Journal of - Spinal Research Foundation
Journal of - Spinal Research Foundation
Journal of - Spinal Research Foundation
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
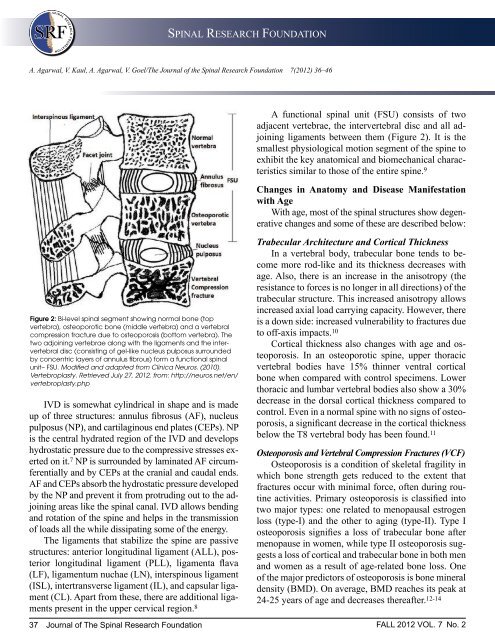
SPINAL RESEARCH FOUNDATIONA. Agarwal, V. Kaul, A. Agarwal, V. Goel/The <strong>Journal</strong> <strong>of</strong> the <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> 7(2012) 36–46Figure 2: Bi-level spinal segment showing normal bone (topvertebra), osteoporotic bone (middle vertebra) and a vertebralcompression fracture due to osteoporosis (bottom vertebra). Thetwo adjoining vertebrae along with the ligaments and the intervertebraldisc (consisting <strong>of</strong> gel-like nucleus pulposus surroundedby concentric layers <strong>of</strong> annulus fibrous) form a functional spinalunit– FSU. Modified and adapted from Clinica Neuros. (2010).Vertebroplasty. Retrieved July 27, 2012, from: http://neuros.net/en/vertebroplasty.phpIVD is somewhat cylindrical in shape and is madeup <strong>of</strong> three structures: annulus fibrosus (AF), nucleuspulposus (NP), and cartilaginous end plates (CEPs). NPis the central hydrated region <strong>of</strong> the IVD and developshydrostatic pressure due to the compressive stresses exertedon it. 7 NP is surrounded by laminated AF circumferentiallyand by CEPs at the cranial and caudal ends.AF and CEPs absorb the hydrostatic pressure developedby the NP and prevent it from protruding out to the adjoiningareas like the spinal canal. IVD allows bendingand rotation <strong>of</strong> the spine and helps in the transmission<strong>of</strong> loads all the while dissipating some <strong>of</strong> the energy.The ligaments that stabilize the spine are passivestructures: anterior longitudinal ligament (ALL), posteriorlongitudinal ligament (PLL), ligamenta flava(LF), ligamentum nuchae (LN), interspinous ligament(ISL), intertransverse ligament (IL), and capsular ligament(CL). Apart from these, there are additional ligamentspresent in the upper cervical region. 8A functional spinal unit (FSU) consists <strong>of</strong> twoadjacent vertebrae, the intervertebral disc and all adjoiningligaments between them (Figure 2). It is thesmallest physiological motion segment <strong>of</strong> the spine toexhibit the key anatomical and biomechanical characteristicssimilar to those <strong>of</strong> the entire spine. 9Changes in Anatomy and Disease Manifestationwith AgeWith age, most <strong>of</strong> the spinal structures show degenerativechanges and some <strong>of</strong> these are described below:Trabecular Architecture and Cortical ThicknessIn a vertebral body, trabecular bone tends to becomemore rod-like and its thickness decreases withage. Also, there is an increase in the anisotropy (theresistance to forces is no longer in all directions) <strong>of</strong> thetrabecular structure. This increased anisotropy allowsincreased axial load carrying capacity. However, thereis a down side: increased vulnerability to fractures dueto <strong>of</strong>f-axis impacts. 10Cortical thickness also changes with age and osteoporosis.In an osteoporotic spine, upper thoracicvertebral bodies have 15% thinner ventral corticalbone when compared with control specimens. Lowerthoracic and lumbar vertebral bodies also show a 30%decrease in the dorsal cortical thickness compared tocontrol. Even in a normal spine with no signs <strong>of</strong> osteoporosis,a significant decrease in the cortical thicknessbelow the T8 vertebral body has been found. 11Osteoporosis and Vertebral Compression Fractures (VCF)Osteoporosis is a condition <strong>of</strong> skeletal fragility inwhich bone strength gets reduced to the extent thatfractures occur with minimal force, <strong>of</strong>ten during routineactivities. Primary osteoporosis is classified intotwo major types: one related to menopausal estrogenloss (type-I) and the other to aging (type-II). Type Iosteoporosis signifies a loss <strong>of</strong> trabecular bone aftermenopause in women, while type II osteoporosis suggestsa loss <strong>of</strong> cortical and trabecular bone in both menand women as a result <strong>of</strong> age-related bone loss. One<strong>of</strong> the major predictors <strong>of</strong> osteoporosis is bone mineraldensity (BMD). On average, BMD reaches its peak at24-25 years <strong>of</strong> age and decreases thereafter. 12-1437 <strong>Journal</strong> <strong>of</strong> The <strong>Spinal</strong> <strong>Research</strong> <strong>Foundation</strong> FALL 2012 VOL. 7 No. 2