Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
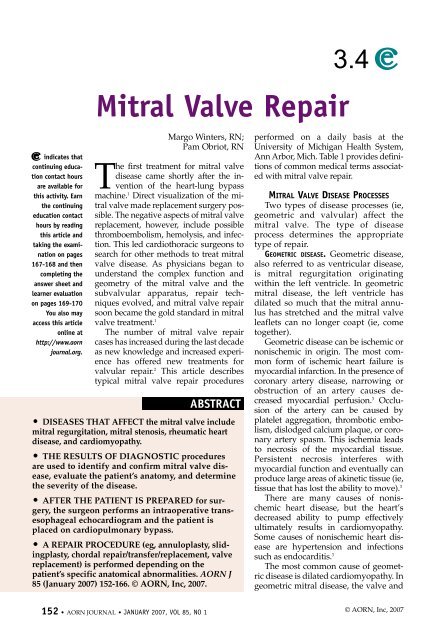
Winters — Obriot JANUARY 2007, VOL 85, NO 1TABLE 1Common Medical Terms Associated with <strong>Mitral</strong> <strong>Valve</strong> <strong>Repair</strong>AnnulusA ring-like structure; a fibrous band of tissue whichserves as the attachment point for the leafletsAnnuloplastySurgical repair of a deformed annulus surroundinga diseased mitral valveBicuspid valveA valve consisting of two leaflets (eg, the mitralvalve)CoaptationThe proper joining or fitting together of two surfaces(eg, mitral valve leaflets)Geometric mitral diseaseA dysfunction of the mitral valve related to dilationof the left ventricleLeft ventricular outflow tractA pathway from which blood exits the left ventricleand passes through the aortic valve<strong>Mitral</strong> regurgitationA backward flowing of blood into the left atrium ofthe heart caused by an incompetent mitral valve<strong>Mitral</strong> stenosisObstruction to the flow of blood through themitral valve, usually caused by narrowing of thevalve orificeSubvalvular apparatusChordae tendineae and papillary muscles withinthe left ventricle that contribute to the geometryand function of the mitral valveTrigoneThree angled section on the ends of the fibrousregion between the aortic and mitral valvesValvular mitral disease<strong>Valve</strong> dysfunction related to issues of the valve orsubvalvular apparatusZone of coaptationRough surface of mitral valve leaflets that jointogether during left ventricular systolesubvalvular apparatus are all normal.The problem is within the ventricle,which has become dilated to the extentthat the normal function of the valve isdisrupted.VALVULAR DISEASE. Valvular mitral diseaseis a process in which the leafletsand/or the annulus have become calcifiedand stiff or fused. In addition to calcification,valvular disease also mayinclude chordal shortening, which maylead to mitral stenosis or regurgitation.In the United States, valvular diseasemost commonly is caused by rheumaticendocarditis. 4 Whatever the etiology,most patients will have some degree ofdilation in the mitral annulus that mustbe repaired. 5MITRAL VALVE ANATOMY AND PHYSIOLOGYThe bicuspid (ie, two leaflet) mitralvalve is located between the left ventricleand left atrium. The valvular complexconsists of the annulus, leaflets,chordae tendineae, and papillary muscles(Figure 1), and in a sense, the leftventricle is the mitral valve. The annulus,a fibrous band of tissue from whichthe leaflets originate, is considered the“hinge line” of the valve leaflets. 6Continuing out from the annulus, thetwo leaflets (ie, anterior and posterior)are pale yellow, thin, fibroelastic membraneswhose anterior surfaces are relativelysmooth. The posterior or ventricularsurfaces are slightly irregularbecause of the attachments to the chordaetendineae.The anterior leaflet is also known asthe anteromedial, septal, or aorticleaflet. 4 The posterior leaflet, alsoknown as the mural leaflet, is furtherdivided into three cusps commonlyknown as P1, P2, and P3. The three posteriorcusps do not have separate functions;they have been named purely forease of describing mitral valve anatomyand locations of regurgitation jets (ie,flashes of backward blood flow).The chordae tendineae are attachedto the inferior surface of the leaflets.These white, cord-like tendons act onlyas guides to assist in the coaptation ofthe two leaflets. The chordae tendineae<strong>AORN</strong> JOURNAL • 153
JANUARY 2007, VOL 85, NO 1Winters — ObriotA transesophagealechocardiogramis a usefulintraoperativetool to moreaccuratelydetermine valveanatomy, annularsize, and thedegree of mitralvalve diseaseand assess for aregurgitant jet.CARDIAC CATHETERIZATION. In mitral valvedisease, cardiac catheterization is used toconfirm the diagnosis, assess ventricularfunction, discover other cardiac lesions,and evaluate coronary anatomy. <strong>Mitral</strong>regurgitation is confirmed by left ventriculographyduring cardiac catheterization.With the patient underlight sedation, a cardiologistinserts a catheterthrough the femoral arteryand injects an x-ray contrastagent into the chamber.Fluoroscopy is usedto document the dye flowas it regurgitates into theleft atrium.TRANSTHORACICECHOCARDIO-GRAM. With acute mitralregurgitation, a surfaceechocardiogram can detectabnormalities attributed toa ruptured chordae papillarymuscle or perforatedvalve leaflet. The goal oftransthoracic echocardiogramis to identify thedegree of regurgitationand valvular abnormality.5 Furthermore, additionalinformation on leftatrial enlargement, rightventricular enlargement,and left ventricular dimensionscan be obtained froman echocardiogram.TRANSESOPHAGEAL ECHOCARDIOGRAM (TEE). Apreoperative TEE allows anatomy to bedefined, assesses the degree of mitralregurgitation, and measures left ventricularfunction. The direction of themitral regurgitation jet seen on a TEEcan identify which leaflet is flailing orprolapsing. An anteriorly directed jetindicates a posterior leaflet prolapse orflail; whereas a posteriorly directed jetindicates an anterior leaflet prolapse orflail. 1 A centrally directed jet may indicateannular dilation.Intraoperatively, the TEE is a usefultool to more accurately• determine valve anatomy,• assess the degree of the mitral valvedisease,• assess the degree of regurgitation,• evaluate left ventricular function,• assess annular size and degree ofenlargement, and• assess for a regurgitant jet.With the patient under anesthesia, a TEEprobe is placed in the patient’s esophagusso that the probe lies behind theheart. The probe will remain in placethroughout surgery. After the surgicalrepair has been performed, the surgeonwill clamp the cardiopulmonary bypass(CPB) cannulas, fill the heart, and checkthe repair using a TEE. Based on thisexamination, the surgeon will decide ifthe repair is adequate. If the surgeondecides that additional repairs are needed,CPB will be reinitiated.PREOPERATIVE PHASE OF SURGERYIn the preoperative holding room,the circulating nurse assesses thepatient and verifies the patient’s identity.Before any narcotics are administered,the nurse confirms the proposedprocedure with the patient and his orher family members, cross checkingthe procedure with the surgical consentand OR schedule, and resolvingany discrepancies with the surgeonbefore the patient is taken to the OR.The nurse performs an examination toassess the patient’s physical health status,emphasizing identification of cardiovascularrisk factors, such as height,weight, presence of hypertension ordiabetes, and use of alcohol or illicitdrugs. He or she further identifies thepatient’s relevant medical history (eg,chronic illnesses, injuries, surgeries),and obtains the patient’s medicationhistory, including medication allergies,and any use of• aspirin or other anticoagulants and156 • <strong>AORN</strong> JOURNAL
JANUARY 2007, VOL 85, NO 1Winters — ObriotFigure 3 • Placement of annuloplastyrings.Figure 4 •C-shapedmitral valveimplant.(Figurecourtesy ofEdwardsLifesciences,Irvine, Calif)support service personnel, such as purchasingand inventory stocking personnel,is essential to an efficient system.The circulating nurse also must maintaina stock of suture and be preparedto use additional suture as the procedureprogresses. Surgeon preferencesheets must be maintained and updatedto indicate the preferred annulardevices and suture.After the surgeon has exposed themitral valve apparatus, he or she opensthe patient’s left atrium using Metzenbaumscissors. The incision extends fromdistal end of the intra-atrial groove to justbelow the SVC. At this point, the surgeonplaces the mitral valve retractor using abasket and one malleable blade to exposethe annulus, leaflet tissue, or disruptedchords. He or she uses a Debakey forcepsand nerve hooks to assess the mitralleaflets and chords and to plan the repair.The surgeon looks forredundant leaflet tissueand calcified or disruptedchords.The surgeon uses a #15blade and Jamison scissorsto dissect any leafletsor chords that need repair.The scrub personprepares the disposable suture guidesand the 2-0 braided, coated, polyestervalve suture. The surgeon performs anynecessary• leaflet repairs using a 4-0 braided,coated, polyester suture;• chordal repairs with a 5-0 monofilamentpolypropylene suture; and• chordal replacement with 4-0expanded, polytetrafluroethylene(ePTFE) suture.He or she then places the suture guides ina triangle around the mitral valve retractorand places 2-0 braided coated polyestersutures in the mitral annulus, alternatinggreen- and white-colored suture.The surgeon tags the trigone sutureswith mosquito clamps on which rubbershodshave been placed. When allsutures are placed, the surgeon sizes theannulus by measuring the anteriorleaflet from annulus to the beginning ofthe zone of coaptation. 5Choosing the appropriate annulussize is based on the theory that undersizingis appropriate for mitral regurgitationwhen it is related to left ventricularenlargement. 5 The circulating nurse confirmsthe size and type of implant withthe surgeon and delivers the implant tothe scrub person. In geometric disease, afull ring is used to reduce the size of thedilated annulus. In valvular disease,however, a C-shaped ring is used to reinforcethe repair. The scrub person placesthe annular implant on the holder andhands it to the surgeon. The surgeonplaces individual 2-0 braided, coated,polyester valve sutures in the annularring or band. One-third of the sutures are160 • <strong>AORN</strong> JOURNAL
Winters — Obriot JANUARY 2007, VOL 85, NO 1SIDEBARProtamine SulfateProtamine sulfate, a mixture of simple proteins obtained from the sperm or testes of suitable speciesof fish, usually salmon, is used to neutralize the anticoagulation effect of heparin. It commonly isused in instances of extracorporeal circulation, such as dialysis or cardiac surgery, in which cardiopulmonarybypass is used. Protamine also is used in some insulin preparations to delay the absorption ofinsulin. Protamine does have anticoagulant effects when administered in the absence of heparin. 1Protamine is supplied in a 10 mg/mL solution for injection. The standard adult dosage is 1 mg IV for every100 units of heparin remaining in the patient. Protamine must be administered slowly over a period of 10minutes because administering it too quickly may result in severe hypotension and anaphylactic reaction.Activated clotting time results should be used to monitor the effect of protamine in neutralizing heparin.Adverse reactions to protamine are an antigen-antibody response that can result in cutaneous symptoms(eg, skin flushing, pruritus) or systemic symptoms (eg, hypotension, bradycardia) and anaphylaxis. 2Precautions related to protamine administration should be taken for patients who have been exposed to protaminein the past through use of protamine-containing insulin or previous heparin neutralization duringdialysis or CPB. Caution should be used for patients with a history of fish allergy as they may develop a sensitivityreaction. Men who have had a vasectomy are at increased risk for a protamine reaction. During avasectomy the normal ejaculatory path is occluded and sperm are absorbed systemically. This systemic reabsorptionmay stimulate antibody production. 3Patients who have an increased risk for protamine reaction may be treated before initiation of CPB.Loubser 4 demonstrated that activation of the anaphylactic response mediated by complement activationis inhibited by high-dose methylprednisolone pretreatment before initiation of CPB. Diphenhydramine andranitidine also can be used as pretreatment for patients with increased risk factors for protamine reaction.Health care providers administering protamine must be aware of possible risk factors that could resultin a protamine reaction. Protamine should only be administered by health care providers who are trainedin resuscitation techniques and the treatment of anaphylactic shock. Health care providers should continuallyassess the patient for flushing, nausea, vomiting, dyspnea, hypotension, and bradycardia andthen promptly treat the patient to avoid potential catastrophic outcomes.1. DRUGDEX DRUG EVALUATIONS—Protamine. In: MICROMEDEX(R) Healthcare Series [subscription databaseonline]. Greenwood Village, Colo: Thomson MICROMEDEX; 2005.2. MARTINDALE-The Complete Drug Reference—Protamine. In: MICROMEDEX(R) Healthcare Series [subscriptiondatabase online]. Greenwood Village, Colo: Thomson MICROMEDEX; 2005.3. Porsche R, Brenner ZR. Allergy to protamine sulfate. Heart Lung. 1999;28:418-428.4. Loubser J. Effect of methylprednisolone on complement activation during heparin neutralization. J CardiovascPharmacol. 1997;29:23-27.cross clamp, and the perfusionist beginsto wean the patient off bypass as a cardiologistperforms a postoperative TEEto assess the function of the repairedvalve, comparing it to the preoperativeTEE. The surgeon also uses the TEE todiagnose the presence of systolic anteriormotion and to identify air in the leftventricle. When it is confirmed thatthere is no air in the heart, the surgeonremoves the left ventricular catheterand antegrade cardioplegia cannulae. Ifthe surgeon identifies air in the heart,the anesthesia care provider places thepatient in a slight Trendelenburg position.The surgeon then manuallymanipulates the heart to allow the air toremain in the left ventricle so the air canbe removed by the ventricular catheter.After the patient is completelyweaned off CPB, the surgeon removesthe SVC and IVC cannulae. The surgeonthen inserts two mediastinal chest tubesand secures them with 0-silk sutures.The anesthesia care provider slowlyadministers protamine, at which pointthe circulating nurse and scrub personbegin the sponge, needle, and instrumentcounts. The surgeon is notified ofany discrepancies in the counts.The surgeon removes the aortic cannula,closes the pericardium, and removesthe sternal retractor. He or sheassesses the sternal edges for bleeding<strong>AORN</strong> JOURNAL • 163
JANUARY 2007, VOL 85, NO 1Winters — ObriotThe nurseinitiates use ofthe incentivespirometer withcoughing anddeep breathingand uses bone wax and electrosurgeryas needed to control bleeding. The surgeonthen closes the sternum usingeight #5 wires, and connects the chesttubes to continuous suction via a threechambered,underwaterseal,pleural drainage system.The surgeon closesthe subcutaneous tissueusing 0 and 2-0 monofilament,polydioxanone sutureand closes the skinwith 4-0 monofilament,poliglecaprone suture. Thecirculating nurse, anesthesiacare provider, and surgeontransport the patientdirectly to the thoracicintensive care unit (ICU).immediately after POSTOPERATIVE PHASEAt University Hospital,extubation and Ann Arbor, Mich, postoperativecare is guided by ahelps the patient critical pathway developedfor the uncomplicatedCBP procedure. Thesit on the side ofsurgical day includes directadmission to the tho-the bed withinracic ICU from the OR.six hours of Initial postoperative laboratorytests include a CBCextubation. with platelets; an electrolyte(eg, potassium)count; and an arterialblood gas. An ICU nurse ensures that achest x-ray is performed when the patientis admitted to the ICU. The nurse ensuresthat the patient regains and maintainsnormothermia by using a temperatureregulatingblanket and warmed IV solutionsand obtains the patient’s vital signs,including assessment of pain• every 15 minutes until rewarming iscomplete (ie, to 37° C [98.6° F]) andthen• every four hours until dischargedfrom the ICU, or as needed.The surgical resident extubates thepatient as soon as possible (ie, usuallywithin four to eight hours) and placesthe patient on 6 L of oxygen via nasalcannula. The ICU nurse monitors thepatient’s mediastinal chest tubes andpleural drainage system for excessive(ie, more than 200 mL/hour) or increasingdrainage. The ICU nurse replacespotassium to maintain levels between4.0 mEq/L and 5.2 mEq/L. He or sheadministers morphine, the pain medicationof choice, as needed and continuesIV administration of antibiotics (eg, cefazolinor vancomycin) for 48 hours. TheICU nurse also administers heparin subcutaneouslyfor platelet counts greaterthan 100,000/mL 3 .When the patient is extubated, thenurse advances the patient’s diet fromclear liquids to full liquids, then to afull liquid, low cholesterol, no-addedsodiumdiet. The nurse initiates use ofthe incentive spirometer with coughingand deep breathing immediately afterextubation and helps the patient sit onthe side of the bed within six hours ofextubation. The cardiologist sets theatrioventricular-sequential pacemakerto fully automatic pacing.On the first postoperative day, thesurgical resident removes the pulmonaryartery catheter and arterial linesafter the patient is determined to behemodynamically stable. The ICU nurseremoves the indwelling urinary catheteron the first postoperative day. The nurseweans the patient from morphine to useof oxycodone/acetaminophen as soonas the patient is able to take oral medicationsand according to the patient’sacceptable pain threshold. The ICUnurse prepares the patient for transfer tothe cardiac step-down unit, usually bythe first postoperative day.In the cardiac step-down unit, theassigned nurse encourages the patientto ambulate in the halls three times perday. The nurse advances the patientfrom a full liquid to a regular diet with164 • <strong>AORN</strong> JOURNAL
Winters — Obriot JANUARY 2007, VOL 85, NO 1no added sodium and low cholesterol.The sternal dressing remains in placeand the nurse reinforces it as needed.The nurse adds one aspirin per day tothe patient’s medication regimen.On the second postoperative day,the surgical resident removes themediastinal chest tubes if drainage isless than 50 mL in eight hours andapplies an occlusive dressing over thechest tube sites for 24 hours. A chestx-ray is taken after the chest tubes areremoved to ascertain that the patient’slungs remain reinflated. The surgicalresident removes the sternal dressingand the nurse cleans the incision withnormal saline, after which the nursecovers the incision only if the wound isdraining. The nurse and physical therapistensure that the patient ambulatesfour times a day. The nurse adds astool softener to the patient’s medicationregimen and begins to teach thepatient and his or her family membersabout the medication regimen to be followedat home after discharge.On the third postoperative day, thenurse ensures that discharge laboratorytests are performed including a CBCwith platelet count. The surgical resident,nurse practitioner, or physician’sassistant removes the pacing wires if thepatient’s heart rhythm is stable. Thenurse begins teaching the patient andhis or her family members aboutwound care and makes final dischargeplans and orders any needed home supplies.The nurse then removes anyremaining peripheral IV lines.The nurse discharges the patient onthe fourth postoperative day withinstructions about medications andwound care. He or she instructs thepatient to continue using the incentivespirometer and performing coughingand deep breathing exercises. Thenurse ensures that an appointment ismade for a one-month follow-up in thecardiac surgery clinic and gives thepatient instructions on how to contactthe surgical resident should any questionsarise.CONCLUSIONTreatment of mitral valve diseasehas evolved from replacement torepair. Improved understanding of theunderlying pathology has been animportant part of this evolution. Avariety of repair techniques used byexperienced surgeons provide patientswith the best possible outcomes.The next phase in the evolution ofmitral valve repair is minimally invasive,robotic-assisted mitral valverepair. 9 This technique uses robotic technologyalong with a right-chest endoscopicapproach. Although use of thistechnique has been reported by othercenters in the United States, it currentlyis not being used for mitral valve repairat the University of Michigan. ❖Margo Winters, RN, BSN, CNOR,was the adult cardiac surgery educationcoordinator at University Hospital,University of Michigan HealthSystem, Ann Arbor, Mich, at the timethis article was written. Currently, sheis a clinical systems trainer for thecomputerized physician order entryproject at the University of Michigan.Pam Obriot, RN, BSN, is a RN firstassistant and cardiac surgery educationcoordinator at University Hospital,University of Michigan Health System,Ann Arbor, Mich.REFERENCES1. Ho SY. Anatomy of the mitral valve.Heart. 2002;88(suppl 4):iv5-10.2. Seifert PC. Cardiac Surgery PerioperativePatient Care. St. Louis: Mosby; 2002.3. Finkelmeier BA. Cardiothoracic SurgicalNursing. Philadelphia: Lippincott,Williams & Wilkins; 1995:21-22.4. Thompson JM, McFarland GK, HirshJE, et al. Mosby’s Clinical Nursing. St Louis:Mosby; 1986.<strong>AORN</strong> JOURNAL • 165