Best Practice Intervention Package - Kansas Foundation for Medical ...
Best Practice Intervention Package - Kansas Foundation for Medical ...
Best Practice Intervention Package - Kansas Foundation for Medical ...
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
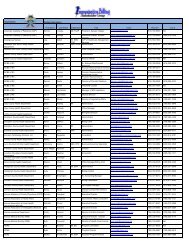
LeadershipThe Cross Settings II BPIP will provide direction to leaders initiating orenhancing care transition processes and practices <strong>for</strong> chronic care patients.Approaching chronic care management within the framework of a continuum ofcare provides the leadership with the ability to view the problem from acommunity perspective. Key practices/interventions that may assistleadership with this include: Disease Management, Self-careManagement Support, and Home Telehealth. These practices arefeatured in BPIP. To further support these topics, the agency success stories focuson:• Working in a care transition community to provide care across thecontinuum with multiple settings and multiple providers• Improving the skills of the nursing clinical staff to maximize the effect of adisease management/telemonitoring program• Using telemonitoring toimprove chronic diseasemanagement and decreaserehospitalizationsInsights are also providedthroughout the BPIP with practicalideas on applying selected bestpractices within an agency. Tools“Rehospitalization may be better viewed as a healthcare system problem than a hospital problem,because care fragmentation is a property ofthe whole system.”“Almost every institution and individualinvolved in a patient’s care can contribute topreventing rehospitalization.” Jencks, 2010, p.757.and resources are abundant in this BPIP, either through embedded links or aspart of this BPIP. Leaders should use the BPIP as a guide to either adopt newtools and/or revise existing tools. Leaders must ensure all agency resources areevidence-based.Rehospitalizations and fragmentation of care delivery are two of the many illsand challenges that plague our health care system. Solutions to overcoming thesechallenges are presented in this BPIP. The BPIP and tools can be used by allhealth care providers in all provider settings based upon the results of their ownneeds’ assessments. Often thesmallest change can make a bigdifference.For example:• Brief Action PlanningChecklist (page 42)• Partnering with Patientsand Families to AccelerateImprovement: ReadinessAssessment (page 43-44)• Tools available through theWeb Links (page 33-37)Using the BPIP across settings:“We have reviewed the fall prevention (BPIP) content ina brief PI meeting held recently with the administrator inattendance. We did not go into great detail at the time;the committee was in<strong>for</strong>med as to the nature of thecontent, some of the tools available to assist the staff, andhow to involve the local PI and Case Management nursesat our local hospital (continuity of care/ transitions ofcare). We plan to incorporate the <strong>Best</strong> <strong>Practice</strong>sinto a bi-partisan (Hospital-Home Health)program. Their patients are ours and vice versa. Wehave already contacted the responsible person at thehospital and she is excited about working together.” GailBatson, RN, MSN. QA/PI Coordinator, Harmony HomeHealth, Inc. Natchitoches, LA- 8 -