevin, I., (1992).A comparison <strong>of</strong> two approaches for identifying reinforcers with severe and pr<strong>of</strong>ound disabilities.Journal <strong>of</strong> Applied Behavior Analysis, 25, 491–498.Iwata, B. A., Riordan, M. M., Wohl, M. K., & Finney, J. W. (1982). Pediatric feeding disorders:Behavioral analysis and treatment. In A. J. Accardo (Ed.), Failure <strong>to</strong> thrive in infancy and earlychildhood: A multi-disciplinary team approach (pp. 296–329). Baltimore: University Park Press.Kerwin, M. E. (1999). Empirically supported treatments in pediatric psychology: Severe feedingdisorders. Journal <strong>of</strong> Pediatric Psychology, 24, 193–214.Lennox, D. B., Miltenberger, R. G., & Donnelly, D. R. (1987). Response interruption and DRL for <strong>the</strong>reduction <strong>of</strong> rapid eating. Journal <strong>of</strong> Applied Behavior Analysis, 20, 279–284.Linscheid, T. R. (1992). Eating problems in children In C. E. Walker, & M. C. Roberts (Eds.), Handbook<strong>of</strong> clinical child psychology. (2nd ed., pp. 451–473). New York: Wiley.Linscheid, T. R., Budd, K. S., & Rasnake, L. K. (1995). Pediatric feeding disorders. In C. R. Roberts(Ed.), Handbook <strong>of</strong> pediatric psychology (2nd ed., pp. 501–515). New York: Guilford.Luiselli, J. K. (1988). Improvement <strong>of</strong> feeding skills in multihandicapped students through <strong>pace</strong>dpromptinginterventions. Journal <strong>of</strong> <strong>the</strong> Multihandicapped Person, 1, 17–30.Palmer, S., Thompson, R. J., & Linscheid, T. R. (1975). Applied <strong>behavior</strong> analysis in <strong>the</strong> treatment <strong>of</strong>childhood feeding problems. Developmental, Medical, and Child Neurology, 17, 333–339.Wright, C. S., & Vollmer, T. R. (2002). Evaluation <strong>of</strong> a treatment package <strong>to</strong> reduce rapid eating. Journal<strong>of</strong> Applied Behavior Analysis, 35, 89–93.Copyright # 2008 John Wiley & Sons, Ltd. Behav. Intervent. 24: 17–22 (2009)DOI: 10.1002/bin