Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
The <strong>EWMA</strong> Journal<br />
ISSN number: 1609-2759<br />
Volume 7, No 2, May, 2007<br />
The Journal of the European<br />
Wound Management Association<br />
Published three times a year<br />
Editorial Board<br />
Carol Dealey, Editor<br />
Sue Bale<br />
Michelle Briggs<br />
Peter Franks<br />
Finn Gottrup<br />
E. Andrea Nelson<br />
Zbigniew Rybak<br />
Peter Vowden<br />
<strong>EWMA</strong> web site<br />
www.ewma.org<br />
For membership application,<br />
correspondence,<br />
prospective publications<br />
and advertising<br />
please contact:<br />
<strong>EWMA</strong> Business Office<br />
Congress Consultants<br />
Martensens Allé 8<br />
1828 Frederiksberg C · Denmark.<br />
Tel: (+45) 7020 0305<br />
Fax: (+45) 7020 0315<br />
ewma@ewma.org<br />
Layout:<br />
Birgitte Clematide<br />
Printed by:<br />
Kailow Graphic A/S, Denmark<br />
Copies printed: 13,000<br />
Prices:<br />
Distributed free of charge to members of<br />
the European Wound Management<br />
Association and members<br />
of co-operating associations.<br />
Individual subscription per issue: 7.50€<br />
Libraries and institutions per issue: 25€<br />
The next issue will be published<br />
October 2007.<br />
Prospective material for publication<br />
must be with the editors<br />
as soon as possible and<br />
no later than 15 July 2007<br />
The contents of articles and letters in<br />
<strong>EWMA</strong> Journal do not necessarily<br />
reflect the opinions of the Editors<br />
or the European Wound<br />
Management Association.<br />
Copyright of all published material<br />
and illustrations is the property of<br />
the European Wound Management<br />
Association. However, provided prior<br />
written consent for their reproduction<br />
obtained from both the Author and<br />
<strong>EWMA</strong> via the Editorial Board of the<br />
Journal, and proper acknowledgement<br />
and printed, such permission will<br />
normally be readily granted.<br />
Requests to reproduce material<br />
should state where material is to<br />
be published, and, if it is abstracted,<br />
summarised, or abbreviated, then<br />
the proposed new text should be sent<br />
to the <strong>EWMA</strong> Journal Editor<br />
for final approval.<br />
Finn Gottrup<br />
Recorder<br />
Judit Daróczy<br />
Christina Lindholm<br />
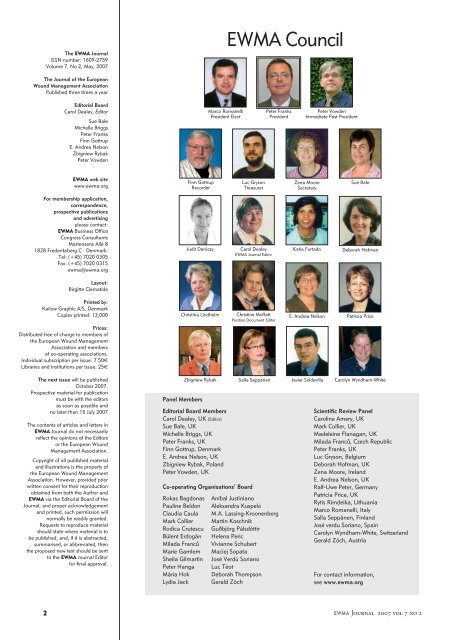
<strong>EWMA</strong> <strong>Council</strong><br />
Zbigniew Rybak Salla Seppänen Javier Soldevilla Carolyn Wyndham-White<br />
Panel Members<br />
Editorial Board Members<br />
Carol Dealey, UK (Editor)<br />
Sue Bale, UK<br />
Michelle Briggs, UK<br />
Peter Franks, UK<br />
Finn Gottrup, Denmark<br />
E. Andrea Nelson, UK<br />
Zbigniew Rybak, Poland<br />
Peter Vowden, UK<br />
Co-operating Organisations’ Board<br />
Rokas Bagdonas<br />
Pauline Beldon<br />
Claudia Caula<br />
Mark Collier<br />
Rodica Crutescu<br />
Bülent Erdogăn<br />
Milada Francu˚<br />
Marie Gamlem<br />
Sheila Gilmartin<br />
Peter Hanga<br />
Mária Hok<br />
Lydia Jack<br />
Marco Romanelli<br />
President Elect<br />
Luc Gryson<br />
Treasurer<br />
Carol Dealey<br />
<strong>EWMA</strong> Journal Editor<br />
Christine Moffatt<br />
Position Document Editor<br />
Peter Franks<br />
President<br />
Aníbal Justiniano<br />
Aleksandra Kuspelo<br />
M.A. Lassing-Kroonenberg<br />
Martin Koschnik<br />
Guðbjörg Pálsdóttir<br />
Helena Peric<br />
Vivianne Schubert<br />
Maciej Sopata<br />
José Verdú Soriano<br />
Luc Tèot<br />
Deborah Thompson<br />
Gerald Zöch<br />
Peter Vowden<br />
Immediate Past President<br />
Zena Moore<br />
Secretary<br />
Katia Furtado<br />
Sue Bale<br />
Deborah Hofman<br />
E. Andrea Nelson Patricia Price<br />
Scientific Review Panel<br />
Caroline Amery, UK<br />
Mark Collier, UK<br />
Madeleine Flanagan, UK<br />
Milada Francu˚, Czech Republic<br />
Peter Franks, UK<br />
Luc Gryson, Belgium<br />
Deborah Hofman, UK<br />
Zena Moore, Ireland<br />
E. Andrea Nelson, UK<br />
Ralf-Uwe Peter, Germany<br />
Patricia Price, UK<br />
Rytis Rimdeika, Lithuania<br />
Marco Romanelli, Italy<br />
Salla Seppänen, Finland<br />
José verdu Soriano, Spain<br />
Carolyn Wyndham-White, Switzerland<br />
Gerald Zöch, Austria<br />
For contact information,<br />
see www.ewma.org<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
3 Editorial<br />
Peter J Franks<br />
Scientific Articles<br />
7 Is it safe to use saline solution to clean wounds?<br />
João Carlos Gouveia, Christina Miguens<br />
15 The cost of pressure ulceration<br />
Peter J Franks<br />
21 Epidemiology of wounds treated in<br />
Community Services in Portugal<br />
Elaine Pina<br />
29 Improving wound assessment through<br />
the provision of digital cameras across<br />
a Primary Care Trust<br />
Alison Hopkins<br />
Background Articles<br />
35 The use of telemedicine in wound care<br />
Rolf Jelnes<br />
39 Lord Joseph Lister: the rise of antiseptic<br />
surgery and the modern place of antiseptics<br />
in wound care<br />
David Leaper<br />
EBWM<br />
44 Abstracts of recent Cochrane Reviews<br />
Sally Bell-Syer<br />
<strong>EWMA</strong><br />
48 <strong>EWMA</strong> Position Document 2007:<br />
Topical Negative Pressure in Wound<br />
Management<br />
Christine Moffatt<br />
50 <strong>EWMA</strong> Journal previous issues<br />
50 International Journals<br />
52 <strong>EWMA</strong> Corporate Sponsors contact data<br />
Conferences<br />
54 Conference calendar<br />
Organisations<br />
55 The XIth Finnish National Wound Management<br />
Conference, 1-2 February 2007 in Helsinki<br />
Salla Seppänen<br />
56 The SSiS is an association for registered nurses<br />
with a professional interest in wounds<br />
Christina Lindholm<br />
57 What’s new in Slovenia?<br />
Helena Kristina Peric<br />
58 Co-operating Organisations<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
<strong>EWMA</strong><br />
is more than a conference<br />
As my time as president comes to a close I wish to reflect back on<br />
my time, to see where <strong>EWMA</strong> has come from and to look to the<br />
future of <strong>EWMA</strong> and its activities.<br />
For those who may not be familiar with the history of the organisation,<br />
<strong>EWMA</strong> was founded at a meeting in Cardiff in 1991, “to promote advancement<br />
of education and research into native epidemiology, pathology,<br />
diagnosis, prevention and management of wounds of all aetiologies”. For<br />
the first 10 years, it undertook an annual meeting held each year mainly<br />
in Harrogate, organised by Macmillan (then EMAP). However in 2000,<br />
we had the opportunity of developing our own way forward. The <strong>EWMA</strong><br />
<strong>Council</strong> elected to work to develop their own meetings, and contracted<br />
Congress Consultants to organize our meetings, starting in Stockholm.<br />
While this was a time of great change, the model we now have has become<br />
so robust that other societies are adopting many of the innovations<br />
developed since that time. It is a great testimony to the past presidents,<br />
<strong>Council</strong> members and other supporters that <strong>EWMA</strong> is the organization<br />
it is today.<br />
It is difficult to identify all the innovations that have taken place, but one<br />
of the areas that deserve specific mention is the development of the Cooperating<br />
Organizations which currently number 38 national organizations<br />
in 29 countries. Indeed <strong>EWMA</strong> has been instrumental in helping to<br />
establish wound organizations in countries that previously did not have<br />
one. <strong>EWMA</strong> today is widely acknowledged as the umbrella organization<br />
that brings together these organizations and represents them on a European<br />
level. We will be seeking to develop this representation further with<br />
closer ties with Eucomed, an organization that represents the wound care<br />
industry in the EU.<br />
Other developments of note include the <strong>EWMA</strong> publications. The <strong>EWMA</strong><br />
Journal is now in its seventh year, and provides an opportunity to present<br />
original research as well as reports from the national societies. It is a testament<br />
to Carol Dealey and her team that the journal is now indexed in<br />
CINAHL. Interest in <strong>EWMA</strong> journal has never been higher and we receive<br />
many approaches from companies, authors and even publishing houses,<br />
who are interested in publishing <strong>EWMA</strong> Journal.<br />
Our other voice is through the Position Documents. The original concept<br />
of Christine Moffatt, these papers have set a high standard and achieved<br />
�
international recognition as reference documents for key issues in wound<br />
management. We are particularly pleased that they are free to access through<br />
the <strong>EWMA</strong> website and are in five major European languages (English,<br />
French, Italian, Spanish & German). While budgetary issues prevent us<br />
from translating them into other languages we do allow all national societies<br />
the opportunity to translate them into their own languages for free<br />
(subject to permission). Please contact <strong>EWMA</strong> Business Office (ewma@<br />
ewma.org) for more information.<br />
Another area of rapid development has been through the Educational<br />
Panel, originally led by Madeleine Flanagan and Finn Gottrup, now led by<br />
Zena Moore. There are many wound care courses undertaken throughout<br />
Europe, with a range of quality. The Educational Panel has developed<br />
<strong>EWMA</strong> curriculum frameworks by which these courses can be compared.<br />
Provided the courses fit the framework, <strong>EWMA</strong> can endorse the wound<br />
care course. Other innovations include the development of a University<br />
module to run in parallel with the <strong>EWMA</strong> meetings, and a Teach the<br />
Teacher project.<br />
For my part, I have developed an interest in supporting societies in developing<br />
evidence to support quality improvements in the care they can<br />
provide to patients. The Central and East European Leg Ulcer project<br />
aims to examine how models of implementation can be used to provide<br />
evidence that can justify the application of evidenced based care to patients.<br />
The study in Poland, the Czech Republic and Slovenia will give the much<br />
needed evidence to justify appropriate education, organization and access<br />
to modern wound care products that Governments require in order to justify<br />
their adoption. It is hoped that this could be a model for other wound<br />
aetiologies and countries to adopt to develop their services further.<br />
As I am about to hand over the presidency to Marco Romanelli, I hope that<br />
<strong>EWMA</strong> members feel that I have represented them fairly, and continued<br />
to work in the same spirit as previous presidents. I would like to thank all<br />
society members, our industry partners and others who have contributed<br />
so much to <strong>EWMA</strong> over the past 18 months. Standing down as President<br />
is hard, as one would like to have achieved more within the time given. I<br />
would have liked to attend more national wound care meetings, though<br />
when I have been unable to do so other <strong>Council</strong> members have been superb<br />
in representing the organization. <strong>EWMA</strong> is an amazingly dynamic<br />
organization. What is often forgotten is that the people who do much of<br />
the work do so without payment for their time. It is a great testament to<br />
all who are involved with <strong>EWMA</strong> that so much can be achieved with the<br />
good will of a small group of individuals committed to making life better<br />
for people in Europe and beyond.<br />
Peter J Franks<br />
<strong>EWMA</strong> President<br />
www.ewma.org<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Mölnlycke Health Care<br />
at <strong>EWMA</strong> 2007<br />
Welcome to our stand A5 to find out more about our dressings with Safetac ®<br />
soft silicone adhesive technology and Xelma ® extracellular matrix protein.<br />
A Satellite Symposium will be held on Thursday May 3 rd at 12:30-14:00:<br />
”Why let the patients suffer when there is help?”<br />
”Getting under the patients´skin – how is their pain?” - chaired by Prof. Keith Harding<br />
”Reducing suffering in patients with hard to heal wounds - New extracellular matrix protein therapy.”<br />
- chaired by Prof. Peter Vowden<br />
For more information please visit www.molnlycke.com<br />
Mölnlycke Health Care AB publ. Box 13080, SE-402 52 Göteborg, Sweden,<br />
Phone +46 31 722 30 00
Less trauma. Less pain. TM<br />
Safetac ® is a patented soft silicone adhesive technology. Dressings with Safetac<br />
technology are atraumatic upon removal. These dressings minimise trauma<br />
to the wound and the surrounding skin, which minimises pain to the patient.<br />
The risk of maceration is minimised by sealing the wound margins.<br />
Would you like to know more about the benefits of Safetac technology, please visit www.safetac.com<br />
Dressings with Safetac technology<br />
������� � ������� �� ���� ������� �� �������� ������� �� ������ ������� �� ����������� ������� �<br />
Mölnlycke Health Care, the word mark and logo symbol are trademarks of Mölnlycke Health Care AB.<br />
Mölnlycke Health Care AB (publ.), Box 13080, SE-402 52 Göteborg, Sweden. Phone +46 31 722 30 00, www.molnlycke.com<br />
H097290703
Is it safe to use saline<br />
solution to clean wounds?<br />
INTRODUCTION<br />
The delivery of wound care has become increasingly<br />
technology based. However, some of the<br />
main problems related to impaired healing in<br />
wounds may be related to basic aspects such as<br />
cleansing, when it would be expected that, since<br />
enough evidence exists to indicate best practice<br />
in relation to the procedure (Blunt, 2001; Ellis,<br />
2004), healthcare professionals should have<br />
knowledge of this evidence.<br />
In primary health care in Portugal, wounds<br />
(chronic or acute) are usually cleansed with a sterile<br />
0.9 % (w/v) sodium chloride solution, usually<br />
termed physiological saline because it is isotonic<br />
for human cells (Flanagan, 1997) and innocuous<br />
and it is, therefore, generally the first choice solution<br />
for cleaning wounds (Davies, 1999). Isotonic<br />
sodium chloride solution is one of the best agents<br />
for cleaning open wounds because it removes debris<br />
and bacteria without cell destruction (Pina,<br />
1999, Cochrane, 2004). The major aim in wound<br />
cleaning is removal of organic and inorganic residues<br />
before application of the dressing thus maintaining<br />
an optimal environment at the wound site<br />
for healing (Morison et al., 1997). Other benefits<br />
of wound cleaning are: (i) to hydrate the wound<br />
surfaces and create a moist medium more favorable<br />
for healing; (ii) to preserve the surrounding<br />
skin, removing residues of glue and excess of<br />
humidity that can cause maceration, as well as<br />
erosion by action of enzymes of the exudates and<br />
toxic bacteria present on skin; (iii) to facilitate<br />
the visualization of the size and extension of the<br />
wound; (iv) to minimize the trauma of the wound<br />
due to the continuous use of adherent materials;<br />
(v) to reduce the risk of infection; and (vi) to<br />
promote the comfort of the ill person. (Morison<br />
et al., 1997; Agreda & Bou, 2004):<br />
The technique of wound cleansing has evolved<br />
through time. Thomlinson (1987) has demonstrated<br />
that the technique of rubbing the wounds<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
(with a swab held on a forceps) from the clean<br />
area to the dirty area, up and down and from the<br />
center to the border, only resulted in distribution<br />
of bacteria upon the surface of the wound. Additionally,<br />
the use of the swab and vigorous rubbing<br />
can cause trauma, especially in epithelial cells, as<br />
well as leave residues (little filaments of the swabs)<br />
that could delay healing by acting as foreign bodies<br />
that could remain in the deep tissues and serve<br />
as a focus of infection (Wood, 1976).<br />
In conclusion, the best choice for wound cleansing<br />
is the irrigation technique. Irrigation consists<br />
of gently removing residues on the surface of the<br />
wound as well as other contaminants (Lawrence,<br />
1997-1998). This is achieved by using fluids at<br />
constant pressure or pulsated pressure (Cooper<br />
et al., 2003).<br />
The optimal pressure for irrigation is achieved<br />
using a 35 ml syringe with a 19 G caliber needle.<br />
The disadvantages of this method are mainly:<br />
- the detachment of the needle during irrigation<br />
with the risk of causing injury to the<br />
patient and/or the professional;<br />
- the production of aerosols that could contaminate<br />
the environment or the professionals.<br />
At present, the professionals of the Health Subregion<br />
of Coimbra perform the cleaning of wounds<br />
by irrigation, using flasks of sodium chloride solution<br />
of 100 cc, 500 cc or 1000 cc, with a transfer<br />
attached. The same flask with transfer is used in<br />
several patients with resulting risk of contamination.<br />
OBJECTIVES<br />
The present study was undertaken with the objective<br />
of evaluating the level of microbial contamination<br />
of physiological saline flasks used in health<br />
centers for wound cleaning and identifying those<br />
microorganisms found.<br />
�<br />
Scientific Article<br />
João Carlos Gouveia<br />
Christina Miguens<br />
C. S. Pampilhosa Serra,<br />
P. Serra.,<br />
Portugal<br />
gouveia.miguens@sapo.pt
MATERIALS AND METHODS<br />
Samples<br />
From February to April of 2005, 44 saline solutions from<br />
22 health care centers localized in the health sub-region<br />
of Coimbra were collected. From each centre two flasks in<br />
use were randomly selected, one from the ER (Emergency<br />
Room) ward and the other from the outpatient clinic. A<br />
triple blind methodology for data analysis was used so<br />
that the professionals in the clinic were not aware at the<br />
time that the study was under way, the microbiologists<br />
did not know where the flasks came from and the person<br />
who analyzed the data also had no idea of the origin of<br />
the flasks.<br />
The samples were transported at 4ºC and maintained<br />
at this temperature until processing.<br />
Processing of samples<br />
At the time of sampling, the flasks of saline solutions were<br />
thoroughly mixed, and 5 ml fractions were removed by<br />
syringe and needle after disinfection of flask surfaces with<br />
Sodium Hypochlorite. The undiluted suspensions were<br />
seeded by the pour-plate technique. For this, 1.0 ml aliquots<br />
were deposited at the center of sterile empty Petri<br />
dishes, followed by 19.0 ml of plate count agar (PCA)<br />
(Biomérieux, France). After homogenization and solidification<br />
of the mixture, the plates, for all samples, were<br />
incubated at 28ºC and 37ºC for 48 hours.<br />
The saline solutions 0.1 ml fractions were evenly spread<br />
over the surface of Blood Agar (Biomérieux, France) and<br />
Sabouraud Chloramphenicol Agar (SAB CHL-D; Biomérieux,<br />
France) with individual sterile, bent-glass Lrods.<br />
We have also tested the transfer of the flasks of saline<br />
solutions for microbial contamination with a sterile cotton<br />
swab that was rubbed vigorously, with rotation, over the<br />
transfer surface. Swabs were immediately applied directly<br />
on Blood agar media by rubbing, with rotation, over the<br />
entire surface twice. These blood Agar plates were incubated<br />
at 37°C for 48 hours and the SAB CHL-D plates<br />
were incubated at 28ºC and 35ºC and examined daily<br />
for a period of 30 days before being declared as culture<br />
negative.<br />
The number of colony forming units (CFU) was determined<br />
in each plate after incubation and the CFU/ml<br />
of saline solutions was calculated by number of colonies<br />
x dilution factor.<br />
Isolation of bacteria<br />
The specimens with no bacterial growth were considered<br />
as negative. Bacterial colonies grown in PCA and Blood<br />
Agar media were selected by their morphological features,<br />
including all observed bacterial varieties. From each culture,<br />
the colonies were transferred to the original type<br />
of medium in the optimal incubation conditions. Every<br />
morphological type was observed using Gram’s stain for<br />
the definition of biochemical tests employed to identify<br />
bacterial species (or genera). Catalase and oxidase tests<br />
were then performed on the developed colonies, followed<br />
by biochemical genera and species identification<br />
tests which used four standardized micro-method systems:<br />
API Staph, API Strep, API 20 E and API Coryne strip test<br />
(BioMérieux, France).<br />
Isolation of Fungi<br />
Culture positive specimens were identified macroscopically<br />
by observation of morphological colonial characteristics<br />
such as texture and color and also microscopically by examination<br />
of conidial morphology.<br />
Amplification and sequencing<br />
When microbial identification was not conclusive when<br />
employing only conventional morphological and biochemical<br />
tests, additional 16S rRNA gene sequence determination<br />
and phylogenetic analysis were used for bacterial<br />
strains and in the case of moulds we performed the<br />
amplification and sequencing of ITS (Internal Transcriber<br />
Spacers) region of 5.8S gene.<br />
Statistical analysis<br />
Statistical analysis was performed with the use of SPSS<br />
11.0 (SPSS Inc., Chicago, USA) for parametric tests. We<br />
used the t Student for dependent samples; a P value of less<br />
than 0.05 was considered statistically significant.<br />
RESULTS<br />
Of the 44 saline solutions analyzed, 54.5% were contaminated.<br />
The saline solutions’ CFU/ml ranged between 1<br />
and 230. The relative distribution of contamination due<br />
to the transfer or the saline solution itself was diverse, corresponding<br />
50% to saline solution, 37.5% to the transfer<br />
and 12.5% to both sources. In terms of relation between<br />
types of ward/contamination, we realized that the flasks<br />
used in the ER were present in a ratio of 2:1 contaminated<br />
flasks to clean, when compared with the flasks collected<br />
in the outpatient clinic with a statistical difference<br />
(p= 0,01) [IC 95%: mean 0,363: 0,143]. A total of 38<br />
strains were isolated, 66% could be identified to species<br />
level using morphological and biochemical tests, the remaining<br />
34% were identified by gene amplification and<br />
sequencing. About 69.6% of the identified strains were<br />
Gram-positive cocci, the second dominant type of strains<br />
were Gram-positive bacilli (13%), and the third dominant<br />
type of strains were Gram-negative bacilli and moulds,<br />
both with 8.7%.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
The distributions of microbial taxa from saline solutions<br />
and transfers are shown in Figure 1. The figure shows<br />
that the number of different taxa in saline solutions was<br />
considerably higher than in transfers.<br />
The most frequent contaminants belonged to normal human<br />
flora (64%), namely Staphylococcus aureus (3 strains),<br />
Kytococcus sedentarius (3 strains), Staphylococcus epidermidis<br />
(2 strains), Enterococcus faecalis (2 strains), Klebsiella pneumoniae<br />
(2 strains), Micrococcus sp. (2 strains), Micrococcus<br />
luteus (1 strain), Staphylococcus haemolyticus (1 strain),<br />
Staphylococcus cohnii cohnii (1 strain), Staphylococcus<br />
lugdunensis (1 strain), Staphylococcus hominis (1 strain),<br />
Streptococcus salivarius (1 strain), Lactobacillus johnsonii<br />
(1 strain), Corynebacterium pseudodiphtheriticum (1 strain)<br />
and Corynebacterium striatum/amycolatum (1 strain).<br />
The second dominant group of microorganisms (36%)<br />
was saprophytes in nature such as, Bacillus sp. (2 strains),<br />
Ochrobactrum sp. (2 strains), Serratia marcescens (2 strains),<br />
Paenibacillus sp. (2 strains), Pantoea spp 3 (1 strain), Jeotgalicoccus<br />
sp. (1 strain), Massilia sp. (1 strain), Aspergillus<br />
fumigatus (1 strain), Aspergillus nidulans (1 strain),<br />
Cladosporium sp. (1 strain) and Penicillium sp. (1 strain).<br />
The number of microbial strains isolated from saline<br />
solutions and transfers are shown in Figure 2. Of the 38<br />
strains isolated, 26 were recovered from saline solutions<br />
and 12 from transfers.<br />
DISCUSSION<br />
In this study, it was observed that the majority of the saline<br />
solutions in use for cleaning wounds were contaminated.<br />
This is due, mainly, to the use of these saline solutions in<br />
multiple patients (through direct or indirect contact or<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
Figure 1.<br />
Relative distribution of different microbial taxa in<br />
saline solutions and transfers. The Gram-positive<br />
cocci group included: Micrococcus, Staphylococcus,<br />
Enterococcus, Streptococcus, Kytococcus<br />
and Jeotgalicoccus. The Gram-positive bacilli<br />
group comprised: Bacillus, Corynebacterium,<br />
Paenibacillus and Lactobacillus. The Gramnegative<br />
bacilli group was represented by:<br />
Ochrobactrum, Massilia, Serratia, Klebsiella and<br />
Pantoae. Finally, the filamentous fungi group was<br />
constituted by: Aspergillus, Cladosporium and<br />
Penicillium.<br />
Figure 2.<br />
Number of strains isolated from saline solutions and transfers.<br />
Scientific Article<br />
droplets). This could constitute a major problem because<br />
the Healthcare Centers from which the samples were collected<br />
provide assistance to an average of 250000 patients<br />
and perform around 35000-50000 dressings annually, for<br />
either chronic or acute wounds.<br />
All the saline solutions collected were flasks of volume<br />
above 100 cc (500 cc or 1000 cc), which are used in consecutive<br />
patients, until the contents are exhausted. No<br />
statistical difference was found between the type of flasks<br />
and the contamination degree. Although the samples were<br />
�
Scientific Article<br />
Table 1.<br />
Microbial species identified from saline solutions and transfers.<br />
In total, 38 strains were independently isolated at 28, 35 and<br />
37ºC, and identified by morphological and biochemical tests,<br />
gene amplification and sequencing.<br />
a Identified by gene amplification and sequencing.<br />
b Represents probably a new species of Jeotgalicoccus,<br />
partial 16S gene sequence was most similar to<br />
Jeotgalicoccus pinnipedialis (95%, strain A/G14/99/10 T ).<br />
c Represents probably a new species of Massilia,<br />
16S gene sequence was most similar to Massilia timonae<br />
(97%, strain UR/MT95 T ).<br />
10<br />
collected in the clinic, the same procedure is adopted in<br />
home care and the flasks may remain in use for several<br />
days.<br />
After perforation of the saline solution flask by the<br />
transfer, it loses its sterility and so it is recommended that<br />
each saline solution flask should be of single-use.<br />
In order to re-use contents, the flasks are fitted with a<br />
transfer that remains attached and consequently there is<br />
additional loss of sterility. It also represents an entrance<br />
point for microorganisms present in the environment, increasing<br />
the probability of contamination. In this context,<br />
the manipulation of the transfer by health professionals<br />
represents an additional source of contamination.<br />
Our results show that, the contamination was mainly<br />
(50%) due to the saline solutions as well as the transfers<br />
(37.5%). Additionally, from some of the contaminated<br />
saline solutions we were able to isolate more than one<br />
�<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
At last, hyaluronic acid with low protein levels and no animal impurities<br />
Manufacturers of skin care and wound care products know<br />
that the natural moisturising, softening and healing properties<br />
of hyaluronic acid are second to none. Even so, most medicalgrade<br />
ingredients contain biological impurities that require the<br />
addition of a disinfectant agent. That is not always good for<br />
tender or damaged tissue. And it is not good for sales either.<br />
Introducing HyaCare ® from Novozymes Biopolymer, the first<br />
hyaluronic acid that is 100% free of animal-derived ingredients.<br />
Based on the safe host strain Bacillus subtilis, HyaCare<br />
is produced without the use of organic solvents. That means<br />
it is completely safe – both for people and the environment.<br />
Best of all, with HyaCare your customers will experience<br />
lasting results, not just temporary relief. Sound like a brand<br />
advantage? And that’s only half the story – so let’s talk.<br />
www.hyacare.com
Scientific Article<br />
bacterial species (data not shown) thus increasing the risk<br />
of wound contamination with multiple species.<br />
Trengove et al. (1996) demonstrated that the presence<br />
of several bacterial species (four or more) colonizing a<br />
wound significantly increases the probability of delayed<br />
healing.<br />
With respect to identification of microorganisms<br />
isolated, we observed that in most cases (64%) they belonged<br />
to the normal human flora, suggesting that the<br />
main source of contamination was human manipulation<br />
of the patient, while the other 36% were probably from<br />
the environment.<br />
It is disturbing to conclude that most of the wounds<br />
cleaned with these flasks, even if they were not colonised<br />
or infected before the treatment, have a higher risk of<br />
becoming infected after it, with all the associated costs<br />
both human and economic. We wished to change practice<br />
and looked for the evidence that the saline could be<br />
contaminated. Although we do not know infection rates<br />
in Portugal, it is logical to conclude that if we use contaminated<br />
solutions there will be a higher inoculum and<br />
therefore a greater risk of infection.<br />
CONCLUSION<br />
The false concept of economic benefits from multi-use<br />
products without taking into account other aspects such as<br />
effectiveness, has led to erratic practices with negative consequences<br />
for patients, namely: (i) increase in the period of<br />
time for the necessary treatments for wound healing; (ii)<br />
increase in the use of systemic antibiotic therapy for infections;<br />
(iii) increased possibility of nosocomial infections;<br />
(iv) increase of costs relative to the wound treatments; and<br />
(v) significant decreasing of quality life of patients (not<br />
published data). In summary, it is urgent that healthcare<br />
professionals adopt single use cleaning solutions in order<br />
to decrease or even eliminate a significant source of wound<br />
contamination. More than the flask size, the level of contamination<br />
will depend on the time it remains in use after<br />
being opened since it is known that each bacterium can<br />
divide in two in a period of just 20 minutes (one bacterium<br />
could yield one million bacteria in six hours) (Alfa<br />
& Sitter, 1991).<br />
It is important that those responsible for wound management<br />
should be alerted to the importance of avoiding<br />
in-use contamination of wound cleansing solutions, but<br />
1<br />
that is not all. Besides the standard precautions such as<br />
hand hygiene and appropriate use of gloves, it is important<br />
to consider that all materials in the proximity of the<br />
patient can become contaminated during wound cleansing<br />
through production of droplets and aerosol particles and<br />
that there is, therefore, also the risk of contamination via<br />
hands and gloves during the procedure.<br />
In relation to the use of transfers, our results suggest<br />
the need of adopting the use of single use saline solution<br />
flasks for wound cleaning, with a system of delivery that<br />
will permit wound irrigation without risk of manipulation.<br />
Although this study refers to saline solutions, the results<br />
should be extrapolated to all materials used in wound care<br />
which are in the proximity of the patient and are used for<br />
other patients (for example, hydrogel, swabs, ointments,<br />
and scissors).<br />
Finally, the results of this study were presented to head<br />
nurses from all the health centers in the region followed<br />
by an educational programme on prevention of cross contamination<br />
of infection during wound care.<br />
We hope that this study may lead to other more allinclusive<br />
studies, which can be lead in hospital wards, to<br />
examine and understand if these results may be extrapolated<br />
to all kind of healthcare services. m<br />
Bibliography<br />
Alfa MJ., Sitter DL. In hospital evaluation of contamination of duodenoscopes: a<br />
quantitative assessment of the effects of drying. J. Hospital Infection, 1991; 19:<br />
89-98.<br />
Agreda, J. & Bou, J. (2004). Atención integral de las heridas crónicas. Madrid, SPA, Sl.<br />
Blunt J (2002) Wound cleansing: ritualistic or research-based practice? Nursing Standard.<br />
16, 1, 33-36.<br />
Cooper, R. et al. (2003). Wound Infection & Microbiology. London, Medical<br />
ommunications, UK Ltd, Johnson & Johnson Medical.<br />
Davies, C. (1999). Wound care. Cleansing rites and wrongs. Nursing Times, 95 (43):<br />
71-72, 75.<br />
Ellis T. CPD: Understanding the act of contamination in wound dressing procedure,<br />
Collegian, Vol. 11, nº 3, 2004, p. 39-41<br />
Fernandez, R., Griffiths, R., Ussia, C. Water for wound cleansing, Cochrane database<br />
Syst Rev, 2002 (4)<br />
Flanagan, M. (1997). Wound Management. Edinburgh: Churchill Livingstone.<br />
Lawrence, H. (1997 Dec 17-1998 Jan 6). Nursing in 1998: on with the new?<br />
Nurs Stand, 12(13-5): 36-37.<br />
Morison, M. et al. (1997). A Colour Guide to the Nursing Management of Chronic<br />
Wounds. London, Mosby.<br />
Pina, E. (1999). Aplicação tópica de antimicrobianos no tratamento de feridas. In Nursing<br />
: formação contínua em enfermagem, 137: 31-34.<br />
Thomlinson, D. (1987). Journal of Infection Control Nursing. To clean or not to clean?<br />
Nursing Times, 83(9): 71-75.<br />
Trengove, N. J. et al. (1996). Qualitative bacteriology and leg ulcer healing. J Wound<br />
Care, 5(6): 277-280.<br />
Wood, R. A. (1976). Disintegration of cellulose dressings in open granulating wounds.<br />
British Medical Journal, 1(6023): 1444-1445.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Find out more during <strong>EWMA</strong> at the KCI Booth and at the KCI Symposium<br />
©2007 KCI Licensing, Inc. All Rights Reserved. All trademarks designated herein are property of KCI, its affiliates and licensors. Those KCI trademarks designated with the “®”, “TM” or “*” symbol are registered<br />
in at least one country where this product/work is commercialized, but not necessarily in all such countries. Most KCI products referenced herein are subject to patents and pending patents.
Making the Choice Clear<br />
AQUACEL ® Ag dressing is the only<br />
antimicrobial with all the benefits<br />
of Hydrofiber ® ConvaTec Technology<br />
• Gels on contact with exudate—absorbs and retains fluid 1<br />
and locks away harmful components contained within exudate* ,2-4<br />
as demonstrated in in vitro testing<br />
• Effective antimicrobial—low concentration of ionic silver kills<br />
a broad range of wound pathogens in the dressing including MRSA 5<br />
as demonstrated in in vitro testing<br />
• Enhances patient comfort—soft and conformable for ease<br />
of application<br />
• Allows for non-traumatic removal—without damaging newly<br />
formed tissue<br />
• Supports healing—by providing a moist environment<br />
*AQUACEL ® dressing has the same composition and Hydrofiber ® Technology as AQUACEL ® Ag dressing.<br />
References: 1. Parsons D, Bowler PG, Myles V, Jones S. Silver antimicrobial dressings in wound management: a comparison of antibacterial,<br />
physical, and chemical characteristics. Wounds. 2005;17(8):222-232. 2. Walker M, Hobot JA, Newman GR, Bowler PG. Scanning electron<br />
microscopic examination of bacterial immobilisation in a carboxymethyl cellulose (AQUACEL ® ) and alginate dressings. Biomaterials. 2003;24:883-890.<br />
3. Bowler PG, Jones SA, Davies BJ, Coyle E. Infection control properties of some wound dressings. J Wound Care. 1999;8(10):499-502. 4. Walker<br />
M, Cochrane CA. Protease sequestration studies: a comparison between AQUACEL ® and PROMOGRAN ® in their ability to sequester proteolytic<br />
enzymes. WHRI 2494 WA139. May 27, 2003. Data on file, ConvaTec. 5. Jones SA, Bowler PG, Walker M, Parsons D. Controlling wound bioburden<br />
with a novel silver-containing Hydrofiber ® dressing. Wound Rep Reg. 2004;12:288-294.<br />
®/TM The following are trademarks of E.R. Squibb & Sons, L.L.C.: AQUACEL Ag and Hydrofiber. ConvaTec is an authorised user.<br />
©2006 E.R. Squibb & Sons, L.L.C. July 2006 GO-06-1047.1<br />
www.aquacelag.com
The cost of pressure ulceration<br />
INTRODUCTION<br />
Pressure ulcers are a major cause of morbidity in<br />
the population, yet it is largely an unseen problem.<br />
It is known that the treatment and prevention of<br />
pressure ulcers is costly to health services, but as<br />
yet there is still little information on precise costs.<br />
Moreover, there is a cost to patients of pressure ulceration,<br />
both in financial terms, but also in terms<br />
of their quality of life. This paper will review some<br />
of the key evidence in respect to both the costs to<br />
society and the costs to individual patients.<br />
MEASURING THE BURDEN OF<br />
PRESSURE ULCERATION ON RELATIVES<br />
AND CARERS<br />
It is important to examine both the costs of providing<br />
the health services to patients suffering from<br />
the disease in question, but also to determine the<br />
costs to patients and relatives since care falls increasingly<br />
outside the formal health services, and<br />
on to patients and their families. Indirect costs<br />
should be derived from estimates of lost production<br />
by the patient or family members caused by<br />
the disease, losses to society caused by the patient<br />
being unable to function to their potential, and<br />
quality of life issues, particularly problems associated<br />
with pain, poor mobility, discomfort and<br />
distress. Relatives and carers provide substantial<br />
support to health services, without which it is<br />
argued that health and social services would collapse<br />
under the burden if such informal care was<br />
not available. In is estimated that some 6.8 million<br />
people in the UK could be defined as carers 1 .<br />
These carers provide support and care to relatives<br />
and friends who are unable to care for themselves<br />
independently. In England the value of informal<br />
carers providing care in the community is estimated<br />
to be £57 billion per year 2 .<br />
THE FINANCIAL COSTS OF PRESSURE<br />
ULCERATION<br />
The costs of pressure ulcer care and prevention are<br />
largely unknown, perhaps due to the fact that it<br />
is a condition largely secondary to other diseases.<br />
However, there has been a long-standing interest<br />
in estimating the costs of pressure ulcers, sometimes<br />
using these costs to calculate which other<br />
services (surgery and bed stays) could instead be<br />
provided 3 .<br />
In 1993, the UK government commissioned<br />
accountants Touche Ross to provide them with<br />
an estimate of health service costs of pressure ulcers<br />
4 . They used existing research where available<br />
and expert opinion where necessary to provide a<br />
theoretical cost of prevention and treatment of<br />
pressure ulceration in an average 600 bedded hospital.<br />
Different models were proposed, depending<br />
on whether the hospital was high or low cost, and<br />
depending on whether there was an active prevention<br />
strategy with treatment, or treatment alone.<br />
The final estimates indicated that with a treatment<br />
strategy alone a low cost hospital would<br />
spend e 901,000 (£644,000) per year on pressure<br />
ulcers whilst a high cost hospital would spend<br />
in the region of e 1,614,000 per year in 1993.<br />
When including a prevention strategy into the<br />
care of patients the low cost hospitals used a similar<br />
budget (e 901,000), but the high cost hospitals<br />
used e 3,794,000.<br />
Most the excess cost associated with prevention<br />
was consumed by additional nursing time spent<br />
assessing and turning the patients. This report<br />
concluded that the cost of pressure prevention<br />
and treatment would cost the UK health service<br />
approximately 0.4-0.8% of the total annual<br />
budget. This analysis was limited in that it only<br />
estimated costs in the acute (hospital) services and<br />
was unable to estimate costs in the community.<br />
Moreover, there was no attempt to estimate indirect<br />
costs, costs to patients, nor any value placed<br />
on the patients’ quality of life.<br />
A more global investigation of cost of pressure<br />
ulceration was undertaken in the Netherlands,<br />
examining the costs in different care settings in-<br />
�<br />
Scientific Article<br />
Peter J Franks<br />
Professor of<br />
Health Sciences<br />
& <strong>EWMA</strong> President<br />
Centre for Research &<br />
Implementation of<br />
Clinical Practice<br />
Faculty of Health &<br />
Human Sciences<br />
Thames Valley University<br />
32-38, Uxbridge Road,<br />
London W5 2BS<br />
Tel: 0208 280 5020<br />
Fax: 0208 280 5285<br />
peter.franks@tvu.ac.uk<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 15
Scientific Article<br />
cluding home care; nursing homes; general hospitals and<br />
university hospitals 5 . Prevalence figures for different pressure<br />
ulcer stages were determined from estimates given<br />
by the Health <strong>Council</strong> for the Netherlands on Pressure<br />
Ulcers 6 . These data were combined with expert opinion<br />
(Dutch Society of Pressure Ulcer Experts) to determine<br />
personnel time, extra days of care, use of special beds and<br />
medical materials. Both low and high estimates were given<br />
to indicate the potential range of costs. Costs were dependent<br />
not only on ulcer stage, but were also highly dependent<br />
on where care took place. As an example of this mean low<br />
and high daily costs of stage II pressure ulcers were highest<br />
when treated in a university hospital (low e 71.6, high<br />
e 110.2) and lowest in the general hospital (low e 23.7,<br />
high e 25.1) with conversion factor e 1= $1.3.<br />
Home care was similar to University Hospital costs<br />
whereas nursing home care was similar to that of the general<br />
hospital costs. The authors estimated annual costs<br />
of pressure ulcer care to be in the range e 371 million to<br />
e 1,695 million per annum for a country with a population<br />
of just 16.5 million, or 1% of the Dutch health care<br />
budget.<br />
More recently, a model of costs of pressure ulcers has<br />
been developed in the UK, which adopted a more epidemiological<br />
approach 7 . It also looked at different health<br />
states for pressure ulcers, namely normal healing; critical<br />
colonisation, cellulitis and osteomyelitis. Each health state<br />
and pressure ulcer grade was ascribed a cost based on the<br />
research evidence and/or expert opinion. The average cost<br />
of healing the different pressure ulcer grades was estimated<br />
at e 1489 for a grade I, e 6,162 for grade II, e 10,238 for<br />
grade III and e 14,771 for grade IV.<br />
In the UK (population 60 million) annual incidence<br />
(new cases) was estimated at 140,000 for grade I, 170,000<br />
for grade II, 50,000 for grade III and 50,000 for grade IV<br />
based on available incidence data 8 . By combining average<br />
costs and number of cases the total cost of pressure<br />
ulcers was estimated at e 214 million (grade I), e 1047<br />
million (grade II), e 544 million (grade III) and e 670<br />
million (grade IV), giving a total cost of all pressure ulcers<br />
at e 2,473 million. This is equivalent of approximately<br />
2.6% of the total current NHS budget.<br />
As expected most cost (90%) was associated with nursing<br />
time, though in-patient stays accounted for 8% of<br />
overall costs and 30% for grades III and IV. Cost for antibiotics,<br />
dressings and pressure relieving equipment was<br />
all relatively low.<br />
Other studies have concentrated on specific costs of pressure<br />
ulceration. In Australia a study was undertaken to<br />
examine the bed days lost to pressure ulceration in 2001-2.<br />
It was estimated that a pressure ulcer led to an extra 4.31<br />
days per patient leading to 398,432 bed days lost and an<br />
16<br />
opportunity cost of AU$ 285 million (e 170.7 million)<br />
in a population of 20.3 million 9,10 .<br />
COSTS TO THE PATIENT: QUALITy OF LIFE<br />
Health related quality of life (HRQoL) is an important<br />
measure of the impact of a condition on the patient’s physical<br />
and mental well being and their ability to function<br />
socially. While most clinicians would accept that HRQoL<br />
is an important measure to determine the impact of disease<br />
on the patient relatively few studies have been undertaken<br />
to assess this.<br />
One influential qualitative study used a phenomenology<br />
approach to determine the impact of the condition<br />
on 8 subjects who mostly were suffering (or had suffered<br />
from) a stage IV pressure ulcer in the USA 11,12 . Key themes<br />
identified were:<br />
n Perceived aetiology of the ulcer<br />
n Life impact and changes<br />
n Psycho spiritual impact<br />
n Extreme painfulness associated with the PU<br />
n Need for knowledge and understanding<br />
n Grieving process<br />
The pressure ulcer had effects on the patients in terms<br />
of their physical, ability, their ability to function socially,<br />
their financial situation, changes in their perceived body<br />
image, and loss of independence and control of their own<br />
lives. Patients who had an ulcer for longer than six months<br />
experienced pessimism and a poorer adherence to treatment,<br />
which left them feeling depressed and frustrated.<br />
Coping with the pressure ulcer was difficult, and patients<br />
felt isolated, particularly when they were often left in a side<br />
room on their own. Patients felt humiliated that health<br />
care professionals were seeing parts of their body which<br />
were normally kept private. The odour from the pressure<br />
ulcer made them feel dirty and they often resorted to deodoriser<br />
to mask the smell. Financial costs were associated<br />
with having to miss work, for medical care, prescriptions<br />
and travel. The theme of living a restricted lifestyle was<br />
examined more recently, with more detail given for the<br />
impact on families 13 .<br />
Pain associated with the pressure ulcer appears to have<br />
a substantial impact on patients and their lives 13,14 . In<br />
the study by Szor 84% of patients with a grade II to IV<br />
experienced pain, even at rest, with 18% reporting this as<br />
excruciating 14 . In addition 88% reported pain at dressing<br />
change. Only 6% reported pain relief being prescribed,<br />
with nursing staff frequently denying the pain their patients’<br />
experienced.<br />
A further study was undertaken using a generic quality<br />
of life tool (SF-36) in 60 patients in the community 15 .<br />
�<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Biatain - Ibu<br />
Advanced moist wound healing<br />
and release of ibuprofen<br />
and Biatain are registered trademarks of Coloplast A/S.<br />
© 2007-2102. All rights reserved Coloplast A/S, 3050 Humlebæk, Denmark.<br />
Peter van der Kluit<br />
wound patient<br />
Brielle, Netherlands<br />
Advanced moist wound healing<br />
• Biatain - Ibu is a unique combination of excellent exudate management<br />
and local sustained release of ibuprofen 1,2<br />
• Biatain - Ibu may reduce wound pain caused by tissue damage 1,3,4,5<br />
• Biatain - Ibu releases ibuprofen locally with no observed systemic effect 1<br />
www.biatain-ibu.coloplast.com<br />
1 Jørgensen B et al. Pain and quality of life for patients with venous leg ulcers: proof of concept of the effi cacy of<br />
Biatain - Ibu, a new pain reducing wound dressing. Wound Repair and Regeneration 2006, 14 (3), 233-239.<br />
2 Steffansen B et al. Novel wound models for characterizing the effects of exudate levels on the controlled release of<br />
ibuprofen from foam dressings. European Wound Management Association, Poster, May 2006, Prague, Czech Republic.<br />
3 Sibbald, RG et al. Decreased chronic (persistent) wound pain with a novel sustained-release ibuprofen foam dressing.<br />
European Wound Management Association, Poster, May 2006, Prague, Czech Republic.<br />
4 Flanagan M et al. Case series investigating the experience of pain in patients with chronic venous leg ulcers<br />
treated with a foam dressing releasing ibuprofen. WorldWideWounds April 2006.<br />
5 Gottrup F et al. Lower pain with Biatain - Ibu: Initial fi ndings from a randomised controlled double-blind clinical<br />
investigation on painful venous leg ulcers. International Wound Journal, Supplement 1, March 2007.<br />
Reclaim a life<br />
with less pain
17 TH CONFERENCE<br />
OF THE EUROPEAN<br />
WOUND MANAGEMENT<br />
ASSOCIATION<br />
Evidence,<br />
Consensus<br />
and Driving<br />
the Agenda<br />
forward<br />
<strong>EWMA</strong>2007 · GLASGOW<br />
2-4 MAY · 2007<br />
DOWNLOAD THE <strong>EWMA</strong> 2007 ABSTRACTS FROM<br />
WWW.<strong>EWMA</strong>.ORG/<strong>EWMA</strong>2007<br />
WWW.<strong>EWMA</strong>.ORG/<strong>EWMA</strong>2007<br />
Compared with the general population, patients with pressure<br />
ulcers experienced greater problems with physical and<br />
social functioning. At present no studies have examined<br />
utility scores of patients with pressure ulceration to determine<br />
the potential deficit associated with the condition<br />
and the potential cost in terms of QALYs (Quality adjusted<br />
life years).<br />
DISCUSSION<br />
In the area of pressure ulceration there has been some<br />
interest in the evaluation of outcomes of treatment, but<br />
very little attention to the overall cost of care, nor impact<br />
on the patients’ quality of life. Surprisingly, health services<br />
do not appear to be aware of the financial burden that<br />
pressure ulceration causes. As an example, the e 2.5 billion<br />
spent on pressure ulceration is equivalent to the cost of<br />
treating mental health in the UK or all community health<br />
services 7 . The cost estimates are highly dependent on the<br />
incidence of pressure ulcers, although few studies have<br />
been undertaken on a population basis to determine this<br />
important aspect of pressure ulcer evidence. The results<br />
from studies so far undertaken have shown that pressure<br />
ulcers lead to a clear deficit in quality of life, though again,<br />
these are based on small local studies of patients.<br />
There is a clear need for governments to understand that<br />
pressure ulceration causes a major financial burden on<br />
them and on patients’ lives. Until the magnitude is appreciated<br />
it is hard to push for cost effective treatments<br />
and prevention strategies on a national basis to rationalise<br />
the care of patients who suffer from this distressing condition.<br />
m<br />
References<br />
1. Maher, J., Green, H. (2000) Carers 2000. London, Office of National Statistics<br />
2. Carers UK (2002a) Without us carers. London, Carers UK.<br />
3. Hibbs, P. (1990) The Economics of Pressure Sore Prevention. In: Pressure Sores:<br />
Clinical Practice and Scientific Approach. Ed Bader, D. London, Macmillan Press<br />
Ltd.<br />
4. Touche Ross. ‘Pressure sores: a key quality indicator’. Department of Health,<br />
Heywood 1993<br />
5. Severens JL Habraken JM, Duivenvoorden S, Frederiks CMA. The cost of illness of<br />
pressure ulcers in the Netherlands. Adv Skin & Wound Care 2002; 15: 72-77.<br />
6. Health <strong>Council</strong> of the Netherlands. Pressure Ulcers. The Hague:<br />
Health <strong>Council</strong> of the Netherlands 1999 (In Dutch).<br />
7. Bennett G, Dealey C & Posnett J. The cost of pressure ulcers in the UK.<br />
Age & Ageing 2004; 33(3):230-5<br />
8. Clark M Watts S. The incidence of pressure sores within a national health service<br />
trust hospital during 1991. J Adv Nurs 1994: 20; 33-6<br />
9. Graves N, Birrell F, Whitby M. Effect of pressure ulcers on length of hospital stay.<br />
Infect Control Hosp Epidemiol 2005; 26(3): 293-7<br />
10. Graves N, Birrell FA Whitby M. Modelling the economic losses from pressure ulcers<br />
among hopsitalized patients in Australia. Wound Repair Regen 2005; 13 (5):462-7<br />
11. Langemo DK, Melland H, Hanson D, Olson B, Hunter S. The lived experience of<br />
having a pressure ulcer: a qualitative analysis. Adv. Skin Wound Care 2000; 13:<br />
225-35<br />
12. Langemo DK. Psychosocial aspects in wound care. Quality of life and pressure<br />
ulcers: what is the impact? Wounds 2005 17(1): 3-7.<br />
13. Hopkins A, Dealey C, Bale S, Defloor T, Worboys F. Patient stories of living with<br />
a pressure ulcer J Adv Nurs. 2006 56(4):345-53.<br />
14. Szor JK, Bourguignon C. Description of pressure ulcer pain at rest and at dressing<br />
change. J Wound Ostomy Continence Nurs. 1999; 26(3):115-20.<br />
15. Franks PJ, Winterberg H, Moffatt CJ. Health related quality of life and pressure<br />
ulceration: assessment in patients treated in the community. Wound Repair &<br />
Regeneration 2002; 10 (3): 133-140.
14 days<br />
undisturbed<br />
healing<br />
Mepitel ® with Safetac ® soft silicone adhesive technology has been clinically tested and used by<br />
many health care professionals around the world since many years back.<br />
One of the major benefits with Mepitel is that it can be left in place for up to 14 days, whilst only<br />
changing the secondary absorbent dressing 1. This is not only cost-effective, but it also helps the<br />
wound to heal in an undisturbed environment. This truly inspires confidence both for the nurse<br />
and for the patient.<br />
What could you do with 14 days undisturbed?<br />
Ref 1: ������������������������������������������������������������������������������������������������������������������������������������������������������������<br />
Mölnlycke Health Care AB (publ), Box 13080, SE-402 52 Göteborg, Sweden, Phone + 46 31 722 30 00, www.molnlycke.com, www.safetac.com<br />
����������������������������������������������������������������������������������������������������������
Listen – Participate - Debate - Act: an interactive symposium at <strong>EWMA</strong><br />
with voting handsets, sponsored by Wound Management, Smith & Nephew Medical Ltd<br />
“Making wound management<br />
the priority – how can we make a<br />
difference?”<br />
The Lomond Auditorium, Scottish Exhibition<br />
Wednesday 2 nd May 2007, 12:00 – 13:30<br />
Chair: Professor Keith Harding<br />
Speakers: Professor Peter Franks, Jacqui Fletcher, John Timmons<br />
Register online at: www.snevents.com
EXTENDED ABSTRACT · PRAGUE 2006<br />
Epidemiology of wounds<br />
treated in Community Services<br />
in Portugal<br />
Abstract<br />
Aim: To characterize patients and types of wounds<br />
treated in community services and assess patients’<br />
views with regard to wounds and care received.<br />
Materials and methods: Cross-sectional study of a<br />
sample of patients with wounds of duration longer<br />
than two weeks. A representative national sample<br />
was calculated taking into account regional<br />
dimensions, population density and urban/rural<br />
mix. Then 148 health centres were randomly selected<br />
and patient information was completed for<br />
a sample of patients in the clinics.<br />
Results: In all 1424 wounds in 1115 patients aged<br />
≥ 18 yrs were assessed. Of these 57.4% were treated<br />
in the clinic and 42.6% in the home. There<br />
was a predominance of female patients (57.7%)<br />
and the average age was 69.9 (clinic) and 77.1<br />
(home) years. Over 80% of patients were retired.<br />
Leg ulcers were the main type of wound followed<br />
by pressure ulcers. Average wound duration was<br />
7.4 months for pressure ulcers and 19.4 months<br />
for leg ulcers. Of 574 clinic patients a significant<br />
number complained of discomfort and pain but<br />
over 90% were satisfied with care received.<br />
Discussion: Patient population was characterized<br />
as elderly, low income and suffering from chronic<br />
underlying disease. Expectations regarding healing<br />
are low. An education / intervention project<br />
has been started to promote evidence-based practice.<br />
INTRODUCTION<br />
Chronic wounds are a major health care concern<br />
in the community. They cause substantial morbidity<br />
and their management is both time consuming<br />
and costly. Phillips 1 studied the aetiology and<br />
epidemiology of chronic cutaneous ulcers in the<br />
USA and found that pressure ulcers and leg ulcers<br />
were the most commonly encountered cutaneous<br />
ulcers. The Canadian Association of Wound Care 2<br />
combined data of significant studies surveying over<br />
14000 patients from 45 Health Care Institutions<br />
and found that 13-17% of pressure ulcers were<br />
found in community care. They found the prevalence<br />
of all types of wounds in persons receiving<br />
community care to be 34-37%. In Germany 3 , a<br />
study of chronic wounds in home care identified<br />
a prevalence of 4.1% for pressure ulcers, 2.7% for<br />
leg ulcers and 1% for diabetic foot ulcers. In India<br />
Gupta et al 4 conducted a prevalence study in an<br />
urban and a rural community and found a prevalence<br />
of 15.03 per 1000 with a predominance of<br />
untreated acute traumatic wounds.<br />
Graham et al 5 conducted a systematic review of<br />
prevalence studies in lower limb ulceration in the<br />
adult population. They identified 22 reports but<br />
differences in populations studied, study design,<br />
case identification procedures, and clinical validation<br />
of wounds prevented pooling of estimates.<br />
They recommend that future studies should include<br />
large numbers of subjects and total populations.<br />
Briggs and Closs 6 reviewed the literature on<br />
the prevalence of leg ulceration and encountered<br />
similar limitations. They therefore suggested that<br />
a combination of questionnaires to health professionals<br />
and a random sample of the population<br />
provide the best method of establishing the true<br />
prevalence.<br />
Until recently, wound management has been a<br />
low priority in Portugal and heavily dependent<br />
on hospital care (outpatient and inpatient). The<br />
approach is traditional, care is not evidence based,<br />
healing rates are low and very little information<br />
is available about the type of wounds treated in<br />
primary care. We conducted a study of leg ulceration<br />
in an urban area in Lisbon7 and identified a<br />
prevalence of 1.41 per 1000 population. The incidence<br />
of pressure ulcers has been studied in hospital<br />
populations in around 80 thousand patients8 for implementation of the Braden risk assessment<br />
scale but little is known about their burden in<br />
the community. Some aspects related to patients’<br />
�<br />
Scientific Article<br />
Elaine Pina MD,<br />
Clinical Microbiologist<br />
Rua Professor Hernani<br />
Cidade 3-2A<br />
1600-630 Lisboa<br />
Portugal<br />
Tel: 351 217583027<br />
elainepina@netcabo.pt<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 1
Scientific Article<br />
views regarding their wounds are also not known. As part<br />
of the leg ulcer study mentioned, a quality of life study 9<br />
reported that patients with leg ulcers showed significantly<br />
higher scores compared with Portuguese normative data<br />
for all domains of the Nottingham Health Profile. Education<br />
programmes are regularly held, many of them sponsored<br />
by industry, but do not seem to be reflected in the<br />
quality of care provided.<br />
This study was conducted in order to identify the burden<br />
of wounds on the individual and the community services<br />
in order to enable us to devise the most appropriate educational<br />
strategies to improve the quality of care in these<br />
patients. Because of the known limitations of definitions<br />
and denominators 5, 6, 10 , we did not attempt to calculate<br />
prevalence rates. We conducted case assessments of persons<br />
with wounds to determine the type of wounds treated in<br />
community services, their care and the patient’s perceptions<br />
related to their wounds and the care received.<br />
METHODS<br />
This was a cross sectional, multicentre, descriptive study<br />
of a sample of patients with wounds presenting at primary<br />
care services in Portugal. The sampling units were<br />
the health centres. After an initial calculation of the probable<br />
number of wounds treated in previous years it was<br />
estimated that to obtain a sample of 1000-1500 wounds in<br />
patients it would be necessary to visit around 120 Health<br />
Centres. The sampling method was undertaken in two<br />
phases. In the first phase the country was stratified by<br />
region (5 regions) taking into account dimensions and<br />
population density so as to obtain a representative national<br />
sample. In the next phase, regions were further subdivided<br />
into their sub-regions and councils in order to account for<br />
the urban/rural mix. Following this, 148 Health Centres<br />
were randomly selected as sampling units. Approval was<br />
obtained from the National Data Protection Committee.<br />
A pilot test was carried in one sub-region (16 health<br />
centres), during one month, involving 127 patients/219<br />
wounds. Only minor changes were made to the questionnaires.<br />
Data were collected between May 2004 and<br />
December 2005 (19 months). Twenty professional interviewers<br />
were trained with respect to the content of the<br />
questions and general characteristics of the wounds studied.<br />
They visited each health centre for a period of 1 to 2<br />
days, monitoring all patients with wounds treated at the<br />
clinic and in home care. The number of home care visits<br />
was determined based on the usual proportion of visits in<br />
relation to the patients seen in the clinic at each centre.<br />
All patients aged 18 or above, with wounds having a duration<br />
of more than two weeks, were included in the study.<br />
Informed consent was obtained for all participants. Since<br />
no validated tools were identified for this type of study,<br />
three data collections tools were devised for use during<br />
the study. They were based on the objectives of the study<br />
and guidelines of best practice. The first one was related<br />
to information provided by the nurse who cared for each<br />
patient and was related to clinical information and care<br />
given. A second questionnaire was directed to the patients<br />
in order to assess their views and satisfaction with the care<br />
received. A classification scale from 1 (minimum) to 5<br />
(maximum) was used to categorize the importance factor.<br />
Finally a third tool was used to assess the resources used in<br />
terms of nursing time and consumables. Statistical analysis<br />
was performed with the SPSS 13.0. A descriptive analysis<br />
of all variables with the absolute and relative frequencies<br />
for the categorical variables and average, standard deviation,<br />
maximum and minimum values for the continuous<br />
variables was obtained. This paper will report on the<br />
epidemiology of wounds treated and patients’ views with<br />
respect to their wounds and treatment received.<br />
RESULTS<br />
Of the 18 sub-regions in the country, 17 (144 health centres)<br />
participated in the study. A total of 1424 wounds<br />
from 1115 individuals (57.7% women and 42.3 men;<br />
national average 52% women) were studied. Of these,<br />
57.4% were seen in the clinic and 42.6% in the home.<br />
The majority of the patients was of low socio-economic<br />
status (only 3% graduated from secondary school). The<br />
average age of patients in the clinic was 69.9 (SD 13.6<br />
min 18 max 96) years (national average is 47 years) and<br />
in the home the average age was 77.1 (SD 10.7 min 22<br />
max 104). Over 80% were retired.<br />
Distribution of wounds by type is presented in table 1.<br />
Leg ulcers (35.6% venous, 2% arterial and 4.3% mixed)<br />
were predominant in the clinic and pressure ulcers in the<br />
home. Pressure ulcers were located predominantly in the<br />
hip (27.3%) sacrum (19.8%) and heel (19.6%). Of the<br />
traumatic wounds, 93% were in the lower limb. Chronic<br />
wounds (n = 981) were analysed in more detail. The median<br />
duration was of three months for pressure ulcers,<br />
12 months for leg ulcers and three months for diabetic<br />
foot ulcers. Because of the long duration of a number of<br />
wounds we established a cut-off of 100 months. Results<br />
showed that, for a cut-off of 100 months, the average<br />
duration was of 7.4 (SD 11.9) months for pressure ulcers<br />
and 19.4 (SD 23.8) months for venous leg ulcers (48 leg<br />
ulcers had a duration of over 8 years) and 9.8 (SD 15.3)<br />
months for diabetic foot ulcers.<br />
�<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
������������������<br />
��������������������������<br />
��������������������������<br />
������������������������<br />
�������������������������<br />
������������������ ���<br />
��������������������<br />
����������������������������<br />
�������������������� ���<br />
�����������������������<br />
������������������������������������<br />
�������������������������<br />
���������� �������������������<br />
��������� ��������������������<br />
��������<br />
���������������<br />
������������<br />
�������������<br />
��������<br />
����������������������������������������������������������������������������������������������������������������<br />
������������������<br />
���������������������������������������<br />
��������������������������������������<br />
�����������������������<br />
�������������<br />
������������������<br />
�������������������������<br />
������������������������<br />
����������������������<br />
��������������������<br />
������������������������<br />
��������������<br />
���������������������<br />
����������������������������<br />
������������<br />
�������������������������<br />
�������������������<br />
������������������<br />
��������<br />
�����������������������������������������������������������������������������������������<br />
�������������������������������������������������������������������������������������������������������������������������������������������������<br />
���������������������������������������������������������������������������������������������������������������������������������������������<br />
��������������������������������������������������������������������������������������������������������������������������������������������������<br />
���������������������������������������������������������������������� ������������������
Scientific Article<br />
Table 1-Distribution of wounds by type<br />
Because of the difficulties in the diagnosis of infection,<br />
we only collected information on the presence of related<br />
signs/symptoms. In 1108 patients, signs of inflammation<br />
or infection (oedema, erythema, pain, local warmth, exudate,<br />
odour) were present (Table 2). About 3% of pressure<br />
ulcers and leg ulcers showed all signs, and around 19% of<br />
ulcers referred showed at least three of them.<br />
Associated co-morbidities: 19.8% of patients with pressure<br />
ulcers and 16% of those with leg ulcers suffered from<br />
diabetes. Venous disease was present in 13.2% of patients<br />
with pressure ulcers and 10% of patients with diabetic foot<br />
ulcer. Of the pressure ulcer patients 9.2% had suffered a<br />
stroke and 3% suffered from hypertension. Other risk<br />
factors studied were malnutrition, smoking habits and alcohol<br />
intake. This was information reported by the health<br />
professionals (no definitions were supplied). Malnutrition<br />
was noted in 31.8% of pressure ulcer patients, in 4.5% of<br />
venous ulcers patients and in 8.2% of diabetic foot ulcer<br />
patients. Less then 4% of the patients referred smoking<br />
and alcohol intake was referred in about 6%. Around 20%<br />
of patients were on antibiotics. The most frequent medications<br />
are presented in table 3.<br />
Patients’ views: The questionnaire about patients’ views<br />
was completed for 574 patients who attended the clinic.<br />
Day-to-day discomfort due to the wound was referred to<br />
as being significant or very significant in more than 41.2%.<br />
Only 18% referred little discomfort. A high number of<br />
patients (70.9%) complained of pain, which ranged from<br />
little (7.5%) to significant or very significant (45%). Prolonged<br />
pain was referred by 57% of those referring pain.<br />
Twenty per cent complained of pain at dressing changes,<br />
Table 2. Signs of inflammation or infection<br />
Table 3. Most frequent medications prescribed<br />
15% of pain on movement and 8% at both; 45% used<br />
analgesic drugs. It is interesting to note that nurses only<br />
mentioned presence of pain in about 30% of the patients<br />
(Table 2).<br />
More than 90% of the patients were satisfied or very satisfied<br />
with the care received and only 7.5% had complaints.<br />
Disinfection of the wound (89.9%) and the dressing used<br />
were considered to be the most significant part of care followed<br />
by communication with the nurse (77.6%).<br />
One third of the patients came to the clinic on foot and<br />
37% used public transport. Others used a motorbike or<br />
family car and 6.8% were transported by ambulance or<br />
the health centre or day care centre transport. About 38%<br />
were accompanied by family or friends but, in most cases,<br />
this did not require absence from work. Waiting time for<br />
attendance was on average 21.4 minutes (SD19.0) with a<br />
minimum of 1 minute and a maximum of 2 hours.<br />
DISCUSSION<br />
This is the first study in the country to address the problem<br />
of wounds treated in community services. In this type of<br />
study in which the health professional supplies information<br />
on patients, some weaknesses can be expected, due to the<br />
high number of people involved, variable knowledge on<br />
�<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Prontosan ®<br />
... cost effective irrigation and dressing of chronic wounds<br />
AVAILABLE ON<br />
UK DRUG TARIFF<br />
<strong>EWMA</strong><br />
Conference<br />
Glasgow<br />
Stand No. I-4<br />
� optimal wound conditioning<br />
� fast and effective removal of wound<br />
coating<br />
� absorption of wound odours<br />
� can be used up to 8 weeks after opening<br />
B. Braun Medical Ltd · OPM Division · Thorncliffe Park · Sheffield · S35 2PW · Tel 0114 225 9000 · Fax 0114 225 9111 · www.bbraun.co.uk<br />
XX-PCE-04-07
NOW AVAILABLE<br />
ON PRESCRIPTION IN<br />
OPAQUE WHITE<br />
Promotes wound<br />
healing in delayed<br />
or non-healing<br />
chronic wounds 1,2<br />
www.kerraboot.com<br />
0800 1077 107<br />
1. Leigh R, Barker S, Murray N, Hurel SJ. The Kerraboot ® : A novel wound dressing device for the management<br />
of leg and foot ulcers. Practical Diabetes Int 2004;21(1):27-30.<br />
2. Edmonds ME et al. Randomised study of Kerraboot ® vs standard wound care in the management of diabetic<br />
neuropathic foot ulcers. Wounds UK, 2006, Vol 2, No 1: 25-31.<br />
Kerraboot ® is a registered trademark of Ark Therapeutics Ltd<br />
© Copyright Ark Therapeutics Limited, 2006.
wound management and attention given to the<br />
questions asked. Discrepancies were identified<br />
in relation to wound categorization. However,<br />
because the method of data collection ensured<br />
confidentiality it was not possible to go back<br />
for clarification. Nevertheless, it was possible to<br />
characterize the population of patients treated in<br />
primary care in Portugal as aged, with a low socio-economic<br />
status and suffering from chronic<br />
underlying disease. Leg ulcers are the predominant<br />
wounds in the clinic and pressure ulcers are<br />
more frequent in the home. Wound duration<br />
is prolonged and healing rates are not known.<br />
However, we conclude that expectations with<br />
regard to healing are low not only in patients,<br />
since they are satisfied with the care received in<br />
spite of the discomfort and pain, but also in the<br />
health professionals. Analysis of the data related<br />
to care and costs (to be published) has also confirmed<br />
that there is a gap between actual practice<br />
and existing evidence that needs to be addressed<br />
in order to improve quality of care. In October<br />
2006 we started a project based on education/<br />
intervention that will be implemented through<br />
2007 and early 2008. At the end of this period<br />
we will repeat the survey in order to assess the<br />
effectiveness of our intervention. m<br />
Acknowledgements<br />
This study was sponsored by Johnson & Johnson Wound Management a<br />
division of Ethicon- Johnson & Johnson Medical, Portugal.<br />
Data collection and statistical analysis was performed by Keypoint,<br />
Scientific Consultants (an independent company working in the field of<br />
clinical trials).<br />
References<br />
1. Phillips TJ. Chronic cutaneous ulcers: aetiology and epidemiology.<br />
J Invest Dermatology 1994 Jun; 102(6):38S-41S<br />
2. Woodbury G. and Houghton P. Canadian Association of Wound Care<br />
www.cawc.net/open/library/research/pandi/index.html accessed<br />
1-11-06<br />
3. Panfil EM, Mayer H et al Wound Management in patients with<br />
chronic wounds in ambulatory nursing – a pilot study. Pflege 2002<br />
Aug; 15(4): 169-176 (German, abstract in PubMed)<br />
4. Gupta N, Gupta SK et al An Indian community-based epidemiological<br />
study of wounds. J Wound Care, 2004 Sep; 13(8): 323-325<br />
5. Graham ID, Harrison MB et al Prevalence of lower-limb ulceration:<br />
A Systematic Review of Prevalence Studies Advances in Skin and<br />
Wound Care, Nov 2003<br />
findarticles.com/p/articles/mi_qa3977/is_200311/ai_n9342478<br />
Accessed on 25.10.2006<br />
6. Briggs M and Closs SJ The prevalence of leg ulceration: a review of<br />
the literature. <strong>EWMA</strong> Journal 2003; 3(2): 14-18<br />
7. Pina E. Furtado K. et al. Leg ulceration in Portugal: prevalence and<br />
clinical history. Eur J Vasc Endovasc Surg. 2005 May, 29(5):549-53<br />
8. Ferreira PL, Miguens C et al. Risco de desenvolvimento de úlceras<br />
de pressão Implementação nacional da Escala de Braden, 2006<br />
(in press)<br />
9. Furtado K. Pina E et al. Quality of life in patients with leg ulcers in<br />
Portugal. Rev Port Cir Cardiotorac Vasc. 2005 Jul-Sep;12(3):169-74.<br />
10. Fletcher J. Measuring the prevalence and incidence of chronic<br />
wounds. Mar 2003. Profession Nurse; 18(7) 384-388<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
Surname:<br />
First name(s):<br />
Profession:<br />
Physician Surgeon Dietician Nurse Pharmacist Other<br />
Work Address:<br />
Address for Correspondence (if different from above):<br />
Tel: Fax:<br />
E-mail:<br />
I enclose a cheque of 25e. Please indicate cheque no.: ___________________________________<br />
Please make cheques payable to: European Wound Management Association<br />
Or: Please debit my account by 25e:<br />
Credit Card type: (Delta, Master Card or Visa). Credit card no:<br />
Expiry Date:<br />
<strong>EWMA</strong> Membership<br />
Become a member of the European Wound Management<br />
Association and you will receive <strong>EWMA</strong> position documents<br />
annually and <strong>EWMA</strong> Journal three times a year.<br />
In addition, you will also have the benefit of obtaining the<br />
membership discount, which is normally 15%,<br />
when registering for the <strong>EWMA</strong> Conferences.<br />
The most important aspect of becoming a member of <strong>EWMA</strong><br />
is the influence this membership can give you. As a <strong>EWMA</strong><br />
member you can vote and even stand for election for the<br />
<strong>EWMA</strong> <strong>Council</strong>, which will give you direct influence on future<br />
developments within European woundhealing.<br />
Please register as a ewma member at www.ewma.org.<br />
A membership only costs 25 EUR a year.<br />
You can pay by credit card as well as bank transfer.<br />
Existing members of <strong>EWMA</strong> can also renew their membership online.<br />
Please use CAPITAL letters<br />
<strong>EWMA</strong> Business Office<br />
Danske Bank, London Cash Management<br />
75 King William Street, London EC4N 7DT, UK<br />
Account No: 93406336. IBAN: GB69DABA30128193406336<br />
BIC/SWIFT: DABAGB2L. Sort code 301281<br />
<strong>EWMA</strong> Membership application<br />
Exact name and initials on the credit card:<br />
_____________________________________<br />
Please return form and enclose cheque to:<br />
<strong>EWMA</strong> Business Office, Congress Consultants<br />
Martensens allé 8, DK-1828 Frederiksberg C, Denmark
We call it QuadraFoam ® because<br />
“Healing-Cleansing-Absorbing-<br />
Moisturising-Comfortable-Easy-<br />
Fast-Acting Dressing” just<br />
didn’t seem as catchy.<br />
QuadraFoam.The first 4-in-1 dressing formulation.<br />
PolyMem, the only QuadraFoam dressing, simplifies your work and improves<br />
healing by effectively cleansing, filling, absorbing, and moistening wounds<br />
throughout the healing continuum. Finally, a dressing that lives up to its name.<br />
Visit booth F1 at <strong>EWMA</strong> to receive a complimentary case study along with a set<br />
of PolyMem samples. Find your local distributor at www.PolyMem.eu.<br />
www.PolyMem.eu<br />
PolyMem and QuadraFoam are trademarks of Ferris, registered or pending in the US Patent and Trademark<br />
Office and in other countries. © 2007 Ferris. All rights reserved. 16W300 83rd St., Burr Ridge, IL 60527<br />
MKL-218,0706
EXTENDED ABSTRACT · PRAGUE 2006<br />
Short Paper<br />
Improving wound assessment<br />
through the provision of<br />
digital cameras across a<br />
Primary Care Trust<br />
Abstract<br />
This paper describes a Trust wide project initiated<br />
by the Tissue Viability service to improve wound<br />
care services and outcomes. Tower Hamlets is<br />
an inner city Primary Care Trust that has both<br />
Elderly Service in-patients plus District Nursing<br />
services. Project funding was secured to provide<br />
digital cameras across the Trust with the aim of:<br />
1. Reducing delay in diagnosis and referral for<br />
specialist review.<br />
2. Improving wound assessment and evaluation<br />
3. Promoting patient partnership<br />
4. Improving multidisciplinary collaboration<br />
within and across services<br />
Meeting the aims of the project was not difficult<br />
because the benefits of digital cameras are plain for<br />
both staff and patients, providing unambiguous<br />
discussion, facilitating patient and staff understanding,<br />
plus instant referral. Whilst the benefits<br />
for utilising this technology are clear, the issues<br />
surrounding the safe handling and storage of data<br />
were a challenge. Different protocols were required<br />
for the various Trust venues and were dependent<br />
on whether computer systems were networked or<br />
linked to GP software; the protocols required for<br />
secure archiving and the associated training will<br />
be presented. This paper also addresses the greatest<br />
challenge of the project, which has proved to be<br />
embedding camera use and the secure archiving of<br />
patient information across the wards and district<br />
nursing teams.<br />
INTRODUCTION<br />
Tower Hamlets Primary Care Trust (THPCT)<br />
has an urban population of 200,000 residents for<br />
whom the District Nursing service is managed<br />
across 17 teams. In addition there are 6 in-patient<br />
wards for Older Peoples services including<br />
four dedicated wound care beds. The Tissue Viability<br />
service works across the Trust and service<br />
boundaries and referrals for wound care advice<br />
and assessments are received by telephone from<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
nursing, medical and allied health professionals.<br />
Guidelines are in place for management of all<br />
wound types and practitioners are expected to<br />
utilise the specific wound, leg ulcer or pressure<br />
ulcer assessment forms.<br />
PROJECT AIMS<br />
Several issues were identified that resulted in the<br />
process of referral, wound assessment and evaluation<br />
not being as robust as they could be, specifically<br />
that:<br />
n Phone referrals and descriptions of the<br />
wound bed could be ambiguous, causing<br />
either a delay in review or an inappropriate<br />
referral.<br />
n Digital cameras were only used by the Tissue<br />
Viability team; Polaroid cameras were used<br />
by some district nursing teams but obtaining<br />
the film was always problematic.<br />
n There was poor wound and surrounding<br />
skin assessment and evaluation.<br />
n There was incomplete wound information<br />
passed between community and rehabilitation<br />
services.<br />
n The patient’s General Practitioner and even<br />
some patients (due to its site) rarely saw the<br />
wounds thereby preventing partnership and<br />
valuable discussion.<br />
Thus the aims of the project were:<br />
1. To reduce delay in diagnosis and referral for<br />
specialist review through email referral and<br />
photography.<br />
2. To improve wound assessment and evaluation<br />
and enhance documentation and team<br />
discussion.<br />
3. To promote patient partnership<br />
4. To improve multidisciplinary collaboration<br />
across and within services<br />
Funding was secured for the provision of digital<br />
cameras and quality colour printers for each District<br />
Nursing team and ward. The aim was for<br />
nursing teams to photograph wounds and email<br />
�<br />
Scientific Article<br />
Alison Hopkins<br />
MSc, DN Cert, RGN.<br />
Clinical Nurse Specialist<br />
(Tissue Viability)<br />
Tower Hamlets Primary<br />
Care Trust<br />
Correspondence:<br />
Tissue Viability<br />
Primary Care<br />
Mile End Hospital<br />
Bancroft Road<br />
London E1 4DG<br />
alison.hopkins@<br />
thpct.nhs.uk
Scientific Article<br />
them to the specialist team for advice and discussion. The<br />
next step was to ensure a correct process for data collection<br />
and storage.<br />
SECURE DATA COLLECTION AND STORAGE<br />
In order to ensure the safe use of digital images, a clear<br />
protocol for use needed to be developed. This was necessary<br />
to enable practitioners to follow a clear process for<br />
image production, storage/archiving and retrieval. This<br />
protocol was based on the THPCT’s guidelines ‘Consent<br />
to Examination and Treatment’ (see original source, Department<br />
of Health guide 1 ). Practitioners needed to be<br />
aware of the legal issues surrounding photographic consent<br />
and the use of the photograph outside patient records, such<br />
as education or publication. [See Box 1]<br />
Box 1<br />
Photographic consent issues<br />
• Informed consent (patient or their relative/carer) can<br />
be obtained through written or verbal means and documented.<br />
• Obtaining consent is a continuous process and not a one<br />
off event.<br />
• Information must be provided: why the photograph is<br />
required, how it will be used, who will see it and how<br />
often photographs may be taken.<br />
• Photographs can be used for education purposes<br />
if the patient cannot be identified.<br />
• Photographs must never be used for publication<br />
without written consent<br />
It is essential that the practitioners were aware that the<br />
photograph is part of the patient’s medical history and<br />
thus must be retrievable at any time. This requires good<br />
0<br />
Fig 1<br />
archiving and images must be saved without alteration.<br />
Records must be kept of the nurse specialist advice given<br />
by phone or email. Thus an email referral form was developed<br />
[Fig 1] that enabled attachment of the photograph<br />
and sections that addressed the assessment and concerns.<br />
The protocol made it explicit that NHS encrypted email<br />
addresses must be used.<br />
One of the problems identified when developing the<br />
protocol was that the IT systems varied across the trust; not<br />
all the nursing teams had access to the GP patient record<br />
systems and thus could not attach the photograph to the<br />
patient’s records. For those teams that were not networked,<br />
we had to ensure that the photographs were not stored on<br />
the computers (in case of theft) and thus had to be deleted<br />
after printing. These variations meant that the protocol<br />
had to be specific to each team’s requirements. However,<br />
this is now no longer an issue because the IT systems have<br />
been standardised across the trust.<br />
Email encryption was also an essential part of ensuring a<br />
secure process. For this reason only trust or NHS servers<br />
must be used. Referrals are usually received by phone in<br />
the specialist service thus it is incumbent on the team to<br />
regularly check emails for referrals. The referring teams<br />
have also been instructed to leave phone messages so that<br />
no delays are incurred.<br />
Two practitioners from each ward or team were trained<br />
in the use of the camera and printer, archiving of photographs<br />
and use and storage of the referral documents.<br />
PROJECT OUTCOMES<br />
The development of protocols and training has enabled<br />
the project aims to be met:<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
1. To reduce delay in diagnosis and<br />
referral for specialist review through<br />
email referral and photography:<br />
With a photograph on the monitor<br />
the ensuing discussion is now based<br />
on what is seen and not imagined!<br />
This has enabled the prompt commencement<br />
of treatment and prioritising<br />
of specialist assessments.<br />
2. To improve wound assessment and<br />
evaluation and enhance documentation<br />
and team discussion: there is<br />
now a clear link to assessment and<br />
evaluation. There is clear evidence of<br />
progress and efficacy of treatment or<br />
deterioration of the wound bed and<br />
surrounding skin. Photographs have<br />
added clarity to team discussions<br />
and aided education.<br />
3. To promote patient partnership: patients<br />
are not always able to see their<br />
wounds, thus digital photography<br />
has promoted understanding, education<br />
and partnership. This outcome<br />
has been of particular benefit as the<br />
immediacy of the image can give<br />
hope and encouragement; patients<br />
like to have their own prints often in<br />
sequence!<br />
4. To improve multidisciplinary collaboration<br />
across and within services:<br />
on discharge or transfer across<br />
services, photography has helped to<br />
improve communication.<br />
DISCUSSION<br />
This project has had successful outcomes<br />
and the tissue viability service has provided<br />
digital cameras and a framework<br />
for their use across the trust. However,<br />
like any new initiative there have been<br />
some challenges that we are still working<br />
on. The greatest challenge to the project,<br />
despite piloting and refining the process,<br />
has been to get some teams to use the<br />
cameras and email referral forms.When<br />
discussing the diffusion of innovation,<br />
Rogers 2 states succinctly that ‘Getting a<br />
new idea adopted, even when it has obvious<br />
advantages, is often very difficult’.<br />
Here, many innovations thus require a<br />
lengthy period before they become widely<br />
adopted. Rogers’ model describes an innovation<br />
curve that separates people into<br />
innovators, early adopters, early majority,<br />
late majority and laggards. Identifying<br />
why we have had so many ‘late majorities’<br />
and laggards can probably be explained<br />
by the poor use of email and computers<br />
by practitioners whose key role is clinical.<br />
This has been identified as a problem<br />
for the trust and is therefore is being<br />
addressed. Despite the enthusiasm for<br />
the cameras and the opportunities this<br />
would bring, it is still another thing for<br />
the clinical staff to do and in a world of<br />
competing priorities camera use is low<br />
in some teams. Thus, the encouragement<br />
and team training continues.<br />
It is worth noting why the trust has<br />
not used camera phones as these are now<br />
in common use and would therefore be<br />
an easier technology to adopt. Firstly, the<br />
cameras were purchased before camera<br />
phones were of a high enough quality.<br />
Secondly, there is the issue of secure archiving<br />
of photographic images; photographs<br />
will be easy to take but not necessarily<br />
downloaded appropriately or the<br />
advice/discussion provided will not be<br />
recorded. The lack of encryption is also<br />
a concern. Given due consideration, cameras<br />
give the trust more control over the<br />
images and so more security.<br />
This paper has presented the development<br />
of a framework that enables digital<br />
images to be recorded within a secure system.<br />
The outcomes have been successful<br />
but, despite the enthusiasm, some practitioners<br />
have been very slow to adopt the<br />
new technology. It is essential that patients<br />
have access to the same assessment,<br />
wound evaluation and referral process<br />
wherever they are in the borough thus<br />
adoption of this new process needs to be<br />
pursued. m<br />
References<br />
1. Department of Health. Good Practice in consent implementation<br />
guide: consent to examination or treatment.<br />
Department of Health. 2001. http://www.dh.gov.uk/<br />
PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/<br />
en?CONTENT_ID=4005762&chk=7ENk2Q (1.12.06)<br />
2. Rogers EM. Diffusion of Innovations. Simon and Schuster<br />
International. 5th Edition. (2003) Page 1<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 1
LESS IS<br />
EXPECT THE MOST<br />
The innovative sorbion sachet S is our modern way to treat moderate to high<br />
exuding wounds with its super absorbent polymers.<br />
The sachet’s osmotic effect ensures rapid absorption of wound fluids – without<br />
drying out the wound. Microorganisms and cell debris are flushed from deep recesses<br />
of the wound and collected in the sorbion sachet S.<br />
This means a better quality of life for the patient. Why? Because the wound is left<br />
undisturbed for a longer period of time, so it is able to heal faster. Therefore<br />
treatment with sorbion sachet S is clearly less expensive than treatment with<br />
other well known wound dressings.<br />
Test sorbion sachet S yourself:<br />
www.sorbion.com or visit us at <strong>EWMA</strong> Conference D1
MORE!<br />
A 10 x 10 cm sorbion sachet S absorbs and binds more than 100 ml!<br />
� The patient gains:<br />
Less pain, more comfort.<br />
� The clinician gains:<br />
Faster healing means, fewer dressing changes,<br />
reduced risks of complications, reduced workload<br />
and recuded costs<br />
� The hospital gains:<br />
Resource demand reduced, faster patient turnaround.<br />
liquid locked<br />
w w w . s o r b i o n . c o m 5224 · www.next-online.com
Contreet / Biatain - Ag<br />
Sustained silver release and<br />
absorption in one dressing<br />
1 Münter K-C et al. Effect of a sustained silver-releasing dressing on ulcers<br />
with delayed healing: the CONTOP study. Journal of Wound Care 2006,<br />
15(5), 199-206.<br />
2 Jørgensen B et al. The silver-releasing foam dressing, Contreet Foam,<br />
promotes faster healing of critically colonised venous leg ulcers: a<br />
randomised, controlled trial. International Wound Journal 2005, 2(1), 64-73.<br />
3 Rayman et al. Sustained silver-releasing dressing in the treatment of<br />
diabetic foot ulcers. British Journal of Nursing 2005, 14(2), 109-114.<br />
4 Ip M et al. Antimicrobial activities of silver dressings: an in vitro comparison.<br />
Journal of Medical Microbiology 2006, 55, 59-63<br />
5 Scanlon E et al. Cost-effective faster wound healing with a sustained<br />
silver-releasing foam dressing in delayed healing leg ulcers - a healtheconomic<br />
analysis. International Wound Journal 2005, 2(2), 150-160.<br />
, Biatain and Contreet are registered trademarks of Coloplast A/S.<br />
© 2007-01/dkcht. All rights reserved Coloplast A/S, 3050 Humlebæk, Denmark.<br />
–<br />
• Contreet / Biatain - Ag reduces the ulcer<br />
area by 45-56% within 4 weeks 1-3<br />
• Contreet / Biatain - Ag kills MRSA faster<br />
than other silver dressings 4<br />
• Contreet / Biatain - Ag provides excellent<br />
exudate management 1-3<br />
• Contreet / Biatain - Ag is a cost-effective<br />
treatment 5<br />
Contreet / Biatain - Ag<br />
Sustained silver release and<br />
absorption in one dressing<br />
Visit<br />
www.woundcare.evidence.coloplast.com<br />
to fi nd all peer-reviewed clinical, laboratory<br />
and health-economic evidence for Coloplast wound dressings.<br />
Faster wound healing<br />
by reducing the barriers<br />
to wound healing
The use of telemedicine<br />
in wound care<br />
Most patients suffering from chronic<br />
wounds are attended to by local district<br />
nurses and may geographically be<br />
far away from specialist centres. A need for specialist<br />
advice may, however, turn up often resulting<br />
in a tedious process for the patient. A remission<br />
note is forwarded to the hospital and the patient is<br />
allocated an appointment, perhaps days or weeks<br />
later in the outpatient clinic. During the waiting<br />
time the wound may have worsened and become<br />
more resistant to treatment.<br />
To deal with this, we have introduced telemedicine<br />
in Soenderjylland, Denmark, as a tool to<br />
communicate, in a fast way, between the wound<br />
care nurses in the local communities and the hospitals.<br />
This concept we have named “Saar-I-Syd”<br />
(“Wounds-in-the South”).<br />
We applied the experiences, from two PhD<br />
projects based in the Department of Endocrinology<br />
M, Aarhus Universityhospital and Centre<br />
for Pervasive Health Care, Alexandra Instituttet,<br />
ISIS Katrinebjerg, Aarhus. In these studies the<br />
technology was developed and tested 1 . In the sec-<br />
Fig 1.<br />
The set-up, diagram<br />
ond study 2 local district nurses in Aarhus participated<br />
in the development of a real-time on-line<br />
teleconsultation, which was proven to be fully<br />
exchangeable to a standard in-hospital consultation.<br />
In “Saar-I-Syd” the web-based database was<br />
adapted to our needs through collaboration with<br />
the software company Dansk Telemedicin A/S.<br />
Telemedical consulations are now used in Soenderjylland<br />
(220.000 inhab.) as an interdisciplinary<br />
tool to remit patients with venous leg ulcers, arterial<br />
ulcers, diabetic foot ulcers, pressure sores<br />
and inflammatory ulcers to the specialists in the<br />
hospitals, to communicate between the different<br />
sectors, thus avoiding visits to the outpatient<br />
clinic, to control quality of the treatment given<br />
and to support the district nurses in their handling<br />
of the patients with chronic wounds.<br />
HOW IS THIS DONE?<br />
When the district nurse sees a patient with a<br />
chronic wound, the patient is registered in our<br />
web-based electronic database. Only healthcare<br />
�<br />
Background Article<br />
Rolf Jelnes, MD1<br />
Niels Ejskjaer, MD 2<br />
1 Saar-I-Syd,<br />
Department of<br />
Vascular Surgery,<br />
Sygehus Soenderjylland,<br />
Aabenraa,<br />
Denmark<br />
2 Diabetic Foot Centre,<br />
Department of Medicine M,<br />
Aarhus University Hospital,<br />
Denmark<br />
rolf.jelnes@get2net.dk<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 5
Background Article<br />
Fig 2. Screendisplay – part of Wound Assessment table Fig 3. Reduction in wound area over time – quality control<br />
professionals, chosen from the list in the database, have access<br />
to the data and the patients give informed consent.<br />
The following data are submitted: personal identification,<br />
medication, concurrent disease, allergy, duration of<br />
wound and a description of the wound. Ankle pressure<br />
and ABI is measured, investigations for neuropathy such<br />
as monofilament and tip term are performed and data<br />
on hgb1ac and swabs are entered and other parameters<br />
relevant for that particular wound.<br />
The district nurse uses a mobile phone to take a photo<br />
of the wound and sends this photo electronically to the<br />
web-based database. We use the N73 with 3.2 megapixels,<br />
giving us photos of outstanding quality. At the same time<br />
data on the treatment of the wound is recorded – wound<br />
status, wound size, the surrounding skin, pain at change<br />
of bandage and during the day – type and VAS. The type<br />
of treatment is entered – debridement – product-compression-pressure<br />
relief etc. All this can be done in the home of<br />
the patients using the mobile telephone and an electronic<br />
pen. A preliminary diagnosis is made.<br />
Finally, the district nurse decides to whom information<br />
is to be submitted. A choice has to be made weather it is<br />
routine or calling for an urgent answer.<br />
The specialists get the information by an sms on their<br />
mobile telephone, indicating that new information has<br />
been entered the database. This means, that advice can be<br />
given, in case of an urgent problem if e.g. the specialist is<br />
attending a conference in South Africa. The only need is<br />
access to the web.<br />
By looking at the data, compression therapy can be prescribed<br />
and, if necessary, a future appointment to the<br />
outpatient’s clinic can be forwarded on the same day,<br />
– typically for duplex scanning of the veins, toe pressure<br />
measurement or a consultation at a chiropodist. Further<br />
medical advice such as glycaemia control is submitted at<br />
the same time.<br />
6<br />
We have now worked with this system for 12 months. 270<br />
patients are now registered in our database. Our personal<br />
experience, working with telemedicine, is as follows:<br />
n A proper diagnosis is made at an early stage<br />
n Adequate treatment – conservative and surgical<br />
– can be started much earlier than previously, thus<br />
shortening the wound treatment period.<br />
n In cases of wound deterioration the patients can<br />
be seen on the same day and an evaluation can be<br />
made.<br />
n Fewer visits to the outpatient’s clinic, as we do not<br />
need to see those patients, which heal according to<br />
our standard.<br />
n Much less troublesome for the patients, as they can<br />
stay in their own surroundings<br />
n Specialist support to the districts nurses, thus improving<br />
their skills – education.<br />
Once the wound is healed, a decision is made on when to<br />
follow up on the recommendations given. This is done by<br />
a notification from the database to the mobile telephone<br />
to the district nurse 14 days prior to the decided followup<br />
time.<br />
We are still working on improving our set-up – i. e.: communication<br />
systems to the GP’s, district nurses records as<br />
well as healthcare economic expenses.<br />
In conclusion, our set-up based on an electronic webbased<br />
wound care record, to which all medical staff have<br />
access, is simple to work with and reliable. We are aware,<br />
that our statements concerning our experiences are undocumented.<br />
Documentation will follow at a later stage.<br />
m<br />
References<br />
1. Larsen SB, Clemensen J, Ejskjaer N. UMTS and telemedicine: a feasibility study.<br />
Accepted for publication oct 2006 J Telem Telecare<br />
2. Clemensen J, Larsen SB, Ejskjaer N. Telemedical treatment at home of diabetic<br />
foot ulcers. J Telem Telecare. 2005;11 Suppl 2:S14-6.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Lohmann & Rauscher<br />
GmbH & Co. KG<br />
P.O.Box 23 43<br />
D-56513 Neuwied<br />
www.lohmann-rauscher.com<br />
Natural HydroBalance.<br />
Simple. Unique!<br />
Suprasorb ® X controls the moisture content<br />
of lightly to moderately exuding wounds.<br />
32097/1206/e<br />
HEALING · PROTECTING · PROVIDING CARE<br />
Suprasorb ® X is able to absorb and release moisture.<br />
Exactly as required. Independently. Simultaneously.<br />
Through its unique structure of biosynthetic HydroBalance fibres.<br />
Suprasorb ® For infected wounds:<br />
X + PHMB<br />
Suprasorb ® X<br />
The intelligent one<br />
among the wound dressings.
SILVERCEL* dressing uses new hydro-alginate technology to complement the effectiveness of silver release. It is a dressing that becomes stronger as it<br />
absorbs, facilitating removal from the wound. Clinically tested, SILVERCEL* dressing encourages healing even in very wet wound situations by providing<br />
an optimal moist wound environment. The sustained and balanced release of silver ions kills a broad spectrum of microorganisms associated with the<br />
bacterial colonization and infection of wounds, including MRSA, MRSE and VRE.<br />
Progressive Strength<br />
S 02 04 - * Trademark of Johnson & Johnson - X-STATIC is a registered Trademark of Noble Fiber Technologies Inc
Lord Joseph Lister:<br />
the rise of antiseptic surgery and<br />
the modern place of antiseptics<br />
in wound care<br />
Evidence, Consensus and Driving the Agenda forward<br />
<strong>EWMA</strong> Glasgow 2-4 May 2007<br />
David leaper gives us his views on<br />
Lord Lister and the role of antiseptics<br />
in current surgical practice.<br />
INTRODUCTION<br />
It is appropriate to remember Lord Joseph Lister<br />
as the European Wound Management Association<br />
comes to Glasgow for its annual meeting in<br />
May of 2007. It was here in Glasgow that the<br />
world witnessed the birth of antiseptic surgery<br />
which was introduced by Lister in the 1860s.<br />
Although antiseptic surgery was superseded by<br />
aseptic surgery, because of its toxicity to operating<br />
theatre personnel as well as the patients’ tissues,<br />
it was a major breakthrough in infection control<br />
at the time. All forms of surgery, but particularly<br />
trauma surgery which Lister specialised in, were<br />
prone to high morbidity and mortality in relation<br />
to surgical site infection 1 . Nevertheless, there is<br />
a still a major role for the use of antiseptics in<br />
wound care, which will have to be reconsidered on<br />
a more widespread basis, as the overuse of antibiotic<br />
therapy is threatening to produce increasing<br />
numbers of resistant and emerging bacteria. There<br />
is some evidence that any microbial resistance has<br />
developed against antiseptics but this is limited,<br />
probably as their action is so general and multifaceted<br />
on bacteria, fungi and viruses as well as<br />
spores.<br />
LORD LISTER<br />
Joseph Lister was born in Essex in 1827 and later<br />
entered University College London as a medical<br />
student where he qualified in 1852. He almost<br />
certainly saw Robert Liston undertake one of the<br />
first amputations there under ether anaesthesia.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
For the first time such operations could be undertaken<br />
without the need for excessive speed<br />
with a patient held down by several burly theatre<br />
attendants, and allowed time for a more careful<br />
procedure! 1<br />
After qualification Lister went to Edinburgh<br />
where he was apprenticed to the famous surgeon<br />
James Syme, who was obviously another surgeon<br />
adept at amputation as he has an eponymous operation<br />
named after him for amputation of the<br />
foot. It is clear that Lister made a good impression<br />
as he was appointed to the Regius Chair of<br />
Surgery in Glasgow in 1860 where he laid down<br />
his foundations of antiseptic surgery. His ability<br />
to impress continued and he was subsequently<br />
appointed as Professor of Clinical Surgery in Edinburgh<br />
in 1869 and ended his clinical career in<br />
the Chair of Surgery at Kings College Hospital in<br />
London 1 . Throughout his life his clinical practice<br />
was really that of an orthopaedic/trauma surgeon<br />
(see figure 1). He contributed to surgical education<br />
and for a time was a member of <strong>Council</strong> of<br />
the Royal College of Surgeons of England.<br />
Lister was honoured further with the award of<br />
a Baronetcy in 1883; he became a Lord in 1897<br />
and was awarded the Order of Merit. He died in<br />
1912 and has a superb public monument left to<br />
his memory in Portland Place in London 2 .<br />
It is interesting to speculate how he devised the<br />
concept of antiseptic surgery. At the time postoperative<br />
infection was rife after the increasingly<br />
ambitious elective surgery, and particularly after<br />
trauma, and was attended by a high complication<br />
rate and mortality. Apparently the public<br />
engineers of Carlisle had taken up the concept,<br />
presumably from their contemporaries in Paris,<br />
�<br />
Background Article<br />
David Leaper<br />
Professor<br />
Wound Healing<br />
Research Unit<br />
University of Wales<br />
College of Medicine<br />
Cardiff<br />
Wales<br />
profdavidleaper@<br />
doctors.org.uk
Background Article<br />
Figure 1. Lord Lister on a ward round<br />
of treating stinking sewage with phenol. Lister became<br />
aware of this and visited Carlisle 2 . One wonders whether<br />
he subsequently may have had some similar thoughts<br />
when walking along the Clyde, which would have been a<br />
similarly unpleasant experience in those days. He was also<br />
aware of the contemporary work of Louis Pasteur; only<br />
a Frenchman would have made the connection between<br />
the spoiling of wine to vinegar because of the recently<br />
recognised, offending bacteria and not simply exposure<br />
to air as was generally thought 2 . Whatever the train of<br />
thought was he brilliantly realised that the destruction of<br />
bacteria, rather than their exclusion which was to come<br />
later as aseptic surgery, from an operative or traumatic<br />
site might reduce the risk of infection. His hypothesis<br />
proved correct.<br />
Lister’s next patient was a boy of 11 years who had suffered<br />
a compound fracture of his left leg. He was treated with<br />
undiluted “carbolic” to all parts of the wound of the leg,<br />
which was simply splinted. The wound was treated with<br />
similar dressings and splits and the patient walked out of<br />
the hospital some six weeks later. A second 32 year old<br />
male patient with a compound fracture of the thigh was<br />
similarly and successfully treated. 3 Before too long the<br />
operating theatre in Glasgow was witnessing the introduction<br />
of 1:20 carbolic hand washing, skin preparation and<br />
of course the famous carbolic spray which can still be seen<br />
at the Royal College of Surgeons of England in London.<br />
The operating theatre environment could not have been<br />
pleasant and certainly would not have impressed modern<br />
theatre managers and health and safety committees.<br />
0<br />
The success of these measures was nevertheless spectacular.<br />
Between 1864-1866 there had been 16 deaths after<br />
35 amputations (a 46% mortality) and between 1867-<br />
1870, after introduction of antiseptic surgery, there were<br />
6 deaths after 40 operations (a 15% mortality). (I make<br />
that statistically significant; Yates’ X 2 , p
Secure fixation when<br />
you and your patients<br />
need it most<br />
For decades, the Mepore ® name has been synonymous with trusted, easy-to-use dressings that<br />
are gentle to the skin. Now we are introducing Mepore ® IV – the latest addition to the Mepore range.<br />
It is a high performance self-adhesive film dressing, designed specifically for secure fixation of<br />
intravascular catheters.<br />
Mepore IV gives you a cost-effective solution that you can rely on. What’s more, it is easy to apply.<br />
For non-ported catheter fixation, use Mepore ® Film (formerly known as Mefilm). Together,<br />
Mepore IV and Mepore Film give you a complete fixation solution for most of your IV/catheter needs.<br />
The symbol and the word mark are both registered trademarks or trademark pendings of Mölnlycke Health Care.<br />
Mölnlycke Health Care AB (publ.), Box 13080, SE-402 52 Göteborg, Sweden. Phone + 46 31 722 30 00. www.molnlycke.com<br />
Even better than you think<br />
H087510701
Background Article<br />
Alcoholic hand rubs have largely replaced antiseptic solutions<br />
for the infection control process against MRSA.<br />
However, they are no substitute for hand washing in soap<br />
and water, or an aqueous antiseptic solution, with adequate<br />
hand drying during an epidemic of Clostridium difficile<br />
enteritis, when patients are in isolation.<br />
It is difficult to understand why dilute aqueous antiseptics<br />
have fallen out of favour for lavage in surgery,<br />
for example as a peritoneal lavage for faecal peritonitis.<br />
It is probably related to a perceived impression of local<br />
and systemic toxicity, particularly with regard to povidone<br />
iodine. In fact allergy is rare and the reports of thyroid<br />
dysfunction sporadic and probably unjustified. It must be<br />
remembered that antiseptics have had little, if any proven,<br />
resistance shown following their use. With the rise of antibiotic<br />
resistance and emergence then a whole rethink<br />
about antiseptic use may have to be made.<br />
Antibiotic impregnation of surgically-implanted, prosthetic<br />
devices and intravascular catheters may also have to<br />
be reconsidered for these same reasons of antibiotic resistance.<br />
Nevertheless some type of antimicrobial prophylaxis<br />
must be used as infection of a vascular or orthopaedic<br />
prosthesis can be a disaster. The recent introduction of<br />
a widely used and safe antiseptic, triclosan, into sutures<br />
for widespread surgical practice, for example, holds great<br />
promise for the prevention of postoperative infection. The<br />
incidence of surgical site infection (SSI) has been found to<br />
be high, with attendant increased healthcare costs, when<br />
appropriate post discharge surveillance is undertaken 6 . A<br />
move away from antibiotic prophylaxis, particularly in<br />
clean surgery where its use is unclear anyway, or for inappropriate<br />
treatment of SSIs has to be welcomed. However,<br />
there is unquestioned value with level I evidence,<br />
of antibiotic prophylaxis in the clean-contaminated and<br />
contaminated categories of surgical operations and this<br />
should not be discarded 7 .<br />
In chronic wound care the use of antiseptics has been<br />
and continues to be controversial. There was a time when<br />
hypochlorite solutions were widely used in open wound<br />
management, including acute wounds such as abscess cavities,<br />
and chronic wounds such as pressure sores and leg<br />
ulcers. Their use for debridement, and preparation of a<br />
recipient wound bed for split thickness grafting, still has<br />
their advocates. However, it is widely held that these agents<br />
should not be used in routine wound management at all<br />
and reserved for their unquestioned role as disinfectants<br />
for clinical surfaces and lavatory seats, and sterilising babies’<br />
bottles 8 .<br />
The emergence of antibiotic resistance is a reason to turn<br />
back to the safe use of the aqueous antiseptics, such as povidone<br />
iodine and chlorhexidine, for wound cleansing and<br />
the reduction of bacterial colonisation of open wounds.<br />
These antiseptics have a role as prophylactics against critical<br />
colonisation and invasive infection. Thereby antibiotic<br />
use may be avoided altogether or be reserved for their use<br />
in treating spreading infection, particularly when there are<br />
systemic signs and the patient needs admission to hospital.<br />
There are entirely adequate and more effective alternatives<br />
to disinfectants such as the hypochlorites for debridement,<br />
and a wider use of topical antiseptics is inevitable if antibiotics<br />
are to be used less. 9<br />
One of the difficulties of antiseptic-impregnated surgical<br />
dressings relates to the fact that most antiseptics are<br />
rapidly inactivated on contact with body fluids, exudate<br />
and necrotic tissue. Slow-release povidone iodine dressings<br />
are already available and their effectiveness is being<br />
improved and, together with the recent introduction of<br />
silver-containing dressings, overcome this disadvantage.<br />
These dressings also offer a barrier to transmission of resistant<br />
of resistant organisms 10 .<br />
Lord Lister would probably be pleased to know that antiseptics<br />
not only have a continued role in modern clinical<br />
practice, but also that their contribution, particularly in<br />
surgery and wound management, is likely to increase.<br />
m<br />
References<br />
1. Fisher RB. Joseph Lister 1827-1912. Macdonald and James, London. 1977<br />
2. Ellis H. The first antiseptic operations (1867). In: Surgical Case Histories of the Past.<br />
Royal Society of Medicine Press, London. 1994<br />
3. Lister J. On a new method of treating compound fracture, abscess, etc, with observations<br />
on the conditions of suppuration. Lancet 1867; 1: 326<br />
4. de Lalla F. Surgical prophylaxis in practice. J Hosp Infect 2002; 50(Suppl A): S9<br />
- S12. Edwards P S, Lipp A, Holmes A. Preoperative skin antiseptics for preventing<br />
surgical wound infections after clean surgery. Cochrane Database Syst Rev. 2004<br />
(3):CD003949.<br />
6. Leaper DJ, van Goor H, Reilly J, Petrosillo N, Geiss HK, Torres AJ, Berger A. Surgical<br />
site infection – a European perspective of incidence and economic burden. International<br />
Wound Journal 2004; 1: 247-273<br />
7. Wong PF, Gilliam AD, Kumar S, Shenfine J, O’Dair GN, Leaper DJ. Antibiotic<br />
regimens for secondary peritonitis of gastrointestinal origin in adults. Cochrane<br />
Database of Systematic Reviews 2005; 2: CD004539<br />
8. Leaper DJ. Eusol. Editorial. British Medical Journal 1992; 304:930-931<br />
9. Teot L, Coessens B, Cooper R, Flour M, Gryson L, Henry F, Lachapelle J-M, Lamme<br />
E, Leaper DJ, Lubbers M, Magliaro A, Meaume S, Monstrey S, Pierard GE, Scuderi<br />
N, Van den Bulck R, Vermassen F, Vranckx JJ. Wound Management. Changing<br />
ideas on antiseptics. De Coker Belgium 2004<br />
10. Leaper DJ. Silver dressings; their role in wound management International wound<br />
Journal 2006; 3: 282-294<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
�����������������������<br />
��������������������<br />
����������������������������<br />
�������������������������������<br />
���������������������������������������������������������������
EBWM<br />
Sally Bell-Syer, MSc<br />
Review Group Co-ordinator<br />
Cochrane Wounds Group<br />
Department of<br />
Health Sciences<br />
Area 4<br />
Seebohm Rowntree<br />
Building<br />
University of York<br />
York,<br />
United Kingdom<br />
sembs1@york.ac.uk<br />
ABSTRACTS OF RECENT<br />
COCHRANE REVIEWS<br />
Topical agents and dressings for<br />
fungating wounds [Review]<br />
Adderley U, Smith R<br />
The Cochrane Database of Systematic Reviews<br />
Copyright © 2005 The Cochrane Collaboration.<br />
Published by John Wiley & Sons, Ltd.2007 Issue2.<br />
ABSTRACT<br />
Background: Fungating wounds arise from primary,<br />
secondary or recurrent malignant disease and are<br />
associated with advanced cancer. A small proportion of<br />
patients may achieve healing following surgical excision<br />
but treatment is usually palliative. Fungating<br />
wound management usually aims to slow disease<br />
progression and optimise quality of life by alleviating<br />
physical symptoms, such as copious exudate, malodour,<br />
pain and the risk of haemorrhage, through<br />
appropriate dressing and topical agent selection.<br />
Objectives: To conduct a systematic review of the<br />
evidence of the effects of dressings and topical agents<br />
on quality of life and symptoms that impact on quality<br />
of life in people with fungating malignant wounds.<br />
Search strategy: We searched the Cochrane Central<br />
Register of Controlled Trials (CENTRAL) and the<br />
Wounds Group Specialised Register in August 2006.<br />
The Cochrane Breast Cancer Group and the Pain and<br />
Palliative Care Group were contacted for relevant<br />
studies. The Allied and Complementary Medicine<br />
(AMED) database was searched in January 2007.<br />
There was no restriction on language or date of publication.<br />
Selection criteria: Randomised controlled trials (RCTs)<br />
or, in their absence, controlled clinical trials (CCTs)<br />
with a concurrent control group, both published and<br />
unpublished, and written in any language, were eligible<br />
for inclusion.<br />
Data collection and analysis: Data extraction was<br />
undertaken by one author and checked for accuracy<br />
by a second author. Two review authors independently<br />
assessed trial quality.<br />
Main results: Two trials involving 63 people were<br />
included. One RCT in women with superficial breast<br />
lesions compared 6% miltefosine solution with placebo<br />
and found that miltefosine delayed tumour progression.<br />
However, this trial had methodological limitations.<br />
A second trial compared topical metronidazole with<br />
placebo and found that metronidazole reduced<br />
malodour. However, this trial also had methodological<br />
limitations and was underpowered.<br />
Authors’ conclusions: There is weak evidence from one<br />
small trial that 6% miltefosine solution applied topically<br />
to people with superficial fungating breast lesions<br />
(smaller than 1cm) who have received either previous<br />
radiotherapy, surgery, hormonal therapy or chemotherapy<br />
for their breast cancer may slow disease<br />
progression. There is insufficient evidence in this review<br />
to give a clear direction for practice with regard to<br />
improving quality of life or managing wound symptoms<br />
associated with fungating wounds. More research is<br />
needed.<br />
Synopsis<br />
Fungating wounds sometimes occur in people with<br />
advanced cancer. Care usually aims to slow down<br />
disease progression and improve quality of life by<br />
relieving physical symptoms using appropriate dressings<br />
and other applied treatments.<br />
There is weak evidence to suggest that patients with<br />
superficial fungating breast lesions (smaller than 1cm)<br />
who have received either previous radiotherapy, surgery,<br />
hormone therapy or chemotherapy for their breast<br />
cancer may extend the time to disease progression by<br />
receiving topical 6% miltefosine solution. There is<br />
insufficient evidence to direct practice with regard to<br />
improving quality of life or managing other wound<br />
symptoms associated with fungating wounds.<br />
Preoperative bathing or showering with<br />
skin antiseptics to prevent surgical site<br />
infection [Review]<br />
Webster J, Osborne S<br />
The Cochrane Database of Systematic Reviews<br />
Copyright © 2005 The Cochrane Collaboration.<br />
Published by John Wiley & Sons, Ltd.2007 Issue2.<br />
ABSTRACT<br />
Background: Surgical site infections (SSIs) are wound<br />
infections that occur after invasive (surgical) procedures.<br />
Preoperative bathing or showering with an antiseptic<br />
skin wash product is a well-accepted procedure for<br />
reducing skin bacteria (microflora). It is less clear<br />
whether reducing skin microflora leads to a lower<br />
incidence of surgical site infection.<br />
Objectives: To review the evidence for preoperative<br />
bathing or showering with antiseptics for the prevention<br />
of hospital-acquired (nosocomial) surgical site infection.<br />
Search strategy: We searched the Cochrane Wounds<br />
Group Specialised Register (December 2005),<br />
the Cochrane Central Register of Controlled Trials<br />
(The Cochrane Library Issue 4, 2005),<br />
MEDLINE (January 1966 to December 2005) and<br />
reference lists of articles.<br />
�<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
COPA<br />
Ultra-soft foam wound dressing<br />
• Super absorbency<br />
• Ultra Softness and superior feel<br />
• Maximum protection<br />
1.5<br />
1.25<br />
1<br />
0.75<br />
0.5<br />
0.25<br />
0<br />
Fluid capacity (cc/cm 2 )<br />
1.24<br />
0.74<br />
COPA Allevyn ® Polymem ®<br />
www.copadressing.com<br />
0.43<br />
COPA’s fluid capacity outperforms the leading competition<br />
Tyco Healthcare UK Limited - 154 Fareham Road - GOSPORT - HAMPSHIRE<br />
UK - PO13 0AS - Tel: +44 (0) 1329 224 411 - Fax: +44 (0) 1329 224 390<br />
Allevyn is a trademark of Smith & Nephew. Polymem is a trademark of Fleming Medical Limited.<br />
Trademark of Tyco Healthcare Group LP or its affiliate © 2006 Tyco Healthcare Group LP. All rights reserved. P-WC-A-Copa/GB
Selection criteria: Randomised controlled trials comparing any<br />
antiseptic preparation used for preoperative full-body bathing or<br />
showering with non-antiseptic preparations in patients undergoing<br />
surgery.<br />
Data collection and analysis: Two authors independently<br />
assessed studies for selection, trial quality and extracted data.<br />
Study authors were contacted for additional information.<br />
Main results: Six trials involving a total of 10,007 participants<br />
were included. Three of the included trials had three comparison<br />
groups. The antiseptic used in all trials was 4% chlorhexidine<br />
gluconate (Hibiscrub). Three trials involving 7691 participants<br />
compared chlorhexidine with a placebo. Bathing with chlorhexidine<br />
compared with a placebo did not result in a statistically<br />
significant reduction in SSIs; the relative risk of SSI (RR) was<br />
0.91 (95% confidence interval (CI) 0.80 to 1.04). When only<br />
trials of high quality were included in this comparison, the RR of<br />
SSI was 0.95 (95%CI 0.82 to 1.10). Three trials of 1443 participants<br />
compared bar soap with chlorhexidine; when combined<br />
there was no difference in the risk of SSIs (RR 1.02, 95% CI 0.57<br />
to 1.84). Two trials of 1092 patients compared bathing with<br />
chlorhexidine with no washing, one large study found a statistically<br />
significant difference in favour of bathing with chlorhexidine<br />
(RR 0.36, 95%CI 0.17 to 0.79). The second smaller study<br />
found no difference between patients who washed with chlorhexidine<br />
and those who did not wash preoperatively.<br />
Authors’ conclusions: This review provides no clear evidence of<br />
benefit for preoperative showering or bathing with chlorhexidine<br />
over other wash products, to reduce surgical site infection.<br />
Efforts to reduce the incidence of nosocomial surgical site infection<br />
should focus on interventions where effect has been demonstrated.<br />
Synopsis<br />
It is unclear whether using chlorhexidine for preoperative<br />
bathing or showering prevents surgical site infection.<br />
Surgical site infection is a serious complication of surgery and<br />
may be associated with increased length of hospital stay for the<br />
patient and higher hospital costs. The use of an antiseptic solution<br />
for pre-operative bathing or showering is widely practiced<br />
in the belief that it will help to prevent surgical site infection.<br />
However, the review found six trials that included over 10,000<br />
patients that did not show clear evidence of benefit for the use<br />
of chlorhexidine solution over other wash products.<br />
Skin grafting for venous leg ulcers [Review]<br />
Jones JE, Nelson EA<br />
The Cochrane Database of Systematic Reviews<br />
Copyright © 2005 The Cochrane Collaboration.<br />
Published by John Wiley & Sons, Ltd.2007 Issue2.<br />
ABSTRACT<br />
Background: Venous leg ulceration is a recurrent, chronic,<br />
disabling condition. It affects up to one in 100 adults at some<br />
time. Standard treatments are simple dressings and compression<br />
bandages or stockings. Sometimes, despite treatment, ulcers<br />
remain open for months or years. Sometimes skin grafts are<br />
used to stimulate healing. These may be taken, or grown into a<br />
dressing, from the patient’s own uninjured skin (autografts), or<br />
6<br />
EBWM<br />
applied as a sheet of bioengineered skin grown from donor cells<br />
(allograft). Preserved skin from other animals, such as pigs, has<br />
also been used (xenografts).<br />
Objectives: To assess the effect of skin grafts for treating venous<br />
leg ulcers.<br />
Search strategy: We searched the Cochrane Wounds Group<br />
Specialised Register (February 2006) and the Cochrane Central<br />
Register of Controlled Trials (The Cochrane Library, Issue 1,<br />
2006).<br />
Selection criteria: Randomised controlled trials (RCTs) of skin<br />
grafts in the treatment of venous leg ulcers.<br />
Data collection and analysis:<br />
Two reviewers independently undertook data extraction and<br />
assessment of study quality.<br />
Main results<br />
We identified 15 trials – generally of poor methodological quality<br />
– involving 768 participants. In 11 trials participants also<br />
received compression bandaging. One trial (31 participants)<br />
compared a dressing with an autograft. Three trials (74 participants)<br />
compared frozen allografts with dressings, and three trials<br />
(47 participants) compared fresh allografts with dressings. Two<br />
trials (345 participants) compared tissue-engineered skin (bilayer<br />
artificial skin) with a dressing. In two trials (71 participants) a<br />
single-layer dermal replacement was compared with standard<br />
care. Four trials compared skin grafting techniques: one trial<br />
(92 participants) compared autografts with frozen allograft, a<br />
second (51 participants) compared a pinch graft (autograft)<br />
with a porcine dermis (xenograft), the third (seven participants,<br />
12 ulcers) compared tissue-engineered skin with a split-thickness<br />
graft, the fourth (10 participants) compared a fresh allograft<br />
with a frozen allograft.<br />
The trials comparing bilayer artificial skin with a dressing<br />
reported a significantly higher proportion of ulcers healing with<br />
artificial skin. There was not enough evidence from the other<br />
trials to determine whether other types of skin grafting increased<br />
the healing of venous ulcers.<br />
Authors’ conclusions:<br />
Bilayer artificial skin, used in conjunction with compression<br />
bandaging, increases the chance of healing a venous ulcer<br />
compared with compression and a simple dressing. Further<br />
research is needed to assess whether other forms of skin grafts<br />
increase ulcer healing.<br />
Synopsis<br />
Applying bilayered tissue-engineered skin under compression<br />
improves healing of venous leg ulcers compared with simple<br />
dressings and compression, but the effect of other types of graft<br />
is not clear.<br />
Approximately 1% of people in industrialised countries have a<br />
leg ulcer at some time, mainly caused by poor blood flow back<br />
from the legs towards the heart. Skin grafts, either using the<br />
patient’s own skin or donor skin/cells, have been evaluated to<br />
see whether they improve the healing of ulcers. The review of<br />
trials found evidence that tissue-engineered skin composed of<br />
two layers increases the chance of healing. There was not<br />
enough evidence to recommend any other type of graft, and<br />
further research is required.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Prof. Christine Moffatt<br />
<strong>EWMA</strong> Position<br />
Document Editor<br />
Director,<br />
Centre for Research<br />
and Implementation<br />
of Clinical Practice<br />
Christine.Moffatt@<br />
exchange.tvu.ac.uk<br />
Correspondence to:<br />
Kathy Day<br />
MEP Ltd,<br />
53 Hargrave Road,<br />
London N19 5SH<br />
kday@mepltd.co.uk<br />
<strong>EWMA</strong> Position Document 2007:<br />
Topical Negative Pressure<br />
in Wound Management<br />
More than a decade after pioneering<br />
researchers experimented with crude<br />
suction apparatus to promote wound<br />
healing, topical negative pressure (TNP) therapy<br />
has revolutionised the field of wound management.<br />
TNP therapy substantially broadens the<br />
scope of treatment and has rapidly become a<br />
first-line intervention for a wide range of complex<br />
wounds. This important development in wound<br />
care is being shown in a growing number of randomised<br />
controlled trials, as well as case studies,<br />
to produce dramatic improvements in clinical<br />
outcomes such as healing rates, hospitalisations<br />
and, in the case of mediastinitis and the open abdomen,<br />
mortality.<br />
The indications and advantages of TNP therapy<br />
have been reviewed extensively (Box 1), however<br />
there remains a crucial need for a better understanding<br />
of when and how to effectively integrate<br />
this therapy into clinical practice.<br />
Box 1<br />
Studies using TNP therapy in various wound types<br />
n Burn wounds 1<br />
n Chronic leg ulcers 2<br />
n Diabetic foot ulcers 3<br />
n Open abdomen including<br />
management of fistulae 4<br />
n Pressure ulcers 5<br />
n Securing a skin graft 6<br />
n Sternal wound infections 7<br />
n Surgical, non-healing wounds 8<br />
n Trauma 9<br />
With these issues in mind, the 2007 <strong>EWMA</strong> position<br />
document – Topical negative pressure in<br />
wound management – presents a European perspective<br />
on the pathophysiological effects and the<br />
technical and practical issues involved in using<br />
TNP therapy. The aim is to provide insights into<br />
the use of the intervention in the clinical setting,<br />
and to enable healthcare professionals to select<br />
and apply therapy safely. The document is published<br />
in five languages (Figure 1) and is available<br />
online at: www.ewma.org.<br />
It should be noted that most clinical trials of TNP<br />
therapy have used the vacuum assisted closure<br />
(V.A.C. ® Therapy) system and therefore it is this<br />
specific device that is described throughout the<br />
document.<br />
In the first of the four papers presented, Gustafsson,<br />
Sjögren and Ingemansson set the scene<br />
by outlining the historical development of TNP<br />
therapy and describing the key components of<br />
the VAC system.<br />
Although TNP therapy has obvious clinical advantages,<br />
it is often considered expensive compared<br />
with alternative options and this may have been<br />
a barrier to its use, particularly in community set-<br />
Figure 1. The 2007 <strong>EWMA</strong> position document is available<br />
in five languages.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Figure 2. Patient and wound specific issues and the role of TNP therapy<br />
tings. Trueman therefore puts forward an economic case<br />
for the intervention in the second paper of the document.<br />
He proposes that we consider the factors listed in Box 2<br />
when analysing the true cost of dressings. He shows that<br />
these may often be sufficient to offset the higher acquisition<br />
costs of the VAC dressings.<br />
Box 2<br />
Factors affecting the cost of wound treatment<br />
The cost of managing chronic wounds<br />
can be influenced by:<br />
n Frequency of dressing changes and<br />
associated nurse time<br />
n Healing rates<br />
n Impact on hospitalisations and adverse events<br />
In the third paper Vowden, Téot and Vowden present a<br />
general therapeutic strategy (using the concept of wound<br />
bed preparation) that can be applied to many different<br />
wound types to help clinicians identify when to use TNP<br />
therapy and how to integrate the technique into overall<br />
wound management (Figure 2). In doing so they stress that<br />
if selected it must be introduced with defined treatment<br />
objectives and clinical endpoints.<br />
For treatment to be safe and effective, however, it is important<br />
to understand how the specific requirements of<br />
individual wound types may affect the application of TNP<br />
therapy. In the final paper, Wild uses the management<br />
of the open abdomen to demonstrate this point. TNP<br />
therapy in this context is effective because it offers the<br />
advantages of the traditional open abdomen technique<br />
while preventing many of the complications.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2<br />
<strong>EWMA</strong><br />
This <strong>EWMA</strong> position document is published at a time<br />
when treatment initiatives in wound care are extremely<br />
common and the requirements of healthcare professionals<br />
and patients are equally challenging. The information<br />
provides a sound overview of TNP therapy, which – in the<br />
hands of clinicians with appropriate, up-to-date knowledge<br />
and practical skills – is producing impressive results<br />
in a variety of wound types. The task now is to ensure that<br />
all suitable patients benefit maximally from its use, both in<br />
the hospital and community setting. m<br />
References<br />
1. Kamolz LP, Andel H, Haslik W, et al. Use of subatmospheric pressure therapy to prevent<br />
burn wound progression in human: first experiences. Burns 2004; 30(3): 253-58.<br />
2. Vuerstaek JD, Vainas T, Wuite J, et al. State-of-the-art treatment of chronic leg ulcers:<br />
a randomized controlled trial comparing vacuum-assisted closure (V.A.C.)<br />
with modern wound dressing. J Vasc Surg 2006; 44(5): 1029-37.<br />
3. Armstrong DG, Lavery LA; Diabetic Foot Consortium. Negative pressure wound<br />
therapy after partial diabetic foot amputation: a multicentre, randomised controlled<br />
trial. Lancet 2005; 366(9498): 1704-10.<br />
4. Wild T, Stortecky S, Stremitzer S, et al. [Abdominal dressing – a new standard in<br />
therapy of the open abdomen following secondary peritonitis?] Zentralbl Chir 2006;<br />
131(Suppl 1): S111-14.<br />
5. Ford CN, Reinhard ER, Yeh D, et al. Interim analysis of a prospective, randomized<br />
trial of vacuum-assisted closure versus the Healthpoint system in the management of<br />
pressure ulcers. Ann Plast Surg 2002; 49(1): 55-61; discussion: 61.<br />
6. Jeschke MG, Rose C, Angele P, et al. Development of new reconstructive techniques:<br />
use of Integra in combination with fibrin glue and negative-pressure therapy for reconstruction<br />
of acute and chronic wounds. Plast Reconstr Surg 2004; 113(2): 525-30.<br />
7. Sjögren J, Gustafsson R, Nilsson J, et al. Clinical outcome after poststernotomy mediastinitis:<br />
vacuum-assisted closure versus conventional therapy. Ann Thorac Surg 2005;<br />
79(6): 2049-55.<br />
8. Moues CM, Vos MC, van den Bemd GJ, et al. Bacterial load in relation to vacuum-assisted<br />
closure wound therapy: a prospective randomized trial. Wound Repair Regen<br />
2004; 12(1): 11-17.<br />
9 Stannard JP, Robinson JT, Anderson ER, et al. Negative pressure wound therapy<br />
to treat hematomas and surgical incisions following high-energy trauma. J Trauma<br />
2006; 60(6): 1301-06.
<strong>EWMA</strong> Journal<br />
Previous Issues<br />
Volume 6, no 2, Fall 2006<br />
The number of leg ulcers increases – a 20-year-questionnaire<br />
study in Pirkanmaa Health Care in Finland<br />
Anna L Hjerppe<br />
An ex-vivo model to evaluate dressings & drugs for wound healing<br />
Johanna M. Brandner, Pia Houdek, Thomas Quitschau,<br />
Ute Siemann-Harms, Ulrich Ohnemus, Ingo Willhardt, Ingrid Moll<br />
Compression therapy of venous ulcers<br />
Hugo Partsch<br />
Seasonal variation of onset of venous leg ulcers<br />
Marian Simka<br />
Determinants and estimation of wound healing achievement after<br />
minor amputation in patients with diabetic foot<br />
Robert Bém, A. Jirkovská, V. Fejfarová, J. Skibová, B. Sixta, P. Herdegen<br />
Leg ulcer prevalence in the Czech Republic:<br />
Omnibus survey results 2006<br />
Zdenek Kucera<br />
Volume 6, no 1, Spring 2006<br />
Focus on silver<br />
Jean-Yves Maillard, Stephen P Denyer<br />
Factors that influence the frequency of rebandaging<br />
Una Adderley<br />
Microengineered hydrogel as a vehicle for grafting<br />
human skin cells<br />
Stephen Britland, Annie Smith<br />
Wound Care in Anatolia<br />
Ali Barutcu<br />
Implementation of a Leg Ulcer Strategy in Central & Eastern Europe<br />
Peter J. Franks<br />
Post Graduate Wound Healing Course Modena, Italy<br />
Deborah Hofman<br />
From The Laboratory to the Patient: Future Organisation and<br />
Care of Problem Wounds. A New Experience<br />
Finn Gottrup<br />
Volume 5, no 2, Fall 2005<br />
Retrospective analysis of topical application of<br />
factor XIII in patients with chronic leg ulcers<br />
Mirjana Ziemer, Claudia Scheumann, Martin Kaatz, Johannes Norgauer<br />
An overview of surgical site infections:<br />
aetiology, incidence and risk factors<br />
Finn Gottrup, Andrew Melling, Dirk A. Hollander<br />
Regulating research and associated activity in the UK<br />
Sue Bale<br />
Article Review – The effectiveness of a hyperoxygenated fatty<br />
acid compound in preventing pressure ulcers<br />
Joan-Enric Torra i Bou, T. Segovia Gómez, J. Verdú Soriano,<br />
A. Nolasco Bonmatí, J. Rueda López, M. Arboix i Perejamo<br />
Article Review – Extended commentary on a trial<br />
E. Andrea Nelson<br />
UK Lymphoedema Framework Project<br />
Philip A. Morgan, Christine J. Moffatt, Debra C. Doherty, Peter J. Franks<br />
German Wound Surgeons 1450-1750<br />
Carol Dealey<br />
The <strong>EWMA</strong> Journals can be downloaded free of charge from www.ewma.org<br />
50<br />
Volume 7, no 2, January 2007<br />
Self-care activities of venous leg ulcer patients in Finland<br />
Salla Seppänen<br />
Smoking is not contra-indicated in maggot debridement<br />
therapy in the chronic wound<br />
Pascal Steenvoorde<br />
Effectiveness of non-alcohol film forming skin protector<br />
on the skins isles inside the ulcers and the healing rate of<br />
venous leg ulcers<br />
Tanja Planinsek Rucigaj<br />
Wound measurement: the contribution to practice<br />
Georgina T. Gethin<br />
Improving education in wound care: crossing<br />
the boundaries of interprofessional learning<br />
Caroline McIntosh<br />
Waterjet debridement of deep and indeterminate depth<br />
thermal injuries<br />
Mayer Tenenhaus<br />
International Journals<br />
The section on International Journals is part of<br />
<strong>EWMA</strong>’s attempt to exchange information on<br />
wound healing in a broad perspective.<br />
Italian<br />
English<br />
Finnish<br />
Acta Vulnologica, vol. 4, no 4, 2006<br />
www.aiuc.it<br />
A Proposal for a bill of rights in wound care<br />
Brambilla R., Coppi C.<br />
Diabetes mellitus and pressure sores: interactions<br />
and strategies<br />
Gallo M., Furlini S., Somà K.<br />
Ulcers induced during therapy with hydroxyurea<br />
in patients with myeloproliferative disorders<br />
Venturi C., Pandolfi R., Motolese A.<br />
Advances in Skin & Wound Care, vol. 20, april 2007<br />
www.aswcjournal.com<br />
Pressure Ulcers in Neonates and Children:<br />
An NPUAP White Paper<br />
Mona Mylene Baharestani, Catherine R. Ratliff<br />
Treatment of Ischemic Wounds with Noncontact,<br />
Low-Frequency Ultrasound: The Mayo Clinic<br />
Experience, 2004-2006<br />
Steven J. Kavros, Jenny L. Miller, Steven W. Hanna<br />
The Treatment of Diabetic Foot Ulcers:<br />
Reviewing the Literature and a Surgical Algorithm<br />
Steven R. Kravitz, James B. McGuire, Sid Sharma<br />
Haava, vol. no 1, 2007<br />
www.suomenhaavanhoitoyhdistys.fi<br />
How MD can utilize the microbiological tests<br />
Sakari Vuorinen<br />
Drains, wound suction an their treatment<br />
Ansa Iivanainen, Helvi Hietanen<br />
Planning of wound treatment<br />
Marja Nidkasaari<br />
Treatment of bullet wounds<br />
Lauri Handolin<br />
Polyurethane foams and amputation wounds<br />
Sirpa Arvonen<br />
Silver in the treatment of burns<br />
Helena Asikainen, Juha M. Venäläinen<br />
The mystery of green net<br />
Jaana Ruohoaho<br />
Vacuum assisted closure in wound management<br />
Tiina Pukki<br />
Honey in the treatment of lec ulcers<br />
Maria Nevalainen<br />
Wound management in intensive care unit<br />
Ritva Sipinen<br />
Developing documentation in wound management<br />
Jonna Saarela, Satu Tuovinen<br />
Tissue viability nurse in communities – a project work<br />
Eija Luotola<br />
Developing infection controlling models for practise<br />
of wound care<br />
Kirsi Terho, Tiina Kurvoien, Marianne Routamaa<br />
Quality of care of diabetic foot<br />
Senja Torvinen<br />
Living with scars<br />
Virpi Hämeen-Anttila<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Spanish<br />
English<br />
English<br />
Helcos 2007, vol 18, no 1<br />
Efficiency of the products for pressure ulcers treatment:<br />
a systematic review with meta-analysis<br />
García Fernández F.P., Pancorbo Hidalgo P.L.,<br />
Verdú Soriano J., Soldevilla Agreda J.J., Rodríguez Palma M.,<br />
Gago Fornells M., Martínez Cuervo F., Rueda López J.<br />
Clinical judgement or assessment scales to identify<br />
patients at risk of developing pressure ulcers?<br />
Rodríguez Torres Mª. del C., Soldevilla Agreda J.J.<br />
International Wound Journal, Mar. 2007, vol. 4, Issue 1<br />
www.blackwellpublishing.com<br />
OASIS ® wound matrix versus Hyaloskin ® in the treatment of<br />
difficult-to-heal wounds of mixed arterial/venous aetiology<br />
M Romanelli, V Dini, M Bertone, S Barbanera, C Brilli<br />
Successful management of deep facial burns in a patient with<br />
extensive third-degree burns: the role of a nanocrystalline silver<br />
dressing in facilitating resurfacing<br />
M Marazzi, A De Angelis, A Ravizza, MN Ordanini, L Falcone,<br />
A Chiaratti, F Crovato, D Calò, S Veronese, V Rapisarda<br />
Paediatric partial-thickness scald burns<br />
– is Biobrane the best treatment available?<br />
A Mandal<br />
Wound bed preparation of difficult wounds:<br />
an evolution of the principles of TIME<br />
C Ligresti, F Bo<br />
Clinical predictors of treatment failure for diabetic foot<br />
infections: data from a prospective trial<br />
BA Lipsky, P Sheehan, DG Armstrong, AD Tice, AB Polis,<br />
MA Abramson<br />
The role of vascular endothelial growth inhibitor in<br />
wound healing<br />
KP Conway, P Price, KG Harding, WG Jiang<br />
Randomised clinical trial of Hydrofiber dressing with silver<br />
versus povidone-iodine gauze in the management of open<br />
surgical and traumatic wounds<br />
F Jurczak, T Dugré, A Johnstone, T Offori, Z Vujovic, D Hollander<br />
Negative pressure wound therapy via vacuum-assisted<br />
closure following partial foot amputation:<br />
what is the role of wound chronicity?<br />
DG Armstrong, LA Lavery, AJM Boulton<br />
Negative pressure wound therapy:<br />
treating a venomous insect bite<br />
MS Miller, M Ortagon, C McDaniel<br />
The International Journal of Lower Extremity<br />
Wounds<br />
vol. 6, no 1, 2007<br />
http://ijlew.sagepub.com<br />
Wound Healing at the Crossroads<br />
Raj Mani<br />
Developing guidelines in the absence of<br />
traditional research evidence: an example from<br />
the lymphoedema framework project<br />
Peter J. Franks, Philip A. Morgan<br />
Growth factors: the promise and the problems<br />
Jeffrey M. Davidson<br />
The development and application of diabetic<br />
foot protocol in Chiang Mai University Hospital<br />
with an aim to reduce lower extremity amputation<br />
in thai population: a preliminary pommunication<br />
K. Rerkasem, N. Kosachunhanun, S. Tongprasert,<br />
K. Khwanngern, A. Matanasarawoot,<br />
C. Thongchai, K. Chimplee, S. Buranapin,<br />
S. Chaisrisawadisuk, A. Manklabruks<br />
An evaluation of the value of group education in<br />
recently diagnosed diabetes mellitus<br />
G. S. Ooi, C. Rodrigo, W. K. Cheong, R. L. Mehta,<br />
G. Bowen, C. P. Shearman<br />
The diabetic foot: perspectives from Chennai,<br />
South India<br />
Vijay Viswanathan<br />
Growth Factors in the Treatment of Diabetic<br />
Foot Ulcers: New Technologies, Any Promises?<br />
N. Papanas and E. Maltezos<br />
English<br />
Scandinavian<br />
German<br />
<strong>EWMA</strong><br />
Journal of Wound Care, April issue, vol. 16, no 4, 2007<br />
www.journalofwoundcare.com; jwc@emap.com<br />
Use of polarised light as a method of pressure ulcer<br />
prevention in an adult intensive care unit<br />
J. Verbelen<br />
Can translocated bacteria reduce wound infection?<br />
V.I. Nikitenko<br />
Venous leg ulcer treatment and practice – part 4:<br />
surgery and pharmaceutical therapies<br />
S. Rajendran, A.J. Rigby, S.C. Anand<br />
Management of bioburden with a burn gel that<br />
targets nociceptors<br />
L. Martineau, H-M. Dosch<br />
Can cycloidal vibration plus standard treatment reduce<br />
lower limb cellulitis treatment times?<br />
S. Johnson, K. Leak, S. Singh, P. Tan, W. Pillay,<br />
R.J. Cuschieri, E. Mostyn<br />
Bacterial profiling using skin grafting, standard culture<br />
and molecular bacteriological methods<br />
A. Andersen, K.E. Hill, P. Stephens, D.W. Thomas,<br />
B. Jorgensen, K.A. Krogfelt<br />
A prospective observational study of the efficacy of a<br />
novel hydroactive impregnated dressing<br />
F. Meuleneire, P. Zoellner, M. Swerev, O. Holfeld, J. Effing,<br />
S. Bapt, N. Tholon, E. Felder, B. Streit, H. Kapp, H. Smola<br />
Wounds (SÅR) vol. 15, no 1, 2007<br />
www.saar.dk<br />
Care and treatment of people with cancer wounds<br />
Betina Lund-Nielsen<br />
Compression therapy of venous leg ulcers<br />
– how can we make it more cost-effective?<br />
Rie Nygaard, Susan F. Jørgensen<br />
Terra Sigillata – a pharmaceutical product used for more<br />
than 2000 years<br />
Annette Frölich<br />
Lymphoedema clinic at Copenhagen Wound Healing Centre<br />
– much-needed developments for patients where no<br />
treatment is possible<br />
Jens Fonnesbech<br />
Higher level and a stronger scientific foundation:<br />
New diploma in wound management<br />
Jens Fonnesbech<br />
Prevention and treatment of diabetic foot ulcers<br />
– commenting on the debate in the Norwegian Parliament<br />
Stortinget<br />
Kirsti Espeseth<br />
Wund Management Issue 2, 2007<br />
Overview<br />
Incidence of Ulcus cruris in Germany:<br />
Data of the German Federal Health Monitoring<br />
K. Kröger<br />
Standards in the Treatment of Wounds<br />
Obsolete products and methods in the treatment<br />
of chronic wounds<br />
W. Sellmer<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 51
Corporate A<br />
Coloplast<br />
Holtedam 1-3<br />
DK-3050 Humlebæk<br />
Denmark<br />
Tel: +45 49 11 15 88<br />
Fax: +45 49 11 15 80<br />
www.coloplast.com<br />
ConvaTec Europe<br />
Harrington House<br />
Milton Road<br />
Ickenham, Uxbridge<br />
UB10 8PU<br />
United Kingdom<br />
Tel: +44 (0) 1895 62 8300<br />
Fax: +44 (0) 1895 62 8362<br />
www.convatec.com<br />
Ethicon GmbH<br />
Johnson & Johnson Wound Management<br />
Oststraße 1<br />
22844 Norderstedt<br />
Germany<br />
Tel: +49 40 52207 230<br />
Fax: +49 40 52207 823<br />
www.jnjgateway.com<br />
KCI Europe Holding B.V.<br />
Parktoren, 6th floor<br />
van Heuven Goedhartlaan 11<br />
1181 LE Amstelveen<br />
The Netherlands.<br />
Tel: +31 (0) 20 426 0000<br />
Fax: +31 (0)20 426 0097<br />
www.kci-medical.com<br />
5<br />
<strong>EWMA</strong> Corporate Sponsor Contact Data<br />
Lohmann & Rauscher<br />
P.O. BOX 23 43 Neuwied<br />
D-56513<br />
Germany<br />
Tel: +49 (0) 2634 99-6205<br />
Fax: +49 (0) 2634 99-1205<br />
www.lohmann-rauscher.com<br />
Mölnlycke Health Care Ab<br />
Box 13080<br />
402 52 Göteborg,<br />
Sweden<br />
Tel: +46 31 722 30 00<br />
Fax: +46 31 722 34 08<br />
www.molnlycke.com<br />
Smith & Nephew<br />
Po Box 81, Hessle Road<br />
HU3 2BN Hull,<br />
United Kingdom<br />
Tel: +44 (0) 1482 225 181<br />
Fax: +44 (0) 1482 328 326<br />
www.smith-nephew.com<br />
Tyco Healthcare<br />
154, Fareham Road<br />
PO13 0AS Gosport<br />
United Kingdom<br />
Tel: +44 1329 224479<br />
Fax: +44 1329 224107<br />
www.tycohealthcare.com<br />
Corporate B<br />
3M Health Care<br />
Morley Street, Loughborough<br />
LE11 1EP Leicestershire<br />
United Kingdom<br />
Tel: +44 1509 260 869<br />
Fax: +44 1 509 613326<br />
www.mmm.com<br />
Activa Healthcare Ltd<br />
1 Lancaster Park<br />
Newborough Road<br />
Needwood<br />
Burton on Trent<br />
Staffordshire<br />
DE13 9PD<br />
Tel: +44 (0) 8450 606 707<br />
Fax: +44 (0) 1283 576808<br />
www.activahealthcare.co.uk<br />
B. Braun Medical<br />
204 avenue du Maréchal Juin<br />
92107 Boulogne Billancourt<br />
France<br />
Tel: +33 1 41 10 75 66<br />
Fax: +33 1 41 10 75 69<br />
www.bbraun.com<br />
Comvita UK Ltd<br />
Unit 3, 55-57 Park Royal Road<br />
London NW10 7LP<br />
United Kingdom<br />
Tel: +44 208 961 4410<br />
Fax: +44 208 961 9420<br />
www.comvita.co.uk<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
Ferris Mfg. Corp.<br />
16W300 83rd Street<br />
Burr Ridge,<br />
Illinois 60527-5848 U.S.A.<br />
Tel: +1 (630) 887-9797<br />
Toll-Free: +1 (630) 800 765-9636<br />
Fax: +1 (630) 887-1008<br />
www.polymem.com<br />
Paul Hartmann AG<br />
Paul-Hartmann-Strasse<br />
D-89522 Heidenheim<br />
Germany<br />
Tel: +49 (0) 7321 / 36-0<br />
Fax: +49 (0) 7321 / 36-3636<br />
www.hartmann.info<br />
Sorbion AG<br />
Hobackestraße 91<br />
D-45899 Gelsenkirchen<br />
Tel: +49 (0)2 09-95 71 88-0<br />
Fax: +49 (0)2 09-95 71 88-20<br />
www.sorbion.com<br />
Laboratoires Urgo<br />
42 rue de Longvic<br />
B.P. 157<br />
21300 Chenôve<br />
France<br />
Tel: (+33) 3 80 44 70 00<br />
Fax: (+33) 3 80 44 71 30<br />
www.urgo.com<br />
Use<br />
the <strong>EWMA</strong> Journal<br />
to profile your company<br />
Deadline for advertising in the<br />
next issue is 1 August 2007<br />
<strong>EWMA</strong><br />
<strong>EWMA</strong> Position Document 2007<br />
Topical Negative Pressure<br />
in Wound Management<br />
Editor: Christine Moffatt<br />
The document is available in English, French,<br />
German, Italian and Spanish, and can be<br />
downloaded from www.ewma.org<br />
Previous Position Documents:<br />
For further details contact<br />
MEP Ltd, 53 Hargrave Road,<br />
London N19 5SH.<br />
www.mepltd.co.uk<br />
or<br />
<strong>EWMA</strong> Business Office,<br />
Congress Consultants,<br />
Martensens Allé 8,<br />
1828 Frederiksberg,<br />
Denmark<br />
Tel: +45 7020 0305<br />
Fax: +45 7020 0315<br />
ewma@ewma.org<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 5
Conferences<br />
Conference Calendar<br />
Conference Theme<br />
SAWC & WHS 2007 (National) Apr/May 28-1 Tampa, Florida USA<br />
17th Conference of the European Wound<br />
Management Association (<strong>EWMA</strong> 2007)<br />
5th international symposium on the<br />
Diabetic Foot<br />
For web link please visit www.ewma.org<br />
Evidence, Consensus and Driving the<br />
Agenda forward<br />
EADV 16th Congress European Dermatology and Venereology<br />
– Strong Past, Stronger Future<br />
May 2-4 Glasgow Scotland<br />
May 9-12 Noordwijkerhout The Netherlands<br />
May 16-20 Vienna Austria<br />
SAfW 4th Congress (National) May 24 Morges Switzerland<br />
11th Symposium of modern Woundhealing<br />
(National)<br />
Jun 1-2 Bregenz Switzerland<br />
12th Congress of the ESDaP (National) Jun 14-17 Wroclaw Poland<br />
Wounds UK Summerconference (National) Jun 22 Warwickshire UK<br />
Tissue Viability and Wound Care Management<br />
(National)<br />
Improving Practise on the Wards Jul 3 London UK<br />
EPUAP 10th European Meeting Ten years of progress, the present and<br />
the future in Pressure Ulcer Prevention and<br />
Management<br />
Aug/Sep 30-01 Oxford UK<br />
VI Congresso Nazionale AIUC Alla scoperta dell’ulcera cutanea cronica Sep 12-15 Genova Italy<br />
SSiS National Congress Sep 24 Sweden<br />
ETRS 17th Annual Meeting Measurements in wound healing<br />
– the conduit between the laboratory and<br />
the clinic<br />
Sep 26-28 Southampton UK<br />
ILDS 21st World Congress of Dermatology Global Dermatology for a globalized world Oct 1-5 Buenos Aires Argentina<br />
APTFeridas 2007 National Congress Nov 7-9 Porto Portugal<br />
Wounds UK 2007 (National) Nov 12-14 Harrogate UK<br />
VII Nacional Congress GNEAUPP Nov Spain<br />
National Meeting DSFS Cancer Wounds Nov 16-17 Nyborg Denmark<br />
XIIth National Wound Management Conference Jan/Feb 31-1 Helsinki Finland<br />
NIFS National Conference Pressure Ulcers Feb 14-15 Bergen Norway<br />
SAWC & WHS 2008 (National) Apr USA<br />
18th Conference of the European Wound<br />
Management Association (<strong>EWMA</strong> 2008)<br />
Wound Healing · Wound Management<br />
– Responsibility and Actions<br />
WUWHS – 3rd Congress Wound Care Efficacy,<br />
Effectiveness & Efficiency<br />
Oxford – European Wound Healing<br />
Summer School<br />
7th Scientific Meeting of the Diabetic Foot Study<br />
Group (DFSG) of the EASD<br />
5<br />
Different aspects of patient wound<br />
management based on therapy innovation<br />
and clinical research<br />
2008<br />
May 14-16 Lisbon Portugal<br />
Jun 4-8 Toronto Canada<br />
Jul Oxford UK<br />
Sep 11-13 Pisa Italy<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
FWCS<br />
Finnish<br />
Wound Care Society<br />
Salla Seppänen, RGN,<br />
Specialist in Medical-<br />
Surgical Nursing, MNSc,<br />
Principal Lecturer,<br />
Oulu University of Applied<br />
Sciences,<br />
Oulainen Department of<br />
Health Care<br />
Finland<br />
salla.seppanen@pp.inet.fi<br />
www.suomenhaavanhoitoyhdistys.fi<br />
The XIth Finnish<br />
National Wound Management Conference<br />
1-2 February 2007 in Helsinki<br />
The Finnish Wound Care Society organised its<br />
annual wound management conference for<br />
2007 on the theme of “Special Issues in<br />
Wound Management”.<br />
The programme included sessions<br />
discussing lower limb amputation, wound<br />
infection, costs of wound care, seamless<br />
services in wound care and wound patients’<br />
quality of life, which focused on pain, nutrition<br />
and living habits.<br />
<strong>EWMA</strong> organised the conference keynote<br />
speaker Professor John Posnett from the UK.<br />
He presented a lecture on the costs and effectiveness<br />
of wound care in which he estimated<br />
that the average cost of chronic wounds in<br />
Finland is now at least 194 billion euros per<br />
year. This presents the Finnish Wound Care<br />
Society with the challenge to develop<br />
evidence-based wound management, which<br />
covers the whole care path of the patient.<br />
The national conference collected together<br />
about 700 health professionals from all over<br />
Finland.<br />
Organisations<br />
The feedback of participants was positive<br />
and encouraging; 75.4% of participants<br />
assessed the conference as good and 21.7%<br />
assessed it as excellent. Most of the participants<br />
(73.4%) stated that they felt that the<br />
conference was useful for their work.<br />
According to the conference feedback, the<br />
content of sessions was relevant, interesting<br />
and professional providing useful tips for<br />
clinical practice.<br />
The conference also attracted corporate<br />
healthcare professionals with 26 corporate<br />
members participating in the conference<br />
exhibition.<br />
The XIIth National Wound Management<br />
Conference will be held on 31/1-1/2.2008 in<br />
Helsinki on the theme of “Modern Wound<br />
Management”.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 55
SSiS<br />
Sårsjuksköterskor i<br />
Sverige<br />
Tissue Viability<br />
Nureses in Sweden<br />
Christina Lindholm<br />
President<br />
christina.lindholm@hv.hkr.se<br />
56<br />
www.sarsjukskoterskor.se<br />
The SSiS is an association for<br />
registered nurses with a professional<br />
interest in wounds<br />
Wound healing is an important field, in which<br />
nursing competence must improve and<br />
become more visible.<br />
Sårsjuksköterskor i Sverige (SSiS)/ Tissue<br />
Viability Nurses in Sweden is a part/section of<br />
the Swedish Society of Nursing (SSF) and also<br />
a Co-operating Organisation within <strong>EWMA</strong><br />
since 2006.<br />
The SSiS is an association for registered<br />
nurses with a professional interest in wounds.<br />
The main purpose of the SSiS is to address<br />
nation wide, strategic issues in wound<br />
management, in close co-operation with politicians,<br />
other national societies and <strong>EWMA</strong>.<br />
We aim to<br />
– promote evidence-based medical and<br />
nursing practice in agreement with laws<br />
and regulations in order to increase quality<br />
of care for persons with wounds or at risk<br />
of developing wounds<br />
– become a meeting place for co-operation<br />
and exchange of knowledge between<br />
interest groups from various specialist<br />
areas in wound healing<br />
– cover, disseminate and promote research,<br />
development and education in wound<br />
healing<br />
– strengthen and clarify the nurse’s role<br />
in wound healing<br />
– improve the wound patients’ physical,<br />
practical and emotional situation<br />
Membership in the SSiS includes free issues<br />
of the <strong>EWMA</strong> Journal and the Danish SÅR<br />
journal, reduced subscription fees for the new<br />
Swedish journal Sår and reduced registration<br />
fees for SSiS and <strong>EWMA</strong> conferences.<br />
Since being established in late 2005, the SSiS<br />
has recruited around 350 members, arranged<br />
two conferences, set up working teams,<br />
established co-operation with the companies,<br />
started a website, www.sarsjukskoterskor.se,<br />
and acted as a point of reference to the<br />
authorities in different wound-related<br />
subjects.<br />
Conferences<br />
Two conferences have been held, both at<br />
the Karolinska University Hospital. They have<br />
attracted more than 400 participants.<br />
International speakers include Tom Defloor,<br />
Mark Collier and Keith Harding. The next<br />
conference on the theme Wound management<br />
– practical aspects and ethical issues –<br />
an interactive session will be held September<br />
24. The Annual General Meeting has been<br />
held on March 26, combined with a meeting<br />
for representatives from the companies.<br />
At present our main efforts are directed<br />
towards expanding the website, planning the<br />
next conference, preparing problem inventories<br />
in the wound healing area, drawing up<br />
competency standards for Swedish nurses<br />
specialising in wound healing and recruiting<br />
more members.<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
WMAS<br />
Slovenian Wound<br />
Management<br />
Association<br />
Helena Kristina Peric<br />
Slovenian<br />
Wound Management Association<br />
Cankarjeva 8<br />
1236 Trzin<br />
Slovenia<br />
helena.peric@siol.net<br />
What’s new in Slovenia?<br />
Slovenian Wound Management Association<br />
(WMAS) has been very active in the past<br />
couple of years. As a very young association it<br />
still suffers from some “childhood” problems<br />
but we are overcoming them more and more.<br />
WMAS is run by professor Zoran M. Arnež.<br />
Vice-presidents are Vanja Vilar and Zdenka<br />
Kramar. The executive board consists of<br />
different professions- doctors of various<br />
specializations, nurses, pharmacists…<br />
As Slovenia is a small country (population less<br />
then 2 million) we always struggle with man<br />
power, so last year we decided to hire a part<br />
time secretary to assist us with administration.<br />
This proved to be a good decision as our plan<br />
of activities is always ambitious enough to<br />
keep us busy.<br />
Some of the major achievements of the association<br />
in the last 2 years are:<br />
n publishing Recommendations for prevention<br />
and treatment of pressure ulcers, Recommendations<br />
for treatment of venous leg ulcers,<br />
Recommendations for treatment of diabetic<br />
foot ulcers and Recommendations for treatment<br />
of malignant wounds. The Recommendations<br />
are very appreciated by health care<br />
professionals. Of course we are aware that this<br />
is just the first step out of many required to<br />
bring wound care in Slovenia to the level<br />
where all patients will be treated adequately<br />
and equally. We would like to expand these<br />
recommendations into detailed guidelines but<br />
what is even more important, we need to find<br />
a way to assist health care professionals to<br />
implement them in practice as much as<br />
possible. In order to do so, some changes<br />
have to be made at macro level (health care<br />
organization, reimbursement…) and some<br />
changes have to be made at micro level<br />
(health care professionals interest and attitude<br />
towards wound care…)<br />
n organization of many educational events<br />
on prevention and treatment of chronic<br />
wounds, including workshops and discussion<br />
forums. Over the past 2 years, more than<br />
thousand people attended these activities.<br />
We also support activities organized by other<br />
institutions who serve as wound care centers<br />
of excellence.<br />
n influencing health care politics to<br />
improve wound care services in Slovenia.<br />
Representatives of WMAS wrote many letters<br />
and paid many visits to Reimbursement<br />
agency, Ministry of health, Health council<br />
etc. Members of WMAS also cooperated with<br />
articles and interviews on the radio, TV and<br />
in the printed media in order to raise awareness<br />
of wound care problematic.<br />
n cooperating with European Wound Care<br />
Association: we maintain regular cooperation<br />
with <strong>EWMA</strong>. Last year we started a joint<br />
project “Implementing leg ulcer strategy in<br />
Eastern Europe” under the leadership of<br />
Peter Franks. We are hoping that this project<br />
will provide evidence which can be used in<br />
our efforts to improve wound care services in<br />
Slovenia. It is one of our major activities for<br />
2007.<br />
This year we are planning similar activities as<br />
in previous years. We have an ambitious plan<br />
we hope to fulfill with <strong>EWMA</strong> support. We<br />
are also looking forward to have some of our<br />
representatives visiting <strong>EWMA</strong> conference as<br />
this is an excellent opportunity to exchange<br />
experience, refresh knowledge and gain new<br />
ideas.<br />
Warm regards from Slovenia on behalf of<br />
WMAS executive board!<br />
Organisations<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 5
5<br />
Co-operating Organisations<br />
Danish Wound<br />
Healing Society<br />
ABISCEP<br />
Wound Management<br />
Association in Belgium<br />
AISLeC<br />
Associazione Infermieristica<br />
per lo Studio Lesioni Cutanee<br />
Italian Nurse Association for<br />
the Study of Cutaneous<br />
Wounds<br />
www.aislec.it<br />
AIUC<br />
Associazione Italiana<br />
Ulcere Cutanee.<br />
Italian Association for<br />
Cutaneous Ulcers<br />
www.aiuc.it<br />
APTFeridas<br />
Portuguese Wound<br />
Management Association<br />
www.aptferidas.com<br />
AWA<br />
Austrian Wound Association<br />
www.a-w-a.at<br />
CNC/BFW<br />
Wound Management<br />
Organisation<br />
www.befewo.org<br />
www.wondzorg.be<br />
CSLR<br />
Czech Wound Management<br />
Society<br />
www.cslr.cz<br />
CWMA<br />
Croatian Wound<br />
Management Association<br />
DGfW<br />
Deutsche Gesellschaft für<br />
Wundheilung<br />
www.dgfw.de<br />
DWHS<br />
Danish Wound Healing<br />
Society<br />
www.dsfs.org<br />
FWCS<br />
Finnish Wound Care Society<br />
www.suomenhaavanhoitoyhdistys.fi<br />
GAIF<br />
Grupo Associativo de<br />
Investigacão em Feridas<br />
www.gaif.net<br />
GNEAUPP<br />
Grupo Nacional para el<br />
Estudio y Asesoramiente en<br />
Ulceras por Presión y Heridas<br />
Crónicas<br />
www.gneaupp.org<br />
GWMA<br />
Greek Wound Management<br />
Association<br />
HWMS/MSKT<br />
Hungarian Lymphoedema<br />
and Wound Managing<br />
Society<br />
ICW<br />
Initiative Chronische Wunden<br />
IWHS<br />
Iceland Wound Healing<br />
Society<br />
www.sums-is.org<br />
LBAA<br />
Latvian Wound Treating<br />
Organisation<br />
LF<br />
Lymphoedema Framework<br />
www.lymphoedemaframework.org<br />
LSN<br />
The Lymphoedema Support<br />
Network<br />
www.lymphoedema.org/lsn<br />
LUF<br />
The Leg Ulcer Forum<br />
www.legulcerforum.org<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2
LWMS<br />
Lithuanian Wound<br />
Management Society<br />
NATVNS<br />
National Association of<br />
Viability Nurse Specialists<br />
(Scotland)<br />
www.natvns.com<br />
NIFS<br />
Norwegian Wound Healing<br />
Association<br />
www.nifs-saar.no<br />
NOVW<br />
Dutch Organisation of<br />
Wound Care Nurses<br />
www.novw.org<br />
PWMA<br />
Polish Wound Management<br />
Association<br />
ROWMA<br />
Romanian Wound<br />
Management Association<br />
SAfW<br />
Swiss Association for<br />
Wound Care<br />
www.safw.ch<br />
SEBINKO<br />
Hungarian Association for<br />
the Improvement of Care of<br />
Chronic Wounds and<br />
Incontinentia<br />
www.sebinko.hu<br />
SFFPC<br />
La Société Française et<br />
Francophone de Plaies et<br />
Cicatrisations<br />
www.sffpc.org<br />
SISS<br />
Swedish Wound Care Nurses<br />
Association<br />
www.sarsjukskoterskor.se<br />
SWHS<br />
Svenskt Sårläkningssällskap<br />
www.sarlakning.com<br />
SWMA<br />
Serbian Wound Management<br />
Association<br />
TVNA<br />
Tissue Viability Nurses<br />
Association<br />
www.tvna.org<br />
TVS<br />
Tissue Viability Society<br />
www.tvs.org.uk<br />
WMAI<br />
Wound Management<br />
Association of Ireland<br />
www.wmaoi.org<br />
WMAS<br />
Slovenian Wound<br />
Management Association<br />
WMAT<br />
Wound Management<br />
Association Turkey<br />
Present your national<br />
wound management<br />
organisation<br />
or write a report about<br />
your organisation’s<br />
latest meeting.<br />
ewma@ewma.org<br />
Deadline<br />
for incoming material for<br />
the next issue is<br />
15 July 2007<br />
Organisations<br />
<strong>EWMA</strong> Journal 2007 vol 7 no 2 5
3 Editorial<br />
Peter J Franks<br />
Scientific Articles<br />
7 Is it safe to use saline solution to clean wounds?<br />
João Carlos Gouveia, Christina Miguens<br />
15 The cost of pressure ulceration<br />
Peter J Franks<br />
21 Epidemiology of wounds treated in<br />
Community Services in Portugal<br />
Elaine Pina<br />
29 Improving wound assessment through<br />
the provision of digital cameras across<br />
a Primary Care Trust<br />
Alison Hopkins<br />
Background Articles<br />
35 The use of telemedicine in wound care<br />
Rolf Jelnes<br />
39 Lord Joseph Lister: the rise of antiseptic<br />
surgery and the modern place of antiseptics<br />
in wound care<br />
David Leaper<br />
EBWM<br />
44 Abstracts of recent Cochrane Reviews<br />
Sally Bell-Syer<br />
<strong>EWMA</strong><br />
48 <strong>EWMA</strong> Position Document 2007:<br />
Topical Negative Pressure in Wound<br />
Management<br />
Christine Moffatt<br />
50 <strong>EWMA</strong> Journal previous issues<br />
50 International Journals<br />
52 <strong>EWMA</strong> Corporate Sponsors contact data<br />
Conferences<br />
54 Conference calendar<br />
Organisations<br />
55 The XIth Finnish National Wound Management<br />
Conference, 1-2 February 2007 in Helsinki<br />
Salla Seppänen<br />
56 The SSiS is an association for registered nurses<br />
with a professional interest in wounds<br />
Christina Lindholm<br />
57 What’s new in Slovenia?<br />
Helena Kristina Peric<br />
58 Co-operating Organisations