ninety years of service - University Hospital Southampton NHS ...
ninety years of service - University Hospital Southampton NHS ...
ninety years of service - University Hospital Southampton NHS ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
FORWARDbyI.C.S.Normand. D.M. ,F.R.C.P.Pr<strong>of</strong>essor <strong>of</strong> Child Health.David Williamson’s fascinating account <strong>of</strong> <strong>Southampton</strong> Children’s <strong>Hospital</strong> will be a source <strong>of</strong> nostalgia for all who knewor worked at Winchester Road but it is far from being just a nostalgic memoir. To many it may come as a surprise to learnhow <strong>Southampton</strong> for so long has kept in the forefront <strong>of</strong> ideas and practice in the care <strong>of</strong> sick children. Above all we reada story <strong>of</strong> extraordinary pr<strong>of</strong>essional devotion and commitment from a staff <strong>of</strong> minuscule size by modern standards butwho, because <strong>of</strong> their common ideals, achieved so much for their small patients with such limited resource behind them.It is now fifteen <strong>years</strong> since the Children’s <strong>Hospital</strong> closed but the tale <strong>of</strong> continuing expansion and innovation in <strong>service</strong>shas not changed. In particular the Children’s Unit increasingly functions as a tertiary and research centre as befits itsposition as the only <strong>University</strong> hospital along the South Coast. Inevitably some <strong>of</strong> the intimacy has gone but there stillremains a real sense <strong>of</strong> the happy family bound together in its pursuit <strong>of</strong> excellence for the care <strong>of</strong> sick children.We must all be grateful for the care and labour David Williamson has put into this volume that provides us with such fineexamples <strong>of</strong> <strong>service</strong> over <strong>ninety</strong> <strong>years</strong>.PREFACEWhen my successor, Dr Chris Rolles, suggested that I should write a short history <strong>of</strong> the old <strong>Southampton</strong> Children’s<strong>Hospital</strong> while there were still some <strong>of</strong> us about who could remember the place, I agreed with some misgivings, knowingthe fallibility <strong>of</strong> my own and, I suspected, other peoples memories. It did however seem important to try to recordsomething about the place, <strong>of</strong> which I, for one, had so many happy memories and which was typical <strong>of</strong> many similarinstitutions <strong>of</strong> it’s period.This booklet falls naturally into two unequal halves, divided by the introduction <strong>of</strong> the National Health Service in 1948, Forthe first section I have had to rely very largely on documentary evidence while for the second I have called upon my ownand other people’s memories and I am most grateful to the very large number <strong>of</strong> persons who have helped me in thisrespect. A letter to the ‘Echo’ produced an excellent response from many ex-staff and patients. I am particularly grateful tothose <strong>of</strong> my colleagues who have supplied me with contributions about their own departments. I would specially like torecord my debt to the late Mr Norman McKeith who not only gave me some fascinating insight into the working <strong>of</strong> thehospital in the thirties, but also undertook some individual research for me. The current <strong>of</strong>ficers in the Health Servicelocally have been most helpful but sadly I have to record that the Service as a whole seems to have little regard forhistorical material. A great many quite basic documents have apparently been destroyed though a few remain in theDistrict <strong>of</strong>fices and some are preserved in the City Archives, I am most grateful to Mr E.J. Ives who lent me his own copies<strong>of</strong> the Annual Reports <strong>of</strong> the H.M.C. and to Miss M.A. Mulady for supplying me with a complete set <strong>of</strong> Children’s <strong>Hospital</strong>Annual reports which had come down to her via the nursing hierarchy, Both have been invaluable.I have also received a large number <strong>of</strong> photographs only a few <strong>of</strong> which has it been possible to reproduce here. Howeverwe intend to collect a selection <strong>of</strong> these together into an album which will be kept in the Department at the General<strong>Hospital</strong>; others together with various source documents will be deposited in the City Archives for safe keeping. I amindebted to The Southern Evening Echo for allowing me to reproduce photographs on pages 7 & 11,I would like to record my appreciation <strong>of</strong> the help given me by Sue Jacob and others at the Department <strong>of</strong> TeachingMedia at the General <strong>Hospital</strong> for’ the art work and also to The Charlotte Frances May Foundation for their generousfinancial support which has made the publication <strong>of</strong> this booklet possible.
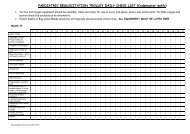
TABLE 1 - Average Number <strong>of</strong> Admissions per Annum.Period 1884-1908 1909-17 1927-36 1884-1908 1909-17DiagnosisAgeTB,Rheumatism529101015Nephritis-14Under 1 year32Respiratory68471-4 <strong>years</strong>238D&V-2125-9 <strong>years</strong>2634Other infection21910+ <strong>years</strong>1211Malnutrition5615Ophthalmia1-Accidents4546Length <strong>of</strong> Stay.Abscess5620Under 2 weeks2920Surgical (Hot)711232-4 weeks1226Surgical (Cold)--541-3 months1730Ts&As2027 413Over 3 months31Other E.N.T.-394OrthopaedicOther inc. Skins456102262Table 2 - In-patients Treated during 1899-1900NO SEX AGE ADMITTED DISCHARGED DISEASE. RESULT1 M 8 <strong>years</strong> May 2 nd July 4 th Eczema Cured2 M 6 <strong>years</strong> June 17 th July 12 th Pneumonia Cured3 F 4 <strong>years</strong> June 18 th July 16 th Injury to leg Cured4 M 2 <strong>years</strong> June 20 th Aug 2 nd Debility Cured5 M 6 <strong>years</strong> July 9 th July 18 th Circumcision Cured6 M 4 <strong>years</strong> July 23 rd Aug 1 st Circumcision Cured7 F 6 <strong>years</strong> July 27 th Aug 13 th Abcess <strong>of</strong> the neck Cured8 M 12 <strong>years</strong> July 30 th Aug 14 th Adenoids and enlarged tonsils Cured9 F 3 <strong>years</strong> July 31 st Sept 15 th Phthisis Improved10 F 4 <strong>years</strong> Aug 2 nd Aug 18 th Adenoids and enlarged tonsils Cured11 M 9 <strong>years</strong> Aug 9 th Oct 9 th Typhoid Cured12 M 7 months Aug 10 th Aug 25 th Diarrhoea and sickness Cured13 F 5 <strong>years</strong> Aug 14 th Sept 28 th Fractured femur Cured14 F 3 <strong>years</strong> Aug 16 th Oct 29 th Rachitis Improved15 M 1½ <strong>years</strong> Aug 18 th Sept 3 rd Diarrhoea and sickness Cured16 M 12 <strong>years</strong> Aug 20 th Oct 20 th Hip joint disease Improved17 F 9 <strong>years</strong> Aug 24 th Oct 5 th Consumption Cured18 F 9 <strong>years</strong> Sept 2 nd Oct 9 th Bright’s disease Cured19 M 6 <strong>years</strong> Sept 14 th Oct 8 th Axilliary abcess Cured20 F 3 <strong>years</strong> Oct 6 th Oct 29 th Adenoids and enlarged tonsils Cured21 F 5 <strong>years</strong> Oct 9 th Nov 19 th Enteric fever Cured22 M 7 <strong>years</strong> Oct 10 th Oct 15 th Circumcision Cured23 F 12 <strong>years</strong> Oct 17 th Oct 31 st Adenoids and enlarged tonsils Cured24 M 12 <strong>years</strong> Oct 20 th Jan 17 th Hip joint disease Improved25 M 11 months Nov 17 th Nov 30 th Bronchitis Cured26 M 9 months Nov 18 th Dec 1 st Diarrhoea and sickness Cured27 F 11 <strong>years</strong> Nov 20 th Jan 10 th Typhoid and pneumonia Cured28 F 6 <strong>years</strong> Nov 28 th Jan 27 th Chorea and burns Improved29 F 3 <strong>years</strong> Nov 29 th Dec 12 th Adenoids and enlarged tonsils Cured30 F 8 <strong>years</strong> Nov 30 th Feb 27 th Fractured femur Cured31 M 1 year Dec 5 th Jan 4 th Burns Cured32 F 5 <strong>years</strong> Dec 5 th Jan 6 th Influenza Cured33 F 13 <strong>years</strong> Jan 3 rd Mch 25 th Boriasis Cured34 F 12 <strong>years</strong> Jan 22 nd Mch 8 th Debility Improved35 M 4 <strong>years</strong> Feb 14 th Mch 22 nd Rachitis Improved36 F 10 <strong>years</strong> Mch 14 th May 30 th Emaciation Improved37 F 3 <strong>years</strong> Mch 17 th Mch 24 th Adenoids and enlarged tonsils Cured38 F 12 <strong>years</strong> Mch 26 th May 26 th Psoriasis Cured39 F 2 <strong>years</strong> Mch 28 th Apr 28 th Rachitis40 F 3 <strong>years</strong> Mch 29 th Apr 30 th Bronchitis and pneumonia Cured41 F 13 <strong>years</strong> Mch 29 th Apr 19 th Chronic meningitis No improvement42 F 4 <strong>years</strong> April 1 st Apr 24 th Bronchitis and pneumonia Cured43 M 10 <strong>years</strong> April 14 th Apr 26 th Debility Improved44 F 6 <strong>years</strong> May 17 th May 23 rd Adenoids Cured45 M 1 year May 18 th June 3 rd Bronchitis Cured46 M 13 <strong>years</strong> May 18 th June 16 th Hip joint disease Improved47 M 7 <strong>years</strong> May 23 rd June 18 th Injury to leg Cured48 F 6 <strong>years</strong> May 24 th June 10 th Ganglion <strong>of</strong> ankle Cured49 M 3 <strong>years</strong> June 5 th June 18 th Pneumonia Cured50 F 7 <strong>years</strong> June 8 th June 16 th Adenoids CuredThe Infant Mortality rate in <strong>Southampton</strong> was well over 100 per 1000 births and remained so until World War I and thedeath rate for children under 5 was also over 100. Even as late as the 1930s the Medical Officer <strong>of</strong> Health reported that36% <strong>of</strong> the children were undernourished, The main causes <strong>of</strong> death in childhood appear to have been gastro-enteritis,measles, scarlet fever, diphtheria and whooping cough. Although the rules <strong>of</strong> the hospital forbade the admission <strong>of</strong>infectious cases, several such are listed including diphtheria, scarlet fever and gonorrhoea. The Isolation <strong>Hospital</strong> was not
In 1903 there was a donation <strong>of</strong> £5 to renew all the house linen. Mrs Milne Stewart established the Linen League in 1910.The members <strong>of</strong> this group undertook to provide all the linen and clothing required by the hospital. A local draper <strong>of</strong>feredspecial prices for certain items e.g. “Red Flannel Jackets for children <strong>of</strong> 3 to 18 <strong>years</strong>— Flannel at 1/6d per yard”. In 1891some minor alterations and additions were made to the building but on the following year the hospital went through adifficult period following “a constant change <strong>of</strong> matrons and several untoward circumstances”. At this time also, DrBeaumont left to be replaced by his partner, Dr W.G. Collins. He was joined in 1895 by Dr R.D.H. Gwillim and Dr HowardSaunders; both became consultants after a few <strong>years</strong>. The latter later recalled his first operation, a tracheostomy on achild with diphtheria performed with the aid <strong>of</strong> a candle-lit reading light held by a nurse. In 1899 for the first time the Hon.Treasurer was able to announce that he had cash in hand at the end <strong>of</strong> the year. In its first fifteen <strong>years</strong> the hospital hadtreated nearly 700 in- patients and 5000 outpatients but it remained a very small institution. <strong>Southampton</strong> was expandingfast and was engulfing the village <strong>of</strong> Shirley. There was strong pressure for increased accommodation at the hospital. Soin 1900, in spite <strong>of</strong> continuing financial difficulties, it was decided to establish a Building Fund to be used either to enlargethe existing house or to purchase a more suitable building for the hospital. In 1911 the original house was purchased for£574 and alterations estimated to cost £1000 were proposed.However in 1912 the Managing Committee received an option to purchase Anglesea House in Winchester Road for£1000 so the plans to enlarge the house in Church Street were abandoned and the move to Anglesea House agreed. Thehouse which had been the home <strong>of</strong> Mr Crowther Smith one <strong>of</strong> the original members <strong>of</strong> the Managing Committee requiredvery little modification in the first place to provide ten beds. An appeal was made for furniture and ‘The Shirley Children’s<strong>Hospital</strong> and Dispensary for Women and Aged Men’ was opened by Mrs Henderson on September 26th 1912 at aninformal ceremony and blessed by the Vicar <strong>of</strong> Shirley while the Band <strong>of</strong> the Borough Police played “admirable selections”in the grounds. The original house in Church Street was sold to the Liberal Club for £500.Prior to 1913 it had been the practice to close the hospital for six weeks each summer for the matron’s holiday duringwhich time the building could be cleaned; however in that year the closure was for two weeks only and after that it wasagreed that the practice should cease and a fully qualified sister be engaged to cover the period. However the wards weresubsequently closed on several occasions in the following <strong>years</strong> on account <strong>of</strong> infections such as German measles,measles and erysipelas.Further development had to be suspended during World War 1 but the work <strong>of</strong> the hospital continued as before. Risingprices and an overdrawn bank balance caused much concern. There was increasing difficulty in recruiting nurses andsalaries had to be increased. Several <strong>of</strong> the medical staff were called up and were difficult to replace. Food rationing wasintroduced in 1918, twelve persons being registered as resident at the hospital. Matron’s Christmas party was reduced toa small tea party for in- patients and a few out-patients.In May 1919 the medical staff proposed that the hospital should be enlarged by converting the existing waiting room anddoctors room into an additional ward. It was soon shown however that it would be more economical to build a new singlestorey wing to house outpatients and some extra beds and it was proposed to install electric lighting. There was also asuggestion that provision should be made for maternity cases but this was not agreed. Another suggestion was made thatthe Vicarage next door should he purchased but this proposal was not acted on for twenty <strong>years</strong>. At this time a largelegacy from the late Mr J.F.Obree became available so it was decided to add a 15 bed ward above the proposed newO.P.s at a total cost <strong>of</strong> £1631. The New Obree Wing was opened by H.R.H.Princess Beatrice, Queen Victoria’s youngestdaughter, who had become Patroness in 1920. She remained Patroness until her death in 1944. At Dr Saunderssuggestion the title <strong>of</strong> the hospital was changed from The ‘Shirley’.... to The ‘<strong>Southampton</strong>’ Children’s <strong>Hospital</strong> andDispensary for Women.With the doctors returning to civilian life there were moves towards increased specialisation. In 1919 Dr Stewart startedan E.N.T. department and two G.P.s were appointed as Hon. Anaesthetist. In 1921 a new Out-patient department for thetreatment <strong>of</strong> skin diseases was set up under Dr Saunders and a Massage Department was added in charge <strong>of</strong> anHonorary Masseuse. It was suggested that some second hand X-ray equipment should be purchased but this wasdeemed to be too expensive and, as two other institutions in the town had such equipment, unnecessary. A ‘five wirehouse telephone’ was donated in 1924.Mr Walter Purvis joined the medical staff as Hon. Surgeon to replace Mr Nelson who had died and Dr Seager Thomasbecame the first Honorary Pathologist. The E.N.T. department became increasingly busy and Mr Norman MacKeith tookover from Mr Stewart in 1926. The remainder <strong>of</strong> medical staff were still G.P.s practicing within about a mile <strong>of</strong> the hospital.The first resident medical <strong>of</strong>ficer, Dr Laurel Heny, was appointed in 1929.The inter-war period saw a marked increase in the number <strong>of</strong> cases treated. In the period 1920-1930 there was a five foldincrease in the number <strong>of</strong> children admitted while the number <strong>of</strong> out-patients trebled. No longer did children come mainlyfrom Shirley and adjacent perishes but the catchment area now included the whole <strong>of</strong> <strong>Southampton</strong> and increasingly fromplaces further afield. However the main cause for this increase was undoubtedly the growing popularity <strong>of</strong> adenotonsillectomy;this operation and other E.N.T. cases accounted for 76.9% <strong>of</strong> surgical admissions. There was also agreater diversity in the types <strong>of</strong> the other cases treated. (Table IIl). There was an increasing amount <strong>of</strong> ‘cold” surgery withcases being admitted for radical cure <strong>of</strong> hernia, undescended testis, phimosis (circumcision).etc while on the “hot” sidethere was a steady flow <strong>of</strong> appendicitis and small numbers <strong>of</strong> intusussception and pyloric stenosis many <strong>of</strong> whom died.The other common causes <strong>of</strong> death were pneumonia, meningitis, gastro enteritis and prematurity. Considerable use was
made <strong>of</strong> local convalescent homes particularly that at Testwood which closed in 1928.To be admitted, a patient now required not only a referral letter from his panel doctor but also two introductory letterswhich would last for one month though an O.P. attendance needed only one letter. A subscriber had at his disposal onesuch letter for every 10/6d subscribed. The unfortunate parents would have to hunt around for a patron with letters tospare before their child could be treated. However emergencies and accidents were treated without question. No chargeswere made and a suggestion that 2/6d be charged for a dental gas was firmly turned down. The rules at this time statedthat “Only women and children <strong>of</strong> those parents who are unable from want <strong>of</strong> means or other urgent cause, to be suitablytreated elsewhere and who after medical examination are shown to be in need <strong>of</strong> treatment are to be admitted aspatients”. One subscriber complained to the committee that a child whose father earned £7 per week should not havebeen treated at the hospital.In 1936 revised rules state that the parents <strong>of</strong> patients who could afford to do so, were to be asked to contribute towardsthe cost <strong>of</strong> treatment and maintenance. There was also mention <strong>of</strong> a Pay Bed ward but this does not appear to have beenestablished. Introductory letters were no longer required.Before the war the hospital had largely relied on subscriptions anddonations for finance but with the increased size and turnover there wasa need to find much more money. The Linen League continued to bevery active and provided not only linen but furnishings for the newnurses’ home. Pound Days also continued. The annual Carnival and flagdays were a valuable source <strong>of</strong> funds. Many <strong>of</strong> the local businessesparticularly the big shipping companies gave large donations butimportant contributions were also made by a number <strong>of</strong> working men’sorganisations notably the <strong>Southampton</strong> Tramwaymen. A ‘Penny in thePound’ scheme whereby some employers deducted that amount from aman’s wages as a form <strong>of</strong> health insurance was introduced to befollowed by other contributory schemes. Various new fund raisingschemes were introduced. A Children’s League was started in 1927 whereby individual schools in the neighbourhoodwere encouraged to support a particular named cot. In 1928 the ‘Gugnunc’ cot was endowed. This was the first <strong>of</strong> severalsuch cots ‘Named in Perpetuity’ each costing the donors £600. Probably the last to be endowed was the ‘Reid’ cot tocommemorate Flight Sgt. John Reid who had been shot down over Germany in 1944. It is sad that all the commemorativeplaques for these cots were lost when the hospital closed in 1974.In 1925 the first part <strong>of</strong> a new nurses’ home fronting Vinery Gardens was opened thus releasing accommodation in themain building for a small ‘tonsil ward’ The remaining half <strong>of</strong> the nurses’ home together with a lecture room was completedin 1931. Further expansion took place in 1927/9 The kitchen was enlarged and linked to a new ward kitchen above by a‘dumb waiter’. The Shirley Wing was added to the front <strong>of</strong> the building providing a new department for Massage, electricaland sunlight treatment together with X-ray on the ground floor and a 15 cot ward and sun balcony above, thus bringingthe total number <strong>of</strong> cots available to 45. New provision was made for the dispensary thus freeing space for a dressingsroom in Out-patients. An oxygen tent was donated in 1938. In 1928 a number <strong>of</strong> ladies volunteered to provide teaching tosome <strong>of</strong> the in-patients, The hospital was visited in 1929 by H.R.H. Prince <strong>of</strong> Wales who was surprised at its small size.In it’s Jubilee Year (1934) plans were made for a very large increase insize to provide up to 100 beds; this was to be achieved in stages over anumber <strong>of</strong> <strong>years</strong>. An appeal was organised for Stage 1 to raise £5000 -£6000 in order to build a new out-patients, a new theatre, a lift and tomake various other improvements. Number 5 Vinery Gardens waspurchased at the same time. At that time the theatre was upstairs byWard 1, The extensions were opened the following year by the Bishop <strong>of</strong>Winchester Dr Garbett, bringing the number <strong>of</strong> beds up to 55. In 1940Oakfield House a substantial Victorian building next door which had beenthe Vicarage, and later belonged to Dr H. Carter, was purchased, It washoped that this would provide additional in-patient accommodationthough in the event it was used for administrative <strong>of</strong>fices andaccommodation for senior nursing staff.At the outbreak <strong>of</strong> World War 2 the children were evacuated to Lord Mayor Treloar’s <strong>Hospital</strong> at Alton but emergenciescontinued to be admitted though they were transferred to Alton as soon as they were fit enough to be moved. Adults werealso admitted to Ward 2 but this practice ceased in 1942. The Children’s <strong>Hospital</strong> also acted as a First Aid Post and wascontinually manned by stretcher bearers during the Blitz on <strong>Southampton</strong>.During the air raids patients who were fit enough were brought down to the central corridor which had been speciallyreinforced and put to bed on benches later to be used in Casualty. Seriously ill children had to remain in the wards upstairsaccompanied by a nurse who was issued with a ‘tin hat’ for’ her’ own protection. In the event the hospital escapedany damage in the air raids though some bombs and also an enemy aeroplane fell uncomfortably close. ln 1942 DrMargaret Desser the R.M.O., herself a refugeefrom Czecho-Slovakia, and Dr K.Slaney received awards for bravery from the Ring for saving air raid casualties from the
ubble <strong>of</strong> a house. However once the worst <strong>of</strong> the Blitz was over children who had been evacuated from the city began todrift home. The <strong>Hospital</strong> routine began to return towards normal and there were more admissions. The O.P. Departmentremained active. Clinics for women continued until 1945 although in the previous year it had been agreed to delete thewords “and Dispensary for Women” from the title <strong>of</strong> the hospital. The nursing routines at this time were fairly rigid; childrenwere bathed on admission and had daily blanket baths. There was also the routine daily ‘head round’. Wounds weredressed daily. But there was little time for nurses to amuse the children and visiting was restricted to one hour onWednesdays and Sundays. Babies’ milk feeds were prepared in the wardkitchens where the food for the older children was also dished out. It wasa very basic diet with breakfast, lunch and tea and lights out at 7 p.m. Inaddition to nursing duties the nurses, who were all resident, wereresponsible for much <strong>of</strong> the cleaning and polishing in the wards and formanning the telephone out <strong>of</strong> <strong>of</strong>fice hours. When the domestic was awayor at weekends the nurses would have to do the washing <strong>of</strong> nappies andwoollens in the little laundry next to the mortuary down the garden! Thenurses were also actively involved in various forms <strong>of</strong> fund raising. A keyperson at this time was Mr Tee the porter/caretaker who not only took thechildren to the theatre but was always available for many jobs about thehospital and with his wife developed the garden to produce vegetablesand kept chickens.Clinically the types <strong>of</strong> cases admitted resembled those before the war but with the advent <strong>of</strong> sulphonamides and laterpenicillin the treatment <strong>of</strong> infections such as meningitis became possible. Small premature babies were still beingadmitted for care and those with gastro- enteritis were nursed in the side ward <strong>of</strong> Ward 2 by the ward staff.Even before the war was over plans were being made for further developments. In 1945 Dr C,E.M. Joad, the popular “Anyquestions” philosopher, launched an appeal on the radio for funds which brought in £1,549 towards the proposed 25 bedward in Oakfield and an up-dating <strong>of</strong> the X-ray Department. In 1947 proposals were put forward to enlarge the hospital to150-200 beds to include an infectious disease unit. The physiotherapy unit was moved to the Oakfield kitchen in order toprovide room for a small gastro-enteritis ward and a milk kitchen was also established.The other major project which was suggested was the provision <strong>of</strong> aconvalescent home. Various properties were considered before it wasagreed to purchase Brixedone House at Bursledon for the sum <strong>of</strong> £15,750.The deal was concluded on the 26 th <strong>of</strong> June 1948 just days before theinauguration <strong>of</strong> the N.H.S. This large country house with extensive outbuildings and grounds overlooking the upper reaches <strong>of</strong> the Hamble Riverhad been the home <strong>of</strong> the Thistlethwaite family before the war but had thenbeen commandeered, first to accommodate families made homeless by theair raids and later by the Navy, who used it as quarters for W.R.N.S.Several new appointments were made to the medical staff, Dr GeorgeOrmiston was appointed Paediatrician in February 1947. He had done much <strong>of</strong> his post-graduate training in the U.S,A.and had worked with Dr Alexis Hartmann in St Louis. He was expert in the field <strong>of</strong> water and electrolyte metabolism. Soonafter his appointment he set up a new Gastro- enteritis unit on the Ground floor in what had previously been the Massagedepartment. Dr Mary Copes who was already working in the area as a Child Psychiatrist was appointed to the Children’shospital in 1948. The number <strong>of</strong> junior medical staff was increased to three.IN THE <strong>NHS</strong>The introduction <strong>of</strong> the National Health Service in 1940 brought major changes to the administration <strong>of</strong> the old Voluntary<strong>Hospital</strong>s such as the <strong>Southampton</strong> Children’s. National funding replaced the previous contributory schemes andvoluntary efforts. Administration became more centralised and pr<strong>of</strong>essional. The Children’s <strong>Hospital</strong> thus became one <strong>of</strong>the <strong>Southampton</strong> Group <strong>of</strong> hospitals, itself part <strong>of</strong> the South West Metropolitan Region whose headquarters were inPortland Place, London. At that time there were only three general children’s hospitals in the South <strong>of</strong> England outsideLondon; Brighton, Bristol and <strong>Southampton</strong> the latter being the only one in the South West Metropolitan Region.Our local managing authority was the Group <strong>Hospital</strong> Management Committee (H.M.C.) with Mr Frank Jennings as itssecretary and chief executive <strong>of</strong>ficer. Each hospital had its own House Committee (in our case combined with Romsey<strong>Hospital</strong>) which took over from the old Managing committee but had decreasingly less power. Mr Bedford who had beenChairman <strong>of</strong> the old committee continued as Chairman until 1955 when he was succeeded by Pr<strong>of</strong>essor Rayment. In histurn he was briefly followed by Dr G.Johnson <strong>of</strong> Romsey and Miss F Wright S.R.N. before Dr W. Angus a local G.P. tookover the committee for many <strong>years</strong>. Medical matters were dealt with by the group Medical Advisory Committee (M.A.C.)comprising a number <strong>of</strong> hospital consultants, but it too had limited executive power. The medical staff <strong>of</strong> the hospital hadour own committee which met once a month. All medical committee meetings were held out <strong>of</strong> working hours and <strong>of</strong>tencontinued late into the night.There were also great changes on the medical front. The previous medical staff, mostly local practitioners living nearby
and supported by others with specialist status, all <strong>of</strong> whom had given their <strong>service</strong>s entirely voluntarily, were graduallyreplaced by nearly whole time specialist consultants. Considering the magnitude <strong>of</strong> these changes they took placeremarkably smoothly with very little acrimony.Dr George Ormiston (1947) and Dr Mary Capes (1948) had both joined the staff <strong>of</strong> the hospital prior to the ‘AppointedDay’ and I was appointed Consultant Paediatrician in November 1949. Like Dr Ormiston,I had responsibilities inWinchester as well as <strong>Southampton</strong>. At that time most consultant appointments were designated “maximum part-time”i.e.9/11ths, so that we were able to have some private practice, In my case this never amounted to very much and laterwhen it was permissible, I opted to go full time. An important feature in those days was the Domiciliary Consultation whichwas quite a formal affair with the G.P. nearly always present. As well as being a valuable perk for the consultant they didgive him a chance to meet the G,P,s and also an opportunity for him to see the inside <strong>of</strong> the patients homes,At the Children’s <strong>Hospital</strong> in 1950 Miss Golay was matron and there were two main wards. Ward I. Gillespie, was dividedinto two sections the main one in the front overlooking Winchester Rd. had beds along one side and cots along the outerand there was also the ‘balcony’, which had previously been enclosed, providing 20 beds in all. In 1951 cubicles wereconstructed along one side <strong>of</strong> the ward with the loss <strong>of</strong> 5 beds. At the top <strong>of</strong> the stairs opposite the ward kitchen there wasa small treatment room with a side ward for skin cases next door. The poor babies with generalised eczema there werenursed naked with their limbs splinted to prevent scratching and painted all over with Gentian Violet. Next to the wardkitchen there was a two-bedded sick bay for nursing staff which later became the treatment room: a severe case <strong>of</strong>tetanus was successfully nursed there for several weeks. Nursing procedures were still quite primitive. With no CentralSterile Supply <strong>service</strong> all instruments etc had to be sterilised on the wards. Urine specimens from infants were collectedby means <strong>of</strong> a glass bird feeder strapped on with ‘Elastoplast’ under the nappy.At the back was Ward II, Obree, which accommodated 11 surgical and 12 ‘clean’ medical cases, Dr Ormiston’s smallgastro-enteris ward on the ground floor with Sister Hughes in charge had six cubicles. Dr Ormiston liked to have aspecimen <strong>of</strong> each baby’s stool on display in an enamel pie-dish at the foot <strong>of</strong> its cot, One nurse has complained that thisput her <strong>of</strong>f rice pudding for life! Dr Ormiston retained sole charge <strong>of</strong> the unit until he retired.Ward I was presided over by Sister “Bunty” Boyce a wonderful person in the very best traditions <strong>of</strong> her pr<strong>of</strong>ession. Shewould <strong>of</strong>ten be found still on duty late at night when one <strong>of</strong> her ‘treasures’ was in danger. She was adored by the childrenas well as by their parents. The whole hospital was delighted when later she was awarded an M.B.E. in recognition <strong>of</strong> herdevoted <strong>service</strong>. She retired in 1966.In 1948 12 children (900 p.a.) were still being admitted to Ward I for Ts& As on alternate days but this ceased with the opening <strong>of</strong> the children’sE.N.T. ward at the General. In the fifties infections such as poliomyelitis,congenital syphilis and tuberculosis were still quite common. There wasusually at least one case <strong>of</strong> TB meningitis requiring daily intrathecalinjections <strong>of</strong> streptomycin in the wards. Miliary tuberculosis too was notuncommon nor were bone and glandular T.B. due to the bovine bacillus.Although most town milk was pasteurised, this <strong>of</strong>ten did not apply inrural districts. Gastro-enteritis was still the dreaded complication forhospitalised infants.In most winters there was an epidemic <strong>of</strong> acute infantile laryngotracheo-bronchitis.Sometimes this almost overwhelmed our facilities.Every available cot would be occupied by a wheezing baby whileoccasionally some had to be accommodated temporarily in odd boxes or drawers. Steam kettles and oxygen tents wereeverywhere. The infant’s condition could deteriorate extremely quickly and it was always difficult to decide just when tocall in the E.N.T.surgeon to do a tracheostomy. One has vivid memories <strong>of</strong> Mr Alex Rusell, himself a severe asthmatic,arriving in haste at the top <strong>of</strong> the stairs by Ward I wheezing as badly as the infant he had come to treat!Cystic fibrosis had only recently been separated <strong>of</strong>f from coeliac disease and most <strong>of</strong> the cases died in infancy. Thesweat test had not yet been invented. The cause <strong>of</strong> coeliac disease itself was still a mystery so that there was no effectivetreatment. Cases <strong>of</strong> ‘pink disease’ were still quite common. These were particularly miserable babies with characteristicitchy pink palms and soles. The condition disappeared as soon as it was shown to have been caused by mercurypoisoning from so-called ‘teething powders’. Childhood diabetes was much less common than it is to-day and there weretwo schools <strong>of</strong> thought regarding the importance <strong>of</strong> strict dietary control.We had very little to <strong>of</strong>fer the unfortunate children with malignant disease. Those with various solid tumours had surgeryand probably radiotherapy at the Royal South Hants <strong>Hospital</strong> but those with leukaemia were usually sent home with aprognosis <strong>of</strong> only a few weeks to live, <strong>of</strong>ten to be readmitted in their terminal phase. A development in the late fifties wasthe gradual appreciation <strong>of</strong> the importance <strong>of</strong> non-accidental injury to children; with hind-sight it was apparent that manysuch cases had been missed, sometimes being mis-diagnosed as infantile scurvy.The streptococcal related disorders <strong>of</strong> acute nephritis and rheumatic fever were quite common. In both cases they weretreated by graduated bed rest .The progress was very gradual, starting in the case <strong>of</strong> rheumatic fever, with three weeksflat on the back without pillows. After a week or so at Winchester Rd the children were transferred to Bursledon so that
they could receive some schooling. The clinical progress was monitored by, among other things, a weekly R.S.R. Thenecessary venepuncture became quite a ritual which was accepted with remarkable stoicism by most <strong>of</strong> the children.Usually there were also several children at Bursledon with nephritis (both types I and II) and others with Still’s disease all<strong>of</strong> whom were treated with graduated bed rest. Sydenham’s chorea also was quite common. Dr Copes and I made astudy in which we suggested that the disorder was not a manifestation <strong>of</strong> rheumatic disease. Fortunately we neverpublished our results as chorea disappeared concurrently with rheumatic fever! Children with these diseases <strong>of</strong>tenremained at Bursledon for six months or more.Bursledon Annexe as it was called, had been a privatehouse. One approached it along a fine drive throughpark-like grounds. On entering the building one cameinto a very large oak panelled hall with a grand oakstaircase and a fine fireplace. The hall made anexcellent play area. Although the Annexe waspurchased in 1948, it was only partially occupied at first,being opened fully in November 1950. On the groundfloor there were three large rooms each opening on tothe veranda which adapted easily to provide 23 longstaybeds for school aged children while three similarrooms upstairs provided an equal number <strong>of</strong> beds foryounger children. A nursery unit for T.B. babies withfeeding problems plus accommodation for two motherswas established in what had been the Nursery wing.Breast feeding was out <strong>of</strong> fashion at that time andalthough the midwives at the Maternity Unit might claima 50% rate on discharge, many <strong>of</strong> the mothers switchedtheir babies to the bottle as soon as they got home. During the war the Government had introduced National Dried Milkwhich was obtained from infant welfare clinics at a subsidised rate. Feeding schedules were generally rigid: four hourlyfeeds x5 being the rule while smaller infants were given half cream milk. Solids in the form <strong>of</strong> cereals such as Farex werenot introduced until the age <strong>of</strong> about six months.The demand on these long-stay (not in any way to be confused with ‘convalescent’!) beds was such that the unit was<strong>of</strong>ten fully occupied particularly on the ground floor. In summer months the children from the ground floor wards werewheeled out in their beds on to the large sunny veranda. The garden was the scene <strong>of</strong> a near tragedy when a group <strong>of</strong>toddlers in a playpen decided to act in unison and succeeded in pushing their pen to the edge <strong>of</strong> the fish pond in themiddle <strong>of</strong> the lawn, into which they plopped one by one! Fortunately none <strong>of</strong> them was drowned and the fish pond wasconverted to a rose bed. Another memorable occasion was when Bursledon was unexpectedly invaded by children fromthe Swanage Children’s <strong>Hospital</strong>, a convalescent home on the cliffs above Peverill Point which suddenly threatened toslide into the sea.One <strong>of</strong> the important assets <strong>of</strong> Bursledon was that children could continue with their education. In December 1949 theHMG requested the Hampshire Education Authority to provide a teacher and Mrs Groll was appointed in May 1950.Bursledon was <strong>of</strong>ficially recognised as a “<strong>Hospital</strong> Special School” in September 1951. In the early days the teaching wasentirely in the wards; the medical and nursing staff having to take great care to disturb the lessons as little as possible.Later, with the changing character <strong>of</strong> the patients, purpose built wooden buildings were erected behind the hospital. I amvery grateful to Mrs Brenda Marshall the last headteacher for giving me her account <strong>of</strong> the school which is included inChapter VIII.On the surgical side in 1950, Mr Richardson was the only surgeon on the staff: he was joined in 1951 by Mr TomRowntree who recalls that at that time the theatre at the Children’s <strong>Hospital</strong> was the best in the city. Mr Richardson retiredin 1968 and Mr John Webster joined the staff In his place. In his time Mr Rowntree was responsible for developing someimportant innovations. In order to reduce the distress <strong>of</strong> extensively burned small children requiring daily dressings, hedecided to try treating them naked under strict barrier control in individual cubicles The results were most satisfactory forpatients and staff alike. He also abandoned the use <strong>of</strong> pelvic drains in cases <strong>of</strong> perforated appendicitis and <strong>of</strong> deepsutures in muscle splitting incisions. The abolition <strong>of</strong> these procedures led to a reduction both <strong>of</strong> discomfort and <strong>of</strong> woundsepsis. Perhaps his most important innovation devised in collaboration with the anaesthetist Dr Pat Shackleton was thethen revolutionary decision to treat hernia cases as Day patients, a practice which was to be further developed by MrAtwell.Ramstedt’s operation for pyloric stenosis was always popular with surgeons. We in <strong>Southampton</strong> never subscribed to theclaim that treatment should be ‘medical’ although a locum for Dr Ormiston who had trained with Dr Jacoby atFarnborough did treat his own cases and even did a Ramstedt’s operation himself. Babies for operation would bebandaged to a crucifix and given a dummy, sometimes dipped into syrup <strong>of</strong> chloral, to suck while the operation wasperformed under local anaesthetic.A controversial question was that <strong>of</strong> the circumcision clinic at that time held weekly in O.P.s by the S.H.O.s. Following aprovocative article by Dr Douglas Gairdner, a paediatrician, in the ‘Lancet’ entitled ‘The fate <strong>of</strong> the Foreskin’ manypaediatricians believed that this mutilating operation was usually unnecessary and should be abolished. At the Children’s
hospital there was pressure to ensure that at very least the S.H.O.s should be properly instructed in the technique.In the early 1960s surgery on hydrocephalus by means <strong>of</strong> the Spitz-Holter valve became possible and the early closure <strong>of</strong>spina-bifida was also widely advocated for all cases. Mr Rowntree accepted this policy with some reluctance. It led to agreat increase in the number <strong>of</strong> survivors many <strong>of</strong> whom had severe medical, surgical and social problems. As the fullimplications <strong>of</strong> this policy became apparent many difficult ethical considerations also came to the fore.On a National level the policy also resulted in an increase in the total surgical work load which together with thedevelopment <strong>of</strong> neonatal surgery led to a government working party calling for’ the establishment <strong>of</strong> Regional PaediatricSurgical Centres throughout the country. This pressure together with the fact that Mr Rowntree had been invited tobecome the first chairman <strong>of</strong> the reorganised Group Medical Executive Committee led to his resignation from S.C.H. andthe appointment in 1969 <strong>of</strong> Mr John Atwell as the first full time Paediatric Surgeon with Regional responsibilities. He wasshortly to be joined by Mr Neil Freeman. One <strong>of</strong> the best remembered persons in the surgical team was Flo Coady. Shecame to the hospital during the war <strong>years</strong> as a Red Cross volunteer and Mr Richardson recalls that at times she ran thetheatre almost single handed. She continued to work in the theatre in different capacities finally as sister for over twenty<strong>years</strong>.Sadly in the end she had to resign because she had never done her general training. During her time in theatre she wasalmost obsessional in her devotion. She made herself available at all hours <strong>of</strong> the day or night seldom taking days <strong>of</strong>f.When the theatre was not in action she would spend hours cleaning and polishing. Subsequently she continued toprovide a very valuable <strong>service</strong> running medical clinics or O.P.s.The Out-patients Department on the ground floor below Ward II was approached along a narrow and dangerous drive tothe side <strong>of</strong> the hospital. In 1950 it was in the charge <strong>of</strong> Sister Jenny Tutcher. There was a fair sized waiting hall with alarge fish tank in front <strong>of</strong> the seats and a small canteen with Gladys in charge, behind.To the left <strong>of</strong> the main entrance was the reception window and records <strong>of</strong>fice. A friendly face at the reception window canmake all the difference to an apprehensive child and it’s mother. We were particularly fortunate in having a succession <strong>of</strong>wonderful people in the <strong>of</strong>fice starting with Miss Yeates and followed by Mrs Jean Foster and later by Mrs Carol Whealey.Some <strong>of</strong> the patients notes were stored in the <strong>of</strong>fice but the rest were in the old stables down the garden next to themortuary; an unpleasant trip for the staff on a wet day. Sharing the <strong>of</strong>fice with the records staff was a medical secretary.Next to the Records <strong>of</strong>fice, Miss May. the Lady Almoner, had a minute <strong>of</strong>fice shared with her clerk. In the corner was thepharmacy with a hatch into the waiting room and a preparation and sterilising room behind. Miss Stevens was thepharmacist in charge in 1950 to be followed by Mr Miller and later Miss Tracey.There were two smallish inter-communicating consulting rooms which housed the O.P. clinics. Each clinic was run in asomewhat different way according to tire consultant’s preference. He was supported by either sister or by a staff nursewho would call the patients in from the waiting hail outside. They would have previously been weighed and measured inCasualty. In my clinics sister also made any necessary follow-up appointments in the room before the patient left. Therewas usually a saucer <strong>of</strong> ‘Smarties’ on the consultant’s desk as well as a selection <strong>of</strong> small toys. In addition to theconsultant and sister there was <strong>of</strong>ten a G.P. Clincal Assistant or student in the room not to mention the patient and hismother. I was very fortunate in that once a week Dr Capes would be using the adjacent consulting room so that I couldeasily get a snap psychiatric opinion on a case without having to wait for a formal appointment. The size <strong>of</strong> the clinicsvaried considerably; if they were mainly ‘old’ patients there could be thirty or more in a session. But probably not morethan ten new patients would be seen at a timeIn the course <strong>of</strong> time special clinics such as cardiac, diabetic, psychosomatic, spastic, adolescent etc were establishedsometimes held jointly with a visiting consultant In addition there were dermatological, E.N.T., physiotherapy and speechclinics mostly for internal referrals only. Once a week the consulting rooms would be cleared for Dentals and a formidablelooking dental chair would replace the usual desk, with the anaesthetic machine in the adjoining room, Except for a few<strong>years</strong> during the war Mr Sanders ran the weekly dental clinic from 1939 until the hospital closed in 1974.The Casually Department was on the other side <strong>of</strong> the waiting room with it’s treatment room complete with a gas heatedsteriliser and anaesthetic machine. Many <strong>of</strong> the children presenting at the department were ‘casuals’ rather’ than truecasualties. It was a busy department which was always open. As well as providing a very valuable <strong>service</strong>, it also gaveimportant experience for the junior staff. Later there was strong pressure to close the department and the open hourswere reduced to 9 a.m. to 5.30 p.m.The Children’s hospital was not the only unit in <strong>Southampton</strong> which treated children :in fact in 1940 there were <strong>of</strong>ficially165 children’s beds in the Group <strong>of</strong> which only 65 were at S.C.H. . A 28 bed ward at the General <strong>Hospital</strong> admittedchildren mostly for Ts and As.. Orthopaedic children were nursed at the Royal South Hants <strong>Hospital</strong> and at Lord MayorTreloar’s at Alton. The Eye <strong>Hospital</strong> had a small children’s ward and at the old Isolation, then the Chest <strong>Hospital</strong>, therewas an old fashioned infectious disease block (Pavilion A.) as well as a modern children’s ward for cardiac cases. Laterwhen Dr McLachlan retired the paediatric staff took over the care <strong>of</strong> the infectious patients (including a few adults) inPavilion A. and included the unit in our junior staff rota.It was several <strong>years</strong> before we were allowed access to the babies in the Maternity Unit. Intensive care for neonates was
very much in its infancy and little specialised equipment was available. Intravenous fluids were either administered into ascalp vein or by cut down. Incubators were usually obtained on hire from Oxygenaire. When in 1955 the wife <strong>of</strong> aninternational banker en route for London, unexpectedly gave birth to premature twins in <strong>Southampton</strong>, a question wasasked in the House <strong>of</strong> Commons a few days later as to the number <strong>of</strong> incubators at <strong>Southampton</strong> General <strong>Hospital</strong>. Theresponse was very gratifying! Exchange transfusion for haemolytic disease <strong>of</strong> the newborn had recently been introducedand I well remember my first successful case in Winchester being reported on the local radio. Once the procedurebecame well established however, it began to take up an unacceptable amount <strong>of</strong> our time and became quite a problem.We were one <strong>of</strong> the first units to develop phototherapy for neonatal jaundice using our own home made apparatus ornatural sunshine when available. We also pioneered the use <strong>of</strong> a plastic oesophageal tube for feeding premature infants.During this period there was almost continuous pressure to close the Children’s <strong>Hospital</strong> on the grounds that it washopelessly out <strong>of</strong> date and that the average bed occupancy was unacceptably low. On this point we were able to showthat this was due to a very high turnover. The average stay in a bed at Winchester Rd being only a few days; in fact therewere periods <strong>of</strong> acute bed shortage. The medical staff agreed that the hospital certainly did need updating but stronglyopposed the suggested closure and transfer to the General <strong>Hospital</strong>. Then in 1956 an unexpected factor came to our aid;this was a very unpleasant outbreak, in <strong>Southampton</strong>, <strong>of</strong> sepsis due to anew type <strong>of</strong> staphylococcus (Phage type 00). Itwas believed to have arrived in the city via the ships from Australia and first presented in the general surgical wards aswound sepsis and in the Maternity Unit as breast abscesses etc. It did not take long to spread to the babies in theMaternity Unit or to Winchester Rd itself. The epidemic in <strong>Southampton</strong> lasted for about two <strong>years</strong> before it burnt itself outbut it was interesting to follow it’s very gradual spread outwards over several <strong>years</strong> to involve in turn centres throughoutthe whole country.At the Children’s <strong>Hospital</strong> we were able to point out the obvious dangers from our out dated sluices and lack <strong>of</strong> isolationfacilities. Local M.P.s became involved and in June 1958 Mr Howard M.P. for <strong>Southampton</strong> Test, tabled a question inParliament asking when the buildings <strong>of</strong> the <strong>Southampton</strong> Children’s <strong>Hospital</strong> would be replaced. The Minister <strong>of</strong> Health,Mr Derek Walker Smith, replied that improvements costing £20,000 would start almost at once. The Managementcommittee had reluctantly agreed to allocate this sum for a major facelift. Again it was argued that this was ‘money downthe drain’ and that an entirely new comprehensive children’s hospital should be built but funds for such an enterprise werenot available.Unfortunately the work necessitated the closure <strong>of</strong> the wards and in July1958 the in-patients were transferred to Willan ward in the Royal SouthHants <strong>Hospital</strong> and the gastro-enteritis babies to the Chest <strong>Hospital</strong>. Outpatientswere held in cramped conditions on the ground floor <strong>of</strong> the Nurseshome. The modernisation involved cubiclization <strong>of</strong> most <strong>of</strong> Ward I, theextension <strong>of</strong> Ward II and the provision <strong>of</strong> new sluices and other equipment.We ended up with 7 cubicles and 10 beds in Ward I and 8 cubicles plus twowards <strong>of</strong> 8 and 4 beds in Ward II. The work took longer than expected buteventually the hospital was reopened in June 1959 by Mrs Victoria King,chairman <strong>of</strong> the H.M.C., supported by three local M.P.s.The question <strong>of</strong> visiting was, for a long time, a thorny one. Until World War IIvisiting was allowed from 2-4 p.m. daily Sundays excepted but then itbecame confined to 1 hour on Wednesday and Sunday afternoons and in 1947 it was banned completely for fear <strong>of</strong> crossinfection. In 1950 however very limited visiting (1 hour on weekdays except Fridays and 1 hour on Sundays) was againpermitted though the parents had to wear facemasks. On a National level Dr John Bowlby and Mr James Robertson hadalerted public opinion to the possible psychological trauma suffered by young children admitted to hospital. Dr MaryCapes strongly supported their views and led a long campaign to liberalise visiting hours not only at the Children’s<strong>Hospital</strong> but also in the other units in <strong>Southampton</strong> admitting children. In the former with the support <strong>of</strong> most <strong>of</strong> the staffshe was very successful and S.C.H. became quite a national model in this respect. ‘Free visiting’ (11 a.m.-7 p.m.) wasestablished experimentally in 1959. In the following year a successful appeal was opened by the League <strong>of</strong> Friends toprovide sleeping accommodation for two mothers in a small attic room on the second floor which was much appreciated.By the middle sixties the number <strong>of</strong> cases <strong>of</strong> rheumatic fever and nephritis had declined sharply and Bursledon becameincreasingly involved with psychosomatic and behavioural disorders. It was no longer necessary to have a residentmedical <strong>of</strong>ficer there. In place <strong>of</strong> the R.M.O. we established the post <strong>of</strong> Clinical Assistant which was held part-time by asuccession <strong>of</strong> married women doctors, the longest serving <strong>of</strong> these was Dr Jean Davies who was appointed early in the1960s and continued until the unit closed in 1988.During the sixties also we became increasingly involved with the care <strong>of</strong> children with chronic handicaps. Previously wehad been concerned mainly with the more obvious types <strong>of</strong> mental handicap such as Diran’ s syndrome but thesechildren tended to disappear into Tatchbury Mount or Cold East and we lost touch. Rubella embryopathy was relativelycommon until vaccination against German measles was introduced. Children with cerebral palsy were cared for by MrsWelch at her house in Rose Road and in 1951 at the purpose built Spastic Centre in Aster Road.In 1962 we were suddenly presented with a number <strong>of</strong> babies with stunted limbs and other serious malformations. It wassoon realised that these cases were being born to mothers who had taken Distaval (thalidomide) in early pregnancy.Many <strong>of</strong> these babies died but some survived with varying degrees <strong>of</strong> handicap. One <strong>of</strong> my cases (Graham) was bornwithout any limbs, eyes or ears, it was thus quite impossible to communicate with him although somehow he did seem
able to respond to a radio placed on his cot and would hum the Beatles tune ‘Yellow Submarine’ Also at this time it firstbecame possible to prevent the development <strong>of</strong> severe mental handicap in cases <strong>of</strong> phenylketonuria by the strictimplementation <strong>of</strong> a very unpleasant dietary regime.It became increasingly apparent that there were a great many handicapped children in the area who required care andwhose families needed support. Their problems were complex and involved many different medical, social andeducational disciplines. It seemed essential to try to coordinate these various bodies in order to provide an integrateddiagnostic and caring <strong>service</strong>. The groundwork for this multi-disciplinary approach was laid down in the later sixties andhas <strong>of</strong> course been greatly expanded since.Also, recognition <strong>of</strong> the rubella and thalidomide types <strong>of</strong> embryopathy together with the fact that for the first time it hadbecame possible to identify human chromosomes and to relate certain syndromes such as Down’s with chromosomeabnormalities, suddenly opened up the whole field <strong>of</strong> the causation and prevention <strong>of</strong> congenital disorders. Dr ElspethWilliams went to London to learn the techniques <strong>of</strong> genetic counselling from Dr Cedric Carter and others and later carriedout a number <strong>of</strong> family studies in the <strong>Southampton</strong> district on certain hereditary disorders such as spina-bifida andcongenital heart disease. When her training was completed she set up a weekly genetic clinic at the Children’s <strong>Hospital</strong>which was one <strong>of</strong> the first in the country. In time this developed into a substantial Regional <strong>service</strong>. We were veryfortunate in having an excellent liaison with Marina Seabright who at the same time was developing a top class laboratorycytogenetic <strong>service</strong> in Salisbury.1969 saw the start <strong>of</strong> a new system <strong>of</strong> medical administration: the main clinical disciplines formed ‘Divisions’ each <strong>of</strong>which provided a representative to serve on the Medical Executive Committee which was given increased authority. TheDivision <strong>of</strong> Child Health comprised not only those consultants with child patients, representatives <strong>of</strong> the junior medical.nursing and administrative staffs but also a G.P. and a senior member <strong>of</strong> the Community Child Health Service. TheDivision proved to be a very valuable forum for the discussion <strong>of</strong> child health matters.We were also very fortunate at this time in having a close liaison with Pr<strong>of</strong>essor Donald Court <strong>of</strong> Newcastle laterPresident <strong>of</strong> the B.P.A. and author <strong>of</strong> the report ‘Fit for the Future’ . His help and advice on many matters involving thehospital was invaluable.The arrival <strong>of</strong> Mr John Atwell in 1969 had a big effect on the surgical side <strong>of</strong> the hospital. As well as developing hisregional commitments the volume and complexity <strong>of</strong> the surgical work at S.C.H. increased dramatically. His particularinterest was in the urinary tract. He was also responsible for a tremendous growth in the amount <strong>of</strong> Day Surgeryperformed; by 1973 well over a thousand such cases were treated annually including hernias and orchidopexies.An essential corollary <strong>of</strong> this was the creation <strong>of</strong> the Paediatric Home Nursing Service which he instituted with the help <strong>of</strong>Miss Isobel Ames and the M.O.H. At first this comprised two children’s trained sisters working within the boundaries <strong>of</strong> thecity but with very close ties with the hospital. This <strong>service</strong> also had the added advantage <strong>of</strong> enabling the earlier discharge<strong>of</strong> post-operative patients. From these early beginnings the <strong>service</strong> has expanded greatly under the direction <strong>of</strong> SisterPeggy Flint and Mr Atwell to become a very important national front runner.The old O.P. department was converted to provide a 5 bed ward for these cases in the previous treatment room and alsoan additional 10 bed surgical ward (Ward III). Casualty was housed in the previous consulting rooms.A new single storied temporary Out Patients building was erected in the car park behind the original block which providedconsiderable additional accommodation for consulting rooms etc.SPECIAL DEPARTMENTSPharmacyA Lady Dispenser was appointed in 1898 in order, it was hoped, to reduce thedrug bill. Miss Martin who was appointed in 1906 was paid 7/6d per week; sheresigned in 1915 for health reasons and her place was taken by MissBurniston the Hon. Secretary who was, fortunately, qualified. She complainedthat the dispensary scales, which were also used for kitchen purposes, hadbecome inaccurate and out <strong>of</strong> date. In 1924 a dispenser was loaned by Bootsfor a while to cover a gap at the hospital. In 1950 the dispensary was incharge <strong>of</strong> Miss Stevens who was followed in 1954 by Mr Miller and later in1959 by Miss TracesI am indebted to the latter for her account <strong>of</strong> “Life in the Pharmacy”“I realised after a very short time that my first impression <strong>of</strong> the Pharmacy wasfar from correct. I was escorted down a very long corridor past the warm smells <strong>of</strong> cooking, then anaesthetics, and into asmall room. The walls were clad from ceiling to floor with shelves, workbenches and banks <strong>of</strong> drawers. It was my firstventure into real pharmacy. Until then my life had been full <strong>of</strong> variety. As a freelance locum I had managed shops
throughout the South and the Isle <strong>of</strong> Wight. The big one was Boots at Henley on Thames during Regatta Week, thesmallest a village pharmacy in the heart <strong>of</strong> the New Forest. When I changed course it was from ‘Chanel’ to carbolicovernight.I was a lost soul in my new post and felt very much the new girl. For the first month or so there was so much to learn. Mytechnician guided me through the colours <strong>of</strong> nurses’ uniforms and other staff, but I had no problem identifying matron. Thefolk in white coats or suits were a study on their own. “Is that a doctor or a surgeon?” “Is that doctor or should I sayMister?” Etc. Very soon I realised that I had joined one big happy family and was singing carols round the wards followedby mince pies and sherry in Oakfield.Life behind the hatch was very busy and each day had its strict routine. The baskets from the wards, theatre, X-ray andPath Lab arrived on a trolley at 9 a.m. These were collected by the porters at 11 a.m. Treatment cards then arrived forany patients requiring special drugs or T.T.O.s (To Take Out). Twice weekly the Bursledon basket arrived accompaniedby their T.T.O.s. We dreaded periods before Christmas and other holidays when so many children were allowed homefor a break.Monday afternoons were a pleasant change. We went “down to the store” and left a note on the door to that effect. Hereorders for dressings and sundries were assembled for the wards and theatre. The room was situated at the back <strong>of</strong> theChapel and was devoid <strong>of</strong> any form <strong>of</strong> heat. It was agony in the winter and the orders were completed in record time! Acup <strong>of</strong> Bovril from Gladys in the canteen quickly revived us.Friday afternoons were unforgettable. It was Skin Clinic time. The mothers regularly visited with their pathetic littleeczema sufferers and patiently wailed for their big bags <strong>of</strong> assorted creams, lotions and syrups. It was a very noisygathering and many friendships blossomed among the mothers over a cup <strong>of</strong> tea and a cake. I must confess that thenoise <strong>of</strong> the toys was curtailed by a careful extraction <strong>of</strong> any squeaks or quacks! Musical instruments were hidden. Oneafternoon a bright little lad hit on the idea <strong>of</strong> using our door as a station for his push-along train. By careful timing I openedthe door and the engine sped along the Pharmacy floor to be lost forever. Another occasion comes to mind when I calledout the name <strong>of</strong> an anti-histamine syrup instead <strong>of</strong> the child’s name. Needless to say no Mum responded and I retreatedinto my hole with a very red face!Other afternoons were spent preparing infusion fluids. The department was responsible for supplying the whole hospital.All the drug supplies were ordered and delivered daily from the Royal South Hants. One day a miracle arrived in the form<strong>of</strong> proprietary infusions. We continued to prepare our special sterile products, particularly the formula to the milk room fordehydrated infants,The problems <strong>of</strong> supplying the various departments with instruments and sundries were many. Stock sizes were too largefor children and infants. Most <strong>of</strong> our orders were sent via the main Supplies department, to the appropriate firms.Proprietary mixtures and syrups were <strong>of</strong>ten unsuitable and needed to be adjusted for the weight and age <strong>of</strong> the child.Many problems were solved by cutting tablets into halves or quarter’s with a scalpel blade and converting the pieces intopowders. Another obstacle would be overcome by emptying ampoules to form the base <strong>of</strong> a required mixture.The Pharmacy also supplied oxygen and other gases to the wards and theatre. lt worked well on anarrangement with British Oxygen on a “full cylinder for an empty” basis. Towards the end, we were fitted with pipedoxygen which saved many dramas from shortage <strong>of</strong> porters to move the “big oxygens”.A big occasion was the Wednesday afternoon Clinical Meeting. These took place regularly and we carefully watched forthe day to arrive. At 3 p.m. our front door was closed, so we rushed round the wards beforehand to top up supplies toeveryone before we were imprisoned! Any further business was conducted from outside through the window over thesink,During the <strong>years</strong> I was there we saw the tragedy <strong>of</strong> the thalidomide babies. It was harrowing to know that a drug on ourshelves could cause so much distress. On a happier note I also saw the advent <strong>of</strong> steroids and cytotoxic drugs and manybroad spectrum antibiotics,It was a sad day when the patients left “to go the General”. I can remember the green van collecting items from the wardswith a teddy bear tied to the front <strong>of</strong> the bonnet. Goodbye to a very special era.Massage DepartmentThis department was set up in 1921 with the appointment <strong>of</strong> MissHounsell as Honorary Masseuse. She requested the purchase <strong>of</strong>electric equipment to give galvanic stimulation and it was agreed toobtain this second hand from R.V. H., Netley. Unfortunately whendelivered it was found to be only suitable for a direct current! Howevershe did give 600 treatments in 1921. Ten <strong>years</strong> later in 1931 therecords show that 1401 massage and 1682 electrical treatments weregiven as well as 438 Swedish Remedial Exercises.
A new department. including X-ray was provided in 1928 on the Ground floor <strong>of</strong> the new Shirley Wing built on to the front<strong>of</strong> the old house. Dr Vincent Rice was appointed to the staff in the following year being in charge <strong>of</strong> massage, electrotherapyand x-ray. The department was run by Mrs Thomas from 1931 to 1947. In that year Dr Ormiston wanted space forhis new gastro-enteritis ward so the physiotherapy section <strong>of</strong> the department was moved across the side drive to the oldkitchens at the back <strong>of</strong> Oakfield. Dr Jim Preston was appointed Director <strong>of</strong> Physical Medicine in 1948 and attended theChildren’s <strong>Hospital</strong> on alternate Thursday afternoons until we moved in 1974. The department consisted <strong>of</strong> three rooms, awaiting room, a treatment room and a storeroom. As well as a desk and couch the treatment room had wall and parallelbars and also ultra-violet and infrared lamps. At first the main referrals were children with asthma and some with minororthopaedic disorders but later those with cerebral palsy and spina-bifida dominated the scene. Many <strong>of</strong> these requiredprolonged physiotherapy and perhaps the provision <strong>of</strong> appliances following orthopaedic operationsX-ray Department“As mentioned above, X-ray equipment was first provided in 1928. After thewar this had become obsolete and an appeal for funds to buy a newmachine was launched. With the transfer <strong>of</strong> Physiotherapy across the drivethe X-ray department became independent and Dr Rice confined hisresponsibilities to radiology. Consultant cover was rather thin for some<strong>years</strong> and I had to do my own screening <strong>of</strong> heart cases. I also did my ownbronchograms using a technique I had learned at Great Ormond Street,which involved the introduction <strong>of</strong> a barbarous cannula through the cricothyroidmembrane. I soon abandoned this method.Dr Ivan Hyde came to the Children’s <strong>Hospital</strong> in 1965 to replace Dr BobCaton, Dr Rice having retired earlier. Anne Arscott was the radiographer incharge assisted by a part-timer doing three sessions. The previoussecretarial cover had been lost. Dr Hyde remembers “The main entrance tothe hospital was by a side door into a small hall around which were clustered the telephone exchange, Matron’s <strong>of</strong>fice, themilk kitchen, the main passage and the entrance to the X-ray department. Immediately inside this door was a sizeableroom containing the x-ray set which was suitable for straightforward radiology and fluoroscopy (with dark adaptation).Opening <strong>of</strong>f this room by a narrow passage were in sequence, the darkroom, a small <strong>of</strong>fice and a lavatory, in which theyalso made the c<strong>of</strong>fee. All film processing was manual, In 1967 Anne Arscott left and was replaced by Sandra Read.During this year David Williamson asked me it I thought an image intensifier would be a suitable objective for the<strong>Southampton</strong> Carnival Appeal, an opportunity not to be missed, The appeal was supported by Dr Horace King, Speaker<strong>of</strong> the House <strong>of</strong> Commons and the machine was handed over by Dr and Mrs King in July 1970. Drs Brunton and Burrowsalso attended the hospital but were replaced by Dr Cook in 1968”.“1969 was a milestone when I was allowed a part-time secretary. She was Sheila Clement, who came as a temp. from thesecretarial agency and stayed with us until her retirement. In May this year JDA arrived and the pace <strong>of</strong> changeincreased”.“The second part-time Radiographer post was filled by a number <strong>of</strong> excellent young ladies - Jenny Bullivant, Hilary Smith,Stella Bowyer. Most <strong>of</strong> our radiographers left to have babies and many <strong>of</strong> them came back to us afterwards in a part-timecapacity and some are still with us. In 1971 we acquired a second part-time secretary, Rosemary Port, also from theagency and she is still with us, soon to retire (1990).“From about 1968 Registrars in training in Radiology came to the Children’s as part <strong>of</strong> their course and they are all nowconsultants.“The thing that stands out most in my recollections is the quality <strong>of</strong> the Radiographers. Their work was <strong>of</strong> a high standardunder very difficult conditions. No one grumbled about working too hard or too long and being such a small hospital therewas a very good rapport with the nursing staff, admin, domestics, porters - everyone employed on the site. The sameapplied to Sheila Clement and Rosemary Port when they were appointed secretaries One never had any demarcationdisputes or rivalries.“John Atwell and Neil Freeman provided us with a substantially increased workload <strong>of</strong> greater complexity. They drew inan enormous amount <strong>of</strong> surgical material, which required more radiological investigations, and all <strong>of</strong> us felt it was apleasure to work with such experts. Working in such a well-defined children’s unit gave us the nucleus to transfer bodily tothe General <strong>Hospital</strong> where we could so easily have been fragmented and separated from the body <strong>of</strong> Paediatrics.Looking back the accommodation and facilities were poor but no worse than those at the General and Royal South Hants.“The neonatal ward was next to the X-ray department which was very convenient as sister would pick up the very sickbabies and transport them for immediate radiology and back to the ward in no time at all. We learned how to handle thesesick infants with confidence and we also learned how to accommodate the increasing volume <strong>of</strong> cases with dispatch. Itwas the time when spina-bifida was treated aggressively - we did enormous numbers <strong>of</strong> micturating cystograms, IVPsand air encephalograms. Congenital abnormalities <strong>of</strong> the Gl and GU tracts also required radiological investigations bothbefore and after operation.“Medical paediatrics did not change in such a revolutionary manner - it was a case <strong>of</strong> more <strong>of</strong> the same. Pr<strong>of</strong> Normand
and his team pointed us in the direction <strong>of</strong> academic disciplines; I think we had to adopt a more academic approach;although it is difficult to describe the changes we encompassed, I hope that we seized the opportunities to stretchourselves”.Radiography was seldom straightforward; Diana Claisse recalls doing micturating cystograms on small children <strong>of</strong>ten withassistance from young helpers from the ward “that with taps running, whistles and cold hands on the tummy, it was morelikely us that wanted to perform than the child,” while Ann Arscott remember’s Dr Caidwell’s Friday afternoon skin clinics -“he used our blackout facilities for detecting rigwur’m with UV light, the Xray room being bigger than the linen cupboard hehad to use if we were busy, We also had the occasional wart charming — he sent children along to Xr’ay - I pointed thexray tube at the <strong>of</strong>fending wart without making an exposure. He seemed to think it was quite effective!”Pathology DepartmentDr Seager Thomas was appointed as Hon. Pathologist in 1925 but he died in 1934 being replaced by Dr Gleave who alsodied in <strong>of</strong>fice in 1952. Dr Steven Dobson from the General <strong>Hospital</strong> then supervised the Children’s <strong>Hospital</strong> until theappointment <strong>of</strong> Dr Joan Guy in 1957. A small laboratory in the attic was established in 1947 staffed by a part-timetechnician who became full time in 1949.Dr Joan Guy has recorded her own memories <strong>of</strong> the department:“When I arrived in <strong>Southampton</strong> at the end <strong>of</strong> 1957 it was suggested that having spent some <strong>years</strong> in paediatrics beforebecoming a pathologist, l might like to take an interest in the Children’s <strong>Hospital</strong>. The Path Lab was a small attic, ill-lit andill ventilated, perishingly cold in winter and unbearably hot in summer reached by a steep narrow flight <strong>of</strong> stairs. Therewas also a post-mortem room next to the mortuary in the old stable block down the garden. The less said about it thebetter and it was with no regret that it was abandoned in 1961 when the first new autopsy room at the General was built.This was certainly more hygienic though less convenient for the clinicians.A technician visited every afternoon to take blood samples, do simple blood counts and E.S.R.s and test urines. It wasquite obvious that this was inadequate so the first step was to increase her hours. The suggestion met with resistance inthe Pathology Deportment but the problem was soon solved when it became known that she was pregnant. In 1958pregnant technicians were rare in the laboratory and were considered an embarrassment, so full time work at theChildren’s <strong>Hospital</strong> was a form <strong>of</strong> honourable banishment and was agreed. This was the beginning <strong>of</strong> a real pathology<strong>service</strong> and by dint <strong>of</strong> scrounging old equipment we began to increase the range <strong>of</strong> work. An old incubator was found sourine and C.S.F. could be cultured and sensitivity tests done. When new microscopes were bought for the Gerreral<strong>Hospital</strong> one <strong>of</strong> their cast-<strong>of</strong>f s was acquired and was much better than our previous one. Sheila stayed to the eighthmonth <strong>of</strong> her pregnancy with everyone becoming increasingly anxious about her negotiating those awful stairs carryingtrays <strong>of</strong> specimens.Hazel replaced Sheila: she was a senior technician, experienced in both haematology and bacteriology. She liked workingon her own and the scope <strong>of</strong> the work increased steadily. When the hospital was up-graded in the early 60’s we lookedfor a better site for the laboratory. A room was available in Oaklands next to the coal-hole. This room measuring aboutl0’x14’ became the lab and the coal-hole about 8’ square became the venesection room. A narrow passage leading intothe hall was blocked <strong>of</strong>f and turned into a washing-up room and a small area <strong>of</strong> the hall with a door leading into the frontgarden blocked <strong>of</strong>f to form the pathologist’s <strong>of</strong>fice. The whole suite was minute but compared with the attic it was palatial.It was painted pink and was convenient for Out-patients, though hazardous as the main door opened directly on to thedrive with a constant flow <strong>of</strong> traffic. Mercifully no-one was ever injured though it was highly dangerous.At this time the pathology <strong>service</strong> was being increasingly used by G.P.s so they were invited to send child patients toWinchester instead <strong>of</strong> to the General <strong>Hospital</strong> where children had been considered noisy, difficult and generallytroublesome. Work increased rapidly and the fight for extra staff began. A nurse-venesector came in the afternoons, thena secretary for two hours a day to type reports. She suffered from the antique typewriter we acquired but struggled on tilla better one became available. A great advance was the acquisition <strong>of</strong> a washer-up for 1 hour each morning. Thisrelieved the technician <strong>of</strong> the time-wasting chore <strong>of</strong> cleaning glassware. An ancient autoclave was found at the Generaland this terrifying piece <strong>of</strong> apparatus was installed and mastered with much trepidation. The hospital van called three orfour times a day to collect specimens. Chemistry results came back much faster. Frank, the van driver, became our greatally in spite <strong>of</strong> occasional fits <strong>of</strong> “temperament” that were hard to bear.This was a time <strong>of</strong> real pleasure for me, working on a one-to- one basis with some <strong>of</strong> our very best technicians. Hazel wassucceeded by Angela and then Della took over. These girls were superb, more like housemen. They were very skilled atvenepuncture and at times they succeeded in putting up drips where new housemen had failed. They were quick to spotthe ill child sent up by G.P.s and always took extra blood for relevant investigations that had not been requested to savethe child a further venepuncture. They learned to take histories <strong>of</strong> recent infections, diet and drugs and frequentlyelucidated the cause <strong>of</strong> an anaemia or purpura, sometimes to the chagrin <strong>of</strong> our clinical colleagues. They could sense anew leukaemia almost as the child came in through the door and would ask the parent to wait while they rushed the countand film through and telephoned me to come at once to confirm the diagnosis and take action. It became accepted thatthe technician post at Winchester Road was one with special responsibilities and we were allowed a junior as it wasthought to be such a good training post. When automated staining machines came on the market we put in for one and itwas a great success having a cycle time <strong>of</strong> 15 minutes. About the same time we also got a blood sugar analyser.
After about six <strong>years</strong> the place began to look shabby, so we put in for redecoration only to be told that we were not on theschedule for another 3-4 <strong>years</strong> but that the walls could be washed. This was not a great success and the place still lookeddingy and unattractive. So we resolved to redecorate the outer room ourselves Angela and I went to town and bought fiverolls <strong>of</strong> enchanting nursery wall—paper. Two <strong>of</strong> the men from the General came and painted the ceiling and window.Every evening after work we stayed on paper hanging while various housemen dropped in to help. Much c<strong>of</strong>fee andsandwiches and the occasional fish and chips were consumed; (these were the days before the Health and Safetyregulations forbade eating and drinking in laboratories). Everyone was delighted with the results especially the childrenwho found the place much less forbidding; everyone that is except for Mr Wood, for we had told no one <strong>of</strong> our plan andhad not asked for permission. When it was discovered, the hospital painters almost threatened to go on strike and had tobe placated. When his wrath had subsided even Mr Wood had to agree that it was a great success and when eventuallythe paper showed signs <strong>of</strong> wear, he agreed to it being replaced <strong>of</strong>ficially.These were very happy and rewarding <strong>years</strong> with the lab staff being integral and respected members <strong>of</strong> the hospital staff.We were sad to leave Winchester Road knowing that it was an end <strong>of</strong> an era for pathology. Present-day lab staff havevirtually no contact with patients. Most routine tests are automated and done in vast batches. Clinicians are rarely seen inlaboratories and are more likely to be known as aggressive voices at the end <strong>of</strong> the telephone. The volume <strong>of</strong> work hasincreased phenomenally as has the sophistication <strong>of</strong> investigations and equipment but what proportion <strong>of</strong> these tests arerelevant and is the overall pattern <strong>of</strong> investigation as cost—effective as it used to be? It is my impression that laboratoriesare not the happy places they were”.Almoner/Social Work DepartmentDuring the thirties if a patient requiring treatment was not adequately covered by one <strong>of</strong> the health insurance schemes,the Secretary, Miss Matthews, would see the parents and make the necessary arrangements. The first whole time LadyAlmoner, Miss Rosamund May was appointed in 1948. She was closely involved with the clinical staff and regularlyattended consultants ward rounds. Her family reports were always interesting and with her own family connections withthe stage seldom lacked drama! Mr Rowntree recalls her tale <strong>of</strong> the mother who brought her third illegitimate baby to thehospital. When Miss May gently suggested that she might consider getting married she replied, “Oh no. When I was 18 Ihad something wrong with my heart, and the doctor said I should never marryMiss May retired in 1969 and was replaced by Miss Jeanne Christie.STAFFA hospital is <strong>of</strong> course more than just a matter <strong>of</strong> bricks and mortar; it is the staff that give it it’s reputation - good or bad.In later <strong>years</strong> at least, the Children’s <strong>Hospital</strong> was fortunate in having a contented staff who worked together as a teamand whose main objective was to serve the patients entrusted to their care.It is sadly not possible to recall all those who at various times during it’s 90 year existence served the hospital in somecapacity or other. I have however attempted to list the more senior members <strong>of</strong> staff in Appendix I.Nursing Staff.The Matron who initially was referred to as (Lady) Superintendent was for many <strong>years</strong> responsible for the housekeepingand general running <strong>of</strong> the hospital as well as performing her nursing duties. At first she was probably supported by justone other nurse with a second in 1892. In 1894 we are told “The Lady Superintendent has also attended to 12 or morecases in the past 12 months”. Presumably she was, ante-dating the present Paediatric Home Nursing Service by a goodmany <strong>years</strong>!By 1911 there appear to have been a sister and a probationer nurse while the Superintendent was given permission toemploy an extra nurse from Mrs Haldane’s agency during the busy season at £1 per month. She herself was paid £40p.a. plus £10 per month for the running expenses <strong>of</strong> the hospital. In addition they were all given a Christmas box by theManaging Committee each year.In 1913 the nursing staff was increased by a staff nurse and a second probationer and it was agreed that the probationersshould be given some formal training though this was not implemented until 1921 The domestic staff appears to haveconsisted <strong>of</strong> a cook/general and a part time charwoman paid 1/- for a half day.In 1918 a Mrs Lambert from New York, applied to spend a month at the hospital in order to receive nursing tuition frommatron.By 1921 the nursing staff comprised: matron, one sister, a night nurse, a staff nurse and two probationers who were
enrolled for one year. At this time it was again suggested that some formal training should be given to the probationers;Dr Gillespie agreed to give lectures and arrangements were also made for the nurses to attend the Royal South Hants<strong>Hospital</strong>.In 1929 the nursing staff had increased to two sisters and two staff nurses. However matron would still go along to the‘village’ to do the shopping. Miss Tomkinson resigned from the post <strong>of</strong> matron after nineteen <strong>years</strong> <strong>service</strong> in 1928 andwas replaced by Miss L. Sellers who had been Assistant Matron at the Royal <strong>Hospital</strong> for Sick Children in Edinburgh. Shein her turn, served for seventeen <strong>years</strong> before having to retire on account <strong>of</strong> ill health. Miss Sellers was succeeded byMiss Golay from Great Ormond Street in 1944.During World War II the nursing staff consisted <strong>of</strong> matron, 4 sisters and 10-12 nurses but they were <strong>of</strong>ten short staffed.The normal working hours were from 7.30 a.m. - 9 p.m. with 2 or 3 hours <strong>of</strong>f and one day <strong>of</strong>f per week. Night duty wasfrom 9 p.m. - 8 a.m. with one late night per week starting at 10 p.m. The night nurses did 4-6 weeks duty running withouta night <strong>of</strong>f. They were paid about £40 - £50 p.a. and discipline was strict.By the end <strong>of</strong> 1948 the number <strong>of</strong> nursing staff had increased to 56 including 6 sisters, 30 students and 11 P.T.S. Thenumber continued to increase quite quickly to reach 91 in 1950. Thereafter there was much concern over decliningnumbers (down to 71 in 1954). Over the following ten <strong>years</strong> numbers again remained fairly steady but the proportion <strong>of</strong>students gradually dropped following the closure <strong>of</strong> the Training school.Nurse TrainingA training school for Sick Children’s nurses was established in the thirties, being <strong>of</strong>ficially recognised in 1936, but it had tobe suspended at the outbreak <strong>of</strong> hostilities, reopening again in 1944 when Miss Morgan from Great Ormond Street wasappointed Sister Tutor The first students then being those whose training had been interrupted by the war. Thereafter theintake was about four students every four months.A classroom had been included in the second part <strong>of</strong> the nurses home opened in 1931 but this was abandoned in favour<strong>of</strong> the ground floor <strong>of</strong> one <strong>of</strong> houses in Vinery Gardens. the upstairs <strong>of</strong> which being occupied by the resident medical<strong>of</strong>ficers. At first there was no P.T.S and no block system - lectures taking place during <strong>of</strong>f-duty hours. Nurses had to go upto London for their final R.S.C.N. exams. After the acquisition <strong>of</strong> the Bursledon Annexe, Miss Morgan was temporarilyappointed as Sister in charge and the P.T.S. was also housed there temporarily. Later the school was at WestwoodHouse for a short while before returning to Winchester Road.In addition to the course for the R.S.C.N. certificate a Preliminary Training School that accepted girls on leaving schooluntil they were 18 and able to start the proper course was initiated. The ‘Block’ system was introduced in September1950. In that year 19 candidates from the hospital sat the final R.S.C.N. exam and 15 passed. Although most <strong>of</strong> thestudents were local girls, some came from a distance, one from Thurso in the far north <strong>of</strong> Scotland and another fromGreece. Several <strong>of</strong> the students who trained at the Children’s <strong>Hospital</strong> later became valued members <strong>of</strong> the permanentnursing staff.Reports from the R.C.N. inspectors however were critical about many <strong>of</strong> the provisions in the hospitals and in 1947 therewas a threat to withdraw recognition. We used the inspector’s criticisms to put pressure on the H.M.C for improvements.Miss Morgan resigned in 1958 to become matron <strong>of</strong> a special Mother and Baby social project in Athens and was neverreplaced. Unfortunately the R.C.N. also stipulated that continued recognition as a training school depended on therebeing a minimum <strong>of</strong> one hundred occupied beds available and in spite <strong>of</strong> much fiddling with figures recognition waseventually withdrawn in 1960.Social ActivitiesWhen Miss Golay took over as matron in 1944 she started regular dances and parties for the nurses which were held inthe O.P. department. Several ex-nurses vividly remember the badly burned airmen coming over from the Marchwoodrehabilitation hospital who were always the most lively and hilarious <strong>of</strong> guests. In their turn, parties <strong>of</strong> nurses would beinvited to social functions at various <strong>service</strong> units in the district. As well as the dances the nurses also produced their ownconcerts, which were put on in O.P.s at Christmas, and <strong>of</strong> course, these provided a good opportunity to put on sometelling skits about senior members <strong>of</strong> staff.The festive season has always been important in hospital calendars From the start funds and gifts were provided forparties for both In- and Out-patients. In 1949 the H.M.C. allowed 5/- per head for Christmas festivities. On Christmas Evethe nurses would sing carols around the illuminated Christmas tree in front <strong>of</strong> the hospital. At about ten o’clock onChristmas morning the hospital would be visited by the Salvation Army Band, who played carols in each <strong>of</strong> the wards inturn. The noise was terrific but they were very popular. As soon as the band had departed Father Christmas’ entouragewould assemble in O.P.s. He and his sleigh (a trolley) would then ascend in the lift accompanied by the loud ringing <strong>of</strong> abell. He too would visit each ward in turn distributing toys to the patients as well as to the visiting children <strong>of</strong> the medicalstaff somewhat to their parent’s embarrassment! As <strong>years</strong> went by fewer and fewer children remained in hospital overChristmas and those that did were usually very sick, with the result that Father Christmas’ visit became something <strong>of</strong> anembarrassment. However it remained a pleasant social occasion when the families <strong>of</strong> the staff were able to meet
together. It was also usual for the mayor to pay us a visit. Those <strong>of</strong> us with commitments at several different hospitalsthroughout the Region had as many as half-a-dozen such visits to pay on Christmas morning. The traditional Christmastea party in Out-patients for a selected number <strong>of</strong> regular attenders was a popular annual event.Shortly after Christmas came Matron’s dance. At first this was held in O.P.s but soon after the war Dr Harold Bower whoowned the Polygon Hotel then, arranged for it to be held there each year. All the staff were invited and matron would alsoinvite men from one <strong>of</strong> the liners to make up numbers. Half way through we all sat down to a good supper though this waslater replaced by c<strong>of</strong>fee and sandwiches. In the early l950s it was a very formal affair with consultants expected to wear‘white ties’. During the dancing we, with our wives, sat at the ‘High table’ going <strong>of</strong>f to do our duty dances with matron andthe senior sisters. In later <strong>years</strong> the dance became rather less formal and perhaps less popular but we were entertainedby the spectacular dancing <strong>of</strong> Miss Tracey, the pharmacist, and her husband.In the summer Matron gave a strawberry tea party on the occasion <strong>of</strong> the nurses prize-giving held on the lawn behindOakfield under the magnificent copper beech tree to which ‘old girls’ were also invited in the hope, perhaps, that theywould re-enlist!Oakfield provided accommodation for matron and the sisters. Matron also had a very small <strong>of</strong>fice just to the left <strong>of</strong> thefront door <strong>of</strong> the hospital. The nurses lived in the nurses home in Vinery Gardens but had their meals in the dining room<strong>of</strong>f the main corridor in the hospital. In time an increasing number <strong>of</strong> nurses chose to be non-resident.Medical StaffThe consultant’s staff room was on the ground floor at Oakfield. Because we felt it was important to keep in touch withone another we tried to arrange that on one day a week (Tuesdays) we should all have lunch together. This was verysuccessful though the newly appointed Pr<strong>of</strong>essor was once heard to remark that it was more like a gardening club than amedical assembly!The first Resident Medical Officer was appointed in 1929. By 1947 there were two. It is said that during the war theR,M.O.s had to be unmarried women because they lived in the nurses quarters. The first male was appointed in 1948. By1950 there were two H.P.s and one B.S. : they lived in one <strong>of</strong> the semi-detached houses facing Vinery Gardens. Our firstregistrar, Dr George Crawshaw, was appointed in 1950 and was shared with Winchester. The number <strong>of</strong> house <strong>of</strong>ficerswas increased to four in 1959 and later to five. It was soon established that, because <strong>of</strong> the relative complexity <strong>of</strong> theirduties, the House Officers should be <strong>of</strong> S.H.O. grade. Rather complicated rotations, at first involving only Bursledon, butlater also the Infectious Disease unit at the Chest <strong>Hospital</strong>, the Special Care Baby Unit at the General and R.H.C.H.Winchester, were established. They were intended not only to cover the outer units but also to give the trainee doctors thewidest possible experience. The frequent moves were not always popular and there were other complaints about the poorliving conditions. However there were usually plenty <strong>of</strong> applicants. In 1958 arrangements were made for the registrar torotate with St George’s <strong>Hospital</strong> in London, the first <strong>of</strong> his two <strong>years</strong> being spent with us. Later in 1972 a Senior Registrarpost rotating with Portsmouth was established.StudentsFor many <strong>years</strong> sporadic students from London teaching hospitals and elsewhere came to <strong>Southampton</strong> to do their‘elective’ in paediatrics. In the late 1960s this practice was formalised when we agreed to take a regular intake <strong>of</strong> fourstudents from the Royal Free <strong>Hospital</strong>; an arrangement, which was much appreciated both by ourselves and the students.Post graduate Medical EducationPost graduate education was always considered important in <strong>Southampton</strong>. On the paediatric side, Dr Ormiston, soonafter his arrival, had started monthly clinical meetings. These were held in out-patients on Wednesday afternoons andwere aimed primarily at G.P.s and Child Welfare doctors but nurses in training were brought along by their sister tutor. Sixto eight children either from the wards or from O.P.s were demonstrated. After an hour the patients would be removedand we would have refreshments before sitting down in the Casualty room. Dr Bower and later Dr Ormiston would takethe chair. After a discussion on the cases there would be two or three more formal presentations by consultants and <strong>of</strong>tenan outside consultant would be invited to contribute. These meetings were very popular and some G.P.s came regularlyfrom many miles away. From time to time more ambitious meetings were also staged.With the rapid development <strong>of</strong> paediatrics we felt the need to keep in touch with our colleagues in other parts <strong>of</strong> thecountry. We were instrumental in founding the South West Metropolitan Paediatric club, which met at various hospitalsthroughout the region. In 1954 we hosted the summer meeting <strong>of</strong> the Paediatric Section <strong>of</strong> the Royal Society <strong>of</strong> Medicine,the first such meeting to be held away from a university centre. The proceedings started in Winchester Cathedral wheremembers were addressed by the Dean. After demonstrations and lunch at the Royal Hampshire County <strong>Hospital</strong> wemoved to Bursledon for further case demonstrations etc. Mr Tom Rowntree created quite an impression by turning up inhis donkey cart! Dr Ormiston and I had analysed our cases <strong>of</strong> nephritis types I and II and arising from this survey myfamilies <strong>of</strong> Alports syndrome came to light. Dr Capes read a paper on paediatric/psychiatric cooperation and I presentedone on the epidemiology <strong>of</strong> round worm infestation based on nearly one hundred cases, mainly related in some way tothe gipsy population. We also hosted similar meetings for the SW. Metropolitan Paediatric Club and later for the South
West Paediatric Club based on Bristol. As well as the academic content, these meetings provided excellent opportunitiesto compare each others units and for informal social activities. It was the pattern to try to lay on some local excursion formembers and their spouses.Medical library facilities were at first very poor. In 1950 we were given an allowance <strong>of</strong> £25 p.a. to provide textbooks andjournals for the hospital. This was supplemented to some extent by donations from consultant staff. There was no GroupLibrary though the other hospitals also had small individual collections. In the early sixties the anaesthetist, Dr PatShackleton was appointed Regional Post-graduate Adviser and in 1966 a Post Graduate Contra comprising a largelecture hall and dining room together with a central library, a tutorial room and <strong>of</strong>fices was opened at the General <strong>Hospital</strong>later to be replaced by the South Academic Block.The Medical SchoolThe high quality <strong>of</strong> post-graduate medical education in <strong>Southampton</strong> and the rest <strong>of</strong> the Region in the sixties was said tohave been one <strong>of</strong> the factors influencing the Minister <strong>of</strong> Health to choose <strong>Southampton</strong> in preference to Hull as the site fora new medical school. This decision in August 1967 was to be a major turning point for hospital practice in the area. Themedical staff <strong>of</strong> the Children’s <strong>Hospital</strong> played an active role in persuading the newly appointed dean, Pr<strong>of</strong>. DonaldAcheson, that a Chair in Child Health should be given a high priority and we participated in the early discussions on thecurriculum. Dr Colin Normand from UCH. was appointed to the Chair in 1970 to be followed shortly by his Senior Lecturer,Dr John Birkbeck, and lecturer, Dr Judith Darmady. These appointments together with an increase in junior staff providedamong other things a very welcome easing <strong>of</strong> the clinical load. A two storey Portacabin was erected in the car park toprovide <strong>of</strong>fice accommodation for them above and a storeroom below.AdministrationThe Secretary’s <strong>of</strong>fice, together with the Administrative <strong>of</strong>fice were at first situated on the ground floor <strong>of</strong> Oakfield but latermoved across to one <strong>of</strong> the Vinery Gardens houses. Miss Ella K.Mathews was still the Secretary in 1950. She was apowerful lady who had been in <strong>of</strong>fice since 1926 and knew everything about the working <strong>of</strong> the hospital. She retired thefollowing year to be replaced by Mr Eric Woods. He was supported in the administrative <strong>of</strong>fice by Miss Foot who did thesecretarial work and Miss Lynch who looked after the accounts. Miss Foot retired 1969 but Miss Lynch continued with usuntil we moved,There were two medical secretaries who were accommodated in different <strong>of</strong>fices and we were fortunate in having asuccession <strong>of</strong> excellent ladies in this role. At first Dr Ormiston had arranged that all the case notes should be typed andthe secretary sat in on O.P.clinics. Although an excellent idea, it had to be abandoned after a while as impractical. Theintroduction <strong>of</strong> tape recorders was a great asset but sadly less personal. An important part <strong>of</strong> the secretaries’ work wasthe typing <strong>of</strong> the patient’s discharge summaries written by the housemen. These were very valuable documents givingdetails <strong>of</strong> the child’s illness together with the investigations and treatment carried out.An valuable innovation in the late sixties was the appointment <strong>of</strong> Ward Clerks to relieve the ward sisters <strong>of</strong> some <strong>of</strong> theirclerical load.THE LEAGUE OF FRIENDSWhen the N.H.S. took over the old Voluntary hospitals their charitable fundswere transferred to the to the so-called Amenity Funds. The Children’s<strong>Hospital</strong>’s Amenity Fund was relatively large and was augmented each yearby many donations and legacies. However we found it extremely difficult toget at the amenity fund money for any project we wished to promote althoughthe H.M.C. sometimes used these ‘Free monies’ to purchase equipment etc,which we did not consider should be covered by the term ‘amenity’. Howeverthe provision <strong>of</strong> a canteen in the O.P. waiting room was entirely justified.The almoner had a special ‘Samaritan Fund’ which she could dispense toneedy families at her own discretion. It had originally been funded largely bythe Union Castle Shipping Line but later the League <strong>of</strong> Friends took on therole.Most <strong>of</strong> the fund raising organisations <strong>of</strong> the old voluntary hospitals were in time replaced by Leagues <strong>of</strong> Friends. TheChildren’s <strong>Hospital</strong> League <strong>of</strong> Friends was inaugurated on November 2nd 1954 at the instigation <strong>of</strong> Mrs M. B. Sloan andothers. She became the first Honorary Secretary and Mrs C.F. Moody Chairman. Mrs Sloan was succeeded as hon. sec.by Mrs D. E. Oxford, who held the post most energetically for 15 <strong>years</strong>. Her husband was also a very active member <strong>of</strong>the committee and is well remembered by the staff <strong>of</strong> the time for his appearance each Christmas on his sleigh wearing ared gown and a white beard! The Oxfords had lost their only child Graham in 1952. Mrs Moody resigned in 1967 to besucceeded by Mrs O. M. Bennion and later in 1970 by Mrs Thompson. Another very valuable member <strong>of</strong> the committee in
its early days was Mr Reggie Fulton who was a tower <strong>of</strong> strength in raising funds and recruiting members particularly fromlocal schools.The League <strong>of</strong> Friends grew rapidly and performed an invaluable <strong>service</strong> in providing funds and also acting as animportant link between the hospital and the general public. The main fund raising events were the twice-yearly fairs whichwere held at Winchester Road in the spring and at Bursledon in the autumn. A regular attender at the former was DrHorace King, M.P. for Itchen and Speaker <strong>of</strong> the House <strong>of</strong> Commons. At the Autumn fair there was usually an exhibition<strong>of</strong> painting by the children in the Annexe some <strong>of</strong> which reached a very high standard. Starting on a relatively modestscale with gifts <strong>of</strong> knitted garments, toys, television, out-door play equipment, etc the Friends soon undertook moreambitious projects. In collaboration with the ‘Elfin’ School <strong>of</strong> Dancing and local W.I.s, they decorated and furnished the‘Mothers Room’ at Winchester Rd and later provided large play huts at both Winchester Rd and Bursledon which werealso used for nurses recreation in the evenings.They also redecorated and furnished hospital chapel as amemorial to Peter Lynch the young son <strong>of</strong> a member <strong>of</strong> thehospital staff. On a more personal level the Friends provided atea trolley for visitors at Bursledon on Sunday afternoons aswell as canteen workers and ‘hostesses’ for out-patients also‘play ladies’ and librarians in the wards. On occasions too, inresponse to appeals from matron, members <strong>of</strong> the Leaguewould temporarily take over duties in the kitchen or on thewards when there was a staff crisis. Later the Friends turnedpart <strong>of</strong> their attention to providing major medical equipmentsuch as piped oxygen in the wards and an image intensifier X-ray. Since the move to the General <strong>Hospital</strong> in 1974 theFriends have continued to support the Children’s Unit thereand at Bursledon until it closed. Visitors to Bursledon could notfail to notice two large play items in the grounds; one was analmost life sized steam engine presented by apprentices at Hawker Siddely and the other an enormous boot-house fromthe Eastleigh Carnival.Mention must also be made <strong>of</strong> the ‘Jackdaw Fund’, This was money collected by the jackdaws in their aviary in East Park.The birds would take coins <strong>of</strong> all denominations from visitors and place them in a container. They started collecting in1948 and by 1955 had taken 38441 different coins averaging over £4 per week. This money was presented to the hospitaleach year, over many <strong>years</strong>, by Mr Moody their keeper and usually put to the purpose <strong>of</strong> purchasing some desirable item<strong>of</strong> equipment; in 1957 he presented a £400 for an incubator.PAEDIATRICS IN WESSEXIt is not possible to follow the development <strong>of</strong> the Children’s <strong>Hospital</strong> in the N.H.S. separately from that <strong>of</strong> paediatrics inthe Region generallyThe first step towards establishing a paediatric <strong>service</strong> in Wessex was the appointment <strong>of</strong> Dr George Ormiston asPaediatrician in February 1947 with responsibilities both at he <strong>Southampton</strong> Children’s and Royal Hampshire county<strong>Hospital</strong>s. His salary was to be £500 each from <strong>Southampton</strong> and Winchester. The term “Paediatrician” was quite new tothis country at this time, having been introduced from North America in the thirties. It is a curious fact that although manychildren’s hospitals were founded in Britain in the second half <strong>of</strong> the nineteenth century only a handful <strong>of</strong> doctors in thiscountry were specialising entirely in childhood illness prior to World War II.At their London H.Q. in November 1949 the Regional Board made three simultaneous appointments viz:- Dr JohnMoseley to the Portsmouth and Isle <strong>of</strong> Wight districts, Dr A.P. Norman to Bournemouth, Dorset and Salisbury, and myselfto <strong>Southampton</strong>. Winchester and Alton.Dr Moseley’s base was at St Mary’s <strong>Hospital</strong> in Portsmouth where he had two large upstairs wards without washbasins, inan old fashioned block. He had a further 20 children’s beds at Portsmouth Royal <strong>Hospital</strong>. Like ourselves he wasexcluded from access to the neonates in the maternity department for several <strong>years</strong>. At Ryde in the Isle <strong>of</strong> Wight therewere 20 children’s beds in the care <strong>of</strong> Dr A Miller. Dr Moseley paid weekly visits there and also to the neonates atNewport.In Bournemouth, Dr Norman had two very gloomy children’s wards in the ex-Poor-law institution at Christchurch. He heldout-patient clinics at the Royal Victoria <strong>Hospital</strong> in Boscombe and at the Cornelia Cottage <strong>Hospital</strong> at Poole. He also hadbeds and clinics in the Dorset County <strong>Hospital</strong> in Dorchester and at the Weymouth and District <strong>Hospital</strong>. In Salisbury hehad a ward at the ex-U.S. Army hutted hospital at Odstock with an O.P. clinic at the General Infirmary.As well as the Children’s <strong>Hospital</strong> in <strong>Southampton</strong> and the Bursledon Annexe, Dr Ormiston and I had a small children’s
ward <strong>of</strong> about 25 beds, in a separate annexe, at the Royal Hampshire County <strong>Hospital</strong> in Winchester. We did not at firsthave access to the newborn in the Maternity Unit at the General <strong>Hospital</strong>. At the time many obstetricians were unwilling tohand over the care <strong>of</strong> the neonates to paediatricians and I must confess that I personally had had practically no training orexperience in neonatology when I was appointed. However, in Winchester, Dr John Penny and Mr Phillip Mitchell werevery willing to give us the run <strong>of</strong> their nurseries and we established a happy and, I think, efficient <strong>service</strong> there.Unfortunately this happy state <strong>of</strong> affairs at Winchester came to an abrupt end when Dr Penny had to retire early for healthreasons and his successor did not hold with paediatricians caring for “his” babies. A bitter dispute ensued which, in spite<strong>of</strong> strong support from the Regional Board, we lost. In the meantime Mr Knowlton and Mr Kilgour at <strong>Southampton</strong> hadrelented and we were now involved, though at first only partially, at the Maternity Unit.Within a year <strong>of</strong> his appointment Dr Norman left to join the staff <strong>of</strong> Great Ormond Street and we in <strong>Southampton</strong> coveredhis area for several months until Dr David Beynon was ready to take over. Dr George Crawshaw who had been our firstregistrar, took over West Dorset as temporary paediatrician. He held this post until December 1955 when Dr DavidVulliamy was appointed.The Wessex Region seceded from the S.W. Metropolitan Region in 1959 having its headquarters In Winchester with thedynamic Dr John Revans as Senior Administrative Medical Officer. Dr Neville Butler was appointed to take over theSalisbury district from Dr Beynon as well as Swindon, which had been separated <strong>of</strong>f from the Oxford Region.We in <strong>Southampton</strong> again had to cover Bournemouth and Poole during Dr Beynon’s long illness though Dr PamelaDavies acted as locum for some <strong>of</strong> the time and again after his tragic death. Dr Beynon was replaced in Bournemouthand East Dorset in September 1961 by Dr Michael Simpkiss.Dr Butler resigned in 1963 to join the staff at Great Ormond Street and Dr Ormiston retired in the same year, This seemedto be an opportune time to reorganise the paediatric <strong>service</strong> in central Wessex. Under the new arrangement Dr JohnGreaves from Teeside took over Winchester with some sessions at <strong>Southampton</strong> and Dr Hughes Davies took overSalisbury with sessions at Winchester and <strong>Southampton</strong>, while I concentrated mainly at <strong>Southampton</strong> with some sessionsat Salisbury. The object <strong>of</strong> this reorganisation was intended to give each paediatrician a place at the <strong>Southampton</strong>Children’s <strong>Hospital</strong> while providing a second string at each <strong>of</strong> the district hospitals to cover <strong>of</strong>f-duty, but it was asomewhat cumbersome arrangement and Dr Hughes Davies soon decided to relinquish his sessions at Winchester. DrLilian Jones took on Swindon in 1964.During the fifties I had established peripheral out-patient clinics in Lymington, Basingstoke, Andover and Hythe. Soonafter his appointment, Dr Greaves improved the cover at Basingstoke and Andover and started a new clinic at Alton.At Portsmouth Dr George Lewis was appointed in July 1965 to support Dr Moseley and in December 1969 Dr TerryMacIntosh was appointed to Basingatoke with some sessions at Winchester, In 1973 he was joined by Dr Judith Darmadywhose contract also included some sessions in Community Paediatrics; the first such contract in Wessex and perhaps inthe U.K.. The importance <strong>of</strong> maintaining pr<strong>of</strong>essional ties with our colleagues stimulated the formation <strong>of</strong> the S. W.Metropolitan Paediatric Club early in the 1950s. Meetings were held at the various centres <strong>of</strong> the Region. However, withthe independence <strong>of</strong> Wessex, which was unique at the time in not having a medical school, loyalties tended to changeand close links were forged with Bristol. Pr<strong>of</strong> Victor Neal and Dr John Apley were particularly helpful and welcoming.Most paediatricians from Wessex joined the South West Paediatric Club which held two meetings each year, the winterone in Bristol/Bath and the summer one at a peripheral centre, We hosted the summer meeting <strong>of</strong> the club in 1967. It wasnot until about 1968 that there were enough paediatricians in Wessex to justify the founding <strong>of</strong> our own club.The establishment <strong>of</strong> the Wessex Medical School in 1971 and the appointment <strong>of</strong> Dr Colin Normand as Pr<strong>of</strong>essor <strong>of</strong> ChildHealth at <strong>Southampton</strong> opened a new chapter for paediatrics in the region. Students were to obtain a significant portion <strong>of</strong>their clinical experience at various regional centres and many <strong>of</strong> the consultant paediatricians were given the titles <strong>of</strong>‘Honorary Clinical Tutor’.Various specialised <strong>service</strong>s were developed on a Regional basis though few were particularly orientated towardschildren.Mr John Atwell’s appointment in 1969 marked the beginning <strong>of</strong> a Regional Paediatric Surgical <strong>service</strong>, which was to bewidely developed.The regional Orthopaedic <strong>service</strong> was based on Lord Mayor Trainers <strong>Hospital</strong> at Alton. Although included in both DrOrmiston’s and my own contracts we never succeeded in establishing a footing in that hospital.The Cardio-thoracic <strong>service</strong> was based on the Chest (Western) <strong>Hospital</strong> and cardioiogists held peripheral clinicsthroughout the region <strong>of</strong>ten in conjunction with local paediatricians.Children for Plastic Surgery and those with severe burns were treated at the Regional Unit at Odstock. Other children withunusual or difficult problems continued to be referred to London and other centres.I am very grateful to my colleagues Dr Mary Capes and Dr Leslie Bartlet for providing the following accounts <strong>of</strong> thedevelopment <strong>of</strong> the Child Psychiatric Services in our area,
“The Development <strong>of</strong> the Child Psychiatry and Child Guidance Service inHampshire” by Dr Mary Capes.Introduction.These recollections stretch back over a period <strong>of</strong> more than 50 <strong>years</strong> and are inevitably a bit hazy but an attempt hasbeen made to describe the start <strong>of</strong> the Child Psychiatric and Child Guidance Services in the Region, how they developedas a result <strong>of</strong> war-time demands, and how this led to the establishment <strong>of</strong> a comprehensive <strong>service</strong> with particularreference to the set up which evolved in the <strong>Southampton</strong> Children’s <strong>Hospital</strong>.General Background.Training in Child Psychiatry with it’s special emphasis on team work with educational psychologists and psychiatric socialworkers first became possible in the twenties at the London Child Guidance Training Centre funded in the beginninglargely by the Commonwealth Centre <strong>of</strong> the U.S.A. Paediatricians, until the mid-forties, had to receive their training in theU.S.A. so the American influence at the time was strong in both newly fledged disciplines. Child psychiatry at first (ratherlike the young cuckoo in it’s varied nests) could be established as part <strong>of</strong> a Mental Treatment Dept as it was inPortsmouth in 1937, or in clinics, generally known as Child Guidance Clinics (on the American pattern), which werebeginning to be set up by Local Authorities, as in <strong>Southampton</strong>, which also was first established in 1937. There were noother such facilities in the Wessex Region and with the outbreak <strong>of</strong> hostilities in 1939 even the <strong>Southampton</strong> clinic wasclosed and Dr Sybil Yates, who ran it, took an appointment elsewhere.However with the outbreak <strong>of</strong> World War II and the expectation <strong>of</strong> heavy bombing, children were evacuatedfrom the cities to the countryside in large numbers coming to Hampshire from Portsmouth and <strong>Southampton</strong> as well asfrom London and, as billetting <strong>of</strong>ficers became increasingly aware <strong>of</strong> the numbers <strong>of</strong> children who failed to settle happilyin their foster homes and were disturbed by the experience, they demanded help from the Hampshire County MedicalOfficer. He contacted the Mental Health Emergency Committee (based in Reading) and they advised the appointment <strong>of</strong>a psychiatric social worker and Miss Marion Opie took on the job. She visited the hostels, mostly in sizeable privatehouses which had been commandeered, and which housed children who were difficult to billet in foster homes, and itsoon became evident to her that the help <strong>of</strong> a child psychiatrist and an educational psychologist was also needed. I wasapproached, and it made sense to transfer my work from Portsmouth to Hampshire, which I did in 1942 in company withMiss Wills, an educational psychologist. The gap left in Portsmouth was filled during the war <strong>years</strong> by Dr Mildred Creak <strong>of</strong>Great Ormond Street <strong>Hospital</strong>, who worked there part-time. She also succeeded in setting up a small in-patient unit at StJames Mental <strong>Hospital</strong>Over in Hampshire we were <strong>of</strong>fered two attic rooms in the Castle, Winchester as our H.Q. and we proceeded to build up 9centres for diagnostic and treatment purposes scattered throughout the County - these were, apart from Winchester(where two Portsmouth Grammar schools were billeted), at Romsey, Basingstoke, Kingsclere, Highclere Castle (with thetoddler evacuees without mothers!), Totton, Lyndhurst, Petersfield and Clanfield. These centres, which were attendedabout once a fortnight, were either based on hostels or were at ordinary school clinics.Over the <strong>years</strong> from 1942-46 the evacuee population steadily decreased but G.P,s, teachers and social workers hadbecome familiar with the <strong>service</strong> and were beginning to refer local children. By the end <strong>of</strong> World War II the clinics hadreally become permanent fixtures, organised by the L.A. The war-time conditions had given a great impetus to ChildPsychiatric and C.G. work, speedy decisions and flexibility were called for too and the experience gained <strong>of</strong> disturbedchildren being admitted to short-term residential centres proved invaluable. In the past, in the more extreme cases, theonly placement for such children had been in the adult wards <strong>of</strong> Mental <strong>Hospital</strong>s, which was clearly undesirable, but noalternative presented itself.By 1948 the <strong>Southampton</strong> authority decided to open their C,G. clinic again and invited me to run it - which invitation Iaccepted in the hope that commitments would be less in a Borough than in a County. Just after this, still in 1948, andmuch more important, the National Health Service was established, and doctors came under contracts to RegionalBoards, with their futures more secure. In our region we were supervised by the South West Metropolitan <strong>Hospital</strong> Board,with the late Sir John Revans as our dynamic and supportive Senior Administrative Medical Officer. The late Pr<strong>of</strong> Sir AlanMoncrieff, taking advantage <strong>of</strong> new N.H.S. possibilities wrote to all the children’s hospitals and paediatric units in the U.K.at that time advising the appointment <strong>of</strong> a Child Psychiatrist to the staff wherever possible, <strong>Southampton</strong> Children’s<strong>Hospital</strong> was sympathetic to this proposal: the post was advertised on a part-time basis and I was appointed late in 1948,with continuing responsibility for the L.A. clinic as well.The Childrens <strong>Hospital</strong>.
This appointment although it was good to be back in the medical field, involved me once more in an entirely new method<strong>of</strong> working: I was as it were out on a limb, the premises being much too limited to house a team. If the children I wasasked to see lived in the Borough, it was possible to refer them on for full investigation and, if necessary, prolongedtreatment at the Health Centre, but for children from the County a flexible and modified type <strong>of</strong> treatment was <strong>of</strong>tennecessary. There was also considerable difficulty in the use <strong>of</strong> beds; if one wanted to admit a patient whenever beds werein short supply my patients understandably, had to make way for emergencies however disruptive it might be to them.This ceased to be a problem when in 1952, Dr Christopher Haffner was appointed to Portsmouth to plan and operate aspecial unit with in-patient and out- patient facilities for disturbed children and their parents. These points apart, much thatwas interesting and experimental was tried out at the hospital, largely initiated as a result <strong>of</strong> the co-operative attitude <strong>of</strong>the paediatricians. A joint round took place regularly at Bursledon when I accompanied Dr Williamson, and also a monthlypsychosomatic clinic was held by both <strong>of</strong> us and, largely owing to the fact that the two out—patient consulting rooms hadan intercommunicating door, a child could be given an (almost) immediate psychiatric interview at the paediatrician’srequest, or be seen by both consultants togethe, thus saving a second journey for long-distance travellers.Possibly most interesting <strong>of</strong> all the combined activities was the presentation <strong>of</strong> cases from time to time at the monthlyclinical meetings when G.P.s, young doctors and nurses attending could be given some further insight into psychologicalproblems and their treatabilityTeenagers were not seen at the Children’s <strong>Hospital</strong> beyond the age <strong>of</strong> 16, and there were fewer referrals in this agegroup but they were <strong>of</strong>ten considerably disturbed. When in-patient treatment seemed advisable they were admitted toLeigh House in Chandlers Ford. This was a special unit for adolescents which the Regional Board had set up when thebuilding became available (it was previously used for treating women with TB.). Dr W. Allchin and Dr Rosenberg wereappointed in 1961 to run the unit which was conveniently near to <strong>Southampton</strong> and Winchester.It became noticeable as the <strong>years</strong> passed that more girls than boys were referred to the Children’s <strong>Hospital</strong>, mainlysuffering from psychosomatic disorders such as feeding problems, asthma and anxiety states whereas more boys, manypresenting with behaviour disorders, were referred to the L.A. Child Guidance Centre, a number coming from the JuvenileCourt, thereby indicating a need for both types <strong>of</strong> facility since behaviour problems would be largely inappropriate seen ina hospital settingVisitingThe whole question <strong>of</strong> children being visited by their families and <strong>of</strong> infants and toddlers being accompanied into hospitalby their mothers was coming under public discussion at the time <strong>of</strong> my appointment. The late Sir James Spence hadreported in 1946 on his Babies <strong>Hospital</strong> where he had had twenty <strong>years</strong> experience <strong>of</strong> admitting mothers as well, and Drand Mrs Pickerill in New Zealand reported very favourably on their plastic surgery unit where they had admitted mothersto counter cross infection. They had found this beneficial in a number <strong>of</strong> ways. These reports coupled with the research <strong>of</strong>Dr John Bowlby on separation anxiety and the late James Robertson into the emotional after effects <strong>of</strong> hospitaladmission, which were in their initial stages, seemed to make a lot <strong>of</strong> sense. I raised both the issue <strong>of</strong> visiting and <strong>of</strong>mother’s being admitted fairly soon after being appointed, appreciating that there would be great difficulty in achieving thelatter owing to the very limited space in the hospital, but the former was discussed at a number <strong>of</strong> medical committeemeetings. Dr Ormiston, who was the first paediatrician to be appointed to the staff in 1947, had come fresh from theU.S.A. and was seriously worried about the degree <strong>of</strong> infection and the high mortality rate in the wards and wasunderstandably apprehensive about any infection being introduced from the outside world. It was finally decided by MrRichardson, the Children’s Surgeon, who was Chairman <strong>of</strong> the committee, that a vote should be taken, which resulted inan equal number <strong>of</strong> votes for and against, leaving him to cast his vote – in favour. At first the visiting was somewhatrestricted but as the worst fears failed to be realised the rules became increasingly relaxed. Some doctors found thevirtual pandemonium after the subdued atmosphere in the wards difficult to take but not the children! I must say thatthough these discussions involved strongly held opinions, the final outcome was accepted without the least acrimony.Several <strong>years</strong> later in 1959, two rooms were set aside so that some mothers, eventually, were able to come into thehospital with their children.It might be <strong>of</strong> interest in this context to make a brief reference to a W.H.O.study group. Dr Begg the medical director <strong>of</strong> theEuropean Office asked me, in 1951, to organise a small conference or study group on the care <strong>of</strong> children in hospitalwhich was to include the respective roles <strong>of</strong> paediatricians and child psychiatrists, the coordination <strong>of</strong> their work and theinter-relation <strong>of</strong> somatic and psychological processes in sick children. The meeting took place in Stockholm where it washosted by Pr<strong>of</strong> Wallgren <strong>of</strong> the Children’s Clinic at the Karolinska <strong>Hospital</strong>, with Sir Alan Moncrieff chairing the clinicalproceedings. The Paediatricians and Child Psychiatrists who presented these had had experience in close cooperationtogether and included Dr R. Bonham-Carter and Dr Soddy from UCH. London, Pr<strong>of</strong> Milton Senn and Dr Solnit from theU.S.A. and two pairs <strong>of</strong> Swedish doctors,and the delegates were largely drawn from Scandinavian Countries. It was alively and useful meeting and in 1955 a report entitled “The Child in <strong>Hospital</strong>” was published by WHO, and was widelydistributed.As a final thought I look back with pleasure at the memory <strong>of</strong> the murals in the anaesthetic room at the Children’s <strong>Hospital</strong>which were painted by Miss M. Wilson, a Winchester artist. These made a rather bare and forbidding room into anattractive one and the children enjoyed counting the colourful balloons as they gradually lost consciousness,
Conclusion.I said in the beginning that these recollections would inevitably be somewhat hazy, but one looks back on those <strong>years</strong>spent at the Children’s <strong>Hospital</strong> (however ramshackle it might have appeared to the architectural eye, and howeverlimited it’s scope), a time <strong>of</strong> excellent rapport between members <strong>of</strong> staff, and with it a sense <strong>of</strong> achievement. In the childpsychiatric field a lot was owed to the foresight and dynamism <strong>of</strong> Sir John Revans whom one found easily accessible andopen to suggestions, ready to try to plan anything that led to the greater well-being <strong>of</strong> patients, Did he appreciate howeverthat “Small could be beautiful” in the sense that some <strong>of</strong> the close liaison between members <strong>of</strong> the staff would be lost in alarger hospital?CHILD PSYCHIATRY AND THE CHILDREN'S HOSPITAL 1965-1975 by Dr LeslieBartletDr Mary Copes retired in 1965 and her place was taken by Dr Leslie Bartlet. He was joined by Dr Brian Crossley in 1969,Both held parallel child guidance appointments and as a consequence there were few “boundary” problems betweenhospital and community. This resulted in fully integrated <strong>service</strong>s whichon the national scene, were quite rare then, butstandard now,As referrals increased, the need to provide treatment as well as diagnostic <strong>service</strong>s built up. When temporary out—patientaccommodation was erected at the back <strong>of</strong> the main hospital more rooms and space was allotted to the child psychiatristsSlowly the elements <strong>of</strong> a child psychiatric team came together. A psychiatric social worker from <strong>Southampton</strong> ChildGuidance clinic was seconded on a sessional basis to help, but the arrangement did not work very well and Miss JeanneChristie was appointed as Paediatric Social Worker in 1969. She agreed to work with the child psychiatrists as well as thepaediatricians and surgeons. A first rate system <strong>of</strong> teamwork developed. The team was further strengthened whets a parttimeclinical psychologist. Mr Christopher Johnson was appointed. Besides working in the team, Mr Johnson developedan assessment, advisory, and treatment <strong>service</strong> <strong>of</strong> his own and he quietly established links with the Local EducationAuthority and the local educational psychologists (a task which, at one stage, was by no means easy). Finally, in 1970, anoccupational therapist was appointed, thus rounding <strong>of</strong>f the team.The late sixties were marked by a growing interest in the needs <strong>of</strong> children with chronic illness and handicap. When DrWilliamson set up a multi-disciplinary assessment <strong>service</strong> psychiatric staff played a part in this from the start. The <strong>service</strong>turned out to be a gateway to new areas <strong>of</strong> work; in particular mental handicap and the emotional disturbances affectingfamilies with handicapped children. The enrichment <strong>of</strong> the staff with psycho-social skills knitted in well with DrWilliamson’s imaginative use <strong>of</strong> the facilities at Bursledon <strong>Hospital</strong> where the need for beds for children with chronicphysical illness was falling <strong>of</strong>f. He and his fellow paediatricians, Dr Tom Hughes-Davies and Dr John Greaves, began to“share” cases with the two child psychiatrists. Bursledon came to play an important role in the unravelling <strong>of</strong> complexproblems that <strong>of</strong>ten presented with psychosomatic symptomatology - Bursledon <strong>Hospital</strong> School under the headship <strong>of</strong>Mrs Brenda Marshall became involved. From that point on it became possible to observe and treat children from medical,social, family, emotional, behavioural and educational standpoints at the same time. Children were customarily admittedfor one to four weeks and parents were encouraged to visit daily. In the early Seventies this system, hinging on short-termadmissions, was unfashionable; indeed faintly heretical. Bowlby’s views held sway and hospitals were seen asemotionally dangerous institutions. Great care was taken to maintain close family contacts during admissions. When preschoolchildren were admitted their mothers usually came in as well. Older children had their parents visiting (or phoningregularly). No emotional damage resulted and the positive consequences were <strong>of</strong>ten significant. Particularly good resultswere obtained with such conditions as enuresis, encopresis, non-specific abdominal pains and headaches, hystericaldysfunctions. sleep disorders and behavioural disorders associated with diabetes, epilepsy and asthma.This way <strong>of</strong> working made great demands on nursing staff. Considerable reorientation was required. Nurses wereexpected to retain their traditional paediatric skills and at the same time become much more flexible, dynamically awareand emotionally involved. In the course <strong>of</strong> time “Bursledon” became an important element in the child health resources <strong>of</strong>the district. Although Bursledon <strong>Hospital</strong> was closed in 1966, the working practices developed there live on. BursiedonHouse on the General <strong>Hospital</strong> site is it’s worthy and valued successor.MEMORIESMention <strong>of</strong> the old Children’s <strong>Hospital</strong> to those with past connections with the place, whether they were patients, parentsor members <strong>of</strong> staff, always brings back old memories, mostly happy ones. These help to add flesh to the bare bones <strong>of</strong> amore factual historical record. Space permits only a fraction <strong>of</strong> these being recorded here.Ts & As in 1913.Mrs Brenda Drew recalls:- “It must have been in late 1912 or early 1913 that my sister (4 <strong>years</strong> my senior) and I had ourtonsils and, I think, adenoids removed. We had been well prepared; we would not feel anything, in fact our next-door
neighbour had had an in-growing toenail removed. She had gone to sleep and had a wonderful dream. This caused mytrouble ..... A jolly ‘Auntie’ was the moral support <strong>of</strong> all the children concerned. I remember waiting in the room next towhat must have been the operating theatre. We were all in our white petticoats and wore rubber bathing-hats but I cannotremember whether they were put on in the operating theatre or before. The first little girl to go in started to cry, but as‘Auntie’ assured us that they were only washing her face and a lot <strong>of</strong> little girls didn’t like having their faces washed, we allfelt very superior - we weren’t babies, I so well remember nurses going into that room carrying what to me looked likevegetable dishes full <strong>of</strong> boiling water and warning us to keep out <strong>of</strong> the way and telling our parents that it was not aserious operation but a very dirty one - I now imagine these must have contained the sterilised instruments for eachpatient. When my turn came I went in happily and as I was “going to sleep and dream”, I curled up on the operating table... I was straightened out on my back and had an evil smelling thing put in my mouth! I realise now that the thing was tohold my mouth open and the unpleasant smell was gas or whatever it was called. The next I knew was waking up on thefloor <strong>of</strong> whatever room it was where we were collected to go home. This was the moment <strong>of</strong> heart breakingdisappointment, It was all over and I didn’t dream! .... We were eventually lifted in to a horse and cab and home to bed.”Appendicectomy in 1926Mrs Dlive Jackson remembers:- .... “At the age <strong>of</strong> 8 yrs I had my appendix removed. I was rushed in at about 10.30 p.m.,and by midnight had been successfully operated on. The operation was performed by Mr Nightingale assisted by my ownfamily doctor, Dr Powell. I can remember that while convalescent we children had to roll bandages; whether it was reallyneeded or just to keep us out <strong>of</strong> mischief I do not know. I also remember getting a severe telling <strong>of</strong>f for complaining thatmy egg was hard boiled .... parents used to bring in eggs so that we could have nice new laid ones.”Another tonsillectomy in 1936Mrs Pellow recalls:- .... “I was taken up with half a dozen or so other children to a very pleasant ward ... the studentnurses who were very young and very pleasant came and practiced bandaging on us. Next morning we were all given arubber bathing-hat and a nightdress to put on. Wrapped in blankets we were led along to the lift and thence to a small sort<strong>of</strong> waiting room. I was the first to go in ... and had to lie down on the table and all around the room in glass cases were themost fearsome looking instruments . I was utterly terrified. Eventually some nurses and doctors came in and a sort <strong>of</strong>mask was put over my face ... I remember waking up with a very sore throat and being very sick ... next day we were alltaken down to out-patients where our parents were waiting to take us home.”During the ‘Blitz’Little Jean Mudge was 5 <strong>years</strong> old in 1940 ... “I was seriously ill with peritonitis and too ill to be moved when there was anair raid. Mum stayed all day and <strong>of</strong>ten had to stay the nights during air raids. She had a mattress to throw over the cotsides to protect me from flying glass.”An unhappy motherMrs Sheriton “... had the boy circumcised when he was five months (1947). They just took him from me and told usmothers to come back in a few hours time. I had nowhere to go... all I could do was to pace up and down the drivewayand hear the babies screaming. In 1955 “our son aged 8 was rushed in with a burst appendix. I was told he was gravelyill, but to go home and get some sleep - no waiting rooms for parents there or sitting by their bedside. Back we camehome an hour’s bus ride, no cars or telephones those days. The anguish <strong>of</strong> waiting for the police to bring bad news ... forthree days he did not know us but he then started trying to pull down all gadgets connected to him. He got very attachedto a sweet nurse, she always sat on his bed reading to him ... he was home after 5 weeks”A mother’s memories <strong>of</strong> Ward I in 1956Mrs Day rushed her 2-year-old daughter to Casualty unconscious with convulsions. She was then admitted. “I wasagreeably surprised when I was asked whether I’d like to stay with her during the day... Judy was in hospital on MotheringSunday and the nursing staff left smell bunches <strong>of</strong> Spring flowers on each child’s locker as a gift from the little ones totheir mothers; this lovely action has remained in my mind ever since.” ... Another sign <strong>of</strong> good hygiene was the washingdown <strong>of</strong> glass partitions. ‘‘I watched two nurses wash these partitions with disinfectant from ceiling to floor (and they werehigh rooms) with long handled brooms.”The first mother to use the Parents Room.Mrs Lowth recalls:— “I spent Christmas 1959 in the hospital with my eldest child aged 6 who had become severelydehydrated with pernicious vomiting ... Charles was so poorly that he was in a small side ward under charge <strong>of</strong> thatmarvellous nurse Sister Boyce. Charles, as did all children, adored her. It was felt advisable ... that I should stay in thehospital and I was actually the first parent to stay in the new Parents Room up in the attic. It was hardly finished and verysparsely furnished then. My husband would come to the hospital and sit with Charles for a few hours to allow me to gethome to organise Christmas with the other children ... Charles rallied and thanks to the wonderful nursing he pulledthrough ... on Christmas Eve ... the nurses invited me to sing carols with them under the illuminated Christmas tree which
stood outside the front <strong>of</strong> the hospital. I was then very pregnant so one <strong>of</strong> the nurses lent me her cloakBursledon in 1956Sandra Walker aged 11 was in Bursledon with rheumatic fever for 4 months. “We used to go for walks, 10 minutes at first,but increasing by 10 minutes at intervals. We were taken down by the river, through the fields, which was a greatexperience. If we felt we had run about too much, we used to rush to put our wrists under a cold tap in the hope <strong>of</strong>bringing our pulse rate down before the nurse could check it. We kept silkworms, which fed on the leaves <strong>of</strong> the mulberrytree by the entrance. We used to wind the fine silk from the cocoons. Sometimes, at night, my bed would be wheeled intothe hall because I kept the other children awake by talking too much. I still do!” Sandra’s elder sister, Pat, was also apatient in Bursledon in 1949 she remembers being warned that if you went upstairs you would encounter the big blackwasherwomen who would grab you and take you away.<strong>Hospital</strong> GhostsMost hospitals have their ghosts and <strong>Southampton</strong> Children’s was no exception. Several nurses recall hearing footstepson the stairs outside Ward II while on night duty but Mary who was a S.E.N.. at the time had a more frighteningexperience. “I was busy with babies feeds at 3 am, on the Gastro-enteritis ward. All was very still in the cubicle; the streetlight was as bright as ever, when a very eerie atmosphere developed. I felt intensely aware <strong>of</strong> something very frighteningand sinister behind me. The window there overlooked the old Vicarage lawn but I dared not turn in that direction for fear <strong>of</strong>what I might see. When I asked the sister on Surgical (Sister Hodges), when taking up the night report, if she was aware<strong>of</strong> this happening, I was a bit surprised to be told never to look over the next garden if this atmosphere occurred again asthere had been some terrible happening in the past. I think she said that someone had been murdered and some horribleapparition had been seen there since.”Casualty staff to the rescue.A memorable event occurred in 1957 when one afternoon an emergency call was received that a man working on the firstfloor <strong>of</strong> a new building up the road had been seriously injured when a reinforced concrete girder snapped and two <strong>of</strong> thesteel rods had transfixed him through his abdomen. Sister Jenny Tutcher and Dr Bridget Jepson immediately rushed toassist. They had to make a very precarious climb across the framework <strong>of</strong> girders to give first aid, The man made acomplete recovery.Nurse Coady and Sister Tutor’s Cat.Miss Morgan remembers when her tortoiseshell cat ‘Bunty’ disappeared one evening and was located high up in a treenear the nurses’ home. Flo Coady, dressed to go home, climbed a ladder with a plate <strong>of</strong> fish, which she held up at arm’slength. In grabbing the cat she dropped the plate <strong>of</strong> fish. Later when travelling home in the bus she was aware that otherpassengers were commenting on her but it was not until she had reached home that she found a large slice <strong>of</strong> fish stillsitting on her shoulder!The Newly-wed Houseman.When we appointed Dr James Scobie as R. M.O. we had no idea that he was about to get married ... “I shall never forgetthe day I arrived at the Children’s <strong>Hospital</strong>. It was January 1st 1962, the day after my wedding and it was snowing.Bursledon seemed a very gloomy place. My wife went back to her work in London the following day, and I started workingwith chronically ill children.The Children’s <strong>Hospital</strong> itself was very busy, especially in winter time. There were two consultant paediatricians. DrGeorge Ormiston was a Scot with a fund <strong>of</strong> amusing stories and a reputation for severity. Dr David Williamson was moreprogressive. His life seemed very varied; one moment visiting gipsy children under a tarpaulin in the forest, the nextattending the <strong>of</strong>fspring <strong>of</strong> grand lords in great hooses interspersed with visits to hospitals in Winchester and Alton.There was a very competent registrar, Dr Eric Jones, and a succession <strong>of</strong> house physicians The junior doctors shared arota involving working at Bursledon, the Children’s <strong>Hospital</strong> and the infectious fever unit at the Chest <strong>Hospital</strong>.My wife used to come down on alternate week-ends when I was on duty, and we were always getting into trouble with thehospital authorities; hanging washing out to dry (forbidden), and complaining about the guest supplement, which includeda fee for having someone else in the one narrow bed, although not even a second towel was provided.At the beginning <strong>of</strong> March we hired, through the almoner, a caravan which we kept, with a licence from the Verderers, inan open meadow on the upper reaches <strong>of</strong> the river Beaulieu, south <strong>of</strong> Ashurst. It was isolated with only occasionalwalkers passing by, though ponies would wake us up at night, scratching themselves on the corners <strong>of</strong> the caravan.Meanwhile I was learning a lot about sick children. There had been some cases <strong>of</strong> smallpox brought by visiting seamen,so there was a big vaccination campaign. Two children with eczema developed the generalised form <strong>of</strong> vaccinia from thevaccination and both died. The only other deaths during the seven months that I worked at the Children’s <strong>Hospital</strong> werefrom leukaemia, effective treatment for which was just beginning.
The house physicians assisted the visiting surgeons, Mr Richardson and Mr Rowntree operating on appendicitis, pyloricstenosis and hernias and that made a break from the routine <strong>of</strong> ward rounds and clinics and was a useful preparation formy next job as a medical <strong>of</strong>ficer in Uganda.”The Head Teacher remembers the Bursledon <strong>Hospital</strong> School.“The 1944 Education Act for the first time mentioned ALL children, which meant that the generous voluntary work <strong>of</strong>educating sick children became the responsibility <strong>of</strong> the local education authorities.Hampshire Education Authority responded to a request from the <strong>Hospital</strong> Management Committee and provided a schoolat the newly opened Bursledon Annexe Initially there was a headteacher and one other full time teacher with some parttimehelp for the nursery age children. In 1962 the staff increased to three full time teachers.There were three wardsdownstairs, which, with the moving <strong>of</strong> a few beds, could be organised into secondary, junior and infant classes. The staffroom and storeroom were on the very top floor and most <strong>of</strong> the necessary equipment was carried up and down daily. Theschool hours were from 10 a.m. to noon and 2 pm. till 3 p.m. This gave the nurses time for treatments and the children amidday rest period. The early finish was for the benefit <strong>of</strong> visitors who were encouraged to come out <strong>of</strong> school hours. Thehead teacher was given a daily ‘schoolbook’ which was a useful record <strong>of</strong> the state health <strong>of</strong> the children. There seemedto be little intteraction between nursing and school staff.There were three head teachers during the first fifteen <strong>years</strong>: I was the fourth being appointed in 1967 and staying until1989 and it was during tny time that major changes took place. A new position was created by the Hampshire EducationAuthority, and Mrs P. Clifford was appointed Administrator for Special Education and, at the same time, Mr Freddie Greenfirst Advisor for Special Education. These two people were a formidable and much respected team. They gave mesupport and encouragement for my philosophy and future plans for the school. (Staff were able to attend in- <strong>service</strong>training, including, for some, a year <strong>of</strong> advanced academic study at <strong>Southampton</strong> <strong>University</strong>.)One <strong>of</strong> the early changes brought about by the new administrator was the creation <strong>of</strong> a Governing Body for the school asapparently there had been no legally constituted team for the head teacher to approach with new ideas. Within the early<strong>years</strong>, Mr A Moody <strong>of</strong> the local firm <strong>of</strong> yacht builders was elected chairman, and he supported and guided the school fortwenty <strong>years</strong>.However the most important change was the advancement <strong>of</strong> medical science which altered thinking with regard tohospital care for sick children. These changes showed in many ways. Most children at Bursledon were ambulant andwore their own clothes The beautiful grounds were used both in school and free time. By the mid 1970s the school hourswere those <strong>of</strong> a normal school and the children were taught in a separate school building provided by the educationauthority. A new department <strong>of</strong> the school was later opened in the Paediatric wards at the General <strong>Hospital</strong>.At Bursledon more and more children with emotional problems were admitted. The variety <strong>of</strong> people working with thesechildren altered the style <strong>of</strong> teaching and nursing. Psychiatrists, psychologists and social workers emphasised the need todiscuss each child carefully before action was taken. Teaching staff were drawn more and more into the working life <strong>of</strong>the hospital. The appointment <strong>of</strong> Dr Jean Davis as clinical assistant responsible for Bursledon was a great asset. Sheheld weekly meetings with the Sister in Charge and the head teacher plus anyone else with a pr<strong>of</strong>essional interest in thechildren, This meeting was vital. The increase in inter-disciplinary meetings and the need to produce written reportsmeant the school needed proper secretarial help. The head teacher was also given extra teaching staff so that liaisontime was possible without depriving the children. The school was able to take more pr<strong>of</strong>essional visitors on a regularbasis. These were the good <strong>years</strong>.The last chapter <strong>of</strong> the school at Bursledon was being written. The numbers <strong>of</strong> children coming there fell belowacceptable levels. There were staff cuts and those who were left were dispirited. Even so, those remaining put on a livelyparty to mark the closure in February 1989.Over the <strong>years</strong> Bursledon had provided a truly loving atmosphere to promote recovery. The school had played it’s part incaring and restoring the children’s confidence, preparing them for their return home. They were matured and helped byexperiences which no other place could have given them,There are so many people who remember their time there; patients and staff alike. There are stories <strong>of</strong> dens in thebamboo clump or under the mulberry tree. Do you remember the numbers <strong>of</strong> children who got stuck up trees? Whosneaked into the girls ward one night and decorated them intimately with toothpaste? Who climbed the front <strong>of</strong> thebuilding and alarmed the teachers quietly marking books in the turret room? In the spring there were the inevitable rows<strong>of</strong> graves <strong>of</strong> buried fledglings with suitable floral tributes. How many town children were delighted to see their firstgoldfinch or the old fox lying in the sun. So many <strong>of</strong> them were amazed to play free on the grass; <strong>of</strong>ten families wouldpicnic on the lawn and one Dutch family actually camped in the grounds while their child recovered from meningitis. It hasbeen said by the more articulate that despite the illness and pain, being in Bursledon was a magical time.
THE LAST LAPIn 1962 Regional plans for the future development <strong>of</strong> the hospitals in <strong>Southampton</strong> were published showing the Board’sintention <strong>of</strong> developing the Royal South Hants and the General hospitals with the eventual absorption <strong>of</strong> the smallerhospitals, including the Children’s.I was invited to join a small working party at the Regional Beard’s <strong>of</strong>fice in Winchester to consider plans for a standardWessex district hospital. At our first meeting it immediately became very clear that the plans were primarily those for anew hospital on the General <strong>Hospital</strong> site and that the Children’s Unit was to be on the top floor <strong>of</strong> the main block. We hadto accept that the Children’s <strong>Hospital</strong> was very out-<strong>of</strong>-date and that it was unrealistic for us to hope that it could bemodernised sufficiently to keep up with current technological advances. We pleaded in vain that the children’s unit shouldbe in a separate building on the site but the plans were already so far advanced that we were only able to make minoralterations.When it became apparent that we would shortly be leaving Winchester Rd, an elaborate plan was put forward by themedical staff to convert the buildings, including Oakfield, into a comprehensive centre for the assessment and care <strong>of</strong>children with handicap. The plan included the transfer <strong>of</strong> the facilities being provided at Bursledon, which would then beclosed. The authorities turned down the plan on the grounds that the boiler would not be up to the job! (It packed up threeweeks before the final move!). It is satisfactory to know that just such a unit has now (1989) been established in the oldGroup Offices on the General <strong>Hospital</strong> site.Long before the final day a commissioning team was set up under Miss Irwin to ensure that the move should be aspainless as possible and, in the event, their hard labours were well rewarded. We had a farewell party for Miss Craddockon May 16th and the actual move took place on May 20th 1974 without a hitch thus bringing to an end <strong>ninety</strong> <strong>years</strong> <strong>of</strong><strong>service</strong> to the children <strong>of</strong> <strong>Southampton</strong> during which time the tiny village hospital had grown up to become an importantcentre <strong>of</strong> paediatric expertise, research, and teaching.The new buildings at the General <strong>Hospital</strong> were formally opened on December 6th 1974 by H.M. the Queen, whosubsequently toured the Children’s Unit on Level G <strong>of</strong> the East Ward Block. Although there can be no doubt that the newunit is much more capacious and has many more facilities, those <strong>of</strong> us who were privileged to serve there, will cast anoccasional nostalgic glance backwards to the old hospital which was such a friendly, happy and caring place.THE SMALL IS BEAUTIFULPostcript: The old hospital building was demolished in the early 1980s and Brixedone House, Bursledon sold in 1989.
APPENDIX 1Medical StaffDr W. Maclean C.B. M.D. Consulting Physician 1884 - 1897Sir T. Longmore C.B. F.R.C.S. Consulting Surgeon. 1884 - 1895Dr C. G. Beaumont Hon. Medical Officer 1884 - 1892Dr E. T. Chamberlain L.R.C.P. “ “ “ 1884 -1893Mr J, McLachlan Dental Surgeon 1884 - 1910Dr J. S. Robertson M.R.C.S. Hon. Medical Officer 1887 - 1890Dr W. G. Collins Hon. “ “ 1892 - 1897DR R. O. H. Gwillim L.R.C.P, Hon. “ “ 1894 -1899Consulting Surgeon 1903 - d.1926Dr Howard Saunders MB. Hon. Medical Officer 1895 - 1929Consulting Physician 1929 - d.1961Dr W. F. Cooper L.R.C.P. Hon. Medical Officer 1898 - 1920Hon. Consulting Physician 1920 - d 1927Dr Walter Purvis M.D. Hon. Medical Officer 1900 -F.R,C.S. Hon. Surgeon 1907 -1923Dr Gillespie. Hon. Medical Officer 1904 - 1938Hon. Consulting Physician 1938 - d 1944Mr Guy Robertson Hon. Dental Surgeon 1910 -1913Mr C. De Foubert “ “ “ 1913 - 1915Mr E. A. Wolter “ “ “ 1915 -Dr R. J. Vernon Hon. Medical Officer 1914 - 1946Hon. Consulting Physician 1946 -Mr H. C. Balls Hon. Dental Surgeon 1917-1939Dr W. Stewart M.B. Hon. Aural Surgeon 1918 - 1925Consulting Aural Surgeon 1925 -Dr Brogden Hon. Anaesthetist 1920 - 1934Dr B.Castles Powell Hon. Medical Officer 1919 - 1940Dr Simpson Hon. Anmesthetist 1921 - 1922Dr L.W.Howlett Hon. Anaesthetist 1922 -1930Dr A,D.Maxwell “ “ 1922 - 1927Mr H. C, G. Nelson M.D. Hon. Surgeon. 1923 -1932Dr Seager Thomas Hon. Pathologist 1923 -d 1933Dr H.Castle “ Medical Officer 1924 - 1941 d.1943Mr Norman McKeith Hon .Aural Surgeon 1925 - 1947Dr Seager Thomas Hon. Pathologist. 1925 - d.1934Mrs Ursula De Foubert Hon. Medical Officer 1926 - 1932Dr G. R, Marshallsay Hon. Medical Officer 1927 - 1947Dr Norman Aldridge Hon. Electro-therapeutic Physician 1927 - 1929Dr D. Vincent Rice “ “ “ “ 1929 - 1950Mr L. A. R. Richardson Hon. Surgeon 1929 - 1967Mr H. J. May Hon. Ophthalmic surgeon 1929 - 193?Dr H.J.Bower Hon. Physician 1929 - 1950Dr H. Oakley White “ Anaesthetist 1932 - 1939“ Physician 1939 - 1950Dr G. C. Havers “ “ 1933 -Mr Raymond Purvis Hon. Surgeon 1934 - 1938Mr A. B. M<strong>of</strong>fat Hon. Ophthalmic surgeon 1937 -Dr A.T. Russell Hon. Anaesthetist 1937 - 1948S. W. Lytle F.R.C.S Hon. Surgeon 1938 - 1950Mr A.Russell Assistant Aural Surgeon 1933 - 1961Dr H. H. Gleave M.R.C.P. Hon. Pathologist 1934 - d. 1952Dr J. Cann ‘ Hon. Anaesthetist 1938 -Mr S. W. Lytle F.R.C.S. Hon. Surgeon 1938 -1950Dr N. E. Slaney Hon. Physician 1939 -1950Mr G. V. Dymott Hon. Dental Surgeon 1939 -Mr W. R. Morgan “ “ “ 1939 -1940Mr J. J. Sanders “ “ “ 1940 -Mr E. Bacon Hon. Ophthlmic Surgeon 1940 -Mr H. H. Langston F.R.C.S. Hon. Orthopedic Surgeon 1943 -Mr B. Sugden Aural Surgeon 1947 -Dr R. B. Boal Hon. Assistant Radiologist 1947 -Dr Mary Capes Hon. Psychiatrist 1948 - 1965Dr George Ormiston Paediatrician 1948 - 1963Mr B. Sugden Hon. Assistant Aural Surgn 1947 -Dr J. Preston Director <strong>of</strong> Phys, Med. 1948 - 197Dr W. L. M. Bigby Hon. Anaesthetist 1948 -Dr C. J. Ball Anaesthetist - 1963Dr A. J. Grimston Cons. Dermatologist 1949? -Dr D. A. J. Wiliamson Cons. Paediatrician 1950 - 1977Dr S. C. Dobson Cons. Pathologist 1951? -Dr R. D. Caton Cons. Radiologist 1952 -
Dr R. House Cons. Anaesthetist 1952 -Mr T. Rowntree Cons. Surgeon 1951 -Dr R. P. W. Shackleton Cons. Anaesthetist 1956 -Dr Joan Guy Cons. Pathologist 1957 -Dr I. W. Caldwell Cons. Dermatologist 1962 -Dr L. B. Bartlet Cons. Psychiatrist 1965 -Dr John Greaves Cons. Paediatrician 1962 -Dr T. H. Hughes-Davis Cons. Paediatrician 1962 -Dr Elspeth Williamson Clinical Geneticist 1963 -Dr F. Brunton. Cons. Radiologist 1965? -Dr Burrows Cons. Radiologist 1965? -Dr L. Langdon Cons. Anaesthetist 1964 -Dr I. Hyde Cons. Radiologist 1965 -Mr J. D. Glanville Cons. E.N.T.Surgeon 1965 -Mr J. H. H. Webster Cons. Surgeon 1966 -Mr J. D. Atwell Cons. Paediatric Surgeon 1968 -Mr Neil Freeman Cons. Paediatric Surgeon 1969 -Dr I. C. S. Normand Pr<strong>of</strong>essor <strong>of</strong> Child Health 1971 -Dr John Birkbeck Senior Lecturer 1972 -Chairmen <strong>of</strong> Managing Committee.Rev A. D. Burton M.A.Rev T. W. H. Jacob.Mr H. W. HayRev Studholme WilsonCaptain J. HendersonMr Robert AshbyCapt H. B. Elwyn R.N,Mr T. E. Plumer PriceMr Herbert AshbyMr A. Bedford J.P.Chairmen <strong>of</strong> House Committee.Mr A BedfordPr<strong>of</strong> J. E. G. RaymentDr G. H. Johnson.Miss E. I. L. Wright S.R.N.Dr W. AngusVicar <strong>of</strong> Shirley.“ “ “Rector <strong>of</strong> Millbrook1884 - 18891889 - 18921892 - 18951895 - 19081908 - 19101910 - 19161916 - 19271927 - 19341934 - 19381918 - 19481948 - 19541955 - 19581958 - 19591959 - 19601960 - 1974Hon. SecretarysCapt MortonMr George Forbes—BassettCapt.MurtonMr Albert SpoonerMr Ellerton Bailey.Captain Barnar’d H.N.Mr B.Winn FordMiss BurnistonSecretarysMiss Ella K.MattthewsMr Eric Woods1884 -18851885 -18931893 - 18961896 - 18981898 - 18991899 - 19011901 - 19111911 - 1926Hon Treasurers.Commissary-General YoungC.B.Mr F. Davis GaleMr T. Isted.Mr Albert SpoonerMr Milne StewartMr R. A. MathewsMr P. J. HarrisMr C. G. ThomasMr M. H, B. Rumbold1884 - 18891889 - 18951895 - 18981898 - 19131913 - 19241924 - 19291929 - 19301930 - 19381938 - 19481926 - 19511952 - 1974
Lady Superintendent Later Matron.Miss Davidson.Miss MorganMiss HickmanMiss SwainMiss HalifaxMiss TomkinsonMiss L. SellarsMiss D. GolayMiss J. LaycockMiss E. DykeMiss E.M.CreedMiss J,Cradock1884 - 18851885 - 18891889 - 18901890 - 18921892 - 19081908 - 19271927 - 19441944 - 19501951 - 19541954 - 19601960 - 19671967 - 1974Sister TutorMiss Morgan 1944 - 1958Ward Sisters.Ward I Ward II. Out-Patients Gastro-enteris Bursledon Theatre.Puddy Short Hayward Hughes Morgan UpstillLillington Bowen Brown Trowbridge SparkesFlower Gibson Tutcher WilliamsBoyce Hodges Oaks Adams PyattLegge Gale Mrs Tatham CoadyFlynnWareAmesJonesPharmacistsMassage.Electro—therapy.? ? 1899 - Miss Hounsell Hon Masseuse 1919Miss Martin 1906 - 1915 Miss Moborly. Hon Masseuse 1923MissBurniston (Hon Sec.) 1915 - 1918 Miss Shrubsall Masseuse 1927Miss Cooper—Poole 1930 - 1937 Mrs Thomas. 1931 - 1947Miss Clark 1937 - 1940 Mrs C.Giabby 1947 - 1949Miss Gibbs 1940 - 1945 Miss YeldMiss Stevens 1946 - 1954 Miss FordMr Miller 1954 - 1955 Miss MitchellMr Yard 1955 - Mrs Tarrant.Miss Tracey 1959 - 1974Radiographers.Almoner/Social WorkerMrs Thomas 1931 - 1947 Miss Rosamund May 1948 - 1967Miss BeanMrs Donald Miss Jeanne Christie 1967 -Mrs Janet Fllis 1962 - 1964Ann Arscott 1964Mrs Sandy Read 1967Elisabeth Nunn 1969Jenny Bullivant 1971Miss Diana ClaisseStelle BowyerMrs Brenda Danby.Miss Hilary Smith.
Analysis <strong>of</strong> Admissions and Deaths for the Year 1931Summary <strong>of</strong> Medical Cases.Acidosis ...................................................3Asthma ....................................................2Anterior poliomyelitis ................1Bacilluria...................................2Bronchitis.................................................1Bronchitis and Diphtheria .........................1Catarrhal Jaundice...................................3CerebraI Diplegia.....................................1Chorea.....................................................3Constipation.............................................2Convulsions ... .........................................9DebiIity.....................................................2Dermatitis and varicella............................1Diabetes Mellitus......................................1Diphtheria ................................................1Dyspepsia ................................................2Eczema....................................................4Eczema and Abcess ................................1Encephalitis Lethargica............................2Gastro-Enteritis........................................1Gastro-Enteritis and Diphtheria ................1Habit Spasm ............................................1Haematomat{bJI~I. ..................................3Haemorrhage...........................................1Herpes Zoster ..........................................1Hydrocephalus.........................................1Hyperpyrexia............................................2Icterus Neonatorum .................................2Impetigo...................................................1Intestinal Spasm ......................................1Lymphatic Leukaemia ............................. 2Lymphangitic .......................................... 1Marasmus .............................................18Meningism.............................................. 1Meningitis .............................................. 3Meningitis and Hydrocephalus................ 1Nephritis ................................................. 1Neuralgia................................................ 1Ophthalmia Neonatorum......................... 1Orchitis ................................................. 1Pericarditis, Endocarditis, andPneumonia .......................................... 1Pertussis ............................................... 1Pleurisy ................................................. 3Pneumonia ............................................30Pneumonia and Diphtheria ..................... 1Poisoning ............................................... 1Pulmonary Embolus ............................... 1Pyelitis................................................... 1Rheumatism .......................................... 5Rickets ................................................... 1Scurvy .................................................... 1Teething ................................................. 1Tie ......................................................... 1Tuberculosis, AbdomInal ........................ 4Miliarv .............................. 1Pulmonarv...................... 1and Diphtheria ................ 1Typhoid and pneumnonia .......... 1____169Summary <strong>of</strong> Surgical Cases.Abcesses ...............................................17Abcesses and Diphtheria .........................1Accident Cases (excludingfractures) ......................................19Adenitis..................................................14Appendicitis...............................16Ascites .....................................................1Burns .....................................................10Burns and Scarlet Fever ..........................1Cellulitis ...................................................3Cleft Palate ..............................................2Cleft Palate and Hare Lip ...........1Congenital Dislocation <strong>of</strong> theHip (4 cases accounting foradmissions)...................................16Concussion ..............................................2Empyema.................................................3Empyema and Varicella ...........................1Epiphvsitis ................................1Ethmoiditis ...............................................2Ethmoiditis and Scarlet Fever ..................1Foreign Bodies (Swallowed).....................3Foreign Bodies (other) .............................2Fractured Skull.........................................3Fracture and Diphtheria ...........................1Other Fractures......................................14Ganglion ..................................................1Hernia .. - ...............................................16Hernia and UndescendedTesticIe ..................................................2Hernia and Varicella.................................1Hordeolum ...............................................1Hydrocelce...............................................1Intussusception........................................3Lymphangioma . ......................................1Mastoiditis .............................................29
Analysis <strong>of</strong> Admissions and Deaths for the Year 1931(continued)Mastoiditis (Diphtheritic)...........................3Naevus... ............................................... 13Neoplasrn ...............................................1Onychia ................................................ ...1Osteomyelitis ... .................................... ...2Otitis Media .......................................... .29Otitis Media (Diphtheritic).........................2Periostitis ... .............................................1Periostitis and Morbilli ..............................1Peritonitis.................................................1Phimosis (N.B. – Not includingthose done in O.P.D.).............................6Plastic Operation on Mastoid... ................2P]astic Operation on Ear..........................1Psoas Abscess ... ....................................1Pvloric Stenosis ......................................1Ranula .....................................................1Sebaceous Cyst.......................................1Septum Deflectum ...................................1Summary <strong>of</strong> SurgicaI Cases—continued.Spina Bifida .............................................1Synovitis ..................................................1Talipes Equino Varus...............................1Talipes Equino Varusand Diphtheria 1Teeth Extraction 1Tonsils and Adenoids606Torticollis and Scarlet Fever ....1Tuberculosis - surgical .............................3Umbilical Hernia and ScarletFever .....................................................1Undescended Testis ................................3Ulceration Vulva.......................................1Whitlow ...................................................1____379Deaths.Accident Case - Fracture andInternal Injuries ................................ ...1Acute Gastro-Enteritis .............................1Burns ... ...................................................1Cellulitis, Trunk and lowerLimbs ... .............................................. ...1Cerebral Diplegia .................................. ...1Congenital Deformity .......................... ...1Convulsions .......................................... ...1Encephalitis ... .........................................1Hare-lip and Cleft Palate,Marasmus .............................................1Heart Disease and Pneumonia ................1Intussusception..................................... ...3Lymphatic Leukaerrmia ...........................1Marasmus ...............................................1Marasmus and CongenitalDefect ................................................. ...1Marasmus and Gastro-Enteritis................2Meningitis ............................................. ...3Meniingitis and Hvdrocephalus ................1Ophthalmia Neonatorum andToxaemia ... ... ................................... ...1Pneumonia and Marasmus ................... ...4Pneumonia ..............................................1Peritonitis ................................................1Pulmonary Embolism ...............................1Pyelitis (admitted 1930)............................1Pvloric Stenosis . .. ..................................1Shock, following Gastrotomy....................1Spina Bifida .............................................1Tuberculosis, Abdominal..........................1Tuberculosis, Miliary .. .............................1___43