Fam ily Eco nom ics and - Center for Nutrition Policy and Promotion ...
Fam ily Eco nom ics and - Center for Nutrition Policy and Promotion ...
Fam ily Eco nom ics and - Center for Nutrition Policy and Promotion ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
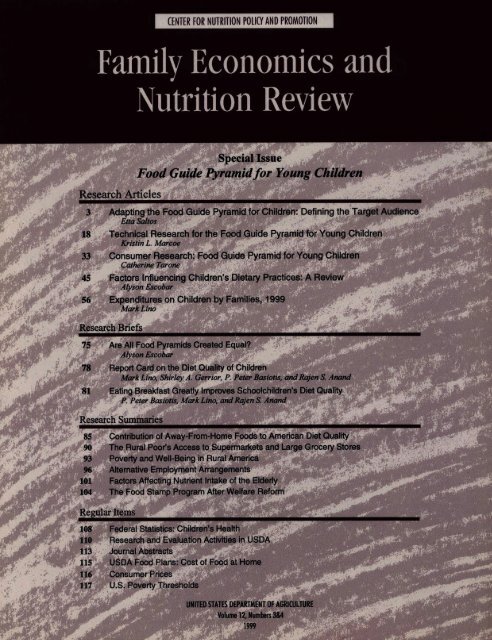
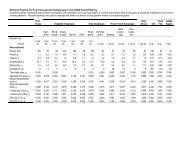
<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong><strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong> <strong>and</strong>Nu tri tion Re viewEdi torJulia M. DinkinsFea tures Edi torMark LinoMan ag ing Edi torJane W. FlemingCon tribu torJoan C. Cour tless<strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong> <strong>and</strong> Nu tri tion Re view iswrit ten <strong>and</strong> pub lished each quar ter by theCen ter <strong>for</strong> Nu tri tion Pol icy <strong>and</strong> Pro mo tion,U.S. Department of Agriculture, Wash ing ton, DC.The Sec re tary of Ag ri cul ture has de ter minedthat pub li ca tion of this pe ri odi cal is ne ces saryin the tran sac tion of the pub li c businessre quired by law of the De part ment.This pub li ca tion is not copy righted. Con tentsmay be re printed with out per mis sion, but creditto <strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong> <strong>and</strong> Nu tri tion Revieww ould be ap pre ci ated. Use of com mer cial ortrade names does not im ply approval or con sti -tute en dorsement by USDA. <strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong><strong>and</strong> Nu tri tion Review is indexed in the fol low ingda taba ses: AGRICOLA, Age line, <strong>Eco</strong> <strong>nom</strong>icLit era ture In dex, ERIC, <strong>Fam</strong> <strong>ily</strong> Stud ies,PAIS, <strong>and</strong> So cio logi cal Abstracts.<strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong> <strong>and</strong> Nu tri tion Re view is<strong>for</strong> sale by the Su per in ten dent of Docu ments.Sub scrip tion price is $12.00 per year ($15.00<strong>for</strong> <strong>for</strong> eign ad dresses). Send sub scrip tionor ders <strong>and</strong> change of ad dress to Su per in -ten d ent of Docu ments, P.O. Box 371954,Pittsburgh, PA 15250- 7954. (See subscrip tio n<strong>for</strong>m on p. 123.)O rigi nal manu scripts are ac cepted <strong>for</strong> pub li -ca tion. (See “guide lines <strong>for</strong> authors” on backin side cover.) Sug ges tions or com ments con -cerning this pub li ca tion should be ad dressedto Julia M. Dink ins, Edi tor, <strong>Fam</strong> <strong>ily</strong> <strong>Eco</strong><strong>nom</strong> <strong>ics</strong><strong>and</strong> Nu tri tion Review, <strong>Center</strong> <strong>for</strong> Nu tri tion<strong>Policy</strong> <strong>and</strong> Pro mo tion, USDA,1120 20th St.NW, Suite 200 North Lobby, Wash ing ton, DC20036. Phone (202) 606-4876.The <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Reviewis no w available at http://www.usda.gov/cnpp(see p. 121).Research Ar ti clesSpe cial IssueFood Guide Pyra mid <strong>for</strong> Young Children3 Adapting the Food Guide Pyramid <strong>for</strong> Children:Defining the Target AudienceEtta Saltos18 Technical Research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> Young ChildrenKristin L. Marcoe33 Consumer Research: Food Guide Pyramid <strong>for</strong> Young ChildrenCatherine Tarone45 Factors Influencing Children’s Dietary Practices: A ReviewAlyson Escobar56 Expenditures on Children by <strong>Fam</strong>ilies, 1999Mark LinoResearch Briefs75 Are All Food Pyra mids Cre ated Equal?Alyson Escobar78 Re port Card on the Diet Qual ity of ChildrenMark Lino, Shirley A. Gerrior, P. Peter Basiotis, <strong>and</strong> Rajen S. An<strong>and</strong>81 Eat ing Break fast Greatly Im proves School chil dren’s Diet QualityP. Pe ter Basiotis, Mark Lino, <strong>and</strong> Rajen S. An<strong>and</strong>Research Sum ma ries85 Contribution of Away-From-Home Foods to Ameri can Diet Quality90 The Ru ral Poor’s Ac cess to Su per mar kets <strong>and</strong> Large Gro cery Stores93 Pov erty <strong>and</strong> Well- Being in Rural America96 Al ter na tive Em ploy ment Arrangements101 Fac tors Af fect ing Nu tri ent In take of the Elderly104 The Food Stamp Pro gram Af ter Wel fare Re<strong>for</strong>mRegular Items108 Fed eral Sta tis t<strong>ics</strong>: Chil dren’s Health110 Re search <strong>and</strong> Evalua tion Ac tivi ties in USDA113 Jour nal Abstracts115 USDA Food Plans: Cost of Food at Home116 Con sumer Prices117 U.S. Pov erty Thresholds118 In dex of Ar ti cles in 1999 Issues119 In dex of Authors in 1999 Issues120 Re view ers <strong>for</strong> 1999 ArticlesVolume 12, Numbers 3&41999
The purpose of this study was to definethe target audience <strong>for</strong> a food guide thatwould be adapted <strong>for</strong> children by recommendingsubgroups within the 2- to 18-year age range <strong>and</strong> ranking the subgroupsin order of greatest need based on dietaryrequirements <strong>and</strong> user dem<strong>and</strong> <strong>for</strong> nutritioneducation materials. Materialsreviewed <strong>for</strong> this study included journalarticles, reference materials (includingthe Recommended Dietary Allowances<strong>and</strong> nutrition textbooks), <strong>and</strong> published<strong>and</strong> unpublished reports from governmentagencies. Criteria used to define <strong>and</strong> rankthe subgroups included the following:• nutrient needs of children,• nutrition recommendations <strong>for</strong>children by authoritative bodies,such as the Dietary GuidelinesAdvisory Committee,• nutritional status of children,including macronutrient <strong>and</strong> micronutrientintake <strong>and</strong> anthropometricmeasurements, <strong>and</strong>• children’s knowledge <strong>and</strong> attitudesregarding nutrition.These criteria were used to define subgroups<strong>and</strong> to list facts in favor of <strong>and</strong>against adapting a food guide <strong>for</strong> eachsubgroup.Nutrient Needs of ChildrenThe Recommended Dietary Allowances(RDA) provide in<strong>for</strong>mation concerningchildren’s nutrient needs, as well as thenutritional needs of the rest of the population(23). The 1989 RDA are expressed<strong>for</strong> the following age-gender groups:children, ages 1 to 3 years; children,ages 4 to 6 years; children, ages 7 to 10years; males, ages 11 to 14 years; females,ages 11 to 14 years; males, ages 15 to18 years; <strong>and</strong> females, ages 15 to 18years.The National Academy of Sciences’Food <strong>and</strong> <strong>Nutrition</strong> Board, however, isin the process of replacing these RDAwith new dietary recommendations:Dietary Reference Intakes (DRI). 2DRI were released recently <strong>for</strong> calcium,phosphorus, magnesium, fluoride,vitamin D, thiamin, riboflavin, niacin,vitamin B6, folate, vitamin B12, pantothenicacid, biotin, <strong>and</strong> choline (31,32).Reference intake values were published<strong>for</strong> the following age groups: 1 to 3 years,4 through 8 years, 9 through 13 years,<strong>and</strong> 14 through 18 years.The current RDA (or AI <strong>for</strong> calcium,fluoride, vitamin D, pantothenic acid,biotin, <strong>and</strong> choline) <strong>for</strong> children were(a) extrapolated from infant or adultresearch results (vitamins A, K, C,B6, B12, riboflavin, niacin, folate,biotin, choline, pantothenic acid,selenium, iodine, <strong>and</strong> manganese),(b) based on growth <strong>and</strong> consumptiondata (energy, protein, iron, phosphorus,<strong>and</strong> potassium),(c) estimated based on weight (fluoride<strong>and</strong> vitamin E),2 The DRI, a set of up to four nutrient-based referencevalues, consist of the Estimated AverageRequirement (EAR), Recommended DietaryAllowances (RDA), Adequate Intake (AI), <strong>and</strong>Tolerable Upper Intake Level (UL). The EARrefers to the da<strong>ily</strong> intake value that is estimatedto meet the nutrient requirement in half of theindividuals in a given age-gender group. The RDAconsist of the average da<strong>ily</strong> intake level that issufficient to meet the nutrient requirement ofnearly all healthy individuals in the age-gendergroup, based on the EAR. The AI is the da<strong>ily</strong>intake value that is estimated to meet the nutrientrequirement of nearly all healthy individuals in theage-gender group <strong>and</strong> is used when an EAR is notavailable to calculate the RDA. The UL definesthe highest level of nutrient intake that is likely topose no risks of adverse health effects in almostall individuals in the general population.(d) based on studies on balance inchildren, but not necessar<strong>ily</strong> withall the above age groups (thiamin,zinc, copper, sodium, calcium, <strong>and</strong>magnesium), or(e) estimated based on biochemicalmarkers (vitamin D) (23,31,32).Because the RDA/AI <strong>for</strong> children werelargely extrapolated or calculated ratherthan determined directly from studies ofchildren, there is no overriding reason<strong>for</strong> using the RDA age-gender cutoffs<strong>for</strong> a children’s food guide. In<strong>for</strong>mationon children’s dietary intakes, nutritionalstatus, <strong>and</strong> dietary recommendations----as well as in<strong>for</strong>mation on their attitudes,knowledge, <strong>and</strong> behavior----must also beconsidered when determining whichgroups of children are most in need ofnutrition guidance.<strong>Nutrition</strong> Recommendations<strong>for</strong> ChildrenRecommendations of theU.S. GovernmentA number of recommendations indicatewhat constitutes a healthful diet <strong>for</strong>children. The Dietary Guidelines <strong>for</strong>Americans, the basis of Federal nutritionpolicy (39), provide advice about foodchoices that promote health <strong>and</strong> preventdisease among healthy Americans 2 yearsold <strong>and</strong> older. The Guidelines adviseAmericans to eat a varied diet with plentyof grain products, vegetables, <strong>and</strong> fruits,while moderating their intakes of fat,saturated fat, cholesterol, sugars, salt<strong>and</strong> sodium, <strong>and</strong> alcoholic beverages. Inaddition to emphasizing the benefits ofphysical activity, the Guidelines providesome specific advice <strong>for</strong> children: theyshould be taught to eat grain products;vegetables <strong>and</strong> fruits; lowfat milkproducts or other calcium-rich foods;beans, lean meat, poultry, fish or other4 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
protein-rich foods; <strong>and</strong> to participate invigorous physical activity. The Guidelinescaution that fat should not be restricted<strong>for</strong> children younger than age 3 2, thatmajor ef<strong>for</strong>ts to change a child’s dietshould be accompanied by monitoringof growth at regular intervals by a healthprofessional, <strong>and</strong> that children shouldnot consume alcoholic beverages. TheGuidelines also recommend that childrenbetween the ages of 2 <strong>and</strong> 5 shouldgradually adopt a diet so that it containsno more than 30 percent of calories fromfat by the time children are about 5 yearsold (39).The report Healthy People 2010 outlinesa national strategy <strong>for</strong> improving significantlythe health of Americans duringthe 2001 to 2010 decade (42). Includedin the 2010 report is a recommendationto reduce fat intake to an average of 30percent of calories or less <strong>and</strong> saturatedfat intake to an average of less than 10percent of calories among people 2 yearsold <strong>and</strong> older. The National CholesterolEducation Program recommends thattotal fat intake averages no more than30 percent of calories (24). Theserecommendations are consistent withthe advice given in the 1990 DietaryGuidelines; the 1995 Dietary Guidelinesamended this advice, stating that childrenbetween the ages of 2 <strong>and</strong> 5 shouldgradually reduce their total fat intakeso that by age 5, they are consumingno more than 30 percent of caloriesfrom fat.Recommendations ofOther OrganizationsSeveral organizations provide dietaryadvice <strong>for</strong> children that is consistentwith the basic principles of the DietaryGuidelines <strong>for</strong> Americans. The American3 In this paper, the use of the terms ‘‘age’’ <strong>and</strong>‘‘ages’’ refers to age in years, unless statedotherwise.Academy of Pediatr<strong>ics</strong>, <strong>for</strong> example,recommends that children eat a widevariety of foods <strong>and</strong> consume enoughcalories to support growth <strong>and</strong> development<strong>and</strong> to reach or maintain advisablebody weight. The Academy also recommendsthat children over the age of 2consume, on average, 30 percent of totalcalories from fat, less than 10 percent ofcalories from saturated fat, <strong>and</strong> less than300 mg of cholesterol per day. However,the Academy cautions that ‘‘recommendationsthat call <strong>for</strong> ‘less than’ 30 percentof calories from fat may lead to theinappropriate use of more restrictivediets’’ (3).The American Heart Association (AHA)concurs with the recommendation of theDietary Guidelines that children betweenthe ages of 2 <strong>and</strong> 5 gradually adopt adiet containing 30 percent or less ofcalories from fat. The AHA also agreeswith the Dietary Guidelines’ recommendationthat diets of young children shouldmaintain the primary emphasis on providingadequate calories <strong>and</strong> nutrients<strong>for</strong> normal physical activity, growth,<strong>and</strong> development (17).Some disagree about the age at whichchildren should adopt a lower fat diet.A joint working group of the CanadianPaediatric Society <strong>and</strong> Health Canadarecommended a longer transition periodto a diet lower in fat, compared withthat recommended by the Dietary Guidelines.The joint working group advisedthat the transition from the high-fat dietduring infancy (about 50 percent ofcalories from fat) to a diet that includesno more than 30 percent of calories asfat <strong>and</strong> 10 percent of calories as saturatedfat take place between the age of 2 <strong>and</strong>the end of linear growth (about age 14<strong>for</strong> females <strong>and</strong> 15 <strong>for</strong> males) (14). Therationale <strong>for</strong> the working group’s recommendationwas based on (1) lack ofOther studies havealso concludedthat it is safe torecommend that fatintake be limited to30 percent of calories<strong>and</strong> saturated fatintake to less than10 percent of calories<strong>for</strong> children 5 yearsold <strong>and</strong> older . . . .1999 Vol. 12 Nos. 3&4 5
evidence that consuming a diet providing30 percent of calories as fat <strong>and</strong>10 percent of calories as saturated fatwould either reduce illness in later lifeor provide short-term health benefits<strong>and</strong> (2) concerns that some childrenconsuming a diet with low fat intakeshave lower energy intakes <strong>and</strong> lowintakes of some nutrients.To support their position, the CanadianPaediatric Society <strong>and</strong> Health Canadacited a publication from the BogalusaHeart Study in which 24-hour recallswere obtained from about 870 10-yearoldswhose diets were stratified by fatintake: those with less than 30 percentof calories from fat had lower intakesof many nutrients than did children withhigher fat intakes. The children with thelower percentage of calories from fatalso had higher intakes of simple carbohydrates(25). The children enrolled inthe Bogalusa Study had not been exposedpreviously to any dietary interventionprograms. There<strong>for</strong>e, it cannot be concluded,on the basis of the BogalusaStudy, that children----whose parents<strong>and</strong> caregivers have been instructed onhow to moderate dietary fat intake----will be unable to meet their nutrientrequirements on a diet containing 30percent of calories from fat.Other researchers have concluded thatchildren can safely follow diets containing30 percent of calories from fat. TheDietary Intervention Study in Children(DISC) is an ongoing, r<strong>and</strong>omized studythat is a controlled clinical trial of dietscontaining lowered fat, saturated fat,<strong>and</strong> cholesterol. About 660 childrenages 8 to 10 who were enrolled in 6centers, located around the country, wereassigned r<strong>and</strong>omly to either controlgroups or groups receiving behavioralintervention to promote their followinga diet providing 28 percent of caloriesfrom total fat, less than 8 percent ofcalories from saturated fat, <strong>and</strong> less than150 mg of cholesterol (less than 75 mg/1,000 calories) per day. After 3 years,dietary levels of total fat, saturated fat,<strong>and</strong> cholesterol <strong>and</strong> blood levels of lowdensitylipoprotein cholesterol (LDL-C)decreased significantly in the interventiongroup, compared with the controlgroup. The two groups, however, didnot differ significantly on measures ofgrowth <strong>and</strong> development: Height, redblood-cellfolate values, serum zinc,retinol <strong>and</strong> albumin levels, sexualmaturation, <strong>and</strong> psychosocial health.The DISC study found that childrengrew <strong>and</strong> developed normally afterbeing instructed on consuming a lowerfat diet. The children in the interventiongroup also had lower LDL-C levels thanthe controls. The researchers concluded,there<strong>for</strong>e, that the diet was effective aswell as safe (19). Other studies have alsoconcluded that it is safe to recommendthat fat intake be limited to 30 percentof calories <strong>and</strong> saturated fat intake toless than 10 percent of calories <strong>for</strong>children 5 years old <strong>and</strong> older(26,29,35).Another recommendation regardingchildren’s diets addresses their requirements<strong>for</strong> dietary fiber. The DietaryGuidelines recommend that individuals2 years <strong>and</strong> older choose a diet withplenty of grain products, vegetables,<strong>and</strong> fruits to provide adequate fiber.But the Guidelines do not set specificnumerical goals <strong>for</strong> fiber intake. TheAmerican Health Foundation publisheda recommendation that a child’s fiberintake be equivalent to his or her ageplus 5 grams (g) a day (‘‘age + 5’’),with the recommendation ranging from8 g a day <strong>for</strong> a child age 3 to 25 g a day<strong>for</strong> a person age 20 (44).<strong>Nutrition</strong>al Status of ChildrenDietary Intake----EnergyData on children’s food consumptionare provided by several national surveys:DHHS’s National Health <strong>and</strong> <strong>Nutrition</strong>Examination Survey (NHANES III),USDA’s Continuing Survey of FoodIntakes by Individuals (CSFII), <strong>and</strong> theMarket Research Corporation of America(MRCA) (1,10,16,37). Median energyintakes below 100 percent of the RDA<strong>for</strong> several age-gender groups werereported in NHANES III results (10).The CSFII 1994-96 reported that overhalf of the children 5 years old <strong>and</strong>younger had energy intakes below theRDA, <strong>and</strong> about 20 percent had energyintakes below 75 percent of the RDA.About 60 percent of males <strong>and</strong> 75 percentof females 6 to 19 years old hadenergy intakes below the RDA (37).Rather than a reflection of actual lowintakes of energy by children, these lowintakes of energy could be the result ofunderreporting the foods eaten or oflow energy expenditures by children.Several studies have reported thatpreschool-age children have energyexpenditures lower than the RDA(6,11,12). In contrast, the prevalenceof overweight among children has beenincreasing (36). According to CSFII1994-96, about 5 to 10 percent of allchildren have energy intakes at or above150 percent of the RDA (37).Dietary Intake----Macronutrients<strong>and</strong> FiberFood consumption surveys report that,on average, children are consumingmore than 30 percent of calories fromtotal fat <strong>and</strong> more than 10 percent ofcalories from saturated fat (fig. 1) (1,10,16,37). Kennedy <strong>and</strong> Goldberg, usingCSFII 1989-91 data, reported that overthree-fourths of all children exceeded6 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Figure 1. Percent of calories from total fat <strong>and</strong> saturated fat in children’s diets exceedsrecommendationsPercent454035302520151050Age <strong>and</strong>gender1-2 years 3-5 years 6-11 yearsmales6-11 yearsfemales12-19 yearsmales12-19 yearsfemales% Calories from total fat% Calories from saturated fatDietary Guidelines recommendation <strong>for</strong> % calories from total fatDietary Guidelines recommendation <strong>for</strong> % calories from saturated fatrecommendations <strong>for</strong> total fat <strong>and</strong>saturated fat (15). Improvement wasslight by 1994, when roughly two-thirdsof all children exceeded the recommendation<strong>for</strong> total fat <strong>and</strong> saturated fat(16). Because of the Guidelines’ recommendation<strong>for</strong> gradual adoption of a dietlow in fat, concern is greater <strong>for</strong> children5 years <strong>and</strong> older than it is <strong>for</strong> children2 to 5 years old. The CSFII 1994-96also reported that adolescent males areconsuming more than 300 mg/day ofcholesterol, the upper limit of cholesterolintake listed on the <strong>Nutrition</strong> Facts label(37).Other studies have confirmed the findingsregarding children’s fat intake: most areconsuming more than the recommendedlevels. About ninety 3- to 5-year-oldchildren enrolled in the FraminghamChildren’s Study 4 consumed an averageof 33 percent of calories from fat (28).Albertson <strong>and</strong> Tobelmann, analyzing1986-88 MRCA data, reported thatamong 825 children ages 7 to 12, thosewho frequently ate ready-to-eat cereal(7 or more times in 14 days) consumeda lower percentage of calories from fat,compared with others who consumedready-to-eat cereals less frequently: 2 to6 times in 14 days or less than 2 timesin 14 days. However, all three groupsconsumed more than 30 percent ofcalories from fat (2).Data from the CSFII 1994-96 showedthat young children’s mean intakes of4 The longitudinal Framingham Children’s Studyexamined factors related to the development ofdietary habits <strong>and</strong> patterns of physical activityduring childhood.dietary fiber met the ‘‘age + 5’’ recommendationof the American HealthFoundation. Children 5 years old <strong>and</strong>younger had mean fiber intakes ofabout 11 g a day. However, older childrenbegan to fall short of the fiber recommendations:males <strong>and</strong> females 6 to 11years old consumed about 14 g <strong>and</strong> 12 gof fiber per day, respectively; their counterparts12 to 19 years old consumed about17 g (males) <strong>and</strong> 13 g (females) per day(37).Dietary Intake----MicronutrientsAmerican children are more likely toget adequate amounts of vitamins <strong>and</strong>minerals than they are to meet DietaryGuideline recommendations <strong>for</strong> total fat<strong>and</strong> saturated fat intake. However, somenutrients are consumed at levels belowrecommended amounts by some groups1999 Vol. 12 Nos. 3&4 7
in the U.S. population. For example,vitamin E <strong>and</strong> zinc are consumed atlevels below 100 percent of the RDAby most children 2 to 19 years old (37).According to CSFII 1994-96, on thedays surveyed, only about 60 percentof children 5 years <strong>and</strong> younger, 60 percentof females 6 to 11 years old, <strong>and</strong>only 28 percent of females 12 to 19 yearsold consumed 100 percent or more ofthe RDA <strong>for</strong> iron. Only about one-thirdeach of males <strong>and</strong> females 12 to 19years old consumed 100 percent ormore of the RDA <strong>for</strong> vitamin A (37).Calcium is another nutrient that childrenconsume at levels below recommendations.Average calcium consumption isbelow the 1989 RDA <strong>for</strong> children 12 to19 years old (fig. 2). In 1994-96, abouthalf of the children 11 years old <strong>and</strong>younger consumed 100 percent or moreof the 1989 RDA <strong>for</strong> calcium; just overone-third of males 12 to 19 years old<strong>and</strong> about 15 percent of females 12 to19 years old consumed 100 percent ormore of the calcium RDA (37). Evenfewer children ages 9 <strong>and</strong> older wouldmeet the new Adequate Intake <strong>for</strong> calcium,which increased to 1,300 mg (31).Compared with other children, adolescents,particularly adolescent females,had the greatest problems in meetingtheir nutrient requirements. Adolescentfemales reported the lowest energyintakes in proportion to their energyrequirement (37). Findings of MRCAdata from 1991-94 show that mostadolescents ages 11 to 17 consumed lessthan 2 servings (the minimalnumber recommended) of fruits a day.Twelve percent of adolescents consumedno fruits in a given day (45).Krebs-Smith et al. examined 3-day datafrom CSFII 1989-91 <strong>for</strong> children <strong>and</strong>adolescents 2 to 18 years old. Evenafter foods were separated into theircomponent ingredients (e.g., credit isgiven <strong>for</strong> vegetables in mixed dishes,such as on pizza or in s<strong>and</strong>wiches),only one in five children consumed therecommended 5 servings of fruits <strong>and</strong>vegetables a day. One-quarter of allvegetables that were consumed wereFrench fries. Children from familieswith higher income consumed moreservings of fruits <strong>and</strong> vegetables,compared with children from familieswith lower income (18).Data from the CSFII 1994-96 alsoshowed that children’s intake of fruits<strong>and</strong> vegetables was low. Only aboutone-fourth of children 2 to 11 years oldconsumed the minimal 3 servings ofvegetables a day that are recommendedby the Pyramid, <strong>and</strong> only about 40 percentof females <strong>and</strong> 55 percent of males12 to 19 years old met the minimal numberof servings. About half of all 2- to 5-yearoldsconsumed the minimal 2 servingsof fruit a day recommended by thePyramid, but this dropped to about onefourth<strong>for</strong> males <strong>and</strong> females 11 to 19years old (37). Low intakes from onefood group could explain some of thelow nutrient intakes, particularly <strong>for</strong>vitamins A <strong>and</strong> C <strong>and</strong> folate.Sodium intakes <strong>for</strong> many children arehigher than 2,400 mg a day, its upperlimit (listed on the <strong>Nutrition</strong> Facts label).Children 6 years old <strong>and</strong> older hadmedian sodium intakes greater than2,400 mg a day according to NHANESdata (which includes allowances <strong>for</strong> saltadded at the table <strong>and</strong> sodium in water<strong>and</strong> medications) (10). In the CSFII1994-96 (which reports only sodiumintake from food), the mean sodiumconsumption <strong>for</strong> all children 3 years old<strong>and</strong> older exceeded 2,400 mg a day.Mean sodium consumption <strong>for</strong> males ages12 to 19 years was 4,407 mg a day (37).Anthropometric IndicesWeight <strong>and</strong> height indicators fromNHANES III show that underweight isa concern <strong>for</strong> about 5 percent of 2- to17-year-olds (only 2 percent of 12- to17-year-old females) (10). Overweight,when defined as a weight <strong>for</strong> heightgreater than the 95th percentile, occurredin 10.9 percent of children ages 6 through17 (36). When overweight was definedas a weight <strong>for</strong> height greater than the85th percentile, the incidence of overweightincreased to 22 percent (36).The prevalence of overweight increasedbetween 1963-65 <strong>and</strong> 1988-91 amongall age-gender groups, with the greatestincrease occurring between 1976-80 <strong>and</strong>1988-91 (36).A study of the prevalence of overweightamong preschool-age children 2 monthsthrough 5 years old found that overweightamong 4- <strong>and</strong> 5-year-old females increasedfrom 5.8 percent in 1971-74 to10 percent in 1988-94. Overweight wasdefined, in this study of NHANES data,as being above the 95 th percentile of theappropriate measures of the National<strong>Center</strong> <strong>for</strong> Health Statist<strong>ics</strong>: weight<strong>for</strong>-lengthor weight-<strong>for</strong>-stature growthcurve. The prevalence of overweight didnot increase among younger children.However, the increase in prevalence ofoverweight in children as young as 4 yearsold suggests that ef<strong>for</strong>ts to prevent overweightshould begin in early childhood(27).The increase in obesity is surprising,because many children are reportingenergy intakes below the RDA. Lackof physical activity may be responsible<strong>for</strong> the increase, <strong>and</strong> the number of hourschildren watch television has been linkedto obesity in this age group (8).8 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Figure 2. Mean calcium intakes of older American children below recommended levelsMilligrams1400120010008006004002000Age <strong>and</strong>gender1-2 years 3-5 years 6-11 yearsmales6-11 yearsfemales12-19 yearsmales12-19 yearsfemalesCalcium intake, mg 1989 RDA, mg 1997 AI, mgConsumer Research----Children’s Knowledge <strong>and</strong>Attitudes About <strong>Nutrition</strong>When adapting a food guide <strong>for</strong> children,USDA staff believe it is useful to findout what children know about nutrition,what their attitudes are about foods <strong>and</strong>nutrition, <strong>and</strong> what nutrition educationprograms have been successful. Childrenhave been the target audience <strong>for</strong> somequalitative <strong>and</strong> quantitative studies;however, in<strong>for</strong>mation about their knowledge<strong>and</strong> attitudes regarding nutrition isfar more scarce than in<strong>for</strong>mation aboutadult’s knowledge <strong>and</strong> attitudes.Qualitative StudiesIn late 1991, in preparation <strong>for</strong> developingnutrition labeling materials <strong>for</strong> children,KIDSNET, Inc., an organization workingon children’s educational issues (in cooperationwith the U.S. Food <strong>and</strong> DrugAdministration [FDA]), sponsored minifocusgroups (3 children in each group)with children 6, 8, <strong>and</strong> 12 years old. Thefocus groups were designed to examinechildren’s attitudes <strong>and</strong> behavior regardingfood, as well as their awareness <strong>and</strong>knowledge of the relationship betweennutrition <strong>and</strong> food. Six focus groups (witha mixture of racial <strong>and</strong> income groups)were conducted in the Washington, DC,area. The children reported having someinfluence over the foods they eat, particularlybreakfast cereals, snack foods,<strong>and</strong> lunches. Some 6-year-olds evenreported making their own lunches.Results from the mini-focus group showedthat the children’s age influenced theirknowledge of nutrition. Twelve-year-oldchildren could name food groups <strong>and</strong>were aware that carbohydrate, protein,fat, vitamins, <strong>and</strong> minerals are found infood. Younger children did not have aclear underst<strong>and</strong>ing of food groups, <strong>and</strong>many children thought of vitamins asproducts that come in a bottle from thedrugstore. However, even though the12-year-old children were fairly knowledgeableabout nutrition, their knowledgedid not carry over to their own dietarypatterns. Taste, instead, was their primaryconsideration in making food choices.In the words of one 12-year-old participant:‘‘We hear ‘Eat right. Don’t dodrugs.’ It’s getting boring, like a brokenrecord, so we just tune it out’’ (30).1999 Vol. 12 Nos. 3&4 9
. . . the increase inprevalence of overweightin children asyoung as 4 years oldsuggests that ef<strong>for</strong>tsto prevent overweightshould begin in earlychildhood . . . .The FDA sponsored two focus groups,each consisting of six to eight females13 to 15 years old from various racial<strong>and</strong> ethnic groups. The purpose of thefocus groups was to determine the typesof nutrition messages the participantswould find compelling <strong>and</strong> to determinewhich <strong>for</strong>mat(s)----<strong>for</strong> messages aboutcalcium----the participants would mostlikely pay attention to. These focusgroups were held in the Washington,DC/Baltimore, MD, metropolitan area.The results revealed that the participantshad a fairly good knowledge of nutrition;they could name nutrients <strong>and</strong> makeassociations between a nutrient <strong>and</strong> itsfunction, <strong>for</strong> example, ‘‘calcium makesyour bones strong.’’ Participants saidthey tended to pay more attention toeating a healthful diet when they wereactively involved in a sport. (Most wereactive in at least one sport.) A frequentlymentioned barrier to healthful eatingwas related to school lunches: lunchperiods were often rushed <strong>and</strong> at oddhours of the day. Participants expresseda preference <strong>for</strong> educational materialsthat contained bold, bright colors <strong>and</strong>little or no text (21).The International Food In<strong>for</strong>mationCouncil sponsored one focus group with9- to 12-year-old children <strong>and</strong> anotherwith 13- <strong>and</strong> 14-year-olds to evaluate aprototype nutrition brochure. All of theparticipants had seen the Food GuidePyramid, <strong>and</strong> all said they already knewabout the importance of eating vegetables,fruits, <strong>and</strong> grain products. The participants,however, believed these conceptswere ‘‘boring, because everyone knowsthat,’’ <strong>and</strong> they believed that in<strong>for</strong>mationabout eating breakfast, smart snacking,<strong>and</strong> balance was important. They alsothought in<strong>for</strong>mation about physicalactivity was important but believed thatactivities portrayed should be relevantto their age group. Activities such asgolf <strong>and</strong> racquetball were perceivedas ‘‘adult’’ sports (9).Because these studies were conductedusing locally available samples <strong>and</strong>were conducted in urban areas, theresults must be interpreted cautiously<strong>and</strong> cannot be generalized to all children.Quantitative StudiesThe Kellogg Company surveyed childrenabout their nutrition knowledge, attitudes,<strong>and</strong> behavior. A nationally representativeschool-based survey was conducted in1988-89 with 5,000 students in Grades3 through 12. Over half of the respondentsin this survey believed nutrition is‘‘very important’’; however, nutritionwas considered less important by olderchildren than by younger ones. Almostthree-quarters of elementary schoolstudents considered nutrition ‘‘veryimportant,’’ compared with about halfof junior high school students <strong>and</strong> onlyabout one-third of high school students(13).The Kellogg survey also found that thepositive attitudes of many children didnot always translate into appropriatebehavior, confirming the results of thequalitative studies referred to earlier inthis paper. Only about one-third of allschool-age children responded ‘‘often’’(rather than ‘‘sometimes’’ or ‘‘rarely’’)to the statement ‘‘I eat the right foods.’’Children who agreed strongly with thestatement that too much cholesterol <strong>and</strong>saturated fat are bad <strong>for</strong> health reportedeating foods high in these componentsas often as did other children, thus demonstratingthat their knowledge did notchange their behavior. The authors ofthe Kellogg survey suggested that lackof sufficient knowledge could be partiallyresponsible <strong>for</strong> this disconnect----the children might know that excessive10 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
dietary cholesterol <strong>and</strong> saturated fat areunhealthful, but they may not knowwhich foods are rich sources of thesecomponents (13).Lack of adult supervision could alsoaccount <strong>for</strong> some of the poor eatinghabits reported by the participants ofthe Kellogg survey. About 60 percentof children reported coming home to anempty house at least once a week, withmore than one-third coming home alonethree or more times a week. These‘‘latchkey’’ children were more likelyto report that they, rather than theirparents, have more control over whatthey eat (60 percent of ‘‘latchkey’’children; 35 percent of all elementaryschoolchildren).Eating away from home frequently couldinfluence children’s diets. According toUSDA’s CSFII 1994-96, about 40 percentof children 5 years old <strong>and</strong> younger<strong>and</strong> over two-thirds of children 6 to 19years old reported eating at least onefood item away from home on the dayof the survey. The most frequentlymentioned sources of food away fromhome were fast-food restaurants, schoolor day care, someone else or gift, <strong>and</strong>stores (37).The Kellogg Survey also found thatalmost one-third of school-age childrenbelieved they were overweight (13).This figure is somewhat higher than the22 percent of children 6 to 17 years oldwho were found to be overweight byNHANES III. This difference raises apossibility: some children whose weightis normal think they are overweight.Thus dieting is a common behavioramong children; about 40 percent ofall school-age children participatingin the Kellogg Survey reported havingbeen on a diet. More females than malesreported dieting, <strong>and</strong> most of the childrenwho reported dieting did so <strong>for</strong> cosmeticreasons rather than <strong>for</strong> health (13).Lack of physical activity has been citedas a possible reason <strong>for</strong> the increase inthe percentage of children who are overweight(6,8,11,12). The Kellogg Survey,on the other h<strong>and</strong>, found that schoolchildrendo consider exercise to beimportant. Elementary schoolchildrenreported taking part in physical activityover five times a week; high schoolstudents reported being involved inphysical activity about four times aweek (13).The Youth Risk Behavior Survey, acomponent of the Youth Risk BehaviorSurveillance System (<strong>Center</strong>s <strong>for</strong> DiseaseControl <strong>and</strong> Prevention), is a nationalschool-based survey of students inGrades 9 through 12. It contains a seriesof questions, parts of which are nutritionordiet-related. Male students respondingto this survey were significantly morelikely than female students to considerthemselves the ‘‘right weight’’ or‘‘underweight’’ (86 vs. 66 percent).Female students were significantly morelikely than male students to report tryingto lose weight at the time of the survey(44 vs. 15 percent). Over one-fourth offemale students who considered themselvesthe ‘‘right weight’’ reported tryingto lose weight. And female studentswere significantly more likely thantheir male counterparts to report eithercurrently or ever having used inappropriatepractices to lose weight: such as,skipping meals, taking diet pills, orinducing vomiting (40).The Youth Risk Behavior Survey askedstudents in Grades 9 through 12 how oftenthey participated in vigorous activity inthe 2 weeks preceding the survey. Vigorousactivity was defined as ‘‘at least 20minutes of hard exercise that made youbreathe heav<strong>ily</strong> <strong>and</strong> made your heartbeat fast’’ (41). About one-third of allstudents reported being vigorouslyactive three or more times a week, butfemale students were half as likely thanmale students to report regular vigorousactivity (25 vs. 50 percent), <strong>and</strong> AfricanAmerican students were less likely thanWhite or Hispanic students to reportregular vigorous activity (30 vs. 40 <strong>and</strong>35 percent, respectively) (41).Studies of <strong>Nutrition</strong> EducationPrograms----What WorksUSDA conducted research to evaluateadults’ comprehension <strong>and</strong> perceivedusefulness of its food guide <strong>and</strong> todevelop a graphic presentation of thefood guide (43). USDA also conductedresearch to determine the effectivenessof the resulting graphic of the FoodGuide Pyramid with three target audiences:children, consumers with lessthan a high school education, <strong>and</strong> lowincomeconsumers. USDA, in 1991,collaborated with DHHS <strong>and</strong> contractedwith private industry (4) to develop <strong>and</strong>test graphic alternatives (including abowl, shopping cart, <strong>and</strong> dinner plate) tothe Food Guide Pyramid <strong>for</strong> conveyingthe key concepts of variety, proportionality,<strong>and</strong> moderation.Qualitative findings indicated thatchildren preferred the Pyramid graphicto the alternatives tested. They, as well,learned the most in<strong>for</strong>mation from thePyramid. Teachers also preferred thePyramid as a teaching tool, comparedwith the alternatives (4). For the quantitativephase of the research, interviewersquestioned 3,017 individuals, including1,523 children in Grades 2 through 10.The children’s responses to the 60-itemquestionnaire indicated that the Pyramidgraphic conveyed the concepts of variety,proportionality, <strong>and</strong> moderation.Younger children (Grades 2 to 3),1999 Vol. 12 Nos. 3&4 11
The <strong>Center</strong> selectedthe preschool-agegroup (2 to 6 years)as the target audience<strong>for</strong> an adapted foodguide . . . .however, understood variety more sothan proportionality <strong>and</strong> moderation (4).Effectiveness of <strong>Nutrition</strong>Education ProgramsThe Food Guide Pyramid adapted <strong>for</strong>children needed to integrate relevantfindings from a recent comprehensivereview on the effectiveness of methodsused in nutrition education. This reviewrevealed that programs using educationalmethods directed at behavioralchange as a goal were more likely thanother programs to be successful----thatis, they were more likely to result in somebehavioral change than were programsthat focused on only distributingin<strong>for</strong>mation (5).Contento et al. recommended that programsbe behaviorally based <strong>and</strong> appropriatelydesigned <strong>for</strong> the child’s stageof cognitive development (5). Preschool<strong>and</strong> early elementary school-age children(4 to 7 years) need activities that allowthem to modify their environment. Providingfood-based activities <strong>and</strong> havingadults model eating behavior are appropriate<strong>for</strong> this age group. Also, parents’or other caregivers’ involvement withchildren in this age group is an importantfactor contributing to success. Olderelementary school-age children (8 throughabout 11 years) still need to have in<strong>for</strong>mationpresented in concrete terms.Food-classification activities <strong>and</strong> modelingby adults are appropriate <strong>for</strong> this agegroup, <strong>and</strong> involvement with parents<strong>and</strong> the community is still important <strong>for</strong>programs targeted <strong>for</strong> this age group.Adolescents (second decade of life)move from concrete to abstract thinking<strong>and</strong> are able to comprehend more abstractin<strong>for</strong>mation, such as the relationshipbetween diet <strong>and</strong> health----present <strong>and</strong>future. They need activities that encouragecritical thinking, such as exploringthe influence of diet on health <strong>and</strong> theenvironment. With this age group, parents’involvement becomes less important,because adolescents are more likely tobe influenced by their peers than bytheir parents or caregivers (5).The quantity <strong>and</strong> quality of existingnutrition education materials <strong>for</strong> specificage groups of children must alsobe considered when selecting a targetaudience. Recently, Swadener reviewedresearch related to nutrition education<strong>for</strong> preschool-age children (33), <strong>and</strong>Lytle reviewed research related to nutritioneducation <strong>for</strong> school-age children(20). Both found that while many nutritioneducation materials are directedtoward children, improvements <strong>and</strong>follow-up are needed to determinewhether the materials are really effective.Swadener found that many nutritioneducation materials developed <strong>for</strong> preschoolchildrendid not include an evaluationcomponent, many programs werenot conducted <strong>for</strong> a sufficient time toresult in changes in attitudes or behavior,<strong>and</strong> few programs were designed <strong>for</strong>use with children from dysfunctional ormarginally functional families. Lytleconcluded that more tools are needed<strong>for</strong> assessment of change in children’s<strong>and</strong> adolescents’ eating behavior <strong>and</strong>that adolescents, in particular, couldbenefit from exposure to strategies thatmodify behavior. Lytle also found thatmore programs are needed: ones thattarget multi-ethnic groups as well asinvolve families of school-age children.12 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Pros <strong>and</strong> cons of adapting the Food Guide Pyramid <strong>for</strong> use with three groups of childrenProsHave special needs, re: fat, smaller serving sizesPeer pressure not a problemConsPreschool age (2 through 6 years)Educational materials must target parents <strong>and</strong> caregivers, not childdirectlyFat message (children this age need more fat) may confuse parents,because this need is temporaryCan reach them through the Special Supplemental Feeding Program<strong>for</strong> Women, Infants, <strong>and</strong> Children <strong>and</strong> the Child <strong>and</strong> Adult CareFeeding ProgramDevelopmentally a good time to reach (e.g., when food habits are stillbeing <strong>for</strong>med)Can counteract exposure to television advertising of high-caloriefoodsNot as many materials targeting this age group as <strong>for</strong> older childrenElementary school age (7 through 11 years)Think nutrition is important but don’t act on it; they are ‘‘reachable’’ Already a large amount of nutrition education material available <strong>for</strong>this audience (however, not all of it is relevant or appropriate)Beginning to take more responsibility <strong>for</strong> their own food choicesCurrent food guide already meets nutrient needsEasier to reach (through a single classroom teacher) than youngeror older children (where nutrition education may be provided by adiverse group of individuals)More problems meeting nutrient needsNot many materials targeting this audienceMake many of own food choicesAdolescents (12 to 18 years)Current food guide already meets nutrient needsDifficult audience to reach----need different ways to communicatefood guide, not necessar<strong>ily</strong> different food guideNeed more individualized messages----e.g., <strong>for</strong> athletes vs. nonathletesPerhaps can turn weight concerns into motivation <strong>for</strong> change1999 Vol. 12 Nos. 3&4 13
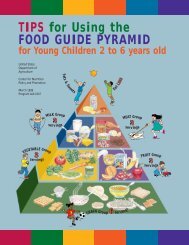
Decision Point----TargetAudience <strong>for</strong> the Food GuidePyramid <strong>for</strong> ChildrenBecause of differences in nutrient needs(23,31,32), current food consumptionpatterns (10,16,37), <strong>and</strong> stages of educationaldevelopment (5), a single foodguide cannot meet the needs of all children2 to 18 years old. Based on children’snutrient needs <strong>and</strong> developmental level,staff of the <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong> identified three age groups<strong>for</strong> which a Pyramid could be developed:• Preschool <strong>and</strong> early elementary age(2 through 6 years)• Elementary school age (7 through11 years)• Middle <strong>and</strong> high school age (12 to18 years)The <strong>Center</strong> staff considered severalfactors when deciding which age groupshould be targeted <strong>for</strong> an adapted foodguide:• Does the existing food guide meetthis group’s dietary needs, or doesthis group have specific nutritional<strong>and</strong> health problems that an adaptedfood guide could help to address?• If the existing food guide meets thegroup’s dietary needs, has it beensuccessful in influencing the group’sbehavior? Is there a need <strong>for</strong> analternate presentation of the existingfood guide to better reach this group?• What nutrition education materialsexist <strong>for</strong> this audience?• What are the educational considerations<strong>for</strong> this group? Will childrenbe able to use the new food guidedirectly? Will they use the materialswith guidance from a parent orcaregiver? Or will the materialsbe developed <strong>for</strong> the parent orcaregiver?• Is there user dem<strong>and</strong> <strong>for</strong> a new foodguide <strong>for</strong> this group?• What is the social effect of thedecision? Will different food guides<strong>for</strong> different ages create confusion?Based on these factors, <strong>Center</strong> stafflisted pros <strong>and</strong> cons <strong>for</strong> developing anadapted food guide <strong>for</strong> each age group(table) <strong>and</strong> considered these issues whenmaking the decision regarding the targetaudience.Implications <strong>and</strong>Recommendations <strong>for</strong> aFood Guide <strong>for</strong> Preschool-AgeChildren (2 to 6 Years)The <strong>Center</strong> selected the preschool-agegroup (2 to 6 years) as the target audience<strong>for</strong> an adapted food guide because thereis a greater need <strong>for</strong> verifying the scientificbasis of the food guide, both froma physiological <strong>and</strong> developmental viewpoint<strong>for</strong> 2- to 6-year-olds than <strong>for</strong> olderchildren. The rationale <strong>for</strong> this conclusionfollows:• Nutrient needs of preschool-agechildren differ from those of olderchildren. The Dietary Guidelines <strong>for</strong>Americans recommend that the levelof dietary fat be gradually decreasedfrom current levels (about 34 percentof calories from fat) to 30 percentof calories by the time the child isabout 5 years old (39). Concernsabout undue food <strong>and</strong> fat restrictions<strong>for</strong> children in this age group, leadingto ‘‘failure to thrive,’’ have beenexpressed by the American Academyof Pediatr<strong>ics</strong> (3). Because the currentFood Guide Pyramid assumes adietary fat intake of 30 percent ofcalories, <strong>Center</strong> staff concluded thatadditional guidance is needed <strong>for</strong>parents <strong>and</strong> caregivers of childrenless than 5 years old.• Following the release of the FoodGuide Pyramid, USDA receivednumerous questions from the ExtensionService; the Dairy Council; theSpecial Supplemental Food Program<strong>for</strong> Women, Infants, <strong>and</strong> Children(WIC); the Child <strong>and</strong> Adult CareFood Program; <strong>and</strong> the media. Theconcern: how to use the food guidewith young children, particularlyregarding children’s need <strong>for</strong> smallerserving sizes.• Developmental concerns regardingfood activities at the preschool levelinclude determining what youngchildren can or should ‘‘learn’’ <strong>and</strong>addressing the physiological <strong>and</strong>emotional issues related to food.Because parents <strong>and</strong> caregivers havea major role in food selection <strong>for</strong>this age group, <strong>Center</strong> staff believedthese children’s attitudes <strong>and</strong> behaviormust also be considered.Adaptation of the food guide <strong>for</strong> thisage group uses the same framework offood groups as the original food guide.Thus the framework blends into laterlearning activities in school whereconcepts are added, <strong>for</strong> example, nutrientcontent of different types of foods;how foods are grown, processed, <strong>and</strong>delivered; how different food itemsare used in different cultures; <strong>and</strong> how‘‘new’’ foods have been historicallyintroduced into the American diet.Using the same framework of foodgroups also makes the new food guidemore practical <strong>for</strong> fam<strong>ily</strong> food managersto use. The process used to adapt thefood guide <strong>for</strong> the preschool <strong>and</strong> earlyelementary-age audience is describedelsewhere in this issue (22,34).14 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
References1. Albertson, A.M., Tobelmann, R.C., <strong>and</strong> Engstrom, A. 1992. Nutrient intakes of 2- to 10-year-old American children: 10-year trends. Journal of the American Dietetic Association92:1492-1496.2. Albertson, A.M. <strong>and</strong> Tobelmann, R.C. 1993. Impact of ready-to-eat cereal consumption onthe diets of children 7-12 years old. Cereal Foods World 38(6):428-431.3. American Academy of Pediatr<strong>ics</strong>, Committee on <strong>Nutrition</strong>. 1998. Statement on cholesterol.Pediatr<strong>ics</strong> 101:141-147.4. Bell Associates, Inc. 1992. An Evaluation of Dietary Guidance Graphic Alternatives.Prepared <strong>for</strong> U.S. Department of Agriculture, Food <strong>and</strong> Consumer Services.5. Contento, I., Balch, G.I., Bronner, Y.L., Paige, D.M., Gross, S.M., Bisignani, L., Lytle, L.A.,Maloney, S.K., White, S.L., Olson, C.M., Swadener, S.S., <strong>and</strong> R<strong>and</strong>ell, J.S. 1995. The effectivenessof nutrition education <strong>and</strong> implications <strong>for</strong> nutrition education policy, programs, <strong>and</strong>research: A review of research. Journal of <strong>Nutrition</strong> Education 27(6):277-422.6. Davies, P.S.W., Gregory, J., <strong>and</strong> White, A. 1995. Energy expenditure in children aged 1.5to 4.5 years: A comparison with current recommendations <strong>for</strong> energy intake. European Journalof Clinical <strong>Nutrition</strong> 49:360-364.7. Dietary Guidelines Advisory Committee. 1995. Report of the Dietary Guidelines AdvisoryCommittee on the Dietary Guidelines <strong>for</strong> Americans. U.S. Department of Agriculture,Agricultural Research Service.8. Dietz, W.H. Jr. <strong>and</strong> Gortmaker, S.L. 1985. Do we fatten our children at the television set?Obesity <strong>and</strong> television viewing in children <strong>and</strong> adolescents. Pediatr<strong>ics</strong> 75:807-812.9. Edelman Public Relations Worldwide. 1995. Report of Focus Groups at Stevens Elementary<strong>and</strong> Poe Middle School. Topline report submitted to International Food In<strong>for</strong>mation Council.10. Federation of American Societies <strong>for</strong> Experimental Biology, Life Sciences ResearchOffice. Prepared <strong>for</strong> the Interagency Board <strong>for</strong> <strong>Nutrition</strong> Monitoring <strong>and</strong> Related Research.1995. Third Report on <strong>Nutrition</strong> Monitoring in the United States: Volume 1. U.S. GovernmentPrinting Office, Washington, DC, 365 pp.11. Fontvielle, A.M., Harper, I.T., Ferraro, R.T., Spraul, M., <strong>and</strong> Ravussin, E. 1993. Da<strong>ily</strong>energy expenditure by five-year-old children, measured by doubly labeled water. Journal ofPediatr<strong>ics</strong> 123:200-207.12. Goran, M.I., Carpenter, W.H., <strong>and</strong> Poehlman, E.T. 1993. Total energy expenditure in4- to 6-year-old children. American Journal of Physiology 264:E706-E711.13. Harris/Scholastic Research. 1989. The Kellogg Children’s <strong>Nutrition</strong> Survey. Conducted<strong>for</strong> the Kellogg Company, Battle Creek, Michigan.14. Joint Working Group of the Canadian Paediatric Society <strong>and</strong> Health Canada. 1993. <strong>Nutrition</strong>Recommendations Update . . . Dietary Fat <strong>and</strong> Children. Ottawa, Ontario: Health Canada,Cat. H39-162/1-1993E. 18 pp.15. Kennedy, E. <strong>and</strong> Goldberg, J. 1995. What are American children eating? Implications <strong>for</strong>public policy. <strong>Nutrition</strong> Reviews 53(5):111-126.1999 Vol. 12 Nos. 3&4 15
16. Kennedy, E. <strong>and</strong> Powell, R. 1997. Changing eating patterns of American children: A viewfrom 1996. Journal of the American College of <strong>Nutrition</strong> 16(6):524-529.17. Krauss, R.K., Deckelbaum, R.J., Ernst, N., Fisher, E., Howard, B.V., Knopp, R.H.,Kotchen, T., Lichtenstein, A.H., McGill, H.C., Pearson, T.A., Prewitt, T.E., Stone, N.J.,Van Horn, L., <strong>and</strong> Weinberg, R. 1996. Dietary Guidelines <strong>for</strong> healthy American adults: Astatement <strong>for</strong> health professionals from the <strong>Nutrition</strong> Committee, American Heart Association.Circulation 94:1795-1800.18. Krebs-Smith, S.M., Cook, A., Subar, A.F., Clevel<strong>and</strong>, L., Friday, J., <strong>and</strong> Kahle, L.L.1996. Fruit & vegetable intakes of children <strong>and</strong> adolescents in the United States. Archives ofPediatric <strong>and</strong> Adolescent Medicine 150:81-86.19. Lauer, R.M., Obarzanek, E., Kwiterovich, P.O., Kimm, S.Y.S., Hunsburger, S.A., Barton,B.A., van Horn, B., Stevens, V.J., Lasser, N.L., Robson, A.M., Franklin, F.A., <strong>and</strong> Simons-Morton, D.G. 1996. Efficacy <strong>and</strong> safety of lowering dietary intake of fat <strong>and</strong> cholesterol inchildren with elevated low-density lipoprotein cholesterol: The Dietary Intervention Study inChildren (DISC). Journal of the American Medical Association 273:1429-1435.20. Lytle, L.A. 1994. <strong>Nutrition</strong> Education <strong>for</strong> School-Aged Children: A Review of Research.Report prepared <strong>for</strong> U.S. Department of Agriculture, Food <strong>and</strong> Consumer Service.21. Macro International. 1995. Adolescent Consumers’ Attitudes Toward Calcium Education<strong>and</strong> Proposed Educational Materials: Focus Groups Report. Prepared <strong>for</strong> the U.S. Food <strong>and</strong>Drug Administration.22. Marcoe, K.L. 1999. Technical research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> Young Children.<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):18-32.23. National Academy of Sciences, National Research Council, Food <strong>and</strong> <strong>Nutrition</strong> Board.1989. Recommended Dietary Allowances (10th ed.). National Academy Press, Washington, DC.24. National Cholesterol Education Program. 1991. Report of the Expert Panel on BloodCholesterol Levels in Children <strong>and</strong> Adolescents. Bethesda, MD: National Institutes of Health,NIH Publication no. 91-2732. 119 pp.25. Nicklas, T.A., Webber, L.S., Koschak, M.L., <strong>and</strong> Berenson, G.S. 1992. Nutrient adequacyof low fat intakes <strong>for</strong> children: The Bogalusa Heart Study. Pediatr<strong>ics</strong> 89(2):221-228.26. Niinikoski, H., Lapinleimu, H., Viikari, J., Ronnemaa, T., Jokinen, E., Seppanen, R.,Terho, P., Tuominen, J., Valimaki, I., <strong>and</strong> Simell, O. 1997. Growth until 3 years of age in aprospective, r<strong>and</strong>omized trial of a diet with reduced saturated fat <strong>and</strong> cholesterol. Pediatr<strong>ics</strong>99(5):687-694.27. Odgen, C.L., Troiano, R.P., Briefel, R.R., Kuczmarski, R.J., Flegal, K.M., <strong>and</strong> Johnson,C.L. 1997. Prevalence of overweight among preschool children in the United States, 1971through 1994. Pediatr<strong>ics</strong> 99(4):e1.28. Oliveria, S.A., Ellison, R.C., Moore, L.L., Gillman, M.W., Garrahie, E.J., <strong>and</strong> Singer,M.R. 1992. Parent-child relationships in nutrient intake: The Framingham Children’s Study.American Journal of Clinical <strong>Nutrition</strong> 56:593-598.29. Shea, S., Basch, C.E., Stein, A.D., Contento, I.R., Irigoyen, M., <strong>and</strong> Zybert, P. 1993. Isthere a relationship between dietary fat <strong>and</strong> stature or growth in children three to five years ofage? Pediatr<strong>ics</strong> 92(4):579-586.16 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
30. Shugoll Research. 1992. Children’s <strong>Nutrition</strong> Label Focus Group Study. Report prepared<strong>for</strong> KIDSNET, Inc., Washington, DC.31. St<strong>and</strong>ing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food <strong>and</strong><strong>Nutrition</strong> Board, Institute of Medicine. 1997. Dietary Reference Intakes <strong>for</strong> Calcium, Phosphorus,Magnesium, Vitamin D, <strong>and</strong> Fluoride. Washington, DC. National Academy Press.32. St<strong>and</strong>ing Committee on the Scientific Evaluation of Dietary Reference Intakes, Food <strong>and</strong><strong>Nutrition</strong> Board, Institute of Medicine. 1998. Dietary Reference Intakes <strong>for</strong> Folate, Other BVitamins, <strong>and</strong> Choline. Washington, DC. National Academy Press.33. Swadener, S.S. 1994. <strong>Nutrition</strong> Education <strong>for</strong> Preschool Children: A Review of Research.Report prepared <strong>for</strong> U.S. Department of Agriculture, Food <strong>and</strong> Consumer Service.34. Tarone, C. 1999. Focus group research on adapting the Food Guide Pyramid <strong>for</strong> YoungChildren. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):33-44.35. Tonstad, S. <strong>and</strong> Sivertsen, M. 1997. Relation between dietary fat <strong>and</strong> energy <strong>and</strong> micronutrientintakes. Archives of Diseases of Childhood 76(5):416-442.36. Troiano, R.P., Flegal, K.M., Kuczmarski, R.J., Campbell, S.M., <strong>and</strong> Johnson, C.L. 1995.Overweight prevalence <strong>and</strong> trends <strong>for</strong> children <strong>and</strong> adolescents: The National Health <strong>and</strong><strong>Nutrition</strong> Examination Surveys, 1963 to 1991. Archives of Pediatric <strong>and</strong> Adolescent Medicine149:1085-1091.37. U.S. Department of Agriculture, Agricultural Research Service. 1998. Food <strong>and</strong> NutrientIntakes by Individuals in the United States by Sex <strong>and</strong> Age, 1994-96, Nationwide Food Surveys.Report No. 96-2. 197 pp.38. U.S. Department of Agriculture, Human <strong>Nutrition</strong> In<strong>for</strong>mation Service. 1992. The FoodGuide Pyramid. Home <strong>and</strong> Garden Bulletin No. 252.39. U.S. Department of Agriculture <strong>and</strong> U.S. Department of Health <strong>and</strong> Human Services. 1995.<strong>Nutrition</strong> <strong>and</strong> Your Health: Dietary Guidelines <strong>for</strong> Americans (4th ed.). U.S. Department ofAgriculture. Home <strong>and</strong> Garden Bulletin No. 232.40. U.S. Department of Health <strong>and</strong> Human Services. 1991. Body-weight perceptions <strong>and</strong>selected weight-management goals <strong>and</strong> practices of high school students----United States,1990. Morbidity <strong>and</strong> Mortality Weekly Reports 40:741,747-750.41. U.S. Department of Health <strong>and</strong> Human Services. 1992. Vigorous physical activity amonghigh school students----United States, 1990. Morbidity <strong>and</strong> Mortality Weekly Reports 41:33-35.42. U.S. Department of Health <strong>and</strong> Human Services. 2000. Healthy People 2010 (ConferenceEdition in Two Volumes). Washington, DC.43. Welsh, S.O., Davis, C., <strong>and</strong> Shaw, A. 1993. USDA’s Food Guide: Background <strong>and</strong>Development. U.S. Department of Agriculture. HNIS Miscellaneous Publication No. 1514.44. Williams, C.L. 1995. Importance of dietary fiber in childhood. Journal of the AmericanDietetic Association 95:1140-1146, 1149.45. Zizza, C.A. <strong>and</strong> Powell, R. 1996. Characterist<strong>ics</strong> distinguishing adolescents by fruitconsumption. Journal of the American Dietetic Association 96:A-91.1999 Vol. 12 Nos. 3&4 17
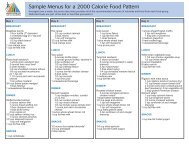
Technical Research <strong>for</strong> theFood Guide Pyramid <strong>for</strong>Young ChildrenKristin L. Marcoe<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>This article describes the technical research <strong>for</strong> the Food Guide Pyramid <strong>for</strong>Young Children. Composites <strong>for</strong> food groups <strong>and</strong> subgroups were developedusing food intake data <strong>for</strong> children 2 to 6 years old. Data were from theContinuing Survey of Food Intakes by Individuals 1989-91. The compositeswere used in creating 1,300- <strong>and</strong> 1,600-calorie Food Guide Pyramid dietpatterns. For children 4 to 6 years old, the 1,600-calorie pattern met allnutrient requirements, except <strong>for</strong> vitamin E. The 1,300-calorie pattern providedthe RDA <strong>for</strong> most nutrients <strong>for</strong> 2- to 3-year-olds <strong>and</strong> 4- to 6-year-olds.The major exceptions were iron <strong>and</strong> zinc <strong>for</strong> both age groups <strong>and</strong> copper<strong>and</strong> vitamin E <strong>for</strong> the 4- to 6-year-olds. When breakfast cereals <strong>for</strong>tifiedwith iron <strong>and</strong> zinc were used in the grain composites, the patterns providedrecommended levels of these nutrients. Children could improve their diet bymaking different food choices, in particular, by eating more dark-green <strong>and</strong>deep-yellow vegetables; legumes; whole grains; <strong>and</strong> lean meat, poultry, orfish.The Food Guide Pyramid<strong>for</strong> Young Children ages2 to 6 years is a nutritioneducation tool to helpteach healthful eating concepts to youngchildren. The technical research conductedin developing <strong>and</strong> documentingthe research base <strong>for</strong> this food guidefollowed procedures similar to thosedescribed in the development <strong>and</strong>documentation of the original foodguide (1,9). Food selections <strong>and</strong> servingsizes reported <strong>for</strong> young children, ina national food consumption survey,were incorporated into diet patternsbased on the Food Guide Pyramid todetermine whether such patterns wouldmeet nutritional goals.A composite was developed <strong>for</strong> eachPyramid food group (e.g., meat, poultry,fish) or subgroup (e.g., whole grain).Composites were based on children’sactual food choices <strong>and</strong> reflected therelative use of individual foods withinthe group or subgroup. An example: thecomposite <strong>for</strong> deep-yellow vegetablesreflected children’s consumption of89 percent as carrots <strong>and</strong> 11 percent asother deep-yellow vegetables. A nutrientprofile was then calculated <strong>for</strong> eachcomposite, after which composites<strong>and</strong> their nutrient profiles were usedto calculate expected nutrient levels in1,300- <strong>and</strong> 1,600-calorie diet patternsbased on the Food Guide Pyramid.The nutrient totals were then analyzedto determine whether children’s nutrientrequirements could be met by dietpatterns that con<strong>for</strong>m to Pyramid recommendations<strong>and</strong> that consist of thefoods most commonly eaten by children.18 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
MethodsData SourcesData on 3-day food <strong>and</strong> nutrient intakesreported in the Continuing Survey ofFood Intakes by Individuals (CSFII)1989-91 <strong>for</strong> 1,053 children 2 to 6 yearsold were used in this study. This dataset was used because when work wasstarted, the data set offered the largestnumber of individuals <strong>and</strong> days <strong>for</strong>analysis. Sample weights were appliedto provide estimates that were representativeof the population. The datathat were used to calculate the nutrientprofiles of the composites <strong>for</strong> the foodgroups <strong>and</strong> subgroups came from theU.S. Department of Agriculture’s(USDA) Nutrient Data Base <strong>for</strong>Individual Intake Surveys, Release 7(1991).The Food Guide Servings Data Basewas used to report the amounts of foodconsumed as numbers of food guideservings. USDA’s <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong><strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong> (CNPP) developedthis data base by using the foodsreported in the CSFII 1989-91. TheFood Guide Servings Data Base consistsof food-item descriptions <strong>and</strong> thenumber of Pyramid servings per 100grams of food. Servings data are provided<strong>for</strong> the 5 major food groups <strong>and</strong>21 subgroups identified in the FoodGuide Pyramid.Most foods, including mixed dishes,were broken down into ingredient components,<strong>and</strong> their food group servingswere calculated <strong>for</strong> more than one foodgroup. When a food code’s typicalserving size, defined in the SurveyCode Book <strong>for</strong> CSFII 1989-91 <strong>and</strong>based generally on median servingsizes reported in USDA food consumptionsurveys, provided less than onefourthof a serving of a Pyramid foodgroup or subgroup, it was usually notcounted. For example, a serving ofoatmeal raisin cookies provided lessthan one-fourth of a Pyramid servingof raisins, so those raisins were notcounted toward fruit servings. Thesesmall amounts were not countedbecause one objective of the originalfood guidance system was ‘‘usability.’’It is unrealistic to expect Americans to‘‘count’’ small amounts of some foodstoward food group servings. However,if several ‘‘other vegetables’’ liketomatoes <strong>and</strong> onions were in smallamounts in a mixture, <strong>and</strong> these amountstogether added up to at least one-fourthserving, these ‘‘other vegetables’’ werecounted toward vegetable servings.ProceduresCNPP began the research process bybreaking down the foods that wereconsumed by children 2 to 6 years old,as reported in the CSFII 1989-91, intonumbers of food group <strong>and</strong> subgroupservings. The Food Guide ServingsData Base was used <strong>for</strong> this process.To identify specific food components,CNPP staff reviewed food codes thatcontributed food guide servings.All food items with similar foodcomponents were grouped in the sameitem-group. For example, broccoli soup<strong>and</strong> broccoli casserole both containedcooked broccoli <strong>and</strong> so were placedin the item-group <strong>for</strong> cooked broccoliwithin the subgroup <strong>for</strong> dark-greenvegetables. A composite was thenconstructed by summing intakes fromall the item-groups within a food group,with each item-group being weightedby the numbers of servings reported<strong>for</strong> children 2 to 6 years old. Then thepercentage contributed by each itemgroupin the food group or subgroupwas calculated. The total number ofservings of cooked broccoli consumed,<strong>for</strong> example, was divided by the totalnumber of servings of dark-greenvegetables consumed. This calculationproduced the percentage of the composite<strong>for</strong> dark-green vegetables that wascooked broccoli. Any item-group totalingless than 1 percent of the compositewas combined with another item-group,based on the similarity in nutrientcomposition or its use in meals.A food code most representative of anitem-group was then selected to representeach food-item group in each ofthe composites. The nutrient values ofthese food codes were used to calculatethe nutrient profiles of the composites.In developing the original nutrientprofiles <strong>for</strong> the food groups <strong>and</strong> subgroups,researchers included foodswith the least amount of fat <strong>and</strong> withoutadded sugars; thus, the originalphilosophical goal of flexibility <strong>for</strong> thefood guide was met. The food guidewas used to show consumers how toobtain nutrients while allowing themflexibility to choose sources of fat <strong>and</strong>added sugars within the fat <strong>and</strong> calorielimits specified (9). In addition, theFood Guide Pyramid is an educationaltool to help put the Dietary Guidelinesinto practice (8).To minimize fat, added sugars, <strong>and</strong>sodium, CNPP staff used the <strong>for</strong>m ofthe food item that was lowest in thesecomponents. For example, the deepyellowvegetable subgroup containedthe item-group <strong>for</strong> sweet potatoes. Torepresent the latter in the composite,CNPP used the code <strong>for</strong> a baked sweetpotato without added fat----despite thefact that children usually eat c<strong>and</strong>iedsweet potatoes. For most vegetable <strong>and</strong>cooked-grain item-groups, CNPP usedfood codes that specified ‘‘no saltadded in preparation.’’ In a few cases,CNPP used the salted <strong>for</strong>m to representpopular vegetables that are canned.Estimates of the percentage selected1999 Vol. 12 Nos. 3&4 19
. . . young children atesomewhat differenttypes <strong>and</strong> amountsof food items withineach food group <strong>and</strong>subgroup than didthe total population.in canned <strong>for</strong>m were calculated fromdata of the food supply (4).Non-<strong>for</strong>tified ready-to-eat <strong>and</strong> cookedbreakfast cereals were used in boththe composites <strong>for</strong> whole grains <strong>and</strong>enriched grains. Hence nutrient profilesof the composites do not overestimatethe nutrients <strong>for</strong> children who do noteat <strong>for</strong>tified breakfast cereals. Nutrientsadded at st<strong>and</strong>ard enrichment levels,as in enriched bread, were included inthe nutrient profiles <strong>for</strong> the composites.Folate <strong>for</strong>tification was not m<strong>and</strong>atedby the Government at the time theCSFII 1989-91 was conducted, so itwas not reflected in any of the nutrientprofiles <strong>for</strong> grain products.Once CNPP chose the food code torepresent each item-group, we calculatedgrams of the food code <strong>and</strong> correspondingnutrient values <strong>for</strong> its portionof the composite serving. Nutrient valueswere then summed across all items inthe food group or subgroup to determinethe composite’s nutrient profileper serving.Composites were not developed <strong>for</strong> themeat alternates (eggs, nuts <strong>and</strong> seeds)or <strong>for</strong> the milk, yogurt, <strong>and</strong> cheesegroup. The nutrient profiles of a foodgroup or subgroup reflect proportionatelythe nutrient content of the foodswithin them; consequently, the nutrientprofile of a food group or subgroupmost reflects the nutrient content ofthe most frequently consumed foodswithin that group.Nutrient profiles <strong>for</strong> the meat alternateswere represented by the nutrients inone large boiled egg <strong>and</strong> 2 tablespoonsof peanut butter, each of which countsas 1 ounce from the meat, poultry, fishgroup. Peanut butter was 90 percent ofyoung children’s servings of nuts <strong>and</strong>seeds in the CSFII 1989-91; thus, peanutbutter’s nutrient profile was used insteadof calculating a composite of allthe different nuts <strong>and</strong> seeds that wereconsumed in small quantities by youngchildren.All legumes were counted as vegetablesin the earlier research on Pyramid foodpatterns (1) <strong>and</strong> so were counted similarlyin this research project. One-halfcup of cooked legumes may be countedas 1 ounce of meat, poultry, or fishrather than 1 serving of vegetables.The nutrient profile <strong>for</strong> the milk, yogurt,<strong>and</strong> cheese group was represented by1 cup of nonfat milk, except <strong>for</strong> vitaminA. The amount of vitamin A used wasthe 76 RE per cup found in whole milk,instead of the 149 RE per cup foundin <strong>for</strong>tified nonfat milk. Thus overestimationof vitamin A was avoided<strong>for</strong> those who consumed non-<strong>for</strong>tifiedwhole milk products.The data on food intake, which wereused to develop the composites, wereexamined to identify the most popularfoods (at the food code level) <strong>and</strong>preparation styles in each item-group.Amounts reported eaten were alsoanalyzed. For each item-group, theaverage number of servings per reportwas calculated. This was the averagequantity of a specified food that waseaten by consumers during an eatingoccasion (at a single time). Then, theaverage number of servings per reportwas calculated <strong>for</strong> each food group orsubgroup.The food-group composites <strong>and</strong> nutrientprofiles <strong>for</strong> young children were comparedwith another set of compositesthat were developed <strong>for</strong> all individualsages 2 years <strong>and</strong> older who provided3 days of data in the CSFII 1989-91(N=11,488).20 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Composites <strong>and</strong> their nutrient profilesindicated that while children do eatsomewhat differently from the rest ofthe population of all individuals ages 2years <strong>and</strong> older, few substantial differencesresulted in the expected nutrientprofile of a composite serving of anyof the food groups or subgroups.Next, the composites <strong>and</strong> nutrientprofiles were used in Food GuidePyramid diet patterns that includedadded fat <strong>and</strong> added sugars. In thesepatterns, a fat composite was used torepresent ‘‘discretionary’’ fat added tothe diet above what would be foundin lean meats <strong>and</strong> <strong>for</strong>ms of the othercomposite foods that were lowest infat. For example, the fat in cakes <strong>and</strong>the margarine spread on bread arediscretionary fats. The nutrient profile<strong>for</strong> the fat composite was based on thepercentages of different animal <strong>and</strong>vegetable fats in the food supply from1989 to 1991 (7).‘‘Added sugars’’ are added to the dietwhen a person either chooses foodsthat contain added sugars as ingredients(e.g., cookies) or adds some <strong>for</strong>m ofsugar (e.g., pancake syrup) to foodsat the table. The nutrient profile <strong>for</strong>added sugars was represented by thenutrients in 1 teaspoon of granulatedsugar.CNPP analyzed the Food Guide Pyramiddiet patterns to determine whetheryoung children’s nutrient requirementswould be met by a diet pattern set at acalorie level close to what children eat<strong>and</strong> based on their food choices withinfood groups. The nutritional objective<strong>for</strong> food energy was to be within therange of the Recommended EnergyIntake (REI) <strong>for</strong> 2- to 6-year-olds.Protein, vitamins, <strong>and</strong> minerals wereto meet the Recommended DietaryAllowances (RDA) <strong>for</strong> young children.The objective <strong>for</strong> dietary fat <strong>for</strong> youngchildren was that after age 2, childrenshould gradually adopt a diet so that itcontains no more than 30 percent ofcalories from fat by the time they are5 years old (8). For this study, the fatlevel was to be the same as the CSFII1989-91 level <strong>for</strong> 2- to 3-year-old children(34 percent of calories from fat)<strong>and</strong> was to decrease in older age groupsto 30 percent of calories by age 5. TheDietary Guidelines <strong>for</strong> Americans alsoadvise that saturated fat be less than 10percent of calories (8). For 2- to 3-yearoldchildren, saturated fat was targetedat the consumption level of 13.6 percentof calories, <strong>and</strong> <strong>for</strong> the older preschooler(5 to 6 years old), saturatedfat was targeted at less than 10 percentof calories. Cholesterol was to average300 milligrams or less per day (3).Food Guide Pyramid diet patterns wereto provide a minimum of ‘‘age (in years)plus 5’’ grams of dietary fiber, recommendedby the American Health Foundation(10). The objective <strong>for</strong> sodiumwas that diet patterns were to provide2,400 milligrams or less per day (3).Diet patterns could include added sugarsin order to meet the targeted calorielevels of 1,300 or 1,600, after caloriesfrom servings of the food groups <strong>and</strong>added fats were totaled.ResultsCompositesTable 1 summarizes the food group<strong>and</strong> subgroup composites <strong>for</strong> youngchildren <strong>and</strong> <strong>for</strong> all individuals ages 2<strong>and</strong> older. For example, in the subgroup<strong>for</strong> dark-green vegetables, cookedbroccoli was about 74 percent of thereported food guide servings of darkgreenvegetables <strong>for</strong> young children;cooked broccoli was 52 percent ofsuch servings <strong>for</strong> all individuals.Table 2 lists the amounts of selectednutrients per serving of the composite<strong>for</strong> each food group <strong>and</strong> subgroup <strong>for</strong>the young child <strong>and</strong> <strong>for</strong> all individuals.Despite differences in food selection,as shown in the composites in table 1<strong>and</strong> described later in this study, thedifferences in the nutrient profilesbetween the young child’s <strong>and</strong> allindividuals’ composites were relativelyminor. As expected, young childrenate somewhat different types <strong>and</strong>amounts of food items within eachfood group <strong>and</strong> subgroup than did thetotal population.Fruit. Children obtained much of theirfruit servings in juice <strong>for</strong>m.Young children consumed a largeshare of their fruit servings as juices----nearly 47 percent, compared with 35percent <strong>for</strong> all individuals (table 1). Thelargest single component of children’sfruit composite was orange juice (23percent), followed by apple juice (20percent).Higher percentages of apple juice <strong>and</strong>grape juice in the composite <strong>for</strong> childrenthan in the composite <strong>for</strong> all individualscontributed to the higher carbohydrate<strong>and</strong> calorie levels in children’s nutrientprofile <strong>for</strong> fruit (table 2). The smalleramount of orange juice in the children’sfruit composite, compared with thecomposite <strong>for</strong> all individuals, waslikely related to the lower potassium,vitamin C, <strong>and</strong> folate levels in thechildren’s nutrient profile. The absenceof cantaloupe in the children’s compositewas associated with a lower vitamin Avalue <strong>for</strong> the children’s fruit composite,compared with that <strong>for</strong> all individuals.1999 Vol. 12 Nos. 3&4 21
Table 1. Food group composites <strong>for</strong> young children <strong>and</strong> all individuals 1AllAllFood group Item-group Child indiv. Food group Item-group Child indiv.PercentPercentFruit Orange juice 22.9 24.3 Legume Kidney beans 17.6 19.6Grapefruit juice - 2.2 Chickpeas - 1.6Apple juice 19.9 6.8 Soybeans - 1.4Grape juice 3.8 1.7 White beans 30.8 26.9Total juice 46.6 35.0 Black beans 3.7 2.7Pinto beans 34.7 32.2Orange, raw 3.9 3.7 Lima beans 5.9 6.7Grapefruit, raw - 2.8 Split peas 3.3 3.8Strawberries 2.1 4.2 Lentils 1.1 1.5Cantaloupe - 3.0 Cowpeas 2.8 3.6Watermelon 4.4 4.4Apple, raw 9.2 10.0 Starchy Corn 18.2 13.5Banana 8.4 10.1 vegetable Potatoes, boiled 66.9 64.9Grapes 4.7 5.2 Potatoes, baked 6.7 12.8Peach, raw 1.8 3.9 Green peas 8.2 8.8Plums, raw 1.3 2.0Raisins 1.6 1.5 Other Tomatoes, ck 40.1 25.5Total raw 37.4 50.8 vegetable Tomatoes, raw 8.1 11.3Tomato juice - 1.4Applesauce 7.1 3.2 Total tomatoes 48.2 38.2Apple, ck* - 1.3Peach, ck, cnd* 5.3 5.5 Green beans, ck 19.1 10.9Pears, ck, cnd 1.5 2.0Pineapple, ck, cnd 2.0 2.4 Iceberg lettuce 11.6 21.6Total canned 15.9 14.4 Cucumber, raw 1.9 3.1Onions, raw - 1.8Dark-green Broccoli, ck 73.9 51.6 Celery, raw 2.1 2.3vegetable Broccoli, raw 2.2 6.7 Green pepper, raw - 1.8Total broccoli 76.1 58.3 Cabbage, raw 4.0 3.6Total raw vegetable 19.6 34.2Spinach, ck 14.1 12.4Mustard greens, ck - 3.0 Celery, ck 1.8 1.2Collards, ck 2.7 7.8 Onions, ck 2.8 2.5Kale, ck 3.0 1.9 Mushrooms, ck 1.5 2.3Turnip greens, ck 2.5 4.8 Cabbage, ck 3.0 4.2Total ck greens 22.3 29.9 Mung bean sprouts 2.4 1.3Cauliflower, ck - 1.4Romaine, etc., raw 1.7 9.9 Zucchini, ck 1.6 2.5Spinach, raw - 2.0 Asparagus, ck - 1.4Total raw greens 1.7 11.9 Total other ck 13.1 16.8Deep-yellow Carrots, ck 41.8 48.5vegetable Carrots, raw 47.0 37.3Total carrots 88.8 85.8Pumpkin, ck 2.3 1.3Sweet potato, ck 5.1 9.2Winter squash, ck 3.7 3.8Total other DY* 11.1 14.322 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 1. ContinuedAllAllFood group Item-group Child indiv. Food group Item-group Child indiv.PercentPercentWhole grain WW* bread 33.2 35.6 Meat,Rye bread - 4.2 poultry, Beef, fresh 18.6 21.4Oatmeal bread 2.5 3.3 fish Pork, fresh 6.2 7.2WW quick bread 2.1 2.4 Pork, cured 2.9 3.2Total breads 37.8 45.5 Lamb 0.7 1.1Total meat cuts 28.4 32.9WW crackers 4.2 2.8Corn tortilla 9.5 11.6 Ground beef 21.5 18.8Popcorn 3.6 5.2Brown rice - 1.6 Beef lunchmeats 8.1 3.6Total snacks/other 17.3 21.2 Pork lunchmeats 4.4 4.9Total lunchmeat 12.5 8.5WW cereal, RTE* & ck 11.5 16.9Oatmeal, ck 15.9 8.4 Liver 0.3 0.5Oat RTE cereals 17.5 8.0Total cereals 44.9 33.3 Chicken 23.0 21.5Turkey 3.9 5.1Enriched White bread 35.1 35.4 Total poultry 26.9 26.6grain French bread 1.4 4.0English muffins 1.1 2.4 Lean finfish 3.3 4.3Flour tortilla 1.4 2.3 Fatty finfish 1.6 1.7Enr* crackers 4.2 2.8 Finfish, cnd 4.5 4.2Total bread/crx* 43.2 46.9 Shellfish 1.0 2.8Total fish 10.4 13.0Enr quick breads 7.1 5.9Biscuit 1.6 2.7Cornbread 2.4 3.3Total quick breads 11.1 11.9Pasta, noodles 13.6 11.5White rice 5.3 6.1Grits 1.5 1.0Total pasta, rice 20.4 18.6Enr flour desserts 14.4 17.8Corn RTE cereals 8.2 3.7Rice RTE cereals 2.7 1.1Total cereals 10.9 4.81 Children 2 to 6 years old <strong>and</strong> all individuals ages 2 years <strong>and</strong> older.- Item-group had
Table 2. Nutrient profiles <strong>for</strong> food group composites <strong>and</strong> milk: Nutrient values per serving <strong>for</strong>young children <strong>and</strong> all individuals 1NutrientDark-greenvegetableChildAllindiv.Deep-yellowvegetableChildAllindiv.ChildLegumeAllindiv.ChildStarchyvegetableAllindiv.ChildOthervegetableAllindiv.Calories, kcal 24 21 34 37 108 109 75 78 21 19Sodium, mg 29 26 43 44 164 155 27 24 100 74Potassium, mg 278 244 205 207 372 368 260 278 205 184Protein, g 2.6 2.1 0.8 0.8 7.2 7.3 1.9 2.0 1.0 1.0Fat, g 0.3 0.3 0.1 0.1 0.3 0.5 0.3 0.2 0.3 0.2Saturated fat, g 0.0 0.0 0.0 0.0 0.1 0.1 0.0 0.0 0.0 0.0Mono.* fat, g 0.0 0.0 0.0 0.0 0.0 0.1 0.1 0.0 0.0 0.0Poly.* fat, g 0.1 0.1 0.1 0.1 0.2 0.2 0.1 0.1 0.1 0.1Cholesterol, mg 0 0 0 0 0 0 0 0 0 0Carbohydrate, g 4.4 3.8 7.9 8.7 19.7 19.5 17.3 17.9 4.4 3.9Fiber, g 2.3 2.0 2.2 2.2 5.6 5.7 2.1 2.0 1.3 1.2Vitamin A, RE 239 238 1685 1723 0 0 6 6 45 38Vitamin C, mg 55 43 5 6 1 1 7 7 12 12Folate, ug 57.9 56.1 10.8 11.4 82.1 84.0 16.6 15.8 16.8 20.6Vitamin B 12, ug 0.0 0.0 0.0 0.0 0.0 0.0 0.0 0.0 0.0 0.0Calcium, mg 55 52 20 21 43 42 7 8 25 20Magnesium, mg 29.3 25.4 9.9 10.3 43.2 43.1 20.0 20.6 12.8 11.1Iron, mg 1.10 0.97 0.39 0.40 2.25 2.27 0.46 0.54 0.61 0.52Zinc, mg 0.38 0.32 0.18 0.19 0.93 0.93 0.32 0.32 0.19 0.18Dark-green vegetable. Broccoli wasthe predominant vegetable in thiscomposite <strong>for</strong> children. Of all thecomposites, the one <strong>for</strong> dark-greenvegetables had the highest vitamin-Cvalue per serving.Cooked broccoli was the largest (74percent) component <strong>and</strong> cooked spinachwas the second largest (14 percent)component of the composite <strong>for</strong> darkgreenvegetables (table 1). Thus thehigh percentage of broccoli helps toexplain the high value of vitamin Cper serving of this composite: 55 mg(table 2). Children consumed muchless cooked greens, raw broccoli, <strong>and</strong>romaine than did all individuals (table 1).Deep-yellow vegetable. This compositewas mostly carrots, <strong>and</strong> it provided thehighest amount of vitamin A of anycomposite.Most (89 percent) of the children’sdeep-yellow vegetable composite wascarrots (table 1). Children ate more rawcarrots than cooked carrots. Eaten primar<strong>ily</strong>in c<strong>and</strong>ied <strong>for</strong>m, sweet potatoesranked a distant second in the composite.One serving of the deep-yellow vegetablecomposite provided 1,685 RE vitamin A<strong>for</strong> children (table 2).Legume. Pinto beans accounted <strong>for</strong>the highest percentage of the children’scomposite <strong>for</strong> legumes. Of all thecomposites, this one contained themost calories <strong>and</strong> fiber per serving.Pinto beans ranked first (35 percent<strong>for</strong> children) in the legume composite(table 1). The top food codes in theitem-group <strong>for</strong> pinto beans were pintobeans without fat <strong>and</strong> refried beans24 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 2. ContinuedNutrientChildMeat, poultry, fishFruit Whole grain Enriched grain (per ounce) Milk 2Allindiv.ChildAllindiv.ChildAllindiv.ChildAllindiv.1 cupnonfatCalories, kcal 74 68 80 78 86 83 56 55 86Sodium, mg 3 2 60 69 104 115 82 67 126Potassium, mg 237 245 60 56 30 31 89 88 406Protein, g 0.7 0.8 2.8 2.6 2.3 2.3 7.7 7.7 8.4Fat, g 0.2 0.2 1.2 1.1 1.1 1.1 2.5 2.4 0.4Saturated fat, g 0.1 0.1 0.2 0.2 0.2 0.3 0.9 0.9 0.3Mono. fat, g 0.0 0.0 0.4 0.4 0.5 0.5 1.0 1.0 0.1Poly. fat, g 0.1 0.1 0.4 0.4 0.3 0.3 0.2 0.2 0.0Cholesterol, mg 0 0 0 0 2 2 22 24 4Carbohydrate, g 18.3 16.8 14.9 15.0 16.3 15.5 0.2 0.1 11.9Fiber, g 1.1 1.2 2.1 2.0 0.6 0.6 0.0 0.0 0.0Vitamin A, RE 12 28 2 2 2 2 9 18 76Vitamin C, mg 24 30 0 0 0 0 1 1 2Folate, ug 23.8 26.9 7.4 7.8 6.5 6.9 2.3 2.4 12.7Vitamin B 12, ug 0.0 0.0 0.0 0.0 0.0 0.0 0.5 0.6 0.9Calcium, mg 13 13 19 20 23 26 4 4 302Magnesium, mg 12.3 13.5 24.6 23.0 7.4 7.4 6.8 7.0 27.8Iron, mg 0.34 0.27 0.81 0.76 0.80 0.80 0.55 0.55 0.10Zinc, mg 0.08 0.10 0.54 0.50 0.20 0.21 1.11 1.10 0.981 Children 2 to 6 years old <strong>and</strong> all individuals ages 2 years <strong>and</strong> older.2 A composite was not developed <strong>for</strong> the milk group. The nutrient profile was based on nonfat fluid milk.*Abbreviations: Mono. -- monounsaturated; Poly. -- polyunsaturated.with added fat. White beans (eatenmostly in pork <strong>and</strong> beans/baked beans)<strong>and</strong> kidney beans (eaten mostly in chilicon carne with beans) were, respectively,the second <strong>and</strong> third largest itemgroups.Legumes contributed the mostcalories <strong>and</strong> dietary fiber per serving ofall the composites; <strong>for</strong> children, onelegume serving provided 108 calories<strong>and</strong> 5.6 g fiber (table 2). Legumes alsoprovided the most copper per servingof all the composites, 0.20 mg.Starchy vegetable. Fried potatoeswere the starchy vegetable mostcommonly eaten by young children.White potatoes were the primaryconstituent of the composite <strong>for</strong> starchyvegetables (table 1); they were mostoften eaten with added fat----as potatochips <strong>and</strong> French fries. Because thecomposite was created using the <strong>for</strong>mof the food lowest in fat, boiled potatoeswere chosen as a proxy <strong>for</strong> fried potatoes.The smaller amount of baked potatoesin the children’s composite, comparedwith that <strong>for</strong> all individuals, contributedto a lower potassium value in children’snutrient profile (table 2). The secondlargest item-group in this compositewas corn (table 1).Other vegetable. Almost half of children’sservings of ‘‘other vegetables’’ were oftomatoes. This composite had one ofthe smallest servings per report (0.5),because the foods in this subgroupwere used in small amounts in manymixed dishes.Tomatoes were the primary component(48 percent) of the composite <strong>for</strong> other1999 Vol. 12 Nos. 3&4 25
Across all the foodgroups <strong>and</strong> subgroups,childrentended to havesmaller servingsizes than did allindividuals.vegetables; a higher percentage of itscooked <strong>for</strong>m was consumed, comparedwith its raw <strong>for</strong>m (table 1). Most of theservings of the cooked <strong>for</strong>m were eatenas ingredients in grain mixtures. Themain sources of raw tomatoes, otherthan those eaten by themselves, wereMexican mixtures (taco/tostada) <strong>and</strong>hamburger s<strong>and</strong>wiches. The large amountof cooked tomatoes, represented ascanned in the composite, was themajor contributor to the 100 mg sodium<strong>and</strong> 205 mg potassium per compositeserving (table 2). The second largestitem-group in the other vegetable composite<strong>for</strong> children was cooked greenbeans (19 percent) (table 1). Lettucerepresented 12 percent of the children’scomposite, <strong>and</strong> the most frequentlyconsumed food was plain lettuce. Onecomposite serving of other vegetablesprovided 12 mg vitamin C, second tothe dark-green vegetable subgroup,55 mg per serving (table 2).Whole grain. About 45 percent of thiscomposite was ready-to-eat <strong>and</strong>cooked cereals; most were <strong>for</strong>tified.Whole-grain cereals were the largestcomponent of the composite <strong>for</strong> wholegrains (table 1). Both the ready-to-eat<strong>and</strong> cooked <strong>for</strong>ms of wheat <strong>and</strong> oatcereals were eaten, <strong>and</strong> the instantvariety was the most consumed typeof all the cooked oatmeals. Many ofthe cereals in the item-groups <strong>for</strong>wheat <strong>and</strong> oat cereal were <strong>for</strong>tified.Children obtained added nutrients byeating these <strong>for</strong>tified cereals. Wholewheatbread was 33 percent of thecomposite <strong>for</strong> whole grains, but crackedwheatbread was the predominant foodcode in the item-group <strong>for</strong> whole-wheatbread. Cracked-wheat bread was in thisitem-group, because the wheat-basedbreads were grouped together. Corntortilla had a fairly large representation(10 percent) in the composite <strong>for</strong> wholegrains. Tortilla chips <strong>and</strong> corn chipswere the top food codes in the itemgroup<strong>for</strong> corn tortilla. For children,one serving from the composite <strong>for</strong>whole grains provided 2.1 g dietaryfiber, 24.6 mg magnesium, <strong>and</strong> 0.5 mgzinc (table 2).Enriched grain. White bread was thelargest component of the children’scomposite <strong>for</strong> enriched grains.White bread was the first (35 percent)<strong>and</strong> ‘‘enriched flour desserts <strong>and</strong> othersources of enriched flour’’ (shortenedto just ‘‘enriched flour desserts’’) wasthe second largest component (14 percent)of the enriched-grain composite(table 1). The term ‘‘desserts’’ wasused to identify the latter item-groupbecause many of the food codes in itwere sweet foods like cookies, doughnuts,pastries, pies, <strong>and</strong> cakes. Enrichedflour in each of these foods wascounted toward servings of enrichedgrains. The enriched flour in pizzacrust was also included in this itemgroup.A low-sugar <strong>and</strong> low-fat foodwas used to represent the item-group<strong>for</strong> enriched flour desserts in the composite,but children were consumingadded sugars <strong>and</strong> fat from these foods.The third largest component of thiscomposite was enriched pasta <strong>and</strong>noodles. The foods in this item-groupthat were most commonly eaten bychildren were macaroni <strong>and</strong> cheese<strong>and</strong> spaghetti with or without tomatosauce. Corn <strong>and</strong> rice ready-to-eatcereals combined were 11 percent ofthe children’s composite; most were<strong>for</strong>tified. Wheat-flour tortillas constituteda separate item-group in thecomposite <strong>for</strong> enriched grains, becausethey were consumed in large amounts.Children ate more wheat-flour tortillasthan English muffins or bagels. (Bagelswere placed in the item-group <strong>for</strong>English muffins.)26 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
As expected, the amount of fiber,magnesium, <strong>and</strong> zinc in the composite<strong>for</strong> enriched grains was lower than inthe composite <strong>for</strong> whole grains.Meat, poultry, fish. Beef was 48 percent<strong>and</strong> poultry 27 percent of the children’scomposite <strong>for</strong> meat, poultry, <strong>and</strong> fish.Children ate most of their beef in ground<strong>for</strong>m: 22 percent of their composite <strong>for</strong>meat, poultry, <strong>and</strong> fish (table 1). Freshbeef, as in steak <strong>and</strong> roast beef, wasabout 19 percent of the children’scomposite <strong>for</strong> meat, poultry, <strong>and</strong> fish.Children’s composite also containedabout 8 percent beef lunch meats----mostly frankfurters. About 12 percentof the children’s composite <strong>for</strong> meat,poultry, <strong>and</strong> fish was frankfurters <strong>and</strong>other lunch meats. Because of theirhigher fat content or water content orboth, 2 ounces of sausages <strong>and</strong> lunchmeats were counted as 1 ounce of leanmeat in the Food Guide Servings DataBase. For example, a child who ate a2-ounce hot dog was credited 1 ounceof lean meat.Chicken, compared with turkey, wasthe most commonly eaten poultry: 23versus 4 percent of the children’s composite.And it was the roasted chickenbreast without skin <strong>and</strong> chicken nuggetsthat accounted <strong>for</strong> 12 percent of allchicken servings. Many of the 188 foodcodes with poultry servings, whichwere reported consumed by children,were various fried chicken parts. Friedchicken was not, however, representedas such in the composite, because theleanest <strong>for</strong>m of a food was used. Allchicken was represented in the compositeby a food code described as ‘‘chicken,boneless, not specified as to part,roasted, light or dark meat, skin noteaten.’’Within the item-group <strong>for</strong> liver, childrenate more chicken liver than beef liver.Because children ate less beef liverthan did all individuals, the children’scomposite contained less of vitamins A<strong>and</strong> B12 (table 2).Canned finfish, mostly tuna in water,was the predominant fish item-group(table 1). For both children <strong>and</strong> all individuals,the top foods consumed in theitem-group <strong>for</strong> lean finfish were fried.Most servings of fatty finfish werefried catfish <strong>for</strong> both children <strong>and</strong> allindividuals. Shrimp was the largestcomponent of the item-group <strong>for</strong> shellfish<strong>for</strong> children <strong>and</strong> all individuals,both of whom ate more servings ofsteamed or boiled shrimp than friedshrimp.The composite <strong>for</strong> meat, poultry, <strong>and</strong>fish contributed the most fat <strong>and</strong> saturatedfat of all the composites (table 2).For children, 1 serving of meat, poultry,<strong>and</strong> fish provided 2.5 g fat, 0.9 g saturatedfat, 7.7 g protein, 22 mg cholesterol,0.5 ug vitamin B12, 0.55 mg iron,<strong>and</strong> 1.11 mg zinc.Milk. Children consumed more wholemilk than did all individuals.Although a composite was not developed<strong>for</strong> the milk group, because thenutrient profile was to be based onnonfat fluid milk, CNPP did analyzehow children consumed their servingsof the milk group. Findings showedthat about 84 percent of children’s servingsfrom the milk group were of fluidmilk, 15 percent were of cheese, <strong>and</strong>1 percent were of yogurt.Children obtained the bulk of theirservings of the milk group by drinkingmilk: about 92 percent of children’s‘‘milk as beverage’’ servings werewhole, 2-percent, 1-percent, or skimmilk. The remaining 8 percent of their‘‘milk as beverage’’ servings werecocoa, milk shakes, chocolate milk,<strong>and</strong> other flavored milks. Young childrenconsumed a larger percentage ofthe category entitled ‘‘milk as beverage’’as whole milk (47 percent) than did allindividuals (35 percent). Children had14 percent of servings from 1-percentor skim milk; all individuals had 21percent from these types of milk.Ice cream <strong>and</strong> ice milk were also part(about 4 percent) of children’s servingsof fluid milk. Children ate less pudding(1 percent of the servings of fluid milk)than ice cream <strong>and</strong> ice milk. Childrenalso obtained fluid milk in mixturessuch as cream sauces <strong>and</strong> soups, butin small amounts.The milk group is represented by 1 cupskim milk, which provides 8.4 g protein,86 calories, 0.3 g saturated fat, <strong>and</strong> 302mg calcium (table 2).Serving SizesAcross all the food groups <strong>and</strong> subgroups,children tended to have smallerserving sizes than did all individuals.Children’s average intake was 1 servingper report <strong>for</strong> fruits <strong>and</strong> juices. Whenchildren ate cooked greens, raw broccoli,<strong>and</strong> romaine (dark-green vegetables),their serving sizes were much smallerthan those <strong>for</strong> all individuals. Childrenhad 0.9 servings, on average, per report.Of all five vegetable subgroups (darkgreen,starchy, etc.), children’s numberof servings per report (0.4) was thesmallest <strong>for</strong> the deep-yellow vegetablesubgroup.Children averaged 0.7 servings perreport <strong>for</strong> legumes <strong>and</strong> 0.8 servings<strong>for</strong> starchy vegetables. Among starchyvegetables, children averaged 0.9 servings<strong>for</strong> potato chips <strong>and</strong> 0.7 servings<strong>for</strong> French fries. Children’s number ofservings per report of other vegetables1999 Vol. 12 Nos. 3&4 27
By selecting foodssomewhat differentlyin the food groups<strong>and</strong> subgroups,children can improvetheir nutrient intakes.averaged 0.5. The number of servingsper report (0.2 <strong>for</strong> children) <strong>for</strong> individualitem-groups was particularly small <strong>for</strong>cooked onions, raw celery, <strong>and</strong> cookedmushrooms, used in small amounts inmany mixed dishes.Children had an average of 1.2 servingsper report from the composite <strong>for</strong>whole grains <strong>and</strong> 1.4 servings perreport from the item-group <strong>for</strong> wholewheatbread. Children averaged 1.2servings per report across all foods inthe composite <strong>for</strong> enriched grains, 1.4servings <strong>for</strong> white bread, <strong>and</strong> 1.3 servings(a little over 1 ⁄ 2 cup) <strong>for</strong> enrichedpasta <strong>and</strong> noodles. The halves of anEnglish muffin or bagel constitute 2servings of grains; children averaged1.4 servings per report.For items in the composite <strong>for</strong> meat,poultry, <strong>and</strong> fish, children averaged1.4 ounces per report. For the milkcomposite, children consumed about3/4 cup of milk (0.8 servings) perreport <strong>and</strong> 2/3 cup of ice cream pereating occasion. For pudding, theaverage amount eaten per report was0.5 servings ( 1 ⁄ 2 cup).Generally, the amounts reported <strong>for</strong>children 2 to 6 years old were about60 to 80 percent of those <strong>for</strong> all individuals.This suggests that it is appropriateto continue to use two-thirds ofthe serving size designated <strong>for</strong> adultsas a serving size <strong>for</strong> 2- to 3-year-oldswhen assessing nutrient levels in FoodGuide Pyramid patterns <strong>for</strong> youngchildren ages 2 to 3 (1,9). Two- tothree-year-olds need two-thirds of theserving size <strong>for</strong> adults, except <strong>for</strong> milk.Two cups of milk are recommended<strong>for</strong> 2- to 3-year-old children. Four- tosix-year-old children need the sameserving sizes designated <strong>for</strong> adults.Food Guide Pyramid DietPatterns <strong>for</strong> Young ChildrenThe REI <strong>for</strong> 1- to 3-year-old childrenis 1,300 calories (2). A 1,600-caloriepattern was considered an appropriateobjective <strong>for</strong> 4- to 6-year-old children.Although the REI <strong>for</strong> 4- to 6-year-oldchildren is 1,800 calories, food consumptiondata reported <strong>for</strong> this agegroup in the CSFII 1989-91 averaged1,533 calories.Focus groups with parents, a consumerresearch aspect of the development ofthe Food Guide Pyramid <strong>for</strong> YoungChildren, indicated that parents wereconcerned that the amount of food theirchildren ate might not be adequateto meet their nutrient needs. 1 It wasimportant to determine whether a dietpattern set at a calorie level close towhat children reportedly eat, <strong>and</strong> basedon their reported food choices withinfood groups, could meet their nutrientrequirements. It is not wise to haveparents feed their children more foodthan needed----considering the prevalenceof childhood obesity in the UnitedStates.CNPP created the diet patterns asfollows. For each food group <strong>and</strong> subgroupcomposite, the nutrients per FoodGuide Pyramid serving were multipliedby the number of servings in the pattern<strong>and</strong> summed. Discretionary fat wasadded to bring the level of total fat inthe 1,600-calorie pattern to 30 percentof calories <strong>and</strong> in the 1,300-caloriepattern to 34 percent of calories, theactual consumption level in the CSFII1989-91 <strong>for</strong> 2- to 3-year-old children.Added sugars, represented as teaspoonsof sugar, were then included to bringcalories to the levels targeted <strong>for</strong> thetwo diet patterns.1 See Tarone (5).28 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 3. Comparison of children’s recommended intake with their consumption: Food group <strong>and</strong>subgroup servings per dayRecommended intake Actual intake 1Food group Food group servings Avg da<strong>ily</strong> servings CSFII 1989-91Subgroup 1,300 calories 1,600 calories 2-6 yrs All individualsFruit 1.33 2.00 1.19 1.12Vegetable 2 servings 3 servings 1.41 servings 2.62 servingsDark-Green 0.29 0.43 0.08 0.13Deep-Yellow 0.38 0.57 0.06 0.14Legume 0.29 0.43 0.08 0.17Starchy 0.38 0.57 0.61 0.94Other 0.67 1.00 0.58 1.25Grain 4 servings 6 servings 4.55 servings 5.50 servingsWhole Grain 2.00 3.00 0.96 1.27Enriched Grain 2.00 3.00 3.59 4.22Meat, poultry, fish 3.33 ounces 5.00 ounces 2.55 ounces 4.37 ouncesMeat, Poultry, Fish 2.86 4.57 2.17 3.95Egg 0.29 0.43 0.24 0.32Nuts <strong>and</strong> Seeds 0.18 0.0 0.14 0.10Milk 2.00 2.00 1.94 1.48Fat, total 49.5 grams 53.4 grams 54.5 grams 70.4 gramsAdded sugars 7 tsp 6 tsp 13.2 tsp 2 19.5 tsp 2Total calories 1,304 kcal 1,613 kcal 1,435 kcal 1,796 kcal1 Calculated by dividing the total weighted number of servings reported over 3 days by 3 <strong>and</strong> then dividing by the weighted number of people in the samples.2 Estimated extra calories from added sugars in foods <strong>and</strong> small amounts of foods not accounted <strong>for</strong> in Food Guide Servings Data Base.The 1,600-calorie pattern contained theminimal number of Food Guide Pyramidservings at the serving size recommendedin the original Food GuidePyramid (table 3). There were 2 servingsof fruit, 3 of vegetables, 6 of grains,5 ounces of meat, <strong>and</strong> 2 cups of nonfatmilk, along with added fat <strong>and</strong> sugars.The 1,300-calorie pattern had the minimalnumbers of Food Guide Pyramidfood group servings reduced in size byone-third <strong>for</strong> all food groups <strong>and</strong> subgroupsexcept milk, to represent theone-third smaller serving size estimated<strong>for</strong> 2- to 3-year-old children. Forexample, 2 servings of fruit multipliedby two-thirds equaled 1.33 Food GuidePyramid fruit servings in the 1,300-calorie pattern.A total of 2 cups of milk was includedin both diet patterns to meet calciumrecommendations. Because there ismore fat permitted in the youngerchild’s diet, CNPP substituted peanutbutter <strong>for</strong> a portion of the meat servingsin developing the 1,300-calorie pattern<strong>for</strong> 2- to 3-year-old children. This meatalternate, which is higher in fat content,represented the percentage of the meatgroup that young children consumed asnuts.1999 Vol. 12 Nos. 3&4 29
Table 4. Nutrient levels in Food Guide Pyramid patterns <strong>for</strong> young children 1RDA 2 orrecommendation1,300-calorie pattern1,600-caloriepatternCSFII 1989-91consumptionChild Child Child ChildNutrient 1-3 yrs 4-6 yrs 2-3 yrs 4-6 yrs 4-6 yrs 2-3 yrs 4-6 yrs- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Kcal - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -Calories (avg) 1,300 1,800 ~1,300 ~1,300 ~1,600 1,288 1,533- - - - - - - - - - - - - - - - - - - Percent of RDA - - - - - - - - - - - - - - - - - - - - - -Protein 16 g 24 g 361 241 325 305 244Calcium 800 mg 800 mg 98 98 109 94 107Magnesium 80 mg 120 mg 259 173 225 219 169Iron 10 mg 10 mg 74 74 110 96 117Zinc 10 mg 10 mg 77 77 107 68 82Copper 0.7 mg 1.0 mg 100 70 100 98 81Vitamin A 400 RE 500 RE 267 214 295 177 162Vitamin E 6 mg 7 mg 98 84 89 78 77Vitamin C 40 mg 45 mg 169 150 220 194 186Niacin 9 mg 12 mg 122 92 130 143 134Vitamin B 6 1.0 mg 1.1 mg 104 95 133 117 126Folate 50 ug 75 ug 329 219 303 378 295Vitamin B 12 0.7 ug 1.0 ug 513 359 460 492 371- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - Percent of Kcal - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - -Fat 3
composite had more polyunsaturatedfat <strong>and</strong> less saturated fat than theamount consumed by children.The 1,300-calorie pattern provided atleast 100 percent of the RDA <strong>for</strong> mostnutrients <strong>for</strong> both 2- to 3-year-olds <strong>and</strong>4- to 6-year-olds. The major exceptionswere the trace minerals----iron <strong>and</strong> zinc<strong>for</strong> both age groups <strong>and</strong> copper <strong>for</strong> the4- to 6-year-olds. The amount of ironprovided by the 1,300-calorie patternwas lower than the amount consumedby children, according to the CSFII1989-91. The reason <strong>for</strong> this difference:composites <strong>for</strong> whole grains <strong>and</strong>enriched grains contained non-<strong>for</strong>tifiedbreakfast cereals, but the cereals childrenate were <strong>for</strong>tified. Additional analysisshowed that when breakfast cerealsincluded in the grain composites werechanged to contain iron <strong>and</strong> zinc at<strong>for</strong>tification levels, the Food GuidePyramid patterns provided recommendedlevels of iron <strong>and</strong> zinc <strong>for</strong> children.The 1,300- <strong>and</strong> 1,600-calorie patternsmet or nearly met objectives <strong>for</strong> fat,saturated fat, cholesterol, sodium, <strong>and</strong>dietary fiber. At 10.5 percent of caloriesin the 1,300-calorie pattern, saturatedfat was somewhat lower than the actuallevel of consumption targeted <strong>for</strong> the2- to 3-year-old child: 13.6 percent.Consumption of Food GroupsTable 3 shows the recommendednumbers of food group <strong>and</strong> subgroupservings <strong>for</strong> the 1,300- <strong>and</strong> 1,600-calorieFood Guide Pyramid patterns developed<strong>for</strong> young children. The numbersof servings <strong>for</strong> vegetables, grains, <strong>and</strong>meat <strong>and</strong> meat alternates were derivedas follows. Originally when the foodguide was developed, the da<strong>ily</strong> servingsof vegetables were divided equallyamong dark-green/deep-yellow, legumes/starchy, <strong>and</strong> other vegetables (1). Forvegetables, ‘‘several’’ servings wasdefined as 3, so several times a weekmeant 3 times a week or 3/7 of 1 servingper day. For the 1,600-calorie pattern,3 vegetable servings were divided into1 serving each from dark-green/deepyellow,legumes/starchy, <strong>and</strong> othervegetables. Hence the 3/7 (0.43) darkgreen<strong>and</strong> 4/7 (0.57) deep-yellowprovided 1 serving per day, the 0.43legumes <strong>and</strong> 0.57 starchy providedanother serving, <strong>and</strong> other vegetablesprovided the third serving per day. Thenumbers of grain servings were basedon the Food Guide Pyramid recommendationto choose ‘‘several’’ servings aday of foods made from whole grains(6). For the meat <strong>and</strong> meat alternates,the number of egg servings was basedon 3 eggs per week, <strong>and</strong> the meat,poultry, fish servings were calculatedby difference (0.43 eggs subtractedfrom 5.0 ounces total meat <strong>and</strong> meatalternates).The Food Guide Servings Data Baseused in this study did not quantify theamount of added sugars in foods.These values were estimated from thecalories in added sugars in foods <strong>and</strong>from the calories in small amounts offoods, such as raisins in oatmeal raisincookies <strong>and</strong> garnishes <strong>and</strong> condiments,which were not counted by the FoodGuide Servings Data Base. Calorieswere then expressed as average da<strong>ily</strong>servings of added sugars, in teaspoons.Thus the average da<strong>ily</strong> servings ofadded sugars may somewhat overestimateactual intakes of sugar. However,these estimated consumption levelsof sugars were much higher than thelevels of 6 teaspoons <strong>and</strong> 7 teaspoons(1,600- <strong>and</strong> 1,300-calorie patterns,respectively) suggested in the FoodGuide Pyramid patterns.ConclusionsChildren ate somewhat differently fromthe rest of the population, as indicatedby composites of the food groups <strong>and</strong>subgroups, which were based onreported food consumption by youngchildren ages 2 to 6 <strong>and</strong> all individualsages 2 <strong>and</strong> older. However, the variationsresulted in few substantial differencesin the nutrient profiles of acomposite serving of any of the foodgroups or subgroups.Young children consumed smallerservings of foods, typically 60 to 80percent of the average amounts <strong>for</strong>individuals of all ages. A serving thatis two-thirds of the original Food GuidePyramid serving is a reasonable estimate<strong>for</strong> assessing nutrient levels inpatterns <strong>for</strong> 2- to 3-year-old children.The 1,300-calorie Food Guide Pyramiddiet pattern, which used the children’scomposites <strong>and</strong> nutrient profiles, metor nearly met objectives <strong>for</strong> most nutrientsexcept <strong>for</strong> iron, zinc, <strong>and</strong> copper.The 1,600-calorie pattern met all of theobjectives except <strong>for</strong> vitamin E. Wheniron <strong>and</strong> zinc were included at regular<strong>for</strong>tification levels in the ready-to-eatcereals used in the grain composites,diet-pattern levels of these nutrients metthe RDA. Breakfast cereals were popularwith young children, so ensuring thatthese cereals are <strong>for</strong>tified with iron<strong>and</strong> zinc can contribute substantiallyto meeting targeted intakes of thesenutrients.Copper was less than the RDA in the1,300-calorie pattern <strong>for</strong> the 4- to 6-year-old, but the older child wouldprobably be consuming closer to 1,600calories. Older children could improvetheir reported copper intake by eatingmore legumes. Both the 1,300- <strong>and</strong>1,600-calorie patterns were somewhat1999 Vol. 12 Nos. 3&4 31
low in vitamin E, but they exceededthe CSFII 1989-91 reported consumptionlevels of this nutrient. It is importantto reduce fat in the diet as childrenage, from 2 to 5 years. Emphasisshould also be given to replacing aportion of animal fats with vegetableoils, both to decrease saturated fatintakes <strong>and</strong> to increase vitamin Eintakes. The results of the analysis onthe RDA showed that most RDA wouldbe met when the children’s compositeswere used in the diet patterns. Byselecting foods somewhat differentlyin the food groups <strong>and</strong> subgroups,children can improve their nutrientintakes.Children’s diets could be improved byincluding more servings of vegetables,especially dark-green <strong>and</strong> deep-yellowvegetables <strong>and</strong> legumes, <strong>and</strong> more wholegrainproducts. Replacing some of theapple <strong>and</strong> grape juices that childrenfrequently drink with more servingsof whole fruit could improve consumptionof nutrients <strong>and</strong> dietary fiber.Replacing some lunch meats withlean meat, poultry, <strong>and</strong> fish may alsoimprove nutrient intakes. Children’sdiets could be improved by theirchoosing foods that contribute morefood guide servings <strong>and</strong> less addedsugars.References1. Cronin, F.J., Shaw, A., Krebs-Smith, S.M., Marsl<strong>and</strong>, P., <strong>and</strong> Light, L. 1987.Developing a Food Guidance System to implement the Dietary Guidelines. Journalof <strong>Nutrition</strong> Education 19:281-302.2. National Academy of Sciences, National Research Council, Food <strong>and</strong> <strong>Nutrition</strong>Board. 1989. Recommended Dietary Allowances (10 th ed.). National AcademyPress, Washington, DC.3. National Research Council. 1989. Diet <strong>and</strong> Health. National Academy Press,Washington, DC.4. Putnam, J.J. <strong>and</strong> Allshouse, J.E. 1996. Food Consumption, Prices, <strong>and</strong> Expenditures,1996: Annual Data, 1970-94. U.S. Department of Agriculture, <strong>Eco</strong><strong>nom</strong>ic ResearchService. Statistical Bulletin No. 928. pp. 59, 61.5. Tarone, C. 1999. Consumer research: Food Guide Pyramid <strong>for</strong> Young Children.<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):33-44.6. U.S. Department of Agriculture, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>. 1996.The Food Guide Pyramid. Home <strong>and</strong> Garden Bulletin No. 252.7. U.S. Department of Agriculture, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>. 1997.U.S. Food Supply Series 1909-1994. (In-house data base.)8. U. S. Department of Agriculture <strong>and</strong> U.S. Department of Health <strong>and</strong> HumanServices. 1995. <strong>Nutrition</strong> <strong>and</strong> Your Health: Dietary Guidelines <strong>for</strong> Americans(4 th ed.). Home <strong>and</strong> Garden Bulletin No. 232.9. Welsh, S.O., Davis, C., <strong>and</strong> Shaw, A. 1993. USDA’s Food Guide: Background<strong>and</strong> Development. U.S. Department of Agriculture, Human <strong>Nutrition</strong> In<strong>for</strong>mationService. Miscellaneous Publication No. 1514.10. Williams, C.L., Bollella, M., <strong>and</strong> Wynder, E.L. 1995. A new recommendation<strong>for</strong> dietary fiber in childhood. Pediatr<strong>ics</strong> 96:985-988.32 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Consumer Research:Food Guide Pyramid <strong>for</strong>Young ChildrenCatherine Tarone<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>Developed specifically as a guide <strong>for</strong> feeding young children, the FoodGuide Pyramid <strong>for</strong> Young Children adapts recommendations of the originalFood Guide Pyramid <strong>and</strong> provides messages, based on the food guide, thatare helpful to parents <strong>and</strong> caregivers in improving the nutritional status of2- to 6-year-olds. A qualitative consumer research study was conducted toidentify needs of the target audience (parents <strong>and</strong> caregivers of 2- to 6-yearoldchildren), to explore, with this audience, messages based on the foodguide, <strong>and</strong> to evaluate prototype educational materials based on the foodguide-based messages directed at behavior change. Parent- <strong>and</strong> caregiverparticipantsrecommended emphasizing the message to ‘‘eat a variety offoods’’ as a theme <strong>for</strong> nutrition education materials that are designed toimprove young children’s diets. They also suggested that a ‘‘child-friendly’’graphic of the Food Guide Pyramid would help young children rememberthe Pyramid. USDA produced a booklet presenting nutrition guidancemessages <strong>and</strong> a ‘‘child-friendly’’ poster of the Food Guide Pyramid.The Food Guide Pyramid isUSDA’s primary nutritioneducation tool designed tohelp healthy Americansselect a diet that is consistent with theDietary Guidelines. The Food GuidePyramid illustrates patterns of foodselection that provide adequate amountsof food energy, protein, vitamins, minerals,<strong>and</strong> dietary fiber <strong>for</strong> good health butare moderate in fats, added sugars, <strong>and</strong>sodium. Adaptation <strong>and</strong> translation ofdietary guidance into dietary practiceare important components of any ef<strong>for</strong>tto help improve diets, including thoseof young children.In Phase I of the project to develop aFood Guide Pyramid <strong>for</strong> Young Children,the <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong><strong>Promotion</strong> (CNPP) developed the technicalnutrition basis <strong>for</strong> adapting theFood Guide Pyramid (6,7). CNPP staffdetermined that the nutrients in thefoods children consume, if eaten inamounts recommended by the originalFood Guide Pyramid, would meet children’snutrient needs. Because Pyramidfood groups <strong>and</strong> recommended numbersof servings resulted in a nutritionallyadequate diet <strong>for</strong> young children, thePyramid graphic could be adapted <strong>for</strong>young children. Also during Phase I,eight message concepts emerged fromthe review of literature (5), discussionswere held with nutrition educators, <strong>and</strong>comparisons were made of actual foodgroup <strong>and</strong> subgroup consumption withthe recommendations of the Food GuidePyramid, as adapted <strong>for</strong> young children1999 Vol. 12 Nos. 3&4 33
(6). The concepts were explored <strong>and</strong>further developed during Phase II.In support of USDA’s nutrition educationef<strong>for</strong>ts to translate dietary guidance intoconsumer behaviors, CNPP conducteda qualitative consumer research study inPhase II. Qualitative research is particularlyuseful <strong>for</strong> gaining insights <strong>and</strong> abetter underst<strong>and</strong>ing of the target audience.Qualitative research consists of openended,structured discussions or interviewswith individuals or small groupsof individuals----the purpose of which isto gather a greater depth of in<strong>for</strong>mationthan can be obtained by using quantitativetechniques (3).CNPP conducted qualitative researchbecause consideration of the target audience,including its wants <strong>and</strong> needs, isthe foundation of this research projectto advance dietary guidance <strong>for</strong> childrenin a way that motivates behavior changein both adults <strong>and</strong> children. Recentresearch on the effectiveness of nutritioneducation programs, includingthose with preschool children, foundthat programs using educational methodsdirected at behavior change as a goalwere more likely to be successful thanprograms that focused on in<strong>for</strong>mationdissemination (4).MethodsThe focus group study was conductedin two rounds. The objectives <strong>for</strong> thefirst round were to assess the nutritionin<strong>for</strong>mation that parents <strong>and</strong> caregiversof 2- to 6-year-old children needed, toidentify the key concerns <strong>for</strong> nutritioneducation, to assess familiarity with theFood Guide Pyramid, <strong>and</strong> to explorenutrition guidance messages (based onthe food guide) <strong>for</strong> young children. Theobjectives <strong>for</strong> the second round wereto determine whether the prototypeseffectively communicated nutritionguidance to the target audience of parents<strong>and</strong> caregivers of 2- to 6-year-olds. Thediscussions <strong>for</strong> the second round weredesigned to assess consumer reactionto the prototype materials (includingtheir reactions to design <strong>and</strong> layout,readability, <strong>and</strong> applicability of themessage concepts) <strong>and</strong> to identify anyconfusing or misleading in<strong>for</strong>mation.SamplesFor the first round, six focus groups,three with parents <strong>and</strong> three withcaregivers, were conducted in January1998. Parents were screened based ontheir ethnicity, household income, <strong>and</strong>educational level. Parents were alsoscreened to ensure that they had at leastone child 2- to 6-years-old <strong>and</strong> had notparticipated in a focus group within thelast 6 months. Caregivers were includedif they cared <strong>for</strong> 2- to 6-year-olds. (Theycould provide in-home care as well ascare in larger facilities.) Twelve peoplewere recruited <strong>for</strong> each group so thatat least eight would attend. Some geographicaldispersion was obtained byconducting one focus group with parents<strong>and</strong> a separate focus group with caregiversin each of three cities----Baltimore(Maryl<strong>and</strong>), Richmond (Virginia), <strong>and</strong>Chicago (Illinois). Fifty-two adultsparticipated in the first round of thestudy.In July 1998 the second round began.One focus group with parents <strong>and</strong> anotherfocus group with caregivers wereheld in each of three cities----Baltimore(Maryl<strong>and</strong>), Richmond (Virginia), <strong>and</strong>Chicago (Illinois)----<strong>for</strong> a total of sixgroups. The screening criteria used <strong>for</strong>the first round were also used <strong>for</strong> thisround. In addition, parents in Richmond<strong>and</strong> Chicago with 5- to 6-year-olds werescreened to have their children participatein a mini-focus group. Twentysevenparents, 25 caregivers, <strong>and</strong> 8children participated in the secondround; none had participated in thefirst round.ProceduresFor the first round of focus group studies,the moderator, with over 10 years ofexperience working with focus groups,led each group through the 2-hoursessions. Each focus group began withintroductions <strong>and</strong> an icebreaker, followedby discussions based on the objectives.The discussions identified goals, benefits,<strong>and</strong> barriers to healthful eating, participants’knowledge of nutrition, <strong>and</strong> theirfeeding practices. The session thenfocused on the nutrition messages of theFood Guide Pyramid <strong>and</strong> how they applyto young children. Discussions ended onthe eight messages regarding nutritionguidance <strong>and</strong> how to communicatethem to young children.All sessions were audio-taped <strong>and</strong> transcribedto obtain participants’ exactresponses to questions. Once transcribed,comments were color-coded <strong>and</strong> groupedaccording to content; this allowed keydiscussion themes to be uncovered. Themoderator <strong>and</strong> his staff recorded <strong>and</strong>reported participants’ verbal <strong>and</strong> nonverbalemotional expressions.After the first round, CNPP developedthe text of the materials to be used withthe participants in the second round.The prototypes were designed <strong>and</strong>produced through USDA’s Office ofCommunications Design <strong>Center</strong>. Toemphasize the variety theme, CNPPused the slogan 1-2-3 Variety in allthree prototypes. The prototype <strong>for</strong> theparents, a full-color, 12-page booklet,A Parents’ Guide to Using the FoodGuide Pyramid, contained an adaptedgraphic of the Food Guide Pyramid.Also included was general nutrition34 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
in<strong>for</strong>mation that gives a better underst<strong>and</strong>ingof1. healthful eating,2. tips on increasing the variety offoods eaten,3. meal planning <strong>and</strong> time-saving tips,4. guidance on specific issues suchas serving sizes <strong>and</strong> fat intakerecommendations related to youngchildren, <strong>and</strong>5. age-appropriate kitchen activities.The brochure Caregivers: Using theFood Guide Pyramid <strong>for</strong> Young Childrenwas based on the assumption that mostcaregivers have access to nutritioneducation materials <strong>and</strong> have someknowledge of the Food Guide Pyramid.The brochure contained the new graphic<strong>and</strong> an explanation of changes madefrom the original Pyramid graphic,including text to make clear that theadapted Food Guide Pyramid doesnot replace the original Pyramid. Alsoincluded were a list of foods to encouragevariety in the diet <strong>and</strong> a step-by-stepfood activity designed to involve youngchildren. The third prototype, a posterof the adapted Food Guide Pyramidgraphic, showed foods (drawn in a realist<strong>ics</strong>tyle <strong>and</strong> shown in single servingsizes when possible) commonly eatenby young children. The names of thefood groups were simplified, <strong>and</strong> thenumber of servings was represented bya single number rather than a range ofnumbers. The symbols <strong>for</strong> fat <strong>and</strong> sugarswere eliminated, <strong>and</strong> food pictures wereused in the tip.One week be<strong>for</strong>e the sessions <strong>for</strong> thesecond round, parent-recruits were sentthe text of the in<strong>for</strong>mation that wasprepared <strong>for</strong> parents; caregiver-recruitswere sent the text of the in<strong>for</strong>mationthat was prepared <strong>for</strong> the caregiver’sbrochure <strong>and</strong> the parents’ booklet.The recruits were instructed to read thematerial be<strong>for</strong>e attending their sessions;thus, focus group time would be used<strong>for</strong> discussion rather than be used, toa great extent, <strong>for</strong> reading.The same moderator who led the firstround of focus groups led the 2-hoursecond-round focus groups. At eachsession, following introductions <strong>and</strong> anicebreaker, participants were shown theprototype poster, The Food Guide Pyramid<strong>for</strong> Young Children, after which it wasdiscussed <strong>and</strong> put aside. Each parentthen received the in<strong>for</strong>mation bookletA Parents’ Guide to Using the FoodGuide Pyramid <strong>for</strong> Young Children, <strong>and</strong>the moderator led a discussion designedto evaluate the booklet. Caregivers weregiven the brochure Caregivers: Usingthe Food Guide Pyramid <strong>for</strong> YoungChildren. Following a discussion toevaluate the brochure, each caregiverwas given the parent booklet. Throughoutthese sessions, the participants wereasked to read <strong>and</strong> respond to severalsections of text <strong>and</strong> to the visualpresentation of the materials.The mini-focus group sessions with thechildren began with parents <strong>and</strong> childrenin the same room. Following a briefintroduction <strong>and</strong> explanation of theprocess, the children were taken to aseparate room where the moderatorshowed them a prototype poster of theFood Guide Pyramid. The moderatorled the children in a discussion of theposter <strong>and</strong> the concept of healthfuleating. The children were not askedabout the other materials intended <strong>for</strong>adults that required an eighth-gradereading level. As with the first round,all sessions in the second round wereaudio-taped, transcribed, color-coded,<strong>and</strong> grouped according to content.The idea of using thegraphic of the FoodGuide Pyramid as ateaching tool, as itturns out, was a newconcept <strong>for</strong> someparents.1999 Vol. 12 Nos. 3&4 35
ResultsThe First RoundThe 27 parent-participants in the firstround of the focus group studies hadat least one child 2 to 6 years olds; 78percent were female. Forty-nine percentwere African American; 37 percent,White; 11 percent, Hispanic; <strong>and</strong> 3percent, Asian. Almost 80 percent hadattended or graduated from college;about 40 percent had a household incomebetween $20,000 <strong>and</strong> $40,000. Of the25 participants who were caregivers,24 percent worked in in-home childcarefacilities.As a qualitative research method, focusgroups are not projectable to any population;however, they provide insightinto how the consumer views the world<strong>and</strong> what the consumer thinks (8). Findingsfrom this focus group research canbe presented under four key discussionthemes: Current Feelings Toward FeedingYoung Children, Current Behavior <strong>and</strong>Knowledge, Food Guide Pyramid, <strong>and</strong><strong>Nutrition</strong> <strong>and</strong> Dietary Behavior. Allquotes from participants are taken fromthe unpublished reports prepared <strong>for</strong>USDA (1).Current Feelings Toward FeedingYoung Children. Identifying the keyconcerns of parents <strong>and</strong> caregivers <strong>for</strong>nutrition education <strong>and</strong> exploringbenefits <strong>and</strong> barriers to an improveddietary pattern in young childrenresulted in a key theme.‘‘One of the most important things toteach them at an early age is to setgood st<strong>and</strong>ards <strong>and</strong> give them a goodfoundation as they grow.’’ (Caregiver)‘‘There are a variety of things wetry to accomplish through healthyeating . . . socialization, nutrition,emotional stability, which are relatedto food.’’ (Caregiver)‘‘It’s important that children learngood nutrition habits, so as they growolder, they will eat right instead ofeating at one fast-food place one day<strong>and</strong> another fast-food place the nextday.’’ (Parent)‘‘If you teach them now, they are moreapt to continue doing it rather than tointroduce them to healthy foods afterthey have eaten years of junk food. Itis easier to do it now.’’ (Parent)Table 1 shows the benefits <strong>and</strong> barriersin the descending order in which theywere mentioned by parents <strong>and</strong> caregivers.Results showed that these parents<strong>and</strong> caregivers think alike whendiscussing the benefits of healthfuleating. They were asked: ‘‘What are thebenefits of preparing healthy meals <strong>for</strong>younger children?’’ Most answered,‘‘good health.’’ The second benefitmentioned more often by both groupswas, ‘‘developing good eating habits atan early age.’’ Caregivers also pointedout that children are better behaved,have longer attention spans, <strong>and</strong> haveenergy to do things when they are fedwell.When it comes to feeding young children,parents most often mentioned the followingbarriers to healthful eating: thelack of time to plan <strong>and</strong> prepare meals,inexperience in dealing with picky eaters,<strong>and</strong> the negative influences of others.‘‘Time is needed in three differentplaces. You have to plan the meal,purchase it, <strong>and</strong> prepare it.’’‘‘I need in<strong>for</strong>mation on what to dowith an extremely picky eater whowon’t eat anything.’’‘‘If they are with somebody else, youdon’t have any control over the foodsthey eat.’’Caregivers seemed at ease whendiscussing nutrition <strong>and</strong> how theyfeed young children. Caregivers rarelymention having difficulty with ‘‘pickyeaters.’’ Instead, they said most childrenwere willing to try a new food if theysaw their friends eating the food. Severalcaregivers said parents were the biggestbarrier to improving children’s diets.‘‘It’s just a lack of knowing what isnutritious <strong>for</strong> a child. They [parents]think that a bag of chips <strong>and</strong> a sodaare nutritious.’’‘‘Parents don’t know what theirchildren are supposed to eat as abalanced meal. I think it’s importantthat we send the in<strong>for</strong>mation home tothe parents so that they [children]can eat healthy <strong>and</strong> be consistentwith what we do.’’Current Behavior <strong>and</strong> Knowledge.All groups were quite knowledgeableabout nutrition, based on the level ofdiscussion of most parents <strong>and</strong> caregivers.When asked to rate themselveson a scale of 1 to 10 on how well theybelieve they provide their children withhealthful <strong>and</strong> nutritious meals, parentsrated themselves ‘‘average’’ to ‘‘aboveaverage’’; caregivers rated themselves‘‘above average’’ to ‘‘excellent.’’ Duringfurther discussion, in spite of their knowledgeof nutrition <strong>and</strong> ratings, manyparents expressed feeling ill-equippedto feed their young children a healthfuldiet. They knew the ‘‘why’s’’ but notthe ‘‘how’s.’’36 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 1. Benefits <strong>and</strong> barriers to improving children’s dietsParents say:Good healthGood eating habitsMinds work betterBetter attitudeFood is a key part of a loving homeParents say:Lack of knowledgeLack of time to plan mealsLack of time to prepare mealsNegative influences of othersPicky eatersCost of food/wasting foodBenefits to improving dietsCaregivers say:Healthy children----less sicknessGood eating habitsEnergyHappy children----happy parentsEmotional, cognitive, social growthFood is a key part of a nurturing environmentBarriers to improving dietsCaregivers say:ParentsWasting food/wasting moneyFood allergies‘‘Not enough of the in<strong>for</strong>mationfocuses on children. What we’ve beendoing is taking adult in<strong>for</strong>mation <strong>and</strong>applying it to children.’’ (Parent)‘‘I think of nutrition <strong>and</strong> feeding mydaughter as a challenge every day.’’(Parent)Most caregivers seemed both knowledgeable<strong>and</strong> com<strong>for</strong>table discussingthe ‘‘do’s’’ <strong>and</strong> ‘‘don’t’s’’ of nutrition aseach concept related to young children;caregivers were very com<strong>for</strong>table withthe ‘‘how’s.’’‘‘The goals of Head Start are prettyclear that nutrition is an integral partof the program.’’During the parents’ discussions, firsttimeparents of very young childrenwere most concerned about servingsizes <strong>and</strong> whether their children wereeating enough. Other parents said theyhad learned to deal with how much foodto give children by offering them smallportions <strong>and</strong> letting the children ask <strong>for</strong>more. Most parents said they did notinsist on having children clean theirplates. A few examples:‘‘They say you shouldn’t overwhelmthem by offering too much.’’ (Parent)‘‘I think you know your children. Allthree of my kids get different portionsbecause I know my son will eat more,<strong>and</strong> one twin girl will eat more thanthe other.’’ (Parent)‘‘When they’re hungry, they will eat.If we could convince parents of that,our jobs would be a lot easier.’’(Caregiver)Food Guide Pyramid. To assessfamiliarity with the original Food GuidePyramid, the moderator showed allgroups the 1992 poster of the FoodGuide Pyramid. Most parents said theyare familiar with the graphic: they seeit on food packages. Some parents alsosaid that their young children are alsofamiliar with it.‘‘My son brought the Pyramid to myattention. He told me, ‘Daddy, thebigger the slot is, the more foodyou’re supposed to have.’ He cameto me at 3 years old <strong>and</strong> told me this.’’Most of the parents were able to discussthe Food Guide Pyramid <strong>and</strong> to speakabout the foods they prepare or do notprepare in each of the food groups.Most were able to identify foods in eachof the groups; a few were surprised thateggs <strong>and</strong> butter were not in the dairygroup. Many parents said they see the1999 Vol. 12 Nos. 3&4 37
Table 2. Reactions of focus groups to key messages based on the Food GuideMessagesReactions1. Increase variety <strong>and</strong> quantity of vegetables eaten ‘‘I’d like to have a food list. I had one when I was pregnant . . . . itwas helpful.’’ (Parent)‘‘There are some vegetables you like. It’s hard to break out <strong>and</strong> havevariety.’’ (Parent)2. Offer a variety of healthful foods, <strong>and</strong> encourage childrento try new foods‘‘It’s very difficult to find foods that all children will eat. Some of themost nutritious foods end up getting thrown in the garbage, <strong>and</strong> that isvery frustrating.’’ (Caregiver)‘‘I always think of the same things, like macaroni <strong>and</strong> cheese orwhatever I usually give them. I don’t think I ever diversify.’’ (Parent)‘‘If they won’t eat it, what’s the point.’’ (Parent)3. Increase the proportion of whole-grain <strong>and</strong> mixed-grain products ‘‘Once in a while [I offer these products to children].’’ ‘‘I tried bagels.What is a whole-wheat cereal? I’m sure we’ve eaten some.’’ (Parent)‘‘We are close to a bread store. Often we go on field trips there. Thechildren like the different kinds of breads.’’ (Caregiver)‘‘You always think kids like white bread <strong>and</strong> grown-ups like darkbread. Not necessar<strong>ily</strong>. Our kids eat dark bread.’’ (Caregiver)4. Emphasize greater use of whole fruits rather than juices ‘‘Children who drink juice eat less food.’’ (Parent)‘‘If they get too much juice then they won’t take in the food. That’sthe big problem. We see a lot of little kids whose parents haven’tstarted feeding them; they just let them drink.’’ (Caregiver)5. Parents <strong>and</strong> caregivers serve as role models <strong>for</strong> healthful eating ‘‘I’m not crazy about carrots, but I will cook them <strong>and</strong> eat them.’’(Parent)‘‘I never tell my kids, ‘Oh, I don’t like that’.’’ (Parent)‘‘In my center, everybody is required to sit down <strong>and</strong> eat with thechildren. That’s one way the children learn. It’s an opportunity <strong>for</strong> ateacher to teach them about nutrition.’’ (Caregiver)6. Be aware that young children need smaller serving size thanadults [need]7. Be aware that children’s appetites can vary day to day <strong>and</strong> do notoverreact to food jags <strong>and</strong> ‘‘picky eaters’’‘‘I’ve been doing it all wrong. I give all of us the same amount offood. My youngest never finished anything. My husb<strong>and</strong> tells me Igive her too much.’’ (Parent)‘‘I think that every child has the potential of being picky . . . . a kid isa kid.’’ (Caregiver)‘‘You have to encourage picky eaters. You sit down with them.’’(Caregiver)‘‘My child actually eats better away from home. She will eat things inher preschool that she will not eat at home because the other childrenaround her are eating them, too.’’ (Parent)8. Encourage parents to participate in physical activity with children ‘‘Oh boy, it’s very evident that I’m not getting enough exercise. It’smainly because of our work schedules. I know it’s important too, butit’s hard to find time to do it a lot of times.’’ (Parent)‘‘My young child is very active. My older child is a couch potato.’’(Parent)1999 Vol. 12 Nos. 3&4 39
Parents <strong>and</strong>caregivers likedthe idea of the FoodGuide Pyramid beingused with youngchildren, but mostsuggested that agraphic <strong>for</strong> youngchildren should be"child-friendly". . . .but if it were not well received, theywould not offer it again <strong>for</strong> about6 months.Message 3: The amount of time spenton this message----‘‘Increase the proportionof whole-grain <strong>and</strong> mixed-grainproducts’’----was brief in all focus groupsconsisting of parents. Many of the parentssaid they eat whole-grain products themselvesbut do not offer them to theirchildren. Caregivers, on the other h<strong>and</strong>,talked quite awhile about the differenttypes of grain products they offer <strong>and</strong>how the children enjoy them.Message 4: Regarding the need to‘‘Emphasize greater use of whole fruitsrather than juices,’’ several parentssaid they let their children drink juicebecause it is easier than cutting up fruit.Many care- givers <strong>and</strong> some parentsrealize that drinking too much juicecould cause eating problems.Message 5: ‘‘Parents <strong>and</strong> caregiversserve as role models <strong>for</strong> healthful eating.’’A few parents did not think their eatinghabits had much to do with their children’shabits, but most said they tried to eathealthfully so their children would dothe same. Most of the caregivers understoodthe importance of sitting <strong>and</strong>eating with the children <strong>and</strong> the importanceof offering foods <strong>for</strong> a healthfuldiet.Message 6: ‘‘Be aware that youngchildren need smaller serving sizes thanadults need.’’ Several parents said theyoffer small amounts of food, but othersoffered children the same amount,regardless of their ages.Message 7: ‘‘Be aware that children’sappetites can vary day to day <strong>and</strong> do notoverreact to food jags <strong>and</strong> ‘picky eaters’.’’Parents mentioned dealing with a ‘‘pickyeater’’ more often than did caregivers.The caregivers believed that having allthe children eat together helped to avoideating problems.Message 8: ‘‘Encourage parents toparticipate in physical activity withchildren’’ was the last educationalmessage based on the food guide. Mostparents believed that their 2- to 6-yearoldswere active enough ‘‘on their own’’<strong>and</strong> that parental involvement was moreimportant with older children whoseactivity levels decrease when the schoolyear begins.These focus group discussions providedinsights into what parents <strong>and</strong> caregiverswant <strong>and</strong> need to improve diets ofyoung children.• Parents want directions. They wantto know what to do; they want touse the Food Guide Pyramid; theywant easy-to-read materials.• Caregivers want activities thatinvolve children, <strong>and</strong> they wantmore in<strong>for</strong>mation on food variety.• Parents <strong>and</strong> caregivers want a more‘‘child-friendly’’ graphic of the FoodGuide Pyramid to use with youngchildren.• Three prototypes are needed: aparent piece, a caregiver piece, <strong>and</strong>a ‘‘child-friendly’’ graphic of theFood Guide Pyramid, all based onone theme: ‘‘Choose a variety offoods <strong>for</strong> a healthful way of eating.’’All messages are simple, positive,behavior-oriented, <strong>and</strong> developmentallyappropriate <strong>for</strong> young children.40 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
The Second RoundIn the second round of the focus groupstudy, all 27 parents had at least onechild between 2 <strong>and</strong> 6 years old. Eightytwopercent of the parents were female;27 percent, African American; 66 percent,White; <strong>and</strong> 5 percent, Hispanic.Eighty-one percent had attended somecollege or had graduated from college,<strong>and</strong> about 30 percent had householdincomes between $20,000 <strong>and</strong> $40,000.Twelve percent of the 25 caregiverswere employed by in-home child-carefacilities that enrolled 2- to 6-year-olds.In addition to the six adult groups, twomini-focus groups with children wereconducted. It was decided that childrenages 5 <strong>and</strong> 6 would have sufficientcommunication skills to participatein the research.The prototypes were well received.They were considered appealing interms of colors, illustrations, <strong>and</strong> their‘‘child-friendly’’ approach. The nutritioncontent was described as relevant, easyto read, <strong>and</strong> easy to underst<strong>and</strong>. Bothparents <strong>and</strong> caregivers considered thematerials valuable tools to communicatekey nutrition messages to help youngchildren make healthful food choices<strong>and</strong> develop good eating habits. Theparticipants were open to the idea ofa Food Guide Pyramid that has beenadapted to meet the needs of youngchildren, <strong>and</strong> they showed interest inthe parents’ booklet <strong>and</strong> caregivers’brochure, which supplement the adaptedgraphic. All quotes from individualsparticipating in the focus groups aretaken from the unpublished reportsprepared <strong>for</strong> USDA (2).Poster Graphic. Most adults thoughtthe graphic would appeal to young childrenbecause of the colors, the realistic‘‘child-friendly’’ art style, <strong>and</strong> the varietyof recognizable food items. Adults saidthe variety concept was communicatedby the many foods illustrated, the pyramidshape with the five main food groups,<strong>and</strong> the number of servings of foodgroups offered each day.‘‘I like the variety of pictures offoods . . . . You can shop in the store<strong>and</strong> show the children those foods<strong>and</strong> the variety of grain foods <strong>and</strong>vegetables.’’ (Parent)‘‘Well, I look at the Pyramid <strong>and</strong> I feellike it’s more user-friendly. For kids,especially if they are too young toread, the pictures are easy to underst<strong>and</strong>.’’(Parent)‘‘It’s a tool <strong>for</strong> teaching childrenabout nutrition. That’s an importantpart of personal teaching, that youhave an adult involved.’’ (Caregiver)‘‘It’s something a child could look at<strong>and</strong> actually underst<strong>and</strong>.’’ (Caregiver)The tip of the Food Guide Pyramidgenerated discussion about the meaningof moderation <strong>and</strong> how adults shoulddeal with young children’s intake ofsugars <strong>and</strong> fat. Many parents wanted toinclude cakes, cookies, <strong>and</strong> snack foodsas foods <strong>for</strong> the tip. A few parentswanted no food pictures in the tipbecause they thought that if their childsaw a can of soda in the tip, the childwould think it was alright to drink sodainstead of milk. Other parents <strong>and</strong> mostcaregivers said the tip could be used toteach about ‘‘sometimes’’ or ‘‘limiteduse’’foods. The discussions indicatethat more guidance about the tip of thePyramid <strong>and</strong> the moderation messageshould be added to the in<strong>for</strong>mationbooklet.The poster included in<strong>for</strong>mation aboutfoods that may be choking hazards <strong>for</strong>very young children. Based on inputfrom both parents <strong>and</strong> caregivers thatthis in<strong>for</strong>mation is important but moreappropriate within the in<strong>for</strong>mation booklet,CNPP deleted the in<strong>for</strong>mation from theposter but left it in the booklet.The 1-2-3 Variety slogan used on thethree prototypes received mixed reviews.About half of the adults tried to figureout ‘‘the meaning’’ while the othersthought it was a whimsical phrase toremind children to eat a variety offoods. Because of the mixed reviews,the slogan was not used in the finalpublications.‘‘I don’t underst<strong>and</strong> the 1-2-3 varietystuck in the middle of the poster. Itdoes not explain what 1-2-3 varietymeans anywhere on the poster.’’(Caregiver)‘‘1-2-3 variety is like ready, set, go.Like 1-2-3, let’s have variety, anattention getter.’’ (Caregiver)The in<strong>for</strong>mation collected from thechildren was limited, but they wereinterested in the poster illustrations,named all the foods, <strong>and</strong> talked aboutthe foods they liked <strong>and</strong> disliked. Theirdiscussions revealed that they do havesome underst<strong>and</strong>ing of the benefits ofhealthful eating:‘‘Eating healthy makes you gethealthy, makes you get strong.’’(Chicago child)‘‘When I drink milk, I get strongmuscles.’’ (Chicago child)Parent Booklet. The parents liked thebooklet because of the tips <strong>and</strong> facts,including the in<strong>for</strong>mation on mealplanning. And they liked the wayin<strong>for</strong>mation was presented in short,1999 Vol. 12 Nos. 3&4 41
highlighted points. Some thought in<strong>for</strong>mationwas new; others saw it more ashelpful <strong>and</strong> useful reminders to whatthey already knew.‘‘It helps you develop. It gives youplanning tools, <strong>and</strong> it gives you good,solid in<strong>for</strong>mation.’’ (Parent)‘‘It’s got everything in here. It’s colorful,<strong>and</strong> I really think parents wouldpick it up <strong>and</strong> read it.’’ (Parent)‘‘The simpler, the better, <strong>and</strong> this issimple. If you get more detailed, it getsto be too overwhelming <strong>and</strong> then theydon’t want to read it.’’ (Caregiver)In general, the focus of the parents’ in<strong>for</strong>mationbooklet (eating <strong>for</strong> a healthfuldiet) was understood, <strong>and</strong> participantswere positive about the key message:eating a variety of foods is healthful.‘‘Something like this reminds us of theimportance of eating the right foods.I’m guilty of just putting something onthe table, <strong>and</strong> it doesn’t always matcheach food group. The picture is a goodreminder.’’ (Parent)Participants liked the reminder aboutsmaller servings <strong>for</strong> 2- to 3-year-olds,<strong>and</strong> they especially liked the food list<strong>for</strong> serving sizes. The ‘‘Points <strong>for</strong> Parents’’addressed the eight nutrition guidancemessages. Parents liked the idea ofoffering whole fruit to their children,<strong>and</strong> many parents said their childrendrink too much juice. They acknowledgedthe importance of being a rolemodel <strong>for</strong> promoting healthful eatinghabits <strong>for</strong> young children.‘‘There are a lot of good ideas <strong>for</strong>parents of ways to get their kids toparticipate more in what they aregoing to eat.’’ (Parent)At the suggestion of many parents,CNPP consolidated the five ‘‘Points <strong>for</strong>Parents’’ sections appearing throughoutthe booklet into one page entitled‘‘Healthy Eating Tips . . . Encouragingfood choices <strong>for</strong> a healthy diet’’ <strong>and</strong>placed it in the first half of the refinedbooklet. Almost everyone liked theartwork, especially the food illustrationson the graphic. Several respondentssuggested that illustrations of youngchildren be included in the booklet <strong>and</strong>added to the poster to communicate thefact that the materials were aimed atyoung children <strong>and</strong> that physical activityis important.Caregiver Brochure. Most caregiversthought the in<strong>for</strong>mation in the caregiverbrochure was useful. They especiallyliked the list of foods, ‘‘Variety fromthe food groups,’’ which contained 300foods divided among the food groupsof the Food Guide Pyramid.‘‘The food list shows the breakdown ofthe grain group, where it says wholegrain <strong>and</strong> then enriched <strong>and</strong> then theones with more fat <strong>and</strong> sugar . . . . Ithink it’s good.’’ (Caregiver)It’s good how you did the vegetablegroup. You put the dark green <strong>and</strong>yellow in their own groups <strong>and</strong> thestarchy foods together in a group.’’(Caregiver)The experiential food activity ‘‘What’sin my taco?’’ was also well received,<strong>and</strong> the caregivers liked the idea ofhaving the recipe <strong>and</strong> instructions tosend home with the children.‘‘I think the activity is nice. It seemsto be something you could do in theclassroom that’s easy <strong>and</strong> interesting.’’(Caregiver)‘‘There’s a recipe on the back. I likethat. I would let the kids take thathome, <strong>and</strong> they could eat this at homeas well.’’ (Caregiver)The caregivers also evaluated the bookletdesigned <strong>for</strong> the parents. Most of themliked the in<strong>for</strong>mation so much that theysuggested that the food list <strong>and</strong> foodactivity from the caregiver brochure beadded to the parents’ booklet to createone in<strong>for</strong>mation booklet <strong>for</strong> everyone.Overall findings indicated that onebooklet <strong>for</strong> everyone, used along withthe poster graphic, would be the mosteffective way to communicate the keymessages based on the food guide. Allparents <strong>and</strong> caregivers thought that anadult would have ‘‘to walk the childthrough’’ the Food Guide Pyramid tohelp the child underst<strong>and</strong> the messages.Participants generally thought the readinglevel <strong>and</strong> amount of in<strong>for</strong>mation weregood in both the booklet <strong>and</strong> brochure.The readability level was determinedusing the Flesch-Kincaid <strong>for</strong>mula thatcalculates the grade level at which areader would underst<strong>and</strong> the material. Agrade-level score of 6-10 is consideredmost effective <strong>for</strong> a general audience.The readability level of the prototypesis Grade 7.8.SummaryLearning the wants <strong>and</strong> needs of parents<strong>and</strong> caregivers <strong>for</strong> nutrition educationof 2- to 6-year-olds can help with thedevelopment of materials that communicatenutrition guidance messages inappropriate <strong>and</strong> useful ways. Knowledgeof what consumers believe, value, need,<strong>and</strong> do is as important as our knowledgeof basic human nutrition (8). Manyparents want <strong>and</strong> need direction----theywant to know what to do to get theirchildren to eat healthfully. Consumers want42 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
1999 Vol. 12 Nos. 3&4 43
specif<strong>ics</strong> about feeding their children----clear, easy, meaningful in<strong>for</strong>mation onwhat they should do. Hence the FoodGuide Pyramid <strong>for</strong> Young Children wascreated to help adults teach healthfuleating behaviors to young children.As a result of this research, USDAdecided to refine <strong>and</strong> produce Food GuidePyramid nutrition education materials<strong>for</strong> use with 2- to 6-year-olds. ReleasedMarch 25, 1999, by Secretary DanGlickman <strong>and</strong> Under Secretary ShirleyR. Watkins, the materials are the 16-page,full-color booklet ‘‘Tips <strong>for</strong> Using theFood Guide Pyramid <strong>for</strong> Young Children2 to 6 Years Old’’ <strong>and</strong> a full-color,24" x 36" poster. Also available are afull-color Food Guide Pyramid graphicfood record----‘‘Plan <strong>for</strong> Your YoungChild . . . The Pyramid Way’’----<strong>and</strong> ablack <strong>and</strong> white reproducible graphicof the Food Guide Pyramid (see figure).These materials may be accessed throughthe CNPP Web site at www.usda.gov/cnpp(PDF <strong>for</strong>mat) or purchased through theGovernment Printing Office (Stock Number001-000-04665-9).USDA plans to cooperate with thepublic <strong>and</strong> private sectors to promotethe Food Guide Pyramid <strong>for</strong> YoungChildren. The graphic is expected tobe in use <strong>for</strong> many years in USDAfood guidance materials <strong>and</strong> programstargeted to young children.References1. Aeffect, Inc. 1998. Adapting the Food Guide Pyramid <strong>for</strong> Young Children. Step 1Management Report. Unpublished report prepared <strong>for</strong> the U.S. Department ofAgriculture, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>.2. Aeffect, Inc. 1998. Adapting the Food Guide Pyramid <strong>for</strong> Young Children. Step 2Management Report. Unpublished report prepared <strong>for</strong> the U.S. Department ofAgriculture, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>.3. Andreasen, A.R. 1995. Marketing Social Change. Jossey-Bass Publishers, SanFrancisco.4. Contento, I. et al. 1995. The effectiveness of nutrition education <strong>and</strong> implications<strong>for</strong> nutrition education policy, programs, <strong>and</strong> research. Journal of <strong>Nutrition</strong> Education27(6):279-283.5. Escobar, A. 1999. Factors influencing children’s dietary practices: A review.<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):45-55.6. Marcoe, K.L. 1999. Technical Research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> YoungChildren. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):18-32.7. Saltos, E. 1999. Adapting the Food Guide Pyramid <strong>for</strong> Children: Defining thetarget audience. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):3-17.8. Sutton, S.M., Layden, W., <strong>and</strong> Haven, J. 1996. Dietary guidance <strong>and</strong> nutritionpromotion: USDA’s renewed vision of nutrition education. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong><strong>Nutrition</strong> Review 9(2):14-21.44 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Factors Influencing Children’sDietary Practices: A ReviewAlyson Escobar<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>This article briefly reviews research on children’s dietary practices <strong>and</strong>discusses factors that affect their food choices <strong>and</strong> behaviors. The influenceof food preferences on actual food selections <strong>and</strong> key factors that determinepreferences in children are explored. Special attention is given to feedingpractices within the child-care setting because the number of meals <strong>and</strong>snacks consumed in day-care homes <strong>and</strong> centers continues to increase.Researchers at the U.S. Departmentof Agriculture (USDA)<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong> (CNPP)used a multistage approach to developthe Food Guide Pyramid <strong>for</strong> YoungChildren. CNPP provided a researchbasedrationale <strong>for</strong> focusing on a foodguide that could be used by parents <strong>and</strong>caregivers of preschool-age children (43).Using data from the Continuing Surveyof Food Intakes by Individuals 1989-91,the <strong>Center</strong> developed composites <strong>for</strong> 1,300-<strong>and</strong> 1,600-calorie Pyramid-based dietpatterns, all of which were based onchildren’s food intake (35).To gather input from the target audience,USDA researchers conducted a twophasefocus group study to obtain participants’evaluations of the prototypegraphic <strong>and</strong> promotional materials (49).CNPP staff conducted additional researchto determine whether any other issuesneeded to be considered in developing<strong>and</strong> promoting a food guide <strong>for</strong> thetarget audience.The early years are a key time <strong>for</strong>experimenting with <strong>and</strong> establishingdietary habits, some of which may havea major influence on the risk <strong>for</strong> developingcertain chronic diseases later inlife. Early experiences with food <strong>and</strong>eating are central to the acquisition offood preferences <strong>and</strong> patterns of foodconsumption (6). Children’s food choicesare further influenced by a wide varietyof environmental <strong>and</strong> lifestyle factors(16, 41) that are important in the development,maturation, <strong>and</strong> modificationof dietary behavior during childhood(24) <strong>and</strong> that are important determinantsof dietary behavior among underserved,ethnically diverse groups of children(13). This paper briefly highlightsseveral influences on young children’sdietary behavior that may have implications<strong>for</strong> feeding as well as communicatingfood <strong>and</strong> nutrition messages toyoung children.Developmental Capabilities <strong>and</strong>Children’s Dietary PracticesChildren’s dietary practices are influencedby their developmental stage,with the years between 2 <strong>and</strong> 6 markedby rapid social, intellectual, <strong>and</strong> emotionalgrowth. Physical growth slowsoverall, with a decrease in growth ratereflected in a decrease in appetite <strong>and</strong>less interest in food (45).Adding to the challenge of feedingyoung children is the emotional growth1999 Vol. 12 Nos. 3&4 45
Young children arecapable of learning tolike <strong>and</strong> accept a widevariety of foods, <strong>and</strong>this learning occursrapidly during the firstfew years of life.that takes place while they are toddlers.Toddlerhood marks the beginning ofchildren’s attempts to establish independence.As a result, children engagein power struggles with parents <strong>and</strong>caregivers. These conflicts often eruptduring feeding situations, with toddlersrefusing to eat until they get what theywant <strong>and</strong> with adults torn between theirneed to control the situation <strong>and</strong> theirdesire to ensure that their child is wellnourished.As children progress into the preschoolyears, their emotional developmentcontinues to affect the feeding situation.Preschoolers are generally less fearfulthan toddlers <strong>and</strong> more eager to stretchtheir limits; to explore their world. Theybehave more consistently <strong>and</strong> are likelyto be active in seeking attention <strong>and</strong>approval from adults. Thus their eatingpatterns become more established, <strong>and</strong>their food preferences are highly influencednot only by adults but also bypeers (45). Birch found that childrenas young as 3 <strong>and</strong> 4 years could bepersuaded to change their selection<strong>and</strong> consumption of different vegetablesas a result of eating meals with theirpeer group whose preferences differedinitially from their own (3). Furthermore,peer influence was strongest <strong>for</strong>the younger children in the group.Preschool children also undergo majorchanges in development of their motorskills <strong>and</strong> other abilities. The progressionfrom large motor skills to finemotor skills that occurs gives parents<strong>and</strong> caregivers a prime opportunity toengage children in food-preparationactivities (26,27). Food preparation canbe used to teach colors, shapes, sizes<strong>and</strong> size comparisons, cultural differences,<strong>and</strong> mathematical concepts (45).Food Preferences <strong>and</strong>Acceptance <strong>and</strong> Children’sFood-Related BehaviorsOne estimate has indicated that 25 to50 percent of the variation in foodconsumption among individuals canbe attributed to preference alone (38).One study of young Mohawk children,<strong>for</strong> example, has found that food preferencesexplained over 70 percent ofthe variation in dietary behavior (25).Another study has provided evidenceof a strong correlation between foodpreferences <strong>and</strong> food choices in childrenas young as 3 years. This research alsosuggests that food preferences may havean even greater effect on children’s foodchoices than on adults’ choices (2).Young children are capable of learningto like <strong>and</strong> accept a wide variety offoods, <strong>and</strong> this learning occurs rapidlyduring the first few years of life. Underst<strong>and</strong>ingthe contribution of early learning<strong>and</strong> experiences to the developmentof food-acceptance patterns (e.g., whichfoods <strong>and</strong> how much of each an individualchooses to eat) can help foster developmentof healthful patterns <strong>and</strong> reduceparents’ <strong>and</strong> caregivers’ anxieties aboutfeeding children (6).Innate <strong>and</strong> Learned FactorsDevelopment of food-acceptance patternsbegins during infancy with certain innatetaste preferences: newborn infantsrespond positively to sweet tastes <strong>and</strong>negatively to sour <strong>and</strong> bitter tastes.While the reflexive nature of infants’responses to these tastes might suggestthat food-acceptance patterns are ‘‘builtin’’<strong>and</strong> difficult to change, researchdoes not support this conclusion (8).Responses to basic tastes change with achild’s repeated experiences with foods.46 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
One preference of young children, morelearned than innate (it appears), is that<strong>for</strong> high-fat foods. Possible explanations<strong>for</strong> this preference <strong>for</strong> fat are thepleasant feeling of satiety it provides inresponse to hunger <strong>and</strong> its associationin many foods containing sugar <strong>and</strong>salt, both of which are preferred tastesamong children (5).A preference <strong>for</strong> high-fat foods mayhave important implications <strong>for</strong> obesityamong children. Research with a groupof 3- to 5-year-old children found acorrelation between their preferences<strong>for</strong> high-fat foods <strong>and</strong> both their totalfat intake <strong>and</strong> triceps skinfold measurements(20). In addition, parents of childrenwith the strongest preferences <strong>for</strong>high-fat foods <strong>and</strong> the highest total fatintakes had higher composite BMIscores than parents of children withlower scores.<strong>Fam</strong>iliarity <strong>and</strong> Food ChoicesChildren tend to prefer foods that arefamiliar, compared with foods that arenot, regardless of the foods’ sensorycharacterist<strong>ics</strong> (48). Birch et al. (8) haveinvestigated children’s tendency to rejectwhat is new <strong>and</strong> how this tendency mightbe altered. The researchers’ conclusion:changing rejection to acceptance canbe as simple as providing a child withopportunities to sample a new food.However, having a child move fromrejection to acceptance of new foodsis a relatively slow process that mayrequire as many as 10 exposures toa new food (48).Building on previous research in thisarea, Skinner (46) found that 2- to 3-year-olds liked over 80 percent of fooditems that had been offered to them. Shecautioned parents <strong>and</strong> caregivers to becareful about prejudging foods theythink a child will not like or eat. She,instead, encouraged parents to do theirbest to expose children to a variety ofnutritious foods to try <strong>and</strong> perhapsaccept into their diet.Other dimensions of foods that contributeto their ultimate acceptance or rejectionby young children include smell,appearance, <strong>and</strong> textural characterist<strong>ics</strong>(e.g., crunchiness, creaminess, <strong>and</strong>greasiness). However, children’s responsesto these characterist<strong>ics</strong> are alsoinfluenced by their prior experienceswith a food.1999 Vol. 12 Nos. 3&4 47
<strong>Fam</strong><strong>ily</strong> Preferences <strong>and</strong> CultureThe social context in which foods arepresented also influences whether theyare accepted: young children who observeadults eating a certain food aremore likely to eat it. Likewise, using afood as a reward or presenting it withsome attention from the adult alsoenhances a child’s acceptance of it (8).But rewarding children <strong>for</strong> eating acertain food tends to decrease theiracceptance of that food.Skinner et al. (46) have found a strongrelationship between the food preferencesof toddlers <strong>and</strong> those of their mothers,fathers, <strong>and</strong> older siblings, but no fam<strong>ily</strong>member appeared to have more influencethan another had on children’spreferences. Likewise, Burt <strong>and</strong> Hertzler(14) have found that mothers’ <strong>and</strong> fathers’food preferences had a positive <strong>and</strong>equal influence on preferences of their5- <strong>and</strong> 6-year-old children.Other studies have also shown positivecorrelations between parents’ <strong>and</strong> theiryoung children’s preferences, but theassociations were not always significant<strong>and</strong> varied somewhat with children’sages (4,14,39). A meta-analysis of fivestudies demonstrated a small but significantcorrelation between the foodpreferences of parents <strong>and</strong> those of theirchildren 2 to 24 years of age (9). Thestrength of the resemblance was similar<strong>for</strong> mothers’ <strong>and</strong> fathers’ preferences.Studies of families’ food preferenceshave identified factors in addition toparents’ preferences that affect children’sfood preferences. Birch (4) concludedthat the resemblances in food preferencesof parents <strong>and</strong> those of 128 preschoolchildren were at least partiallyexplained by cultural similarities. However,other studies obtained somewhatdifferent results. Pliner (40) found thatthe food preferences of children 24 to83 months old matched those of theirreal fam<strong>ily</strong> more closely than those of‘‘pseudo’’ families (unrelated familiesfrom the same socioeco<strong>nom</strong>ic group).Effects of Parental Concerns,<strong>Nutrition</strong> Knowledge, Beliefs,<strong>and</strong> PracticesAlthough research indicates that youngchildren overall are likely to meet theirnutrient needs, parents continue toexpress concerns about their children’sdietary habits. In spite of the rise inchildhood obesity, parents of youngchildren are more apt to report beingconcerned about the perceived lack offood children consume than about thetypes of food consumed or the eatingenvironment (47). Parents had severalprimary concerns about children’seating habits:• Not eating enough. (Seventeenpercent describe their child as a‘‘picky eater.’’)• Eating too many sweets.• Eating a limited number of foods.(Meats <strong>and</strong> vegetables are mostoften disliked.)• Not drinking enough milk.Some studies have explored the effectsof parents’ nutrition knowledge on theirchildren’s knowledge <strong>and</strong> dietarypractices. Contento et al. found that Lati<strong>nom</strong>others’ nutrition knowledge <strong>and</strong> attitudestoward nutrition were positivelycorrelated with nutrient intakes of their4- to 5-year-old children (15). Kirks et al.(31) found that involving parents in anutrition education program <strong>for</strong> primarygradestudents increased the diversity<strong>and</strong> quality of students’ diets. Furthermore,a 5-year follow-up with the samestudents showed that they continued toeat a better quality diet than studentswhose parents had not participated inthe original nutrition education intervention(32). Thus parental involvementappeared to increase the fam<strong>ily</strong>’s overallnutrition knowledge as well as thelikelihood that nutrition in<strong>for</strong>mationwould be integrated into fam<strong>ily</strong> foodshopping<strong>and</strong> food-preparation practices.Compared with other children, thosefrom families whose mothers consideredhealthfulness an important criterion<strong>for</strong> selecting foods consumed dietssignificantly lower in calories, fat,saturated fat, <strong>and</strong> sucrose <strong>and</strong> higher infiber <strong>and</strong> vitamin A (15). Oliveria et al.,examining the relationship betweennutrient intakes of parents <strong>and</strong> their3- to 5-year-old children participatingin the Framingham Children’s Study,found a modest but significant associationbetween parents’ <strong>and</strong> children’sintakes <strong>for</strong> most nutrients (37). Theassociation was stronger betweenmothers <strong>and</strong> children than fathers <strong>and</strong>children, <strong>and</strong> the strength of the associationincreased with the number of mealsparents consumed at home.Stanek (47) identified other parentingbehaviors that were correlated positivelywith the nutrient adequacy (defined asnumber of servings from the major foodgroups) of the diets of 2- to 5-year-olds:• Having the child prepare food or setthe table.• Allowing the child to make decisionsabout the type of food eaten.• Giving small portions when servinga new food.• Using discussion versus other techniquesto persuade the child to eat.• Forcing the child to eat a few bitesof a food.• Praising the child <strong>for</strong> eating healthfulfoods.48 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Stanek also found a positive correlationbetween the quality of the home environment(measured as degree of cohesion,expressiveness, <strong>and</strong> conflictwithin the fam<strong>ily</strong>) <strong>and</strong> the nutrientadequacy of the children’s diets. Childrenwho ate with parents, siblings, orboth at mealtime also had better diets,defined as more servings from the fivebasic food groups.Effects of Maternal Employmenton Children’s Dietary BehaviorMaternal employment is another factorthat has been studied in relation to fam<strong>ily</strong>food consumption patterns <strong>and</strong> children’sdiets in the United States. Kirk ranked,from most important to least important,influences on working mothers’ foodchoices <strong>for</strong> their families: <strong>Nutrition</strong>,time, catering to fam<strong>ily</strong> members’ desires,budget, management <strong>and</strong> organization,health, season <strong>and</strong> weather, <strong>and</strong> socialization(30). Johnson concluded thatincreased time pressure was one ofthe most significant factors affectingchildren’s food choices: in general, themore hours women work outside thehome, the fewer hours they spend preparingmeals <strong>and</strong> the more meals theirchildren eat away from home. Thisincrease in away-from-home eating,however, represents primar<strong>ily</strong> mealseaten in schools <strong>and</strong> child-care centers,which often have a positive effect onchildren’s overall nutrient intakes.Negative effects of maternal employmenton children’s dietary status havenot yet been identified (28).<strong>Fam</strong><strong>ily</strong> Influences on OtherAspects of Children’s DietaryBehaviorInvestigators have examined how familiesaffect children’s attitudes toward nutrition,awareness of nutrition, the timethey spend eating, <strong>and</strong> their ability toregulate their energy intake. Gillespie<strong>and</strong> Achterberg (23) found, among1999 Vol. 12 Nos. 3&4 49
Parents, caregivers,<strong>and</strong> nutrition educatorshave significant rolesin helping childrendevelop healthfulfood-related behaviors.parents participating in a nutrition educationprogram, more positive attitudestoward nutrition <strong>and</strong> higher scores onan instrument measuring fam<strong>ily</strong> interactions.Parents participating in the nutritioneducation program, compared withother parents, also reported discussingfood <strong>and</strong> nutrition top<strong>ics</strong> with theirfamilies more frequently. Involvingchildren in food-related decisions <strong>and</strong>activities can increase their awarenessof nutrition <strong>and</strong> bring about changes indietary behavior. Anliker found that boththe quantity <strong>and</strong> specificity of parents’messages about foods were correlatedpositively to children’s nutritionknowledge (1).Klesges, in studies of the effects ofparental influences on preschool children’sfood selections , found thatparental encouragement to eat wascorrelated positively with the amountof time children spent eating (33,34).Both actual <strong>and</strong> threatened parentalmonitoring of food choices <strong>for</strong> a givenmeal had a marked effect on children’sfood selections by lowering total calories<strong>and</strong> sugar content of the meal.Young children’s ability to regulate theirtotal energy intake is well documented(7,44), although children vary tremendouslyin what <strong>and</strong> how much they eat.Johnson <strong>and</strong> Birch examined the relationshipsamong 3- to 5-year-old children’seating behavior, adiposity, <strong>and</strong>familial factors: such as parents’adiposity, eating style, diet history,<strong>and</strong> child-feeding practices (29). Theresults of their study: individual differencesin ability to self-regulate energyintake were related to adiposity, withthe fattest children being the least precisein this regulation. This is particularlypronounced in girls (6). Childrenwho were the least responsive to theenergy content of their diet also hadparents who reported using the mostrigid controls over their children’seating.Another study, with 3-year-olds, foundthat the children with more control overfood choices were significantly moreaware of the role of foods in energybalance, <strong>and</strong> those children who weremore involved in food-related activitieshad significantly higher levels of nutritionawareness (1). The study also foundthat the mothers of these children hadsome similar characterist<strong>ics</strong>: they weremore educated, more permissive, <strong>and</strong>employed outside the home.Child-Care Programs <strong>and</strong>Children’s Dietary BehaviorThe nutrient contribution of foodsserved <strong>and</strong> the food choices by childrenin child-care settings have a substantialeffect on the overall quality of children’sdiets. Briley et al. (12) found that thenutrition knowledge <strong>and</strong> practices offood service personnel in child-caresettings had a major influence on themenus served there. USDA’s 1997evaluation of the food preparers of theChild <strong>and</strong> Adult Care Feeding Program(CACFP) 1 found that they had a reasonablygood underst<strong>and</strong>ing of generalnutrition <strong>and</strong> Dietary Guidelines principles(22). The combination of meals <strong>and</strong>snacks offered by CACFP providerssupplied more than half of the RDA<strong>for</strong> energy <strong>and</strong> two-thirds of the RDA<strong>for</strong> other key nutrients (22). However,earlier research studies conducted onsiteat several licensed child-care centersfound that menus did not meet children’snutrient requirements consistently, even1 CACFP provides Federal funds <strong>for</strong> meals <strong>and</strong>snacks served to children in nonresidential daycarecenters. CACFP has established minimalmeal-pattern requirements <strong>for</strong> child-care providers;it specifies both meal components <strong>and</strong> minimalportion sizes according to children’s age (22).50 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
when CACFP meal-pattern requirementswere followed (10,17,19). Nutrientsreported below 50 percent of the RDAin menus designed <strong>for</strong> preschoolers atcertain sites included calories, iron, zinc,<strong>and</strong> vitamin A (10,12,17). In addition,menus often exceeded recommendedguidelines <strong>for</strong> fat, saturated fat, <strong>and</strong>sodium.Another study conducted in fam<strong>ily</strong> daycarehomes in Texas found that menuswere adequate <strong>for</strong> all nutrients, exceptiron; however, adequacy depended inpart on serving amounts of foods thatwere twice the minimum serving requiredby the CACFP (11). Studiesprior to USDA’s 1997 study had identifiednumerous gaps in providers’knowledge of nutrition that affectedthe nutrient adequacy of meals <strong>and</strong>snacks that were served (10,11,12,19).Other factors that influence what isserved to young children at child-carecenters include requirements of the foodprogram, staff perceptions of children’sfood preferences, history of the foodprograms at the center, <strong>and</strong> cost (12).Studies reveal that centers sometimesfailed to serve required portions offoods because providers did not believechildren would eat the whole amount(12). In general, providers rarely talkedwith the children about the sources offood or it’s benefit to them. They, however,did coax children to eat theirmeals <strong>and</strong> snacks.Food <strong>and</strong> nutrition practices in childcareprograms extend beyond what foodschildren are served. Nahikian-Nelmsexamined the nutrition knowledge,attitudes, <strong>and</strong> behaviors of caregiversin child-care settings to determinewhether attitudes <strong>and</strong> behaviors thoughtto be important in the development ofgood eating habits were typicallypracticed (36). Results indicated thatwhile caregivers held beliefs that wereexpected to have a positive effect onchildren’s dietary behavior, caregiversalso engaged in mealtime behaviors thatwere inconsistent with their beliefs <strong>and</strong>experts’ recommendations. For example,caregivers sometimes failed to dinewith children, or they consumed foodsthat were different from those being consumedby the children. Also,mealtimes were often dominated bycaregivers’ rule-setting behaviors thatprecluded any opportunity to discussfood <strong>and</strong> nutrition top<strong>ics</strong> with thechildren.1999 Vol. 12 Nos. 3&4 51
ConclusionsThis literature review, focusing on children’sdietary practices, complementsthe findings from the other componentsof the USDA project to develop a foodguide <strong>for</strong> young children (35,43,49).Overall, the review indicates associationsbetween young children’s foodpreferences <strong>and</strong> the food-related practicesof their parents <strong>and</strong> caregivers.Parents, caregivers, <strong>and</strong> nutritioneducators have significant roles inhelping children develop healthfulfood-related behaviors. Findings indicatethat parents <strong>and</strong> child-care providersshould choose developmentally appropriatefoods, provide structured meals<strong>and</strong> snacks, <strong>and</strong> ensure a pleasant eatingenvironment. Parents <strong>and</strong> caregiversmust be persistent <strong>and</strong> patient in offeringchildren a variety of both new <strong>and</strong> familiarfoods to promote children’s acceptanceof new foods. Child-care providers,important co-participants with parentsin helping children learn about <strong>and</strong>practice healthful eating habits, areresponsible <strong>for</strong> making a variety ofnutritious foods available <strong>and</strong> <strong>for</strong>serving as role models <strong>for</strong> the childrenin their care.Helping parents underst<strong>and</strong> the importanceof learning <strong>and</strong> experience in the<strong>for</strong>mation of children’s food preferencesmay enable them to foster developmentof healthful eating patterns <strong>and</strong> lessentheir anxieties about child feeding.<strong>Nutrition</strong> educators can help parents <strong>and</strong>caregivers of young children identify<strong>and</strong> develop appropriate food-relatedbehaviors, as well as teach them how toavoid undesirable ones. Educators shouldcarefully assess parents’ <strong>and</strong> caregivers’needs in developing programs or materials<strong>for</strong> them <strong>and</strong> their children. Top<strong>ics</strong> thatmay be appropriate <strong>for</strong> discussion rangefrom food composition <strong>and</strong> nutrientneeds to stages of child development<strong>and</strong> fam<strong>ily</strong> communication skills.The Food Guide Pyramid <strong>for</strong> YoungChildren 2 to 6 Years Old (50) wasdeveloped as a tool <strong>for</strong> parents <strong>and</strong>caregivers to use both to feed youngchildren <strong>and</strong> to communicate food<strong>and</strong> nutrition messages to them. It wasdeveloped with focus group input fromboth parents <strong>and</strong> caregivers about thenutritional needs of young children <strong>and</strong>key concerns <strong>and</strong> barriers to meetingthose needs at home <strong>and</strong> in the childcaresetting.Materials that accompany the adaptedfood guide highlight several of the findingsfrom research on children’s dietarypractices, including (1) the importanceof offering children a variety of foods tomeet their nutritionl needs; (2) the needto introduce <strong>and</strong> continually reintroducethe same foods to children; (3) the principlethat parents <strong>and</strong> caregivers areresponsible <strong>for</strong> offering children nutritiousfood choices, while children areresponsible <strong>for</strong> deciding what <strong>and</strong> howmuch they eat; (4) the importance ofbeing flexible with amounts of foodsserved at a given eating occasion; <strong>and</strong>(5) the need to involve all fam<strong>ily</strong> membersin making healthful food choices. TheFood Guide Pyramid <strong>for</strong> Young Childrenalso stresses the importance of rolemodeling <strong>and</strong> the need <strong>for</strong> parents <strong>and</strong>caregivers to work together to improvechildren’s dietary habits. Numerouspractical tips <strong>and</strong> h<strong>and</strong>s-on, developmentallyappropriate activities areprovided to help parents <strong>and</strong> caregiversintroduce food-preparation skills toyoung children.Focusing on changing what childrenlike to eat through repeated exposureto healthful foods <strong>and</strong> parental <strong>and</strong>community involvement in modelinghealthful eating behavior is more likelyto be effective in reaching young childrenthan simply teaching to increasenutrition knowledge (25). To be successfulin promoting <strong>and</strong> rein<strong>for</strong>cing dietsconsistent with the Dietary Guidelines<strong>and</strong> the Food Guide Pyramid, nutritioneducators <strong>and</strong> programs need to targetall environments of the preschoolchild----home, school, <strong>and</strong> community(42).52 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
References1. Anliker, J., Laus, M., Samonds, K., <strong>and</strong> Beal, V. 1990. Parental messages <strong>and</strong> thenutrition awareness of preschool children. Journal of <strong>Nutrition</strong> Education 22:24-29.2. Birch, L. 1979. Preschool children’s food preferences <strong>and</strong> consumption patterns.Journal of <strong>Nutrition</strong> Education 11:189-192.3. Birch, L. 1980. Effects of peer models’ food choices <strong>and</strong> eating behaviors onpreschoolers’ food preferences. Child Development 51:489-496.4. Birch, L. 1980. The relationship between children’s food preferences <strong>and</strong> thoseof their parents. Journal of <strong>Nutrition</strong> Education 12:14-18.5. Birch, L. 1992. Children’s preferences <strong>for</strong> high-fat foods. <strong>Nutrition</strong> Reviews50:249-255.6. Birch, L. 1996. Children’s food acceptance patterns. <strong>Nutrition</strong> Today 31(6):234-240.7. Birch, L., Johnson, S., Andresen, G., Peters, J., <strong>and</strong> Schulte, M. 1991. Thevariability of young children’s energy intake. New Engl<strong>and</strong> Journal of Medicine324:232-235.8. Birch, L., Johnson, S., <strong>and</strong> Fisher, J. 1995. Children’s eating: The developmentof food acceptance patterns. Young Children 50(2):71-78.9. Borah-Giddens, J. <strong>and</strong> Falciglia, G. 1993. A meta-analysis of the relationship infood preferences between parents <strong>and</strong> children. Journal of <strong>Nutrition</strong> Education25:102-107.10. Briley, M., Buller, A., Roberts-Gray, C., <strong>and</strong> Sparkman, A. 1989. What is on themenu at the child care center? Journal of the American Dietetic Association 89:771-774.11. Briley, M., Coyle, E., Roberts-Gray, C., <strong>and</strong> Sparkman, A. 1989. <strong>Nutrition</strong>knowledge <strong>and</strong> attitudes <strong>and</strong> menu planning skills of fam<strong>ily</strong> day-care providers.Journal of the American Dietetic Association 89:694-695.12. Briley, M., Roberts-Gray, C., <strong>and</strong> Simpson, D. 1994. Identification of factorsthat influence the menu at child care centers: A grounded theory approach. Journalof the American Dietetic Association 94:276-281.13. Bronner, Y.L. 1996. <strong>Nutrition</strong>al status outcomes <strong>for</strong> children: Ethnic, cultural,<strong>and</strong> environmental contexts. Journal of the American Dietetic Association 96:891-900.14. Burt, J. <strong>and</strong> Hertzler, A. 1978. Parental influence on the child’s food preference.Journal of <strong>Nutrition</strong> Education 10:127-128.15. Contento, I., Basch, C., Shea, S., Gutin, B., Zybert, P., Michela, J., <strong>and</strong> Rips, J.1993. Relationship of mothers’ food choice criteria to food intake of preschool children:Identification of fam<strong>ily</strong> subgroups. Health Education Quarterly 20: 243-259.16. Crockett, S. <strong>and</strong> Sims, L. 1995. Environmental influences on children’s eating.Journal of <strong>Nutrition</strong> Education 27:235-249.17. Domer, J.A. 1983. <strong>Nutrition</strong> in a private day care center. Journal of the AmericanDietetic Association 82:290-293.1999 Vol. 12 Nos. 3&4 53
18. Dunn, P., Lackey, C., Kolasa, K., <strong>and</strong> Mustian, R. 1994. <strong>Nutrition</strong> educationinterests of parents of 5- to 8-year-old children. Journal of <strong>Nutrition</strong> Education26:284-286.19. Drake, M. 1992. Menu evaluation, nutrient intake of young children, <strong>and</strong> nutritionknowledge of menu planners in child care centers in Missouri. Journal of <strong>Nutrition</strong>Education 24:145-148.20. Fisher, J. <strong>and</strong> Birch, L. 1995. Fat preferences <strong>and</strong> fat consumption of 3- to 5-year-old children are related to parental adiposity. Journal of the American DieteticAssociation 95:759-764.21. Food <strong>and</strong> Consumer Service, U.S. Department of Agriculture. 1995. Child <strong>and</strong>Adult Care Food Program: <strong>Nutrition</strong> Guidance <strong>for</strong> Child Care <strong>Center</strong>s. Alex<strong>and</strong>ria,VA.22. Food <strong>and</strong> Consumer Service, U.S. Department of Agriculture. 1997. EarlyChildhood <strong>and</strong> Child Care Study: <strong>Nutrition</strong>al Assessment of the Child <strong>and</strong> AdultCare Food Program. Alex<strong>and</strong>ria, VA.23. Gillespie, A. <strong>and</strong> Achterberg, C. 1989. Comparison of fam<strong>ily</strong> interaction patternsrelated to food <strong>and</strong> nutrition. Journal of the American Dietetic Association 89: 509-512.24. Hammer, L. 1992. The development of eating behavior in childhood. PediatricClin<strong>ics</strong> of North America 39:379-394.25. Harvey-Berino, J., Hood, V., Rourke, J., Terrance, T., Dorwaldt, A., <strong>and</strong> Secker-Walker, R. 1997. Food preferences predict eating behavior of very young Mohawkchildren. Journal of the American Dietetic Association 97:750-753.26. Hertzler, A. 1989. Preschoolers’ food h<strong>and</strong>ling skills----motor development.Journal of <strong>Nutrition</strong> Education 21:100B.27. Hertzler, A. <strong>and</strong> DeBord, K. 1994. Preschoolers’ developmentally appropriatefood <strong>and</strong> nutrition skills. Journal of <strong>Nutrition</strong> Education 26:166B.28. Johnson, R., Crouter, A., <strong>and</strong> Smiciklas-Wright, H. 1993. Effects of maternalemployment on fam<strong>ily</strong> food consumption patterns <strong>and</strong> children’s diets. Journal of<strong>Nutrition</strong> Education 25:130-133.29. Johnson, S. <strong>and</strong> Birch, L. 1994. Parents’ <strong>and</strong> children’s adiposity <strong>and</strong> eatingstyle. Pediatr<strong>ics</strong> 94:653-661.30. Kirk, M. <strong>and</strong> Gillespie, A. 1990. Factors affecting food choices of workingmothers with young families. Journal of <strong>Nutrition</strong> Education 22:161-168.31. Kirks, B., Hendricks, D., <strong>and</strong> Wyse, B. 1982. Parent involvement in a nutritioneducation program <strong>for</strong> primary grade students. Journal of <strong>Nutrition</strong> Education14:137-140.32. Kirks, B. <strong>and</strong> Hughes, C. 1986. Long-term behavioral effects of parent involvementin nutrition education. Journal of <strong>Nutrition</strong> Education 18:203-206.33. Klesges, R.C., Malott, J.M., Boschee, P.F., <strong>and</strong> Weber, J.M. 1986. The effectsof parental influences on children’s food intake, physical activity, <strong>and</strong> relativeweight. International Journal of Eating Disorders 5:335-346.54 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
34. Klesges, R., Stein, R., Eck, L., Isbell, T., <strong>and</strong> Klesges, L. 1991. Parental influenceon food selection in young children <strong>and</strong> its relationship to childhood obesity. AmericanJournal of Clinical <strong>Nutrition</strong> 53:859-864.35. Marcoe, K.L. 1999. Technical research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> YoungChildren. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):17-31.36. Nahikian-Nelms, M. 1997. Influential factors of caregiver behavior at mealtime:A study of 24 child-care programs. Journal of the American Dietetic Association97:505-509.37. Oliveria, S., Ellison, R., Moore, L., Gillman, M., Garrahie, E., <strong>and</strong> Singer, M.1992. Parent-child relationships in nutrient intake: The Framingham Children’sStudy. American Journal of Clinical <strong>Nutrition</strong> 56:593-598.38. Pilgrim, F. J. 1961. What foods do people accept or reject? Journal of the AmericanDietetic Association 38:439-443.39. Pliner, P. 1983. <strong>Fam</strong><strong>ily</strong> resemblance in food preferences. Journal of <strong>Nutrition</strong>Education 15:137-140.40. Pliner, P. <strong>and</strong> Pelchat, M. 1986. Similarities in food preferences between children<strong>and</strong> their siblings <strong>and</strong> parents. Appetite 7:333-342.41. Ray, J. <strong>and</strong> Klesges, R. 1993. Influences on the eating behavior of children.Annals of the New York Academy of Sciences 699:57-69.42. Reed, D. 1996. Focus groups identify desirable features of nutrition programs<strong>for</strong> low-income mothers of preschool children. Journal of the American DieteticAssociation 96:501-503.43. Saltos, E. 1999. Adapting the Food Guide Pyramid <strong>for</strong> Children: Defining thetarget audience. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):3-16.44. Shea, S., Stein, A., Basch, C., Contento, I., <strong>and</strong> Zybert, P. 1992. Variability <strong>and</strong>self-regulation of energy intake in young children in their everyday environment.Pediatr<strong>ics</strong> 90:542-546.45. Sigman-Grant, M. 1992. Feeding preschoolers: Balancing nutritional <strong>and</strong> developmentalneeds. <strong>Nutrition</strong> Today July/August.46. Skinner, J., Carruth, B., Moran, J., Houch, K., Schmidhammer, J., Reed, A.,Coletta, F., Cotter, R., <strong>and</strong> Ott, D. 1998. Toddlers’ food preferences: Concordancewith fam<strong>ily</strong> members’ preferences. Journal of <strong>Nutrition</strong> Education 30:17-22.47. Stanek, K., Abbott, D., <strong>and</strong> Cramer, S. 1990. Diet quality <strong>and</strong> the eating environmentof preschool children. Journal of the American Dietetic Association 90:1582-1584.48. Sullivan, S. <strong>and</strong> Birch, L. 1990. Pass the sugar, pass the salt: Experience dictatespreference. Developmental Psychology 26:546-551.49. Tarone, C. 1999. Consumer research: Food Guide Pyramid <strong>for</strong> Young Children.<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review 12(3&4):33-44.50. U.S. Department of Agriculture. 1999. Tips <strong>for</strong> Using the Food Guide Pyramid<strong>for</strong> Young Children Two to Six Years Old. Program Aid 1647.1999 Vol. 12 Nos. 3&4 55
Expenditures on Childrenby <strong>Fam</strong>ilies, 1999Mark Lino<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>Since 1960 the U.S. Department of Agriculture has provided estimates ofexpenditures on children from birth through age 17. This article presentsthe most recent estimates <strong>for</strong> husb<strong>and</strong>-wife <strong>and</strong> single-parent families. Dataare from the 1990-92 Consumer Expenditure Survey. The Consumer PriceIndex is used to update income <strong>and</strong> expenditures to 1999 dollars. Data <strong>and</strong>methods used in calculating child-rearing expenses are described. Estimatesare provided <strong>for</strong> major components of the budget by age of the child, fam<strong>ily</strong>income, <strong>and</strong> region of residence. Expenses on the younger child in a twochild,husb<strong>and</strong>-wife household <strong>for</strong> the overall United States averaged $6,080to $13,800 in 1999, depending on the child’s age <strong>and</strong> fam<strong>ily</strong> income group.Adjustment factors <strong>for</strong> number of children in the household are also provided.Results of this study can be used in developing State child support guidelines<strong>and</strong> foster care payments <strong>and</strong> in developing fam<strong>ily</strong> educational programs.Since 1960 the U.S. Departmentof Agriculture (USDA)has provided estimates ofexpenditures on childrenfrom birth through age 17. These estimatesare used in setting child supportguidelines <strong>and</strong> foster care payments <strong>and</strong>in developing educational programson parenthood. This study presents thelatest child-rearing expense estimates,which are based on 1990-92 expendituredata updated to 1999 dollars. The studypresents these new estimates <strong>for</strong> husb<strong>and</strong>wife<strong>and</strong> single-parent families. It brieflydescribes the data <strong>and</strong> methods used incalculating child-rearing expenses 1 <strong>and</strong>then discusses the estimated expenses.1 The report ‘‘Expenditures on Children by <strong>Fam</strong>ilies:1999 Annual Report’’ provides a more detaileddescription of the data <strong>and</strong> methods. To obtain acopy, contact USDA, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>, 1120 20th Street NW, Suite 200North Lobby, Washington, DC 20036 (telephone:202-418-2312) or download fromhttp://www.usda.gov/cnpp).The estimates are provided <strong>for</strong> the overallUnited States. The child-rearing expenseestimates <strong>for</strong> husb<strong>and</strong>-wife families arealso provided <strong>for</strong> urban areas in fourregions (Northeast, South, Midwest,<strong>and</strong> West) <strong>and</strong> rural areas throughoutthe United States 2 to adjust partially <strong>for</strong>price differentials <strong>and</strong> varying patternsof expenditures. For single-parent families,estimates are provided only <strong>for</strong> the overallUnited States because of limitationsin the sample size. Expenditures onchildren are estimated <strong>for</strong> the majorbudgetary components: Housing, food,transportation, clothing, health care,child care <strong>and</strong> education, <strong>and</strong> miscellaneousgoods <strong>and</strong> services. The boxdescribes each expenditure component.2 Urban areas are defined as Metropolitan StatisticalAreas (MSA’s) <strong>and</strong> other places of 2,500 or morepeople outside an MSA; rural areas are places ofless than 2,500 people outside an MSA.56 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Categories of Household ExpendituresHousing expenses consists of shelter (mortgage interest, property taxes, or rent; maintenance <strong>and</strong> repairs; <strong>and</strong> insurance),utilities (gas, electricity, fuel, telephone, <strong>and</strong> water), <strong>and</strong> house furnishings <strong>and</strong> equipment (furniture, floor coverings, majorappliances, <strong>and</strong> small appliances). For homeowners, housing expenses do not include mortgage principal payments; in theConsumer Expenditure Survey, such payments are considered to be part of savings. So, total dollars allocated to housing byhomeowners are underestimated in this report.Food expenses consists of food <strong>and</strong> nonalcoholic beverages purchased at grocery, convenience, <strong>and</strong> specialty stores, includingpurchases with food stamps; dining at restaurants; <strong>and</strong> household expenditures on school meals.Transportation expenses consists of the net outlay on purchase of new <strong>and</strong> used vehicles, vehicle finance charges, gasoline <strong>and</strong>motor oil, maintenance <strong>and</strong> repairs, insurance, <strong>and</strong> public transportation.Clothing expenses consists of children’s apparel such as diapers, shirts, pants, dresses, <strong>and</strong> suits; footwear; <strong>and</strong> clothing servicessuch as dry cleaning, alterations <strong>and</strong> repair, <strong>and</strong> storage.Health care expenses consists of medical <strong>and</strong> dental services not covered by insurance, prescription drugs <strong>and</strong> medical supplies notcovered by insurance, <strong>and</strong> health insurance premiums not paid by employer or other organization.Child care <strong>and</strong> education expenses consists of day care tuition <strong>and</strong> supplies; baby-sitting; <strong>and</strong> elementary <strong>and</strong> high school tuition,books, <strong>and</strong> supplies.Miscellaneous expenses consists of personal care items, entertainment, <strong>and</strong> reading materials.DataThe 1990-92 Consumer ExpenditureSurvey (CE) is used to estimate expenditureson children. Administered by theBureau of Labor Statist<strong>ics</strong> (BLS), theCE collects in<strong>for</strong>mation on sociodemographiccharacterist<strong>ics</strong>, income,<strong>and</strong> expenditures of households.The CE has been conducted annuallysince 1980 <strong>and</strong> interviews about 5,000households each quarter over a 1-yearperiod. Each quarter is deemed an independentsample by BLS; thus, the totalnumber of households in the 1990-92survey is about 60,000.Husb<strong>and</strong>-wife <strong>and</strong> single-parent familieswere selected from these households <strong>for</strong>this study if (1) they had at least onechild of their own----age 17 or under----inthe household, (2) they had six or fewerchildren, (3) there were no other relatedor unrelated people present in the householdexcept their own children, <strong>and</strong> (4)they were complete income reporters.Complete income reporters are householdsthat provide values <strong>for</strong> majorsources of income, such as wages <strong>and</strong>salaries, self-employment income, <strong>and</strong>Social Security income. Quarterly expenditureswere annualized. The sampleconsisted of 12,850 husb<strong>and</strong>-wife households<strong>and</strong> 3,395 single-parent households.BLS weighting methods were used toweight the sample to reflect the U.S.population of interest. Although basedon 1990-92 data, the expense estimateswere updated to 1999 dollars by usingthe Consumer Price Index (CPI-U).(Expenditure <strong>and</strong> income data <strong>for</strong> 1990<strong>and</strong> 1991 were first converted to 1992dollars; then all 3 years of data wereupdated to 1999 dollars.)MethodsThe CE collects overall householdexpenditure data <strong>for</strong> some budgetarycomponents (housing, food, transportation,health care, <strong>and</strong> miscellaneousgoods <strong>and</strong> services) <strong>and</strong> child-specificexpenditure data <strong>for</strong> other components(clothing, child care, <strong>and</strong> education).Multivariate analysis was used to estimatehousehold <strong>and</strong> child-specificexpenditures. Income level, fam<strong>ily</strong>size, <strong>and</strong> age of the younger child werecontrolled so that estimates could bemade <strong>for</strong> families with these varyingcharacterist<strong>ics</strong>. Regional estimateswere derived by controlling <strong>for</strong> region.1999 Vol. 12 Nos. 3&4 57
The three income groups of husb<strong>and</strong>wifehouseholds were determined bydividing the sample <strong>for</strong> the overall UnitedStates into equal thirds. The incomegroups were be<strong>for</strong>e-tax income under$31,000, between $31,000 <strong>and</strong> $52,160,<strong>and</strong> over $52,160 in 1992 dollars.For each income level, the estimateswere <strong>for</strong> husb<strong>and</strong>-wife families withtwo children. The younger child wasin one of six age categories: 0-2, 3-5,6-8, 9-11, 12-14, <strong>and</strong> 15-17. Householdswith four members (two children) wereselected as the st<strong>and</strong>ard because in 1990-92 this was the average household sizeof two-parent families. The focus wason the younger child in a householdbecause the older child was sometimesover age 17.The estimates are based on CE interviewsof households with <strong>and</strong> withoutspecific expenses; so <strong>for</strong> some families,expenditures may be higher or lowerthan the mean estimates, depending onwhether they incur the expense. Thisparticularly applies to child care <strong>and</strong>education <strong>for</strong> which about 50 percentof families in the study had no expenditure.Also, the estimates only coverout-of-pocket expenditures on childrenmade by the parents <strong>and</strong> not by others,such as gr<strong>and</strong>parents or friends. Forexample, the value of clothing gifts tochildren from gr<strong>and</strong>parents would notbe included in clothing expenses.Regional income categories were basedon the national income categories in1992 dollars, updated to 1999 dollarsby using regional CPI’s. The regionalincome categories were not divided intoequal thirds <strong>for</strong> each region as was done<strong>for</strong> the overall United States.After the various overall household <strong>and</strong>child-specific expenditures were estimated,these total amounts were allocatedamong the four fam<strong>ily</strong> members(husb<strong>and</strong>, wife, older child, <strong>and</strong> youngerchild). The estimated expenditures <strong>for</strong>clothing <strong>and</strong> child care <strong>and</strong> educationwere only <strong>for</strong> children. It was assumedthat these expenses were equally allocatedto each child; there<strong>for</strong>e, the estimatedexpenditures were divided bytwo (the number of children in thehousehold).Because the CE did not collect expenditureson food <strong>and</strong> health care by fam<strong>ily</strong>member, data from other Federal studieswere used to apportion these budgetarycomponents to children by age. Foodbudget shares as a percentage of totalfood expenditures----<strong>for</strong> the youngerchild in a husb<strong>and</strong>-wife household withtwo children----were determined byusing the 1994 USDA food plans (9).These shares were estimated by age ofthe child <strong>and</strong> household income level.The food budget shares were thenapplied to estimated household foodexpenditures to determine food expenseson children. Health care shares, as apercentage of total health care expenses<strong>for</strong> the younger child in a husb<strong>and</strong>-wifehousehold with two children, were calculatedfrom the 1987 National MedicalExpenditure Survey (4). These shareswere estimated by age of the child <strong>and</strong>applied to estimated household healthcare expenditures to determine expenseson children.No research base exists <strong>for</strong> allocatingestimated household expenditures onhousing, transportation, <strong>and</strong> miscellaneousgoods <strong>and</strong> services among householdmembers. Two of the most commonapproaches <strong>for</strong> allocating these expensesare the marginal cost method <strong>and</strong> theper capita method.The marginal cost method measuresexpenditures on children as the differencein expenses between couples withchildren <strong>and</strong> equivalent childless couples.This method depends on developmentof an equivalency measure; however,there is no universally accepted measure.Proposed methods have produceddifferent estimates of expenditureson children. 3 Some of the marginalcost approaches assume that parentsor couples do not alter expenditures onthemselves after a child is added to ahousehold. Also, couples without childrenoften buy larger-than-needed homes atthe time of purchase in anticipationof children. Comparing the expendituresof childless couples with expendituresof similar couples that have childrencould lead to underestimated expenditureson children. Lastly, the marginalcost method does not provide a directestimate of how much is spent on achild. It estimates how much moneyfamilies with children must be compensatedto bring the parents to the sameutility level (as gauged by an equivalencescale) of couples without children. Thisis a different question from ‘‘how muchdo parents spend on children?’’For these reasons, the USDA uses theper capita method to allocate housing,transportation, <strong>and</strong> miscellaneous goods<strong>and</strong> services among household members.The per capita method allocates expensesamong household members in equalproportions. Although the per capitamethod has limitations, these limitationswere considered less severe than thoseof the marginal cost approach.3 For a review of equivalency measures <strong>and</strong> estimatesof expenditures on children resulting fromthem, see U.S. Department of Health <strong>and</strong> HumanServices, Office of the Assistant Secretary <strong>for</strong>Planning <strong>and</strong> Evaluation, 1990, Estimates ofExpenditures on Children <strong>and</strong> Child SupportGuidelines (11).58 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Figure 1. Estimated 1999 annual fam<strong>ily</strong> expenditures on a child,by be<strong>for</strong>e-tax income level <strong>and</strong> age of child 1Dollars16,00014,00012,00010,0008,0006,0004,0002,00000-2 3-5 6-8 9-11 12-14 15-17Age of childLess than $36,800 $36,800 - $61,900 More than $61,9001 U.S. average <strong>for</strong> the younger child in husb<strong>and</strong>-wife families with children.A major limitation of the per capitamethod is that expenditures <strong>for</strong> an additionalchild may be less than averageexpenditures. Consequently, adjustment<strong>for</strong>mulas were devised to estimateexpenditures on one child or three ormore children <strong>for</strong> households of differentsizes. These <strong>for</strong>mulas are discussed laterin the paper. Transportation expensesresulting from employment activitiesare not related to expenses on children,so these costs were excluded from theestimated household transportationexpenses. Data used to estimate workrelatedtransportation expenses werefrom a 1990 U.S. Department of Transportationstudy (12).Although the USDA uses the per capitaapproach rather than a marginal costapproach in allocating housing, transportation,<strong>and</strong> miscellaneous expendituresto children in a household, a USDA studyexamined how these expenses would beallocated using different marginal costapproaches (5) . These approachesproduced estimates of expenditures onchildren <strong>for</strong> housing <strong>and</strong> miscellaneousgoods <strong>and</strong> services below those producedby the per capita method. In addition,these approaches produced estimates oftransportation expenditures on childrenabove those produced by the per capitamethod.Estimated Expenditures onChildren by Husb<strong>and</strong>-WifeHouseholdsEstimates of fam<strong>ily</strong> expenditures on theyounger child in husb<strong>and</strong>-wife householdswith two children are presented in tables2 through 7 on pp. 68-73. The estimatesare <strong>for</strong> the overall United States, urbanregions of the country, <strong>and</strong> overall ruralareas. Household income levels wereupdated to 1999 dollars by using theall-items category of the CPI-U, <strong>and</strong>expenditures were updated by using theCPI <strong>for</strong> the corresponding item (i.e., theCPI’s <strong>for</strong> housing, food, etc.). Regionalestimates were updated to 1999 dollarsby using the regional CPI’s. The followingsubsections highlight the child-rearingexpense estimates <strong>for</strong> the younger childin a two-child household <strong>for</strong> the overallUnited States by income level, budgetarycomponent, <strong>and</strong> age of the child. Childrearingexpenses by region are alsodiscussed.Income LevelEstimated expenses on children varyconsiderably by household income level(fig. 1). Depending on age of the child,the annual expenses range from $6,080to $7,150 <strong>for</strong> families in the lowestincome group (1999 be<strong>for</strong>e-tax incomeless than $36,800), from $8,450 to$9,530 <strong>for</strong> families in the middle-incomegroup (1999 be<strong>for</strong>e-tax income between$36,800 <strong>and</strong> $61,900), <strong>and</strong> from $12,550to $13,800 <strong>for</strong> families in the highestincome group (1999 be<strong>for</strong>e-tax incomemore than $61,900). On average, householdsin the lowest group spend 28 percentof their be<strong>for</strong>e-tax income per yearon a child; those in the middle-incomegroup, 18 percent; <strong>and</strong> those in the highestincome group, 14 percent. The rangein these percentages would be narrowerif after-tax income were considered,because a greater percentage of incomein higher income households goes towardtaxes.Although families in the highest incomegroup spend slightly less than twice theamount that families in the lowest incomegroup spend on a child, on average, theamount varies by budgetary component.In general, expenses on a child <strong>for</strong> goods<strong>and</strong> services considered to be necessities(such as food <strong>and</strong> clothing) do not1999 Vol. 12 Nos. 3&4 59
vary as much as those considered tobe discretionary (such as miscellaneousexpenses) among households in the threeincome groups. For example, clothingexpenses on a child age 15-17 average$680 in the lowest income group <strong>and</strong>$1,030 in the highest income group, a51-percent difference. Miscellaneousexpenses on the same age child average$630 in the lowest income group <strong>and</strong>$1,590 in the highest income group, a152-percent difference.Budgetary ComponentHousing accounts <strong>for</strong> the largest shareof total child-rearing expenses; figure 2shows this <strong>for</strong> families in the middleincomegroup. Based on an average <strong>for</strong>the six age groups, housing accounts <strong>for</strong>33 percent of child-rearing expenses <strong>for</strong>a child in the lowest <strong>and</strong> middle-incomegroups <strong>and</strong> 37 percent in the highestincome group. Food is the second largestaverage expense on a child <strong>for</strong> familiesregardless of income level. It accounts<strong>for</strong> 20 percent of child-rearing expenses<strong>for</strong> a child in the lowest income group,18 percent in the middle-income group,<strong>and</strong> 15 percent in the highest incomegroup. Transportation is the third largestchild-rearing expense, making up 13 to14 percent of child-rearing expensesacross income levels.Across the three income groups, miscellaneousgoods <strong>and</strong> services (personalcare items, entertainment, <strong>and</strong> readingmaterials) is the fourth largest expenseon a child <strong>for</strong> families (10 to 13 percent).Clothing (excluding that received asgifts or h<strong>and</strong>-me-downs) accounts <strong>for</strong>6 to 8 percent of expenses on a child<strong>for</strong> families, child care <strong>and</strong> educationaccounts <strong>for</strong> 8 to 11 percent, <strong>and</strong> healthcare accounts <strong>for</strong> 5 to 7 percent of childrearingexpenses across income groups.Estimated expenditures <strong>for</strong> health careinclude only out-of-pocket expensesFigure 2. Estimated fam<strong>ily</strong> expenditures on a child throughage 17, by budgetary share 1Total expenditures in 1999 dollars = $160,1401 U.S. average <strong>for</strong> the younger child in middle-income (1999 be<strong>for</strong>e-tax income between$36,800 <strong>and</strong> $61,900), husb<strong>and</strong>-wife families with two children.(including insurance premiums not paidby an employer or other organization)<strong>and</strong> not that portion covered by healthinsurance.Age of ChildExpenditures on a child are lower in theyounger age categories <strong>and</strong> higher in theolder age categories. Figure 3 depictsthis <strong>for</strong> families in the middle-incomegroup. This held across income groupseven though housing expenses, the highestchild-rearing expenditure, generallydecline as the child ages. The decline inhousing expenses reflects diminishinginterest paid by homeowners over thelife of a mortgage. Payments on principalare not considered part of housing costsin the CE; they are deemed to be part ofsavings.For all three income groups, food,transportation, clothing, <strong>and</strong> healthcare expenses related to child-rearinggenerally increase as the child’s ageincreases. Transportation expenses arehighest <strong>for</strong> a child age 15-17, when heor she would start driving. Child care<strong>and</strong> education expenses are highest <strong>for</strong> achild under age 6. Most of this expensemay be attributable to child care at thisage. The estimated expense <strong>for</strong> childcare <strong>and</strong> education may seem low <strong>for</strong>those with the expense. It should beremembered that the estimates reflectthe average of households with <strong>and</strong>without the expense.60 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Figure 3. Estimated 1999 annual fam<strong>ily</strong> expenditures on a child, by age <strong>and</strong> budgetary share 1Percent1008060$8,450 $8,660 $8,700 $8,650 $9,390 $9,530MiscellaneousChild care <strong>and</strong> educationClothingHealth careTransportation40Food20Housing00-2 3-5 6-8 9-11 12-14 15-17Age of child1 U.S. average <strong>for</strong> the younger child in middle-income (1999 be<strong>for</strong>e-tax income between $36,800 <strong>and</strong> $61,900), husb<strong>and</strong>-wife families with twochildren.RegionChild-rearing expenses in the regionsof the country reflect patterns observedin the overall United States: in eachregion, expenses on a child increase withhousehold income level <strong>and</strong>, generally,with age of the child. Overall childrearingexpenses are highest in the urbanWest, followed by the urban Northeast,<strong>and</strong> urban South. Figure 4 shows totalchild-rearing expenses by region <strong>and</strong>age of a child <strong>for</strong> middle-income families.Child-rearing expenses are lowest in theurban Midwest <strong>and</strong> rural areas. Muchof the difference in expenses on a childamong regions is related to housingcosts. Total housing expenses on a childare highest in the urban West <strong>and</strong> urbanNortheast <strong>and</strong> lowest in rural areas.However, child-rearing transportationexpenses are highest <strong>for</strong> families inrural areas. This likely reflects the longertraveling distances <strong>and</strong> the lack ofpublic transportation in these areas.Adjustments <strong>for</strong> Older Children<strong>and</strong> Household SizeThe expense estimates on a child representexpenditures on the younger childat various ages in a husb<strong>and</strong>-wife householdwith two children. It cannot beassumed that expenses on the olderchild are the same at these various ages.Expenses may vary by birth order. Themethod described on pp. 57-59 wasrepeated to determine whether a differenceexists, the extent of this difference,<strong>and</strong> how the expenditures may be adjustedto estimate expenses on an olderchild. The focus was on the older childin each of the same age categories asthose used with the younger child. Atwo-child fam<strong>ily</strong> was again used as thest<strong>and</strong>ard. Household income <strong>and</strong> regionof residence were not held constant, sofindings are applicable to all families.On average, <strong>for</strong> husb<strong>and</strong>-wife householdswith two children, expenditures do notvary by birth order. So, the expendituresin tables 2 through 7 reflect those oneither child in a two-child fam<strong>ily</strong>. Thus,annual expenditures on children in ahusb<strong>and</strong>-wife, two-child fam<strong>ily</strong> may beestimated by summing the expenses <strong>for</strong>the two appropriate age categories. Forexample, annual expenditures on childrenages 9-11 <strong>and</strong> 15-17 in a husb<strong>and</strong>-wifefam<strong>ily</strong> in the middle-income group <strong>for</strong>the overall United States would be$18,180 ($8,650 + $9,530). For specificbudgetary components, annual expenseson an older child vary, compared withthose on a younger child: families spend1999 Vol. 12 Nos. 3&4 61
Figure 4. Estimated 1999 annual fam<strong>ily</strong> expenditures on a child,by region <strong>and</strong> age 11 U.S. average <strong>for</strong> the younger child in middle-income, husb<strong>and</strong>-wife families with two children.For the urban West, the middle-income group had a 1999 be<strong>for</strong>e-tax income between $36,900<strong>and</strong> $62,000; the urban Northeast, between $36,500 <strong>and</strong> $61,400; <strong>for</strong> the urban South, between$36,800 <strong>and</strong> $61,900; <strong>for</strong> the urban Midwest, between $37,100 <strong>and</strong> $62,400; <strong>and</strong> <strong>for</strong> rural areas,between $37,200 <strong>and</strong> $62,600.more on clothing <strong>and</strong> education <strong>for</strong> anolder child but less on transportation.The estimates should also be adjusted ifa household has only one child or morethan two children. <strong>Fam</strong>ilies will spendmore or less on a child depending on thenumber of other children in the household<strong>and</strong> eco<strong>nom</strong>ies of scale. Multivariateanalysis was used to estimateexpenditures <strong>for</strong> each budgetary componentto derive these figures. Householdsize <strong>and</strong> age of the younger child werecontrolled; household income level <strong>and</strong>region of the country were not. Theresults, there<strong>for</strong>e, are applicable to allfamilies. These expenditures were thenassigned to a child by using the methoddescribed earlier. Compared with expenditures<strong>for</strong> each child in a husb<strong>and</strong>-wife,two-child fam<strong>ily</strong>, expenditures <strong>for</strong> thechild in a one-child fam<strong>ily</strong> average 24percent more <strong>and</strong> <strong>for</strong> those with three ormore children, 23 percent less on eachchild.There<strong>for</strong>e, to adjust the figures in tables2 through 7 to estimate annual overallexpenditures on an only child, users ofthis report should add 24 percent to thetotal expense <strong>for</strong> the child’s age category.To estimate expenditures on three ormore children, users should subtract23 percent from the total expense <strong>for</strong>62 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
each child’s age category <strong>and</strong> then sumthe totals. As an example of adjustmentsneeded <strong>for</strong> different numbers of children,the total expenses <strong>for</strong> a middle-incomefam<strong>ily</strong> in the overall United States on achild age 15-17 with no siblings wouldbe $11,820 ($9,530 x 1.24). The totalexpenses on three children ages 3-5,12-14, <strong>and</strong> 15-17 would be $21,240(($8,660 + $9,390 + $9,530) x .77). Fora particular budgetary component, thepercentages may be more or less. Asfam<strong>ily</strong> size increases, food costs perchild decrease less than housing <strong>and</strong>transportation costs per child decrease.Expenditures bySingle-Parent <strong>Fam</strong>iliesThe estimates of expenditures on childrenby husb<strong>and</strong>-wife families do not applyto single-parent families, a group thataccounts <strong>for</strong> an increasing percentageof families with children. There<strong>for</strong>e,separate estimates of child-rearingexpenses in single-parent householdswere made by using the CE data. Mostsingle-parent families in the surveywere headed by a woman: 90 percent.Expenditures on Children Over TimeSince 1960 the U.S. Department of Agriculture (USDA) has been providingestimates of expenditures on children from birth through age 17. The originalestimates were based on the 1960 Consumer Expenditure Survey. The figurebelow examines how these expenditure estimates have changed over time at5-year intervals. Depicted are the average total expenditures on a child frombirth through age 17 in a middle-income, husb<strong>and</strong>-wife fam<strong>ily</strong>. Expendituresare in <strong>nom</strong>inal (not adjusted <strong>for</strong> inflation) dollars.Expenses to raise a child to age 18 have increased dramatically even when adjusted<strong>for</strong> inflation, from $25,230 in 1960 ($142,000 in 1999 dollars) to $160,140 in1999. New components of child-rearing costs, particularly child care, are amongfactors causing this increase. In 1960 child care expenses were negligible becausemany mothers were not in the labor <strong>for</strong>ce. In 1999 child care expenses were amongthe largest expenditures made on preschool children by middle-income families.Total expenditures on a child <strong>for</strong> the first 18 years of life 1The method used in determining childrearingexpenses <strong>for</strong> two-parent householdswas followed. Multivariate analysiswas used to estimate expenditures <strong>for</strong>each budgetary component. Controlvariables were income level, householdsize, <strong>and</strong> age of the younger child (thesame age categories as used with childrenin two-parent families). A single parentwith two children was used as thest<strong>and</strong>ard <strong>for</strong> household size.Income groups of single-parent households(be<strong>for</strong>e-tax income under $31,000<strong>and</strong> $31,000 <strong>and</strong> over in 1992 dollars,inflated to 1999 dollars) were selectedto correspond with the income groups1 Average expenditures <strong>for</strong> a middle-income, husb<strong>and</strong>-wife fam<strong>ily</strong>, not adjusted <strong>for</strong> inflation.1999 Vol. 12 Nos. 3&4 63
Estimating Future CostsThe estimates presented in this study represent household expenditures on a child of a certain age in 1999. To estimate theseexpenses <strong>for</strong> the first 17 years, future price changes need to be incorporated in the figures. To do this, a future cost <strong>for</strong>mula isused such that:Cf = Cp (1 + i) nwhere:Cf = projected future annual dollar expenditure on a child of a particular ageCp = present (1999) annual dollar expenditure on a child of a particular agei = projected annual inflation (or deflation)n = number of years from present until child will reach a particular ageAn example of estimated futureexpenditures on the younger child in ahusb<strong>and</strong>-wife fam<strong>ily</strong> with two children<strong>for</strong> each of the three income groups <strong>for</strong>the overall United States is presented.The example assumes a child is bornin 1999 <strong>and</strong> reaches age 17 in the year2016. The example also assumes thatthe average annual inflation rate overthis time is 4.3 percent (the averageannual inflation rate over the past 20years) (10). Thus total fam<strong>ily</strong> expenseson a child through age 17 would be$174,090, $236,660, <strong>and</strong> $344,800 <strong>for</strong>households in the lowest, middle, <strong>and</strong>highest income groups, respectively.In 1999 dollars, these figures wouldbe $117,390, $160,140, <strong>and</strong> $233,850.Inflation rates other than 4.3 percentcould be used in the <strong>for</strong>mula if projectionsof these rates vary in the future.Also, it is somewhat unrealistic toassume that households remain in oneincome category as a child ages. Formost families, income rises over time.In addition, such projections assumechild-rearing expenditures change onlywith inflation, but parental expenditurepatterns also change over time.Estimated annual expenditures on a child born in 1999, by income group 1Income groupYear Age Lowest Middle Highest1999
used in estimating child-rearing expendituresin husb<strong>and</strong>-wife households. Thisincome includes child support payments.The two higher income groups of twoparentfamilies (income between $31,000<strong>and</strong> $52,160 <strong>and</strong> over $52,160 in 1992dollars) were combined because only17 percent of single-parent householdshad a be<strong>for</strong>e-tax income of $31,000<strong>and</strong> over. The sample was weighted toreflect the U.S. population of interest.Children’s clothing <strong>and</strong> child care <strong>and</strong>education expenditures were dividedbetween the two children in the oneparenthousehold. For food <strong>and</strong> healthcare, household member shares were calculated<strong>for</strong> a three-member household(single parent <strong>and</strong> two children, with theyounger child in one of the six age categories).The USDA food plans <strong>and</strong> the1987 National Medical Expenditure Surveyfindings were used to do this. Theseshares <strong>for</strong> the younger child in a singleparentfam<strong>ily</strong> were then applied to estimatedfood <strong>and</strong> health care expendituresto determine expenses on the youngerchild in each age category.Housing, transportation, <strong>and</strong> miscellaneousexpenditures were allocated amonghousehold members on a per capitabasis. Transportation expenses wereadjusted to account <strong>for</strong> nonemploymentrelatedactivities in single-parent families.Income <strong>and</strong> expenses were updated to1999 dollars.Child-rearing expense estimates <strong>for</strong>single-parent families are in table 8,p. 74. For the lower income group (1999be<strong>for</strong>e-tax income less than $36,800), acomparison of estimated expenditureson the younger child in a single-parentfam<strong>ily</strong> with two children with those ofthe younger child in a husb<strong>and</strong>-wifefam<strong>ily</strong> with two children is presented intable 1. As discussed earlier, 83 percentof single-parent families <strong>and</strong> 33 percentof husb<strong>and</strong>-wife families were in thislower income group. More single-parentthan husb<strong>and</strong>-wife families were in thebottom range of this lower income group.Average income <strong>for</strong> single-parent familiesin the lower income group is $15,400;<strong>for</strong> husb<strong>and</strong>-wife families it is $23,000.However, total expenditures on a childthrough age 17 are, on average, only 5percent lower in single-parent householdsthan in two-parent households.Single-parent families in this lowerincome group, there<strong>for</strong>e, spend a largerproportion of their income on childrenthan do two-parent families. On average,housing expenses are higher; whereas,transportation, health care, child care <strong>and</strong>education, <strong>and</strong> miscellaneous expenditureson a child are lower in singleparentthan in husb<strong>and</strong>-wife households.Child-related food <strong>and</strong> clothing expendituresare similar, on average, in single<strong>and</strong>two-parent families.For the higher income group of singleparentfamilies (1999 be<strong>for</strong>e-tax incomeof $36,800 <strong>and</strong> over), child-rearingexpense estimates are about the sameas those <strong>for</strong> two-parent households inthe be<strong>for</strong>e-tax income group of $61,900<strong>and</strong> over. Total expenses, in 1999 dollars,<strong>for</strong> the younger child through age 17are $234,780 <strong>for</strong> single-parent familiesversus $233,850 <strong>for</strong> husb<strong>and</strong>-wifefamilies. Child-rearing expenses <strong>for</strong>the higher income group of single-parentfamilies, there<strong>for</strong>e, also are a largerproportion of income than they are inhusb<strong>and</strong>-wife families. Thus, expenditureson children do not differ muchbetween single-parent <strong>and</strong> husb<strong>and</strong>-wifehouseholds. What differs is householdincome levels. Because single-parentfamilies have one less potential earnerthan do husb<strong>and</strong>-wife families, on average,their total household income is lower,1999 Vol. 12 Nos. 3&4 65
Table 1. A comparison of estimated 1999 expenditures on a child bylower income single-parent <strong>and</strong> husb<strong>and</strong>-wife families 1Age of child<strong>and</strong> child-rearing expenses are a greaterpercentage of this income.Estimates cover only out-of-pocketchild-rearing expenditures made by theparent with primary care of the child<strong>and</strong> do not include child-related expendituresmade by the parent without primarycare or made by others, such as gr<strong>and</strong>parents.Such expenditures could not beestimated from the data. Overall expensesby both parents on a child in a singleparenthousehold are likely greater thanthis study’s estimates.The procedure detailed earlier wasrepeated to determine the extent of thedifference in expenditures on an olderchild in single-parent households. Thefocus was on the older child, <strong>and</strong> afam<strong>ily</strong> with two children was used asthe st<strong>and</strong>ard. On average, single-parenthouseholds with two children spend7 percent less on the older than on theyounger child (in addition to age-relateddifferences). This contrasts with husb<strong>and</strong>wifehouseholds whose expenditures areunaffected by birth order.Single-parenthouseholdsAs with husb<strong>and</strong>-wife households,single-parent households spend moreor less if there is only one child or threeor more children. Multivariate analysiswas used to estimate expenditures <strong>for</strong>each budgetary component to determinethese differences. Household size <strong>and</strong>age of the younger child were controlvariables. Expenditures were thenassigned to a child by using the methoddescribed earlier. Compared with expenditures<strong>for</strong> the younger child in a singleparent,two-child fam<strong>ily</strong>, expenditures<strong>for</strong> an only child in a single-parenthousehold average 35 percent more,<strong>and</strong> those with three or more childrenaverage 28 percent less on each child.Other Expenditureson ChildrenHusb<strong>and</strong>-wifehouseholds0 - 2 $5,090 $6,0803 - 5 5,770 6,2106 - 8 6,480 6,3109 - 11 6,070 6,33012 - 14 6,540 7,15015 - 17 7,240 7,050Total (0 - 17) $111,570 $117,3901 Estimates are <strong>for</strong> the younger child in two-child families in the overall United States with 1999 be<strong>for</strong>etaxincome less than $36,800.Expenditures on a child that were estimatedin this study are composed ofdirect parental expenses made on a childthrough age 17 <strong>for</strong> seven major budgetarycomponents. These direct expendituresexclude costs related to childbirth<strong>and</strong> prenatal health care. In 1996 theseparticular health care costs averaged$7,090 <strong>for</strong> a normal delivery <strong>and</strong> $11,450<strong>for</strong> a Cesarean delivery (7). These costsmay be reduced by health insurance.One of the largest expenses made onchildren after age 17 is the cost of acollege education. The College Board(2) estimates that in 1999-2000, averageannual tuition <strong>and</strong> fees are $3,274 at4-year public colleges <strong>and</strong> $12,894 at4-year private colleges. Annual room<strong>and</strong> board is $4,533 at 4-year publiccolleges <strong>and</strong> $5,224 at 4-year privatecolleges. For 2-year colleges in 1999-2000, average annual tuition <strong>and</strong> feesare $1,608 at public colleges <strong>and</strong> $7,744at private colleges. Annual room <strong>and</strong>board is $4,474 at 2-year private colleges.No estimates of room <strong>and</strong> board aregiven <strong>for</strong> 2-year public colleges. Otherparental expenses on children after age17 include those associated with childrenliving at home or, if children do not liveat home, gifts <strong>and</strong> other contributions tothem.The estimates do not include all governmentexpenditures on children. Examplesof excluded expenses are public education,Medicaid, <strong>and</strong> school meals. Theactual expenditures on children (byparents <strong>and</strong> the government) would behigher than reported in this study, especially<strong>for</strong> the lowest income group.Indirect child-rearing costs are also notincluded in the estimates. Althoughthese costs are typically more difficultto measure than are direct expenditures,they can be substantial. The time involvedin rearing children is considerable. Inaddition, one or both parents may needto cut back on hours spent in the labor<strong>for</strong>ce to care <strong>for</strong> children, thus reducingcurrent earnings <strong>and</strong> future careeropportunities. The indirect costs of childrearing may exceed the direct costs. Formore on these indirect costs, see Bryantet al. (1), Irel<strong>and</strong> <strong>and</strong> Ward (3), Longman(6), <strong>and</strong> Spalter-Roth <strong>and</strong> Hartmann (8).66 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
References1. Bryant, W.K., Zick, C.D., <strong>and</strong> Kim, H. 1992. The Dollar Value of HouseholdWork. College of Human <strong>Eco</strong>logy, Cornell University, Ithaca, NY.2. The College Board. 1999. Trends in College Pricing 1999. [On-line]. Available:www.collegeboard.org.3. Irel<strong>and</strong>, T.R. <strong>and</strong> Ward, J.O. 1995. Valuing Children in Litigation: <strong>Fam</strong><strong>ily</strong> <strong>and</strong>Individual Loss Assessment. Lawyers <strong>and</strong> Judges Publishing Company, Inc., Tucson, AZ.4. Lefkowitz, D. <strong>and</strong> Monheit, A. 1991. Health Insurance, Use of Health Services,<strong>and</strong> Health Care Expenditures. National Medical Expenditure Survey ResearchFindings 12. U.S. Department of Health <strong>and</strong> Human Services, Public Health Service,Agency <strong>for</strong> Health Care <strong>Policy</strong> <strong>and</strong> Research Publication No. 92-0017.5. Lino, M. <strong>and</strong> Johnson, D.S. 1995. Housing, transportation, <strong>and</strong> miscellaneousexpenditures on children: A comparison of methodologies. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> Review8(1):2-12.6. Longman, P.J. 1998 (March 30). The Cost of Children. U.S. News & World Report124(12):50-58.7. Mushinski, M. 1998. Average charges <strong>for</strong> uncomplicated vaginal, Cesarean <strong>and</strong>VBAC deliveries: Regional variations, United States, 1996. Statistical Bulletin79(3):17-28.8. Spalter-Roth, R.M. <strong>and</strong> Hartmann, H.I. 1990. Unnecessary Losses: Costs toAmericans of the Lack of <strong>Fam</strong><strong>ily</strong> <strong>and</strong> Medical Leave. Institute <strong>for</strong> Women’s <strong>Policy</strong>Research, Washington, DC.9. U.S. Department of Agriculture, Agricultural Research Service. 1994. Cost offood at home. <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> Review 7(4):45.10. U.S. Department of Commerce, Bureau of the Census. 1999. Statistical Abstractof the United States, 1999. [119th ed.]11. U.S. Department of Health <strong>and</strong> Human Services, Office of the Assistant Secretary<strong>for</strong> Planning <strong>and</strong> Evaluation. 1990. Estimates of Expenditures on Children <strong>and</strong>Child Support Guidelines.12. U.S. Department of Transportation, Federal Highway Administration. 1994.1990 Nationwide Personal Transportation Study.1999 Vol. 12 Nos. 3&4 67
Research BriefsThe following are reprinted <strong>Nutrition</strong>Insights, a publication of the <strong>Center</strong><strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>.Insight 2April 1997Are All Food PyramidsCreated Equal?Alyson Escobar<strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>Public Confusion OverHealthy EatingIn a consumer survey, three of fourAmericans said there is too much conflictingin<strong>for</strong>mation about diet (Howare Americans Making Food Choices?ADA/IFIC, 1994).Contributing to this confusion are severaldietary pyramids that have begun tocompete <strong>for</strong> the public’s attention: TheUSDA Food Guide Pyramid (see graphicbelow), the Mediterranean Pyramid, theAsian Pyramid, <strong>and</strong> the Latin AmericanPyramid, among others. What do thesepyramids, all with seemingly differentmessages, mean <strong>for</strong> the Americanconsumer? So the question is, Are allfood pyramids created equal?USDA Pyramid is Well KnownSixty percent of Americans are familiarwith the USDA Food Guide Pyramid.The USDA Food Guide Pyramid <strong>and</strong>the Dietary Guidelines <strong>for</strong> Americansare key components of USDA’s food<strong>and</strong> nutrition guidance system.The 1995 Dietary Guidelines <strong>for</strong> Americansprovide nutrition guidance <strong>for</strong> healthyAmericans 2 years of age <strong>and</strong> older. TheFood Guide Pyramid helps consumersimplement the Guidelines by suggestingtypes <strong>and</strong> amounts of foods <strong>for</strong> peopleof different ages <strong>and</strong> sexes.USDA Food Guide Pyramid1999 Vol. 12 Nos. 3&4 75
<strong>Nutrition</strong> InsightsMediterranean Diet Pyramid1.What are the Mediterranean, Asian,<strong>and</strong> Latin American Diet Pyramids?The Mediterranean, Asian, <strong>and</strong> LatinAmerican Diet Pyramids were producedby Oldways Preservation <strong>and</strong> ExchangeTrust of Cambridge, Massachusetts.Oldways, a nonprofit company, developedthese diet pyramids to illustratetraditional diets of cultures that epidemiologicalstudies have associated withgood health.2. What, if anything, do the USDAFood Guide Pyramid <strong>and</strong> the OldwaysDiet Pyramids have in common?USDA’s Food Guide Pyramid <strong>and</strong> theOldways Diet Pyramids have much incommon. All illustrate eating patternsconsistent with current nutritional recommendations,<strong>and</strong> each can be used toplan diets consisting of different fooditems. Common emphases of all threePyramids include eating plenty of grainproducts <strong>and</strong> vegetables <strong>and</strong> fruits.Physical activity, moderation in consumptionof alcoholic beverages, <strong>and</strong>enjoyment of meals are healthy lifestylefactors emphasized by the OldwaysPyramids <strong>and</strong> the Dietary Guidelines<strong>for</strong> Americans.©Copyright 1994 Oldways Preservation & Exchange Trust.Asian Diet PyramidUSDA’s Food Guide Pyramid is basedon American eating patterns. Flexibilityin food choices is an important objectiveof the USDA Food Guide. Thus, a personcan eas<strong>ily</strong> choose to eat ‘‘Mediterranean,’’‘‘Asian,’’ or ‘‘Latin American style’’within the framework of the USDAFood Pyramid.In fact, several other pyramids have beendeveloped. The Puerto Rican Pyramid,the Vegetarian Pyramid, <strong>and</strong> the ‘‘SoulFood’’ Pyramid all use the USDA FoodGuide Pyramid framework but emphasize©1995 Oldways Preservation & Exchange Trust.76 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
a more selective range of foods. Thesepyramids, used in conjunction with theguidance offered by USDA, can helpthe public choose foods that fit aspecific ethnic or cultural diet.3. How do the Oldways Diet Pyramidsdiffer from the USDA Food GuidePyramid?The Oldways Diet Pyramids weredesigned to illustrate proportions ratherthan specific types <strong>and</strong> amounts of food.Detailed in<strong>for</strong>mation on serving sizes<strong>and</strong> numbers of servings of foods arenot provided. In addition, levels of totalfat <strong>and</strong> saturated fat are not specified.Since they represent cultural eatingpatterns, the Oldways Pyramids includea more limited range of foods than theUSDA Food Guide Pyramid. A majordifference between the Mediterranean<strong>and</strong> Asian Diet Pyramids <strong>and</strong> the USDAFood Guide Pyramid is their distinctionbetween plant <strong>and</strong> animal proteins. TheOldways Pyramids group plant-basedproteins----legumes, soybeans, nuts, <strong>and</strong>seeds----separately from animal proteinsfound in meat, poultry, eggs, <strong>and</strong> dairyproducts.Red meat is included only occasionallyin both the Mediterranean <strong>and</strong> AsianPyramids (a few times a month or less),while poultry <strong>and</strong> eggs appear slightlymore often. The Asian Diet Pyramidcontains limited dairy products, consideringthem ‘‘optional’’ <strong>and</strong> to be eatenin their lowfat <strong>for</strong>ms only. Another importantdistinction among the Pyramidsconcerns fat. Fat in the Oldways Pyramidscomes largely from vegetable oils highin monounsaturated fats, such as oliveoil in the Mediterranean Pyramid <strong>and</strong>peanut oil in the Asian.4. How can consumers use the USDA<strong>and</strong> Oldways Pyramids to makehealthy food choices?Neither USDA’s Food Guide Pyramidnor the Oldways Pyramids can conveyall that consumers need to know tomake food choices <strong>for</strong> a healthy diet.USDA’s Food Guide Pyramid is accompaniedby additional in<strong>for</strong>mation, suchas the number of servings from eachfood group appropriate <strong>for</strong> people ofdifferent age, sex, <strong>and</strong> calorie needs.To help consumers become healthier,USDA is participating in The DietaryGuidelines Alliance, a public-privatepartnership of health organizations, foodindustry associations, <strong>and</strong> the FederalGovernment. The mission is to motivateconsumers to change their eating <strong>and</strong>activity patterns by providing them withpositive, simple messages based onDietary Guidelines principles.In 1996, the Alliance kicked off its‘‘It’s All About You’’ campaign to helpconsumers integrate Dietary Guidelinesprinciples into their day-to-day lives.For more in<strong>for</strong>mation, contact the InternationalFood In<strong>for</strong>mation Council,1100 Connecticut Avenue, NW, Suite 430,Washington, DC 20036, <strong>and</strong> ask <strong>for</strong>Reaching Consumers with MeaningfulHealth Messages: A H<strong>and</strong>book <strong>for</strong><strong>Nutrition</strong> <strong>and</strong> Food Communicators.The H<strong>and</strong>book will be available onthe IFIC Web site in May athttp://ificinfo.health.org.The USDA Food Guide Pyramid (HG-252) is available on the CNPP Web siteat http://www.usda.gov/fcs/cnpp.htm<strong>and</strong> is also available in bulk quantitiesfrom the Government Printing Office(202) 512-1800.1999 Vol. 12 Nos. 3&4 77
Insight 9October 1998Report Card on theDiet Quality of ChildrenMark LinoShirley A. GerriorP. Peter BasiotisRajen S. An<strong>and</strong><strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>The diet quality of children <strong>and</strong> adolescentsstead<strong>ily</strong> declines as they get older.This decline in diet quality is a concern----poor eating patterns established inchildhood usually transfer to adulthood.Such patterns, as well as inactivityamong American children, are majorfactors in the increasing rate of obesityover the past decades. This <strong>Nutrition</strong>Insight uses the Healthy Eating Index(HEI) to examine the diet of Americanchildren ages 2 to 18 to identify thecomponents of their diet that contributeto this deterioration. Data used <strong>for</strong>analysis are from the U.S. Departmentof Agriculture’s (USDA) 1994-96Continuing Survey of Food Intakes byIndividuals, a nationally representativesurvey containing in<strong>for</strong>mation on thediets of about 5,000 children.Healthy Eating Index:How It Is ComputedThe HEI, computed on a regular basis byUSDA, is a summary measure of people’sdiet quality. The HEI provides an overallpicture of the type <strong>and</strong> quantity offoods people eat, their compliance withspecific dietary recommendations, <strong>and</strong>the variety in their diets. The Indexconsists of 10 components, each representingdifferent aspects of a healthfuldiet.Components 1-5 measure the degreeto which a person’s diet con<strong>for</strong>ms toUSDA’s Food Guide Pyramid servingrecommendations <strong>for</strong> the five majorfood groups: Grains (bread, cereal, rice,<strong>and</strong> pasta), vegetables, fruits, milk(milk, yogurt, <strong>and</strong> cheese), <strong>and</strong> meat(meat, poultry, fish, dry beans, eggs,<strong>and</strong> nuts). Component 6 measures totalfat consumption as a percentage of totalfood energy (calorie) intake. Component7 measures saturated fat consumptionas a percentage of total food energyintake. Components 8 <strong>and</strong> 9 measuretotal cholesterol intake <strong>and</strong> total sodiumintake, respectively. And component10 measures the degree of variety in aperson’s diet.Each component of the Index has amaximum score of 10 <strong>and</strong> a minimumscore of zero. Intermediate scores arecomputed proportionately. High componentscores indicate intakes close torecommended ranges or amounts; lowcomponent scores indicate less compliancewith recommended ranges oramounts. The maximum combinedscore <strong>for</strong> the 10 components is 100. AnHEI score above 80 implies a good diet;an HEI score between 51 <strong>and</strong> 80 impliesa diet that needs improvement; an HEIscore less than 51 implies a poor diet.Healthy Eating Index: Overall<strong>and</strong> Component ScoresMost children have a diet that needsimprovement or is poor (figure). Aschildren get older, their overall HEIscore declines (table). Consequently,78 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Healthy Eating Index rating by children’s age group, 1994-96Healthy Eating Index: Overall <strong>and</strong> component mean scores <strong>for</strong> children, 1994-96 (percent of children meetingthe dietary recommendations <strong>for</strong> each component in parentheses)Children 2-3 Children 4-6 Children 7-10 Females 11-14 Males 11-14 Females 15-18 Males 15-18Overall HEI score 73.8 67.8 66.6 63.5 62.2 60.9 60.71. Grains 8.3(54)2. Vegetables 5.9(31)3. Fruits 7.0(53)4. Milk 7.2(44)5. Meat 6.3(28)6. Total fat 7.4(40)7. Saturated fat 5.4(27)8. Cholesterol 9.0(83)9. Sodium 8.8(64)10. Variety 8.4(64)7.2(27)4.9(16)5.3(29)7.4(44)5.3(14)7.3(38)5.6(28)8.9(83)8.1(53)7.9(53)7.6(31)5.1(20)4.3(18)7.6(49)5.5(17)7.2(35)5.7(28)8.7(80)6.8(34)8.1(54)6.7(16)5.5(24)3.9(14)5.2(15)5.7(15)7.2(37)5.8(31)8.5(78)7.1(39)7.8(51)7.2(29)5.4(23)3.5(9)6.2(27)6.5(28)6.8(33)5.7(32)7.6(69)5.2(21)8.1(58)6.3(17)5.8(26)3.1(12)4.2(12)5.8(21)7.1(38)6.6(42)8.4(77)6.9(37)6.7(37)7.5(34)6.3(35)2.8(11)6.1(28)6.9(36)6.8(34)6.0(35)6.7(58)3.7(15)7.8(51)1999 Vol. 12 Nos. 3&4 79
the percentage having a good dietdeclines, <strong>and</strong> the percentage having adiet that needs improvement or is poorincreases (figure). For children ages 2to 3, 35 percent have a good diet, <strong>and</strong>5 percent have a poor diet. For males15 to 18 years old, only 6 percent havea good diet, <strong>and</strong> 21 percent have a poordiet. Much of the decline in diet quality<strong>for</strong> children occurs between the agegroups 2 to 3 <strong>and</strong> 4 to 6. During thisperiod, the percentage of childrenhaving a good diet falls from 35 to 16percent, <strong>and</strong> the percentage having adiet that needs improvement rises from60 to 75 percent. There is also a noticeabledecline in diet quality between the7 to 10 <strong>and</strong> 11 to 14 age groups, withthe percentage of children having agood diet falling from 14 to 7 percent.The decline in children’s diet as they getolder is linked to declines in their fruit<strong>and</strong> milk component scores of the HEI.The average fruit score falls from 7.0<strong>for</strong> children ages 2 to 3 to 3.1 <strong>for</strong>females <strong>and</strong> 2.8 <strong>for</strong> males ages 15 to18. Only 11 to 12 percent of these olderchildren meet the dietary recommendation<strong>for</strong> fruit (table). The milk groupscore increases as children get older,until ages 7 to 10, where it peaks at 7.6.It then declines considerably. Femalesages 15 to 18 have a particularly lowmilk score----4.2. Only 12 percent ofthese girls meet the dietary recommendation<strong>for</strong> milk servings.Although children ages 2 to 3 have thebest total fat score, only 40 percent meetthe dietary recommendation. Males ages11 to 18 have the lowest fat score: 6.8,<strong>and</strong> about one-third meet the dietaryrecommendation. Children ages 2 to 3<strong>and</strong> 4 to 6 have the lowest scores <strong>for</strong>saturated fat at 5.4 <strong>and</strong> 5.6, respectively,with 27 to 28 percent meeting the dietaryrecommendation. Females ages 15 to 18have the best saturated fat score at 6.6.But, only 42 percent meet the dietaryrecommendation.Cholesterol <strong>and</strong> sodium scores are relativelygood <strong>for</strong> preschoolers, with mostof these children meeting the dietaryrecommendations. The cholesterol scoredeclines stead<strong>ily</strong> as children get older.It falls from 9.0 <strong>for</strong> children ages 2 to 3to 6.7 <strong>for</strong> males ages 15 to 18. Femalesages 11 to 18 have higher cholesterolscores than do their male counterparts.The cholesterol component is the onlyHEI component <strong>for</strong> which the majorityof children in all age groups meet thedietary recommendation of 300 milligramsor less of dietary cholesterol each day.However, males ages 15 to 18 need towork harder to meet this goal becauseonly 58 percent meet this guidance. Thesodium score also declines as childrenget older. The sodium score averages8.8 <strong>for</strong> children ages 2 to 3 <strong>and</strong> declinesto 6.9 <strong>for</strong> females <strong>and</strong> 3.7 <strong>for</strong> malesages 15 to 18. Only 15 percent of malesages 15 to 18 meet the recommendationof 2,400 milligrams or less of sodiumeach day.ConclusionThe diet of most children needs substantialimprovement in order to meet thedietary recommendations with respectto fruits, vegetables, <strong>and</strong> milk products.Both teenage girls <strong>and</strong> boys are particularlydeficient in their consumption offruits <strong>and</strong> milk. Twelve percent or lessof adolescents ages 15 to 18 meet thedietary recommendation <strong>for</strong> fruits. Only12 percent of girls ages 15 to 18 meetthe dietary recommendation <strong>for</strong> milk.And males ages 11 to 18 need to decreasetheir sodium intake.This <strong>Nutrition</strong> Insight provides a betterunderst<strong>and</strong>ing of the types of dietarychanges needed to improve children’seating patterns. <strong>Nutrition</strong> professionalsmay use these results to tailor theirnutrition education programs aimed atimproving children’s dietary habits.Note: For additional results <strong>and</strong> moredetails on the Healthy Eating Index <strong>and</strong>how it is computed, the reader shouldsee Bowman, S.A., Lino, M., Gerrior,S.A., <strong>and</strong> Basiotis, P.P. 1998. TheHealthy Eating Index: 1994-96. U.S.Department of Agriculture, <strong>Center</strong><strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>.CNPP-5. Available athttp://www.usda.gov/cnpp.80 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Insight 15December 1999Eating Breakfast GreatlyImproves Schoolchildren’sDiet QualityP. Peter BasiotisMark LinoRajen S. An<strong>and</strong><strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong><strong>and</strong> <strong>Promotion</strong>We reported in a previous <strong>Nutrition</strong>Insights that the quality of most Americanchildren’s diet needs improvement.According to 1994-96 survey data, 88percent of children ages 6 to 18 have adiet that is poor or needs improvement;only 12 percent have a good diet. Whilenumerous studies have examined thecontribution of breakfast in improvingbehavior <strong>and</strong> learning at school, thecontribution of eating breakfast, particularlythrough the School BreakfastProgram (SBP), to overall diet qualityhas received less attention. The SBPoffers a nutritious breakfast to all childrenwho attend schools participating in theprogram. This <strong>Nutrition</strong> Insights examinesthe association of children eating breakfastwith the overall quality of their diet.Data from the 1994-96 ContinuingSurvey of Food Intakes by Individuals(CSFII) were analyzed. The CSFII is anationally representative survey containingin<strong>for</strong>mation on people’s consumptionof foods <strong>and</strong> nutrients. The quality ofchildren’s diet was assessed by usingthe Healthy Eating Index (HEI).Children between the ages of 6 <strong>and</strong> 18(school-age children) in low- <strong>and</strong> higherincome households were examinedseparately because diet quality variesby household income level. Householdswith an income below 185 percent ofthe poverty threshold were defined aslow income because this is the incomecut-off <strong>for</strong> children in these householdsbeing eligible <strong>for</strong> a free or reduced-priceschool breakfast or lunch. Data collectedduring a weekend, the summer, orDecember were omitted in order toexamine the effects of the SBP; the datathus represented a typical school day.The sample size used in this analysiswas 1,295 children. Data were weightedto represent the population.The Healthy Eating IndexThe HEI, computed on a regular basisby the U.S. Department of Agriculture(USDA), is a summary measure of theoverall quality of people’s diet. TheIndex is based on 10 components. Fivecomponents measure the degree towhich a person’s diet con<strong>for</strong>ms to theUSDA’s Food Guide Pyramid servingrecommendations <strong>for</strong> the major foodgroups: Grains (bread, cereal, rice, <strong>and</strong>pasta), vegetables, fruits, milk (milk,yogurt, <strong>and</strong> cheese), <strong>and</strong> meat (meat,poultry, fish, dry beans, eggs, <strong>and</strong> nuts).Four components measure the compliancewith dietary recommendations <strong>for</strong>total fat, saturated fat, cholesterol, <strong>and</strong>sodium intake. The final componentevaluates the extent of variety in the diet.Each component of the Index has amaximum score of 10 <strong>and</strong> a minimumscore of zero. The maximum overallscore <strong>for</strong> the 10 components combined1999 Vol. 12 Nos. 3&4 81
is 100. High component scores indicateintakes close to recommended rangesor amounts; low component scores indicateless compliance with recommendedranges or amounts. An HEI score above80 implies a good diet, an HEI scorebetween 51 <strong>and</strong> 80 implies a diet thatneed improvement, <strong>and</strong> an HEI scoreless than 51 implies a poor diet.Children’s Consumption ofBreakfastOverall, 67 percent of children in lowincomehouseholds ate breakfast at homeor some place other than school, such asa restaurant/fast-food establishment,19 percent ate breakfast at school, <strong>and</strong>14 percent did not eat breakfast (fig. 1).For children in higher income households,82 percent ate breakfast at home or someplace other than school, 16 percent didnot eat breakfast, <strong>and</strong> 2 percent atebreakfast at school (fig. 2).Effects of BreakfastConsumption on the HEIChildren in both low- <strong>and</strong> higher incomehouseholds who consume breakfast hada higher overall HEI score than childrenwho do not consume breakfast. (HEIscores were not calculated <strong>for</strong> childrenin higher income households who atebreakfast at school because of the smallsample size.) Among children in lowincomehouseholds, those who ate aschool breakfast had a statisticallysignificant higher HEI score (67) thanchildren who ate breakfast at home orelsewhere (63) <strong>and</strong> children who didnot eat breakfast (57) (see table). Allgroups of children, however, had anaverage HEI score that indicates theirdiet needs improvement.For the HEI components, regardless ofincome level, children who ate breakfasthad significantly better component scores<strong>for</strong> grains, fruits, milk products, <strong>and</strong>variety than children who did not eatbreakfast. The differences are particularlynoticeable <strong>for</strong> children in lowincomehouseholds who ate a schoolbreakfast. Among children in low-incomehouseholds, those who ate a schoolbreakfast had an average fruit score of5.4, compared with 2.1 <strong>for</strong> those whodid not eat breakfast. Likewise, amongchildren in low-income households,those who ate a school breakfast hadan average milk score of 8.8, comparedwith 4.4 <strong>for</strong> children who did not eatbreakfast. Milk is a required food in theSBP, <strong>and</strong> fruit juice is one of the mostfrequently served foods in the SBP.The average variety score <strong>for</strong> lowincomechildren who ate a schoolbreakfast was 9.0, compared with6.2 <strong>for</strong> low-income children whodid not eat breakfast.Children in low-income householdswho ate a school breakfast had asignificantly lower HEI componentscore----meaning less compliance withthe recommendation----<strong>for</strong> saturated fat(3.7) than children who ate breakfastelsewhere (5.4). The reasons <strong>for</strong> this areunclear <strong>and</strong> may not be directly attributableto the SBP. However, some schoolsparticipating in the SBP serve foodsrelatively high in saturated fat, such assausages <strong>and</strong> butter. Among childrenin higher income households, thosewho ate a breakfast had a better totalfat score than those who did not eatbreakfast.Do Results Hold AfterControlling <strong>for</strong> Other Factors?Figure 1. Breakfast consumption:Children in low-income householdsFigure 2. Breakfast consumption:Children in higher incomehouseholds82 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
HEI <strong>and</strong> component scores by breakfast consumption: Children in low<strong>and</strong>higher income householdsNobreakfastLow incomeEat breakfastNot at school At schoolHigher incomeNobreakfastEat breakfastNot at schoolOverall HEI 57 a 63 b 67 c 60 a 68 bGrains 5.9 a 7.3 b 7.1 b 6.4 a 7.6 bVegetables 5.9 5.7 5.9 6.1 5.5Fruits 2.1 a 3.7 b 5.4 c 2.6 a 4.6 bMilk 4.4 a 6.5 b 8.8 c 4.7 a 7.2 bMeat 6.2 6.4 6.9 6.1 5.5Total fat 6.3 6.6 6.0 6.4 a 7.5 bSaturated fat 5.0 5.4a 3.7 b 5.4 6.2Cholesterol 8.5 a 7.3 b 7.9 8.3 8.9Sodium 6.7 6.1 6.3 6.8 6.2Variety 6.2 a 8.1 b 9.0 c 6.8 a 8.5 bNote: Means with different superscripts are significantly different at .05.It could be that other factors besidesconsuming breakfast, particularly abreakfast at school, are affecting thediets of children. These other factorsinclude household characterist<strong>ics</strong>(income, size, region/urbanization,<strong>and</strong> food stamp participation) <strong>and</strong>child characterist<strong>ics</strong> (age, gender, race,ethnic origin, vitamin/mineral use,health status, <strong>and</strong> being on a specialdiet). Multivariate analysis is a statisticalmethod that takes into account theeffects of these other factors. Suchanalysis confirmed the descriptiveresults of this study. Among childrenin both low- <strong>and</strong> higher income households,those who ate breakfast had astatistically significantly better overalldiet, as measured by the HEI. Childrenwith higher grain, fruit, milk, <strong>and</strong>variety scores; eating a breakfast atschool was associated with even betterfruit, milk, <strong>and</strong> variety scores.Clearly, then, breakfast is a veryimportant contributor to the quality ofAmerican schoolchildren’s overall diet.Note: For more details on the HealthyEating Index <strong>and</strong> how it is computed,the reader should see Bowman, S.A.,Lino, M., Gerrior, S.A., Basiotis, P.P.1998. The Healthy Eating Index: 1994-96.U.S. Department of Agriculture, <strong>Center</strong><strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>.CNPP-5. This report is available athttp://www.usda.gov/cnpp.who ate a school breakfast had an evenbetter overall diet. For all children,consuming breakfast was associated1999 Vol. 12 Nos. 3&4 83
84 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Research SummariesContribution ofAway-From-HomeFoods to AmericanDiet QualityEating out has become increasinglypopular <strong>for</strong> Americans. In 1970, 26 percentof total food expenditure was spentaway from home; by 1996, that sharewas 39 percent. Reasons <strong>for</strong> this trendinclude the growing number of womenworking outside the home, more twoearnerhouseholds, higher incomes,smaller households, <strong>and</strong> more af<strong>for</strong>dable<strong>and</strong> convenient fast-food outlets.This study analyzes food intake surveydata collected by the U.S. Departmentof Agriculture (USDA) over the pasttwo decades to compare the nutritionalquality of home <strong>and</strong> away-from-homefoods. 1 Also, it examines how the qualityhas changed over time. This historicalcomparison shows how dining out influencesspecific dietary components:excessive intakes of total fat, saturatedfat, cholesterol, <strong>and</strong> sodium <strong>and</strong> lowintakes of fiber, calcium, <strong>and</strong> iron.The Data: 1977-95Individual food intakes were collectedin two decennial surveys conducted byUSDA----the Nationwide Food ConsumptionSurveys (NFCS) of 1977-78<strong>and</strong> 1987-88. In 1985 USDA started theContinuing Survey of Food Intakes byIndividuals (CSFII) <strong>for</strong> relatively smallnational samples. During 1989-91 three1 Home <strong>and</strong> away-from-home foods are definedbased on where foods are obtained, not where theyare eaten. Home food is purchased at a retail store<strong>and</strong> food away from home is purchased mainlyfrom foodservice establishments. Both food athome <strong>and</strong> food away from home can be eaten athome or away from home.separate 1-year surveys collected in<strong>for</strong>mationon individual food intakes fromnationally representative samples. Again,in 1994-96, three separate 1-year CSFIIsurveys were conducted.Data <strong>for</strong> this study were from sevenyear-round, nationwide surveys of individualfood intakes: NFCS 1977-78,NFCS 1987-88, CSFII 1989, CSFII1990, CSFII 1991, CSFII 1994, <strong>and</strong>CSFII 1995. The CSFII 1985-86 datawere excluded because they did notrepresent all Americans. The first fivesurveys collected dietary intakes <strong>for</strong>3 consecutive days----a 1-day recall <strong>and</strong>a 2-day record; the latter two surveysrecorded 2 nonconsecutive days of foodconsumption. For the most accuratecomparison of the seven surveys’ data,only the first day from each survey wasincluded in the analysis.Intake data <strong>for</strong> children under age 2,pregnant <strong>and</strong> lactating women, <strong>and</strong> individualswith incomplete dietary intakedata were excluded from this analysis.Sources of away-from-home food weregrouped into five categories: Fast-foodplaces; schools, camps, day-care centers;restaurants; other public eating places,including residential dining facilities,bars, soup kitchens, <strong>and</strong> meals on wheels;<strong>and</strong> other (a catch-all category, includingvending machines <strong>and</strong> someone’s home).Meals <strong>and</strong> snacks consisting of a combinationof home <strong>and</strong> away-from-homefoods were classified according to thehighest caloric component.Meal <strong>and</strong> Snack EatingPatternsThe number of meals consumed byAmericans has remained stable over thepast two decades at 2.6 or 2.7. Snacking,however, increased from less than oncea day in 1987-88 to 1.6 times a day in1999 Vol. 12 Nos. 3&4 85
Table 1. Meal <strong>and</strong> snack eating patterns of Americans, 1 1977-951977-78 1987-88 1989 1990 1991 1994 1995NumberMeals per day 2.7 2.6 2.6 2.6 2.6 2.7 2.6Snacks per day 1.1 0.9 1.2 1.2 1.4 1.5 1.6PercentMeals eaten away from home 2 16 24 24 23 27 28 29Snacks eaten away from home 2 17 20 20 18 18 21 22All meals <strong>and</strong> snacks eaten awayfrom home 2 16 23 23 22 24 26 27Restaurant 2 4 4 4 4 6 5Fast food 3 7 7 7 7 8 9School 3 3 2 2 2 3 2 2Other public 3 2 2 2 2 2 2Others 6 8 8 7 8 8 91 Ages 2 <strong>and</strong> older, excluding pregnant <strong>and</strong> lactating women <strong>and</strong> those who did not provide complete dietary intake data.2 Away from home presents the aggregate of fast foods, restaurants, schools, other public places, <strong>and</strong> others.3 Schools are classified as a separate category <strong>for</strong> children only; <strong>for</strong> adults, they are included in ‘‘others.’’Compiled by <strong>Eco</strong><strong>nom</strong>ic Research Service, USDA, from NFCS 1977-78, NFCS 1987-88, CSFII 1989-91, <strong>and</strong> CSFII 1994-95, first-day intake data.1995 (table 1). The percentage of mealseaten away from home increased from16 percent in 1977-78 to 29 percent in1995, <strong>and</strong> the percentage of snacksaway from home rose from 17 percentin 1977-78 to 22 percent in 1995.The increasing frequency of dining outmeans that Americans are getting moreof their nutrients from away-from-homesources (table 2). For example, awayfrom-homefoods provided 34 percentof total calories in 1995, up from 18percent in 1977-78. Away-from-homefoods also provided 38 percent of totalfat intake in 1995, more than double the18 percent provided in 1977-78. Thus,the nutritional quality of food away fromhome has become increasingly importantin determining the overall nutritionalquality of diets in the United States.<strong>Nutrition</strong>al Quality of Home<strong>and</strong> Away-From-Home FoodsThe nutritional quality of foods wascompared by using the nutrient-to-caloriedensity (nutrient density), which measuresthe amount of a nutrient or food component<strong>for</strong> each 1,000 calories of that food.For fat <strong>and</strong> saturated fat, the proportionof total calories that come from fat <strong>and</strong>saturated fat were used as measures ofdensity.A ‘‘benchmark’’ density was derived bydividing the recommendation 2 <strong>for</strong> a givennutrient or food component by an individual’sreported caloric intake in 1,0002 Dietary recommendations were from the DietaryGuidelines <strong>for</strong> Americans <strong>and</strong> other healthauthorities.calories. The benchmark density representsthe nutrient density an individual’sdiet would have to reach to meet thedietary recommendation <strong>for</strong> that caloriclevel. When the nutrient is consumed inamounts higher (lower) than the recommendedlevels, the benchmark density<strong>for</strong> that nutrient will be lower (higher)than the nutrient density. Benchmarkdensities vary from year to year becausecaloric intakes vary from year to year.For any nutrient, a higher caloric intakemeans less of that nutrient is needed per1,000 calories to meet the same recommendedintake level. There<strong>for</strong>e, anincrease in caloric intake means alower benchmark density.86 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 2. Consumption of selected nutrients <strong>and</strong> food components in away-from-home foods, 1 as part of totaldiet, 1977-951977-78 1987-88 1989 1990 1991 1994 1995PercentCalories 18 27 27 26 29 31 34Total fat 18 28 29 28 32 35 38Saturated fat NA 28 29 28 31 33 37Cholesterol NA 26 25 25 30 32 34Sodium NA 27 26 26 30 32 34Fiber NA 22 23 22 25 26 27Calcium 17 23 23 22 25 26 29Iron 16 22 22 21 25 26 27NA = Not available.1 Away from home presents the aggregate of fast foods, restaurants, schools, other public places, <strong>and</strong> others.Compiled by <strong>Eco</strong><strong>nom</strong>ic Research Service, USDA, from NFCS 1977-78, NFCS 1987-88, CSFII 1989-91, <strong>and</strong> CSFII 1994-95, first-day intake data.Caloric IntakeBecause of potential underreporting,caloric <strong>and</strong> nutrient intake estimatesfrom dietary recall surveys usuallyrepresent a lower limit of actual intakes.Also, the method of conducting dietaryrecall interviews has changed over theyears to improve the accuracy of reporting.Reported trends in caloric <strong>and</strong> nutrientintakes may reflect these changes <strong>and</strong>must be considered when interpretingresults.Average caloric intake declined from1,876 calories per person per day in1977-78 to 1,807 calories in 1987-88,then rose stead<strong>ily</strong> to 2,043 calories in 1995(table 3). The percentage of Americansage 2 <strong>and</strong> older who consumed the recommendedenergy allowance (REA) ormore rose from 22 percent in 1987-88to 31 percent in 1995. Even so, theproportion of adults in the United Stateswho were considered overweight in1988-94 was more than one in three(35 percent), an increase from one infour in 1976-80.Some of the observed increase in caloricintake may be due to increased eatingout. Away-from-home food was eatenat 16 percent of all meals <strong>and</strong> snacks in1977-78 <strong>and</strong> accounted <strong>for</strong> 18 percentof total caloric intake; in 1995, awayfrom-homefood accounted <strong>for</strong> 27 percentof all meals <strong>and</strong> snacks <strong>and</strong> 34 percentof total caloric intake. These numberssuggest that when eating away fromhome, people eat either larger quantitiesor higher calorie foods----or both----thanwhen eating at home.As the number of meals <strong>and</strong> snackseaten at fast-food places <strong>and</strong> restaurantshas increased over the past two decades,so has the percentage of total caloriesconsumed from these locations. Fastfoodplaces accounted <strong>for</strong> 3 percent oftotal caloric intake in 1977-78 but 12percent in 1995; restaurants’ share oftotal calories was 3 percent in 1977-78<strong>and</strong> 8 percent in 1995.Fat <strong>and</strong> Saturated FatThe benchmark densities <strong>for</strong> fat <strong>and</strong>saturated fat are no more than 30 <strong>and</strong>10 percent of total calories, respectively.Over the past two decades, Americanshave eaten less fatty foods. Fat providedan average of 33.6 percent of total caloriesin 1995, considerably less than the 41.1percent of 1977-78. Fat density declined<strong>for</strong> both home foods (from 41.1 percentin 1977-78 to 31.5 percent in 1995) <strong>and</strong>away-from-home foods (from 41.2percent to 37.6 percent).Restaurant foods had a considerablyhigher fat density (46.2 percent) thaneither fast foods (41.6 percent) or schoolfoods (40.1 percent) in 1977-78. Fatdensity of restaurant foods declined to40.1 percent in 1995, fast foods to 39.3percent, <strong>and</strong> school foods to 35.7 percent.The saturated fat density of Americ<strong>and</strong>iets was first measured in 1987-88.Home foods had a lower saturated fatdensity than away-from-home foods;this density declined in both types of1999 Vol. 12 Nos. 3&4 87
Table 3. Caloric intake <strong>and</strong> sources <strong>for</strong> Americans, 1 1977-951977-78 1987-88 1989 1990 1991 1994 1995CaloriesAverage caloric intake 1,876 1,807 1,837 1,853 1,883 2,006 2,043PercentPeople consuming more than REA 2 26 22 24 26 26 28 31Portion of total calories:At home 82 73 73 74 71 69 66Away from home 3 18 27 27 26 29 31 34Restaurants 3 5 7 6 6 8 8Fast foods 3 8 9 9 9 11 12Schools 3 3 3 2 2 3 2 2Other public 3 2 3 2 3 3 2Others 6 9 7 8 9 7 91 Ages 2 <strong>and</strong> older, excluding pregnant <strong>and</strong> lactating women <strong>and</strong> those who did not provide complete dietary intake data.2 REA = Recommended energy allowance (per day).3 Away from home presents the aggregate of fast foods, restaurants, schools, other public places, <strong>and</strong> others.4 Schools are classified as a separate category <strong>for</strong> children only; <strong>for</strong> adults, they are included in ‘‘others.’’Compiled by <strong>Eco</strong><strong>nom</strong>ic Research Service, USDA, from NFCS 1977-78, NFCS 1987-88, CSFII 1989-91, <strong>and</strong> CSFII 1994-95, first-day intake data.foods through 1994. Since 1989, saturatedfat density in school foods has beenhigher than in other away-from-homelocations----14.2 percent of calories in1995. The saturated fat density of homefoods in 1995 was 10.9 percent <strong>and</strong>that <strong>for</strong> all away-from-home foods,12.8 percent.CholesterolThe recommended da<strong>ily</strong> cholesterolintake used to set the Da<strong>ily</strong> Value <strong>for</strong>nutrition labeling is 300 milligrams (mg)or less. This recommended intake isfixed, regardless of caloric intake. In1987-88, when cholesterol content ofU.S. diets was first measured, averagecholesterol intake was 286 mg per personper day. In 1995, it was 268 mg. Thus,cholesterol levels have been safelybelow the benchmark level. Cholesteroldensities in both home (161 in 1987-88to 129 in 1995) <strong>and</strong> away-from-home(151 in 1987-88 to 134 in 1995) foodshave been markedly reduced during thepast decade. Compared with all othersources, restaurant food has been consistentlyhigher in cholesterol, with densitiesof 215 in 1978-88 <strong>and</strong> 176 in 1995.Males ages 12 to 39 (who tend to eatmore than others yet have identicalcholesterol recommendations) are thosemost likely to exceed the benchmarklevel of 300 mg per day.SodiumSodium intakes as defined in the NFCS<strong>and</strong> CSFII include sodium occurringnaturally in foods, as well as that addedduring food processing <strong>and</strong> food preparation.These intakes do not includesodium added at the table. The NationalAcademy of Sciences recommendsfewer than 2,400 mg of sodium per day,regardless of age <strong>and</strong> gender. As withcholesterol, those who consume morecalories have lower benchmarks than dothose consuming fewer calories.Average da<strong>ily</strong> sodium intake increasedfrom 3,023 mg in 1987-88 to 3,348 mgin 1995. The sodium densities of home<strong>and</strong> away-from-home foods are fairlysimilar----both substantially higher thanthe benchmark density. Restaurantfoods contain much more sodium thanother away-from-home foods, eventhough some decline has been observedsince 1991. Overconsumption of sodiumis a problem <strong>for</strong> most consumers except<strong>for</strong> young children <strong>and</strong> elderly womenwho tend to consume less calories thanothers.88 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
CalciumThe 1989 Recommended Da<strong>ily</strong> Allowances(RDA) <strong>for</strong> calcium, used in thisstudy, were 1,200 mg <strong>for</strong> those ages 11to 24 <strong>and</strong> 800 mg <strong>for</strong> all others. In 1997,the Institute of Medicine of the NationalAcademy of Sciences issued new dietaryrecommendations <strong>for</strong> several nutrients.The recommended calcium intakes <strong>for</strong>many Americans (children age 9 <strong>and</strong>older <strong>and</strong> adults age 25 <strong>and</strong> older) wereraised.A higher percentage of Americans metthe 1989 calcium RDA in 1995 than in1977-78. The calcium density of homefoods showed a general increase, whilethat of away-from-home foods declinedslightly. In 1995, the calcium density ofaway-from-home foods was 21 percentbelow the benchmark. School foods,however, had a calcium density 62 percenthigher than home foods, 95 percenthigher than fast foods, <strong>and</strong> 137 percenthigher than restaurant foods.Insufficient calcium intake is a moresevere problem <strong>for</strong> teenage girls <strong>and</strong>women because of their higher calciumrequirements <strong>and</strong> their lower foodconsumption. In 1995, only 18 percentof girls ages 12 to 17 met their calciumRDAs.Dietary FiberTwo separate benchmarks were used <strong>for</strong>dietary fiber: <strong>for</strong> those ages 2 to 20, ‘‘ageplus 5’’ (recommended by the AmericanHealth Foundation), <strong>and</strong> <strong>for</strong> those age 21<strong>and</strong> older, a Da<strong>ily</strong> Value of 11.5 gramsper 1,000 calories (recommended by theFDA). Average fiber intake increasedfrom 12.7 grams in 1978-88 to 15.2grams in 1995. Eighteen percent ofAmericans met fiber intake recommendationsin 1978-88; 24 percent met therecommendations in 1995. Over thepast decade, fiber densities of homefoods increased slightly----from 7.5 gramsper 1,000 calories in 1987-88 to 8.1 in1995. Fiber densities <strong>for</strong> away-fromhomefoods increased even less----from5.8 in 1987-88 to 6.1 in 1995. For children,school foods declined in fiber density,from 7.6 grams per 1,000 calories in1987-88 to 7.1 in 1995. Fiber densitiesof fast foods trended upward but remainedlow at 5.6 grams in 1995. The fiberdensity of restaurant foods increasedfrom 5.8 grams per 1,000 calories in1987-88 to 6.2 grams in 1995. Theincreased popularity of these eating placeswill make it difficult <strong>for</strong> Americans toachieve fiber intake recommendations.Dietary IronThe RDAs <strong>for</strong> iron are 12 mg <strong>for</strong> malesages 11 to 18, 15 mg <strong>for</strong> females 11 to50, <strong>and</strong> 10 mg <strong>for</strong> children 2 to 10.Because of the increased consumptionof iron-<strong>for</strong>tified breakfast cereals athome, iron density rose more rapidly<strong>for</strong> home foods than <strong>for</strong> away-fromhomefoods. However, iron densities ofboth home <strong>and</strong> away-from-home foods increased.Since 1987-88 children’s <strong>and</strong>adults’ average da<strong>ily</strong> consumption ofdietary iron exceeded the RDAs. Thepercentage of children <strong>and</strong> adults whomet their RDA <strong>for</strong> iron increased from42 percent in 1977-78 to 61 percent in1995. Iron densities of restaurant foods,school foods, <strong>and</strong> fast foods have shownan upward trend over the past twodecades.Low iron intake is common amongteenage girls <strong>and</strong> women----who havethe highest requirements <strong>and</strong> typicallylow food consumption. Only one inthree women ages 18 to 39 met theiriron RDAs in 1995.ConclusionAway-from-home foods generally containmore of the nutrients overconsumed<strong>and</strong> less of the nutrients underconsumedby Americans. The increased popularityof dining out may make it more difficultto improve the overall nutritional qualityof diets. Because this trend is expectedto continue, nutrition policy, educationalprograms, <strong>and</strong> promotion strategies couldaddress nutritional quality of food awayfrom home <strong>and</strong> consumers’ foodchoices when eating out.Food away from home does not have todiffer nutritionally from food preparedat home. Consumer dem<strong>and</strong> <strong>for</strong> suchfoods, however, must be strong enoughto create an eco<strong>nom</strong>ic incentive <strong>for</strong>increased marketing of nutritious itemsby restaurants <strong>and</strong> fast-food establishments.Consumers may have a differentattitude about food away from homethan food at home. They may consider itas an occasional treat that does not havethe same effect on the overall diet as foodat home. Consumers may not realize theextent to which eating out has becomea part of their usual diets. To the degreethat consumer attitudes are a barrier tochange, nutrition education <strong>and</strong> promotionstrategies may be able to in<strong>for</strong>mconsumers of the effect of away-fromhomefood on overall diet quality.Source: Lin, B-H., Frazao, E., <strong>and</strong> Guthrie, J.,1999, Away-From-Home Foods IncreasinglyImportant to Quality of American Diet, AgriculturalIn<strong>for</strong>mation Bulletin No. 749, U.S. Departmentof Agriculture <strong>and</strong> U.S. Department of Health<strong>and</strong> Human Services.1999 Vol. 12 Nos. 3&4 89
The Rural Poor’sAccess toSupermarkets <strong>and</strong>Large GroceryStoresA recent study by the U.S. Departmentof Agriculture’s (USDA) <strong>Eco</strong><strong>nom</strong>icResearch Service (ERS) found thatretail food prices varied with the typeof store <strong>and</strong> its location. Compared withmetro areas, rural areas support fewersupermarkets <strong>and</strong> a larger percentageof smaller grocery stores. Also, ruralhouseholds face supermarket pricesabout 4 percent higher than thoseavailable to suburban households.Nationwide, supermarket prices average10 percent lower than prices in othergrocery stores, such as ‘‘mom <strong>and</strong> pop’’stores or convenience stores. Supermarketscan take advantage of eco<strong>nom</strong>ies of scale(as sales increase, costs per unit decline)by having smaller markups----<strong>and</strong>, thus,lower prices. The larger physical sizeof supermarkets also allows <strong>for</strong> greaterproduct variety <strong>and</strong> more eco<strong>nom</strong>icalbr<strong>and</strong>s (store-label <strong>and</strong> generic) <strong>and</strong>package sizes.Although poor households spent 76.7percent of food stamps in supermarketsnationwide, rural supermarkets accounted<strong>for</strong> just 58.9 percent of all rural foodstamp redemptions. In low-incomerural areas, supermarkets accounted <strong>for</strong>only 52.8 percent of total redemptions.Because of price differences betweensupermarkets in rural <strong>and</strong> suburban areas,<strong>and</strong> the lower use of supermarkets inpoor rural areas, poor rural householdsface food prices that are 2.5 percenthigher, on average, than other ruralhouseholds face <strong>and</strong> that are 3.1 percenthigher than those suburban householdsface.ERS investigated access to food storesin 36 rural, high-poverty countiesbordering the Mississippi River. Priorstudies have focused on households inurban metro areas because they account<strong>for</strong> three-quarters of the total U.S. population.The selection of this particulararea----the Lower Mississippi Deltaregion----supports the work of the<strong>Nutrition</strong> Intervention ResearchLarge food retailer sales <strong>and</strong> food stamp redemptions, by store sales class,Lower Delta core countiesLow-income households spend more in smaller supermarkets <strong>and</strong> grocery stores than in larger supermarkets.1 Annual sales $6 million or more.2 Annual sales $2 million up to $6 milion.3 Annual sales $500,000 up to $2 million.Source: Food <strong>and</strong> <strong>Nutrition</strong> Service, U.S. Department of Agriculture.90 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 1. Net accessibility of all households to larger food retailers: Lower Delta core counties 1The net accessibility ratio exceeded 1.0 in 38 percent of ZIP Codes, representing 72.4 percent of the total population in theLower Delta region.Net accessibility ratio(R)ZIP CodesZIP CodehouseholdsZIP CodepopulationZIP Codehouseholds without carNumberLess than 0.5 0 0 0 00.5 - 0.749 22 9,567 28,319 1,5700.75 - 1.0 102 65,832 198,526 11,950More than 1.0 76 197,389 584,508 37,89236-county total 200 272,788 811,353 51,412Percent share 2Less than 0.5 0 0 0 00.5 - 0.749 11.0 3.5 3.5 16.40.75 - 1.0 51.0 24.1 24.5 18.1More than 1.0 38.0 72.4 72.0 19.21 Net accessibility ratio = (accessible food sales)/(accessible food expenditures).2 Percentages may not sum to 100 due to rounding.Source: <strong>Eco</strong><strong>nom</strong>ic Research Service, USDA.Initiative (NIRI), a consortium of sevenpartners, including USDA <strong>and</strong> six highereducation <strong>and</strong> research institutionslocated in the region. The aim of NIRIis to improve the health <strong>and</strong> well-beingof people in the Lower Delta region,<strong>and</strong> one of its objectives is to improveaccess to af<strong>for</strong>dable, quality food bylow-income households.The 36-county area where the studywas conducted contained 222 large foodretail outlets with gross sales in 1993of $909 million; food stamp redemptionin these stores totaled $113 million.Supermarkets with annual sales of $6million or more accounted <strong>for</strong> 54.3 percentof gross sales but only 42.4 percentof food stamp redemptions (figure).The availability of large food retailerscan be gauged by the average number ofsquare miles per store <strong>for</strong> a given area.For example, in the 36 counties, therewas one supermarket per 190.5 squaremiles; <strong>for</strong> all rural counties in Arkansas,Louisiana, <strong>and</strong> Mississippi, there wasone supermarket per 153.5 square miles.When large grocery stores are included,the average square miles per largeretailer in all rural counties improvedto 101.6.Household access to larger grocery storeswas determined, <strong>and</strong> the level of accessibleannual food dollars in the area wherethe study was conducted was separatedinto ZIP Code quartiles. ZIP Codes inthe quartile with the highest food salesaccounted <strong>for</strong> 57.2 percent of the populationin the area where the study wasconducted. The level of household foodexpenditures available to a retail foodlocation was also separated into ZIPCode quartiles. The highest quartileaccounted <strong>for</strong> 51.4 percent of the populationin the area included in the study.Net accessibility ratios were calculatedby dividing accessible food sales byaccessible food expenditures <strong>and</strong> thentabulated (table 1). Of the 200 ZIP Codesthat made up the core study area, 124had accessibility ratios less than 1.0----indicating that food expenditures werenot fully satisfied by accessible largeretailers.A separate analysis of low-incomehouseholds showed that they are lesslikely to travel a considerable distanceto reach large retail outlets, because lowincomehouseholders may not own or1999 Vol. 12 Nos. 3&4 91
Table 2. Net accessibility of low-income households to large food retailers: Lower Delta core counties 1The net accessibility ratio exceeded 1.0 in only 22.5 percent of Lower Delta ZIP Codes, representing less than one-third of thetotal low-income population.Net accessibility ratio(R)ZIP CodesZIP Codelow-incomehouseholds 2ZIP Codelow-incomepopulation 3ZIP Codehouseholdswithout carNumberLess than 0.5 9 7,209 21,626 na0.5 - 0.749 35 21,698 65,097 na0.75 - 1.0 111 49,137 245,051 naMore than 1.0 45 81,683 147,412 na36-county total 200 159,727 479,186 naPercent share 4Less than 0.5 4.5 4.5 4.5 na0.5 - 0.749 17.5 13.6 13.6 na0.75 - 1.0 55.5 51.1 51.1 naMore than 1.0 22.5 30.8 30.8 na1 Net accessibility ratio = (accessible food stamp redemptions)/(accessible food stamp issuances).2 Estimated.3 Based on 130 percent of poverty household income threshold.4 Percentages may not sum to 100 due to rounding.na = Not available.Source: <strong>Eco</strong><strong>nom</strong>ic Research Service, USDA.have access to transportation, or theymay not be able to af<strong>for</strong>d it. As a proxy<strong>for</strong> food purchases by low-incomehouseholds <strong>and</strong> sales by large retailers,aggregate ZIP Code-level data (obtainedfrom the Food <strong>and</strong> <strong>Nutrition</strong> Service ofthe U.S. Department of Agriculture)were used. These data include foodstamp redemptions by large retailers<strong>and</strong> food stamp issuances made tohouseholds from each ZIP Code inthe Lower Delta region.The ratio of accessible food stampredemptions to accessible food stampissuances was calculated <strong>for</strong> each ZIPCode in the same way as was the netaccessibilityratio <strong>for</strong> all households.Of the 200 ZIP Codes in the 36-countycore area, only 45 (22.5 percent) hadratios exceeding 1.0 (table 2). Comparedwith all households, low-income householdsappear to be located disproportionatelyin areas of net-accessibilityshortfalls. Within the 36 counties, arelatively large share of the total areahad insufficient net accessibility. Giventheir low-income status, households inthese areas were less likely to travel tolarge retailers beyond the 30-mile retailrange. Instead, they needed to rely moreon small grocery stores <strong>and</strong> conveniencestores that offer fewer selections <strong>and</strong>generally higher prices.Source: Kaufman, P.R., 1999, Rural poor haveless access to supermarkets, large grocery stores,Rural Development Perspectives 13(3):19-25.92 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Poverty <strong>and</strong>Well-Being inRural AmericaFour aspects of rural poverty <strong>and</strong> wellbeingare discussed <strong>and</strong> compared withurban America: The rural poverty rate,the socioeco<strong>nom</strong>ic well-being of ruralchildren, levels of food security in ruralhouseholds, <strong>and</strong> housing problems inrural America.Rural Poverty RateIn 1996 the poverty rate in rural Americawas 15.9 percent, essentially unchangedfrom 1995. The urban poverty rate in1996 was 13.2 percent. The rural povertyrate varied by only 1.6 percentagepoints in the last 8 years.Poverty rates, by race/ethnicity <strong>and</strong> residence, 1996Poverty rates are highest <strong>for</strong> rural minorities, nearly three times those of Whites <strong>and</strong>substantially higher than those of urban minorities.Percent40302010012.27.5Whitenon-Hispanic35.226.933.4 33.728.9 28.6Black Hispanic NativeAmericanNonmetroMetro15.913.2All race-ethnicgroupsSource: Calculated by ERS using data from the March 1997 Current Population Survey.Poverty rates among rural minoritieswere nearly three times as high as <strong>for</strong>rural Whites <strong>and</strong> substantially higherthan those of urban minorities (figure).The poverty rate was highest <strong>for</strong> ruralBlacks, followed by rural Native Americans<strong>and</strong> rural Hispan<strong>ics</strong>. Poverty rateswere higher <strong>for</strong> female-headed familiesthan <strong>for</strong> other household types, <strong>and</strong> ruralBlacks <strong>and</strong> Native Americans hadhigher percentages of householdsheaded by a female than did rural Whites.Rural minorities had, on average, lesseducation than rural Whites, <strong>and</strong> educationwas a strong predictor of income.Even <strong>for</strong> people with similar educationin households of the same type, povertyrates <strong>for</strong> rural minorities were abouttwice those of non-Hispanic Whites.Differences also may be caused bydiscrimination in employment <strong>and</strong>wages <strong>and</strong> concentrations of minoritiesin areas that are unable to attract highwageemployers.In 1996, 3.2 million rural children underthe age of 18 lived in families with incomebelow the poverty level. While the povertyrate <strong>for</strong> all rural children was 22.4 percent,the rates <strong>for</strong> rural Black children<strong>and</strong> <strong>for</strong> rural Hispanic children weretwice as high: 46.2 <strong>and</strong> 41.2 percent,respectively. Most rural poor children(61.9 percent) lived in single-parentfamilies, <strong>and</strong> the poverty rate <strong>for</strong> thesefamilies was 47.3 percent, comparedwith 12 percent <strong>for</strong> rural children intwo-parent families. More than half ofthe rural poor lived in families headedby single women (or were women livingalone).Almost two-thirds of rural poor peoplelived in families with at least one workingmember or, if they lived alone, werethemselves employed. Among ruralhouseholds with full-time workers, thepoverty rate was 5.0 percent.Rural poverty rates were highest in theSouth <strong>and</strong> West (18.7 <strong>and</strong> 18.4 percent,respectively); over half of the rural poor(51.6 percent) lived in the South. TheNortheast was the only region where thepoverty rate was higher <strong>for</strong> urban areasthan <strong>for</strong> rural areas.The Socioeco<strong>nom</strong>ic Well-Beingof Rural ChildrenThe Personal Responsibility <strong>and</strong> WorkOpportunity Reconciliation Act of 1996requires that the U.S. Bureau of the Censusprovide each State with a current annualestimate of the poverty rate <strong>for</strong> its childrenless than 6 years old. If the rate hasincreased by more than 5 percent overthe previous year’s rate <strong>and</strong> that increaseis attributable to the effects of welfarere<strong>for</strong>m, the State must submit a correctiveaction plan.1999 Vol. 12 Nos. 3&4 93
A comparison of urban <strong>and</strong> rural childrenshows marked differences in their socioeco<strong>nom</strong>icwell-being, region of residence,<strong>and</strong> racial/ethnic background. There was,however, considerable similarity in theirage, fam<strong>ily</strong> structure, parental education,<strong>and</strong> absence of a wage earner. Thepoverty rate <strong>for</strong> all urban <strong>and</strong> ruralchildren was highest in the South <strong>and</strong>West----about 25 percent in both regions<strong>for</strong> urban children <strong>and</strong> about 30 percentin both regions <strong>for</strong> rural children.Although rural children were less likelyto be minorities than were urban children(24 <strong>and</strong> 38 percent, respectively), povertyrates remain much higher <strong>for</strong> ruralminority children than <strong>for</strong> rural Whitechildren.Rural minority children tended to beconcentrated in two regions. About 89percent of rural Black children livedin the South, <strong>and</strong> 45 percent of NativeAmerican children lived in the West.Rural Hispanic children resided mostlyin two regions----the South (47 percent)<strong>and</strong> the West (44 percent). Over onehalfof rural Black children living inthe South were poor.The poverty rate <strong>for</strong> children in familieswith no earners was higher <strong>for</strong> urbanchildren (92 percent) than <strong>for</strong> ruralchildren (87 percent). Rural minoritychildren more often lived in familieswith no earners than did rural Whitechildren: White, 5 percent; Black, 19percent; Hispanic, 8 percent; <strong>and</strong> NativeAmerican, 12 percent.Social welfare programs contribute tochildren’s well-being by providing cashor in-kind assistance to needy families.In 1996, 1.2 million rural children livedin families participating in Aid to <strong>Fam</strong>ilieswith Dependent Children (AFDC),which was replaced by the TemporaryAssistance to Needy <strong>Fam</strong>ilies (TANF)program. TANF provides time-limitedPercentage of households experiencing food insecurity, 1995Levels of food insecurity were very similar in rural <strong>and</strong> urban households; food insecurity wasmost prevalent among racial <strong>and</strong> ethnic minorities <strong>and</strong> in single-parent families with children.Category Nonmetro Metro U.S. totalPercentage of householdsAll households 12.2 11.9 11.9Census regionNortheast 9.7 10.4 10.3Midwest 10.3 10.8 10.6South 13.3 12.3 12.5West 14.9 13.6 13.8Race <strong>and</strong> ethnicity (of household head)White non-Hispanic 10.3 8.1 8.7Black 28.3 23.5 24.2Hispanic 21.3 26.2 25.7Household structureTwo-parent families with children 12.9 11.1 11.5Single-parent families with children 32.8 32.2 32.3Multiple-adult households, no children 6.9 6.3 6.4Single men living alone 13.3 12.9 13.0Single women living alone 10.2 11.4 11.1Percentage of persons 1Age0-17 20.4 19.7 19.818-64 12.9 11.9 12.165 <strong>and</strong> over 5.5 5.5 5.51 Food security is determined at the household level. In the age breakdown, the numbers represent thepercentage of persons in each age category living in households classified as food insecure.Source: Prepared by ERS using data from the Current Population Survey Food Security Supplement,April 1995.benefits to needy families, mostlyheaded by single parents, <strong>and</strong> providesassistance in finding employment <strong>for</strong>the parents.Changes in the TANF program willtrigger changes in the Food StampProgram, a program with much higherchild participation rates than AFDC.Among the most important changes thataffect children are the reduction of foodstamp benefits from 103 to 100 percentof the Thrifty Food Plan <strong>and</strong> the restrictionof food stamp eligibility <strong>for</strong> manylegal immigrants. These changes couldaffect 2.8 million or 20 percent of ruralchildren.<strong>Fam</strong>ilies of rural minority children relymore on government assistance programsthan do families of rural White children.Forty-five percent of rural Black children,94 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
36 percent of Native American children,<strong>and</strong> 29 percent of Hispanic childrenlived in families that received food stamps,compared with 14 percent of rural Whitechildren. Also, 15 percent of rural Black<strong>and</strong> Native American children lived infamilies that participated in the housingsubsidy program that helps needy familiespay their rent, compared with 5 percentof rural White children.Levels of Food Insecurity inRural HouseholdsUSDA’s food assistance programs areintended not only to prevent hunger,but also to ensure that all citizens----especially all children----have regularaccess to the quantity <strong>and</strong> quality offood needed <strong>for</strong> an active, healthy life.USDA <strong>and</strong> the Department of Health<strong>and</strong> Human Services have developed asurvey to monitor food insecurity <strong>and</strong>hunger in the United States. Householdsare said to be food insecure when theydo not have assured access, in sociallyacceptable ways, to enough food <strong>for</strong> anactive, healthy life.During the year prior to April 1995,only 12 percent of rural <strong>and</strong> urbanhouseholds could be classified as foodinsecure (table). Within urban areas,food security was more prevalent incentral cities (16.1 percent) than in suburbanareas (9.5 percent). Regionally,food insecurity was highest in the ruralWest (14.9 percent) <strong>and</strong> lowest in therural Northeast (9.7 percent). Ruralurb<strong>and</strong>ifferences were not substantialin any region.Overall, food insecurity was much moreprevalent among Blacks (24.2 percent)<strong>and</strong> Hispan<strong>ics</strong> (25.7 percent) than amongWhites (8.7 percent). The householdtype that experienced the highest ratesof food insecurity was the single-parentfam<strong>ily</strong>: nearly one-third of these familieswere classified as food insecure. Thelowest rates of food insecurity wereobserved in multiple-adult, no-children,households----6.4 percent. Among thoseliving alone, food insecurity was moreprevalent among men than amongwomen, even though the poverty rate<strong>for</strong> women living alone was substantiallyhigher than that <strong>for</strong> men livingalone.Hunger in the United States is intermittent<strong>and</strong> often hidden. However, one ormore household members experiencedrepeated, poverty-related hunger in 4.1percent of U.S. households. More than10 percent <strong>for</strong> rural Blacks as well assingle-parent families with children inboth rural <strong>and</strong> urban areas experiencedhunger.Less than 1 percent of households experiencedwhat is characterized as severehunger: adults going whole days withouteating, reducing the size of children’smeals, <strong>and</strong> children being hungry becausethere is not enough money to buy food.Estimating the percentage of childrenwho experience poverty-related hungeris indirect <strong>and</strong> uncertain, <strong>and</strong> the qualityof children’s diets is often reduced evenin households in which adult hunger isless severe.Housing Problems inRural AmericaRecent changes in Federal housing programshave added flexibility, increasedthe role of State <strong>and</strong> local governments,<strong>and</strong> emphasized the inclusion of segmentsof the population <strong>and</strong> geographicareas that were deemed underserved byexisting housing <strong>and</strong> home mortgagemarkets. Public policy is clearly gearedtoward promoting greater homeownership,as demonstrated by governmenttax policies <strong>and</strong> program initiatives. Therate of homeownership is at an all-timehigh, with nearly two-thirds of all U.S.households <strong>and</strong> three-fourths of ruralhouseholds owning their home in 1995.In the first quarter of 1998 U.S. medianhousehold income was 34 percent morethan needed to af<strong>for</strong>d the median-pricedhome. According to this widely usedindicator, housing has not been soaf<strong>for</strong>dable since 1973.In 1995 homeownership was higheramong nonmetro than among metrohouseholds <strong>for</strong> each of the populationgroups. Ownership was the dominantpattern <strong>for</strong> all nonmetro groups but not<strong>for</strong> metro Black, Hispanic, or poor households.Whereas nearly 80 percent ofnonpoor White households in nonmetroareas owned their home, comparablefigures <strong>for</strong> Hispanic <strong>and</strong> Black householdswere only 62 <strong>and</strong> 68 percent, respectively.Housing that lacks complete plumbingfacilities <strong>for</strong> the exclusive use of residentswas a problem in 1995 <strong>for</strong> less than2 percent of U.S. households. In 1960,30 percent of nonmetro <strong>and</strong> 7 percent ofmetro homes lacked complete plumbingfacilities. Housing expenses were moreof an urban than a rural problem <strong>for</strong> allthe population groups considered. Asexpected, excessive housing expenseswere mostly a problem <strong>for</strong> the poor.Over 2 percent of nonmetro householdshad housing expenses that consumedover half the household’s income.Homeownership rates among the 65-<strong>and</strong>olderpopulation were 84 percent in nonmetro<strong>and</strong> 76 percent in metro areas----well above the overall levels in 1995. Themedian home equity of elderly nonmetrohomeowners was over $60,000, becausemore than 85 percent owned their homefree <strong>and</strong> clear of mortgage debt.Source: Rural Conditions <strong>and</strong> Trends, 1998,9(2):81-101.1999 Vol. 12 Nos. 3&4 95
AlternativeEmploymentArrangementsIn<strong>for</strong>mation on workers in four alternativeemployment arrangements wascollected in the February 1997 CurrentPopulation Survey (CPS) <strong>and</strong> comparedwith similar in<strong>for</strong>mation obtained in theFebruary 1995 CPS. In general, the proportionof total employment accounted<strong>for</strong> by each arrangement, as well as thecharacterist<strong>ics</strong> of workers, had notchanged significantly.People employed in two of thesearrangements----temporary help agencyworkers <strong>and</strong> contract company workers----are employees of one company <strong>and</strong>carry out assignments <strong>for</strong> another.Workers in a third arrangement----workers on call----do not have an establishedschedule <strong>for</strong> reporting to work.The fourth arrangement----independentcontractors----consists of workers whoare not employees in the traditional sensebut those who work <strong>for</strong> themselves.Being the largest group, independentcontractors accounted <strong>for</strong> two-thirds ofworkers in alternative arrangements <strong>and</strong>6.7 percent of all workers. The proportionof workers in the various alternativearrangements was unchangedbetween 1995 <strong>and</strong> 1997. However, thenumber of workers in the four arrangementsincreased by about 400,000 overthe 2-year period.This report covers demographic <strong>and</strong> jobcharacterist<strong>ics</strong>, earnings, <strong>and</strong> benefits ofworkers in each alternative arrangement<strong>and</strong> compares them with workers intraditional arrangements. Classificationof workers was made without regard totheir contingent status (whether theirjob was temporary) or their part-timestatus. Part-time workers were classifiedin an alternative arrangement only if theymet the criteria <strong>for</strong> that arrangement.Independent ContractorsIn February 1997, 8.5 million people wereidentified as independent contractors,independent consultants, or freelanceworkers. Most independent contractors(88 percent) were self-employed. Abouthalf of all self-employed individuals wereidentified as independent contractors,rather than as other types of self-employedworkers, such as shop or restaurantowners.Two-thirds of independent contractorswere men; they were older <strong>and</strong> hadmore education than the average worker(table 1). Nearly 70 percent weremarried, compared with 59 percent oftraditional workers. About 26 percentworked less than 35 hours in a typicalweek, compared with 18 percent oftraditional workers; however, nearly30 percent of independent contractorsworked 49 hours or more in a typicalweek, compared with only 17 percentof traditional workers.The most common occupations <strong>for</strong> maleindependent contractors were managers,construction craftworkers, proprietors,writers <strong>and</strong> artists, <strong>and</strong> real estate <strong>and</strong>insurance salespersons. For women, themost frequently occurring occupationswere managers, writers <strong>and</strong> artists, realestate <strong>and</strong> insurance salespersons, doorto-doorsales, <strong>and</strong> child-care providers.Compared with workers in the otheralternative arrangements, independentcontractors liked their employmentarrangement----84 percent preferred it toa traditional job. Men reported that theyliked being their own boss, <strong>and</strong> womensaid they liked the flexibility of scheduling<strong>and</strong> the ability to meet fam<strong>ily</strong> obligations.Only 3.5 percent of independent contractorsreported that they were contingent ortemporary workers, the lowest percentageof the alternative arrangements. Medianyears in the arrangement were greaterthan those <strong>for</strong> traditional workers withtheir current employer, 7.7 years versus4.8 years.Among full-time workers, earnings ofmale independent contractors were higherthan those of their counterparts in traditionalemployment, whereas earningsof female independent contractors werelower (table 2). The gender gap in earningswas greater among independentcontractors (52 percent) than amongtraditional workers (28 percent). Healthinsurance coverage was reported byalmost three-quarters of independentcontractors; women were more likelythan men to have coverage, <strong>and</strong> womenwith coverage were more likely toobtain it through a spouse or other fam<strong>ily</strong>member (38 percent) than by purchasingit on their own (25 percent). About 37percent of independent contractors hadsome type of pension coverage.On-Call WorkersThese workers report to the job only whenspecifically asked to do so, although itmay be <strong>for</strong> several days, or even weeks,in a row. Workers who are often on callinclude substitute teachers, constructionworkers, nurses, <strong>and</strong> truckdrivers. Peoplewith regularly scheduled work who alsomight be on call after hours (medicalresidents <strong>and</strong> computer technicians)were not included in this category. InFebruary 1997, there were 2 millionon-call workers.96 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Table 1. Employed persons with alternative <strong>and</strong> traditional work arrangements, by selected characterist<strong>ics</strong>,February 1997 [percent distribution]CharacteristicIndependentcontractorsWorkers with alternative arrangementsTemporary WorkersOn-call help provided byworkers agency workers contract firmsWorkers withtraditionalarrangementsAgeTotal, 16 years <strong>and</strong> older (thous<strong>and</strong>s) 8,456 1,996 1,300 809 114,199Percent 100.0 100.0 100.0 100.0 100.016 to 19 years .8 9.7 6.1 2.0 5.020 to 24 years 2.4 11.9 16.5 8.2 9.825 to 34 years 18.3 22.4 30.3 34.2 25.435 to 44 years 31.1 25.4 21.5 31.1 27.745 to 54 years 26.5 14.4 16.2 14.2 20.455 to 64 years 13.9 9.7 6.7 7.7 9.265 years <strong>and</strong> older 7.0 6.5 2.8 2.7 2.5SexMen, 16 years <strong>and</strong> older 66.6 49.0 44.7 69.8 52.7Women, 16 years <strong>and</strong> older 33.4 51.0 55.3 30.2 47.3Race <strong>and</strong> Hispanic originWhite 90.7 89.3 75.1 81.6 84.8Black 5.3 7.8 21.3 12.9 10.9Hispanic origin 7.3 13.3 12.3 6.3 9.6Educational attainmentTotal, 25 to 64 years (thous<strong>and</strong>s) 7,590 1,437 970 705 94,424Percent 100.0 100.0 100.0 100.0 100.0Less than a high school diploma 8.7 13.4 11.1 7.1 9.7High school graduate, no college 30.3 28.7 30.7 36.9 32.8Less than a bachelor’s degree 26.8 32.0 36.3 23.3 28.0College graduate 34.1 25.9 21.9 32.7 29.5Note: Workers with traditional arrangements are those who do not fall into any of the ‘‘alternative arrangements’’ categories. Details <strong>for</strong> the above race <strong>and</strong>Hispanic-origin groups will not sum to totals because data <strong>for</strong> the ‘‘other races’’ group are not presented, <strong>and</strong> Hispan<strong>ics</strong> are included in both the White <strong>and</strong>Black population groups. Details <strong>for</strong> other characterist<strong>ics</strong> may not sum to totals because of rounding.1999 Vol. 12 Nos. 3&4 97
Table 2. Median weekly earnings of full-time workers with alternative <strong>and</strong> traditional work arrangements,by selected characterist<strong>ics</strong>, February 1997CharacteristicIndependentcontractorsOn-callworkersTemporaryhelpagency workersWorkersprovided bycontract firmsWorkers withtraditionalarrangementsAge <strong>and</strong> sexTotal, 16 years <strong>and</strong> older $587 $432 $329 $619 $51016 to 19 years (1) 243 (1) (1) 23720 to 24 years 478 328 286 (1) 32825 years <strong>and</strong> older 590 457 364 681 550Men, 16 years <strong>and</strong> older 621 508 385 685 57816 to 19 years (1) (1) (1) (1) 25220 to 24 years 523 328 312 (1) 34325 years <strong>and</strong> older 624 524 406 727 613Women, 16 years <strong>and</strong> older 409 286 305 439 45016 to 19 years (1) (1) (1) (1) 21720 to 24 years (1) (1) 252 (1) 30925 years <strong>and</strong> older 414 287 323 439 479Race <strong>and</strong> Hispanic originWhite 603 455 324 675 524Black 399 378 332 394 428Hispanic origin 438 321 281 (1) 357Educational attainmentLess than a high school diploma 398 289 265 (1) 302High school graduate, no college 512 423 310 491 427Some college, no degree 581 498 306 522 494Associate’s degree 523 558 433 (1) 519College graduate 752 521 497 910 7691 Data not shown where base is less than 75,000.Note: Workers with traditional arrangements are those who do not fall into any of the ‘‘alternative arrangement’’ categories.On-call workers, compared with traditionalworkers, were more likely to befemale (51 percent <strong>and</strong> 47 percent,respectively). And more of the womenwho were on-call workers, comparedwith traditional workers, had children(61 vs. 56 percent). The percentage ofon-call workers who were Hispanic washigher than that <strong>for</strong> the general work<strong>for</strong>ce(13 vs. 10 percent). Also, about22 percent of those on call were underthe age of 25, compared with 15 percentof traditional workers. Male on-callworkers were less likely than other maleworkers to have graduated from college,whereas female on-call workers weremore likely to have a college education.More than half (53 percent) of on-callworkers worked part time in a typicalweek; only 18 percent of traditionalworkers did so. Among those 20 years<strong>and</strong> older, women on call were muchmore likely (68 percent) than men (28percent) to work part time.98 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
On-call workers who were male werelikely employed as construction craftworkers,motor vehicle operators, <strong>and</strong>cleaners, helpers, <strong>and</strong> constructionlaborers. Female on-call workers weremost often working as substitute teachers,clerical workers, food preparationworkers, nurses, <strong>and</strong> retail salesclerks.About half of on-call workers wouldhave preferred a traditional job. Mostmen gave an eco<strong>nom</strong>ic reason <strong>for</strong> beingon-call workers, <strong>and</strong> the most oftencited reason was that the current job wasthe only one the individual could find.Most women, on the other h<strong>and</strong>, gave apersonal reason----most often the reasonwas schedule flexibility.Among full-time workers, on-callworkers who worked full time earnedabout 85 percent of the median earnedby traditional workers. However, womenearned only 56 percent of what menearned in on-call arrangements, comparedwith 78 percent in traditionaljobs. Health insurance coverage wasreported by about two-thirds of on-callworkers, but only 20 percent received itfrom their current employer. Only 31percent reported that they were eligible<strong>for</strong> health insurance coverage from theiremployer, compared with 73 percent oftraditional workers. About one-fourthof on-call workers were eligible <strong>for</strong> anemployer-provided pension; 19 percentwere actually included in a plan.Temporary Help AgencyWorkersTemporary help agencies place, screen,evaluate, <strong>and</strong> sometimes train workerswith client organizations. Thus theseworkers are employed (<strong>and</strong> paid) byone company while per<strong>for</strong>ming work<strong>for</strong> another. In February 1997, temporaryhelp agencies (including a small numberof agency staff) had 1.3 million employees.The number of workers in this arrangementincreased by 10 percent over the2-year period since February 1995, comparedwith 2.8 percent <strong>for</strong> traditionalemployment.Workers employed by temporary helpagencies were more likely than otherworkers to be young, female, Black, orHispanic. Nearly one-fourth were underthe age of 25. Only 16 percent wereattending high school or college, comparedwith 43 percent of young peopleworking in a traditional job. A majorityof temps had at least 1 year of college----but fewer had a college degree, comparedwith traditional workers (22 percent <strong>and</strong>30 percent, respectively). About 55 percentof temps were female, comparedwith 47 percent of traditional workers.The percentage of temps who wereBlack (21 percent) was nearly doublethat <strong>for</strong> other workers, <strong>and</strong> the sharewho were Hispanic also exceeded thatin the general work<strong>for</strong>ce. More Hispanicmen than women worked as temps.Most (80 percent) temps worked a fulltimeweek of at least 35 hours. Amongthose who worked part time, 41 percentwould have preferred a full-time job----compared with only 18 percent of traditionalworkers. Whereas 41 percent ofmale temps worked as operators, fabricators,or laborers, about half of femaletemps held clerical jobs.Nearly 60 percent of all temps said theywould prefer a traditional job. Whenasked why they were working as temps,35 percent stated it was the only typework they could find. Also, 18 percenthoped the temporary job would lead topermanent employment. Personal reasonswere cited less often by the temps thanby independent contractors <strong>and</strong> on-callworkers.The survey confirmed that peopleemployed by temporary help agenciescan be assigned to one client <strong>for</strong> arelatively long time. The median currenttenure in the assignment was about5 months; the median tenure in theemployment arrangement was 6 months.Nearly all temps were assigned to justone client during the reference week;80 percent were registered with justone temp agency.Temporary help agency workers had thelowest earnings of workers in the fouralternative arrangements <strong>for</strong> full-timeworkers. Median earnings were abouttwo-thirds those of traditional workers,reflecting the fact that clerical <strong>and</strong>machine operator jobs typically held bythese workers pay lower-than-averagewages. Rates of health insurance coverage<strong>and</strong> pension benefits were the lowest ofthe arrangements studied. Only 26 percentof temp workers were eligible <strong>for</strong>their employer’s health insurance coverage,<strong>and</strong> an even smaller percentage----only 7 percent----obtained healthinsurance through their employer.Pension coverage was even lower;about 1 temp in 10 was eligible <strong>for</strong> anemployer’s pension plan; only 4 percentparticipated in such a plan.Contract Company WorkersThese individuals worked <strong>for</strong> a companythat provides employees or their servicesto other organizations under contract.They usually worked <strong>for</strong> one customerat a time at the customer’s work site.This arrangement grew by 24 percentbetween 1995 <strong>and</strong> 1997; even so, inFebruary 1997, contract companyworkers consisted of just 0.6 percentof all workers.Contract workers were primar<strong>ily</strong> male(70 percent) <strong>and</strong> between the ages of 251999 Vol. 12 Nos. 3&4 99
<strong>and</strong> 44 (65 percent). Among femaleworkers, 66 percent had children. Mostcontract workers worked full time, butwomen were much more likely to workpart time than were men (36 percent <strong>and</strong>8 percent, respectively).Contract company workers weremore likely than workers in traditionalarrangements to hold professional, technical,service, <strong>and</strong> precision-productionjobs. Comparatively few held managerial,sales, <strong>and</strong> clerical positions. Onehalfof male workers were in service<strong>and</strong> precision-production occupations,compared with 28 percent of men intraditional arrangements. More than 60percent of women were in professional<strong>and</strong> service occupations, comparedwith 34 percent of women in traditionalarrangements.About 40 percent of contract companyworkers had worked in the arrangement<strong>for</strong> 1 year or less. Yet, more than 80percent believed they could remainindefinitely on their current assignment.ConclusionOf the four alternative arrangementsexamined here, independent contractingwas the largest. Generally, workers inthis arrangement preferred it to a traditionalarrangement, viewed their jobs aspermanent, worked full time, <strong>and</strong> werequite highly paid.In contrast, many workers in otherarrangements might have preferredmore job security, higher pay, <strong>and</strong>more hours. However, each arrangementincludes workers who were satisfiedwith their job situation. Thus thereappears to be as much variation in thecharacterist<strong>ics</strong> of the jobs <strong>and</strong> workerswithin each type of employmentarrangement as there is betweendifferent types of arrangements.Source: Cohany, S.R., 1998, Workers in alternativeemployment arrangements: A second look,Monthly Labor Review 121(11):3-21.Median weekly earnings <strong>for</strong> contractcompany employees were higher thanearnings <strong>for</strong> workers in any otherarrangement, including a traditionalarrangement <strong>for</strong> full-time workers.Women, however, earned only 64 percentof men’s earnings. Almost 70 percentof contract company workers wereeligible <strong>for</strong> employer-provided healthinsurance, <strong>and</strong> one-half received it fromtheir employer----the highest rates of anyalternative arrangement. Nearly half ofthe workers in the arrangement wereeligible <strong>for</strong> their employer’s pensionplan, <strong>and</strong> 36 percent participated inthe plan. These percentages also werethe highest among the alternativearrangements.100 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Factors AffectingNutrient Intake ofthe ElderlyThe number of Americans age 60 <strong>and</strong>over is exp<strong>and</strong>ing rapidly: from about5 million in 1900 to about 42 million in1990, a figure that is expected to morethan double by 2030. The elderly, whoare about 18 percent of the population,account <strong>for</strong> about 30 percent of allhealth care expenditures in the UnitedStates.Poor nutritional status is a primaryconcern <strong>for</strong> the elderly. <strong>Nutrition</strong>allyinadequate diets can contribute to orexacerbate chronic <strong>and</strong> acute diseases <strong>and</strong>hasten the development of degenerativediseases associated with aging. In thepast, it has been difficult to determinethe scope of nutritional problems amongthe aged; however, methods of assessingdietary intake have improved. Providingin<strong>for</strong>mation on the relationship of socioeco<strong>nom</strong>ic<strong>and</strong> other factors to nutrientintake is basic to improving the health<strong>and</strong> well-being of the elderly.The purpose of this study was to estimatethe effect of a number of selected characterist<strong>ics</strong>of households <strong>and</strong> their memberson nutrient intake of the elderly. Datawere from the U.S. Department of Agriculture’s(USDA) 1989-91 ContinuingSurvey of Food Intakes by Individuals(CSFII). The sample consisted of individuals60 years of age or older who werethe <strong>nom</strong>inal head of their household. Inhouseholds with both a female <strong>and</strong> malehead of household, only the female’snutrient intake was considered. Elderlyindividuals who were not <strong>nom</strong>inal headsof households were excluded from thisanalysis, thus the focus was on thoseelderly who had some auto<strong>nom</strong>y inTable 1. Mean nutrient intake of the elderly <strong>and</strong> comparison with 1989Recommended Dietary Allowances 1NutrientMeanintakeWomenmaking their food choices. The finalsample consisted of 1,373 women <strong>and</strong>193 men; their average age was 71.Multiple regressions were used toexplain nutrient intake. Twelve nutrientswere selected <strong>for</strong> study because previousresearch has found that diets of theelderly are often below recommendedlevels 1 <strong>for</strong> these nutrients: Energy, protein,fat, vitamin E, vitamin C, niacin, vitaminB6, calcium, phosphorus, magnesium,iron, <strong>and</strong> zinc. The sample’s mean intakesfell below the RDA <strong>for</strong> energy, vitamins1 Dietary studies frequently define an adequate,nutritious diet as one that fulfills the RecommendedDietary Allowances (RDA). The RDA specify thelevels of average intake of nutrients essential <strong>for</strong>maintaining normal body functioning <strong>for</strong> a healthypopulation. Diets under 100 percent of the RDAare asssociated with, but not necessar<strong>ily</strong> mean,deficiency.Percent ofrecommendedallowanceMeanintakeMenPercent ofrecommendedallowanceEnergy (kcal) 1,345.3 70.8 1,733.0 75.3Protein (gm) 56.1 112.2 71.9 114.1Total fat (gm) 50.6 NA 67.8 NAVitamin E (mg) 6.4 80.0 7.3 73.0Vitamin C (mg) 87.9 146.5 92.3 153.8Niacin (mg) 16.4 125.4 20.7 138.0Vitamin B6 (mg) 1.4 87.5 1.7 85.0Calcium (mg) 572.5 71.5 693.1 86.6Phosphorus (mg) 893.2 111.6 1,127.1 140.9Magnesium (mg) 212.6 75.9 248.6 88.8Iron (mg) 11.4 114.0 13.9 139.0Zinc (mg) 8.3 69.2 10.2 85.01 Mean intakes calculated using the1989-91 CSFII 3-year household weights.E <strong>and</strong> B6, calcium, magnesium, <strong>and</strong> zinc;however, during the 3-day reportingperiod, the variation was wide (table 1).Among women, over one-third hadnutrient intakes below the RDA <strong>for</strong>energy <strong>and</strong> <strong>for</strong> each nutrient (exceptfat----<strong>for</strong> which no RDA exists). Amongmen, over one-third had intakes belowthe RDA <strong>for</strong> energy <strong>and</strong> each nutrient,except niacin <strong>and</strong> phosphorus (table 2).Socioeco<strong>nom</strong>ic characterist<strong>ics</strong> of elderlyindividuals that influenced nutrientintake were gender, race, educationalattainment, <strong>and</strong> employment status ofthe household head. General householdcharacterist<strong>ics</strong> investigated includeddegree of urbanization, geographic region,socialization available, food stampparticipation, <strong>and</strong> receipt of surpluscommodity foods.1999 Vol. 12 Nos. 3&4 101
Table 2. Percentage of elderly falling below 1989 Recommended DietaryAllowances <strong>for</strong> selected nutrientsResultsNutrient Women MenEnergy (kcal) 89 83Protein (gm) 38 37Vitamin E (mg) 79 80Vitamin C (mg) 40 48Niacin (mg) 34 23Vitamin B6 (mg) 68 72Calcium (mg) 82 68Phosphorus (mg) 41 20Magnesium (mg) 83 86Iron (mg) 51 35Zinc (mg) 87 88Note: Recommended Dietary Allowances are <strong>for</strong> adults 51 years of age <strong>and</strong> over.Source: Elderly Heads of Household, Continuing Survey of Food Intakes by Individuals, 1989-91, U.S.Department of Agriculture.EducationThis characteristic of the household headwas associated directly with nutritionalknowledge <strong>and</strong> a more balanced diet <strong>for</strong>individuals in the household. In householdswith both a female <strong>and</strong> male head,education of the female head served as aproxy <strong>for</strong> nutritional knowledge in thehousehold. (In elderly households, itwas assumed that the female would bethe primary decisionmaker who selected<strong>and</strong> prepared the food.) Consumption ofmost of the selected nutrients tended tobe related positively to additional <strong>for</strong>maleducation <strong>and</strong> was statistically significant<strong>for</strong> vitamins C, E, <strong>and</strong> B6, niacin,calcium, phosphorus, <strong>and</strong> magnesium.Region <strong>and</strong> Degree ofUrbanizationElderly residents in the South consumedfewer calories <strong>and</strong> less protein, fat, vitaminsC <strong>and</strong> B6, niacin, phosphorus, <strong>and</strong>magnesium than did the elderly in theNortheast. Levels of nutrient intake <strong>for</strong>elderly residents in the South were notsignificantly different from those in theMidwest or West, although the Southernelderly consumed more calcium th<strong>and</strong>id the Midwestern elderly. Findingsshowed that urban elderly residents consumedlower amounts of most nutrientsthan did nonurban elderly, although thiswas statistically significant <strong>for</strong> iron only.The literature reports that the degree ofurbanization reflects the potential <strong>for</strong>the production of home foods, diversityof types of stores, differences in cultural<strong>and</strong> eco<strong>nom</strong>ic opportunities, <strong>and</strong> exposureto mass media.SocializationSome researchers theorize that theelderly experience a decrease in appetite<strong>and</strong> interest in food when they eat alone,with the result being poor nutritionalintake. This study examined the sizeof the household. If the householdcontained other members, then theopportunity <strong>for</strong> meal socialization waspresent. However, this factor was notsignificant <strong>for</strong> any nutrient studied.Poverty, Food Stamp Participation,<strong>and</strong> Receipt of Surplus FoodA measure of the household’s ability topurchase a nutritionally adequate dietis the amount of household income asa percentage of the appropriate povertythreshold. As reflected by this index,poverty was related to significantlylower intake of all the selected nutrientsexcept vitamin E, calcium, <strong>and</strong> iron. Useof food stamps increases an individual’sfood expenditures. And although someresearchers have found a significanteffect of food stamp participation onnutrient intake, this study found norelationship between the two factors.Similarly, receipt of commodity foods 2was not a significant factor affectingnutrient intake. These findings havebeen confirmed in previous studies.Race, Age, <strong>and</strong> Gender of IndividualResults of this study suggest that nutrientconsumption by the elderly differsbased on race. Compared to elderlyWhites, elderly Blacks consumed fewercalories <strong>and</strong> less total fat, vitamins E<strong>and</strong> B6, niacin, calcium, phosphorus,magnesium, iron, <strong>and</strong> zinc. Hispanic2 Commodity foods are distributed through theCommodity Supplemental Food Program, fromwhich both funds <strong>and</strong> commodity foods aredonated to States to supplement the diets ofvarious target populations, including persons60 years <strong>and</strong> older.102 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
elderly consumed more protein, comparedwith elderly Whites. Intake ofprotein <strong>and</strong> niacin was significantlyhigher among the ‘‘young’’ elderly----those between 60 <strong>and</strong> 70 years old----than it was <strong>for</strong> those over 70 years old.Compared with elderly men’s diets,those of elderly women were significantlylower in all nutrients studiedexcept <strong>for</strong> vitamin C.Employment of Head of HouseholdEmployment of the head of householdcould reflect a more active lifestyle <strong>for</strong>elderly residents in the household. Inthis study, employment status was notsignificantly related to nutrient intake.Sensitization to the RelationshipBetween Diet <strong>and</strong> HealthThe hypothesis stated that a goodpredictor of nutrient intake might be aperson’s knowledge about the relationshipbetween diet <strong>and</strong> health. Data fromthe Diet <strong>and</strong> Health Knowledge Survey,which was conducted among the 1989-91 CSFII households, were linked toin<strong>for</strong>mation on food consumption, <strong>and</strong>thus, nutrient intake. This variablehad a minimal effect on respondents’nutrient intake, except <strong>for</strong> vitamin C<strong>and</strong> magnesium.ConclusionsSeveral characterist<strong>ics</strong> of the elderly <strong>and</strong>their households influenced their nutrientintake: education, income, urbanization,race, age <strong>and</strong> gender, <strong>and</strong>, to some extent,region. These exploratory findings indicatethat food <strong>and</strong> nutrition programs<strong>for</strong> the elderly would be most effectiveif directed toward residents in central cities,the less educated, <strong>and</strong> Blacks. Budgeting<strong>and</strong> planning low-costnutritious meals should be emphasizedbecause of the relationship betweensocioeco<strong>nom</strong>ic status (income <strong>and</strong>education variables) <strong>and</strong> nutrient intakes.<strong>Nutrition</strong>al well-being is integral toelders’ overall health, independence,<strong>and</strong> quality of life. <strong>Policy</strong>makers needto seek effective methods of achievingoptimal nutrition in the older population,<strong>and</strong> researchers should strive to providebetter measurements of the variation innutrient intake <strong>and</strong> their relationships tosocioeco<strong>nom</strong>ic <strong>and</strong> other factors.Source: Weimer, J.P., 1998, Factors AffectingNutrient Intake of the Elderly, Agricultural<strong>Eco</strong><strong>nom</strong>ic Report No. 769, U.S. Department ofAgriculture, <strong>Eco</strong><strong>nom</strong>ic Research Service.1999 Vol. 12 Nos. 3&4 103
The Food StampProgram AfterWelfare Re<strong>for</strong>mThe Personal Responsibility <strong>and</strong> WorkOpportunity Reconciliation Act of 1996(PRWORA) dramatically changed Federalwelfare policy. The Act eliminated theentitlement program Aid to <strong>Fam</strong>ilieswith Dependent Children (AFDC),replacing it with a fixed block grantthat gave States the fundamental roleof helping poor families <strong>and</strong> that addednew work requirements <strong>for</strong> recipients.PRWORA ended eligibility <strong>for</strong> manyaliens <strong>and</strong> placed time limits on benefits<strong>for</strong> able-bodied, childless adults. TheCongressional Budget Office estimatedthe savings to the Federal Governmentto be $54.2 billion through 2002.About half of the expenditure cutsdirectly affect food stamps, now theonly Federal entitlement, except <strong>for</strong>Medicaid, available to all low-incomehouseholds. Lower transfer paymentslead low-income households to reducetheir food expenditures, change the typesof food consumed, <strong>and</strong> reduce their expenditureson other goods. Lower foodexpenditures <strong>and</strong> changing patterns offood consumption, particularly <strong>for</strong>children, may have significant effectson nutrition <strong>and</strong> long-term consequences<strong>for</strong> cognitive development, medicaloutlays, <strong>and</strong> productivity losses.This study focuses on three interrelatedeco<strong>nom</strong>ic phe<strong>nom</strong>ena: the implicationsof decreasing food stamp benefits onfood production <strong>and</strong> consumption <strong>and</strong>the general eco<strong>nom</strong>y; the effect of changesin the macroeco<strong>nom</strong>ic environment onpoverty, Food Stamp Program participation,<strong>and</strong> budget outlays <strong>for</strong> food stamps;<strong>and</strong> the potential <strong>for</strong> State governmentsto shift the burden of supporting the poorto the Food Stamp Program, therebyputting greater emphasis on the FoodStamp Program as a social safety net.The Food Stamp ProgramFederal spending on food stamps hastraditionally exceeded Federal expenditureson both AFDC <strong>and</strong> housing assistanceprograms. The Federal Governmentfunds the benefits under the Food StampProgram but shares costs to administerthe program with State <strong>and</strong> localgovernments.To participate in the Food Stamp Program,households must meet eligibility requirementsbased on citizenship, income, <strong>and</strong>asset ownership. Gross monthly incomeof most households cannot exceed 130percent of the Federal poverty guidelines,which, in 1998, defined the povertythreshold <strong>for</strong> a fam<strong>ily</strong> of three (singleparent <strong>and</strong> two children) as $1,445 permonth. Another eligibility requirementstates that households may have no morethan $2,000 in assets ($3,000 if at leastone member of the household is age 60or older). The home, however, is notcounted as an asset.The maximum value of food stamps ahousehold receives varies by householdsize <strong>and</strong> is adjusted annually <strong>for</strong> changesin the cost of the Thrifty Food Plan.Because households are assumed tospend about 30 percent of their incomeon food, a household’s food stamp allotmentis equal to the maximum allotment<strong>for</strong> that household’s size, minus 30 percentof the household’s net income. In1996 the average food stamp householdreceived a monthly food stamp benefitof $174 <strong>and</strong> had an average of 2.5people in the household.The characterist<strong>ics</strong> of householdsreceiving food stamps vary. In 1996, 60percent of food stamp households hadchildren, 20 percent had disabled persons,<strong>and</strong> 16 percent had elderly persons.About 60 percent of the children wereschool-age, <strong>and</strong> over two-thirds of theadults were women. Over 90 percentof the food stamp households lived inpoverty, <strong>and</strong> most food stamp householdswith children were headed by a singleparent receiving support from TANF----Temporary Assistance to Needy <strong>Fam</strong>iliesProgram. 1 About one-quarter of foodstamp households had earned income.For the average food stamp householdheaded by a single female with twochildren, food stamps accounted <strong>for</strong>about 25 percent of the fam<strong>ily</strong>’s householdresources. If the <strong>nom</strong>inal dollarvalue of food stamp benefits is addedto income, the distribution of povertystatus among food stamp recipientsdiffers significantly (table).PRWORA stipulated that by 1997,25 percent of the single-parent familiesreceiving TANF benefits must work atleast 20 hours a week, <strong>and</strong>, by 2002,50 percent must work at least 30 hoursa week. For two-parent families, 90 percentmust work a combined 35 hours aweek by 1999. If States do not meetthese requirements, their grant from theFederal Government will be cut eachyear----providing States with an impetusto move families into the workplace <strong>and</strong>off welfare. Under TANF, recipient1 Under the block-grant structure of TANF, everyState is given a fixed sum of Federal money(based on recent spending levels <strong>for</strong> AFDC) <strong>and</strong>,with a wide latitude, the States are free to designhow to provide this assistance. For example,instead of cash assistance, States can use fundsto set up job training programs to give recipientsskills to enter the work <strong>for</strong>ce.104 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Effect of food stamp benefits on poverty, 1995Gross income as apercentage of thepoverty thresholdfamilies can receive benefits funded byFederal monies <strong>for</strong> a lifetime total ofonly 5 years. PRWORA cut more fundsfrom the Food Stamp Program than anyother program: through reductions inhousehold benefits <strong>and</strong> restrictions ineligibility. Expenditures <strong>for</strong> the FoodStamp Program are projected to declineby about $22 billion between 1997 <strong>and</strong>2002. However, because the FoodStamp Program was not placed underblock-granting authority, the program’sentitlement status was retained <strong>and</strong>the national nutritional safety net waspreserved.Effect of Cuts in FederalAssistanceThe net effect of the new law is todecrease significantly outlays <strong>for</strong> foodstamps. Reductions in food stamp benefitswill cause low-income families todecrease spending on food <strong>and</strong> othergoods such as housing, clothing, <strong>and</strong>medical care. The eco<strong>nom</strong>ic effects ofcuts in food stamp benefits are not limitedto the production <strong>and</strong> consumption offood but ripple throughout the eco<strong>nom</strong>y.Distribution of household income relative to poverty thresholdWithoutfood stampsFood stampsincludedas incomePercentchange100% 9 15 6Source: U.S. Department of Agriculture, 1998.The effects of decreasing governmenttransfers to low-income households onfood production <strong>and</strong> consumption, <strong>and</strong>on the general eco<strong>nom</strong>y, are estimatedin two complementary general equilibriumstudies. The studies focus on howchanges in relative sectoral profitabilityaffect changes in output, returns, <strong>and</strong>the flow of resources into <strong>and</strong> out ofthe farm sector.One model simulates the effects oneco<strong>nom</strong>ywide output <strong>and</strong> employmentfrom reducing Food Stamp Programbenefits. Starting from a 1993 base,the model simulates eco<strong>nom</strong>ywideadjustments, given a $4-billion annualaverage decline in the Food StampProgram <strong>for</strong> 5 years. Although all ofthe food stamps are spent on food, fundspreviously spent on food are reallocatedto other needs, such as housing, clothing,or medicare. This marginal propensity toconsume out of food stamps (called thesupplementation effect) implies that theinitial effect of a $23-billion decrease inFood Stamp Program benefits wouldbe a decline of $5 to $10 billion over6 years in retail food spending <strong>and</strong> adecline of $18 to $13 billion over 6 yearsin nonfood spending.According to this model, the new welfarelegislation may affect the agriculturalsector <strong>and</strong> the general eco<strong>nom</strong>y in thefollowing ways:• Retail food spending would decrease;• Dem<strong>and</strong> <strong>for</strong> agricultural commoditieswould decrease;• Commodity prices <strong>and</strong> farm incomewould decrease;• Capital <strong>and</strong> labor would be reallocatedto nonfood sectors.In the short run, the eco<strong>nom</strong>ywide effectswould be negative. But, if the reducedgovernment expenditures <strong>for</strong> transferpayments to low-income families areinjected back into the eco<strong>nom</strong>y as a taxcut, the short-term effects are mitigated.A second model simulates the combinedeffects of cutting transfer payments <strong>and</strong>reducing the taxation of capital by decreasingthe tax on capital gains. Cuttingtransfer payments proportionally acrossall income classes by $10 billion----while increasing the capital gainsexclusion----draws resources into foodproduction, leading to lower prices <strong>and</strong>an increased consumption of goods <strong>and</strong>services by all income classes. Proportionallyredistributing the budget shortfallover all income classes to offsetthe tax reduction still leaves sufficientincome to increase consumption: expenditures<strong>for</strong> food, housing, <strong>and</strong> transportationincrease by nearly $1.5 billion.Food expenditures alone increase by$535 million. Restoring a 30-percentcapital gains exclusion increases nationalwelfare by about $800 million.1999 Vol. 12 Nos. 3&4 105
<strong>Eco</strong><strong>nom</strong>ic Cycles <strong>and</strong> theSocial Safety NetPost World War II legislation, such asThe Employment Act of 1946, committedthe Federal Government to manageovertly the macroeco<strong>nom</strong>y by usingwelfare as a social safety net duringcyclical eco<strong>nom</strong>ic downturns. PRWORAeliminated the entitlement status ofwelfare benefits. States, there<strong>for</strong>e, arenot obligated to exp<strong>and</strong> programs in timesof greatest need. Since funding is primar<strong>ily</strong>through capped block grants to the States,spending <strong>for</strong> welfare is unlikely to increasewhen programs need to exp<strong>and</strong> duringeco<strong>nom</strong>ic downturns. Hence, it is likelythat the Food Stamp Program willbecome more important as a cyclicalsafety net.During a recession, unemployment ratesrise <strong>and</strong> real wages fall. For the averagehousehold, the amount of money available<strong>for</strong> food drops. Food stamps alleviatethe situation as more families becomeeligible----<strong>and</strong> current recipients qualify<strong>for</strong> additional food stamps. It is possible,however, <strong>for</strong> the number of poor toincrease without observing an increasein the number of food stamp recipientsor <strong>for</strong> the number of poor to remain constantwhile observing an increase in thenumber of food stamp recipients. Thesechanges may occur because not all poorpersons qualify <strong>for</strong> food stamps, <strong>and</strong> allpeople below the poverty thresholdmeet the income test but may not meetthe asset test. Also, about 30 to 40 percentof families eligible <strong>for</strong> food stampschoose not to participate in the program.The effects of changing macroeco<strong>nom</strong>icconditions on food stamp participation<strong>and</strong> poverty were estimated. The effectof a 1-percentage point increase in theunemployment rate (combined with a0.07-percentage point decline in theinflation rate) led to a 0.29-percentagepoint increase in the food stamp participationrate <strong>and</strong> a 0.32-percentage pointincrease in the poverty rate after 1 year.Other simulations illustrate the effectsof a mild recession, a more severe recession,<strong>and</strong> a continued robust eco<strong>nom</strong>y<strong>for</strong> the years 1997-2004. Overall, outlays<strong>for</strong> food stamps increase in eachsituation because of the trend effects ofthe number of people in poverty----<strong>and</strong>the increase occurs most slowly in thecase of a continued robust eco<strong>nom</strong>y.Since 1992 the growth rate has not beennegative during any quarter, <strong>and</strong> welfarecaseloads in every State have declinedsharply. The President’s Council of<strong>Eco</strong><strong>nom</strong>ic Advisors found that 44 percentof the decline was due to eco<strong>nom</strong>icexpansion, <strong>and</strong> 31 percent was due tochanges in the States’ welfare programs.Other studies attribute an even higherproportion to eco<strong>nom</strong>ic expansion.The number of food stamp recipientsdeclined from 25.9 million in January1996 to 19.3 million in June 1998.Because the U.S. Department of Health<strong>and</strong> Human Services has determinedthat 90 percent of AFDC/TANF recipientsare also food stamp recipients <strong>and</strong>families tend to move on <strong>and</strong> off multiplewelfare programs, the decline in foodstamp participation must be attributedto both welfare re<strong>for</strong>m <strong>and</strong> the eco<strong>nom</strong>icexpansion.If welfare re<strong>for</strong>m has produced permanentchanges in welfare caseloads, theeffect of future recessions on the ratesof food stamp participation will bemitigated. However, if the recent declinein food stamp participation is due primar<strong>ily</strong>to eco<strong>nom</strong>ic expansion, thedecline is temporary. Then during thenext recession, the rates of food stampparticipation will increase (followinghistorical patterns). As families are <strong>for</strong>cedoff TANF because of the expiration oftime limits <strong>and</strong> enter a contracting labormarket, incomes will fall <strong>and</strong> food stampbenefits will increase. Also, if Statestransfer funds from cash to noncashassistance programs, such as subsidizedday care, the income of TANF recipientswill fall----leading to an increase in foodstamp benefits.Fiscal Effect of Block GrantsThe 5-year time limit on TANF benefitswill eventually <strong>for</strong>ce a number of welfarerecipients off the TANF welfare program.Unless their TANF income is replacedwith wage income, the recipients’ netincome will decrease, <strong>and</strong> their foodstamp allotment will increase. Also,State welfare programs that shift moneyaway from direct cash assistance (tononcash support such as child-carevouchers, transportation subsidies, <strong>and</strong>educational programs) will increase thepressure on the Food Stamp Program.Food stamps are a fairly close substitute<strong>for</strong> cash assistance <strong>and</strong> 100 percentfinanced by the Federal Government.Have State legislatures allowed federallyfinanced food stamp benefits <strong>and</strong> federallysubsidized Medicaid benefits tosubstitute <strong>for</strong> AFDC/TANF? No definitiveestimate of the effect of block grantson State cash welfare expenditures ispossible as yet. A review of literature,however, indicates that ‘‘on averageState governments will reduce overallspending on AFDC/TANF <strong>and</strong> Medicaidby approximately 30 percent.’’ Foodstamp spending would increaseaccordingly.106 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
ConclusionsThe re<strong>for</strong>m of the U.S. welfare systemis having far-reaching effects on theFood Stamp Program. Lower transferpayments lead to reduced expenditureson food, changes in the types of foodconsumed, <strong>and</strong> reduced expenditures onother goods by low-income households.The potential eco<strong>nom</strong>ic effects of thenew welfare legislation on the agriculturalsector <strong>and</strong> the general eco<strong>nom</strong>ydepend on the size of the reduction inbenefits <strong>and</strong> the <strong>for</strong>m of the program.Substantial changes in incentives <strong>and</strong> thestructure of the welfare program willincrease the prominence of the Food StampProgram as a cyclical social safety net.Passage of the PRWORA left the FoodStamp Program as one of the only remainingentitlement programs availableto almost all low-income households.Source: Gundersen, C., LeBlanc, M., <strong>and</strong> Kuhn, B.,1999, The Changing Food Assistance L<strong>and</strong>scape:The Food Stamp Program in a Post-Welfare Re<strong>for</strong>mEnvironment, U.S. Department of Agriculture,<strong>Eco</strong><strong>nom</strong>ic Research Service, Agricultural <strong>Eco</strong><strong>nom</strong>icReport No. 773.1999 Vol. 12 Nos. 3&4 107
Regular ItemsFederal Statist<strong>ics</strong>: Children’s HealthChildren’s health is key to their well-being <strong>and</strong> future development, both of which may be hindered by several factors. Childrenwhose activities are limited by one or more chronic health conditions may need more specialized care than children without suchlimitations. Thus access to health care is important. Children with health insurance coverage (either public or private) are more likelythan children without coverage to have access to health care. Finally, children’s health <strong>and</strong> development depend on a sufficientdiet <strong>and</strong> the ability of the children’s households to have access at all times to enough nourishment <strong>for</strong> an active, healthy life(food security).Most children are in very goodor excellent health according toparents:Parental reports of children’s healthprovide one indicator of children’shealth status. In 1996 most children(81 percent) were reported to be invery good or excellent health. But thesereports of their health status vary byhousehold income. Sixty-five percentof children in families below the povertyline were reported to be in very goodor excellent health, compared with 84percent of children in families livingat or above the poverty line.Percentage of children under age 18 in very good or excellenthealth, 1996Percent90807060504030201008184All children At or above poverty Below poverty65Source: <strong>Center</strong>s <strong>for</strong> Disease Control <strong>and</strong> Prevention, National <strong>Center</strong> <strong>for</strong> Health Statist<strong>ics</strong>,National Health Interview Survey, 1996.Some children, though, are limitedin activity because of health:Distribution of children ages 5 to 17 with any limitation in activityresulting from chronic conditions, 1996In 1996, 6.1 percent of children ages 5to 17 had a limitation in activity resultingfrom chronic health conditions. Theselimitations, reported by the parent, areassociated with chronic health conditions(e.g., asthma, hearing impairment, ordiabetes) that usually last more than3 months. Activities that were limitedinclude going to school, playing, <strong>and</strong>any other activities of children.Source: <strong>Center</strong>s <strong>for</strong> Disease Control <strong>and</strong> Prevention, National <strong>Center</strong> <strong>for</strong> Health Statist<strong>ics</strong>,National Health Interview Survey, 1996.108 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Percentage of children under age 18 without health insurancecoverage, 1998Percent353025201510515.419.73025.2Some children are also withouthealth insurance coverage:Children with health insurance have agreater likelihood of obtaining medicalattention to maintain their well-being.In 1998, 15.4 percent of children underage 18 were without health insurancecoverage. This percentage was higher<strong>for</strong> Black children (19.7 percent),Hispanic children (30 percent) whomay be of any race, <strong>and</strong> children inpoor households (25.2 percent).0All Black Hispanic PoorSource: U.S. Census Bureau, Housing <strong>and</strong> Household <strong>Eco</strong><strong>nom</strong>ic Statist<strong>ics</strong> Division, CurrentPopulation Survey, 1998.Distribution of children under age 18 in households experiencingfood insecurity, 1998Source: U.S. Department of Agriculture, <strong>Eco</strong><strong>nom</strong>ic Research Service <strong>and</strong> Food <strong>and</strong> <strong>Nutrition</strong> Service,1998 Food Security Supplement to the Current Population Survey.And some children are food insecure:Food security includes the ready availabilityof sufficient, nutritionally adequate,<strong>and</strong> safe food <strong>and</strong> the assurance thatfamilies can obtain adequate food withoutrelying on emergency feeding programsor resorting to desperate ef<strong>for</strong>ts to securefood. In 1998 most children under age18 (80.3 percent) resided in householdsthat were defined as food secure. However,14.9 percent of children resided inhouseholds experiencing food insecuritywithout hunger, <strong>and</strong> 4.8 percent resided inhouseholds experiencing food insecuritywith hunger. Food insecure householdsexperiencing hunger report having greaterdifficulty obtaining food <strong>and</strong> decreasedfood intakes.1999 Vol. 12 Nos. 3&4 109
Research <strong>and</strong> Evaluation Activities in USDAFrom the <strong>Eco</strong><strong>nom</strong>icResearch ServiceFood Assistance <strong>and</strong> <strong>Nutrition</strong>Research Small Grants ProgramExecutive Summaries of1998 Research GrantsFood assistance programs----Food Stamps,the Special Supplemental <strong>Nutrition</strong>Program <strong>for</strong> Women, Infants <strong>and</strong> Children(WIC), the school meals programs,<strong>and</strong> others----have been a major componentof public assistance to the poorsince their origins in the 1930’s. Foodassistance <strong>and</strong> nutrition assistance havebecome increasingly important to thesocial safety net as a result of welfarere<strong>for</strong>m. To stimulate new research onthese programs <strong>and</strong> to broaden theparticipation of social science scholarsin food <strong>and</strong> nutrition assistance research,the USDA <strong>Eco</strong><strong>nom</strong>ic Research Service(ERS) partnered with five academicinstitutions <strong>and</strong> research institutes in1998 to establish the Small GrantsProgram <strong>for</strong> Food <strong>and</strong> <strong>Nutrition</strong> AssistanceResearch. ERS <strong>and</strong> the partnerinstitutions competitively award smallgrants <strong>for</strong> 1-year research projects.What follows is a summary compilationof the research findings related tochildren from the first set of smallgrants awarded in the summer <strong>and</strong> fallof 1998. For a listing of all projectsfunded <strong>and</strong> research findings to date,see www.ers.usda.gov.Nativity, Recency of Migration,<strong>and</strong> Legal Status Effects on FoodExpenditures <strong>and</strong> Child Well-beingShawn Malia Kanaiaupuni, Departmentof Sociology, University of Wisconsin<strong>and</strong> Katharine M. Donato, Departmentof Sociology, Louisiana State UniversityRecent years have witnessed growingdebate about the integration prospects ofU.S. immigrants. Widespread attentionhas focused on the costs of immigration,especially in cities that suffered from adeep recession in the late 1980’s. Sincethen, public concern about immigrantsin the U.S. eco<strong>nom</strong>y has led to welfarere<strong>for</strong>m that limited public assistance tolegal immigrants. Some studies reportedthat immigrants imposed costs to U.S.taxpayers through their use of educational<strong>and</strong> welfare services. Steadygrowth in undocumented migrationhas accompanied these changes. By theend of the 1980’s, estimates suggesteda gross inflow of 3.8 million peoplefrom Mexico alone, which representeda substantial increase from the estimated99,000 people two decades earlier.Research has accumulated considerableevidence about the challenges that confrontindividuals with uncertain legalstatus in the United States. Undocumentedhouseholds tend to be poor, often livingbelow established poverty thresholds.Like other immigrants, those withoutdocuments are especially likely to bemedically underserved, uninsured, <strong>and</strong>relying on emergency medical care,all of which increase the risks of preventabledeath. Many are ineligibleor afraid to use public service programsdesigned to help poor families. Yet todate, primar<strong>ily</strong> because of data limitations,we know little about the effects ofundocumented legal status on socialbehavior <strong>and</strong> outcomes.Kanaiaupuni <strong>and</strong> Donato address thisquestion with new data from a longitudinal,bi-national project (Health <strong>and</strong> MigrationSurvey) that surveys households inMexico <strong>and</strong> in the United States. Thedata from this report come from a totalof 262 households r<strong>and</strong>omly chosen intwo neighborhoods, one in Houston <strong>and</strong>the other just north of San Diego. Theyuse these data to examine the healtheffects of legal status, nativity, <strong>and</strong>recency of migration. Because childrenare often the ones who suffer the mostin non-legal households----they areburdened with the fears <strong>and</strong> abilities oftheir parents in addition to overt hostility<strong>and</strong> discrimination from U.S. residents<strong>and</strong> institutions----the authors examinethe effects of household legal status onchild health <strong>and</strong> food security.Kanaiaupuni <strong>and</strong> Donato use multivariateanalysis to predict household foodexpenditures, breastfeeding behavior,current illness, <strong>and</strong> overall health statusof 232 children under age 7 in theirsample, all but 40 of whom are U.S.citizens. Their findings provide furtherevidence of the costs of illegal status <strong>for</strong>immigrants <strong>and</strong> their children: childrenare much better off if both parents havelegal documents----having more food,more income, <strong>and</strong> consequently, betterhealth status. Children with at least oneundocumented parent suffer significanthealth costs. Their chances of poor healthare between three <strong>and</strong> eight times higherthan those of children with legal parents.Results also suggest that the advantagesconferred by legal status are insensitive110 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
to time; net of legal status, children ofrecent immigrants are no healthier thanthose whose parents have lengthier U.S.exposure. The authors anticipate futureresearch that will explore the mechanismsthat contribute to these results. To date,their findings suggest that children livingin undocumented households wouldbenefit from targeted public health, foodassistance, <strong>and</strong> nutrition policies.Effects of Participation in FoodAssistance Programs on Children’sHealth <strong>and</strong> Development: EvidenceFrom NLSY ChildrenLori Kowaleski-Jones, Department of<strong>Fam</strong><strong>ily</strong> <strong>and</strong> Consumer Studies, Universityof Utah <strong>and</strong> Greg J. Duncan, Institute<strong>for</strong> <strong>Policy</strong> Research, NorthwesternUniversityEstablished in 1972, the goal of theSpecial Supplemental <strong>Nutrition</strong> Program<strong>for</strong> Women, Infants, <strong>and</strong> Children (WIC)has been to increase the nutrition level<strong>and</strong> general well-being of children. TheWIC program is currently one of thefastest growing Federal assistance programs.Program expenditures <strong>for</strong> WIChave almost tripled in the past two decades,from $1.3 billion in 1980 to $3.7billion in 1997. Part of the popularityof WIC has been because it is one of themost directly targeted <strong>and</strong> interventionistof the Federal welfare programs. Evaluationsof this program testify to its valuein reducing infant mortality, rates of lowbirthweight, <strong>and</strong> early childhood anemia.However, many WIC program evaluationswere conducted be<strong>for</strong>e 1990,<strong>and</strong> though of high quality, many eitherrelied on data from a single State orcompared results across selected States.More current research is needed toexamine the potential benefits of WICparticipation among a nationally representativesample of women <strong>and</strong> theirchildren.Much of the previous work on the effectsof WIC has focused on infant birth weight,nutrient intakes, presence of anemia,<strong>and</strong> propensity of mothers to breastfeedtheir infants. Because of data limitations,fewer studies have estimated the potentialeffects of WIC participation ondevelopmental infant measures, suchas motor <strong>and</strong> social functioning <strong>and</strong>temperament. This is un<strong>for</strong>tunate becausedevelopmental outcomes are importantpredictors of later childhood social <strong>and</strong>behavioral development.This study investigates the effects ofWIC participation on birth weight, motor<strong>and</strong> social skills, <strong>and</strong> temperament <strong>for</strong> anational sample of children born between1990 <strong>and</strong> 1996 to women from theNational Longitudinal Survey of Youth.The authors use sibling fixed-effectmodels to account <strong>for</strong> potential unmeasuredheterogeneity among the mothersof children in this sample. Ordinary LeastSquare <strong>and</strong> fixed-effect regression resultsconfirm the positive effect of prenatal WICparticipation on infant birth weight foundin other studies. Fixed-effect estimatesalso suggest that prenatal WIC participationis associated with lower scores onmeasures of difficult temperament.Patterns of Food Stamp <strong>and</strong> WICParticipation <strong>and</strong> Their Effects onthe Health of Low-Income ChildrenBon Joo Lee, Lucy Mackey-Bilaver, <strong>and</strong>Robert M. Goerge, Chapin Hall <strong>Center</strong><strong>for</strong> Children, University of ChicagoThe primary purposes of this study areto examine (1) patterns of participationin the Food Stamp Program (FSP) <strong>and</strong>the Special Supplemental <strong>Nutrition</strong>Program <strong>for</strong> Women, Infants, <strong>and</strong>Children (WIC) during the time ofwelfare re<strong>for</strong>m in Illinois; <strong>and</strong> (2) theeffects of WIC on young children’shealth outcomes. The authors use aunique linked data set based on population-leveladministrative data on allbirths, food stamp <strong>and</strong> WIC participation,<strong>and</strong> Medicaid eligibility <strong>and</strong> claims inIllinois between 1990 <strong>and</strong> 1998.Lee et al. estimate that about 65 percentof all children born in Illinois during thestudy period received some combinationof WIC, food stamps, <strong>and</strong> Aid to <strong>Fam</strong>iliesWith Dependent Children/ TemporaryAssistance <strong>for</strong> Needy <strong>Fam</strong>ilies (AFDC/TANF) by age 5. While this overallprogram participation rate changed verylittle across birth cohorts, the authorsfound a considerable shift in participationpatterns across the three programs.As welfare re<strong>for</strong>m was implementedin Illinois, both FSP <strong>and</strong> AFDC/TANFparticipation rates declined substantiallywhile WIC participation rates continuedto increase. Further, most of the decreasein food stamp participation was due todrops in entries to TANF.The authors found some evidence tosuggest that in recent years, familieswith young children are turning moreto WIC to provide essential food items<strong>for</strong> their young children. They also foundthat spells of service receipt <strong>for</strong> bothfood stamps <strong>and</strong> WIC have becomeshorter in recent years, although shorterspells are more noticeable in the FoodStamp Program than in WIC.Two findings relate to the effects of WICon health services <strong>and</strong> outcomes in thisstudy. Lee et al. show first that childrenreceiving WIC are more likely to receivepreventive health care services throughthe Early Periodic Screening, Diagnosis<strong>and</strong> Treatment program (required of StateMedicaid programs through Title XIX1999 Vol. 12 Nos. 3&4 111
of the Social Security Act) than are thosenot receiving WIC. Second, amongchildren enrolled in Medicaid, WICparticipants are significantly less likelyto be diagnosed with health problemsassociated with inadequate nutritionthan are nonparticipants.The Consequences of Food Insecurity<strong>for</strong> Child Well-Being: An Analysisof Children’s School Achievement,Psychological Well-Being, <strong>and</strong> HealthLori Reid, Department of Sociology,Florida State UniversityThe effect of food insecurity on childwell-being has been the subject of muchresearch in developing countries. Witha few exceptions, research on food insecurityin the United States has focusedon examining the causes of food insecurity,potential solutions, <strong>and</strong> more recently,on assessing the incidence of food insecurity.Very little research has attemptedto analyze the effect of food insecurityon child well-being in the United States.Reid uses the 1997 Child DevelopmentSupplement to the Panel Study of IncomeDynam<strong>ics</strong> to examine the effects of foodinsecurity on the school achievement,psychological well-being, <strong>and</strong> healthof children.The analyses provide evidence thatfood insecurity affects a child’s schoolachievement <strong>and</strong> psychological wellbeing.They do not support a hypothesizednegative influence of food insecurityon child health. Reid used children’sassessment scores <strong>for</strong> the letter-word,application, passage comprehension, <strong>and</strong>calculation subtests of the WoodcockJohnson test as measures <strong>for</strong> schoolachievement. She found that foodinsecurity negatively affects children’sscores on the letter-word, passagecomprehension, <strong>and</strong> calculation subtests.Similarly, using indices of external <strong>and</strong>internal behavior problems as measuresof psychological well-being, her resultsshow food insecurity increases the numbersof both external <strong>and</strong> internal behaviorproblems that children exhibit. However,Reid finds no effect of food insecurityon child health when measured byheight-<strong>for</strong>-age <strong>and</strong> weight-<strong>for</strong>-age,indicators often used in developingcountry studies.Influence of Food Stamps on the<strong>Nutrition</strong>al Status of Inner-CityPreschoolers From Hart<strong>for</strong>d, CT,Who Receive WIC BenefitsRafael Perez-Escamilla, Ann M. Ferris,<strong>and</strong> Linda Drake, Department of <strong>Nutrition</strong>alSciences, University of Connecticut<strong>and</strong> Lauren Haldeman, Jessica Peranick,Marcia Campbell, Donna Morgan,Yu-Kuei Peng, Georgine Burke, <strong>and</strong>Bruce A. Bernstein, Hispanic HealthCouncil, Inc., Hart<strong>for</strong>d Hospital,Connecticut Children’s Medical <strong>Center</strong><strong>and</strong> St. Francis HospitalPerez-Escamilla et al. compare the food<strong>and</strong> nutrition situations of low-incomepreschoolers who received food stampswith those who did not. The 100 childrenparticipating in the study were recruitedin the waiting areas of the two largesthospitals in Hart<strong>for</strong>d. The average ageof the sampled children was 2.6 years.Fifty percent were female, <strong>and</strong> 84 percentwere Hispanic. According to their caretakers,all had been enrolled in WIC atsome point in the preceding year, <strong>and</strong>95 percent were receiving WIC benefitsat the time of the study. Groups werecomparable in demographic characterist<strong>ics</strong>,but the socioeco<strong>nom</strong>ic statusof the food stamp group was lower thanthat of the group that did not receivefood stamps.Perez-Escamilla et al. report that amongthe food stamp group in their sample, theaverage monthly food stamp allotmentof $260 represented 96 percent ofmonthly food expenditures. Seventyfourpercent of the households were foodinsecure as measured by the Radimer/Cornell hunger scale. Among those withmonthly household incomes of less than$1,000, food stamp caretakers tended tobe more food secure than non-foodstamp caretakers (77.8 vs. 54.5 percent).Logistic regression results indicate that‘‘How long food stamps last each month’’was positively associated with foodsecurity even after controlling <strong>for</strong> monthlyincome, monthly food stamp allotment,household size, maternal education, <strong>and</strong>vehicle availability. Twenty-four hourrecall data indicate that food stamp preschoolerstended to have higher intakesof iron, zinc, <strong>and</strong> folate than did nonfoodstamp preschoolers. Among thosewith monthly household incomes of lessthan $1,000, food stamp children had asignificantly higher intake of fiber <strong>and</strong>of riboflavin, niacin, pantothenic acid,B6, <strong>and</strong> D vitamins than did non-foodstamp children. Food stamp childrenalso consumed more sodas <strong>and</strong> had ahigher caffeine intake, compared withtheir counterparts.The authors draw four conclusions fromthese results. First, among the very poor,food stamp children live in more foodsecure households. Second, how longfood stamps last is an important determinantof food security. Third, food stampsprovide children with higher intakes ofessential nutrients. Fourth, they concludethat nutrition education is needed tomaximize the nutritional value of foodspurchased with food stamps.112 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Journal AbstractsThe following abstracts are reprinted verbatim as they appear in the cited source.Bartfield, J. 2000. Child support <strong>and</strong>the postdivorce eco<strong>nom</strong>ic well-beingof mothers, fathers, <strong>and</strong> children.Demography 37(2):203-213.This article provides national estimatesof the current <strong>and</strong> potential impact ofprivate child support transfers on theeco<strong>nom</strong>ic well-being of custodial <strong>and</strong>noncustodial families following maritaldissolution. Mothers <strong>and</strong> children faredramatically worse than fathers aftermarital dissolution; these differences,however, would be much more pronouncedin the absence of private childsupport. Simulations of four existingchild support guidelines show thatsubstantial increases in eco<strong>nom</strong>ic wellbeingamong mother-custody familiesare possible within the structure of theexisting child support system, withminimal impact on poverty amongnonresident fathers. Under all of theseguidelines, however, custodial-motherfamilies would continue to fare substantiallyworse than nonresidentfathers.Greene, A.D. <strong>and</strong> Moore, K.A. 1999.Nonresident father involvement <strong>and</strong>child well-being among young childrenin families on welfare (Abstract No.159). In H.E. Peters, R.D. Day, <strong>and</strong>Guest Editors (Eds.) Fatherhood:Research, Interventions <strong>and</strong> Policies,Part I. Marriage & <strong>Fam</strong><strong>ily</strong> Review29(2/3).This study uses early descriptive datafrom the National Evaluation of Welfareto Work Strategies (NEWWS) ChildOutcome Study, a sub-study of thelarger r<strong>and</strong>om assignment evaluationof the Federal JOBS program, to answertwo timely <strong>and</strong> important questions.First, what factors predict father involvementamong nonresident fathersof young children who receive welfare?And second, is nonresident fatherinvolvement associated with betteroutcomes <strong>for</strong> these children? The threemeasures of nonresident father involvementexamined are father-child visitation,<strong>for</strong>mal child support paymentsreceived through the welfare office,<strong>and</strong> in<strong>for</strong>mal child support, such asmoney given directly to the mother,groceries, clothes, or other items.Findings reveal that while only 16.6%of fathers provided child supportthrough the <strong>for</strong>mal system during thepast year, a considerably larger proportion,42.3%, provided in<strong>for</strong>mal childsupport, <strong>and</strong> 67% visited at least oncein the past year. In<strong>for</strong>mal support <strong>and</strong>father-child visitation are the mosthighly correlated <strong>for</strong>ms of involvement,<strong>and</strong> they share many of the same predictors.Only two predictors are significant<strong>and</strong> in the same direction <strong>for</strong> allthree measures of nonresident fatherinvolvement. Father’s residence in thesame state as the focal child <strong>and</strong> theprovision of support <strong>for</strong> the child fromthe father’s fam<strong>ily</strong> are associated witha higher likelihood of his involvement.In general, findings <strong>for</strong> the child wellbeingmeasures show that monetary <strong>and</strong>material contributions from the father,especially contributions providedin<strong>for</strong>mally, are positively associatedwith more positive child well-beingoutcomes.Byrd-Bredbenner, C. <strong>and</strong> Grasso, D.2000. What is television trying tomake children swallow?: Contentanalysis of the nutrition in<strong>for</strong>mationin prime-time advertisements.Journal of <strong>Nutrition</strong> Education32:187-195.The purpose of this study was to identify,content analyze, <strong>and</strong> describe thenutrition-related in<strong>for</strong>mation (NRI) incommercials aired during the top-rated,prime-time network shows viewedheav<strong>ily</strong> by the age 2- to 11-year-oldcategory. A total of 17.5 hours ofprograms were videotaped during fall1998. The NRI in the commercials wascontent analyzed by two researchersusing the instrument developed <strong>for</strong>this study. Nearly one-quarter of thesampled programming (258 minutes)was used <strong>for</strong> commercial time. Of the700 commercials shown, 67% wereadvertisements <strong>for</strong> goods <strong>and</strong> services,32% were promotions <strong>for</strong> upcomingtelevision programs, <strong>and</strong> 1% was publ<strong>ics</strong>ervice announcements. One-third ofthe commercials contained NRI in the<strong>for</strong>m of references that were verbal,written, visual <strong>and</strong>/or that showedpeople eating. NRI was most commonin advertisements <strong>for</strong> products <strong>and</strong>services <strong>and</strong> was present in all productcategories (e.g., electron<strong>ics</strong>, automotive,financial services, foods <strong>and</strong> beverages).Approximately half of the NRI in food<strong>and</strong> beverage advertisements (N = 108)was misleading or inaccurate. The mostfrequently used claim to promote foods<strong>and</strong> beverages was taste; nutrition promotionalclaims were used much lessoften. Television must be recognized1999 Vol. 12 Nos. 3&4 113
as a major source of nutrition (mis)-in<strong>for</strong>mation. An awareness of the NRIon television can help nutrition educatorsaid clients in making food choices morein line with current recommendations.This study’s findings also point to theneed to develop consumer educationprograms that equip individuals of allages with the skills needed to assessthe validity of nutrition in<strong>for</strong>mationpresented via television. In addition, itis clear that nutrition educators need toadvocate <strong>for</strong> more advertisements <strong>for</strong>healthful foods <strong>and</strong> work with advertisersto help them send positive, accuratenutrition messages.Keane, C.R., Lave, J.R., Ricci, E.M.,<strong>and</strong> LaVallee, C.P. 1999. The impactof a children’s health insuranceprogram by age. Pediatr<strong>ics</strong> 104(5):1051-1058.Objectives. 1) To examine age variationin unmet need/delayed care, access,utilization, <strong>and</strong> restricted activitiesattributable to lack of health insurancein children be<strong>for</strong>e they receive healthinsurance; <strong>and</strong> 2) to examine the effectof health insurance on these indicatorswithin each age group of children (inyears).Methods. We use cohort data on childrenbe<strong>for</strong>e <strong>and</strong> after receiving healthinsurance. The study population consistsof 750 children, 0 through 19 yearsof age, newly enrolling in two children’shealth programs. The families of thenewly enrolled children were interviewedat the time of their enrollment(baseline), <strong>and</strong> again at 6 months <strong>and</strong>1 year after enrollment. The dependentvariables measured included access toregular provider, utilization, unmetneed or delayed health care, <strong>and</strong> restrictionson activities attributable to healthinsurance status. All these indicatorvariables were examined by age groups(0-5, 6-10, 11-14, <strong>and</strong> 15-19 years ofage). X 2 tests were per<strong>for</strong>med to determinewhether these dependent variablesvaried by age at baseline.Using logistic regression, odds ratioswere calculated <strong>for</strong> baseline indicatorsby age group of child, adjusting <strong>for</strong>variables commonly found to be associatedwith health insurance status <strong>and</strong>utilization. Changes in indicator variablesfrom be<strong>for</strong>e to after receiving healthinsurance within each age group weredocumented <strong>and</strong> tested using theMcNemar test. A comparison groupof families of children enrolling newly12 months later were interviewed toidentify any potential effects of trend.Results. All ages of children saw statisticallysignificant improvements inaccess, reduced unmet/delayed care,dental utilization, <strong>and</strong> childhoodactivities. Be<strong>for</strong>e obtaining healthinsurance, older children, comparedwith younger children, were morelikely to have had unmet/delayed care,to have not received health care, to havelow access, <strong>and</strong> to have had activitieslimited by their parents. This patternheld <strong>for</strong> all types of care except dentalcare. Age effects were strong <strong>and</strong>independent of covariates. After beingcovered by health insurance, the majorityof the delayed care, low utilization,low access, <strong>and</strong> limited activities in theolder age groups (11-14 <strong>and</strong> 15-19 years)was eliminated. Thus, as levels of unmetneed, delayed care, <strong>and</strong> limitations inactivities approached zero in all agegroups by 1 year after receipt of healthinsurance, age variation in these variableswas eliminated. By contrast, agevariation in utilization remained detectableyet greatly reduced.Conclusion. Health insurance willreduce unmet need, delayed care, <strong>and</strong>restricted childhood activities in all agegroups. Health care professionals <strong>and</strong>policy makers also should be awareof the especially high health care delay,unmet need, <strong>and</strong> restricted activities experiencedby uninsured older children.The new state children’s health insuranceprograms offer the potential to eliminatethese problems. Realization of thispotential requires that enrollmentcriteria, outreach strategies, <strong>and</strong> deliverysystems be effectively fashioned sothat all ages of children are enrolledin health insurance.Rank, M.R. <strong>and</strong> Hirschl, T.A. 1999.The eco<strong>nom</strong>ic risk of childhood inAmerica: Estimating the probabilityof poverty across the <strong>for</strong>mative years.Journal of Marriage <strong>and</strong> the <strong>Fam</strong><strong>ily</strong>61(4):1058-1067.This article estimates the proportionof children in the United States whowill experience poverty at some pointduring their childhood. These proportionsare derived through a set of lifetables built from 25 waves of longitudinaldata. They represent a fundamentallydifferent approach to studyingpoverty than either a cross-sectionalor poverty spell methodology. Ourdata indicate that between the ages of1 year <strong>and</strong> 17 years, 34% of Americanchildren will spend at least 1 year belowthe poverty line, 40% will experiencepoverty at the 125% level, <strong>and</strong> 18%will face extreme poverty (below 50%of the poverty line). A series of bivariate<strong>and</strong> multivariate life tables reveal thatrace, fam<strong>ily</strong> structure, <strong>and</strong> parentaleducation all have a sizeable impact onthe likelihood of experiencing poverty.During the 17 years of childhood, 69%of Black children, 81% of children innonmarried households, <strong>and</strong> 63% ofchildren whose head of household hadfewer than 12 years of education willbe touched by poverty.114 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Official USDA Food Plans: Cost of Food at Home at Four Levels,U.S. Average, June 2000 1WEEKLY COSTMONTHLY COSTAGE-GENDERGROUPSThriftyplanLow-costplanModeratecostplanLiberalplanThriftyplanLow-costplanModeratecostplanLiberalplanINDIVIDUALS 2CHILD:1 year $15.70 $19.20 $22.60 $27.40 $68.00 $83.20 $97.90 $118.702 years 15.70 19.20 22.60 27.40 68.00 83.20 97.90 118.703-5 years 17.00 21.10 26.10 31.30 73.70 91.40 113.10 135.606-8 years 21.00 28.10 35.00 40.70 91.00 121.80 151.70 176.409-11 years 25.00 31.80 40.80 47.20 108.30 137.80 176.80 204.50MALE:12-14 years 25.80 36.00 44.70 52.60 111.80 156.00 193.70 227.9015-19 years 26.50 37.20 46.30 53.50 114.80 161.20 200.60 231.8020-50 years 28.40 36.90 46.10 55.90 123.10 159.90 199.80 242.2051 years <strong>and</strong> over 25.70 35.20 43.30 52.00 111.40 152.50 187.60 225.30FEMALE:12-19 years 25.90 31.00 37.80 45.60 112.20 134.30 163.80 197.6020-50 years 25.80 32.30 39.40 50.50 111.80 140.00 170.70 218.8051 years <strong>and</strong> over 25.30 31.40 39.00 46.60 109.60 136.10 169.00 201.90FAMILIES:FAMILY of 2 3 :20-50 years 59.60 76.10 94.10 117.00 258.40 329.90 407.60 507.1051 years <strong>and</strong> over 56.10 73.30 90.50 108.50 243.10 317.50 392.30 469.90FAMILY OF 4:Couple, 20-50 years <strong>and</strong>children----1-2 <strong>and</strong> 3-5 years 86.90 109.50 134.20 165.10 376.60 474.50 581.50 715.306-8 <strong>and</strong> 9-11 years 100.20 129.10 161.30 194.30 434.20 559.50 699.00 841.901 Basis is that all meals <strong>and</strong> snacks are purchased at stores <strong>and</strong> prepared at home. For specific foods <strong>and</strong> quantities of foods in the Low-Cost,Moderate-Cost, <strong>and</strong> Liberal Plans, see <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> Review, No. 2 (1983); <strong>for</strong> specific foods <strong>and</strong> quantities of foods in the ThriftyFood Plan, see Thrifty Food Plan, 1999, Executive Summary, CNPP-7A. The Thrifty Food Plan is based on 1989-91 data, <strong>and</strong> the otherthree food plans are based on 1977-78 data updated to current dollars using the Consumer Price Index <strong>for</strong> specific food items.2 The costs given are <strong>for</strong> individuals in 4-person families. For individuals in other size families, the following adjustments are suggested:1-person----add 20 percent; 2-person----add 10 percent; 3-person----add 5 percent; 5- or 6-person----subtract 5 percent; 7- (or more) person----subtract 10 percent.3 Ten percent added <strong>for</strong> fam<strong>ily</strong> size adjustment.1999 Vol. 12 Nos. 3&4 115
Consumer PricesAverage percent change <strong>for</strong> major budgetary componentsAnnual average percent change fromDecember of previous year to December:Percent change12 months endingGROUP 1990 1995 1999 with June 2000All Items 6.1 2.5 2.7 3.7Food 5.3 2.1 1.9 2.3Food at home 5.8 2.0 1.7 2.2Food away from home 4.5 2.2 2.3 2.4Housing 4.5 3.0 2.2 3.2Apparel 5.1 0.1 -0.5 -2.0Transportation 10.4 1.5 5.4 8.6Medical care 9.6 3.9 3.7 4.1Recreation NA 2.8 0.8 1.2Education <strong>and</strong> communication NA 4.0 1.6 1.2Other goods <strong>and</strong> services 7.6 4.3 5.1 5.4Price per pound <strong>for</strong> selected food itemsPrice per pound unless otherwise noted (as of December in each year) JuneFood 1990 1995 1999 2000Flour, white, all purpose $ .24 $ .24 $ .27 $ .31Rice, white, long grain, uncooked .49 .55 .50 NASpaghetti <strong>and</strong> macaroni .85 .88 .88 .83Bread, white .70 .84 .90 .92Beef, ground, uncooked 1.63 1.40 1.53 1.56Pork chops, center cut, bone-in 3.32 3.29 3.21 3.33Chicken, fresh, whole .86 .94 1.05 1.07Tuna, light, chunk 2.11 2.00 2.03 1.95Eggs, Grade A, large, per dozen 1.00 1.16 .92 .84Milk, fresh, lowfat, per gallon NA 2.31 2.83 2.64Butter, salted, grade AA, stick 1.92 1.73 2.27 2.53Apples, red delicious .77 .83 .92 .92Bananas .43 .45 .49 .51Oranges, navel .56 .64 .64 .70Potatoes, white .32 .38 .39 .38Lettuce, iceberg .58 .61 .67 .69Tomatoes, field grown .86 1.51 1.41 1.32Broccoli NA .76 1.00 1.24Carrots, short trimmed <strong>and</strong> topped .43 .53 .52 .59Onions, dry yellow NA .41 NA NAOrange juice, frozen concentrate per 16 oz. 2.02 1.57 1.82 1.80Sugar, white, 33-80 oz. pkg. .40 .39 .41 .41Margarine, stick .87 .79 NA NAPeanut butter, creamy 2.09 1.78 1.86 1.89Coffee, 100% ground roast 2.94 3.51 3.35 3.43NA = Data not available.Selected items from CPI Detailed Reports, Bureau of Labor Statist<strong>ics</strong>, various issues. Price changes are <strong>for</strong> all urban consumers. Food pricesare U.S. city average.116 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
U.S. Poverty ThresholdsWeighted average poverty thresholds 1 <strong>for</strong> nonfarm families of specified size, 1975-99<strong>Fam</strong>ilies of 2 persons or moreUnrelated individuals2 personsCalendaryearAllagesUnderage 65Age 65or olderAll agesHouseholderunderage 65Householderage 65or older3persons4persons5persons6personsAnnual averageCPI, all items(1982-84 = 100)1975 $2,724 $2,797 $2,581 $3,506 $3,617 $3,257 $4,293 $5,500 $6,499 $7,316 53.81976 2,884 2,959 2,730 3,711 3,826 3,445 4,540 5,815 6,876 7,760 56.91977 3,075 3,152 2,906 3,951 4,072 3,666 4,833 6,191 7,320 8,261 60.61978 3,311 3,392 3,127 4,249 4,383 3,944 5,201 6,662 7,880 8,891 65.21979 3,689 3,778 3,479 4,725 4,878 4,390 5,784 7,412 8,775 9,914 72.61980 4,190 4,290 3,949 5,363 5,537 4,983 6,565 8,414 9,966 11,269 82.41981 4,620 4,729 4,359 5,917 6,111 5,498 7,250 9,287 11,007 12,449 90.91982 4,901 5,019 4,626 6,281 6,487 5,836 7,693 9,862 11,684 13,207 96.51983 5,061 5,180 4,775 6,483 6,697 6,023 7,938 10,178 12,049 13,630 99.61984 5,278 5,400 4,979 6,762 6,983 6,282 8,277 10,609 12,566 14,207 103.91985 5,469 5,593 5,156 6,998 7,231 6,503 8,573 10,989 13,007 14,696 107.61986 5,572 5,701 5,255 7,138 7,372 6,630 8,737 11,203 13,259 14,986 109.61987 5,778 5,909 5,447 7,397 7,641 6,872 9,056 11,611 13,737 15,509 113.61988 6,024 6,155 5,674 7,704 7,958 7,158 9,435 12,092 14,305 16,149 118.31989 6,311 6,451 5,947 8,076 8,343 7,501 9,885 12,675 14,990 16,921 124.01990 6,652 6,800 6,268 8,512 8,794 7,906 10,419 13,360 15,800 17,835 130.71991 6,932 7,086 6,532 8,867 9,164 8,238 10,857 13,921 16,457 18,590 136.21992 7,141 7,299 6,729 9,132 9,441 8,489 11,187 14,343 16,951 19,146 140.31993 7,357 7,517 6,930 9,410 9,726 8,741 11,521 14,764 17,459 19,710 144.51994 7,551 7,710 7,107 9,655 9,977 8,964 11,817 15,141 17,896 20,223 148.21995 7,761 7,929 7,309 9,935 10,259 9,221 12,156 15,570 18,407 20,808 152.41996 7,992 8,163 7,525 10,226 10,562 9,491 12,517 16,029 18,951 21,418 156.91997 8,178 8,350 7,698 10,468 10,806 9,709 12,803 16,404 19,387 21,880 160.51998 8,310 8,480 7,818 10,636 10,973 9,863 13,001 16,655 19,682 22,227 163.01999 2 8,500 8,667 7,991 10,869 11,214 10,080 13,290 17,028 20,115 22,719 166.61 The poverty thresholds are used by the Bureau of the Census to prepare its statistical estimates of the number of individuals <strong>and</strong> families in poverty.The poverty guidelines are a simplified version of these poverty thresholds <strong>and</strong> are issued by the U.S. Department of Health <strong>and</strong> Human Services<strong>for</strong> administrative purposes. The poverty guidelines are used to determine whether a person or fam<strong>ily</strong> is financially eligible <strong>for</strong> assistance or services undera particular Federal program.2 These average poverty thresholds were derived by increasing the 1998 thresholds by a factor of 1.022086, which reflects the percent change in theaverage annual Consumer Price Index (CPI-U) between 1998 <strong>and</strong> 1999.1999 Vol. 12 Nos. 3&4 117
Index of Authors in 1999 IssuesAuthor Article Title Issue No. Page No.Abdel-Ghany, Mohamed Identifying the Poor <strong>and</strong> Their Consumption Patterns 2 15An<strong>and</strong>, RajenCruciferous Vegetables <strong>and</strong> Human Breast Cancer:An Important Interdisciplinary Hypothesis in the Fieldof Diet <strong>and</strong> Cancer 2 26An<strong>and</strong>, Rajen S. Report Card on the Diet Quality of Children 3/4 78An<strong>and</strong>, Rajen S. Eating Breakfast Greatly Improves Schoolchildren’s Diet Quality 3/4 81Basiotis, P. Peter Report Card on the Diet Quality of Children 3/4 78Basiotis, P. Peter Eating Breakfast Greatly Improves Schoolchildren’s Diet Quality 3/4 81Bente, Lisa Household Expenditures on Vitamins <strong>and</strong> Minerals by Income Level 2 39Biedebach, MarkCruciferous Vegetables <strong>and</strong> Human Breast Cancer: An ImportantInterdisciplinary Hypothesis in the Field of Diet <strong>and</strong> Cancer 2 26Bowman, Shanthy A. Diets of Individuals Based on Energy Intakes From Added Sugars 2 31Dinkins, Julia M. Household Expenditures on Vitamins <strong>and</strong> Minerals by Income Level 2 39Escobar, Alyson Factors Influencing Children’s Dietary Practices: A Review 3/4 45Escobar, Alyson Are All Food Pyramids Created Equal? 3/4 75Gates, Gail E. Folate Intake <strong>and</strong> Supplement Use in Women of Childbearing Age 1 14Gerrior, ShirleyTrends in Availability of Foods <strong>and</strong> Nutrients: A ComparisonBetween the United States <strong>and</strong> Italy, 1961-92 1 26Gerrior, Shirley A. Dietary Changes in Older Americans From 1977 to 1996:Implications <strong>for</strong> Dietary Quality 2 3Gerrior, Shirley A. Report Card on the Diet Quality of Children 3/4 78Holmes, Tawni W. Folate Intake <strong>and</strong> Supplement Use in Women of Childbearing Age 1 14Jevning, RonCruciferous Vegetables <strong>and</strong> Human Breast Cancer: An ImportantInterdisciplinary Hypothesis in the Field of Diet <strong>and</strong> Cancer 2 26Kendall, Anne<strong>Nutrition</strong> <strong>and</strong> Dairy Industry Benefits Associated WithPromoting Lowfat Milk: Evidence From the 1989 CSFII 1 3Khan, Laura Kettel<strong>Nutrition</strong> <strong>and</strong> Dairy Industry Benefits Associated WithPromoting Lowfat Milk: Evidence From the 1989 CSFII 1 3Lino, Mark Household Expenditures on Vitamins <strong>and</strong> Minerals by Income Level 2 39Lino, Mark Expenditures on Children by <strong>Fam</strong>ilies, 1999 3/4 56Lino, Mark Report Card on the Diet Quality of Children 3/4 78Lino, Mark Eating Breakfast Greatly Improves Schoolchildren’s Diet Quality 3/4 81Marcoe, Kristin L. Technical Research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> Young Children 3/4 18Mathios, Alan<strong>Nutrition</strong> <strong>and</strong> Dairy Industry Benefits Associated WithPromoting Lowfat Milk: Evidence From the 1989 CSFII 1 3Nayga Jr., Rodolfo M. Factors Associated With the Intake of Dietary Supplements 1 43Pelletier, David L.<strong>Nutrition</strong> <strong>and</strong> Dairy Industry Benefits Associated WithPromoting Lowfat Milk: Evidence From the 1989 CSFII 1 3Reed, Debra B. Factors Associated With the Intake of Dietary Supplements 1 43Saltos, EttaAdapting the Food Guide Pyramid <strong>for</strong> Children: Defining theTarget Audience 3/4 3Sharpe, Deanna L. Identifying the Poor <strong>and</strong> Their Consumption Patterns 2 15Tarone, Catherine Consumer Research: Food Guide Pyramid <strong>for</strong> Young Children 3/4 33Zizza, ClaireTrends in Availability of Foods <strong>and</strong> Nutrients: A ComparisonBetween the United States <strong>and</strong> Italy, 1961-92 1 26118 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Index of Articles in 1999 IssuesIssue No.Page No.Food <strong>and</strong> <strong>Nutrition</strong><strong>Nutrition</strong> <strong>and</strong> Dairy Industry Benefits Associated With Promoting Lowfat Milk:Evidence From the 1989 CSFII 1 3Folate Intake <strong>and</strong> Supplement Use in Women of Childbearing Age 1 14Trends in Availability of Foods <strong>and</strong> Nutrients: A Comparison Between the United States <strong>and</strong> Italy, 1961-92 1 26Factors Associated With the Intake of Dietary Supplements 1 43The Diet Quality of Americans: Strong Link With <strong>Nutrition</strong> Knowledge 1 49Dietary Changes in Older Americans From 1977 to 1996: Implications <strong>for</strong> Dietary Quality 2 3Diets of Individuals Based on Energy Intakes From Added Sugars 2 31The Diet Quality of American Indians: Evidence From the Continuing Survey of Food Intakesby Individuals 2 44Factors Influencing Children’s Dietary Practices: A Review 3/4 45Technical Research <strong>for</strong> the Food Guide Pyramid <strong>for</strong> Young Children 3/4 18Consumer Research: Food Guide Pyramid <strong>for</strong> Young Children 3/4 33Adapting the Food Guide Pyramid <strong>for</strong> Young Children: Defining the Target Audience 3/4 3Are All Food Pyramids Created Equal? 3/4 75Report Card on the Diet Quality of Children 3/4 78Eating Breakfast Greatly Improves Schoolchildren’s Diet Quality 3/4 81*Contribution of Away-From-Home Foods to American Diet Quality 3/4 85Expenditures <strong>and</strong> <strong>Eco</strong><strong>nom</strong>ic Status*Earnings of Husb<strong>and</strong>s <strong>and</strong> Wives in Dual-Earner <strong>Fam</strong>ilies 1 54*Retirement Prospects of Baby Boomers 1 56Identifying the Poor <strong>and</strong> Their Consumption Patterns 2 15Household Expenditures on Vitamins <strong>and</strong> Minerals by Income Level 2 39*Supplemental Security Income Program Participation by Noncitizens 2 47*Who Gained the Most During the 1990’s Expansion? 2 55*The Food-at-Home Budget: Changes Between 1980 <strong>and</strong> 1992 2 57Expenditures on Children by <strong>Fam</strong>ilies, 1999 3/4 56*Access to Supermarkets <strong>and</strong> Large Grocery Stores by the Rural Poor 3/4 90*Poverty <strong>and</strong> Well-Being in Rural America 3/4 93*Alternative Employment Arrangements 3/4 96*The Food Stamp Program After Welfare Re<strong>for</strong>m 3/4 104HealthFacts About Childhood Obesity <strong>and</strong> Overweightness 1 52*Clinical Guidelines: Identification, Evaluation, <strong>and</strong> Treatment of Overweight <strong>and</strong> Obesity in Adults 1 59Cruciferous Vegetables <strong>and</strong> Human Breast Cancer: An Important InterdisciplinaryHypothesis in the Field of Diet <strong>and</strong> Cancer 2 26*A Dietary Assessment of the U.S. Food Supply 2 51*Factors Affecting Nutrient Intake of the Elderly 3/4 1011999 Vol. 12 Nos. 3&4 119
<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Reviewgratefully acknowledges the reviewers of manuscripts <strong>for</strong> 1999 issues.Jane Allshouse<strong>Eco</strong><strong>nom</strong>ic Research ServiceU.S. Department of AgricultureShanthy BowmanAgricultural Research ServiceU.S. Department of AgricultureKaren M. Chapman-NovakofskiUniversity of IllinoisCecilia EnnsAgricultural Research ServiceU.S. Department of AgricultureNancy ErnstNational Institutes of HealthLesley Fels TinkerFred Hutchinson Cancer Research <strong>Center</strong>Pamela S. HainesThe University of North Carolina at Chapel HillPatricia HammerschmidtMichigan State UniversityLisa HarnackUniversity of MinnesotaAnn HertzlerVirginia Polytechnic Institute & State UniversityKatrina A. HoltGeorgetown UniversityJoyce JonesKansas State UniversityPhillip R. Kaufman<strong>Eco</strong><strong>nom</strong>ic Research ServiceU.S. Department of AgricultureRuth KavaAmerican Council on Science & HealthSue Krebs-SmithNational Cancer InstituteMichele LawlerMaternal <strong>and</strong> Child Health BureauCalvin McCausl<strong>and</strong>Enrich International, Inc.Sharon MickleAgricultural Research ServiceU.S. Department of AgricultureRodolfo M. Nayga Jr.Texas A&M UniversityJames P. O’HalloranNeurocomp SystemsCarol Ol<strong>and</strong>erFood <strong>and</strong> <strong>Nutrition</strong> ServiceU.S. Department of AgricultureJohn ParkCornell UniversityBill PasseroBureau of Labor Statist<strong>ics</strong>U.S. Department of LaborJean PenningtonNational Institutes of HealthBarry PopkinThe University of North Carolina at Chapel HillJeanie RaderU.S. Food <strong>and</strong> Drug AdministrationJean SkinnerUniversity of TennesseeJanice StuffARS Children’s <strong>Nutrition</strong> Research <strong>Center</strong>U.S. Department of AgricultureKatherine SykesAgricultural Research ServiceU.S. Department of AgricultureSusan WelshCooperative State Research, Education, <strong>and</strong> Extension ServiceU.S. Department of AgricultureWells WillisCooperative State Research, Education, <strong>and</strong> Extension ServiceU.S. Department of AgricultureBrenda LisiMaternal <strong>and</strong> Child Health Bureau120 <strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review
Guidelines <strong>for</strong> Authors<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> Review is a peer-reviewed quarterly journalpublished by the <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>; Food, <strong>Nutrition</strong>, <strong>and</strong>Consumer Services; U.S. Department of Agriculture.• All manuscripts must follow the guidelines of Publication Manual of theAmerican Psychological Association, 4th Edition.• The manuscript text <strong>for</strong> feature articles, including references, abstract (lessthan 150 words), tables, <strong>and</strong> figures, is limited to 30 pages. Include a separatetitle page with author’s full name, title, affiliation, full address, <strong>and</strong> telephone number.• The manuscript text <strong>for</strong> research briefs, including references, tables, <strong>and</strong> figures,is limited to 10 pages. No abstract is required.• Include tables or figures only if they are necessary to underst<strong>and</strong> or clarify thepaper. No more than six figures <strong>and</strong>/or tables will be published with an article,<strong>and</strong> no more than three will be published with a research brief.• Manuscripts may not be submitted elsewhere while under consideration by thejournal.• All authors <strong>and</strong> coauthors must sign a release acknowledging that contents ofthe journal are in the public domain.• Upon acceptance of articles, authors must send the revised manuscript oncomputer disk, along with two hard (paper) copies. WordPerfect is the preferredword-processing program.• Please send four copies to the editor:Julia M. Dinkins, PhD<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> ReviewUSDA, <strong>Center</strong> <strong>for</strong> <strong>Nutrition</strong> <strong>Policy</strong> <strong>and</strong> <strong>Promotion</strong>1120 20th Street NW, Suite 200 North LobbyWashington, DC 20036-3406(202) 606-4876
<strong>Fam</strong><strong>ily</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong> <strong>and</strong> <strong>Nutrition</strong> ReviewEdi to rial BoardCheryl Achter berg Alan S. LevyThe Schreyer Honors Col lege Cen ter <strong>for</strong> Food Safety <strong>and</strong> Ap plied <strong>Nutrition</strong>The Penn syl va nia State Uni ver sity U.S. Food <strong>and</strong> Drug Ad min istra tionRonette BriefelMathe matica Pol icy Re search, Inc.Robin DouthittDe part ment of Con sumer SciencesUni ver sity of Wisconsin- MadisonDavid B. EastwoodDe part ment of Ag ri cul tural <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong><strong>and</strong> Ru ral SociologyUni ver sity of TennesseeSuzanne MurphyCan cer Re search Cen ter of HawaiiUni ver sity of HawaiiRodolfo NaygaDe part ment of Ag ri cul tural <strong>Eco</strong><strong>nom</strong><strong>ics</strong>Texas A&M UniversityJane SchuchardtRe search, Edu ca tion, <strong>and</strong> <strong>Eco</strong><strong>nom</strong><strong>ics</strong>U.S. De part ment of Ag ri cul tureJay Hirschman David SmallwoodFood <strong>and</strong> Nu tri tion Serv ice <strong>Eco</strong> <strong>nom</strong>ic Re search Serv iceU.S. De part ment of Ag ri cul ture U.S. De part ment of Ag ri cul tureEileen Kennedy Wells Wil lisRe search, Edu ca tion, <strong>and</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong> Re search, Edu ca tion, <strong>and</strong> <strong>Eco</strong> <strong>nom</strong> <strong>ics</strong>U.S. De part ment of Ag ri cul ture U.S. De part ment of Ag ri cul tureJoyce Jones<strong>Fam</strong> <strong>ily</strong> Stud ies <strong>and</strong> Hu man ServicesKan sas State University