Graduation World Tour 2009 - Ward Rounds - Northwestern University
Graduation World Tour 2009 - Ward Rounds - Northwestern University
Graduation World Tour 2009 - Ward Rounds - Northwestern University
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
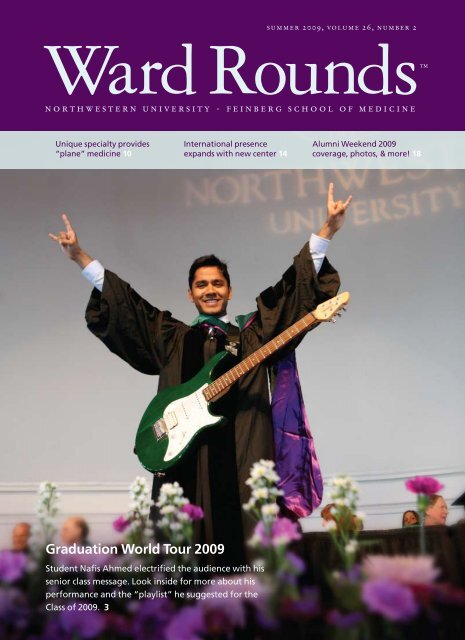
<strong>Ward</strong> <strong>Rounds</strong> NewsDean’s MessageWhat are the odds of becoming a U.S. astronaut?About one in a million with an even slimmer chanceof actually traveling in space, according to NASA.So <strong>Northwestern</strong> must have the magic touch. ThisMarch medical school alumnus Michael R. Barratt,MD ’85, GME ’89, arrived at the International SpaceStation, becoming <strong>Northwestern</strong>’s second astronautphysician,after Joseph P. Kerwin, MD ’57, to live andwork in space. In our first feature, we explore the specialtyof aerospace medicine—an area of expertise that started Dr. Barratt onhis path to becoming an astronaut.This year we launched a Center for Global Health that will help us developand share our strengths in clinical care, research, and education around theworld. In the second feature, learn more about the plans and goals of thisexciting new international enterprise under of the leadership of facultymember Robert L. Murphy, MD, GME ’84.At Alumni Weekend <strong>2009</strong>, former <strong>Northwestern</strong> students reconnected,reminisced, and “made history” with their old classmates and mentors at areunion event that celebrated the medical school’s sesquicentennial or 150thyear. In our third feature, we offer a photo album of the good times thatwere enjoyed this April and invite you to mark your calendar for AlumniWeekend 2010!Alignment, innovation, and impact continue to drive our strategic vision aswe help shape the future of medicine as leaders and innovators. In the finalfeature, we profile David Mahvi, MD, new chief of the Division of Gastrointestinaland Oncologic Surgery, who brings his expertise as a teacher, inventor,and surgeon to <strong>Northwestern</strong>.Best regards,MD degree gives gradsbackstage pass to lifeOn a warm spring day, excitement ran high as 167 medical studentsreceived their diplomas at <strong>Northwestern</strong>’s graduation convocationon May 14 at Chicago’s Navy Pier Grand Ballroom.This always momentous ceremony held extra special importanceas it marked the school’s sesquicentennial year.Proud parents, friends, and relatives gathered to snap photos,give pats on the back, and send out a few enthusiastic shouts asthe students filed into the ballroom.“We are absolutely thrilled to see this day come,” said AmyFinn, mother of new graduate Ian Finn of Boston, who was oneof 12 students graduating with dual MD/PhD degrees. “We aregrateful to the Feinberg School of Medicine for providing our sonthe opportunity for a bright future.”Dean Larry Jameson and <strong>Northwestern</strong> <strong>University</strong> PresidentHenry Bienen conferred the degrees and applauded the 150thgraduating class on their accomplishments. “Today you join theworld’s most respected and distinguished profession,” said DeanJameson. “You will find that your patients now refer to you asdoctor, even though some of them could be your grandparents.They trust you with their most precious possession: their health.<strong>Northwestern</strong> has prepared you well for this next chapter.”Class president Josephine Ni presented faculty member JamesJ. Paparello, MD, assistant professor of medicine in the Divisionof Nephrology, with the <strong>2009</strong> George H. Joost Award for teachingexcellence. She noted his unintimidating nature and ability toexplain complex concepts in simple terms.Keynote speaker and proud alumnus James R. Webster Jr.,MD ’56, GME ’64, told graduates that they have the best jobs intown with a degree that offers them “a backstage pass to life witha priceless opportunity to interact with human beings at the mostdifficult and delicate times of their lives, including literally lifeand death.” This professor of medicine and emeritus director ofthe medical school’s Buehler Center on Aging, Health, and Society,encouraged them to be agents of change whether it be to helpsolve the problems of the national health care system or affect the“behavioral choices that account for how long and how wellpeople live.”A geriatric medicine specialist, Dr. Webster went on toexplain that diet, exercise, and lifestyle choices play as large a rolein health outcomes as genetic makeup. He called on the graduatesto use their leadership skills and the new “bully pulpit implicit inJ. Larry Jameson, MD, PhDVice President for Medical Affairs andLewis Landsberg DeanAbove: Collegementor Dr. IrwinBenuck hoods newgraduate KaraGleason. Left: It isall smiles for KristinBerona and JeffreyBackes.2 ward rounds summer <strong>2009</strong>wardroundsonline.com 3
My Doctor is My CopilotHigh-flying specialty takes alums to great heights | By Cheryl SooHooThis year the medical schoolproudly celebrates its 150th birthdayhere on planet Earth. OnApril 16, alumnus Michael R. Barratt,MD ’85, GME ’89, also noted a significantmilestone—his big 5-0—220 milesabove Earth on the International SpaceStation (ISS) where he unfurled a purpleand white sesquicentennial banner inhonor of his alma mater.A NASA astronaut and flight engineerfor the Expedition 19 space mission,Dr. Barratt blasted off on March 26 fromthe Baikonur Cosmodrome in Kazakhstanaboard a Russian Soyuz TMA-14spacecraft. This first space flight for Dr.Barratt makes him the second medicalschool alumnus to live and work in space;on May 25, 1973, physician-astronautJoseph P. Kerwin, MD ’57, served onNASA’s first-manned Skylab 2 mission.Going boldly where still few havegone before, Dr. Barratt arrived at theISS thanks, in part, to his expertise inaerospace medicine. “I went into medicinebecause I liked working with people,”said Dr. Barratt in an oral historyproduced by NASA. “It was a relativelyHovering in military helicopters thesize of 15-passenger vans has givenflight surgeon Dr. Christine Stehmana heightened appreciation for theresponsibility she has to ensure thehealth and welfare of her squadron.broad field, but as I went through it, I realized that I’d liketo broaden out a little bit further, and started realizing thatthere was this entity called aerospace medicine, that I loveto fly and do a lot of other things that were outside of thenormal office routine.”A broad field in its own right, aerospace medicineinvolves the health, safety, and performance of personsengaged in air and space travel, according to the AerospaceMedical Association (AsMA). The extreme environmentalaspects of this specialty area require knowledge of theeffects of microgravity, radiation exposure, G-forces, andhypoxia, to name a few conditions, on the human body.While Dr. Barratt completed a “civilian” aerospacemedicine residency and master’s degree program at WrightState <strong>University</strong> in Dayton, Ohio, other specialists oftenobtain their training via the military where they haveaccess to flying personnel. For example, 38 percent ofAsMA’s membership of 3,000 has military ties. For thesmall, but significant, number of <strong>Northwestern</strong> alumniwho count themselves as aerospace medicine specialists,serving in the military began as a way to finance their medicaleducations and give back to their country. It has alsoallowed them to care for a high-flying patient population,ensure the safety of those involved in air and space travel,and offer general clinical services. Such has been the casefor three alumni of the medical school—featured here inthis <strong>Ward</strong> <strong>Rounds</strong> story—whose aerospace medicineexpertise gives new meaning to the “friendly” skies.Navy Lt. Christine R. Stehman, MD ’04, doesn’tspeak either of the two official languages ofAfghanistan—Pashto and Dari (EasternPersian)—but that didn’t stop her from volunteering torun an Afghan women’s health clinic during a recentdeployment. In March Dr. Stehman returned to the statesafter serving as the flight surgeon for a squadron of some300 Marines stationed on a NATO base outside of Kandahar.In addition to her assigned duties, she provided healthcare services to spouses and children of members of theAfghan National Army who were being mentored bycoalition forces.Explains Dr. Stehman, “They didn’t have a lot offemale health care providers to see these women who,because of cultural restrictions, aren’t allowed to take offtheir burkas in front of men.” Filling this void until a permanentfemale physician could take over the clinic, shehelped to raise awareness about the importance of improvingthe medical treatment of Afghan women.Dr. Stehman attended <strong>Northwestern</strong> on a Navyscholarship. After graduating from the medical school in2004, she completed a one-year internship at Naval MedicalCenter San Diego. At that point she was ready for oneof five operational tours, working either with undersea,shipboard, clinic, Fleet Marine Force (a branch of theNavy), or flying units. She chose flight surgery training—a combination of six months of specialty coursework andon-the-job experience—because it offered a skill set that10 ward rounds summer <strong>2009</strong>wardroundsonline.com 11
she felt would likely not come along once she traded theNavy for civilian life. In fact, this summer she left the military—althoughshe remains on active reserve—and startedan emergency medicine residency at Chicago’s StrogerHospital of Cook County on July 1.“We treat a relatively healthy population of peoplewho must stay in top shape,” explains Dr. Stehman abouther former job. Based at the Marine Corps Air StationMiramar, she cared for helicopter squadron personnel. “Ifsomeone is not paying attention or they do somethingwrong with a helicopter, a lot of people could die.”Dr. Stehman’s duties as a flight surgeon—a term fromthe past used for all military physicians even though mostwere and continue to be primary care specialists—focusedon general internal medicine concerns with a little preventivemedicine or orthopaedic work thrown into the mix.She also provided human-factors counsel for investigationsof aviation mishaps as well as advised commandingofficers on medical matters from grounding a pilot tosending a Marine home from a deployment. The “flight”in her title required that Dr. Stehman log time in the air.She flew as part of a helicopter crew. Describing the militarycopters she traveled in as hovering 15-passenger vans,she literally served as a backseat “flier.”Dr. James Oliver always had the greatestconfidence in fliers both in and outside of themilitary. “The pilots who fly commercial planesare absolutely fabulous,” says this AF colonel.“The one who recently landed the plane in theHudson River—that was beyond belief.”“The pilots in these helicopters can’t see beyond 3p.m. and 9 p.m.,” says Dr. Stehman. “The crew helps themwith seeing down and back.”While flying became very much a part of her job, Dr.Stehman enjoyed her military air travel due to the trust sheplaced in those whose health she oversaw. “I liked flyingwith my guys and doing what we did,” she says. “If youstuck me in a little Cessna, I don’t know how excited Iwould be about that.”The fighter pilot had recorded 3,000 hours flyingF-106 fighters. Capable of making sharp turns andpulling out of dives with ease, the F-106 was thego-to plane for “dogfights” in the air 50 or so years ago.One day assigned to fly an F-105 bomber, the pilot didwhat he had always done in the F-106—he dove towardthe ground at high speed. Unfortunately the sharp pullouthe expected didn’t occur.As the Air Force (AF) accident investigation boardtried to figure out how an experienced fighter pilot couldmake such a fatal error, it was a physician sitting on theboard who provided the answer. “I had been the flight surgeonfor a squadron of F-106 fliers so I knew how thoseplanes reacted,” explains Col. James H. Oliver, MD ’57,MPH, now retired and living in Upland, Indiana. “Theboard thought this pilot should have been able to pull theplane out of its dive but I asked, ‘Have you ever flown anF-105? If you had, you would have never tried a deep dive,expecting the plane to pull out of it quickly.’”In this case, the pilot paid dearly for his mistake. Yetfor Dr. Oliver, who helped analyze the human factorsinvolved in several accident board investigations duringhis more than 20 years of active duty in the Air Force, thisparticular incident didn’t follow the usual pattern. Rarelydid pilot error cause an aviation accident, according to Dr.Oliver, whose area of medical expertise gave him specialinsight into the world of aviation.Drafted into the military like many of his fellow physiciansat the time, Dr. Oliver chose aerospace medicinebecause he liked working with pilots and flying. “As aflight surgeon you are basically a general practitioner whocares for pilots and their families and periodically you getto fly on an airplane,” he says. “If the pilots feel you are a‘good guy’ you might even get to pilot the plane!”Dr. Oliver spent his first four years in the military as aflight surgeon stationed at Elmendorf AFB in Alaska. Hethen went on to an aerospace medicine residency at the<strong>University</strong> of California at Berkeley for one year and atBrooks AFB in Texas for another two years. Dr. Oliverlogged 1,800 hours of flight time during his career and flewin 27 different airplanes in which he often sat in the copilot’sseat. Stationed in Thailand during the Vietnam War,he flew some 50 combat missions in large helicopter gunships.Following the common practice of flight surgeons,Dr. Oliver took to the air not only to better understand thephysical stresses that flight places on pilots and passengersbut also, and most importantly, to strengthen patient-physicianrelationships. Close bonds help keep the lines ofcommunication open so that pilots feel comfortable discussingrather than hiding their health concerns. “Mostpilots are scared to death of doctors because they fearbeing grounded because of health reasons,” says Dr. Oliver.“You have the potential to ruin a pilot’s life.”In 1978 Dr. Oliver retired from the military althoughhe remains a “regular” officer and could still be called forduty. He went into private practice in preventive and generalinternal medicine first in Kansas and then Indiana andprovided Federal Aviation Administration (FAA)-required physicals for commercial and recreational pilotsas a certified FAA senior aeromedical examiner. He retiredfrom medicine in 2007.Dr. Oliver had the good fortune of combining twointerests—medicine and aviation—in a long and enjoyablecareer. He passed on the latter passion to son Bradley, nowan AF major and F-18 fighter pilot working at the Pentagonin Washington.When Jon M. Casbon, MD ’80, completed his familypractice residency at St. Joseph’s Hospital inPhoenix in 1984, it was time to pay back the AirForce for financing his <strong>Northwestern</strong> education.Although he completed training to become a flight surgeon,the Air Force had other plans. It first assigned Dr.Casbon to practice family and primary care medicine andthen steadily promoted him to leadership roles at bases inthe United States and Europe.Moving up in the ranks to his current position as anAF colonel stationed at Offutt AFB in Nebraska, Dr. Casbondidn’t practice aerospace medicine until August 2003when he became commander of the 89th Aerospace MedicineSquadron located at Andrews AFB in Maryland. Inthis role he led and directed some 160 military and civilianpersonnel in areas of aerospace medicine ranging fromflight medicine and bioenvironmental engineering to aeromedicalstaging for the reception and care of wounded soldiersreturning from Iraq and Afghanistan. He also got tosee a lot of “very important” people land and take off fromAndrews, home of the official U.S. presidential aircraftknown as “Air Force One.”“At Andrews I finally got to use the ‘wings’ I hadearned so many years before in flight surgery school,”remarks Dr. Casbon. “So in 2003 I had my first real exposureto the specialty and I decided, ‘Hey, I really like it.This is what I want to do,’ and that’s when I had mymidlife crisis!”So in 2005 at age 49, Dr. Casbon enrolled in the AirForce’s aerospace medicine residency program at BrooksAFB—one of only four accredited U.S. residency programsin the specialty. As part of the curriculum, he earnedan MPH degree at Johns Hopkins <strong>University</strong> in 2006. Ayear later he became board certified in aerospace medicineand then opted for a third year in his residency program toachieve accreditation in occupational medicine. Dr. Casboncompleted his training in July 2008 and moved on toAlthough he has served the Air Force for a quarterof a century, Dr. Jon Casbon had a “midlife crisis,”went back to school, and completed an aerospacemedicine residency in 2008.his next assignment as commander of the 55th MedicalOperations Squadron at Offutt AFB. In charge of guiding300 military and civilian personnel providing primary andspecialty care to 29,000 individuals, Dr. Casbon—ironically—doesnot have any aerospace medicine responsibilities.He does, however, serve as the base’s occupationalmedicine consultant in matters pertaining to flight medicineas well as traditional concerns of the specialty such ashearing protection, exposure to hazardous chemicals, andworkers’ compensation.“Aerospace medicine, like other specialties, has links topreventive as well as occupational medicine,” explains Dr.Casbon, who enjoys the epidemiological aspects of preventingdisease and reducing occupational hazards. “Aviator isan occupation, and there are many different types of aviationoccupations from flying to repairing planes.”In regard to his own career in aerospace medicine, Dr.Casbon is once again paying back the military for hisrecent graduate medical education. Although currently ina clinical role and not in charge of fliers, his situation couldchange. After all, in the past 12 years, he has moved every24 months to different AF jobs and bases. Says Dr. Casbon,who has already served 25 years in the military,“Well, the Air Force still has a commitment of a few moreyears from me due to my residency training, so you neverknow. I could get to use my wings in the future.”As Dr. Casbon and his fellow <strong>Northwestern</strong> alumnihave discovered, practicing the specialty of aerospacemedicine presents many opportunities outside the usualoffice environment that can take off at a moment’s notice.From flying off to the “wild blue yonder” to residing inspace as Dr. Barratt is now exploring, practitioners of thisunique area of medicine feel especially fortunate for theircolorful and exciting experiences—from below as well ashigh above the Earth’s atmosphere.wardroundsonline.com 13
Going GlobalNew Center for Global Health travels a two-way streetwhen robert l. murphy, md, gme ’84, plans, he plans big. but world-size strategyis required when you are the director of the medical school’s new center forglobal health and have been entrusted with the internationalization ofnorthwestern university feinberg school of medicine.Although the school has been involved in global healthresearch and education programs for students for manyyears, the new center coordinates current educationalefforts, provides more robust research opportunities, andmoves <strong>Northwestern</strong> into a larger arena.In his recent State of the School address, Dean J. LarryJameson described his goal to move the school’s ranking tothe top 10 of medical schools in the United States by 2020.Those premier academic institutions all have programs inglobal health. “<strong>Northwestern</strong> must go global if it is tobecome a major American university medical school,”says Dr. Murphy. That’s where his plan comes into play.Five years from now, he envisions a center that will bea substantial globally oriented enterprise with activeresearch and teaching components, including exchangesby Janet DeRaleauamong <strong>Northwestern</strong> faculty, partner faculty, and students.Additional faculty members and an increase in thenumber of grants and philanthropic support will anchorthe center. Add to that further development of relationshipswith partners in Africa and expansion to an Asiansite. In Europe, he sees the medical school partnering withselect universities, formalizing relationships with them,and establishing a <strong>Northwestern</strong> office in a major Europeancapital, probably Paris.Dr. Murphy, an internationally regarded infectiousdiseases physician, scientist, and educator, began his tenureat the medical school in 1981 and became John PhilipPhair Professor of Infectious Diseases in 2001. Hefounded the International AIDS Education Project in themid-1990s and continues as its director. In 2003 he wasappointed Nigeria country director for the President’sEmergency Plan for AIDS Relief (PEPFAR), and in 2008received the first of two Fogarty International ResearchCollaboration Awards from the National Institutes ofHealth. Dr. Murphy has gathered a group of medicalprofessionals with experience in global and public healthto lead center projects. Most have lived and worked inunder-resourced countries. They understand the culturesand have profound respect for the people. He calls themthe “troops.”Shannon R. Galvin, MD, the center’s associate directorfor research and assistant professor of medicine, hascome to <strong>Northwestern</strong> from the <strong>University</strong> of North Carolina(UNC)—home to an established global health center.While on staff at UNC, she lived and worked in thehospital wards in Lilongwe, Malawi. A poor country insouthern Africa, residents of Malawi suffer from widespreadfamine as well as high rates of HIV and child mortality.“The people are wonderful and friendly,” she says.“They make do with what they have. Children play withcars made of chicken wire and soccer balls made of rolledup bags.” This ingenuity is reflected in the Malawian HIVtreatment program, she notes, which has started thousandsof people on HIV medications in a very resource-constrainedsetting.The center’s director for African Research, BabafemiO. Taiwo, MD, a native of Nigeria, came to <strong>Northwestern</strong>five years ago as a fellow in infectious diseases. Now anassistant professor of medicine, his focus will be on HIVresearch and related problems such as hepatitis, tuberculosis,and malaria. Within the Division of Infectious Diseases,he will oversee two HIV research-related grants: theFogarty and PEPFAR. Dr. Taiwo brings a “bidirectionalperspective,” he says, achieved by having trained andworked in both Nigeria and the United States. Dr. Taiwonotes, “Having staff with diverse backgrounds enhancesthe center’s credibility to its mission of trying to engage aglobal community.”Words like “bidirectional” and “bilateral” help guidethe global health center’s mission and goals. Global healthcare in Dr. Galvin’s mind means encouraging medical studentsand faculty and those of partnering countries to domuch more than pass each other coming and going likehighway traffic. “It’s more about having a sense of whatyour partner country is capable of achieving and listeningto the people—your colleagues—when they tell you whatthey need,” she says. Dr. Murphy agrees. “The concept ofpeople from the United States and elsewhere going to poorcountries, doing studies, and writing reports is long gone.Whether it’s us going over there and doing some training forthem or them coming here and getting training and thengoing back, it’s a two-way street in the global setting.”Oche Agbaji, MD, co-principal investigator of thePEPFAR grant based in Jos, Nigeria, exemplifies thedirection the center is taking. Although a highly competentphysician, Dr. Agbaji required training in the basics ofclinical research such as drafting protocols and manuscriptwriting. Through a Fogarty grant, he recentlyspent one month in this country, two weeks of whichwere spent studying at <strong>Northwestern</strong> and the <strong>University</strong>of Chicago. “It’s important to understand that weare from two different parts of the globe in terms ofdevelopment and issues,” he remarks, “but there arethings we can gain from each other.”Adding a unique twist to the makeup of the centerare pharmacologists Kimberly K. Scarsi, PharmD, MSc,research assistant professor of medicine, and KristinDarin, PharmD, research associate. Both will play majorroles in training Nigerian and other African medicalprofessionals in the use of HIV medication, includingunderstanding side effects, drug interactions, and theprinciples and implementation of pharmacokinetic studies.Dr. Scarsi first worked internationally when shetraveled to Botswana in 2005. A trip to Nigeria cameAbove: Successful global medicine efforts require the expertise ofhealth care professionals around the world such as Remi Olaitan,chief pharmacist for the PEPFAR-Nigeria program, shown hereshopping at an outdoor market in Lagos.Below: Research is an important component of the new Center forGlobal Health led by Dr. Robert Murphy. He stands outside of theJohn R. Flanagan Biosafety Level-3 Laboratory, the largest highcontainmentvirology laboratory of its kind in Chicago.14 ward rounds summer <strong>2009</strong>wardroundsonline.com 15
shortly thereafter. She feels that the center staff’s practicalexperience in resource-limited countries helps themquickly assess what is practical and what is not. “How doyou deliver health care when there is no running water,electricity, or doctors?” she asks, pointing out that she andher center colleagues have already faced these questionsand found answers.She describes a typical clinic scene as a mass of people,who patiently wait for hours to be seen. “When you cometo the clinic in the morning 100 to 200 patients are waitingfor you,” she describes. “Not only are they sitting in avery warm room not complaining, but they also are gratefulthat they are able to obtain this quality of health care.”Dr. Scarsi’s respect carries over to the in-country healthcare workers, too. She was grateful to meet these clinicianswho work without complaint until every last patient hasbeen seen. “Here we work from the heart, not for themoney,” she recalls one Nigerian pharmacist telling her.Giving Backto the <strong>World</strong>Robert J. Havey, MD ’80, GME ’84, and his associates atChicago Lake Shore Medical Associates (CLSMA) havecome up with a unique way to give back—to the world.Through solicitations to their patients, they’ve raised morethan $230,000 in support of the new Center for GlobalHealth. This fundraising has made it possible for 63 studentsto visit several different sites, including Bolivia,Jamaica, Nicaragua, and South Africa. Their Global HealthInitiative fund provides financial support to <strong>Northwestern</strong>medical students who would like to travel to underresourcedclinics around the globe to further their education.Through flyers in the waiting room, postings on theirweb site, and an annual fundraising event, CLSMA offersits patients an opportunity to provide charitable supportthat will make a difference in both global health care andthe future of primary care medicine.Playing integral roles in the development of the new center are (fromleft), Dr. Kimberly Scarsi, Adam Koon, and Drs. Babafemi Taiwo,Shannon Galvin, Baiba Berzins, and Kristin Darin.“We are helping the people of our community and thatis all anyone can hope for in a career.”What started in 2005 as six sites in Nigeria has grownto 35, making personal visits to each site prohibitive in thetypical 10- to 12-day visits conducted throughout the year.Now Drs. Scarsi and Darin focus on more “central training,”where staff from each of the sites attend a trainingsession in a central location and then take the knowledgeback to their clinics.The center’s plans also include hiring an administratorto manage travel arrangements, visas, and grants, as well asan assistant director to coordinate all activities.Medical students have served as one of the biggestmotivators for the establishment of the Center for GlobalHealth. Today’s students enter <strong>Northwestern</strong> having traveledextensively and expect such opportunities as part oftheir continuing education. Medical student SaraPatrawala from Rochester, New York, for example, studiedin Germany while working on her undergraduatedegree in environmental sciences at <strong>Northwestern</strong>. Lastyear she spent eight weeks in India working on a project:she compared obstetric perspectives between patients in afree clinic for the poor versus one that served a more affluentpopulation.In addition to student interest, all physicians increasinglyrequire knowledge of global diseases as the worldbecomes a smaller place. Consider that the acronym AIDSrequires no explanation anywhere in the world. The diseasenot only influences the physical health of people but alsohas impacted total economies and upset the balance ofpower politically. Today global health issues play a role inthe practice of every physician whether he or she practicesin Cairo, Egypt, or Cairo, Illinois.Russell G. Robertson, MD, chair of the Departmentof Family and Community Medicine, serves as associatedirector of education for the center. Three existing departmentprograms will serve as the framework for studenttravel experiences. Students can choose from programsoffered by the Office of Medical Education (OME), theOffice of International Program Development (IPD), andthe Office of Global Health Education and CommunityServices (GHECS), explains Adam Koon, MPH, whohelps coordinate global health education for the center.Koon has traveled to under-resourced countries as part ofhis MPH studies. He recently joined <strong>Northwestern</strong> fromEmory <strong>University</strong>.Those interested in traditional study experiences inEurope and other developed countries can choose from anumber of formal affiliations offered by OME, includingprograms in Japan, Taiwan, France, Sweden, Germany,and the Czech Republic. If students desire an establishedcurriculum with formal rotations in China, Uganda, SouthAfrica, or Mexico, they can take advantage of IPD offerings.Finally, through an affiliation with the HeartlandAlliance for Human Needs and Human Rights, GHECSoffers clinical internships in Mexico and Guatemala thatrun from four to eight weeks. These shorter jaunts typicallyinterest students completing their early years of medicalschool and looking for summer experiences. Oftenfourth-year students hoping to complete their electivesabroad will work in clinics where there is a strong <strong>Northwestern</strong>faculty presence.Recalling her senior year experience, Elizabeth K.Wolf, MD ’08, spent one month in Palacios, Bolivia, lastyear completing a family medicine rotation in a rural clinicremotely run by medical school faculty member Mark E.Molitch, MD, professor of medicine. “I saw unusualconditions such as Chagas disease,” recalls Dr. Wolf,“a parasitic ailment that I would never have seen in theUnited States.”The Department of Family and Community Medicinealso administers two different scholarships tosupport student travel through affiliated and unaffiliatedprograms at <strong>Northwestern</strong>. Recipients of the Ken andRuth Davee Scholarship as well as the Global HealthInitiative funding (see sidebar on opposite page) conductprimary care rotations and community health projects indeveloping countries.Students often seek global health opportunities fortwo reasons: a cultural and/or educational experience or towork on a project. Both have merit. Students in the firstgroup typically shadow physicians and “see what healthcare is like in another setting,” explains Dr. Murphy, addingthat such an opportunity can be the beginning of asocial consciousness that may lead to a different careerpath later in life. Those seeking project-related experiencesvisit a location where medical professionals need an extrapair of hands to manage data, help in a lab, or perhaps evensee patients under the supervision of a licensed physician.The center has already set up some of these projects inSenegal, Malawi, Nigeria, Uganda, Kenya, and Tanzania.Despite the medical school’s enthusiasm and support,the center will clearly need to focus its efforts to become asuccess, according to Dr. Murphy. Building sustainablereciprocal relationships takes time. He sees little expansionin Latin America or Africa beyond <strong>Northwestern</strong>’s presentpartnerships. Asia, however, is wide open, particularlyVietnam and Cambodia. On the European front, Dr. Murphylooks forward to a growing relationship with France’sPierre et Marie Curie <strong>University</strong>–Paris, which ranks 39thout of the top 50 universities in the world.Multifaceted, the center also serves as a testament tothe school’s objective of providing volunteer medical servicesand relieving human suffering. Emphasizes Dr. Murphy,“Our mission in global health care is to help as manypeople as possible and to answer the important medicalquestions relevant to the people of the world.”In Botswana native dancers welcomed members of the PEPFARprogram, including Drs. Murphy, Scarsi, and Darin, who attended theglobal group’s annual tri-country meeting involving Nigeria,Tanzania, and Botswana.Learn more about the new Centerfor Global Health!Visit <strong>Ward</strong><strong>Rounds</strong>Online.com today!16 ward rounds summer <strong>2009</strong> wardroundsonline.com 17
Making HistoryAlums reconnect at one very historic alumni weekendA reunion event unlike any other, Alumni Weekend <strong>2009</strong> celebrated not only milestone reunionyears for <strong>Northwestern</strong> medical as well as physical therapy (PT) graduates but also the medicalschool’s 150th anniversary. Nearly 700 medical alumni, faculty, students, guests, and staffparticipated in 31 events that featured a special bus tour of Chicago sites significant in the historyof the medical school. The Department of Physical Therapy and Human Movement Sciencesmoved its usually scheduled fall Alumni Weekend to spring to join in on the festivities. Sixty-eightPT alumni and guests participated in their department’s reunion activities, which included theSesquicentennial Ball held at the Ritz-Carlton hotel. A <strong>Ward</strong> <strong>Rounds</strong> Alumni Weekend photoalbum is worth many more words and photos than we can print here. So please enjoy thesememorable snapshots and make your plans for next year’s reunion. For more unforgettableAlumni Weekend moments, check out www.wardroundsonline.com.36: Dr. Mary Jadhon Cunningham(’84) and husband Josephtraveled from their home inManlius, New York, to participatein Alumni Weekend.7: A campus tour of the NikonImaging Center holds the attentionof (from left) Drs. SanfordElton (’59), Bud Miller (’59),Ralph Baehr (’59), and JamesMonge (’55).8: Nathan Davis, the great-greatgreat-grandsonof founderDr. Nathan Smith Davis, signs<strong>Northwestern</strong>’s “charter” at, fittingly,the Nathan Smith DavisClub reception.11: Dean Larry Jameson (left)congratulates this year’s DistinguishedAlumni Award recipient,Dr. David Skorton (’74).4 562: Alumni Weekend was a familyaffair for (from left) Dr. SharonKrejci Mowat (’99) and herparents, Drs. James Krejci andCharlotte Kutsunai (’59).23: From one Medical AlumniAssociation leader to another,outgoing president Dr. BonnieTyplin (’74) passes the traditional“tie” and gavel to incomingpresident Dr. F. DouglasCarr (’78) at the reuniondinner-dance event.4: Dr. Laura Gordon (’82)returns to the medical schoolafter enjoying one of the weekend’sChicago tours.7 85: Longtime Class of 1959representative, Dr. Paul Urnestakes a moment to catchup with a friend at theSesquicentennial Ball.18 ward rounds summer <strong>2009</strong> wardroundsonline.com 19
9We have more photosfrom Alumni Weekend!Visit us online at www.wardroundsonline.com1213610: PT alums reconnecting atan Alumni Weekend researchposter presentation include(from left) Tim Hennum (’99),Bill Condon (’99), and Tim’swife Leanna Hennum (’98).11: Future medical alums fromthe Class of 2012 (from left)Nitin Yerram and LauraMatthews experience reunionfun with third-year studentMartin Pham.141012: Dr. Richard Boronow (’59)and wife Kathryn warm upthe dance floor at theSesquicentennial Ball.13: Happy 150th anniversary,<strong>Northwestern</strong>!14: A State of the School presentationgave alumni an updateabout their alma mater.1511Class of 19599: Front row: Meryl Haber, Glenn Faith, Martha BrooksWhitworth, Harvey Doorenbos, Theodore Greenlee, andRichard Boronow. Second row: William Rossing, KeithPetersen, Mary Ann Smith Frable (GME ’64), Joel West,Paul Urnes, Kathryn Davis Mahaffey, Sanford Antin, andPaul Bubala. Third row: Lee Rogers, Leonard Young, JohnRomine, George Kaplan, Richard Blonsky (GME ’63),Nancy Cheney Jeffrey (GME ’62), James Lindsey (GME’64), and Barbara Bear. Fourth row: Joseph Carey, MichaelMiech, Ralph Berggren, Richard Mladick, Marshall Cherkas,Sanford Elton, Barry Rubin, August “Bud” Miller,and Charlotte Kutsunai. Fifth row: Frank Stuart, WillardFry, W. Max Cloud, Robert Heyburn, Robert Lindberg(GME ’60), Gerald Berkowitz, Peter Van Vliet, JackFrable, and Terry Dynes. Last row: Henry Head (GME’65), David Criswell, Robert Richter (GME ’65), RalphBaehr, and Preston Dilts.15: Students Kevin Day andNourolhoda Birouti intentlylisten to Dr. Charles Modlin(’87) at an alumni-student mentoringluncheon held duringthe reunion weekend.join us next year!ALUMNI WEEKEND 2010APRIL 9–1020 ward rounds summer <strong>2009</strong> wardroundsonline.com 21
teacherinventorsurgeonConsummate academicianDavid Mahvi leads divisionBy Michael NyquistInnovation remains vital to advancing surgicaltechniques. For Dr. David Mahvi, invention comesas naturally as performing surgery and teaching thetools of his trade as the medical school’s chief ofgastrointestinal and oncologic surgery.The tools and techniques of surgical oncology evolverapidly. “We now do some pancreatic surgery laparoscopically,”says David M. Mahvi, MD, chief of theDivision of Gastrointestinal (GI) and Oncologic Surgery.“There wasn’t even a laparoscope when I was in residencytraining.” Dr. Mahvi, James R. Hines, MD, Professor ofSurgery, who joined the medical school and <strong>Northwestern</strong>Memorial Hospital (NMH) last July, has played a prominentrole in designing devices to ablate, or destroy, tumorsin abdominal organs. He and colleagues at his former institution,the <strong>University</strong> of Wisconsin-Madison (UW), holdseveral patents for such devices. One, a multiprobe microwaveablation system, has been used in clinical practicesince 2006.For more than a decade energy-based therapies, such ascryoablation and radiofrequency (RF) ablation, have supplementedor replaced tumor resection via the scalpel—the gold standard for removing tumors. These technologieshave made such operations minimally invasive and faster.“Each approach has its strengths and weaknesses,” says Dr.Mahvi. “Cryoablation usually works just fine, but earlyon, there were some complications in using it on the liver.As the tissue thawed, it would crack, and you’d get lots ofbleeding. RF ablation works, but the tumors tend to recurabout 20 percent of the time.”With the early use of both types of ablation, complicationrates were higher in larger tumors and in those nearmajor vasculature. A “heat sink” effect that raised or loweredthe temperature at the margins of the tumor allowedsome malignant cells to survive freezing or burning.Attempting to improve on these therapies, Dr. Mahvi andbiomedical engineer John G. Webster, PhD, at UW, conductedsome early work with microwaves in animal models.Microwaves heat tissue faster to higher temperatures,which reduces the heat sink effect because less time is availablefor blood flow to carry the heat away. But becausethese approaches are so new, evaluating their effectivenessis a “moving target,” according to Dr. Mahvi.Dr. Mahvi’s research in this area continues with his UWcollaborators, focusing on liver, pancreatic, and metastaticcolorectal cancers. “David is a world-renowned authorityin complex tumors of the hepatobiliary-pancreatic tract,”says Nathaniel J. Soper, MD, Loyal and Edith Davis Professorand chair of surgery. “Our plans include enhancingprograms and services in that field as well as expanding thescope of services in GI oncology generally. David is a personof great intellect and integrity, who works well withpeople across disciplines.”Dr. Soper, a GI surgeon, knew Dr. Mahvi through variousnational organizations. For the Society for Surgery ofthe Alimentary Tract, Dr. Mahvi serves as president-elect.“This is probably the most prestigious GI surgery organizationin the U.S.,” says Dr. Soper. “His nomination to bepresident is a tribute to his accomplishments. It’s a realfeather in our cap that we could recruit him here.”Dr. Mahvi enrolled at the Medical <strong>University</strong> ofSouth Carolina in Charleston as an MD/PhD studentin pathology in the late 1970s. However, duringhis required surgical rotation, “I found I had no interestin doing anything but surgery,” he recalls. “I was excited toget up in the morning and go to the OR.” The decision toswitch was easy, but the conversation with his respectedpathology mentor was not.Despite the specialty change, he was still committed toconducting research. So he searched for the best surgeryprograms that also required research training. He choseDuke <strong>University</strong> Medical Center in Durham, North Carolina,where he completed a general surgery residency and atwo-year research fellowship in tumor immunology from1981–89. That same combination of clinical surgery andresearch drew him to UW’s Section of Surgical Oncology.Dr. Mahvi remarks, “It was exactly the right environmentfor starting my career.”Julian C. Schink, MD, GME ’86, today professor ofobstetrics and gynecology and chief of the Division ofGynecologic Oncology at <strong>Northwestern</strong>, met Dr. Mahviat UW. “David and I collaborated on patient care and gotto know each other well,” says Dr. Schink, who had joinedthe UW faculty in 1992. “In our world of multidisciplinarycare, he’s someone whose judgment I absolutely trust. Hesees the big picture quickly and takes care of surgical issueswith an economy of motion and emotion.”22 ward rounds summer <strong>2009</strong> wardroundsonline.com 23
They also worked together on clinical research andadministrative duties for UW and its cancer center. “I wasexcited to see him come to <strong>Northwestern</strong>,” continues Dr.Schink. “David always puts patients first, with science andeducation as top-tier priorities. He appropriately delegatesresponsibility, expects excellence, and leads by example.”Dr. Mahvi directed the general surgery residency atUW from 2000–08 and twice won the top residency teachingaward (1998 and 2003). “Teaching is a blast,” he says. “Ialways like having graduate students, residents, and juniorfaculty around. They bring energy and fresh perspectives—Inever look at teaching as a one-way interaction.”Dr. Mahvi hit the ground running when he arrived at<strong>Northwestern</strong>. In his first winter quarter, he taught studentsin NUvention, a course jointly run by the business,engineering, law, and medical schools that focuses onproduct development and licensing. Much to the students’benefit, Dr. Mahvi gladly shared his practical experienceand expertise. As soon as he arrived on campus, he startedworking with surgical residents. Says Dr. Soper, “Severalresidents in their last years of surgical training have told methat the experience on Dr. Mahvi’s service was the best onethey’ve had in their entire residency. That’s remarkablegiven the short time he’s been here.”<strong>Northwestern</strong> emphasizes general surgery training,rather than specialized fellowships, for a good reason:nearly 80 percent of U.S. surgical residents do not feelcomfortable going directly into practice after five years ofgeneral surgery training. Explaining the medical school’sDr. Mahvi enjoys sharing his research interests aswell as his clinical ones with surgical residents suchas Dr. Ashley Hardy.approach to this challenge, Dr. Soper says, “We limit thenumber of fellowships to provide opportunities for surgicalresidents to work on the most diverse, complex general surgerycases. In the future, as the caseload increases, we mayadd a few highly specialized fellowships in strategic areas.”To provide general surgery residents with cross-disciplinaryresearch experiences, Dr. Mahvi is writing a traininggrant application with Terrence A. Barrett, MD,professor of medicine and chief of the Division of Gastroenterology,to more closely align research training in theirspecialties. “We want GI surgery and gastroenterologyeducation to become one, instead of differentiating thembased on who’s a surgeon and who’s a gastroenterologist,”explains Dr. Mahvi. “We work together in caring forpatients and conducting research, and we have many trainingopportunities at <strong>Northwestern</strong>.”Dr. Mahvi’s research focus changed dramatically fromNational Institutes of Health-supported basic sciencestudies of tumor immunology and relatedgenetic therapies earlier in his career. “That line of workran into regulatory problems because of the death of aresearch participant in a non-cancer clinical trial at the<strong>University</strong> of Pennsylvania in 1999,” recalls Dr. Mahvi.“Gene therapy research was shut down completely for twoyears in the U.S., and we had to redo all our protocols.That set us back so far that it was pretty discouraging.”He was also conducting clinical research on cryo- andRF ablation, including projects with Dr. Schink. Anotheropportunity in the mid-1990s with a spine surgeon introducedDr. Mahvi to three-dimensional computer modelingand other engineering techniques applied to designing surgicaltools and procedures. Although this work took himoutside of his patient care skill set, he found the engineeringaspects straightforward and fun. He and his colleaguesended up helping a company design laparoscopic tools toaccess the spine.“David Mahvi has a great appreciation for what engineerscan do,” says John G. Webster, PhD, professor emeritusof biomedical engineering at UW, who has beencollaborating with Dr. Mahvi on energy-based ablationtools since 2000. “He wrote a big grant with us thatallowed me to recruit electrical engineering PhD studentsto do the work on tumor ablation.”The inventive process starts with Dr. Mahvi describingthe clinical problem. “We might propose 10 solutions,”says Dr. Webster. “Then he’ll tell us why nine of themwon’t work, and we’ll build the 10th one.” Dr. Mahvi triesout the new tools in porcine models.One such project aims to improve liver tumor resection.“If you have a tumor near the end of a lobe, you canjust cut it off and the lobe grows back,” says Dr. Webster.“But the surgery takes about an hour and may includeexcessive blood loss. We came up with something like arake that penetrates through the edge of a tumor. Then yourun electricity sequentially through pairs of tines and cauterizea plane through there. You cut away what’s outsidethat plane and it doesn’t bleed.”“It’s cool when it works the way we want it to,” addsDr. Mahvi. “It’s not quite there yet.”Using computer modeling requires inputting numerousparameters to make the simulation as accurate as possible.For example, normal liver and liver tumor tissues havedifferent electrical characteristics. Due to his large surgicalcaseload, Dr. Mahvi can send his fellow researchersmany different tissue samples so they can make thenecessary measurements.Because this work is supported by federal funds, patentsfor tools ready for human clinical trials are given tothe Wisconsin Alumni Research Foundation—the technologytransfer operation for UW. The researchers haveno proprietary interests in the final product that reachesthe market.Dr. Mahvi also has a federal Small Business InnovationResearch grant for another microwave ablation projectwith a collaborator at his medical school alma mater.“Attracting federal funding validates your work. People inyour field believe your idea is valuable enough to support,”says Dr. Mahvi. He adds with a grin, “However, it’s kind ofmiserable writing grants all the time.”At <strong>Northwestern</strong> Dr. Mahvi has already made immediatecontributions to organizing multidisciplinaryclinical care teams. He helped revamp the bariatricsurgery service that resides in surgical oncology, directedby Alexander P. Nagle, MD, GME ’03, assistant professorof surgery. By fostering a more collaborative service, Dr.Mahvi feels they have streamlined the patient care experience.He shares, “The service received a Center of Excellenceaward from the American Society for BariatricSurgery, so the surgeons are good at what they do. We’vejust enhanced the structure so that they can be even better.”He was also instrumental in developing the new PelvicHealth Center at NMH, codirected by Janet E. Tomezsko,MD, assistant professor of obstetrics and gynecology andhead of the Section of Urogynecology; Anne-Marie Boller,MD, assistant professor of surgery in Dr. Mahvi’s division;and John C. Hairston, MD, GME ’01, associate professorSurgical morbidity and mortality conferences provideDr. Mahvi and his colleagues with perfect opportunitiesto share ideas and foster collaboration in his divisionand department and across the <strong>University</strong> and beyond.of urology. “The team includes colorectal surgery, urogynecology,and urology,” explains Dr. Mahvi. “Someonewith a pelvic problem can walk in the door, have a completeworkup, and leave with a treatment plan the sameday. Previously, seeing those three specialists might take amonth.” NMH is building new space for the center, withcompletion expected later this year.“These initiatives are easy to achieve here because theschool and hospital leadership is terrific,” says Dr. Mahvi.“I feel the energy, and the potential is enormous.”That includes improving care for people withpancreatic cancer, a disease with a poor prognosis. “Manytumors have essentially been cured by chemotherapy orother methods,” says Dr. Soper. “Pancreatic cancer isnowhere near that. That’s why we need people like Dr.Mahvi and others at the Robert H. Lurie ComprehensiveCancer Center to specifically work on ways to treat thesetumors because we usually don’t find them until they’rerelatively advanced.”Dr. Soper expects Dr. Mahvi to expand his own personalpractice in surgery of the pancreas, bile duct, andliver and recruit more people to help in those areas. Anadmirer of Dr. Mahvi’s dry sense of humor and sense offun, Dr. Soper looks forward to more contributions fromthe new GI chief. He says, “Dr. Mahvi has demonstratedstrengths in research, education, and patient care that makehim an exceptional role model for those who aspire to beacademic surgeons.”And as some surgeons-in-training at <strong>Northwestern</strong>have already found out, Dr. Mahvi has enjoyed teachingthem as much as they have relished learning from him.24 ward rounds summer <strong>2009</strong> wardroundsonline.com 25
Alumni NewsPresident’s Messagealumni profileWhat happens in Vegas . . .comes to <strong>Northwestern</strong>Alumni awards honorcontributions, serviceThis year’s sesquicentennial celebrationshave given us a broad perspectiveon the dramatic changes that haveoccurred at the medical school. Thepresent day reflects an acceleration ofthis process at <strong>Northwestern</strong> and forour country. This nation’s electoratedemanded change last November, andhealth care will undoubtedly experiencesome changes these next severalyears. The national policies currentlyunder debate are not insignificant: insurance coverage, reimbursement,delivery system reform, information technologyadoption, workforce development. All are likely to undergo fundamentaltransformations. I am confident that <strong>Northwestern</strong> willadapt to meet these challenges and continue to provide our countrywith medical leadership. As alumni, we need to ensure thatthe medical school has the resources to offer a place for the bestand brightest.My own professional journey has provided me many opportunitiesfor change. For a young man raised on the high plains ofWyoming, <strong>Northwestern</strong> provided a unique urban experience forlearning. After postgraduate work on both coasts, I settled into atraditional internal medicine solo practice in Cody, Wyoming. Ispent the following decade practicing with a multispecialty groupin Billings, Montana, that later merged with the local hospital toform an integrated system with a regional presence. The call forleadership prompted me then to pursue a management degree andtransition into a full-time administrative role.After 27 years the medical landscape looks far different fromwhen I entered medicine, yet some say the change is not enough.We don’t know exactly what the future holds in health care orspecifically what shape it will take but, for whatever lies ahead,we are fortunate to have the tools for lifelong learning weobtained at <strong>Northwestern</strong> to guide us!All the best,F. Douglas Carr, MD ’78President, Alumni AssociationKeeping a low profile suits Las Vegas-based internist Stephen H.Miller, MD ’82, just fine. His accomplishments, however, andsome of his patients have gotten his name out before the public inways he hasn’t always anticipated.“About five years ago I got a call from my medical schoolclassmate Kenny Heiferman [MD ’82, GME ’88],” recalls Dr.Miller. “He said that he saw my name in People magazine. I wasquoted discussing the health of Roy [Horn of entertainment duoSiegfried and Roy].” In 2003 a tiger severely wounded the famedmagician during a show at the Mirage Hotel in Las Vegas. AsHorn’s longtime physician at that time, Dr. Miller provided hisexpert opinion on his celebrity patient’s prognosis.Since 1985 Dr. Miller has practiced medicine in Las Vegas,where he has built a diversified practice by coordinating physicalexams for the Nevada Federal Bureau of Investigation, conductingnumerous clinical drug studies, and developing strong andclose bonds with his patients. Some of these individuals, gratefulfor the care and personal attention Dr. Miller has provided them,also have boosted this medical school alum’s profile—especiallyat his alma mater.Although this native of Cleveland has only been back to theChicago campus once since graduating, Dr. Miller thought of<strong>Northwestern</strong> when one of his patients wanted to express hisgratitude through a generous gift. In 2006 Sidney Kramer, whopassed away earlier this year, helped to establish the Stephen H.Miller, MD, Scholarship with a $100,000 gift in recognition of Dr.Miller’s compassionate and excellent care. Since its inception, severalmedical students have benefited from the Miller scholarshipduring their first and second years in school.“I have a passion and great amount of respect for <strong>Northwestern</strong>,”says Dr. Miller, who is one of five siblings in his family of sixto become a physician. “It wasn’t a hard decision to direct thefunds to the medical school to support the education of students.”Other patients of Dr. Miller have also donated to the scholarshipfund, which has grown to about $120,000 to date. Dr. Millerhopes that one day the scholarship will cover a year’s tuition for asingle medical student.For a recent holder of the Miller scholarship, <strong>Northwestern</strong>’sinfluence on Dr. Miller lifted a weight off this now third-year student’sshoulders. “Receiving the scholarship meant that I didn’thave to try and work during my first two years of medicalschool,” shares Emily C. Zander of Cupertino, California, whoinitially had considered finding a part-time job. “[Not having towork] made it so much easier to focus on my studies.”Fortunately for Zander and other Miller scholars, includingthe current scholarship holder, Alexander Kieger, who just completedhis first year of medical school, what happened in Vegasdidn’t necessarily stay there thanks to one alum’s fond memoriesof his medical school days.Cheryl SooHooAlumni Weekend <strong>2009</strong> provided theperfect opportunity to recognize<strong>Northwestern</strong> alumni for their outstandingcontributions to medicine and societyat an awards presentation held at the sesquicentennialball the evening of April 25.Charles S. Modlin Jr., MD ’87,received the first annual Daniel Hale WilliamsAward for Meritorious Service toUnderserved Communities. A transplantsurgeon at the Cleveland Clinic, Dr. Modlinhas long had a passion for eliminatinghealth care disparities, expanding communityoutreach, and enhancing the healthcare and education of minority patients.Starting an annual Minority Men’s HealthFair seven years ago that now draws morethan 2,000 participants, he also is founderand director of the clinic’s Minority Men’sHealth Center in the Glickman Urologicaland Kidney Institute.The award that <strong>Northwestern</strong>bestowed upon Dr. Modlin bears thename of the medical school’s first AfricanAmerican graduate from the Class of1883. Dr. Williams, a pioneer surgeon,founded Chicago’s Provident Hospital—one of the first to welcome African Americanand other minority patients.The medical school’s DistinguishedAlumni Award went to David J. Skorton,Dr. Charles Modlin (right) becomesthe first recipient of the medical school’sDaniel Hale Williams Award.MD ’74, who has served as president ofCornell <strong>University</strong> since July 1, 2006. Anexperienced administrator, cardiologist,musician, biomedical researcher, andnational leader in research ethics, Dr. Skortonhoned his leadership skills at the <strong>University</strong>of Iowa (UI) where he joined thefaculty in 1980. In 2002 he was appointedvice president for research and externalrelations and was selected as UI presidentthe following year. While at UI, he continuedto study and play saxophone and fluteand hosted a weekly jazz program on theuniversity’s public FM radio station.Accepting his award at the podiumfrom Dean Larry Jameson, Dr. Skortonlooked out into the audience and asked,“Where are you, Class of 1974?” As hisclassmates cheered at a nearby table, heturned to them and said, “You reallyhelped me through school to first becomea doctor and then a bureaucrat. This is ahuge day for me, and it is wonderful to seeso many of my old friends.”Three other alumni were applaudedfor their service and contributions to theiralma mater. Lee F. Rogers, MD ’59,received the Dean’s Award, given for outstandingcontributions by an alumnus/afaculty member. Dr. Rogers served as professorand chair of radiology at <strong>Northwestern</strong>from 1974 to 1995. Alumniservice awards went to Walter W. Huurman,MD ’62, and Paul D. Urnes, MD ’59,who received the same honor in 1989.Out of this worldWhen astronaut Michael R. Barratt, MD’85, GME ’89, packed for his trip to theInternational Space Station (ISS) in Marchhe carried with him the essentials, whichincluded a special banner commemoratingthe medical school’s 150th anniversary.Dr. Barratt requested a “flyingmemento” from his alma mater in August2008. “I wish to take this opportunity tohonor my past involvement in yourschool,” he wrote in a letter to <strong>Northwestern</strong>.“I plan to unpack the item and takephotographs within the setting of the ISS,then return the item to you after the flight.”Carrying the purple and white bannerin his official flight kit, Dr. Barratt madegood on his promise by sending <strong>Ward</strong><strong>Rounds</strong> a photo from out of this world.On May 29 three new members joinedDr. Barratt and the crew of Expedition 19,who have been in space since March 26.This addition to the group marks thebeginning of Expedition 20 and six-personcrew operations. For the first time, all fiveof the international partner agencies arerepresented on the ISS. They are NASA,the Russian Federal Space Agency, theJapan Aerospace Exploration Agency, theEuropean Space Agency, and the CanadianSpace Agency.In addition to helping advance the ISS’mission of “extending the permanenthuman presence in space,” Dr. Barratt gotthe opportunity to watch on his laptopcomputer the new Star Trek movie. ParamountPictures transferred the movie—released in early May—to NASA’sMission Control in Houston, which thenuplinked the film to the space station,according to NASA.In an interview with <strong>Ward</strong> <strong>Rounds</strong> in2007, Dr. Barratt shared with readers thatone of his childhood heroes was Dr.“Bones” McCoy from the Star Trek televisionseries.Above: With planet Earth in the background,astronaut Michael Barratt displaysthe sesquicentennial banner speciallymade for his trip.26 ward rounds summer <strong>2009</strong>wardroundsonline.com 27
Alumni NewsRIC president and CEOhighlights hospital’spast, present, futureThe medical school’s not the only institutionon campus with a rich history. Providingan overview of the past, present,and future direction of the RehabilitationInstitute of Chicago (RIC), guest speakerJoanne C. Smith, MD, MBA, GME ’92,RIC president and CEO, spoke at theApril 25 meeting of the Alumni AssociationNational Board held during AlumniWeekend <strong>2009</strong>.Dr. Smith’s presentation followed theorganization’s progression from its humblebeginnings in a renovated warehouseon Ohio Street in 1952 to its present20-story flagship center on the <strong>Northwestern</strong>campus. Designated as the #1rehabilitation hospital in the country byU.S. News & <strong>World</strong> Report every yearsince 1991, the RIC’s evolution as theleader in physical medicine and rehabilitationhas reflected, in part, society’s changingview of people with disabilities.The RIC traces its roots back to PaulB. Magnuson, MD, former chair of theDepartment of Orthopaedic Surgery atthe medical school. Dr. Magnuson helpedestablish rehabilitation medicine as a specialtyafter <strong>World</strong> War II by founding thefirst school of physical therapy in thecountry at Wesley Memorial Hospital. In1952 the RIC was incorporated, and itsdoors opened two years later thanks to Dr.Magnuson’s successful fundraising efforts.“The steps are so interesting!” said Dr.Smith, showing the group of alumni boardmembers a photo of the first RIC buildingwhere patients entering the front doorsencountered an intimidating flight ofstairs. Beginning as an outpatient center,the facility eventually started taking inthose individuals who needed moreintensive care.The 1970s brought not only the creationof today’s RIC hospital on SuperiorStreet, but also a change in attitude towardindividuals learning to cope and live withdisabilities thanks to the leadership ofHenry B. Betts, MD, former chair ofphysical medicine and rehabilitation aswell as president and CEO of the RIC andchair of its foundation. Remarked Dr.Smith, “Our product back then was tograduate patients who became productiveand contributing members of society.” Formany decades Dr. Betts, who remains onfaculty as a professor of physical medicineand rehabilitation, and his patients lobbiednational and local government to allowgreater access and fewer societal barriers.Representative forthe Class of 1967Dr. Andrew Bunta(left) emphasizeshis point duringthe Alumni AssociationNationalBoard meeting,while board memberDr. WalterHuurman looks on.Dr. Joanne Smith shares her vision fora new RIC building that will allow theinstitute to expand its clinical andresearch initiatives.“We’ve come a long way,” said Dr.Smith, noting the flap over sprinter OscarPistorius’ tryout for the 2008 BeijingOlympics. Some argued that his two carbonfiber prosthetic legs gave him anunfair advantage. Today modern technologyhas allowed the creation of bionicarms, and now with robot-assisted therapy,patients can increase the frequency andduration of their therapy sessions toachieve greater and faster improvement andrecovery. Dr. Smith added, “Impossible isno longer a part of our medical lexicon.”Currently there are some 52 millionAmericans living with disability. As theU.S. population grows older and lives longer,the demand for advances in rehabilitationmedicine will increase substantially,according to Dr. Smith. Driven by thesedemographic as well as market forcesreshaping the field, the RIC plans to reinventitself with the creation of a newbuilding either on or near the medical centercomplex.Future expansion will allow for additionalcare discoveries based on the institute’sresearch initiatives. They will beinfluenced by new findings in bionic medicine,nanotechnology, brain-machineinterfaces, and the use of smart devices, toname a few. Dr. Smith shared that the RICof tomorrow will continue to meld thebest of clinical care with the best of science.As the hospital moves forward, itplans to support a wide range of clinical trials,measure outcomes, and innovate newstandards in care, among them a cuttingedgephysical plant that will allow laboratoriesto coexist with patient care to quicklybring scientific discoveries to the bedside.A written and videosummary of theDean’s <strong>2009</strong> State ofthe School Address isavailable online!Find expanded coverage of alumninews at <strong>Ward</strong><strong>Rounds</strong>Online.com.J. Larry Jameson, MD, PhD, vice presidentfor medical affairs and Lewis LandsbergDean of <strong>Northwestern</strong> <strong>University</strong>Feinberg School of Medicine, also spoke tothe group about the state of the school. Henoted that the nation’s economic downturnhas had an impact on the medical schooland that some belt tightening is inevitable.Dean Jameson has made scholarshipsand financial aid one of his priorities tohelp decrease student debt and give<strong>Northwestern</strong> a more competitive edge inattracting students. He also highlightedthe school’s move from 20th to 19th placein the May release of the <strong>2009</strong> U.S. News& <strong>World</strong> Report rankings. “The questionis whether this is a fluctuation or a trend,”said the dean, noting that the school hasheld steady at a ranking of 20 or 21 fornearly a decade. Sharing with the nationalboard the school’s goal to move into thetop 10 of medical schools by 2020, Dr.Jameson expressed some concern over theflattening of research dollars and itsimpact on <strong>Northwestern</strong>.In closing, the dean said that donationsfrom alumni provide a “key fuel forthe medical center,” but that activities suchas mentoring existing students and helpingto attract top students are also invaluable.Ginny Darakjian, assistant dean foralumni affairs, reported that this year’sAlumni Weekend was the best attended todate, with nearly 700 alumni, faculty, students,guests, and staff participating in 31events. During the reunion weekend,incoming alumni board president F.Douglas Carr, MD ’78, replaced Bonnie L.Typlin, MD ’74, with James A. Hill, MD’74, professor of orthopaedic surgery at<strong>Northwestern</strong>, becoming president-elect.The next meeting of the National AlumniAssociation Board will be held October 24.Janet DeRaleauProgress Notes Awards & HonorsIn May the MassachusettsMedicalSociety (MMS)honored Erwin A.Stuebner Jr., MD’70, of Williamstown,Mass., withits <strong>2009</strong> Award forDistinguished Serviceto the society.Recognized for his strong commitment tothe goals of the society, this retired physicianhas been a member of MMS’ board oftrustees and numerous committees andtask forces addressing such issues as pharmaceuticalgifts, hospital closings, andhealth care reform.Sharon Krejci Mowat, MD ’99, ofDanville, Calif., a pediatric hospitalist, waselected medical staff president of KaiserPermanente’s Walnut Creek Medical Centerin Northern California.In AprilMarleta Reynolds,MD, GME ’85,professor of surgeryat <strong>Northwestern</strong>,was appointedsurgeon-in-chiefand head of theDepartment ofSurgery at Children’sMemorial Hospital. Dr. Reynoldshad served on an interim basis in theseroles since last September.The <strong>University</strong> of Mississippi MedicalCenter named Richard C. Boronow, MD’59, of Brandon, Miss., an honorary physicianin 2008.Colby Shad Thaxton, MD ’04, PhD’07, assistant professor of urology at<strong>Northwestern</strong>, was named <strong>2009</strong>Researcher of the Year by Bioscience Technology.Announced in the magazine’s Mayissue, the award recognizes Dr. Thaxtonfor his research using gold nanoparticlesto develop new therapeutics for atherosclerosis.Dr. Thaxton and his team builtartificial nanostructures to mimic HDL,known as good cholesterol, and its cholesterol-removingproperties that take “bad”cholesterol, or LDL, deposits to the liverfor excretion.A. HerbertAlexander, MD’73, of Sun Valley,Idaho, received theJohn R. SealAward from theSociety of MedicalConsultants to theArmed Forces lastOctober inBethesda, Md. The award recognizes outstandingcontributions to military medicinethrough research and patient care. Dr.Alexander also serves as associate editorin-chiefof the American Journal ofOrthopedics.G. Klaud Miller, MD ’75, GME ’78, ofEvanston, Ill., was appointed associateeditor of the Journal of Arthroscopic andRelated Surgery. He has also passed theCertificate of Added Qualification inSports Medicine from the AmericanBoard of Orthopaedic Surgery. Dr. Milleris an assistant professor of clinical orthopaedicsurgery at <strong>Northwestern</strong>.The National Alliance on Mental Illnesspresented James M. Laster, MD ’69,MPH, of Virginia Beach, Va., with theExemplary Psychiatry Award during theannual conference of the American PsychiatricAssociation last year. This awardrecognizes psychiatrists who have “gonethe extra mile” in providing excellent clinicalcare and educating family members,consumers, and the public to reduce thestigma surrounding mental illness. Dr.Laster also received this honor in 1993.Diane E. Wallis, MD ’79, of DownersGrove, Ill., received the American HeartAssociation’s Go Red for Women Awardlast year. This program helps fundresearch, conducts public and professionaleducational programs, and advocates forthe protection of women’s heart health.Alexian Brothers Medical Center inElk Grove Village, Ill., named Daniel M.Sauri, MD ’99, of Chicago its 2008 Physicianof the Year.28 ward rounds summer <strong>2009</strong> wardroundsonline.com 29
Alumni NewsGuess who came to AlumniWeekend <strong>2009</strong>?Find out at <strong>Ward</strong><strong>Rounds</strong>Online.com.Send items for Progress Notes to ward-rounds@northwestern.eduor to the street address on page 32.Progress NotesCycling to eradicate malnutrition in Burma1944Robert E. Heerens, MD, of Rockford,Ill., continues in retirement to give healthtalks to seniors groups. During 2008 hegave 98 presentations.1950David E. Streitmatter, MD, GME ’51, ofDallas moved last year to an apartment inthe Presbyterian Villas North. He retiredfrom internal medicine in 1993 but stillenjoys taking advantage of CME opportunitiesand maintaining his licenses.1953Lester R. Dragstedt II, MD, of DesMoines, Iowa, is retired chief of surgery ofthe Des Moines VA Medical Center. Herecently celebrated his 80th birthday andone month later, his 50th wedding anniversary.Never one to sit still, he continuesto play indoor doubles tennis three times aweek, followed by playing bridge. Hewrites, “<strong>Northwestern</strong> was definitely theright medical school for me!”Simon K. Myint, MD, of New Hall,Calif., continues his volunteering ways. Sofar this year he has offered his services as avisiting surgeon in Mexico, Haiti, andNepal. He writes, “Still teaching medicalstudents at Charles Drew <strong>University</strong> ofMedicine and Science in Los Angeles. At81, I am not finished (yet)!”1959Harvey E. Doorenbos, MD, of Holland,Mich., enjoyed an interesting career thattook him to far-flung places. After trainingin general surgery, he served as a medicalmissionary in the Sultanate of Oman,which at the time had a traditional Bedouinculture. From there he worked inEthiopia during communist rule. Nowretired, he works eight months a year inhospitals in Kenya, Sudan, Malawi, Liberia,and India. Willard A. Fry, MD, ofWinnetka, Ill., a Francophile, is a memberof Mayor Daley’s Chicago Greetersprogram, meeting with French touristsvisiting the city. He also sits on theChicago-Paris Sister Cities Committee.Southwest alums catch up on alma materScottsdale, Arizona, provided a desert backdrop for a <strong>Northwestern</strong> Alumni Brunch heldMarch 8. Twenty-nine alumni and guests participated in the event, which featuredupdates about the medical center complex from medical school Dean Larry Jameson and<strong>Northwestern</strong> Memorial Hospital HealthCare President and Chief Operating Officer DeanHarrison. Dr. Jeffrey Glassroth, vice dean and chief academic officer, discussed medicaleducation and future changes in the curriculum at the medical school. Here Dean Jamesontakes the opportunity to spend time with alumni from the Class of 1958, Drs. PhilipScheerer (left) and Gene Laker.Theodore K. Greenlee, MD, of Seattle,associate professor emeritus of orthopaedicsurgery and sports medicine at the<strong>University</strong> of Washington, continues tocover surgery and clinics at the Seattle VAMedical Center. A member of the CoastGuard Auxiliary, he assists in boardingforeign freight vessels. Michael J. Miech,MD, of Long Beach, Calif., certainlyenjoys travel. He and wife Marilyn havebeen on more than 50 cruises—in Januarythey spent four weeks on the Queen MaryII. Richard Mladick, MD, of VirginiaBeach, Va., a retired plastic surgeon, keepsbusy boating, hiking, and traveling amongmany other pursuits. Never “bored,” hestill speaks at professional meetings.1960Theodore C. Rozema, MD, of Landrum,S.C., was invited by the Indian government’sDefense Research and DevelopmentOrganization last December tolecture at the International Conference onMolecular Mechanisms of Disease inGwalior. From there he gave a similar lectureat the International Conference onTranslational Pharmacology and the 41stAnnual Conference of the Indian PharmacologicalSociety. Back home, he conductsresearch in the Trial to Assess ChelationTherapy, which is funded by the NIH.1964Josephine T. Colbach, MD, of West Linn,Ore., is enjoying her third year of retirementafter 37 years in emergency medicine/urgentcare with NorthwestPermanente in the Portland area, whilehusband Edward M. Colbach, MD, continuesto practice psychiatry and serves asa clinical professor at Oregon Health Sciences<strong>University</strong>. Both history buffs andnature lovers, they spend their time reading,hiking, and working on their smalltree farm. Phillip W. Thieman, MD,MPH, of Montreal, Quebec, Canada,reports that he retired to Palm Springs,Calif.; New York City; Fort Lauderdale,Fla.; and Cape Cod before moving toCanada for his “final resting place.” Thisgeneral surgeon served in the Navy andwas an attending at Columbia-Presbyterianin New York. In 1978 he returned toactive duty as a commander surgeon andflight surgeon stationed in Iceland andthen in the states in Maine, Massachusetts,and New York.1979Irwin Benuck, MD, of Chicago, professorof clinical pediatrics at <strong>Northwestern</strong>,served as a college mentor to 43 of themedical students who graduated this May.Sandra A. Eisele, MD, MBA, of Cincinnatiproudly received her business degreefrom Notre Dame. It was “a wonderfulchallenge,” she writes.1981Christopher M. Rembold, MD, of Charlottesville,Va., professor of medicine incardiovascular disease at the <strong>University</strong>of Virginia, and his lab team have beenstudying the role of calcium, HSP20, andpaxillin in smooth muscle contraction andrelaxation. They are in their 22nd year offunding. He and wife Kristen Staby (BSJ’79) have two daughters: Karen is in herthird year at medical school at <strong>Northwestern</strong>,and Ingrid is studying history atMerton College of the <strong>University</strong> ofOxford in England.1988Mark K. Urman, MD, of Beverly Hills,Calif., was listed in the “Super Doctors”section of the December 2008 issue ofLos Angeles magazine, as one of the bestcardiologists in Southern California. Heis medical director of The Heart Centerat Cedars-Sinai Medical Center in LosAngeles.1989Edward J. Schloss, MD, of Cincinnatiqualified for and ran in the Boston Marathonin 2007. He will repeat the challengein <strong>2009</strong>. Dr. Schloss is director of cardiacelectrophysiology in the Ohio Heart andVascular Center at the Christ Hospital.1990Carolyn R. Stern, MD, of Rochester,N.Y., a family physician, is founder andpartner of DeafDOC.org, an organizationdevoted to building partnerships betweenthe deaf and hard-of-hearing community,interpreters, and health care providers. InBruce F. Scharschmidt, MD ’70, of San Francisco and his son, Brent, cycled fromCentral Thailand to the Burmese border in late March to raise money to improve thehealth of displaced people residing in Burma’s border areas. Their 10-hour “Biking forBurma” ride netted more than $17,500 to support a malnutrition program launched byBrent, a volunteer with California-based Planet Care/Global Health Access Program. Onedollar feeds a malnourished child for a day. The trip over mountainous terrain alsoinvolved “two flat tires and a kilogram of sunblock” during the Scharschmidt family’sjourney. Spouse and mom Peggy S. Crawford, MD ’73, followed by car.February Dr. Stern and other deaf healthcare professionals held a symposium forthe National <strong>University</strong> Corporation:Tsukuba <strong>University</strong> of Technology, sharingtheir educational and technologicalchallenges and successes.1992Rajneesh Agrawal, MD, of Las Vegas,Nev., a neuro-interventional radiologist,announced the birth of Audrey Rose inApril 2008. The family’s newest additionjoins siblings Alex and Anna Grace.1993Alisa A. Bromberg, MD, of Pacific Palisades,Calif., tells her classmates, “I reallywish I could have made our 15-yearreunion but our second baby was due theweekend before. Micah, now 8-1/2months, joins big brother Levy, 3-1/2years. Between private practice in pediatricsand raising two boys, we are busy.”1994Anita Khanna, MD, of Denver was marriedto Charles R. Caulson on February14. A longtime Coloradoan, Dr. Khannamaintains a private practice in adolescentand adult psychiatry. Elisabeth K. Shim,MD, of Los Angeles was named one of LosAngeles’ Super Doctors in 2008. A dermatologist,she has launched her own skin carecompany called Verdura; its sunscreen wasnamed one of the best new sunscreens of2008 by Allure and Lucky magazines.1999Sharon Krejci Mowat, MD, of Danville,Calif., this year celebrated her 10-yearmedical school reunion along with hermother, Charlotte Kutsunai Krejci, MD’59, of Diablo, Calif., who celebrated her50th. Lorena L. Shih, MD, and husbandThomas J. Walsh, MD ’00, report thatthey are delighted to have returned to“rainy Seattle” along with their toddlertwins, Gabrielle and Graham. Lorenajoined Pediatric Associates, a private pediatricpractice, and Tom is an assistant professorin urology at the <strong>University</strong> ofWashington. Shelly Vaziri-Flais, MD,GME ’02, of New Lenox, Ill., mother ofidentical twin boys, wrote the AmericanAcademy of Pediatrics’ upcoming book,Raising Twins, from Pregnancy to Preschool—Advicefrom a Pediatrician Momof Twins, which will be available in bookstoresOctober 1.30 ward rounds summer <strong>2009</strong> wardroundsonline.com 31
Alumni NewsUpcoming EventsProgress Notes2000Alpesh A. Patel, MD, of Salt Lake City andwife Angela Chaudhari, MD, announcedthe birth of twin boys, Ashym and Aryan,on February 18. Dr. Patel is assistant professorof orthopaedic surgery and neurosurgeryat the <strong>University</strong> of Utah.2004Taruna J. Madhav, MD, of Cincinnati iscompleting her residency in orthopaedicsurgery at the <strong>University</strong> of Cincinnatiand will continue with training in handsurgery at the Philadelphia Hand Centeruntil August 2010.GME PROGRAMSEmergency MedicineEugene Saltzberg, MD, GME ’74, ofHighland Park, Ill., joined the faculty ofRoslyn Franklin <strong>University</strong> of Medicineand Science in the Department of EmergencyMedicine.Obstetrics and GynecologyAllan T. Bombard, MD, GME ’88, MBA,of San Diego recently completed his masterof business administration degree throughthe <strong>University</strong> of San Diego. In January hewas named chief medical officer for Sequenom,Inc. He also serves as clinical professorof obstetrics and gynecology at AlbertEinstein College of Medicine.Other ProgramsCell and Molecular BiologyLekha Gopalakrishnan, PhD ’95, JD, ofDallas has joined the business law firm ofWinstead, specializing in intellectual propertypractice. After earning her PhD degreefrom <strong>Northwestern</strong>, she received her JDdegree from the <strong>University</strong> of Texas.Prosthetics and OrthoticsChristopher Weiss, cert. ’06, of ParkRidge, Ill., has completed his residency andboards and now serves as a staff orthotist atScheck and Siress Prosthetics, Orthotics,Inc., in Chicago’s Lincoln Park area.32 ward rounds summer <strong>2009</strong>Alum puts her heart into surgical missionsWhen she’s not working at Doernbecher Children’s Hospital in Portland, Oregon, VeronicaC. Swanson, MD ’92, regularly takes part in cardiac surgical missions to countries in needof advanced health care services. In February Dr. Swanson traveled to Ghana, where shehelped to open a new hospital. Last fall she spent time in Peru, continuing a collaborationwith local surgical teams. Interacting with both adult and pediatric surgical patients, Dr.Swanson spent some quality time with Sebastian (above)—the first child to undergo heartsurgery in Arequipa, Peru. Closer to home, Portland Monthly magazine recently recognizedDr. Swanson as one of Portland’s top doctors in the specialty of pediatric anesthesiologyfor 2008 in its annual publication released earlier this year.Send Us Your Progress Notes!MAIL US!Office of Communications<strong>Northwestern</strong> <strong>University</strong>Feinberg School of Medicine303 East Chicago Avenue, Rubloff 9th floorChicago, Illinois 60611-3008E-MAIL US!ward-rounds@northwestern.eduVISIT THE WEB!www.wardroundsonline.comBe sure to include the year the MD degree was received or the GMEor Other Program was completed. Photos submissions also arewelcomed. Please note: Progress Notes appearing in the print editionof <strong>Ward</strong> <strong>Rounds</strong> may be posted on www.wardroundsonline.com andare password-protected.In MemoriamJames R. Armstrong, MD ’36, of SantaRosa, Calif., died January 25, <strong>2009</strong>.John P. Birdzell, MD ’36, of CrownPoint, Ind., died March 1, <strong>2009</strong>.Henry B. Blumberg, MD ’42, of Shoreview,Minn., died January 3, <strong>2009</strong>.Ercil R. Bowman Jr., MD ’55, of PortTownsend, Wash., died February 7, <strong>2009</strong>.John R. Brobeck, MD ’37, of Media, Pa.,died March 6, <strong>2009</strong>.Roger A. Brown, MD ’44, of Provo,Utah, died December 21, 2008.Maurice M. Burkholder, MD ’43, GME’48, of Boise, Idaho, died January 13, <strong>2009</strong>.Price C. Campbell, MD ’50, of Richmond,Texas, died March 24, <strong>2009</strong>.Earl T. Carter, MD ’48, MS ’50, of Rochester,Minn., died February 19, <strong>2009</strong>.Owen Deneen, MD ’47, of Bloomington,Ill., died December 20, 2008.Leslie K. Diaz Jr., MD, GME ’01, of Hopkins,Minn., died March 2, <strong>2009</strong>.Eva Schiffer Grimes, MD ’59, GME ’60,of Indianapolis died April 1, <strong>2009</strong>.Arthur T. Haebich, MD ’49, of Glenview,Ill., died January 30, <strong>2009</strong>.William T. Haeck, MD ’64, of BocaRaton, Fla., died November 15, 2008.Isobel D. Hartley, BSN ’60, of La Jolla,Calif., died March 13, <strong>2009</strong>.John D. Johnson, MD ’52, of SolanaBeach, Calif., died January 10, <strong>2009</strong>.Welburne D. Johnson II, MD ’80, ofCookeville, Tenn., died January 26, <strong>2009</strong>.L. Beaty Pemberton, MD ’62, of PrairieVillage, Kan., died March 8, <strong>2009</strong>.Benjamin R. Riordan, MD ’48, ofNampa, Idaho, died December 25, 2008.Francis M. Sellers, MD ’46, of SouthBend, Ind., died March 4, <strong>2009</strong>.Bernard Simon, MD ’57, of Boca Raton,Fla., died February 9, <strong>2009</strong>.Harold Pratt Sutherland, MD ’54, of SaltLake City died February 12, <strong>2009</strong>.Jerome D. Tossy, MD, GME ’59, of LosAltos, Calif., died February 18, <strong>2009</strong>.Carl E. Wenger, MD ’48, of Sherwood,Ark., died January 14, <strong>2009</strong>.Paul L. Winter, MD ’56, of Palos Heights,Ill., died February 9, <strong>2009</strong>.Gilbert Won, MD ’63, of Foster City,Calif., died April 7, <strong>2009</strong>.July 30 –31Management of Multiple Sclerosis: Select Topics / RIC, 345East Superior Street, Chicago. Fee: $450. For more information,call RIC, 312/238-6042.August 14–16Controversies, Conversations in Laser and CosmeticSurgery / Fairmont Southampton, 101 South Shore Road,Southampton, Bermuda. Fee: $1,295 for physicians; $695 for residentsand fellows. For more information, call SkinCare Physicians,617/848-1647.August 28Founders’ Day Convocation / Official opening of the academicyear at <strong>Northwestern</strong> <strong>University</strong> Feinberg School of Medicine,2:30 p.m., Thorne Auditorium, Arthur Rubloff Building, 375East Chicago Avenue, Chicago. All members of the medicalschool community are invited to attend. For more information,call the Augusta Webster, MD, Office of Medical Education,312/503-0440.October 1–4Eleventh Annual Lynn Sage Breast Cancer Symposium /Fairmont Chicago, 200 North Columbus Drive, Chicago. Fee:$350 before August 15 for physicians, $425 after August 15;$150/$225 for students, residents, and fellows; and $250/$325 fornurses. For more information, call the Robert H. Lurie ComprehensiveCancer Center of <strong>Northwestern</strong> <strong>University</strong>, 312/695-1304.October 3–5Updates on Strategies in Lymphedema Management / RIC,345 East Superior Street, Chicago. For more information, callRIC, 312/238-4251.November 21Twelfth Annual Liver Review Meetings: Impact on ClinicalPractice / NMH, Conference Center, Feinberg Pavilion, 251 EastHuron Street, Chicago. For more information, call NMH’sDepartment of Physician Services, 312/926-7975.Additional photographyMaria Corley, p. 4Jim Coit, pp.10–11Larry Larson, pp. 10, 13Mary Hanlon and Jim Ziv, pp. 18–21
<strong>Northwestern</strong> <strong>University</strong>Office of Communications<strong>Northwestern</strong> <strong>University</strong>Feinberg School of Medicine303 East Chicago Avenue, Rubloff 9th floorChicago, Illinois 60611-3008Change Service RequestedNonprofit OrganizationU.S. PostagePAID<strong>Northwestern</strong> <strong>University</strong>