Guidelines for INFECTION CONTROL POLICY - Safdarjung Hospital
Guidelines for INFECTION CONTROL POLICY - Safdarjung Hospital
Guidelines for INFECTION CONTROL POLICY - Safdarjung Hospital
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
CONTRIBUTORSCreated by : Dr. Rajni Gaind, Dr. Monorama DebApproved by : Medical Superintendent, SJHDate of Creation : September, 2008Modified on : August 18, 20102
CONTENTSIntroduction 4Hosptial Infection Control Team (HICT) Members 5<strong>Hospital</strong> <strong>Guidelines</strong> <strong>for</strong> Prevention And Control of Infections 6Surveilance and Reporting of Infection 8Disinfection Policy 10Isolation Policy 12Investigation of an Outbreak 13Antimicrobial Policy 15Annexure 1 Policy on <strong>Hospital</strong> Waste ManagementAnnexure 2 Policy on Management of Sharps, Needle Stick Injury & Body Fluids Exposure3
HOSPITAL <strong>INFECTION</strong> <strong>CONTROL</strong> TEAM (HICT) MEMBERSThe role of the HICT is to implement the annual programme and policies, and provide infectioncontrol advice on a 24-hour basis. The team is responsible <strong>for</strong> the following:• Surveillance of infections and monitoring methods of control• Rapid identification and investigation of outbreaks or potentially hazardous procedures• Giving advice on the management of patients with infection, particularly those in isolation• Providing a staff training programme in infection control and auditing compliance• Preparing the annual infection control programme• Preparing monthly infection control reports• Producing and maintaining up-to-date hospital infection control policies• Assisting different departments across the hospital in their ef<strong>for</strong>ts to reduce healthcareassociatedinfectionsThe ICT consists of the following members:• Head of the institute Chairperson• Addl. Medical Superintendent Member• All heads of Department Members• Nodal officer HMW Members• Nursing in charges all patient care units Members• CPWD Incharge Members• Infection Control Nurses Members• HOD Microbiology Member Secretary• Infection control officer (Senior Microbiologist) MemberAll staff plays an important part in the control of healthcare-associated infections. Staff shouldapply the procedures and precautions in all of the HIC policies at all times to ensure safepractice <strong>for</strong> themselves and the patient. Good clinical practice can substantially reducehealthcare acquired infections. Senior staff has managerial responsibility to ensure that all oftheir staff follow good infection control practice and comply fully with HIC policies.Terms and Conditions• Commitment towards Maintenance of Surveillance over hospital acquired infections.• Develop a system <strong>for</strong> identifying, reporting, analyzing, investigating and controlling hospitalacquired infections.• Develop and implement preventive and corrective programmes in specific situations whereinfection hazards exist.• Advice the Medical Superintendent on matters related to the proper use of antibiotics,develop antibiotic policies and recommend remedial measures when antibiotic resistantstrains are detected.• Review and update hospital infection control policies and procedures from time to time.• Help to provide employee health education regarding matters related to hospital acquiredinfections.• Shall meet regularly - once a month and as often as required.5
HOSPITAL GUIDELINES FOR PREVENTION AND <strong>CONTROL</strong> OF <strong>INFECTION</strong>SNo. Topic Details1. Infection control policy Started in 1998; revised in 2001,(Ensuring adequate and trained human March and August 2010.resources <strong>for</strong> infection control e.g. aminimum of one infection control nurseper 250 beds)Infection Control committeeChairperson: Medical superintendent(The details of the responsibilities are Secretary: HOD Microbiologyenclosed in Annexure -1)Members:Addl. MS, SJHHeads of all clinical departmentsNursing Superintendent(NS), SJHExecutive Engineer, Civil, CPWDExecutive Engineer, Electrical, CPWDStore OfficerInfection Control Nurses(ICN) -2ICO: MicrobiologistICN: 2 Staff NursesBiomedical Waste Management Addl. MS, SJH(BMW) TeamMS, SJHExecutive engineer, Civil, CPWDExecutive engineer, Electrical, CPWDStore OfficerDDAICN2. Standard precautions Followed in all health care areas3. Hand hygiene guidelines Strictly observed to be and monitored4. Safe injection practices There is a model Injection Centre inSJH as a patient safety initiative.5. Minimize invasive procedures Invasive procedures are done when essential.6. Patient isolation policy Isolation policy in place at SJH7. Disinfection and sterilization policy Practiced and monitored regularly.8. Antimicrobial policy Attached as Annexure 19. Safe environment (including Ensured to the best possible extentwater, air, temperature &under the limited resources.housekeeping) monitoring10. Maintenance & Cleanliness / Housekeeping guidelines followed byInfrastructurethe designated staff11. Biomedical Waste Management Practiced as per government regulations,(BMWM) guidelinesand waste audit done at monthly intervals.(Annexure 2)6
12. Training and education of HCW Conducted by the department of BMWMon HIC Practices, including BMWM on monthly basis, every Pre and post& PEP <strong>for</strong> HIV &HBVevaluation tests conducted in the trainingprogram. Certificates issued only if theyachieve 60% marks in the post evaluationtest. (Annexure 3)13. Occupational safety guidelines Additional MS is the designated safetyofficer. Hepatitis B and H1N1 immunizationis being done <strong>for</strong> all at risk, as andwhen required.Post exposure prophylaxis(PEP) <strong>for</strong> HIV/HBV in place at SSKH &KSCH. (Annexure 3)14. Outbreak investigation policy All outbreaks are investigated, analyzedand reported to the Chairperson, andappropriate measures are taken to controlthe outbreaks.15. Audits of infection control Done regularly by the HIC team7
SURVEILLANCE AND REPORTING OF <strong>INFECTION</strong>Statutory NotificationsAll notified by Secretary, <strong>Hospital</strong> Infection Control Team to the MS of SJH.Prompt notification and reporting of disease is essential.The objectives of notification are:1. Regulatory obligation by Govt. of India. All notifiable and reportable diseases must bereported to concern authorities.2. To collect accurate and complete epidemiological in<strong>for</strong>mation on the disease.3. To ensure prompt and appropriate control measures to prevent the spread of infection.Any patient suffering from a notifiable/reportable disease when detected shall becommunicated to the designated authority immediately.ACTIVE SURVEILLANCEActive surveillance of Healthcare associated Infections (HCAI)The microbiology department shall be responsible <strong>for</strong> reporting any in<strong>for</strong>mation about infectionssuspected to be hospital acquired on prescribed <strong>for</strong>mat to Infection Control Nurse (ICN). TheICN in consultation with ICO may proceed <strong>for</strong> investigation of HCAI.Active surveillance of High Risk AreasActive surveillance shall be done at least <strong>for</strong> high risk areas.High risk areas under various setting include:• Intensive care units (NICU, PICU, ICUs – CTVS, CCU, Burns, Trauma, Respiratory,H1N1)• Operation Theatres• Dialysis Unit• Burns Unit• Transfusion services unit• Food handlers• Drinking water• CSSDOperation TheatresBoth surface contamination and air quality will be investigated periodically. Culture swabs andair sampling plates will be sent from Operation Theatres periodically atleast once in a month.Fogging of OTs will be done on the basis of these reports and/or clinical procedures carriedout in the operating areas. No routine fogging is recommended. Any civil or engineering worksshould invite fogging of OTs.ParameterComplianceSurface swabsOnce in MonthAir SamplingOnce in MonthDisinfectant MonitoringOnce in Month, (In- Use disinfectant method,Glutaraldehyde monitoring strip)8
Schedule may be changed to increased frequency in case of suspected increase in infectionrate from OTs.Sampling of in-use disinfectants: 1ml of sample of in-use disinfectants, hand wash agents aresent to microbiology laboratory in a sterile container once a month preferably when othersampling (Air and surface) is being carried out.Records are kept with nursing incharge OT and the results produced in HICC meetings. In caseof unacceptable results, decisions on corrective measures are taken by HICC.Intensive care unitsMonitoring of device associated infections needs to be done on regular basis. The basicindicators required ventilator associated pneumonia (VAP), catheter linked blood stream infections(CLBSI) and catheter associated urinary tract infections (CAUTI). VAP, CLBSI and CAUTIepisodes are monitoredRegular active surveillance is recommended through the emergence /clustering of positivecultures cases or similar clinical case clustering.In case of surveillance following surveillance specimens must be collected:Surveillance samples:• Clinical Materialo Central line tips with blood cultureo ET tube secretions <strong>for</strong> microscopy and cultureo Urine samples from catheterized patientso Others• Environmental Samplingo Water samples from humidifierso Sampling of drugs prepared <strong>for</strong> patientso Ventilatorso Wallso Floorso Suction tubingo Disinfectants on dressing trolleyso OthersSurveillance clinical samples are sent to microbiology lab on basis of clinical data or microbiologicalreports. Analyses of data are presented at the subsequent HICC meeting. Records aremaintained by ICO. At our hospital the surveillance is carried out once in every two weeks <strong>for</strong>each area mentioned above (clinical and environmental sampling). The data will be presentedin HICC meetings.Transfusion services unitEnvironmental sampling shall be done once in a week. Blood component bags – FFP andplatelets shall be screened <strong>for</strong> contamination, as and when required. The record will be maintainedby blood bank officer and chairman/Secretary HICC and presented in HICC meetings.WardsNo active surveillance is required <strong>for</strong> routine non-ICU patient care units. Active surveillanceis recommended whenever clustering of positive cultures from cases are seen in the laboratory.Sampling should be done in consultation with ICN under guidance of microbiologist.Food handlersScreening of food handlers is recommended every four month. Samples include stool samples<strong>for</strong> ova, cyst and cultures <strong>for</strong> typhoid carriers. Records to be maintained by the dietician andICN.9
Drinking WaterBacteriological surveillance is to be done monthly. Potable water testing is routinely carried out<strong>for</strong> bacterial cultures in laboratory from all patient care units, hospital kitchen, canteens andhostels – once in a month.Centralised Sterilised Supplies DepartmentAir and surface sterility is monitored from sterile zone. Bowie Dick test and use of biologicalindicators <strong>for</strong> steam sterilisation is carried out. Disinfectant screening is also done. Recordsto be kept by CSSD.PASSIVE SURVEILLANCEReporting of hospital acquired infectionsPassive Clinical ReportingIt will be mandatory <strong>for</strong> clinicians to fill the prescribed <strong>for</strong>m <strong>for</strong> every admitted patient and the<strong>for</strong>m may be sent to Infection Control Nurse (ICN).Passive Microbiological ReportingIn an event of clustering of cases passive surveillance is initiated. Respective clinicians arein<strong>for</strong>med about the suspected clustering and surveillance specimens are collected. The reportthus generated from the study is sent to the concerned physicians and surgeons. This is beingdone regularly.HAND HYGIENE• Training and compliance needs to be monitored. Availability of hand rubs, Soaps handtowels and water should be ensured. Foot operated and wall mounted dispensing stationsare required. Hand hygiene training programme <strong>for</strong> doctors, nursing staff, students andhousekeeping staff is done regularly once a month <strong>for</strong> each category of staff. Handhygiene compliance is not yet initiated.MULTIDISCIPLINARY CONTINUING EDUCATION PROGRAMMEContinuous education programme is conducted on regular basis <strong>for</strong> all categories of staffensuring each staff attends the programme at least once in three months.DIS<strong>INFECTION</strong> <strong>POLICY</strong>DIS<strong>INFECTION</strong>Disinfection is a process where most microbes are removed from defined object or surface,except spores.Disinfectants can be classified according to their ability to destroy different categoriesof micro-organisms:• High Level disinfectants : glutaraldehyde 2%, ethylene oxide• Intermediate Level disinfectant : alcohols, chlorine compounds, hydrogen peroxide,chlorhexidene, glutaraldehyde(short term exposure)• Low level disinfectants : benzalkonium chloride, some soapsGENERAL GUIDELINES FOR DIS<strong>INFECTION</strong>:Critical instruments/equipments (that are those penetrating skin or mucous membrane) shouldundergo sterilisation be<strong>for</strong>e and after use. e.g. surgical instruments.10
Semi-critical instruments /equipments (that are those in contact with intact mucous membranewithout penetration) should undergo high level disinfection be<strong>for</strong>e use and intermediate leveldisinfection after use. e.g. endotracheal tubesNon-critical instruments /equipments (that are those in contact with intact skin and no contactwith mucous membrane) require only intermediate or low level disinfection be<strong>for</strong>e and after use.e.g. ECG electrodesDisinfectants that are in useGlutaraldehyde:Can be used up to 14 days after activation,Contact time - For disinfection 15-30 minutes- For sterilization 8-10 hoursSterilium :Contains 2-propanol, 1-propanol, macetronium ethyl sulphateContact time <strong>for</strong> patient care hand wash : 1.5 ml <strong>for</strong> 30 secondsContact time <strong>for</strong> surgical hand wash : 9 ml <strong>for</strong> 3 minutesEcoshield :Contains stabilized hydrogen peroxide 11% w/v with 0.01% w/v, diluted silver nitratesolution.For surface disinfection: 10% v/v solution in de-ionized water with contact time of 60minutes.For fumigation: 1 litre of 20% v/v solution /1000 cu ft of space in 60 minutes.Bacillocid :Contains chemically bound <strong>for</strong>maldehyde, glutaraldehyde and benzalkonium chloride.Used as surface disinfectant at 2% solution in operation theatres and at 0.5% in wards anddressing rooms.Sprayed onto wet surfaces with a low pressure sprayer and allowed to dry slowly.Betadine:Iodophor .This is a high level disinfectant. Used <strong>for</strong> surgical hand scrub, skin disinfection.Tincture Iodine:For part preparation in operation theatres and blood specimen collection.Sodium Hypochlorite:Used <strong>for</strong> containing blood spills at 10%, disinfecting counter tops and other hard surfaces at1 %.Used in laboratory <strong>for</strong> decontamination of waste from equipment and glassware at 5%.Alcohol (70%) :Used <strong>for</strong> disinfection of non-disposable patient care items in/out- patient departments and alsoin laboratory <strong>for</strong> cleaning of microscope lenses and surfaces of critical work surfaces.ALDEHYDEGlutaraldehyde may be used in places like the endoscopy unit, cardiac catheterization labs.Formaldehyde is used <strong>for</strong> fumigation.11
Endoscopes - cleaning and disinfection1. Mechanical cleaning : This is the most important step. Flush the air/water channel <strong>for</strong> 10-15 seconds to eject any blood or mucus. Aspirate detergent through the biopsy/suctionchannel to remove gross debris. Use a cleaning brush suitable <strong>for</strong> the instrument andchannel size to brush through the suction channel.2. Disinfection : The endoscope and all internal channels should be soaked in 2% glutaraldehyde<strong>for</strong> 20 minutes.3. Rinsing : Following disinfection, rinse the instrument internally and externally to removeall traces of disinfectant.4. Drying : Dry the endoscope externally. Flush air through each channel.STEAM STERILIZATIONMicrobiological indicators are used once a week: namely spores of Bacillus stearothermophilus<strong>for</strong> steam sterilizers and Bacillus subtilis <strong>for</strong> ethylene oxide. Vials are removed from sterilizersand sent to microbiology laboratory where they are incubated at relevant temperatures <strong>for</strong> 48hours. Report is sent to ICN.An expiry date is given <strong>for</strong> sterile articles based on the packing material used.FOGGING :Eco-shield is used <strong>for</strong> fogging using Fog spraying machine.Operation theatres are fogged once a week and if necessary such as in case of a septic woundbeing drained.Other patient care areas regular fogging not recommended.Necessary decision is taken by in charge of concerned patient care area.FLOOR MOPPINGGeneral cleaning by plain soap and water in non-critical care areas.In critical care areas generous mopping using wet cloth by 0.5% Sodium Hypochlorite solution.BEDDING AND BLANKETImpermeable covers, mattresses should be mopped with 0.1% Sodium hypochlorite solution orspirit.Blanket may be sent <strong>for</strong> laundry or dry cleaning.Monitoring of biomedical waste management practicesICN shall take daily rounds in pre-<strong>for</strong>matted round sheet and will look into the biomedical wastemanagement of various hospital areas.Bedside teaching by ICNs will be undertaken.ISOLATION <strong>POLICY</strong>Aim :• To prevent the transmission of pathogenic microorganisms within the healthcaresettingThe patients of following disease categories should be treated under isolation.• Severe influenza cases, SARS, Open case of tuberculosis, Anthrax, C. diphtheriae,Pertussis, Pneumonic plague, Chicken pox, and patients suffering from multidrug resistantpathogens/MRSA.12
• The isolation of the patient would be done taking following into consideration:(1) Separate ward/room/area is designated <strong>for</strong> keeping the patient.(2) Isolation wards/area has double door entry with a separate changing room withavailability of Personal Protective Equipment (PPE) and disinfectants and a handwashing area providing negative pressure with adequate air changes (6-12/hour) andHEPA filtered air in case of patients suffering from respiratory pathogens.(3) Central air conditioning and use of desert air coolers is not permitted.(4) Adequate distancing between patient beds (3-6 feet) to be ensured.(5) Overcrowding to be avoided in isolation ward/area.(6) Unauthorised Visitor’s entry is to be prohibited.(7) Nobody is allowed to enter the ward without donning adequate PPE.(8) As far as possible dedicated health care staff to be posted <strong>for</strong> isolation ward.(9) Regular daily cleaning and proper disinfection of isolation wards to be done at leasttwice a day. in addition, special attention should be given to cleaning and disinfectingfrequently touched surfaces to prevent aerosolisation. Damp sweeping/wet moppingto be per<strong>for</strong>med.(10) Standard precautions which include barrier nursing to be followed with special stresson hand hygiene using soap water and alcoholic hand rubs (Preferably foot operated)and the procedures should be adequately displayed <strong>for</strong> the same.(11) Appropriate use of PPE should be strictly adhered to e.g. use of face masks,N95 masks, gloves, gowns, aprons , shoe covers, head covers etc as per therequirement (The procedures of donning/undonning of PPE will be displayed).(12) Sharing of equipments among the patients to be avoided, if unavoidable, ensure thatreusable equipments are disinfected be<strong>for</strong>e use on other subjects(Equipments likeThermometer, Nebulisers ,Stethoscopes, BP apparatus cuff to be dedicated <strong>for</strong> eachpatient).(13) All the equipments coming in contact with the patient should be disinfected.(14) Use of mobile phones by healthcare staff to be avoided inside the isolation area.(15) Appropriate waste disposal facilities to be available in the isolation area, All wasteto be treated as infectious and should be segregated and disinfected be<strong>for</strong>e removalfrom the isolation area.(16) All paper work/record keeping should be done outside the isolation area.(17) Sample collection to be done using appropriate PPE, following standard work precautions.Sample to be packaged/transported in triple packaging.(18) Used linen to be handled as little as possible with minimum agitation and should betransported in closed containers and should be labelled as infectious be<strong>for</strong>e sendingto laundry <strong>for</strong> washing.(19) Regular training on PPE, standard precautions and other infection control <strong>for</strong> thehealthcare workers and providers shall be under taken.INVESTIGATION OF AN OUTBREAKThe occurrence of two or more similar cases relating to place and time is identified as a clusteror an outbreak and needs investigation to discover the route of transmission of infection, andpossible sources of infection in order to apply measures to prevent further spread. If the casesoccur in steadily increasing numbers and are separated by an interval approximating theincubation period, the spread of the disease is probably due to person to person spread. Onthe other hand if a large number of cases occur following a shared exposure e.g. an operation,it is termed a common source outbreak, implying a common source <strong>for</strong> the occurrence of thedisease.13
Epidemiological methodsThe investigation of an outbreak may require expert epidemiological advice on procedures.Formulation of a hypothesis regarding source and spread is made be<strong>for</strong>e undertaking microbiologicalinvestigations in order that the most appropriate specimens are collected.Steps to be taken to investigate an outbreakStep 1• Recognition of the outbreak. Is there an increase in the number of cases of a particularinfection or a rise in prevalence of an organism? Such findings indicate a possible outbreak.• Preliminary investigation must begin by developing a case definition, identifying the site,pathogen and affected population. Define the outbreak in time, person and place.• Determination of the magnitude of the problem and if immediate control measures arerequired. If so general control measures such as isolation or cohorting of infected cases;strict hand washing and asepsis should be immediately applied.• Verification of the diagnosis. Each case should be reviewed to meet the definition.• Confirmation that an outbreak exists by comparing the present rate of occurrence withthe endemic rate should be made.Step 2• The appropriate departments, personnel and the hospital administration should be notifiedand involved.Step 3• Additional cases must be searched <strong>for</strong> by examining the clinical and microbiological ecords.• Line listing <strong>for</strong> every case, patient details, place and time of occurrence and infectiondetails should be developed.• An epidemic curve based on place and time of occurrence should be developed, the dateanalyzed, the common features of the cases e.g. age, sex, exposure to various riskfactors, underlying diseases etc. should be identified.• A hypothesis based on literature search and the features common to the cases; shouldbe <strong>for</strong>mulated about suspected causes of the outbreak.• Microbiological investigations depending upon the suspected epidemiology of the causativeorganism should be carried out. This will include (a) microbial culture of cases, carriersand environments (b) epidemiological typing of the isolates to identify clonal relatedness.• The hypothesis should be tested by reviewing additional cases in a case control study,cohort study, and microbiological study.Step 4• Specific control measures should be implemented as soon as the cause of outbreak isidentified.• Monitoring <strong>for</strong> further cases and effectiveness of control measures should be done.• A report should be prepared <strong>for</strong> presentation to the HICC, departments involved in theoutbreak and administration.Immediate control measuresControl measures should be initiated during the process of investigation. An intensive reviewof infection control measures should be made and general control measures initiated at once.General measures include:• Strict hand washing• Intensification of environmental cleaning and hygiene• Adherence to aseptic protocols• Strengthening of disinfection and sterilization14
Microbiological StudyMicrobiological study is planned depending upon the known epidemiology of the infectionproblem. The study is carried out to identify possible sources and routes of transmission.The investigation may include cultures from other body sites of the patient, other patients, staffand environment. Careful selection of specimens to be cultured is essential to obtain meaningfuldata.Specific control measuresSpecific control measures are instituted on the basis of nature of agent and characteristics ofthe high-risk group and the possible sources. These measures may include :• Identification and elimination of the contaminated product• Modification of nursing procedures• Identification and treatment of carriers• Rectification of lapse in clinical technique or procedureEvaluation of efficacy of control measures• The efficacy of control measures should be evaluated by a continued follow-up of casesafter the outbreak, clinically as well as microbiologically. Control measures are effectiveif cases cease to occur or return to the endemic level.The outbreak will be documented and the records should be kept with HICC and should bepresented in HICC meeting.ANTIMICROBIAL <strong>POLICY</strong>The annual antibiogram is released from the microbiology department. Antibiotic susceptibilitytests is analyzed regularly on a quarterly basis and the common resistance patterns of thebacterial isolates are reported and discussed in the HICC meetings and the antibiotic policy isreviewed accordingly. Present Antibiotic policy is published as separate documentAntibiotic policy is prepared in consultation with respective clinical departmentsAntibiotic policy shall be prepared using following general principles:1. Data is analyzed on a quarterly basis as per hospital records)(a) Common etiological agents as per(i) site of infection(ii) age groups(iii) patient location – outdoor (OPD), indoor (wards & critical care areas)(b) Antibiogram data as per(i) site of infection(ii) age groups(iii) patient location – outdoor (OPD), indoor (wards & critical care areas)(c) Unusually resistant organisms to be confirmed and submitted <strong>for</strong> further characterizationto National Centre <strong>for</strong> Disease Control (NCDC) <strong>for</strong>2. Standard treatment guidelines [categorization of patients as per age and Communityacquired infections (CAI) / Health care associated infections (HCAI)](a) <strong>Guidelines</strong> <strong>for</strong> empirical antimicrobial therapy as per common clinical syndrome(i) Adults & older children1. Blood Stream Infections (BSI)2. Meningitis3. UTI15
(ii)4. Pneumonia(a) Community Acquired Pneumonia (CAP)(b) Ventilator Associated Pneumonia (VAP)5. GIT Infections6. Conjunctivitis7. Otitis Media8. Tonsilltitis / Pharyngitis9. Skin and Soft Tissue Infection (SSTI)10. Genitali Infections11. OsteomyelitisNeonates (special conditions)1. Sepsis2. Meningitis(iii) Infants & Small Children (special conditions)1. Meningitis2. Sepsis3. Pneumonia(b) Classification of Antimicrobials into first line, second line and reserve group of drugs(c) Chemoprophylaxis(i) Pre-operative antimicrobials(ii) Other invasive procedures(iii) Special high risk groups e.g. Prophylaxis <strong>for</strong> rheumatic fever, splenectomypatients, immuno-compromised patients(d) Special clinical syndromes (e.g. STIs as per government guidelines)4. Prescription auditing (not being done at present; will be initiated in collaboration with thedepartment of Pharmacology) as per(i) age groups(ii) patient location – outdoor (OPD), indoor (wards & critical care areas)5. Quarterly and annual review of surveillance data generated from antibiograms (done) &prescription auditing (planned).6. Education and training <strong>for</strong> all infection control activities being coordinated by the departmentof Microbiology, in collaboration with the <strong>Hospital</strong> Infection Control Committee.16
Annexure-1Policy on‘<strong>Hospital</strong> Waste Management’10.5.10Dr. K.T. Bhowmik, Dr Sunita Singal,Department of HWM17
ACKNOWLEDGEWe would like to place on record, that valuable contributions were made by *Dr K SBeghotia, in the preparation of the policy. He per<strong>for</strong>med an exchaustive review of the draft,which helped in the finalization of this policy document.Our special thanks are also due, to Mr. Ajay Wadhwa Sanitary superintendent, <strong>for</strong> hisinputs and unstinted support throughout the preparation of this document.Dr. Sunita Singal,Nodal OfficerDepartment of HWM, VMMC & <strong>Safdarjung</strong> <strong>Hospital</strong>*Dr K S Baghotia is State Programme Officer, Govt. of Delhi, Directorate of Health Service,F-17, Karkadooma, Delhi-11003218
CONTENTSTOPIC SUB-TOPIC PAGE NO.1. INTRODUCTION The Objectives of Waste Management PolicyStrategies of Waste Management 5<strong>Hospital</strong> Waste Management Committee & ItsFunction2. PRACTICES IN THE Policy on Segregation of WastesPATIENT-CARE Bins and LinersAREAS/CLINICAL Disinfection and MutilationAREAS Labeling, Collection, Storage and Recording of 7Waste in the Clinical AreasTransportation3. TREATMENT EquipmentMaintenance of Equipment: 11Storage, Quantification and Treatment of theWaste Storage Site4, FINAL DISPOSAL Disposal of non sharpsDisposal of Sharps:Recycling Policy: 13Record Keeping and Reporting of Data5. MANAGEMENT OF Liquid and chemical waste managementWASTE FROM Laboratories, Blood BankSPECIAL AREAS: RNTCP LaboratoryMercury and Lead Waste 14Disposal of Radioactive waste Disposal ofRadioisotope/Nuclear WasteE-Waste:Effluent Treatment Plant6. SAFETY ISSUES AND PPE & Vaccination of the Health Care WorkersOTHER PROTOCOLS Liquid spill managementMercury Spill Management 17Sharps Injury Management7. TRAINING Induction and refresher training 198. MONITORING AND Monitoring, supervision and Evaluation 20SUPERVISION9. FUTURE BACK-UP <strong>for</strong> Treatment of wastePROPOSALSRefresher Training of the StaffPublic Awareness/IEC Material 21Composting of Kitchen and Horticulture waste10. ABBREVIATIONS Abbreviations/Glossary 22GLOSSY11. ANNEXURES Pro<strong>for</strong>ma Samples 2719
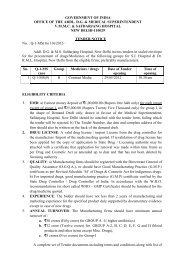
1. INTRODUCTIONAll over the world, the modern hospitals and Healthcare institutions use a wide varietyof drugs chemicals, radioactive substances, and per<strong>for</strong>m a variety of investigations and surgicalprocedures. The advent of state of art sophisticated newer technologies, the disposables i.e.,syringes gloves and other devices all of which ultimately become part of the hospital waste.This has brought in tis wake, risks of unauthorized and illegal reuse/misuse of these devicesand an enormous increase in the quantum of waste from hospitals.The Ministry of Environment and Forests, Govt. of India notified the Bio-Medical Waste(Management and Handling) Rules on 27th July, 1998; under the provisions of Environment Act1986. These rules have been framed to regulate the disposal of various categories of Bio-MedicalWaste as envisaged therein; so as to ensure the safety of the staff, patients, public and theenvironment.In order toe comply with the BMW Rules safdarjung hospitals has set up requisite biomedicalwaste treatment facilities incinerator, microwave system <strong>for</strong> the treatment of waste andall other requisite arrangements as per guidelines o.THE OBJECTIVES OF WASTE MANAGEMENT <strong>POLICY</strong>:The Bio-Medical Waste Management policy of Safdarjang hospitals has been drafted to meetthe following broad objectives:-(i) Provide a system of management of potentially infectious and hazardous waste as perguidelines and recommendations of Biomedical Wastes (Management and Handling Rules)1998.(ii) Identifying, defining & classifying the various categories of waste being generated in thehospitals.(iii) Segregation of various categories of waste in separate color coded containers at the siteof generation, so that each category is treated in a suitable manner to render it harmless.(iv) Disinfection/decontamination of infected items at the site of generation immediately afteruse.(v) Onsite appropriate ‘‘treatment technology’’ to be used depending upon the category ofwaste.(vi) Creating a system where all categories and personnel are responsible as well as accountable<strong>for</strong> proper waste management.(vii) Environment and patient friendly safety norms.STRATEGIES OF WASTE MANAGEMENT :Following strategies will be adopted to meet the broad objectives of the Bio-Medical WasteManagement in <strong>Safdarjung</strong> hospital :1) A system will be established of management of potentially infectious and hazardous asper guidelines and recommendations of Biomedical Wastes (Management and HandlingRules) 1998.2) Waste will be classifying the various categories being generated in the hospital.3) Use of separate color coded containers <strong>for</strong> Segregation of various categories of wasteat the point of generation,4) Disinfection/decontamination of infected items at the site generation immediately afteruse.5) Onsite appropriate ‘‘treatment technology’’ will be used depending upon the category ofwaste.6) Establishing a system where all categories of personnel perceive responsible as well asaccountable <strong>for</strong> proper waste management.7) Adoption of Environment and patient friendly safety norms.20
HOSPITAL WASTE MANAGEMENT COMMITTEE AND IT’S FUNCTIONA hospital Waste Management Committee, has been <strong>for</strong>med which function under the Chairmanshipof the Medical Superintendent. It is a broad based committee with representative from variousclinical departments, including Medical store, sanitation, Nursing and engineering Depts. Thecommittee holds meetings periodically.Function of the Committee :• Implementation of the Bio-Medical Waste (Management and Handlings) Rules publishedin gazette of India of 27th July, 1988; under the provisions of Environment Act 1986in the hospital.• Monitor and ensure effective, hospital waste management in the <strong>Hospital</strong>.• Organize proper and timely; training program <strong>for</strong> all categories of workers.• Responsible <strong>for</strong> ensuring good waste management practices and waste minimization.AUTHORISATION : The hospital has been authorized <strong>for</strong> generation, collection and treatmentof the Bio medical waste as per rule.2. PRACTICES IN THE PATIENT-CARE AREAS/CLINICAL AREAS :<strong>POLICY</strong> ON SEGREGATION OF WASTE :The hospital should ensure that clinical and general wastes is segregated at source and placedin color coded plastic bags and containers prior to collection and disposal at the site generationin all patient care areas/clinical areas. There is no mixing of waste.Yellow, Blue and Black colored bags are used <strong>for</strong> segregation*.Segregation is the responsibility of the generator of wastes i.e. the doctors, nurses orparamedical personnel.Segregation is done <strong>for</strong> each of the following:• Infectious non sharps• Infectious sharp• Disposable plastic items• Glass• General waste• Paper/ cardboards• Cytotoxic/radiological/radioactive• Microbiological/pathological wastes*Read bags contain Cadmium which gives toxic emissions if incinerated hence not used in SJH.21
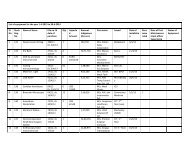
Biomedical Waste Management ‘Segregation Chart’Yellow Bag (one)BlackCategory 1,2, 3,6Bag (one)Category5,9,10Items Non Infected Infected General andhouseholdcontaminated I/V Bottles-1 Syringes-2 Gloves-3 1/V sets -4 type ofwith blood orwastebody fluid, Blood Give a nick, Destroy/cut the After Catheters paper, peelsbags and blood Collect, tie hub with needle Clipping tubings, Ryles leftovertransfusion set when 3/4ths syringes and tube, Suction food(non-PVC), full and send destroyer, disinfecton tubes,Cotton swabs, <strong>for</strong> disposal. disinfect in Collect urobes,body tissues, bleach solution <strong>for</strong> disposals Oxygen Mask All expired/body parts, (1%, <strong>for</strong> 30 when etc, give a medicines,organ tissues, minutes). 3/4th full. nick incinerationMicorobiology and Collect and Collect and Ash andBiotechnical send <strong>for</strong> final send <strong>for</strong> solidwaste without disposal when disposal when chemicalschemical 3/4 full. 3/4the full. sent totreatment Puncture proof securedContainerlandfillDestroyedNeedles, ScalpelBlades, OtherMetal SharpsNB: No PVC material should be placed in yellow bag.Any material treated with hypo-chlorite solution should never be sent <strong>for</strong> incineration22
Color-coded bags & Category wise TreatmentColor Coding Type of Container-1 Treatment option as perWaste Category Schedule 1Yellow Bags Cat. 1, Cat. 2 and Cat. 3, IncinerationCat. 6.Blue Bags Cat. 4, Cat. 7. Chemical Treatment Microwavingand shreddingBlack Bags Cat. 5 and Cat. 9 and Disposal in municipal landfillCat. 10. (solid)SEPARATE PUNCTURE PROOF CONTAINERSSeparate Puncture proof Containers are used i.e., one <strong>for</strong> each of following:• Metallic sharps in a container with hypochlorite solution and• Glass vials, broken glass.CARDBOARD BOXES• Paper/cardboards• othersBINS AND LINERS :The container comprises of an inner bag of color depending on the type of waste, and shouldmatch the chosen outer container is a plastic bin with handles, and of a size which will dependon the amount of waste generated. The inner polythene bag should be leak proof, and shouldfit into the container with one-fourth of the polythene bag turned over the rim.LINERS/PLASTIC BAGS: MATERIALS USED:Biodegradable plastic bags of 3 colors yellow, and black are used, to line the same coloredbins with the specifications ad guidelines of BMW Rules:-• Gauze – 225 (55 microns) if low density• Gauze-100 (25 microns), if high densityYellow and Blue bags are marked with Biohazard symbol and hospital logo.Black bags – <strong>Hospital</strong> logo and name.BINS :Containment of waste : An optimum number of easy to use, Standard, uni<strong>for</strong>m, covered, footoperatedbins of 3 colors i.e., yellow, blue and black, of appropriate size would be placed atidentified places in all clinical areas.DIS<strong>INFECTION</strong> OF BINS :Chemical disinfection of the waste bins using hypochlorite solution should be done frequentlyat a separate washing facility in the hospital.DIS<strong>INFECTION</strong> AND MUTILATION OF SHARPS :In order to render them harmless to waste handlers a Pre-Treatment of the infectious wastegenerated in the patient-care areas is required, prior to transportation <strong>for</strong> onsite treatment anddisposal. It is required <strong>for</strong> the following infectious items;• Syringes• Needles• Catheters, I/V sets, gloves23
To ensure the disinfection/pretreatment of the waste without at the site of generation, thefollowing guidelines/advisory is followed in all areas:-1. Use of needle destroyer the needles and then the same is put into the puncture proofcontainer containing hypochlorite solution.2. After use, the nozzle of Syringes is to be cut with the needle destroyer. Draw some bleachsolution into the syringe or separate the piston and barrel, and place it in the containerwith a sieve having 1% hypochlorite solution <strong>for</strong> 30 minutes. After 30 minutes the syringeare placed in the blue bags by lifting the inner sieve.3. In the gloves are clipped immediately after use by the dedicated pair of scissors placedin the area to prevent reuse and the dipped in 1% hypochlorite solution in a bucket <strong>for</strong>30 minutes <strong>for</strong> disinfection. After disinfection they should be placed in a blue bag.4. All plastic items IV bottles, urobags, brains etc. are given a nick putting in blue bag. Eachbag is labeled and securely tied when three-fourths full.COLLECTION STORAGE, LABELING, AND RECORDING OF WASTEAll the biomedical waste is labeled as waste type, site of generation, date of generation be<strong>for</strong>etransportation from the generation site. Waste is stored in the areas of generation at an identifiedsafe area, <strong>for</strong> an interim period after which it is transported <strong>for</strong> onsite treatment and finaldisposal. During this period it is the responsibility of the waste. No untreated bio-medical wasteshall be kept stored beyond a period of 48 hours.Collection si done- Daily from all areas- Done twice daily or more frequently <strong>for</strong>m labor rooms/ OTs- Label is filled up by staff on duty and given to waste collectorsEach patient care area has been provided with the waste receipt book to record the quantity/number of yellow and blue gabs handed over the HCW. All the staff are required to duly fullin the waste book color wise mentioning the number and size of bags handed over and signthe slip <strong>for</strong> further record.TRANSPORTATION :<strong>Hospital</strong> waste is transported in securely tied bags from the site of generation to the treatmentfacility (incinerator premises) through designated route, on dedicated, color coded, covered andleak proof wheel barrows/Trolleys. At the waste treatment premises verification of the number/size of the bags is done <strong>for</strong> each trolley by the sanitation staff <strong>for</strong> recording and quantificationbe<strong>for</strong>e disposal.Chemical disinfection of the trolleys using hypochlorite solution is being at the waste storagesite.3. TREATMENT FACILITIES :EQUIPMENT :<strong>Safdarjung</strong> hospital has the following Equipment <strong>for</strong> in-house treatment of waste:1. Incinerator : 3 units of incinerator were installed in 1994 having chimney height of30 meters each, capacity 150-175 kg/hr. Only one is equipped with APCD and is inuse.2. Microwave : Microwave with a capacity of 60 Litres per cycle is available at the wastesite. All the infectious plastic waste is disinfected in Microwave.3. Shredder Machine : One indigenous type and one ‘Bometic’ shredder machine isinstalled in 1998. It is used to shred plastic and PVC materials such as I.V. bottles,disposable syringes, IV tubing etc. after they have been micro waved at the site ofgeneration24
MAINTENANCE OF EQUIPMENTMaintenance of Incinerators is done by CPWD Electrical Engineers. The operator posted byCPWD is maintaining the record of the operations of incinerator, temperature of the incineratorchambers and hours of operation of the incinerator as per CPCB requirements. The parametersare recorded everyday, manually at present under supervision of junior Engineer CPWD(Electrical) and Sanitary Supervisor (S. S) and are available <strong>for</strong> inspection any time.OPERATING PARAMETERS OF EQUIPMENT :The incinerator and microwave operate as per parameters give by BMW <strong>Guidelines</strong>. Culture ofthe treated waste is periodically per<strong>for</strong>med and monitored.STORAGE AT THE MAIN WASTE STORAGE SITE :There is adequate space to store the wastes transported from various clinical areas while awaitingfinal treatment and disposal. In the storage areas, wastes are stacked with clear distinction asper the color coding of the waste. There is warning signboard prominently placed at the entrance.Adequate security and guarded gate is provided at the facility to prevent unauthorized accessto the site by humans and livestock. The premise has provision <strong>for</strong> locking. The site hassufficient electricity and water supply. There is adequate open space <strong>for</strong> municipal trucks tohave easy access <strong>for</strong> collection.QUANTIFICATION :Counting of bags and verifying with the labels from each area is done at the collection siteby the staff posted there. The yellow bags containing the infectious waste are counted andthe number is confirmed from the receipt from each area. After this the weighing of all yellow/blue is done. The data is recorded and maintained area-wise/Department-wise.TREATMENT :After this all the Yellow bags are directly sent <strong>for</strong> incineration. Ash from the incineratoris collected in black bags and kept along with the general waste. The waste is non toxic andnon infectious, and is taken by civic authorities.The blue bags containing disposable plastic (Syringes, IV canulas and bottles) are dulyverified in number from the receipt at the site. The infected plastics and gloves are then putin the microwave <strong>for</strong> disinfection/treatment.After treatment, in the microwave all plastics are shredded in the shredding machine. Aftershredding the granular plastic is stored in blue bags till final disposal. These bags should belabeled as with Cytotoxic symbol. There should be a separate storage facility <strong>for</strong> untreated andtreated waste.4. FINAL DISPOSALDISPOSAL OF NON SHARPS:Black bags containing expired/discarded medicines along with ash from the incinerator are takenaway by the NDMC truck <strong>for</strong> disposal to a secured landfill everyday.Blue bags:The shredded material so obtained from the shredded is placed and stored in blue bags. It isthen sold <strong>for</strong> recycling to Govt. authorized vendors every <strong>for</strong>tnight or earlier if required.DISPOSAL OF SHARPS :All metallic sharps are received in puncture-proof containers.Deep pits <strong>for</strong> sharps have been made in a safe areas as per guidelines of BMW. Currentlyfourth pit is in use. All sharps are poured in the pits after weighing and recording. Encapsulationoption of disposal of sharps will be started after fourth pit is full.25
RECYCLING <strong>POLICY</strong> :The hospital follows the principle of reducing, and favors policy of recyclingAll disinfected and shredded plastics, gloves, glass, cardboard etc. are sold to Govt. approvedvendors/Kabariwalas at Govt. approved rates.RECORD KEEPING AND REPORTING OF DATA :Maintenance of the records :The following records are being maintaining by the HWM Dept. :i) Incinerator parametersii) Microwave parameters.iii) Each patient care area has been provided with the waste Receipt book. All the staffare requested to duly fill up the waste book code wise with nos. of beg and signthe slip <strong>for</strong> further record.iv) Quantity of infectious waste received from various areasv) Quantity of plastic wastevi) Quantity of waste sold to vendorvii) Annual reportsviii) Monthly reportsix) Authorization from DPCC,x) Consent to establishxi) Recyclable wastexii) Sharps Injury register.xiii) Immunization registerxiv) Miscellaneous correspondence liaison with other department DPCC etc.The monthly and annual reports are sent to MOHFW and the requisite in<strong>for</strong>mation is providedto CPCB/DPCC whenever required.5. MANAGEMENT OF WASTE FROM SPECIAL AREAS :LIQUID AND CHEMICAL WASTES MANAGEMENT :Chemical disinfection of the liquid waste, at the areas of generation e.g., Labor rooms, OTs,labs etc is done. These liquid wastes should be disinfected by chemical treatment using at least1% sodium hypochlorite solution <strong>for</strong> a contact period of 30 Minutes and them discharged intodrains/sewers where it is taken care of by the principle of dilution and dispersal.LABORATORIES, BLOOD BANK :• The blood sample glass vials, plastic vials etc. from all he laboratories is chemicallydisinfected in the respective labs. The discarded disinfected vials are packed in blueplastic bag <strong>for</strong> final disposal.• The Microbiology cultures plates/dishes, stalks are locally autoclaved be<strong>for</strong>e transportingto the waste premises <strong>for</strong> final disposal.• The discarded blood bags are brought by a responsible staff member, (Doctor ortechnician) double packed in yellow bags and sealed. At the incinerator premises thesealed bag is weighed <strong>for</strong> record purpose and then incinerated in the presence ofboth the blood bank technician and the incinerator operator. Both of them sign andrecord the same.DISCARDED MEDICINES AND CYTOTOXIC DRUGS:• The discarded medicines and cytotoxic drugs, which need to the disposed, shouldbe certified by Head of the concerned department, put in a yellow bag, tied andsealed.26
• Labelled as with ‘Cytotoxic’• Weighed, and weight should be written over it• Send <strong>for</strong> incineration through 2 responsible staff members from the ward, who willget it incinerated in the presence of Sanitary Inspector.• After incineration all three staff members will record the same and duly put theirsignatures on the document.• A copy of the same may be sent to M.S. <strong>for</strong> in<strong>for</strong>mationMERCURY AND LEAD WASTE, DENTAL OPDs :– Our hospital has stopped purchase of mercury-based BP Instrument and Thermometers andtheir use is being phased out. The mercury waste generated is ‘contained’, awaiting appropriatedisposal options e.g., handing over to Govt. approved vendors. Similarly the Lead waste is alsobeing contained awaiting suitable and safe disposal options.Mercury amalgum fillings are not being used in dental fillings are present.DISPOSAL OF BIOMEDICAL WASTE GENERATED IN THE RNTCP LABORATORY (DOTSCENTRE)Sputum cups and broom sticks : The use of cups made from biodegradable poly propylenepoyethylene will be encouraged. The lids will be removed from used cups. Then the cups andlids will be placed in the disinfectant 5% Phenol provided by the RNTPCP or hypochlorite solutionovernight. The broom sticks will be placed in the separate container having similar disinfectant.Next the cups, lids and broomsticks will be autoclaved provided to the RNTTCP Centre. Theautoclaved cups and lids will be sent <strong>for</strong> shredding and further disposal in blue bags. Thechemically disinfected and autoclaved broomsticks can be disposed of as general waste. Theleft over fluid after chemical disinfection will be drained in hospital drainage.Used slides: The slides will be disinfected by immersion in 5% Phenol <strong>for</strong> a minimum of 30minutes. After that it is disposed of with other hospital sharps. Breaking of slides is notrecommended. The used chemical solution will be drained away in the hospital drain.WASTE FROM RADIOLOGY :The fixer and developer and contained and then sold periodically to Govt. authorized vendor<strong>for</strong> recycling.DISPOSAL OF RADIOACTIVE WASTEThe department of radiotherapy is not generating Radio-Active waste <strong>for</strong> disposal. The departmentuses sealed sources. The depleted sources are sent back to BARC by the Authorized Agentsof equipment concerned.DISPOSAL OF RADIOISOTOPE/NUCLEAR WASTE1. The hospital is authorized by the competent authority, i.e. Atomic Energy RegulatoryBoard of India, Mumbai – 400094 vides letter no. AERB/RSD/RIA-Auth/DL-07/2009/3166 dated March 17, 2009.2. At present we are using RIA / IRMA kits which contain radioactive 125-lodine. Theabove authorization is <strong>for</strong> the procurement and use of the radioactive material in ourdepartment. It also specifies the numbers of kits which we can use per months.3. After use, the radioactive material is disposed into the sewerage system in thehospital. The quantity disposed by per day is much less than the maximum limiton total discharge per day.E-WASTE :Electronic Waste–Some called E-Waste. A term loosely applied to consumer and businesselectronic equipment that is near or at the end of its useful life. It includes, computers, computer27
peripherals, telephones, answering machines, radios, stereo equipment, tape players/recorders,phonographs, video cassette players/recorders, compact disc players/recorders, calculators, andsome appliances. Certain components of some electronic products contain materials that renderthem hazardous, depending on their condition and density. Nonfunctioning CRTs (cathode raytubes) from television and monitors are considered as hazardous. There<strong>for</strong>e, nonfunctioningCRTs from television and monitors are banned from the trash. All electronic waste will be‘contained’ in the area of use. E-waste recyclers authorized by Central Pollution Control Boardwill be contacted <strong>for</strong> collection and final disposal of E-waste.As per guidelines issued by DGHs, a clause <strong>for</strong> Buy back policy may be included at the timeof tendering <strong>for</strong> purchase of electronic Equipment <strong>for</strong> minimization of E-waste.EFFLUENT TREATMENT PLANT :The design and operation of wastewater treatment system <strong>for</strong> hospital is a. These liquideffluents, directly rejected in the network drainage of laboratories, and other clinical areas ofthe hospital, can contribute under certain physico-chemical conditions to the presence of thevirus in the urban sewer network and in the wastewater treatment plant. <strong>Hospital</strong> wastewaterreveals the presence of molecules chlorinated in high concentrations and in a punctual way thepresence of heavy metals such as mercury and sliver. DPCC has issued notice that 500 ormore bedded hospitals should install the ETP in their hospitals. ETP of Safdarjang <strong>Hospital</strong> isunder process and is likely to be functional shortly.6. SAFETY ISSUES AND OTHER PROTOCOLSPPE & VACCINATION OF THE HEALTH CARE WORKERS:All waste handlers have been provided with Masks, Caps, Gum Boots, Gloves, and Disposableapron which they are expected to wear while dealing with the waste. All health care workers arevaccinated against Hepatitis B and tetanus.DEALING WITH SPILLAGE :Liquid spill management :For small volume spills:• Cover spills of infected or potentially infected material on the floor with paper towel/blotting paper/news paper. Pour 5% Phenol or freshly prepared 5% hypochloritesolution.• Leave <strong>for</strong> 30 minutes <strong>for</strong> contact• Then it wipe with gauze or cloth with gloved hands.• The gauze or cloth used to wipe is to be considered as noninfectious waste anddiscarded in general waste.For large volume spills:• Wear gloves.• Mop with absorbent cotton/gauze and discard it to infectious waste bin• Cover spills of infected or potentially infected material on the floor with paper towel/blotting paper/news paper. Pour 5% Phenol or freshly prepared 5% hypochloritesolution.• Allow it <strong>for</strong> 30 min contact period.• Wipe thoroughly with gloved hands using cotton or gauze and treat the gauze as sooninfectious waste and dispose accordingly.NB : Any material treated wit hypo-chlorite solution should never be sent <strong>for</strong> incineration28
MERCURY SPILL MANAGEMENT :If accidental spill of mercury occurs it is to be collected in a special manner as follows :• Spilled mercury should be collected with a ‘‘mercury spill kit’’- containing nitrile gloves,N-95 face mask, 2 pieces of cardboards, 2 plastic containers, cello tape, andflashlight.• Do not touch mercury.• Remove all jewelry, wear gloves, masks.• Use flashlight to locate and cardboards to bring mercury beads together.• Collect with an eyedropper of a syringe and carefully place it or ‘contain’ in a bottlecontaining water.• Any remaining beads of mercury should be picked up with a sticky tape and placein the plastic bag, properly labeled.• The bottle should be sealed with a tape, labeled as hazardous waste and securelystored inside another plastic container; awaiting final disposal to Govt. nominated orauthorized mercury dealers.• After mercury has been recovered the spill area should be covered with calciumsulfide or sodium thiosulfate to neutralize it.• Reporting <strong>for</strong>mats will be used to report and register any mercury spills/leakages.SHARPS INJURY MANAGEMENTThe commonest cause of injury while handling the waste is inappropriate segregation whereinsharp waste is deposited in containers meant <strong>for</strong> non sharp waste. When sharp injury occursfollowing procedures is to be followed.(i) Stop the procedure immediately and wash the wound with soap and water, encouragebleeding the apply antiseptic.(ii) Immediately report to Nodal officer in Casualty <strong>for</strong> First aid and emergencytreatment or any other action and follow-up advice, if required. ‘PEP’ is provided iscasualty round the clock as per MOHFW guidelines.(iii) Retention, if possible of the item and details of its source <strong>for</strong> identification ofpossible infection.(iv) Investigation, determination and implementation of remedial measures.(v) Recording of Sharp injury: Needle Sticks/ Sharp injury should be recorded as perthe Per<strong>for</strong>ma provided by BMW <strong>Guidelines</strong>. (Annexure I). This Per<strong>for</strong>ma is availablein casually.Training needs of different categories of persons are identified and training is providedregularly, as well as in<strong>for</strong>mally onsite during inspection or supervisory rounds. The objectivesof training are to increase awareness, improve practices, change attitudes and monitor thesystem.INDUCTION TRAINING OF THE NEWLY RECRUITED STAFF:‘Induction Training is provided to each of the fresh new employee, involved in patient-careservice in the hospitals, whether a Doctor, a Nurse a Technician or a Group D staff. It is apre-requisite <strong>for</strong> the release of first salary.REFRESHER TRAINING OF ALL THE STAFF MEMBERS OF VMMC & SJH:A regular training of the staff CME’s, Workshops, are the essential part to maintain the <strong>Hospital</strong>Waste Management (HWM) at the best. It is necessary to conduct the regular refresher trainingof all the staff members of the hospital. The Department of HWM organizes ‘Regular Training’,every month and it has become a permanent feature. A ‘training calender’ <strong>for</strong> all categoriesof staffs of the hospitals has been prepared.29
8. MONITORING AND SUPERVISIONA Monitoring Team which includes Nodal officers, Nursing Sisters, Technicians and Sanitationstaff is responsible <strong>for</strong> supervision of segregation practices in the specific area, allocated tothem. The Nursing Sister in charge of the area is expected is take a round of the area everydayand record the findings in the observations Daily observation Per<strong>for</strong>ma attached herewith(Annexure II). This Per<strong>for</strong>ma is displayed/available in each clinical area. The DNS of each zoneensure proper compliance of Daily monitoring of waste management practices in the clinicalareas by the ANS/Nursing Sister.The technicians of Laboratories and O Ts will be responsible, <strong>for</strong> the are of their workAny adversity should be reported to are Nodal Officer, who will take appropriate action and ifrequired intimate the same to the higher authorities. The Area Nodal officers will take periodicround of their area, record using ‘Monitoring Per<strong>for</strong>ma’ (Annexure ‘III’) and address any issues.They may also take appropriate action, and in<strong>for</strong>m the respective HODs, and HWM Committee.All the Sanitary Inspectors as well as Health Inspectors will be responsible <strong>for</strong> the wastemanagement practices in the area already allocated to them <strong>for</strong> supervision of sanitation.Regular rounds are taken by CMO, Nodal Officer of HWM. The observation reports of thefindings are sent to the respective HOD <strong>for</strong> remedial action through Medical Superintended.Surprise rounds are also being taken by Addl. MS & MS from time to time in the patient careareas. The random checking of the waste receipts, bags <strong>for</strong> segregation of waste are beingdone at the waste storage site, as a part of audit and any deficiencies / observation are sentto the HOD <strong>for</strong> remedial action.9. FUTURE PROPOSALS :BACK-UP EQUIPMENT FOR TREATMENT OF WASTE:- Backup <strong>for</strong> Microwave and shredder to be procured..- Alternative options of ‘Encapsulation’/outsourcing <strong>for</strong> disposal of metallic sharps, soas to discontinue making any more ‘pits’ or outsourcing <strong>for</strong> disposal of metallicsharps- Autoclave/Hydroclave- Installation of ETP- ‘OUTSOURCING OF WASTE’‘SHARPS INJURY’ (NEEDLE STICK INJURY)A specific protocol <strong>for</strong> prevention of risks of Hepatitis B to HCW of our hospital due to Sharpsinjury (NSI) is being worked out.PATIENT AND ATTENDANT EDUCATION AND AWARENESS :At the time of admission to hospital a briefing regarding the segregation policy of the hospitalshould be given by the Staff nurses and the same is rein<strong>for</strong>ced everyday. Al leaflet of ’Do’s& Don’ts’ will be prepared and given to all attendants of patients at the time of admission.PUBLIC AWARENESS/IEC ACTIVITIES :In order to involve the public and seek co-operation, it is essential to generate awareness byall possible means. This can be achieved through IEC activities. This would help to keep thehospital clean. Public redress system of the hospital can also be used to propagate the samemessage.Posters in the working clinical areas to serve as reminders of segregation protocols will beprepared, and distributed in the whole to be displayed at the prominent points.30
FUTURE PROPOSAL FOR DISPOSAL OF RADIOSOTOPE/NUCLEAR WASTE• The immediate plan is to construct two separate tanks <strong>for</strong> liquid radioactive wastematerial. First one is filled and then sealed <strong>for</strong> a period of 10 half life of the radioactivematerial put into it. During this period the radio active waste is stored is second tank.By the second tank becomes full, the first completes 10 half lives and comes to thelevel of background radioactivity. This waste is discarded safely in sewer system.This becomes a continuous process.COMPOSTING OF KITCHEN AND HORTICULTURE WASTE :It is proposed to generate manure by composting waste from kitchen, horticulture and disinfecteddiscarded blood. Four pits <strong>for</strong> the same can be made in identified areas. For fifteen days thewaste can be put in one pit, in the second pit <strong>for</strong> the next 15 days and so on. It Compostinggenerally takes 45-60 days, and the manure is ready.BIOFUEL, BIOGAS (BIO-CNG, BIO-PNG) and manure production from General wet/kitchenwaste, using BARC developed Technology may also be considered if feasible.As & when a new, heavy duty shredding machine is produced by the hospital or outsourcingis decided, instead of four only 2 blue plastic bags will be used <strong>for</strong> segregation of plasticwaste, one <strong>for</strong> infectious plastic and 2nd <strong>for</strong> non-infectious plastic. The current shredders donot take up mixed plastic items <strong>for</strong> shredding.10. ABBREVIATIONS AND GLOSSARY OF TERMS:ANSAssistant Nursing SuperintendentAPCDAir Pollution Control DeviceBMWBio-medical WasteCat.CategoryCMEContinuing Medical EducationCMOChief Medical BoardCPCBCentral Pollution Control BoardDMSDeputy Medical SuperintendentDNSDeputy Nursing SuperintendentDPCCDelhi Pollution Control CommitteeHCF(s)Health-care facility (facilities)HCWHealth-Care Waste. HCW is made up of HCRW and HCGW.HCWHealth Care WorkerHCWMHealth-care Waste ManagementHIVHuman Immunodeficiency VirusHODHead of the DepartmentHWM<strong>Hospital</strong> Waste managementMSMedical superintendentOPDsOut Patient DepartmentPPEPersonal Protective EquipmentRNTCPRevised National Tuberculosis Control ProgrammeAir pollution The presence of a material or substance in the air which may beharmful to either the natural or human environment, which includesnay material present in sufficient concentrations <strong>for</strong> a sufficienttime, and a number of circumstance, to interfere significantly withthe com<strong>for</strong>t, health or welfare of persons or with the full use andenjoyment of property.31
Anatomic wasteBiomedical andhealth-care wasteChemical wasteCollectionContainerDecontaminationDisinfectantDisposalExposureCytotoxic wasteHIV/AIDSIncinerationInfectious health-IrradiationConsisting of recognizable body partssolid or liquid waste arising <strong>for</strong>m health-care (medical) activitiessuch as diagnosis, monitoring, treatment, prevention of disease oralleviation of handicap in human or animals, including related research,per<strong>for</strong>med under the supervision of a medical practitioner or veterinarysurgeon or another person authorized by virtue of this professionalqualificationsConsisting of/or containing chemical substances.the act of removing accumulated containerized solid waste from thegenerating source. Private collection of solid and liquid waste byindividuals or companies from residential, commercial, health facilityor industrial premises. The arrangements <strong>for</strong> the service are madedirectly between the owner or occupier of the premises and thecollectorvessel in which waste is placed <strong>for</strong> handling, transportation. storageand/or eventual disposal. The waste container is a component of thewaste package.the process of reducing or eliminating the presence of harmfulsubstances such as infectious agents so as to reduce the likelihoodof disease transmission from those substanceschemical agent that is able to reduce the viability of micro-organismsIntentional burial, deposit, discharge, dumping, placing or release ofnay waste material into or on any air, land or water.the amount of radiation or pollutant present in a particular environment(i.e. human, natural) which represent a potential health threat to theliving organisms in that environmentcytotoxic/Genotoxic waste is highly hazardous and may havemutagenic, terato-genic, or carcinogenic properties. It raises serioussafety problems, both inside hospitals and after disposal, andshould be given special attention. Genotoxic waste may includecertain cytostatic (antineoplastic) drugs. These powerful drugs havespecific destructive action on action cells (often used in chemotherapyof cancer).HIV (Human Immuno-deficiency Virus) is the virus that causesAIDS (Acquired Immune Deficiency Syndrome). Over time, infectionwith HIV can weaken the immune system to the point that thesystem has difficulty fighting off certain infections that in turn canlead to death.discarded materials from health-care activities on humans or animalswhich have the potential of transmitting infectious agents to humans.These include discarded materials or equipment <strong>for</strong>m the diagnosis,treatment and prevention of disease, assessment of health statusor identification purposes, that have been in contact with blood andits derivatives, tissues, tissue fluids, or wastes from infectionisolation wards.exposure to radiation of wavelengths shorter than those of visiblelight (gamma, x-ray or ultraviolet) <strong>for</strong> medical purpose, the destructionof bacteria in milk or other foodstuffs or initiation of polymerizationof monomers or vulcanization of rubber.the application of activities such as waste reduction, reuse andrecycling care waste to minimize the amount of waste that requiresdisposal.32
Minimization (ofwaste)MonitoringOn-site facilityPharmaceuticalPressurizedcontainersRadioactive wasteRecyclingRiskSanitary landfillSegregationSharpsSterllizationPeriodic or continuous surveillance or testing to determine the levelof compliance with statutory requirements and/or pollutant levels invarious media or in humans, animals and other living things.a clinical and related waste treatment, storage or disposal facilitythat is located on the generating siteconsisting of/or containing pharmaceuticalsconsists of containers (full or empty) with pressurized liquid, gas orpowdered materials.material contaminated with a radioisotope which arises from themedicalor research use of radionuclides. It may be in a solid, liquid orgaseous <strong>for</strong>ma term embracing the recovery and reuse of scrape or wastematerial <strong>for</strong> manufacturing or other purposes.Probability that a hazard will cause harm and the severity of thatharmcharacterized by the controlled and organized deposit of wasteswhich is then covered regularly (daily) by the staff present on site.Appropriate engineering preparations of the site and a favorablegeological setting (providing an insolation of wastes from theenvironment) are requiredthe control of all the factors in the physical environment thatexercise or can exercise a deleterious effect on human physicaldevelopment, health and survival.sharps are a subcategory of infectious health-care waste andinclude objects that are sharp and can cause injuriesa process used to reach a state of free of viable micro-organisms.Note that in a sterilization process, the nature of microbiologicaldeath or reduction is described by an experiment function. There<strong>for</strong>,the number of micro-organisms that survive a sterillization processcan be expressed in terms of probability. While the probability maybe reduced to a very low number, it can never be reduced to zero.the placement of waste isolation, environment and health protectionand human control (e.g. monitoring <strong>for</strong> radioactivity, limitation ofaccess) are provided. This is done with the intention that the wastewill be subsequently retrieved <strong>for</strong> treatment and conditioning and/or disposal (or clearance of radioactive waste)Storageany method, technique or process <strong>for</strong> altering the biological, chemicalor physical characteristics or waste to reduce the hazards it presentsand facilitate, or reduce the costs of, disposal. The basic treatmentobjective include volume reduction, disinfection, neutralization orother change of composition to reduce hazards, including removalor radionuclides from radioactive wasteWaste management all the activities-administrative and operational - involved in thehandling, treatment, conditioning, storage, transportation and disposalof waste33
11. ANNEXURES :Recording of Sharp Injury:Needle Stick/Sharp injury should be recorded as per the following protocol.Needle Stick/Sharp Injury ProtocolName of H.V.W. :Section of H.C.W. :Employment No. :History of InjuryDate of Needle Stick/ Sharp Injury :Date of Reporting To Casualty :Site & Depth of Injury :Nature of Injury: Needle Prick/ Sharp Cut/ Laceration/ Splash of Fluids/ Splattered GlassHistory of Hepatitis B Immunization: Date : Intradermal/ IntramuscularAnti HBs Titer (Date of Test)HBsAgYes/NoHIVYes/NoAction Taken in CasualtyHep. B. VaccinationHBsAgYes/NoHBsAgYes/NoTetanus ToxoidYes/No.Source of injury (if available)Serum sent <strong>for</strong> : (report to be entered in follow: up visit)HIVHbsAg34
PERFORMA OF BIOMEDICAL WASTE MANAGEMENTSAFDARJUNG HOSPITAL, NEW DELHI - 110029Ward No. MONTH :Date Working Sharp Proper segregation in Hypochlor Any SignaconditionCont different bags Ite. Remar ture ofof the ainer solution ks ANSNeedle Yellow Blue Black NursingDestroyerSister1.2.3.4.5.6.7.8.9.10.11.12.13.14.15.16.17.18.19.20.21.22.23.24.25.26.27.28.29.30.31.35
Annexure : IIIOFFICE OF THE PRINCIPAL & MEDICAL SUPERINTENDENTVMMC & SAFDARJUNG HOSPITAL NEW DELHI - 110029No. CMO (HWM)/Inspetion/200 Dated :MONITORING/ROUND RECORDDuring various inspections conducted in your __________________________________ on_______________________ following deficiencies as regard the implementation of Bio MedicalWaste Management and handling Rules 1998, were found.1.2.3.4.Sister-In-charge is directed to take effective steps immediately to correct.(Area Nodal officer/Chief Medical Officer)<strong>Hospital</strong> Waste ManagementCopy to :1. Head of Dept. <strong>for</strong> necessary action2. DNS/ANS3. Copy <strong>for</strong> in<strong>for</strong>mation to Addl Medical Superintendent36
ANNEXURE-2PROTOCOL FOR MANAGEMENT OFSHARPS/NEEDLESTICK INJURY/BLOOD BODYFLUID EXPOSURE.Dept. of Machine & Dept. of <strong>Hospital</strong> Waste Management<strong>Safdarjung</strong> <strong>Hospital</strong>New Delhi37
ANNEXURE-I (PERFORMA)RECORD OF SHARPS/NEEDLE STICK INJURY/BLOOD, BODY FLUID EXPOSUREName of HCW: Age: Sex : M/FDepartment: Category of HCW: Regd.no. :HISTORY OF INJURY:Date of InjuryDate of reporting to casualty:How the injury was sustained (while per<strong>for</strong>ming which procedure)_______________________________________________________________________________Nature and source of injury : Needle prick/ Sharp cut/Laceration/Splash of FluidsHepatitis B Immunization status of HCW & source :Exposed HCWVaccinated – Yes/No:Incompletely vaccinated 1 :Unvaccinated:Previous H/O infection with HB 2SourceUnknown/unavailable <strong>for</strong> testingUnknown/but available <strong>for</strong> testingKnown HBsAg- PositiveKnown HBsAg-NegativeHIV status of ‘Source’ : Negative/Positive/UnknownAction taken in Casualty :1. Help.B vaccination initiated : Yes/No.2. HBIG : Yes/No If yes, indication:3. TT: 4. Anti Retro Treatment 5. Any otherInvestigation advised to HCW in Casualty :Haemogram, LFT, KFT, HBsAg, HIV(if consent is given).Refer to ART clinic, R.no.557 <strong>for</strong> all above investigations and further follow-up.Investigation of source patient, if available:HIVHBsAGRemarks if any.Signatue of CMO/Nodal Officer on duty (Casualty)1. Received only 1 or 2 doses of Hep.B vaccine2. Persons who have previously been infected with HB are immune to reinfection and donot require postexposure prophylaxisDept. of Medicine & Dept. of Hosp. Waste Management, SJH.38
ANNEXURE-IIRECOMMENDED POSTEXPOSURE PROPHYLAXIS FOR EXPOSURE TO HEPATITIS B VIRUSVaccination TREATMENT TREATMENT TREATMENTstatus of exposedworkersSource Source Source 2Hbs Ag Positive HBsAg Unknown or notnegativeavailable <strong>for</strong>testing1. Unvaccinated HBIG x 1 and Initiate HB Initiate HBinitiate HB vaccine vaccine vaccineseriesseries2. Previouslyvaccinated• Serum anti-body No treatment No treatment No treatmenttitre known > bodymiu• Serum anti-body HBIG + 1 dose of No treatment 1 dose of HBtitre unknown or Hep.B vaccine< 10 miu3. Incomplete HBIG + Initiate Initiatevaccination 1 vaccination vaccination vaccination1Received only 1 or 2 doses of Hepatitis B vaccine2If source High risk treat as HbsAG positive.* Persons who wave previously been infected with HBV are immune to reinfection and donot require postexposure prophylaxis* HBsAg-Hepatitis B surface antigen* HBIG- Hepatitis B immune globulin; dose 0.06 ml/kg intramuscularly.RECOMMENDED POSTEXPOSURE PROPHYLAXIS FOR EXPOSURE TO HIV(Emergency dose to be given in Casualty)- Tablet Zidovudine 300mg + Lamivudine 150 mg.(Duovir) 1 Tab. BD+- Tablet. Indinavir 800mg. 1 Tab.BDPlease see attached annexure III and copy of NACO Guildelines <strong>for</strong> Post ExposureProphylaxis <strong>for</strong> Occupational Exposure(PEP) to HIV/AIDS(Annexure IV)Dep. of Medicine & Dept. of Hosp. Waste Management, SJH39
ANNEXURE-IIITHREE STEPS TO HIV POST-EXPOSURE PROPHYLAXIS (PEP)AFTER OCCUPATIONAL EXPOSUREStep-I : Determine the exposure code (EC)Is source material blood – bloody fuid, semen/vaginal fuild orother normally sterile fluid or tissue ?YesNoNo PEPRequiredWhat type ofexposure occurred ?Mucous members or skinintegrity compromised(e.g. Dermatitis, openwould)VolumeIntack SkinNo PEPPercutaneouse exposure :SeveritySeveritySmall :Few DropsLarge : Majorsplash & / orlong durationLess severe :Solid needle,scratchMore severe : Largebore hollow needledeep puncture,visible blood, needleused in blood vesselEC 1Of sourceEC 2 EC 2 EC 340
Step-II : Determine the HIV STATUS Code (HIV SC)What is the HIV status of the exposure source ?HIV Negative HIV Positive Status unknown Status unknownNo PEP Low titre exposure :Asymptomatic andHigh CD 4countHigh titre exposure :Advanced AIDS,primary HIV, highviral load or low CD 4HIV SCunkonownHIV SCHIV SCStep 3 : Determine Post-Exposure Prophylaxis(PEP) RecommendationEC HIV SC PEP1 1 Consider basic1 2 Recommend basic regimen2 1 Recommend expanded regimen3 1 or 2 Recommend expanded regimen1,2,3, Unknown If exposure setting suggests risks of HIVExposure, consider basic regimenBasic Regimen : Zidovucine (AZT)-600 in divided doses (300 mg) twice a day or 200 mg (thricea day) <strong>for</strong> 4 weeks + Lamiondine (3TC)- 150 mg twice a day <strong>for</strong> 4 weeks.Expanded Regimen : Basic regimen + Indinavir-800 mg thrice a day. or any other proteaseinhibitor.Pregnancy and PEPBased on limited in<strong>for</strong>mation, anti retroviral therapy taken during 2 nd and 3 rd trimester ofpregnancy has not caused serious side effects in mother and infants. There is very littlein<strong>for</strong>mation on the safety in the 1sr trimester. If the HCW is pregnant a time of exposure toHIV, the designated authority or physician must be consulted about the use of the drugs andPEP.Dept. of Medicine & Dept. of Hesp. Waste Management, SJH41