NPSF Research Grants Program - NPSF Patient Safety Congress
NPSF Research Grants Program - NPSF Patient Safety Congress
NPSF Research Grants Program - NPSF Patient Safety Congress
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
harm to staff and other patients and through indirect harm via its impact on staff’s<br />
ability to provide safe and empathic care. This session will describe the work of a<br />
multidisciplinary “Tiger Team,” including an improved definitional framework for<br />
DPB, identification of patient- and staff-related factors associated with DPB, and<br />
the pharmacological and nonpharmacological strategies undertaken thus far to<br />
eliminate it from the hospital and ambulatory environments.<br />
Upon completing this session, attendees will be able to:<br />
• State a structured definition of disruptive patient behavior that can be used to<br />
improve classification of safety events<br />
• Define the root causes of disruptive patient behavior from both a neurobiological<br />
and a systems level<br />
• Describe pharmacological and nonpharmacological strategies that may help to<br />
eliminate disruptive patient behavior<br />
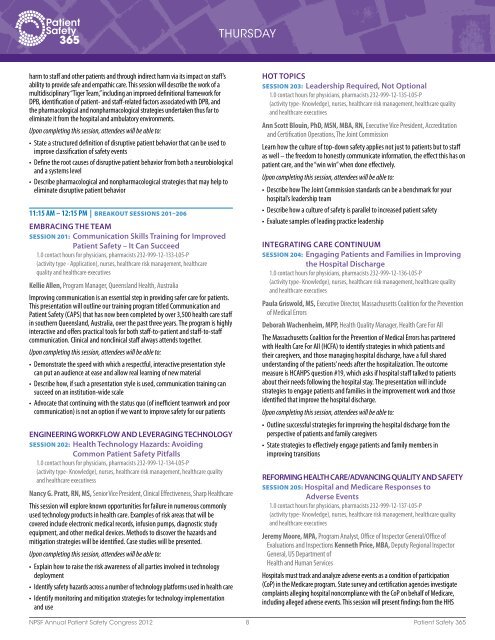
11:15 AM – 12:15 PM | Breakout SeSSionS 201–206<br />
EMBRACiNG thE tEAM<br />
SeSSion 201: Communication Skills training for improved<br />
<strong>Patient</strong> <strong>Safety</strong> – it Can Succeed<br />
1.0 contact hours for physicians, pharmacists 232-999-12-133-L05-P<br />
(activity type - Application), nurses, healthcare risk management, healthcare<br />
quality and healthcare executives<br />
Kellie Allen, <strong>Program</strong> Manager, Queensland Health, Australia<br />
Improving communication is an essential step in providing safer care for patients.<br />
This presentation will outline our training program titled Communication and<br />
<strong>Patient</strong> <strong>Safety</strong> (CAPS) that has now been completed by over 3,500 health care staff<br />
in southern Queensland, Australia, over the past three years. The program is highly<br />
interactive and offers practical tools for both staff-to-patient and staff-to-staff<br />
communication. Clinical and nonclinical staff always attends together.<br />
Upon completing this session, attendees will be able to:<br />
• Demonstrate the speed with which a respectful, interactive presentation style<br />
can put an audience at ease and allow real learning of new material<br />
• Describe how, if such a presentation style is used, communication training can<br />
succeed on an institution-wide scale<br />
• Advocate that continuing with the status quo (of inefficient teamwork and poor<br />
communication) is not an option if we want to improve safety for our patients<br />
ENGiNEERiNG WORkFLOW AND LEvERAGiNG tEChNOLOGY<br />
SeSSion 202: health technology hazards: Avoiding<br />
Common <strong>Patient</strong> <strong>Safety</strong> Pitfalls<br />
1.0 contact hours for physicians, pharmacists 232-999-12-134-L05-P<br />
(activity type- Knowledge), nurses, healthcare risk management, healthcare quality<br />
and healthcare executivess<br />
Nancy G. Pratt, RN, MS, Senior Vice President, Clinical Effectiveness, Sharp Healthcare<br />
This session will explore known opportunities for failure in numerous commonly<br />
used technology products in health care. Examples of risk areas that will be<br />
covered include electronic medical records, infusion pumps, diagnostic study<br />
equipment, and other medical devices. Methods to discover the hazards and<br />
mitigation strategies will be identified. Case studies will be presented.<br />
Upon completing this session, attendees will be able to:<br />
• Explain how to raise the risk awareness of all parties involved in technology<br />
deployment<br />
• Identify safety hazards across a number of technology platforms used in health care<br />
• Identify monitoring and mitigation strategies for technology implementation<br />
and use<br />
ThURSDAY<br />
hOt tOPiCS<br />
SeSSion 203: Leadership Required, Not Optional<br />
1.0 contact hours for physicians, pharmacists 232-999-12-135-L05-P<br />
(activity type- Knowledge), nurses, healthcare risk management, healthcare quality<br />
and healthcare executives<br />
Ann Scott Blouin, PhD, MSN, MBA, RN, Executive Vice President, Accreditation<br />
and Certification Operations, The Joint Commission<br />
Learn how the culture of top-down safety applies not just to patients but to staff<br />
as well – the freedom to honestly communicate information, the effect this has on<br />
patient care, and the “win win” when done effectively.<br />
Upon completing this session, attendees will be able to:<br />
• Describe how The Joint Commission standards can be a benchmark for your<br />
hospital’s leadership team<br />
• Describe how a culture of safety is parallel to increased patient safety<br />
• Evaluate samples of leading practice leadership<br />
iNtEGRAtiNG CARE CONtiNuuM<br />
SeSSion 204: Engaging <strong>Patient</strong>s and Families in improving<br />
the hospital Discharge<br />
1.0 contact hours for physicians, pharmacists 232-999-12-136-L05-P<br />
(activity type- Knowledge), nurses, healthcare risk management, healthcare quality<br />
and healthcare executives<br />
Paula Griswold, MS, Executive Director, Massachusetts Coalition for the Prevention<br />
of Medical Errors<br />
Deborah Wachenheim, MPP, Health Quality Manager, Health Care For All<br />
The Massachusetts Coalition for the Prevention of Medical Errors has partnered<br />
with Health Care For All (HCFA) to identify strategies in which patients and<br />
their caregivers, and those managing hospital discharge, have a full shared<br />
understanding of the patients’ needs after the hospitalization. The outcome<br />
measure is HCAHPS question #19, which asks if hospital staff talked to patients<br />
about their needs following the hospital stay. The presentation will include<br />
strategies to engage patients and families in the improvement work and those<br />
identified that improve the hospital discharge.<br />
Upon completing this session, attendees will be able to:<br />
• Outline successful strategies for improving the hospital discharge from the<br />
perspective of patients and family caregivers<br />
• State strategies to effectively engage patients and family members in<br />
improving transitions<br />
REFORMiNG hEALth CARE/ADvANCiNG QuALitY AND SAFEtY<br />
SeSSion 205: hospital and Medicare Responses to<br />
Adverse Events<br />
1.0 contact hours for physicians, pharmacists 232-999-12-137-L05-P<br />
(activity type- Knowledge), nurses, healthcare risk management, healthcare quality<br />
and healthcare executives<br />
Jeremy Moore, MPA, <strong>Program</strong> Analyst, Office of Inspector General/Office of<br />
Evaluations and Inspections Kenneth Price, MBA, Deputy Regional Inspector<br />
General, US Department of<br />
Health and Human Services<br />
Hospitals must track and analyze adverse events as a condition of participation<br />
(CoP) in the Medicare program. State survey and certification agencies investigate<br />
complaints alleging hospital noncompliance with the CoP on behalf of Medicare,<br />
including alleged adverse events. This session will present findings from the HHS<br />
<strong>NPSF</strong> Annual <strong>Patient</strong> <strong>Safety</strong> <strong>Congress</strong> 2012 8 <strong>Patient</strong> <strong>Safety</strong> 365