March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
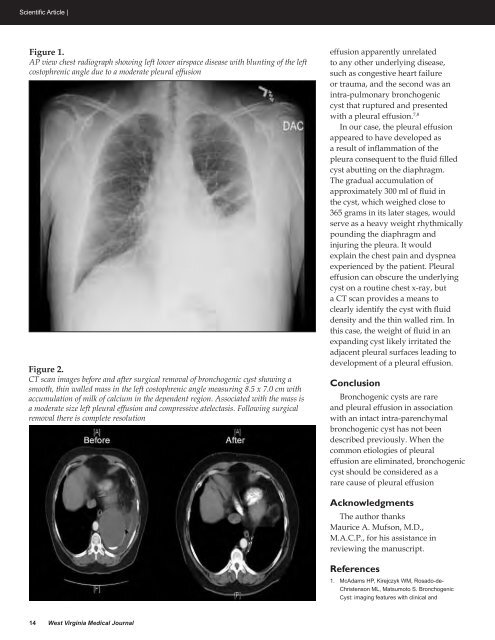
Scientific Article |Figure 1.AP view chest radiograph showing left lower airspace disease with blunting of the leftcostophrenic angle due to a moderate pleural effusionFigure 2.CT scan images before and after surgical removal of bronchogenic cyst showing asmooth, thin walled mass in the left costophrenic angle measuring 8.5 x 7.0 cm withaccumulation of milk of calcium in the dependent region. Associated with the mass isa moderate size left pleural effusion and compressive atelectasis. Following surgicalremoval there is complete resolutioneffusion apparently unrelatedto any other underlying disease,such as congestive heart failureor trauma, and the second was anintra-pulmonary bronchogeniccyst that ruptured and presentedwith a pleural effusion. 7,8In our case, the pleural effusionappeared to have developed asa result of inflammation of thepleura consequent to the fluid filledcyst abutting on the diaphragm.The gradual accumulation ofapproximately 300 ml of fluid inthe cyst, which weighed close to365 grams in its later stages, wouldserve as a heavy weight rhythmicallypounding the diaphragm andinjuring the pleura. It wouldexplain the chest pain and dyspneaexperienced by the patient. Pleuraleffusion can obscure the underlyingcyst on a routine chest x-ray, buta CT scan provides a means toclearly identify the cyst with fluiddensity and the thin walled rim. Inthis case, the weight of fluid in anexpanding cyst likely irritated theadjacent pleural surfaces leading todevelopment of a pleural effusion.ConclusionBronchogenic cysts are rareand pleural effusion in associationwith an intact intra-parenchymalbronchogenic cyst has not beendescribed previously. When thecommon etiologies of pleuraleffusion are eliminated, bronchogeniccyst should be considered as arare cause of pleural effusionAcknowledgmentsThe author thanksMaurice A. Mufson, M.D.,M.A.C.P., for his assistance inreviewing the manuscript.References1.McAdams HP, Kirejczyk WM, Rosado-de-Christenson ML, Matsumoto S. BronchogenicCyst: imaging features with clinical and14 <strong>West</strong> <strong>Virginia</strong> <strong>Medical</strong> Journal