22 SLEEP MEDICINE JANUARY 2011 • CHEST PHYSICIANHome Testing for Sleep Apnea Not InferiorBY SUSAN LONDONElsevier Global Medical NewsVANCOUVER, B.C. – Recent researchon the use <strong>of</strong> home testing for the diagnosis<strong>of</strong> obstructive sleep apnea and initiation<strong>of</strong> therapy suggests that “hometesting is here to stay,” Dr. Charles W.Atwood Jr., FCCP, said at CHEST 2010,the annual meeting <strong>of</strong> the <strong>American</strong><strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>.For more than 30 years, physicianshave relied on the traditional polysomnographyperformed in the sleeplaboratory to diagnose sleep apnea, accordingto Dr. Atwood. But with growingawareness <strong>of</strong> the condition and its prevalence,the number <strong>of</strong> people needingtesting could overwhelm capacity.“If you take the millions and millionsand millions <strong>of</strong> people in the UnitedStates alone who have sleep apnea andtry to feed them through the relativelysmall funnel <strong>of</strong> traditional sleep labs,then you are going to have big bottlenecks,”he said, adding that such bottlenecksalready exist in some areas.However, home-testing devices mustmeet certain key requirements before theyare ready for widespread use. For example,CLASSIFIEDSAlso available at www.imngmedjobs.comPROFESSIONAL OPPORTUNITIESMetro South CarolinaHospital employed joining well establishednine physician Pulmonary/CCgroup in desirable Blue Ridge Metroarea two hours to Atlanta and Charlotteassociated with a growing 450 bed hospitalsystem. 1-10 call. Excellent negotiablesalary, bonus and benefits. DONO-HUE AND ASSOCIATES 800-831-5475F: 314-984-8246E/M: donohueandassoc@aol.comPulmonology/CriticalCare <strong>Physicians</strong>Practice Opportunity for BC/BE Pulmonology/CriticalCare <strong>Physicians</strong> inBeautiful Hendersonville, Western NorthCarolina. Sleep Medicine preferred butnot required. Full-time or Part-time availability.Competitive salary & benefits. NoVisa sponsorship available. For consideratione-mail CV to:lilly.bonetti@pardeehospital.orgor Fax CV to 828-694-7722.Moving?Look to Classified Notices for practicesavailable in your area.For Deadlines and MoreInformation Contact:Rhonda Beamer443-512-8899 Ext 106FAX: 443-512-8909Email: rhonda.beamer@wt-group.comthey have to be simpler than those used inthe lab. “Perhaps we can get by withfewer [physiological] signals, but we needto understand what the key signals are,”commented Dr. Atwood, a pulmonologistand sleep medicine specialist with the VAPittsburgh Healthcare System and theUniversity <strong>of</strong> Pittsburgh Medical Center.Home testing devices will also need tobe accurate, with high sensitivity andspecificity, and “there is no single deviceI would say today that is perfect in boththese regards,” he noted. Finally, theymust be easy to use and durable, giventhe demands <strong>of</strong> in-home use.Roughly 95 studies conducted between1990 and 2006 evaluated home testing(also called portable monitoring) for thediagnosis <strong>of</strong> obstructive sleep apnea. Collectively,they had some limitations, suchas their single-site nature, small andusually homogeneous populations, andvarying degrees <strong>of</strong> rigor in design.“And they frequently focused on thehighest-risk subjects: These were middleagedmen who were overweight, snored,and were sleepy, so [they were] the verylow-hanging fruit for typical sleep apnea,”Dr. Atwood said.These studies showed some mixed re-Pulmonary/Critical CareThe VA Medical Center in Milwaukee,Wisconsin is a large tertiary care facilityaffiliated with the Medical <strong>College</strong> <strong>of</strong>Wisconsin. Openings exist for pulmonaryand critical care medicine physicians tojoin the section <strong>of</strong> Pulmonary, CriticalCare Medicine and Sleep Medicine.Qualified candidates must be Board certifiedor eligible in Pulmonary Diseaseand Critical Care Medicine and have thequalifications for a Faculty appointmentat the Medical <strong>College</strong> <strong>of</strong> Wisconsin.Fellowship training in sleep medicine isa plus. Pr<strong>of</strong>essional and academic opportunitiesexist through the Medical <strong>College</strong><strong>of</strong> Wisconsin and the Department <strong>of</strong>Veterans Affairs. Interested candidatesshould send a current Curriculum Vitae,referencing Pulmonary, to: Clement J.Zablocki VA Medical Center, Human ResourcesAttn: Prudy Kitterman, 5000 W.National Avenue, Milwaukee, WI 53295,prudy.kittermann@va.gov fax to 414-382-5296. Additional inquiries should bedirected to Andreea Antonescu, MD at414-384-2000 X42765 or email toandreea.antonescu-turcu@va.govDisclaimer<strong>Chest</strong> Physician assumes the statementsmade in classified advertisements are accurate,but cannot investigate the statementsand assumes no responsibility or liabilityconcerning their content. ThePublisher reserves the right to decline,withdraw, or edit advertisements. Every effortwill be made to avoid mistakes, butresponsibility cannot be accepted for clericalor printer errors.sults when it came to the diagnosticperformance <strong>of</strong> home testing relative tolab testing. “There is no perfect study, atleast so far, in this area, but some havecome pretty close,” he commented.Three more-recent studies suggest thathome testing is at least not inferior to labtesting for sleep apnea diagnosis and initiation<strong>of</strong> continuouspositive airwaypressure (CPAP)therapy, accordingto Dr. Atwood.In the first study,conducted in 68people with a highlikelihood <strong>of</strong> sleepapnea, the apneahypopneaindex onCPAP and Sleep Apnea Quality <strong>of</strong> Life Indexscores at 3 months did not differ significantlybetween a sleep lab and anambulatory approach (Ann. Intern. Med.2007;146:157-66). The rate <strong>of</strong> adherenceto CPAP was better with the latter.In the second study, which involved102 patients with sleep apnea symptomsand no major comorbidities, all <strong>of</strong> a variety<strong>of</strong> sleep and quality <strong>of</strong> life outcomesafter 4 weeks <strong>of</strong> CPAP weresimilar with a standard lab diagnosis andtreatment approach vs. a home approach(<strong>Chest</strong> 2010;138:257-63).The third study, the Veterans SleepApnea Treatment Trial (VSATT), is thelargest study <strong>of</strong> home testing in NorthAmerica to date, according to Dr. Atwood,one <strong>of</strong> the principal investigators.“The VA is ill equipped to managesleep apnea in a conventional way becausewe have relatively few numbers <strong>of</strong>traditional sleep labs,” he noted.“Our study differed from basically all <strong>of</strong>the other studies in the literature in thatwe had very broad inclusion criteria andvery nonrestrictive exclusion criteria,”Dr. Atwood noted. For example, patientswith comorbidities could participate aslong as their condition was stable.Patients were randomized to lab testingor home testing, followed by initiation <strong>of</strong>CPAP for those with positive results.Among the 223 who were started onCPAP, the home and lab groups had‘Functionalimprovement withCPAP for sleepapnea is not worsewhen treated inthe home settingvs. the sleep lab.’DR. ATWOODsimilar demographics. The average apneahypopneaindex was 41 for the former and45 for the latter. The Functional Outcomes<strong>of</strong> Sleep Questionnaire (FOSQ)total score was about 15 in each group.Results showed that the mean adjustedimprovement in FOSQ total score betweenbaseline and 3 months was identicalin the twogroups, at 1.79points. And withineach group, patientshad significantimprovementsin the total score aswell as its individualcomponents.Both home andlab groups also hadsignificant improvements on the EpworthSleepiness Scale (–2.6 and –2.9, respectively),the mental health component<strong>of</strong> the 12-item Short Form Health Survey(+2.5 and +3.0), and the Center for EpidemiologicStudies–Depression scale(–1.4 and –2.2). Neither group improvedsignificantly on the psychovigilance taskor the physical health component <strong>of</strong> the12-item Short Form Health Survey.When it came to adherence, whichwas monitored with smart cards, themean adjusted number <strong>of</strong> CPAP hoursdaily was 3.42 in the home group and2.99 in the lab group, a difference thatwas not significant. Cost-effectivenessanalyses are still ongoing.“We concluded that the functional improvementwith CPAP for sleep apnea isnot worse when treated in the home settingvs. the sleep lab,” Dr. Atwood said.“We believe ... home-based sleep apneadiagnosis and initiation <strong>of</strong> CPAP therapyis an effective way to treat sleep apnea.”While home testing won’t entirely replacelaboratory polysomnography, Dr.Atwood suggested trying to “integratehome sleep testing with full polysomnographyin a clinically rational way.”Dr. Atwood reported that he receivedresearch support from Embla, Resmed,and Respironics, and is a consultant toEmbla and Itamar Medical, all <strong>of</strong> whichmanufacture testing and treatment devicesfor sleep disorders.■Satisfaction With Medicine Low Among U.S. <strong>Physicians</strong>New ZealandNorwayNetherlandsUnited KingdomSwedenItalyFranceCanadaUnited StatesAustraliaD A T A W A T C H36545454495449596668SatisfiedVerysatisfiedGermany 34 50 20% 40% 60% 80% 100%Note: Data collected from 10,320 primary care physicians from February to July 2009.Source: The Commonwealth Fund1215302127183535822ELSEVIER GLOBAL MEDICAL NEWS
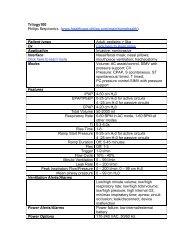
JANUARY 2011 • CHEST PHYSICIAN SLEEP MEDICINE 23CPAP Reverses Left Atrial,Ventricular RemodelingBY BRUCE JANCINElsevier Global Medical NewsSAN ANTONIO – Six months <strong>of</strong> continuouspositive airway pressure therapymarkedly improved adverse left ventricularand atrial remodeling in patientswith moderate to severe obstructivesleep apnea in a prospective study.Diastolic as well as systolic abnormalitieswere reversed, raising the welcomeprospect that CPAP is likely to preventthe development <strong>of</strong> one <strong>of</strong> the mostdreaded complications <strong>of</strong> severe obstructivesleep apnea (OSA) – chronicheart failure – although this point remainsspeculative, Dr. Saleh Al-Mutairisaid at the annual meeting <strong>of</strong> the AssociatedPr<strong>of</strong>essional Sleep Societies.He recruited 32 patients with newlydiagnosed moderate to severe OSA forthe study, which involved serial followupby cardiac magnetic resonance(CMR), echocardiography, and cardiacbiomarkers through 6 months <strong>of</strong> individuallytitrated CPAP therapy.The subjects averaged 51 years <strong>of</strong> age,with a mean baseline apnea-hypopneaindex <strong>of</strong> 53 events/hr and a body massindex <strong>of</strong> 34.5 kg/m 2 . None <strong>of</strong> the participantshad known cardiac disease. Adherenceto CPAP was good. Thepatients’ weight didn’t change significantlyduring the study, and those beingtreated for hypertension remained onthe same doses <strong>of</strong> medication throughoutthe follow-up period.Other studies have shown improvementin left ventricular dysfunction withCPAP, but they were short-term trials.This is the first study with follow-up aslong as 6 months using both CMR andechocardiography, said Dr. Al-Mutairi <strong>of</strong>the University <strong>of</strong> Manitoba, Winnipeg.He focused on the CMR results becausehe considers that technology morereliable than echocardiography for assessingventricular size and function.The echo findings, however, corroboratedthe CMR results.Most <strong>of</strong> the left ventricular measurementsfollowed during the study wereabnormal at baseline. The 6-month resultsincluded a 25% reduction frombaseline in left ventricular end-diastolicvolume and a 19% decrease in left ventricularmass. (See box, above right.)Dr. Al-Mutairi drew particular attentionto the 30% reduction in left atrial volumeindex, which he considers highly encouraging.“The treatment <strong>of</strong> OSA with CPAPmay prevent the left atrial remodelingmeasured by CMR and echo as the leftatrial volume index. This is a very importantpoint, given the association betweenthe left atrial volume andcardiovascular events,” he observed.There was no significant change inC-reactive protein, brain natriuretic peptide,or other cardiac biomarkers duringthe 6 months <strong>of</strong> CPAP use.The mechanism by which OSA isthought to predispose to heart failure involvesan exaggerated negative thoracicpressure in response to the apneicepisodes. This presumably leads to increasedleft ventricular systolic transmuralpressure, which the left atriumresists, with resultant increased complianceand atrial overstretching, Dr. Al-Mutairi explained.Dr. Al-Mutairi reported having no financialconflicts.■TYGACIL ® (tigecycline) Brief SummarySee package insert for full Prescribing Information. For further product information and current package insert, pleasevisit www.wyeth.com or call our medical communications department toll-free at 1-800-934-5556.INDICATIONS AND USAGETYGACIL is indicated for the treatment <strong>of</strong> adults with complicated skin and skin structure infections caused byEscherichia coli, Enterococcus faecalis (vancomycin-susceptible isolates), Staphylococcus aureus (methicillinsusceptibleand -resistant isolates), Streptococcus agalactiae, Streptococcus anginosus grp. (includes S. anginosus,S. intermedius, and S. constellatus), Streptococcus pyogenes, Enterobacter cloacae, Klebsiella pneumoniae, andBacteroides fragilis.TYGACIL is indicated for the treatment <strong>of</strong> adults with complicated intra-abdominal infections caused by Citrobacterfreundii, Enterobacter cloacae, Escherichia coli, Klebsiella oxytoca, Klebsiella pneumoniae, Enterococcus faecalis(vancomycin-susceptible isolates), Staphylococcus aureus (methicillin-susceptible and -resistant isolates),Streptococcus anginosus grp. (includes S. anginosus, S. intermedius, and S. constellatus), Bacteroides fragilis,Bacteroides thetaiotaomicron, Bacteroides uniformis, Bacteroides vulgatus, Clostridium perfringens, andPeptostreptococcus micros.TYGACIL is indicated for the treatment <strong>of</strong> adults with community-acquired pneumonia infections causedby Streptococcus pneumoniae (penicillin-susceptible isolates), including cases with concurrent bacteremia,Haemophilus influenzae (beta-lactamase negative isolates), and Legionella pneumophila.CONTRAINDICATIONSTYGACIL is contraindicated for use in patients who have known hypersensitivity to tigecycline.WARNINGS AND PRECAUTIONSAnaphylaxis/Anaphylactoid ReactionsAnaphylaxis/anaphylactoid reactions have been reported with nearly all antibacterial agents, includingTYGACIL, and may be life-threatening. TYGACIL is structurally similar to tetracycline-class antibiotics andshould be administered with caution in patients with known hypersensitivity to tetracycline-class antibiotics.Hepatic EffectsIncreases in total bilirubin concentration, prothrombin time and transaminases have been seen in patients treatedwith tigecycline. Isolated cases <strong>of</strong> significant hepatic dysfunction and hepatic failure have been reported in patientsbeing treated with tigecycline. Some <strong>of</strong> these patients were receiving multiple concomitant medications. Patientswho develop abnormal liver function tests during tigecycline therapy should be monitored for evidence <strong>of</strong> worseninghepatic function and evaluated for risk/benefit <strong>of</strong> continuing tigecycline therapy. Adverse events may occur after thedrug has been discontinued.Mortality Imbalance and Lower Cure Rates in Ventilator-Associated PneumoniaA study <strong>of</strong> patients with hospital acquired pneumonia failed to demonstrate the efficacy <strong>of</strong> TYGACIL. In this study,patients were randomized to receive TYGACIL (100 mg initially, then 50 mg every 12 hours) or a comparator. In addition,patients were allowed to receive specified adjunctive therapies. The sub-group <strong>of</strong> patients with ventilator-associatedpneumonia who received TYGACIL had lower cure rates (47.9% versus 70.1% for the clinically evaluable population)and greater mortality (25/131 [19.1%] versus 14/122 [11.5%]) than the comparator.Use During PregnancyTYGACIL may cause fetal harm when administered to a pregnant woman. If the patient becomes pregnantwhile taking tigecycline, the patient should be apprised <strong>of</strong> the potential hazard to the fetus. Results <strong>of</strong> animal studiesindicate that tigecycline crosses the placenta and is found in fetal tissues. Decreased fetal weights in rats and rabbits(with associated delays in ossification) and fetal loss in rabbits have been observed with tigecycline [see USE INSPECIFIC POPULATIONS].Tooth DevelopmentThe use <strong>of</strong> TYGACIL during tooth development (last half <strong>of</strong> pregnancy, infancy, and childhood to the age <strong>of</strong>8 years) may cause permanent discoloration <strong>of</strong> the teeth (yellow-gray-brown). Results <strong>of</strong> studies in rats withTYGACIL have shown bone discoloration. TYGACIL should not be used during tooth development unless other drugsare not likely to be effective or are contraindicated.Clostridium difficile-Associated DiarrheaClostridium difficile-associated diarrhea (CDAD) has been reported with use <strong>of</strong> nearly all antibacterial agents, includingTYGACIL, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters thenormal flora <strong>of</strong> the colon leading to overgrowth <strong>of</strong> C. difficile. C. difficile produces toxins A and B which contribute tothe development <strong>of</strong> CDAD. Hypertoxin producing strains <strong>of</strong> C. difficile cause increased morbidity and mortality, as theseinfections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patientswho present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reportedto occur over two months after the administration <strong>of</strong> antibacterial agents. If CDAD is suspected or confirmed, ongoingantibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolytemanagement, protein supplementation, antibiotic treatment <strong>of</strong> C. difficile, and surgical evaluation should be institutedas clinically indicated.Patients With Intestinal PerforationCaution should be exercised when considering TYGACIL monotherapy in patients with complicated intra-abdominalinfections (cIAI) secondary to clinically apparent intestinal perforation. In cIAI studies (n=1642), 6 patients treated withTYGACIL and 2 patients treated with imipenem/cilastatin presented with intestinal perforations and developed sepsis/septic shock. The 6 patients treated with TYGACIL had higher APACHE II scores (median = 13) versus the 2 patientstreated with imipenem/cilastatin (APACHE II scores = 4 and 6). Due to differences in baseline APACHE II scores betweentreatment groups and small overall numbers, the relationship <strong>of</strong> this outcome to treatment cannot be established.Tetracycline-Class EffectsTYGACIL is structurally similar to tetracycline-class antibiotics and may have similar adverse effects. Such effectsmay include: photosensitivity, pseudotumor cerebri, and anti-anabolic action (which has led to increased BUN, azotemia,acidosis, and hyperphosphatemia). As with tetracyclines, pancreatitis has been reported with the use <strong>of</strong> TYGACIL.SuperinfectionAs with other antibacterial drugs, use <strong>of</strong> TYGACIL may result in overgrowth <strong>of</strong> non-susceptible organisms, including fungi.Patients should be carefully monitored during therapy. If superinfection occurs, appropriate measures should be taken.Development <strong>of</strong> Drug-Resistant BacteriaPrescribing TYGACIL in the absence <strong>of</strong> a proven or strongly suspected bacterial infection is unlikely to provide benefitto the patient and increases the risk <strong>of</strong> the development <strong>of</strong> drug-resistant bacteria.ADVERSE REACTIONSBecause clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinicaltrials <strong>of</strong> a drug cannot be directly compared to rates in the clinical trials <strong>of</strong> another drug and may not reflect the ratesobserved in practice.In clinical trials, 2514 patients were treated with TYGACIL. TYGACIL was discontinued due to adverse reactions in7% <strong>of</strong> patients compared to 6% for all comparators. Table 1 shows the incidence <strong>of</strong> treatment-emergent adversereactions through test <strong>of</strong> cure reported in 2% <strong>of</strong> patients in these trials.Table 1. Incidence (%) <strong>of</strong> Adverse Reactions Through Test <strong>of</strong> CureReported in 2% <strong>of</strong> Patients Treated in Clinical StudiesBody System TYGACIL Comparators aAdverse Reactions (N=2514) (N=2307)Body as a WholeAbdominal pain 6 4Abscess 3 3Asthenia 3 2Headache 6 7Infection 8 5Cardiovascular SystemPhlebitis 3 4Digestive SystemDiarrhea 12 11Dyspepsia 2 2Nausea 26 13Vomiting 18 9Hemic and Lymphatic SystemAnemia 4 5Metabolic and NutritionalAlkaline Phosphatase Increased 4 3Amylase Increased 3 2Bilirubinemia 2 1BUN Increased 3 1Healing Abnormal 4 3Hypoproteinemia 5 3SGOT Increased b 4 5SGPT Increased b 5 5Nervous SystemDizziness 3 3Skin and AppendagesRash 3 4Key Cardiac Magnetic Resonance ChangesWithin 6 Months <strong>of</strong> CPAPBaselineFollow-upLeft ventricularend-systolic volume 68 mL 53 mLLeft ventricularend-diastolic volume 199 mL 150 mLLeft ventricular mass 184 g 149 gLeft atrial volume index 49 mL/m 2 34 mL/m 2Notes: Based on a study <strong>of</strong> 32 patients with moderate to severe obstructive sleepapnea. All reductions are statistically significant.Source: Dr. Al-MutairiaVancomycin/Aztreonam, Imipenem/Cilastatin, Lev<strong>of</strong>loxacin, Linezolid.bLFT abnormalities in TYGACIL-treated patients were reported more frequently in the post therapy period than thosein comparator-treated patients, which occurred more <strong>of</strong>ten on therapy.In all Phase 3 and 4 studies that included a comparator, death occurred in 3.9% (147/3788) <strong>of</strong> patients receivingTYGACIL and 2.9% (105/3646) <strong>of</strong> patients receiving comparator drugs. An increase in all-cause mortality has beenobserved across phase 3 and 4 clinical studies in TYGACIL treated patients versus comparator. The cause <strong>of</strong>this increase has not been established. This increase should be considered when selecting among treatmentoptions. (See Table 2.)Table 2. Patients with Adverse Events with Outcome <strong>of</strong> Death by Infection TypeTYGACIL Comparator Risk Difference*Infection Type n/N % n/N % % (95% CI)Approved IndicationscSSSI 12/834 1.4 6/813 0.7 0.7 (-0.5, 1.9)cIAI 40/1382 2.9 27/1393 1.9 1.0 (-0.3, 2.2)CAP 12/424 2.8 11/422 2.6 0.2 (-2.3, 2.7)Combined 64/2640 2.4 44/2628 1.7 0.7 (-0.0, 1.6)Unapproved IndicationsHAP 65/467 13.9 56/467 12.0 1.9 (-2.6, 6.4)Non-VAP a 40/336 11.9 42/345 12.2 -0.3 (-5.4, 4.9)VAP a 25/131 19.1 14/122 11.5 7.6 (-2.0, 16.9)RP 11/128 8.6 2/43 4.7 3.9 (-9.1, 11.6)DFI 7/553 1.3 3/508 0.6 0.7 (-0.8, 2.2)Combined 84/1148 7.2 61/1018 6.0 1.2 (-1.0, 3.4)CAP = Community-acquired pneumonia; cIAI = Complicated intra-abdominal infections; cSSSI = Complicated skin andskin structure infections; HAP = Hospital-acquired pneumonia; VAP = Ventilator-associated pneumonia; RP = Resistantpathogens; DFI = Diabetic foot infections.* The difference between the percentage <strong>of</strong> patients who died in TYGACIL and comparator treatment groups.aThese are subgroups <strong>of</strong> the HAP population.Note: The studies include 300, 305, 900 (cSSSI), 301, 306, 315, 316, 400 (cIAI), 308 and 313 (CAP), 311 (HAP), 307[Resistant gram-positive pathogen study in patients with MRSA or Vancomycin-Resistant Enterococcus (VRE)], and 319(DFI with and without osteomyelitis).In comparative clinical studies, infection-related serious adverse events were more frequently reported for subjectstreated with TYGACIL (7%) versus comparators (6%). Serious adverse events <strong>of</strong> sepsis/septic shock were morefrequently reported for subjects treated with TYGACIL (2%) versus comparators (1%). Due to baseline differencesbetween treatment groups in this subset <strong>of</strong> patients, the relationship <strong>of</strong> this outcome to treatment cannot beestablished [see WARNINGS AND PRECAUTIONS].The most common treatment-emergent adverse reactions were nausea and vomiting which generally occurred duringthe first 1 – 2 days <strong>of</strong> therapy. The majority <strong>of</strong> cases <strong>of</strong> nausea and vomiting associated with TYGACIL and comparatorswere either mild or moderate in severity. In patients treated with TYGACIL, nausea incidence was 26% (17% mild, 8%moderate, 1% severe) and vomiting incidence was 18% (11% mild, 6% moderate, 1% severe).In patients treated for complicated skin and skin structure infections (cSSSI), nausea incidence was 35% for TYGACILand 9% for vancomycin/aztreonam; vomiting incidence was 20% for TYGACIL and 4% for vancomycin/aztreonam. Inpatients treated for complicated intra-abdominal infections (cIAI), nausea incidence was 25% for TYGACIL and 21%for imipenem/cilastatin; vomiting incidence was 20% for TYGACIL and 15% for imipenem/cilastatin. In patients treatedfor community-acquired bacterial pneumonia (CABP), nausea incidence was 24% for TYGACIL and 8% for lev<strong>of</strong>loxacin;vomiting incidence was 16% for TYGACIL and 6% for lev<strong>of</strong>loxacin.Discontinuation from tigecycline was most frequently associated with nausea (1%) and vomiting (1%).For comparators, discontinuation was most frequently associated with nausea (