Diabetes guidance 1766.pdf - East Cheshire NHS Trust
Diabetes guidance 1766.pdf - East Cheshire NHS Trust
Diabetes guidance 1766.pdf - East Cheshire NHS Trust
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
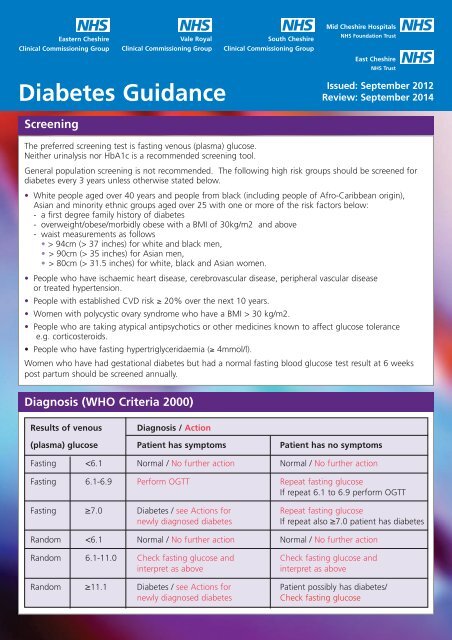
<strong>East</strong>ern <strong>Cheshire</strong>Vale RoyalSouth <strong>Cheshire</strong>Clinical Commissioning Group Clinical Commissioning Group Clinical Commissioning Group<strong>Diabetes</strong> GuidanceMid <strong>Cheshire</strong> Hospitals<strong>NHS</strong> Foundation <strong>Trust</strong><strong>East</strong> <strong>Cheshire</strong><strong>NHS</strong> <strong>Trust</strong>Issued: September 2012Review: September 2014ScreeningThe preferred screening test is fasting venous (plasma) glucose.Neither urinalysis nor HbA1c is a recommended screening tool.General population screening is not recommended. The following high risk groups should be screened fordiabetes every 3 years unless otherwise stated below.• White people aged over 40 years and people from black (including people of Afro-Caribbean origin),Asian and minority ethnic groups aged over 25 with one or more of the risk factors below:- a first degree family history of diabetes- overweight/obese/morbidly obese with a BMI of 30kg/m2 and above- waist measurements as follows• > 94cm (> 37 inches) for white and black men,• > 90cm (> 35 inches) for Asian men,• > 80cm (> 31.5 inches) for white, black and Asian women.• People who have ischaemic heart disease, cerebrovascular disease, peripheral vascular diseaseor treated hypertension.• People with established CVD risk ≥ 20% over the next 10 years.• Women with polycystic ovary syndrome who have a BMI > 30 kg/m2.• People who are taking atypical antipsychotics or other medicines known to affect glucose tolerancee.g. corticosteroids.• People who have fasting hypertriglyceridaemia (≥ 4mmol/l).Women who have had gestational diabetes but had a normal fasting blood glucose test result at 6 weekspost partum should be screened annually.Diagnosis (WHO Criteria 2000)Results of venousDiagnosis / Action(plasma) glucose Patient has symptoms Patient has no symptomsFasting
HbA1c as a Diagnostic Test for <strong>Diabetes</strong>While fasting glucose is still recommended as the initial screening test for suspected diabetes, WHO (2011) hasnow recommended that HbA1c can be used as a diagnostic test for diabetes in most situations, as outlinedin the following paragraph. The main exceptions are rapid onset diabetes (as HbA1c reflects glycaemiaover the preceding 2–3 months) and some genetic, haematological and other disorders; in particularhaemoglobinopathies, anaemia and other diseases associated with changes in red cell turnover (e.g. malaria,drug-induced haemolysis) or glycation rates (e.g. chronic renal disease). In these situations, HbA1c is notrecommended as the sole test to diagnose diabetes.An HbA1c of ≥48 mmol/mol is recommended as the cut point for diagnosing diabetes.An HbA1c level ≥48 mmol/mol can therefore be used to confirm a diagnosis of diabetes in an asymptomaticindividual with a fasting glucose ≥7.0 mmol/L or random glucose ≥11.1 mmol/L, thus precluding the needfor a repeat glucose measurement or oral glucose tolerance test. However, an HbA1c value
The Newly Diagnosed Diabetic PatientDifferentiate between Type 1 and Type 2 diabetes.Features suggesting Type 1 include; Ketonuria (2+ on dipstick), Rapid weight loss, Short history of symptoms(weeks rather than months) and Age < 50 years.If Type 1 suspected consider admission or discuss with the on-call medical team / hospital diabetesteam for investigations to exclude ketoacidosis.All children aged 15mmol/L or- Patient remains symptomatic despite lifestyle changes• Advise patients that diabetes is a condition that they may need to tell theDVLA about depending on their treatment, complications and type ofdriving. Patients should check their particular situation by looking atthe DVLA website www.dvla.gov.ukPatients may need to discuss matters with their car insurer.NB. The aim is to reach targets for BP, lipids and HbA1c within 12 months for all patients.
LifestyleHealthy Lifestyle• Stop smoking• Healthy diet:- Eat regular meals including moderate portions of high fibre complex carbohydrate- Eat a balanced diet following the plate model* Weight loss: Half the plate should be vegetables, a quarter carbohydrates and a quarter protein.* Weight maintenance: Equal servings of carbohydrate, protein and vegetables.• Aim for at least 5 portions of a combination of fruit, vegetables or salad daily.• Oily fish twice per week.• Reduce total and saturated fat intake. Where fat is used, recommend mono-unsaturated fats such as oliveor rapeseed oil. Avoid food containing high levels of total fat (≥ 20g per 100g) or saturated fat (≥ 5g per 100g).• Reduce intake of sugary foods and avoid sweetened drinks.• Reduce salt intake to 28 kg/m 2 .• Only initiate orlistat if patient has made dietary and lifestyle changes showing motivation to lose weightfor 4-6 weeks previously. Consider referral to dietitian.• Patients should be followed up at least monthly for the first 3 months. Set targets for weight loss andconsider cessation of orlistat if these are not met. Note that the NICE advice that the weight loss target of5% of bodyweight in the first 3 months may need to be less stringent for patients with type 2 diabetes.• Patients should be encouraged to use the manufacturer’s website www.mapassist.co.uk• Weight loss and medication should be reviewed regularly and medication stopped if weight loss is notmaintained or weight is regained.• Orlistat should only be continued beyond 12 months if the risks and benefits have been discussed withthe patient. See BNF.
Glycaemic ControlHbA1c MeasurementHbA1c is the primary test for assessing medium-term glycaemic control. It should usually be measured every6 months and more frequently if glycaemic control is poor. However, HbA1c measurements more often thanevery 2 months are not usually appropriate due to its long half-life.Reporting of HbA1c results in the UK changed on 1st June 2011 following preparation of a new standardfor calibrating HbA1c assays by the International Federation of Clinical Chemistry and Laboratory Medicine(IFCC). Results are now reported in new IFCC units (mmol/mol haemoglobin) only; use of DCCT-alignedtraditional units (%) for reporting results has ceased. The equation relating the new and old units is:DCCT-HbA1c (%) = [IFCC-HbA1c (mmol/mol)/10.93] + 2.15Diabetic subjects should be involved in setting targets for glycaemic control, taking into account side effectsof treatment, effect of the management regimen on quality of life, and risk of hypoglycaemia. Those withhigher HbA1c levels should be informed that any reduction in level towards the agreed target is advantageousto future health.Tight glycaemic control reduces the incidence of microvascular complications.Type 1 (DCCT 1993) Reducing HbA1c from 75 to Reduced retinopathy by 63%54 mmol/mol Hb Reduced albuminuria by 54%Type 2 (UKPDS 1998) Reducing HbA1c from 63 to Reduced retinopathy by 21%53 mmol/mol Hb Reduced albuminuria by 34%NICE <strong>guidance</strong> CG87 (2009) recommends a target of 48 mmol/mol Hb for patients with type 2 diabetes andto avoid pursuing highly intensive management to levels below 48 mmol/mol Hb. Other evidence (ACCORD,NEJM 2008) suggests that the most appropriate HbA1c target is ≤53 mmol/mol Hb.Laboratory tests for the annual diabetes reviewThe core annual review laboratory tests for all patients with diabetes are HbA1c, lipids (preferably fasting),renal profile and urine albumin/creatinine ratio.Other annual review tests are only needed in selected patients, as follows:• Thyroid function tests in Type 1 diabetes; they are not indicated in Type 2 diabetes.• Vitamin B12 (without folate) if on metformin, particularly if there is peripheral neuropathy (but not neededif on B12 replacement).• Liver function tests (LFTs) if on pioglitazone. [LFTs should also be done before starting metformin/statin/fibratetherapy, and 3 / 12 months following statin/fibrate initiation or a change in dose, but not subsequently ifLFTs are then normal.]• Glucose (preferably fasting) in the occasional patient with a variant haemoglobin in whom HbA1c cannotbe determined reliably; it is not indicated in other patients.• Full blood count is not required.
Self-Monitoring of Blood GlucoseThe purpose of self-monitoring includes:• Assessing changes in glucose control due to medication and lifestyle changes• Monitoring changes during inter-current illness• Ensuring safety during activities such as driving• Surveillance for hypoglycaemia - risk factors include treatment with insulin/sulphonylurea, older patient,long duration of diabetes, irregular meals, renal impairment, prior hypos, hypo unawareness, alcoholexcess, inter-current illness and fastingSelf Monitoring of Blood Glucose (SMBG) is essential for all type 1 patients and those type 2 patients usinginsulin, to enable insulin dose titration and manage hypoglycaemic events.Self-monitoring should be discussed with newly diagnosed people with type 2 diabetes, including interpretationand actions depending on the results. It may not be appropriate to start home monitoring at the initialappointment for all patients. Factors that would encourage the early initiation of home monitoring would include:• Higher initial fasting plasma glucose (>15 mmol/L)• Higher initial HbA1c values• Patient motivation.• Vocational drivers.It is important to agree a plan with the patient. More intensive monitoring may be required during the initialstages of management when making changes to lifestyle and medication. Once stable, patients may expectto reduce the frequency of monitoring, and for some patients (especially those controlled with diet alone ordiet + metformin), HbA1c monitoring may be sufficient.Patients need to acquire a good monitoring technique and should receive education in the use of a bloodglucose meter (including Quality Control checks). The choice of meter and strips should be based on thepatient’s specific needs. [Note that vocational drivers may need a device that records ≥ 3 months data tosupport DVLA application.]The plan of care will include when to test, interpreting the results and explaining any actions needed. Thepatient should be encouraged to reflect upon blood glucose records to inform their self-management decisions.Blood glucose monitoring can only be truly cost effective if patients have good monitoring skills and theknowledge to act upon reliable results.Ketone monitoringAll patients with Type 1 diabetes should be prescribed Ketostix by Primary Care. Some patients with Type 2may also benefit.It is important that patients are fully informed of the symptoms of ketoacidosis and how to interpret theKetostix result and the appropriate actions to take.Primary and Secondary Care have agreed that should capillary blood ketone testing be required following aSecondary Care assessment of the patient’s individual clinical needs the corresponding ketone testing stripswill be prescribed exclusively by Secondary Care.
Self-Monitoring of Blood Glucose - continuedBlood glucose patterns can be used to guide medication adjustment to improve glycaemic control.1. Patients managed by diet ± oral antihyperglycaemic medicationOnce-daily pre-prandial blood glucose monitoring (staircase method)e.g. Breakfast Lunch Evening Meal SupperDay 1xDay 2xDay 3xDay 4xOnce the medication and the patient’s lifestyle are stable it is sufficient for this to occur once weekly,on varying days, to provide information for both the patient and the Practice Nurse.Ultimately, once stable, HbA1c may be sufficient.2. Biphasic Insulin RegimenTwice daily pre-prandial blood glucose monitoringe.g. Breakfast Lunch Evening Meal SupperDay 1 x xDay 2 x xDay 3 x xDay 4 x xOnce stable, revert to daily pre-prandial blood glucose monitoring (staircase method)3. Basal Bolus Insulin RegimenDuring periods of high activity or unstable control, perform pre-prandial tests before each meal and ifsymptoms of hypoglycaemia occur. Once stable, reduce testing regimen to before breakfast and staggerat least one other time during the day (either pre-prandially or 2-hours post-prandial).4. Metformin + basal insulinTwice daily until stable then once daily while stable.5. Class 2 drivers with insulin, SU or Glinide (repaglinide/netaglinide)At least twice daily [See 2] and then before they drive.Note: 2-hour post-prandial blood glucose testing may be appropriate when HbA1c remains above targetdespite satisfactory pre-prandial readings.
Glycaemic Control in Type 2 <strong>Diabetes</strong>Non-Insulin therapyThe first line drug is metformin.• It should be prescribed in all appropriate patients as the standard release tablet with a usual maximumdaily dose of 2 grams in divided doses.• The modified release formulation should be offered if the patient is intolerant of the standard releaseformulation prior to trialling other classes of medication. See BNF.• Prescribe with caution if eGFR is
Glycaemic Control in Type 2 <strong>Diabetes</strong>Step 1 - diet and lifestyle advice• Provide advice on diet and activity as per previous section. Refer to a dietitian.• Agree target HbA1c – generally ≤ 48mmol/mol Hb, or individually agreed with the patient• Proceed to step 2 after 6-8 weeks if symptoms remain uncontrolled despite lifestyle change.• Otherwise check HbA1c at 3-4 months. If target not achieved move to Step 2.HbA1c Target Achieved• Continue• Review HbA1c 6- to 12-monthlyStep 2 - Monotherapy.Start monotherapy if HbA1c target, generally ≤ 48mmol/mol Hb, is not achieved.This remains the target after monotherapy unless agreed otherwise with thepatient.• Metformin is first-line. Start with low doses and titrate up to maximum 2g/day individed doses. Use modified release form if standard preparation is not tolerated.• Reassess monthly during dosage titration.• Prescribe with caution if eGFR is
Insulin therapyThe range of insulin is as follows (alphabetical); the prescribing choices should be governed by NICE criteriaShort-acting insulinHuman soluble insulin:Rapid acting human insulin analogues:Actrapid ,Humulin S, Insuman RapidApidra, Humalog, NovoRapid,Intermediate-acting insulinHuman NPH insulin:Humulin I Insulatard, or Insuman BasalHuman NPH biphasic insulin: Humulin M3, Insuman Comb 15, Insuman Comb 25,Insuman Comb 50Biphasic human analogue insulins: Humalog Mix25, Humalog Mix50, NovoMix 30Long-acting human insulin analogues:Insulin detemir (Levemir) Insulin glargine (Lantus)Type 1Patients should be offered a Basal Bolus regimen of long acting insulin analogue and short acting prandialinsulin analogue as first line as this regimen offers the best prospect for work/lifestyle and glycaemic control.For some patients a twice daily biphasic insulin analogue regimen (Pre-mix) may be fully appropriate.If glycaemic control is adequate with a non-analogue insulin regimen then there is no need to alter therapy.Type 2In patients with Type 2 diabetes the expectation is that NICE CG87 is followed.• If other measures do not keep HbA1c to < 58 mmol/mol Hb (or other agreed target) discuss benefits andrisks of insulin treatment.• Insulin treatment should be initiated with a Structured Education Plan which should include a specificrange of knowledge/skill criteria.• Although NICE CG 87 suggests that insulin treatment should begin with human NPH insulin taken atbed time or twice daily according to need, locally the preferred option is pre-mixed human biphasicNPH insulin.• Consider pre-mixed preparations of insulin analogues (including short acting insulin analogues) ratherthan pre-mixed human insulin preparations if- immediate injection before a meal is preferred, or- hypoglycaemia is a problem, or- blood glucose levels rise markedly after meals.• Alternatively, consider a once-daily long acting insulin analogue (insulin detemir, insulin glargine) if- the person needs help with injecting insulin and a long acting insulin analogue would reduce injectionsfrom twice to once daily, or- the person’s lifestyle is restricted by recurrent symptomatic hypoglycaemic episodes, or- the person would otherwise need twice daily basal insulin plus oral glucose lowering drugs, or- the person cannot use the device to inject NPH insulin• Consider switching to a long acting insulin analogue (insulin detemir, insulin glargine) from an NPHinsulin if the person- does not reach target HbA1c because of hypoglycaemia, or- has significant hypoglycaemia with NPH insulin irrespective of HbA1c level, or- cannot use the delivery device for NPH insulin but could administer a long acting insulin analogue, or- needs help to inject insulin and could reduce the number of injections with a long acting analogue.• Review use of sulphonylurea if hypoglycaemia occurs with insulin plus sulphonylurea. The continuedco-administration administration of metformin may well be appropriate - review.
Insulin therapy - continuedPatients with type 2 <strong>Diabetes</strong> where either a decision to initiate insulin therapy has been made ora change of treatment is indicated.Scenario 1 such as a working middle aged maleThe patient has a relatively set daily routine including meal and work time. HbA1c is greater than69mmol/mol Hb.• Oral agents, especially Metformin and / or pioglitazone, are to be continued unless there is a significantreason to stop them.• Start a biphasic NPH human insulin, such as Humulin M3 or Insuman 25, in a twice a day regimen andadjust doses according to the need.• If there is failure to achieve the target HbA1c after a period of 6 months and/or frequent hypoglycaemicepisodes (especially pre-prandial) and/or post prandial glycaemic excursions are unacceptably high and/orpatient’s eating and/or work patterns become erratic consider a comprehensive Practice Nurse / DSN anddietitian review of lifestyle, exercise, weight and diet before altering the choice of insulin.• If there is no improvement consider a biphasic analogue insulin like Novomix 30 or Humalog Mix25 in atwice a day regimen. If there is repeated failure to achieve HbA1c target or further problems considerfurther DSN review prior to a further change of therapy.• Finally consider a basal bolus regimen.Scenario 2 such as a sight impaired lady in her 70’sThe Patient is on maximum tolerated oral therapy but the HbA1c is above the one set for the individual soinitiation of insulin is indicated. Patient lives alone and/or requires someone to do his/her insulin injection andthere is risk of overnight hypoglycaemic episodes and/or otherwise patient would need a twice a day insulinregimen with either an isophane / NPH insulin or biphasic insulin.• Start once daily analogue basal insulin and adjust dose as needed.• Continue all oral agents unless there is a reason to alter them.• Review the situation with other insulin therapy options if there is failure to achieve the targets or anychange in the individual’s circumstances.Scenario 3 such as a shift worker in their 40’sThe patient has ‘poor’ glycaemic control with HbA1c greater than 69mmol/mol Hb and has erratic meals,meal times and work pattern that is difficult to change or the patient has to inject just before a meal andthe patient’s glycaemic control is ‘very poor’ (HbA1c greater than 86mmol/mol Hb).• Start with a comprehensive review of diet, lifestyle and weight by a Practice Nurse/Dietitian/DSN.• Start a basal bolus regimen with analogue mealtime insulin (like Novorapid or Humalog or Apidra) at eachmeal and a basal insulin (like detemir or glargine) once a day.• A basal bolus regimen with human mealtime short acting insulin (like Humulin S) with each meal and abasal human insulin ( Humulin I, Insulatard or Insuman ) may be considered in exceptional situationswhere there is a strong reason to do so. Usually this group of patients need a basal bolus regimen withanalogue insulin.• Adjust doses as needed.• Oral agents especially Metformin and / or pioglitazones are to be continued unless there is a significantreason to stop them. Ideally, all insulin secretogogues should be stopped with any basal bolus regimenunless there is a compelling reason to leave them on.
Insulin therapy - continuedScenario 4 such as an office worker in their 60’sHbA1c is less than 69mmol/mol Hb and has a set meal and work pattern. The patient’s preference is for nomore than one or two insulin injections a day.• Continue with all oral agents unless there is a significant reason to reduce the dose or stop one ormore agents.• Start human NPH insulin (Humulin I, Insulatard or Insuman) at bed time or in the morning at breakfasttime. Adjust doses as needed.• If there is a failure to achieve the HbA1c targets consider making the regimen twice a day i.e., twice a dayof NPH isophane insulin along with oral agents.• Consider human biphasic insulin (like Humulin M3 or Insuman 25) in twice a day regimen, especially ifthere are high excursions of glucose postprandially.• The next step is to consider biphasic analogue insulin (like Novomix 30 or Humalog Mix 25) in a twice aday regimen.• Finally consider a basal bolus regimen with human or analogue insulin.• Oral agents especially metformin and / or pioglitazone should be continued with twice a day biphasichuman or analogue insulin regimens unless there is a reason.Insulin PumpsThe use of insulin pumps for patients who fulfil the criteria stated in NICE TA 151 (July 2008) is supportedlocally. Referrals for assessment of the patient’s current management should be made initially to the DSNteam and then if appropriate, onward referral will be made for local consultant review or directly to theinsulin pump service in Liverpool or Manchester.
HypertensionBP targets are the same for Type 1 and Type 2 diabetes. Always treat to the following targets:Uncomplicated hypertension ≤ 140/80(i.e. no end-organ damage)Hypertension with end-organ damage ≤ 130/80Note: Lower targets may be appropriate for people with more advanced renal disease, as advised byrenal physicians.Monitor the BP of people who have attained the recommended BP targets every 4-6 months, and check forpossible adverse effects of antihypertensive therapy, including the risks from unnecessarily low blood pressure.Tight BP control can significantly reduce the incidence of microvascular and macrovascular complications ofdiabetes (UKPDS)Outcome Relative risk reduction (tight Number Needed to Treat (NNT)vs conventional control) for tight BP control to prevent1 event over 10 yearsAny diabetes-related end-point 24% 6<strong>Diabetes</strong>-related deaths 32% 15Myocardial infarction 21% 20Stroke 44% 20Microvascular disease 37% 14Interventions to control BP• Lifestyle measures- Smoking cessation- Salt reduction to
Lipid TherapyLipidsAll patients with Type 1 and Type 2 diabetes aged >40 years should be viewed as at high risk ofcardiovascular disease (CVD) and should be offered a statin. The Heart Protection Study (HPS) showedthat these patients benefited from simvastatin 40 mg at night for primary prevention if they had a totalcholesterol level >3.5 mmol/L.Total and LDL CholesterolIdeally, lipids should be measured on a 12-hour fasting sample, but this can be impractical in diabetes.Total and HDL cholesterol can be measured with reasonable accuracy on a random sample, providingtriglycerides do not exceed 2.2 mmol/L.Secondary causes of lipid abnormalities such as excess alcohol, hypothyroidism and liver disease shouldbe investigated and managed in those with significant hypercholesterolaemia (>7.5 mmol/L) and/orhypertriglyceridaemia (>4.0 mmol/L).NICE (2009 CG87) recommends to treat to achieve total cholesterol of
Lipids - continuedHDL Cholesterol and TriglyceridesLow HDL cholesterol (2.2 mmol/L) are both independent riskfactors for CVD.The first priority in patients with raised triglycerides is to improve diet and glycaemic control, as insulinresistance often increases levels.Statins remain the cornerstone of lipid-lowering therapy, but consider adding a fibrate if fasting triglyceridesexceed 2.2 mmol/L despite optimal statin therapy and adequate glycaemic control.Earlier addition of a fibrate may be appropriate if triglycerides are high (>4.0 mmol/L) despite goodglycaemic control. It may be appropriate to discuss these patients with a diabetologist or lipidologist.Fenofibrate as Supralip 160 mg daily is the preferred fibrate choice.In mild/moderate renal impairment (CKD stages 3 or 4), exercise caution in using fibrates because of anincreased risk of rhabdomyolysis. In these cases a lower dose of fenofibrate as Lipantil Micro may be used.Fibrates are contra-indicated in severe renal disease (CKD stage 5).Specialist ReferralConsider discussion with or referral to a lipidologist or diabetologist if:• Familial hypercholesterolaemia is a possibility;• Satisfactory targets are not reached, despite intervention as outlined above;• HDL cholesterol is significantly decreased (10 mmol/L) due to the risk of pancreatitis.
RetinopathyScreening will be provided via the Retinopathy Screening Service. Patients with no retinopathy /background retinopathy will be screened annually and the service will advise of the need for morefrequent screening or referral to ophthalmology.Antithrombotic Treatment• Aspirin is not recommended for the primary prevention of cardiovascular events in patients withdiabetes.• Aspirin 75mg dispersible should be considered as secondary prevention in establishedcardiovascular disease.• Clopidogrel 75mg daily is an alternative when aspirin cannot be tolerated.• Clopidogrel 75mg daily should be used in combination with aspirin 75mg daily for a limitedtime period following acute MI (1 month for STEMI and 1 year for NSTEMI) and some coronaryprocedures including stents.• Following thrombotic stroke aspirin 300mg daily is given for 2 weeks followed by clopidogrel75mg daily long term.• Following TIA aspirin 300mg daily is given for 2 weeks, then reducing to 75mg daily in combinationwith dipyridamole MR 200mg twice daily.Neuropathic Pain• Assess for symptoms of neuropathic pain annually and if present assess severity.• Where local measures and simple analgesics do not provide sufficient relief considerpharmacological management and if necessary referral to a specialist pain clinic.• NICE <strong>guidance</strong> (CG96) recommends duloxetine (Cymbalta 60mg daily) first-line and amitriptyline(10-75mg daily) as an alternative if duloxetine is contra-indicated or ineffective. Nortriptyline(starting dose 10mg) can be considered if amitriptyline is not tolerated.• NICE <strong>guidance</strong> recommends pregabalin if duloxetine / amitriptyline are not sufficiently effective orwell tolerated, but local <strong>guidance</strong> continues to recommend gabapentin as a lower cost alternativeto pregabalin with a similar NNT.
Screening for Diabetic NephropathySend first void early morning urinesample annually for urine albumincreatinine ratio (UACR) in a 10 mLplain Sarstedt Monovette tube (or aplain white top Universal container)ANDMeasure serum creatinine andeGFR annuallyUACR > 2.5 mg/mmol (men)UACR > 3.5 mg/mmol (women)YESRepeat twice within 3-6 monthsRemember false positives from UTI,menstruation or intercurrent illness.Check MSSUNO CKD 3 (i.e. eGFR≥ 30 and 1.0 g / 24hours)NOYESRefer toRenal Team
Foot assessmentAll patients require an annual assessment including:• Symptoms – claudication, pain, history of ulcer• Inspection – callus, deformity, presence of ulcer• Examination – skin condition, pulses present, sensitivity to 10g pressure, vibration perception.Note the use of heel balm (e.g. Dermatonics, Flexitrol) may be appropriate for those with very dry skin.Categorise into risk groups for follow up as per table.Risk Category Indicators of Risk Category ManagementLow current risk Normal sensation and Annual review by primaryPalpable pulses andcare teamNo current or previous ulcers and No podiatry input requiredNo deformity andNo skin changes andNormal visionIncreased Risk Neuropathy or Annual review by primaryAbsent pulses orcare team andPrevious vascular surgery orRefer patient for regularSignificant visual loss orpodiatry input (3 to 6 monthlyCannot reach own feetreview)High risk Neuropathy or Absent pulses AND Annual review by primarySkin changes or Deformity orcare team andPrevious ulcerRefer patient for regular podiatrycare (1 to 3 monthly review)
Active Foot DiseaseUlcerRefer to Specialist Podiatry Team: 01270 273 033Low grade ulcers / systemically well:Initial Actions:• Swab wound• Provide empirical antibiotic treatment for 7 days.- Co-amoxiclav 500/125mg tdsOr for penicillin-allergic patients- Doxycycline 100mg bd + metronidazole 400mg tds.• Dress with an antimicrobial dressing- Low exudate wounds – Inadine or Urgotul SSD or Atrauman silver- High exudate wounds – Aquacel Ag- Silver dressings should be stopped once the course of antibiotics is complete- For further advice contact Tissue Viability Nurse (contact 01270 275315).• Ensure foot is elevated and rested.• Consider Admission if systemically unwell.Diabetic foot infections range from simple acute cellulitis to chronic osteomyelitis and always requireaggressive management. In more complex patients (e.g. those over 75 years and / or history of C. difficilediarrhoea) discussion with microbiologist is recommended.If first line treatment has not worked then consider swab result or discuss with microbiologist.Systemically unwell / limb threatening infection:This is a Medical Emergency. Admit for assessment and treatment according to hospital antibiotic guidelines.Critical IschaemiaIndicated by pain at rest, pale/mottled feet, gangrene or claudication.Refer to Vascular Consultant or admit to hospital as an emergency.
Contact Details<strong>Diabetes</strong> UKWeb: www.diabetes.org.ukAddress: Central Office, Macleod House, 10 Parkway, London NW1 7AATelephone: 020 7424 1000Careline: 0845 120 2960DVLAWeb:www.dvla.gov.ukCommunity ServicesECT <strong>Diabetes</strong> Specialist Nursing TeamTelephone: 01270 415414/01625 663375ECT Specialist <strong>Diabetes</strong> Dietetic ServiceTelephone: 01270 612428 / 01625 661126ECT Podiatry Central OfficeTelephone: 01270 275349ECT Specialist Podiatry TeamTelephone: 01270 273 033ECT Tissue Viability NurseTelephone: 01270 275315Diabetic Retinopathy Screening ServiceDiabetic Retinopathy Screening Service Co-ordinatorDiabetic Retinopathy Screening Service DepartmentEagle Bridge Health & Wellbeing CentreDunwoody WayCrewe<strong>Cheshire</strong>CW1 3AWTelephone: 01270 275523 / 275524Fax: 01270 509632The service can also be contacted on Diabetic.Retinopathy@nhs.net only if sendingfrom an <strong>NHS</strong> mail account.