March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
March/April - West Virginia State Medical Association
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
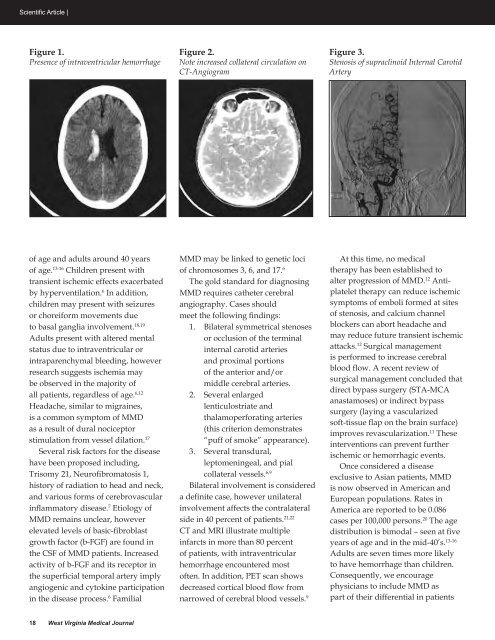
Scientific Article |Figure 1.Presence of intraventricular hemorrhageFigure 2.Note increased collateral circulation onCT-AngiogramFigure 3.Stenosis of supraclinoid Internal CarotidArteryof age and adults around 40 yearsof age. 13-16 Children present withtransient ischemic effects exacerbatedby hyperventilation. 6 In addition,children may present with seizuresor choreiform movements dueto basal ganglia involvement. 18,19Adults present with altered mentalstatus due to intraventricular orintraparenchymal bleeding, howeverresearch suggests ischemia maybe observed in the majority ofall patients, regardless of age. 6,12Headache, similar to migraines,is a common symptom of MMDas a result of dural nociceptorstimulation from vessel dilation. 17Several risk factors for the diseasehave been proposed including,Trisomy 21, Neurofibromatosis 1,history of radiation to head and neck,and various forms of cerebrovascularinflammatory disease. 7 Etiology ofMMD remains unclear, howeverelevated levels of basic-fibroblastgrowth factor (b-FGF) are found inthe CSF of MMD patients. Increasedactivity of b-FGF and its receptor inthe superficial temporal artery implyangiogenic and cytokine participationin the disease process. 6 FamilialMMD may be linked to genetic lociof chromosomes 3, 6, and 17. 6The gold standard for diagnosingMMD requires catheter cerebralangiography. Cases shouldmeet the following findings:1. Bilateral symmetrical stenosesor occlusion of the terminalinternal carotid arteriesand proximal portionsof the anterior and/ormiddle cerebral arteries.2. Several enlargedlenticulostriate andthalamoperforating arteries(this criterion demonstrates“puff of smoke” appearance).3. Several transdural,leptomeningeal, and pialcollateral vessels. 6,9Bilateral involvement is considereda definite case, however unilateralinvolvement affects the contralateralside in 40 percent of patients. 21,22CT and MRI illustrate multipleinfarcts in more than 80 percentof patients, with intraventricularhemorrhage encountered mostoften. In addition, PET scan showsdecreased cortical blood flow fromnarrowed of cerebral blood vessels. 9At this time, no medicaltherapy has been established toalter progression of MMD. 12 Antiplatelettherapy can reduce ischemicsymptoms of emboli formed at sitesof stenosis, and calcium channelblockers can abort headache andmay reduce future transient ischemicattacks. 12 Surgical managementis performed to increase cerebralblood flow. A recent review ofsurgical management concluded thatdirect bypass surgery (STA-MCAanastamoses) or indirect bypasssurgery (laying a vascularizedsoft-tissue flap on the brain surface)improves revascularization. 11 Theseinterventions can prevent furtherischemic or hemorrhagic events.Once considered a diseaseexclusive to Asian patients, MMDis now observed in American andEuropean populations. Rates inAmerica are reported to be 0.086cases per 100,000 persons. 20 The agedistribution is bimodal – seen at fiveyears of age and in the mid-40’s. 13-16Adults are seven times more likelyto have hemorrhage than children.Consequently, we encouragephysicians to include MMD aspart of their differential in patients18 <strong>West</strong> <strong>Virginia</strong> <strong>Medical</strong> Journal