RJCS Nr 1 - 2 / 2010 - Academia Oamenilor de Stiinta din Romania
RJCS Nr 1 - 2 / 2010 - Academia Oamenilor de Stiinta din Romania
RJCS Nr 1 - 2 / 2010 - Academia Oamenilor de Stiinta din Romania
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
GLOBAL WARMING AND INTERNATIONAL SECU<strong>Romania</strong>n<br />
Journal of Cardiovascular Surgery<br />
Revista Societăţii Române <strong>de</strong> Chirurgie Cardiovasculară<br />
Volum 9, Anul IX, nr. 1-2, <strong>2010</strong><br />
Editor-in Chief & Foun<strong>din</strong>g Editor:<br />
Vasile Cân<strong>de</strong>a (Bucureşti)<br />
Associate Editors:<br />
Bârsan, M. (Cluj-Napoca) Deac, R. (Târgu-Mureş)<br />
Droc, I. (Bucureşti)<br />
Iliescu, V. (Bucureşti) Moldovan, H. (Bucureşti)<br />
Wendt, D. (Essen)<br />
Managing Editors:<br />
Luminiţa Iliuţă (Bucureşti) Vasilescu, A. (Bucureşti)<br />
Assistant Editors:<br />
Adriana Milea (Bucureşti)<br />
Editorial Board:<br />
An<strong>de</strong>rcou, A., Cluj-Napoca, <strong>Romania</strong> Laufer, G., Vienna, Austria<br />
Bracale, G., Naple, Italy Mironiuc, A., Cluj-Napoca, <strong>Romania</strong><br />
Băilă, S., Bucharest, <strong>Romania</strong> Mureşan, H., Bucharest, <strong>Romania</strong><br />
Bloch, G., Paris, France Noirhomme, P., Brussels, Belgium<br />
Cerin, G., Novara, Italy Nottin, R., Paris, France<br />
Cormier, J. M., Paris, France Palombo, D., Genoa, Italy<br />
Dessouter, P., Paris, France Păcescu, Maria, Bucharest, <strong>Romania</strong><br />
Di Donato, R., Rome, Italy Rădulescu, B., Bucharest, <strong>Romania</strong><br />
Diena, M., Turin, Italy Raithel, D., Nurenberg, Germany<br />
Dobre, M., Lund, Swe<strong>de</strong>n Scridon, T., Cluj-Napoca, <strong>Romania</strong><br />
Droc, I., Bucharest, <strong>Romania</strong> Socoteanu, I., Timişoara, <strong>Romania</strong><br />
Frigiola, A., Milan, Italy Suciu, H., Targu Mures, <strong>Romania</strong><br />
Gaşpar, M., Timişoara, <strong>Romania</strong> Tinică, G., Iaşi, <strong>Romania</strong><br />
Ginghină, Carmen, Bucharest, <strong>Romania</strong> Tschirkov, A., Sofia, Bulgary<br />
Goleanu, V., Bucharest, <strong>Romania</strong> Ţintoiu, I., Bucharest, <strong>Romania</strong><br />
Iliescu, V., Bucharest, <strong>Romania</strong> Vasile, R., Bucharest, <strong>Romania</strong><br />
Ionescu, M., Monte Carlo, Monaco Veith, F., New York, U.S.A.<br />
Iosifescu, A., Bucharest, <strong>Romania</strong> Vicol, C., Munich, Germany<br />
Lobonţiu, A., Paris, France Wölner, E., Vienna, Austria<br />
Revistă acreditată CNCSIS categoria C (cod 230)<br />
1
Tehnoredactare computerizată: Mihai SINDILE (<strong>Aca<strong>de</strong>mia</strong> <strong>Oamenilor</strong> <strong>de</strong> Ştiinţă <strong>din</strong> România)<br />
Volum 9, Anul IX, nr. 1-2, <strong>2010</strong><br />
Percutaneous tracheostomy in ICU patients un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy<br />
Ion MICLEA, Violeta BERCAN, Şerban BUBENEK<br />
Institutul <strong>de</strong> Urgenţă pentru Boli Cardiovasculare, “Prof. Dr. C.C. Iliescu”, Bucharest<br />
Microsimulation and clinical outcomes analysis support a lower age threshold for<br />
use of biological valves. Microsimulation bioprostheses<br />
Serban Stoica 1, Kimberley Goldsmith 2, Nikolaos Demiris 2, Prakash Punjabi 3,<br />
Geoffrey Berg 4, Linda Sharples 2, Stephen Large 5<br />
1) Bristol Royal Children's Hospital; 2) Medical Research Council Biostatistics Unit, Cambridge;<br />
3) Hammersmith Hospital, London; 4) Gol<strong>de</strong>n Jubilee National Hospital, Glasgow;<br />
5) Papworth Hospital, Cambridge, UK<br />
The 23-rd Annual Meeting of the European Association for Cardio-Thoracic<br />
Surgery Vienna, Austria, 17-21 October 2009<br />
Grigore Tinică, Diana Ciurescu<br />
University of Medicine and Pharmacy “Gr. T. Popa” Iasi, Cardiovascular Institute Iasi<br />
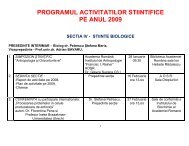
Schema <strong>de</strong> program 21<br />
Programul susţinerii lucrărilor pe secţiuni 23<br />
VOLUMUL DE REZUMATE 34<br />
Grupul <strong>de</strong> lucrări « CORD » (vineri 1 octombrie) 34<br />
Grupul <strong>de</strong> lucrări « CHIRURGIE VASCULARĂ » 46<br />
Grupul <strong>de</strong> lucrări « CORD » (sâmbătă 2 octombrie) 60<br />
Simpozionul Societăţii Române <strong>de</strong> Anestezie-Terapie Intensivă Cardiacă şi<br />
Tehnologie Extracorporeală (SRATICTE)<br />
Grupul <strong>de</strong> lucrări « CONGENITALI » 81<br />
Grupul <strong>de</strong> lucrări « NURSING » 86<br />
2<br />
03<br />
08<br />
17<br />
21<br />
71
ISSN 1583-3534, Ion Miclea, Violeta Bercan, Şerban Bubenek ■ <strong>2010</strong>, vol. 9, no. 1-2, pp. 3-7<br />
Percutaneous tracheostomy<br />
in ICU patients un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy<br />
Dr. Ion MICLEA PhD. MD, Dr. Violeta BERCAN, MD,<br />
Conf. univ. dr. Şerban BUBENEK PhD, MD<br />
Institutul <strong>de</strong> Urgenţă pentru Boli Cardiovasculare<br />
“Prof. Dr. C.C. Iliescu”, Bucharest, <strong>Romania</strong><br />
Mo<strong>de</strong>rn intensive care involves a series of maneuvers that were formerly the exclusive<br />
preserve of surgery. Current technology provi<strong>de</strong>s special medical kits for percutaneous<br />
tracheostomy, pleural punctures, intra-aortic balloon pump, etc., facilitating these maneuvers,<br />
which have become common in intensive care units. Percutaneous tracheostomy occupies an<br />
important place in airway management of critical ill patient.<br />
The term “tracheostomy” <strong>de</strong>rives from Greek, since 1649, from the words “tracheia artery” –<br />
“rough artery” and “stoma” – “open or mouth”<br />
� in 1500 B.C. the first reference related to this procedure was ma<strong>de</strong>, in Hindu book of<br />
medicine “Rig Veda”<br />
� in 400 B.C., Hippocrates con<strong>de</strong>mned trahoestomia for fear of carotid artery injury<br />
� Alexan<strong>de</strong>r the Great had used “the sword to puncture soldier’s trachea to prevent<br />
suffocation”<br />
� in 100 B.C. Asclepia<strong>de</strong>s of Bithynia ma<strong>de</strong> the first selective tracheostomy, but the patient<br />
did not survive<br />
� in 100 A.D., Galen and Antyluss <strong>de</strong>scribed the incision between the third and fourth ring<br />
� in 1546, Antonio Musa Brasavolo ma<strong>de</strong> the first successful tracheostomy<br />
� in 1860, Evans Conway reported a mortality 68%<br />
� the one that establishes gui<strong>de</strong>lines for making traheostomies was Dr. Chevalier Jackson,<br />
in 1909, <strong>de</strong>scribing a long incision, avoi<strong>din</strong>g cricoids, the isthmus division, safe and slow<br />
surgery, and postoperative care.<br />
� in 1957, Shelton and associates <strong>de</strong>scribed the first percutaneous tracheostomy,<br />
published in JAMA, which is used in a trocar inserted blindly into the trachea<br />
� in 1969, Toye and Weinstein <strong>de</strong>scribed percutaneous Sel<strong>din</strong>ger technique, published in<br />
the journal “Surgery”<br />
� in 1985, Pasquale Ciaglia published “percutaneous dilatative tracheostomy”, by<br />
Sel<strong>din</strong>ger technique<br />
� in 1989, Paul and collaborators <strong>de</strong>scribed the first percutaneous tracheostomy ma<strong>de</strong><br />
un<strong>de</strong>r bronchoscopic control<br />
Nowadays, percutaneous tracheostomy became very important in comparision to<br />
conventional surgical traheostomy. Dilatation technique is consi<strong>de</strong>red the gold standard. There<br />
are more than 600 publications related to percutaneous tracheostomy that were mentioned after<br />
1985.<br />
3
<strong>Romania</strong>n Journal of Cardiovascular Surgery ■ <strong>2010</strong>, vol. 9, no. 1-2, pp. 4<br />
- Need for prolonged mechanical ventilation in cases of:<br />
� treatment refractory pneumonia<br />
� severe chronic obstructive pulmonary disease<br />
� acute respiratory distress syndrome<br />
� severe brain injury<br />
� multiple organ system dysfunction<br />
The Council on Critical Care of the American College of Chest Physicians<br />
recommends tracheostomy in patients who are expected to require<br />
mechanical ventilation for longer than 7 days. (1999)<br />
- Airway obstruction due to following:<br />
� inflammatory disease<br />
� congenital anomaly (laryngeal hypoplasia, vascular web)<br />
� foreign body that cannot be dislodged with Heimlich and basic cardiac life<br />
support maneuvers<br />
� supraglottic or glottic pathologic conditions (neoplasm, bilateral vocal cord<br />
paralysis)<br />
� laryngeal trauma or stenosis<br />
� facial fractures that may lead to upper airway obstruction<br />
� e<strong>de</strong>ma (trauma, burns, infection, anaphylaxis)<br />
- Need for improved pulmonary toilet<br />
- Ina<strong>de</strong>quate caugh due to chronic pain or weakness<br />
- Aspiration and the inability to handle secretions<br />
- Prophylaxis (preparation for extensive head and neck procedures and the convalescent<br />
period)<br />
- Severe sleep apnea not amendable to continuous positive airway pressure <strong>de</strong>vices<br />
- Absolute contraindications:<br />
� patients age younger than 8 years<br />
� necessity of emergency airway access because of acute airway compromise<br />
� gross distortion of the neck anatomy due to<br />
� hematoma<br />
� tumor<br />
� thyromegaly<br />
� high innominate artery<br />
- Relative contraindications<br />
� patient obesity with short neck that obscures neck landmarks<br />
� medically uncorectable blee<strong>din</strong>g diatheses<br />
� prothrombin time or activated partial thromboplastin time more than 1,5 times<br />
the reference range<br />
� platelet count less than 50.000/µl<br />
� blee<strong>din</strong>g time longer than 10 minutes<br />
� need for positive end-expiratory pressure of more than 20 cm of water<br />
� evi<strong>de</strong>nce of infection in the soft tissues of the neck at the prospective surgical<br />
site<br />
4
- Facilitates<br />
� weaning from positive pressure ventilation and sedation<br />
� removal of secretion by aspiration<br />
� long-term airway management<br />
- Prevents aspiration from the pharynx or gastrointestinal tract<br />
- Separates the oropharyngeal flora from the pulmonary flora<br />
� a relatively simple technique suitable for trained staff in the critical care setting<br />
� it does not require an operating theatre<br />
� minimal blood lost<br />
� infection rates for percutaneous tracheostomy range from 0 to 3,3%, whereas those<br />
for open tracheostomy have been reported to be as high as 36%<br />
� stenosis rates for percutaneous tracheostomy range from 0 to 9%<br />
� small and neat stoma of dilatational tracheostomy generally results in a more<br />
cosmetic scar<br />
- Emergency tracheostomy (controversial)<br />
- Difficult to palpate the anatomical landmarks:<br />
� Very obese patients<br />
� Short or bull neck<br />
� Enlarged thyroid<br />
� Nonpalpable cricoid cartilage<br />
� Gross <strong>de</strong>viation of trachea<br />
- Infection at or near the inten<strong>de</strong>d site for tracheostomy<br />
- In paediatric age group (controversial)<br />
- Previous neck surgery may distort the anatomy<br />
- Unstable cervical spine fracture<br />
- Required PEEP>15 cm H2O, as oxygenation may be compromised during the procedure<br />
- Malignancy at the site of tracheostomy<br />
- Uncontrolled coagulapathy, consi<strong>de</strong>red as a relative contraindication<br />
During percutaneous tracheostomy it is possible to puncture the endotracheal tube, or its<br />
cuff, with the needle, which can lead to airway <strong>de</strong>pressurization, with the risk of difficult ventilation<br />
or gastric aspiration. To minimize this risk, there is the possibility of withdrawing the intubation tube<br />
un<strong>de</strong>r vi<strong>de</strong>olaryngoscopic control. The endotracheal tube is withdrawn until its cuff is seen<br />
between the vocal cords. The balloon is than inflated, and the percutaneous tracheostomy<br />
continues in the classical technique. Any reposition of the endotracheal tube, or patient’s<br />
intubation can be more easily controlled un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy than with direct laryngoscopy.<br />
The anaesthetist position during vi<strong>de</strong>olaryngoscopy is more convenient than that of direct<br />
5
laryngoscopy. With the Gli<strong>de</strong>scope <strong>Romania</strong>n Journal the of image Cardiovascular of the Surgery trachea ■ <strong>2010</strong>, vol. and 9, no. the 1-2, vocal pp. 6<br />
cords is transmitted<br />
on the screen.<br />
Most of the tracheostomy kits used in ICU are manufactured by Portex. These inclu<strong>de</strong><br />
scalpel, needle with 14G flexula, 10-cc syringe, gui<strong>de</strong> wire with introducing <strong>de</strong>vice, dilator,<br />
gui<strong>de</strong>wire dilating forceps, tracheostomy tube with mandren, two bands for tube fixation.<br />
Tracheostomy tubes are of different sizes, varying accor<strong>din</strong>g to the diameter and length.<br />
The patient should be a<strong>de</strong>quately anesthetised, to avoid movements, and monitored<br />
using standard techniques. The neck is exten<strong>de</strong>d by placing a fluid bag, or a sandbag, or a pillow<br />
un<strong>de</strong>r the shoul<strong>de</strong>rs. The area around the inten<strong>de</strong>d site is cleaned with antiseptic solution and<br />
surroun<strong>de</strong>d by sterile drapes.<br />
The anaesthetist that manages the airway of the patient prepares the vi<strong>de</strong>olaryngoscope.<br />
He also has aspiration equipment and different sizes of endotracheal tubes. The patient should be<br />
preoxygenated by ventilation with 100% oxygen for at least 5 minutes before starting the<br />
procedure.<br />
The anaesthetist that performs the tracheostomy is sterile equipped; he is the one that<br />
surrounds the area with sterile drapes.<br />
The anaesthetist that controls the airway should suction the pharynx, <strong>de</strong>flate the cuff of the<br />
endotracheal tube, with draw the tube un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy, until the cuff is seen between<br />
the vocal cords. After that he reinflates with the cuff entirely above the vocal cords and continues<br />
the mechanical ventilation of the patient.<br />
The anaesthetist that performs the tracheostomy should locate the thyroid cartilage<br />
between thumb and forefinger, i<strong>de</strong>ntify and mark the anatomical landmarks (thyroid cartilage,<br />
cricoid cartilage, tracheal rings, sternal notch, and possible insertion sites). The i<strong>de</strong>al site is<br />
between the second and third tracheal rings, although a space one higher or lower may be<br />
employed. After that he introduces the needle between the tracheal rings until the position of the<br />
needle tip in the trachea is confirmed (loss of resistance). The needle is withdrawn, the 14G<br />
cannula is left in place, the flexible gui<strong>de</strong>wire is inserted through the cannula, and the position is<br />
checked using the vi<strong>de</strong>olaryngoscope. The 14G cannula is withdrawn, the gui<strong>de</strong>wire is left in<br />
place. The dilator is slid over the wire, through the soft tissues into the trachea; with gentle<br />
si<strong>de</strong>ways movements of the dilator, push the dilator forward to penetrate the anterior wall, dilating<br />
both the tissues and tracheal wall. The dilator is now withdrawn, and the gui<strong>de</strong>wire dilating<br />
forceps is introduced. Using two hands, open the forceps to dilate the tracheal wall sufficiently to<br />
accept the tracheostomy tube. After that the forceps is withdrawn in the open position, and the<br />
tracheostomy cannula (tube) is slid over the gui<strong>de</strong>wire into the trachea. If correct positioned, the<br />
gui<strong>de</strong>wire and the obturator with lumen are withdrawn. He inflates the cuff of the tracheal tube,<br />
suctions the trachea and tracheostomy tube to establish a clear airway and transfers the<br />
breathing system to the tracheostomy tube. The procedure is finished after confirmation of<br />
successful tube placement. One should secure the tracheostomy tube with the supplied cotton<br />
tapes. The endotracheal tube is withdrawn after confirmation of correct placement of the<br />
tracheostomy tube un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy.<br />
Early complications<br />
� Hypoxia during the procedure, due to failure of ventilation<br />
� Pneumothorax, pneumomediastinum, creation of false passage, and<br />
subcutaneous emphysema, due to the placement of the tracheostomy tube in the<br />
paratracheal space<br />
� Damage or injury to the posterior tracheal wall may lead to tracheo-oesophageal<br />
fistula<br />
� Major blee<strong>din</strong>g is unusual<br />
� Minor blee<strong>din</strong>g can usually be controlled by pressure or occasionally suture<br />
6
� Haemorrhage into the airway is potentially dangerous as it may result in a blood<br />
clot obstructing the airway<br />
� Needle puncture on the lateral wall of trachea may lead to stenosis<br />
� Secondary haemorrhage may occur from infection or erosion of vessels<br />
Late complications:<br />
� Subglottic stenosis – the inci<strong>de</strong>nce of subglottic stenosis is lower in percutaneous<br />
tracheostomy than that in open surgical procedure<br />
� Percutaneous tracheostomy is a safer maneuver the more trained the team is<br />
� The risk of infection and subglottic stenosis is lower for percutaneous tracheostomies<br />
� When ma<strong>de</strong> un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy control. The maneuvre is safer, because it<br />
ensures a good ventilation of the patient<br />
1. Positioning the tracheal tube during percutaneous tracheostomy: another use for<br />
vi<strong>de</strong>olaryngoscopy - M. Gillies*, J. Smith and C. Langrish - British Journal of Anaesthesia<br />
2008 101(1):129<br />
2. Modification of percutaneous tracheostomy by direct visualisation of endotracheal tube<br />
positioning with Gli<strong>de</strong>scope prior to performing procedure - Juan D. Pulido, MD*, Faisal<br />
Usman, MD, James D. Cury, MD, Abubakr A. Bajwa, MD, Kathryn Koch, MD and Luis Laos,<br />
MD - University of Florida, Jacksonville, FL - 2009 by the American College of Chest<br />
Physicians.<br />
3. Early clinical experience with a new vi<strong>de</strong>olaryngoscope (Gli<strong>de</strong>Scope) in 728 patients –<br />
Richard M. Cooper, John A. Pacey Michael J. Bishop and Stuart A. McCluskey – Canadian<br />
Journal of Anesthesia, 2005, 191-198<br />
7
ISSN 1583-3534, Şerban Stoica et al. ■ <strong>2010</strong>, vol. 9, no. 1-2, pp. 8-16<br />
Microsimulation and clinical outcomes analysis support a lower age<br />
threshold for use of biological valves. Microsimulation bioprostheses<br />
Serban Stoica 1 , Kimberley Goldsmith 2 , Nikolaos Demiris 2 , Prakash Punjabi 3 ,<br />
Geoffrey Berg 4 , Linda Sharples 2 , Stephen Large 5<br />
1) Bristol Royal Children's Hospital;<br />
2) Medical Research Council Biostatistics Unit, Cambridge;<br />
3) Hammersmith Hospital, London;<br />
4) Gol<strong>de</strong>n Jubilee National Hospital, Glasgow;<br />
5) Papworth Hospital, Cambridge, UK<br />
*Correspon<strong>din</strong>g author. Tel: +44 1480 830541, Fax: +44 1480 831315,<br />
Email: stephen.large@papworth.nhs.uk<br />
Background: We aimed to characterize contemporary results of aortic valve<br />
replacement (AVR) in relation to type of prosthesis and subsequent competing hazards.<br />
Methods: 5470 consecutive AVR ± coronary artery bypass grafting (CABG) patients were<br />
studied. Microsimulation of survival and valve-related outcomes was performed based on<br />
meta-analysis and patient data inputs, with separate mo<strong>de</strong>ls for age, gen<strong>de</strong>r and CABG.<br />
Survival was validated against the United Kingdom Heart Valve Registry.<br />
Results: Patient survival at 1, 5 and 10 years was 90%, 78% and 57% respectively. The<br />
crossover points at which bio- and mechanical prostheses conferred similar life expectancy (LE)<br />
was 59 years for males and females (no significant difference between prosthesis types<br />
between the ages of 56-69 for men, and 58-63 for women). The improvement in event-free LE<br />
for mechanical valves is greater at younger ages with a crossover point of 66 years for males<br />
and 67 years for females. Long-term survival was in<strong>de</strong>pen<strong>de</strong>ntly influenced by age, male<br />
gen<strong>de</strong>r, and concomitant CABG, but not by type of prosthesis. In bioprostheses the most<br />
common long-term occurrence is structural <strong>de</strong>terioration. For men aged 55, 65 and 75 at initial<br />
operation it has a lifetime inci<strong>de</strong>nce of 50%, 30% and 13% respectively. The simulation output<br />
showed excellent agreement with registry data.<br />
Conclusion: For Bioprostheses can be implanted selectively in patients below 65 without<br />
significant long-term adverse effects.<br />
Keywords: Aortic valve, replacement; Heart valve, bioprostheses; Heart valve,<br />
mechanical<br />
Prosthesis choices for aortic valve replacement (AVR) between the ages of 50 and 70<br />
years are not standardized, even in the absence of other factors that reduce life expectancy. Of<br />
the two trials comparing mechanical vs. biological valves one found superior survival with<br />
mechanical valves [1]. In practice the trend is towards using more bioprostheses but the evi<strong>de</strong>nce<br />
for that is not strong. Thus it remains unclear how the blee<strong>din</strong>g hazard for mechanical valves<br />
compares long-term with the risk of structural <strong>de</strong>generation of bioprostheses. Randomized trials for<br />
8
such few and remote outcomes, Şerban Stoica as well et al. ■ as <strong>2010</strong>, longitu<strong>din</strong>al vol. 9, no. 1-2, pp. follow-up, 9<br />
are logistically difficult,<br />
particularly when the valve industry innovates constantly.<br />
Bioprostheses below the age of 65 are supported by some recent publications [2-4],<br />
discouraged by others [5], whereas another view is that patient factors are more important in<br />
<strong>de</strong>termining long-term outcomes [6]. Some of the studies have used microsimulation of the<br />
patients’ course with point estimate inputs not allowing for variability (<strong>de</strong>terministic inputs) [2, 3].<br />
The aim of this study was to analyse life expectancy and complication rates for United Kingdom<br />
(UK) patients un<strong>de</strong>rgoing AVR with bio- and mechanical prostheses. Age, gen<strong>de</strong>r, concomitant<br />
coronary artery bypass grafting (CABG) and other patient factors are examined using simulation<br />
of the lifetime after AVR surgery with non-<strong>de</strong>terministic inputs incorporating variability.<br />
5470 consecutive AVR ± coronary artery bypass grafting (CABG) procedures (5433<br />
patients) at 3 centers between 1993-2006 were studied. Patient data were used to study<br />
perioperative mortality. A microsimulation mo<strong>de</strong>l was constructed to predict life histories for the<br />
study patients, using patient data wherever possible for inputs. Since <strong>de</strong>tailed follow up<br />
information was not available for study patients this was supplemented with results from a metaanalysis<br />
of valve-related morbidity and mortality. Validation of the simulation results, inclu<strong>din</strong>g<br />
overall survival, was carried out against data from the UK Heart Valve registry (UKHVR). UKHVR<br />
contains reoperation and survival statistics for individual patients but no follow up on valve-related<br />
events.<br />
Patients and valves<br />
Patient information from the three centers was collected prospectively. Patients data were<br />
<strong>de</strong>-i<strong>de</strong>ntified to maintain confi<strong>de</strong>ntiality. Table 1 shows a list of valves used in the study period<br />
(1993-2006) and Table 2 shows patient characteristics. Homografts and valve repairs were<br />
exclu<strong>de</strong>d.<br />
Perioperative survival<br />
Estimates of operative <strong>de</strong>ath from first and subsequent AVR were taken from the multiple<br />
variable analysis of perioperative mortality from the three participating centres. The effects of<br />
age, gen<strong>de</strong>r, prosthesis type, concomitant CABG, creatinine and reoperation on perioperative<br />
mortality were studied using logistic regression. Variables such as the New York Heart Association<br />
score for breathlessness (NYHA) and left ventricular (LV) function were not recor<strong>de</strong>d consistently in<br />
the databases and so did not appear in the final mo<strong>de</strong>l. Manual stepwise selection based on the<br />
likelihood ratio statistic was used to <strong>de</strong>tect variables for the multivariable mo<strong>de</strong>ls. The Hosmer and<br />
Lemeshow statistic for the final mo<strong>de</strong>l showed no evi<strong>de</strong>nce of poor fit (p = 0,53). For each age<br />
group, different survival probabilities were estimated for 4 subgroups <strong>de</strong>fined by sex<br />
(male/female) and concomitant CABG surgery (yes/no), accor<strong>din</strong>g to results from the logistic<br />
regression.<br />
Meta-analysis<br />
In the absence of long term follow up of valve-related events for UK patients, a systematic<br />
review of the literature and random effects meta-analysis were performed [7], while for other<br />
event rates we had similar inputs and mo<strong>de</strong>l assumptions as Puvimanasinghe (2004) [3] (Table E1).<br />
PubMed was searched between 1990-2009 with the Boolean string “aorta OR aortic AND valve<br />
replacement”. The search was limited to articles on humans published in English in core clinical<br />
journals and resulted in 2085 hits.<br />
Inclusion criteria:<br />
1) outcomes of AVR listed in table E1 with prostheses listed in Table 1, size ≥ 19 mm;<br />
2) concomitant procedure, if present, CABG or mitral valve replacement (all mitral<br />
patients in combined series, with or without concomitant AVR, were subsequently exclu<strong>de</strong>d);<br />
3) gui<strong>de</strong>line compliant, or in the spirit of published gui<strong>de</strong>lines [8];<br />
9
data;<br />
4) follow-up available in ≥ 95% of patients.<br />
Table 1. Types of valves inserted<br />
Type of valve Number inserted (%)<br />
Aortech 556 10,2<br />
Aspire/Elan 188 3,4<br />
ATS 477 8,7<br />
Bjork-Shiley 35 0,7<br />
Carbomedics 182 3,3<br />
Carpentier Edwards 959 17,5<br />
Carpentier Edwards Perimount 1.315 24,0<br />
Edwards Prima 144 2,6<br />
Edwards Mira 41 0,7<br />
Medtronic Mosaic 72 1,3<br />
Sorin Bicarbon 114 2,1<br />
St Ju<strong>de</strong> mechanical 889 16,3<br />
St Ju<strong>de</strong> tissue 139 2,5<br />
Starr Edwards 32 0,6<br />
Toronto stentless 195 3,6<br />
Other (Autologous pericardial, AorTech, Edwards Tekna,<br />
Shelhigh, Sorin Soprano, Sorin Pericarbon, TissueMed)<br />
42 0,7<br />
10<br />
Total 5.470 100<br />
Exclusion criteria:<br />
1) Absence of any morbidity data;<br />
2) Linearized occurrence rate of events unpublished or unobtainable from the published<br />
3) Specialized series (redo, small aortic root, extremes of age);<br />
4) Overlapping or previously published series, in which case the last report was chosen.<br />
Forty-seven articles met the criteria, containing 28,623 patients and 152,075 patient-years<br />
follow-up (Table E2). Where necessary linearized occurrence rates and their standard errors were<br />
calculated with the available data (see supplementary data). For embolism, valve thrombosis<br />
and non-structural dysfunction we used a random rate, simulated from a distribution obtained by<br />
meta-analysis. For endocarditis we assumed a constant rate for the first six months and a smaller<br />
constant rate thereafter. For structural valve <strong>de</strong>terioration we assumed an increasing rate over<br />
time for bioprostheses [3] and a zero event rate for mechanical valves. Finally, for haemorrhage<br />
we employed a constant rate over time for bioprostheses and an exponentially increasing rate for<br />
mechanical valves [9]. Estimates of reoperation and <strong>de</strong>ath rates associated with these events are<br />
from the literature [3].<br />
Microsimulation<br />
<strong>Romania</strong>n Journal of Cardiovascular Surgery ■ <strong>2010</strong>, vol. 9, no. 1-2, pp. 10<br />
Conditional on perioperative survival, the microsimulation for studying valve outcomes was<br />
similar to that <strong>de</strong>scribed in <strong>de</strong>tail by the Rotterdam group [2, 3, 10]. Briefly, after AVR a number of<br />
factors influence the trajectory between the states alive and <strong>de</strong>ceased: background, additional<br />
and operative mortality, and valve-related events. Background mortality was taken from<br />
government life tables [11]. Additional mortality reflects the increased hazard of <strong>de</strong>ath for a<br />
patient un<strong>de</strong>rgoing AVR as compared to the general population [3]. Heart rhythm and function or<br />
type and severity of valve disease can contribute to this hazard. We used an accepted simulation<br />
method [10], with an additional loop to incorporate the uncertainty about event rates. Life<br />
histories of 50,000 individuals and 100 event rates for each age group were simulated using the<br />
following steps:
1. Random event rates Şerban were Stoica drawn et al. ■ <strong>2010</strong>, for vol. valve-related 9, no. 1-2, pp. 11<br />
morbidity and its sequelae of<br />
reoperation and subsequent <strong>de</strong>ath.<br />
2. A random probability of <strong>de</strong>ath from operation/reoperation was drawn from its<br />
distribution. This was used to <strong>de</strong>ci<strong>de</strong> if a simulated individual survived the initial operation. If so, the<br />
main body of the simulation continued.<br />
3. Based on UK mortality tables, adjusted for the additional mortality related to AVR, a<br />
random age was sampled that became the age-at-<strong>de</strong>ath of the individual should no valverelated<br />
event occur.<br />
4. Using the occurrence rates in Table E1 and the event rates from step 1, a random age at<br />
which each event may occur was simulated. If all of these times were greater than the age-at<strong>de</strong>ath<br />
in step 3, the simulation en<strong>de</strong>d and that was the age-at-<strong>de</strong>ath. Otherwise the event that<br />
correspon<strong>de</strong>d to the shortest time was assumed to occur first. The mortality rate associated with<br />
each event was used to <strong>de</strong>termine whether the individual died due to the event or not. In the<br />
former the age-at-<strong>de</strong>ath was (re)set to the time at which the event occurred. If the individual<br />
survived the event but required surgery because of the event, any additional surgical mortality<br />
was also simulated. Thereafter, the time to the next event was <strong>de</strong>termined, possibly altering some<br />
event probabilities conditional on the simulated individual history. This procedure continued until<br />
the simulated individual died or reached the random age-at-<strong>de</strong>ath of step 3.<br />
5. Steps 2–4, were repeated 50,000 times for each valve type and life expectancy (LE),<br />
event free life expectancy (EFLE) and the probabilities of valve-related events were calculated<br />
from the simulated individual histories. In or<strong>de</strong>r to estimate the distributions of these outputs, steps<br />
1-4 were repeated for 100 draws from the event rate distributions.<br />
Validation<br />
Using UKHVR data from the three centers an observed (empirical) survival curve for the<br />
patients was constructed using Kaplan-Meier methods. Predicted survival curves from the<br />
simulation were compared with UKHVR observed survival curves. Estimates of uncertainty for the<br />
mo<strong>de</strong>l resulted from probabilistic sensitivity analysis and are represented graphically in the output.<br />
The effects of age, gen<strong>de</strong>r, prosthesis type, concomitant CABG and creatinine levels on long-term<br />
survival were studied using Cox proportional hazards mo<strong>de</strong>ls. In addition to patient survival,<br />
prosthesis lifetimes were calculated. Patients were consi<strong>de</strong>red to have had the event (1st<br />
prosthesis failure or operative <strong>de</strong>ath) if they had a 2nd AVR operation, died perioperatively at<br />
initial surgery, or died of any valve-related or cardiovascular cause of <strong>de</strong>ath. Otherwise patients<br />
were censored. For second prosthesis lifetime only patients having had a 2nd AVR operation were<br />
inclu<strong>de</strong>d.<br />
Patients and valves<br />
Between 1993-2006 5470 consecutive AVR operations were performed in 5433 patients<br />
(2239 mechanical and 3231 biological valves). Table 2 shows patients' characteristics. Patients<br />
with tissue valves were ol<strong>de</strong>r, more likely to be women and have concomitant CABG (all p <<br />
0.001). There were slightly more reoperations for which mechanical valves were implanted (2% of<br />
mechanical versus 1% of tissue, p < 0.001). Patients given tissue valves had higher NYHA scores,<br />
and were more likely to have non-insulin <strong>de</strong>pen<strong>de</strong>nt diabetes, atrial fibrillation/flutter<br />
preoperatively, higher risk scores and lower creatinine clearance (all p < 0.001).<br />
In univariate analysis patients receiving bioprostheses had 1.6 times the odds of dying<br />
perioperatively as compared to mechanical valve patients (Table 3). In multiple variable analyses,<br />
type of prosthesis and gen<strong>de</strong>r were not associated with perioperative mortality when other<br />
characteristics were analysed. Concomitant CABG was associated with 1.4 higher odds of <strong>de</strong>ath<br />
(p = 0.05). Each 10 years increment in age had a 1.5 times increases in the odds of operative<br />
mortality (p < 0.001). A 10 unit increase in creatinine levels was associated with a 5% increase in<br />
the risk of <strong>de</strong>ath soon after the valve operation (p < 0.001). These results were taken to the next<br />
stage.<br />
11
Table 2. Patient characteristics by prosthesis type<br />
Characteristic<br />
12<br />
Mechanical<br />
prosthesis,<br />
n=2.239<br />
Tissue<br />
prosthesis,<br />
n=3.231<br />
p-value<br />
Peri-operative mortality, n (%) yes 82 (4) 188 (6) < 0.001<br />
Mean age (SD) 58,5 (11.6) 74.1 (7.5) < 0.001<br />
Male gen<strong>de</strong>r, n (%) 1.567 (70) 1.836 (57) < 0.001<br />
Concomitant CABG, n (%) 445 (20) 1.195 (38) < 0.001<br />
Greater than 1st operation, n (%) 49 (2) 22 (1) < 0.001<br />
NYHA, n (%) asymptomatic 77 (9) 30 (2) < 0.001<br />
n (%) I 132 (16) 130 (10)<br />
n (%) II 297 (35) 434 (33)<br />
n (%) III 287 (34) 612 (46)<br />
n (%) IV 61 (7) 116 (9)<br />
LV function, n (%) normal (>50%) 1.261 (60) 1899 (61) 0.64<br />
n (%) mo<strong>de</strong>rate impairment (30-50%) 655 (31) 917 (30)<br />
n (%) severe impairment (
CI Confi<strong>de</strong>nce Interval<br />
Microsimulation<br />
Figures 1 and 2 show differences in life expectancy (LE) and event-free life expectancy<br />
(EFLE) after AVR between bioprosthetic and mechanical valves for men and women with and<br />
without CABG. Men had a small but consistent survival benefit in receiving a mechanical valve for<br />
patients up to about age 59. Although this was the crossover point, there was no significant<br />
difference between bioprostheses and mechanical valves between the ages of 56 and 69. The<br />
improvement in EFLE was greater at younger ages and bioprostheses were favored after the age<br />
of 66, although there was no significant difference between the two types of valves between the<br />
ages of 62 and 68. For women, the crossover points at which the valve types conferred the same<br />
LE and EFLE were approximately the same as for men (59 and 67 respectively). Patients who had<br />
AVR and CABG had only slightly shorter LE and EFLE than those having AVR alone. The only<br />
difference in mo<strong>de</strong>l inputs for the combined procedure was a small but significant increase in<br />
operative <strong>de</strong>ath rate. Fig. 3 illustrates valve-related complications for males. Table E3 summarizes<br />
valve-related complications for both sexes. The plots and tables for males show that prosthetic<br />
endocarditis had an estimated lifetime probability of 6-13% <strong>de</strong>pen<strong>din</strong>g on age at first procedure.<br />
Although it was more common for mechanical valves the differences were small. Non-valve<br />
systemic thromboembolism had a slightly higher estimated inci<strong>de</strong>nce in recipients of bioprostheses<br />
compared to mechanical valves, in agreement with inputs from table E1. Haemorrhage, as<br />
expected, was significantly more common among mechanical valve patients. Structural valve<br />
disease was frequent for bioprostheses with a lifetime probability of 58%, 50%, 40%, 30%, 20% and<br />
13% for men aged 50, 55, 60, 65, 70 and 75 respectively at initial operation. Valve thrombosis was<br />
fairly uncommon, occurring with a lifetime probability of less than 8% in male mechanical valve<br />
patients and less than 0.2% in male bioprosthesis patients, in all age groups. Non-structural valve<br />
dysfunction was also uncommon, with a marginally higher occurrence for the mechanical group,<br />
with a lifetime probability of 3.6% and 4.3% for 50 year olds, <strong>de</strong>creasing to 1.8 and 2.0% for 75 year<br />
olds for the bioprosthesis and mechanical groups respectively. Event rates were slightly higher in<br />
general for females, probably related to their longer LE, but had a similar distribution (Table E3).<br />
Validation and long-term survival<br />
Şerban Stoica et al. ■ <strong>2010</strong>, vol. 9, no. 1-2, pp. 13<br />
Mo<strong>de</strong>l predicted patient survival at 1, 5 and 10 years was 90%, 78% and 57% (Fig. 4),<br />
whereas first valve survival was 91%, 85% and 71% respectively. These agreed well with registry<br />
data. In multiple variable analyses, long-term survival was adversely affected by increasing age,<br />
male gen<strong>de</strong>r and CABG but not tissue prosthesis, although there were clearly age-specific<br />
differences between valve types (Table 4). Redo AVR operations were captured via the UKHVR:<br />
there were 74 during the study period (68 first time and 6 second time). The most common causes<br />
of redos were intrinsic valve failure (22%), prosthetic endocarditis (12%) and <strong>de</strong>hiscence (9%). Fig.<br />
4 shows that the UKHVR actuarial survival curves for mechanical and valves compared with<br />
predicted survival from the simulation for a 65 year old man. The registry curves lie almost entirely<br />
within the confi<strong>de</strong>nce bounds for the mo<strong>de</strong>l.<br />
Table 4. Relationship between survival and patient characteristics<br />
Characteristic<br />
Univariate HR (95% CI),<br />
p-value<br />
Multiple variable HR (95% CI),<br />
p-value<br />
Tissue prosthesis<br />
1.99 (1.76, 2.26)<br />
p
increments) (mmol/L) p
any mathematical mo<strong>de</strong>ling, is as good as its inputs. Oversimplifications are inevitable in places,<br />
for example by assuming that valve-related complications are constant over time and<br />
in<strong>de</strong>pen<strong>de</strong>nt of patient age and time elapsed from surgery.<br />
An analysis of quality of life outcomes in middle-aged patients un<strong>de</strong>rgoing AVR highlighted<br />
some significant downsi<strong>de</strong>s of mechanical valves [12]. Our results support the notion that quality of<br />
life divi<strong>de</strong>nds are not associated with a <strong>de</strong>crease in quantity of life by implanting bioprostheses<br />
selectively below the age of 65.<br />
Acknowledgement<br />
Maria Benedicta Edwards, from the United Kingdom Heart Valve Registry, assisted in linking<br />
our data to the registry.<br />
Figure legends 1<br />
Figure 1. Mean difference (95% confi<strong>de</strong>nce limits) in life-expectancy between<br />
bioprostheses and mechanical valves by age. Values above 0 favour bioprostheses.<br />
Figure 2. Mean difference (95% confi<strong>de</strong>nce limits) in event-free life-expectancy between<br />
bioprostheses and mechanical valves by age. Values above 0 favour bioprostheses.<br />
Figure 3. Lifetime probability of valve-related complications for males, AVR only.<br />
A. Endocarditis<br />
B. Thromboembolism<br />
C. Hemorrhage<br />
Figure 4. Kaplan-Meier survival estimates from combined analysis of UK AVR patients<br />
compared to simulation predicted survival for 65 year old men with CABG The first curve<br />
from the top shows the UK general life expectancy for 65 year old men, and the second<br />
curve down shows background mortality after AVR as incorporated in the mo<strong>de</strong>l. The<br />
mo<strong>de</strong>l prediction is shown as dots and the solid lines are 95% confi<strong>de</strong>nce bands. All these<br />
hypothetical survival curves are exten<strong>de</strong>d to 100 years of age. The two shorter curves are<br />
Kaplan-Meier estimates for 65 year old men from the UK Heart Valve Registry data.<br />
1 Imaginile nu ne-au parvenit până la închi<strong>de</strong>rea ediţiei, dar se vor insera în numărul viitor<br />
15
1. Bonow RO, Carabello BA, Kanu C, et al. ACC/AHA 2006 gui<strong>de</strong>lines for the management<br />
of patients with valvular heart disease. Circulation 2006; 114:e84-231.<br />
2. Puvimanasinghe JP, Steyerberg EW, Takkenberg JJ, et al. Prognosis after aortic valve<br />
replacement with a bioprosthesis: predictions based on meta-analysis and<br />
microsimulation. Circulation 2001; 103:1535-1541.<br />
3. Puvimanasinghe JP, Takkenberg JJ, Edwards MB, et al. Comparison of outcomes after<br />
aortic valve replacement with a mechanical valve or a bioprosthesis using<br />
microsimulation. Heart 2004; 90:1172-1178.<br />
4. Rizzoli G, Mirone S, Ius P, et al. Fifteen-year results with the Hancock II valve: a multicenter<br />
experience. J Thorac Cardiovasc Surg 2006; 132:602-609.<br />
5. Brown ML, Schaff HV, Lahr BD, et al. Aortic valve replacement in patients aged 50 to 70<br />
years: improved outcome with mechanical versus biological prostheses. J Thorac<br />
Cardiovasc Surg 2008; 135:879-884.<br />
6. Lund O, Bland M. Risk-corrected impact of mechanical versus bioprosthetic valves on<br />
long-term mortality after aortic valve replacement. J Thorac Cardiovasc Surg 2006; 132:20-<br />
26.<br />
7. DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986; 7:177-188.<br />
8. Edmunds LH, Clark RE, Cohn LH, Grunkemeier GL, Miller DC, Weisel RD. Gui<strong>de</strong>lines for<br />
reporting morbidity and mortality after cardiac valvular operations. Ann Thorac Surg 1996;<br />
62:932-935.<br />
9. van <strong>de</strong>r Meer FJ, Rosendaal FR, Van<strong>de</strong>nbroucke JP, Briet E. Assessment of a blee<strong>din</strong>g risk<br />
in<strong>de</strong>x in two cohorts of patients treated with oral anticoagulants. Thromb Haemost 1996;<br />
76:12-16.<br />
10. Takkenberg JJ, Puvimanasinghe JP, Grunkemeier GL. Simulation mo<strong>de</strong>ls to predict<br />
outcome after aortic valve replacement. Ann Thorac Surg 2003; 75:1372-1376.<br />
11. Government Actuary Department. http://www.gad.gov.uk/Demography%5FData/ (9<br />
May 2008).<br />
12. Ruel M, Kulik A, Lam BK, et al. Long-term outcomes of valve replacement with mo<strong>de</strong>rn<br />
prostheses in young adults. Eur J Cardiothorac Surg 2005; 27:425-33.<br />
16
The 23-rd Annual Meeting of the<br />
European Association for Cardio-Thoracic Surgery<br />
Vienna, Austria, 17-21 October 2009<br />
Grigore Tinică, Diana Ciurescu<br />
University of Medicine and Pharmacy “Gr. T. Popa” Iasi, Cardiovascular Institute Iasi<br />
The 2009 Meeting of the EACTS was held in the Austrian capital of Vienna. It was atten<strong>de</strong>d<br />
by more than 3800 <strong>de</strong>legates – approximately 1700 adult cardiac surgeons and over 500 cardiothoracic<br />
surgeons – form around the world, eager to learn about programs focusing on novel<br />
therapies in cardiac and thoracic surgery. The conference provi<strong>de</strong>d an invigorating programme<br />
with a great number of high- quality presentations that covered both cardiovascular and thoracic<br />
topics.<br />
As ever, the first day hosted the TechnoCollege, which featured significant talks on the<br />
evolving technologies cardio-thoracic surgeons are facing. It offered a rich programme of<br />
Cardiac (inclu<strong>de</strong>d aortic surgery, mitral valve surgery, heart failure and the future of coronary<br />
surgery), Thoracic (entitled “Advances in chest wall surgery and osteosynthesis”, focused on<br />
anterior chest wall <strong>de</strong>formities, chest wall tumors, reconstruction and traumas: flail chest) and, for<br />
the first time <strong>de</strong>dicated one track of TechnoCollege to Congenital surgery (concentrated on<br />
hybrid set-ups in congenital heart disease and on the role of imaging in congenital heart<br />
diseases). For the first time this year TechnoCollege inclu<strong>de</strong>d not only adult cardiac and thoracic<br />
surgery but also a paediatric surgery course. The adult cardiac course focuses on aortic surgery,<br />
minimally invasive and transcatheter valve surgery and surgery for heart failure. It was a lively<br />
<strong>de</strong>bate on controversial topics for the treatment of aortic dissections such as the role of stenting of<br />
the <strong>de</strong>scen<strong>din</strong>g aorta and hemi versus full arch replacement as the method of choice.<br />
New approaches for mitral valve repair dominate the second session inclu<strong>din</strong>g a<br />
technique for echo gui<strong>de</strong>d beating heart mitral valve repair presented by Nikolay Vasilyev from<br />
Boston Children Hospital and a new sutureless annuloplasty system presented by Per Wierup from<br />
Aarhus.<br />
A number of vi<strong>de</strong>os expan<strong>de</strong>d the valve-in-valve transcatheter technique, the concepts<br />
for sutureless mitral valve repair and a radiofrequency adjustable mitral ring.<br />
The paediatric course focused on hybrid procedures and new imaging techniques such as<br />
DynaCT and 3D MRI for intraoperative guidance.<br />
This year were submitted 11 innovations and the 2009 TechnoCollege award went to Dr<br />
Edward Boyle, the foun<strong>din</strong>g CEO of Clear Catheter Systems and the co-inventor of the PleuraFlow<br />
Active Tube Clearance System. This novel <strong>de</strong>vice was <strong>de</strong>veloped by cardio-thoracic surgeons to<br />
keep chest drains clear after heart and lung surgery. It allows actively clearing of the internal<br />
diameter of a chest tube in a reproducible, sterile fashion, removing any obstructing or occlu<strong>din</strong>g<br />
material towards the drainage canister. A gui<strong>de</strong> tube is connected between the implanted chest<br />
tube and a blood connection canister. Within the gui<strong>de</strong> tube there is a gui<strong>de</strong> wire with a loop set<br />
at 90 <strong>de</strong>grees that can be advanced in and out of the tube to clear any occlu<strong>din</strong>g material such<br />
as clot. The external and internal magnet coupling is the key innovation making this <strong>de</strong>vice very<br />
simple while maintaining this sterile environment within the tubing. A first in man feasibility testing is<br />
planned for late 2009 with an anticipated commercial launch in early, <strong>2010</strong>.<br />
The first day of meeting consisted of a series of post-graduated courses on a wi<strong>de</strong> range of<br />
topics, inclu<strong>din</strong>g the key areas in adult cardiac – entitled “Cardiovascular interventions in the<br />
el<strong>de</strong>rly”; in thoracic surgery, congenital surgery – which incorporated a multi-disciplinary panel<br />
that discussed the transposition of great arteries, tracheo bronchial stenosis and an interactive<br />
17
vi<strong>de</strong>o session focusing on surgery for complete atrio-ventricular canal; in vascular surgery – with a<br />
specific focus on aortic disease, open and endovascular repair; in perfusion – where it examined<br />
the role of arterial embolism during cardiopulmonary bypass, haemostasis and anticoagulation;<br />
with a closer look at minimized bypass circuits, cardio-pulmonary bypass in non-cardiac surgery<br />
and left heart assist <strong>de</strong>vices; in basic science – looking at the pathophysiology and metabolic<br />
aspects of heart failure, as well as the impact of stem cells in future of heart transplantation and<br />
myocardial restructuring.<br />
The congress officially opened on the following day with the presi<strong>de</strong>ntial address by Enrino<br />
Ren<strong>din</strong>a, the EACTS presi<strong>de</strong>nt (Rome, Italy), one of the keynote lectures “In the name of the<br />
muse” on “quality in education and education to quality” and the importance of continuing<br />
learning and spen<strong>din</strong>g a lifetime in a profession that never fails to rejuvenate one’s enthusiasm.<br />
The meeting honoured guest lecture was that of Luigi Frati, Rome, Italy, entitled<br />
“Regenerative medicine, a look to the future” – stem cell based regenerative therapy is<br />
un<strong>de</strong>rgoing experimental and clinical trials in or<strong>de</strong>r to prevent or limit the consequences of<br />
<strong>de</strong>creased contractile function and compliance of damaged ventricles/hearts following<br />
myocardial infarction or in patients presenting non ischaemic dilated cardiomyopathies. In fact,<br />
several technologies have been <strong>de</strong>scribed over the past ten years to create a functional<br />
myocardium mainly by using bone-marrow <strong>de</strong>rived cells, but they turn a fibroblastic not functional<br />
fate when are injected into the heart. This group <strong>de</strong>scribed and patented a method to obtain<br />
contractile cardiospheres from adult mouse and human hearts: an increase of physiological<br />
functions has been observed following the injection of these cells into the heart of infracted mice.<br />
This year’s cardiac surgery sessions have been <strong>de</strong>signed to bring the latest evi<strong>de</strong>nce and<br />
technological <strong>de</strong>velopments and issues affecting contemporary practice.<br />
The session grafts in cardiac surgery discussed the latest results from several cases series,<br />
scoring systems for predicting graft patency, as well as utilizing with MDCT for assessing graft<br />
patency.<br />
Michael Mack discussed the lessons learned from coronary surgery and future implications:<br />
After five years of steady <strong>de</strong>cline, the number of coronary artery bypass procedures<br />
appears to have reached a plateau and in some areas of the world are actually increasing.<br />
The outcomes of a number of recent trials inclu<strong>din</strong>g SYNTAX, BARI 2D and the Endoscopic<br />
Vein Harvest substudy of the PREVENT IV Trial are likely to have some impact on the practice of<br />
coronary surgery. The results from FREEDOM Trial comparing CABG and PCI in multi-vessel disease<br />
in diabetics and a soon to be initiated trial in left main disease may also further <strong>de</strong>fine the role of<br />
surgery.<br />
The SYNTAX Trial enrolled 1800 patients in 83 centers in Western Europe and the US. The<br />
results at two years continue to favour CABG compared with PCI in patients with LM or 3VD.<br />
MACCE was 23.3% with PCI vs. 16.3% with CABG (p=0.0003).<br />
The BARI 2D trial compared a strategy of immediate revascularization by either CABG or<br />
PCI at investigator discretion to an initial approach of medical therapy in diabetic patients.<br />
The PREVENT IV study was a randomized study of 24000 patients un<strong>de</strong>rgoing CABG in 2002-<br />
3 treated with a <strong>de</strong>coy to prevent intimal hyperplasia in saphenous vein grafts. A recently<br />
published non-randomised substudy of this trial revealed that harvest of saphenous vein grafts by<br />
an Endoscopic technique was associated with a higher graft failure rate and <strong>de</strong>ath at three years<br />
compared with open harvest. This has not been confirmed in a randomized trial but all aspects of<br />
the Endoscopic harvest technique are now being re-examined.<br />
The FREEDOM trial of CABG vs. PCI with drug-eluting stent in diabetics is nearing<br />
completion of enrolment (December 2009). The primary endpoint of two-year <strong>de</strong>ath, stroke,<br />
myocardial infarction will be reached in 2011 with results available in 2012.<br />
18
Highlighted transfemoral and transapical aortic valve implantation, and the early results<br />
from the SOURCE registry and one-year follow-up results from the TRAVERCE clinical trial.<br />
Anson Cheung (St. Paul’s Hospital, Vancouver, Canada) showed that there is an<br />
expan<strong>din</strong>g population of complex and high-risk el<strong>de</strong>rly patients with prosthetic valve dysfunction<br />
who require redo procedures. The group from Vancouver had successfully treated patients with<br />
prosthetic valve dysfunctions in the aortic, mitral and tricuspid position, using Edwards Sapien<br />
transcatheter valve. They had successfully performed twelve transcatheter valve-in-valve<br />
implantations – five aortic, six mitral and one tricuspid.<br />
Saibal Kar (Cedars Sinai Medical Center, Los Angeles, USA) showed that the double orifice<br />
technique of mitral valve repair using the MitraClip system is effective in selected patients with<br />
functional or <strong>de</strong>generative mitral regurgitation. Over 700 patients have been treated with the<br />
MitraClip system in North America and Europe. Data from the initial cohort and the high risk<br />
registry support safety, efficacy and sustained clinical benefit in majority of patients. In addition<br />
there is evi<strong>de</strong>nce of favourable remo<strong>de</strong>ling of the left ventricle. Surgical options were preserved in<br />
patients who required a re-intervention following a MitraClip procedure. The EVEREST II<br />
randomised clinical trial has completed enrollment, and clinical results will be available next year.<br />
Robotic mitral valve repair of a complex bileaflet prolapse (Barlow’s), a new technique of<br />
chordal replacement for mitral valve plasty with multiple loops with one knot technique and mitral<br />
valve repair; ‘respect rather than resect’ technique.<br />
Ottavio Alfieri (S.Raffaele University Hospital, Milan, Italy) says that the radiofrequency<br />
adjustable mitral valve ring seems to be a useful new tool in the surgical armamentarium for mitral<br />
valve repair. The MiCardia adjustable ring is activated using a removable epicardial lead that<br />
<strong>de</strong>livers radiofrequency energy from an external generator. To date, it has been implanted in 31<br />
patients affected either by <strong>de</strong>generative or ischaemic mitral insufficiency, enrolled in the DYNA<br />
study, which is currently ongoing. Six beating heart activations have been successfully carried out<br />
in humans to correct some <strong>de</strong>gree of postoperative mitral incompetence. The concept of<br />
reversible adjustment is potentially of great utility, because the possibility of increasing the anteroposterior<br />
dimension of the prosthetic ring allows correction of post-operative SAM.<br />
Rafael Garcia Fuster (University General Hospital of Valencia, Spain) conclu<strong>de</strong>d that<br />
preservation of annulo-ventricular continuity through the chordae ten<strong>din</strong>ae is an important<br />
<strong>de</strong>terminant of post-operative left-ventricular function and survival after mitral valve surgery for<br />
mitral valve insufficiency. Valve repair is the procedure of choice, but when valve replacement is<br />
inevitable, every effort should be ma<strong>de</strong> to preserve both anterior and posterior chordopapillary<br />
apparatus.<br />
Antonio Grimaldi and Ottavio Alfieri (University Vita-Salute, San Raffaele, Scientific Institute,<br />
Milan, Italy) show that restrictive annuloplsty for functional mitral regurgitation can potentially<br />
reduce mitral leaflet opening without creating a clinically relevant mitral stenosis or an impaired<br />
cardiac adaptation to exercise and further studies will be necessary to test the clinical impact of<br />
un<strong>de</strong>rsized rings in larger populations.<br />
The session discussing the transposition of the great arteries and related lesions studied<br />
outcomes from double switch operations for atrio-ventricular discordance, and ask whether the<br />
length between the top of the interventricular septum and the aortic valve on indications for a<br />
biventricular repair impacts on outcomes; the <strong>de</strong>legates had the chance to learn about<br />
biventricular repair of complex left ventricular outflow tract obstruction in neonates and infants;<br />
the surgical management of congenital heart <strong>de</strong>fects associated with heterotaxy syndrome; as<br />
well as the results from a 30-year, nationwi<strong>de</strong> population-based study, examining mortality among<br />
Danish congenital heart <strong>de</strong>fects patients diagnosed before one year of age.<br />
19
Assessing the technical evolution of acute-type A dissection, as well as technological<br />
enhancements such as MDCT- based intra-operative navigation system for thoraco-abdominal<br />
aortic aneurysm repair. The vascular section examined aortic dissection with a examination of<br />
branched open stent grafting technique for reoperation after repaired type A dissection and<br />
asses the long-term results of hybrid endovascular repair for thoracoabdominal aortic aneurysms.<br />
William Wang (Scripps Memorial Hospital, La Jolia, USA) conclu<strong>de</strong><strong>de</strong> that significantly<br />
enlarged atria should be reduced by utilizing an aggressive biatrial reduction with reef imbricate<br />
suture technique concomitantly with a full Cox maze procedure for AF.<br />
Kazuo Yamanaka (Tenri Hospital, Nara, Japan) showed that left atrial appendage<br />
preservation contributed to improved total booster function of left atrium and left atrial<br />
appendage without stroke and systemic embolic events in patients with sinus rhythm after the<br />
Maze procedure for chronic AF and mitral valve disease.<br />
Interact CardioVasc Thorac Surg 2009; 9:S57-S119.<br />
doi:10.1510/icvts.2009.0000S7© 2009 Abstracts. Suppl. 2 to Vol. 9 (October 2009)<br />
20
Joi 30 septembrie <strong>2010</strong>,<br />
Restaurant Hotel Hilton<br />
19:00 ��Deschi<strong>de</strong>rea festivă<br />
Vineri 1 octombrie <strong>2010</strong><br />
Sala Diamond Sala Saphire Sala Ruby<br />
CORD CHIRURGIE VASCULARĂ<br />
SESIUNEA I: Transplant cardiac.<br />
Chirurgia valvelor cardiace<br />
Mo<strong>de</strong>ratori: Radu Deac, Marcus<br />
Kamler, Vlad Iliescu<br />
09:00 – 11:00 �<br />
SESIUNEA V<br />
Mo<strong>de</strong>ratori: Ş. Rădulescu,<br />
G. Szendro, J-Baptiste Ricco -<br />
10:45 – 11:00 – Discuţii 10:50 – 11:00 - Discuţii<br />
Sesiunea II: Tumorile Cardiace,<br />
complicaţii ale chirurgiei<br />
cardiace<br />
Mo<strong>de</strong>ratori: Traian Scridon,<br />
Reinhard Moidl, I. Maniţiu<br />
11:00-11:30, Pauza <strong>de</strong> cafea<br />
11:30 – 13:30 �<br />
Sesiunea VI:<br />
Mo<strong>de</strong>ratori: Marina Păcescu, F.<br />
Spineli, P. Bergeron -<br />
13:00 – 13:30 - Discuţii 13:15 – 13:30 - Discuţii<br />
13:30 – 14:30 Masa <strong>de</strong> prânz ��<br />
14:30-17:00 �<br />
Sesiunea III:<br />
Chirurgia valvei aortice<br />
Mo<strong>de</strong>ratori: Gelu Cerin, Gunter<br />
Laufer, Guido Lanzilo, M. Laskar<br />
16:30-17:00 Pauza <strong>de</strong> cafea<br />
17:00 – 18:00 - Sesiunea IV<br />
Chirurgia valvei mitrale,<br />
endocardita bacteriană<br />
14:30-15:30 Sesiunea VII:<br />
Mo<strong>de</strong>rator: I. Droc<br />
SIMPOZION VASAPROSTAN<br />
15:30 – 15:50 Sesiunea VII:<br />
Mo<strong>de</strong>rator: I. Droc<br />
15:50 – 16:00 - Discuţii<br />
16:00-16:30 Pauza <strong>de</strong> cafea<br />
16:30-17:00 - Sesiunea VIII:<br />
Mo<strong>de</strong>ratori: Ş. Rădulescu, I. Droc<br />
17:00-18:00 �<br />
Sesiunea VIII:<br />
Mo<strong>de</strong>ratori: Ş. Rădulescu, I. Droc<br />
21<br />
-<br />
Adunare Generală<br />
SRCCV
Mo<strong>de</strong>ratori: Grigore Tinică,<br />
Batrinac A., Moscalu V.<br />
18:00 – 18:30 - Sesiunea IV<br />
Chirurgia valvei mitrale,<br />
endocardita bacteriană<br />
Mo<strong>de</strong>ratori: Grigore Tinică,<br />
Batrinac A., Moscalu V.<br />
18:30 – 19:00 - Discuţii<br />
18:00-19:00 �<br />
22<br />
- -<br />
ORA 20:00 - �� Cina Festivă - Restaurant Hotel Hilton<br />
Sâmbătă 2 octombrie <strong>2010</strong><br />
Sala Diamond Sala Saphire Sala Ruby<br />
CORD<br />
Sesiunea IX:<br />
Chirurgia arterelor coronare<br />
Mo<strong>de</strong>ratori: Gerard Bloch, H.<br />
Moldovan, Tintoiu I.<br />
Simpozionul Societăţii<br />
Române <strong>de</strong> Anestezie-Terapie<br />
Intensivă Cardiacă şi<br />
Tehnologie Extracorporeală<br />
(SRATICTE)<br />
09:00 – 11:00 �<br />
Sesiunea XII: Anemia si transfuzia in<br />
chirurgia cardiaca<br />
Mo<strong>de</strong>rator: Ioan Vlad<br />
Sesiunea XIII<br />
Mo<strong>de</strong>rator: Victor Diaconescu<br />
CONGENITALI<br />
Sesiunea XVI<br />
Mo<strong>de</strong>ratori: Horaţiu Suciu,<br />
Andrei Iosifescu, Chira<br />
Manuel<br />
10:45 – 11:00 – Discuţii 10:50 – 11:00 - Discuţii 10:40 – 11:00 - Discuţii<br />
Sesiunea X<br />
Mo<strong>de</strong>ratori: Tintoiu I.,<br />
R. Deac, G. Tinica<br />
11:00-11:30, Pauza <strong>de</strong> cafea<br />
11:30 – 13:30 �<br />
Sesiunea XIV: Siguranţa pacientului<br />
în timpul circulaţiei extracorporeale<br />
Mo<strong>de</strong>ratori: Dan Longrois (Paris) şi<br />
Daniela Filipescu<br />
Sesiunea XVII<br />
Mo<strong>de</strong>ratori: Chira Manuel,<br />
Mariana Andreica, Rodica<br />
Manasia, Angela Butnariu<br />
13:20 – 13:30 - Discuţii 13:00 – 13:30 - Discuţii 13:00 – 13:30 - Discuţii<br />
13:30 – 14:30 Masa <strong>de</strong> prânz ��<br />
Sesiunea XI<br />
Mo<strong>de</strong>ratori: Horia Mureşan,<br />
P. Bergeron, Şerban Stoica<br />
14:30-17:00 �<br />
Sesiunea XV<br />
Mo<strong>de</strong>ratori:<br />
Ion Miclea, Mihai Luchian<br />
16:15 – 17:00 - Discuţii 16:30 – 17:00 - Discuţii<br />
17:00-17:30 Pauza <strong>de</strong> cafea<br />
14:30-15:30<br />
NURSING<br />
ORA 17:30 - Îmbarcarea la Hotel Hilton, pentru plecarea la Baza <strong>de</strong> tratament Bazna<br />
ORA 19:00 - �� Cina Festivă - Restaurant Expro, Baza <strong>de</strong> tratament Bazna
Vineri 1 octombrie <strong>2010</strong><br />
Sala Diamond<br />
Grupul <strong>de</strong> lucrări « CORD »<br />
Sesiunea I<br />
Transplant cardiac. Chirurgia valvelor cardiace<br />
Mo<strong>de</strong>ratori: Radu Deac, Marcus Kamler, Vlad Iliescu<br />
ORA AUTORI TITLUL LUCRĂRII<br />
09.00 – Deac Radu, Suciu H.<br />
Actualităţi în transplantarea cardiacă - <strong>2010</strong>.<br />
09.15<br />
IUBCVT Tg. Mureş. CCV I Update in cardiac transplantation - <strong>2010</strong><br />
Zece ani <strong>de</strong> transplantare cardiacă la IUBCVT Tg.<br />
09.15 –<br />
Mureş 1999-<strong>2010</strong>.<br />
09.30<br />
Ten years of heart transplantation at IUBCVT Tg.<br />
Mureş 1999-<strong>2010</strong><br />
09.30 –<br />
09.40<br />
09.40 –<br />
10.00<br />
10.00 –<br />
10.15<br />
10.15 –<br />
10.30<br />
10.30 –<br />
10.45<br />
Suciu Horaţiu, Deac R., Mihaela Ispas, Anca<br />
Sin, Cotoi O., Matei M., Opriş C., Mihaela<br />
Melinte, Terezia Preda<br />
IUBCVT Tg. Mureş<br />
Vlad Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “Prof Dr.<br />
C.C.Iliescu” Bucureşti<br />
Marian Gaspar<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
Markus Kamler<br />
Institutul Inimii Hilarion, Essen<br />
V. Saplacan, C. Ivascau, F. Dugenet, M<br />
Massetti<br />
University Hospital of Caen, France<br />
23<br />
Reconstrucţia valvelor atrioventriculare - între<br />
teorie şi practică<br />
Chirurgia valvulară: progres şi realitate<br />
Valvular surgery, between progres and reality.<br />
Chirurgia minim invazivă a valvei mitrale<br />
ECLS în şocul cardiogen şi stopul circulator<br />
ECLS in cardiogenic shock and cardiac arrest<br />
Baza <strong>de</strong> date a Societăţii Europene <strong>de</strong> Chirurgie<br />
Cardio-Toracică<br />
10.45 – 11.00 Discuţii<br />
11.00 – 11.30 Coffe Break<br />
Sesiunea II<br />
Tumorile Cardiace, complicaţii ale chirurgiei cardiace<br />
Mo<strong>de</strong>ratori: Traian Scridon, Reinhard Moidl, I. Maniţiu<br />
ORA AUTORI TITLUL LUCRĂRII<br />
11.30 –<br />
11.45<br />
11.45 –<br />
12.00<br />
12.00 –<br />
12.10<br />
12.10 –<br />
12.20<br />
12.20 –<br />
12.30<br />
12.30 –<br />
12.40<br />
Traian Scridon<br />
Institutul Inimii “ N. Stăncioiu” Cluj-Napoca<br />
Manolache Gh, Batrinac A., Moscalu V, Ureche<br />
A., Morozan V., Turcanu G, Barnaciuc S., Ghicavii<br />
N.<br />
Institute of Cardiology, Republic of Moldova<br />
I. Maniţiu, Gabriela Eminovici, Minodora Teodoru,<br />
Rodica Moga, Ruxandra Dobrin, C. Balan<br />
Spitalul Clinic Ju<strong>de</strong>ţean Sibiu<br />
Lucian Stoica, Eugen Bitere, Laurenţiu Gafencu,<br />
Dumitrita-Alina Gafencu<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong> Boli<br />
Cardiovasculare “ Prof Dr. George I.M. Georgescu”, Iaşi<br />
L.F. Dorobanţu, O. Stiru, A. Pro<strong>de</strong>a, A. Georgescu,<br />
Daniela Filipescu, V.A. Iliescu<br />
Clinica <strong>de</strong> Chirurgie Cardiovascularã, Institutul <strong>de</strong> Boli<br />
Cardiovasculare "Prof. Dr. C.C. Iliescu", Bucureşti<br />
Minodora Teodoru, I. Maniţiu, Gabriela Eminovici,<br />
Rodica Moga, C. Balan, Raluca Matei, Cristina<br />
Chircu<br />
Spitalul Clinic Ju<strong>de</strong>ţean Sibiu<br />
Tumori cardiace<br />
The strategies in diagnosis and surgical<br />
treatment of heart tumors<br />
Rolul ecografiei în diagnosticul şi rezolvarea<br />
chirurgicală a tumorilor cardiace<br />
Chist hidatic cardio-pericardic.<br />
Cardiopericardic hydatid cyst<br />
Caz unic <strong>de</strong> histiocitom fibros malign <strong>de</strong><br />
ventricul drept cu implantare la nivelul<br />
ban<strong>de</strong>letei mo<strong>de</strong>ratoare<br />
Particularităţi ale cazurilor <strong>de</strong><br />
trombembolism pulmonar în experienţa<br />
Clinicii <strong>de</strong> Cardiologie Sibiu
12.40 –<br />
12.50<br />
12.50 –<br />
13.00<br />
Reinhard Moidl<br />
Department of Cardiothoracic Surgery,<br />
University of Vienna, Vienna, Austria<br />
Prisăcaru I, Ureche A., Turcanu G., Manolache<br />
Gh., Moscalu V., Batrinac A.<br />
Institute of Cardiology, Chişinău, Republic of Moldova<br />
24<br />
Treatment of <strong>de</strong>ep sternal wound<br />
infections with V.A.C. Therapy<br />
Treatment of sternal <strong>de</strong>hiscence after heart<br />
operation<br />
13.00 – 13.30 Discuţii<br />
13.30 – 14.30 Pauza <strong>de</strong> prânz<br />
Sesiunea III<br />
Chirurgia valvei aortice<br />
Mo<strong>de</strong>ratori: Gelu Cerin, Gunter Laufer, Guido Lanzilo, M. Laskar<br />
ORA AUTORI TITLUL LUCRĂRII<br />
14.30 –<br />
14.45<br />
Horia Muresian<br />
The University Hospital of Bucharest<br />
Anatomia chirurgicală a rădăcinii aortei<br />
14.45 –<br />
15.00<br />
15.00 –<br />
15.20<br />
15.20 –<br />
15.40<br />
15.40 –<br />
15.50<br />
15.50 –<br />
16.00<br />
16.00 –<br />
16.10<br />
16.10 –<br />
16.20<br />
16.20 –<br />
16.30<br />
Gelu Cerin<br />
Cardiology Unit in Cardiac Surgery Dpt. San Gau<strong>de</strong>nzio<br />
Clinic, Novara, Italy<br />
C. Lanzilo, Marco Diena<br />
Cardiac Surgery Dpt. San Gau<strong>de</strong>nzio Clinic,<br />
Novara, Italy, Novara, Italy<br />
Gunther Laufer<br />
Univ.-Klinik für Chirurgie, Klin, Viena- Austria<br />
Marian Gaspar, Gunther Laufer, Călin Jusca,<br />
Daniel Nica, Ionel Droc, Petre Deutsch<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
M Laskar*, C. Eveno*, T. Bourguignon**, A.<br />
Piccardo***, L. Roussel***, E. Bergoend**, M.<br />
Aupart**, E. Cornu*, T. Caus***, M. Marchand**.<br />
* CHU Dupuytren, ** Hôpital Trousseau,<br />
*** Hôpital Sud<br />
Moscalu V., Batrinac A, Manolache gh., Ureche A,<br />
Turcan Gr., Morozan V., Barnaciuc S., Voitov S.,<br />
Ghicavii N.,. Guzgan Iu.<br />
Institute of Cardiology, Cardiac Surgery Departament,<br />
Chisinau, Republic of Moldova<br />
Dumitraşcu George<br />
Spitalul Militar <strong>de</strong> Urgenţă Sibiu<br />
Wich patients for aortic valve repair? Role<br />
of Echocardiography<br />
Aortic valve repair – when and how to do<br />
it?<br />
Progres in aortic valve surgery<br />
“Homograft – ROSS operation, Timişoara,<br />
experience 1997 – <strong>2010</strong>”<br />
Remplacement valvulaire aortique<br />
conventionnel chez le sujet <strong>de</strong> plus <strong>de</strong> 85<br />
ans. Resultants a court et long terme a<br />
propos d’une serie <strong>de</strong> 164 patients operes.<br />
Conventional aortic valvular replacement<br />
in patients over 85. Short and long term<br />
results about 164 patients<br />
Functional principle in <strong>de</strong>termining the<br />
assessment criteria for valvular aortic<br />
reconstructive correction<br />
Cătălin Constantin Badiu, Walter Eichinger, Sabine<br />
Stenoza aortică severă asimptomatică –<br />
festina lente?<br />
Should root replacement with aortic valve-<br />
Bleiziffer, Grit Hermes, Ina Hettich, Bernhard Voss, sparing be offered to patients with severe<br />
Robert Bauernschmitt, Rudiger Lange.<br />
aortic regurgitation or bicuspid aortic<br />
German Heart Centre Munich, Munich, Germany valves?<br />
16.30 – 17.00 Coffe Break<br />
Sesiunea IV<br />
Chirurgia valvei mitrale, endocardita bacteriană<br />
Mo<strong>de</strong>ratori: Grigore Tinică, Batrinac A., Moscalu V.<br />
ORA AUTORI TITLUL LUCRĂRII<br />
17.00 –<br />
17.15<br />
17.15 –<br />
17.30<br />
B. Radulescu, R. Vasile, A. Vasilescu, Luminiţa<br />
Iliuta, Y. Hashem, A. Mărginean, D. Filipescu, H.<br />
Moldovan, V. Iliescu<br />
Boli Cardiovasculare « Prof. Dr. C.C. Iliescu », Bucureşti<br />
Batrinac Aureliu, Moscalu V, Manolache gh.,<br />
Ureche A, Morozan V., Guzgan Iu., Voitov S.,<br />
Tratamentul chirurgical al endocarditei<br />
bacteriene <strong>de</strong> rădăcină aortică<br />
Correction of ischemic mitral valve<br />
regurgitation with a new method of
17.30 –<br />
17.45<br />
17.45 –<br />
18.00<br />
18.00 –<br />
18.10<br />
18.10 –<br />
18.20<br />
18.20 –<br />
18.30<br />
Barnaciuc S., Vitalie V. Moscalu<br />
Institute of Cardiology, Cardiac Surgery Departament,<br />
Chişinău, Republic of Moldova<br />
Moscalu Vitalie, Batrinac A., Manolache Gh.,<br />
Ureche A, Ghicavii N., Manolache S., Moscalu V.<br />
Institute of Cardiology, Heart Surgery Department,<br />
Chişinău, Republic of Moldova<br />
Dumitrasciuc G., Nica D., Feier H., Jusca C.,<br />
Cioata D., Ionac A,. Merce A., Gaspar M.<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
Grigore Tinică, Mihail Enache, Diana Ciurescu,<br />
Alexandru Ciucu, Oana Bartoş, Daniel<br />
Dăscălescu, Victor Diaconescu, Sânziana<br />
Patrulea, Bogdan Aparaschivei<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong> Boli<br />
Cardiovasculare “ Prf Dr. George I. M. Georgescu”, Iaşi<br />
Kovacs Judit, Jung Janos, Simona Gurzu, Azamfirei<br />
L., Sanda-Maria Copotoiu, Baloş Sorin, Suciu H.,<br />
Ruxandra Copotoiu, Mezei T.<br />
IUBCVT, Morphopathology, SCJM, Tg. Mureş<br />
Batrinac A., Morozan V., Ureche A., Manolache<br />
Gh., Voitov S., Barnaciuc S., Ghicavii N., Guzgan<br />
Iu., Moscalu V.<br />
Institute of Cardiology, Cardiac Surgery Departament,<br />
Chişinău, Republic of Moldova<br />
25<br />
annuloplasty<br />
18.30 – 19.00 Discuţii<br />
Prevention of systolic anterior motion (SAM)<br />
after mitral valve repair<br />
Aspecte ale chirurgiei valvei mitrale la<br />
pacienţii cu disfuncţie sistolică a<br />
ventriculului stâng<br />
Mitral valve surgery in patients with left<br />
ventricular systolic disfunction.<br />
Sala Saphire<br />
Grupul <strong>de</strong> lucrări « CHIRURGIE VASCULARĂ »<br />
Revascularizarea arterei coronare drepte.<br />
Certitu<strong>din</strong>i şi controverse.<br />
Right coronary artery revascularization.<br />
Certainty and controversy.<br />
Pancreatita acută după intervenţii<br />
chirurgicale cardiace.<br />
Acute pancreatitis after cardiac surgery<br />
An adjunctive procedure for surgical left<br />
ventricular remo<strong>de</strong>ling using papillary<br />
muscle sling<br />
Sesiunea V<br />
Mo<strong>de</strong>ratori: Ş. Rădulescu, G. Szendro, J-Baptiste Ricco<br />
ORA AUTORI TITLU<br />
09.00 –<br />
09.15<br />
09.15 –<br />
09.30<br />
09.30 –<br />
09.45<br />
09.45 –<br />
10.00<br />
10.00 –<br />
10.10<br />
10.10 –<br />
10.20<br />
10.20 –<br />
10.35<br />
10.35 –<br />
10.50<br />
Rădulescu Şerban<br />
Spitalul Clinic Ju<strong>de</strong>ţean <strong>de</strong> Urgenţă, Universitatea <strong>de</strong><br />
Medicină şi Farmacie "Iuliu Haţieganu", Cluj-Napoca,<br />
Chirurgie II<br />
Gabriel Szendro - Conferinţă<br />
Department of Vascular Surgery, Soroka Medical<br />
Center, Beer Sheva, Israel<br />
Sorin Băilă<br />
Institutul <strong>de</strong> Boli Cardiovasculare “C.C. Iliescu”<br />
Bucureşti<br />
Horia Mureşian<br />
Horia Mureşian<br />
The University Hospital of Bucharest<br />
The University Hospital of Bucharest<br />
Horia Mureşian<br />
The University Hospital of Bucharest<br />
Jean-Baptiste Ricco<br />
University of Poitiers, France<br />
Jean-Baptiste Ricco<br />
University of Poitiers, France<br />
10.50 – 11.00 Discuţii<br />
Chirugia vasculară – Ten<strong>din</strong>ţe actuale în<br />
<strong>Romania</strong><br />
Minimally invasive new technique for fempop<br />
bypass<br />
Locul endarterectomiei <strong>de</strong> artera carotidă<br />
în tratamentul stenozelor critice carotidiene<br />
simptomatice şi asimptomatice<br />
Aneurysm of aberrant right subclavian<br />
artery, Kommerell diverticulum and common<br />
carotid trunk-single stage surgical repair<br />
without cardiopulmonary bypass<br />
Simultaneous bilateral carotid<br />
endarterectomy personal experience in 90<br />
patients<br />
The surgery for vertebro-basilar arterial<br />
insufficiency<br />
Carotid surgery: actual strategy<br />
How to write a paper in cardiovascular<br />
surgery
11.00 – 11.30 Coffe Break<br />
Sesiunea VI<br />
Mo<strong>de</strong>ratori: Marina Păcescu, F. Spineli, P. Bergeron<br />
ORA AUTORI TITLU<br />
11.30 –<br />
11.45<br />
11.45 –<br />
12.00<br />
12.00 –<br />
12.10<br />
12.10 –<br />
12.20<br />
12.20 –<br />
12.30<br />
12.30 –<br />
12.40<br />
12.40 –<br />
12.50<br />
12.50 –<br />
13.00<br />
13.00 –<br />
13.15<br />
Francesco Spinelli, Francesco Stilo, Filippo<br />
Bene<strong>de</strong>tto, Giovanni De Caridi, Michele La<br />
Spada.<br />
Unit of Vascular Surgery, Department of<br />
Cardiovascular and Thoracic Surgery, University of<br />
Messina, Italy<br />
Marina Păcescu, S. Băilă, DF Barzoi, R. Halpern,<br />
Mădălina Gavanescu<br />
Department of Vascular Surgery, “C.C. Iliescu”<br />
Emergency Institute of Cardiovascular Disease,<br />
Bucharest<br />
Claudia Gherman, H. Silaghi, Anca Cristea B.<br />
Olaru, F. Deme, A. Oprea, S. Rădulescu, A.<br />
Mironiuc<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
Claudia Gherman, Ioana Constantinescu, H.<br />
Silaghi, B. Stancu, B. Olaru, F. Deme, A. Eni, S.<br />
Rădulescu, A. Mironiuc, D. Pamfil, Ioana<br />
Petricele, Iulia Pop<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
I. Droc, Pinte Fl., Călinescu F., Deaconu St., Niţă<br />
A, Dumitraşcu M., Popovici A.<br />
Centrul clinic <strong>de</strong> urgenţă <strong>de</strong> boli cardiovasculare “Dr.<br />
Constantin Zamfir”, Bucureşti<br />
S. Rădulescu, A. Zanfir, C Gherman<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
NJ Tesoiu, Marina Păcescu, SL Băilă, DF Barzoi, I.<br />
Diaconescu, F Coşa, R. Halpern, Isabella Oprea,<br />
Mirela Marcu, A<strong>din</strong>a Stoica, M. Croitoru, Daniela<br />
Mitcov<br />
Institutul <strong>de</strong> Boli Cardiovasculare “C. C. Iliescu”<br />
Bucureşti<br />
Grigore Tinică*, Mihail Enache*, Diana<br />
Ciurescu**, Vasile Cepoi***, Andrei Dumbravă**,<br />
Vasile Astarastoae*<br />
*University of Medicine<br />
and Pharmacy “Gr. T. Popa” Iaşi<br />
**Cardiovascular Institute, Iaşi<br />
***Clinical and Experimental Cardiovascular Research<br />
Foundation<br />
D. Trandafir, Silvia Condu, R. Nechifor*, B.<br />
Dorobat*, Cristina Tudor**, Ana Filimon<br />
Department of Cardiovascular Surgery<br />
* Department of Radiology<br />
** Department of Anesthesiology University Hospital of<br />
Bucharest<br />
13.15 – 13.30 Discuţii<br />
26<br />
An aggressive treatment improves midterm<br />
survival and amputation- free survival in CLI<br />
patient<br />
Standard of care for popliteal Artery<br />
Aneurysm<br />
Aprecieri asupra rolului adipocitokinelor<br />
“cheie” în iniţierea şi progresia leziunilor<br />
ateromatoase <strong>din</strong> afecţiunile vasculare<br />
periferice.<br />
Consi<strong>de</strong>rations on the role of the “key”<br />
adipocytokines in the initiation and<br />
pregression of atherosclerotic lesions on<br />
peripheral arterial disease<br />
Aportul genomilor în studiul aplicării unor<br />
gene în afecţiuni arteriale periferice.<br />
Contribution of genomics in studies that<br />
involves the gehes in peripheral arterial<br />
disease<br />
Management of critical limb ischemia<br />
Complicaţii postoperatorii în chirurgia<br />
convenţională a bolii varicoase.<br />
Postoperative complications in the<br />
conventional surgery of varicose vein<br />
disease<br />
Patologia cardiovasculară asociată şi<br />
rezultatele imediate în trombembolectomia<br />
arterială chirugicală pentru ischemia acută<br />
a membrului superior – 10 ani <strong>de</strong><br />
experienţă.<br />
Cardiovascular Un<strong>de</strong>rlying pathology and<br />
early results în surgical arterial<br />
thromboembolectomy for upper limb acute<br />
ischemia - 10 years experience<br />
Educarea interesului pentru chirurgia<br />
cardiovasculară la stu<strong>de</strong>nţii medicinişti la<br />
şcoala <strong>de</strong> vară.<br />
Raising medical stu<strong>de</strong>nts interest in<br />
cardiovascular surgery through surgery<br />
summer school<br />
The use of aortic iliac endovascular<br />
prothesis for infrarenal abdominal aortic<br />
aneurysm – case report
13.30 – 14.30 Pauza <strong>de</strong> masă<br />
Sesiunea VII<br />
Mo<strong>de</strong>rator: I. Droc<br />
ORA AUTORI TITLU<br />
14.30 –<br />
15.30<br />
15.30–<br />
15.40<br />
15.40 –<br />
15.50<br />
Simpozion Vasaprostan<br />
I. Droc, Pinte Fl, Cristian G, Dumitraşcu M.,<br />
Deaconu St., Călinescu F, Murgu V.<br />
Centrul clinic <strong>de</strong> urgenţă <strong>de</strong> boli cardiovasculare “Dr.<br />
Constantin Zamfir”, Bucureşti<br />
Daniel Nica, M. Gaşpar, P. Deutsch, D. Cioata,<br />
C. Juşca, G. Dumitraşciuc, H. Feier, A. Merce, A.<br />
Ionescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara, Clinica <strong>de</strong><br />
Chirurgie Cardiovasculară II<br />
27<br />
Chirurgie clasică versus endovasculară în<br />
tratamentul anevrismului <strong>de</strong> aortă<br />
abdominală.<br />
Open Surgery versus endovascular<br />
treatment for abdominal aortic aneurysms<br />
Abordarea chirurgicală a anevrismelor <strong>de</strong><br />
aortă abdominală: experienţa clinică ian.<br />
2003- <strong>de</strong>c. 2009. Surgical approach of<br />
abdominal aortic aneurysms: clinical<br />
experience ian 2003- <strong>de</strong>c 2009<br />
15.50 – 16.00 Discuţii<br />
16.30 – 17.00 Coffe Break<br />
Sesiunea VIII<br />
Mo<strong>de</strong>ratori: Ş. Rădulescu, I. Droc<br />
ORA AUTORI TITLU<br />
16.30 –<br />
16.40<br />
16.40 –<br />
16.50<br />
16.50 –<br />
17.00<br />
17.00 –<br />
17.10<br />
17.10 -<br />
17.20<br />
17.20 –<br />
17.30<br />
17.30 -<br />
17.35<br />
17.35 –<br />
17.40<br />
Silaghi H, Magnan PE, Branchereau A, Gherman<br />
C, Mironiuc A<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
Alina Silaghi, H. Silaghi, T. Scridon, A. Mironiuc, Ş.<br />
Rădulescu, M. Grino<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
Institutul Inimii “ N. Stăncioiu” Cluj-Napoca<br />
Jerzicska E., Balos S., Suciu H., Deac R.<br />
IUBCVT, Tg. Mureş<br />
NJ Tesoiu<br />
Institutul <strong>de</strong> Urgenţă pentru Boli Cardiovasculare “ Prof.<br />
Dr. C.C. Iliescu”, Bucureşti<br />
Silvia Condru, D. Trandafir*, S. Rurac*, Cristina<br />
Tudor**, Florentina Mihăescu**<br />
*Department of Cardio-Vascular Surgery, University<br />
Hospital Bucharest<br />
**Department of Anaesthesia and Intensive Care<br />
University Hospital Bucharest<br />
A. Oprea, A. Eni, O. An<strong>de</strong>rcou, A. Buleandră,<br />
Diana Turcu, S. Rădulescu<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
Dr. Mihălcescu Daniel, Dr. Creţu Magdalena, Dr.<br />
Radu Mădălina, dr. Lazar Ovidiu, Dr. Cârjaliu<br />
Ionuţ, Dr. Tica Talida, Dr. Stanciu Crina, Dr. Popa<br />
Cherecheanu Matei, Dr. Lazăr Mihaela, Dr.<br />
Goleanu Viorel, Dr. Buica Dana<br />
Centrul <strong>de</strong> boli cardiovasculare « Agrippa Ionescu »<br />
Dr. Mihălcescu Daniel, Dr. Creţu Magdalena, Dr.<br />
Radu Mădălina, dr. Lazăr Ovidiu, Dr. Carjaliu<br />
Ionuţ, Dr. Tica Talida, Dr. Stanciu Crina, Dr. Popa<br />
Tratamentul endovascular în<br />
pseudoanevrismele aortei abdominale.<br />
Endovascular procedures for abdominal<br />
aorta false aneurysms<br />
Expresia citokinelor inflamatorii la nivelul<br />
ţesutului adipos epicardic şi relaţia cu<br />
boala aterosclerotică coronariană<br />
Răsunetul revascularizaţiei carotidiene<br />
asupra parenchimului cerebral – sindromul<br />
<strong>de</strong> hiperperfuzie cerebrală<br />
125 ani <strong>de</strong> la naşterea lui Nicolae<br />
Hortolomei - moştenirea în domeniul<br />
chirurgiei vasculare.<br />
125 years from the birth of Nicolae<br />
Hortolomei - vascular surgery heritage<br />
Popliteal Artery Entrapment Syndrome<br />
Giant External Carotid Aneurysm: case<br />
report.<br />
Anevrism gigant <strong>de</strong> arteră carotidă<br />
externă<br />
Tratamentul stenozelor, fistulelor arteriovenoase<br />
pentru hemodializa<br />
Sindromul <strong>de</strong> furt sangvin post FAV - abord<br />
chirurgical
17.40 –<br />
17.50<br />
Cherecheanu Matei, Dr. Lazăr Mihaela, Dr.<br />
Goleanu Viorel, Dr. Buica Dana<br />
Centrul <strong>de</strong> boli cardiovasculare « Agrippa Ionescu »<br />
D.F. Bărzoi, M. Păcescu, I. Diaconescu, N. J.<br />
Teşoiu, R. Halpern, I. Oprea, E. Mărginean, O.<br />
Moraru, O. Udrică, A. D. Iancu, A. Stoica, S.L.<br />
Băilă<br />
Vascular Surgery Department, “C. C. Iliescu”<br />
Cardiovascular Diseases Institute, Bucharest, <strong>Romania</strong><br />
Sâmbătă 2 octombrie <strong>2010</strong><br />
Sala Diamond<br />
Grupul <strong>de</strong> lucrări « CORD »<br />
Sesiunea IX<br />
Chirurgia arterelor coronare<br />
Mo<strong>de</strong>ratori: Gerard Bloch, H. Moldovan, Tintoiu I.<br />
28<br />
Reconstrucţii arteriale in Boala Ocluzivă<br />
Infrainghinală- experienţa secţiei în 13 ani<br />
Arterial reconstructions in Infrainguinal<br />
Occlusive Disease- our <strong>de</strong>partment’s<br />
experience over 13 years<br />
ORA AUTORI TITLU<br />
9.00 –<br />
9.15<br />
9.15 –<br />
9.30<br />
9.30 –<br />
9.45<br />
9.45 –<br />
10.00<br />
10.00 –<br />
10.15<br />
10.15 –<br />
10.30<br />
10.30 –<br />
10.45<br />
Deac Radu<br />
IUBCVT, Tg. Mureş<br />
Gerard Bloch<br />
Spitalul American <strong>din</strong> Paris<br />
Horaţiu Moldovan<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof. Dr. C.C. Iliescu”<br />
Bucureşti<br />
Grigore Tinică<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong> Boli<br />
Cardiovasculare, Iaşi<br />
Grigore Tinică, Diana Ciurescu, Igor Ne<strong>de</strong>lciuc,<br />
Mihail Enache, Vasile Astarastoae.<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculara, Institutul <strong>de</strong> Boli<br />
Cardiovasculare, Iaşi<br />
Ţintoiu Ion<br />
Spitalul Militar Bucureşti<br />
Adrian Molnar<br />
Institutul Inimii “ N. Stăncioiu” Cluj-Napoca<br />
10.45 – 11.00 Discuţii<br />
11.00 – 11.30 Coffe Break<br />
Sesiunea X<br />
Mo<strong>de</strong>ratori: I. Ţintoiu I., R. Deac, G. Tinică<br />
Revascularizarea miocardică – ghidul ESC<br />
<strong>2010</strong>.<br />
Myocardial revascularization – Gui<strong>de</strong>lines<br />
ESC <strong>2010</strong><br />
Actual indications for CABG (coronary<br />
artery bypass grafting<br />
Ruptura <strong>de</strong> sept interventricular post<br />
infarct miocardic acut<br />
Revascularizarea chirurgicală coronariană<br />
total arterială. Argumente şi fapte. Totally<br />
arterial coronary revascularization.<br />
Argument and facts.<br />
Organizarea sălii <strong>de</strong> operaţie hibri<strong>de</strong><br />
cardiovasculare.<br />
Making of the cardiovascular hybrid<br />
operating room<br />
Rezistenţa la tratamentul antiplachetar şi<br />
restenoza în stent sau graft<br />
Chirurgia off pump versus on pump în<br />
revascularizarea miocardică<br />
ORA AUTORI TITLU<br />
11.30 –<br />
11.45<br />
11.45 –<br />
12.00<br />
I. Droc, Tintoiu I.<br />
Centrul clinic <strong>de</strong> urgenţă <strong>de</strong> boli cardiovasculare<br />
“Dr. Constantin Zamfir”, Spitalul Militar Bucureşti<br />
Clara Alexandrescu<br />
Centre Cardio-Thoracique du Monaco, Monte<br />
Carlo<br />
CABG after instent restenosys<br />
Care este cea mai bună modalitate imagistică<br />
înainte <strong>de</strong> chirurgia aortei?. What is the best<br />
imagistic modality before surgery for aortic<br />
valve and aortic root?<br />
12.00 – L. Stoica, E. Bitere, E. Ciobanu, G. Tinica Ruptura cardiacă postinfarct miocardic acut-
12.10 Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong><br />
Boli Cardiovasculare “ Prof Dr. George I. M.<br />
Georgescu”, Iaşi<br />
12.10 –<br />
12.20<br />
12.20 –<br />
12.30<br />
12.30 –<br />
12.40<br />
12.40 –<br />
12.50<br />
12.50 –<br />
13.00<br />
13.00 –<br />
13.10<br />
13.10 –<br />
13.20<br />
R.Vasile, B.Rădulescu, A.Mărginean,<br />
S.Marin, O.Ghenu, H.Moldovan, V.Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “Prof Dr.<br />
C.C.Iliescu” Bucureşti<br />
Raicea V., Moraru L., Serban V., Deac R<br />
IUBCVT Tg. Mureş<br />
Grigore Tinica, Mihail Enache, Diana<br />
Ciurescu, Alexandru Ciucu, Flavia Antoniu,<br />
Oana Bartoş, Victor Prisacari.<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong><br />
Boli Cardiovasculare “ Prof Dr. George I. M.<br />
Georgescu”, Iaşi<br />
Diana Ciurescu, Igor Ne<strong>de</strong>lciuc, Mihail<br />
Enache, Dumitriţa Gafencu, Grigore Tinica<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară,<br />
Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof Dr. George I. M. Georgescu”, Iaşi<br />
Moraru L., Raicea V., Şerban V., Bica Lucia,<br />
Raicea C., Deac R.<br />
IUBCVT Tg. Mureş CCV I<br />
Deac R., Raicea V, Moraru L., Suciu H.<br />
IUBCVT, Tg. Mureş<br />
R. Vasile, B. Rădulescu, A. Vasilescu,<br />
Luminiţa Iliuţă, H. Moldovan, V. Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr.<br />
C.C.Iliescu” Bucureşti<br />
29<br />
prezentare <strong>de</strong> caz.. Cardiac rupture after<br />
myocardial infarction- case study<br />
Infarct miocardic acut postoperator,prin spasm<br />
<strong>de</strong> artera coronara dreaptă in<strong>de</strong>mnă<br />
Complicaţii mecanice ale infarctului miocardic<br />
acut: <strong>de</strong>fectul septal ventricular.<br />
Mechanical complication of acute myocardial<br />
infarction: Ventricular septal <strong>de</strong>fect<br />
Revascularizarea miocardică concomitentă<br />
tratamentului chirurgical al altor patologii<br />
cardiace. Comparaţie cu EACTS adult cardiac<br />
Surgical Database report.<br />
Miocardial revascularization combined with<br />
surgical treatment of other cardiac<br />
pathologies. Comparation with EACTS adult<br />
cardiac Surgical Database report<br />
Revascularizarea hibridă – un pas înainte în<br />
medicina cardiovasculară.<br />
Hybrid revascularisation – one step forward in<br />
cardiovascular medicine<br />
Recoltarea chirurgicală a arterei radiale –<br />
comparaţie între tehnica scheletizată şi cea<br />
pediculată<br />
Utilizarea arterei radiale în revascularizarea<br />
arterială miocardică.<br />
Use of radial artery in myocardial arterial<br />
revascularization<br />
Revascularizare miocardică folosind arterele<br />
mamare scheletizate<br />
13.20 – 13.30 Discuţii<br />
13.30 – 14.30 Pauza <strong>de</strong> prânz<br />
Sesiunea XI<br />
Mo<strong>de</strong>rator: Horia Mureşan, P. Bergeron, Şerban Stoica<br />
ORA AUTOR TITLU<br />
14.30 –<br />
14.40<br />
14.40 –<br />
14.50<br />
Grigore Tinica, Alexandru Ciucu, Mihail Enache,<br />
Diana Ciurescu, Flavia Antoniu, Mihalea Grecu,<br />
Oana Bartoş, Victor Prisacari, Daniel Dăscălescu.<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară,<br />
Institutul <strong>de</strong> Boli Cardiovasculare, Iaşi<br />
Raicea V., Moraru L., Serban V., Deac R.<br />
IUBCVT, Tg. Mureş<br />
Aportul chirurgical în controlul furtunii<br />
electrice la pacient cu <strong>de</strong>fibrilator<br />
implantabil şi anevrism gicant <strong>de</strong> ventricul<br />
stang.<br />
The importance of surgery in controlling<br />
the electrical storm in a patient with an<br />
implantable cardioverter and left<br />
ventricular anevrysm<br />
Disecţie acută <strong>de</strong> aortă ascen<strong>de</strong>ntă<br />
asociată cu disecţie carotidiană bilaterală<br />
- prezentare <strong>de</strong> caz.<br />
Acute dissection of ascen<strong>din</strong>g aorta with<br />
bilateral disection of carotid arteries - case<br />
report<br />
14.50 –<br />
15.00<br />
Horia Mureşian<br />
The University Hospital of Bucharest<br />
Surgical choices for aortic arch syndrome<br />
Feier Horea, Gaşpar M, Merce A., Nica D., Opţiuni <strong>de</strong> tratament ale rupturii<br />
15.00 – Deutsch P., Milovan Slovenski<br />
posttraumatice <strong>de</strong> aortă.<br />
15.10<br />
Treatment options for traumatic aortic<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara transection<br />
15.10 – O.Stiru, L.F. Dorobantu, O.Ghenu, Daniela Pseudonaevrism rupt <strong>de</strong> aortă asce<strong>de</strong>ntă
15.20 Filipescu, V.A.Iliescu<br />
15.20 –<br />
15.30<br />
15.30 –<br />
15.40<br />
15.40 –<br />
16.00<br />
16.00 –<br />
16.15<br />
16.15 -<br />
17.00<br />
Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof Dr. C.C.Iliescu” Bucureşti<br />
B. Rădulescu, R.Vasile, A.Vasilescu, Luminiţa<br />
Iliuţă, Y.Hashem, A.Mărginean, Mihaela Crăciun,<br />
S.Bubenek, H.Moldovan, V.Iliescu<br />
Spitalul Clinic Ju<strong>de</strong>ţean <strong>de</strong> Urgenţă, Universitatea <strong>de</strong><br />
Medicină şi Farmacie "Iuliu Haţieganu",<br />
Cluj-Napoca, Chirurgie II<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Bucureşti<br />
P. Bergeron*, A. Petrosyan *, J. Bellos**, F.<br />
Markatis**, T. Abdulamit*, A. El Shazly, J.C.<br />
Tratour*.<br />
* Saint-Joseph Hospital, Marseille, France<br />
** 1st surgical clinic Laikon Hospital University of Athens<br />
Medical School<br />
Şerban Stoica*, Kimberley Goldsmith**, Nicolaos<br />
Demiris**, Prakash Punjabi***, Geoffrey Berg****,<br />
Linda Sharples**, Stephen Large*****<br />
* Bristol Royal Children’s Hospital, USA<br />
** Medical Research Council Biostatistics Unit,<br />
Cambridge<br />
*** Hammersmith Hospital, London<br />
****Gol<strong>de</strong>n Jubilee National Hospital, Glasgow<br />
***** Papworth Hospital, Cambridge, UK<br />
I Droc, I. Mocanu, Murgu V., Deaconu St., Pinte Fl<br />
Discutii<br />
Centrul clinic <strong>de</strong> urgenţă <strong>de</strong> boli cardiovasculare<br />
“Dr. Constantin Zamfir”<br />
16.15 – 17.00 Discuţii<br />
30<br />
dupa proteazre aortică – rezolvare<br />
chirurgicală.<br />
Anevrism gigant <strong>de</strong> crosă aortică –<br />
rezolvare chirurgicală.<br />
New approach for extend Type II TAAA in<br />
High risk patients"<br />
Microsimulation of clinical outcomes<br />
analysis support a lower age threshold for<br />
use of biological valves<br />
Chirurgia carotidiană şi coronariană:<br />
strategie actuală.<br />
Carotid and Coronary Surgery - actual<br />
strategy.<br />
SALA Saphire<br />
Simpozionul Societăţii Române <strong>de</strong> Anestezie-Terapie Intensivă<br />
Cardiacă şi Tehnologie Extracorporeală (SRATICTE)<br />
Sesiunea XII<br />
Anemia si transfuzia in chirurgia cardiaca<br />
Mo<strong>de</strong>rator: Ioan Vlad<br />
ORA AUTORI TITLU<br />
09.00 -<br />
09.15<br />
09.15 -<br />
09.35<br />
09.35 -<br />
09.50<br />
Daniela Filipescu (Bucureşti)<br />
Ioana Grigoraş (Iaşi)<br />
Stanca Asztalos, Antonela Mureşan, Sanda<br />
Negruţiu, Luminiţa Slabu, Carmen Steiu, Ioan<br />
Vlad (Cluj Napoca)<br />
09.50 - 10.00 Discuţii<br />
Paradoxul anemie-transfuzie în chirurgia<br />
cardiacă<br />
Este administrarea perioperatorie <strong>de</strong> fier o<br />
soluţie ? Metabolismul fierului la pacientul<br />
critic<br />
Reducerea necesarului transfuzional în<br />
chirurgia cardiacă<br />
How to reduce allogenic blood transfusion<br />
in cardiac surgery
Sesiunea XIII<br />
Mo<strong>de</strong>rator: Victor Diaconescu<br />
ORA AUTORI TITLU<br />
10.00 -<br />
10.10<br />
10.10 -<br />
10.20<br />
10.20 -<br />
10.30<br />
10.30 -<br />
10.40<br />
10.40 -<br />
10.50<br />
Carmen Movileanu, Roxana Toma, Mihaela<br />
Melinte, Horatiu Suciu (Tg. Mureş)<br />
Gabriela Olaru, Pavel Morar, Irina Modrigan,<br />
Horaţiu Suciu (Tg. Mureş)<br />
S. Balos, Judit Kovacs, Radu Deac, Horaţiu Suciu<br />
(Tg. Mureş)<br />
S. Baloş, Judit Kovacs, Horaţiu Suciu (Tg. Mures)<br />
Anca Pro<strong>de</strong>a, Mihail Luchian, Oana Ghenu,<br />
Ioana Marinică, Alina Păunescu, Simona Marin,<br />
Laura Dima, Daniela Filipescu, Cezar Macarie<br />
10.50 - 11.00 Discuţii<br />
31<br />
Probleme curente în practica<br />
transfuzională pediatrică<br />
Particularităţi hematologice în patologia<br />
cianogenă postoperatorie<br />
Factori <strong>de</strong> risc ai disfuncţiei renale după<br />
chirurgia cardiacă<br />
Clasificarea AKI sau RIFLE în evaluarea<br />
prognosticului insuficienţei renale acute<br />
asociate chirurgiei cardiace<br />
N-GAL-marker precoce al disfuncţiei<br />
renale în chirurgia cardiacă?<br />
Sesiunea XIV<br />
Siguranţa pacientului în timpul circulaţiei extracorporeale<br />
Mo<strong>de</strong>ratori: Dan Longrois (Paris) şi Daniela Filipescu<br />
ORA AUTORI TITLU<br />
11.30 -<br />
11.50<br />
11.50 -<br />
12.00<br />
12.00 -<br />
12.20<br />
12.20 -<br />
12.30<br />
12.30 -<br />
12.40<br />
12.40 -<br />
12.50<br />
12.50 -<br />
13.00<br />
Dan Longrois (Paris)<br />
Oana Ghenu, Mihai Luchian, Victor Pavel, Gabi<br />
Olteanu, Horaţiu Moldovan, Vlad Iliescu, Daniela<br />
Filipescu (Bucureşti)<br />
Monitoring and Safety Issues in<br />
Cardiopulmonary Bypass<br />
Locul ECMO în chirurgia cardiacă<br />
Dan Longrois (Paris) Experienţa clinica cu ECMO<br />
Victor Diaconescu (Iaşi)<br />
Vasile Murgu, Cristian Gabriel, Laura Vămanu,<br />
Andreea Teo<strong>de</strong>rescu, Andreea Tifrea, Anca Filip,<br />
Ionel Droc, Ion Tintoiu (Bucureşti)<br />
Jozsef Budai (Tg. Mures)<br />
Iu. Guzgan, E. Vîrlan, I. Matcovschi, V. Moscalu,<br />
S. Manolache, A. Batrinac (Republica Moldova)<br />
Circulaţia extracorporeală <strong>de</strong> la disfuncţia<br />
neurocognitivă în trecut, la<br />
postcondiţionare în viitor?<br />
Filtrarea leucocitară selectivă a<br />
cardioplegiei cu sânge şi a celei terminale<br />
(Hot shot) - strategie <strong>de</strong> protecţie<br />
miocardică în timpul CEC<br />
Rezistenţa la heparină - importanţa<br />
problemei pentru circulaţia<br />
extracorporeală<br />
The advantages of intermittent warm<br />
blood cardioplegia supplemented with<br />
Mg ++<br />
13.00 – 13.30 Discuţii<br />
13.30 – 14.30 Pauza <strong>de</strong> prânz<br />
Sesiunea XV<br />
Mo<strong>de</strong>ratori: Ion Miclea, Mihai Luchian<br />
ORA AUTOR TITLU<br />
14.30 -<br />
14.40<br />
14.40 -<br />
14.50<br />
Ion Miclea, Violeta Bercan, Serban Bubenek<br />
(Bucuresti)<br />
Ovidiu Lazar, Tica Talida, Crina Stanciu, A<strong>din</strong>a<br />
Mitulescu, IonCarjaliu, Marian Butusina, Viorel<br />
Goleanu (Bucureşti)<br />
Traheostomia percutană în terapia<br />
intensivă sub control vi<strong>de</strong>olaringoscopic<br />
Proteina C reactivă înalt specifică în<br />
optimizarea predicţiei morbidităţii şi<br />
mortalităţii în chirurgia <strong>de</strong> revascularizare<br />
miocardică faţă <strong>de</strong> scorurile clasice
14.50 -<br />
15.00<br />
15.00 -<br />
15.10<br />
15.10 -<br />
15.20<br />
15.20 -<br />
15.30<br />
15.40 -<br />
15.50<br />
15.50 -<br />
16.00<br />
16.00 –<br />
16.10<br />
16.10 –<br />
16.20<br />
16.20 –<br />
16.30<br />
Ioan Vlad (Cluj-Napoca)<br />
Mihai Luchian, Ioana Marinică, Alina Păunescu,<br />
Oana Ghenu, Simona Marin, Anca Pro<strong>de</strong>a,<br />
Ovidiu Chioncel, Luminiţa Iliuţă, Oana<br />
Mihăilescu, Horaţiu Moldovan, Vlad Iliescu,<br />
Daniela Filipescu (Bucureşti)<br />
Roxana Toma, Sorin Păşcanu, Mihai Chiloflischi,<br />
Horaţiu Suciu (Tg. Mureş)<br />
D. Dăscălescu, V. Diaconescu, S. Patrulea, B.<br />
Aparaschivei, A. Ciucu, L. Stoica, G. Tinica (Iasi)<br />
Victor Diaconescu (Iaşi)<br />
Radu Mihai Dumitrescu, Cristina Anca Tudor,<br />
Elena Copaciu (Bucureşti)<br />
Oana Mihăilescu, Alina Păunescu, Mihai<br />
Luchian, Anca Pro<strong>de</strong>a, Oana Ghenu, Ioana<br />
Marinică, Simona Marin, Laura Dima, Ovidiu<br />
Chioncel, Luminiţa Iliuţă, Sorin Maximeasa,<br />
Horaţiu Moldovan, Vlad Iliescu, Daniela Filipescu<br />
(Bucureşti)<br />
Daniela Manea, Mihai Luchian, Alina Păunescu,<br />
Ioana Marinică, Anca Pro<strong>de</strong>a, Oana Ghenu,<br />
Simona Marin, Daniela Filipescu (Bucureşti)<br />
Cristina Ciochină, Mihai Luchian, Oana Ghenu,<br />
Ioana Marinică, Alina Păunescu, Simona Marin,<br />
Anca Pro<strong>de</strong>a, Ovidiu Chioncel, Luminiţa Iliuţă,<br />
Oana Mihăilescu, Daniela Filipescu (Bucureşti)<br />
SALA Ruby<br />
Grupul <strong>de</strong> lucrări « CONGENITALI »<br />
32<br />
Levosimendan în chirurgia cardiacă<br />
pediatrică<br />
Levosimendan la pacienti hemofiltrati<br />
postoperator<br />
Levosimendan in patients with<br />
postoperative haemofiltration<br />
Terlipresina - terapie "<strong>de</strong> salvare" în socul<br />
cardiogen postoperator<br />
Doza stress <strong>de</strong> hidrocortizon în timpul<br />
operaţiei la pacienţii cu risc crescut în<br />
chirurgia cardiacă<br />
Efecte antiinflamatorii ale combinaţiei<br />
xilină-morfină<br />
Anestezia loco-regională (blocul cervical)<br />
în chirurgia carotidiană - evaluare<br />
retrospectivă a experienţei <strong>din</strong> Clinica <strong>de</strong><br />
Chirurgie Vasculară SUUB"<br />
Este troponina predictivă post chirurgie<br />
cardiacă?<br />
Is Troponin a predictive biomarker in<br />
cardiac surgery?<br />
Rolul ROTEM în sângerarea post chirurgie<br />
cardiacă<br />
Ce aduce nou ghidul <strong>de</strong> resuscitare în<br />
chirurgia cardiacă?<br />
Sesiunea XVI<br />
Mo<strong>de</strong>ratori: Horaţiu Suciu, Andrei Iosifescu, Chira Manuel<br />
ORA AUTOR TITLU<br />
9.00 –<br />
9.15<br />
9.15 –<br />
9.30<br />
9.30 –<br />
9.45<br />
9.45 –<br />
10.00<br />
10.00 –<br />
10.15<br />
10.15 –<br />
10.30<br />
Suciu Horaţiu<br />
IUBCVT, Tg. Mureş<br />
Andrei Iosifescu, Lucian Dorobantu, Sorin<br />
Maximeasa, Traian Anca, Cristian Boroş, Vlad<br />
Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Andrei Iosifescu, Alexandru Cornea, Traian Anca,<br />
Ioana Ghiorghiu, Platon Pavel, Ioana Marinică,<br />
Vlad Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Bucureşti<br />
Dr. Ilona Cucu, dr. Vasile Sirbu, dr. Liviu Maniuc,<br />
dr. Oleg Repin<br />
Institute of Cardiology, Republic of Moldova<br />
Şerban Stoica*, Esther Carpenter**, Eduardo da<br />
Cruz**, James Todd**, Thomas Fagan**, Max<br />
Mitchell**, David Campbell**, Dunbar Ivy**,<br />
Francois Lacour- Gayet***<br />
*Bristol Royal Children’s Hospital, USA<br />
** Denver Children’s Hospital, USA<br />
***Montefiore Hospital, New York, USA<br />
Suciu H., Paşcanu S., Matei M., Roxana Toma,<br />
Anca Sglimbea, Opris C., Deac R.<br />
Actualităţi în chirurgia pediatrică<br />
Update in pediatric cardiac surgery<br />
Tratamentul chirurgical al afecţiunilor<br />
congenitale ale căii <strong>de</strong> ieşire <strong>din</strong> ventriculul<br />
stâng<br />
Stenoza infundibulară pulmonară extrinsecă<br />
secundară pericarditei constrictive la copil–<br />
prezentarea unui caz tratat chirurgical<br />
Baloon angioplasty of pulmonary artery<br />
valve<br />
Outcomes of the complex arterial switch<br />
operation<br />
Corecţia chirurgicală a transpoziţiei marilor<br />
vase - experienţa a 80 <strong>de</strong> cazuri.
10.30 –<br />
10.40<br />
IUBCVT, Tg. Mureş Surgical correction of Transposition of Great<br />
Arteries - experience of 80 cases<br />
Lucian Stoica, Eugen Bitere, Dumitriţa-Alina<br />
Gafencu, Laurentiu Gafencu, Grigore Tinica<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară,<br />
Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof. Dr. George I. M. Georgescu”, Iaşi<br />
Originea anormală a arterei coronare stângi<br />
<strong>din</strong> artera pulmonară asociată cu<br />
regurgitare mitrală.<br />
Anomalous origin of left coronary artery from<br />
the pulmonary artery in associatin with mitral<br />
regurgitation<br />
10.40 – 11.00 Discuţii<br />
11.00 – 11.30 Coffe Break<br />
Sesiunea XVII<br />
Mo<strong>de</strong>ratori: Chira Manuel, Mariana Andreica, Rodica Manasia, Angela Butnariu<br />
ORA AUTORI TITLU<br />
11.30 –<br />
11.45<br />
11.45 –<br />
12.00<br />
12.00 –<br />
12.15<br />
12.15 –<br />
12.30<br />
12.30 –<br />
12.40<br />
12.40 –<br />
13.00<br />
Chira Manuel, Simona Opriţa<br />
Institutul Inimii “ Niculae Stăncioiu” Cluj<br />
Cecilia Lazea*, Rodica Manasia,* Simona<br />
Opriţa**, Mircea Bârsan**, Svetlana Encica**<br />
* Clinica Pediatrie I “Axente Iancu” Cluj<br />
**Institutul Inimii “ Niculae Stăncioiu” Cluj<br />
Angela Butnariu, Daniela Iacob<br />
Clinica Pediatrie III, Universitatea <strong>de</strong> Medicină şi<br />
Farmacie “Iuliu Haţieganu” Cluj-Napoca<br />
Mariana Andreica*, Simona Cainap*, Andreea<br />
Răchişan*, Simona Opriţa**, Cecilia Lazea**,<br />
Manuel Chira**, Nicolae Miu*<br />
* Clinica Pediatrie II Cluj-Napoca<br />
** Institutul Inimii “Niculae Stăcioiu” Cluj-Napoca<br />
*** Clinica Pediatrie I Cluj-Napoca<br />
Popa Cherecheanu Matei, Goleanu Viorel,<br />
Butusina Marian, Lazar Ovidiu, Lazar Mihaela,<br />
Mihalcescu Daniel, Creţu Magdalena, Radu<br />
Mădălina, Tănăsescu Dragoş.<br />
Spitalul Clinic <strong>de</strong> Urgenţă Militar, Bucureşti<br />
Rodica Manasia, Cecilia Lazea<br />
Clinica Pediatrie I “Axente Iancu” Cluj<br />
33<br />
Intervenţii chirurgicale vs cardiologie<br />
intervenţională în tratamentul<br />
malformaţiilor chirurgicale"<br />
Tumori cardiace în practica cardiacă<br />
Aspecte pediatrice ale îngrijirii<br />
perioperatorii la copilul mic cu<br />
malformaţie cardiacă congenitală<br />
Abordarea clinică şi terapeutică a<br />
malformaţiilor cardiace congenitale –<br />
cazuistica Clinicii Pediatrie II Cluj-Napoca<br />
Chilotorax post cură chirurgicală a<br />
<strong>de</strong>fectului septal interatrial<br />
Aspecte <strong>din</strong> viaţa copilului cardiac<br />
13.00 – 13.30 Discuţii<br />
13.30 – 14.30 Pauza <strong>de</strong> prânz<br />
SALA Ruby<br />
Grupul <strong>de</strong> lucrări « NURSING »<br />
ORA AUTOR TITLU<br />
14.30 –<br />
14.40<br />
14.40 –<br />
14.50<br />
14.50 –<br />
15.00<br />
15.00 –<br />
15.10<br />
15.10 –<br />
15.20<br />
15.20 –<br />
15.30<br />
As. Aurica Farcane, Prof Dr. Petru Deutsch.<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
As Daniela Demea, Prof. Dr. Marian Gaspar<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
As Georgeta Teuca<br />
Anestezie şi Terapie Intensivă, Institutul Inimii<br />
“N. Stăncioiu”, Cluj-Napoca<br />
As. Alina Ganea<br />
Bloc operator<br />
Cătinean Mihaela Carmen, dr. Vlad Horea Ioan<br />
Institutul Inimii <strong>de</strong> urgenţă pentru boli cardiovasculare”<br />
Nicolae Stăncioiu” Cluj-Napoca, Clinca <strong>de</strong> anestezie şi<br />
terapie intensivă<br />
As. Szabo Noemi, dr. A. Molnar<br />
Institutul Inimii <strong>de</strong> urgenţă pentru boli cardiovasculare”<br />
Concentratul trombocitar obţinut prin<br />
afereza, tehnologie <strong>de</strong> interes pentru<br />
hematologia transfuzională<br />
Rolul bancii <strong>de</strong> celule si tesuturi in<br />
cresterea eficientizarii transplantului<br />
Transpozitia <strong>de</strong> vase mari – indicaţii şi risc<br />
operator<br />
Rezultate imediate în protezarea valvei<br />
aortice pentru stenoză.<br />
Protocol <strong>de</strong> reducere necesarului <strong>de</strong><br />
transfuzii alogene în chirurgie cardiacă<br />
Chirurgia coronariană off pump, avantaje<br />
şi <strong>de</strong>zavantaje.
Nicolae Stăncioiu” Cluj-Napoca, Clinca <strong>de</strong> anestezie şi<br />
terapie intensivă<br />
Vineri 1 octombrie <strong>2010</strong>, Sala Diamond<br />
Grupul <strong>de</strong> lucrări « CORD »<br />
Sesiunea I - Transplant cardiac. Chirurgia valvelor cardiace<br />
Update in cardiac transplantation – <strong>2010</strong><br />
Prof. dr. Deac R., conf. dr. Suciu H.,<br />
IUBCVT, Targu Mures<br />
International Society of Heart and Lung Transplantation with its database updates the<br />
medical community with progress in the domain. The main reason of this activity is the increased<br />
number of heart transplant patients who need follow up or medical asistance outsi<strong>de</strong> the<br />
specialized centers and thus the medical community should be kept informed. More than that,<br />
the procedure of heart trasplantation is no longer an experimental technique but a method of<br />
treatment for terminal heart diseases above the medico - surgical armamentarium so far. The<br />
surgical technique most commonly used is the orthotopic heart transplantation, bicaval<br />
technique. A modification of this technique by performing the aortic anastomosis first shortens the<br />
ischemia by one hour. Utilisation of a blood artificial perfusion system to keep the donor heart<br />
beating extends the duration of the transfer to recipient for more than 5 hours. Immunosuppresive<br />
medication more efficient and with less si<strong>de</strong>-effects (everolimus, sirolimus) is already un<strong>de</strong>r clinical<br />
trials. Blood assays of rejection related gene expression proved already ”noninferior” to<br />
myocardial biopsy,which still remains ”the gold standard”.<br />
Utilization of statins 1-2 weeks after the transplant is recommen<strong>de</strong>d disregar<strong>din</strong>g the level<br />
of cholesterol. Male recipients who receive male donor hearts have a longer survival in<br />
comparison with female recipients who have a survival with 3,6 % less at 5 years. Males who<br />
receive female donor hearts have a mortality risk of 15% higher.<br />
Median survival after heart transplantation is now 10 years.The longevity after heart<br />
transplantation has reached 31 years with good quality of life. A case of a child transplanted at 6<br />
month of age at Stanford University, USA, is now 28 years old without immunossupresive therapy,<br />
acquiring imunological tolerance, the gol<strong>de</strong>n dream of transplantation<br />
Actualităţi în transplantarea cardiacă – <strong>2010</strong><br />
Societatea Internaţională <strong>de</strong> Transplantare a Inimii şi Plămânilor prin baza sa <strong>de</strong> date<br />
actualizată anual documentează progresele înregistrate în domeniu şi susţin proce<strong>de</strong>ul <strong>de</strong><br />
transplantare cardiacă ortotopică ca o metodă <strong>de</strong> tratament a bolior cardiace incurabile pînă în<br />
anii <strong>din</strong> urmă. Principalul scop al acestei actualizări este numărul crescut al pacienţilor cu<br />
transplant cardiac care necesită dispensarizare sau asitenţă medicală înafara centrelor<br />
specializate <strong>de</strong>spre care comunitatea medicală trebuie informată. Tehnica chirurgicală cea mai<br />
<strong>de</strong>s efectuată este transplantarea ortotopică a inimii <strong>de</strong> tip bicav. Menţinerea inimii în stare <strong>de</strong><br />
perfuzie con-tinuă într-un sistem <strong>de</strong> perfuzie artificială cu sânge permite prelungirea duratei <strong>de</strong><br />
transfer <strong>de</strong> la donator la receptor peste 5 ore în bună stare <strong>de</strong> funcţionare. O modificare tehnică<br />
constând în efectuarea iniţială a anasto-mozei aortice scurtează ischemia cordului donator cu 1<br />
oră. Medicaţie imunosupresivă mai eficientă şi cu mai puţine efecte secundare (everoli-mus,<br />
sirolimus) se află în trialuri clinice. Teste serice <strong>de</strong> rejecţie ”gene expression related” s-au dovedit<br />
non-inferioare supravegherii imunosu-presiei prin biopsia miocardică invazivă, <strong>de</strong>şi aceasta<br />
rămâne ”standardul <strong>de</strong> aur”. Utilizarea statinelor <strong>de</strong> la 1-2 săptămâni după transplant este<br />
recomandată indiferent <strong>de</strong> nivelul colesterolului. Receptorii bărba i care primesc inimi <strong>de</strong><br />
donatori bărbaţi au o supravieţuire mai lungă <strong>de</strong>cât femeile care indiferent <strong>de</strong> genul donatorului<br />
au o supravieţuire cu 3,6% mai mică la 5 ani. Bărbaţii care primesc inimi <strong>de</strong> femei au un risc <strong>de</strong><br />
mortalitate cu 15% mai mare. Supravieţuirea mediană după transplantarea cardiacă este acum<br />
<strong>de</strong> 10 ani. Longevitatea după transplantare cardiacă a atins 31 <strong>de</strong> ani în bună stare <strong>de</strong> sănătate.<br />
Este <strong>de</strong>scris cazul unui copil <strong>de</strong> 6 luni operat la Universitatea Stanford, SUA, care a împlinit 28 <strong>de</strong><br />
ani fără terapie imuno-supresivă dobân<strong>din</strong>d toleranţă imunologică visul <strong>de</strong> aur al transplantării.<br />
34
Ten years of heart transplantation at IUBCVT Târgu Mureş 1999 – <strong>2010</strong><br />
Zece ani <strong>de</strong> transplantare cardiacă la IUBCVT Tg. Mureş 1999-<strong>2010</strong><br />
Conf. dr. Suciu H., prof. dr. Deac R., dr. Mihaela Ispas, dr. Paşcanu S.,<br />
dr. Roxana Toma, prof. dr. Anca Sin, dr. Cotoi O., dr. Matei M.,<br />
dr. Opris C., dr. Mihaela Melinte, asist. med. Terezia Preda<br />
IUBCVT Tg. Mureş<br />
Heart transplantation became a method of treatment of terminal heart diseases above<br />
the medico-surgical armamentarium. The database of International Society of Heart and Lung<br />
Transplantation witnesses the progress in the domain. The procedure was introduced in the<br />
Emergency Institute of Cardiovascular Disease and Transplantation Targu Mures in 1999 when the<br />
first heart transplantation was performed. Between 1999 and <strong>2010</strong> there were transplanted 38<br />
patients with the ortothopic bicaval heart transplantation. The patients were HLA tested<br />
retrospectively. The immunosuppresion used consisted in triple drug therapy (calineurin inhibitors –<br />
Cyclosporine or Prograf, MMF and corticoids) after induction with Thymoglobulin. Cytomegalovirus<br />
prophilaxis with Gancylovir and Valgancyclovir was performed. The first 2 patients reached 1o<br />
years of longevity in good health. The number of heart transplantation performed annually<br />
increased with the number of donors available. In <strong>2010</strong>, 7 cardiac transplants were performed.<br />
The early and late complications are presented. The results and quality of life of the transplanted<br />
patients justify the continuation of heart transplantation program in our unit.<br />
Zece ani <strong>de</strong> transplantare cardiacă la IUBCVT Tg. Mureş 1999-<strong>2010</strong><br />
Transplantarea ortotopică a inimii a <strong>de</strong>venit o metodă <strong>de</strong> tratament a bolilor cardiace<br />
terminale care se află <strong>de</strong>asupra resurselor <strong>de</strong> tratament medico-chirurgicale clasice. Baza <strong>de</strong><br />
date a Societăţii Internaţionale <strong>de</strong> Transplantare a Inimii şi Plămânilor documentează anual<br />
progresele înregistrate în domeniu. In Institutul <strong>de</strong> Urgenţă pentru Boli Cardiovascu-lare şi<br />
Transplant acest proce<strong>de</strong>u a fost introdus în 1999, când a fost transplantat primul pacient. Intre<br />
1999 şi <strong>2010</strong> au fost transplantaţi 38 <strong>de</strong> pacienţi cu proce<strong>de</strong>ul <strong>de</strong> transplant cardiac ortotopic tip<br />
bicav. Pacienţii a fost testaţi HLA retrospectiv. Terapia imunosupresivă aplicată a con-stat în<br />
inducţie cu Timoglobulină şi corticoizi, apoi terapia <strong>de</strong> întreţinere cu inhibitori <strong>de</strong> calcineurină<br />
(Ciclosporină, Prograf) şi MMF (mycofenolat mofetil). Profilaxia infecţiei cu Cytomegalovirus a fost<br />
efectuată cu Gan-ciclovir şi Valganciclovir. Primii 2 pacienţi au <strong>de</strong>păşit longevitatea <strong>de</strong> 10 ani.<br />
Numărul transplantelor cardiace efectuate anual a crescut cu numă-rul donatorilor disponibili. In<br />
anul <strong>2010</strong> au fost efectuate 7 transplante cardiace. Sunt prezentate complicaţiile imediate şi<br />
tardive înregistrate. Rezultatele obţinute şi calitatea vieţii pacienţilor operaţi justifică continu-area<br />
transplantării cardiace în unitatea noastră.<br />
Vlad Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof Dr. C.C.Iliescu” Bucureşti<br />
Marian Gaspar<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
Markus Kamler<br />
Institutul Inimii Hilarion, Essen<br />
Reconstrucţia valvelor atrioventriculare - între teorie<br />
şi practică<br />
Chirurgia valvulară: progres şi realitate<br />
Valvular surgery, between progres and reality.<br />
Chirurgia minim invazivă a valvei mitrale<br />
ECLS in cardiogenic shock and cardiac arrest<br />
V. Saplacan, C. Ivascau, F. Dugenet, M. Massetti<br />
University Hospital of Caen, France - Spitalul Univesitar Caen, Franta<br />
Frequently the patients in cardiogenic shock or refractory cardiac arrest need<br />
mechanicals assistance like ECLS (Extra-Corporal Life Support) for having a chance of survival.<br />
The implant <strong>de</strong>cision is a complex one and must evaluate multiple parameters like the<br />
gravity of the patient status, the treatments already administrated, the possibility of myocardial<br />
recovery, the possible of cardiac transplantation and the operating risks.<br />
The advantages of ECLS make of this type of mechanical assistance a first line choice for<br />
the treatment of ineluctable heart failure.<br />
We present a literature review of the results of ECLS in cardiogenic shock and cardiac<br />
arrest and we will discuss the results of ECLS assistance at University Hospital of Caen.<br />
35
ECLS in socul cardiogen si stopul circulator<br />
In mod frecvent, pacientii aflati in soc cardiogenic grav sau in stop cardiac refractar<br />
manevrelor <strong>de</strong> resuscitare au nevoie <strong>de</strong> asistenta circulatorie mecanica <strong>de</strong> tip ECLS (Extra-<br />
Corporal Life Support) pentru a reusi sa supravietuiasca.<br />
Decizia <strong>de</strong> implantare a ECLS e complexa si ia in calcul multipli parametri, precum<br />
gravitatea cazului, tratamentele <strong>de</strong>ja administrate, posibilitatea recuperarii miocardice sau a<br />
transplantului cardiac precum si riscurile operatorii.<br />
Avantajele asistentei <strong>de</strong> tip ECLS fac <strong>din</strong> acest dispozitiv o alegere <strong>de</strong> prima intentie in<br />
tratamentul insuficientei cardiace refractare.<br />
Prezentarea noastra face o analiza a literaturii in ceea ce priveste asistenta ECLS in socul<br />
cardiogen si stopul cardiac refractar, asociata discutiei rezulatelor ECLS <strong>din</strong> cadrul Spitalului<br />
Universitar <strong>din</strong> Caen.<br />
Baza <strong>de</strong> date a Societăţii Europene <strong>de</strong> Chirurgie Cardio-Toracică<br />
Sesiunea II - Tumorile Cardiace, complicaţii ale chirurgiei cardiace<br />
Traian Scridon<br />
Institutul Inimii “ N. Stăncioiu” Cluj-Napoca<br />
Tumori cardiace<br />
The strategies in diagnosis and surgical treatment of heart tumors<br />
Manolache Gh., Batrînac A., Moscalu V., Ureche A.,<br />
Morozan V., Ţurcanu G., Barnaciuc S., Ghicavii N.<br />
Institute of Cardiology, Chisinau, Republic of Moldova<br />
Primary and secondary heart tumors can <strong>de</strong>velop within any level of heart structure<br />
myocardium, endocardium or pericardium.<br />
The inci<strong>de</strong>nce of heart tumors is very little. It can be probably based on the peculiarities of<br />
metabolism within the myocardium, the coronary blood circuit and the reduced system of<br />
lymphatic connections.<br />
The objective of the work paper: The prior choice of pre-operative methods of diagnosis<br />
and the <strong>de</strong>termination of the surgical approach <strong>de</strong>pends on the localization and on the clinical<br />
and morphological shape of the heart neoplasm.<br />
Materials and methods: Records on surgical interventions in 69 patients with cardiac tumors<br />
subjected to treatment during 1983-2009 were analyzed. The age of patients ranged 15-73 (the<br />
average age was 53,2) inclu<strong>din</strong>g 20 (30%) men and 49 (70%) women. In 64 (92,8%) patients the<br />
tumors were benign and in 5 patients (7,2%) – malignant.<br />
The diagnosis and the localization of cardiac tumors are performed by the contemporary<br />
methods of research, EcoCG, nuclear-magnetic resonance, selective coronary angiography,<br />
myocardial scintigraphy.<br />
Displaying the same clinical symptoms as the rheumatic valve disease, primary cardiac<br />
tumors are characterized by a short-term evolution of the disease and by a progressive cardiac<br />
<strong>de</strong>compensation, refractory to medical treatment.<br />
Results: All the patients have been operated upon in conditions of cardio-pulmonary<br />
bypass with radical removal of benign cardiac tumor, simultaneously in some cases was<br />
performed the mitral valvuloplasty with or without tricuspid valve annuloplasty. In the case of<br />
malign tumors, the approach and the volume of operations varied <strong>de</strong>pen<strong>din</strong>g on the localization,<br />
on the stage of the disease and on the possibilities of neoplasm-removal. The left atrial myxoma<br />
has been most frequently met, in 56 (81,2%) patients, rhabdomyoma - 2 cases, mesothelioma - 2<br />
patients, the fibroma and hemangioma respectively 1 case, leimyoma - 2 cases. The cardiac<br />
sarcoma has been met in 5 (7,2%) cases. The post operative lethality has constituted 8,7% (6<br />
cases). 63 patients were supervised during the long-term post operative period. A favorable<br />
evolution of all clinical symptoms has been observed, as well as the data on hemodynamics,<br />
<strong>de</strong>termined by the use of echocardiography. The surgery has been successfully un<strong>de</strong>rgone in 2<br />
36
cases (2,9%) of tumor relapse which have been i<strong>de</strong>ntified (1 LA myxoma and 1 RA, RV<br />
leiomyoma).<br />
Conclusions: Once i<strong>de</strong>ntified, primary cardiac tumors must be surgically removed.<br />
Patients’ age and the severity of heart failure cannot be regar<strong>de</strong>d as a counter-indication for<br />
surgery. Since malign cardiac tumors are given an unfavorable forecast, the surgical treatment is<br />
combined with the specific treatment inclu<strong>din</strong>g chemotherapy and X-Ray treatment for the sake<br />
of patient’s life prolongation.<br />
Rolul ecocardiografiei in diagnosticul si rezolvarea chirurgicala a tumorilor cardiace<br />
I. Manitiu, Gabriela Eminovici, Minodora Teodoru,<br />
Rodica Moga, Ruxandra Dobrin, C. Balan<br />
Spitalul Clinic Ju<strong>de</strong>tean Sibiu<br />
Introducere: Tumorile cardiace reprezinta o patologie rara evoluand cu manifestari<br />
sistemice si cardiace, in momentul cand simptomatologia <strong>de</strong>vine evi<strong>de</strong>nta tumora atingand<br />
dimensiuni importante.<br />
Material si metoda: Am studiat un numar <strong>de</strong> 12 cazuri diagnosticate cu tumori<br />
intracardiace in Clinica Cardiologie Sibiu intre anii 2000-2009, observand tipul tumorii, tabloul<br />
clinic, evolutia si tratamentul chirurgical urmat.<br />
Rezumat: Majoritatea tumorilor erau mixoame atriale solitare, intalnindu-se si un caz <strong>de</strong><br />
tumora maligna. S-au studiat anumite caracteristici ecocardiografice specifice diferitelor tipuri <strong>de</strong><br />
tumori, localizarea intracardiaca fiind in majoritatea cazurilor atriul stang, importanta<br />
diagnosticului precoce precum si a tratamentului corect chirurgical care a fost realizat in 8<br />
(66,66% ) cazuri cu evolutie favorabila ulterioara si aparitia complicatiilor in 4 (33,33%) cazuri.<br />
Concluzii: Rezolvarea chirurgicala a tumorilor cardiace este favorabila si minime<br />
complicatii atunci cand ea este efectuata <strong>de</strong> catre o echipa cu experienta.<br />
Cardiopericardic hydatid cyst with anaphylactic shock<br />
Lucian Stoica, Eugen Bitere, Laurenţiu Gafencu, Dumitriţa-Alina Gafencu, Grigore Tinică<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculara, Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof. Dr. George I.M. Georgescu”, Iaşi<br />
Cardiovascular Surgery Clinic, Cardiovascular Diseases Institute<br />
“Prof. Dr. George I.M. Georgescu”, Iaşi<br />
Of all the parasitic diseases that can affect the heart and pericardium (Trypanosoma,<br />
Toxoplasmosis, Schistosomiasis, Trichinosis), the echinococosis is the only one which requires<br />
(sometimes in emergency) surgical treatment. The cardiac and pericardial localization are very<br />
rare, seen in about 1-1,5% of patients with echinococcosis.<br />
In this paper we will present the case of a 20 year old man, with no medical history, who<br />
was admitted to the hospital after being resuscita<strong>de</strong>d from anaphylactic shock.<br />
The imagistic exams (echocardiography, CT-scan) showed multiple cystic structures insi<strong>de</strong><br />
the pericardium (extracardiac) with no other sites and he was transferred in emergency to<br />
hospital IBCV "Prof. Dr. George. I.M. Georgescu" from Iasi. The surgical procedure inclu<strong>de</strong>d total<br />
and partial resection of multiple hydatid cysts with extracorporeal circulation (without crossclamping).<br />
The pathologic exam confirmed the diagnose.<br />
In the postoperative period the patient began the treatment with albendazol and hepatic<br />
protectors. He went home 10 days after the procedure with very good status. Clinical control after<br />
6 mouths shows very good evolution and no recidive.<br />
Keywords: cardiopericardic hydatid cyst, echinococosis<br />
Chist hidatic cardio-pericardic manifestat prin şoc anafilactic<br />
Dintre parazitozele ce pot afecta cordul şi pericardul (trypanosoma, toxoplasmoza,<br />
malaria, schistostomiaza, trichinoza etc.), echinococoza este singura care impune, cel mai<br />
frecvent, tratament chirurgical (uneori <strong>de</strong> urgenţă) iar localizarea cardio-pericardică reprezintă<br />
doar 1-1,5% <strong>din</strong> totalul localizărilor chisturilor hidatice, cu variaţii în funcţie <strong>de</strong> statistici.<br />
Lucrarea are scopul <strong>de</strong> a prezenta cazul unui pacient în varsta <strong>de</strong> 20 ani, fără<br />
antece<strong>de</strong>nte patologice semnificative, resuscitat după un şoc anafilactic, la care explorările<br />
37
imagistice (ecocardiografie şi CT toracoabdominal) <strong>de</strong>celează multiple formaţiuni chistice<br />
intrapericardice extracardiace fara alte localizari. Pacientul este transferat <strong>de</strong> urgenţă în clinica<br />
noastra şi se intervine chirurgical practicându-se rezecţia chiştilor pericardici multipli şi chistectomii<br />
parţiale sub circulaţie extracorporeală <strong>de</strong> asistare. Examenul anatomopatologic a confirmat<br />
diagnosticul. Postoperator se iniţiaza tratament cu albendazol şi protectoare hepatice. Pacientul<br />
se externează la 10 zile postoperator cu stare generală bună, controlul clinic la 6 luni aratnad<br />
absenta recidivelor.<br />
Cuvinte cheie: chist hidatic pericardic, echinococoză<br />
L.F. Dorobanţu, O. Stiru, A. Pro<strong>de</strong>a, A. Georgescu,<br />
Daniela Filipescu, V.A. Iliescu<br />
Clinica <strong>de</strong> Chirurgie Cardiovascularã, Institutul <strong>de</strong> Boli<br />
Cardiovasculare "Prof. Dr. C.C. Iliescu", Bucureşti<br />
Caz unic <strong>de</strong> histiocitom fibros malign <strong>de</strong> ventricul<br />
drept cu implantare la nivelul ban<strong>de</strong>letei<br />
mo<strong>de</strong>ratoare<br />
Particularitati ale cazurilor <strong>de</strong> trombembolism pulmonar<br />
in experienta Clinicii <strong>de</strong> Cardiologie Sibiu<br />
Minodora Teodoru, I. Manitiu, Gabriela Eminovici,<br />
Rodica Moga, C. Balan, Raluca Matei, Cristina Chircu<br />
Spitalul Clinic Ju<strong>de</strong>tean Sibiu<br />
Introducere: Trombembolismul pulmonar reprezinta o patologie cu un tablou clinic si o<br />
evolutie cu mare diversitate ce necesita rezolvare terapeutica diferita si adaptata fiecarui caz.<br />
Materiale si meto<strong>de</strong>: Au fost studiate 72 cazuri <strong>de</strong> trombembolism pulmonar internate in<br />
Clinica Cardiologie Sibiu in perioada anilor 2007-2009.<br />
Rezultate: S-au studiat prevalenta trombembolismului pulmonar in perioada mentionata,<br />
atitu<strong>din</strong>ea terapeutica, ce a constat in tratament medicamentos in 93% (67 pacienti) cazuri, si<br />
chirurgical in 7% (5 pacienti) cazuri, observandu-se mai ales corelatia cu factorii prognostici.<br />
Concluzii: Tratamentul trombembolismului pulmonar este unul complex si presupune o<br />
colaborare interdisciplinara intre cardiolog si chirurg, cu evolutie favorabila atunci cand<br />
interventia chirurgicala este efectuata in cazuri selectate.<br />
Treatment of sternal <strong>de</strong>hiscence after heart operation<br />
38<br />
Reinhard Moidl<br />
Department of Cardiothoracic Surgery,<br />
University of Vienna, Vienna, Austria<br />
Objective: Post-sternotomy wound complications are a major cause of cardiac surgical<br />
morbidity, resulting in increased average hospital cost of this contingent of patients.<br />
It was <strong>de</strong>veloped a protocol for care and treatment of patients with such a complication.<br />
Method. From January 2000 to April 30, <strong>2010</strong> (10 years 4 months) were treated 34 patients<br />
(22 men and 12 women) with sternal <strong>de</strong>hiscence. Of them with mediastinitis clinic were 24<br />
patients, and no signs of infectious -10. The diagnosis was established at 5-17 days after surgery.<br />
The mean age was 60 years (40-71ani) 14 were obese, and only two had diabetes. Treatment is<br />
carried out in two stages: (1) postoperative wound early processing, inclu<strong>din</strong>g removal of metal<br />
sutures, with daily dressings until complete removal of infected tissue (2) Operation a) mobilizing<br />
the subcutaneous tissue and muscle layers separated, b) recovery the wound by applying a<br />
retrosternal irrigation, c) applying sternum osteosynthesis - Robiscek technique, d) application<br />
lavage system, e) - wound closure in layers. In acute cases of <strong>de</strong>hiscence, osteosynthesis is carried<br />
out urgently.<br />
Results: The cure rate was 98%, the stay in hospital for 14 days (range 12-16 days), with only<br />
one <strong>de</strong>ath caused by hepatorenal failure. In two patients <strong>de</strong>veloped sternal osteomyelitis, which<br />
required long-term treatment (3-6 months)<br />
Conclusion: Using this protocol is effective and saves the patient from using adjacent<br />
tissues (muscles of the abdomen, chest, or even omentum) to cure the infection, and leaves the<br />
patient without cosmetic consequences.
Treatment of sternal <strong>de</strong>hiscence after heart operation<br />
Prisacaru I., Ureche A., Turcanu G., Manolache Gh., Moscalu V., Batrinac A.<br />
Insitute of Cardiology, Chisinau, Republic of Moldova<br />
Objective: Postoperative sternal wound infection with <strong>de</strong>hiscence carries a high morbidity<br />
rate, resulting in increased average hospital cost of this group of patients. We <strong>de</strong>veloped a<br />
standard protocol of care to treat this complication, achieving primary closure and cure of the<br />
infection.<br />
Method: During the period of 10 years (from January 2000 to April 30, <strong>2010</strong>), 2450 patients<br />
had been operated on heart and great vessels, trough a median sternotomy approach 34 (1,38%)<br />
of them (22 men and 12 women) with sternal <strong>de</strong>hiscence. 24 patients had a clinical manifestation<br />
of mediastinitis, another 10 patients had no signs of infections. The diagnosis had been established<br />
between 5th to 17th days after surgery. The mean age was 60 years (40-71 ages): 14 being obese,<br />
and only two had diabetes. Treatment entailed (1) <strong>de</strong>bri<strong>de</strong>ment without removal of bone, (2)<br />
bilateral dissection of skin and subcutaneous tissue as one layer, (3) the wound recovery by<br />
applying a retrosternal irrigation-suction system posterior and another one anterior to the sternum,<br />
(4) applying sternum osteosynthesis - Robiscek technique, (5) a single-layer closure of the<br />
subcutaneous tissue and skin.<br />
Results: The rate of recovery was 98% (32/34); hospital stay was 14 days (range, 12-16 days),<br />
with only one <strong>de</strong>ath caused by hepatorenal failure. At two patients had <strong>de</strong>veloped sternal<br />
osteomelitis, which had required long-term treatment almost (3-6 months).<br />
Conclusion: Our protocol aims to cure the infection and to re-establish normal chest<br />
stability without the use of muscle or omental flaps, sparing the sternum and leaving the patient<br />
anatomically intact and fit for normal activities.<br />
Sesiunea III - Chirurgia valvei aortice<br />
Surgical Choices For Aortic Arch Syndrome<br />
Anatomia chirurgicală a rădăcinii aortei<br />
Horia MURESIAN<br />
Cardiovascular Surgery, The University Hospital of Bucharest<br />
Background. Severe and symptomatic stenotic-occlusive lesions of one or more arch<br />
vessels ask for an elaborate clinical and imagistic diagnosis and for varied but individually-applied<br />
surgical techniques, especially in patients having a life expectancy of 15 years or more.<br />
Materials and methods. The author presents his personal experience with 28 consecutive<br />
patients admitted for cerebrovascular insufficiency (inclu<strong>din</strong>g major stroke) and/or upper limb<br />
ischemia over a 4 year period. The following bypasses were used: ascen<strong>din</strong>g aorta-to-bilateral<br />
carotid artery: 4 cases; ascen<strong>din</strong>g aorta-to-carotid and subclavian artery: 4 cases;<br />
brachiocephalic trunk-to-carotid and subclavian artery: 1 case; subclavian-to-bilateral carotid<br />
artery: 1 case; subclavian-to-carotid artery: 3 cases; carotid-to-subclavian or axillary artery: 15<br />
cases.<br />
Results. Global mortality was 3,57%. One major hemispheric stroke occurred (3,57%). No<br />
postoperative cranial nerve palsies were encountered.<br />
Conclusions. Different surgical techniques can be applied for the treatment of the aortic<br />
arch syndrome. The ascen<strong>din</strong>g aorta represents a valuable donor vessel; alternatively, the<br />
brachiocephalic trunk, the subclavian or the carotid artery – can be used as well, especially in<br />
severely diseased patients. Doppler ultrasound examination doubled by arch and 4-vessel<br />
angiogram, represent the major steps in a thorough and efficient diagnostic workup. The<br />
complete revascularization can be contemplated even in patients with associated diseases but<br />
otherwise with a longer life expectancy.<br />
Gelu Cerin<br />
Cardiology Unit in Cardiac Surgery Dpt. San Gau<strong>de</strong>nzio<br />
Clinic, Novara, Italy<br />
C. Lanzilo, Marco Diena<br />
Cardiac Surgery Dpt. San Gau<strong>de</strong>nzio Clinic,<br />
Novara, Italy, Novara, Italy<br />
Wich patients for aortic valve repair? Role of<br />
Echocardiography<br />
Aortic valve repair – when and how to do it?<br />
39
Gunther Laufer<br />
Univ.-Klinik für Chirurgie, Klin, Viena- Austria<br />
Marian Gaspar, Gunther Laufer, Călin Jusca,<br />
Daniel Nica, Ionel Droc, Petre Deutsch<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
Progres in aortic valve surgery<br />
“Homograft – ROSS operation, Timişoara,<br />
experience 1997 – <strong>2010</strong>”<br />
Remplacement valvulaire aortique conventionnel chez le sujet <strong>de</strong> plus <strong>de</strong> 85 ans.<br />
Résultats à court et long terme à propos d’une série <strong>de</strong> 164 patients opérés.<br />
M. Laskar (1), C. Eveno (1), T. Bourguignon (2), A. Piccardo (3),<br />
L. Roussel (3), E. Bergoend (2), M. Aupart (2), E. Cornu (1),<br />
T. Caus (3), M. Marchand (2)<br />
(1) CHU Dupuytren, 87042 Limoges<br />
(2) Hôpital Trousseau, 37044 Tours<br />
(3) Hôpital Sud, 80054 Amiens<br />
Objectifs: Le remplacement valvulaire aortique chez le sujet très âgé bénéficie <strong>de</strong> <strong>de</strong>ux<br />
innovations thérapeutiques importantes, la chirurgie endovalvulaire et l’apparition <strong>de</strong>s valves<br />
« sans suture ». Pour évaluer correctement le bénéfice <strong>de</strong> ces nouvelles techniques il nous paraît<br />
important d’évaluer la qualité <strong>de</strong>s résultats <strong>de</strong> la chirurgie conventionnelle. Dans ce but nous<br />
avons mené une étu<strong>de</strong> rétrospective multicentrique réunissant l’expérience <strong>de</strong> trois centres <strong>de</strong><br />
chirurgie cardiaque français sur les résultats à court et long terme <strong>de</strong> la chirurgie conventionnelle<br />
chez les sujets <strong>de</strong> plus <strong>de</strong> 85 ans.<br />
Matériel et métho<strong>de</strong>: Cette étu<strong>de</strong> a porté sur 164 patients consécutifs opérés dans trois<br />
centres <strong>de</strong> chirurgie cardiaque <strong>de</strong> janvier 1987 à décembre 2009. Il s’agissait <strong>de</strong> 87 femmes (53%)<br />
et <strong>de</strong> 77 hommes (47%). L’âge moyen <strong>de</strong> la cohorte était <strong>de</strong> 86,5 ans avec <strong>de</strong>s extrêmes <strong>de</strong> 85 à<br />
91 ans. L’Euroscore logistique moyen était <strong>de</strong> était <strong>de</strong> 13,5 et l’Euroscore inférieur à 10 chez 50%<br />
<strong>de</strong>s patients, entre 10 et 20 chez 35% et supérieur à 20 chez 15%. 53 pts (32%) ont bénéficié <strong>de</strong><br />
geste revascularisation coronaire associée.<br />
Résultats: La mortalité hospitalière a été <strong>de</strong> 9,8%. Le délai moyen <strong>de</strong> séjour en soins intensifs<br />
a été <strong>de</strong> 6,64 jours et le délai moyen <strong>de</strong> séjour dans le service a été <strong>de</strong> 9,74 jours. Le taux <strong>de</strong><br />
survie, mortalité hospitalière incluse est <strong>de</strong> 84% à 6 mois, 79% à un an, 75% à <strong>de</strong>ux ans, 62% à 4 ans<br />
et 52% à 5 ans. Aucun patient n’a dû être réopéré pour sa pathologie valvulaire.<br />
Conclusion: Le remplacement valvulaire aortique conventionnel donne un résultat<br />
durable au prix d’une mortalité et d’une morbidité péri-opératoire faible même chez les sujets très<br />
âgés. La place <strong>de</strong> chacune <strong>de</strong>s techniques alternatives reste à évaluer en fonction du statut <strong>de</strong>s<br />
patients surtout s’il s’avère que la qualité du résultat n’est pas aussi pérenne que celui <strong>de</strong> la<br />
chirurgie conventionnelle.<br />
Conventional aortic valvular replacement in patients over 85.<br />
Short and long term results about 164 patients.<br />
Objectives: New technologies such as endovlaves and sutureless valves are changing the<br />
perspective of aortic valve replacement in el<strong>de</strong>rly patients. It seems necessary to have a good<br />
evaluation of the results of the conventional surgery to evaluate in the future the results of these<br />
technologies. The aim of this retrospective study was to collect the experience of three French<br />
cardiac surgery centers to evaluate the short and long term results of conventional aortic valve<br />
replacement in patients over 85.<br />
Methods: The survey collects the experience of 164 patients operated from January 1987<br />
to December 2009. The patients were 87 female (53%) and 77 male (47%). The mean age was 86.<br />
5 (from 85 to 91). The mean logistic Euroscore was 13. 5 and the Euroscore was less than 10 in 50%<br />
of the pts, between 10 and 20 in 35% and over 20 in 15%. 53% had an associated coronary<br />
revascularization.<br />
Results: Hospital mortality was 9,8%. The mean ICU stay was 6,64 days and the mean<br />
hospital stay was 9,7 days. The overall survival rate was 84% at 6 months, 79% at one year, 75% at<br />
two years, 62% at four years, and 52% at five years. No patient had to be reoperated for the<br />
valvular pathology<br />
Conclusion: Conventional aortic valvular replacement has a low hospital mortality and<br />
morbidity even in el<strong>de</strong>rly patients and gives a long-lasting good result. The place of the new<br />
technologies has to be evaluated regar<strong>din</strong>g the patient condition moreover if the result is not as<br />
reliable as the conventional surgery.<br />
40
"Functional principle" in <strong>de</strong>termining the assessment criteria<br />
for valvular aortic reconstructive correction<br />
V. Moscalu, A. Batrînac, Gh. Manolache, A. Ureche, Gr. Ţurcan,<br />
V. Morozan, S. Barnaciuc, S. Voitov, N. Ghicavîi, Iu. Guzgan<br />
Institut of Cardiology, Cardiac Surgery Department, Chişinău, Republic of Moldova<br />
The functional approach of the aortic valve is based on better knowledge of anatomy of<br />
aortic valve and pathophysiology of aortic regurgitation.<br />
The difficulty of aortic valve plasties lies in recognizing precise lesions responsible for aortic<br />
regurgitation and selection of suitable operation techniques.<br />
Material and methods: The study group inclu<strong>de</strong>d 185 polivalvular patients, whom were<br />
performed reconstructive techniques of operation in the aortic position. Etiology of aortic<br />
pathologies was of "rheumatic, <strong>de</strong>generative diseases, infective endocarditis and trauma”. In<br />
most of cases there was settled by ECO-cardiography a complex mechanism of aortic<br />
insufficiency. As a starting point for choosing of operation techniques was used the reconstructive<br />
oriented classification published by G. El. Khoury and co-authors (2009).<br />
Thus, in the type I lesion various annuloplasty techniques were performed; in type II – tissues<br />
redundancy and cusps’ prolapse was corrected through cusp plicaţion, triangular resection and<br />
free margin resuspension; type III was managed by comissurotomy, parietal resection of cusps.<br />
Results: Postoperative mortality comprised 3,2% (6 patients). Eco-cardiography has been<br />
stated an obvious dramatic evolution in transvalvular gradient <strong>de</strong>creasing, also significantly<br />
<strong>de</strong>creased the <strong>de</strong>gree of aortic insufficiency after reconstructive correction. A minimal residual<br />
regurgitation was registered in 44 (23,8%) patients. A follow up study was managed at 5 to 10<br />
years postoperatively; recurrence of pathologies was <strong>de</strong>tected in 19 (10,6%) cases. Eight (4,4%)<br />
patients required reoperaţions. Survival was 81. 6±4,8% at 10 years after aortic valve<br />
reconstruction, much higher compared to patients who un<strong>de</strong>rwent its prosthesis.<br />
Conclusions: Ao valve reconstructive techniques are an accepted alternative to valvular<br />
prosthesis. There is a series of mandatory conditions in carrying out these operations:<br />
� Presence of an acceptable anatomy for applying reconstructive procedures;<br />
� Knowledge of <strong>de</strong>velopmental mechanism of valvular incompetence;<br />
� Equipped with supplies, materials and <strong>de</strong>vices specially <strong>de</strong>signed for this operations;<br />
� Accumulation of surgical experience by a <strong>de</strong>dicated team, inclu<strong>din</strong>g a cardiologist,<br />
specializing in eco-cardiography and an expert surgeon, which might make surgical<br />
planning before entering the operating room.<br />
Stenoza aortica severa asimptomatica – festina lente?<br />
Dumitraşcu George,<br />
Spitalul Militar <strong>de</strong> Urgenta Sibiu<br />
Pacientii cu stenoza aortica severa simptomatici beneficiaza <strong>de</strong> tratament chirurgical <strong>de</strong><br />
protezare valvulara. Se estimeaza ca fiecare al treilea pacient cu stenoza aortica severa este<br />
asimptomatic iar managementul acestuia este controversat si <strong>de</strong>seori reprezinta o provocare. La<br />
pacientii neselectati protezarea valvulara aortica prematura este grevata <strong>de</strong> riscul chirurgical, iar<br />
protezarea intarziata datorata nerecunoasterii simptomelor poate agrava prognosticul, <strong>de</strong> aceea<br />
estimarea riscului, a indicatiilor si momentului operator <strong>de</strong>vine foarte importanta. Ecocardiografia<br />
reprezinta examenul standard pentru evaluarea si urmarirea pacientilor insa parametrii actuali<br />
folositi sunt limitati in a estima <strong>de</strong>butul simptomelor si a prognosticului clinic, aceeasi limitare<br />
aplicandu-se si parametrilor clinici, testelor <strong>de</strong> stress si altor meto<strong>de</strong> imagistice. Aceasta lucrare<br />
trece in revista cele mai relevante studii clinice si ghidurile actuale pentru managementul stenozei<br />
aortice asimptomatice subliniind importanta i<strong>de</strong>ntificarii pacientilor cu risc inalt.<br />
41
Should root replacement with aortic valve-sparing be offered to patients with severe<br />
aortic regurgitation or bicuspid aortic valves?<br />
Catalin Constantin Badiu, Walter Eichinger, Sabine Bleiziffer, Grit Hermes,<br />
Ina Hettich, Bernhard Voss, Robert Bauernschmitt, Rüdiger Lange<br />
Objective: To examine the results of root replacement with aortic valve-sparing in patients<br />
with bicuspid aortic valve (BAV) or severe aortic regurgitation (AR).<br />
Methods: Between 2000 and <strong>2010</strong> one hundred forty patients (mean age 47±17,5 years)<br />
un<strong>de</strong>rwent aortic valve-sparing procedures for ascen<strong>din</strong>g aortic aneurysm or dissection. Patients<br />
were assigned to three different groups accor<strong>din</strong>g to the aortic valve pathology: BAV (n=19),<br />
tricuspid aortic valve (TAV) with AR < severe (n=65), and TAV with severe AR (n=56). Remo<strong>de</strong>ling of<br />
the aortic root was performed in 29 (20. 7%) patients, reimplantation of the aortic valve in 111<br />
(79,3%) and a concomitant cusp repair in 59 (42%). All patients were prospectively studied with<br />
annual clinical assessment and echocardiography.<br />
Results: Overall actuarial five years survival was 97. 8±1. 5% without differences between<br />
the groups. Actuarial five years freedom from aortic valve related reoperation was 92. 2±3. 2% in<br />
all patients, 100% in patients with a BAV, 98±1,9% in patients with a TAV and AR
aorto-coronaries by-passes - 145 (mean average 3,2 per patient). In 5 cases it was used aortic<br />
valve prosthesis, and tricuspid annuloplasty in 4 cases.<br />
Results: Post operative lethality constitutes 6,5% (3 cases). As a result EchoCG showed a<br />
<strong>de</strong>creased gra<strong>de</strong> of IMI, averagely from 2, 76, before surgery, through 1, 13 - after. In all of the<br />
cases was mentioned a good mobility of the valve cusps with an average transvalve gradient at<br />
5, 77±1, 06 mmHg. Fibrous ring diameter <strong>de</strong>creased from 37, 8±2,2 till 29, 59±1,1 mm.<br />
Hemodynamic effect of annuloplasty was confirmed through consi<strong>de</strong>rable diminishing of the<br />
heart cavities and with an spectacular increase of the LVEF from 39, 42±2,6% till 54, 28±3,3%. The<br />
relapse of mitral insufficiency was not registered during long follow-up period.<br />
Conclusion: Mitral valve annuloplasty with “3 sutures” is an effective and time sustainable<br />
procedure. Selective application of sutures on the annulus fibrosis leads to good cusps cooptation<br />
and removal of the tensioned cordage phenomenon, i. e. to a complex correction of valvular<br />
insufficiency. Its simplicity and possibility of performing through different surgical approaches<br />
reduces aortal clamping time.<br />
Dumitrasciuc G., Nica D., Feier H., Jusca C.,<br />
Cioata D., Ionac A,. Merce A., Gaspar M.<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
Aspecte ale chirurgiei valvei mitrale la pacienţii cu<br />
disfuncţie sistolică a ventriculului stâng<br />
Mitral valve surgery in patients with left ventricular<br />
systolic disfunction.<br />
Prevention of systolic anterior motion (SAM) after mitral valve repair<br />
V. Moscalu, A. Batrînac, Gh. Manolache, A. Ureche, N. Ghicavîi, S. Manolache, V. V. Moscalu<br />
Institute of Cardiology, Heart Surgery Department, Chişinău, Moldova<br />
Objective: The purpose of this study was to explore the geometric changes that predispose<br />
to left ventricular outflow (LVOT) obstruction after mitral valve repair<br />
Methods: Between January 2005 and December 2009 were performed 114 operations of<br />
mitral valve repair. Etiologies inclu<strong>de</strong>d myxomatous <strong>de</strong>generation, endocarditis, ischemia and<br />
rheumatic valve disease. All the cases were assessed by Eco-cardiography the mechanism of<br />
mitral regurgitations, the dimensions of anterior and posterior mitral valve leaflet (AMVL and<br />
PMVL), the distance between the leaflet coaptation point and the annular plane, also the risk<br />
factors for SAM. The inci<strong>de</strong>nce of SAM was 2. 6% (3 cases).<br />
Results: We note that the patients with SAM and LVOT obstruction had the elongation<br />
AMVL ≥ 2,7 cm, elongated PMVL > 1,5 cm and annular dilatation > 3,8 cm. The LV diastolic volume<br />
ranged from 118 till 165 ml (small ventricle), in 1 case was assessed the hypertrophic septum.<br />
Extensive posterior leaflet resection without sli<strong>din</strong>g plasty was performed in 2 cases. The size of<br />
implanting semirigid ring was 28, 30 mm, 1 patient received paraannular suture annuloplasty. The<br />
fluid challenge and inotrop withdrawal solve the SAM and LVOT obstruction in 2 cases, 1 patient<br />
nee<strong>de</strong>d reoperation.<br />
Conclusion: The oversized rigid ring annuloplasty in <strong>de</strong>generative mitral insufficiency may<br />
cause an anterior shift of the coaptation point and increases the displacement of the redundant<br />
leaflet tissue in the LVOT. The resection of PMVL, sli<strong>din</strong>g valvuloplasty and large ring annuloplasty<br />
help to minimize the risk of SAM.<br />
Right Coronary Artery Revascularization. Certainty and Controversy<br />
Grigore Tinică, Mihail Enache, Diana Ciurescu, Alexandru Ciucu, Oana Bartos, Victor Prisacari,<br />
Daniel Dăscălescu, Victor Diaconescu, Sânziana Patrulea, Bogdan Aparaschivei<br />
Cardiovascular Surgery Department,<br />
Cardiovascular Institute, “Prof. Dr. George I. M. Georgescu”, Iasi<br />
Aim: The current study is oriented towards the statistical processing and interpretation of<br />
the coronary artery by-pass grafting procedures in which the radial artery was used as a graft on<br />
the right coronary artery.<br />
Materials and method: We studied retrospectively all the patients un<strong>de</strong>rgoing a CABG<br />
procedure at IBCV “Prof. Dr. George I. M. Georgescu” Iasi during 2000-august <strong>2010</strong>. Out of a total<br />
of 963 patients, we selected a group of 181 patients in which the radial artery was used as a graft<br />
for the right coronary artery.<br />
43
Results: In 163 (90,05%) patients there was only one graft on the right coronary artery, and<br />
in 18 (9,94%) patients there were two grafts on the right coronary artery (in 16 patients the radial<br />
artery was mounted sequentially and in 2 patients the radial artery was used alongsi<strong>de</strong> the right<br />
internal mammary artery). In our study group 12,70% of patients un<strong>de</strong>rwent complex surgical<br />
procedures (CABG concurrent with other intra- and extracardiac procedures). The overall<br />
mortality was 1,65%.<br />
Conclusions: This study reveals an ascen<strong>din</strong>g trend in the inci<strong>de</strong>nce of the CABG<br />
procedures that incorporate the radial artery as a graft for the right coronary artery in the period<br />
2000-august <strong>2010</strong> in our clinic. The overall mortality was 1,65%, results that are superior to those<br />
quoted in the reference literature. Our experience proves that the radial artery is in<strong>de</strong>ed a graft<br />
that can be mounted successfully on the right coronary artery and therefore disputes the studies<br />
that disregard this arterial graft’s patency.<br />
Revascularizarea arterei coronare drepte. Certitu<strong>din</strong>i şi controverse<br />
Obiective: Prezenta lucrare urmareste prelucrarea si interpretarea statistica a pacientilor<br />
supusi unei interventii <strong>de</strong> revascularizare miocardica chirurgicala, la care s-a utilizat artera radiala<br />
drept graft pentru artera coronara dreapta.<br />
Materiale si meto<strong>de</strong>: Am realizat un studiu retrospectiv asupra tuturor pacientilor supusi<br />
unei interventii chirurgicale <strong>de</strong> revascularizare miocardica la IBCV Iasi in perioada 2000-august<br />
<strong>2010</strong>. Astfel, <strong>din</strong>tr-un total <strong>de</strong> 963, am selectat un lot <strong>de</strong> 181 <strong>de</strong> pacienti la care s-a utilizat artera<br />
radiala drept graft pentru artera coronara dreapta.<br />
Rezultate: La 163 (90.05%) <strong>de</strong> pacienti s-a montat un singur graft pe ACD, iar la 18 pacienti<br />
(9.94%) s-au realizat doua pontaje in sistemul coronarian drept (la 16 pacienti artera radiala a fost<br />
dispusa secvential, iar la 2 pacienti s-a utilizat artera radiala impreuna cu artera mamara interna<br />
dreapta). Din acest lot <strong>de</strong> pacienti, 12.70% au necesitat cura chirurgicala a altor patologii intra- si<br />
extracardiace. Mortalitatea globala inregistrata a fost <strong>de</strong> 1,65%.<br />
Concluzii: Inci<strong>de</strong>nta utilizarii arterei radiale drept graft pentru artera coronara dreapta a<br />
cunoscut un trend ascen<strong>de</strong>nt in perioada 2000-august <strong>2010</strong> in clinica noastra. Mortalitatea<br />
globala inregistrata a fost <strong>de</strong> 1,65%, cu mult sub datele citate in literatura <strong>de</strong> specialitate.<br />
Experienta clinicii noastre dove<strong>de</strong>ste astfel ca artera radiala reprezinta un graft ce poate fi folosit<br />
cu succes la nivelul arterei coronare drepte si combate studiile ce <strong>de</strong>sconsi<strong>de</strong>ra patenta acestui<br />
graft arterial.<br />
Acute pancreatitis after cardiac surgery: a morphologic study<br />
Dr. Kovacs Judit, prof. dr. Jung J., dr. Gurzu Simona, prof. dr. Azamfirei L.,<br />
prof. dr. Copotoiu Sanda-Maria, dr. Balos S., conf. dr. Suciu H., dr. Copotoiu Ruxandra, dr. Mezei T.<br />
UMF Târgu Mureş, IUBCVT Târgu Mureş<br />
Etiology of pancreatitis is well known and although the enzymatic lesion is the key point in<br />
its <strong>de</strong>velopment, pancreatic ischemia caused by hypoperfusion in cardiogenic shock is an<br />
important etiological factor.<br />
Materials and methods. We conducted a retrospective study which inclu<strong>de</strong>d patients who<br />
un<strong>de</strong>rwent cardiac surgery at IUBCVT Targu-Mures between 2004-2009, to <strong>de</strong>termine the<br />
inci<strong>de</strong>nce and risk factors for acute pancreatitis. Patients with known pancreatic lesions were<br />
exclu<strong>de</strong>d.<br />
Results and discussion. During this period acute pancreatitis was suspected in 2 patients,<br />
but this was not confirmed in any of them after the clinical examination and laboratory tests.<br />
However, in 12 patients who un<strong>de</strong>rwent cardiac surgery, post mortem we found pancreatic<br />
necrosis. It is interesting that no patient had clinical or laboratory signs suggestive for an acute<br />
pancreatitis. All patients had unfavorable postoperative evolution, with hemodynamic instability,<br />
high doses of inotropics and <strong>de</strong>veloped multiple organ dysfunction and sepsis during<br />
hospitalization in intensive care.<br />
Conclusion: Acute pancreatitis is a rare complication after cardiac surgery, but if it<br />
<strong>de</strong>velops, most often lead to patients <strong>de</strong>ath. The main risk factors were cardiogenic shock and<br />
systemic inflammatory syndrome of sepsis.<br />
Pancreatita acută după intervenţii chirurgicale cardiace<br />
44
Etiologia pancreatitei este bine cunoscută şi cu toate că leziunea enzimatică este factorul<br />
principal în <strong>de</strong>zvoltarea ei, ischemia pancreatică cauzată <strong>de</strong> hipoperfuzia <strong>din</strong> stările <strong>de</strong> şoc<br />
cardiogen este un factor cauzal important.<br />
Materiale şi meto<strong>de</strong>. Am efectuat un studiu retrospectiv care a cuprins pacienţii operaţi<br />
pe cord <strong>de</strong>schis la IUBCVT Tg-Mureş în perioada 2004-2009, pentru a <strong>de</strong>termina inci<strong>de</strong>nţa şi factorii<br />
<strong>de</strong> risc ai pancreatitei acute. Au fost excluşi pacienţii cu leziuni pancreatice cunoscute.<br />
Rezultate şi discuţii. În această perioadă s-a ridicat suspiciunea <strong>de</strong> pancreatită acută la 2<br />
pacienţi, dar acesta nu a fost confirmat la nici unul <strong>din</strong>tre ei în urma examenului clinic şi<br />
paraclinic. Cu toate acestea, la 12 pacienţi operaţi pe cord, <strong>de</strong>cedaţi şi autopsiaţi am constatat<br />
leziuni pancreatice necrotico-hemoragice. Este interesant, că nici un pacient nu a avut semne<br />
clinice sau paraclinice sugestive pentru o pancreatită acută. Toţi pacienţii au avut o evoluţie<br />
postoperatorie nefavorabilă, cu instabilitate hemo<strong>din</strong>amică, doze mari <strong>de</strong> inotropice şi au<br />
<strong>de</strong>zvoltat disfuncţie multiplă <strong>de</strong> organe şi sepsis în cursul internării în terapie intensivă.<br />
Concluzii: Pancreatita acută este o complicaţie rară după chirurgia cardiacă, dar dacă<br />
se <strong>de</strong>zvoltă, <strong>de</strong> cele mai multe ori duce la <strong>de</strong>cesul pacientului. Ca factori <strong>de</strong> risc principali putem<br />
aminti şocul cardiogen şi sindromul inflamator generalizat <strong>din</strong> sepsis.<br />
An adjunctive procedure for surgical left ventricular<br />
remo<strong>de</strong>ling using papillary muscle sling<br />
A. Batrînac, V. Morozan, A. Ureche, Gh. Manolache,<br />
S. Voitov, S. Barnaciuc, N. Ghicavîi, Iu. Guzgan, V. Moscalu<br />
Institute of Cardiology, Cardiac Surgery Department, Moldova, Chisinau<br />
Objectives: The aim of the study was to evaluate the left ventricular hemo<strong>din</strong>amic<br />
parameters after the remo<strong>de</strong>ling of left ventricle using papillary muscle sling technique accor<strong>din</strong>g<br />
to Hvass and possibility of improving mitral valve competence.<br />
Materials and methods: Since January 2006 to March <strong>2010</strong> there were done 32 cases of left<br />
ventricular remo<strong>de</strong>ling accor<strong>din</strong>g to Hvass technique and 1 case of right ventricle papillary<br />
muscle approximation in tricuspid valve insufficiency. There were 29 men and 3 women. Mean<br />
age of patients was 54 ± 8 (39 - 66) years old, 26 patients un<strong>de</strong>rwent the intervention for ischemic<br />
heart disease (left ventricular aneurism) and 6 - for cardiac valvulopathies of diverse etiology.<br />
All the patients had NYHA III-IV, pulmonary hypertension (SPRV 50–70 mmHg), mitral<br />
insufficiency (II-IV gr.), and dilated fibrous annulus of mitral valve (38 – 46 mm).<br />
To perform papillary muscle sling was used a piece of Gor-Tex 4-0 vascular prosthesis. In 26<br />
patients with ischemic cardiomiopathy where performed following surgical techniques: CABG +<br />
left ventricular aneurysmoplasty + left ventricular remo<strong>de</strong>ling accor<strong>din</strong>g to Hvass + mitral valve<br />
annuloplasty (12); CABG + left ventricular remo<strong>de</strong>ling accor<strong>din</strong>g to Hvass + mitral and tricuspid<br />
valve annuloplasty (4); CABG + left ventricular aneurysmoplasty + left ventricular remo<strong>de</strong>ling<br />
accor<strong>din</strong>g to Hvass (10).<br />
Six patients with valvular diseases un<strong>de</strong>rwent: Bentall operation + mitral and tricuspid<br />
valvuloplasty + Hvass procedure (2); mitral valve replacement + tricuspidal valve annuloplasty +<br />
MAZE III procedure + Hvass procedure for left ventricle (1); mitral valve replacement + tricuspid<br />
valvuloplasty + Hvass procedure (2); David operation + mitral and tricuspid valvuloplasty + Hvass<br />
procedure (1).<br />
Results: In all patients, which un<strong>de</strong>rwent left ventricular remo<strong>de</strong>ling accor<strong>din</strong>g to Hvass<br />
procedure, the ejection fraction increased from 39 ± 8% (mean average before the intervention)<br />
till 49 ± 5% after the surgery. Left ventricular diastolic volume <strong>de</strong>creased from 254 ± 81 ml prior to<br />
the intervention to 173 ± 40 ml after. There was obtained the regression of the mitral valve<br />
insufficiency up to I – II gra<strong>de</strong> and the <strong>de</strong>creasing of annulus fibrosis diameter to 28, 6 mm.<br />
One patient <strong>de</strong>veloped on the 11 th day after the intervention the rupture of the posteromedial<br />
papillary muscle followed by an urgent reintervention – mitral valve replacement, which<br />
successfully was performed.<br />
In a patient with right ventricular remo<strong>de</strong>ling through muscular pillars approximation, the<br />
cavity dropped to 28 mm. (prior to operation right ventricular size was 40 mm). Also was practiced<br />
De Vega – Cabrol annuloplasty, which allowed the complete treatment of the tricuspid valve<br />
regurgitation.<br />
In the early postoperative period one patient died due to cardiac and renal failure.<br />
45
Conclusions: Using of Hvass technique with the approximation of papillary muscles for left<br />
ventricular remo<strong>de</strong>ling offers benefits by <strong>de</strong>creasing its diastolic volume, consi<strong>de</strong>rable<br />
improvement of cooptation and regression of mitral regurgitation, with increasing ejection fraction<br />
of the left ventricle.<br />
Sala Saphire<br />
Grupul <strong>de</strong> lucrări « CHIRURGIE VASCULARĂ »<br />
Rădulescu Şerban<br />
Spitalul Clinic Ju<strong>de</strong>ţean <strong>de</strong> Urgenţă, Universitatea <strong>de</strong><br />
Medicină şi Farmacie "Iuliu Haţieganu", Cluj-Napoca,<br />
Chirurgie II<br />
Gabriel Szendro - Conferinţă<br />
Department of Vascular Surgery, Soroka Medical<br />
Center, Beer Sheva, Israel<br />
Sorin Băilă<br />
Institutul <strong>de</strong> Boli Cardiovasculare “C.C. Iliescu”<br />
Bucureşti<br />
Sesiunea V<br />
Chirugia vasculară – Ten<strong>din</strong>ţe actuale în <strong>Romania</strong><br />
Minimally invasive new technique for fem-pop bypass<br />
Locul endarterectomiei <strong>de</strong> artera carotidă în<br />
tratamentul stenozelor critice carotidiene<br />
simptomatice şi asimptomatice<br />
Aneurysm of Aberrant Right Subclavian Artery,<br />
Kommerell Diverticulum and Common Carotid Trunk-Single-Stage Surgical Repair without<br />
Cardiopulmonary Bypass<br />
Horia MURESIAN<br />
Cardiovascular Surgery, University Hospital of Bucharest<br />
Background. The most common anomaly of the aortic arch and branches, is an aberrant<br />
right subclavian artery (ARSA) that arises from the proximal <strong>de</strong>scen<strong>din</strong>g thoracic aorta, occurring<br />
in 0, 5% of the population. Mostly asymptomatic, ARSA can become symptomatic in ol<strong>de</strong>r age<br />
due to atherosclerotic stiffening of the arterial walls, aneurysmal dilatation or to the presence of a<br />
common carotid trunk – lea<strong>din</strong>g to the so-called dysphagia lusoria. The aortic origin may be<br />
dilated in the form of the Kommerell diverticulum, contributing to a greater extent to the clinical<br />
symptoms. Surgical repair usually inclu<strong>de</strong> a two-stage operation with right subclavian and<br />
vertebral artery reimplantation and respectively, resection of the aneurysm – the latter step being<br />
performed un<strong>de</strong>r cardiopulmonary bypass.<br />
Materials and methods. We present the case of a 70 years old patient admitted with<br />
severe dysphagia and hoarseness from left vocal cord paresis produced by the association of a<br />
Kommerell diverticulum, atherosclerotic aneurysm of ARSA and common carotid trunk. A singlestage<br />
operation without the use of cardiopulmonary bypass, through a median sternotomy was<br />
performed: resection of the diverticulum and ARSA aneurysm, ascen<strong>din</strong>g aorta-to-right subclavian<br />
prosthetic bypass.<br />
Results. The patient recovered uneventfully, being discharged on the sixth postoperative<br />
day without any complications and free of dysphagia. The vocal cord paresis remitted by the<br />
fourth week postoperatively.<br />
Conclusions. This is the first report of a single-stage surgical repair without the aid of<br />
cardiopulmonary bypass of an ARSA, Kommerell diverticulum and common carotid trunk through<br />
a median sternotomy approach. Various other surgical and combined procedures are critically<br />
analysed.<br />
46
Simultaneous Bilateral Carotid Endarterectomy Personal Experience In 90 Patients<br />
Horia MURESIAN<br />
Cardiovascular Surgery, University Hospital of Bucharest<br />
Background. Although rarely performed the simultaneous bilateral carotid endarterectomy<br />
(SBCE) is generally indicated for bilateral symptomatic stenosis > 70% with intraplaque<br />
hemorrhage, ipsilateral symptomatic stenosis > 70% with contralateral severe asymptomatic<br />
stenosis and plaque hemorrhage, or bilateral > 80% stenosis.<br />
Materials and methods. The author presents his personal experience with 90 consecutive<br />
patients with SBCE performed either as a singular procedure or combined with vertebral or<br />
subclavian artery revascularization. Thirty nine patients were operated un<strong>de</strong>r general anesthesia,<br />
while 51 patients un<strong>de</strong>r loco-regional anesthesia (double cervical plexus block) allowing for a<br />
safer monitoring of the patients during the procedure and for selective shunting.<br />
Results. Global mortality was 1,1%. One minor hemispheric one major hemispheric stroke<br />
occurred. No postoperative cranial nerve palsies were encountered.<br />
Conclusions. SBCE represents a valuable surgical alternative in selected groups of patients.<br />
Loco-regional anesthesia enables a more precise monitoring of the patients and facilitates the use<br />
of this procedure in individuals with multiple and/or severe associated diseases: diabetes, chronic<br />
renal failure, cardiac failure and chronic lung disease.<br />
The Surgery for Vertebro-Basilar Arterial Insufficiency<br />
Horia MURESIAN<br />
Cardiovascular Surgery, University Hospital of Bucharest<br />
Background. When compared with the carotid system arterial diseases in the vertebrobasilar<br />
system are more difficult to diagnose and treat. Moreover, there is no unanimous opinion<br />
between centers and specialists, regar<strong>din</strong>g the timing of surgical treatment in the vertebro-basilar<br />
system and the necessary procedures to be applied. Concomitant lesions in the carotid arteries<br />
and their branches ren<strong>de</strong>r the clinical picture even more protean and more difficult to interpret.<br />
Materials and methods. A number of 38 consecutive patients with lesions affecting either<br />
solely the vertebro-basilar system or with associated lesions in the carotid system were operated<br />
over a three-year period. The surgical techniques were multiple and generally complex – as<br />
required by the severity of the arterial lesions or by the clinical manifestations. The main diagnostic<br />
elements and the resultant surgical procedures are extensively presented.<br />
Results. Revascularization of the vertebro-basilar system was highly-successful in the series<br />
studied with no mortality and with only a minor postoperative stroke in the carotid territory. In spite<br />
of their complexity the surgical manoeuvres did not complicate the intra- and the postoperative<br />
course of the patients. Intraoperative monitorization was facilitated by the use of loco-regional<br />
anesthesia.<br />
Conclusions. The <strong>de</strong>tailed diagnostic workup and a rich armamentarium of surgical<br />
techniques addressing the vertebro-basilar system represent necessary conditions for a proper<br />
and efficient approach to the patient with cerebrovascular disease. The author’s experience with<br />
a number of 38 cases draws attention toward this particular anatomic district, clinically<br />
manifesting mostly in non-characteristic ways, a system with a particular physiology, requiring<br />
individualized surgical indications and techniques.<br />
Jean-Baptiste Ricco<br />
University of Poitiers, France<br />
Carotid surgery: actual strategy<br />
How to write a paper in cardiovascular surgery<br />
47
Sesiunea VI<br />
An aggressive treatment improves midterm survival<br />
and amputation-free survival in CLI patients<br />
Francesco Spinelli, Francesco Stilo, Filippo Bene<strong>de</strong>tto, Giovanni De Caridi, Michele La Spada<br />
Unit of Vascular Surgery, Department of Cardiovascular and Thoracic Surgery,<br />
University of Messina, Italy.<br />
Background: CLI is a serious diseases lea<strong>din</strong>g to 44% of limb loss in 1 year. Previous reports<br />
have been principally focused on patency rate and technical success. The aim of this study was<br />
to un<strong>de</strong>rline the midterm results of surgical and endovascular treatment of CLI patients in term of<br />
functional results and impact on survival.<br />
Methods: We retrospectively analyzed the clinical data of 284 consecutive patients with<br />
CLI, who un<strong>de</strong>rwent primary treatment, between February 2004 and August 2008. A total of 201<br />
male (average age 71,08 years) and 83 female (average age 73,15 years) un<strong>de</strong>rwent 340<br />
operations: 80 EV procedures (23,5%), 160 tibial or plantar bypass graft (47%), and 100 hybrid<br />
procedures (29,4%). The indications to the type of treatment have been evaluated clinically and<br />
by ultrasound. In 56 patients (16. 4%) the procedures were bilateral. Sixty-five percent of the<br />
patients were diabetic, 13% had mild renal insufficiency (serum creatinine level > 2 mg/dL), and<br />
15% were in ESRD. Fifty-height percent had relevant cardiovascular comorbidities. The follow-up<br />
was performed by clinical and echo-duplex evaluation at 1-3-6-12 months and then every 6<br />
months up to 5 years. We retrospectively analyzed midterm results in terms of survival and<br />
amputation-free survival, and valued the predictive factors on <strong>de</strong>ath and limb loss.<br />
Results: All patients were revascularized; we didn't perform any primary amputation for CLI.<br />
The in-hospital survival and amputation-free survival were respectively 96,1% vs. 93%. The mean<br />
follow-up was 22. 25 months. During the follow-up 143 addition procedures (42%) were performed<br />
to assist the patency in 105 limbs (30,8%). Only 5 patients (1,8%) were lost of follow-up. Ninety-one<br />
<strong>de</strong>aths were recor<strong>de</strong>d (32,6%) and 36 limbs were amputated. Overall survival and amputationfree<br />
survival were 83,3% vs. 75,6%, 68,4% vs. 56,1%, 60,9% vs. 45,6% respectively at 1-, 3- and 5-years.<br />
The analysis showed that diabetes and dialysis are a prognostic factor for minor amputation and<br />
<strong>de</strong>ath respectively.<br />
Conclusion: Ev procedures and pedal bypass grafting <strong>de</strong>termined good functional limb<br />
salvage. The final end point of these procedures in CLI patients with advanced diseases has to be<br />
consi<strong>de</strong>red the survival and not only the patency. The precise selection of treatment based both<br />
on clinical and on morphological evaluation of patients allowed good early results. The good<br />
midterm results in term of survival and amputation-free survival were due to a strict follow-up that<br />
<strong>de</strong>termined multiple procedures of assistance. The aggressive and well-timed use of this two<br />
therapeutical options on CLI patients was the key point of this experience.<br />
Standard of Care for Popliteal Artery Aneurysm<br />
Marina Pacescu, SL Baila, DF Barzoi, R Halpern, Madalina Gavanescu<br />
Departement of Vascular Surgery,<br />
“C. C. Iliescu” Emergency Institute of Cardiovascular Disease, Bucharest, <strong>Romania</strong><br />
Popliteal artery aneurysms are the most common peripheral aneurysms. The aim of this<br />
study is to compare the standard of care in vascular patients with popliteal aneurysms between<br />
two periods: 1980-2004 (PI) and 2004 – 2009 (PII).<br />
Material and method: All file records of patients with popliteal aneurysm treated in our<br />
Clinic between 1980 and 2009 were retrospectively analyzed.<br />
Results: 26 patients (22 males and 4 females) with 26 popliteal aneurysms were in PI (1,04<br />
patients / year), and 15 patients (all males) with 17 politeal aneurysm were treated in PII (3<br />
patients / year). Mean age was 53 and 65. 8 in PI and PII respectively. All treated popliteal<br />
aneurysms had a diameter above 2,5 cm.<br />
0% (PI) and 6% (PII) of patients were asymtomatic, 19% (PI) and 35% (PII) were claudicants,<br />
27% (PI) and 35% (PII) had chronic rest pain, 0% (PI) and 18% (PII) had distal necrosis. 19% (PI) and<br />
0% (PII) of popliteal aneurysms were ruptured.<br />
48
All patients had digital substraction angiography. 46% (PI) and 18% (PII) had CT, 29% (PI)<br />
and 27% (PII) had MRI and 0% (PI) and 65% (PII) had Duplex echography.<br />
The procedure of choice was bypass of the aneurysm with vein or prosthetic graft<br />
associated by exclusion of aneurysm by proximal and distal ligature (50% (PI) and 71% (PII)),<br />
complete resection of aneurysm (19% (PI) and 12% (PII)), or partial resection of aneurysm with<br />
endo-suture of collaterals (23% (PI) and 6% (PII)).<br />
Distal thrombolysis for thrombosis of distal arterial trunks was performed in 3 cases (PI) with<br />
one good result. Distal thrombectomy was performed in 15% of cases (PI) and 29% of cases (PII).<br />
Primary amputation for irreversible ischemia was performed in 2 cases (8%) (PI).<br />
Secondary amputation after bypass thrombosis was performed in 3 cases (12%) (PI).<br />
Limb salvage was 81% in PI and 100% in PII.<br />
Conclusion: Early <strong>de</strong>tection and open repair of popliteal aneurysms can be done with<br />
good results.<br />
Aprecieri asupra rolul adipocitokinelor ”cheie” în iniţierea şi progresia leziunilor<br />
ateromatoase <strong>din</strong> afectiunile vasculare periferice<br />
Claudia Gherman 1, H. Silaghi 1, Anca Cristea 2, B. Olaru 1,<br />
F. Deme 1, A. Oprea 1, S. Rădulescu 1, A. Mironiuc 1<br />
1 Clinica Chirurgie II, 2Clinica Medicală I, U. M. F. “Iuliu Hatieganu" Cluj-Napoca<br />
Introducere. Arteriopatia cronică obliterantă a membrelor inferioare constituie un domeniu<br />
cu răspândire largă dar putin studiat, comparativ cu afectiunile cardio-metabolice.<br />
Ipoteza <strong>de</strong> cercetare. Scopul studiului l-a constituit extin<strong>de</strong>rea caracteristicilor clinice la<br />
pacientii cu arteriopatie cronica obliteranta <strong>de</strong> natură aterosclerotică prin posibila <strong>de</strong>terminare<br />
<strong>de</strong> noi markeri ai aterogenezei.<br />
Material si metoda. S-a luat in studiu un lot <strong>de</strong> 85 <strong>de</strong> pacienţi cu arteriopatie cronică<br />
obliterantă ateroscleotică a membrelor inferioare care au fost internati si tratati în Clinica<br />
Chirurgie II Cluj-Napoca şi un lot martor <strong>de</strong> un număr egal <strong>de</strong> pacienţi sănătoşi. Evaluarea<br />
factorilor <strong>de</strong> risc a fost facută întrebuinţând meto<strong>de</strong>le anamnestice şi examinările paraclinice.<br />
Factorilor <strong>de</strong> risc tradiţionali enunţaţi li s-au adăugat aprecieri ale nivelurilor serice ale rezistinei,<br />
adiponectinei, leptinei si α-TNF.<br />
Rezultate. In urma studiului efectuat s-a constatat diferenţă distinct semnificativă în ceea<br />
ce priveşte valoarea adiponectinei la arteriopaţi comparativ cu lotul martor. Diferenţă<br />
semnificativ statistic în ceea ce priveşte valoarea rezistinei s-a constatat pe loturile luate in studiu –<br />
media la arteriopaţi fiind distinct semnificativ mai mare <strong>de</strong>cât media coronarienilor fumători. TNFα,<br />
citokină inflamatorie eliberată în cantităţi mari la pacienţii obezi sau diabetici, are rol în iniţierea<br />
şi propagarea leziunilor aterosclerotice, dar nu a suferit variatii semnificative in studiul nostru.<br />
Concluzii. Corelând datele studiului nostru am putea trage concluzia conform căreia unii<br />
<strong>din</strong>tre parametrii urmăriţi pot fi corelaţi cu severitatea leziunilor <strong>din</strong> arteriopatia aterosclerotică.<br />
Dacă acest lucru se confirmă, aceşti factori pot fi eventual consi<strong>de</strong>raţi ca posibili factori<br />
predictivi, care <strong>de</strong>schid noi perspective <strong>de</strong> cercetare în domeniu.<br />
Aportul genomicii in studiul implicarii unor gene in afectiunile arteriale periferice<br />
Claudia Gherman 1, Ioana Constantinescu1, B. Stancu 1, B. Olaru 1, F. Deme 1, A. Eni 1, S.<br />
Rădulescu 1, A. Mironiuc 1, D. Pamfil 2, Ioana Petricele 2, Iulia Pop 2<br />
1 Clinica Chirurgie II, U. M. F. “Iuliu Ha ieganu" Cluj-Napoca,<br />
2 Platforma <strong>de</strong> Biotehnologie, USAMV Cluj-Napoca<br />
Introducere. Elucidarea importanţei geneticii moleculare în procesul aterosclerotic<br />
reprezintă o sarcină importantă aflată încă în stadiu incipient.<br />
Ipoteza <strong>de</strong> cercetare. Gena adiponectinei umane, cunoscută şi sub <strong>de</strong>numirile: ACDC;<br />
ADPN; APM1; APM-1; GBP28; ACRP30; adiponectin; ADIPOQ, este localizată pe cromozomul 3q27,<br />
la un locus cu susceptibilitate pentru sindromul metabolic şi diabetul <strong>de</strong> tip 2. Nivelele plasmatice<br />
ale adiponectinei s-au dovedit a fi scăzute în cazul diabetului <strong>de</strong> tip 2 şi a obezităţii, iar studii mai<br />
recente o implica si in ateroscleroza cu diferitele sale localizari. Aceste argumente ne-au<br />
<strong>de</strong>terminat sa intreprin<strong>de</strong>m studiul <strong>de</strong> fata.<br />
49
Material si metoda Pentru a genotipiza cei 65 <strong>de</strong> pacienţi cu afectiuni arteriale periferice<br />
<strong>de</strong> natura aterosclerotica ai lotului luat in studiu, pe lângă metoda bazată pe secvenţierea ADNului<br />
<strong>de</strong> interes, s-a utilizat şi metoda PCR-RFLP, aceasta prezentând costuri mai scăzute şi o uşurinţă<br />
mai mare <strong>de</strong> realizare. Pentru a fi validată metoda PCR-RFLP, rezultatele acesteia au fost<br />
comparate cu cele obţinute în urma secvenţierii probelor.<br />
Rezultate. Analizele <strong>de</strong> tip BLASTN au confirmat faptul că secventa produsului PCR<br />
corespun<strong>de</strong> cu secventa ADN i<strong>de</strong>ntificată în banca <strong>de</strong> gene a NCBI. Analizarea<br />
cromatogramelor a permis i<strong>de</strong>ntificarea unui singur polimorfism în poziţia 156, corespunzător<br />
rs1501299, respectiv în poziţia 7448975 a ADN genomic al ADIPOQ NC_000003. 10.<br />
Concluzii. Datele obtinute confirmă că strategia experimentală aplicată pentru<br />
i<strong>de</strong>ntificarea polimorfismelor la nivelul genei adiponectinei umane este corectă si permite<br />
evi<strong>de</strong>ntierea cu o precizie ridicată a tuturor modificărilor la nivel <strong>de</strong> secventă nucleotidică.<br />
Management of critical limb ischemia<br />
I. Droc, Florina Pinte, Francisca Blanca Calinescu, St. Deaconu, Nita A., Dumitrascu M., Popovici A.<br />
Army’s Center for Cardiovascular Diseases Bucharest<br />
Critical ischemia of the lower limbs represent the most severe form in the evolution of the<br />
lower limb atherosclerotic disease. The viability of the limb is threatened by the high risk of major<br />
amputation, around 25% per year. The general prognosis of the patient is also compromised.<br />
The preoperative evaluation resi<strong>de</strong>s in Echo Doppler, Angio MRI scanner and more less in<br />
arteriography.<br />
Surgical treatment remains the classical gold standard, but endoluminal treatment gains<br />
terrain, becoming the first choice in certain localizations (for ex. iliac). There are also situations<br />
when neither procedure can be applied, or they have both failed. Medical therapies, such as<br />
prostanoids, gene and cell therapy should not be forgotten.<br />
In our institution between January 2007 and May 2009, we operated on 164 patients<br />
(femuro-popliteo-tibial revascularization) of which 71% (130 patients) un<strong>de</strong>rwent classic open<br />
surgical intervention and 21% (34 patients) endovascular intervention.<br />
Regar<strong>din</strong>g the distal anasthomosis we used preformed PTFE prostheses (Distaflo-<br />
IMPRA/Bard) in 5 cases and the Miller cuff in 2 cases.<br />
The follow-up was between 1 and 24 months with an average of 12 months.<br />
Primary permeability in patients with “cuff” or distaflo was 96% in the first month and 92% at<br />
6 months.<br />
In conclusion, endovascular treatment, when it is feasible can be regar<strong>de</strong>d as first-choice<br />
treatment for patients with multiple lesions, or for those who present high risk for surgery.<br />
S. Rădulescu, A. Zanfir, C Gherman<br />
Second Surgical Clinic, University of Medicine and<br />
Pharmacy “Iuliu Haţieganu”, Cluj Napoca<br />
Complicaţii postoperatorii în chirurgia convenţională a<br />
bolii varicoase.<br />
Postoperative complications in the conventional<br />
surgery of varicose vein disease<br />
Cardiovascular Un<strong>de</strong>rlying Pathology And Early Results In Surgical Arterial<br />
Thromboembolectomy For Upper Limb Acute Ischemia – 10 Years Experience<br />
Patologia cardiovasculară asociată şi rezultatele imediate în trombembolectomia arterială<br />
chirugicală pentru ischemia acută a membrului superior – 10 ani <strong>de</strong> experienţă.<br />
NJ Tesoiu, Marina Pacescu, SL Baila, DF Barzoi, I Diaconescu, F Cosa, R Halpern, Isabella Oprea,<br />
Mirela Marcu, A<strong>din</strong>a Stoica, M Croitoru, Daniela Mitcov<br />
Institute for Emergencies in Cardiovascular Diseases “Prof. Dr. CC Iliescu”, Bucharest, <strong>Romania</strong><br />
Background: Fogarty balloon catheter surgical treatment is the most common used in<br />
upper limb arterial thromboembolic acute ischemia. The presence of cardiovascular un<strong>de</strong>rlying<br />
pathology is the major cause of postoperative complications and <strong>de</strong>aths. Re-operations as well as<br />
local complications are relatively important events in these patients. Upper limb thromboembolism<br />
should be consi<strong>de</strong>red as one manifestation of a systemic embolism and as imposing severe<br />
anticoagulant therapy.<br />
50
Objectives: To present the cardiovascular un<strong>de</strong>rlying pathology and the early results in<br />
patients with surgical upper limb arterial thromboembolectomy performed in emergency in the<br />
same location within a 10 years period of time.<br />
Material and Methods: Retrospective study of the operative files of 250 consecutive<br />
patients operated between January the 1-st 1998 and December the 31-st 2007 regar<strong>din</strong>g<br />
cardiovascular pathologic circumstances in which acute upper limb ischemia caused by arterial<br />
thromboembolism appeared and the early postoperative results.<br />
Results: There were 142 women (median age 71 years, limits 23-90 years) and 108 men (median<br />
age 70 years, limits 42-92 years). Cardiovascular pathologic circumstances were represented by<br />
atrial fibrillation – 132 cases, coronary artery disease – 52 cases, cardiac valvulopathy – 28 cases,<br />
conduction disturbances – 13 cases, stroke sequels – 28 cases, systemic hypertension – 75 cases,<br />
cor pulmonale – 8 cases, diabetes mellitus – 16 cases, aortic dissecting aneurysm – 1 case. Very<br />
good results were obtained in 222 cases. Re-operation for re-embolisation in the same or different<br />
territory (26 cases) and for local complications (2 cases) resulted in limb preservation in 22 cases;<br />
five major amputations (arm and forearm) were imposed and one patient died.<br />
Conclusions: Upper limb acute ischemia caused by arterial thromboembolism arrived<br />
more often in women than in men, in el<strong>de</strong>rly and with serious cardiovascular un<strong>de</strong>rlying pathology<br />
requiring a<strong>de</strong>quate therapy patients. Very good early results were obtained in 89% of the cases.<br />
Re-operations resulted in limb salvation in 78% of the cases. Survival rate was 97%.<br />
Keywords: Cardiovascular pathology, Surgical thromboembolectomy, Upper limb acute ischemia<br />
Patologia cardiovasculară asociată şi rezultatele imediate în trombembolectomia arterială<br />
chirugicală pentru ischemia acută a membrului superior – 10 ani <strong>de</strong> experienţă.<br />
Premize: Tratamentul chirurgical cu sonda cu balon <strong>de</strong>scrisa <strong>de</strong> Fogarty este cel mai<br />
utilizat in ischemia acuta tromboembolica arteriala a membrului superior. Prezenta patologiei<br />
asociate cardiovasculare constituie cauza majora a complicatiilor postoperatorii si <strong>de</strong>ceselor.<br />
Reinterventiile si complicatiile locale sunt evenimente relative importante la acesti pacienti.<br />
Tromboembolismul membrului superior ar trebui consi<strong>de</strong>rat ca o manifestare a embolismului<br />
sistemic si ca impunand tratament anticoagulant sever.<br />
Obiective: Prezentarea patologiei cardiovasculare asociate si rezultatelor imediate la<br />
pacientii cu tromboembolectomie arteriala la membrul superior efectuata in urgenta in acelasi<br />
serviciu intr-o perioada <strong>de</strong> timp <strong>de</strong> 10 ani.<br />
Material si metoda: Studiu retrospective asupra fiselor operatorii pentru 250 pacienti<br />
consecutivi operati intre 1 ianuarie 1998 si 31 <strong>de</strong>cembrie 2007 in ceea ce priveste circumstantele<br />
patologice cardiovasculare in care apare ischemia acuta a membrului superior prin<br />
tromboembolism arterial si rezultatele postoperatorii imediate.<br />
Rezultate: Au fost operati 142 femei (varsta medie 71 ani, limite 23-90 ani) si 108 barbati<br />
(varsta medie 70 ani, limite 42-92 ani). Circumstantele patologice cardiovasculare au fost<br />
reprezentate <strong>de</strong> fibrilatia atriala – 132 cazuri, boala arteriala coronariana – 52 cazuri, valvulopatia<br />
cardiaca – 28 cazuri, tulburarile <strong>de</strong> conducere – 13 cazuri, sechelele atacului cerebral – 28 cazuri,<br />
hipertensiunea arteriala – 75 cazuri, cordul pulmonar – 8 cazuri, diabetul zaharat – 16 cazuri si<br />
anevrismul disecant <strong>de</strong> aorta – 1 caz. Rezultate foarte bune au fost obtinute in 222 cazuri.<br />
Reinterventia pentru reembolizare in acelasi teritoriu sau un altul (26 cazuri) si pentru complicatii<br />
locale (2 cazuri) a condus la salvarea membrului in 22 cazuri; s-au impus 5 amputatii majore (brat<br />
si antebrat) si un pacient a <strong>de</strong>cedat.<br />
Concluzii: Ischemia acuta a membrului superior provocata <strong>de</strong> tromboembolism arterial a aparut<br />
mai ales la femei fata <strong>de</strong> barbati si la pacienti varstnici si cu patologie cardiovasculara grava<br />
asociata. Rezultate foarte bune au fost obtinute in 89% <strong>din</strong>tre cazuri. Reinterventia a dus la<br />
salvarea membrului in 78% <strong>din</strong>tre cazuri. Rata <strong>de</strong> supravietuire a fost 97%.<br />
Cuvinte cheie: Patologie cardiovasculara, Tromboembolectomie chirurgicala, Ischemie acuta a<br />
membrului superior.<br />
51
Surgery Summer School Might Raise Medical Stu<strong>de</strong>nts Interest In Cardiovascular Surgery<br />
Educarea interesului pentru chirurgia cardiovasculară la stu<strong>de</strong>nţii medicinişti la şcoala <strong>de</strong> vară<br />
Grigore Tinica 1, Andrei Dumbrava 2, Diana Ciurescu 2,<br />
Mihail Enache 1, Vasile Cepoi 3, Vasile Astarastoae 1<br />
1Univesity of Medicine and Pharmacy "Gr. T. Popa" Iasi, <strong>Romania</strong><br />
2Cardiovascular Institute, Iasi, <strong>Romania</strong><br />
3Clinical and Experimental Cardiovascular Research Foundation<br />
Objectives. A <strong>de</strong>cline in applicants to Cardiovascular Surgery Training Programs has been<br />
observed in the late years, in European countries (e. g., Gott et al., 2006). Consequently, increased<br />
efforts in recruiting trainees toward the field are required. In the present study, we tested the<br />
hypothesis that organizing international stu<strong>de</strong>nt groups in the summer break for mentored<br />
instructions in cardiovascular <strong>de</strong>partment and operating room will enhance the interest of junior<br />
medical stu<strong>de</strong>nts for cardiovascular surgery.<br />
Materials-methods. The participants, medical stu<strong>de</strong>nts interested in surgery from different<br />
countries (USA, Canada, UK, Portugal, France, Netherlands, Germany, Italy, Malta, Slovenia,<br />
Serbia, Macedonia, Kosovo, Egypt) received mentored training for two weeks, in a <strong>de</strong>partment of<br />
cardiovascular surgery with state of the art technology. It consisted from an initial lecture<br />
presented by an experienced cardiovascular surgeon, followed by practical simulations in the<br />
“vet lab” (consisting of mentored dissections and practicing surgical suture using hearts and great<br />
vessels from pigs and cows) and by participation, as direct observers, in the operating room. Their<br />
perception and interest regar<strong>din</strong>g the cardiovascular surgery have been assessed by<br />
questionnaire, before and after the summer school.<br />
Results. Sixtythree medical stu<strong>de</strong>nts participated in summer schools in the last years.<br />
Initially, most of them (77. 3%) were interested in pursuing a career in surgery, majority (72. 7%)<br />
being neutral regar<strong>din</strong>g a preference for a career in cardiovascular surgery (only 3 stu<strong>de</strong>nts [4,<br />
75%] were <strong>de</strong>termined to choose cardiovascular surgery as their specialization). At the end of the<br />
summer school, more than a half (57%) of them agreed or strongly agreed to a career in<br />
cardiovascular surgery (p < 0. 001). When asked to select an eventual optional course for the<br />
following year, less than a third (31, 3%) of the stu<strong>de</strong>nts selected cardiovascular surgery before<br />
summer school versus almost two thirds (61, 4%) at the end of it (p < 0. 001).<br />
Discussion. It is critical to expose medical stu<strong>de</strong>nts to cardiovascular surgery early, in their<br />
preclinical years, if we want them to choose a career in this field. Our program, similar (<strong>de</strong>spite<br />
being shorter) to that of the Johns Hopkins Medical School from Baltimore, Maryland (Allen et al.,<br />
2009) offered them a broad spectrum of what cardiac surgery is all about. In our opinion, this kind<br />
of program, aimed to attracting medical stu<strong>de</strong>nts through operative skills training proved to be<br />
successful in encouraging stu<strong>de</strong>nts to pursue a cardiovascular resi<strong>de</strong>ncy.<br />
Conclusions. The surgery summer school and the introduction of stu<strong>de</strong>nts to the reality of<br />
an operating theatre and the procedures used during cardiovascular surgery have proved to be<br />
an effective way of attracting medical stu<strong>de</strong>nts to cardiovascular specialty. Participating in the<br />
international surgery summer school improves attitu<strong>de</strong>s towards cardiovascular surgery as a<br />
career choice and correlates with a greater interest in selecting an optional cardiovascular<br />
surgery course for the following year of study in the university.<br />
The <strong>Romania</strong>n Society of Cardiovascular Surgery should organize, with the help of its<br />
members, stu<strong>de</strong>nt groups for summer courses in different centers to promote the cardiovascular<br />
surgery specialty among the stu<strong>de</strong>nts.<br />
References<br />
1. J. G. Allen, E. S. Weiss, N. D. Patel, D. E. Alejo, T. P. Fitton, J. A. Williams, C. J. Barreiro, L. U. Nwakanma, S. C.<br />
Yang, D. E. Cameron. Inspiring Medical Stu<strong>de</strong>nts to Pursue Surgical Careers: Outcomes From Our Cardiothoracic<br />
Surgery Research Program, Ann Thorac Surg, 2009; 87 (6): 1816 - 1819.<br />
2. Gott VL, Patel ND, Yang SC, Baumgartner WA. Attracting outstan<strong>din</strong>g stu<strong>de</strong>nts (premedical and medical) to a<br />
career in cardiothoracic surgery, Ann Thorac Surg 2006: 82: 1-3<br />
Obiective: În ultimii ani, s-a observat o scă<strong>de</strong>re a numărului <strong>de</strong> aplicanţi pentru<br />
programele <strong>de</strong> instruire în chirurgia cardiovasculară, în ţările europene (e.g., Gott et al., 2006),<br />
astfel că sunt necesare eforturi sporite în atragerea stagiarilor către acest domeniu. În studiul <strong>de</strong><br />
faţă, am verificat ipoteza că organizarea <strong>de</strong> grupuri stu<strong>de</strong>nţeşti internaţionale, în cursul<br />
vacanţelor <strong>de</strong> vară, pentru training în laboratorul <strong>de</strong> chirurgie (“vet lab”) şi în sala <strong>de</strong> operaţie<br />
cardiovasculară, ar putea spori interesul stu<strong>de</strong>nţilor medicinişti pentru chirurgia cardiovasculară.<br />
52
Materiale şi meto<strong>de</strong>. Participanţii, stu<strong>de</strong>nţi la medicină interesaţi <strong>de</strong> domeniul chirurgical,<br />
<strong>din</strong> diferite ţări (SUA, Canada, Marea Britanie, Portugalia, Franţa, Olanda, Germania, Italia, Malta,<br />
Slovenia, Serbia, Macedonia, Kosovo, Egipt), au primit training supravegheat, cu o durată <strong>de</strong><br />
două săptămâni, într-un <strong>de</strong>partament <strong>de</strong> chirurgie cardiovasculară cu tehnologie <strong>de</strong> ultimă oră.<br />
Acesta a constat <strong>din</strong>tr-un curs iniţial introductiv, ţinut <strong>de</strong> către un chirurg cardiovascular cu<br />
experienţă, urmat <strong>de</strong> simulări practice în “vet lab” (disecţii îndrumate şi exersarea suturii<br />
chirurgicale, utilizând inimi şi vase mari <strong>de</strong> porc şi vacă) şi <strong>de</strong> participarea, în calitate <strong>de</strong><br />
observatori direcţi, la intervenţiile chirurgicale cardiovasculare curente. Percepţia şi interesul<br />
privitoare la chirurgia cardiovasculară au fost evaluate prin metoda chestionarului, înaintea şi la<br />
finalul şcolii <strong>de</strong> vară.<br />
Rezultate. Şaizeci şi trei <strong>de</strong> stu<strong>de</strong>nţi la medicină au participat la şcolile <strong>de</strong> vară în ultimii ani.<br />
Iniţial, cei mai mulţi (77,3%) erau interesaţi în a continua o carieră în chirurgie, majoritatea (72,7%)<br />
<strong>de</strong>clarându-se neutri în ceea ce priveşte alegerea preferenţială a chirurgiei cardiovasculare<br />
(doar 3 stu<strong>de</strong>nţi [4,75%] se <strong>de</strong>clarau hotărâţi în a o alege drept specializare). La sfârşitul şcolii <strong>de</strong><br />
vară, mai mult <strong>de</strong> jumătate (57%) <strong>din</strong>tre stu<strong>de</strong>nţi se <strong>de</strong>clarau <strong>de</strong> acord sau puternic <strong>de</strong> acord cu<br />
alegerea unei cariere în chirurgie cardiovasculară (p < 0,001). Rugaţi să-şi selecteze un curs<br />
opţional pentru anul următor, mai puţin <strong>de</strong> o treime (31,3%) <strong>din</strong>tre stu<strong>de</strong>nţi au ales chirurgia<br />
cardiovasculară înaintea începerii şcolii <strong>de</strong> vară, comparativ cu aproape două treimi (61,4%)<br />
după terminarea acesteia (p < 0,001).<br />
Discuţii. Este esenţial a atrage stu<strong>de</strong>nţii la medicină către chirurgia cardiovasculară, în anii<br />
lor preclinici, dacă se urmăreşte îndrumarea opţiunii lor către o carieră în acest domeniu.<br />
Programul nostru, similar (<strong>de</strong>şi mai scurt) celui <strong>de</strong> la Şcoala <strong>de</strong> Medicină Johns Hopkins <strong>din</strong><br />
Baltimore Maryland (Allen et al., 2009), le-a oferit un spectru larg <strong>de</strong>spre ce înseamnă chirurgia<br />
cardiacă. În opinia noastră, acest tip <strong>de</strong> program, care are drept scop atragerea stu<strong>de</strong>nţilor la<br />
medicină, prin formarea competenţelor chirurgicale s-a dovedit a fi <strong>de</strong> succes în încurajarea<br />
stu<strong>de</strong>nţilor <strong>de</strong> a urma un rezi<strong>de</strong>nţiat în chirurgia cardiovasculară<br />
Concluzii. Şcoala <strong>de</strong> Vară <strong>de</strong> chirurgie cardiovasculară şi introducerea stu<strong>de</strong>nţilor în<br />
realitatea unei săli <strong>de</strong> operaţie cardiovasculară şi a procedurilor folosite în timpul intervenţiei<br />
chirurgicale cardiovasculare pare a se dovedi o modalitate eficientă <strong>de</strong> atragere a stu<strong>de</strong>nţilor<br />
medicinişti către această specialitate. Participarea la şcoala <strong>de</strong> vară internaţională <strong>de</strong> chirurgie<br />
îmbunătăţeşte atitu<strong>din</strong>ea faţă <strong>de</strong> chirurgia cardiovasculară în alegerea unei cariere şi se<br />
corelează cu un interes crescut în optarea pentru un curs facultativ <strong>de</strong> chirurgie cardiovasculară<br />
în cadrului anului următor <strong>de</strong> studiu în universitate. Societatea Romană <strong>de</strong> Chirurgie<br />
Cardiovasculară ar putea să organizeze, cu ajutorul membrilor săi, grupuri <strong>de</strong> stu<strong>de</strong>nţi pentru<br />
cursuri <strong>de</strong> vară în diferite ţări pentru a promova specialitatea chirurgiei cardiovasculare în rândul<br />
acestora<br />
BIBLIOGRAFIE<br />
1. J. G. Allen, E. S. Weiss, N. D. Patel, D. E. Alejo, T. P. Fitton, J. A. Williams, C. J. Barreiro, L. U. Nwakanma, S. C.<br />
Yang, D. E. Cameron, et al. Inspiring Medical Stu<strong>de</strong>nts to Pursue Surgical Careers: Outcomes From Our<br />
Cardiothoracic Surgery Research Program. Ann Thorac Surg, 2009; 87(6): 1816 - 1819.<br />
2. Gott VL, Patel ND, Yang SC, Baumgartner WA. Attracting outstan<strong>din</strong>g stu<strong>de</strong>nts (premedical and medical) to a<br />
career in cardiothoracic surgery. Ann Thorac Surg, 2006;82:1-3<br />
The use of aortic iliac endovascular prosthesis for infrarenal abdominal aortic aneurysm<br />
D. Trandafir, Silvia Condu, R. Nechifor*, B. Dorobat*, Cristina Tudor**, Ana Filimon<br />
Department of Cardiovascular Surgery, *Department of Radiology,<br />
**Department of Anesthesiology University Hospital of Bucharest<br />
The abdominal aortic aneurysm usually present frequent in el<strong>de</strong>rly patients with serious<br />
cardiovascular comorbidities that pose a great challenge to the atten<strong>din</strong>g surgeon. Surgical<br />
repair involve major risks for this patients.<br />
We report a case of a 63 years old patient where we choose elective endovascular repair.<br />
The patient associate comorbidities such as major surgical abdominal interventions, smoking,<br />
obesity, hypertension, hiperlipemy<br />
It was performed the implantation of the aortic iliac Gore Exclu<strong>de</strong>r endovascular prosthesis<br />
with iliac extension with both femoral arteries surgical abort, un<strong>de</strong>r peridural anesthesia.<br />
The patient received 2 units of blood transfused and 2 units of fresh frozen plasma.<br />
The average hospitalization time was 7 days.<br />
53
The intervention was a success, the abdominal aortic aneurysm was repaired without<br />
endoleak, surgical inci<strong>de</strong>nts with well vascularisated legs with peripheral pulses in all the elations<br />
points.<br />
Simpozion Vasaprostan<br />
Sesiunea VII<br />
Mo<strong>de</strong>rator: I. Droc<br />
Open Surgery versus endovascular treatment for abdominal aortic aneurysms<br />
Chirurgie clasică versus endovasculară în tratamentul anevrismului <strong>de</strong> aortă abdominală.<br />
I. Droc, Pinte Fl, Cristian G, Dumitrascu M., Deaconu St., Calinescu F, Murgu V.<br />
Army, s Center for cardiovascular diseases, Bucharest, <strong>Romania</strong><br />
Endovascular abdominal aortic aneurysm repair (EVAR) was introduced by Parodi in 1991,<br />
and since then, the technique has gained popularity due to the significant advantages over open<br />
repair. Several large randomized, controlled, multicentre trials (EVAR1, DREAM) have reported a<br />
reduction in morbidity and mortality associated with EVAR. Two recent studies have specifically<br />
examined the results of AAA repair in high risk cohorts. Sicard et al. (2006) reported a mortality rate<br />
of 2,9% for EVAR and 5,1% for open repair. Bush et al. (2007) found the EVAR mortality rate to be<br />
3,4% compared to 5,2% in the open group.<br />
Our study examined the outcomes of patients with AAA un<strong>de</strong>rgoing EVAR in terms of AAA<br />
related mortality, complication rate and reintervention rate, in or<strong>de</strong>r to inform the ongoing<br />
management <strong>de</strong>bate.<br />
In our <strong>de</strong>partment, between july 2008 and <strong>de</strong>c. 2009, 11 patients un<strong>de</strong>rvent EVAR for AAA,<br />
un<strong>de</strong>r epidural anaesthesia. We used different types of endografts (Anaconda-1p, Medtronic<br />
Talent -3p, Powerlink-7p). The mean hospitalisation time was 3 days. The follow up was done by CTscan<br />
in paralel with dopler ultrasound at 1, 3, 6 months and at 1year postop. No endoleaks or<br />
infection on postop.<br />
Trusting the inevitable progress of newer technology we believe that, in the future, the<br />
great majority of AAAs will be treated via EVAR. The <strong>de</strong>vices will continue to improve, as it will<br />
<strong>de</strong>ployment techniques. For now until greater <strong>de</strong>vice durability is established EVAR remains an<br />
imperfect long-term treatment and requires regular life-long graft surveillance, and it should be<br />
limited to those with large AAAs and „suitable anatomy”, specifically those who prezent high risk<br />
for open repair.<br />
Daniel Nica, M. Gaşpar, P. Deutsch, D. Cioata,<br />
C. Juşca, G. Dumitraşciuc, H. Feier, A. Merce, A.<br />
Ionescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara, Clinica <strong>de</strong><br />
Chirurgie Cardiovasculară II<br />
Surgical approach of abdominal aortic aneurysms:<br />
clinical experience ian 2003- <strong>de</strong>c 2009<br />
Surgical Approach of Abdominal Aortic Aneurysms Clinical Experience,<br />
Jan 2003 – <strong>de</strong>c 2009<br />
D. Nica, M. Gaspar, P. Deutsch, D. Cioata, C. Jusca,<br />
G. Dumitrasciuc, H. Feier, A. Merce, A Ionescu.<br />
Timisoara Cardiovascular Medicine Institute, cardiovascular Surgery Department II<br />
Objectives: to analyse the results of surgical approach in abdominal aortic aneurysms<br />
showing the importance of different therapeutic strategies <strong>de</strong>pendig on elective or emergency<br />
caracter of the cases.<br />
Methods: retrospective study inclu<strong>din</strong>g patients from Cardiovascular Surgery Department II<br />
of Timisoara Cardiovascular Diseases Institute operated between january 2003 – <strong>de</strong>cember 2009,<br />
based upon the analysis of epi<strong>de</strong>miological, clinical and surgical data from the medical files. We<br />
analized 60 cases (5,08%) of abdominal aortic aneurysm, from which 57 with infrarenal aneurysm<br />
and 3 with toraco-abdominal aneurysm. There were 20 emergency cases (33,3%) and 40 elective<br />
cases (66,6%), diagnosed using abdominal ecography 41,6%, abdominal-CT, 28,3%,<br />
54
angiocoronarography, 66,6%, multislice 64-CT, 33,3%, angio-MRI, 3,33%. Demografic data revealed<br />
gen<strong>de</strong>r male predominance (90%), and in ptients over 60 years old (81,6%). Associated morbidity<br />
was chronic ischemic heart disease (50%), peripheral arterial disease (25%), arterial hypertension<br />
(66,6%), dyslipi<strong>de</strong>mia (50%).<br />
Results: Complex medical and surgical therapy, reprezented by emergency operation<br />
(30%) and elective operation 70%, surgical tehnique used was aneurysm rezection and restoring<br />
the arterial flow by interposition of tubular prosthesis (43,3%), or by-pass aorto-bbifemural (56,6%).<br />
The evolution was favorable in most cases (85%), but in emergency operations evolution was<br />
unfavorable (15%), with complications such as lower limb ischemia (1,66%), retroperitoneal<br />
blea<strong>din</strong>g (3,33%), upper gastrointestinal blea<strong>din</strong>g (3,33%), cerebral stroke (1,66%), multiple sitems<br />
and organs failure (1,66%), lea<strong>din</strong>g to an overall mortality of (10%).<br />
Conclusions: Aortic abdominal aneurysms predominantly affects male patients over 60<br />
years of age, reprezenting a redoubtable cardiovascular pathology. While elective operated<br />
cases, even with asociated pathology, have good results with favorable postoperative evolution,<br />
emergency operated cases for ruptured aneurysms presents severe evolution with still high<br />
mortality rate.<br />
Abordarea chirurgicală a anevrismelor <strong>de</strong> aortă abdominală: experienţa clinică ian. 2003- <strong>de</strong>c. 2009.<br />
Obiective: Analiza rezultatelor tratamentului chirurgical al anevrismelor <strong>de</strong> aorta<br />
abdominala cu importanta diferentierii strategiei terapeutice in functie <strong>de</strong> caracterul electiv sau<br />
<strong>de</strong> urgenta al cazului.<br />
Material şi metodă: Studiu retrospectiv cuprinzând pacienţi operaţi in Clinica <strong>de</strong> Chirurgie<br />
Cardio-Vasculară II a IBCV Timişoara în perioada ianuarie 2003 – <strong>de</strong>cembrie 2009 şi realizat prin<br />
analiza aspectelor epi<strong>de</strong>miologice, clinice, chirurgicale <strong>din</strong> baza <strong>de</strong> date. Din 4889 <strong>de</strong> interventii<br />
chirurgicale, au fost 1181 (24%) <strong>de</strong> operatii vasculare <strong>din</strong> care am analizat 60 <strong>de</strong> cazuri cu<br />
anevrism <strong>de</strong> aorta abdominala (5,08%), <strong>din</strong> care 57 (95%) cu anevrism <strong>de</strong> aorta abdominala<br />
infrarenala şi 3 (5%) cazuri cu anevrism <strong>de</strong> aorta toraco-abdominala, evi<strong>de</strong>ntiate prin ecografie<br />
abdominala – 25 cazuri (41,6%), CT abdominal – 17 cazuri (28,3%), angiocoronarografie – 40 cazuri<br />
(66,6%), angio-CT- „64-slice” – 20 cazuri (33,3%), angio-RMN – 2 cazuri (3,33%). Au fost 20 <strong>de</strong> cazuri<br />
(33,3%) prezentate in urgenta, iar 40 cazuri (66,6%) reglate. Datele <strong>de</strong>mografice indica<br />
predominenta clara la bărbaţi 54 (90%) şi la pacienţi cu vârsta peste 60 <strong>de</strong> ani 49 (81,6%).<br />
Diagnosticul imagistic: Morbiditatea asociata a fost: cardiopatie ischemica cronica – 30 cazuri<br />
(50%), arteriopatie cronica obliteranta periferica – 15 cazuri (25%), HTA – 40 cazuri (66,6%),<br />
dislipi<strong>de</strong>mie – 30 cazuri (50%).<br />
Rezultate: Tatamentul complex, medical si chirurgical: interventia chirurgicala efectuata<br />
<strong>de</strong> urgenta - 18 cazuri (30%), si reglata 42 cazuri (70%), reprezentata <strong>de</strong> rezectia anevrismului cu<br />
refacerea fluxului arterial prin interpozitie <strong>de</strong> proteza tubulara – 26 cazuri (43,3%), sau prin by-pass<br />
aorto-bifemural – 34 cazuri (56,6%). Evolutia favorabila in 51 cazuri (85%), nefavorabila 9 cazuri<br />
(15%) – <strong>din</strong> care 8 cazuri la operatiile <strong>de</strong> urgenta, complicatiile severe fiind hemoragie<br />
retroperitoneala, HDS, AVC, IRA, MSOF, ischemie periferica, <strong>de</strong>terminand o mortalitate <strong>de</strong> 10% (6<br />
cazuri).<br />
Concluzii: Anevrismele aortei abdominale afecteaza predominant barbatii peste 60 ani,<br />
reprezintand o patologie cardiovasculara redutabila. Cazurile operate electiv, chiar cu patologie<br />
asociata, au rezultate bune cu evolutie favorabila, insa cazurile <strong>de</strong> anevrism rupt operate in<br />
urgenta, au evolutie nefavorabila, cu o mortalitate inca mare.<br />
Sesiunea VIII<br />
Endovascular procedures for abdominal aorta false aneurysms<br />
Tratamentul endovascular în pseudoanevrismele aortei abdominale<br />
Silaghi H 1, Magnan PE 2, Branchereau A 2, Gherman C 1, Mironiuc A 1<br />
1 2 nd Surgical Clinic, U. M. Ph. “Iuliu Haţieganu”, Cluj-Napoca<br />
2 Service <strong>de</strong> Chirurgie Vasculaire, Hôpital Timone, Marseille, France<br />
Introduction: Anastomotic false aneurysms are rare but severe complications after<br />
reconstructive surgery of the abdominal aorta, lea<strong>din</strong>g mainly to ruptures and aorto-enteric fistula.<br />
FAAA represent a formal surgery indication, being associated to high mortality risk. Endovascular<br />
55
false aneurysm repair (EVFAR) avoids recurrent approach and aortic clamping, representing a<br />
low-risk alternative for open surgery that records eloquent mortality, ranging 8-28%.<br />
Method: 15 patients (15 men) were submitted to EVFAR between March 2001-October<br />
2005. A former Dacron graft was used for aortic reconstruction in all cases. Mean age was 72<br />
years (ranging 54-85) and mean <strong>de</strong>lay between former surgery and FAAA <strong>de</strong>tection was 15 years<br />
(ranging 9-20). 11 patients out of 15 were asymptomatic. Mean FAAA diameter was 59 mm (43-70<br />
mm). In 11 patients, we used aorto-uniiliac <strong>de</strong>gressive stent-grafts associated to a cross-over<br />
bypass, while in 4 patients tubular aortic stent-grafts were used. 6 patients required preoperative<br />
embolisation procedure.<br />
Results: All stent-grafts were successfully <strong>de</strong>ployed. Mean procedure <strong>de</strong>lay was 135<br />
minutes (60-220 minutes). Mean X-ray exposure was 14 minutes (10-25 minutes). EVFAR procedures<br />
required an average quantity of 150ml contrast product (100-230ml). Mean in-hospital stay was 10.<br />
6 days (5-24 days), no perioperative <strong>de</strong>ath was recor<strong>de</strong>d. During the 5-years postoperative<br />
surveillance, 5 <strong>de</strong>aths were recor<strong>de</strong>d (2 cardiac complications, 1 stroke, 1 pulmonary cancer, 1<br />
highway acci<strong>de</strong>nt); 1 stent-graft occlusion required an axillo-femoral bypass; 2 distal stent-graft<br />
stenosis required PTA.<br />
Conclusions: EVFAR must be consi<strong>de</strong>red especially for high risk patients offering similar<br />
results to open surgery. Preoperative embolisation and other associated surgical procedures are<br />
frequently required. Long-term surveillance is necessary for the assessment of final results.<br />
Expresia citokinelor inflamatorii la nivelul ţesutului adipos epicardic şi relaţia cu boala<br />
aterosclerotică coronariană<br />
1 Alina Silaghi, 2 Horaţiu Silaghi, 3 Traian Scridon,<br />
2 Aurel Mironiuc, 2 Şerban Rădulescu 4 Michel Grino<br />
1 Clinica Endocrinologică Spitalul Clinic Ju<strong>de</strong>ţean Cluj,<br />
2 Clinica Chirurgie II UMF "Iuliu Haţieganu" Cluj, 3 Institutul Inimii UMF "Iuliu Haţieganu"Cluj<br />
4 INSERM U626, Faculté <strong>de</strong> Mé<strong>de</strong>cine, Aix-Marseille Université, Marseille, France<br />
Introducere: Ţesutul adipos epicardic (TAE) este un <strong>de</strong>pozit ectopic <strong>de</strong> ţesut adipos situat<br />
în contact direct cu miocardul <strong>de</strong> care nu este <strong>de</strong>spărţit printr-o fascie. TAE înconjură vasele inimii<br />
şi poate influenţa homeostazia coronariană prin sinteza citokinelor inflamatorii.<br />
Scop: Evaluarea expresiei principalelor citokine inflamatorii şi stabilirea unei legături cu<br />
statusul coronarian<br />
Material şi metodă: S-au realizat biopsii <strong>de</strong> TAE şi ţesut adipos subcutanat (TAS) <strong>de</strong> la 32<br />
pacienţi, 11 femei si 21 bărbaţi, cu vârsta între 36 şi 72 ani, cu IMC-ul mediu <strong>de</strong> 27,2±1,2; 18 fiind<br />
coronarieni şi 14 non-coronarieni. Am studiat prin qRT-PCR expresia principalelor adipokine<br />
inflamatorii: IL-1, IL-6, TNF-α, MCP-1<br />
Rezultate: Intre cele două grupuri, coronarieni şi non coronarieni, există o diferenţă <strong>de</strong><br />
expresie a MCP-1, dar ea este nu semnificativă statistic nici pentru TAS (p = 0,28) şi nici pentru TAE<br />
(p = 0,9). Utilizând un test <strong>de</strong> tip Wilcoxon, am comparat expresia ARNm al TNF-α între TAE si TAS în<br />
grupul <strong>de</strong> pacienţi fără coronaropatie, diferenţa găsită fiind nesemnificativă statistic (p = 0,17). In<br />
grupul <strong>de</strong> pacienţi coronarieni am găsit o diferenţă semnificativă a expresiei TNF-α între TAE si TAS<br />
utilizând acelasi tip <strong>de</strong> test (p = 0, 037). La pacienţii coronarieni am găsit o crestere semnificativă a<br />
expresiei IL-6 si IL-1ß în TAE fata <strong>de</strong> TAS utilizând acelasi tip <strong>de</strong> test (p = 0,031).<br />
Concluzii: TAE se caracterizează printr-un nivel crescut al expresiei adipokinelor inflamatorii<br />
şi ar putea contribui printr-un efect local la agravarea bolii aterosclerotice coronariene.<br />
Cuvinte cheie: ţesut adipos epicardic, citokine inflamatorii, boala aterosclerotică<br />
coronariană<br />
Cerebral response after carotid artery revascularisation<br />
Cerebral hiperperfusion syndrome<br />
Răsunetul revascularizaţiei carotidiene asupra parenchimului cerebral – sindromul <strong>de</strong> hiperperfuzie cerebrală<br />
Dr. Jerzicska E., dr. Balos S., conf. dr. H. Suciu, prof. dr. R. Deac,<br />
IUBCVT, Târgu Mureş<br />
The syndrome of cerebral hiperperfusion (SCH) is a relatively new clinical entity, a new<br />
concept with different symptoms and signs integrated along the years in other categories of<br />
pathology. It is specific for carotid revascularisation and has a unique patho-physiology<br />
56
mechanism. The authors studied the current literature with the intention to clarify this chapter of<br />
revascularisation complications. Our experience in this domain is presented and compared in a<br />
study during 4 years from 2005-2008, based on clinical evaluation of 247 patients after the<br />
operation for internal carotid artery revascularisation. As a result of this evaluation we found SCH<br />
with patogenic mechanism, with clinical manifestations and we suggested procedures for<br />
prevention. Risk factors for SCH are presented with ad<strong>de</strong>d personal observations suggesting<br />
means for imagistic recognition. The inci<strong>de</strong>nce of this complication is smaller in our group of<br />
pactients in comparison with the data from literature suggesting the th efficiency of treatment<br />
protocol. The main objective of the study is an earlier rehabilitation after internal carotid artery<br />
revascularisation.<br />
Răsunetul revascularizaţiei carotidiene asupra parenchimului cerebral – sindromul <strong>de</strong> hiperperfuzie cerebrală<br />
Sindromul <strong>de</strong> hiperperfuzie cerebrala (SHC) este o entitate clinică relativ nouă conceptual,<br />
diferitele manifestări fiind integrate <strong>de</strong>-a lungul timpului în alte categorii <strong>de</strong> patologie. Este specific<br />
pentru revascularizarea carotidiană şi are mecanism fiziopatologic unic. Am studiat literatura<br />
curentă, cu intenţia <strong>de</strong> a clarifica acest capitol al complicaţiilor revascularizarii carotidiene.<br />
Experienţa noastră în acest domeniu este prezentată şi comparată într-un studiu cuprinzând o<br />
perioada <strong>de</strong> 4 ani, <strong>din</strong> 2005-2008, bazat pe evaluarea clinică postoperatorie a 247 pacienţi cu<br />
revascularizare carotidiană. Ca rezultat al acestei evaluări, am regăsit SHC, subliniind mecanismul<br />
patogen, cu manifestările clinice, respectiv am propus proceduri preventive şi curative. Sunt<br />
prezentaţi factorii <strong>de</strong> risc în SHC, adăugând observaţiile noastre, respectiv am <strong>de</strong>scris posibilităţile<br />
<strong>de</strong> diagnostic imagistic. In lotul nostru inci<strong>de</strong>nţa acestei complicaţii este mai mică faţă <strong>de</strong> datele<br />
<strong>din</strong> literatura <strong>de</strong> specialitate, subliniind eficienţa protocolului <strong>de</strong> tratament care ne-a permis<br />
atingerea acestei inci<strong>de</strong>nţe a SHC. Asigurarea unei recuperări cât mai rapi<strong>de</strong> postrevascularizaţie<br />
carotidiană este obiectivul primordial.<br />
125 Years from the Birth of Nicolae Hortolomei – Vascular Surgery Heritage<br />
NJ Tesoiu<br />
Institute for Emergencies in Cardiovascular Diseases “Prof. Dr. CC Iliescu”, Bucharest, <strong>Romania</strong><br />
The basis for today‘s vascular surgery rests on achievements from the past; many<br />
nationalities have been involved as well as numerous individuals. History is the essence of<br />
innumerable biographies.<br />
It is a great honor for <strong>Romania</strong>n surgeons to rend homage in <strong>2010</strong> to Nicolae Hortolomei<br />
(1885-1961), preeminent representing of the <strong>Romania</strong>n school of surgery and consi<strong>de</strong>red foun<strong>de</strong>r<br />
of the physiologic surgery in <strong>Romania</strong>, on the occasion of the anniversary of 125 years from his<br />
birth.<br />
Born in Husi, he graduates in 1909 the Faculty of Medicine in Iasi and becomes professor of<br />
surgical pathology in Iasi and then in Bucharest and full member of the <strong>Romania</strong>n Aca<strong>de</strong>my<br />
(1945). Complex personality, equally preoccupied by organizing, practice, research, education<br />
and science, he has valuable nationally and internationally recognized contributions in all surgical<br />
fields inclu<strong>din</strong>g transplantology. He is co-editor with I Turai to the first <strong>Romania</strong>n surgical treatise.<br />
He reaches the climax of the professional activity in the middle of the XX-th century in<br />
conducting a group of young enthusiasts in foun<strong>din</strong>g cardiac and vascular surgery in <strong>Romania</strong>,<br />
from experimental stage to clinical practice and from complex evaluation to surgical, anesthetic<br />
and intensive care aspects at Coltea Hospital in Bucharest. He approaches congenital and<br />
acquired heart disor<strong>de</strong>rs and vascular diseases: arterial stenoses and aneurysms, arteriovenous<br />
fistulas, arterial and portal hypertension, superior vena caval obstruction, cervical rib, carotid body<br />
tumors, as well as the surgery of sympathetic nervous system. His disciples continue and <strong>de</strong>velop<br />
these specialties at Fun<strong>de</strong>ni Hospital in Bucharest.<br />
Impressive personality marking the evolution of the <strong>Romania</strong>n surgery he remains an<br />
example of professional <strong>de</strong>votement for newer generations.<br />
125 Ani <strong>de</strong> la nasterea lui Nicolae Hortolomei – Mostenirea în domeniul chirurgiei vasculare<br />
Bazele chirurgiei vasculare actuale sunt constituite <strong>de</strong> rezultatele obtinute in trecut; multe<br />
nationalitati si numeroase personalitati sunt implicate. Istoria este suma mulor biografii.<br />
Este o mare onoare pentru chirurgii romani sa omagieze in <strong>2010</strong> pe Nicolae Hortolomei<br />
(1885-1961), reprezentant proeminent al scolii chirurgicale romanesti si consi<strong>de</strong>rat fondatorul<br />
chirurgiei fiziologice in <strong>Romania</strong>, cu ocazia aniversarii a 125 ani <strong>de</strong> la nasterea sa.<br />
57
Nascut la Husi, absolvent in 1909 al Facultatii <strong>de</strong> Medicina <strong>din</strong> Iasi, <strong>de</strong>vine profesor <strong>de</strong><br />
patologie chirurgicala la Iasi si apoi la Bucuresti si membru al Aca<strong>de</strong>miei Romane (1945).<br />
Personalitate complexa, preocupat in mod egal <strong>de</strong> organizare, practica, cercetare, educatie si<br />
stiinta, are contributii valoroase recunoscute pe plan national si international in toate domeniile<br />
chirurgiei, inclusiv transplantologie. Este co-redactor cu I Turai la primul tratat <strong>de</strong> chirurgie<br />
romanesc.<br />
Atinge maximul carierei profesionale la mijlocul secolului al XX-lea conducand un grup <strong>de</strong><br />
tineri entuziasti in fundamentarea chirurgiei cardiace si vasculare in <strong>Romania</strong>: <strong>de</strong> la nivel<br />
experimental la aplicatia clinica si <strong>de</strong> la evaluare complexa la aspectele chirurgicale, anestezice<br />
si <strong>de</strong> terapie intensiva in cadrul Spitalului Coltea <strong>din</strong> Bucuresti. Abor<strong>de</strong>aza bolile cardiace<br />
congenitale si dobandite si bolile vasculare: stenozele si anevrismele arteriale, fistulele<br />
arteriovenoase, hipertensiunea arteriala si hipertensiunea portala, obstructia <strong>de</strong> vena cava<br />
superioara, coasta cervicala, tumorile corpusculului carotidian, precum si chirurgia sistemului<br />
nervos simpatic. Discipolii sai continua si <strong>de</strong>zvolta aceste specialitati la Spitalul Fun<strong>de</strong>ni <strong>din</strong><br />
Bucuresti.<br />
Personalitate impresionanta marcand evolutia chirurgiei in <strong>Romania</strong>, ramane un exemplu<br />
<strong>de</strong> <strong>de</strong>votament profesional pentru noile generatii.<br />
Popliteal Artery Entrapment Syndrome<br />
Silvia Condu, D Trandafir*, S. Rurac*, Cristina Tudor**, Florentina Mihaescu**<br />
Department of Vascular Surgery, University Hospital Bucharest, <strong>Romania</strong><br />
*) Department of Cardio-Vascular Surgery, University Hospital Bucharest, <strong>Romania</strong><br />
**) Department of Anaesthesia and Intensive Care University Hospital Bucharest, <strong>Romania</strong><br />
Popliteal Artery Entrapment Syndrome is a rare condition which may cause severe<br />
ischemic disability among young adults. It is caused by the anomalous anatomic relationships of<br />
the musculoten<strong>din</strong>ous structures surroun<strong>din</strong>g the popliteal artery creating extrinsic compression of<br />
the artery.<br />
We report a case where duplex ultrasonography, arteriography and magnetic resonance<br />
imaging were used to diagnose and to establish the level of vascular damage and the anatomic<br />
type of the syndrome.<br />
We used a median surgical approach, resection of the occlu<strong>de</strong>d segment and operative<br />
reconstruction with autologous safen vein graft, in addition to <strong>de</strong>compression of the vessel and<br />
resection of aberrant muscle.<br />
The result was favourable with complete recovery and absence of ischemic symptoms<br />
and with patient verified by angiografic examination 6 moths post surgery.<br />
Giant External Carotid Aneurysm: Case report<br />
Anevrism gigant <strong>de</strong> arteră carotidă externă<br />
A. Oprea, A. Eni, O. An<strong>de</strong>rcou, A. Buleandra, Diana Turcu, S. Radulescu<br />
IInd Vascular Surgical Clinic, Cluj-Napoca<br />
Aneurysms of the extracranial carotid artery are extremely rare. The most frequently are<br />
the aneurysms of the common carotid artery, followed by the internal carotid, then the aneurysms<br />
of the external carotid artery.<br />
We report a case of a 72- year-old female patient with an external carotid aneurysm. The<br />
patient presented with a lateral cervical mass, dyspnoea and dysphagia. The diagnosis was<br />
ma<strong>de</strong> on investigation with carotid Doppler ultrasound and confirmed with computerized<br />
tomography. Ligation of the origin of the external carotid artery was followed by the<br />
disappearance of the compressive syndrome and the remission of the symptoms.<br />
Anevrismele arterei caroti<strong>de</strong> extracraniene sunt extrem <strong>de</strong> rare. Dintre acestea cele mai<br />
frecvente sunt cele ale caroti<strong>de</strong>i comune, urmata <strong>de</strong> cele ale caroti<strong>de</strong>i interne, pe ultimul loc<br />
fiind cele ale caroti<strong>de</strong>i externe. Prezentam cazul unei paciente <strong>de</strong> 72 ani care prezinta un<br />
anevrism <strong>de</strong> artera carotida externa. Pacienta se interneaza pentru aparitia unei formatiuni<br />
tumorale laterocervicale, insotita <strong>de</strong> disfagie si disfonie.Diagnosticul a fost pus utilizind echografia<br />
Doppler si a fost confirmat prin angioCT spiral. Ligatura arterei caroti<strong>de</strong> externe si a colateralelor<br />
transanevrismal a dus la rezolvarea sindromului compresiv cu disparitia simptomatologiei.<br />
58
Dr. Mihălcescu Daniel, Dr. Creţu Magdalena, Dr.<br />
Radu Mădălina, dr. Lazar Ovidiu, Dr. Cârjaliu<br />
Ionuţ, Dr. Tica Talida, Dr. Stanciu Crina, Dr. Popa<br />
Cherecheanu Matei, Dr. Lazăr Mihaela, Dr.<br />
Goleanu Viorel, Dr. Buica Dana<br />
Centrul <strong>de</strong> boli cardiovasculare « Agrippa Ionescu »<br />
Dr. Mihălcescu Daniel, Dr. Creţu Magdalena, Dr.<br />
Radu Mădălina, dr. Lazăr Ovidiu, Dr. Carjaliu<br />
Ionuţ, Dr. Tica Talida, Dr. Stanciu Crina, Dr. Popa<br />
Cherecheanu Matei, Dr. Lazăr Mihaela, Dr.<br />
Goleanu Viorel, Dr. Buica Dana<br />
Centrul <strong>de</strong> boli cardiovasculare « Agrippa Ionescu »<br />
Tratamentul stenozelor, fistulelor arterio-venoase<br />
pentru hemodializa<br />
Sindromul <strong>de</strong> furt sangvin post FAV - abord chirurgical<br />
Arterial Reconstructions In Infrainguinal Occlusive Disease<br />
- Our Department’s Experience Over 13 Years<br />
Reconstrucţii arteriale în boala ocluzivă infrainghinală- experienţa secţiei în 13 ani<br />
D.F. Bărzoi, M. Păcescu, I. Diaconescu, N.J. Teşoiu, R. Halpern, I. Oprea,<br />
E. Mărginean, O. Moraru, O. Udrică, A.D. Iancu, A. Stoica, S.L. Băilă<br />
Secţia Chirurgie Vasculară, Institutul <strong>de</strong> Boli Ccardiovasculare<br />
<strong>de</strong> Urgenţă “C.C. Iliescu”, Bucureşti, România<br />
Vascular Surgery Department, “C.C. Iliescu” Cardiovascular Diseases Institute, Bucharest, <strong>Romania</strong><br />
Aim. The aim of this retrospective study is to present our experience with direct<br />
reconstructive surgery in infrainguinal arterial occlusive disease over a period of 13 years.<br />
Materials and methods. During the last thirteen years, we performed arterial<br />
reconstructions for infrainguinal occlusive disease in 1996 patients. There were 1710 men and 286<br />
women; their median age was 62.5 years (range 20-95). There were 425 (21.3%) diabetics and<br />
1687 (84.5%) smokers. 1474 (73.8%) had critical ischaemia (stage III Fontaine- 697; stage IV<br />
Fontaine- 777), 447 had disabling claudication. The angiography was performed in 97.4% of cases.<br />
408 operations were redo interventions. There were 1166 conduits to the proximal popliteal artery,<br />
555 to the distal popliteal artery and 168 to the crural arteries. We used autologous material in<br />
1198 patients and prostheses in 798 patients (vein- cuffs in 82, composite grafts in 60).<br />
Results. During the first 30 days, there were 19 <strong>de</strong>aths (mortality- 1.1%) and 107 major<br />
amputations (amputation rate- 5.3%). 1870 patients were dismitted with functional grafts.<br />
Conclusions. Over this period we performed an increasing number of operations. We<br />
registered an increasing number of el<strong>de</strong>rly patients (450 patients over 70 years ) and a high level<br />
of associated cardiovascular pathology (hypertension 46.9%, cardiac ischaemia 23.6%). The<br />
hospital stay was too long (mean=19.6 days) and we used too many prostheses (39.9%). Overall,<br />
there were good results (amputation rate 5.3% and mortality 1.1%)<br />
Scopul. Scopul acestei lucrări retrospective este prezentarea experienţei noastre cu reconstrucţiile<br />
arteriale directe în boala ocluzivă infrainghinală, pe o perioadă <strong>de</strong> 13 ani.<br />
Material şi metodă. În ultimii 13 ani, colectivul nostru a efectuat reconstrucţii arteriale directe în boala<br />
ocluzivă infrainghinală la 1996 pacienţi, 1710 bărbaţi şi 286 femei, cu vârstă medie <strong>de</strong> 62,5 ani (extreme = 20-<br />
95 ani). Dintre aceşti pacienţi, 425 (21,3 %) aveau diabet zaharat, iar 1687 (84,5%) erau fumători. Indicaţia<br />
chirurgicală a fost ischemia critică la 1474 bolnavi (73,8%), <strong>din</strong>tre care 697 erau în stadiul III Fontaine, iar 777 în<br />
stadiul IV Fontaine; 447 <strong>din</strong>tre pacienţi aveau claudicaţie intermitentă. S-a efectuat arteriografie la 97,4 %<br />
<strong>din</strong>tre cazuri. 408 operaţii au fost reintervenţii. Anastomozele distale s-au efectuat la nivelul popliteei<br />
proximale (1166 cazuri), popliteei distale (555 cazuri) şi 168 la arterele crurale. S-a folosit material autolog la<br />
1198 pacienţi şi proteze la 798 (cu vein- cuff la 82, grafturi compozite la 60).<br />
Rezultate. La 30 zile, s-au înregistrat 19 <strong>de</strong>cese (mortalitate= 1,1%) şi 107 amputaţii majore (5,3%). 1870<br />
pacienţi au fost externaţi cu grefoane funcţionale.<br />
Concluzii. De-a lungul perioa<strong>de</strong>i analizate, colectivul nostru a efectuat un număr <strong>din</strong> ce în ce mai<br />
mare <strong>de</strong> operaţii, la pacienţi <strong>din</strong> ce în ce mai vârstnici (450 peste 70 ani) şi cu numeroase asocieri<br />
patologice, mai ales cardiovasculare (hipertensiune 46,9%, ischemie cardiacă 23,6%). Durata <strong>de</strong> spitalizare a<br />
fost lungă ( în medie 19,6 zile). S-au utilizat prea multe proteze (39,9%). Pe ansamblu, rezultatele obţinute au<br />
fost bune: 5,3% amputaţii majore şi 1,1% mortalitate.<br />
59
Sâmbătă 2 octombrie <strong>2010</strong><br />
Sala Diamond<br />
Grupul <strong>de</strong> lucrări « CORD »<br />
Sesiunea IX<br />
Chirurgia arterelor coronare<br />
Myocardial revascularization – ESC and EACTS gui<strong>de</strong>lines <strong>2010</strong><br />
Revascularizarea miocardică – Ghidul ESC şi EACTS <strong>2010</strong><br />
Prof. dr. Deac Radu,<br />
IUBCVT Târgu Mureş, Clinica Chirurgie Cardiovasculară I.<br />
European Society of Cardiology and European Association of Cardiothoracic Surgery<br />
revised recently the Gui<strong>de</strong>lines for Myocardial Revascularisation (MR) based on the comparison<br />
between procedures of myocardial revascularisation in coronary heart diseases. The Gui<strong>de</strong>lines<br />
are based on the <strong>de</strong>tailed analysis of the available evi<strong>de</strong>nce at the moment of writing. It is<br />
recommen<strong>de</strong>d to be taken into account at the moment of clinical judgement which does not<br />
exclu<strong>de</strong> the individual responsibility of the health professionals to take a<strong>de</strong>cquate individual<br />
<strong>de</strong>cisions in patients with their consultation. It is also the responsibility of health professionals to<br />
verify the rules and regulations amenable to drugs and <strong>de</strong>vices at their prescriptions to the<br />
patients. The 2 main pro<strong>de</strong>ures of MR are PCI and CABG. The gui<strong>de</strong>lines begin with the chapter of<br />
risk stratification of the patients followed up by the process for <strong>de</strong>cision making and patient<br />
informa-tion. The <strong>de</strong>cision making is multidisciplinary (Heart Team). Strategies for pre-intervention<br />
diagnosis and imaging inclu<strong>de</strong>: <strong>de</strong>tection of coronary artery disease, <strong>de</strong>tection of ischaemia,<br />
hybrid / combined imaging, invasive tests and their prognostic value and <strong>de</strong>tection of myocardial<br />
viability. Revascularization for stable CAD <strong>de</strong>tailed evi<strong>de</strong>nce basis for revascularisation, impact of<br />
ischaemia bur<strong>de</strong>n on prognosis, optimal medical therapy vs PCI and PCI with drug-eluting stents<br />
vs bare metal stents, also CABg vs. medical therapy, PCI vs CABG.<br />
Concerning MR in non-ST segmaent elevation in ACS inten<strong>de</strong>d early invasive or<br />
conservative strategies, risk stratification, timing of angiography & intervention, PCI and CABG. For<br />
revasculari-sation in ST-segment elevation myocardial infraction the gui<strong>de</strong>lines reviews the<br />
strategies and cardiogenic shock and mechanical complications. Procedural aspects of CABG<br />
and PCI are <strong>de</strong>tailed. Antithrombotic pharmacotherapy, secondary prevention and strategies for<br />
follow up are the last chapters of the Gui<strong>de</strong>lines<br />
Revascularizarea miocardică – Ghidul ESC şi EACTS <strong>2010</strong><br />
Societatea Europeană <strong>de</strong> Cardiologie (ESC) şi Asociaţia Europeană <strong>de</strong> Chirurgie<br />
Cardiotoracică (EACTS) au revizuit recent recomandările pentru revascularizarea miocardică<br />
bazat pe comparaţia între procedurile <strong>de</strong> revascularizare miocardică (RM) în cardiopatia<br />
coronariană. Acestea au la bază analiza minuţioasă a dovezilor existente la momentul redactării.<br />
Se recomandă luarea lor în consi<strong>de</strong>rare în momentul ju<strong>de</strong>căţii clinice, ceea ce nu exclu<strong>de</strong><br />
responsabilitatea individuală a profesioniştilor <strong>din</strong> sănătate <strong>de</strong> a lua <strong>de</strong>cizii a<strong>de</strong>cvate individual la<br />
pacienţi cu consultarea acestora. De asemenea, este responsabilitatea profesioniştilor <strong>din</strong><br />
sănătate să verifice regulile şi reglementările aplicabile medicamentelor şi dispozitivelor medicale<br />
în momentul indicării/prescrierii acestora. Cele 2 proce<strong>de</strong>e majore <strong>de</strong> RM sunt bypass-ul aortocoronarian<br />
chirurgical (BAC) şi intervenţia coronară percutanată (PCI). Recomandările au la<br />
început un capitol <strong>de</strong>spre stratificarea <strong>de</strong> risc a pacienţilor, urmat <strong>de</strong> procesul <strong>de</strong> luare a <strong>de</strong>ciziei<br />
şi informarea pacientului. In cadrul strategiilor înainte <strong>de</strong> intervenţie sunt <strong>de</strong>scrise: <strong>de</strong>tectarea bolii<br />
coronare, <strong>de</strong>tectarea ischemiei, imagistica combinată hibridă, testele invazive cu valoarea<br />
prognostică şi <strong>de</strong>tectarea viabilităţii miocardice. In capitolul <strong>de</strong>spre RM pentru angina stabilă sunt<br />
trecute în revistă dovezile existente pentru revascularizare, terapia medicală optimă, RM cu PCI şi<br />
aplicare <strong>de</strong> stenturi DES sau BMS, apoi RM prin BAC cu comparaţie între proceduri. Un alt capitol<br />
este <strong>de</strong>dicat RM în ACS fără supra<strong>de</strong>nivelare ST cu referire la stratificarea <strong>de</strong> risc, intenţia <strong>de</strong><br />
rezolvare invazivă sau conservativă, momentul angiografiei coronare şi al intervenţiei <strong>de</strong> PCI sau<br />
BAC. RM în AMI cu elevare ST tratează strategiile <strong>de</strong> reperfuzie, şocul cardiogen şi complicaţiile<br />
mecanice. Sunt <strong>de</strong>scrise procedurile <strong>de</strong> PCI şi BAC. Farmaco-terapia antitrombotică, prevenţia<br />
secundară şi procedurile <strong>de</strong> follow up încheie recomandările.<br />
60
Gerard Bloch<br />
Spitalul American <strong>din</strong> Paris<br />
Horaţiu Moldovan<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof. Dr. C.C. Iliescu”<br />
Bucureşti<br />
Grigore Tinică<br />
Clinica <strong>de</strong> Chirurgie Cardiovasculară, Institutul <strong>de</strong> Boli<br />
Cardiovasculare, Iaşi<br />
Actual indications for CABG (coronary artery bypass<br />
grafting<br />
Ruptura <strong>de</strong> sept interventricular post infarct miocardic<br />
acut<br />
Revascularizarea chirurgicală coronariană total<br />
arterială. Argumente şi fapte.<br />
Totally arterial coronary revascularization. Argument<br />
and facts.<br />
Making of The Cardiovascular Hybrid Operating Room<br />
Organizarea sălii <strong>de</strong> operaţie hibri<strong>de</strong> cardiovasculare<br />
Prof dr. Grigore Tinica, Diana Ciurescu, Igor Ne<strong>de</strong>lciuc, Mihail Enache, Vasile Astarastoae<br />
Universiy of Medicine and Pharmacy „Gr. T. Popa” Iaşi<br />
Cardiovascular Surgery Clinic,<br />
Cardiovascular Institute „Prof. Dr. George G. M. Georgescu” IASI<br />
Background. The recent improvements in the treatment of cardiovascular diseases has<br />
established the hybrid strategies as an alternative treatment for a variety of cardiovascular<br />
conditions. These <strong>de</strong>velopments have led to the installation of hybrid operating suites that are<br />
optimal for both open surgery and endovascular procedures. These units require special training,<br />
planning and <strong>de</strong>sign. Important issues inclu<strong>de</strong>: quality of the imaging equipment, radiation<br />
bur<strong>de</strong>n, ease of use of the equipment, need for specially trained personnel, ergonomics, ability to<br />
perform both open and percutaneous procedures, sterile environments, as well as quality and<br />
efficiency of patient care.<br />
Methods. Before planning a room with an interdisciplinary usage by cardiovascular<br />
surgeons, interventionalists, anaesthesiologists, a clear vision for the utilization should be<br />
established. A literature search i<strong>de</strong>ntified articles pertinent to the key issues during the <strong>de</strong>cisionmaking<br />
process of creating the optimal endovascular suite. Workflow was analyzed and an<br />
observational study of the operating room was performed.<br />
Results and conclusion. The most important feature of working in a hybrid operating room<br />
should be the ability to attain best treatment of cardiovascular patients. Establishment of an<br />
endovascular operating room suite has the benefit of a sterile environment, the possibility of<br />
performing hybrid procedures and conversions when necessary. With the growing trend toward<br />
endovascular procedures during surgery, the hybrid operating room will become an integral part<br />
of every cardiovascular center. This new concept will play an important role for minimally invasive<br />
surgery. As a consequence, better quality and service can be provi<strong>de</strong>d to the individual patient.<br />
The trend towards hybrid techniques is more a revolution than a evolution.<br />
Keywords: hybrid room, integrated or, angiography-or, high-tech or, minimally invasive,<br />
cardiovascular surgery.<br />
Ţintoiu Ion<br />
Spitalul Militar Bucureşti<br />
Adrian Molnar<br />
Institutul Inimii “ N. Stăncioiu” Cluj-Napoca<br />
I. Droc, Tintoiu I.<br />
Centrul clinic <strong>de</strong> urgenţă <strong>de</strong> boli cardiovasculare<br />
“Dr. Constantin Zamfir”, Spitalul Militar Bucureşti<br />
Clara Alexandrescu<br />
Centre Cardio-Thoracique du Monaco, Monte<br />
Carlo<br />
Rezistenţa la tratamentul antiplachetar şi restenoza în<br />
stent sau graft<br />
Chirurgia off pump versus on pump în revascularizarea<br />
miocardică<br />
Sesiunea X<br />
CABG after instent restenosys<br />
Care este cea mai bună modalitate imagistică înainte <strong>de</strong><br />
chirurgia aortei?<br />
What is the best imagistic modality before surgery for aortic<br />
valve and aortic root?<br />
61
Case Study: Cardiac Rupture After Myocardial Infarction<br />
Ruptura cardiacă postinfarct miocardic acut - prezentare <strong>de</strong> caz<br />
L. Stoica, E. Bitere, E. Ciobanu, G. Tinica<br />
Cardiovascular Surgery Department,<br />
Cardiovascular Institute “Prof. Dr. George I. M. Georgescu”, Iasi<br />
Despite the progresses acheved in early miocardic revascularisation, cardiac rupture<br />
remains an important factor of hight mortality post acute miocardial infarction, frequentely by<br />
electromechanical dissociation with sud<strong>de</strong>n <strong>de</strong>ath, on patients without history of angina.<br />
The presentation discusses the case of a 73 years old patient, smoker, chronic ethanol<br />
consumer, without any angina symptoms, known with obliterating arteriopathy of lower limbs, with<br />
chronic ischemia of his left lower limb stage III, admitted for surgical treatment of this pathology.<br />
During his admittance he suffers an acute miocardic infarction, followed by cardiac rupture, with<br />
cardiac tampona<strong>de</strong>. The patient is tachicardic, SR 120 b/min, BP 110/70 un<strong>de</strong>r inotrop support, QS<br />
in C1, rS in C2 on EKG; on echocardiography - apex with diskinezia, wraped in trombus, lateral wall<br />
akinezia, with apparently solution of discontinuity on the LV apex, without Doppler flux (wraped in<br />
thrombus), organized thrombus in the pericardial sac, pericardial fluid of max. 4 cm below RV with<br />
diastolic collapse of RV; EF 64%, EFvol. 30% (visualy); on coronarography - right dominance, first<br />
marginale of circumflex artery ocllusion.<br />
A promt surgycal intervention by closing the rupture with autologus patch of pericardium<br />
and dacron patch, stabilised with bioglue is performed. On postoperative echocardiography we<br />
note the absence of pericardial fluid, LV with mo<strong>de</strong>rately diminishet, hipokinezia of lateral wall<br />
and the apex, EF 60%, EFvol 40 – 45%. On EKG SR75b/min with small progression of R wave in C1 –<br />
C2. Patients <strong>de</strong>velopement is favorable, without angina or dyspnoea.<br />
Within a month after cardiac surgery the patient comes back in or<strong>de</strong>r to un<strong>de</strong>rgo surgical<br />
treatment for chronic ischemia of his left lower limb. On echocardiography at 4 months after<br />
surgery he has EF 60%, preserved LV global systolic function, LV inferior wall hipokinesia, absence<br />
of pericardic fluid.<br />
Conclusions: Immediate surgical treatment allowed a positive vital outcome in a patient<br />
with subacute cardiac rupture post AMI<br />
R. Vasile, B. Rădulescu, A. Mărginean, S.<br />
Marin, O. Ghenu, H. Moldovan, V. Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “Prof Dr.<br />
C.C.Iliescu” Bucureşti<br />
Infarct miocardic acut postoperator, prin spasm <strong>de</strong> artera<br />
coronara dreaptă in<strong>de</strong>mnă<br />
Acquired ventricular septal <strong>de</strong>fect:<br />
mechanical complication of acute myocardial infarction<br />
Dr. Raicea V., Dr. Moraru L., Dr. Serban V., Dr Bica L.,<br />
Dr Raicea C., prof. dr. Deac R. – IUBCVT Târgu-Mureş<br />
Ventricular septal <strong>de</strong>fect (VSD) represents a rare and severe complication of acute<br />
myocardial infarction (AMI) – having absolute surgical indication. Four clinical cases operated<br />
upon in the Clinic of Cardiovascular Surgery of the IUBCVT Târgu-Mureş in between 2009-<strong>2010</strong> are<br />
presented. There were 3 females and 1 male with the age in between 50-72 years. VSD appeared<br />
at 1 day post AMI (2 cases) respectively at 1 week post IMA (2 cases), the operation being<br />
performed at around 1 month from the date of infarction. VSD was situated in the antero-septal<br />
region (3 cases) – oclusion of left anterior <strong>de</strong>scen<strong>din</strong>g artery, respectively 1 case in the posteroinferior<br />
region – oclusion of right coronary artery. All the cases presented mo<strong>de</strong>rat-severe<br />
secondary pulmonary hypertension (PA>60 mmHg), LVEF was between 35-40%. Preoperatively,<br />
none of the patients received IABP support (one case nee<strong>de</strong>d mo<strong>de</strong>rate inotropic support). The<br />
operations were performed by closure of the VSD with armed isolated sutures (3 cases),<br />
respectively one case required reconstruction of the left ventricle and closure of the VSD with the<br />
same patch. Surgical myocardial revascularisation was performed concomitently. The<br />
postoperative evolution was good in 3 cases. One patient died 30 days postoperatively.<br />
62
Complicaţia mecanică a infarctului miocardic acut: <strong>de</strong>fectul septal ventricular dobândit.<br />
Defectul septal ventricular (DSV) reprezintă o complicaţie rară, severă a infarctului<br />
miocardic acut (IMA) având indicaţie chirurgicală absolută. In lucrare sunt prezentaţi 4 pacienţi<br />
(3 femei şi 1 bărbat) cu vârsta cuprinsă între 50-72 ani, operaţi în Clinica <strong>de</strong> Chirurgie<br />
Cardiovasculară a IUBCVT Tîrgu Mureş în intervalul 2009 - <strong>2010</strong>. DSV s-a <strong>de</strong>zvoltat la 1 zi post IMA (2<br />
cazuri), respectiv la 1 săptămână post IMA (2 cazuri), operaţia efectuându-se la aproximativ 1<br />
lună <strong>de</strong> la data infarctului miocardic. DSV a fost situat antero-septal (3 cazuri) – ocluzie artera<br />
<strong>de</strong>scen<strong>de</strong>ntă anterioară, respectiv 1 caz cu localizare postero-inferioară – ocluzie artera coronară<br />
dreaptă. Toate cazurile au prezentat hipertensiune pulmonară secundară (PAP peste 60 mmHg).<br />
FEVS <strong>de</strong>terminată echocardiografic a fost situată între 35-40%. Nici unui pacient nu a fost asistat<br />
IABP. Un pacient a necesitat suport inotropic mo<strong>de</strong>rat. Operaţiile au constat în închi<strong>de</strong>rea DSV cu<br />
fire izolate armate (3 cazuri), respectiv un caz a necesitat reconstraucţie <strong>de</strong> VS şi exclu<strong>de</strong>re DSV<br />
cu acelaşi petec, concomitent efectuându-se revascularizarea chirurgicală a miocardului.<br />
Evoluţia postoperatorie a fost favorabilă la 3 cazuri. A fost înregistrat un <strong>de</strong>ces la 30 zile<br />
postoperator prin insufcien ă multiplă <strong>de</strong> organe.<br />
Miocardial revascularization combined with surgical treatment of other cardiac<br />
pathologies. Comparison with eacts adult cardiac surgical database report<br />
Revascularizarea miocardică concomitentă tratamentului chirurgical al altor patologii cardiace.<br />
Comparaţie cu EACTS adult cardiac Surgical Database report<br />
Grigore Tinică, Mihail Enache, Diana Ciurescu,<br />
Oana Bartos, Alexandru Ciucu, Flavia Antoniu, Victor Prisacari<br />
Cardiovascular Surgery Department,<br />
Cardiovascular Institute “Prof. Dr. George I. M. Georgescu”, Iasi<br />
Aim: The current work is oriented towards the statistical processing and interpretation of<br />
the coronary artery by-pass grafting procedures integrated with concurrent surgical procedures<br />
for other intracardiac pathologies.<br />
Materials and method: This retrospective study inclu<strong>de</strong>s all the patients un<strong>de</strong>rgoing a<br />
CABG procedure at IBCV “Prof. Dr. George I. M. Georgescu” Iasi during 2000-august <strong>2010</strong>. Out of<br />
a total of 963 patients, 759 un<strong>de</strong>rwent only CABG, 195 un<strong>de</strong>rwent CABG+other intracardiac<br />
procedures and 9 un<strong>de</strong>rwent CABG+other extracardiac procedures. The intracardiac surgical<br />
procedures concurrent with CABG revealed in our study group were as followed: CABG+Ao valve<br />
(100 patients), CABG+Mi valve (30 patients), CABG+Ao valve+Mi valve (8 patients), CABG+Ao<br />
valve+other (14 patients), CABG+Mi valve+other (7 patients), CABG+Ao valve+Mi valve+other (5<br />
patient), CABG+aneurism of the left ventricle (18 patients), CABG+ascendant Ao (7 patients),<br />
CABG+other (7 patients). We compared the group of patients un<strong>de</strong>rgoing CABG+aortic valve<br />
replacement and CABG+mitral valve procedures with the similar groups from the 4-th EACTS adult<br />
cardiac surgical database report.<br />
Results: The overall postoperative mortality was 1% in the group of patients with<br />
CABG+aortic valve replacement versus 5,5% in EACTS database and 3,33% vs. 8,6% in the group of<br />
patients with CABG+mitral valve procedures. In both groups of patients, the female mortality was<br />
0% (EACTS values for CABG+Ao valve was 7,50% and for CABG+Mi valve was 10,40%).<br />
Conclusions: Our study indicates an upgra<strong>de</strong> in the inci<strong>de</strong>nce of the CABG procedures<br />
concurrent with additional intracardiac surgical procedures, from 16,49% in the first half of the<br />
studied period up to 21,57% in the second half. This reflects the fact that the ischemic heart<br />
disease morbidity markers are increasing and the patient needs to un<strong>de</strong>rgo more complex<br />
cardio-vascular surgical procedures, <strong>de</strong>spite the remarkable scientific progress registered in the<br />
medical and interventional cardiology field. The results registered in out clinic are superior to those<br />
quoted in the reference literature, <strong>de</strong>spite the increased complexity of the surgical procedures<br />
performed.<br />
Revascularizarea miocardică concomitentă tratamentului chirurgical al altor patologii cardiace.<br />
Comparatie cu EACTS Adult Cardiac Surgical Database Report<br />
Obiective: Aceasta lucrare urmareste prelucrarea si interpretarea statistica a interventiilor<br />
chirurgicale <strong>de</strong> revascularizare miocardica si a proce<strong>de</strong>elor chirurgicale concomitente pentru<br />
alte patologii cardiace.<br />
63
Materiale si metoda: Acest studiu retrospectiv cuprin<strong>de</strong> toti pacientii supusi unei interventii<br />
<strong>de</strong> revascularizare miocardica chirurgicala la IBCV “Prof. Dr. George. I. M. Georgescu” Iasi intre<br />
anii 2000- august <strong>2010</strong>. Dintr-un total <strong>de</strong> 963 <strong>de</strong> pacienti, 759 au fost supusi doar la CABG, 195<br />
CABG+alte proceduri intracardiace si 9 CABG+proceduri extracardiace. Procedurile chirurgicale<br />
intracardiace concomitente cu CABG au fost: CABG+valva Ao (100 pacienti), CABG+valva Mi<br />
(30 pacienti ), CABG+valva Ao+valva Mi (8 pacienti), CABG+valva Ao+alte (14 pacienti),<br />
CABG+valva Mi+alte (7 pacienti), CABG+valva Ao+valva Mi+alte (5 pacienti), CABG+anevrism VS<br />
(18 pacienti), CABG+aorta ascen<strong>de</strong>nta (7 pacienti), CABG+alte (7 pacienti). Au fost comparate<br />
loturile <strong>de</strong> pacienti operati cu by-pass aorto- coronarian asociat cu protezare aortica si proceduri<br />
mitrale cu loturile similare <strong>din</strong> 4-th EACTS adult cardiac surgical database report<br />
Rezultate: Mortalitatea postoperatorie globala a fost <strong>de</strong> 1% la pacientii cu protezare<br />
aortica asociata cu by-pass aorto-coronarian fata <strong>de</strong> 5,5% in baza <strong>de</strong> date EACTS si <strong>de</strong> 3,33% fata<br />
<strong>de</strong> 8,6% la pacientii cu patologie valvulara mitrala asociata. In ambele grupuri <strong>de</strong> pacienti,<br />
mortalitatea feminina a fost 0% (EACTS CABG+valva Ao=7.50% iar EACTS CABG+valva Mi=<br />
10.40%).<br />
Concluzii: Studiul efectuat evi<strong>de</strong>ntiaza o usoara crestere a inci<strong>de</strong>ntei interventiilor<br />
chirurgicale <strong>de</strong> revascularizare miocardica ce necesita cura chirurgicala concomitenta a unor<br />
patologii intracardiace aditionale, <strong>de</strong> la 16.49% in prima jumatate a <strong>de</strong>ceniului studiat la 21.57% in<br />
a doua jumatate. Aceasta reflecta faptul ca indicii morbiditatii cardiopatiei ischemice sunt in<br />
crestere, pacientul avand indicatie pentru interventii chirurgicale cardio-vasculare <strong>din</strong> ce in ce<br />
mai complexe, in ciuda progreselor stiintifice inregistrate in ultimul <strong>de</strong>ceniu in domeniul<br />
cardiologiei medicale si interventionale. Rezultatele obtinute in clinica noastra sunt superioare<br />
celor citate <strong>de</strong> literatura <strong>de</strong> specialitate, in ciuda complexitatii sporite a interventiilor chirurgicale<br />
efectuate.<br />
Hybrid Revascularization – A Step Forward In Cardiovascular Procedures<br />
Revascularizarea hibridă – un pas înainte în medicina cardiovasculară<br />
Diana Ciurescu, Igor Ne<strong>de</strong>lciuc, Mihail Enache, Dumitrita Gafencu, Grigore Tinica<br />
Cardiovascular Surgery Clinic, Cardiovascular Institute IASI<br />
Objective. A hybrid therapy combines the treatments traditionally available only in the<br />
catheterization laboratory with those traditionally available in the operating room to offer patients<br />
the best available therapies for any cardiovascular lesion.<br />
We sought to evaluate clinical and angiographic outcomes of hybrid procedures in patients<br />
receiving both PCI and other cardiovascular intervention.<br />
Methods. We retrospectively analyzed 113 patients with CAD who were referred to our<br />
institution for myocardial ischemia and un<strong>de</strong>rwent hybrid procedures. Between January 2002 and<br />
January 2009, a totally of 113 patients un<strong>de</strong>rwent hybrid procedures. In this series, the hybrid<br />
sequence, in all cases, inclu<strong>de</strong>d a PCI performed in the cardiac catheterization laboratory,<br />
followed by CABG in 23 patients, by valvular replacement in 6 patients (aortic and mitral), by<br />
carotid endarterectomy and surgical angioplasty in 12 patients and by peripheral vascular<br />
reconstructions in 82 patients.<br />
PCI was performed using femoral or radial artery access using gui<strong>de</strong>d catheter techniques and<br />
the surgical CABG, valvular replacement and the peripheral vascular interventions were<br />
performed accor<strong>din</strong>g to our current standard gui<strong>de</strong>lines.<br />
Results. Clinical follow-up was carried out in 100% of eligible patients. Information about inhospital<br />
outcomes was obtained from an electronic centralized clinical database. After<br />
discharge, all clinical follow-up data were prospectively collected by scheduled clinical<br />
evaluations or direct telephone interviews. Angiographic follow-up was performed at 6-9 months<br />
after the procedure. It was performed at an earlier time if clinically indicated.<br />
Discussions. The key requirement in all of these approaches is the need for collaboration<br />
between cardiac surgeons, vascular surgeons and interventional cardiologists to obtain optimal<br />
patient outcomes.<br />
Conclusions. Hybrid revascularization is offered as an alternative strategy for patients with<br />
complex cardiovascular diseases. Hybrid CABG/PCI may be reserved for higher risk patients who<br />
are not candidates for conventional surgery. In these patients, assosiation of PTA and surgery may<br />
help reduce risk.<br />
64
Revascularizarea hibridă – un pas înainte în procedurile cardiovasculare<br />
Obiective. Terapia hibridă combină procedurile disponibile, în mod tradiţional, numai în<br />
laboratorul <strong>de</strong> cateterism, cu cele disponibile numai în sala <strong>de</strong> operaţie pentru a oferi pacienţilor<br />
cele mai bune tratamente pentru orice tip <strong>de</strong> leziune cardiovasculară.<br />
În prezenta lucrare, am evaluat rezultatele clinice şi angiografice ale procedurilor hibri<strong>de</strong> la<br />
pacienţii cu proceduri coronariene intervenţionale (PCI) şi alte intervenţii chirurgicale<br />
cardiovasculare asociate.<br />
Meto<strong>de</strong>. Am analizat retrospective cazurile a 113 pacienţi coronarieni internaţi în clinica<br />
noastră pentru ischemie miocardică şi cărora li s-au practicat proceduri hibri<strong>de</strong> cardiovasculare.<br />
Între ianuarie 2002 şi ianuarie 2009, s-au efectuat proceduri hibri<strong>de</strong> cardiovasculare la un număr<br />
<strong>de</strong> 113 pacienţi. La această serie <strong>de</strong> pacienţi, secvenţa hibridă, în toate cazurile, a inclus<br />
proceduri intervenţionale coronariene efectuate în laboratorul <strong>de</strong> cateterism cardiac, urmate <strong>de</strong><br />
BAC la 23 <strong>de</strong> pacienţi, înlocuiri valvulare la 6 pacienţi (aortice şi mitrale), endarterectomii<br />
carotidiene şi plastii <strong>de</strong> lărgire la 12 pacienţi şi intervenţii chirurgicale vasculare periferice la 82 <strong>de</strong><br />
pacienţi. Procedurile intervenţionale coronariene s-au efectuat prin abord femural sau radial,<br />
utilizând cateterismul cardiac, în timp ce BAC, înlocuirile valvulare şi intervenţiile <strong>de</strong> chirurgie<br />
vasculară au respectat gui<strong>de</strong>line-urile standard actuale.<br />
Rezultate. Urmărirea clinică a fost realizată la 100% <strong>din</strong> pacienţii eligibili. Informaţiile <strong>de</strong>spre<br />
rezultatele intraspitaliceşti au fost obţinute <strong>din</strong>tr-o bază <strong>de</strong> date electronică centralizată. După<br />
externare, toate datele clinice <strong>de</strong> urmărire au fost colectate prospectiv prin evaluări regulate<br />
clinice sau interviuri directe prin telefon. Urmărirea angiografică a fost efectuată la 6-9 luni după<br />
procedură.<br />
Discuţii. Cerinţa esenţială în toate aceste abordări o reprezintă necesitatea colaborării<br />
între chirurgii cardiaci, vasculari şi cardiologii intervenţionişti pentru a obţine rezultate optime.<br />
Concluzii. Revascularizarea hibridă reprezintă o alternativă în managementul pacienţilor<br />
cu boli complexe cardiovasculare. Ea este rezervată cazurilor cu risc crescut, pacienţilor care nu<br />
sunt candidaţi acceptaţi pentru revascularizarea chirurgicală convenţională. La aceştia,<br />
alternative <strong>de</strong> asociere a procedurilor chirurgicale şi <strong>de</strong> stentare a celorlalte artere afectate<br />
poate reduce riscul procedural.<br />
Surgical harvesting of Radial Artery –<br />
comparison between skeletonized ans pedicled grafts<br />
Recoltarea chirurgicală a arterei radiale – comparaţie între tehnica scheletizată şi cea pediculată<br />
Dr. Moraru L., dr. Raicea V., dr. Serban V., dr. Bica Lucia, Dr. Raicea C., prof. dr. Deac R.<br />
IUBCVT Târgu Mures<br />
Radial artery (RA) represents an arterial conduit which may be successfully used in<br />
coronary surgery. The surgical technique of harvesting RA and utilization in coronary surgery is<br />
presented. The techniques <strong>de</strong>scribed were applied in 45 patients operated upon in the Clinic of<br />
Cardiovascular Surgery at Institute for Cardiovascuar Diseases and Transplantation in Târgu Mures,<br />
<strong>Romania</strong>, between 2008-<strong>2010</strong>. In 31 patients this conduit was harvested “pedicled” (the RA and<br />
adjacent veins) and in 14 patients “skeletonized” (RA was dissected apart from the adjacent<br />
veins). In both methods the “no touch” technique with vessel snares for gentle manipulation /<br />
dissection, was used, also metallic clips for haemostasis at the collateral branches. The conduits<br />
were flushed with saline without undue pressure. The harvest time was comparable for both<br />
methods (mean 34 minutes vs 42 minutes). The length of the conduit was also comparable (mean<br />
13,9 cm vs 14,4 cm). No local complication was noted in utilization of the both techniques. The<br />
diameter of the graft and its uniformity was greater with the “pedicled” method (mean 2,4 mm vs<br />
1,3 mm) – which corelated positively with the post-bypass flow measurements. In conclusion the<br />
“pedicled” surgical harvesting of the radial artery offers a arterial graft with superior and uniform<br />
diameter associated with a a<strong>de</strong>quate length for the patients with total arterial myocardial<br />
revascularisation. Morphologic observations will be ad<strong>de</strong>d to functional data (arterial spasm, flow<br />
in the RA, patency rate).<br />
Recoltarea chirurgicală a arterei radiale – comparaţie între tehnica scheletizată şi cea pediculată<br />
Artera radială (AR) reprezintă un grefon arterial ce poate fi folosit cu succes în chirurgia<br />
coronariană. In IUBCVT Târgu Mure între anii 2008-<strong>2010</strong> au fost operaţi 45 <strong>de</strong> pacienţi la care AR<br />
stângă a fost utilizată pentru revascularizarea chirurgicală a miocardului în asociaţie cu alte tipuri<br />
65
<strong>de</strong> grefoane. In 31 cazuri acest conduct a fost recoltat”pediculat”, (păstrarea periarterială a<br />
venelor adiacente), iar în celelalte 14 cazuri AR a fost preparată”scheletizat” (eliberarea AR <strong>din</strong>tre<br />
venele aferente). In ambele variante s-a utilizat metoda atraumatică”no touch” cu şnururi <strong>de</strong><br />
hemostază pentru manipulare / disecţie şi utilizare <strong>de</strong> clipuri metalice pentru hemostaza<br />
colateralelor. Timpul <strong>de</strong> recoltare a fost comparabil (medie 34 minute vs 42 minute), lungimea<br />
grefonului a fost <strong>de</strong> asemenea comparabilă (medie 13,9 cm vs 14,4 cm), fără a exista complicaţii<br />
locale post recoltare, în nici una <strong>din</strong>tre cele două variante utilizate. Diametrul grefonului arterial a<br />
fost mai mare, respectiv mai uniform în cazul meto<strong>de</strong>i”pediculat” (medie 2,4 mm vs 1,3 mm) –<br />
fapt corelat pozitiv cu valorile <strong>de</strong> <strong>de</strong>bit măsurate post-bypass. In concluzie recoltarea<br />
chirurgicală”pediculată” a AR oferă un conduct arterial cu un diametru superior mai uniform<br />
asociat cu o lungime corespunzătoare pentru pacienţii cu revascularizare miocardică totală<br />
arterială. Observaţiile morfologice vor fi completate cu datele funcţionale (spasme arteriale,<br />
<strong>de</strong>bite prin AR, permeabilitate).<br />
Use of radial artery in myocardial arterial revascularization<br />
Utilizarea arterei radiale în revascularizarea arterială miocardică<br />
Prof. dr. Deac R., dr. Raicea V., dr. Moraru L., dr. Suciu H.,<br />
IUBCVT, Târgu Mureş<br />
The search for an i<strong>de</strong>al graft for myocardial revascularisation still continues. The<br />
advantages of arterial grafts are obvious, but the number of such graft is limited to both mamary<br />
arteries of the patients. The alterna-tives arterial grafts are one radial artery (RA) and gastroepiploic<br />
artery. We exten<strong>de</strong>d our experience in total arterial revascularisation with the use of<br />
autologous left radial artery in 45 patients operated upon between 2008-<strong>2010</strong>. There were 1<br />
female and 44 males, with the age between 43-71 years, in whom left RA was used for arterial<br />
myocardial revascularisation. The coronary artery grafted with RA involved: left marginal (16), left<br />
circomflex (10), RCA (7), LAD (5), D1 (2), Intermediate ves. (1), RCA and intermediate vessel – 2<br />
segments (1), RCA / ADP (1), LAD + Cx (1), LAD + RCA (1). The majority of RA were associated to<br />
other arterial grafts (LIMA, RIMA) isolated or with both mamary arteries. There were no <strong>de</strong>ath in this<br />
series. In 2 occasions RA graft were associated with autologus veins, and in 3 cases RA graft were<br />
implanted proximally in other grafts (LIMA, vein). As a routine RA were implanted proximally in<br />
ascen<strong>din</strong>g aorta. In the interval studied no RA grafts occlu<strong>de</strong>d or stenosed. In one case at 8<br />
months after the operation, the RA received a endocoronary stent for kinking. Rarely (2 cases), a<br />
RA spasm was noted intraoperatively and was managed by drugs. To note that RA was used only<br />
in one women. The interval in which the RA grafts were studied is not long enough to evaluate the<br />
patency rate yet. The quality of the RA arterial grafts <strong>de</strong>serve further surgical evaluation.<br />
Utilizarea arterei radiale în revascularizarea arterială miocardică<br />
Cercetarea pentru un conduct i<strong>de</strong>al pentru revascularizare miocardică continuă.<br />
Avantajele conductelor arteriale sunt evi<strong>de</strong>nte, dar numărul lor este încă limitat la cele 2 artere<br />
mamare interne. Alternativele sunt o arteră radială şi artera gastro-epiploică. Am extins<br />
experienţa noastră în revascu-larizarea totală arterială a miocardului cu utilizarea arterei radiale<br />
stângi (AR) autologe la 45 <strong>de</strong> pacienţi operaţi între 2008-<strong>2010</strong>. Genul pacienţilor a fost cel feminin<br />
la o pacientă şi masculin la 44 <strong>de</strong> pacienţi cu vârsta între 43-71 <strong>de</strong> ani. Arterele coronare<br />
revascularizate cu AR au fost: artera marginală stâgă (16), circumflexă stângă (10), ACD (7), ADA<br />
(5), D1(2), Vas intermediar (1), ACD şi vas intermediar – 2 segmente <strong>de</strong> AR (1), ACD/ADP (1),<br />
ADA+Cx (1), ADA+ACD (1). Utilizarea AR a fost asociată altor tipuri <strong>de</strong> conducte (AMIS,AMID)<br />
izolate sau cu ambele artere mamare interne. Nu au fost înregistrate <strong>de</strong>cese. In 2 cazuri AR a fost<br />
asociată cu utilizarea <strong>de</strong> venă autologă, iar în 3 cazuri AR au fost implantate proximal în alte<br />
artere (AMIS; venă). De rutină, AR a fost implantată proximal în aorta ascen<strong>de</strong>ntă la majoritatea<br />
cazurilor. In intervalul studiat nu s-au înregistrat ocluzii sau stenoze <strong>de</strong> AR, exceptând un caz în<br />
care la 8 luni postoperator a necesitat implantare <strong>de</strong> stent endocoronar pentru o cudură<br />
<strong>de</strong>terminată <strong>de</strong> poziţionare. De notat că AR a fost utilizată la o singură pacientă. Intervalul la care<br />
conductele <strong>de</strong> AR au fost analizate nu este suficient <strong>de</strong> lung pentru a evalua încă durabilitatea<br />
permeabilităţii acestora. Calităţile oferite <strong>de</strong> grefele <strong>de</strong> AR justifică evaluarea chirurgicală în<br />
continuare.<br />
R. Vasile, B. Rădulescu, A. Vasilescu,<br />
Luminiţa Iliuţă, H. Moldovan, V. Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr.<br />
C.C.Iliescu” Bucureşti<br />
Revascularizare miocardică folosind arterele mamare<br />
scheletizate<br />
66
Sesiunea XI<br />
The Importance Of Surgery In Controlling The Electrical Storm In A Patient With An Implantable<br />
Cardioverter And Left Ventricular Anevrysm<br />
Aportul chirurgical în controlul furtunii electrice la pacient cu <strong>de</strong>fibrilator implantabil şi anevrism gicant <strong>de</strong><br />
ventricul stang.<br />
Grigore Tinica, Alexandru Ciucu, Mihail Enache, Diana Ciurescu, Flavia Antoniu,<br />
Mihalea Grecu, Oana Bartos, Victor Prisacari, Daniel Dascalescu<br />
Cardiovascular surgery clinic IAŞI, Cardiovascular Institute IASI<br />
Introduction: An implantable cardioverter (ICD) is a first-line therapy for many patients who<br />
are at risk of sud<strong>de</strong>n <strong>de</strong>ath from ventricular arrhythmias. An electrical storm is <strong>de</strong>fined as multiple<br />
occurrences (two) of ventricular tachycardia/fibrillation within a 24-hours period. Inci<strong>de</strong>nce 10-<br />
20% of implanted ICD patients This is a medical emergency and a poor prognostic marker in<br />
patients with an ICD.<br />
Material and methods: We report here on a successful treatment of electrical storm that<br />
was refractory to amiodarone and β-blockers in a 60-years-old ICD recipient who un<strong>de</strong>rwent<br />
surgery for ischemic cardiomyopathy and huge LV aneurysm. The preoperative ejection fraction<br />
was very low, 16% and TAPSE was 11mm LV aneurysm resection, Cooley left ventricular<br />
remo<strong>de</strong>lling and surgical revascularization of the myocardium with the left IMA on LAD<br />
anastomosed in Y fashion with the left radial artery sequentially on the obtuse marginal artery and<br />
on the posterolateral artery of ACX was performed un<strong>de</strong>r extracorporeal circulation.<br />
Results: At 15 months the graft patency was verified by arteriography, left ventricular<br />
function by ultrasound and ventriculography, and also was recor<strong>de</strong>d the ICD history. And the ICD<br />
did not recor<strong>de</strong>d any therapeutic episo<strong>de</strong>s, the postoperative ejection fraction increasing to 45-<br />
50%.<br />
Conclusions: Electrical storms are frequent in patients with IHD and ICD. Management<br />
requires use of both simple and sophisticated methods. Surgical management could be an<br />
effective treatment for patients with huge aneurysm and refractory electrical storms to<br />
antiarrhytmic drugs.<br />
Aportul chirurgical în controlul furtunii electrice la pacient cu <strong>de</strong>fibrilator implantabil şi<br />
anevrism gicant <strong>de</strong> ventricul stang.<br />
Introducere: Defibrilatorul implantabil (ICD) este o terapie <strong>de</strong> primă linie pentru pacienţii<br />
expuşi riscului <strong>de</strong> moarte subită prin aritmii ventriculare. Furtuna electrică este <strong>de</strong>finită ca prezenţa<br />
a cel puţin două episoa<strong>de</strong> <strong>de</strong> tahicardie / fibrilaţie ventriculară într-o perioadă <strong>de</strong> 24 <strong>de</strong> ore.<br />
Aceasta reprezintă o urgenţă medicală şi un marker <strong>de</strong> prognostic slab la pacienţii cu ICD.<br />
Material si meto<strong>de</strong>: Prezentăm tratamentul cu succes al unei furtuni electrice, refractară la<br />
amiodaronă şi β-blocante, la un pacient <strong>de</strong> 60 <strong>de</strong> ani, cu <strong>de</strong>fibrilator implantabil, căruia i s-a<br />
practicat o intervenţie chirurgicală pentru cardiomiopatie ischemică şi anevrism gigant <strong>de</strong> VS.<br />
Fractia <strong>de</strong> ejectie preoperatorie era foarte mica, 16%, TAPSE 11mm. Sub circulatie<br />
extracorporeala s-a practicat rezectia anevrismului <strong>de</strong> VS , remo<strong>de</strong>larea VS prin proce<strong>de</strong>ul<br />
Cooley modificat si revascularizarea chirurgicala a miocardului cu AMI stanga pe LAD<br />
anastomozata in Y cu artera radiala stanga secvential pe artera marginala obtuza si artera<br />
posterolaterala <strong>din</strong> ACX<br />
Rezultate: La 15 luni a fost verificata patenta grafturilor prin arteriografie, functia<br />
ventriculara stanga prin ecografie si ventriculografie si, <strong>de</strong> asemenea, a fost inregistrat istoricul<br />
<strong>de</strong>fibrilatorului, iar <strong>de</strong>fibrilatorul nu a mai inregistrat episoa<strong>de</strong> terapeutice, fractia <strong>de</strong> ejectie<br />
crescand postoperator la 45-50%.<br />
Concluzii: Furtunile electrice sunt frecvente la pacienţii cu <strong>de</strong>fribilator implantabil si<br />
cardiomiopatie ischemica. Managementul acestora necesită utilizarea unor meto<strong>de</strong> simple şi a<br />
unora sofisticate. Managementul chirurgical ar putea reprezenta o soluţie eficientă pentru<br />
pacienţii cu anevrism gigant <strong>de</strong> VS şi furtuni electrice refractare tratamentului antiaritmic.<br />
67
Acute ascen<strong>din</strong>g aorta dissection asociated<br />
with bilateral carotid arteries dissection – case report<br />
Disecţie acută <strong>de</strong> aortă ascen<strong>de</strong>ntă asociată cu disecţie carotidiană bilaterală - prezentare <strong>de</strong> caz<br />
Dr. Raicea V., Dr. Moraru L., Dr. Serban V., Dr. Bica Lucia, Dr. Raicea C., prof. dr. Deac R.<br />
IUBCVT Tg-Mures<br />
A patient of a 32 years old, was admitted in one clinic of neurology with the diagnostic of<br />
stroke and left hemiparesis. At 4 days after the admission the echoDoppler examination at the<br />
carotidian level <strong>de</strong>monstrated dissection of the right common carotid artery, the CT examination<br />
and the echocardiography showing acute dissection of the ascen<strong>din</strong>g aorta, aortic arch and<br />
<strong>de</strong>scen<strong>din</strong>g aorta (tip A) with dissection on both common carotid arteries, mo<strong>de</strong>rate aortic<br />
regurgitation and hemopericardium. The emergency operation performed in the Clinic of<br />
Cardiovascular Surgery of IUBCVT Târgu Mures consisted in bilateral aorto-carotidian vascular<br />
bypass with a Dacron prosthesis, before initiating extracorporeal circulation, then correction of<br />
ascen<strong>din</strong>g aorta dissection at supracoronary level with dacron prosthesis and aortic valvuloplasty.<br />
The postoperator evolution was satisfactory, the follow up echocardiography showing trivial aortic<br />
regurgitation and normal flow in the carotid arteries.<br />
Disecţie acută <strong>de</strong> aortă ascen<strong>de</strong>ntă asociată cu disecţie carotidiană bilaterală - prezentare <strong>de</strong> caz<br />
Se prezintă cazul unui pacient <strong>de</strong> 32 ani, internat într-o clinica <strong>de</strong> neurologie cu<br />
diagnosticul <strong>de</strong> acci<strong>de</strong>nt vascular cerebral ischemic drept cu hemipareză stângă. La 4 zile după<br />
<strong>de</strong>butul simptomatologiei examenul echoDoppler carotidian <strong>de</strong>celează disecţia arterei caroti<strong>de</strong><br />
comune drepte, examenul CT şi echografia cardiacă ulterioară evi<strong>de</strong>nţiind disecţie acută <strong>de</strong><br />
aortă ascen<strong>de</strong>ntă, arc aortic şi aorta <strong>de</strong>scen<strong>de</strong>ntă (tip A) cu disecţie pe ambele artere caroti<strong>de</strong><br />
comune şi insuficienţă aortică mo<strong>de</strong>rată cu hemopericard. Se intervine chirurgical <strong>de</strong> urgenţă<br />
practicându-se bypass aorto-carotidian bilateral pe arterele caroti<strong>de</strong> comune (pre-bypass<br />
cardio-pulmonar) cu proteză <strong>de</strong> dacron, înlocuire <strong>de</strong> aortă ascen<strong>de</strong>ntă supracoronarian cu<br />
proteză <strong>de</strong> dacron şi valvuloplastie aortică. Evoluţia pacientului a fost favorabilă, echografia <strong>de</strong><br />
control postoperator <strong>de</strong>monstrând insuficienţă aortica minoră şi flux carotidian normal.<br />
Surgical Choices for Aortic Arch Syndrome<br />
Horia MURESIAN<br />
Cardiovascular Surgery, University Hospital of Bucharest<br />
Background. Severe and symptomatic stenotic-occlusive lesions of one or more arch<br />
vessels ask for an elaborate clinical and imagistic diagnosis and for varied but individually-applied<br />
surgical techniques, especially in patients having a life expectancy of 15 years or more.<br />
Materials and methods. The author presents his personal experience with 28 consecutive<br />
patients admitted for cerebrovascular insufficiency (inclu<strong>din</strong>g major stroke) and/or upper limb<br />
ischemia over a 4 year period. The following bypasses were used: ascen<strong>din</strong>g aorta-to-bilateral<br />
carotid artery: 4 cases; ascen<strong>din</strong>g aorta-to-carotid and subclavian artery: 4 cases;<br />
brachiocephalic trunk-to-carotid and subclavian artery: 1 case; subclavian-to-bilateral carotid<br />
artery: 1 case; subclavian-to-carotid artery: 3 cases; carotid-to-subclavian or axillary artery: 15<br />
cases.<br />
Results. Global mortality was 3,57%. One major hemispheric stroke occurred (3,57%). No<br />
postoperative cranial nerve palsies were encountered.<br />
Conclusions. Different surgical techniques can be applied for the treatment of the aortic<br />
arch syndrome. The ascen<strong>din</strong>g aorta represents a valuable donor vessel; alternatively, the<br />
brachiocephalic trunk, the subclavian or the carotid artery – can be used as well, especially in<br />
severely diseased patients. Doppler ultrasound examination doubled by arch and 4-vessel<br />
angiogram, represent the major steps in a thorough and efficient diagnostic workup. The<br />
complete revascularization can be contemplated even in patients with associated diseases but<br />
otherwise with a longer life expectancy.<br />
Feier Horea, Gaşpar M, Merce A., Nica D.,<br />
Deutsch P., Milovan Slovenski<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
O. Stiru, L.F. Dorobantu, O.Ghenu, Daniela<br />
Filipescu, V.A.Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare<br />
“Prof Dr. C.C.Iliescu” Bucureşti<br />
Opţiuni <strong>de</strong> tratament ale rupturii posttraumatice <strong>de</strong><br />
aortă.<br />
Treatment options for traumatic aortic transection<br />
Pseudonaevrism rupt <strong>de</strong> aortă asce<strong>de</strong>ntă dupa<br />
proteazre aortică – rezolvare chirurgicală.<br />
68
B. Rădulescu, R.Vasile, A.Vasilescu, Luminiţa<br />
Iliuţă, Y.Hashem, A.Mărginean, Mihaela Crăciun,<br />
S.Bubenek, H.Moldovan, V.Iliescu<br />
Spitalul Clinic Ju<strong>de</strong>ţean <strong>de</strong> Urgenţă, Universitatea <strong>de</strong><br />
Medicină şi Farmacie "Iuliu Haţieganu",<br />
Cluj-Napoca, Chirurgie II<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Bucureşti<br />
Anevrism gigant <strong>de</strong> crosă aortică – rezolvare<br />
chirurgicală.<br />
New approach for extend Type II TAAA In High risks patients<br />
P. Bergeron*, A. Petrosyan*, J. Bellos**, F. Markatis**, T. Abdulamit*, A. El shazly, J. -C. Trastour*<br />
*: Saint-Joseph Hospital, Marseille – France<br />
**: 1 st surgical clinic Laikon Hospital University of Athens Medical School<br />
Extend type II thoraco abdominal aortic aneurysms (TAAA) involving Arch Vessels and the<br />
visceral arteries remains a challenging operation when affecting High Risk Patients (HRP).<br />
Recently, Hybrid surgery has gained popularity for High Risk Patients (1). The other options<br />
are branched stent grafting which is still experimental, time consuming with a high radiation<br />
exposure, and the conventional surgical repair which carries a high risk of morbidity and mortality<br />
for such patients and which is still indicated for low risk patients.<br />
Stentgraft technology offer new alternatives when combined to standard surgery. 2 ways<br />
can be followed to simplify the management of type II TAAA:<br />
- What we call: the “down staging aneurysms operation”<br />
- The total antegra<strong>de</strong> <strong>de</strong>branching technique<br />
Technique and personal experience<br />
In our experience these 2 different techniques have been used for type II TAAA. In a Group<br />
a, a “down staging operation” was performed using a staged hybrid operation started by a Stent<br />
Graft from the arch to the distal <strong>de</strong>scen<strong>din</strong>g thoracic aorta and was followed by surgical repair<br />
un<strong>de</strong>r partial CPB limited to the celiac aorta (5 patients). In fact, this allow to convert an extend<br />
type II TAAA to a more limited type IV TAAA (fig 1). In a group b, a staged hybrid operation starting<br />
by <strong>de</strong>branching the aorta from sternotomy to supra aortic vessels and visceral arteries was<br />
followed by an exten<strong>de</strong>d stentgrafting (5 patients). We now favour this second attitu<strong>de</strong> which<br />
avoids cardiopulmonary bypass and aortic clamping. The surgical approach is a median<br />
sternotomy combined to mid upper laparotomy associated to pericardial and diaphragm<br />
division. It is well tolerated even in el<strong>de</strong>rly patients and allows easy access to celiac axis (CA),<br />
superior mesenteric artery (SMA), right renal artery (RAA). Access to the left renal artery is more<br />
difficult and may benefit from a combined stent grafting and bypass accor<strong>din</strong>g to the V. O. R. T.<br />
E. C. technique <strong>de</strong>scribed by Lachat. M (2) or extra anatomic bypass.<br />
Rerouting the visceral arteries is done from the ascen<strong>din</strong>g Aorta with a partial clamping.<br />
This implantation site is quite always undiseased offering a good anterogra<strong>de</strong> high flow.<br />
Combined bypass to the supra aortic vessels is associated when nee<strong>de</strong>d.<br />
Post operative course and follow up.<br />
During the 30 D period, one patient died in group A, zero in group B. There was no<br />
paraplegia in these series. Two patients presented a prolonged hospital stay due to a respiratory<br />
failure and a pancreatic fistula. The other patients were discharged at day 10 after 2 days of ICU.<br />
Summary<br />
This preliminary experience seems to be promising. This new approach for rerouting the supra<br />
aortic and visceral arteries before stent grafting type II TAAA lowers the surgical injury and is<br />
particularly <strong>de</strong>signed for HRP who cannot benefit from conventional surgery un<strong>de</strong>r Cardio<br />
pulmonary bypass (CPB).<br />
References<br />
1. Donas KP, Czerny M, Guber I, Teufelsbauer H, Nanobachvili J. [Hybrid open-endovascular<br />
repair for thoracoabdominal aortic aneurysms: current status and level of evi<strong>de</strong>nce] Eur J Vasc<br />
Endovasc Surg. 2007 Nov; 34 (5): 528-33. Epub 2007 Aug 1.<br />
2. Lachat M, Mayer D, Criado FJ, Pfammatter T, Rancic Z, Genoni M, Veith FJ.<br />
[New Technique to Facilitate Renal Revascularization with Use of Telescoping Self-Expan<strong>din</strong>g Stent<br />
Grafts: VORTEC.] Vascular. 2008 Mar-Apr; 16 (2): 69-72.<br />
69
Microsimulation and clinical outcomes analysis support a lower age threshold for use of<br />
biological valves. Microsimulation bioprostheses<br />
Serban Stoica, a Kimberley Goldsmith, b Nikolaos Demiris,<br />
b Prakash Punjabi, c Geoffrey Berg, d Linda Sharples, b Stephen Large e<br />
aBristol Royal Children's Hospital; bMedical Research Council Biostatistics Unit,<br />
Cambridge; cHammersmith Hospital, London; dGol<strong>de</strong>n Jubilee National Hospital,<br />
Glasgow; ePapworth Hospital, Cambridge, UK<br />
Background: We aimed to characterize contemporary results of aortic valve replacement<br />
(AVR) in relation to type of prosthesis and subsequent competing hazards.<br />
Methods: 5470 consecutive AVR ± coronary artery bypass grafting (CABG) patients were<br />
studied. Microsimulation of survival and valve-related outcomes was performed based on metaanalysis<br />
and patient data inputs, with separate mo<strong>de</strong>ls for age, gen<strong>de</strong>r and CABG. Survival was<br />
validated against the United Kingdom Heart Valve Registry.<br />
Results: Patient survival at 1, 5 and 10 years was 90%, 78% and 57% respectively. The<br />
crossover points at which bio- and mechanical prostheses conferred similar life expectancy (LE)<br />
was 59 years for males and females (no significant difference between<br />
prosthesis types between the ages of 56-69 for men, and 58-63 for women). The improvement in<br />
event-free LE for mechanical valves is greater at younger ages with a crossover point of 66 years<br />
for males and 67 years for females. Long-term survival was in<strong>de</strong>pen<strong>de</strong>ntly influenced by age, male<br />
gen<strong>de</strong>r, and concomitant CABG, but not by type of prosthesis. In bioprostheses the most common<br />
long-term occurrence is structural <strong>de</strong>terioration. For men aged 55, 65 and 75 at initial operation it<br />
has a lifetime inci<strong>de</strong>nce of 50%, 30% and 13% respectively. The simulation output showed excellent<br />
agreement with registry data.<br />
Conclusion: Bioprostheses can be implanted selectively in patients below 65 without<br />
significant long-term adverse effects.<br />
Carotid and Coronary Surgery - actual strategy<br />
I. Droc, I. Mocanu, Murgu V., Deaconu St., Pinte Fl<br />
Army’s Center for cardiovascular diseases, Bucharest, <strong>Romania</strong><br />
Lacking randomised trials, a major controversy remains the optimal management of<br />
patients who presents concomitant carotid and coronary artery disease.<br />
The main question is whether staged or simultaneous endarterectomy (CEA) will reduce<br />
peri-operative morbidity and mortality after cardiac surgery. The reported results were<br />
encouraging using either of the two strategies, but there is no consensus as to which is preferable.<br />
Recently carotid artery angioplasty with stenting (CAS) represents a potential alternative to CEA<br />
mostly in 'high-risk for CEA patients. CAS offers a less invasive, safer therapeutic option for cardiac<br />
patients who un<strong>de</strong>rwent or will un<strong>de</strong>rwent CABG. In some particular situations CAS+CABG, such a<br />
strategy might be harmful. In particular, the need for dual antiplatelet therapy after CAS can be<br />
balanced with avoi<strong>din</strong>g unnecessary blee<strong>din</strong>g complications after cardiac surgery.<br />
During 1-year period, between 01.01.2007 – 31.12.2007, at the Army’s Center of<br />
Cardiovascular Diseases 375 consecutive patients were referred for coronary surgery. 49 patients<br />
(13,3%) were found to have combined carotid and coronary disease. 37 patients (10%) un<strong>de</strong>rwent<br />
staged carotid endarterectomy (CEA) and coronary artery bypass grafting (CABG), with a mean<br />
of 30±6 days between the interventions, and 12 patients (3,3%) un<strong>de</strong>rwent CABG and CEA<br />
simultaneously. The mean age was 62,8± 4,7 years and 32 patients (65%) were males. The majority<br />
of the cases (82%) presented triple vessel disease and 16,7% had left main disease. The carotid<br />
disease was unilateral in 43 patients (87,7%) and bilateral in 2 (4%), and 36 (74,0%) were<br />
neurologically asymptomatic.<br />
The overall morbidity and mortality after the two procedures is 19,2% (Randall, 2006) and<br />
after simultaneous procedure is 17,4% (Rutherford 2005).<br />
In conclusion the presence of carotid stenosis is per se a marker of risk.<br />
There is a need for a randomized controlled trial focusing on combined or staged surgical<br />
approach or endovascular therapy.<br />
70
SALA Saphire<br />
Simpozionul Societăţii Române <strong>de</strong> Anestezie-Terapie Intensivă<br />
Cardiacă şi Tehnologie Extracorporeală (SRATICTE)<br />
Sesiunea XII - Anemia si transfuzia in chirurgia cardiaca<br />
Daniela Filipescu (Bucureşti) Paradoxul anemie-transfuzie în chirurgia cardiacă<br />
Ioana Grigoraş (Iaşi)<br />
Este administrarea perioperatorie <strong>de</strong> fier o soluţie ?<br />
Metabolismul fierului la pacientul critic<br />
How to reduce allogenic blood transfusion in cardiac surgery<br />
Reducerea necesarului transfuzional în chirurgia cardiacă<br />
Stanca Aszalos, Muresan A, Negrutiu S, Slabu L, Steiu C, Vlad I<br />
Anesthesia and Intensive Care Unit, Institutul Inimii “N. Stancioiu” Cluj-Napoca<br />
Perioperative blood conservation is an important requirement in mo<strong>de</strong>rn cardiac surgery.<br />
On one hand allogenic blood transfusion is accompanied by a significant number of serious<br />
complications (technical, infectious or immune) and is associated with an increase in<br />
postoperative mortality. On the other hand in our mo<strong>de</strong>rn society the banked blood availability<br />
does not match the necessities and allogenic transfusion is associated with significant economic<br />
costs. There are three conceptual ways to avoid allergenic blood transfusions: tolerating a lower<br />
hematocrit, reducing the intra and postoperative blood loss and autologous transfusion. Cardiac<br />
surgery patients do not tolerate well extreme anemia and in or<strong>de</strong>r to avoid allogenic transfusion in<br />
such patients a complex approach following precise protocols is nee<strong>de</strong>d. In or<strong>de</strong>r to reduce the<br />
perioperative blood loss a number of pre, intra and postoperative measures and drugs are<br />
available, and these measures imply a close cooperation between surgeons, anesthetists and<br />
perfusionists. Autologous transfusion can be planned and performed in advance of a major<br />
operation, acute, performed immediate before the operation with concomitant hemodilution or<br />
may be accomplished by intraoperative blood salvage. All these methods have their own<br />
advantages and disadvantages and their use in a particular case must follow strict gui<strong>de</strong>lines and<br />
protocols.<br />
Reducerea necesarului transfuzional in chirurgia cardiaca<br />
Reducerea necesarului transfuzional reprezinta o cerinta importanta a chirurgiei cardiace<br />
mo<strong>de</strong>rne. Pe <strong>de</strong> o parte transfuzia este asociata cu un numar <strong>de</strong> complicatii redutabile (tehnice,<br />
infectioase si imunologice) si este insotita <strong>de</strong> cresterea mortalitatii postoperatorii. Pe <strong>de</strong> alta parte<br />
in societatea mo<strong>de</strong>rna necesarul <strong>de</strong> sange a <strong>de</strong>pasit <strong>de</strong>mult resursele disponibile iar costurile<br />
economice sunt semnificative. Reducerea numarului <strong>de</strong> transfuzii poate fi realizata pe trei cai:<br />
tolerarea unui hematocrit scazut, reducerea pier<strong>de</strong>rilor <strong>de</strong> sange si transfuzia autologa. Pacientii<br />
supusi interventiilor chirurgicale pe cord tolereaza mai greu anemia severa si in cazul lor evitarea<br />
transfuziei alogene necesita o abordare complexa urmarind protocoale stricte. Reducerea<br />
pier<strong>de</strong>rilor <strong>de</strong> sange perioperatorii presupune un complex <strong>de</strong> masuri pre, intra si postoperatorii in<br />
aplicarea carora sunt implicati atat chirurgul cat si anestezistul si perfuzionistul si care includ<br />
tehnici si substante medicamentoase diferite. Transfuzia autologa poate fi si programata,<br />
preoperatorie, acuta intraoperatorie cu hemodilutie sau poate face apel la tehnicile <strong>de</strong><br />
recuperare a sangelui <strong>din</strong> campul operator. Toate aceste meto<strong>de</strong> au avantajele si <strong>de</strong>zavantajele<br />
lor iar utilizarea la un pacient anume trebuie strict individualizata si efectuata dupa ghiduri si<br />
protocoale precise.<br />
Carmen Movileanu, Roxana Toma, Mihaela<br />
Melinte, Horatiu Suciu (Tg. Mureş)<br />
Gabriela Olaru, Pavel Morar, Irina Modrigan,<br />
Horaţiu Suciu (Tg. Mureş)<br />
Sesiunea XIII<br />
Probleme<br />
pediatrică<br />
curente în practica transfuzională<br />
Particularităţi hematologice în patologia cianogenă<br />
postoperatorie<br />
71
Risk factors of renal dysfunction after cardiac surgery<br />
Factorii <strong>de</strong> risc ai disfuncţiei renale după intervenţii chirurgicale cardiace<br />
Dr. Balos S., dr. Kovacs Judit, dr. Mitre R., Jerzicska E., dr. Suciu H., prof. dr. Deac R.,<br />
IUBCVT Targu-Mureş, UMF Targu-Mureş<br />
Renal dysfunction is a relatively common complication of cardiac surgery, its <strong>de</strong>velopment<br />
significantly increasing postoperative morbidity and mortality.<br />
Material and methods. We conducted a retrospective study at IUBCVT Târgu-Mureş, from<br />
01/01/2009 to 01/07/<strong>2010</strong>, to <strong>de</strong>termine risk factors for renal dysfunction and the efficiency of<br />
diuretics and continuous veno-venous hemodialysis therapy in the prevention and therapy of this<br />
syndrome.<br />
Results and discussion. During this period 1067 patients had un<strong>de</strong>rwent cardiac surgery, of<br />
which 74 (6,9%) <strong>de</strong>veloped renal dysfunction / failure. Renal dysfunction <strong>de</strong>veloped in patients<br />
with complex surgery with prolonged cardiopulmonary bypass, those with postoperative<br />
hemodynamic instability requiring treatment with high doses of inotropics and vasoconstrictors to<br />
maintain blood pressure and cardiac output. 34 patients required renal replacement therapy, the<br />
rest of the patients respon<strong>din</strong>g favorably to diuretics.<br />
Conclusions. Cardiac surgery is associated with a relatively high inci<strong>de</strong>nce of renal<br />
dysfunction. Pathogenesis of this syndrome after open heart surgery is complex and involves<br />
hemodynamic and inflammatory changes as well. Therefore the treatment to prevent the<br />
<strong>de</strong>velopment of acute tubular necrosis should inclu<strong>de</strong> rapid hemodynamic stabilisation and<br />
euvolemia.<br />
Factorii <strong>de</strong> risc ai disfuncţiei renale după intervenţii chirurgicale cardiace<br />
Disfuncţia renală este o complicaţie relativ frecventă a chirurgiei cardiace, <strong>de</strong>zvoltarea<br />
acesteia creşte semnificativ morbiditatea şi mortalitatea postoperatorie.<br />
Material şi meto<strong>de</strong>. Am efectuat un studiu clinic retrospectiv în IUBCVT Tg-Mureş, în<br />
perioada 1.01.2009 – 1.07.<strong>2010</strong>. pentru a <strong>de</strong>termina factorii <strong>de</strong> risc ai disfuncţiei renale<br />
şi eficienţa terapiei cu diuretice şi prin hemodializă veno-venoasă continuă în prevenirea şi terapia<br />
acestui sindrom.<br />
Rezultate şi discuţii. În această perioadă s-a intervenit chirurgical pe cord <strong>de</strong>schis la 1067<br />
pacienţi, <strong>din</strong>tre care la 74 (6,9%) a aparut o disfuncţie/ insuficienţă renală. Disfuncţia renală s-a<br />
<strong>de</strong>zvoltat la pacienţii cu intervenţii chirurgicale complexe, cu bypass cardiopulmonar prelungit,<br />
cu instabilitate hemo<strong>din</strong>amică postoperatorie, care au necesitat tratament cu doze mari <strong>de</strong><br />
inotropice şi vasoconstrictoare pentru menţinerea tensiunii arteriale şi a <strong>de</strong>bitului cardiac.<br />
Epurarea extrarenală a fost necesară la 4 pacienţi. Ceilalţi pacienţi au răspuns favorabil la terapia<br />
cu diuretice.<br />
Concluzii. Chirurgia cardiacă este asociată cu o inci<strong>de</strong>nţă relativ crescută a disfuncţiei<br />
renale. Patogeneza acestui sindrom după intervenţii pe cord <strong>de</strong>schis este complexă, şi implică<br />
modificări hemo<strong>din</strong>amice şi inflamatorii <strong>de</strong>opotrivă. De aceea terapia pentru prevenirea necrozei<br />
tubulare acute trebuie să cuprindă stabilizarea hemo<strong>din</strong>amică rapidă şi asigurarea euvolemiei.<br />
AKI or RIFLE classification in evaluating the prognosis<br />
of cardiac surgery associated acute renal failure<br />
Clasificarea AKI sau RIFLE în evaluarea prognosticului insuficienţei renale acute asociate chirurgiei cardiace<br />
Dr. Balos S., dr. Kovacs Judit, dr. Mitre R., conf. dr. Suciu H., prof. dr. Deac R., IUBCVT Târgu-Mureş,<br />
Renal dysfunction is a complex syndrome, with clinical and laboratory manifestations<br />
ranging from minor changes in serum creatinine to anuria and even metabolic coma. In recent<br />
years two scores were <strong>de</strong>veloped to diagnose renal dysfunction. Our study aim to compare them<br />
in terms of prognostic assessment of acute renal failure associated with cardiac surgery.<br />
Materials and methods. We conducted a study on 44 patients with open heart surgery in<br />
IUBCVT Targu-Mureş, between 09/01/2009 to 06/30/<strong>2010</strong>, who <strong>de</strong>veloped various <strong>de</strong>grees of renal<br />
dysfunction in the postoperative period. In these patients we calculated and compared the AKI<br />
score and RIFLE score and studied the progression of the renal syndrome in terms of these scores.<br />
Results and discussion. AKI criteria allowed to i<strong>de</strong>ntify more patients having acute renal<br />
dysfunction (100% vs. 75%) and more patients were classified at stage I (risk group in RIFLE<br />
classification) (12 vs. 4), but we observed no differences for stage II (renal dysfunction in RIFLE<br />
72
classification) and stage III (renal failure in RIFLE classification). Mortality was higher in renal failure<br />
accor<strong>din</strong>g to RIFLE criteria and in stage III in AKI criteria.<br />
Conclusions. AKI criteria are more sensitive in i<strong>de</strong>ntifying patients at risk for renal<br />
dysfunction / failure after open heart surgery, but there were no differences in the estimation of<br />
postoperative mortality between the two scales.<br />
Clasificarea AKI sau RIFLE în evaluarea prognosticului insuficienţei renale acute asociate chirurgiei cardiace<br />
Disfuncţia renală este un sindrom complex, cu manifestări clinice şi paraclinice variate,<br />
pornind <strong>de</strong> la modificări minore ale creatininei serice până la anurie şi chiar comă metabolică. În<br />
ultimii ani au apărut mai multe scoruri pentru diagnosticarea şi stadializarea disfuncţiei renale.<br />
Scopul lucrării a fost compararea acestor date în ceea ce priveşte evaluarea prognosticului<br />
insuficienţei renale acute asociate chirurgiei cardiace.<br />
Materiale şi meto<strong>de</strong>. Am efectuat un studiu clinic pe 44 pacienţi operaţi pe cord <strong>de</strong>schis la<br />
IUBCVT Târgu-Mureş în perioada 1.09.2009-30.06.<strong>2010</strong>, la care s-au <strong>de</strong>zvoltat diferite gra<strong>de</strong> <strong>de</strong><br />
disfuncţie renală în perioada postoperatorie. La aceşti pacienţi s-a calculat şi comparat scorul<br />
RIFLE, scorul AKI şi s-a studiat evoluţia bolii în funcţie <strong>de</strong> aceste scoruri.<br />
Rezultate şi discuţii. Criteriile AKI au permis i<strong>de</strong>ntificarea mai multor pacienţi ca având<br />
disfuncţie renală acută (100% faţă <strong>de</strong> 75%) şi au clasificat mai mulţi pacienţi în stadiul I (grupa <strong>de</strong><br />
risc în clasificarea RIFLE) (12 vs. 4), dar nu am observat diferenţe pentru stadiul II (disfuncţe în<br />
clasificarea RIFLE) şi pentru stadiul III (insuficienţă renală în clasificarea RIFLE). Mortalitatea a fost<br />
mai mare în caz <strong>de</strong> insuficienţă renală acută conform criteriilor RIFLE respectiv stadiul III conform<br />
criteriilor AKI.<br />
Concluzii. Criteriile AKI sunt mai sensibile în i<strong>de</strong>ntificarea pacienţilor cu risc crescut pentru a<br />
<strong>de</strong>zvolta disfuncţie / insuficienţă renală după intervenţii pe cord <strong>de</strong>schis, dar nu există diferenţe în<br />
ceea ce priveşte estimarea mortalităţii postoperatorii între cele două scale.<br />
N-GAL - early marker for acute renal injury in cardiac surgery?<br />
Anca Pro<strong>de</strong>a, Mihail Luchian, Alina Paunescu, Ioana Marinica, Oana Ghenu, Simona Marin, Oana<br />
Mihailescu, Laura Dima, Ovidiu Chioncel, Luminita Iliuta, Daniela Filipescu, Cezar Macarie<br />
Department of Cardiac Anesthesia & Intensive Care<br />
Emergency Institute for Cardiovascular Disease, Bucharest, <strong>Romania</strong><br />
Background: Postoperative acute kidney injury (AKI) is a frequent complication after<br />
cardiac surgery and is related to different mechanisms. AKI is typically diagnosed by measuring<br />
serum creatinine concentrations but unfortunately creatinine is very insensitive to even substantial<br />
<strong>de</strong>cline in glomerular filtration rate. The purpose of our study is to analyze the utility of plasmatic<br />
neutrophil gelatinase-associated lipocalin (N-GAL) <strong>de</strong>termination for <strong>de</strong>tection of early kidney<br />
injury in unselected patients admitted in intensive cardiac care unit post cardiac surgery with<br />
cardiopulmonary bypass (CPB).<br />
Method: Plasma N-GAL level was <strong>de</strong>termined preoperatively (baseline value), 2 hours<br />
postoperatively and in the first postoperative day in consecutive cardiac on pump surgery<br />
patients. Patients with abnormal preoperative creatinine value were exclu<strong>de</strong>d. AKI was <strong>de</strong>fined as<br />
an increase in serum creatinine >50% from baseline within the first 72 hours post operatively. N-GAL<br />
was <strong>de</strong>termined with ELISA test kitt with maximal normal value of 106 ng/ml. Maximal values of N-<br />
GAL in patients with and without AKI were assessed using logistic regression. The analysis of ROC<br />
curve was utilized for <strong>de</strong>termination of sensitivity, specificity and cutoff value of postoperative N-<br />
GAL predicting postoperative AKI.<br />
Results: 22 patients (17 men and 5 women) were inclu<strong>de</strong>d. 6 patients (27,3%) had AKI and<br />
5 patients (83,3%) from the group of AKI had a N-GAL value of more than 106 ng⁄ml. In the group<br />
without AKI, 11 (68,7%) patients had an abnormal N-GAL value. Plasma N-GAL levels after CPB<br />
were higher in patients who subsequently <strong>de</strong>veloped AKI than in those who did not (180,5 (103-<br />
218) ng/ml vs. 133 (42-232) ng/ml, p
Sesiunea XIV - Siguranţa pacientului în timpul circulaţiei extracorporeale<br />
Monitoring and Safety Issues in Cardiopulmonary<br />
Dan Longrois (Paris)<br />
Bypass<br />
Oana Ghenu, Mihai Luchian, Victor Pavel, Gabi<br />
Olteanu, Horaţiu Moldovan, Vlad Iliescu, Daniela Locul ECMO în chirurgia cardiacă<br />
Filipescu (Bucureşti)<br />
Dan Longrois (Paris) Experienţa clinica cu ECMO<br />
Cardio Pulmonary By-Pass Between Neurocognitive Deficits<br />
in the Past to Postconditioning in the Future?<br />
Circulaţia extracorporeală <strong>de</strong> la disfuncţia neurocognitivă în trecut, la postcondiţionare în viitor?<br />
Diaconescu Victor Mihail<br />
IBCV “Prof. Dr. Ge. I. M. Georgescu” Iaşi<br />
Neurocognitiv <strong>de</strong>ficits in cardiac surgery was linked to CPBP. In the last period of time this<br />
issue is <strong>de</strong>nied. Recently enough, there were published laboratory data on cardiac and neuronal<br />
postconditioning that could be induced by perfusion changed technique. We inclu<strong>de</strong> some data<br />
on preconditioning. The new policy in CPBP may inclu<strong>de</strong> the possibility of postconditioning in the<br />
management of el<strong>de</strong>rly patient.<br />
Bibliografie. Jakob Vinten-Johansen Postconditioning and Controlled Reperfusion, The<br />
Nerve of It All Anesthesiology 2009; 111: 1177–9<br />
Lidocaine intravenous is it better?<br />
Victor Mihail Diaconescu<br />
Secţia ATI Institutul <strong>de</strong> Boli Cardiovasculare „Prof.Dr. Ge IM Georgescu” Iaşi<br />
Postoperative pain remains an incomplete solved issue. There are studies that <strong>de</strong>monstrate<br />
the utility of associated intravenous and continuously lidocaine to opioids in anesthesia and in<br />
postoperative anlgesia. The administered lidocaine reduces the amount of necessary opioids for<br />
anesthesia and postoperative analgesia and facilitates the gastrointestinal function recovery. The<br />
link between pain, proinflamatory cytokins and the modulatory action of lidocain on cytokins is<br />
the main mechanism in the recent studies.<br />
Method: we random separated two groups of patients – the Saline group and the<br />
Lidocaine group; the last one received lidocaine intravenous continouslly 2mg/kg/h and<br />
morphine per cardiac anesthesia, then 1,3mg/kg/h in the postoperative analgesia along with<br />
tramadol and acetaminophen.<br />
Conclusion: the opioid consumption was reduced and the intestinal recovery was 12 hours<br />
faster. We assume that lidocaine administered as part of the analgesia protocol is a good option<br />
to reduce the opioid consumption and si<strong>de</strong> effects.<br />
Blood Cardioplegia Leukocyte Filtration – a Myocardial Protection Strategy.<br />
Filtrarea leucocitara a cardioplegiei cu sange - strategie <strong>de</strong> protectie miocardică în timpul CEC.<br />
V. Murgu, I. Mocanu, G. Cristian, I. Droc, G. Sandu, I. Tintoiu, Andreea Teodorescu, Laura Vamanu,<br />
Andreea Tifrea, Anca Filip, Florina Pinte, I. Tintoiu.<br />
SIRS (Systemic Inflammatory Response Syndrome) and especially SIRAB (Systemic<br />
Inflammatory Response Syndrome After cardiopulmonary Bypass) may be life threatening in<br />
extreme cases.<br />
Ischemia reperfusion injury is a manifestation of SIRS involving both humoral and cellular<br />
systemic response, particularly polymorfonuclear leukocytes activation.<br />
Neutrophyl activation involves two major mechanisms: 1) contact of circulating leukocytes<br />
with artificial surfaces and (2) ischemia reperfusion injury after the release of the aortic clamp.<br />
SLF (Strategic Leukocyte Filtration) implies the use of the leukocyte filters only during the<br />
early postischemic reperfusion phase.<br />
74
Mechanisms of the leukocyte <strong>de</strong>pleting filters involve al least four kinds of leukocyte<br />
entrapment: blocking, bridging, interception and adhesion.<br />
On the other hand SLF (Selective Leukocyte Filtration) of blood cardioplegia adresses to a highly<br />
pathogenic situation with repetitive 20 min. periods of ischemia followed by a short reperfusion<br />
phase during cardioplegic reinfusion.<br />
Our study using systemic leukocyte filtration in the due respect of what means today SLF<br />
(Strategic Leukocyte Filtration) and TLC (Total Leukocyte Control) reveals better results using<br />
arterial vs venous line leukocyte filters during CPB in terms of acute phase response markers<br />
(Reactive CP, IL- 6), leukocyte activation markers (elastase, MPO- Myloperoxidase), injury<br />
myocardial reperfusion markers (T Troponin, CKMB, lactic acid- from blood coronary sinus),<br />
inotropic suport, ejection fraction, ICU stay, etc.<br />
Leukocyte Filtration of blood cardioplegia reduces myocardial ischemia and improves<br />
cardiac function as <strong>de</strong>termined by stroke work in<strong>de</strong>x, limits necrosis, reduces CKMB concentration,<br />
limits the oxidative damage (MDA in coronary sinus blood) and reduces the inotropic support.<br />
Keywords: SIRS, SIRAB, Ischemia/reperfusion injury TLC (Total Leukocyte Control), SLF<br />
(Strategic Leukocyte Filtration)<br />
Jozsef Budai (Tg. Mures)<br />
Rezistenţa la heparină - importanţa problemei pentru<br />
circulaţia extracorporeală<br />
The advantages of intermittent warm blood cardioplegia supplemented with Mg++<br />
Guzgan Iu., Vîrlan E., Matcovschi I., Moscalu V., Manolache S., Batrinac A.<br />
Institute of Cardiology, Republic of Moldova<br />
Combined crystalloid blood cardioplegic solution (2 parts crystalloid, one part venous<br />
blood), elaborated and implemented by our specialists, assured a good protection of<br />
myocardium, during the operations also with a long Ao cross-clamping time. This is proved through<br />
results of more then 3000 of interventions with CPB since 1995 and by clinical, morphological and<br />
biochemical studies. The revising of temperature protocol and the necessity of exten<strong>din</strong>g the time<br />
between reperfusions accor<strong>din</strong>g to techniques performed by surgeons <strong>de</strong>termined the need in<br />
other tactics related to myocardial protection.<br />
Purpose of study: Evaluation of the efficacy of intermittent warm blood cardioplegia<br />
supplemented with Mg++ for more lasting protection of myocardium during cardiac arrest.<br />
Material and methods: The study was performed throughout two groups of patients with no<br />
significant difference in preoperative clinical conditions, who un<strong>de</strong>rwent operations with CPB<br />
during the February-March <strong>2010</strong> period. In Ist group (control) intermittent cold crystalloid-blood<br />
cardioplegia (8-10 oC) was <strong>de</strong>livered every 20 minutes, rectal temperature <strong>de</strong>creased to 30±1,5 oC.<br />
In the 2nd group of patients temperature was maintained at 35,5±1,1 oC with applying the warm<br />
blood cardioplegia accor<strong>din</strong>g to Calafiore protocol subsequently modified by Casalino et al. by<br />
ad<strong>din</strong>g the magnesia sulfate and exten<strong>din</strong>g the period of ischemia up to 25 minutes. The efficacy<br />
of myocardial protection was done using clinical and functional parameters: the frequency of<br />
spontaneous cardiac rhythm restoration; emergence of electrocardiographic changes; the<br />
frequency of applying of cardio version after the reperfusion; the requirement in inotropes during<br />
the first two days after the intervention; length of staying in ICU.<br />
Rezults: Besi<strong>de</strong>s the convenience of cardioplegic process management, in group II of<br />
patients were noted several moments of obvious superiority of warm blood cardioplegy<br />
performed at intervals of 25 minutes of ischemia. Spontaneous restoration of rhythm was 48% in<br />
group I and in II - 72%. As the absolute number of cardioversion remained practically equal in both<br />
groups, the II group had fewer patients whom were applied cardioversions after reperfusion. AV<br />
blocks occurred at equal. Number of patients requiring inotropic support in the early days was<br />
more representative of the control group. Average length of stay in ICU was 2.5 ± 0.3 for study<br />
group to 2.9 ± 0.4 for control group.<br />
Conclusions: Intermittent warm blood cardioplegia with Mg + + allows safe extension of the<br />
period of ischemia between reperfusions to 25 minutes and has a positive impact on some clinical<br />
and functional parameters of patients in the immediate postoperative period.<br />
75
Sesiunea XV<br />
Percutaneous tracheostomy in ICU patients un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy<br />
Traheostomia percutană în terapia intensivă sub control vi<strong>de</strong>olaringoscopic<br />
Ion Miclea, Violeta Bercan, Şerban Bubenek<br />
Institutul <strong>de</strong> Urgenţă pentru Boli Cardiovasculare “Prof. Dr. C.C. Iliescu”, Bucharest, <strong>Romania</strong><br />
Mo<strong>de</strong>rn intensive care involves a series of maneuvers that were formerly the exclusive<br />
preserve of surgery. Current technology provi<strong>de</strong>s special medical kits for percutaneous<br />
tracheostomy, pleural punctures, intra-aortic balloon pump, etc., facilitating these maneuvers,<br />
which have become common in intensive care units. Percutaneous tracheostomy occupies an<br />
important place in airway management of critical ill patient.<br />
Nowadays, percutaneous tracheostomy became very important in comparision to<br />
conventional surgical traheostomy. Dilatation technique is consi<strong>de</strong>red the gold standard. There<br />
are more than 600 publications related to percutaneous tracheostomy that were mentioned after<br />
1985.<br />
Indications of tracheostomy: - Need for prolonged mechanical ventilation, Airway<br />
obstruction, Need for improved pulmonary toilet, Ina<strong>de</strong>quate caugh due to chronic pain or<br />
weakness, Aspiration and the inability to handle secretions, Prophylaxis (preparation for extensive<br />
head and neck procedures and the convalescent period), Severe sleep apnea not amendable<br />
to continuous positive airway pressure <strong>de</strong>vices.<br />
Vi<strong>de</strong>olaryngoscopy during percutaneous tracheostomy<br />
During percutaneous tracheostomy it is possible to puncture the endotracheal tube, or its<br />
cuff, with the needle, which can lead to airway <strong>de</strong>pressurization, with the risk of difficult ventilation<br />
or gastric aspiration. To minimize this risk, there is the possibility of withdrawing the intubation tube<br />
un<strong>de</strong>r vi<strong>de</strong>olaryngoscopic control. The endotracheal tube is withdrawn until its cuff is seen<br />
between the vocal cords. The balloon is than inflated, and the percutaneous tracheostomy<br />
continues in the classical technique. Any reposition of the endotracheal tube, or patient’s<br />
intubation can be more easily controlled un<strong>de</strong>r vi<strong>de</strong>olaryngoscopy than with direct laryngoscopy.<br />
The anaesthetist position during vi<strong>de</strong>olaryngoscopy is more convenient than that of direct<br />
laryngoscopy. With the Gli<strong>de</strong>scope the image of the trachea and the vocal cords is transmitted<br />
on the screen.<br />
Role Of The Highly Specific C-Reactive Protein In Perioperatory Risk Evaluation Of Surgical<br />
Myocardial Revascularization<br />
Proteina C reactivă înalt specifică în optimizarea predicţiei morbidităţii şi mortalităţii în<br />
chirurgia <strong>de</strong> revascularizare miocardică faţă <strong>de</strong> scorurile clasice<br />
Lazăr Ovidiu, Goleanu Viorel, Tică Talida, Stanciu Crina,<br />
Mitulescu A<strong>din</strong>a, Cârjaliu Ionuţ, Butuşină Marian<br />
The experience of C.B.C.V. “Agrippa Ionescu”<br />
The highly specific C-reactive protein – hsCRP, reprezents an in<strong>de</strong>pen<strong>de</strong>nt factor with a<br />
highly predictive value for postoperative complications, that can occur after surgical myocardial<br />
revascularization (CABG).<br />
The aim of our retrospective study consists in the evaluation of suplimentary informations<br />
and in the optimization, in terms of predictive value, of the currently used clasical scores for<br />
preoperatory risc asessment (mortality and morbidity) and ICU admision of CABG.<br />
The study inclu<strong>de</strong>s 70 pacients with indication for CABG. Preoperatory we calculated<br />
several mortality and morbidity risk asessment scores as follows: EUROSCORE, PARSONNET,<br />
ACC/AHA, BIAGIOLI, ICU ADMISION HIGGINS.<br />
The patinets were followed for 30 days after CABG.<br />
Results: The hsCRP level, consi<strong>de</strong>red “cut-off” is 3, 3 mg/l. The patients presenting high<br />
levels of hsCRP were also inclu<strong>de</strong>d in the group with an increased inci<strong>de</strong>nt of mortality and<br />
morbidity.<br />
76
Levosimendan in pediatric cardiac surgery<br />
– preliminary conclusions based on two case reports<br />
Vlad Ioan H.<br />
Anesthesia and Intensive Care Unit, Institutul Inimii “N. Stancioiu” Cluj-Napoca<br />
The objective of this paper is to <strong>de</strong>scribe our preliminary experience with levosimendan in<br />
pediatric cardiac surgery patients.<br />
The two patients have been operated and treated in the cardiovascular surgery<br />
<strong>de</strong>partment of the Heart Institute “N. Stancioiu” in Cluj-Napoca. The first patient was a one year<br />
old infant who was admitted for the surgical correction of a severe mitral regurgitation and a<br />
persistent ductus arteriosus with severe pulmonary hypertension and heart failure. The second<br />
patient was a newborn with coarctation of the aorta, persistent ductus arteriosus, atrial and<br />
ventricular septal communications, gra<strong>de</strong> III tricuspid regurgitation, pulmonary hypertension<br />
cardiogenic shock and respiratory failure. The first patient received a single dose of levosimendan<br />
while the second patient received two doses. The efficiency and safety of the treatment with<br />
levosimendan were appreciated by the monitoring of hemodynamic parameters (heart rate,<br />
arterial pressure, central venous pressure) and by echocardiography. Additionally, the need for<br />
concomitant therapy with “classical” inotropes was also taken into account. The hemodynamic<br />
parameters remained stable during and after the levosimendan infusion and echocardiography<br />
showed an increase in myocardial contractility. Both patients have received long term inotropic<br />
support reflecting the fact thatnumerous factors are involved in the etiology of the low cardiac<br />
output syndrome.<br />
Levosimendan is a safe and efficient therapeutic alternative in pediatric cardiac surgery.<br />
The inotropic effect is good, rapid and long lasting, the si<strong>de</strong> effects are minimal and it can be<br />
combined with other inotropes. Additional studies in this setting and a treatment protocol are still<br />
necessary before routinely use levosimendan in pediatric cardiac surgery.<br />
Key words: levosimendan, pediatric cardiac surgery, low cardiac output<br />
Levosimendan in chirurgia cardiaca pediatrica - consi<strong>de</strong>ratii pe marginea a doua<br />
prezentari <strong>de</strong> caz.<br />
Obiectivul acestei lucrari il constituie <strong>de</strong>scrierea si interpretarea constatarilor facute in<br />
urma utilizarii levosimendanului la doi copii operati pe cord si care au prezentat disfunctie<br />
miocardica severa.<br />
Cei doi pacienti au fost operati si urmariti in Clinica <strong>de</strong> chirurgie cardiovasculara a<br />
Institutului Inimii <strong>din</strong> Cluj-Napoca. Este vorba <strong>de</strong>spre o fetita <strong>de</strong> un an care s-a prezentat pentru<br />
corectia chirurgicala a unei insuficiente mitrale congenitale severe si a unui canal arterial<br />
permeabil cu hipertensiune pulmonara si insuficienta cardiaca NYHA III si <strong>de</strong>spre un nou nascut<br />
care a fost internat cu diagnosticul <strong>de</strong> coarctatie <strong>de</strong> aorta, persistenta canalului arterial, <strong>de</strong>fect<br />
septal interatrial, <strong>de</strong>fect septal interventricular, insuficienta tricuspidiana gradul III, hipertensiune<br />
pulmonara, soc cardiogen, insuficienta respiratorie acuta.<br />
In primul caz s-a administrat o doza unica <strong>de</strong> levosimendan in timp ce la cel <strong>de</strong> al doilea<br />
pacient s-au administrat doua doze.<br />
Eficienta si siguranta tratamentului au fost apreciate prin urmarirea parametrilor<br />
hemo<strong>din</strong>amici (frecventa cardiaca, presiune arteriala, presiune venoasa), a aspectului<br />
ecocardiografic si a necesarului <strong>de</strong> inotrope “clasice”. Parametrii hemo<strong>din</strong>amici au ramas stabili<br />
in timpul si dupa administrarea levosimendanului in timp ce ecocardiografia a aratat o crestere a<br />
contractilitatii miocardice. Tratamentul inotrop asociat a fost <strong>de</strong> durata, reflectand etiologia<br />
plurifactoriala a sindromului <strong>de</strong> <strong>de</strong>bit cardiac scazut.<br />
In concluzie levosimendanul constituie o alternativa terapeutica viabila in chirurgia<br />
cardiaca pediatrica, atuurile sale fiind efectul inotrop bun, rapid si <strong>de</strong> durata, lipsa efectelor<br />
secundare majore si posibilitatea <strong>de</strong> asociere cu alte antiaritmice. Ar fi insa utile studii care sa<br />
plaseze exact levosimendanul in lista inotropelor utilizate perioperator, eventual chiar un algoritm<br />
<strong>de</strong> administrare similar cu ce <strong>de</strong> la adulti.<br />
Cuvinte cheie: levosimendan, chirurgie cardiaca pediatrica, sindrom <strong>de</strong> <strong>de</strong>bit cardiac<br />
scazut.<br />
77
Levosimendan in patients with postoperative haemofiltration<br />
Levosimendan la pacienti hemofiltrati postoperator<br />
Mihail Luchian, Ioana Marinica, Alina Paunescu, Oana Ghenu, Simona Marin, Anca Pro<strong>de</strong>a, Ovidiu<br />
Chioncel, Luminita Iliuta, Oana Mihailescu, Horatiu Moldovan, Vlad Iliescu, Daniela Filipescu<br />
Department of Cardiac Anesthesia & Intensive Care<br />
Emergency Institute for Cardiovascular Disease, Bucharest, <strong>Romania</strong><br />
Background: Levosimendan is a new ino-dilator drug with a special pharmacokinetics. The<br />
half-life is approximately 1 hour. However, its metabolites have a long half-life explaining the<br />
hemodynamic effects after the administration of the drug. In contrast to levosimendan, the<br />
metabolites are dialyzable. Data on the use of levosimendan in patients requiring continuous renal<br />
replacement therapy (CRRT) are scarce.<br />
Method: We present our experience with levosimendan (0,1 μg/kg/hour over 24 hours<br />
without bolus) in twelve consecutive patients with refractory cardiogenic shock after ST-elevation<br />
myocardial infarction (3 patients) or after cardiac surgery (9 patients), who <strong>de</strong>veloped multiorgan<br />
dysfunction syndrome and also required CRRT. Hemodynamic effects were registered<br />
invasively and monitored over 72 hours post infusion. Measured parameters were: cardiac<br />
output/in<strong>de</strong>x (CO/CI), pulmonary artery occlusion pressure (PaOP), left ventricular ejection<br />
fraction (LVEF), mixed venous oxygen saturation (SvO2) and cardiac power (CPO). Length of stay<br />
(LOS) in cardiac intensive care (CICU) and in-CICU mortality was also registered. Data were<br />
expressed as mean ± standard <strong>de</strong>viation (SD). Fisher’s exact test and non-paired t-test were used<br />
when appropriate. P-value
Scopul lucrarii: Sindromul <strong>de</strong> raspuns inflamator sistemic (SIRS) si sindromul vasodilatator<br />
afecteaza pacientii dupa chirurgia cardiaca cu circulatie extracorporeala. Studii anterioare au<br />
<strong>de</strong>monstrat beneficiile utilizarii cortizonului in doze mici perioperator. Scopul lucrarii este<br />
<strong>de</strong>monstrarea efectelor benefice ale administarii <strong>de</strong> hemisuccinat <strong>de</strong> hidrocortizon doar in ziua<br />
operatiei la pacientii cu risc crescut.<br />
Material si metoda: Studiu prospectiv pe o serie <strong>de</strong> 52 <strong>de</strong> pacienti consecutivi cu risc<br />
crescut in chirurgia cardiaca. Jumatate <strong>din</strong> pacienti (26) au primit 100 mg HHC iv bolus la inductia<br />
anesteziei si 100 mg HHC in perfuzie lenta pe tot parcursul operatiei.<br />
Concluzii: Am masurat parametri paraclinici (lactat), clinici (durata ventilatiei mecanice,<br />
durata <strong>de</strong> se<strong>de</strong>re in terapie intensiva, utilizarea <strong>de</strong> vasopresor) inci<strong>de</strong>nta complicatiilor (fibrilatie<br />
atriala, infectii), mortalitate. Utilizarea dozei stress <strong>de</strong> HHC doar in timpul operatiei are efecte<br />
benefice la pacientii cu risc crescut in chirurgia cardiaca.<br />
Victor Diaconescu (Iaşi) Efecte antiinflamatorii ale combinaţiei xilină-morfină<br />
Anestezia loco-regionala (blocul cervical) in chirurgia carotidiana – evaluare retrospectiva a<br />
experientiei <strong>din</strong> Clinica <strong>de</strong> Chirurgie Vasculara a SUUB<br />
Dr. Dumitrescu Radu Mihai medic specialist ATI,<br />
Dr. Tutor Cristina Anca medic specialist ATI, Sef Lucrari Dr. Copaciu Elena medic primar<br />
ATI-Clinica ATI Spitalul Universitar <strong>de</strong> Urgenta Bucuresti<br />
Introducere: Endarterectomia carotidiana (CEA) reprezinta o preocupare constanta a<br />
clinicii noastre; in intervalul <strong>de</strong> timp studiat (martie 2009-iunie <strong>2010</strong>) au fost realizate 142 <strong>de</strong><br />
proceduri sub anestezie loco-regionala, unilaterale sau bilaterale simultane reprezentand 42,90%<br />
<strong>din</strong> totalul interventiilor. Alegerea tehnicilor <strong>de</strong> anestezie loco-regionala (ALR) a avut drept<br />
premise raportarile <strong>din</strong> literatura <strong>de</strong> specialitate privind stabilitatea hemo<strong>din</strong>amica superioara si<br />
rata mai redusa a complicatiilor cardio-respiratorii perioperatorii (Magnadottir), inci<strong>de</strong>nta mai<br />
redusa a acci<strong>de</strong>ntelor vasculare cerebrale si a atacurilor ischemice tranzitorii (Zvara) precum si<br />
datele privind monitorizarea neurologica si <strong>de</strong>cizia aplicarii shuntului intraoperator<br />
(Stoughton).Tehnica anestezica a constat <strong>din</strong> injectarea unei dilutii <strong>de</strong> anestezic local<br />
(ropivacaina), dupa o tehnica modificata, realizandu-se un bloc cervical superficial si profund.<br />
Monitorizarea intraanestezica a fost una standard (inclusiv TA invaziv cu abord radial, EKG in 5<br />
<strong>de</strong>rivatii cu monitorizarea <strong>de</strong> segment ST).<br />
Obiective: evaluarea inci<strong>de</strong>ntelor legate <strong>de</strong> ALR precum si a evenimentelor neurologice<br />
majore in cazul interventiilor <strong>de</strong> CEA precum si raportarea lor la cifrele <strong>din</strong> literatura; aprecierea<br />
nivelului <strong>de</strong> siguranta a tehnicii anestezice.<br />
Loturile <strong>de</strong> pacienti studiati au cuprins: 50 <strong>de</strong> pacienti supusi CEA bilaterala simultana si 87<br />
<strong>de</strong> pacienti supusi CEA unilaterala (58,62% stanga si 41,37% dreapta). Au mai fost realizate 12<br />
interventii complexe sub ALR combinata (bloc cervical si interscalenic) pentru by-pass subclaviocarotidian<br />
(ipsi sau contralateral) si reimplantare <strong>de</strong> artera vertebrala simultan cu CEA unilaterala.<br />
Indicatorii <strong>de</strong>mografici: 73,23% barbati si 26,76% femei cu o repartitie a varstelor medii 65,31 ani<br />
respectiv 70 ani (CEA unilaterala) si 66 ani respectiv 64,53 ani (CEA bilaterala). Timpul mediu pana<br />
la externare a fost <strong>de</strong> 6,04 zile in cazul CEA unilaterala si 5,93 zile in cazul CEA bilaterala fiind<br />
influentat <strong>de</strong> tehnica anestezica in cazul unor pacienti cu patologie asociata complexa si<br />
incadrati in clasa <strong>de</strong> risc anestezic ASA III-IV.<br />
Rezultate si concluzii: Superioritatea ALR folosite s-a dovedit in monitorizarea a<strong>de</strong>cvata a<br />
statusului neurologic (pastrarea contactului verbal si monitorizarea functiei motrice a membrului<br />
superior contralateral); <strong>de</strong>cizia montarii shuntului temporar intraoperator a fost luata in 5 cazuri <strong>de</strong><br />
CEA unilaterala (5,87%) si 11 cazuri <strong>de</strong> CEA bilaterala (22%). Din punct <strong>de</strong> ve<strong>de</strong>re al inci<strong>de</strong>ntelor<br />
legate <strong>de</strong> tehnica anestezica s-au inregistrat: 3 cazuri <strong>de</strong> mioclonii faciala si 2 cazuri <strong>de</strong> convulsii<br />
cupate rapid la benzodiazepine (3,52%). In 2 cazuri s-a realizat convertirea la anestezie generala<br />
prin lipsa <strong>de</strong> cooperare a pacientilor. A existat un sindrom coronarian acut intraoperator si un<br />
acci<strong>de</strong>nt vascular cerebral major prin tromboza ACC urmat <strong>de</strong> <strong>de</strong>cesul pacientului la 10 zile<br />
postoperator; in 4 cazuri s-a observat si documentat AVC ischemic cu evolutie in curs <strong>de</strong><br />
recuperare la momentul externarii (3,52%). Pentru 2 cazuri care au prezentat hematom<br />
laterocervical s-a reintervenit precoce pentru controlul hemostazei. Tehnica anestezica s-a<br />
dovedit avand un profil <strong>de</strong> siguranta superior, cu cifre referitoare la inci<strong>de</strong>nte similare celor <strong>din</strong><br />
literatura.<br />
79
Oana Mihăilescu, Alina Păunescu, Mihai<br />
Luchian, Anca Pro<strong>de</strong>a, Oana Ghenu, Ioana<br />
Marinică, Simona Marin, Laura Dima, Ovidiu<br />
Chioncel, Luminiţa Iliuţă, Sorin Maximeasa,<br />
Horaţiu Moldovan, Vlad Iliescu, Daniela Filipescu<br />
(Bucureşti)<br />
Este troponina predictivă post chirurgie cardiacă?<br />
Is Troponin a predictive biomarker in cardiac surgery?<br />
Oana Mihailescu, Alina Paunescu, Oana Ghenu, Mihai Luchian, Anca Pro<strong>de</strong>a, Simona Marin,<br />
Ovidiu Chioncel, Luminita Iliuta, Sorin Maximeasa, Horatiu Molovan, Vlad Iliescu, Daniela Filipescu<br />
Introduction: Cardiac biomarker sensitivity is crucial for <strong>de</strong>tecting postoperative<br />
myocardial infarction (POMI) and consequently, for prediction of outcome after cardiac surgery.<br />
The aim of our study was to evaluate the perioperative dynamics of troponin I and its value in risk<br />
stratification after coronary artery bypass grafting (CABG) surgery.<br />
Methods: This study is a prospective observational one. Troponin I levels were measured<br />
preoperatively, in the first 24 hours and on the 7th day after CABG surgery. At the same time<br />
periods, the following were also assessed: ECG, total creatinine kinase and MB fraction, and transthoracic<br />
echocardiography images. Demographic and surgical data, medications, duration of<br />
extracorporeal circulation (ECC) and of aortic cross clamping, postoperative complications, ICU<br />
and hospitalization length of stay (LOS), and mortality were recor<strong>de</strong>d. Statistical analyses using<br />
area un<strong>de</strong>r the curve (AUC) examined in receiver operating characteristic (ROC) curves in a<br />
multivariable mo<strong>de</strong>l and compared analysis of variance (Oneway ANOVA) were performed.<br />
Results: 158 patients were inclu<strong>de</strong>d, 122 men and 36 women, with a mean age of 60 years.<br />
Mean troponin I levels increased in the first day after surgery as compared to baseline values<br />
(mean value 5.078± 9.38 ng/ml) and fall until the 7 th day (mean value 0.38± 0.825 ng/ml).<br />
Preoperatively all the values of troponin I were normal. POMI was diagnosed in 5 (3.16 %) patients.<br />
In these patients the mean value of troponin I was 36.3 ng/ml. A significant correlation between<br />
the value of troponin I in first postoperative day and the duration of ECC (r=0.231, p=0.004) was<br />
<strong>de</strong>tected. We found two in<strong>de</strong>pen<strong>de</strong>nt predictors for relative <strong>de</strong>crease of troponin I in the<br />
postoperative period: the need of positive inotropic therapy (p=0.005) and the left ventricular<br />
mass (r= 0.206; p=0.023). No relevant correlations between the values of troponin I and<br />
postoperative complications, mortality, ICU LOS or hospital LOS were found.<br />
Conclusion: Troponin I level increased in all patients after CABG surgery in the first<br />
postoperative day as compared to baseline and fall until the 7 th day. However, the relative<br />
<strong>de</strong>crease on the 7 th postoperative day was smaller in patients on positive inotropic therapy and in<br />
patients with higher left ventricular mass. In our study the values of troponin I were not correlated<br />
with postoperative complications and had no value for risk stratification after CABG surgery.<br />
Role of ROTEM in post cardiac surgery blee<strong>din</strong>g<br />
Daniela Manea, Mihail Luchian, Alina Paunescu, Ioana Marinica,<br />
Anca Pro<strong>de</strong>a, Oana Ghenu, Simona Marin, Daniela Filipescu<br />
Department of Cardiac Anesthesia & Intensive Care<br />
Emergency Institute for Cardiovascular Disease, Bucharest, <strong>Romania</strong><br />
Background: Cardiac surgery still associates a high postoperative blee<strong>din</strong>g risk. This risk is<br />
accompanied by increased morbidity and mortality and it is also closely connected to increased<br />
transfusion <strong>de</strong>mand. We analyzed the utility of thromboelastometry (ROTEM) in the management<br />
of significant postoperative blee<strong>din</strong>g after cardiac surgery in patients with cardiopulmonary<br />
bypass (CPB).<br />
Method: We analyzed ROTEM parameters (EXTEM, INTEM, HEPTEM and FIBTEM) in patients<br />
aged over 18 years, operated on CPB during a 4 month period and having a chest drainage over<br />
400 ml in the first 6 postoperative hours. Demographic data, type of intervention, CPB and aortic<br />
cross-clamp duration and minimal temperature on CPB were registered. Haematocrit,<br />
haemoglobin, platelet count, APTT, INR and the level of fibrinogen were measured preoperatively,<br />
at the end of the intervention, in the first 6 postoperative hours, and during the 6-12 postoperative<br />
80
hours. The blood transfusion products (packed red blood cells –PRBC, fresh frozen plasma-FFP and<br />
platelet concentrate-PC) as well as the hemostatic reintervention and complications were also<br />
registered.<br />
Results: There were 7 patients (5 males, 2 females with a mean age of 59±12, 4 years) that<br />
met the proposed criteria. The mean drainage in the first 6 postoperative hours was 907±567 ml<br />
(400-2100) and 1164±505ml (800-2250) during the first 12 postoperative hours. 5 patients were on<br />
aspirin preoperatively and all 7 patients received tranexamic acid (3-6 g) during the intervention.<br />
At least one ROTEM parameter was affected in all 7 patients. The inci<strong>de</strong>nce of hemostatic<br />
reintervention was 42, 8% (3 patients). Following the ROTEM algorithm for coagulation factors and<br />
protamin supplementation we succee<strong>de</strong>d to avoid haemostatic reintervention in 4 patients. The<br />
blood product usage (mean values) during the first 6/12 hours was: PRBC 2, 4±1, 13/4, 14±2, 03<br />
units, FFP 2, 86±2, 73/3, 57±3, 36 units, and PC 0, 57±1, 51/1±2, 6 units. There was an increased<br />
inci<strong>de</strong>nce (28. 6%) of prolonged mechanical ventilation, atrial fibrillation, acute renal failure and<br />
neurologic dysfunction in our study group.<br />
Conclusions: Evaluation of blee<strong>din</strong>g cause post cardiac surgery is difficult. The presence of<br />
coagulation abnormalities do not rule out a surgical source. The use of ROTEM parameters may<br />
differentiate the cause and optimize the management of blee<strong>din</strong>g reducing the number of<br />
reinterventions to control haemostasis after cardiac surgery.<br />
Cristina Ciochină, Mihai Luchian, Oana Ghenu,<br />
Ioana Marinică, Alina Păunescu, Simona Marin,<br />
Anca Pro<strong>de</strong>a, Ovidiu Chioncel, Luminiţa Iliuţă,<br />
Oana Mihăilescu, Daniela Filipescu (Bucureşti)<br />
Suciu Horaţiu<br />
IUBCVT, Tg. Mureş<br />
Andrei Iosifescu, Lucian Dorobantu, Sorin<br />
Maximeasa, Traian Anca, Cristian Boroş, Vlad<br />
Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Bucureşti<br />
Andrei Iosifescu, Alexandru Cornea, Traian Anca,<br />
Ioana Ghiorghiu, Platon Pavel, Ioana Marinică,<br />
Vlad Iliescu<br />
Institutul <strong>de</strong> Boli Cardiovasculare “ Prof Dr. C.C.Iliescu”<br />
Bucureşti<br />
Ce aduce nou ghidul <strong>de</strong> resuscitare în chirurgia<br />
cardiacă?<br />
SALA Ruby<br />
Grupul <strong>de</strong> lucrări « CONGENITALI »<br />
Sesiunea XVI<br />
Actualităţi în chirurgia pediatrică<br />
Update in pediatric cardiac surgery<br />
Tratamentul chirurgical al afecţiunilor congenitale ale<br />
căii <strong>de</strong> ieşire <strong>din</strong> ventriculul stâng<br />
Stenoza infundibulară pulmonară extrinsecă<br />
secundară pericarditei constrictive la copil–<br />
prezentarea unui caz tratat chirurgical<br />
Baloon angioplasty of pulmonary artery valve<br />
Ilona Cucu, Vasile Sirbu, Liviu Maniuc, Oleg Repin<br />
Institute of Cardiology, Republic of Moldova<br />
The aim of the study: Evaluation of immediate and long-term results after the valve balloon<br />
angioplasty in isolated pulmonary artery stenosis.<br />
Material and methods: During the period 1998-2009 years were ma<strong>de</strong> 187 balloon<br />
angioplasties of pulmonary artery valve. Average age of patients was 5,8 +/- 2,6 years (0-18),<br />
children up to one year -22 patients (11,7%), above 18 years - 59 patients (31,5%). Out of them 25<br />
patients had systolic gradient between pulmonary artery and right ventricle 50 mmHg; in 139<br />
patients (74,6%) gradient VD / AP between 50-100mmHg; in 23 patients the gradient RV/PA><br />
100mmHg.<br />
81
Results: Analysis of pulmonary artery valve balloon angioplasty revealed that satisfactory<br />
results with a low restenosis rate which were seen in group of patients from 1 to 5 years; in group of<br />
patients with PG VD/PA <br />
100mmHg prior to procedure 112 + / -7,7, after – 48,3 + / -8,6.<br />
The patients group from 5-18 years < 50mmHg before the procedure had 51,5 + / -2,8, after<br />
– 6,7 +/-3,5; in the group with GP VD/PA from 50-100mmHg before the intervention was 89,2 +/-7,3,<br />
after – 23,3 +/-3,4; in group GP VD/AP > 100mmHg prior the procedure 125,8 +/-5,7, after – 52,3 +/-<br />
8,6.<br />
Complications were <strong>de</strong>termined in 31 patients: papillary muscle rupture – 1 pacient, 2<br />
patients – ileofemoral thrombosis, 19 patients - transient heart rhythm disor<strong>de</strong>rs, in 8 patients -<br />
allergic reaction. There was a fatal case of acute heart failure in the period immediately after<br />
surgery in patient 3 months diagnosed with severe mitral valve stenosis with PA 154mmHg<br />
gradient.<br />
Long-term results were studied in 112 patients (59,9%) from 6 months to 9 years. Repeated<br />
angioplasty was performed in 20 patients; 3 patients were operated due to RV outflow tract<br />
stenosis and 3 patients - due to valve ring hypoplazy.<br />
Conclusion: Analysis of data received <strong>de</strong>monstrated that balloon angioplasty of PA valve<br />
is a less traumatic and effective method to treat PA valve isolated stenosis. Improving the material<br />
engineering, the intervention technique allows reducing to a minimum of complications during<br />
intervention and obtaining acceptable results.<br />
Outcomes of the complex arterial switch operation<br />
Serban Stoica 1, Esther Carpenter 2, Eduardo da Cruz 2, James Todd 2, Thomas Fagan 2, Max Mitchell 2,<br />
David Campbell 2, Dunbar Ivy 2, Francois Lacour-Gayet 3<br />
1 - Bristol Royal Children's Hospital, UK<br />
2 - Denver Children's Hospital, USA<br />
3 - Montefiore Hospital, New York, USA<br />
Purpose: Morbidity and mortality comparison of simple (sASO) and complex arterial switch<br />
operations (cASO).<br />
Methods: 93 consecutive patients un<strong>de</strong>rgoing arterial switches between 2003-2009 were<br />
analyzed. Of these 45 had sASO (48%) and 48 (52%) cASO, <strong>de</strong>fined as one or several of the<br />
following: weight
Surgical correction of Transposition of Great Arteries – experience of 80 cases<br />
Conf.dr. Suciu H., dr. Paşcanu S., dr. Matei M., dr. Roxana Toma,<br />
dr. Anca Sglimbea, dr. Opriş C., prof. dr. Deac R.,<br />
IUBCVT Targu Mures<br />
Introduction: Surgery for transposition of great vessels (TGA) has <strong>de</strong>veloped spectacularly<br />
in recent <strong>de</strong>ca<strong>de</strong>s, the”arterial switch” representing along with the”Fontan circulation” two of the<br />
great therapeutic achievements in congenital surgery. Recent years have contributed to<br />
overcoming the last obstacles in arterial switch procedure. Today's”arterial switch” solution should<br />
represent the standard for patients with transposition of great vessels worldwi<strong>de</strong>.<br />
Purpose: presentation of personal experience (one center, one surgeon) and<br />
periprocedural surgical management of TGA in a total of 80 cases operated on between 2004-<br />
<strong>2010</strong> in the Clinic of Cardiovascular Surgery Adults and Children II, IUBCVT, Targu - Mures.<br />
Material / Method: The study group inclu<strong>de</strong>d 80 newborns and infants, aged 7 days – 3<br />
months, with TGA, operated upon in the past five years in our unit. The present study concerned:<br />
the geographic origin, gen<strong>de</strong>r, age, time of diagnosis, associated perinatal pathology, type of<br />
TGA, associated pathology, coronary anatomy, clinical and biological status at time of admission<br />
in our clinic, the need for other medical / interventional procedures, preoperative complications,<br />
age at the time of surgery, surgical technique, bypass time and ischemia time, number of days of<br />
intubation, inotropic requirements, number of days in intensive care, postoperative complications.<br />
Results: Mortality was reduced alongsi<strong>de</strong> with the learning curve. Unlike other centers<br />
abroad, the number of patients in critical condition (due to late diagnosis and inappropriate<br />
management before admission to our center) is substantially larger, requiring a bigger number of<br />
days spent in the ICU facilities. Coronary anatomy is a risk factor only in the case of single coronary<br />
artery. The techniques for correction of the the mismatch at the level of great arteries were<br />
nee<strong>de</strong>d in 7 cases. Other surgical technical difficulties or palliative techniques (left ventricular<br />
reconditioning) were nee<strong>de</strong>d in 2 cases. Time of CPB and the time of ischemia compared with<br />
other centers abroad was with 15-20% longer in our group. The number of days of mechanical<br />
ventilation and intensive care was bigger, especially in connection with postoperative infectious<br />
complications.<br />
Conclusions: ”Arterial switch” for TGA correction represent the optimal therapy, carried out<br />
with good results, after reaching the plateau of learning curve, regardless of anatomical features<br />
of the lesion. Short-term results are <strong>de</strong>termined by the child's condition before surgery and<br />
postoperative complications, requiring a more effective collaboration with cardiologists and<br />
paediatricians in the neonatal centers of the teritory.<br />
Corectia chirurgicală a Transpoziţiei marilor vase - experienţa a 80 <strong>de</strong> cazuri<br />
Introducere: Chirurgia în transpoziţia <strong>de</strong> mari vase (TVM) a evoluat spectaculos în ultimele<br />
<strong>de</strong>cenii, switch-ul arterial reprezentând, alături <strong>de</strong> circulaţia Fontan una <strong>din</strong> marile realizări<br />
terapeutice în chirurgia congenitalilor. Ultimii ani au contribuit la <strong>de</strong>păşirea ultimelor dificultăţi în<br />
efectuarea switch-ului arterial cum sunt anomaliile <strong>de</strong> artere coronare. etc. Actualmente ”switchul<br />
arterial” ar trebui să reprezinte soluţia <strong>de</strong> elecţie pentru pacientul cu transpoziţie <strong>de</strong> mari vase<br />
oriun<strong>de</strong> în lume.<br />
Obiectiv: prezentarea experienţei personale (un centru, un operator) în managementul<br />
periprocedural şi chirugical al transpoziţiei <strong>de</strong> mari vase la un număr <strong>de</strong> 80 <strong>de</strong> cazuri, operate în<br />
perioada 2004-<strong>2010</strong> la nivelul Clinicii Chirurgie Cardiovasculara II Adulti şi Copii, IUBCVT, Târgu<br />
Mureş.<br />
Material / Metoda: Lotul <strong>de</strong> studiu inclu<strong>de</strong> 80 <strong>de</strong> nou născuţi şi sugari, cu vârste cuprinse<br />
între 7 zile şi 3 luni, operaţi pentru TVM in ultimii 5 ani în clinica noastră. La aceştia s-a urmărit: zona<br />
<strong>de</strong> provenienţă, sexul, vârsta, momentul diagnosticului, patologia perinatală asociată, tipul <strong>de</strong><br />
TVM, leziunile asociate, anatomia coronarelor, statusul clinic şi biologic la preluarea pacientului în<br />
unitatea noastră, necesitatea efectuării altor manevre medicale / interventionale, complicaţii<br />
preoperatorii, vârsta la momentul operaţiei, tehnica operatorie, timpul <strong>de</strong> by-pass cardiopulmonar,<br />
timpul <strong>de</strong> ischemie, numărul <strong>de</strong> zile <strong>de</strong> intubaţie oro-traheală, necesarul <strong>de</strong> inotropice,<br />
numărul <strong>de</strong> zile <strong>de</strong> terapie intensiva, complicaţii postoperatorii.<br />
Rezultate: Mortalitatea operatorie s-a redus paralel cu curba <strong>de</strong> învăţare, încadrându-se în<br />
prezent în media europeană. Spre <strong>de</strong>osebire <strong>de</strong> alte centre <strong>din</strong> străinătate, numărul <strong>de</strong> pacienţi<br />
83
<strong>de</strong>compensaţi la preluare (datorită diagnosticării tardive sau a managementului impropriu<br />
anterior internării în centrul nostru) este substanţial mai mare, necesitând într-un număr mai mare<br />
<strong>de</strong> cazuri îngrijiri <strong>de</strong> terapie intensivă. Anatomia coronarelor reprezintă un risc doar în cazul unei<br />
coronarei unice. Tehnici <strong>de</strong> compensare a mismatch-ului vaselor mari au fost necesare în 7 cazuri.<br />
Tehnici paleative sau <strong>de</strong> recondiţionare ventriculară au fost necesare în 2 cazuri. Timpul <strong>de</strong><br />
circulatie extracoropreală şi timpul <strong>de</strong> ischemie comparativ cu alte centre <strong>din</strong> străinătate a fost<br />
cu 15-20% mai prelungit. Numărul <strong>de</strong> zile <strong>de</strong> ventilaţie mecanică şi necesarul <strong>de</strong> zile <strong>de</strong> terapie<br />
intensivă este mai lung în cazul prezenţei complicaţiilor postoperatorii infecţioase şi a<br />
chilotoracelui.<br />
Concluzii: ”Swich-ul arterial” in TVM este terapia optimă, realizabilă cu rezultate bune,<br />
după atingerea platoului curbei <strong>de</strong> învăţare, indiferent <strong>de</strong> particularităţile anatomice ale leziunii.<br />
Rezultatele pe termen scurt sunt condiţionate <strong>de</strong> starea copilului anterior intervenţiei şi <strong>de</strong><br />
complicaţiile postoperatorii, necesitând o colaborare mult mai eficientă cu centrele <strong>de</strong><br />
neonatologie şi cardiologii pediatrii <strong>din</strong> teritoriu.<br />
Anomalous origin of left coronary artery from the pulmonary artery<br />
in association with mitral regurgitation<br />
Lucian Stoica, Eugen Bitere, Dumitrita-Alina Gafencu, Laurentiu Gafencu, Grigore Tinică<br />
Cardiovascular Surgery Clinic, Cardiovascular Diseases Institute “Prof. Dr. George I. M.<br />
Georgescu”, Iaşi<br />
Anomalous origin of left coronary artery from the pulmonary artery is a rare malformation,<br />
first <strong>de</strong>scribed by Brooks in 1885, with an inci<strong>de</strong>nce rate of 1 in 300 000 newborns. The<br />
consequences are myocardial ischemia, myocardial infarction, congestive heart failure, mitral<br />
insufficiency (ischemic and/or ventricular dilatation) and <strong>de</strong>ath in early ages if not treated.<br />
Although there is consensus regar<strong>din</strong>g the surgical techniques of left coronary artery<br />
reimplantation, there are different opinions about the surgical correction of the mitral<br />
regurgitation at the time of the initial operation. We present you two clinical cases diagnosticated<br />
and treated at IBCV “Prof. Dr. George I. M. Georgescu” from Iasi. These patients had gra<strong>de</strong> II<br />
mitral insufficiency, which was not surgically corrected (on purpose). The later echocardiographic<br />
studies showed mitral regurgitation regression, improved contractility and <strong>de</strong>creased left<br />
ventricular volume.<br />
Case 1: 21 year old female, with low effort tolerance, was diagnose initially with<br />
myocardial fibroelastosis. The further echocardiographic study revealed the presence of dilatative<br />
cardiomyopathy and gra<strong>de</strong> II mitral insufficiency (ischaemic mechanism). The imagistic exams<br />
performed at IBCV “Prof. Dr. George I. M. Georgescu” Iasi showed the anomalous origin of left<br />
coronary artery from the pulmonary artery. The operative technique was the direct reimplantation<br />
of the anomalous coronary artery onto aorta and the closure of the pulmonary artery with an<br />
autologous pericardium patch. The postoperative evolution was free of complications and the<br />
patient went home after 8 days. After one year the clinical and echocardiographic control shows<br />
very good evolution, with mitral insufficiency gra<strong>de</strong> regression and significant increase of effort<br />
tolerance.<br />
Case 2: 2 year old male with dyspnea and frequent respiratory infections was evaluated<br />
(echocardiography and coronarography) at IBCV “Prof. Dr. George I. M. Georgescu” from Iasi<br />
and the diagnoses was anomalous origin of left coronary artery from the pulmonary artery. The<br />
surgical technique was the translocation of the left main from the pulmonary artery to the aorta.<br />
The postoperative evolution was very good and the patient went home after 12 days. In a time<br />
period of three years the clinical controls showed a good evolution, with increase effort tolerance<br />
and normal statural and pon<strong>de</strong>ral <strong>de</strong>velopment.<br />
Conclusion: After successful revascularization, the late results are good, left ventricular<br />
function recovers and the mitral regurgitation <strong>de</strong>creases even if the disease is diagnose in the<br />
adult period.<br />
Keywords: anomalous origin of left coronary artery from the pulmonary artery, coronary<br />
anomaly, mitral insufficiency<br />
Originea anormală a arterei coronare stângi <strong>din</strong> artera pulmonară asociată cu regurgitare mitrală<br />
Originea anormală a arterei coronare stângi <strong>din</strong> artera pulmonară este o malformaţie<br />
rară, <strong>de</strong>scrisă prima dată <strong>de</strong> Brooks în 1885, cu o inci<strong>de</strong>nţă <strong>de</strong> 1 la 300000 <strong>de</strong> naşteri vii. Poate<br />
84
cauza ischemie miocardică, infarct, insuficienţă cardiacă congestivă, insuficienţă mitrală<br />
ischemică şi/sau prin dilatare <strong>de</strong> inel mitral şi <strong>de</strong>ces la vârste mici.<br />
Dacă pentru tehnicile <strong>de</strong> reimplantare a arterei coronare stângi în aortă există un<br />
consens, în ceea ce priveşte corecţia regurgitării mitrale opiniile sunt diferite. Prezentăm două<br />
cazuri diagnosticate şi operate la IBCV "Prof. Dr. George I.M. Georgescu" Iaşi care aveau<br />
regurgitare mitrală gradul II şi la care <strong>de</strong>liberat nu s-a realizat un gest chirurgical pe valva mitrală.<br />
Controalele ecocardiografice ulterioare au arătat regresia semnificativă a insuficienţei mitrale,<br />
ameliorarea contractilităţii şi reducerea volumului ventricular stâng.<br />
Caz 1: Pacientă în varsta <strong>de</strong> 21 ani, simptomatică prin toleranţă scăzută la efort, a fost<br />
diagnosticată iniţial cu fibroelastoză miocardică, ulterior conturându-se ecografic aspectul <strong>de</strong><br />
cardiomiopatie dilatativa şi insuficienţă mitrală gradul II (prin mecanism ischemic). Este explorată<br />
imagistic la IBCV "Prof. Dr. George I.M. Georgescu" Iaşi, evi<strong>de</strong>nţiindu-se originea trunchiului<br />
principal coronar stâng în artera pulmonară. S-a practicat reimplantarea arterei coronare stângi<br />
la nivelul aortei si reconstrucţia arterei pulmonare cu petec <strong>de</strong> pericard autolog. Evoluţia<br />
postoperatorie a fost favorabilă, iar pacienta a fost externată la 8 zile postoperator. Controlul<br />
clinic şi ecografic la un an evi<strong>de</strong>nţiază o evoluţie favorabilă cu regresia insuficienţei mitrale şi<br />
creşterea semnificativă a capacităţii <strong>de</strong> efort.<br />
Caz 2: Pacient în vârstă <strong>de</strong> 2 ani, cu dispnee la eforturi mici şi infecţii respiratorii repetate,<br />
este investigat imagistic (ecocardiografic şi coronarografic) la IBCV "Prof. Dr. George I.M.<br />
Georgescu" Iaşi şi se stabileşte diagnosticul <strong>de</strong> origine anormală a arterei coronare stângi <strong>din</strong><br />
artera pulmonară. Se practică translocarea trunchiului arterei coronare stângi <strong>din</strong> artera<br />
pulmonară în aortă iar pacientul este externat la 12 zile postoperator cu stare generală bună.<br />
Controalele clinice periodice efectuate timp <strong>de</strong> 3 ani arată o evoluţie favorabilă cu toleranţă<br />
bună la efort şi <strong>de</strong>zvoltare staturo-pon<strong>de</strong>rală normală.<br />
Concluzii: Reimplantarea arterei coronare stângi în aortă conduce la normalizarea<br />
perfuziei miocardice şi, pe termen lung, la ameliorarea contractilităţii ventricolului stâng şi regresia<br />
insuficienţei mitrale, chiar la pacienţi diagnosticaţi la vârsta adultă.<br />
Cuvinte cheie: origine anormală a arterei coronare stângi în artera pulmonară, anomalie<br />
coronariană, insuficienţă mitrală<br />
Chira Manuel, Simona Opriţa<br />
Institutul Inimii “ Niculae Stăncioiu” Cluj<br />
Cecilia Lazea*, Rodica Manasia,* Simona<br />
Opriţa**, Mircea Bârsan**, Svetlana Encica**<br />
* Clinica Pediatrie I “Axente Iancu” Cluj<br />
**Institutul Inimii “ Niculae Stăncioiu” Cluj<br />
Angela Butnariu, Daniela Iacob<br />
Clinica Pediatrie III, Universitatea <strong>de</strong> Medicină şi<br />
Farmacie “Iuliu Haţieganu” Cluj-Napoca<br />
Mariana Andreica*, Simona Cainap*, Andreea<br />
Răchişan*, Simona Opriţa**, Cecilia Lazea**,<br />
Manuel Chira**, Nicolae Miu*<br />
* Clinica Pediatrie II Cluj-Napoca<br />
** Institutul Inimii “Niculae Stăcioiu” Cluj-Napoca<br />
*** Clinica Pediatrie I Cluj-Napoca<br />
Popa Cherecheanu Matei, Goleanu Viorel,<br />
Butusina Marian, Lazar Ovidiu, Lazar Mihaela,<br />
Mihalcescu Daniel, Creţu Magdalena, Radu<br />
Mădălina, Tănăsescu Dragoş.<br />
Spitalul Clinic <strong>de</strong> Urgenţă Militar, Bucureşti<br />
Rodica Manasia, Cecilia Lazea<br />
Clinica Pediatrie I “Axente Iancu” Cluj<br />
Sesiunea XVII<br />
Intervenţii chirurgicale vs cardiologie intervenţională în<br />
tratamentul malformaţiilor chirurgicale"<br />
Tumori cardiace în practica cardiacă<br />
Aspecte pediatrice ale îngrijirii perioperatorii la copilul<br />
mic cu malformaţie cardiacă congenitală<br />
Abordarea clinică şi terapeutică a malformaţiilor<br />
cardiace congenitale – cazuistica Clinicii Pediatrie II<br />
Cluj-Napoca<br />
Chilotorax post cură chirurgicală a <strong>de</strong>fectului septal<br />
interatrial<br />
Aspecte <strong>din</strong> viaţa copilului cardiac<br />
85
As. Aurica Farcane, Prof Dr. Petru Deutsch.<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
As Daniela Demea, Prof. Dr. Marian Gaspar<br />
Institutul <strong>de</strong> Boli Cardiovasculare Timişoara<br />
SALA Ruby<br />
Grupul <strong>de</strong> lucrări « NURSING »<br />
Concentratul trombocitar obţinut prin afereza,<br />
tehnologie<br />
transfuzională<br />
<strong>de</strong> interes pentru hematologia<br />
Rolul bancii <strong>de</strong> celule si tesuturi in cresterea<br />
eficientizarii transplantului<br />
Transpoziţia <strong>de</strong> vase mari - indicaţii şi risc operator<br />
Georgeta Teuca<br />
- Anestezie şi Terapie Intensivă, Institutul Inimii “ N.Stăncioiu”, Cluj- Napoca<br />
Prezentarea <strong>de</strong> faţă intitulată ”Transpoziţia <strong>de</strong> vase mari - indicaţii şi risc operator”<br />
cuprin<strong>de</strong> în ansamblu totalitatea intervenţiilor/ manoperelor medicale care se efectuează în<br />
clinica <strong>de</strong> chirurgie cardiovasculară la pacienţii internaţi cu această patologie.<br />
Chirurgia cardiacă a bolilor congenitale are o <strong>din</strong>amică <strong>de</strong> <strong>de</strong>zvoltare şi perfec ionare<br />
ieşită <strong>din</strong> comun. Dacă înainte operaţiile în bolile congenitale se efectuau la vârstă înaintată, 10-<br />
15 ani, acestea se efectuează la copilul mic, preşcolar, la nou născuţi, perinatal şi chiar prenatal<br />
intrauterin.<br />
Aproximativ 3% <strong>din</strong>tre copii se nasc cu diferite malformaţii congenitale, anomaliile<br />
cardiace congenitale situându-se pe primul loc cu o pon<strong>de</strong>re <strong>de</strong> 8: 1000 <strong>de</strong> nou născuţi vii.<br />
Până în ultimele <strong>de</strong>ca<strong>de</strong> se consi<strong>de</strong>ra că 8% <strong>din</strong>tre <strong>de</strong>fectele cardiace congenitale se<br />
datorează aberaţiilor cromozomiale, 2% sunt consecutive teratogenilor <strong>de</strong> mediu ce acţionează<br />
în perioada cardiogenezei produsului <strong>de</strong> concepţie, iar restul <strong>de</strong> 90% sunt multifactoriale.<br />
Transpozi ia <strong>de</strong> vase mari este un <strong>de</strong>fect congenital cianogen, în care ambele vase mari<br />
pornesc <strong>din</strong> ventriculul opus. Dată fiind amploarea malforma iei cardiace i complicaţiile pe<br />
care le poate produce în cazul nerezolvării în primele zile <strong>de</strong> viaţă, se impune intervenţia <strong>de</strong><br />
urgenţă încă <strong>din</strong> primele zile după naştere.<br />
În cadrul prezentei lucrări sunt <strong>de</strong>scrise aspectele fiziologice ale cordului normal la nou<br />
născut, malformaţiile asociate ce pot însoţi transpozi ia <strong>de</strong> vase mari, precum şi intervenţiile pre,<br />
intra operatorii.<br />
Aspectele supuse cercetării - studiul pe care l-am realizat este unul retrospectiv,<br />
(1.01.2005- 1.01.2009), vizând cazurile operate în <strong>de</strong>cursul a 4 ani - prezintă date statistice<br />
referitoare atât la vârsta mamei, patologii asociate în <strong>de</strong>cursul sarcinii, Rh-ul mamei, patologii<br />
asociate ale copilului, precum i date referitoare la durata spitalizării şi manopere efectuate<br />
acestuia.<br />
Un rol important în acordarea îngrijirilor medicale acestor micu i pacienţi revine<br />
asistentelor medicale <strong>de</strong> pe Terapie Intensivă. Cunoaşterea patologiei, evoluţiei postoperatorii, a<br />
posibilelor complicaţii, <strong>de</strong>celarea lor, anunţarea <strong>din</strong> timp a medicului terapist, contribuie la<br />
asigurarea calităţii îngrijirilor acordate acestei categorii <strong>de</strong> pacienţi.<br />
As. Alina Ganea<br />
Bloc operator<br />
Rezultate imediate în protezarea valvei aortice pentru<br />
stenoză.<br />
Protocol <strong>de</strong> reducere necesarului <strong>de</strong> transfuzii alogene in chirurgie cardiaca<br />
Protocol of reductions required allogenic transfusion in Surgery Cardiac<br />
as. Cătinean Mihaela Carmen, dr. Vlad Horea Ioan<br />
Institutul Inimii <strong>de</strong> urgen ă pentru boli cardiovasculare” Nicolae Stăncioiu” Cluj-Napoca, Clinca<br />
<strong>de</strong> anestezie i terapie intensivă<br />
Heart Institute emergency cardiovascular disease "Nicholas Stancioiu"<br />
Cluj-Napoca, Clinca of anesthesia and intensive care<br />
Obiective: Scopul acestui protocol este <strong>de</strong> a îmbunătăţi gestionarea perioperatorie a<br />
transfuziei <strong>de</strong> sânge şi <strong>de</strong> a reduce riscul apariţiei efectelor adverse asociate cu transfuzia,<br />
hemoragia sau cu anemia.<br />
86
Metoda: S-a efectuat un studiu experimental i comparativ între două loturi <strong>de</strong> pacien i<br />
opera i pe cord: Lotul I –lotul experimental si Lotul II – lotul <strong>de</strong> control<br />
Rezultate: Rezultatele au evi<strong>de</strong>ntiat reducerea necesarului transfuzional in Lotul I.<br />
Concluzii: Interven iile chirurgicale cardiace cu bypass cardio-pulmonar se pot face fără<br />
administrare <strong>de</strong> sânge alogen, ca urmare a elaborarii acestui protocol.<br />
Objectives: The purpose of this protocol is to improve the management of perioperative<br />
blood transfusion and reduce the risk of adverse effects associated with transfusions, blee<strong>din</strong>g or<br />
anemia.<br />
Method: An experimental study was performed and compared between two groups of<br />
patients operated on heart: Lot I-control group and Lot II-experimental group.<br />
Results: The results have shown to reduce transfusion requirements in group I.<br />
Conclusions: cardiac surgery with cardio-pulmonary bypass can be done without<br />
allogeneic blood administration, following the elaboration of this Protocol.<br />
As. Szabo Noemi, dr. A. Molnar<br />
Institutul Inimii <strong>de</strong> urgenţă pentru boli cardiovasculare”<br />
Nicolae Stăncioiu” Cluj-Napoca, Clinca <strong>de</strong> anestezie şi<br />
terapie intensivă<br />
Chirurgia coronariană off pump, avantaje şi<br />
<strong>de</strong>zavantaje.<br />
Management of Global Cardiovascular Risk<br />
- role of sanitary education and active monitoring-<br />
Dana Marginean<br />
“Niculae Stancioiu” Heart Institute, Cluj-Napoca<br />
The mo<strong>de</strong>rn concept of therapy for a patient with heart disor<strong>de</strong>rs implies, besi<strong>de</strong>s the<br />
specific treatment of the disease, non-pharmacological and pharmacological measures applied<br />
in the purpose of minimizing the global cardiovascular risk.<br />
In this paper we monitored: 1. The evaluation of the role of the general nurse in changing lifestyle<br />
and the modification of some risk factors, 2. The assessment of the impact of correcting the<br />
modifiable risk factors and 3. The possibility of improving the compliance to treatment of patients.<br />
The material of study was performed on 870 hospitalized patients in the first trimester of<br />
2009 at the Heart Institute, patients who presented three or more traditional risk factors of which at<br />
least one factor belonging to the category of modifiable factors. There were two groups, of 50<br />
patients each, <strong>de</strong>limited: Group A <strong>de</strong>signed to the educative active intervention and Group B,<br />
the witness group. Each patient signed a written consent and was monitored on the basis of some<br />
<strong>de</strong>dicated questionnaires. Active medical education was ma<strong>de</strong> by using specific information<br />
materials for each risk factor.<br />
The results obtained after one year of active education and monitoring revealed the<br />
following: A group – quit smoking in 66% cases, more than 1/3 patients lost weight, 25% reaching a<br />
normal BMI, the dislipi<strong>de</strong>my got normal values for 16 patients out of 28, glicolized hemoglobin<br />
reached normal values in 75% of cases, sport became a regular habit for 56% of patients and salt<br />
consumption <strong>de</strong>creased in a controlled manner at 64% of patients. Global compilation to<br />
treatment maintained in 84% of cases and after one year there was registered a reduction of<br />
specific medication intake with 30% or at least a reduction of the intake dose with 20%. In the B<br />
group (the witness group) none of the patients quit smoking, weight loss was registered in 10% of<br />
cases, the dislipi<strong>de</strong>my and glicated hemoglobin got normal values for 20% of the patients,<br />
respectively for 27% of patients, while only 6% ma<strong>de</strong> sport and salt consumption relative reduction<br />
was registered in 30% of the patients. The compliance to treatment was significantly reduced in<br />
32% of cases and the reduction of medication or of the dose was insignificant (4% and 8%).<br />
The survey attests the importance and effectiveness of active medical education taught<br />
by the medical nurse where the amendment of the risk factors is concerned, with indubitable<br />
impact on cardiovascular morbid-mortality on medium and long term.<br />
87