Patient Assessment - Usmra.com
Patient Assessment - Usmra.com
Patient Assessment - Usmra.com
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
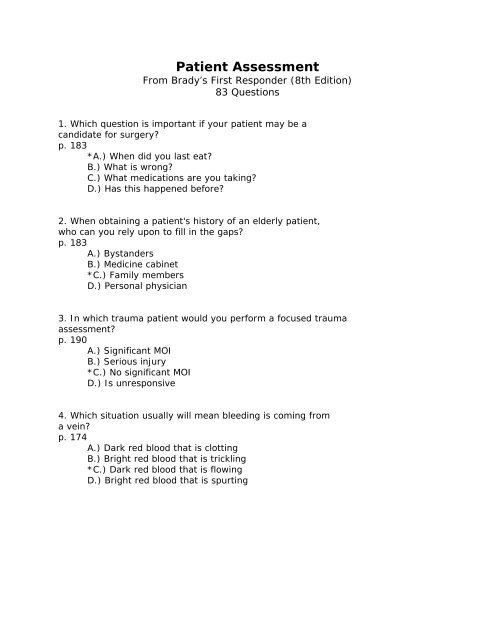
<strong>Patient</strong> <strong>Assessment</strong>From Brady’s First Responder (8th Edition)83 Questions1. Which question is important if your patient may be acandidate for surgery?p. 183*A.) When did you last eat?B.) What is wrong?C.) What medications are you taking?D.) Has this happened before?2. When obtaining a patient's history of an elderly patient,who can you rely upon to fill in the gaps?p. 183A.) BystandersB.) Medicine cabinet*C.) Family membersD.) Personal physician3. In which trauma patient would you perform a focused traumaassessment?p. 190A.) Significant MOIB.) Serious injury*C.) No significant MOID.) Is unresponsive4. Which situation usually will mean bleeding is <strong>com</strong>ing froma vein?p. 174A.) Dark red blood that is clottingB.) Bright red blood that is trickling*C.) Dark red blood that is flowingD.) Bright red blood that is spurting
5. What should be used to determine the condition of thepatient's skin?p. 189A.) Top of the forearmB.) Underside of the forearm*C.) Back of the handD.) Palm of the hand6. Where on the patient is the carotid pulse taken?p. 174A.) GroinB.) WristC.) Armpit*D.) Neck7. Which type of breathing will be seen when the patient isin shock?p. 188A.) SlowedB.) Wheezing*C.) Rapid, shallowD.) Deep, gasping8. Where should skin color, temperature and moisture beassessed when possible?p. 188A.) LegB.) StomachC.) Arm*D.) Forehead9. Which step is most often not needed on a trauma patientwhen there is no significant MOI?p. 178A.) Focused trauma assessmentB.) <strong>Patient</strong> history*C.) Detailed physical examD.) Vital signs
10. What may need to be done to check for suspected internalinjuries in an unresponsive patient?p. 192A.) Push with force over the areaB.) Take the patient's blood pressureC.) Wake up the patient with medication*D.) Remove clothing over the area11. When does your actual assessment of a patient begin?p. 170A.) Assessing the patient’s circulation*B.) Determining level of responsivenessC.) Assessing the patient's airwayD.) Forming a general impression12. What should be done to check for rib fractures in thetrauma patient?p. 194*A.) Gently apply pressure on the sides of the chest with yourhandsB.) Firmly apply pressure on the sides of the chest with yourhandsC.) Firmly apply pressure on the top of the chest with yourhandsD.) Gently apply pressure on the top of the chest with yourhands13. What should be done after baseline vitals have beenobtained for a trauma patient with no significantmechanism of injury?p. 159A.) Contact dispatch operator*B.) Detailed physical examC.) Chief <strong>com</strong>plaint examD.) Scene size-up14. Which is NOT always done for the focused history and examof a trauma patient?p. 161*A.) <strong>Patient</strong> historyB.) Physical examC.) Determine MOID.) Take vital signs
15. Which pulse must be checked before initiating CPR?p. 185A.) RadialB.) Brachial*C.) CarotidD.) Femoral16. What is performed based on the patient's chief <strong>com</strong>plaint?p. 157A.) Ongoing assessment*B.) Focused historyC.) Baseline vitalsD.) Detailed physical exam17. What is the normal range for the pulse of a child between5 and 12 years of age?p. 186*A.) 70 to 110 beats per minuteB.) 60 to 100 beats per minuteC.) 120 to 160 beats per minuteD.) 60 to 105 beats per minute18. Which is designed to trigger questions about what thepatient was doing when the pain began?p. 196A.) ProvocationB.) SeverityC.) Time*D.) Onset19. What can the patient do to allow you to evaluate themovement of the facial muscles?p. 192A.) GrimaceB.) Pout*C.) SmileD.) Stick out his tongue
20. What should be considered in a patient who has suffered afall?p. 166*A.) Spine injuryB.) Chest injuryC.) Arm injuryD.) Internal injury21. Which question in the bystander interview will a familymember be better able to answer?p. 183-184A.) Did you see anything else?B.) What happened?*C.) Does the patient take any medications?D.) Did the patient <strong>com</strong>plain of anything before this happened?22. Which pulse should be checked when the patient is NOTbreathing?p. 174A.) Femoral*B.) CarotidC.) BrachialD.) Radial23. Which is designed to determine what the pain feels like tothe patient?p. 197A.) Onset*B.) QualityC.) SeverityD.) Region or radiate24. What is the last step taken when performing patientassessment?p. 163A.) Detailed physical examB.) Ongoing assessmentsC.) Communication*D.) Documentation
25. Which of the following is NOT a usual place to find aMedicAlert medallion?p. 184A.) Neck*B.) WaistC.) AnkleD.) Wrist26. Who should be questioned when treating a patient with asevere mechanism of injury?p. 160A.) Dispatch*B.) FamilyC.) <strong>Patient</strong>D.) Other victims27. What amount of time should it take to perform the rapidtrauma assessment as a maximum?p. 191A.) Four minutes*B.) Two minutesC.) Three minutesD.) One minute28. What is the primary goal of the scene size-up?p. 163A.) ReconB.) <strong>Patient</strong> locationC.) Resource allocation*D.) Safety29. Where on the scale is the patient who is talking with you?p. 170A.) Painful*B.) AlertC.) UnresponsiveD.) Verbal
30. What should be looked for that would indicate the patientis in respiratory distress?p. 193*A.) Jugular vein distentionB.) Skull deformitiesC.) Facial bone fracturesD.) Impaled objects in the chest31. Which of the following conditions may pupils that reactsluggishly indicate?p. 193*A.) ShockB.) Drug usageC.) Brain injuryD.) Cardiac arrest32. Which aspect of the pulse is being described with normal,rapid or slow?p. 185A.) StrengthB.) Rhythm*C.) RateD.) Steadiness33. Almost what amount of a child's total blood volume can belost before blood pressure is affected by blood loss?p. 175-176A.) One-third*B.) One-halfC.) Three-fourthsD.) Two-thirds34. Which is your concern when checking for serious bleeding?p. 174*A.) Total amount of blood lostB.) Location of the injuryC.) Total time the patient has been bleedingD.) Speed of the bleeding
35. Which is important to note about an elderly patient'spulse?p. 174*A.) RateB.) Rate or regularityC.) Rate and regularityD.) Regularity36. Which type of breathing will be seen with an airway injurydue to heat?p. 188A.) Gurgling*B.) CrowingC.) WheezingD.) Snoring37. How may the skin present when the patient is sufferingfrom a diabetic emergency/p. 190A.) Hot, moistB.) Cool, moist*C.) Cold, dryD.) Hot, dry38. Which will be seen with stroke or a brain injury?p. 187A.) No pulseB.) Rapid, weak pulse*C.) Slow, strong pulseD.) Rapid, strong pulse39. What is the first rule of emergency care?p. 198*A.) Do no further harmB.) Conduct a head to toe examinationC.) Take vital signsD.) Watch the patient's skin for color changes
40. What is the bottom of the range of normal respiration ratefor an adult patient?p. 185A.) 7 breaths per minuteB.) 5 breaths per minute*C.) 8 breaths per minuteD.) 6 breaths per minute41. How many times the height of a pediatric patient wouldbegin to constitute a significant mechanism of injury?p. 178A.) Four to five times their heightB.) One to two times their heightC.) Three to four times their height*D.) Two to three times their height42. What should be the maximum amount of time it takes for thenail bed to be<strong>com</strong>e pink in color after being pressed?p. 175A.) 3 secondsB.) 4 seconds*C.) 2 secondsD.) 1 second43. Which should be done when you are treating a medicalpatient who is unresponsive?p. 177*A.) Rapid physical examB.) Focused physical examC.) Focused trauma assessmentD.) Rapid trauma assessment44. What should you do if you arrive and a person with ahigher level of training is caring for the patient?p. 167A.) Leave the sceneB.) Take over the case*C.) Offer to assistD.) Crowd control
45. Why is the age of a child important?p. 182A.) It may assist in contacting the parentsB.) It may make them more at ease with you*C.) It may determine the type of care givenD.) It may create a legal case46. What is indicated when the radial pulse is absent, but acarotid pulse can be found?p. 186A.) Heart attackB.) Stroke*C.) ShockD.) Diabetes47. Which is considered a subjective finding?p. 177A.) <strong>Patient</strong> historyB.) Signs*C.) SymptomsD.) Vital signs48. Which is the most useful distal pulse?p. 195*A.) Posterior tibial pulseB.) Anterior tibial pulseC.) Anterior popliteal pulseD.) Posterior popliteal pulse49. Where should you begin the rapid trauma assessment?p. 192A.) ChestB.) Waist*C.) HeadD.) Feet50. What would blood or clear fluid in the ear be a strongindicator of?p. 193A.) Cardiac injuryB.) Ear injury*C.) Skull fractureD.) Brain injury
51. What is your best source of information when examining amedical patient?p. 181A.) Family membersB.) BystandersC.) Medicine cabinet*D.) Alert patient52. What should you say to the patient after you haveidentified yourself as an Emergency Medical Responder?p. 167*A.) "May I help you?"B.) "Are you hurt?"C.) "Do you know where you are?"D.) "What happened?"53. Which term should be used when asking the patient aboutmedications they make be taking?p. 183A.) AssistersB.) Recreational drugsC.) Drugs*D.) Medication54. Which place on the scale is the patient who responds to aloud verbal stimulus from you?p. 170A.) AlertB.) Unresponsive*C.) VerbalD.) Painful55. What is the normal range of the pulse rate for an adult?p. 185A.) 80 to 120 beats per minuteB.) 70 to 110 beats per minuteC.) 50 to 90 beats per minute*D.) 60 to 100 beats per minute
56. What is the upper acceptable limit of rate of respirationin a child between six and ten years old?p. 188A.) 15 breaths per minuteB.) 50 breaths per minuteC.) 25 breaths per minute*D.) 30 breaths per minute57. What is the first thing on the neck that should be checkedduring the rapid trauma assessment?p. 193*A.) Cervical spineB.) Thoracic spineC.) Circle of WillisD.) Mandible58. With which type of patient may you be too involved innecessary patient care to perform a detailed physicalexam?p. 198*A.) Unresponsive medicalB.) Responsive traumaC.) Unresponsive traumaD.) Responsive medical59. Which does the medical patient rarely require?p. 179A.) Vital signsB.) <strong>Patient</strong> history*C.) Detailed physical examD.) Focused physical exam60. How often should seriously ill or injured patients bereassessed?p. 199A.) Every fifteen minutesB.) Every twenty minutesC.) Every ten minutes*D.) Every five minutes
61. Which pulse should be taken in an infant or small child?p. 175A.) Carotid*B.) BrachialC.) FemoralD.) Radial62. What should be NOT used to take the radial pulse?p. 186A.) Ring fingerB.) Middle finger*C.) ThumbD.) Index finger63. Which is an assessment of the patient's ABCs to detect andcorrect any immediate life-threatening problems?p. 161*A.) Initial assessmentB.) Detailed physical examC.) Focused historyD.) Rapid trauma assessment64. What should be used when inspecting the abdomen fortenderness?p. 194A.) Back side of the fingersB.) Knuckles of the handC.) Heel of the hand*D.) Palm side of the fingers65. What is the first thing the Emergency Medical Respondershould do once at the scene?p. 157A.) Focused history*B.) Scene size-upC.) Physical examD.) Initial assessment
66. What is the first thing that you do when performing theinitial assessment of the patient?p. 168A.) Assess the patient's airway and breathingB.) Make a decision on the priority of the patient fortransport*C.) Form general impression of the patientD.) Assess the patient's mental status67. What is the last thing that needs to be determined duringscene size-up at a trauma call?p. 164A.) Number of patientsB.) The mechanism of injury*C.) Additional resources neededD.) The scene's safety68. How should you press the pelvis to check for injuries?p. 194A.) In and up at the same time*B.) In and down at the same timeC.) In and then downD.) In and then up69. What will determining the MOI and NOI allow the EmergencyMedical Responder to do?p. 166A.) Initiate a medical evaluationB.) Diagnose the patient's illness*C.) Deal with up<strong>com</strong>ing <strong>com</strong>plicationsD.) Determine the cause of the issue70. Which of the following is NOT considered a significantmechanism of injury for an adult?p. 178A.) Falls greater than 20 feet (6 m)B.) Altered mental statusC.) Ejection from a vehicle*D.) Medium-speed vehicle collision
71. Which is a quick, less detailed head-to-toe assessment ofthe most critical patients?p. 176A.) MOI assessmentB.) <strong>Patient</strong> historyC.) Focused assessment*D.) Rapid assessment72. What should the Emergency Medical Responder be concernedwith after his own safety is ensured?p. 163A.) Safely identify and provide care for problems that areserious*B.) Safely detect and correct life-threatening problems in thepatientC.) Safely identify and provide care for problems that maybe<strong>com</strong>e seriousD.) Safely monitor the patient to quickly detect any changesin his condition73. What may be present in the elderly patient that can makeassessing mental status very difficult?p. 172A.) Diabetes*B.) DementiaC.) StrokeD.) Hearing loss74. What color is the skin when the patient is experiencingliver abnormalities?p. 189A.) PinkB.) BlueC.) Red*D.) Yellow75. What does the "B" stand for in BP-DOC?p. 191A.) BonesB.) BumpsC.) Burns*D.) Bleeding
76. What should be done while you watch the chest for movementwhen assessing breathing?p. 172*A.) Listen to the breathsB.) Talk to the patientC.) Take the pulseD.) Count the breaths77. What will the Emergency Medical Responder NOT try toac<strong>com</strong>plish with a patient?p. 157A.) Make the patient <strong>com</strong>fortableB.) Care for signsC.) Care for symptoms*D.) Diagnose the problem78. Which statement about conducting the focused physical examis NOT correct?p. 197A.) Do not put words in the patient's mouth*B.) Paraphrase the history when transferringC.) Use the patient's words during documentationD.) Provide the patient with choices79. What should you do if you find a guard dog on site at theincident?p. 165A.) Keep an eye on it while you workB.) Restrain the dog yourself*C.) Stay back until it is restrainedD.) Ask the patient to <strong>com</strong>e to you80. What does the "L" in SAMPLE stand for?p. 183A.) Limit of liability*B.) Last oral intakeC.) Light in the eyesD.) Level of pain
81. What is the last step of the patient assessment?p. 158A.) Scene size-upB.) Detailed physical exam*C.) Ongoing assessmentD.) Baseline vital signs82. How much time should determining breathing status take ata maximum?p. 174A.) 15 seconds*B.) 10 secondsC.) 20 secondsD.) 25 seconds83. What should be used to check for priapism in a malepatient when it is not obvious?p. 194A.) ElbowB.) Palm of your handC.) Forearm*D.) Back of your hand