Antiemetics - BMC HealthNet Plan
Antiemetics - BMC HealthNet Plan
Antiemetics - BMC HealthNet Plan
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
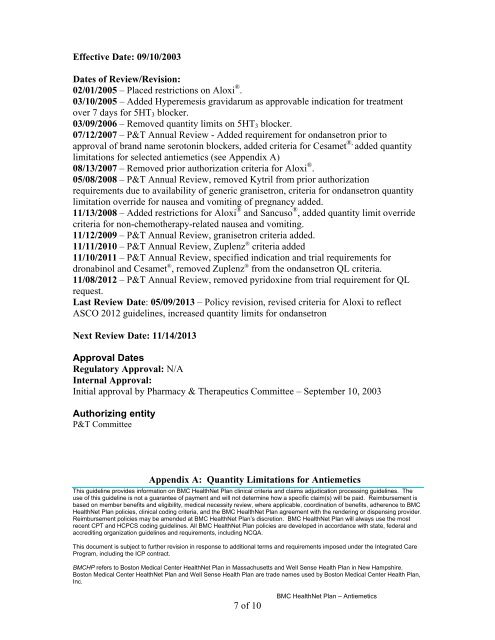
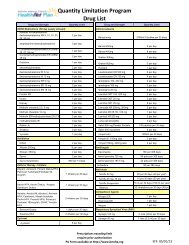
Effective Date: 09/10/2003Dates of Review/Revision:02/01/2005 – Placed restrictions on Aloxi ® .03/10/2005 – Added Hyperemesis gravidarum as approvable indication for treatmentover 7 days for 5HT 3 blocker.03/09/2006 – Removed quantity limits on 5HT 3 blocker.07/12/2007 – P&T Annual Review - Added requirement for ondansetron prior toapproval of brand name serotonin blockers, added criteria for Cesamet ®, added quantitylimitations for selected antiemetics (see Appendix A)08/13/2007 – Removed prior authorization criteria for Aloxi ® .05/08/2008 – P&T Annual Review, removed Kytril from prior authorizationrequirements due to availability of generic granisetron, criteria for ondansetron quantitylimitation override for nausea and vomiting of pregnancy added.11/13/2008 – Added restrictions for Aloxi ® and Sancuso ® , added quantity limit overridecriteria for non-chemotherapy-related nausea and vomiting.11/12/2009 – P&T Annual Review, granisetron criteria added.11/11/2010 – P&T Annual Review, Zuplenz ® criteria added11/10/2011 – P&T Annual Review, specified indication and trial requirements fordronabinol and Cesamet ® , removed Zuplenz ® from the ondansetron QL criteria.11/08/2012 – P&T Annual Review, removed pyridoxine from trial requirement for QLrequest.Last Review Date: 05/09/2013 – Policy revision, revised criteria for Aloxi to reflectASCO 2012 guidelines, increased quantity limits for ondansetronNext Review Date: 11/14/2013Approval DatesRegulatory Approval: N/AInternal Approval:Initial approval by Pharmacy & Therapeutics Committee – September 10, 2003Authorizing entityP&T CommitteeAppendix A: Quantity Limitations for <strong>Antiemetics</strong>This guideline provides information on <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> clinical criteria and claims adjudication processing guidelines. Theuse of this guideline is not a guarantee of payment and will not determine how a specific claim(s) will be paid. Reimbursement isbased on member benefits and eligibility, medical necessity review, where applicable, coordination of benefits, adherence to <strong>BMC</strong><strong>HealthNet</strong> <strong>Plan</strong> policies, clinical coding criteria, and the <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> agreement with the rendering or dispensing provider.Reimbursement policies may be amended at <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong>’s discretion. <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> will always use the mostrecent CPT and HCPCS coding guidelines. All <strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> policies are developed in accordance with state, federal andaccrediting organization guidelines and requirements, including NCQA.This document is subject to further revision in response to additional terms and requirements imposed under the Integrated CareProgram, including the ICP contract.<strong>BMC</strong>HP refers to Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> in Massachusetts and Well Sense Health <strong>Plan</strong> in New Hampshire.Boston Medical Center <strong>HealthNet</strong> <strong>Plan</strong> and Well Sense Health <strong>Plan</strong> are trade names used by Boston Medical Center Health <strong>Plan</strong>,Inc.7 of 10<strong>BMC</strong> <strong>HealthNet</strong> <strong>Plan</strong> – <strong>Antiemetics</strong>