Trauma History and Physical - PageOut
Trauma History and Physical - PageOut
Trauma History and Physical - PageOut
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
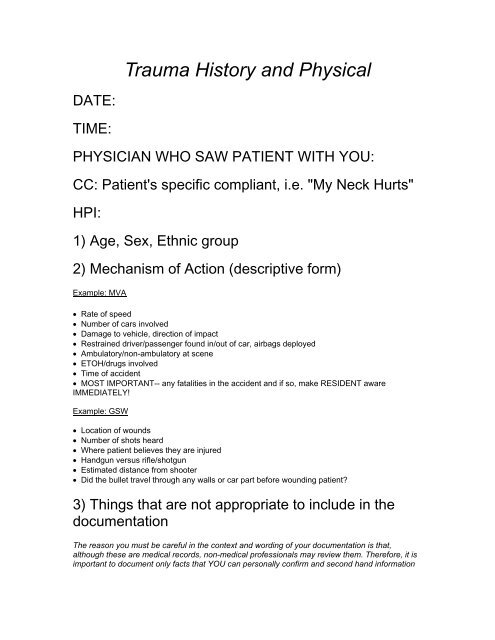
<strong>Trauma</strong> <strong>History</strong> <strong>and</strong> <strong>Physical</strong>DATE:TIME:PHYSICIAN WHO SAW PATIENT WITH YOU:CC: Patient's specific compliant, i.e. "My Neck Hurts"HPI:1) Age, Sex, Ethnic group2) Mechanism of Action (descriptive form)Example: MVA• Rate of speed• Number of cars involved• Damage to vehicle, direction of impact• Restrained driver/passenger found in/out of car, airbags deployed• Ambulatory/non-ambulatory at scene• ETOH/drugs involved• Time of accident• MOST IMPORTANT-- any fatalities in the accident <strong>and</strong> if so, make RESIDENT awareIMMEDIATELY!Example: GSW• Location of wounds• Number of shots heard• Where patient believes they are injured• H<strong>and</strong>gun versus rifle/shotgun• Estimated distance from shooter• Did the bullet travel through any walls or car part before wounding patient?3) Things that are not appropriate to include in thedocumentationThe reason you must be careful in the context <strong>and</strong> wording of your documentation is that,although these are medical records, non-medical professionals may review them. Therefore, it isimportant to document only facts that YOU can personally confirm <strong>and</strong> second h<strong>and</strong> information
that is directly relevant to the medical care of the individual. We all like a good story, but themedical record is not the appropriate place for them.• Do not describe people involved other than the patient; i.e. do not document that the patientstated "his girlfriend shot him".• Do not describe aspects of MVAs that indicate "fault", i.e. do not document "a car ran a redlight <strong>and</strong> hit patient's car."• Do not describe people, including patient, as a "drug dealer, pimp, assailant," etc.• Do not document second-h<strong>and</strong> information that does not contribute to the medical care of thepatient.• Do not document aspects of the MOA in a way that place blame/fault in a legal sense onpeople involved directly or indirectly in events.• Do no describe injuries as self-inflicted• Do not assign exit or entrance wounds when there is more than one GSW4) Pre-Hospital Carea) How transported (ambulance, air, personal car)b) What medical intervention was given up to this point (fluids, monitoring, backboard, C-collar)c) Has the patient, at any time, been unconscious, hypotensive or dropped oxygen saturationd) Was the patient transferred or brought from the scene5) How is the Patient Now?a) Awake, alert <strong>and</strong> oriented to person, place, time?b) Confused?c) Respiratory distress?d) Is the patient able to interact <strong>and</strong> communicate?PMH: self-explanatoryPSH: self-explanatoryMeds: including aspirin, BC powder, Goodies, Coumadin, Plavix, etc. (These can all predisposeto bleeding)Allergies: self-explanatorySpecific Mechanism of Action <strong>and</strong> What to Include:MVA• Driver/passenger; front/back seat• Seatbelt? Airbag? Shoulder harness?• Speed• Damage to vehicle, with specific location of patient in relation to damage/impact.• Loss of Consciousness? (LOC)• Was the seat back, windshield or steering wheel broken?• Were there any fatalities in the accident?• Were others injured in the accident?• Prolonged extrication?
GSW to Extremities• How many shots heard?• H<strong>and</strong>gun versus rifle?• Distance from shooter?• Ability to use extremity after being shot.• Was there "jet-like" or aggressive bleeding at the scene.• Attempt to quantify how much blood-loss at the scene/in transport (small, moderate, large)• Where was the patient st<strong>and</strong>ing in relation to the shooter?KSW• How may times stabbed• Motion/trajectory of knife (upper movement, straight in, slash)• Amount <strong>and</strong> character of bleeding at scene/in transport.• Length <strong>and</strong> type of instrument used (i.e., steak knife vs. stiletto).• Other types of injuries (i.e. assault with fist or kicked?).Assault• Where on the body was the patient hit?• What they were hit with <strong>and</strong> how may times?• Where they hit in head or neck, <strong>and</strong> if so was there loss of consciousness?• Nausea or Vomiting since injuries?• Were there other mechanisms involved (i.e. KSW, thrown from car)?Same Level Fall• Why did they fall? Has this happened before?• Ambulatory/non-ambulatory after fall?• Loss-of-consciousness?• Is the patient on blood thinners?• Where does the patient hurt?• What position was their body in on impact?Fall• How high were they?• Did patient hit anything on way down?• What position was the body in at time of impact?• Loss-of-consciousness?• Ambulatory/non-ambulatory after?• Was ETOH/drugs involved?* IF NOT IMMOBILIZED-- have nurse place patient on a spine board <strong>and</strong> C-collar immediately!
<strong>Physical</strong> Exam: note vitals upon presentationGeneral:• Glasgow coma scale score should be recorded for ALL patients.• Is patient in distress?Head:• Atraumatic/normocephalic = no wounds.• Note location <strong>and</strong> describe wounds found.• Is there a depressed skull fracture on exam?Ears:• Is there any fluid leaking from the ears?• Look for hemotympanum (blood behind the eardrum indicates Basilar Skull Fracture).Eyes:• Pupil size <strong>and</strong> reaction.• Extra Ocular Muscles Movement• Contusions?• Bony step off of orbitNose:• Any fluid or blood drainage?• Note obvious deformities.Mouth:• Loose teeth?• Malocclusion?• Tongue laceration (WATCH AIRWAY!!!)Neck:• Look for crepitus, indicating pneumothorax or tracheal injury.• Is trachea midline or deviated (tension pnemothorax)• Are there distended neck veins?• Note any abrasions/seat belt marks• Make sure the head is stabilized if C-collar is on.• Do not remove C-collar without Resident present!!!Chest:• Listen for breath sounds, <strong>and</strong> if they are equal (looking for pneumothorax).• Is the heart rhythm regular?• Are there abrasions or echymosis of the chest wall?
• Are the clavicles intact?• Is the chest wall tender?• Is there crepitus?Abdomen:• Note abrasions/ecchymosis/wounds.• Is the abdomen distended?• Is there tenderness?• Is there rebound <strong>and</strong> if so, where?• Are there surgical scars (note location)?Pelvis:• Push on ASIS anterior-to-posterior, then from lateral to medial on iliac wings to determinestability.• If there is excess motion or creptius, tell someone about this. No one else should manipulatethe pelvis if suspected to be unstable. This can cause damage to veins in pelvis <strong>and</strong> bleeding.• Note rectal/vaginal exam/blood at the meatus, scrotal hematoma.Extremities:• Note <strong>and</strong> describe any deformities or wounds.• Evaluate range of motion of all extremities.• Document presence of pulses at the radial, femoral, dorsalis pedis, posterior tibial regions (allbilaterally) <strong>and</strong> then show in diagram.• Note: when documenting GSW, do not designate "entrance/exit wounds", simply document"two wounds" versus "one wound."• Document gross muscle strength <strong>and</strong> symmetry.• Document gross sensory exam.• If there is any active bleeding, notify someone immediately!Spine:• After having someone log roll the patient, press on the spinous process of T1-L5 <strong>and</strong> note anytenderness or deformity.• If you do not know how to log roll, have someone show you; serious injury can occur if doneimproperly.• Note <strong>and</strong> document abrasions <strong>and</strong> other wounds.Lab Documentation:• CBC• BMP• P Amylase:• U/AX-rays:• Chest, lateral C spine; pelvis• CTL = cervical, thoracic, lumbar spinal x-rays
• CT scans: HCAP = head, chest, abdomen, pelvis• X-ray areas of tenderness, swelling, lacerations, one joint above <strong>and</strong> below long bone inquestion• Impression: your diagnosis (ex: 1. assault, 2. fractured femur, 3. GSW)• Plan: what you will do to address the diagnoses.Special Note:The purpose of this rotation is for you to have exposure to procedures <strong>and</strong> suturing <strong>and</strong> to beginlearning to identify life-threatening injuries by taking a good history <strong>and</strong> physical. The trauma H &P differs from that of other medical specialties, in that you are attempting to identify ACUTEinjuries. Chronic diseases <strong>and</strong> disorders must be considered, but the acute life threatening issuesare paramount.It is also important to have fun during this rotation. Make the most out of this time, because veryfew medical students have access to such an environment. Some of you may think that onlythose interested in surgery should be on this rotation, but all of us will be faced with traumapatients during our years in practice. It is probably even more important for those of you who arenot going into surgery because you may never have this exposure again in your training.Make sure that if you are not comfortable with a procedure or even taking an H & P, that you askone of the residents to help you. We are all happy to help <strong>and</strong> to teach, but be patient becausethe trauma center is very busy.I hope that this guide helps you get your feet on the ground <strong>and</strong> that you enjoy the <strong>Trauma</strong>Surgery Rotation!!!~Benjamin T. Rush, General Surgery