Download PDF - American College of Chest Physicians
Download PDF - American College of Chest Physicians
Download PDF - American College of Chest Physicians
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
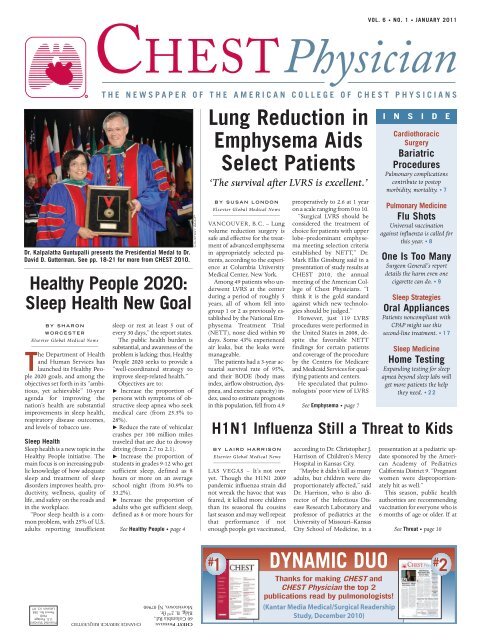
VOL. 6 • NO. 1 • JANUARY 2011Dr. Kalpalatha Guntupalli presents the Presidential Medal to Dr.David D. Gutterman. See pp. 18-21 for more from CHEST 2010.Healthy People 2020:Sleep Health New GoalBY SHARONWORCESTERElsevier Global Medical NewsThe Department <strong>of</strong> Healthand Human Services haslaunched its Healthy People2020 goals, and among theobjectives set forth in its “ambitious,yet achievable” 10-yearagenda for improving thenation’s health are substantialimprovements in sleep health,respiratory disease outcomes,and levels <strong>of</strong> tobacco use.Sleep HealthSleep health is a new topic in theHealthy People initiative. Themain focus is on increasing publicknowledge <strong>of</strong> how adequatesleep and treatment <strong>of</strong> sleepdisorders improves health, productivity,wellness, quality <strong>of</strong>life, and safety on the roads andin the workplace.“Poor sleep health is a commonproblem, with 25% <strong>of</strong> U.S.adults reporting insufficientsleep or rest at least 5 out <strong>of</strong>every 30 days,” the report states.The public health burden issubstantial, and awareness <strong>of</strong> theproblem is lacking; thus, HealthyPeople 2020 seeks to provide a“well-coordinated strategy toimprove sleep-related health.”Objectives are to: Increase the proportion <strong>of</strong>persons with symptoms <strong>of</strong> obstructivesleep apnea who seekmedical care (from 25.5% to28%). Reduce the rate <strong>of</strong> vehicularcrashes per 100 million milestraveled that are due to drowsydriving (from 2.7 to 2.1). Increase the proportion <strong>of</strong>students in grades 9-12 who getsufficient sleep, defined as 8hours or more on an averageschool night (from 30.9% to33.2%). Increase the proportion <strong>of</strong>adults who get sufficient sleep,defined as 8 or more hours forSee Healthy People • page 4COURTESY ACCPLung Reduction inEmphysema AidsSelect Patients‘The survival after LVRS is excellent.’BY SUSAN LONDONElsevier Global Medical NewsVANCOUVER, B.C. – Lungvolume reduction surgery issafe and effective for the treatment<strong>of</strong> advanced emphysemain appropriately selected patients,according to the experienceat Columbia UniversityMedical Center, New York.Among 49 patients who underwentLVRS at the centerduring a period <strong>of</strong> roughly 5years, all <strong>of</strong> whom fell intogroup 1 or 2 as previously establishedby the National EmphysemaTreatment Trial(NETT), none died within 90days. Some 43% experiencedair leaks, but the leaks weremanageable.The patients had a 3-year actuarialsurvival rate <strong>of</strong> 95%,and their BODE (body massindex, airflow obstruction, dyspnea,and exercise capacity) index,used to estimate prognosisin this population, fell from 4.9BY LAIRD HARRISONElsevier Global Medical NewsLAS VEGAS – It’s not overyet. Though the H1N1 2009pandemic influenza strain didnot wreak the havoc that wasfeared, it killed more childrenthan its seasonal flu cousinslast season and may well repeatthat performance if notenough people get vaccinated,preoperatively to 2.6 at 1 yearon a scale ranging from 0 to 10.“Surgical LVRS should beconsidered the treatment <strong>of</strong>choice for patients with upperlobe–predominant emphysemameeting selection criteriaestablished by NETT,” Dr.Mark Ellis Ginsburg said in apresentation <strong>of</strong> study results atCHEST 2010, the annualmeeting <strong>of</strong> the <strong>American</strong> <strong>College</strong><strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>. “Ithink it is the gold standardagainst which new technologiesshould be judged.”However, just 119 LVRSprocedures were performed inthe United States in 2008, despitethe favorable NETTfindings for certain patientsand coverage <strong>of</strong> the procedureby the Centers for Medicareand Medicaid Services for qualifyingpatients and centers.He speculated that pulmonologists’poor view <strong>of</strong> LVRSSee Emphysema • page 7H1N1 Influenza Still a Threat to Kidsaccording to Dr. Christopher J.Harrison <strong>of</strong> Children’s MercyHospital in Kansas City.“Maybe it didn’t kill as manyadults, but children were disproportionatelyaffected,” saidDr. Harrison, who is also director<strong>of</strong> the Infectious DiseaseResearch Laboratory andpr<strong>of</strong>essor <strong>of</strong> pediatrics at theUniversity <strong>of</strong> Missouri–KansasCity School <strong>of</strong> Medicine, in aI N S I D ECardiothoracicSurgeryBariatricProceduresPulmonary complicationscontribute to postopmorbidity, mortality. • 7Pulmonary MedicineFlu ShotsUniversal vaccinationagainst influenza is called forthis year. • 8One Is Too ManySurgeon General’s reportdetails the harm even onecigarette can do. • 9Sleep StrategiesOral AppliancesPatients noncompliant withCPAP might use thissecond-line treatment. • 17Sleep MedicineHome TestingExpanding testing for sleepapnea beyond sleep labs willget more patients the helpthey need. • 22presentation at a pediatric updatesponsored by the <strong>American</strong>Academy <strong>of</strong> PediatricsCalifornia District 9. “Pregnantwomen were disproportionatelyhit as well.”This season, public healthauthorities are recommendingvaccination for everyone who is6 months <strong>of</strong> age or older. If atSee Threat • page 10Presorted StandardU.S. PostagePAIDPermit No. 384Lebanon Jct. KYCHEST PHYSICIAN CHANGE SERVICE REQUESTED60 Columbia Rd.,Bldg. B, 2 nd flr.Morristown, NJ 079601DYNAMIC DUO# # 2Thanks for making CHEST andCHEST Physician the top 2publications read by pulmonologists!(Kantar Media Medical/Surgical ReadershipStudy, December 2010)
November was Pulmonary Hypertension Awareness Month.Here’s how you can help.Don’t wait,refer earlysEarly referrals to a PH Specialist help providecomprehensive care 1-3Turn the page to learn about the advantages<strong>of</strong> early referrals to PH Specialists… 1,2RVU00224B © 2010 Pfizer Inc. All rights reserved
November was Pulmonary Hypertension Awareness Month.Here’s how you can help.Don’t wait,refer earlyPH Specialists encourage early referrals <strong>of</strong> PAH patientsregardless <strong>of</strong> WHO Functional Class (I, II, III, IV)* 1-4Patients receive comprehensive caresA full support system for PAH patients, including comprehensive medical care,reimbursement opportunities, education, and counseling 5-7Patients gain access to information on the latest clinical trials 1-3,5-7sPatients’ participation helps build clinical trials that provide reliable data relevantto the PAH population 1,3,8,9Help optimize care for your PAH patients with early referrals.Please visit www.PHAssociation.org for more information.*Adapted from the New York Heart Association (NYHA).References: 1. Barst RJ, Gibbs JSR, Gh<strong>of</strong>rani HA, et al. Updated evidence-based treatment algorithm in pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54(1)(suppl S):S78–S84. 2. McLaughlin VV, Archer SL, Badesch DB, et al. ACCF/AHA 2009 expert consensus document on pulmonary hypertension: a report <strong>of</strong> the<strong>American</strong> <strong>College</strong> <strong>of</strong> Cardiology Foundation Task Force on Expert Consensus Documents and the <strong>American</strong> Heart Association developed in collaboration with the<strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>; <strong>American</strong> Thoracic Society, Inc.; and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009;53(17):1573-1619.3. Badesch DB, Abman SH, Simonneau G, Rubin LJ, McLaughlin VV. Medical therapy for pulmonary arterial hypertension: updated ACCP evidence-based clinicalpractice guidelines. <strong>Chest</strong>. 2007;131:1917–1928. 4. McGoon M, Gutterman D, Steen V, et al. Screening, early detection, and diagnosis <strong>of</strong> pulmonary arterial hypertension:ACCP evidence-based clinical practice guidelines. <strong>Chest</strong>. 2004;126:14S–34S. 5. Temple University Hospital. Temple Lung Center & Pulmonologists. http://pulmonary.templehealth.org/content/default/htm. Accessed September 24, 2010. 6. Stanford University. Stanford Pulmonary Hypertension Program. http://pulmonary.stanford.edu/patientcare/hyperten.html. Accessed September 24, 2010. 7. Pulmonary Hypertension Clinic, Mayo Clinic in Rochester, Minn. Cardiovascular Diseases inMinnesota. http://www.mayoclinic.org/cardiovascular-disease-rst/pulmhyperclinic.html. Accessed September 24, 2010. 8. McLaughlin VV, Badesch DB, Delcroix M, etal. End points and clinical trial design in pulmonary arterial hypertension. J Am Coll Cardiol. 2009;54(suppl 1):S97-S107. 9. Humbert M, McLaughlin VV. The 4th WorldSymposium on Pulmonary Hypertension. J Am Coll Cardiol. 2009;54:S1-S2.RVU00224B © 2010 Pfizer Inc. All rights reserved
4 NEWS JANUARY 2011 • CHEST PHYSICIANNew COPD, Tobacco Goals SetHealthy People • from page 1those aged 18-21 years, and 7 or morehours for those aged 22 years and older(from 69.6% to 70.9%).Respiratory DiseaseThe respiratory disease category focuseson asthma and chronic obstructive pulmonarydisease, and the main goal is to“promote respiratory health through betterprevention, detection, treatment, andeducation efforts,” according to the report,which states that asthma affects 23million people in the United States andCOPD affects 13.6 million U.S. adults.The cost to the health care system ishigh, and society pays through higherhealth insurance rates and lost productivityand tax dollars. Annual expendituresfor asthma alone are estimated atnearly $21 billion.Healthy People 2020 seeks to reduceasthma-related deaths, hospitalizations,emergency department visits, activitylimitations, and missed school or workdays, and to increase the proportion <strong>of</strong>asthma sufferers who receive appropriatecare. Improved surveillance at thestate level is another goal.IN THIS ISSUENews From the <strong>College</strong> • 14Editorial Advisory BoardCHEST PHYSICIAN’s editorialboard gains new members and adeputy editor. • 14CHEST PHYSICIAN Is OnlineCHEST PHYSICIAN is available onthe Web at www.chestnet.org/accp/chest-physician.For example, goals for 2020 in regardto asthma-related deaths include reductionsfrom 11.0 to 6.0 deaths per 1 millionpeople aged 35-64 years,and from 43.3 to 22.9 per1 million people aged65 and older. Goals regardingannual asthmarelatedhospitalizationinclude a reduction from 41.4to 18.1 per 10,000 children under age 5,from 11.1 to 8.6 per 10,000 people aged5-64 years, and from 25.3 to 20.3 per10,000 adults aged 65 years and older.Goals regarding appropriate asthmacare include improvements in the number<strong>of</strong> patients who receive written asthmamanagement plans, instructions for inhaleruse, education about appropriate responseto an asthma episode, andfollow-up visits each year.COPD-related objectives include reducingactivity limitations, deaths, hospitalizations,and emergency departmentvisits, and improving diagnosis amongadults with abnormal lung function.Specific goals include a reduction from23.2 to 18.7 in the percentage <strong>of</strong> adultswith COPD aged 45 years and olderwith activity limitations from COPD,and a reduction from 112.4 to 98.5 in thenumber <strong>of</strong> COPD-related deaths per10,000 people aged 45 years and older.Tobacco UseTobacco use is not a new topic in theHealthy People initiative, but ongoing effortsto reduce use are needed, accordingto the report, because tobacco use remainsthe single most preventable cause<strong>of</strong> death and disease in the United States.About 443,000 <strong>American</strong>s die from tobacco-relatedillnesses each year, and forevery 1 who dies, 20 more suffer with atleast one serious tobacco-related illness.Healthy People 2020 seeks to “providea framework for action to reduce tobaccouse to the point that it is no longer apublic health problem for the nation.”More than 4 decades <strong>of</strong> evidence hasshown that the toll tobacco use takes onfamilies and communities can be significantlyreduced by fully funding tobaccocontrol programs, increasing the prices<strong>of</strong> tobacco products, enactingsmoke-free policies, controllingaccess to products,reducing tobaccoadvertising and promotion,implementing antitobaccomedia campaigns, andencouraging and assisting users to quit.Healthy People 2020 addresses tobaccouse prevalence, health system changes,and social and environmental changes.Among the key goals for adults are: Reducing the percentage <strong>of</strong> adult cigarettesmokers (from 20.6% to 12.0%). Reducing the percentage <strong>of</strong> adultusers <strong>of</strong> smokeless tobacco (from 2.3%to 0.3%). Reducing the percentage <strong>of</strong> adult cigarsmokers (from 2.2% to 0.2%).In adolescents, goals include reducingthe percentage <strong>of</strong> those who used tobaccoin the past month from 26% to21%, and reducing the percentages whosaid they used cigarettes, smokeless tobacco,and cigars in the past month from19.5% to 16%, from 8.9% to 6.9%, andfrom 14% to 8%, respectively.Initiation <strong>of</strong> tobacco use among children,adolescents, and young adults isalso addressed, with a goal <strong>of</strong> reducingit among those aged 12-17 years from7.7% to 5.7%, and among those aged 18-25 years from 10.8% to 8.8%.Numerous goals are also set in regardto health system changes, and social andenvironmental changes.For example, the report calls for increasesin comprehensive Medicaid coveragefor nicotine dependency treatment,increased tobacco screening and counselingin health care settings, reductions inthe proportion <strong>of</strong> nonsmokers exposed tosecondhand smoke, increases in the proportion<strong>of</strong> persons covered by worksitepolicies that prohibit smoking, and increasesin tobacco-free environments inschool facilities and at school events.Efforts should be made to eliminatestate laws that preempt stronger local tobaccocontrol laws, to reduce illegal salesto minors, and to reduce exposure to tobaccoadvertising and promotion among6th-12th graders. Also, federal and statetaxes on tobacco products should be increased,the report states.Healthy People 2020 has been in developmentsince 2007. A panel <strong>of</strong> healthexperts drew on input from public andprivate health <strong>of</strong>ficials, preventive medicineexperts, representatives from 2,000health organizations, and thousands <strong>of</strong>public comments.The initiative expands upon topics fromHealthy People 2010, and will incorporatethe Internet and other media in spreadingthe message. The ultimate goals,according to HHS <strong>of</strong>ficials, are to avoidpreventable diseases and to promote improvedquantity and quality <strong>of</strong> life. ■COMMENTARYDr. Paul A. Selecky, FCCP,comments: Each <strong>of</strong> these topicsis very importanttog o o dhealth,and <strong>of</strong>tengo hand inhand, e.g.,C O P Dand tobaccouse. It’salso good news that sleep finallygot on the HHS radar. It is thethird important pillar <strong>of</strong> goodhealth, along with regular exerciseand a balanced diet. We area sleep-deprived nation with a“National Sleep Debt,” a termcoined by William Dement, atrue pioneer in sleep medicine.Sleeping longer on the weekendwill not repay that debt.AMERICAN COLLEGE OF CHEST PHYSICIANSEditor in Chief Paul A. Selecky, M.D., FCCPDeputy Editor W. Michael Alberts, MD, FCCPPresident David D. Gutterman, MD, FCCPExecutive Vice President and CEO Paul A. Markowski, CAESenior Vice President, Communications Stephen J. WelchManager, Editorial Resources Pamela L. GoorskyMedical Copy Editor II Peggy E. Perona, R.D.Section EditorsMarilyn G. Foreman, M.D., FCCP - Pulmonary Perspectives EditorLoren J. Harris, M.D., FCCP - Pulmonary Perspectives Deputy EditorNeil Halpern, M.D., FCCP - Critical Care CommentaryJames Parish, M.D., FCCP - Sleep StrategiesEDITORIAL ADVISORY BOARDJoseph Barney, M.D., FCCP, AlabamaJun Chiong, M.D., FCCP, CaliforniaStephen Field, M.D., FCCP, CalgaryRichard Fischel, M.D., FCCP, CaliforniaStuart M. Garay, M.D., FCCP, New YorkCarl Kaplan, M.D., FCCP, MissouriBurt Lesnick, M.D., FCCP, GeorgiaDarcy D. Marciniuk, M.D., FCCP, SaskatchewanJeana O’Brien, M.D., FCCP, TexasMarcos I. Restrepo, M.D., MSc, FCCP, TexasNirupam Singh, M.D., FCCP, CaliforniaE-mail: chestphysiciannews@chestnet.orgCHEST PHYSICIANCHEST PHYSICIAN, the newspaper <strong>of</strong> the <strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong><strong>Physicians</strong>, provides cutting-edge reports from clinical meetings, FDAcoverage, clinical trial results, expert commentary, and reporting onthe business and politics <strong>of</strong> chest medicine. Each issue also providesmaterial exclusive to the members <strong>of</strong> the <strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong><strong>Physicians</strong>. Content for CHEST PHYSICIAN is provided by InternationalMedical News Group and Elsevier Global Medical News. Content forNEWS FROM THE COLLEGE is provided by the <strong>American</strong> <strong>College</strong> <strong>of</strong><strong>Chest</strong> <strong>Physicians</strong>.The statements and opinions expressed in CHEST PHYSICIAN do notnecessarily reflect those <strong>of</strong> the <strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>,or <strong>of</strong> its <strong>of</strong>ficers, regents, members, and employees, or those <strong>of</strong> thePublisher. The <strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>, its <strong>of</strong>ficers,regents, members, and employees, and Elsevier Inc. do not assumeresponsibility for damages, loss, or claims <strong>of</strong> any kind arising fromor related to the information contained in this publication, includingany claims related to products, drugs, or services mentioned herein.Address Changes: Fax changes <strong>of</strong> address (with old mailing label)to 973-290-8245.POSTMASTER: Send change <strong>of</strong> address (with old mailing label) toCHEST PHYSICIAN, 60 B Columbia Rd., 2 nd flr., Morristown, NJ 07960.CHEST PHYSICIAN (ISSN 1558-6200) is published monthly for the<strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong> by Elsevier Inc.,60 B Columbia Rd., 2 nd flr., Morristown, NJ 07960, 973-290-8200,fax 973-290-8250.©Copyright 2011, by the <strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>ELSEVIER SOCIETY NEWS GROUP,A DIVISION OF INTERNATIONAL MEDICAL NEWSGROUPPresident, IMNG Alan J. Imh<strong>of</strong>fDirector, ESNG Mark BrancaEditor in Chief Mary Jo M. DalesExecutive Editors Denise Fulton, Kathy ScarbeckManaging Editor Leanne SullivanCirculation Analyst Barbara Cavallaro, 973-290-8253,b.cavallaro@elsevier.comExecutive Director, Operations Jim ChiccaDirector, Production and Manufacturing Yvonne Evans StrussProduction Manager Judi ShefferCreative Director Louise A. KoenigDisplay Advertising Manager The Walchli Tauber Group: 443-512-8899,fax 443-512-8909, greg.pessagno@wt-group.comADVERTISING OFFICES 60 B Columbia Rd., 2 nd flr., Morristown, NJ07960, 973-290-8200, fax 973-290-8250CLASSIFIED ADVERTISING OFFICES The Walchli Tauber Group, 2225 OldEmmorton Rd., Suite 201, Bel Air, MD 21015, 443-512-8899EDITORIAL OFFICES 5635 Fishers Lane, Suite 6000,Rockville, MD 20852, 240-221-4500, fax 240-221-2541
FOR THE TREATMENT OF EXOCRINE PANCREATIC INSUFFICIENCYDUE TO CYSTIC FIBROSIS OR OTHER CONDITIONS 1An FDA-approved, next-generation pancreatic enzyme that’sDESIGNED TO GETTO THE RIGHT PLACEAT THE RIGHT TIME 2-3Designed to deliver improved fat absorption 4 ...t Mean coefficient <strong>of</strong> fat absorption (CFA) was 88.3% for patients treated with ZENPEP vs 62.8% forpatients treated with placebo (primary endpoint) in the pivotal trial <strong>of</strong> patients aged ≥7 years 4t 91% (n=29 <strong>of</strong> 32) <strong>of</strong> patients achieved a CFA >80% 4t Results were achieved without the use <strong>of</strong> concomitant agents such as PPIs, H 2 -antagonists,and motility agents 4... with improved symptom control, even when switchedfrom a previous enzyme 4t 100% (N=19) <strong>of</strong> children with PI due to CF switched to ZENPEP from a previous unapproved pancreaticenzyme had improved or maintained their level <strong>of</strong> symptom control (secondary endpoint) 4– In this open-label, uncontrolled trial <strong>of</strong> patients aged 1 to 6 years, parents/guardians reported that 47%<strong>of</strong> patients switched to ZENPEP had improved symptom control (n=9) and 53% maintained symptomcontrol (n=10) 4 *– ZENPEP is not interchangeable with any other pancrelipase product, and requires a new prescriptionImportant Safety Informationt Fibrosing colonopathy is a rare serious adverse reaction associated with high-dose use <strong>of</strong> pancreatic enzyme replacementproducts and most commonly reported in pediatric patients with CF. Exercise caution when doses <strong>of</strong> ZENPEP exceed2500 lipase units/kg <strong>of</strong> body weight per meal (or greater than 10,000 lipase units/kg <strong>of</strong> body weight per day)t Exercise caution when prescribing ZENPEP to patients with gout, renal impairment, or hyperuricemia and when administeringpancrelipase to a patient with a known allergy to proteins <strong>of</strong> porcine origint To avoid irritation <strong>of</strong> oral mucosa or inactivation <strong>of</strong> enzymes, do not chew ZENPEP capsules or beads or retain in the moutht There is theoretical risk <strong>of</strong> viral transmission with all pancreatic enzyme products, including ZENPEPPlease read Brief Summary <strong>of</strong> Prescribing Information on adjacent page and provideMedication Guide to patients prescribed ZENPEP.*Reports were subjective and recorded in a daily diary form. 4References: 1. ZENPEP [package insert]. Yardley, PA: Eurand Pharmaceuticals, Inc.; 2010. 2. Data on file MED-0151, Eurand Pharmaceuticals, Inc.,Yardley, PA. 3. Data on file MED-0152, Eurand Pharmaceuticals, Inc., Yardley, PA. 4. Wooldridge JL, Heubi JE, Amaro-Galvez R, et al. EUR-1008pancreatic enzyme replacement is safe and effective in patients with cystic fibrosis and pancreatic insufficiency. J Cyst Fibros. 2009;8(6):405-417.©2011EurandPharmaceuticals,Inc.Allrightsreserved. PrintedinUSA. ZEN 03202 1/11PRECISELY THE WAY IT SHOULD BE TM
6 PALLIATIVE CARE JANUARY 2011 • CHEST PHYSICIANCancer Patients Benefit From Earlier Palliative CarePrescription onlyBrief Summary <strong>of</strong> Prescribing Information (for Full Prescribing Information and Medication Guide, refer to package insert)INDICATIONS AND USAGEZENPEP is a combination <strong>of</strong> porcine-derived lipases, proteases, and amylases indicated for the treatment <strong>of</strong> exocrine pancreatic insufficiency dueto cystic fibrosis or other conditionsDOSAGE AND ADMINISTRATIONDosageZENPEP is not interchangeable with any other pancrelipase product.Infants (up to 12 months)@ Infants may be given 2,000 to 4,000 lipase units per 120 mL <strong>of</strong> formula or per breast-feeding.@ Do not mix ZENPEP capsule contents directly into formula or breast milk prior to administration.Children Older than 12 Months and Younger than 4 Years@ Enzyme dosing should begin with 1,000 lipase units/kg <strong>of</strong> body weight per meal to a maximum <strong>of</strong> 2,500 lipase units/kg <strong>of</strong> body weight permeal (or less than or equal to 10,000 lipase units/kg <strong>of</strong> body weight per day), or less than 4,000 lipase units/g fat ingested per day.Children 4 Years and Older and Adults@ Enzyme dosing should begin with 500 lipase units/kg <strong>of</strong> body weight per meal to a maximum <strong>of</strong> 2,500 lipase units/kg <strong>of</strong> body weight per meal(or less than or equal to 10,000 lipase units/kg <strong>of</strong> body weight per day), or less than 4,000 lipase units/g fat ingested per day.Limitations on Dosing@ Dosing should not exceed the recommended maximum dosage set forth by the Cystic Fibrosis Foundation Consensus ConferencesGuidelines.AdministrationZENPEP should be swallowed whole. For infants or patients unable to swallow intact capsules, the contents may be sprinkled on s<strong>of</strong>t acidic food,e.g., applesauce.DOSAGE FORMS AND STRENGTHS@ 5,000 USP units <strong>of</strong> lipase; 17,000 USP units <strong>of</strong> protease; 27,000 USP units <strong>of</strong> amylase. Capsules have a white opaque cap and body, printed with“EURAND 5”@ 10,000 USP units <strong>of</strong> lipase; 34,000 USP units <strong>of</strong> protease; 55,000 USP units <strong>of</strong> amylase. Capsules have a yellow opaque cap and white opaquebody, printed with “EURAND 10”@ 15,000 USP units <strong>of</strong> lipase; 51,000 USP units <strong>of</strong> protease; 82,000 USP units <strong>of</strong> amylase. Capsules have a red opaque cap and white opaquebody, printed with “EURAND 15”@ 20,000 USP units <strong>of</strong> lipase; 68,000 USP units <strong>of</strong> protease; 109,000 USP units <strong>of</strong> amylase. Capsules have a green opaque cap and white opaquebody, printed with “EURAND 20”CONTRAINDICATIONSNone.WARNINGS AND PRECAUTIONS@ Fibrosing colonopathy is associated with high-dose use <strong>of</strong> pancreatic enzyme replacement. Exercise caution when doses <strong>of</strong> ZENPEP exceed2,500 lipase units/kg <strong>of</strong> body weight per meal (or greater than 10,000 lipase units/kg <strong>of</strong> body weight per day).@ To avoid irritation <strong>of</strong> oral mucosa, do not chew ZENPEP or retain in the mouth.@ Exercise caution when prescribing ZENPEP to patients with gout, renal impairment, or hyperuricemia.@ There is theoretical risk <strong>of</strong> viral transmission with all pancreatic enzyme products including ZENPEP.@ Exercise caution when administering pancrelipase to a patient with a known allergy to proteins <strong>of</strong> porcine origin.ADVERSE REACTIONS@ The most common adverse events (≥6% <strong>of</strong> patients treated with ZENPEP) are abdominal pain, flatulence, headache, cough, decreased weight,early satiety, and contusion.@ There is no postmarketing experience with this formulation <strong>of</strong> ZENPEP.To report SUSPECTED ADVERSE REACTIONS, contact EURAND Pharmaceuticals, Inc. at 1-800-716-6507 or FDA at 1-800-FDA-1088 orwww.fda.gov/medwatch.DRUG INTERACTIONSNo drug interactions have been identified. No formal interaction studies have been conducted.USE IN SPECIFIC POPULATIONSPediatric Patients@ The safety and effectiveness <strong>of</strong> ZENPEP were assessed in pediatric patients, ages 1 to 17 years.@ The safety and efficacy <strong>of</strong> pancreatic enzyme products with different formulations <strong>of</strong> pancrelipase in pediatric patients have been described inthe medical literature and through clinical experience.See PATIENT COUNSELING INFORMATION in Prescribing Information and FDA-approved Medication Guide.Marketed by:Eurand Pharmaceuticals, Inc.Yardley, PA 19067©2011 Eurand Pharmaceuticals, Inc. All rights reserved. ZEN 1506 1/11.Rev January 2011BY SUSAN BIRKElsevier Global Medical NewsCHICAGO – Oncologists and otherswho care for cancer patients can improveoutcomes by integrating palliativecare into standard treatment earlier –even as early as the time <strong>of</strong> diagnosis, Dr.Charles F. von Gunten said at the ChicagoSupportive Oncology Conference.Doing so would require clinicians toexpand their definition <strong>of</strong> palliative carefar beyond the traditional boundaries <strong>of</strong>hospice, which begins only toward theend <strong>of</strong> life when other therapies are nolonger working, said Dr. von Gunten <strong>of</strong>the University <strong>of</strong> California, San Diego,and provost at the Institute for PalliativeMedicine at San Diego.He called on clinicians to rethink thetraditional “either-or” approach to cancertreatment – in which care consists <strong>of</strong>either therapies aimed at reducing orcuring the illness or care designed to easesuffering and improve the quality <strong>of</strong> life– and to adopt a “both-and” model insteadthat employs both standard therapies andpalliative interventions simultaneously.Dr. von Gunten noted the growing accumulation<strong>of</strong> data during the past 20years demonstrating the effectiveness <strong>of</strong>palliative care.One recent study, for example, foundthat early palliative care significantly improvedquality <strong>of</strong> life and mood amongpatients with metastatic non–small celllung cancer as compared with standardcare (N. Engl. J. Med. 2010;363:733-42).Although significantly fewer patients inthe early palliative care group than in thestandard treatment group received aggressiveend-<strong>of</strong>-life care (33% vs. 54%),median survival was significantly longeramong patients receiving early palliativecare (11.6 months vs. 8.9 months).“Palliative care delivered by hospiceprograms in the [United States] is betterthan standard <strong>of</strong> care at the end <strong>of</strong> life,”Dr. von Gunten said. “That has beenproven. ... We should get rid <strong>of</strong> this language<strong>of</strong> ‘choice’: ‘Hospice is a choice ifyou want it; antibiotics are a choice ifyou want it; chemotherapy is a choice ifyou want it.’ We’re past that. This is thestandard <strong>of</strong> care, and it should be advocatedthat way by all <strong>of</strong> us.”But palliative care still has a way to gobefore it becomes an integral part <strong>of</strong> cancertreatment, although some progresshas been made, he said. According to arecent survey, 98% <strong>of</strong> NCI-designatedcancer centers and 78% <strong>of</strong> communitycancer centers report having palliativecare programs (JAMA 2010;303:1054-61).“This is huge progress from 10 yearsago, when they couldn’t even say theword,” Dr. von Gunten said. “However,in most <strong>of</strong> those places – 92% – it’s justone physician, <strong>of</strong>ten part-time.”More sobering, he said, is a 1998 membershipsurvey by the <strong>American</strong> Society<strong>of</strong> Clinical Oncologists in which 90% <strong>of</strong>oncologists reported “trial and error” astheir primary source <strong>of</strong> informationabout palliative care. “How enthusiasticwould you be about a doctor who wasgoing to take out your anus, and yousaid, ‘Doctor, how did you learn aboutthis?’ and he said, ‘Oh, trial and error,’ ”Dr. von Gunten said.Of those surveyed, 73% said theylearned from colleagues and role models.“That’s great, except where did colleaguesand role models learn? Trial anderror,” he said. And 38% <strong>of</strong> oncologistssaid the most significant source <strong>of</strong> theirinformation about palliative care was atraumatic experience. The underlyingmessage is that no one is teaching palliativecare to oncologists, he said.Dr. von Gunten had no disclosures. ■COMMENTARYDr. Paul Selecky, FCCP, comments:The New England Journal<strong>of</strong> Medicine study was ahallmark example <strong>of</strong> the potentialimpact <strong>of</strong> palliative care onhealth quality and quantity <strong>of</strong>life. Along that line, pulmonologistsshould provide a treatmentprogram for our patientswith progressive chronic lungdiseases (COPD, IPF) that includesthe specific treatment <strong>of</strong>dyspnea that persists despite appropriatetreatment <strong>of</strong> the disease.The ACCP ConsensusStatement on the management<strong>of</strong> dyspnea in advanced lungdisease can be found in <strong>Chest</strong>2010;137:674-91.
JANUARY 2011 • CHEST PHYSICIAN CARDIOTHORACIC SURGERY 7Respiratory Events a Risk After Bariatric SurgeryBY DIANA MAHONEYElsevier Global Medical NewsLAS VEGAS – Pulmonary complicationsfollowing bariatric surgery occurinfrequently but are associated with significantlyincreased rates <strong>of</strong> postoperativemorbidity and mortality, accordingto a large national study that also identifiedmodifiable preoperative risk factorsfor poor pulmonary outcomes.In an analysis <strong>of</strong> data from the <strong>American</strong><strong>College</strong> <strong>of</strong> Surgeons’ 2007 NationalSurgical Quality Improvement Program(NSQIP) – a prospective database comprisingmore than 200,000 inpatient andoutpatient operations done at 183 representativeU.S. hospitals – postoperativepneumonia and postoperative respiratoryfailure were the most common non–wound-related complications reportedamong 12,252 patients who underwentbariatric surgery, together accounting for26% <strong>of</strong> the overall 30-day morbidity rate,Dr. Prateek K. Gupta said at the annualmeeting <strong>of</strong> the <strong>American</strong> Society forMetabolic and Bariatric Surgery.“In comparison, renal complicationsand cardiac complications accounted for7% and 2%, respectively, <strong>of</strong> postoperativemorbidity,” he noted. The analysis includedpatients who underwent Rouxen-Ygastric bypass, adjustable gastricbanding, and gastroplasty.Specifically, postoperative pneumoniawas reported in 72 patients and postoperativerespiratory failure (defined asreintubation after extubation or a totalduration <strong>of</strong> ventilator-assisted respirationsfor a period <strong>of</strong> 48 hours) was reportedin 86 patients, said Dr. Gupta <strong>of</strong>Creighton University in Omaha, Neb.In patients with postoperative pneumonia,“2.78% died within 30 postoperativedays, compared with 0.17% <strong>of</strong>patients without pneumonia,” Dr. Guptasaid, and 10.47% <strong>of</strong> patients with respiratoryfailure died within 30 days, comparedwith 0.12% <strong>of</strong> patients withoutrespiratory failure.Patients with these pulmonary complicationsalso had significantly longerhospital stays. “The median length <strong>of</strong>stay for postoperative pneumonia patientswas 14 days, compared with2 days for patients without pneumonia,and a similar, significant trend was observedin patients with respiratory failure,”Dr. Gupta reported.In multivariate analyses, a history <strong>of</strong>heart failure was a major risk factor forpostoperative pneumonia, with an adjustedodds ratio <strong>of</strong> 10.7. “To ourknowledge, [heart failure] was not previouslyshown to be a risk factor forpneumonia,” he noted. “The associationcould be due to perioperative worsening<strong>of</strong> cardiopulmonary function,although the precise reasons are unclear.”Additional risk factors for postoperativepneumonia included history <strong>of</strong> strokewith neurologic deficit (OR, 9.8), consumption<strong>of</strong> more than two alcoholdrinks per day (OR, 9.0), history <strong>of</strong> severeCOPD (OR, 4.5), an open wound (OR,3.8), and higher <strong>American</strong> Society <strong>of</strong>Anesthesiologists Physical Status classification(OR, 2.0), Dr. Gupta said.With respect to postoperative respiratoryfailure, “patients with a history <strong>of</strong>myocardial infarction within 6 monthsprior to surgery had 50 times increasedrisk for this complication,” he said.Other preoperative risk factors for respiratoryfailure included receiving a preoperativetransfusion <strong>of</strong> more than fourunits <strong>of</strong> blood within 72 hours <strong>of</strong> surgery(OR, 19.0), consumption <strong>of</strong> more thantwo alcohol drinks per day (OR, 7.8), history<strong>of</strong> severe COPD (OR, 4.6), and hypertension(OR, 2.4), Dr. Gupta reported.Patients whose bariatric surgery wasdeemed “emergent” were six times morelikely to experience respiratory failurethan were those who had nonemergentprocedures, “but the nature <strong>of</strong> the emergencieswas unclear,” Dr. Gupta noted.Awareness <strong>of</strong> the preoperative risksthat might lead to pulmonary complicationsis important for patient optimizationand selection prior to surgery, Dr.Gupta stressed.The use <strong>of</strong> specific strategies to optimizemodifiable risk factors in bariatricpatients may help “control the incidence<strong>of</strong> postoperative pneumonia and respiratoryfailure, thereby improving surgicaloutcomes,” said Dr. Gupta, who reportedhaving no relevant disclosures. ■COMMENTARYDr. Jeana O’Brien, FCCP, comments:This report by Dr.Guptaprovidesinteresting,butnot surprising,informationabout anincreasedfrequency<strong>of</strong> pulmonary complications inbariatric surgery patients. Unfortunately,the NSQUIP databasedoes not include all theelements necessary to furtherascertain all important riskfactors. This information shouldalert bariatric specialists to theneed for frequent inclusion <strong>of</strong>pulmonologists in the preop aswell as postoperative care <strong>of</strong>these patients on a routine basis.Patients Met NETT CriteriaEmphysema • from page 1is the main factor contributingto its underuse. “Most pulmonologistsdo not support thisprocedure,” commented Dr.Ginsburg, who is associate director<strong>of</strong> the division <strong>of</strong> generaland thoracic surgery atColumbia University in NewYork. “We have some pulmonologistswho havehad great experiencesand continue to sendus patients, but I thinkthe vast number <strong>of</strong>pulmonologists do notsend patients.”His center has had amultidisciplinary LVRSteam for 15 years, henoted. Between January2004 and April 2009, theteam performed the surgery onpatients with emphysema whostrictly met the NETT inclusionand exclusion criteria, as well asall CMS selection requirements.Only patients falling intoNETT group 1 (upper lobe–predominant disease, low exercisecapacity) or group 2 (upperlobe–predominant disease, highexercise capacity) were included,he said. Patients with non–upper lobe–predominant disease(group 3 or group 4) or high-riskfeatures were excluded.On average, the 49 patientswere 63 years old and had anFEV 1 (forced expiratory volumein 1 second) <strong>of</strong> 25% <strong>of</strong> predicted,a carbon monoxide diffusingcapacity <strong>of</strong> 27% <strong>of</strong> predicted,and a maximal workload <strong>of</strong>37 watts. They were nearlyequally split between group 1and group 2.LVRS ‘can beperformed withvery low surgicalrisk, significantbenefit, and fairlypredictableresults.’DR. GINSBURGAll <strong>of</strong> the patients underwentbilateral LVRS. Twenty percenthad their surgery through a mediansternotomy, before 2005,when the center switched tovideo-assisted thoracic surgery.“We try to take out anywherefrom 30% to 40% <strong>of</strong> the lungvolume to really make room forthe remaining good lung to ventilate.… We have to be fairly aggressivewith this operation,” henoted. “The goal <strong>of</strong> lung reductionis really to allow the goodlung space to inhale and overcomethe inspiratory restraintthat exists in these patients.”None <strong>of</strong> the patients diedduring surgery, their hospitalstay, or the first 90 postoperativedays, Dr. Ginsburg reported.They had a median length <strong>of</strong>stay <strong>of</strong> 8 days. Most (92%) weredischarged to home, while therest were discharged to an inpatientrehabilitation facility.“Of note, 47% <strong>of</strong> our patientshad no major complications,”he commented. By far, the leadingmajor complication was aprolonged air leak (one lastingmore than a week), seen in43%. But these leaks were manageablemainly with Heimlichvalves that were removed atfollow-up <strong>of</strong>fice visits.“The air leak issue, eventhough it [is common] and certainlyleads to prolonged length<strong>of</strong> stay in these patients, I thinkclinically it’s not that big <strong>of</strong> anissue,” Dr. Ginsburg said.Among other complications,two patients had to be reintubatedand receive a tracheostomy,but both were weaned<strong>of</strong>f the ventilator and extubatedbefore discharge. Three patientsdeveloped pneumonia.“The survival after LVRS isexcellent,” with 1- and 3-year actuarialrates <strong>of</strong> 98% and 95%, respectively.“If you think aboutwhat you’d expect in actual survivalfor patients who have apreoperative FEV 1 <strong>of</strong> 25%, Ithink in and <strong>of</strong> themselves theseare fairly impressive numbers.”Among the 44 patients withfollow-up data, the BODE indexfell from 4.9 preoperatively to2.6 at 1 year (P less than .0001).“One <strong>of</strong> the criticisms <strong>of</strong> earlydata for lung reduction wasthat there was a significantamount <strong>of</strong> missing data, andmissing data skewed the resultsto benefit surgery,” Dr. Ginsburgcommented.Therefore, the analysis wasrepeated with imputation <strong>of</strong> theworst possible scores for thefive patients with missing data.The BODE index still fell significantly,from 4.9 to 3.0 (P lessthan .0001).On average, the reduction inthis index was greater amongCOMMENTARYgroup 1 patients than amongtheir group 2 counterparts (–2.9vs. –1.9; P less than .02).Patients also had significantimprovements in all four <strong>of</strong> theindividual components <strong>of</strong> theBODE index before imputation,and in two <strong>of</strong> the components(FEV 1 and dyspnea index) afterimputation <strong>of</strong> worst possiblevalues for the patients withmissing data.“LVRS now, in 2010, usingthe lessons from NETT, can beperformed with very low surgicalrisk, significant benefit, andfairly predictable results,” Dr.Ginsburg concluded.Dr. Ginsburg reported that heis a consultant for PneumRx. ■Dr. Richard Fischel, FCCP, comments: This article discussesa very interesting point. Despite a nationwide andvery expensive study sponsored by the NIH known as theNETT or national emphysema treatment trial whichshowed a signficant improvement in quality <strong>of</strong> life for patientsundergoing LVRS or lung volume reduction surgery,the procedure is infrequently performed.The results discussedfrom the Columbia University experience are excellentand consistent with those achieved at qualityprograms with appropriate patient selection worldwide.The reasons for low utilization <strong>of</strong> surgical LVRS are nodoubt multifactorial but, <strong>of</strong> course, are significantly influencedby the attitudes <strong>of</strong> pulmonologists in relation tothe procedure. I believe we should remain diligent in ourefforts to educate physicians and the public regarding therisks and the benefits <strong>of</strong> LVRS so that appropriate candidatescan be <strong>of</strong>fered an opportunity to achieve an improvedquality <strong>of</strong> life.
8 PULMONARY MEDICINE JANUARY 2011 • CHEST PHYSICIANSurvey Checks Temp <strong>of</strong> Flu Prevention EffortsExperts support nearly universalvaccination for 2010-2011 season.BY HEIDI SPLETEElsevier Global Medical NewsWASHINGTON – Of 400 U.S.physicians surveyed online, 95%said they have received flu vaccinationsfor the 2010-2011 fluseason or plan to do so, accordingto data collected by theNational Foundation for InfectiousDiseases.These results are encouraging,because they show thatmore physicians are practicingwhat they preach about flu vaccination,said Dr. WilliamSchaffner, president <strong>of</strong> theNFID, said at a press conferenceon influenza sponsoredby the foundation.“I am optimistic that we arebecoming a culture <strong>of</strong> prevention,”Dr. Schaffner said.“Plenty <strong>of</strong> flu vaccine is anticipatedfor this year,” alongwith a plentiful supply <strong>of</strong> antiviralmedication, he emphasized,and vaccines are availableat pharmacies as well as doctors’<strong>of</strong>fices.“Flu vaccination is the bestway to protect yourself againstthe flu,” said Dr. ThomasBY BRUCE JANCINElsevier Global Medical NewsVAIL, COLO. – Acceptance <strong>of</strong> the pandemic2009 H1N1 influenza vaccine byU.S. health care workers was, in a word,“terrible,” Dr. Adriana Weinberg declared.A mere 37% <strong>of</strong> physicians and otherhealth care workers were vaccinatedagainst the pandemic virus, Dr. Weinbergreported at the annual conferenceon pediatric infectious diseases sponsoredby the Children’s Hospital, Denver.Uptake <strong>of</strong> the vaccine by two notablyhigh-risk patient groups – pregnantwomen, and children and adolescentsaged 6 months to 17 years – was equallypoor at 38% and 37%, respectively, saidDr. Weinberg, pr<strong>of</strong>essor <strong>of</strong> medicine,pediatrics, and pathology, and medical director<strong>of</strong> the clinical virology laboratoryat the University <strong>of</strong> Colorado Hospital,also in Denver. These data were providedto the National Vaccine Advisory Committeeby the Centers for Disease Controland Prevention.Among parents and other careproviders for infants less than 6 months<strong>of</strong> age, vaccine acceptance was evenworse at 14%.Moreover, only 25% <strong>of</strong> adults aged24-64 years with immunosuppression orother chronic medical conditions placingthem at elevated risk for increased flumorbidity got vaccinated. That wasFrieden, director <strong>of</strong> the Centersfor Disease Control and Prevention.Every year thousands<strong>of</strong> <strong>American</strong>s die from influenza,he said.For the 2010-2011 flu season,the CDC recommends universalvaccination for everyoneaged 6 months and older.Several vaccination optionsare available, including a flushot, a nasal spray, and a highdosevaccine for older adults,Dr. Frieden said.Dr. Daniel Jernigan, deputydirector <strong>of</strong> the influenza divisionin the CDC’s National Centerfor Immunization andRespiratory Diseases, said thatthis year’s vaccine contains antibodiesagainst three flu viruses:influenza B, influenza A(H3N2), and influenza A(H1N1).Approximately 119 milliondoses <strong>of</strong> 2010-2011 flu vaccinealready have been distributed inthe United States, with a total <strong>of</strong>160 million doses anticipated,Dr. Jernigan said.There is no need for a separateH1N1 vaccine this year, henoted.essentially the same rate as in the overallU.S. population, including bothhigh-priority and non–high-priorityindividuals.As a result <strong>of</strong> this low uptake, manymillions <strong>of</strong> soon-to-expire doses <strong>of</strong> pandemic2009 H1N1 influenza monovalentvaccine are being destroyed.In several studies, the main reasoncited by health care workers and pregnantwomen for not accepting the vaccinewas fear <strong>of</strong> side effects, especiallyGuillain-Barré syndrome, which was anissue with the 1976 swine flu vaccine.The safety concerns proved baseless thistime around, as evidenced by consistentlyreassuring findings from threeseparate sources: the Vaccine SafetyDatalink, the Vaccine Adverse Event ReportingSystem, and the Emerging InfectionsProgram.For example, there were no deaths andno cases <strong>of</strong> Guillain-Barré syndromeamong recipients <strong>of</strong> 438,376 doses <strong>of</strong> thevaccine in managed care organizationsApproximately 119 million doses <strong>of</strong> 2010-2011 flu vaccinealready have been distributed, Dr. Daniel Jernigan said.So far this year, the H3N2virus has been the most commonlyseen, Dr. Jernigan said.While children were disproportionatelyaffected by the 2009H1N1 virus, “when H3N2 isdominant, we see more illnessin children and older adults,”he said.Another important reason tovaccinate children is that theyare incredibly efficient atspreading the flu – to theirpeers, family members, andother close contacts, said Dr.Judith S. Palfrey, past president<strong>of</strong> the <strong>American</strong> Academy <strong>of</strong>Pediatrics.Dr. Palfrey said that childrenunder 9 years <strong>of</strong> age who havenever been vaccinated againstthe flu should receive two dosesthis year, given at about fourweeks apart. One dose is sufficientfor previously vaccinatedchildren, she said. A completealgorithm for childhood vaccinationis available at the <strong>American</strong>Academy <strong>of</strong> Pediatrics Website.More information about thisyear’s influenza vaccine is availableat the CDC’s flu Web sitecdc.gov/flu.Although influenza vaccinationis recommended for mostparticipating in the VaccineSafety Datalink. And duringsurveillance for Guillain-Barrésyndrome conducted throughthe Emerging Infections Program,the rate <strong>of</strong> cases was1.92/100,000 person-yearsamong vaccine recipients, comparedwith 1.21/100,000 personyearsamong nonrecipients.That 0.7/100,000 person-years excess <strong>of</strong>Guillain-Barré syndrome associated withthe pandemic H1N1 vaccine is similar tothat associated with the seasonal influenzavaccine, according to Dr. Weinberg.One audience member said the reasona lot more families in his practice didn’t getvaccinated against H1N1 wasn’t fear <strong>of</strong>side effects; it was that he and other <strong>of</strong>ficebasedphysicians in his community didn’tget shipments <strong>of</strong> the vaccine until after thesecond and as it turned out, final, wave <strong>of</strong>the 2009 pandemic had passed.Dr. Weinberg agreed that lack <strong>of</strong>timely vaccine availability caused by longdelays in the cumbersome manufacturingprocess was a huge problem. A potentialsolution would be to produce influenzavaccines in cell culture instead <strong>of</strong> eggs,something the Food and Drug Administrationis very reluctant to allow, althoughone such flu vaccine was recently approvedin Europe. Another answer wouldbe to identify common epitopes that confercross-strain protection against allHEIDI SPLETE/ELSEVIER GLOBAL MEDICAL NEWSindividuals, some people shouldnot receive the flu vaccine.According to the CDC, individualswho are allergic to eggsor who have had a history <strong>of</strong>severe reaction to an influenzavaccination should not bevaccinated, nor should anyonewho has developed Guillian-Barré syndrome within 6 weeksafter receiving an influenzavaccine.Those with a moderate to severeillness that includes a fevershould wait until they recoverbefore getting vaccinated.And children younger than 6months <strong>of</strong> age should not receiveany type <strong>of</strong> flu vaccine.The press conference wassponsored by the NationalFoundation for Infectious Diseasesin partnership with theNational Influenza VaccineSummit.The press conference wasalso supported in part by theCenters for Disease Controland Prevention and by unrestrictededucational grants tothe NFID from Flu VaccineBusiness Practices Initiative(c/o HIDA), Genentech, Glaxo-SmithKline, MedImmune,Merck and Co., Novartis Vaccines,Pfizer, San<strong>of</strong>i Pasteur,and Walgreens.■Most Health Care Workers Skipped 2009 H1N1 VaccineVITALSMajor Finding: Only 37% <strong>of</strong> physicians andother health care workers were vaccinatedagainst the pandemic virus.Data Source: CDC data provided to theNational Vaccine Advisory Committee.Disclosures: Dr. Weinberg disclosed servingas a consultant to MedImmune, Astellas,GlaxoSmithKline, and Merck.influenza strains, so a new vaccinewouldn’t have to be created in advance<strong>of</strong> every flu season.“There has been a big push on this.There are some good candidate epitopesemerging in the last year. We shall see,”the virologist said.The vaccine being manufactured forthe coming 2010-2011 flu season containsantigens for a pandemic 2009 H1N1 influenzavirus as well as a seasonalinfluenza A H3N2 Perth 2009 virus andan influenza B Brisbane 2008 virus. Theimmunization schedule recommendedby the CDC calls for a single dose <strong>of</strong> thevaccine for adults and children olderthan age 10 years. Children aged6 months to 9 years are to receive twodoses 21 days apart unless they are in theminority who received the pandemicH1N1 monovalent vaccine last season, inwhich case they are to get a single dose<strong>of</strong> the trivalent vaccine. Despite this recommendation,a recent randomized controlledtrial concluded that a single dosemay be sufficiently immunogenic inyoung children (JAMA 2010;303:37-46).“We do anticipate circulation <strong>of</strong> thepandemic H1N1 strain in the next flu season,but I have to caution you that in theSouthern Hemisphere, where influenzaseason is going on right now, there isvery, very little pandemic H1N1. Whatpredominates are the A H3N2 and the BBrisbane,” she said.■Pages 8a—8f
JANUARY 2011 • CHEST PHYSICIAN PULMONARY MEDICINE 9Surgeon General: Even One Cigarette Is HarmfulBY ALICIA AULTElsevier Global Medical NewsWASHINGTON – For the first time, there is evidence<strong>of</strong> immediate and direct harm done by smoking evenone cigarette, according to the 30th annual U.S. SurgeonGeneral’s Office report on smoking.Surgeon General Regina M. Benjamin said at a pressbriefing that previous reports from her <strong>of</strong>fice honed inon the various diseases that smoking could cause.“This report focuses on how tobacco smoke causesdamage to every organ in your body,” she said.When asked why this report could make a differencewhen so many previous warnings have not convincedall <strong>American</strong>s to quit smoking, Dr. Benjamin said thatshe thinks that the direct evidence <strong>of</strong> harm will personalizethe message.The 700-page “Report <strong>of</strong> the Surgeon General: HowTobacco Smoke Causes Disease: The Biology and BehavioralBasis for Smoking-Attributable Disease” determinedthat tobacco smoke contains 7,000 chemicals,hundreds <strong>of</strong> which are known to be toxic and 70 <strong>of</strong>which are carcinogenic, she noted.The report describes multiple insults to the body fromthose chemicals, including changes in DNA that can leadto cancer; damage to the lining <strong>of</strong> the lungs; obstructivepulmonary disease and bronchitis; stress on the vasculatureand cardiovascular disease; and an increased risk<strong>of</strong> heart attack, stroke, and aortic aneurysm.Smoking also interferes with the effectiveness <strong>of</strong>chemotherapy and the control <strong>of</strong> blood sugar andleads to fertility problems, including difficulty conceiving,miscarriage, and preterm birth. Just onecigarette can trigger a heart attack or stroke, she said.In addition, the report examined the effects <strong>of</strong> secondhandsmoke, finding that even brief exposure cancause cardiovascular disease and can also trigger acutecardiac events, such as heart attack. Babies exposed tosecondhand smoke are more likely to die <strong>of</strong> suddeninfant death syndrome.The report highlights the increasingly addictive properties<strong>of</strong> today’s cigarettes, many <strong>of</strong> which are designedto enhance nicotine absorption and its crossing <strong>of</strong> theblood-brain barrier, Dr. Benjamin said.Department <strong>of</strong> Health and Human Services SecretaryKathleen Sebelius said at the briefing that the reportshows that “there is no safe level <strong>of</strong> exposure totobacco smoke,” and, she added, “if you’re a smoker,the best time to quit is right now.”John R. Seffrin, Ph.D., CEO <strong>of</strong> the <strong>American</strong> CancerSociety Cancer Action Network, agreed. “Today’sreport makes it clear, once again, that there is no suchthing as a safe cigarette and no such thing as a safe level<strong>of</strong> exposure to secondhand smoke for nonsmokers,”he said in a statement.Ms. Sebelius noted that, every day, 4,000 <strong>American</strong>sunder 18 years old try their first cigarette, and 1,000 becomedaily smokers. Some 1,200 <strong>American</strong>s die everyday as a result <strong>of</strong> tobacco-related causes, she said, andthe report is part <strong>of</strong> the Obama administration’s ongoingstrategy to completely eliminate tobacco use.The Surgeon General’s report is available atwww.surgeongeneral.gov. The <strong>of</strong>fice has also createda consumer-friendly version <strong>of</strong> the report and a printable,one-page fact sheet for physicians to use in discussingthe report with their patients.■COMMENTARYDr. Philip Marcus, FCCP, comments: In 1964,the first Surgeon General’s report on the effects<strong>of</strong> smoking on health wasreleased. In the next 46years, extensive data fromthousands <strong>of</strong> studies haveconsistently substantiatedthe devastating effects <strong>of</strong>smoking on the lives <strong>of</strong>millions <strong>of</strong> <strong>American</strong>sand others around theworld. Yet today in theUnited States, tobacco use remains the singlelargest preventable cause <strong>of</strong> death and diseasefor both men and women.Now, this 2010 report <strong>of</strong> the Surgeon Generalexplains beyond a shadow <strong>of</strong> a doubt howtobacco smoke causes disease, essentially validatingearlier findings, and expands andstrengthens the science behind these findings.Armed with this irrefutable data, the time hascome to mount a full-scale assault on thetobacco epidemic.More than 1,000 people are killed every dayby cigarettes, and one-half <strong>of</strong> all long-termsmokers are killed by smoking-related diseases.This report should lay the issue to restat this time, and hopefully there can be a truereduction in cigarette smoking and a concomitantend to the epidemic <strong>of</strong> smokingrelatedillnesses.observed in an additional 22 patients 12 to 17 years <strong>of</strong> age who were treated withDULERA in another clinical trial. The safety and efficacy <strong>of</strong> DULERA have not beenestablished in children less than 12 years <strong>of</strong> age.Controlled clinical studies have shown that inhaled corticosteroids maycause a reduction in growth velocity in pediatric patients. In these studies, themean reduction in growth velocity was approximately 1 cm per year (range 0.3to 1.8 per year) and appears to depend upon dose and duration <strong>of</strong> exposure.This effect was observed in the absence <strong>of</strong> laboratory evidence <strong>of</strong> hypothalamicpituitary-adrenal(HPA) axis suppression, suggesting that growth velocity is a moresensitive indicator <strong>of</strong> systemic corticosteroid exposure in pediatric patients thansome commonly used tests <strong>of</strong> HPA axis function. The long-term effects <strong>of</strong> thisreduction in growth velocity associated with orally inhaled corticosteroids, includingthe impact on final adult height, are unknown. The potential for “catch up” growthfollowing discontinuation <strong>of</strong> treatment with orally inhaled corticosteroids has notbeen adequately studied.The growth <strong>of</strong> children and adolescents receiving orally inhaledcorticosteroids, including DULERA, should be monitored routinely (e.g., viastadiometry). If a child or adolescent on any corticosteroid appears to have growthsuppression, the possibility that he/she is particularly sensitive to this effect shouldbe considered. The potential growth effects <strong>of</strong> prolonged treatment should beweighed against clinical benefits obtained and the risks associated with alternativetherapies. To minimize the systemic effects <strong>of</strong> orally inhaled corticosteroids,including DULERA, each patient should be titrated to his/her lowest effective dose[see Dosage and Administration (2.2)].8.5 Geriatric UseA total <strong>of</strong> 77 patients 65 years <strong>of</strong> age and older (<strong>of</strong> which 11 were 75 yearsand older) have been treated with DULERA in 3 clinical trials up to 52 weeks induration. Similar efficacy and safety results were observed in an additional 28patients 65 years <strong>of</strong> age and older who were treated with DULERA in anotherclinical trial. No overall differences in safety or effectiveness were observedbetween these patients and younger patients, but greater sensitivity <strong>of</strong> some olderindividuals cannot be ruled out. As with other products containing beta 2 -agonists,special caution should be observed when using DULERA in geriatric patients whohave concomitant cardiovascular disease that could be adversely affected bybeta 2-agonists. Based on available data for DULERA or its active components, noadjustment <strong>of</strong> dosage <strong>of</strong> DULERA in geriatric patients is warranted.8.6 Hepatic ImpairmentConcentrations <strong>of</strong> mometasone furoate appear to increase with severity <strong>of</strong>hepatic impairment [see Clinical Pharmacology (12.3)].10 OVERDOSAGE10.1 Signs and SymptomsDULERA: DULERA contains both mometasone furoate and formoterolfumarate; therefore, the risks associated with overdosage for the individualcomponents described below apply to DULERA.Mometasone Furoate: Chronic overdosage may result in signs/symptoms<strong>of</strong> hypercorticism [see Warnings and Precautions (5.7)]. Single oral doses up to8000 mcg <strong>of</strong> mometasone furoate have been studied on human volunteers withno adverse reactions reported.Formoterol Fumarate: The expected signs and symptoms with overdosage<strong>of</strong> formoterol are those <strong>of</strong> excessive beta-adrenergic stimulation and/or occurrenceor exaggeration <strong>of</strong> any <strong>of</strong> the following signs and symptoms: angina, hypertensionor hypotension, tachycardia, with rates up to 200 beats/min., arrhythmias,nervousness, headache, tremor, seizures, muscle cramps, dry mouth, palpitation,nausea, dizziness, fatigue, malaise, hypokalemia, hyperglycemia, and insomnia.Metabolic acidosis may also occur. Cardiac arrest and even death may beassociated with an overdose <strong>of</strong> formoterol.The minimum acute lethal inhalation dose <strong>of</strong> formoterol fumarate in ratsis 156 mg/kg (approximately 63,000 times the MRHD on a mcg/m 2 basis). Themedian lethal oral doses in Chinese hamsters, rats, and mice provide even highermultiples <strong>of</strong> the MRHD.10.2 TreatmentDULERA: Treatment <strong>of</strong> overdosage consists <strong>of</strong> discontinuation <strong>of</strong> DULERAtogether with institution <strong>of</strong> appropriate symptomatic and/or supportive therapy. Thejudicious use <strong>of</strong> a cardioselective beta-receptor blocker may be considered, bearingin mind that such medication can produce bronchospasm. There is insufficientevidence to determine if dialysis is beneficial for overdosage <strong>of</strong> DULERA. Cardiacmonitoring is recommended in cases <strong>of</strong> overdosage.Manufactured by 3M Health Care Ltd.,Loughborough, United Kingdom.Manufactured for Schering Corporation, a subsidiary <strong>of</strong>Whitehouse Station, NJ 08889 USA.Copyright © 2010 Schering Corporation, a subsidiary <strong>of</strong> Merck & Co., Inc.All rights reserved. U.S. Patent Nos. 5889015; 6057307; 6677323; 6068832;7067502; and 7566705. The trademarks depicted in this piece are owned bytheir respective companies.6/10 32704107T-JBS
10 PEDIATRIC CHEST MEDICINE JANUARY 2011 • CHEST PHYSICIANH1N1 Isn’t OverThreat • from page 1least 90% <strong>of</strong> the population were vaccinated, herd immunitywould protect even those people who can’t bevaccinated, such as infants under 6 months <strong>of</strong> age andothers with contraindications, Dr.Harrison said.Given last year’s experience,that’s not likely to happen. U.S.health <strong>of</strong>ficials hoped to haveenough antigen for 229 milliondoses. In the end, only 162 milliondoses were produced, anddespite widespread publicityabout the danger <strong>of</strong> H1N1, only94 million doses were used, hesaid. “Everyone wanted the vaccine in August, and noone wanted it in December.”The reason the pandemic didn’t kill as many peopleas feared may have been that elderly people, normallythe most at risk, had some residual immunity from aswine flu outbreak in the 1960s and a vaccine used atthat time, Dr. Harrison said.Vaccination <strong>of</strong> children is particularly important becauseso many attend schools and day care facilities,where they play a key role in spreading the virus. Veryyoung children are particularly vulnerable, with hospitalizationrates comparable to those <strong>of</strong> the elderly.While results from studies have varied, combiningBY ROBERT FINNElsevier Global Medical NewsThe Advisory Committee on ImmunizationPractices voted to recommendthat a seasonal influenza vaccinemanufactured by CSL Biotherapies forthe U.S. market not be used in children betweenthe ages <strong>of</strong> 6 months and 8 years.The company’s trivalent influenza vaccine(TIV) sold under the trade nameAfluria in the United States was associatedwith a large increase in the risk <strong>of</strong>fevers and febrile seizures in children inAustralia and New Zealand. In April2010, authorities in those two countriesrecommended that physicians suspenduse <strong>of</strong> CSL’s influenza vaccines in childrenaged 5 years and under. In response,the company voluntarily withdrew itsvaccine from markets in the southernhemisphere.In the northern hemisphere, CSL’s influenzavaccines have been approved foruse in Germany, the United Kingdom,and the United States. In June 2010, authoritiesin the United Kingdom recommendedthat physicians avoid usingCSL’s influenza vaccine in children aged5 and under.In making their recommendation,members <strong>of</strong> the Centers for DiseaseControl and Prevention’s Advisorytheir data suggests the vaccine confers about a 68% immunityrate in children, Dr. Harrison said.The vaccine is available in two forms: trivalent, inactivatedinfluenza vaccine (TIV) and live, attenuated influenzavaccine (LAIV). The TIV vaccine is anintramuscular injection <strong>of</strong> killed viruses. It can be givento anyone over 6 months <strong>of</strong> age who is not allergic‘Maybe [H1N1influenza] didn’tkill as manyadults, butchildren weredisproportionatelyaffected.’DR. HARRISONto the vaccine. Egg allergies are nolonger considered an absolute contraindication,Dr. Harrison said,but the vaccine should be given topeople with egg allergies only if anallergist is present. “I don’t knowhow practical that is,” he said.LAIV is administered via an intranasalspray. Most people aged2-49 years can get the vaccine thisway, with the exception <strong>of</strong> childrenunder 5 years <strong>of</strong> age with reactive airways diseasessuch as asthma, anyone with a high-risk medical condition,and pregnant women.Unlike last year, when two vaccineswere <strong>of</strong>fered, one for seasonal flu andone for H1N1, this year one vaccinewill protect against three strains: A/California/7/2009 (H1N1),which caused last season’s pandemic. B/Brisbane/60/2008, the same seasonalstrain from last season, which isalready prevalent in the SouthernHemisphere.Committee on Immunization Practices(ACIP) noted that there should be adequatesupplies <strong>of</strong> seasonal influenza vaccineeven in the absence <strong>of</strong> Afluria.Other manufacturers are expected tosupply 145-150 million doses <strong>of</strong> the vaccinein the United States; the largestnumber <strong>of</strong> doses ever used in one fluseason was 114 million.During the course <strong>of</strong> a teleconferencesponsored by ACIP, representatives<strong>of</strong> San<strong>of</strong>i-Aventis, GlaxoSmithKline, Novartis,and MedImmune all said thatthey had adequate supplies <strong>of</strong> vaccine,and they were willing to increase productionif necessary to compensate forthe 6-12 million doses that CSL hadbeen expected to provide.According to the CDC’s medical epidemiologistDr. Tim Uyeki, CSL’s vaccinewas associated with a ninefoldincrease in the risk <strong>of</strong> febrile seizures,compared with other manufacturers’vaccines in children aged 6 monthsthrough 4 years in Australia. The ratewas nine per 1,000 doses in these children,compared with an expected rate <strong>of</strong>one per 1,000 doses. The rate <strong>of</strong> febrileseizures was especially high in childrenaged 3-4 years given Fluvax Junior, one<strong>of</strong> CSL’s two versions <strong>of</strong> this year’s TIV.The rate in those children was 15 per1,000 doses.Febrile seizures occurred an average <strong>of</strong>7.2 hours after the child received a dose<strong>of</strong> vaccine, with a range <strong>of</strong> 5.9-8.4 hours.Dr. Uyeki said that no explanation for theincreased risk <strong>of</strong> fever and febrile seizureshas been identified.Although there was no apparent increasein febrile seizures in children aged5-8 years, children in that age group didexperience an increase in the incidence <strong>of</strong>fever. Sixteen percent <strong>of</strong> children in thatCOMMENTARY A/Perth/16/2009 (H3N1), a new strain already detectedin Iowa.Most children aged 6 months to 8 years should receivetwo doses <strong>of</strong> the vaccine, Dr. Harrison said. Childrenwho received one or two H1N1 2009 pandemic vaccinationsin 2009-2010 and two doses <strong>of</strong> seasonal vaccine,or who were vaccinated prior to 2009-2010 and also gotat least one H1N1 2009 pandemic dose in 2009-2010,need only one vaccination this season, according to theCenters for Disease Control and Prevention guidelines.For those children who do get influenza, antiviraldrugs are available. The 2009 H1N1 pandemic strain andH3N2 are almost completely resistant to adamantanes,but have little or no resistance to oseltamivir or zanamivir.When commercially manufactured TamifluOral Suspension (12 mg/mL) is not available, it ispossible to compound Tamiflu (oseltamivir) 75-mgcapsules to suspension for children. Instructionsare available on the Food and Drug AdministrationWeb site at www.fda.gov/downloads/drugs/drugsafety/informationbydrugclass/Dr. Burt Lesnick, FCCP, comments:At press time, my homestate <strong>of</strong> Georgia is the only statewith epidemic influenza, althoughit is mainly influenzaB. Clinicians are advised to keepabreast <strong>of</strong> their local virologyand respond accordingly.age group experienced a fever followinga dose <strong>of</strong> a CSL flu vaccine, comparedwith 9% <strong>of</strong> children receiving anothermanufacturer’s vaccine.ACIP members voted to include childrenaged 5-8 years in their recommendationin order to increase the simplicityand consistency <strong>of</strong> the public healthmessage. Other ACIP recommendationsregarding flu vaccination in children,both for the seasonal TIV and for pandemicinfluenza A(H1N1), involve childrenage 6 months to 8 years, and mostmembers believed it would be confusingto have this new recommendationcover children age 6 months to 5 years.They did agree, however, that childrenaged 5-8 years could receive the CSLvaccine if they were at especially highrisk from influenza and if no other vaccinewas available.ucm147992.pdf.How do physicians knowwhen to use an antiviral?Rapid tests for H1N1 workthis season – unlike last season,Dr. Harrison said.Dr. Harrison disclosed a financialrelationship withGlaxoSmithKlineGroup.Avoid Afluria Flu Vaccine in Children Under 9 YearsCHILDREN AGED 5-8 YEARS CANRECEIVE THE CSL VACCINE IFTHEY ARE AT ESPECIALLY HIGHRISK FROM INFLUENZA AND NOOTHER VACCINE IS AVAILABLE.Vaccine■Several committee members voicedconcern about providers who may alreadyhave placed orders for the CSL vaccine.Since most vaccine from othermanufacturers has already been allocated,they worried that it would be toolate for some clinicians to change theirorders. In response, a representative fromthe <strong>American</strong> Medical Association recommendedthat providers visit theAMA’s Influenza Vaccine AvailabilityTracking System (IVATS) at www.preventinfluenza.org/ivats. A spreadsheetat that site lists names and contactinformation for distributors who havevaccine available.While several members <strong>of</strong> ACIP disclosedthat they had relationships withvaccine manufacturers, only memberswith no such conflicts <strong>of</strong> interest werepermitted to vote.■D A T A W A T C HWorld H1N1 Flu Vaccine Sales, 2009(in millions/market share)Pandemrix(GlaxoSmithKline) $1,190 / 35%Focetria (Novartis)Humenza (San<strong>of</strong>i Pasteur)MedImmune H1N1 Intranasal(Astra Zeneca)Panvax H1N1 (CSL)Celvapan H1N1 (Baxter)Other$160 / 5%$50* / 1.5%$50* / 1.5%$365 / 11%$620 / 18%$950 / 28%*EstimatedNote: Based on annual reports <strong>of</strong> vaccine concerns, trade media coverage, companyWeb sites, and medical and government literature.Source: Kalorama InformationELSEVIER GLOBAL MEDICAL NEWS
Did you knowREVATIO samples arejust a phone call away?Order REVATIO StarterSamples by phoneContact the REVATIO Sample FulfillmentProgram by calling 1-866-833-9559IndicationREVATIO is indicated for the treatment <strong>of</strong> pulmonary arterial hypertension(WHO Group I) to improve exercise ability and delay clinical worsening.Delay in clinical worsening was demonstrated when REVATIO was addedto background epoprostenol therapy. The efficacy <strong>of</strong> REVATIO has notbeen adequately evaluated in patients taking bosentan concurrently.Important Safety InformationDo not use REVATIO in patients taking organic nitrates in any form, eitherregularly or intermittently. Consistent with its known effects on the nitricoxide/cGMP pathway, sildenafil was shown to potentiate the hypotensiveeffects <strong>of</strong> nitrates.Before starting REVATIO, physicians should carefully consider whethertheir patients with underlying conditions could be adversely affected bythe mild and transient vasodilatory effects <strong>of</strong> REVATIO on blood pressure.Pulmonary vasodilators may significantly worsen the cardiovascularstatus <strong>of</strong> patients with pulmonary veno-occlusive disease (PVOD) andadministration <strong>of</strong> REVATIO to these patients is not recommended. Shouldsigns <strong>of</strong> pulmonary edema occur when sildenafil is administered, thepossibility <strong>of</strong> associated PVOD should be considered.Caution is advised when PDE5 inhibitors, such as REVATIO, areadministered with α-blockers as both are vasodilators with bloodpressure lowering effects.In PAH patients, the concomitant use <strong>of</strong> vitamin K antagonists andREVATIO resulted in a greater incidence <strong>of</strong> reports <strong>of</strong> bleeding (primarilyepistaxis) versus placebo. The incidence <strong>of</strong> epistaxis was higher inpatients with PAH secondary to CTD (sildenafil 13%, placebo 0%) thanin PPH patients (sildenafil 3%, placebo 2%).Co-administration <strong>of</strong> REVATIO with potent CYP3A4 inhibitors, eg,ketoconazole, itraconazole, and ritonavir, is not recommended as serumconcentrations <strong>of</strong> sildenafil substantially increase. Co-administration <strong>of</strong>REVATIO with CYP3A4 inducers, including bosentan; and more potentinducers such as barbiturates, carbamazepine, phenytoin, efavirenz,nevirapine, rifampin, and rifabutin, may alter plasma levels <strong>of</strong> eitheror both medications. Dosage adjustment may be necessary.Non-arteritic anterior ischemic optic neuropathy (NAION) has beenreported post-marketing in temporal association with the use <strong>of</strong> PDE5inhibitors for the treatment <strong>of</strong> erectile dysfunction, including sildenafil.It is not possible to determine if these events are related to PDE5inhibitors or to other factors. <strong>Physicians</strong> should advise patients to seekimmediate medical attention in the event <strong>of</strong> sudden loss <strong>of</strong> vision whiletaking PDE5 inhibitors, including REVATIO.Sudden decrease or loss <strong>of</strong> hearing has been reported in temporalassociation with the intake <strong>of</strong> PDE5 inhibitors, including REVATIO. It is notpossible to determine whether these events are related directly to the use<strong>of</strong> PDE5 inhibitors or to other factors. <strong>Physicians</strong> should advise patients toseek prompt medical attention in the event <strong>of</strong> sudden decrease or loss <strong>of</strong>hearing while taking PDE5 inhibitors, including REVATIO.REVATIO should be used with caution in patients with anatomicaldeformation <strong>of</strong> the penis or patients who have conditions which maypredispose them to priapism.REVATIO contains sildenafil, the same active ingredient found inVIAGRA ® . Combinations <strong>of</strong> REVATIO with VIAGRA or other PDE5inhibitors have not been studied. Patients taking REVATIO should nottake VIAGRA or other PDE5 inhibitors.Patients with the following characteristics did not participate in thepreapproval clinical trial: patients who have suffered a myocardialinfarction, stroke, or life-threatening arrhythmia within the last 6 months,unstable angina, hypertension (BP >170/110), retinitis pigmentosa, orpatients on bosentan. The safety <strong>of</strong> REVATIO is unknown in patients withbleeding disorders and patients with active peptic ulceration. In thesepatients, physicians should prescribe REVATIO with caution.The most common side effects <strong>of</strong> REVATIO (placebo-subtracted) wereepistaxis (8%), headache (7%), dyspepsia (6%), flushing (6%), andinsomnia (6%). Adverse events <strong>of</strong> REVATIO injection were similar to thoseseen with oral tablets.The most common side effects <strong>of</strong> REVATIO (placebo-subtracted) as anadjunct to intravenous epoprostenol were headache (23%), edema (14%),dyspepsia (14%), pain in extremity (11%), diarrhea (7%), nausea (7%), andnasal congestion (7%).Please see Brief Summary <strong>of</strong> Prescribing Information on the following pages.www.REVATIO.comRVU00163B ©2010 Pfizer Inc All rights reserved. Printed in USA/February 2010
12 PEDIATRIC CHEST MEDICINE JANUARY 2011 • CHEST PHYSICIANLive, Inactivated Flu Vaccines Equally Cost EffectiveBY MARY ANN MOONElsevier Global Medical NewsDespite recent reports that the intranasallive attenuated influenzavaccine might cause more adverseevents in young children than does theinactivated influenza vaccine, the costeffectiveness<strong>of</strong> the two approaches remainscomparable, according to a recentstudy.In a mathematical simulation model,both the live attenuated vaccine and theinactivated vaccine yielded similar costeffectivenessratios <strong>of</strong> less than $40,000per quality-adjusted life year (QALY)among children under 5 years, whichcompares well with other well-acceptedpediatric interventions, said Lisa A. Prosser,Ph.D., <strong>of</strong> the University <strong>of</strong> MichiganHealth System, Ann Arbor, and her associates(Arch. Pediatr. Adolesc. Med. 2010[doi:10.1001/archpediatrics.2010.182]).The investigators assessed the costeffectiveness<strong>of</strong> each <strong>of</strong> the vaccines and<strong>of</strong> no vaccination using a mathematicalsimulation model that estimated the effectson influenza-related health outcomesin a hypothetical cohort <strong>of</strong> healthychildren aged 6 months to 4 years.The live attenuated vaccine was projectedto avert more influenza episodes,influenza-related hospitalizations, anddeaths than was the inactivated vaccine.However, this benefit was somewhatcounterbalanced by an increase in adverseevents with the live attenuated vaccine.Under different conditions, the modelshowed that cost-effectiveness ratiosranged from $20,000/QALY to $33,000/QALY with the live attenuated vaccineand $21,000/QALY to $37,000/QALYwith the inactivated vaccine.This study was funded by the Centersfor Disease Control and Preventionthrough the Harvard/CDC Joint Initiativein Vaccine Economics. No financialconflicts <strong>of</strong> interest were reported. ■REVATIO ® (SILDENAFIL)Brief Summary <strong>of</strong> Prescribing InformationINDICATIONS AND USAGE: REVATIO ® is indicated for the treatment <strong>of</strong> pulmonary arterialhypertension (WHO Group I) to improve exercise ability and delay clinical worsening. Thedelay in clinical worsening was demonstrated when REVATIO was added to backgroundepoprostenol therapy.Limitation <strong>of</strong> UseThe efficacy <strong>of</strong> REVATIO has not been adequately evaluated in patients taking bosentan concurrently.DOSAGE AND ADMINISTRATIONPulmonary Arterial Hypertension (PAH)REVATIO TabletsThe recommended dose <strong>of</strong> REVATIO is 20 mg three times a day (TID). REVATIO tabletsshould be taken approximately 4-6 hours apart, with or without food.In the clinical trial no greater efficacy was achieved with the use <strong>of</strong> higher doses.Treatment with doses higher than 20 mg TID is not recommended. Dosages lowerthan 20 mg TID were not tested. Whether dosages lower than 20 mg TID are effectiveis not known.REVATIO InjectionREVATIO injection is for the continued treatment <strong>of</strong> patients with pulmonary arterialhypertension (PAH) who are currently prescribed oral REVATIO and who are temporarilyunable to take oral medication.The recommended dose is 10 mg (corresponding to 12.5 mL) administered as anintravenous bolus injection three times a day. The dose <strong>of</strong> REVATIO injection does not needto be adjusted for body weight.A 10 mg dose <strong>of</strong> REVATIO injection is predicted to provide pharmacological effect <strong>of</strong>sildenafil and its N-desmethyl metabolite equivalent to that <strong>of</strong> a 20 mg oral dose.CONTRAINDICATIONSUse with Organic NitratesDo not use REVATIO in patients taking organic nitrates in any form, either regularly orintermittently. Consistent with its known effects on the nitric oxide/cGMP pathway,sildenafil was shown to potentiate the hypotensive effects <strong>of</strong> nitrates.Hypersensitivity ReactionsREVATIO is contraindicated in patients with a known hypersensitivity to sildenafil or anycomponent <strong>of</strong> the tablet.Rare cases <strong>of</strong> hypersensitivity have been reported in association with the use <strong>of</strong> sildenafilincluding anaphylactic reaction/shock events and anaphylactoid reaction. The majority <strong>of</strong>reported events were non-serious hypersensitivity reactions.WARNINGS AND PRECAUTIONSCardiovascular EffectsREVATIO has vasodilatory properties, resulting in mild and transient decreases in bloodpressure. Before prescribing REVATIO, carefully consider whether patients with certainunderlying conditions could be adversely affected by such vasodilatory effects(e.g., patients with resting hypotension [BP < 90/50], fluid depletion, severe left ventricularoutflow obstruction, or autonomic dysfunction).Pulmonary vasodilators may significantly worsen the cardiovascular status <strong>of</strong> patientswith pulmonary veno-occlusive disease (PVOD). Since there are no clinical data onadministration <strong>of</strong> REVATIO to patients with veno-occlusive disease, administration <strong>of</strong>REVATIO to such patients is not recommended. Should signs <strong>of</strong> pulmonary edema occurwhen REVATIO is administered, consider the possibility <strong>of</strong> associated PVOD.As there are no controlled clinical data on the safety or efficacy <strong>of</strong> REVATIO in the followinggroups, prescribe with caution for:• Patients who have suffered a myocardial infarction, stroke, or life-threatening arrhythmiawithin the last 6 months;• Patients with coronary artery disease causing unstable angina;• Patients with hypertension (BP > 170/110);• Patients currently on bosentan therapy.Use with Alpha-blockersPDE5 inhibitors, including sildenafil, and alpha-adrenergic blocking agents are bothvasodilators with blood pressure-lowering effects. When vasodilators are used incombination, an additive effect on blood pressure may be anticipated. In some patients,concomitant use <strong>of</strong> these two drug classes can lower blood pressure significantly,leading to symptomatic hypotension. In the sildenafil interaction studies with alphablockers,cases <strong>of</strong> symptomatic hypotension consisting <strong>of</strong> dizziness andlightheadedness were reported [see Drug Interactions]. No cases <strong>of</strong> syncope or faintingwere reported during these interaction studies. The safety <strong>of</strong> combined use <strong>of</strong> PDE5inhibitors and alpha-blockers may be affected by other variables, including intravascularvolume depletion and concomitant use <strong>of</strong> anti-hypertensive drugs.Effects on BleedingIn humans, sildenafil has no effect on bleeding time when taken alone or with aspirin. In vitro studieswith human platelets indicate that sildenafil potentiates the anti-aggregatory effect <strong>of</strong> sodiumnitroprusside (a nitric oxide donor).The combination <strong>of</strong> heparin and sildenafil had an additive effecton bleeding time in the anesthetized rabbit, but this interaction has not been studied in humans.The incidence <strong>of</strong> epistaxis was 13% in patients taking sildenafil with PAH secondary toconnective tissue disease (CTD). This effect was not seen in primary pulmonaryhypertension (PPH) (sildenafil 3%, placebo 2%) patients. The incidence <strong>of</strong> epistaxis wasalso higher in sildenafil-treated patients with a concomitant oral vitamin K antagonist(9% versus 2% in those not treated with concomitant vitamin K antagonist).The safety <strong>of</strong> REVATIO is unknown in patients with bleeding disorders or active peptic ulceration.Use with Ritonavir and Other Potent CYP3A InhibitorsThe concomitant administration <strong>of</strong> the protease inhibitor ritonavir (a highly potentCYP3A inhibitor) substantially increases serum concentrations <strong>of</strong> sildenafil; therefore,co-administration <strong>of</strong> ritonavir or other potent CYP3A inhibitors with REVATIO is not recommended.Effects on the EyeAdvise patients to seek immediate medical attention in the event <strong>of</strong> a sudden loss <strong>of</strong> visionin one or both eyes while taking PDE5 inhibitors, including REVATIO. Such an event may bea sign <strong>of</strong> non-arteritic anterior ischemic optic neuropathy (NAION), a cause <strong>of</strong> decreasedvision including permanent loss <strong>of</strong> vision, that has been reported postmarketing in temporalassociation with the use <strong>of</strong> all PDE5 inhibitors, including sildenafil, when used in thetreatment <strong>of</strong> erectile dysfunction. It is not possible to determine whether these events arerelated directly to the use <strong>of</strong> PDE5 inhibitors or to other factors. <strong>Physicians</strong> should alsodiscuss the increased risk <strong>of</strong> NAION with patients who have already experienced NAION inone eye, including whether such individuals could be adversely affected by use <strong>of</strong>vasodilators, such as PDE5 inhibitors [see Adverse Reactions].There are no controlled clinical data on the safety or efficacy <strong>of</strong> REVATIO in patients withretinitis pigmentosa, a minority whom have genetic disorders <strong>of</strong> retinal phosphodiesterases.Prescribe REVATIO with caution in these patients.Hearing ImpairmentAdvise patients to seek prompt medical attention in the event <strong>of</strong> sudden decrease or loss <strong>of</strong>hearing while taking PDE5 inhibitors, including REVATIO.These events, which may beaccompanied by tinnitus and dizziness, have been reported in temporal association to the intake<strong>of</strong> PDE5 inhibitors, including REVATIO. It is not possible to determine whether these events arerelated directly to the use <strong>of</strong> PDE5 inhibitors or to other factors [see Adverse Reactions].Combination with other PDE5 inhibitorsSildenafil is also marketed as VIAGRA ® . The safety and efficacy <strong>of</strong> combinations <strong>of</strong> REVATIOwith VIAGRA or other PDE5 inhibitors have not been studied. Inform patients taking REVATIOnot to take VIAGRA or other PDE5 inhibitors.Prolonged ErectionUse REVATIO with caution in patients with anatomical deformation <strong>of</strong> the penis(e.g., angulation, cavernosal fibrosis, or Peyronie’s disease) or in patients who haveconditions, which may predispose them to priapism (e.g., sickle cell anemia, multiplemyeloma, or leukemia). In the event <strong>of</strong> an erection that persists longer than 4 hours,the patient should seek immediate medical assistance. If priapism (painful erectiongreater than 6 hours in duration) is not treated immediately, penile tissue damageand permanent loss <strong>of</strong> potency could result.ADVERSE REACTIONSThe following serious adverse reactions are discussed elsewhere in the labeling:• Hypotension [see Warnings and Precautions]• Vision loss [see Warnings and Precautions]• Hearing loss [see Warnings and Precautions]• Priapism [see Warnings and Precautions]Clinical Trials ExperienceBecause clinical trials are conducted under widely varying conditions, adverse reactionrates observed in the clinical trials <strong>of</strong> a drug cannot be directly compared to rates in theclinical trials <strong>of</strong> another drug and may not reflect the rates observed in practice.Safety data were obtained from the 12 week, placebo-controlled clinical study and anopen-label extension study in 277 treated patients with pulmonary arterial hypertension.Doses up to 80 mg TID were studied.The overall frequency <strong>of</strong> discontinuation in REVATIO-treated patients at the recommendeddose <strong>of</strong> 20 mg TID was 3% and was the same for the placebo group.In the placebo-controlled trial in pulmonary arterial hypertension, the adverse drug reactionsthat were reported by at least 3% <strong>of</strong> REVATIO patients treated at the recommended dosage(20 mg TID) and were more frequent in REVATIO patients than placebo patients, are shownin Table 1. Adverse events were generally transient and mild to moderate in nature.Table 1. REVATIO All Causality Adverse Events in ≥ 3% <strong>of</strong> Patients and More Frequent(> 1%) than PlaceboADVERSE EVENTS Placebo Revatio 20 mg TID Placebo-% (n=70) (n=69) SubtractedEpistaxis 1 9 8Headache 39 46 7Dyspepsia 7 13 6Flushing 4 10 6Insomnia 1 7 6Erythema 1 6 5Dyspnea exacerbated 3 7 4Rhinitis nos 0 4 4Diarrhea nos 6 9 3Myalgia 4 7 3Pyrexia 3 6 3Gastritis nos 0 3 3Sinusitis 0 3 3Paresthesia 0 3 3nos: Not otherwise specifiedAt doses higher than the recommended 20 mg TID, there was a greater incidence <strong>of</strong>some adverse events including flushing, diarrhea, myalgia and visual disturbances.Visual disturbances were identified as mild and transient, and were predominatelycolortinge to vision, but also increased sensitivity to light or blurred vision.The incidence <strong>of</strong> retinal hemorrhage at the recommended sildenafil 20 mg TID dosewas 1.4% versus 0% placebo and for all sildenafil doses studied was 1.9% versus0% placebo. The incidence <strong>of</strong> eye hemorrhage at both the recommended dose andat all doses studied was 1.4% for sildenafil versus 1.4% for placebo. The patientsexperiencing these events had risk factors for hemorrhage including concurrentanticoagulant therapy.
JANUARY 2011 • CHEST PHYSICIAN PEDIATRIC CHEST MEDICINE 13VITALSInfant Vaccinations Met Goals <strong>of</strong> Healthy People 2010Major Finding: Vaccination coverage remainedat 90% or greater for most routinevaccines administered to children 19-35months <strong>of</strong> age in the United States in 2009.Data Source: The 2009 National ImmunizationSurvey <strong>of</strong> U.S. households, with reportsverified for 17,313 children whose providersprovided vaccination records.Disclosures: Dr. Schuchat had no relevantdisclosures.In a placebo-controlled fixed dose titration study <strong>of</strong> REVATIO (starting withrecommended dose <strong>of</strong> 20 mg TID and increased to 40 mg TID and then 80 mg TID)as an adjunct to intravenous epoprostenol in pulmonary arterial hypertension, theadverse events that were reported were more frequent than in the placebo arm (>6%difference) are shown in Table 2.Table 2. REVATIO-Epoprostenol Adverse Events More Frequent (> 6%) than PlaceboADVERSE EVENTS Placebo Revatio Placebo-Subtracted% Epoprostenol Epoprostenol %(n = 131) (n = 134)Headache 34 57 23Edema^ 13 25 14Dyspepsia 2 16 14Pain in extremity 6 17 11Diarrhea 18 25 7Nausea 18 25 7Nasal congestion 2 9 7^includes peripheral edemaREVATIO InjectionREVATIO injection was studied in a 66-patient, placebo-controlled study at doses targetingplasma concentrations between 10 and 500 ng/mL (up to 8 times the exposure <strong>of</strong> therecommended dose).Adverse events in PAH patients were similar to those seen with oral tablets.Postmarketing ExperienceThe following adverse reactions have been identified during postapproval use <strong>of</strong> sildenafil(marketed for both PAH and erectile dysfunction). Because these reactions are reportedvoluntarily from a population <strong>of</strong> uncertain size, it is not always possible to reliably estimatetheir frequency or establish a causal relationship to drug exposure.Cardiovascular EventsIn postmarketing experience with sildenafil at doses indicated for erectile dysfunction,serious cardiovascular, cerebrovascular, and vascular events, including myocardial infarction,sudden cardiac death, ventricular arrhythmia, cerebrovascular hemorrhage, transientischemic attack, hypertension, pulmonary hemorrhage, and subarachnoid and intracerebralhemorrhages have been reported in temporal association with the use <strong>of</strong> the drug. Most, butnot all, <strong>of</strong> these patients had preexisting cardiovascular risk factors. Many <strong>of</strong> these eventswere reported to occur during or shortly after sexual activity, and a few were reported tooccur shortly after the use <strong>of</strong> sildenafil without sexual activity. Others were reported to haveoccurred hours to days after use concurrent with sexual activity. It is not possible todetermine whether these events are related directly to sildenafil, to sexual activity, to thepatient’s underlying cardiovascular disease, or to a combination <strong>of</strong> these or other factors.Decreases in and Loss <strong>of</strong> VisionWhen used to treat erectile dysfunction, non-arteritic anterior ischemic optic neuropathy(NAION), a cause <strong>of</strong> decreased vision including permanent loss <strong>of</strong> vision, has beenreported postmarketing in temporal association with the use <strong>of</strong> phosphodiesterase type 5(PDE5) inhibitors, including sildenafil. Most, but not all, <strong>of</strong> these patients had underlyinganatomic or vascular risk factors for developing NAION, including but not necessarilylimited to: low cup to disc ratio (“crowded disc”), age over 50, diabetes, hypertension,coronary artery disease, hyperlipidemia and smoking. It is not possible to determinewhether these events are related directly to the use <strong>of</strong> PDE5 inhibitors, to the patient’sunderlying vascular risk factors or anatomical defects, to a combination <strong>of</strong> these factors,or to other factors [see Warnings and Precautions].Loss <strong>of</strong> HearingCases <strong>of</strong> sudden decrease or loss <strong>of</strong> hearing have been reported postmarketing intemporal association with the use <strong>of</strong> PDE5 inhibitors, including REVATIO. In some <strong>of</strong> thecases, medical conditions and other factors were reported that may have also played a rolein the otologic adverse events. In many cases, medical follow-up information was limited. Itis not possible to determine whether these reported events are related directly to the use <strong>of</strong>REVATIO, to the patient’s underlying risk factors for hearing loss, a combination <strong>of</strong> thesefactors, or to other factors [see Warnings and Precautions].Other EventsThe following list includes other adverse events that have been identified duringpostmarketing use <strong>of</strong> REVATIO. The list does not include adverse events that are reportedfrom clinical trials and that are listed elsewhere in this section. These events have beenchosen for inclusion either due to their seriousness, reporting frequency, lack <strong>of</strong> clearalternative causation, or a combination <strong>of</strong> these factors. Because these reactions werereported voluntarily from a population <strong>of</strong> uncertain size, it is not possible to reliablyestimate their frequency or establish a causal relationship to drug exposure.Nervous system: Seizure, seizure recurrenceDRUG INTERACTIONSNitratesConcomitant use <strong>of</strong> REVATIO with nitrates in any form is contraindicated[see Contraindications].Ritonavir and other Potent CYP3A InhibitorsConcomitant use <strong>of</strong> REVATIO with ritonavir and other potent CYP3A inhibitors is notrecommended [see Warnings and Precautions].Alpha-blockersUse caution when co-administering alpha-blockers with REVATIO because <strong>of</strong> additive bloodpressure-lowering effects [see Warnings and Precautions].BY DAMIAN McNAMARAElsevier Global Medical NewsATLANTA – Vaccination <strong>of</strong> U.S.infants 19-35 months <strong>of</strong> age remainshigh at 90% or greater forroutine immunizations, accordingto results <strong>of</strong> the 2009 National ImmunizationSurvey released by theCenters for Disease Control andPrevention.This means vaccine coverage in2009 met or exceeded the 90% goalset by the national Healthy People2010 initiative.This survey <strong>of</strong> vaccinations for17,313 children nationwide revealedthat less than 1% <strong>of</strong> young childrenborn between January 2006 andJuly 2008 received no vaccinations(MMWR 2010;59:1171-7).“Today’s report is generally veryreassuring, despite concerns we’veseen in the past about whetherIn drug-drug interaction studies, sildenafil (25 mg, 50 mg, or 100 mg) and the alpha-blockerdoxazosin (4 mg or 8 mg) were administered simultaneously to patients with benignprostatic hyperplasia (BPH) stabilized on doxazosin therapy. In these study populations,mean additional reductions <strong>of</strong> supine systolic and diastolic blood pressure <strong>of</strong> 7/7 mmHg,9/5 mmHg, and 8/4 mmHg, respectively, were observed. Mean additional reductions <strong>of</strong>standing blood pressure <strong>of</strong> 6/6 mmHg, 11/4 mmHg, and 4/5 mmHg, respectively, were alsoobserved. There were infrequent reports <strong>of</strong> patients who experienced symptomatic posturalhypotension. These reports included dizziness and light-headedness, but not syncope.AmlodipineWhen sildenafil 100 mg oral was co-administered with amlodipine, 5 mg or 10 mg oral, tohypertensive patients, the mean additional reduction on supine blood pressure was 8 mmHgsystolic and 7 mmHg diastolic.USE IN SPECIFIC POPULATIONSPregnancyPregnancy Category BNo evidence <strong>of</strong> teratogenicity, embryotoxicity, or fetotoxicity was observed in pregnant rats or rabbitsdosed with sildenafil 200 mg/kg/day during organogenesis, a level that is, on a mg/m 2 basis, 32-and 68-times, respectively, the recommended human dose (RHD) <strong>of</strong> 20 mg TID. In a rat pre- andpostnatal development study, the no-observed-adverse-effect dose was 30 mg/kg/day (equivalentto 5-times the RHD on a mg/m 2 basis).There are, however, no adequate and well-controlled studies<strong>of</strong> sildenafil in pregnant women. Because animal reproduction studies are not always predictive <strong>of</strong>human response, this drug should be used during pregnancy only if clearly needed.Labor and DeliveryThe safety and efficacy <strong>of</strong> REVATIO during labor and delivery has not been studied.Nursing MothersIt is not known if sildenafil or its metabolites are excreted in human breast milk. Becausemany drugs are excreted in human milk, caution should be exercised when REVATIO isadministered to a nursing woman.Pediatric UseSafety and effectiveness <strong>of</strong> sildenafil in pediatric pulmonary hypertension patients have notbeen established.Geriatric UseClinical studies <strong>of</strong> REVATIO did not include sufficient numbers <strong>of</strong> subjects aged 65 and over todetermine whether they respond differently from younger subjects. Other reported clinicalexperience has not identified differences in responses between the elderly and younger patients. Ingeneral, dose selection for an elderly patient should be cautious, reflecting the greater frequency <strong>of</strong>decreased hepatic, renal, or cardiac function, and <strong>of</strong> concomitant disease or other drug therapy.Hepatic ImpairmentNo dose adjustment for mild to moderate impairment is required. Severe impairmenthas not been studied.Renal ImpairmentNo dose adjustment is required (including severe impairment CLcr < 30 mL/min).OVERDOSAGEIn studies with healthy volunteers <strong>of</strong> single doses up to 800 mg, adverse events weresimilar to those seen at lower doses but rates and severities were increased.In cases <strong>of</strong> overdose, standard supportive measures should be adopted as required. Renaldialysis is not expected to accelerate clearance as sildenafil is highly bound to plasmaproteins and it is not eliminated in the urine.NONCLINICAL TOXICOLOGYCarcinogenesis, Mutagenesis, Impairment <strong>of</strong> FertilitySildenafil was not carcinogenic when administered to rats for up to 24 months at60 mg/kg/day, a dose resulting in total systemic exposure (AUC) to unbound sildenafil andits major metabolite 33 and 37 times, for male and female rats respectively, the humanexposure at the RHD <strong>of</strong> 20 mg TID. Sildenafil was not carcinogenic when administered tomale and female mice for up to 21 and 18 months, respectively, at doses up to a maximallytolerated level <strong>of</strong> 10 mg/kg/day, a dose equivalent to the RHD on a mg/m 2 basis.Sildenafil was negative in in vitro bacterial and Chinese hamster ovary cell assays todetect mutagenicity, and in vitro human lymphocytes and in vivo mouse micronucleusassays to detect clastogenicity.There was no impairment <strong>of</strong> fertility in male or female rats given up to 60 mg sildenafil/kg/day, adose producing a total systemic exposure (AUC) to unbound sildenafil and its major metabolite <strong>of</strong> 19and 38 times for males and females, respectively, the human exposure at the RHD <strong>of</strong> 20 mg TID.PATIENT COUNSELING INFORMATION• Inform patients <strong>of</strong> contraindication <strong>of</strong> REVATIO with regular and/or intermittent use <strong>of</strong> organic nitrates.• Inform patients that sildenafil is also marketed as VIAGRA for erectile dysfunction.Advise patients taking REVATIO not to take VIAGRA or other PDE5 inhibitors.• Advise patients to seek immediate medical attention in the event <strong>of</strong> a sudden loss <strong>of</strong>vision in one or both eyes while taking REVATIO. Such an event may be a sign <strong>of</strong> NAION.• Advise patients to seek prompt medical attention in the event <strong>of</strong> sudden decrease or loss <strong>of</strong>hearing while taking REVATIO. These events may be accompanied by tinnitus and dizziness.RX onlyRevised: November 2009RVU00106A ©2010 Pfizer Inc All rights reserved. Printed in USA/January 2010U.S. Pharmaceuticalsparents are continuing to have their childrenvaccinated, and despite some resurgencesin vaccine-preventable diseasesin particular areas,” Dr. Anne Schuchat,director <strong>of</strong> the National Center for Immunizationand Respiratory Diseases atthe CDC, said during a telebriefing.Some substantial variation in vaccinecoverage between states was again revealedby this annual survey, suggestingthat there is still work to be done in somecommunities.Dr. Schuchat addressed the outbreak<strong>of</strong> pertussis cases in California, responsiblefor nine infant deaths since January2010. The coverage in California for fourdoses <strong>of</strong> DTaP, the pertussis-containingshot for babies, was 83%, according tostate records. “We don’t think it’s thecoverage level in babies and toddlers thatis leading to that pertussis challenge inCalifornia.” Instead, “we think the challengewith those pertussis cases is the increasingvaccination <strong>of</strong> teens and adults,”she said, although “it continues to be importantfor babies and toddlers to gettheir DTaP doses.”The CDC strongly recommendseveryone aged 11 years and older, particularlynew parents and those in closecontact with young children, receivethe vaccination against pertussis. Dr.Schuchat said, “The situation in Californiais serious, and we are working togetherwith the California healthdepartment to really promote uptake <strong>of</strong>the pertussis vaccine for teens andadults.”The survey showed national coveragefor MMR vaccinations experienced “asignificant but not large” drop from 92%in 2008 to 90% in 2009. “That might bea warning sign <strong>of</strong> larger drops to comeor a small change that, because our surveyis so large, was statistically significant,”Dr. Schuchat said. Even thoughnational coverage numbers are 90%,“you can still have large pockets <strong>of</strong> susceptiblechildren.”“Those two examples [pertussis andmeasles] show that we cannot let ourguard down,” Dr. Schuchat said.The survey also revealed a substantialdrop in coverage for one vaccine,Haemophilus influenzae B (Hib). A total <strong>of</strong>84% <strong>of</strong> children aged 19-35 months receivedthe three recommended doses inthe survey. This represents a decrease <strong>of</strong>more than 6 percentage points vs. 2008that “really just reflects the nationalshortage” <strong>of</strong> this vaccine between December2007 and September 2009, Dr.Schuchat said. She commended cliniciansfor following recommendations todrop the booster shot during this shortage,and added that the vaccine is nowreadily available.Other survey findings indicate that44% <strong>of</strong> children received full coveragefor the rotavirus vaccine during infancy.This is the first national survey data to reportadoption <strong>of</strong> the rotavirus vaccinesince its U.S. licensure in 2006. “That isreally good uptake <strong>of</strong> this vaccine. Ofcourse, we’re already seeing a very importantdrop in disease caused by therotavirus,” Dr. Schuchat said. ■
14 NEWS FROM THE COLLEGE JANUARY 2011 • CHEST PHYSICIANDr Stuart M. Garay, FCCP, is a practicingpulmonologistandClinical Pr<strong>of</strong>essor<strong>of</strong> Medicineat the NewYork UniversitySchool <strong>of</strong> Medicine.He isPresident <strong>of</strong>University<strong>Physicians</strong> Network,a physicianfounded,owned, and operatedorganization that is committedto helping member physicians copewith the changes and challenges <strong>of</strong> thehealth-care business environment. DrGaray is a member <strong>of</strong> the PracticeOperations NetWork Steering Committee.In the past, he has served onthe ACCP Board <strong>of</strong> Regents as a Regentat Large; as a member <strong>of</strong> theCHEST scientific program committee;and on the steering committee <strong>of</strong> theClinical Pulmonary Medicine Net-Work. Dr Garay’s clinical and researchinterests include airway diseases rangingfrom asthma to bronchiectasis, mycobacterialinfections, and sleep apnea.CHEST Physician Editorial Advisory BoardGains New Members and a Deputy EditorDR STUART M. GARAY,FCCPHe has participated in numerous clinicaltrials for asthma and COPD, and hehas published more than 50 papersand chapters on various topics in pulmonarymedicine. He is co-editor <strong>of</strong> atext, Tuberculosis.Dr Darcy D. Marciniuk, FCCP, is aPr<strong>of</strong>essor <strong>of</strong>Medicine andHead <strong>of</strong> theDivision <strong>of</strong>Respirology,Critical Care,and Sleep Medicineat theUniversity <strong>of</strong>Saskatchewan,Saskatoon, SK,Canada. DrMarciniuk receivedhis Doctor<strong>of</strong> Medicine from the University <strong>of</strong>Saskatchewan and had specialty trainingin internal medicine and respiratorymedicine at the University <strong>of</strong>Western Ontario and at the University<strong>of</strong> Manitoba. He returned to Saskatoonin 1990, where he assumed hiscurrent faculty position with theUniversity <strong>of</strong> Saskatchewan.CELEBRATIONOF PEDIATRICPULMONOLOGY2011April 8-10Ft. Lauderdale, FloridaCo-ChairsLeRoy M. Graham, MD, FCCPDennis Gurwitz, MBBCh, FAAPDon’t miss this state-<strong>of</strong>-the-art update in clinicalpediatric pulmonology, featuring the latestresearch in pulmonology, sleep, pulmonary-GIdisorders, and surgery. The course will combineplenary-style lectures, question and answersessions, interactive small group workshops,and case presentations, allowing attendees tobenefit from a wide variety <strong>of</strong> learning methods.Many sessions will be interactive, so you canaddress specific issues that impact you practice.Who Should AttendPediatric PulmonologistsGeneral PediatriciansFamily <strong>Physicians</strong>Pediatric IntensivistsAllergistsPediatric Nurse PractitionersRespiratory TherapistsWatch for more details.www.chestnet.orgDR DARCY D.MARCINIUK, FCCPDr Marciniuk is currently President-Designate <strong>of</strong> the ACCP, a member <strong>of</strong>the ACCP Board <strong>of</strong> Regents, and aTrustee <strong>of</strong> The CHEST Foundation. Hehas held a number <strong>of</strong> leadership positionsin the ACCP, including Governor<strong>of</strong> Saskatchewan; Chair <strong>of</strong> the PulmonaryPhysiology, Function, and RehabilitationNetWork; and Co-Chair <strong>of</strong>CHEST 2005. Dr Marciniuk is PastChair <strong>of</strong> the Royal <strong>College</strong> <strong>of</strong> <strong>Physicians</strong>and Surgeons <strong>of</strong> Canada ExaminationCommittee in Respirology and isa Past President <strong>of</strong> the Canadian ThoracicSociety. He has published morethan 90 peer-reviewed publications,chapters, and reviews. His interests inpulmonary medicine include COPDand clinical physiology and exercise.Dr Marcos I. Restrepo, MSc, FCCP,is an AssistantPr<strong>of</strong>essor <strong>of</strong>Medicine in theDivision <strong>of</strong>Pulmonary/Critical CareMedicine at theUniversity <strong>of</strong>Texas HealthScience Centerat San Antonio.He is the Directorat the MedicalIntensiveDR MARCOS I.RESTREPO, MSC, FCCPCare Unit at the South Texas VeteransHealth Care System, Audie L. MurphyDivision. He completed his residencyin internal medicine and fellowships ininfectious diseases, pulmonary disease,and critical care medicine at the University<strong>of</strong> Texas Health Science Centerat San Antonio. Dr Restrepo is an investigatorfor VERDICT, which aims totranslate medical evidence into clinicalpractice. He has been an author or coauthor<strong>of</strong> more than 60 journal articlesand 7 book chapters and has lecturednationally and internationally. Dr Restreposerves on the ACCP RespiratoryCare NetWork Steering Committeeand previously was on the <strong>Chest</strong> InfectionsNetWork Steering Committee.He serves as a reviewer for 14 journals,including CHEST, Critical Care Medicine,and <strong>American</strong> Journal <strong>of</strong> Respiratory andCritical Care Medicine. Dr Restrepo’sprimary research interests include immunomodulationin sepsis and pneumonia,appropriate application <strong>of</strong>interventions to prevent and treat criticallyill patients with severe infections,and improving health outcomes andquality <strong>of</strong> care <strong>of</strong> patients in the ICUwith pneumonia and sepsis.Dr W. Michael Alberts, FCCP,has agreed toassume theDeputy Editorin Chief rolefor CHESTPhysician andwork with DrSelecky duringthe final year <strong>of</strong>his term in2011. Dr Albertswill then DR W. MICHAELtake over asALBERTS, FCCPEditor in Chieffrom 2012 through 2015. We thankDr Alberts for his continued leadershipservice to CHEST Physician. ■CHEST Goes Mobile on iPhone ® ,iPod touch ® , and iPad ®Among the most trustedsources for cutting-edgeoriginal research in the multidisciplinaryspecialties <strong>of</strong> chestmedicine, the CHEST journal isnow available as an app for theiPhone ® , iPod touch ® , andiPad ® .The CHEST Journal App allowsreaders to browse the tables<strong>of</strong> contents from the threemost recent issues and papers inpress, view abstracts, and—during thefree-trial period, lasting until June2011—read full-text articles.*Top features include the abilities to PrescriptionOpiate/OpioidDrug Abuse: A NewEpidemic.By Susan Y. Kim-Katz,PharmD; and Ilene B. Anderson,PharmDJanuary Lessonsview tables and figures in anenhanced format, use side navigationto jump to differentparts <strong>of</strong> an article, mark andsave or e-mail links to favoritearticles to read later, and accessreferenced content through anin-app Web browser.The CHEST Journal App canbe downloaded by searching“CHEST Journal” in the AppStore SM or on iTunes®. ■*After the free-trial period expires, full-textcontent will be made available to subscribersthrough a one-time log-in. Respiratory Manifestations<strong>of</strong> GastroesophagealReflux.By Lindsey B. Roenigk,MD; and Susan M.Harding, MD, FCCPwww.chestnet.org/accp/pccsu
JANUARY 2011 • CHEST PHYSICIAN NEWS FROM THE COLLEGE 15GuidelinesMoving ForwardIn ongoing efforts to strengthen its internationallyrecognized guideline development,publication, and dissemination, theACCP has hired two new employees withnotable backgrounds contributive towardthis end.Rebecca Diekemper, MPH, comes to theACCP from BJC HealthCare in St Louis,where she served as a clinical epidemiologist.In addition to reviewing guidelines and theprimary evidence, Rebecca has performedsome systematic reviews and developed atool to assess systematic reviews, which hasbeen compared to the Guyatt-Oxman andother such tools. She will be primarily workingon the lung cancer guidelines, managing thePolicy and Procedures Subcommittee, andassisting with the full HSP Committee.Joe Ornelas, DC, MS, MA, is working towardcompleting a PhD in health policy andadministration at the University <strong>of</strong> IllinoisSchool <strong>of</strong> Public Health. In various jobs inacademic and hospital settings, he has conductedextensive literature reviews, performedprobability-based decision analysesfor cost-effectiveness and cost-utility evaluations,and worked on many projects requiringdata management and analysis. Joewill work primarily on the antithromboticand immunosuppressives guidelines and willmanage the HSP Guidelines Subcommittee.■New HHS/CCSC Awards Program AnnouncedReducing the incidence <strong>of</strong>healthcare-associated infections(HAIs) is a priority for theACCP. A new national awards program,Achievements in EliminatingHealthcare-Associated Infections,cosponsored by the US Department<strong>of</strong> Health and Human Services(HHS) and the Critical Care SocietiesCollaborative (CCSC), will annuallyrecognize teams <strong>of</strong> critical care pr<strong>of</strong>essionalsand health-care institutionsBY DR RICHARD S.MASTER FCCPEditor in Chief, CHESTthat achieve excellence and notable,sustained improvements in preventingHAIs, specifically infections involvingcritical care. The awards programintends to motivate the health-carecommunity to achieve wide-scale reductionand elimination <strong>of</strong> HAIs andfurther motivate other clinicians, hospitalexecutives, and facilities to improveclinical practice throughutilization <strong>of</strong> evidence-based guidelines.The ACCP actively participatesThis Month in CHEST: Editor’s PicksIRWIN, Effects <strong>of</strong> Bronchoconstriction,Minute Ventilation, and Deep Inspirationon the Composition <strong>of</strong>Exhaled Breath Condensate.By Dr J. S. Debley et al. Interpreting Lung FunctionData Using 80% Predicted andFixed Thresholds MisclassifiesMore Than 20% <strong>of</strong> Patients.By Dr M. R. Miller et al. Factors at Admission AssociatedWith Bleeding Risk in Medical Patients:Findings From theIMPROVE Investigators.By Dr H. Decousus et al. Beneficial Effects <strong>of</strong>Treatment With Anti-IgEAntibodies (Omalizumab)in a Patient With SevereAsthma and NegativeSkin-Prick Test Results.By Dr M. van den Berge et al.SPECIAL FEATURE Seventh Edition <strong>of</strong> the CancerStaging Manual and StageGrouping <strong>of</strong> Lung Cancer:Quick Reference Chart andDiagrams.By Dr O. Lababede et al.in the CCSC, along with the <strong>American</strong>Association <strong>of</strong> Critical-CareNurses, <strong>American</strong> Thoracic Society,and Society <strong>of</strong> Critical Care Medicine.The initial phase <strong>of</strong> the awardsprogram will emphasize success relatedto reducing and eliminatingcentral line–associated bloodstreaminfections and ventilator-associatedpneumonia. Applications are dueJanuary 29, 2011. For questions,contact awards@aacn.org. ■EDITORIALS Developing ComplementaryClinical Guidelinesfor PulmonaryRehabilitation in COPD:Why Add More? By Dr R.Goldstein; and Dr D.Marciniuk. The Journal and 2011:A Time for Stocktaking. By Dr R. S.Irwin; and N. Augustyn.TRANSLATING BASIC RESEARCH INTOCLINICAL PRACTICE Systemic Manifestations <strong>of</strong>COPD. By Dr Y. Nussbaumer-Ochsner;and Dr K. F. Rabe.AMERICAN COLLEGE OF CHEST PHYSICIANS2011EducationCalendarSleep Medicine 2011January 27-30Tempe, AZMechanical Ventilation 2011August 30San Antonio, TXACCP Simulation Programfor Advanced Clinical EducationCelebration <strong>of</strong> PediatricPulmonology 2011April 8-10Ft. Lauderdale, FLACCP Critical Care MedicineBoard Review 2011August 26-30San Antonio, TXACCP Sleep MedicineBoard Review 2011August 26-29San Antonio, TXLung Pathology 2011August 30San Antonio, TXABIM Critical CareMedicine and PulmonaryDisease SEP ModulesAugust 30San Antonio, TXACCP Pulmonary MedicineBoard Review 2011August 31-September 4San Antonio, TXCHEST 2011October 22-27Honolulu, HawaiiBasic and AdvancedBronchoscopy SkillsFebruary 11-13Orlando, FLAugust 5-7Chicago, ILMechanical VentilationFebruary 25-27Chicago, ILDifficult Airway ManagementMarch 18-20July 22-24Northbrook, ILUltrasonography:Fundamentals in Critical CareApril 15-17Balitmore, MDFocused Pleural andVascular UltrasoundSeptember 22-23Chicago, ILCritical Care EchocardiographySeptember 24-25Chicago, ILwww.chestnet.org/accp/events(800) 343-2227 or +1 (847) 498-1400
16 NEWS FROM THE COLLEGE JANUARY 2011 • CHEST PHYSICIANCritical CareThe Kansas Sepsis ProjectSevere sepsis is a common cause <strong>of</strong>mortality, representing the most commoncause <strong>of</strong> death in noncoronaryICUs (Bone et al. <strong>Chest</strong>. 1992;101[6]:1644). Sepsis is rapidly increasing inincidence, projected to affect over1,000,000 patients per year in theUnited States by 2020 (Angus et al. CritCare Med. 2001;29[7]:1303-1310). Ruralpatients develop severe sepsis in similarproportion to urban patients, yet accessto critical care services in rural areas islimited.Telemedicine can help to bridge thegap between the mostly urban supply <strong>of</strong>intensivists and underserved rural patientsand their local physicians (Marcinet al. J Pediatr. 2004;144[3]:375). Varioustechniques have been utilized to addressthis need, ranging from video consultationto teleICU, with reasonable evidencethat such care is comparable tohands-on ICU care (Hersh et al. BMCMedical Informatics and Decision Making.2001;1:5). To further explore uses <strong>of</strong>telemedicine in the specialty <strong>of</strong> criticalcare medicine, a CME/performanceimprovement project dealing with improvingcare <strong>of</strong> patients with sepsis inrural Kansas was implemented via theEli Lilly Distinguished Scholar Award <strong>of</strong>The CHEST Foundation. An objective<strong>of</strong> the project is to empower rural physiciansto appropriately care for their ownpatients with sepsis, as an alternative toreal-time telemedicine consultation.The Kansas Sepsis Project bringsCME and performance improvementto rural Kansas areas via telemedicinein both educational and advisory roles.The project provides a novel methodfor rural medical practitioners to obtainCME credit while performingsepsis quality improvement projectsthat are eligible for maintenance <strong>of</strong>board certification. The overall goal <strong>of</strong>the project is to demonstrate astatewide reduction in sepsis mortalitythrough widespread provider participation,paving the way for similar projectsin other rural states.Dr Lucas R. Pitts; andDr Steven Q. Simpson, FCCP,NetWork Vice-Chair and Third Eli Lillyand Company Distinguished Scholar inCritical Care MedicineCardiovascular Medicine and SurgeryRisk <strong>of</strong> Acute Kidney Injury With SameAdmission Cardiac Catheterization andCardiac SurgeryAcute kidney injury (AKI) after opencardiac operations is associated with increasedmorbidity and short-term andlong-term mortality. Prevention <strong>of</strong> AKIduring and after surgery is <strong>of</strong> paramountimportance. The Acute KidneyInjury Network definition <strong>of</strong> AKI is a0.3 mg/dL or 50% increase in baselinecreatinine value. It is common practiceto provide diagnostic cardiac catheterizationand cardiac surgery in the sameadmission. This practice may lead to ahigher risk <strong>of</strong> AKI with attendant increasedrisks for a higher morbidity andmortality. The question, therefore,remains as to the optimal timing <strong>of</strong> cardiacsurgery following cardiac catheterization.A recent prospective study fromthe Northern New England CardiovascularDisease Study Group looked atthe incidence <strong>of</strong> AKI after cardiaccatheterization in 668 patientsundergoing nonemergentcardiac surgeryduring the same hospitaladmission (367 patients)or a later admission (301patients) (Kramer et al.Ann Thorac Surg. 2010;90[5]:1418).The incidence <strong>of</strong> AKIwas 50.2% in the sameadmission group vs33.7% for the later admissiongroup. The differencewas highly significant (P=.009).Patients undergoing surgery at a lateradmission had a 45% reduction in AKI.The authors concluded that “it is safeand possibly beneficial in terms <strong>of</strong>renal protection, to send patients homeafter cardiac catheterization with aplan for surgery during subsequent admission.”Dr G. Hossein Almassi, FCCPNetWork Vice-ChairAllied HealthSleep Disorders Specialty Exam AccreditedThe National Board for RespiratoryCare (NBRC) invested several yearsdeveloping an examination for respiratorytherapists specializing in sleep disordersand therapeutic intervention.Candidates must be credentialed respiratorytherapists with clinical experiencein the testing, monitoring,diagnosis, and treatment <strong>of</strong> patientswith sleep disorders. Successful candidatesreceive either the CRT-SDS orRRT-SDS federally trademarked credentialdesignation depending onwhether they attempted the examinationas a CRT or an RRT.The specialty examination was developedin accordance with stringent psychometricand other standards putforth by the National Commission forCertifying Agencies. This body also accreditsthe registered polysomnographictechnologist (RPSGT)examination <strong>of</strong>fered by the Board <strong>of</strong>Registered Polysomnographic Technologists(BRPT). Both the RPSGT andsleep disorders specialty (SDS) examinationswere developed based on jobcontent identified by national jobanalysis research.Test specifications for the NBRC’sSDS examination can be reviewed andprinted by accessing the NBRC Website at nbrc.org and clicking on the“Examinations” tab. An online, fulllength,free practice examination isalso available.The new specialty examination wasdeveloped in response to requests fromNETWORKSSepsis, Acute Kidney Injury, Sleep Disorders, Fluthe NBRC’s sponsors. The Board <strong>of</strong>Trustees is pleased to announce thenew examination was recently accreditedby the National Commission for CertifyingAgencies (NCCA), continuing along tradition <strong>of</strong> NCCA accreditationfor all <strong>of</strong> the NBRC’s credentialing programs.The NBRC was one <strong>of</strong> the firstfour organizations to have its examinationsaccredited in 1977when the NCCA wasformed, and it is the onlyorganization to continuouslymaintain accreditation<strong>of</strong> its credentialingprograms for more than30 years.Gary A. Smith, CRT,FAARCNetWork SteeringCommittee Member<strong>Chest</strong> InfectionsInfluenza: Brief Comments on the Recent2009 Influenza A(H1N1) Epidemic andObservations on VaccineSporadic outbreaks <strong>of</strong> highly virulentavian H5N1 influenza and the recentoutbreak <strong>of</strong> a pandemic A(H1N1) virushave heightened concerns about theeventual emergence <strong>of</strong> a particularlydeadly pandemic virus. Influenza Avirus represents one <strong>of</strong> the most prominentviral pathogens <strong>of</strong> modern times.Infection with this microbe results in anestimated 36,000 deaths 1 and over200,000 hospitalizations 2 in the UnitedStates annually, with a projected totaleconomic burden in excess <strong>of</strong> 80 billionUS dollars per year. 3 According to theCenters for Disease Control and Prevention,the incidence <strong>of</strong> influenzavirus infection in the US populationmay reach 20% during a typical flu season;however, this figure can increasesubstantially during periods <strong>of</strong> pandemicinfluenza. Although influenza istypically a self-limiting disease, seriouscomplications can occur, including primaryviral pneumonia, secondary bacterialpneumonia, myositis, andneurologic syndromes. The risk <strong>of</strong>mortality and disease complications iselevated for certain populations, includingthe young, old, immunosuppressed,and immunocompromised.During the most recent pandemic,infection/disease was witnessed inunique populations, such as pregnantwomen and children, with substantialmortality observed. Elderly individualswere not as predisposed, reflecting previousserologic evidence <strong>of</strong> prior exposureto similar influenza virus strains.The epidemic demonstrated differencesin treatment efficacy for drugs; potentialutilities <strong>of</strong> intensive support, includingalternate ventilatory modes such as extracorporealmembrane oxygenation;and difficulties in administering and allocatingresources. Interactions amongphysicians, health-care delivery systems,and administrations were stressed. Theability <strong>of</strong> influenza A virus to infectmillions <strong>of</strong> people each year speaks tothe resilient nature <strong>of</strong> this pathogenand to the necessity for developing improvedmethods <strong>of</strong> disease preventionand treatment.Although commercial influenza vaccineshave been available since the mid-1900s, a number <strong>of</strong> key challengescontinue to limit the efficacy <strong>of</strong> thesevaccines. The rapid mutation rate <strong>of</strong>immunodominant glycoproteins on thevirus surface necessitates annual revision<strong>of</strong> the vaccine and requires abroad network <strong>of</strong> laboratories to cooperativelyperform surveillance on circulatinginfluenza virus strainsthroughout the year. Importantly, currentstrain-specific vaccines are only30% to 50% effective in preventing hospitalizationand pneumonia in the elderlyand are about 70% effective inpreventing illness in healthy adults.Most recently (late 2010), severalgroups have observed disturbing trends<strong>of</strong> mistrust <strong>of</strong> vaccine formulations(individual components), which haveresulted in refusal <strong>of</strong> vaccination byhealth-care persons <strong>of</strong> all types, includingphysicians and nurses.Despite the extensive variability instrains <strong>of</strong> seasonal influenza, some researchinvestigations have indicated thepotential for developing universallyprotective immune responses againstinfluenza viruses. Over the pastdecade, an array <strong>of</strong> conserved influenzavirus epitopes have been identified,and the ability <strong>of</strong> both cell-mediatedimmune components and humoral immunecomponents to elicit crossprotectiveimmunity to heterologousinfluenza A viruses have been documented.Moreover, the improvement<strong>of</strong> influenza vaccine immunogenicityvia inclusion <strong>of</strong> molecular adjuvantsand modification <strong>of</strong> vaccine modalityhas been widely reported but rarelywithin the context <strong>of</strong> a universal influenzavaccine. Development <strong>of</strong> amaximally efficacious vaccine in primatesmay require alternative approaches,such as a combinatorialformulation containing both immunomodulatorycomponents andconserved influenza antigens.Further research is necessary to refineapproaches to management <strong>of</strong> influenza,both in prevention andtreatment.1. Molinari NA, Ortega-Sanchez IR,Messonnier ML, et al. The annual impact<strong>of</strong> seasonal influenza in the US:measuring disease burden and costs.Vaccine. 2007;25(27):5086-5096.2. Thompson W, Weintraub E,Dhankhar P, et al. Estimates <strong>of</strong> US influenza-associateddeaths made usingfour different methods. Influenza OtherRespi Viruses. 2009;3(1):37-49.3. Thompson WW, Shay DK, WeintraubE, et al. Influenza-associated hospitalizationsin the United States.JAMA. 2004;292(11):1333-1340.Dr Joel F. Aldrich; andDr Richard E. Winn, FCCP,NetWork Steering Committee MemberPages 16a—16b
JANUARY 2011 • CHEST PHYSICIAN NEWS FROM THE COLLEGE 17TRATEGIESOptimal management requires collaboration witha dentist trained in dental sleep medicine.Although the first reported case <strong>of</strong>oral appliance use was by PierreRobin in 1934, 1,2 recognition <strong>of</strong>the effectiveness <strong>of</strong> these devices intreating sleep-disordered breathing didnot gain momentum until the early1980s. As oral appliances have evolvedand dentists have gained expertise intheir use, these devices have becomean important part <strong>of</strong> the management<strong>of</strong> patients with sleep-disorderedbreathing. At present, oral appliancesare recommended as second-line managementfor patients with obstructivesleep apnea (OSA) who have mild tomoderate disease and who prefer anoral appliance or are intolerant <strong>of</strong> continuouspositive airway pressure(CPAP) therapy. 3,4The <strong>American</strong> Academy <strong>of</strong> SleepMedicine’s practice parameters for oralappliance management <strong>of</strong> OSA notesthat oral appliances are indicated inpatients with mild to moderate OSAwho prefer the use <strong>of</strong> an oral applianceto CPAP.Oral appliances are also recommendedfor those patients who do notrespond to CPAP, who are not appropriatecandidates for CPAP, or who failtreatment attempts with CPAP. 4 Oralappliances should be fitted by qualifieddentists who are trained and have experiencein the care <strong>of</strong> oral health. Theseappliances improve sleep-disorderedbreathing and subjective measures <strong>of</strong>sleepiness when compared with notreatment or placebo. 5,6 AlthoughCPAP is more effective at improvingsleep-disordered breathing than areoral appliances, oral appliances producesignificant improvements in measures<strong>of</strong> sleep-disordered breathing,blood pressure, and quality <strong>of</strong> life. 5-7 Ofnote, oral appliances outperformed upperairway surgery in a head-to-headtrial. 8Oral appliances have been identifiedby several names, including mandibularrepositioning appliances (MRAs),mandibular repositioning devices(MRDs), mandibular advancementsplints (MASs), mandibular advancementdevices (MADs), and tonguerepositioning or tongue retainingdevices (TRDs).Dr JamesParish, FCCPSection Editor,Sleep StrategiesThese appliances are divided intotwo categories: those that advance themandible (MRA, MAS, MRD, andMADs) and those that reposition andretain the tongue in a forward position(TRDs). Since TRDs are not FDAapprovedand have not been extensivelystudied, they will not be discussed furtherhere.For clarity, the term “mandibularrepositioning appliances” will be usedin this discussion. MRAs are viewed bythe US Food and Drug Administrationas class 2 medical devices. MRAs aretypically made in two pieces (upperand lower) and then connected. Theycan be rigid (monobloc) or adjustable(duobloc), with the upper and lowerportions attached by a hook or screwassembly or by elastic bands. They aremost <strong>of</strong>ten made <strong>of</strong> acrylic resin andwell adapted to the teeth for retentionpurposes.Adjustable devices are more popularand effective, as they can incrementallyadvance the lower jaw forwardand downward. Many adjustable devicesallow for lateral movements <strong>of</strong>the mandible. This attribute is especiallybeneficial for patients with OSAwho experience bruxism. Devicesmade <strong>of</strong> thermoplastic (also known as“boil and bite”) are not consideredcustom-made appliances and do notperform as well. 9How MRAs WorkMRAs work by moving the mandibledown and forward, which opens theposterior airspace and pulls the tongueforward. Mandibular protrusion bymeans <strong>of</strong> an MRA results in a significantincrease in the airway diameter,especially in the oropharyngeal crosssectionalarea, in both obese andnonobese subjects. 5,10,11 This increasein airway caliber results in increasedairflow, reduced snoring, and improvedsleep-disordered breathing.Side Effects and ContraindicationsSide effects <strong>of</strong> MRAs include temporomandibularjoint and facial pain or discomfort,temporomandibular jointnoises, minor tooth movement,changes in occlusion, and skeletalchanges, including increased facialheight. 5,11,12Although oral appliances can be usedsuccessfully in patients who grind theirteeth, use <strong>of</strong> an MRA that allows foradequate lateral and anterior-posteriormovement may be less likely to exacerbatetemporomandibular joint pain.Most side effects that with MRAs areminor and temporary and do notOral Appliances for theTreatment <strong>of</strong> Patients WithObstructive Sleep Apneasignificantly affect appliance use. 5,11,12Contraindications to the use <strong>of</strong>MRAs include severe temporomandibularjoint pain, insufficientteeth to retain the appliance during usage(eight teeth is probably the minimum),teeth that are compromised byperiodontal disease, and a limitedmandibular range <strong>of</strong> motion. 10Oral Appliance Management <strong>of</strong> thePatient With OSAOral appliances are an importantpart <strong>of</strong> the armamentarium for OSAmanagement. Optimal management<strong>of</strong> patients with sleep-disorderedbreathing requires collaboration betweena sleep physician and a dentistwho is well trained in dental sleepmedicine.When evaluating a patient with OSAfor an oral appliance, the dentist does adental sleep workup, which includes athorough review <strong>of</strong> the medical history,an evaluation <strong>of</strong> the nasal cavity,and an in-depth evaluation <strong>of</strong> the oralcavity and the temporomandibularjoints and associated structures. Impressionsfor study and working modelsare taken, as well as a panoramic radiographor other imaging.After an appliance is inserted, thedentist needs to follow up with the patienton a weekly or biweekly basis toassess if the appliance is having an effect.If the appliance is not having aneffect, it is then titrated (by moving themandibular, or lower unit, forward)until it does or it is determined that itis not going to work.A maximum titration <strong>of</strong> 75% <strong>of</strong> thepatient’s protrusion is generally consideredthe endpoint for titration. A repeatsleep study is recommended toassess the efficacy <strong>of</strong> the appliance,once it has been titrated, 4 but it is theauthor’s experience that this happensrarely.Once efficacy <strong>of</strong> the appliance isconfirmed, continued follow-up by thedentist is essential in order to assesstooth movement and other side effects.The patient is generally seen every 6months for the first year and at leastonce a year thereafter.The ACCP Sleep Medicine NetWorkcollaborated with the <strong>American</strong> Academy<strong>of</strong> Or<strong>of</strong>acial Pain to produce aprintable patient education brochureabout oral appliances. This is availableon the ACCP Web site at www.accpstorage.org/newOrganization/patients/oralAppliances.pdf.References1. Cartwright RD, Samelson CF. Theeffects <strong>of</strong> a nonsurgical treatment forobstructive sleep apnea: the tongueretainingdevice. JAMA. 1982;248(6):705-709.2. Krishnan V, Collop NA, Scherr SC.An evaluation <strong>of</strong> a titration strategyfor prescription <strong>of</strong> oral appliances forsleep apnea. <strong>Chest</strong>. 2008;133(5):1135-1140.3. Hoekema A, Stegenga B, WijikstrPJ, vander Hoeven JH, Meinesz AF,de Bont LGM. Obstructive sleep apneatherapy. J Dent Res. 2008;87(9):882-887.4. Kusida CA, Morgenthaler TI, LittnerMR, et al. Practice parameters forthe treatment <strong>of</strong> snoring and obstructivesleep apnea with oral appliancesand update for 2005. Sleep. 2006;29(2):240-243.5. Ferguson KA, Cartwright R, RogersR, Schmidt-Nowara W. Oral appliancesfor snoring and obstructivesleep apnea: a review. Sleep. 2006:29(2):244-262.6. Otsuka R, Ribeiro de Almeida F,Lowe AA, Linden W, Ryan F. Theeffect <strong>of</strong> oral appliance therapy onblood pressure in patients with obstructivesleep apnea. Sleep Breath.2006;10(1):29-36.7. Lam B, Sam K, Mok WY, et al. Randomisedstudy <strong>of</strong> three non-surgicaltreatments in mild to moderate obstructivesleep apnoea. Thorax.2007;62(4):354-359.8. Walker-Engstrom ML, Tegelberg A,Wilhelmsson B, Ringqvist I. 4-year follow-up<strong>of</strong> treatment with dental applianceor uvulopalatopharyngoplasty inpatients with obstructive sleep apnea: arandomized study. <strong>Chest</strong>. 2002;121(3):739-746.9. Vanderveken OM, Devolder A,Marklund M, et al. Comparison <strong>of</strong> acustom-made appliance and a thermoplasticoral appliance for the treatment<strong>of</strong> mild sleep apnea. Am J Respir CritCare Med. 2008;178(2):197-202.10. Hiyama S, Tsuiki S, Ono T, KurodaT, Ohyama K. Effects <strong>of</strong> mandibularadvancement on supine airway size innormal subjects during sleep. Sleep.2003;26(4):440-445.11. Pantin CC, Hillman DR, TennantM. Dental side effects <strong>of</strong> an oral deviceto treat snoring and obstructive sleepapnea. Sleep. 1999;22(2):237-240.12. Marklund M, Stenlund H, FranklinKA. Mandibular advancement devicesin 630 men and women with obstructivesleep apnea and snoring: tolerabilityand predictors <strong>of</strong> treatment success.<strong>Chest</strong>. 2004;125(4):1270-1278.Dr Elmer A. Villalon, DMDOr<strong>of</strong>acial Pain and Dental Sleep MedicinePueblo, CODr Barbara Phillips, MSPH, FCCPPr<strong>of</strong>essor, Division <strong>of</strong> Pulmonary, CriticalCare and Sleep MedicineUniversity <strong>of</strong> Kentucky <strong>College</strong> <strong>of</strong>MedicineLexington, KY
18 NEWS FROM THE COLLEGE JANUARY 2011 • CHEST PHYSICIANAfter only a few weeks, anamazing amount <strong>of</strong> activityhas transpired sinceCHEST 2010! The meeting wasvery successful with over 4,700DR DAVID D. attendees. Kudos to Drs BobGUTTERMAN, FCCP Levy and Ann O’Donnell for awell-run and educationallystimulating conference. I wish to thank the dozens <strong>of</strong>people who took my <strong>of</strong>fer and introduced themselvesduring CHEST and talked about how they would liketo be more involved with the <strong>College</strong>. Their enthusiasmwas one <strong>of</strong> the highlights <strong>of</strong> the meeting for me.In the past several weeks, the ACCP leadership andstaff have been studying the many comments and suggestionsmade during the annual meeting with regardto our ongoing review <strong>of</strong> NetWorks, approach to advocacy,and the ACCP Governors. We are also finalizingour approach to conflict <strong>of</strong> interest, with a policy andimplementation plan to be distributed soon. The<strong>College</strong> will define individual and societal guidelinesand procedures for appropriate restriction <strong>of</strong> bias andensuring compliance across all ACCP activities andfunctions.I would like to update you on two promises I madeduring the Opening Ceremony in Vancouver. Criticalto the success <strong>of</strong> our new strategic plan is enhancedcommunication that supports bidirectional input. Toenhance collaboration between ACCP members andPresidential leaders, the <strong>College</strong> is launching a newblog on its Web site. From the Presidents will featurePRESIDENT’S REPORTProgress and Congratulationsregular blogs from me, as ACCP President; Dr SuhailRao<strong>of</strong>, FCCP, ACCP President-Elect; Dr Darcy D.Marciniuk, FCCP, ACCP President-Designate; and DrKalpalatha K. Guntupalli, FCCP, ACCP ImmediatePast President, about the <strong>College</strong>, medical and healthcareissues, the pr<strong>of</strong>ession, and other member-relatedtopics <strong>of</strong> interest. First, we want to directly informmembers regarding issues important to the ACCP.Second, we want to encourage two-way conversationsby soliciting feedback from members. Importantly, thisis a direct link between membership and the President.The more engaged our members, the more informedthe leadership will be. More thorough vetting<strong>of</strong> issues and projects should lead to stronger finalproducts. This is one step in a more comprehensiveapproach to improved communication that includes aregular Leadership Newsletter and the ACCP News-Brief, which is e-mailed to all members. Our communicationefforts set a new standard just last month,when CHEST became the first North <strong>American</strong> respiratory-focusedjournal to have its own iPhone® andiPad® app. As we modernize our IT systems, look formore innovations to come!Progress has been made on my goal to create aPresidential Task Force on Diversity and Disparity. Iam excited to announce that Dr Marilyn Foreman,MS, FCCP, Department <strong>of</strong> Medicine, MorehouseSchool <strong>of</strong> Medicine in Atlanta, GA, has agreed tochair this task force. Dr Foreman will select task forcemembers and convene an initial meeting at theACCP <strong>of</strong>fices in January 2011. The work <strong>of</strong> this taskforce is a critical component <strong>of</strong> the <strong>College</strong>’s effort toremove barriers to effective patient care that arebased on cultural, ethnic, and societal status. MarilynLederer, CPA, Executive Director <strong>of</strong> The CHESTFoundation, will oversee staffing <strong>of</strong> this task force.I anticipate that the task force will develop a planwith two components. First, the plan will align withthe <strong>College</strong>’s strategic plan, allowing us to more consistentlytap into the inherent diversity <strong>of</strong> our membershipand staff in conducting our business. Second,the plan should inform our efforts to eliminate disparitiesin health care through education, legislation,guideline dissemination, and incorporation <strong>of</strong> bestpractices in health-care delivery.Finally, I wish to recognize two major achievements<strong>of</strong> Dr Suhail Rao<strong>of</strong>, FCCP, President-Elect <strong>of</strong>the ACCP. He has been selected as a Master <strong>of</strong> the<strong>American</strong> <strong>College</strong> <strong>of</strong> <strong>Physicians</strong>. This honor recognizeshis stellar personal character and eminence inthe practice <strong>of</strong> medicine. In addition, Dr Rao<strong>of</strong> hasbeen nominated for membership in the FleischnerSociety, the pre-eminent international society for thoracicradiology. Dr Rao<strong>of</strong> ’s wisdom, leadership, anddedication continue to be <strong>of</strong> exceptional benefit tothe ACCP.I hope everyone had a safe and enjoyable holidayseason, and I extend my best wishes for the newyear. Holiday tip: As you shovel snow from yourdriveway this winter, think about Hawaii andCHEST 2011 to keep warm. It has worked for mealready this season!■CHEST Journal AppComplete full-text articles from CHESTare now available for the iPhone®, iPodtouch®, and iPad®. <strong>Download</strong> the appfor free trial access through June 2011.■ View the table <strong>of</strong> contents, abstract, fulltext, and figures/tables.■ Use enhanced image viewing, includinga full-screen option, and scroll through afigure/table-only view <strong>of</strong> each article.■ Save articles for later reading, or e-mailarticle links to yourself and colleagues.■ Click linked references to view relatedabstracts through the in-app Web browser.The CHEST Foundation is pleased to introduce itsnew OneBreath campaign, an exciting public-facingcampaign that incorporates its three pillars: education,care, and community. OneBreath: Make The Most Of Itemphasizes that living well means breathing well andinspires people to take care <strong>of</strong> their lungs and heart,never taking their next breath for granted.The Foundation’s mission remains the same: toprovide prevention and education programs andvaluable resources in cardiopulmonary and criticalcare medicine. The four focus areas <strong>of</strong> tobaccoprevention and cessation, humanitarian service,clinical research, and critical care/end-<strong>of</strong>-life care,continue to be the core programming elements.Learn MoreSearch “CHEST Journal” in the App Storeor the iTunes® Store.Support OneBreath and Learn Moreonebreath.org
JANUARY 2011 • CHEST PHYSICIAN NEWS FROM THE COLLEGE 19Poster Contest Spreads MessageTo Love Your Lungs“Love Your Lungs” Poster Contestwinner Bailey Selecky’s winningdesign was displayed on T-shirtsfor participants <strong>of</strong> the CHEST 2010 5KWalk/Run held on Tuesday, November 2.“Being healthy and breathing strong isvery important to me as I am a studentathlete and need to be in great physicalshape in order to compete and play toCOURTESY BAILEY SELECKYthe best <strong>of</strong> my ability,” says Bailey. Shealso thanks the Ambassadors Group forletting her help spread the importantmessage to “Love Your Lungs.” Eachyear, the Ambassadors Group sponsorsthe poster contest, which is open toall youth, ages 8 to 14. Contactlfulton@chestnet.org for 2011 entryforms or more information. ■The winning poster in the “Love Your Lungs” Poster Contest was created byBailey Selecky, a student athlete who enjoys “being healthy and breathing strong.”COURTESY ACCPProduct <strong>of</strong> the MonthCHESTSoundings – CHEST 2010Symposia WebcastsThe CHESTSoundings Webcastsprovide you with the opportunity toreview the clinical information relevantto the chest pr<strong>of</strong>essional healthcarecommunity presented duringthe Morning Educational Symposiasessions during CHEST 2010.The Webcast presentations can beconveniently viewed at www.chestnet.org/accp/chestsoundings.These resources present varioushot-topic medical issues relevant toyour clinical practice and the careyou provide to your patients.We trust this educational mediumwill prove useful and also serve as acatalyst for you to share your innovativeideas, opinions, and challengesfaced within your own medical community.This resource is fun and collaborative.After you view the activities,you may claim credit via the ACCPcontinuing medical education site athttps://accp.chestnet.org/loginWA/LoginDispatchAction.do?wa=cme3. ■COPD AllianceSpirometer GiveawayRegistered RespiratoryTherapist and asthmaeducator DianeRhodes <strong>of</strong> San Antoniowas the winner <strong>of</strong>the COPD Alliancespirometer giveawayduring CHEST 2010.Members <strong>of</strong> the newlylaunched COPD Alliance presentedMs. Rhodes with a new Nddspirometer as part <strong>of</strong> the Alliance’smission to encourage the earlydiagnosis <strong>of</strong> COPD. Ms. Rhodesplans to use the spirometer forscreeningthe employees<strong>of</strong>the schooldistrictwhere she works; doing communityscreenings at clinics in theSan Antonio area; and monitoringlung function in more than 200children with asthma who shecounsels.■October 30 - November 4Vancouver, BC, CanadaSpecialty Medicine.Specialty Codes.Best <strong>of</strong> CHEST 2010 On DemandPurchase over 100 sessions and slides presented at CHEST 2010,so you can review clinical content at your convenience.NN<strong>Download</strong> mp4 and mp3 files, or watch on CD-ROM.Transfer content to an iPhone®, iPad, or iPod® touch.Focused tracks also available:Pulmonary Arterial HypertensionInterventional and Bronchoscopy ProceduresCOPDAdvanced UltrasonographyNew! 15th EditionFor a coding resource as preciseand specialized as the medicine youpractice, turn to Coding for <strong>Chest</strong>Medicine 2011. Perfect for physicians,nonphysician providers, practiceadministrators/managers, <strong>of</strong>ficemanagers, and business managers.ACCP Member $125Nonmember $160Product #18112011Learn More and Orderwww.dcprovidersonline.com/accpTHE AUTHORITY IN CLINICAL CHEST MEDICINEcurrentproceduralterminologyPr<strong>of</strong>essional EditionCPT® 2011Pr<strong>of</strong>essionalEditionMember $105*Nonmember $105*Product #1812*Plus shipping and handlingYour Trusted Source!The only <strong>of</strong>ficial CPT ® codebook with rulesand guidelines from the AMA’s CPT Editorial Panelwww.chestnet.org
20 NEWS FROM THE COLLEGE JANUARY 2011 • CHEST PHYSICIANVolunteers Reach Out toChildren During Annual MeetingThe CHEST Foundation and the ACCPIndustry Advisory Council 2010Community Outreach EventOn Monday, November 1, duringCHEST 2010, more than 40 ACCPandAmbassadors Group–membervolunteers attended a training sessionand then boarded a bus toLaura Secord Elementary School inVancouver. This was the 12th yearthat volunteers from both the USand international locations reachedout to children in the annual CHESTmeeting’s host city to present aboutlung health and the dangers <strong>of</strong>tobacco. Approximately100 6thgraders interactedwith the presentersand “student buddies”during thisprogram, whichutilizes differentaspects <strong>of</strong> TheFoundation’s LungLessons SM program.Comments gatheredafter the programindicate that themessage made itOctober 22 - 27Honolulu, Hawaiito the young listeners and included:“I learned a lot more about howsmoking affects your lungs. I willnever smoke, so I can stay healthyand live longer.”“I learned that rat poison is incigarettes.”“All cigarettes are bad, even if they(advertisers) say it’s good.”The ACCP Industry AdvisoryCouncil presented a $10,000 grant toVancouver School District 39, whichincludes Laura Secord ElementarySchool. The funds will be used forhealth education classes and otherenrichment activities.■Monir Almassi (left) and Dr Norma Braun present tipsfor good lung health to elementary schoolchildren.CHEST 2011OpportunitiesCall for AbstractsSubmit an abstract <strong>of</strong> your original investigative workfor presentation at the meeting. Submission is free toACCP members.Watch for details and submission opportunities,coming January 31.www.accpmeeting.orgSubmission deadline: May 4Call for Case ReportsACCP affiliate members are invited to submit casereports for presentation during special sessions.Watch for details and submission opportunities,coming January 31.www.accpmeeting.orgSubmission deadline: May 4The CHEST Foundation 2011Awards ProgramMore Than $500,000 To Be AwardedThe CHEST Foundation tradition <strong>of</strong> recognizing andrewarding health-care pr<strong>of</strong>essionals for volunteerservice, leadership, and clinical research continuesin 2011. You could be eligible.Watch for details and application opportunities,coming in January.onebreath.orgApplication deadline: May 4COURTESY ACCPMany Winners at CHEST2010—Congratulations!ACCP Honor Awards S<strong>of</strong>fer Award for EditorialExcellenceArmin Ernst, MD, FCCP Alton Ochsner AwardRelating Smoking andHealthJerome S. Brody, MDKenneth E. Warner, PhDCanadian ThoracicSociety Awards CTS Annual ChristieMemorial LecturerJerome A. Dempsey, PhD CTS Institute <strong>of</strong> Circulatoryand Respiratory HealthDistinguished Lecturer inthe Respiratory SciencesJames C. Hogg, MD, PhD,FCCPThe CHEST FoundationAwards Third GlaxoSmithKlineDistinguished Scholar inRespiratory HealthSandra G. Adams, MD,FCCP D. Robert McCaffree, MD,Master FCCP HumanitarianAwards$10,000 HumanitarianAwardRobert C. Hyzy, MD,FCCP$7,500 HumanitarianAwardsMargaret A. Clark, RRTKevin R. Flaherty, MD,FCCPSyed S. Naqvi, MD, FCCPC. Sola Olopade, MD,FCCP$5,000 Ambassadors GroupHumanitarian RecognitionAwardLata R. Casturi, MA <strong>American</strong> Lung Associationand The CHESTFoundation Asthma ClinicalPatient Care ResearchAwardShamsah Kazani, MBBS Roger C. Bone Advancesin End-<strong>of</strong>-Life Care AwardDee W. Ford, MD, FCCP Alpha-1 Foundation andThe CHEST FoundationClinical Research Award inCOPD and Alpha-1 Antitrypsin(AAT) DeficiencyAnn E. Tilley, MD Association <strong>of</strong> SpecialtyPr<strong>of</strong>essors and TheCHEST Foundation <strong>of</strong> theACCP Geriatric DevelopmentResearch AwardJessica Y. Chia, MD The CHEST FoundationCalifornia Chapter ClinicalResearch/MedicalEducation AwardHubert Chen, MD, FCCP The CHEST Foundationand the RespiratoryHealth Association<strong>of</strong> Metropolitan ChicagoClinical ResearchAward in Women’sLung HealthJacob Allan Udell, MDAlfred S<strong>of</strong>fer ResearchAward Winners$1,500 award winnersMary Cataletto, MD,FCCPMatthew J. Schuchert,MD$1,000 award winnersSneh Arora, PhDChristopher Carroll, MD,FCCPLee Morrow, MD, FCCPRan Wang, MDYoung InvestigatorAward Winners$2,000 award winnersTakahiro Nakajima, MDBryon N. Johnson, DO$1,250 award winnersLaura Barber, MDMichelle Kompare, MDAra Chrissian, MDAbdelbaset MohamedSaleh, MDTop Five Poster AwardWinnersWilliam Carroll, MDRenee Benson, MDCaroline Chapman, PhDDavid S. Hui, MD, FCCPJi-Young SonCase Report AwardWinnersThomas C. Iden III, MDAditya Gupta, MBBSRupesh K. Dave, MDNishant Gupta, MDJarrod T. Bruce, MDAnkur Kalra, MDAbhijit A. Raval, MDDavid Wallace, MDHeba Ismail, MBChBJamie L. Bessich, MDJorge E. GuerreroEspinosa, MDGarrett Bird, MDKrithika Ramachandran,MDSonali Bose, MDNichole T. Tanner, MDSunita Mulpuru, MDJessica E. Freyer, MDArvind Ponnambalam,MDLeon C. Bass, MDAnushya Chelvanathan,MBChBMuhammad T. Akbar, MDLuis A. Martin-Del-Campo, MDSurya Prakash Bhatt,MDTomio Miyai, MDCHEST 2010 BingoWinners CHEST BingoAlesia S. Svymbersky, PAAndre L. Smith, MD,FCCPRita Wittmann, MDBrent Toney, DOAnwar M. Haque, MD COPD BingoMaximiliano A. TamaeKakazu, MDChamani Illamperuma,MBBSLeticia MendozaMuzquiz, MD, FCCPJane Wheeler, MDMaria Paz B. Meteo, MD PAH BingoTony Abed, MD, FCCPEricilia Arias, MD, FCCPSteven Chambers, MD,FCCPMichael Gabrilovich, MD,PhD, FCCPNelson Yu, MDBest Educational Activity,Clinical Resource CenterClusters AirwayBroncus Technologies,Inc. CardiovascularGilead Sciences, Inc. Critical CareSimbionix USA Corporation DiagnosticsMorgan Scientific Inc. Pr<strong>of</strong>essional DevelopmentCOPD Alliance SleepResMedCHEST ChallengeWinners First Place: NationalCapital ConsortiumPulmonary andCritical Care FellowshipProgramCPT Matthew AboudaraLT Gregory Fuhrer, MC,USNLT Scott Parrish, MC,USN Second Place: MaimonidesMedical CenterPrashant Gundre, MBBSArjun Madhavan, MBBSKavan Ramachandran,MBBS Third Place: Baylor<strong>College</strong> <strong>of</strong> MedicineSoma Jyothula, MBBSAmarbir Mattewal, MDVishal Sawhney, MDPages 20a—20b
JANUARY 2011 • CHEST PHYSICIAN NEWS FROM THE COLLEGE 21Humanitarian Award Winners, Outgoing Chair HonoredThe CHEST Foundation’s12th Annual Making aDifference Awards Ceremonyand Presentation duringCHEST 2010 focused on theD. Robert McCaffree, MD,Master FCCP HumanitarianAward winners. This year’saward winners and their projectswere: Margaret A. Clark, RRT,Not One More Life AsthmaClinic, Atlanta, GA Dr Kevin R. Flaherty, FCCP,Faith Medical Clinic, Pinckney,MI Dr Robert C. Hyzy, FCCP,Toward a Sustainable Model <strong>of</strong>Care Delivery to the Indigent<strong>of</strong> Belen, Peru Dr Syed S. Naqvi, FCCP,Sustainable Health-care InitiativesNow Empowering(SHINE), USA in Affiliationwith Comprehensive DisasterResponse Services (CDRS) inChikar, District Muzaffarabad,Pakistan Dr C. Sola Olopade, FCCP,Protecting Women and ChildrenFrom Exposure toIndoor Air Pollution FromBurning Biomass in Eruwa,Abanla, and Igbo Ora, NigeriaHumanitarian award winners (L-R): Margaret A. Clark, RRT;Dr Kevin R. Flaherty, FCCP; Dr Robert C. Hyzy, FCCP;Dr Syed S. Naqvi, FCCP; and Dr C. Sola Olopade, FCCP.The Ambassadors GroupHumanitarian Award winnerwas Lata R. Casturi, MA, ProjectS.I.E.S.T.A. (Students Involvedin the Education AboutSleep Hygiene for Teen Adolescents),Houston, TX.Each award winner prepareda video clip <strong>of</strong> their project,and these will be postedon The Foundation’s YouTubechannel very soon. We encourageyou to take the timeto view them (www.youtube.com/user/<strong>Chest</strong>Foundation).The CHEST Foundationwas proud to have the followingcorporate partnerssponsor this year’s dinner:AstraZeneca LP; BoehringerIngelheim Pharmaceuticals,Inc.; Eisai, Inc.; Genentechand Novartis; Gilead Sciences,Inc.; Merck & Co., Inc.;Ortho-McNeil Janssen Pharmaceuticals;Pfizer, Inc.; andsan<strong>of</strong>i-aventis, US.Another highlight <strong>of</strong> theevening was a tribute to outgoingChair <strong>of</strong> The CHESTFoundation Board <strong>of</strong>Trustees, Dr Robert G. Johnson,FCCP. A tribute videowas shown depictingHonoree Dr Robert G. Johnson, FCCP (left), outgoing Chair <strong>of</strong>The CHEST Foundation Board, with Dr John C. Alexander Jr, FCCP.Dr Johnson’s long career asACCP’s Past President (2000)and the many accomplishmentsduring his tenure onThe Foundation’s Board(2000-2010). Close friends andcolleagues took the opportunityto participate in thisfarewell tribute by sharingsome <strong>of</strong> their own humorousstories.Dr Johnson’s contributionsto The CHEST Foundationinclude the formation <strong>of</strong> aDevelopment CommitteeGlimpses <strong>of</strong> CHEST 2010 in Vancouverresponsible for the oversight <strong>of</strong>fundraising and establishingendowments, as well as thereorganization <strong>of</strong> the AwardsCommittee to become arepository for all <strong>College</strong>awards. The Foundation ispleased that Dr Johnson hasaccepted the role <strong>of</strong> Chair <strong>of</strong>the OneBreath: Make TheMost Of It initiative and willremain a resource to TheCHEST Foundation as itlaunches this importantinitiative.■COURTESY ACCPCHEST Challenge winners from the National CapitalConsortium Pul/CC Fellowship Program.Dr Alfred S<strong>of</strong>fer, Master FCCP, takes a turn atvirtual reality learning in Experience ACCP.Meeting attendees appreciated the chance to learnnew procedures through simulation.PHOTOS COURTESY ACCPPictures from CHEST2010 are available forviewing and purchase atwww.lagniappestudio.com/chest2010. Plannow to attend CHEST2011, Oct. 22-27, in Honolulu,Hawaii.There was plenty <strong>of</strong> activity at Experience ACCP in theexhibit hall.The Cyber Café gets more popular among meeting attendees with everypassing year.
22 SLEEP MEDICINE JANUARY 2011 • CHEST PHYSICIANHome Testing for Sleep Apnea Not InferiorBY SUSAN LONDONElsevier Global Medical NewsVANCOUVER, B.C. – Recent researchon the use <strong>of</strong> home testing for the diagnosis<strong>of</strong> obstructive sleep apnea and initiation<strong>of</strong> therapy suggests that “hometesting is here to stay,” Dr. Charles W.Atwood Jr., FCCP, said at CHEST 2010,the annual meeting <strong>of</strong> the <strong>American</strong><strong>College</strong> <strong>of</strong> <strong>Chest</strong> <strong>Physicians</strong>.For more than 30 years, physicianshave relied on the traditional polysomnographyperformed in the sleeplaboratory to diagnose sleep apnea, accordingto Dr. Atwood. But with growingawareness <strong>of</strong> the condition and its prevalence,the number <strong>of</strong> people needingtesting could overwhelm capacity.“If you take the millions and millionsand millions <strong>of</strong> people in the UnitedStates alone who have sleep apnea andtry to feed them through the relativelysmall funnel <strong>of</strong> traditional sleep labs,then you are going to have big bottlenecks,”he said, adding that such bottlenecksalready exist in some areas.However, home-testing devices mustmeet certain key requirements before theyare ready for widespread use. For example,CLASSIFIEDSAlso available at www.imngmedjobs.comPROFESSIONAL OPPORTUNITIESMetro South CarolinaHospital employed joining well establishednine physician Pulmonary/CCgroup in desirable Blue Ridge Metroarea two hours to Atlanta and Charlotteassociated with a growing 450 bed hospitalsystem. 1-10 call. Excellent negotiablesalary, bonus and benefits. DONO-HUE AND ASSOCIATES 800-831-5475F: 314-984-8246E/M: donohueandassoc@aol.comPulmonology/CriticalCare <strong>Physicians</strong>Practice Opportunity for BC/BE Pulmonology/CriticalCare <strong>Physicians</strong> inBeautiful Hendersonville, Western NorthCarolina. Sleep Medicine preferred butnot required. Full-time or Part-time availability.Competitive salary & benefits. NoVisa sponsorship available. For consideratione-mail CV to:lilly.bonetti@pardeehospital.orgor Fax CV to 828-694-7722.Moving?Look to Classified Notices for practicesavailable in your area.For Deadlines and MoreInformation Contact:Rhonda Beamer443-512-8899 Ext 106FAX: 443-512-8909Email: rhonda.beamer@wt-group.comthey have to be simpler than those used inthe lab. “Perhaps we can get by withfewer [physiological] signals, but we needto understand what the key signals are,”commented Dr. Atwood, a pulmonologistand sleep medicine specialist with the VAPittsburgh Healthcare System and theUniversity <strong>of</strong> Pittsburgh Medical Center.Home testing devices will also need tobe accurate, with high sensitivity andspecificity, and “there is no single deviceI would say today that is perfect in boththese regards,” he noted. Finally, theymust be easy to use and durable, giventhe demands <strong>of</strong> in-home use.Roughly 95 studies conducted between1990 and 2006 evaluated home testing(also called portable monitoring) for thediagnosis <strong>of</strong> obstructive sleep apnea. Collectively,they had some limitations, suchas their single-site nature, small andusually homogeneous populations, andvarying degrees <strong>of</strong> rigor in design.“And they frequently focused on thehighest-risk subjects: These were middleagedmen who were overweight, snored,and were sleepy, so [they were] the verylow-hanging fruit for typical sleep apnea,”Dr. Atwood said.These studies showed some mixed re-Pulmonary/Critical CareThe VA Medical Center in Milwaukee,Wisconsin is a large tertiary care facilityaffiliated with the Medical <strong>College</strong> <strong>of</strong>Wisconsin. Openings exist for pulmonaryand critical care medicine physicians tojoin the section <strong>of</strong> Pulmonary, CriticalCare Medicine and Sleep Medicine.Qualified candidates must be Board certifiedor eligible in Pulmonary Diseaseand Critical Care Medicine and have thequalifications for a Faculty appointmentat the Medical <strong>College</strong> <strong>of</strong> Wisconsin.Fellowship training in sleep medicine isa plus. Pr<strong>of</strong>essional and academic opportunitiesexist through the Medical <strong>College</strong><strong>of</strong> Wisconsin and the Department <strong>of</strong>Veterans Affairs. Interested candidatesshould send a current Curriculum Vitae,referencing Pulmonary, to: Clement J.Zablocki VA Medical Center, Human ResourcesAttn: Prudy Kitterman, 5000 W.National Avenue, Milwaukee, WI 53295,prudy.kittermann@va.gov fax to 414-382-5296. Additional inquiries should bedirected to Andreea Antonescu, MD at414-384-2000 X42765 or email toandreea.antonescu-turcu@va.govDisclaimer<strong>Chest</strong> Physician assumes the statementsmade in classified advertisements are accurate,but cannot investigate the statementsand assumes no responsibility or liabilityconcerning their content. ThePublisher reserves the right to decline,withdraw, or edit advertisements. Every effortwill be made to avoid mistakes, butresponsibility cannot be accepted for clericalor printer errors.sults when it came to the diagnosticperformance <strong>of</strong> home testing relative tolab testing. “There is no perfect study, atleast so far, in this area, but some havecome pretty close,” he commented.Three more-recent studies suggest thathome testing is at least not inferior to labtesting for sleep apnea diagnosis and initiation<strong>of</strong> continuouspositive airwaypressure (CPAP)therapy, accordingto Dr. Atwood.In the first study,conducted in 68people with a highlikelihood <strong>of</strong> sleepapnea, the apneahypopneaindex onCPAP and Sleep Apnea Quality <strong>of</strong> Life Indexscores at 3 months did not differ significantlybetween a sleep lab and anambulatory approach (Ann. Intern. Med.2007;146:157-66). The rate <strong>of</strong> adherenceto CPAP was better with the latter.In the second study, which involved102 patients with sleep apnea symptomsand no major comorbidities, all <strong>of</strong> a variety<strong>of</strong> sleep and quality <strong>of</strong> life outcomesafter 4 weeks <strong>of</strong> CPAP weresimilar with a standard lab diagnosis andtreatment approach vs. a home approach(<strong>Chest</strong> 2010;138:257-63).The third study, the Veterans SleepApnea Treatment Trial (VSATT), is thelargest study <strong>of</strong> home testing in NorthAmerica to date, according to Dr. Atwood,one <strong>of</strong> the principal investigators.“The VA is ill equipped to managesleep apnea in a conventional way becausewe have relatively few numbers <strong>of</strong>traditional sleep labs,” he noted.“Our study differed from basically all <strong>of</strong>the other studies in the literature in thatwe had very broad inclusion criteria andvery nonrestrictive exclusion criteria,”Dr. Atwood noted. For example, patientswith comorbidities could participate aslong as their condition was stable.Patients were randomized to lab testingor home testing, followed by initiation <strong>of</strong>CPAP for those with positive results.Among the 223 who were started onCPAP, the home and lab groups had‘Functionalimprovement withCPAP for sleepapnea is not worsewhen treated inthe home settingvs. the sleep lab.’DR. ATWOODsimilar demographics. The average apneahypopneaindex was 41 for the former and45 for the latter. The Functional Outcomes<strong>of</strong> Sleep Questionnaire (FOSQ)total score was about 15 in each group.Results showed that the mean adjustedimprovement in FOSQ total score betweenbaseline and 3 months was identicalin the twogroups, at 1.79points. And withineach group, patientshad significantimprovementsin the total score aswell as its individualcomponents.Both home andlab groups also hadsignificant improvements on the EpworthSleepiness Scale (–2.6 and –2.9, respectively),the mental health component<strong>of</strong> the 12-item Short Form Health Survey(+2.5 and +3.0), and the Center for EpidemiologicStudies–Depression scale(–1.4 and –2.2). Neither group improvedsignificantly on the psychovigilance taskor the physical health component <strong>of</strong> the12-item Short Form Health Survey.When it came to adherence, whichwas monitored with smart cards, themean adjusted number <strong>of</strong> CPAP hoursdaily was 3.42 in the home group and2.99 in the lab group, a difference thatwas not significant. Cost-effectivenessanalyses are still ongoing.“We concluded that the functional improvementwith CPAP for sleep apnea isnot worse when treated in the home settingvs. the sleep lab,” Dr. Atwood said.“We believe ... home-based sleep apneadiagnosis and initiation <strong>of</strong> CPAP therapyis an effective way to treat sleep apnea.”While home testing won’t entirely replacelaboratory polysomnography, Dr.Atwood suggested trying to “integratehome sleep testing with full polysomnographyin a clinically rational way.”Dr. Atwood reported that he receivedresearch support from Embla, Resmed,and Respironics, and is a consultant toEmbla and Itamar Medical, all <strong>of</strong> whichmanufacture testing and treatment devicesfor sleep disorders.■Satisfaction With Medicine Low Among U.S. <strong>Physicians</strong>New ZealandNorwayNetherlandsUnited KingdomSwedenItalyFranceCanadaUnited StatesAustraliaD A T A W A T C H36545454495449596668SatisfiedVerysatisfiedGermany 34 50 20% 40% 60% 80% 100%Note: Data collected from 10,320 primary care physicians from February to July 2009.Source: The Commonwealth Fund1215302127183535822ELSEVIER GLOBAL MEDICAL NEWS
JANUARY 2011 • CHEST PHYSICIAN SLEEP MEDICINE 23CPAP Reverses Left Atrial,Ventricular RemodelingBY BRUCE JANCINElsevier Global Medical NewsSAN ANTONIO – Six months <strong>of</strong> continuouspositive airway pressure therapymarkedly improved adverse left ventricularand atrial remodeling in patientswith moderate to severe obstructivesleep apnea in a prospective study.Diastolic as well as systolic abnormalitieswere reversed, raising the welcomeprospect that CPAP is likely to preventthe development <strong>of</strong> one <strong>of</strong> the mostdreaded complications <strong>of</strong> severe obstructivesleep apnea (OSA) – chronicheart failure – although this point remainsspeculative, Dr. Saleh Al-Mutairisaid at the annual meeting <strong>of</strong> the AssociatedPr<strong>of</strong>essional Sleep Societies.He recruited 32 patients with newlydiagnosed moderate to severe OSA forthe study, which involved serial followupby cardiac magnetic resonance(CMR), echocardiography, and cardiacbiomarkers through 6 months <strong>of</strong> individuallytitrated CPAP therapy.The subjects averaged 51 years <strong>of</strong> age,with a mean baseline apnea-hypopneaindex <strong>of</strong> 53 events/hr and a body massindex <strong>of</strong> 34.5 kg/m 2 . None <strong>of</strong> the participantshad known cardiac disease. Adherenceto CPAP was good. Thepatients’ weight didn’t change significantlyduring the study, and those beingtreated for hypertension remained onthe same doses <strong>of</strong> medication throughoutthe follow-up period.Other studies have shown improvementin left ventricular dysfunction withCPAP, but they were short-term trials.This is the first study with follow-up aslong as 6 months using both CMR andechocardiography, said Dr. Al-Mutairi <strong>of</strong>the University <strong>of</strong> Manitoba, Winnipeg.He focused on the CMR results becausehe considers that technology morereliable than echocardiography for assessingventricular size and function.The echo findings, however, corroboratedthe CMR results.Most <strong>of</strong> the left ventricular measurementsfollowed during the study wereabnormal at baseline. The 6-month resultsincluded a 25% reduction frombaseline in left ventricular end-diastolicvolume and a 19% decrease in left ventricularmass. (See box, above right.)Dr. Al-Mutairi drew particular attentionto the 30% reduction in left atrial volumeindex, which he considers highly encouraging.“The treatment <strong>of</strong> OSA with CPAPmay prevent the left atrial remodelingmeasured by CMR and echo as the leftatrial volume index. This is a very importantpoint, given the association betweenthe left atrial volume andcardiovascular events,” he observed.There was no significant change inC-reactive protein, brain natriuretic peptide,or other cardiac biomarkers duringthe 6 months <strong>of</strong> CPAP use.The mechanism by which OSA isthought to predispose to heart failure involvesan exaggerated negative thoracicpressure in response to the apneicepisodes. This presumably leads to increasedleft ventricular systolic transmuralpressure, which the left atriumresists, with resultant increased complianceand atrial overstretching, Dr. Al-Mutairi explained.Dr. Al-Mutairi reported having no financialconflicts.■TYGACIL ® (tigecycline) Brief SummarySee package insert for full Prescribing Information. For further product information and current package insert, pleasevisit www.wyeth.com or call our medical communications department toll-free at 1-800-934-5556.INDICATIONS AND USAGETYGACIL is indicated for the treatment <strong>of</strong> adults with complicated skin and skin structure infections caused byEscherichia coli, Enterococcus faecalis (vancomycin-susceptible isolates), Staphylococcus aureus (methicillinsusceptibleand -resistant isolates), Streptococcus agalactiae, Streptococcus anginosus grp. (includes S. anginosus,S. intermedius, and S. constellatus), Streptococcus pyogenes, Enterobacter cloacae, Klebsiella pneumoniae, andBacteroides fragilis.TYGACIL is indicated for the treatment <strong>of</strong> adults with complicated intra-abdominal infections caused by Citrobacterfreundii, Enterobacter cloacae, Escherichia coli, Klebsiella oxytoca, Klebsiella pneumoniae, Enterococcus faecalis(vancomycin-susceptible isolates), Staphylococcus aureus (methicillin-susceptible and -resistant isolates),Streptococcus anginosus grp. (includes S. anginosus, S. intermedius, and S. constellatus), Bacteroides fragilis,Bacteroides thetaiotaomicron, Bacteroides uniformis, Bacteroides vulgatus, Clostridium perfringens, andPeptostreptococcus micros.TYGACIL is indicated for the treatment <strong>of</strong> adults with community-acquired pneumonia infections causedby Streptococcus pneumoniae (penicillin-susceptible isolates), including cases with concurrent bacteremia,Haemophilus influenzae (beta-lactamase negative isolates), and Legionella pneumophila.CONTRAINDICATIONSTYGACIL is contraindicated for use in patients who have known hypersensitivity to tigecycline.WARNINGS AND PRECAUTIONSAnaphylaxis/Anaphylactoid ReactionsAnaphylaxis/anaphylactoid reactions have been reported with nearly all antibacterial agents, includingTYGACIL, and may be life-threatening. TYGACIL is structurally similar to tetracycline-class antibiotics andshould be administered with caution in patients with known hypersensitivity to tetracycline-class antibiotics.Hepatic EffectsIncreases in total bilirubin concentration, prothrombin time and transaminases have been seen in patients treatedwith tigecycline. Isolated cases <strong>of</strong> significant hepatic dysfunction and hepatic failure have been reported in patientsbeing treated with tigecycline. Some <strong>of</strong> these patients were receiving multiple concomitant medications. Patientswho develop abnormal liver function tests during tigecycline therapy should be monitored for evidence <strong>of</strong> worseninghepatic function and evaluated for risk/benefit <strong>of</strong> continuing tigecycline therapy. Adverse events may occur after thedrug has been discontinued.Mortality Imbalance and Lower Cure Rates in Ventilator-Associated PneumoniaA study <strong>of</strong> patients with hospital acquired pneumonia failed to demonstrate the efficacy <strong>of</strong> TYGACIL. In this study,patients were randomized to receive TYGACIL (100 mg initially, then 50 mg every 12 hours) or a comparator. In addition,patients were allowed to receive specified adjunctive therapies. The sub-group <strong>of</strong> patients with ventilator-associatedpneumonia who received TYGACIL had lower cure rates (47.9% versus 70.1% for the clinically evaluable population)and greater mortality (25/131 [19.1%] versus 14/122 [11.5%]) than the comparator.Use During PregnancyTYGACIL may cause fetal harm when administered to a pregnant woman. If the patient becomes pregnantwhile taking tigecycline, the patient should be apprised <strong>of</strong> the potential hazard to the fetus. Results <strong>of</strong> animal studiesindicate that tigecycline crosses the placenta and is found in fetal tissues. Decreased fetal weights in rats and rabbits(with associated delays in ossification) and fetal loss in rabbits have been observed with tigecycline [see USE INSPECIFIC POPULATIONS].Tooth DevelopmentThe use <strong>of</strong> TYGACIL during tooth development (last half <strong>of</strong> pregnancy, infancy, and childhood to the age <strong>of</strong>8 years) may cause permanent discoloration <strong>of</strong> the teeth (yellow-gray-brown). Results <strong>of</strong> studies in rats withTYGACIL have shown bone discoloration. TYGACIL should not be used during tooth development unless other drugsare not likely to be effective or are contraindicated.Clostridium difficile-Associated DiarrheaClostridium difficile-associated diarrhea (CDAD) has been reported with use <strong>of</strong> nearly all antibacterial agents, includingTYGACIL, and may range in severity from mild diarrhea to fatal colitis. Treatment with antibacterial agents alters thenormal flora <strong>of</strong> the colon leading to overgrowth <strong>of</strong> C. difficile. C. difficile produces toxins A and B which contribute tothe development <strong>of</strong> CDAD. Hypertoxin producing strains <strong>of</strong> C. difficile cause increased morbidity and mortality, as theseinfections can be refractory to antimicrobial therapy and may require colectomy. CDAD must be considered in all patientswho present with diarrhea following antibiotic use. Careful medical history is necessary since CDAD has been reportedto occur over two months after the administration <strong>of</strong> antibacterial agents. If CDAD is suspected or confirmed, ongoingantibiotic use not directed against C. difficile may need to be discontinued. Appropriate fluid and electrolytemanagement, protein supplementation, antibiotic treatment <strong>of</strong> C. difficile, and surgical evaluation should be institutedas clinically indicated.Patients With Intestinal PerforationCaution should be exercised when considering TYGACIL monotherapy in patients with complicated intra-abdominalinfections (cIAI) secondary to clinically apparent intestinal perforation. In cIAI studies (n=1642), 6 patients treated withTYGACIL and 2 patients treated with imipenem/cilastatin presented with intestinal perforations and developed sepsis/septic shock. The 6 patients treated with TYGACIL had higher APACHE II scores (median = 13) versus the 2 patientstreated with imipenem/cilastatin (APACHE II scores = 4 and 6). Due to differences in baseline APACHE II scores betweentreatment groups and small overall numbers, the relationship <strong>of</strong> this outcome to treatment cannot be established.Tetracycline-Class EffectsTYGACIL is structurally similar to tetracycline-class antibiotics and may have similar adverse effects. Such effectsmay include: photosensitivity, pseudotumor cerebri, and anti-anabolic action (which has led to increased BUN, azotemia,acidosis, and hyperphosphatemia). As with tetracyclines, pancreatitis has been reported with the use <strong>of</strong> TYGACIL.SuperinfectionAs with other antibacterial drugs, use <strong>of</strong> TYGACIL may result in overgrowth <strong>of</strong> non-susceptible organisms, including fungi.Patients should be carefully monitored during therapy. If superinfection occurs, appropriate measures should be taken.Development <strong>of</strong> Drug-Resistant BacteriaPrescribing TYGACIL in the absence <strong>of</strong> a proven or strongly suspected bacterial infection is unlikely to provide benefitto the patient and increases the risk <strong>of</strong> the development <strong>of</strong> drug-resistant bacteria.ADVERSE REACTIONSBecause clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinicaltrials <strong>of</strong> a drug cannot be directly compared to rates in the clinical trials <strong>of</strong> another drug and may not reflect the ratesobserved in practice.In clinical trials, 2514 patients were treated with TYGACIL. TYGACIL was discontinued due to adverse reactions in7% <strong>of</strong> patients compared to 6% for all comparators. Table 1 shows the incidence <strong>of</strong> treatment-emergent adversereactions through test <strong>of</strong> cure reported in 2% <strong>of</strong> patients in these trials.Table 1. Incidence (%) <strong>of</strong> Adverse Reactions Through Test <strong>of</strong> CureReported in 2% <strong>of</strong> Patients Treated in Clinical StudiesBody System TYGACIL Comparators aAdverse Reactions (N=2514) (N=2307)Body as a WholeAbdominal pain 6 4Abscess 3 3Asthenia 3 2Headache 6 7Infection 8 5Cardiovascular SystemPhlebitis 3 4Digestive SystemDiarrhea 12 11Dyspepsia 2 2Nausea 26 13Vomiting 18 9Hemic and Lymphatic SystemAnemia 4 5Metabolic and NutritionalAlkaline Phosphatase Increased 4 3Amylase Increased 3 2Bilirubinemia 2 1BUN Increased 3 1Healing Abnormal 4 3Hypoproteinemia 5 3SGOT Increased b 4 5SGPT Increased b 5 5Nervous SystemDizziness 3 3Skin and AppendagesRash 3 4Key Cardiac Magnetic Resonance ChangesWithin 6 Months <strong>of</strong> CPAPBaselineFollow-upLeft ventricularend-systolic volume 68 mL 53 mLLeft ventricularend-diastolic volume 199 mL 150 mLLeft ventricular mass 184 g 149 gLeft atrial volume index 49 mL/m 2 34 mL/m 2Notes: Based on a study <strong>of</strong> 32 patients with moderate to severe obstructive sleepapnea. All reductions are statistically significant.Source: Dr. Al-MutairiaVancomycin/Aztreonam, Imipenem/Cilastatin, Lev<strong>of</strong>loxacin, Linezolid.bLFT abnormalities in TYGACIL-treated patients were reported more frequently in the post therapy period than thosein comparator-treated patients, which occurred more <strong>of</strong>ten on therapy.In all Phase 3 and 4 studies that included a comparator, death occurred in 3.9% (147/3788) <strong>of</strong> patients receivingTYGACIL and 2.9% (105/3646) <strong>of</strong> patients receiving comparator drugs. An increase in all-cause mortality has beenobserved across phase 3 and 4 clinical studies in TYGACIL treated patients versus comparator. The cause <strong>of</strong>this increase has not been established. This increase should be considered when selecting among treatmentoptions. (See Table 2.)Table 2. Patients with Adverse Events with Outcome <strong>of</strong> Death by Infection TypeTYGACIL Comparator Risk Difference*Infection Type n/N % n/N % % (95% CI)Approved IndicationscSSSI 12/834 1.4 6/813 0.7 0.7 (-0.5, 1.9)cIAI 40/1382 2.9 27/1393 1.9 1.0 (-0.3, 2.2)CAP 12/424 2.8 11/422 2.6 0.2 (-2.3, 2.7)Combined 64/2640 2.4 44/2628 1.7 0.7 (-0.0, 1.6)Unapproved IndicationsHAP 65/467 13.9 56/467 12.0 1.9 (-2.6, 6.4)Non-VAP a 40/336 11.9 42/345 12.2 -0.3 (-5.4, 4.9)VAP a 25/131 19.1 14/122 11.5 7.6 (-2.0, 16.9)RP 11/128 8.6 2/43 4.7 3.9 (-9.1, 11.6)DFI 7/553 1.3 3/508 0.6 0.7 (-0.8, 2.2)Combined 84/1148 7.2 61/1018 6.0 1.2 (-1.0, 3.4)CAP = Community-acquired pneumonia; cIAI = Complicated intra-abdominal infections; cSSSI = Complicated skin andskin structure infections; HAP = Hospital-acquired pneumonia; VAP = Ventilator-associated pneumonia; RP = Resistantpathogens; DFI = Diabetic foot infections.* The difference between the percentage <strong>of</strong> patients who died in TYGACIL and comparator treatment groups.aThese are subgroups <strong>of</strong> the HAP population.Note: The studies include 300, 305, 900 (cSSSI), 301, 306, 315, 316, 400 (cIAI), 308 and 313 (CAP), 311 (HAP), 307[Resistant gram-positive pathogen study in patients with MRSA or Vancomycin-Resistant Enterococcus (VRE)], and 319(DFI with and without osteomyelitis).In comparative clinical studies, infection-related serious adverse events were more frequently reported for subjectstreated with TYGACIL (7%) versus comparators (6%). Serious adverse events <strong>of</strong> sepsis/septic shock were morefrequently reported for subjects treated with TYGACIL (2%) versus comparators (1%). Due to baseline differencesbetween treatment groups in this subset <strong>of</strong> patients, the relationship <strong>of</strong> this outcome to treatment cannot beestablished [see WARNINGS AND PRECAUTIONS].The most common treatment-emergent adverse reactions were nausea and vomiting which generally occurred duringthe first 1 – 2 days <strong>of</strong> therapy. The majority <strong>of</strong> cases <strong>of</strong> nausea and vomiting associated with TYGACIL and comparatorswere either mild or moderate in severity. In patients treated with TYGACIL, nausea incidence was 26% (17% mild, 8%moderate, 1% severe) and vomiting incidence was 18% (11% mild, 6% moderate, 1% severe).In patients treated for complicated skin and skin structure infections (cSSSI), nausea incidence was 35% for TYGACILand 9% for vancomycin/aztreonam; vomiting incidence was 20% for TYGACIL and 4% for vancomycin/aztreonam. Inpatients treated for complicated intra-abdominal infections (cIAI), nausea incidence was 25% for TYGACIL and 21%for imipenem/cilastatin; vomiting incidence was 20% for TYGACIL and 15% for imipenem/cilastatin. In patients treatedfor community-acquired bacterial pneumonia (CABP), nausea incidence was 24% for TYGACIL and 8% for lev<strong>of</strong>loxacin;vomiting incidence was 16% for TYGACIL and 6% for lev<strong>of</strong>loxacin.Discontinuation from tigecycline was most frequently associated with nausea (1%) and vomiting (1%).For comparators, discontinuation was most frequently associated with nausea (
TYGACIL is in the 2009 IDSA/SIS guidelines forcIAI and the 2009 SIS guidelines for cSSSI. 1,2Expanded broad-spectrumcoverage 3 * is on your side*TYGACIL does not cover Pseudomonas aeruginosa.TYGACIL is indicated for the treatment <strong>of</strong> adults with:• Complicated skin and skin structure infections caused by Escherichia coli, Enterococcus faecalis (vancomycin-susceptible isolates), Staphylococcus aureus(methicillin-susceptible and -resistant isolates), Streptococcus agalactiae, Streptococcus anginosus grp. (includes S. anginosus, S. intermedius, and S. constellatus),Streptococcus pyogenes, Enterobacter cloacae, Klebsiella pneumoniae, and Bacteroides fragilis• Complicated intra-abdominal infections caused by Citrobacter freundii, Enterobacter cloacae, Escherichia coli, Klebsiella oxytoca, Klebsiella pneumoniae, Enterococcusfaecalis (vancomycin-susceptible isolates), Staphylococcus aureus (methicillin-susceptible and -resistant isolates), Streptococcus anginosus grp. (includes S. anginosus,S. intermedius, and S. constellatus), Bacteroides fragilis, Bacteroides thetaiotaomicron, Bacteroides uniformis, Bacteroides vulgatus, Clostridium perfringens, andPeptostreptococcus micros• Community-acquired bacterial pneumonia caused by Streptococcus pneumoniae (penicillin-susceptible isolates), including cases with concurrent bacteremia,Haemophilus influenzae (beta-lactamase negative isolates), and Legionella pneumophilaImportant Safety Information• TYGACIL is contraindicated in patients with known hypersensitivity to tigecycline• Anaphylaxis/anaphylactoid reactions have been reported with nearly all antibacterial agents, including tigecycline, and may be life-threatening. TYGACIL shouldbe administered with caution in patients with known hypersensitivity to tetracycline-class antibiotics• Isolated cases <strong>of</strong> significant hepatic dysfunction and hepatic failure have been reported in patients being treated with tigecycline. Some <strong>of</strong> these patients werereceiving multiple concomitant medications. Patients who develop abnormal liver function tests during tigecycline therapy should be monitored for evidence <strong>of</strong>worsening hepatic function. Adverse events may occur after the drug has been discontinued• The safety and efficacy <strong>of</strong> TYGACIL in patients with hospital-acquired pneumonia have not been established• An increase in all-cause mortality has been observed across phase 3 and 4 clinical studies in TYGACIL-treated patients versus comparator-treatedpatients. The cause <strong>of</strong> this increase has not been established. This increase in all-cause mortality should be considered when selecting amongtreatment options• TYGACIL may cause fetal harm when administered to a pregnant woman• The use <strong>of</strong> TYGACIL during tooth development may cause permanent discoloration <strong>of</strong> the teeth. TYGACIL should not be used during tooth developmentunless other drugs are not likely to be effective or are contraindicated• Acute pancreatitis, including fatal cases, has occurred in association with tigecycline treatment. Consideration should be given to the cessation <strong>of</strong> the treatmentwith tigecycline in cases suspected <strong>of</strong> having developed pancreatitis• Clostridium diffi cile-associated diarrhea (CDAD) has been reported with use <strong>of</strong> nearly all antibacterial agents, including TYGACIL, and may range in severity frommild diarrhea to fatal colitis• Monotherapy should be used with caution in patients with clinically apparent intestinal perforation• TYGACIL is structurally similar to tetracycline-class antibiotics and may have similar adverse effects. Such effects may include: photosensitivity, pseudotumorcerebri, and anti-anabolic action (which has led to increased BUN, azotemia, acidosis, and hyperphosphatemia). As with tetracyclines, pancreatitis has beenreported with the use <strong>of</strong> TYGACIL• To reduce the development <strong>of</strong> drug-resistant bacteria and maintain the effectiveness <strong>of</strong> TYGACIL and other antibacterial drugs, TYGACIL should be used only totreat infections proven or strongly suspected to be caused by susceptible bacteria. As with other antibacterial drugs, use <strong>of</strong> TYGACIL may result in overgrowth <strong>of</strong>non-susceptible organisms, including fungi• The most common adverse reactions (incidence >5%) are nausea, vomiting, diarrhea, abdominal pain, headache, and increased SGPT• Prothrombin time or other suitable anticoagulant test should be monitored if TYGACIL is administered with warfarin• Concurrent use <strong>of</strong> antibacterial drugs with oral contraceptives may render oral contraceptives less effective• The safety and effectiveness <strong>of</strong> TYGACIL in patients below age 18 and lactating women have not been establishedPlease see brief summary <strong>of</strong> Prescribing Information on adjacent page.References: 1. Solomkin JS, Mazuski JE, Bradley JS, et al. Diagnosis and management <strong>of</strong> complicated intra-abdominalinfection in adults and children: guidelines by the Surgical Infection Society and the Infectious Diseases Society <strong>of</strong> America.Clin Infect Dis. 2010;50:133-164. 2. May AK, Stafford RE, Bulger EM, et al. Treatment <strong>of</strong> complicated skin and s<strong>of</strong>t tissueinfections. Surg Infect. 2009;10:467-499. 3. TYGACIL ® (tigecycline) Prescribing Information, Wyeth Pharmaceuticals Inc.268776-01 © 2010 Pfizer Inc. All rights reserved. Printed in USA/August 2010