here - eshre
here - eshre
here - eshre
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
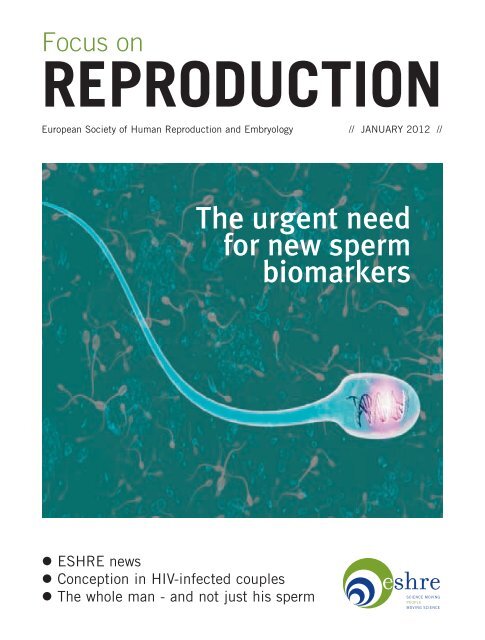
Focus onREPRODUCTIONEuropean Society of Human Reproduction and Embryology // JANUARY 2012 //The urgent needfor new spermbiomarkers• ESHRE news• Conception in HIV-infected couples• The whole man - and not just his sperm
European Societyof Human Reproduction and Embryology28 th Annual MeetingIstanbul - Turkey1 to 4 July 2012The information in this announcementis subject to change.For updated information consultthe ESHRE web-site at www.<strong>eshre</strong>.eu
EXECUTIVE COMMITTEEChairmanAnna Veiga (ES)Chairman ElectJuha Tapanainen (FI)MembersCarlos Calhaz-Jorge (PT)Ursula Eichenlaub-Ritter (DE)Roy Farquharson (GB)Anis Feki (CH)Niels Lambalk (NL)Jolieneke Schoonenberg-Pomper (NL)Antonis Makrigiannakis (GR)Milan Macek Jr. (CZ)Cristina Magli (IT)Jacques De Mouzon (FR)Miodrag Stojkovic (RS)Anne-Maria Suikkari (FI)Etienne Van den Abbeel (BE)Ex-officio membersLuca Gianaroli (IT)(Past Chairman)Françoise Shenfield (GB)(SIG Sub-committee)FOCUS ON REPRODUCTIONEDITORIAL COMMITTEEBruno Van den EedeHans EversRoy FarquharsonJoep GeraedtsLuca GianaroliMilan Macek Jr.Juha TapanainenAnna VeigaSøren ZiebeSimon Brown (Editor)Focus on Reproductionis published byThe European Society of HumanReproduction and EmbryologyMeerstraat 60Grimbergen, Belgiumwww.<strong>eshre</strong>.euAll rights reserved.The opinions expressed in thismagazine are those of theauthors and/or persons interviewedand do not necessarily reflect theviews of ESHRE.JANUARY 2012Cover picture:Science Photo LibraryCONTENTSFocus onREPRODUCTION• Chairman’s introductionThe scientific heart of our society is driven by the SpecialInterest Groups, Task Forces and Working Groups, and anew Working Group on culture media within the SIGsEmbryology and Safety and Quality in ART has recentlybeen put in place. Its goals are to establish contacts withthe culture media manufacturers to provide clearerinformation to professionals, to develop guidelines onculture media requirements, and to promote basic researchin this field. Experts have been invited to join the WorkingGroup and to develop an ESHRE consensus position paperfor Human Reproduction. As an embryologist, I believe that the contribution ofESHRE on this matter will be of paramount importance and I applaud theinitiative of, among others, Arne Sunde, the Working Group co-ordinator.Another important project in progress is our collaboration with the EuropeanAssociation of Tissue Banks (EATB) and the European Eye Banks Association. Werecently organised a very well attended session on ART at the EATB meeting inBarcelona in November and are now working on a joint project for the training ofinspectors for ART centres and for the European coding system.I am also pleased to say that our ‘star’ project, the ESHRE Study into theEvaluation of oocyte Euploidy by Microarray analysis - ‘ESTEEM’ - co-ordinatedby our past chairman Joep Geraedts, will start in February. This randomised trialwill include 600 PGS cycles performed in seven different European centres andaims to estimate the likelihood of euploid embryos in future ART cycles and toimprove birth rates in older patients. Our partner in the project, the biotechcompany BlueGnome, will provide arrays and technical training. This is ESHRE’sfirst randomised trial for many years, and we expect the results to be of greatimportance.Our relationship with the ASRM continues to progress, with exchange sessionsat our annual meetings and precongress courses representing a fruitfulcollaboration. Joint plans are already advanced for this year’s annual meetings inIstanbul and San Diego. So it gives me great pleasure to invite you to our first jointmeeting of ‘The Best of ASRM and ESHRE’, to be held in Cortina d’Ampezzo,Italy, at the beginning of March. Along with our American colleagues, we haveproduced an attractive scientific and social programme in an exceptional location.Good science and nice skiing will be provided!Anna VeigaESHRE Chairman 2011-2013NEWS4 Annual meeting 2012 Istanbul6 ESHRE news7 Paul Devroey bows out from the VUB8 Regulatory news10 Thirty years since the first hMG birth13 The best of ESHRE and ASRM14 The Whole Man Campus workshop16 From the PGD Consortium17 From the Special Interest Groups24 From the Task ForcesFEATURES27 The urgent need for newsperm biomarkersSheena Lewis asks ifsperm DNA damage is amore reliable diagnostictool than semen analysis31 Conception in HIVinfectedcouplesAugusto Semprinireviews the risksof transmissionand the appropriatefertility techniquesFocus on Reproduction January 2012 3
ANNUAL MEETING 2012Istanbul abstract deadline is 1st FebruaryCity of rich cultures will be reflected in opening ceremony and congress partyA summer in Istanbul is the enticing backdrop to this year’sannual meeting of ESHRE. For those travelling from theEast, Istanbul has been dubbed ‘the last eastern city’ - andlast western city when travelling from the West. ButThe Istanbul Congress & Exhibition Center, venue for ESHRE’s27th annual meeting.whatever the direction, Istanbul, located on two continents,has a rich social and cultural heritage, which is certain tocomplement the very latest from a packed scientificprogramme.The invited programme and precongress courses for thisyear’s meeting are already in place, and deadline for thesubmission of abstracts is 1st February. All abstracts will bescored (blind and weighted) by ESHRE’s InternationalScientific Committee. Last year’s event in Stockholmprompted more than 1400 abstract submissions, and asimilar response is expected this year.Our congress centre, the Istanbul Convention &Exhibition Center, is in easy reach of the airports and inwalking distance of many of the major hotels. The congresscentre is located near Taksim square, Istanbul’s centralshopping, tourist and leisure district considered the heart ofthe modern city.We are preparing a number of events to reflect theinimitable nature of Istanbul, from the opening ceremonyitself in the congress centre to the congress party, whichwill be held in Suada (roughly translated as ‘water island’)4 Focus on Reproduction January 2012
a small island located on the Bosphorusand accessible by a short boat tride. Amodern glass covered building on theisland will be our main location fordining and dancing with friends, amidthe beauty of the Bosphorus on awonderful summer night.Timur GürganChairman Local Organising CommitteeThe congress party on Tuesday night willbe held on Suada, a floating resortlocated on the Boshporus with apanormaic view of Istanbul.Abstracts must be submitted online and according to designated topicsAll abstracts must arrive via the ESHRE website nolater than 1st February. Abstracts should be submittedin English only.Investigators should note the following:• Anyone submitting an abstract can only be the firstauthor for one abstract.• The material presented should be unpublished andoriginal, and not yet have been presented at any othermeeting.• All abstracts will be refereed ‘blind’, ie, without thenames and addresses of the authors.• Authors are requested to indicate their preference fororal and/or poster presentation on the abstractsubmission form. Abstracts submitted but not selectedfor oral presentation can be referred to the postersessions. The decisions of the selection committee arefinal.• All accepted abstracts and the index of authors willbe published in the abstract book, a monograph to theHuman Reproduction journals.T<strong>here</strong> are four topic categories: basic science, clinicalscience, mixed (basic/clinical), and paramedical.When basic science, clinical science or mixed areselected, one of the following topics should beselected:• Cross border reproductive care• Developing countries and infertility• Early pregnancy (including miscarriage, recurrentmiscarriages, abortion, termination of pregnancy,ectopic pregnancy, molar pregnancy)• Embryology (including IVF/ICSI, gamete and embryoselection, culture, cryopreservation, vitrification,developmental biology)• Endometriosis, endometrium, implantation andfallopian tube• Ethics and law• Female (in)fertility (including oogenesis, diagnostictests, prognostic models, intrauterine insemination,oocyte donation, body weight effects, smoking, ageing,immunology, sexually transmitted diseases)• Andrology (including male (in)fertility,spermatogenesis, diagnostic tests, treatment, MESA,TESA, TESE, sperm donation, environmental factorsrelated to male fertility, immunology)• Male and female contraception• Male and female fertility preservation (includingoncofertility, medical indications, social freezing,laboratory techniques)• Psychology and counselling• Quality and safety of ART therapies (includingguidelines, accreditation, EUTCD, certification,complications: premature labour, malformations,neonatal risks, multiple pregnancy, long-term follow-upof children)• Reproductive (epi)genetics (including (epi)geneticcauses of infertility, PGD, PGS, prenatal diagnosis)• Reproductive endocrinology (including ovarian reservetesting, ovarian stimulation, IVM, POF, PCOS, infancy,disorders of sexual development, puberty, adolescence,menopause )• Reproductive epidemiology and health economics• Reproductive surgery (female and male)• Stem cells• Translational research (including new ideas,hypotheses, new thinking, immediate applicability inpractice).Paramedical categories are either ‘laboratory’ or‘nursing’.More information on abstracts - with details of wordcounts, key words, title and for online submission - canbe found on the ESHRE website under ‘AnnualMeeting’.Focus on Reproduction January 2012 5
ESHRE NEWSESHRE’s array CGH trial ready for randomisationESTEEM will be the firstrandomised trial of 23chromosome testing of polarbodies using array CGHThe pilot study showed thatreliable identification of thechromosomal status of anoocyte is possible in about 90%of polar body biopsy attempts.Randomisation in ESHRE’s trial to evaluateoocyte euploidy by array CGH is expected tobegin in February. The study, which will beperformed in women aged between 36 and41 years, has two primary aims: to estimatethe likelihood of having no euploid embryosin future ART cycles and to improve livebirth rates in women of advanced maternalage.The study, now known as ESTEEM (theESHRE Study into The Evaluation of oocyteEuploidy by Microarray analysis), aims torecruit around 600 couples (at least 266 perstudy arm) at seven PGS centres.Project arrangements with collaboratingpartner BlueGnome are already in place, andall centres have had microarray training fortwo days. Polar body biopsy training hasbeen provided by the two reference centresin Bonn and Bologna.It has now been agreed that the steeringcommittee will comprise Joep Geraedts (wholed the PGS Task Force behind the pilotstudy), Veerle Goossens (from ESHRE’sEmbryo certification goes internationalThe Portuguese embryologist Carlos Planchahas taken over as co-ordinator of theEmbryologist Certification SteeringCommittee. The scheme, which continues toexceed all expectations, saw almost 90 clinicalembryologists gain certification in 2011, and20 seniors.This year will be the first in which thescheme becomes open to embryologists fromoutside Europe, with certification examstaking place in Istanbul. In this first year (forwhich applications were open until November2011) only the senior certification is available.It will also be possible in the near future that all ESHRE-certifiedembryologists can if they wish renew their certificate through a newcontinuing embryology education credit (CEEC) scheme. ‘We consider thescheme a stimulus for the continuous update of knowledge,’ explainsKersti Lundin, co-ordinator of the SIG Embryology. ‘It will provide apractical framework for continuous education through attending meetingsand workshops, and a recognition of publications and other activities byclinical embryologists. However, this is a voluntary activity, and, as withall academic certificates, t<strong>here</strong> is no loss of validity implied from apreviously obtained ESHRE clinical embryology certification.’ Creditsmay be earned in three-year blocks according to the type of activityundertaken.Central Office), and John Collins (whowrote the trial protocol). Datamanagement, monitoring and training willbe in the hands of Clinical Trial CenterMaastricht, an academic researchorganisation able to provide onlinerandomisation (which will allowstratification according to age and centre).The study is expected to last around twoyears.Three ESHREguidelines now indevelopmentThree ESHRE guidelines are currentlyin development, according to ESHRE'sresearch specialist NathalieVermeulen. The first, an update of theendometriosis guideline, hascompleted its initial stages (topicselection, development group andscope) and preliminary searches forevidence, and is now in the process ofsummarising/grading evidence andformulating recommendations. Hopesare that the finished text will be readyfor publication later this year.A psychology and counsellingguideline completed its scoping inStockholm last year and will beginevidence searches early this year.Publication is expected in early 2013.And a guideline on premature ovarianinsufficiency, proposed by the SIGReproductive Endocrinology, has alsocompleted scoping and hopes to finishits evidence searches and gradingbefore the end of this year, with a viewto publication in 2013.Nathalie reported to ESHRE’sExecutive Committee that standardguidelines are likely to take around twoyears to develop and complete.Other proposals under considerationinclude the diagnosis and treatment offemale genital tract malformations,and guidelines for the provision andmanagement of sperm cryopreservationin cancer patients.6 Focus on Reproduction January 2012
Paul Devroey bows out from the VUBPaul Devroey, Chairman of ESHRE from2005 to 2007, will retire as Professor ofReproductive Medicine at the DutchspeakingFree University of Brussels(VUB) in September this year, and willbecome Emeritus Professor the followingmonth. He was succeeded (in October2011) as Clinical Director of the Centrefor Reproductive Medicine by HermanTournaye, whose history at the VUBstretches back to student days.A valedictory symposium in honour ofDevroey, held at the VUB in September,attracted more than 500 participants, andwith them of course came a generousrecognition of the part he and Brusselshave played in the recent history ofreproductive medicine.Bart Fauser, reviewing Devroey’sinfluence as an investigator, said he wasnow the world’s most cited author inreproductive medicine, and repeated theadvice of Hans Evers to those aspiring towrite a citation classic: ‘They shouldconcoct a new clinical treatment,preferably in ART, think up a fancyacronym, publish it in English, in ajournal with a high impact factor, and askDevroey and/or Van Steirteghem as a coauthor.’Filippo Ubaldi, a former VUB traineehimself, reported that 194 publications inpeer review journals have had an ex-Brusseliensis as first author - among themKolibianakis, Papanikolaou, Nagy, Liu,Platteau and Palermo.Devroey’s own history with ESHRE datesback to the Society's foundation, when <strong>here</strong>presented Belgium on the first andsecond Advisory Committees (from 1986to 1990) and, with André VanSteirteghem, organised ESHRE's secondannual meeting in Brussels in 1986(having served on the organisingcommittee of the first meeting in Bonn in1985). Today he remains an activemember of ESHRE’s SIG Ethics & Law,and of its position paper writing groups -which he has always described as some ofESHRE’s most important achievements.From the top, among an array ofinternational and ex-Brusseliensisspeakers were Bart Fauser, PeterNagy and Filippo Ubaldi.Twenty years this month since the world’s first ICSI birthThe picture left was taken in 1993 when André Van Steirteghemreported data from the VUB’s first ICSI series at ESHRE’s annualmeeting in Thessaloniki, three years after the first (inadvertent)fertilisation in 1990. Following trials in animal models, withethical approval secured and pre-conditions in place (karyotyping,prenatal diagnosis), the VUB's first ICSI embryo had beentransferred in 1991, and the first baby born in January 1992. Theevent was reported (along with four pregnancies) to the Lancet (byPalermo, Joris, Devroey and Van Steirteghem). Data from allsubsequent patient series appeared in Human Reproduction, whichno doubt had a lasting effect on the journal’s impact factor.Focus on Reproduction January 2012 7
REGULATORY NEWS// UPDATES FROM THE MINISTRIES //Denmark reverses its decisionon IVF medication co-paymentJust 12 months after introducing a patient co-payment system for ARTmedication and a treatment fee at all public clinics, the Danishgovernment has gone back to its old system of free access for up tothree completed IVF cycles and (almost) full reimbursement formedication. The revised system will come into force this month.In explaining the move the government said ‘the public health systemshould be characterised by equal access for everybody’ and that ‘copaymentfor assisted reproduction will lead to social inequality anddiscrimination against less wealthy patients’.The introduction of payment in 2011 prompted protests from allhealth professionals, who forecast that the move would result in fewerchildren born in Denmark and would compromise safety and research.However, the immediate effect was a 23% drop in the number ofIVF/ICSI treatments performed at the public clinics and a 30% drop inreferrals. With Danish clinics now responsible for around 10% of allchildren born, the effect on Danish birth rates would be marked.Whilst t<strong>here</strong> was a common perception in Denmark - as elsew<strong>here</strong> -that infertility was increasingly the result of lifestyle choices, we wereable to show in arguing against the co-payment scheme that in morethan 90% of all cases treated in the public system the cause of infertilitywas related to a disease defined as a registered diagnosis by theNational Board of Health.Further, it was shown (as described by Connolly et al in HumanReproduction 2011) that a decline in IVF babies would result in a netloss in tax revenue for Denmark when the perspective shifted to thelong term. We were also supported in our protests by the patientorganisations, who organised Facebook pages which attracted morethan 30,000 friends, all objecting to the introduction of patientpayment. Thus, the new Danish Government confirmed in October that‘in order to ensure that infertility patients are not treated worse thanother patients’ the system of co-payment for assisted reproduction,sterilisation and re-fertilisation would be revoked.Søren Ziebe, Rigshospitalet, Copenhagen. . . while Catalonia ends free access to fertilitydrugs for patients in the private sectorCiting Spain’s critical financial situation as an explanation, healthauthorities in the four provinces of Catalonia have discontinued theprovision of free fertility drugs for IVF patients in the private sector.Since 1997 the cost of all drugs for fertility treatment was reimbursed bythe Catalan health services, regardless of whether patients were treated inthe private or public system. Free access continues in the public sector.Policy in the Czech Republic is also to reimburse the full costs of threecycles, whether in the private or public sector, with a co-payment ofaround €1900. However, t<strong>here</strong> are new proposals that from January thisyear reimbusement with co-payment will be extended to four cycles oncondition that the patient accepts SET for the first two cycles.UK’s HFEA agrees fixedsum compensation for allgamete donationFollowing a public consultation andmany months of public agonising,Britain’s regulator, the HumanFertilisation and Embryology Authority,agreed in October to compensate spermdonors a fixed sum of £35 per visit andegg donors a fixed sum of £750 percycle of donation. The move, said theHFEA, was ‘a proactive approach todonor recruitment, retention and care’which provides donors with a level ofcompensation ‘which better reflects theirexpenses’ and their inconvenience.So far, UK policy had allowed spermand egg donors to claim only‘reasonable’ expenses, such as travelcosts, and a modest daily amount forloss of earnings, with a limit of £250 foreach course of sperm or egg donation.In announcing the one-off fee, theHFEA was at pains to remove any hint ofpayment or inducement from the newpolicy; this was strictly compensation,based, according to the HFEA, on theprecedence models of Denmark (forsperm donation) and Spain (for eggdonation).The Chair of the HFEA said that thelevel of compensation would ‘not deterthose interested in donation’ but would‘retain donors already in the system,without attracting those who are merelyfinancially motivated’.UK treatments using donor eggs hadfallen to a recent all-time low in 2009 ofjust 1254 cycles and the HFEA clearlythought that ‘compensation’ was one wayto resolve the ‘crisis’.The HFEA’s announcement also gaveits seal of approval to egg-sharing, atechnique which in its consultation hadbeen described as ‘controversial’. Thissystem of ‘benefits in kind’, said theHFEA, which is now well established inBritain, ‘should be allowed to continue’as before.8 Focus on Reproduction January 2012
Almost one in five women having IVF in UK is40 or over; but treatments continue to riseThe UK’s latest report on IVF activity for 2010shows that almost 20% of all fresh IVF and ICSIcycles performed in Britain were in women aged 40or over. The figures represent a considerableincrease, having almost doubled over the past 13years, and are thought likely to be replicated inmany other European countries.A recent study from Maastricht foundthat the average age of patientsattending a first consultationincreased from 27.7 years in1985 to 31.4 years in 2008,a rise of almost four yearsin just two decades. Theproportion of women of35 years or older almostquadrupled to 31%.And world datagat<strong>here</strong>d by ICMART for2007 and reported atESHRE’s annual meetinglast year estimated thatalmost 16% of women havingART were over the age of 40.The latest HFEA report puts theaverage age of women in the UK having IVF andICSI (as well as donor insemination) in 2010 at35 years. Twenty years ago, the average age was33.6 years.The report also disclosed that in 2010 a totalof 45,264 women received 57,652 IVF or ICSItreatments, an increase of 5.9% on thenumber of cycles in 2009. This toois consistent with recent year-onyeartrends calculated byESHRE’s EIM Consortiumand by ICMART.The pregnancy ratefrom these UK cycleswas 33.4% per transfer.However, in 200924.9% of live births inpatients aged 18–34years were multiple, arate only marginallylower than the 29.4%multiple rate of 2008.Age range of IVF/ICSI patients in UK clinics in2010, from the HFEA’s latest annual report.Netherlands poised to reduce reimbursed IVF cyclesHolland’s minority government (of liberals and Christian Democrats) has been in power for little more than a year but hasalready announced cost-cutting measures in IVF to the tune of €30 million a year. This, they say, must be achieved byexcluding a second and third cycle from the state’s reimbursement scheme - which would reduce the number of reimbursedIVF cycles in the Netherlands from three to one. In announcing the measures, the government invited those involved topropose alternative ways to raise the €30 million a year.‘We calculated that the additional cost of a twin pregnancy compared to a singleton was around €5000 per pregnancy,’said Hans Evers, from the Academic Hospital of Maastricht. ‘The extra costs involved in the delivery and in the first fourweeks range from €2000 in the case of a healthy twin to €30,000 in the case of a twin with complications, such asprematurity.’ Evers added that the long-term costs submitted to the government were only rough estimates, but rangedfrom €900-7000 per year per child with a minor handicap to €1800-20,000 per year per child with a severe handicap.The Dutch calculations were based on 2009 data; 16,769 IVF treatment cycles were performed, resulting in 4386ongoing pregnancies and 469 twin pregnancies, for a multiple pregnancy rate of 10.7%. Of these twins, 85% were born towomen below 38 years of age.‘Estimating the average lifetime additional costs of a twin at € 75,000,’ explained Evers, ‘we argued that by decreasingthe number of twins to zero by performing single embryo transfer in all women below 38 years, we would save 85% x 469twins x €75,000 per year - that’s €29.9 million. We thought this would meet the government’s requirements, which wouldleave the number of reimbursed cycles at three.’However, despite the logic of the proposal and the clinics’ promise to adopt a strategy of only SETs in all women under38, the Minister of Health was not impressed. The cost savings would be made outside the area of IVF, and many of thecost savings were considered ‘lifetime’, so would not bring an immediate return. The signs are, says Evers, that theNetherlands will now lose its three cycle reimbursement policy in 2013, and become yet another example of how IVFseems the soft option when it comes to cost-cutting in health budgets.Focus on Reproduction January 2012 9
NEWS// UPDATES FROM EUROPE //European court now rules infavour of Austria’s donation lawThe Grand Chamber of theEuropean Court of Human Rightshas ruled that Austria’s ban onsperm and egg donation was not inbreach of the European Conventionon Human Rights. The ruling wasmade following an appeal by theAustrian authorities and reverses aprevious Court judgement whichhad found that the ban on gametedonation was a breach of the convention.The case dates back more than a decade, to when two Austrian coupleswishing to conceive a child through egg and sperm donation complainedto the Court on two counts: that Austria’s ban violated their right torespect for family life (under Article 8) and that the ban amounted todiscriminatory treatment (under Article 14). In April 2010 the Courtupheld the complaints in what appeared to be a landmark judgement.However, at the Austrian government’s request the case was referredback on appeal to the Grand Chamber, which now - in November lastyear - has ruled that t<strong>here</strong> was in fact no violation of Article 8 inAustria’s original legislation.The Court noted that, although t<strong>here</strong> was a clear trend across Europein favour of allowing gamete donation for IVF, the emerging consensuswas still ‘under development and was not based on settled legalprinciples’. For example, the Court noted that all ‘relevant legalinstruments’ in Europe were either ‘silent’ on the question of gametedonation or, in the case of the EUTCD, leaving the decision (on whetheror not to use) to individual member states.According to the judgement, the original Austrian legislation had tried‘to avoid the possibility that two women could claim to be the biologicalmother of the same child’. They had thus approached this controversialissue ‘carefully’ and ‘had not banned individuals from going overseas forinfertility treatment unavailable in Austria’. Thus, while the Courtconcluded that t<strong>here</strong> had been no violation of the Convention, it stillemphasised the importance of keeping legal and fast-moving scientificdevelopments in the field of ART under review.Of some concern to ESHRE - and as reported in the May 2011 issueof Focus on Reproduction - ESHRE was not allowed to submit writtencomment in advance of the appeal, its evidence being deemed‘inadmissible’ (despite ESHRE’s favourable legal advice to the contrary).The final judgement, however, notes that the governments of Italy andGermany were allowed to submit comment (in support of the Austrianposition), along with the European Centre for Law and Justice (‘aChristian-inspired organisation’, see http://eclj.org/About/), AktionLeben, an Austrian organisation ‘for the protection of human life’(whose spokesman following the judgement said that ‘egg donation isusually based on the exploitation of women’), and the Italian SOSInfertilita Onlus association.Thirty yearsAnna Pia Ferraretti‘When I arrived in Norfolk inOctober 1981 the atmosp<strong>here</strong> wasalready tense and exciting. For<strong>here</strong>, at the IVF unit of the Eastern VirginiaMedical School, the USA's first ongoingpregnancy from IVF was progressing nicely toterm. The Norfolk group, which had beenopened the year before by Howard andGeorgeanna Jones after their 'retirement' fromJohns Hopkins in Baltimore, at the timeincluded Jairo Garcia, Anibal Acosta andLucinda Veek, plus a very nice group ofnurses and secretaries (who greatly helpedme with my terrible English!). I was the firstforeign fellow of the IVF unit, sent to Norfolkat the request of my professor, CarloFlamigni, who hoped I would be able to starta clinical programme at Bologna Universitywhen I returned.That first IVF baby in the USA, ElizabethJordan Carr, was born 30 years ago, on 28thDecember 1981 at the Norfolk GeneralHospital, delivered by Mason Andrews (thenchairman of the ObGyn department).Elizabeth is now working at the Boston Globenewspaper, and in 2010 delivered her firstbaby, conceived naturally. I had heldElizabeth in my arms on the day of her birthand will never forget that moment.Unlike Louise Brown, Elizabeth did notachieve fame as a result of her conception -she was already the 15th IVF baby to be born(12 of them in Melbourne) - and very fewpeople now remember that she was the firstsuccessful birth using hMG for ovarianstimulation. This was important, and tounderstand why we must go back to the veryfirst days of IVF, when the most controversialissue for the few people working in IVF wasthe natural or the stimulated cycle.After the birth of Louise Brown (from anatural cycle) Bob Edwards had tried at least100 hMG cycles, but without term deliveries.According to his reports, hMG (which he hadused in relatively high doses) was not suitablebecause of its luteal phase effects.Georgeanna Jones, a reproductiveendocrinologist with huge experience of hMGin anovulatory patients, was not convinced byBob's conclusions, but she and Howard10 Focus on Reproduction January 2012
since the world’s first hMG babyremembers the first IVF birth in the USAfollowed his natural-cycle advice whenthe Norfolk programme began.During that first year of 1980, 41Norfolk patients had IVF, but only ninereached embryo transfer and nopregnancies were obtained. This was abig disappointment, even raisingdoubts over the whole concept of IVF.Thus, after long discussionsGeorgeanna managed to convinceHoward that it was crucial to return tohMG. If hMG could work inanovulatory patients, why not inovulatory? Morever, at the beginning of1981, Trounson and Wood inMelbourne were already reporting theirfirst IVF pregnancies in stimulatedcycles (although with clomiphene).But Georgeanna opted for hMGbecause of its more physiologicalnature, and at a lower dose than inBob's approach. She chose the samedose as used in anovulatory patients -a fixed dose of two ampoules per dayfor three days (starting the first, thirdor fifth day of the cycle depending onGeorgeanna andHoward Jones, eachreceiving honorarymembership of ESHREat the 1998 annualmeeting in Gothenburg.cycle length) and reduced to oneampoule for the next three days. Thedosage was then readjusted accordingto response, but during the whole of1981 no more than two ampoules perday were ever used; all that varied wasthe duration of stimulation. Today wewould call this a mild stimulationprotocol. And then the pregnanciesstarted: seven from 55 egg retrievalsand 31 transfers. All went to term,without miscarriages, and spirits rose.So, when I arrived in October 1981,this was the protocol in use.Ultrasound was already available formonitoring, but it was difficult tointerpret and the most importanttriggers for hCG administration wereestradiol levels and biologicalparameters (vaginal cells and cervicalmucus) as an index of oocytematurity. My first task was a dailyanalysis of the cervical mucus andvaginal smear of all the IVF patients,while Jairo did the ultrasoundevaluation. I remember that two orthree days of coasting before hCG wereconsidered necessary by Gerogeanna,to let the oocytes complete maturationwithout any additional stimulus.In the following year, 1982,Georgeanna tested several newprotocols, notably increasing theamount of hMG in the first two days ofstimulation, then increasing FSH (byadding Metrodin) and finally usingFSH alone for the whole stimulation.We had daily meetings to discuss eachcase according to the differentprotocols, to understand the effects ofFSH and LH on follicular developmentand oocyte viability. Georgeanna wasalways trying to find a physiologicalexplanation for each observeddifference, Jairo to translate intopractice Georgeanna's observations, ANNA PIA FERRARETTI:‘GEORGEANNA WAS THEFIRST TO SUGGEST THATEXCESSIVE FSH (± LH)MIGHT HAVE ADETRIMENTAL EFFECT ONOOCYTE QUALITY.’Focus on Reproduction January 2012 11
Howard totranslate thestatistics intodata, Lucinda todescribe the lookof each oocyteand cumulus cellin detail, andAnibal to be themoderator of thediscussion. Veryoften, a telephonecall would bemade to BobEdwards inEngland, and oncein a while GaryHodgen would come in to the meetingswith updates on his animal studies. Asfor me, I was taking in as much as Icould from these energetic debates,and getting closer day by day to theconcept of IVF as seen by Georgeanna- my first paper was published with herand the rest of the group (on LH levelsduring stimulation with hMG) in 1983.Reading her reports and personalnotes today from this early period, Irecognise that most of her observationshave become routinely accepted. Somenow seem obvious (but were not at allat the time !), for instance:- ‘FSH is the essential gonadotrophinfor multiple follicular recruitment butFSH alone is also able to sustaincomplete follicle maturation.’- ‘Three different types of ovarianresponse can be identified: low (20%),intermediate (60%) and high (20%).’- ‘The number of follicles depends onthe amount of FSH given during day 3-5 of the cycle; however, the number offollicles that can berecruited is variableand depends on t<strong>here</strong>sidual store of eggs.This seems relatedmainly to patient age.’But t<strong>here</strong> is arecurrent observationin her early papersthat was completelyneglected fortoo many years. Shewrote: ‘Continuingwith high amountsof FSH or hMGafter the recruitmentperiod (after day 5) may result in anincreased number of follicles but adecreased number of viable oocytes incomparison to those cycles stimulatedwith lower amount of FSH and LH.’As we are now aware, more vigorousstimulation protocols were pursued inthe late 1980s, particularly afterGnRH agonist down-regulation wasintroduced. Certainly, this prompted asignificant increase in the efficacy ofIVF, but was also accompanied by areciprocal increase in complicationssuch as OHSS and multiplepregnancies. And despite these variousinnovations and the introduction of yetfurther protocols, it is still the casethat only some 7-10 % of all fresh IVFoocytes actually produce a baby - andthis value has remained relativelyconstant over the past 30 years.Nevertheless, only in the pastdecade or so have investigatorsproposed milder forms of stimulation,as recommended by Fauser in 1999:‘Use of the lowest possible doses forovarian stimulation not only reducesthe risk of OHSS but also increasesthe relative proportion of geneticallynormal oocytes.’ Progress, however,has been very slow and only morerecently has resistance to mildstimulation been noticeably reduced.Today, mild stimulation is stillconsidered a new trend in our field,but Georgeanna was the first tosuggest that excessive FSH ( ± LH)might have a detrimental effect onoocyte quality.After a year in Norfolk I returned toBologna to set up an IVF programmewith Luca Gianaroli, then returningfrom Melbourne w<strong>here</strong> he spent timeworking with the late Carl Wood andAlan Trounson. Of course, we toodiscussed the protocol to use: Norfolk(FSH/hMG) or Monash (CC + hMG)?We decided to test both, and in thefirst years of our programme 549patients received the Monash and 979the Norfolk protocol - with a clinicalpregnancy rate of 13% in the former18% the latter. So the clomipheneprotocol was abandoned in favour ofgonadotrophins. Georgeanna wouldhave been happy with that, as shewould also be knowing that for manyyears we have been using mildstimulation in our younger patients.But ironically the mild stimulation weare using today is the Monashprotocol: clomiphene from cycle day 3to 7 plus a little FSH on cycle days 5,7 and 9. She may not have approved,but I can now confirm that clomiphenecan work very well in IVF!Anna Pia FerrarettiSISMER, Bologna, ItalyCarl Wood, IVF pioneer: 1929-2011The death of Carl Wood, who with Alan Trounson and John Leeton inMelbourne established the irrevocable place of stimulated cycles in IVF, wasannounced in September. Wood’s group at Monash achieved the world’s firstIVF pregnancy in 1973, which was to miscarry, and several other notable firsts:in 1983 the first live birth from a frozen embryo and that same year the firstbirth from a donor oocyte. Twelve of the world’s first 15 IVF births wereconceived at Monash by Wood’s team. Like Robert Edwards in Britain, Woodfaced much public opposition to his work and accusations that IVF encouragedthe destruction of embryos. As a Roman Catholic, Wood himself was muchrelieved when the techniques of embryo freezing were perfected. In the face ofsuch opposition he always encouraged discussion, advocacy and consensus.12 Focus on Reproduction January 2012
ESHRE NEWS// THE BEST OF ESHRE AND THE ASRM //Something for everyonein the Italian DolomitesA programme of lectures and debatesconceived on both sides of the AtlanticThe scientific programme of the first ‘best practice’ meeting ofESHRE and the ASRM is now complete. The three-day meeting,set to be held in the Italian skiing resort of Cortina d’Ampezzo inMarch, is, according to ASRM chairman Roger Lobo, ‘anexperiment’, but one which both societies have devised to provideopportunities for both learning and networking. Mornings will befree for social activities, while the scientific programme laststhroughout the afternoon and early evening. Subjects have beenchosen for their topicality and for their relative difference inapproach between Europe and the USA.Presently, the ‘best of’ meetings are foreseen as annual eventsalternating between leisure venues in Europe and the USA.Cortina d’Ampezzo, this year’s venue, is located in the Dolomitesin northern Italy and is considered one of Europe’s foremostskiing locations.Details about registration, hotel accommodation and transportare presented on the ESHRE website.LecturesBack-to-back sessions, during which different topics and practices will beanalysed from the American and European points of viewDebates, in which two experts will discuss controversial issues, illustratingdifferent point of views and supporting different theories and approachesCutting-edge lectures, aiming to illustrate innovations and new findings inreproductive medicine and embryologyThursday 1st March14.30-15.30 The information brought by the sperm into the oocyteC. Barratt (GB)15.00-15.30 Fertilization and unexplained failureC. Combelles (USA)15.30-16.20 Should a single embryo be transferred in all IVF patients?K. Lundin (SE) and G.D. Adamson (USA)16.20-16.50 PCO: Diagnosis and approaches to therapyB. Tarlatzis (GR)17.10-180018.00-19.0019.00-19.30Oocyte cryopreservation: standard or experimental practice?E. Van den Abbeel (BE) and G.L. Schatman (USA)Intrauterine Insemination versus fast-track IVF: Bestpractices for unexplained infertilityF. van der Veen (NL) and R. Reindollar (USA)Perinatal outcome and ART techniquesK. Barnhart (USA)Friday 2nd March14.30-15.30 The impact of oocyte quality on embryo developmentM. C. Magli (IT)15.00-15.30 Environmental toxins and their impact on fertilityR.Z. Sokol (USA)15.30-16.20 POR: stimulation and oocyte qualityA.P. Ferraretti (IT) and L. Schatman (USA)16.20-16.50 PCO with hyperandrogenism is really PCOS?R. Legro (USA)17.10-180018.00-19.0019.00-19.30Saturday 3rd March14.30-15.30 Culture media supplementation and culture conditionsA. Sunde (Norway)15.00-15.30 Epidemiology of reproductionKurt Barnhart (USA)15.30-16.20 Preimplantation genetic testing: Current technology andglobal experience - When to do and by what technique(s)J. Geraedts (NL) and N.Treff (USA)16.20-16.5017.10-180018.00-19.0019.00-19.30Menopause. Carcinogenesis of ovarian cancer: the incessantmenstruation hypothesisP.G. Crosignani (IT)The “timing” hypothesis revisited.R. Lobo (USA)Who is the most important for a successful outcome in ART?The clinician or the embryologist?L. Rienzi (IT) and G.L. Schatman (USA)Repeated implantation failureA. Makrigiannakis (GR)Efficacy of new surgical techniquesS. Gordts (BE)Natural cycle, mild stimulation and conventional stimulationB. Fauser (NL) and R. Reindollar (USA)Day 3 vs day 5 embryo transferA. Veiga (ES) and US speaker TBAInnovation in the medical treatment of Endometriosis.G.D. Adamson (USA)Focus on Reproduction January 2012 13
ESHRE NEWS// CAMPUS MEETING: SIGs ANDROLOGY, PSYCHOLOGY & COUNSELLING //The whole man, and not just his sperm, arepreferred under the diagnostic spotlight‘Low sperm count is not a diagnosis, it’s a physical sign’A debate in the main scientific session of this year’sannual meeting in Istanbul will ask: ‘Should wetreat the man or just use the sperm?’ As everwith ESHRE debates, the contest, pitchingmoral rectitude against practical expedience,will be enthusiastically heard - and no doubtwill end without a runaway winner.Had the same question been posed at aCampus workshop held in September inSeville, t<strong>here</strong> would have been no contest. Forthis was an event which, from its initialplanning, set out from the very premise that ‘thewhole man’, and not just his sperm, was theessential focus of investigation in the infertilecouple. ‘Sperm are too frequently used for thediagnosis of male infertility,’ said Australianandrologist Anne Jequier. ‘It’s a sad situation,but it’s cost effective and to some extent itworks.’Her talk - as well as those of others - waspeppered with salutary anecdotes of menpresenting with infertility but eventuallydiagnosed with testicular cancer and othermalignancies. Indeed, an unpublishedstudy of genito-urinary ultrasoundfindings from 1203 men attending herown fertility clinic in Perth foundtesticular cancers in five of them, renal lesions in 48, andtesticular microlithiasis in 66. ‘Diagnosis is what we want,’said Jequier. ‘Infertility is not a diagnosis, it’s a symptom.Low sperm count is not a diagnosis, it’s a physical sign.The diagnosis is the cause of the low sperm count.’During questions and playing the role of ‘devil'sadvocate’, Sheena Lewis, the new co-ordinator of the SIGAndrology, asked how examination or investigationsin the man might ever be useful if the outcome isalways IVF or ICSI. Such a question, of course, lies atthe heart of many charges levelled today againstthe treatment of infertility (both male andfemale) - that clinics have foresaken theclassical diagnostic paradigm in favour of anexclusively prognostic model. In women, forexample, why perform diagnostic laparoscopyif the treatment will still be IVF?This Campus meeting was organised bytwo of ESHRE’s SIGs, Andrology andPsychology & Counselling, and t<strong>here</strong> was nodoubt w<strong>here</strong> opinions on this sensitive matterlay. Indeed, as Uschi Van den Broeck madeclear, a diagnosis of infertility can be just asdevastating for men as for women andrequires just as much care in delivering thenews. A man’s ‘stereotype’ response tosuch news, said Uschi, might range fromdenial, to aggression and even to loss ofcontrol. But whatever the response, itnevertheless seemed clear from thesepresentations that men do respond to theirinfertility differently from women. Indeed,asked psychologist Tewes Wischman fromthe Institute of Medical Psychology inHeidelberg, do men ‘suffer’ less thanwomen, ‘or do they even suffer at all’?Data presented by Wischman indicated that for 49% ofwomen but only 15% of men infertility was the mostupsetting experience of their lives. Of course, as Wischmanreadily acknowledged, men may simply respond differentlyto any kind of stress, whether infertility or not, but t<strong>here</strong>USCHI VAN DEN BROECK:‘A DIAGNOSIS OFINFERTILITY CAN BE JUSTAS DEVASTATING FORMEN AS FOR WOMEN.’PETRA THORN: ‘MENCONSIDERING DI ORADOPTION MAY OFTENNEED MANY MONTHS TOACCEPT THE TREATMENTAS A REAL ALTERNATIVE.’14 Focus on Reproduction January 2012
Men need fertility preservation tooChemotherapy may have a similarly adverse effect onsemen parameters in men as on ovarian function inwomen. Roelof Menkveld, the Past Co-ordinator of theSIG Androogy, confirmed that both sperm functionand DNA status may each be affected, with aresulting increased risk of azoospermia and poorsperm function. Fertility preservation, he said, aheadof cancer treatment will provide an opportunity forlater conception through IUI or ART. Citing a study of2005 (Agarawal and Allamaneni), Menkveld reportedthat sperm volume, count and motility in 205adolescent cancer patients were almost half that ofcontrols, and in patients with testicular cancer andleukaemia sperm concentrations were considerablylower. The most negative effect of chemotherapyappears to be on DNA integrity. In 2007 Schmidt etal showed that before treatment 91% of a studygroup had fat<strong>here</strong>d a child, which fell to 67% aftertreatment.However, while semen cryopreservation will providea means of preserving fertility, cryoprservation itselfwill reduce sperm motility and reduce fertilisationpotential.So far, he added, the 'usefulness' of cryopreservedsemen seems limited, with studies suggesting anuptake of around 5% following cancer treatment.Menkveld's own experience, from a pool of 64 cancerpatients, has so far found an uptake rate of only4.7% - although he and others have emphasised thatthe storage of sperm gives hope and confidence tomany young men that they do have a future after theircancer treatment.Volume (ml)Count (106/ml)Motility (%)Morphology(% normal)Before freezingMean (SD) Range2.8 ± 1.5 0.5 - 7.039 ± 29 0.1 - 10045 ± 11 0 - 605.8 ± 5.2 1.0 - 18After freezingMean (SD) Range--18 ± 13 4.5 - 40.023 ± 12 0 - 40.0--The effect of cryopreservation on semen parameters in 64cancer patients (Menkveld unpublished data).does seem to be a degree of stigmatisation about infertilityfor men which women don’t feel. ‘Women with fertilityproblems tend to be pitied,’ said Wischman citing a 1992study of Nachtigall et al, ‘w<strong>here</strong>as men are more likely toencounter insulting slurs on their manhood.’ Even the basicsemen analysis, he added, has sexual connotations in itsdemand for a semen sample.Despite the gender differences, Wischman concluded thatmen do indeed suffer on account of their infertility, but feelthey have fewer outlets than women to express theirfeelings - and of course counselling should recognise thesedifferences and provide its information and support in away which acknowledges the differences. He also showedthat men felt a need to be strong for their partners, andthus tend to hide their own feelings.This same gender gap is apparent in how men react toparenthood following treatment by donor insemination -what Petra Thorn, a former co-ordinator of the SIGPsychology & Counselling, called a ‘shift from biologicalto social fatherhood’. She proposed that only biologicalfatherhood is considered by many men as ‘real’fatherhood, and that men considering DI or adoption mayoften need many months to accept the treatment as arealistic alternative. And even as the child grows t<strong>here</strong> maywell remain tensions for the man - between his own role asa ‘social’ parent and his partner’s as the ‘biological’ parent.Similar tensions might be played out over disclosure anddonor identity. Again, said Petra, these are tensions anddifficulties which counselling can help explore and resolve.Thus, if the proper place of a man in the fertility clinicrequires full investigation and the sensitive support ofcounselling, how important are the conventional tests ofbasic semen analysis? Anthony Hirsh, an andrologist fromLondon, left no doubt that sperm dysfunction represents‘the largest defined cause of human subfertility’. But t<strong>here</strong>was also evidence that many of the studies on which thelatest WHO reference values for semen analysis were basedwere in fact methodologically unreliable - with inconsistentstandards evident in laboratory methods, statisticalmethods and results.And, as Sheena Lewis made clear in her presentation(and as she explains in more detail on page 27) semenanalysis itself has limited diagnostic value for maleinfertility - and is not predictive for ART outcome.Techniques such as IMSI or tests for birefringence havesought to provide a non-invasive dimension beyondconventional semen analysis, while the latest sperm DNAtests now seem able to improve ART results in both malefactor and unexplained infertility.Of course, bubbling beneath the surface of this meetingwas the fact that ICSI can now - according to AnthonyHirsh - ‘treat’ 98% of all cases of male factor infertility,though not always successfully. And the long-term followupstudies of ICSI babies performed at the Free UniversityHospital in Brussels are accumulating ‘reassuring data’ inthe overall health, gonadal function and psychologicaldevelopment of the children born. So the debate inIstanbul, that treatment should be directed at the man andnot just his sperm, will not be easily won. But <strong>here</strong> was astrong case in favour, that infertility may mean to a manmore than just a sperm deficiency, and that thepsychological implications, as well as the physiological,require a broad interpretation.Simon BrownFocus on ReproductionFocus on Reproduction January 2012 15
PGD CONSORTIUM// THE PAST YEAR IN REVIEW //Trends from a decade of PGD: ten years ofdata collection now seen in perspectiveA manuscript summarising data collections I-Xhas now been accepted for publication. Thepaper aims to review the massive amount ofdata collected so far by the Consortium and tolook at the data from a more distant perspectiveand consider trends in the whole field of PGDas they changed over the decade. Datacollection XI was late being submitted forpublication but should have been submittedbefore the end of 2011.Consortium statutes now being revisedWorking groupsVery exciting developments have taken place inthe array-based PGD working group. ESHRE’sExecutive Committee has agreed to consider thedevelopment of a guidelines document forarray-based PGD, and we are presently puttingtogether a development group. A new externalquality assessment scheme for array-based PGDis also being developed to assess testing qualityaround the world. This EQA, following a pilotstudy, will be open to any labs using arraybasedtechnology to assess aneuploidy in humanembryos.The Accreditation working group held a verysuccessful workshop in conjunction withEurogenetest in Athens, Greece, titled TowardsAccreditation of a PGD Laboratory. Thisworkshop will be repeated this year in Istanbulin the Autumn.The Misdiagnosis and Monitoring workinggroup continues to work on publication of the follow-updata from amplification-based and FISH-based PGD tests.This will be a landmark paper, featuring follow-up ofuntransferred embryos following PGD testing.The Molecular Methods working group continues todevelop a database of primers and protocols to aid Fulland Transport Member laboratories in developingcustomised PGD testing methods for patients in need oftests for monogenic disorders.Finally, the the Consortium Steering Committee hasbegun to develop a plan to help educate laboratoriesthrough a lab visitation and exchange scheme as well asoffering online learning opportunities (case studies,discussion, etc). This will hopefully be a big hit.Gary HartonChair PGD ConsortiumThe statutes which govern the organisation and running of theConsortium are now being revised before ratification of theExecutive Committee. Following their approval, a new SteeringCommittee will be put in place. The current Committee (most ofwhom are pictured above) comprises Gary Harton (US, Chair),Joanne Traeger-Synodinos (GR, Deputy Chair), Joyce Harper (GB,Past Chair), Céline Moutou (FR), Katerina Vesela (CZ), SiobanSengupta (GB), Georgia Kokkali (GR), Leeanda Wilton (AU),Martine De Rycke (BE), Tugce Pehlivan (TR), Pamela Renwick(GB), Edith Coonen (NL) and Francesco Fiorentino (IT).Participants in last year’s accreditation workshop held in Athens.The meeting will be repeated later this year in Istanbul.16 Focus on Reproduction January 2012
SPECIAL INTEREST GROUPS// EMBRYOLOGY //Culture media high on the agenda for IstanbulWorkshopsTime passes quickly, and it is againtime to report our activities. Since thelast issue of Focus on Reproductionin September, we have had aworkshop in St Petersburg, Russia, incollaboration with the SIGReproductive Endocrinology and theParamedical group. T<strong>here</strong> were almost 200 participants,and the evaluation was very positive indeed.Joint workshops are often very successful because of theopportunity to expand knowledge to topics outside ourmain area of interest, to subjects that often overlap witheach other. It is a great opportunity to work together withother SIGs and Task Forces.So, for 2012 we have plans for more joint workshops.The first is an event organsied with the SIG ReproductiveGenetics and Task Force Basic Science, the 7th workshopon Mammalian folliculogenesis and oogenesis due to takeplace in Stresa, Italy, on 19-21st April. The course has ascientific focus, with topics covering the full circle fromprimordial cells, through meiosis and maturation, to theinfluence of maternal health and diet.In the autumn we are planning a practically orientedcourse with the SIG Andrology, The best sperm for the bestoocyte to take place in Greece in October, the exact datestill to be decided. Check on the website for updates!Culture media in Istanbul 2012Although now cold and dark, we have a summer meetingto look forward to . . . our precongress course at theannual meeting in Istanbul, which will be focused on IVFculture media. This is a very hot topic indeed. We knowthat culture media are becoming more and more complex,enriched with different supplements, with compositions notfully known by the users. It has been shown that differentculture media have different effects, not only on embryoquality and implantation rates, but also on pregnancyoutcome such as fetal growth and birth weight. Thisimplies that culture media affect in<strong>here</strong>nt factors, possiblyrelated to epigenetics. Our precongress course in Istanbul,Culture media: the best environment for gametes andembryos, will consider what oocytes and embryos need -and perhaps do not need - and how embryo culture andenvironment might influence early development.Embryology certificationThe clinical embryology certification exam in Istanbul isSteering committeeKersti Lundin (SE), Co-ordinatorMaria José de los Santos (ES), DeputyJosephine Lemmen (DK), DeputyCristina Magli (IT), Past Co-orindatorAna Sousa Lopes (BE), Junior Deputythe first for which embryologistsfrom outside Europe have beenallowed to apply. The procedure ismoving along well.We are also pleased to announce thatESHRE certified embryologists cannow renew their certification throughthe new CEEC (ContinuousEmbryology Education Credit) system to be launched verysoon. As reported on page 6, this is a voluntary scheme tostimulate continual learning by clinical embryologists, tovalidate their attendance at meetings and workshops andrecognise publications and other activities. However, thescheme does not imply any loss of validity from apreviously obtained ESHRE clinical embryologycertification.The Atlas of Embryology: from oocytes to preimplantationembryosWe are happy and proud to announce that the newembryology atlas is not far off completion. The workinggroup, led very efficiently by Gayle Jones, has done afantastic job, together with the ESHRE’s Central Office andIT team. The atlas, in an electronic format, will contain alarge number of pictures of oocytes, zygotes, cleavage stageembryos and blastocysts, fresh and frozen, groupedaccording to development and scoring. We believe that itwill be very valuable for embryologists to share a commonnomenclature as well as having a dynamic reference andlearning tool.Kersti LundinCo-ordinator SIG EmbryologyA first glimpse of how the Atlas of Embryology will look.Focus on Reproduction January 2012 17
SPECIAL INTEREST GROUPS// STEM CELLS //EU ruling bans patents on inventions whoseprocesses involve human embryonic stem cellsThe Court of Justice of theEuropean Union ruled in Octoberthat an invention is excluded from‘patentability’ w<strong>here</strong> theimplementation of the processrequires either the prior destructionof human embryos or their prioruse as base material, even if in the patent application thedescription of that process does not refer to the use ofhuman embryos. 1 This ruling, which was made public in apress release dated 18th October 2011, was delivered afterGreenpeace claimed that a patent held by the Germanscientist Oliver Brüstle was invalid because it described thedifferentiation of human embryonic stem cells intoneuronal progenitors.The CJEU’s chain of reasoning was briefly as follows:human embryos (including embryos obtained after somaticcell nuclear transfer and parthenogenetically activatedembryos) are protected by Directive 98/44/EC on the legalprotection of biotechnological inventions. As hESCderivation is usually achieved through the destruction of ahuman embryo, hESC are thus included in the concept of‘human embryo’. The court further concluded that the usesof human embryos (and thus hESC) which are not‘patentable’ should include scientific research as well as‘industrial and commercial’ purposes.The ruling has led to a flurry of reactions fromdistraught European scientists, supported by theirAmerican colleagues, who at times could not conceal a hintof Schadenfreude. Indeed, Googling ‘stem cells EU ruling’between 18th October and 22nd November uncoveredabout 170,000 hits. Here, we quote a few of the commentsfrom a wide spectrum of journals and papers, and startwith the hapless Professor Brüstle, who said: ‘With thisunfortunate decision, the fruits of years of translationalresearch by European scientists will be wiped away and leftto the non-European countries. European researchers mayconduct basic research, which is then implementedelsew<strong>here</strong> in medical procedures, which will eventually bere-imported to Europe. How do I explain that to the youngscientists in my lab?’ 2Similarly and on the same website (eurostemcell.org), thewell known stem cell biologist Austin Smith commented:‘This unfortunate decision by the Court leaves scientists ina ridiculous position. We are funded to do research for thepublic good, yet prevented from taking our discoveries tothe market place w<strong>here</strong> they could be developed into newmedicines. One consequence is that the benefits of ourSteering committeeKaren Sermon (BE), Co-ordinatorRita Vassena (ES), DeputyAnis Fekis (CH), DeputyCarlos Simon (ES), Past Co-ordinatorresearch willbe reaped inAmerica andAsia.’Catherine Verfaillie,another high-profile stem cell researcher, said in NatureReviews Drug Discovery: ‘The decision is strange becausethe EU Commission allows us to do innovative research –and indeed funds such research on established ESC lines,but as a result of this decision much of this work will nownot be valorizable.’ 3And from across the Atlantic a comment from RobertLanza in the Wall Street Journal, which we cannot helpthinking was made with a wry chuckle: ‘Of all theintellectual work being done in Europe, if something issuccessful it will now be [commercialised] by a companyoutside Europe. Europe is basically exporting itsresearch—it is unfortunate.’ 4Indignant outcries were also heard from the ethical andlegal corner. In the same Nature Reviews Drug Discoveryarticle as Catherine Verfaillie, Julian Hitchcock, senior lifescience intellectual property solicitor and regenerativemedicine specialist at Field Fisher Waterhouse, London,said: ‘The decision represents a dangerous expansion ofthe legal concept of human dignity laid down in the EUCharter of Fundamental Rights . . . But by giving theblastocysts rights that are the same as those of humanbeings, the dignity of patients has been seriously harmedbecause the mechanism by which new treatments aredeveloped has been impeded.’ 3 However, the same JulianHitchcock is quoted in a Nature news article as saying:‘Even a restrictive interpretation should allow companiesto patent the technologies needed to turn human ES cellsinto treatments, rather than patenting proceduresinvolving the cells themselves . . . Growth media,equipment and chemicals that help scientists to work withstem cells could all be patented in Europe without runningafoul of the high court’s ruling. For instance, Peter Coffeyat the Institute of Ophthalmology in London and his teamare working with the drug giant Pfizer to develop ahuman-ES-cell-based treatment for macular degeneration,18 Focus on Reproduction January 2012
a progressive disease of the retina that causes blindness.Their patents cover the placement of their retinal cells inthe eye, not the cells themselves.’Indeed, it was even suggested that the absence of pressurefor patenting might even create an atmosp<strong>here</strong> for freerresearch in Europe. 5 This of course would depend on theexplicit condition that research-granting agencies changetheir policies in favour of more and more translationalresearch which is easily ‘valorised’. As a career-longresearcher, scrabbling year after year for the sustenance ofgranting agencies for fundamental research with everdecreasing budgets, I have doubts about this evolution.Hearing the influential voices that have spoken outagainst the ruling (for example, Austin Smith in Naturecomments, 6 ) creating an environment conducive to researchand development in our field of ART, embryology and stemcells in the EU remains an uphill struggle. Conservativeopinions, sometimes coming from unexpected corners suchas Greenpeace, seep into regulation via laws which areabused to ends different from their initial aim. Here again,as in so many places, scientists should come out of theirlabs as citizens, voicing their opinion in political arenas. Inmy lab, everyone withdrew their Greenpeace membership.A small and perhaps empty gesture, but it’s a start.Karen SermonCo-ordinator SIG Stem CellsReferences1. Court of Justice of the European Union: Judgment in Case C-34/10: Oliver Brüstle v Greenpeace e.V. The press release isreproduced on the SIG Stem cells page of the ESHRE website.2. European Court bans stem cell patents. http://www.eurostemcell.org/story/european-court-bans-stem-cell-patents.3. EU bans embryonic stem cell patents but decision may havelimited implications. Charlotte Harrison. Nature Reviews DrugDiscovery, published online 11 November 20114. Patent Ruling Sets Back EU Stem-Cell Scientists. G Naikhttp://online.wsj.com/article/SB10001424052970204346104576639010759884794.html5. European ban on stem-cell patents has a silver lining.Researchers can work without fear of action over patentinfringement. Ewen Callaway. Nature 2011; 478: 441.6. Smith A, et al. Nature 2011; 472: 418.KAREN SERMON: ‘CREATINGAN ENVIRONMENTCONDUCIVE TO RESEARCHAND DEVELOPMENT IN OURFIELD IN THE EU REMAINSAN UPHILL STRUGGLE// REPRODUCTIVE GENETICS //Publication planned on the dynamics and ethics of PGSWe ran three successful Campusworkshops in 2011.Building on our previouslysuccessful courses in London (2007),Athens (2008), Strasbourg (2009)and Porto (2010), a Basic Geneticsfor ART Practitioners course washeld in September 2011 in Bucharest,Romania, with a total of 82 participants registered andvery positive course evaluations. This was a greatopportunity to promote ESHRE (and our learningopportunities) in Eastern Europe. This same course will berun in Rome on 7th September 2012.In October a joint meeting of the SIG RG and SIG Ethics& Law was held in Maastricht titled Comprehensivepreimplantation screening: dynamics and ethics. T<strong>here</strong> wasmuch discussion on this rapidly advancing field of genetictesting and what it will mean for reproductive medicine. Apublication is planned of the issues discussed.Our third Campus event was held in Athens in Octoberand was a joint meeting with EuroGentest and the PGDConsortium on Accreditation of a Preimplantation GeneticDiagnosis Laboratory. This is the third qualitySteering committeeJoyce Harper (GB), Co-ordinatorClaudia Spits (BE), DeputyUrsula Eichenlaub-Ritter (DE), DeputyStéphane Viville (FR), Past Co-ordinatorTania Milachich (BG), Junior Deputymanagement meeting organised bythe PGD Consortium, and a similarfourth workshop is planned forIstanbul in 2012.The precongress course inStockholm, From genes to gestation,was organised with the SIG EarlyPregnancy. In Istanbul our course is ajoint venture with the SIG Safety and Quality in ART andis titled Known and unknown congenital, genetic andepigenetic risks for children born following ART: basic andclinical data, with an excellent line-up of speakers.In 2005, a meeting jointly organised by ESHRE and theEuropean Society of Human Genetics was held in Sevilleand resulted in the publication of a paper in 2006 by Soiniet al (The interface between assisted reproductivetechnologies and genetics: technical, social, ethical andlegal issues) in Human Reproduction and the EuropeanJournal of Human Genetics. We now feel it is time torevisit this important topic, so a joint ESHRE/ESHGmeeting will be held in Brussels in March 2012.Joyce HarperCo-ordinator SIG Reproductive GeneticsFocus on Reproduction January 2012 19
SPECIAL INTEREST GROUPS// REPRODUCTIVE SURGERY //A possibility of certification in laparoscopic surgeryLast year we hosted two verysuccessful, fully booked workshops inLeuven - with targeted lectures, drylab and live surgery - and organised acollaborative meeting with the RCOGin London. The latter increasedvisibility of the SIG RS and proved animportant platform for ESHRE toattract interest from other societies in reproductive surgery,education and important technical skills.This year our aim is to provide the highest educationalvalue and to increase both attendance at our meetings andinterest in ESHRE. With this in mind we will hold twofurther training courses in 2012, both in Leuven, inFebruary and November. In addition, we are organising aworkshop in Larnaca, Cyprus, on 16-17th March onReproduction and the management of fibroids, which willcover topics from basic research to operative techniques.We have recently raised the difficult issue of managingcongenital uterine pathology and have set up with theEuropean Society for Gynaecological Endoscopy (ESGE) atask force aiming to improve diagnosis and treatment.Our future plansOur basic training courses in Leuven will continue into2013 (in February and November) and we are makingplans for two further workshops - one in Romania in Aprilor May 2013 on The importance of reproductive surgery inincreasing pregnancy rates in ART, and a second inThessaloniki, Greece, in September on Female genital tractcongenital malformations: an update. The former, organisedSteering committeeVasilios Tanos (CY), Co-ordinatorTC Li (GB), DeputyGregoris Grimbizis (GR), DeputyNatasa Kenda Suster (SI), Junior DeputyMarco Gergolet (IT), Past Co-ordinatorby Razvan Sokolov, will reviewminimally invasive techniques forthe diagnosis and treatment ofinfertility, including the treatment ofuterine anomalies and the effect ofmyometrial pathology in successfulART. The latter, organised byGregoris Grimbizis, will examinethe aetiology, pathophysiology and genetic background ofcongenital anomalies, the different diagnostic techniques,and treatments.Certification in laparoscopic surgeryA report from the Dutch ministry of health in 2007 foundtraining in laparoscopic surgery variable and inadequatelystructured, highlighting a more general concern that thestandards which a future laparoscopist must meet in orderto operate - either independently or under supervision -have not been adequately established.Against this background the SIG RS has recently beenconsidering the idea of a programme of certification inlaparoscopic surgery in collaboration with the ESGE. Ouridea is that ESGE would take responsibility for the basiccertification, and ESHRE for subspecialty certification. Itis our opinion that such an arrangement would be anattractive package, not just for the provision of systematiclearning and certification at the general and subspecialtylevels, but also to increase support for ESHRE’sprecongress courses and scientific sessions.Vasilios TanosCo-ordinator SIG Reproductive Surgery// REPRODUCTIVE ENDOCRINOLOGY //High attendances justify integrated training programmesThe past year has continued in thepattern of 2010 with three wellattendedworkshops, a basic trainingworkshop and a precongress course inStockholm with 200+ participants. Wecovered a wide range of subjects, fromthe oncological impact of ART inGermany in February, topericonception care in the infertility clinic in the UK inMay, to the most common endocrine disorder in our field,PCOS, in Bulgaria, in December. Last year's precongresscourse in Stockholm was on ovarian ageing, which seemsto be gradually replacing the classic causes of infertility asthe main reason for referral of patients to IVF treatment.Steering committeeGeorg Griesinger (DE), Co-ordinatorFrank Broekmans (NL), DeputyEfstratios Kolibianakis (GR), DeputyAdam Balen (GB), Past Co-ordinatorDaniela Romualdi (IT), Junior DeputyBasic training workshopsOur training workshop in 2010 inKiev and 2011 in St Petersburgattracted very high attendances - 202and 185 participants - reflecting theneed for such high-quality basictraining from ESHRE. With theseresponses in mind, we have proposedto ESHRE’s Executive Committee the construction of a coordinatededucation strategy for basic training among allthe SIGs, with at least one basic training course a yearoutside the EU. This would meet an undoubted educationalneed and increase ESHRE’s influence as the major scientificrepresentative in reproductive medicine. 20 Focus on Reproduction January 2012
EARLY PREGNANCY //An audience response system for ESHRE courses?The SIG Early Pregnancy coorganisedtwo meetings in thelatter half of 2011. Our jointmeeting with European Society ofReproductive Immunology inCopenhagen in August, onintegrating clinical, epidemiologicaland immunological aspectsof early pregnancy complications,was a great success, with 165participants, most of whom stayeduntil the last session of the last day!At the ASRM congress inOrlando we took part in a popularexchange workshop which focusedon the diagnosis and managementof pregnancy of unknown location,chromosome testing in patients withrecurrent miscarriage, recurrentmiscarriage terminology andevidence-based management ofrecurrent miscarriage. DivergingEuropean and American viewswere discussed, and it was fascinating to experience theuse of an audience response system (ARS) enablingsmart phone answers to questions embedded in thepresentations. ARS seems an exciting tool for activatingthe audience and encouraging immediate feed-backduring lectures. We hope ESHRE will consider an ARSsystem in future precongress courses.Future activitiesOur precongress course in Istanbul will be titledGamete quality and ovarian reserve as markers forearly pregnancy loss. The faculty will review theevidence (or lack of) that markers of poor sperm orSteering committeeOle B Christiansen (DK), Co-ordinatorMariette Goddijn (NL), Deputy Co-ordinatorSiobhan Quenby (GB), Deputy Co-ordinatorMarcin Rajewski (PL), Junior DeputyRoy Farquharson (GB), Past Co-ordinatorThe 2011 joint ESHRE/ASRM workshop facultyfor early pregnancy: from left to right, RoyFarquharson (GB), Kurt Barnhardt (US), MarietteGoddijn (NL), Ole Christiansen (DK),WilliamKutteh (US), and Mary Stephenson (US)oocyte quality are predictive ofbiochemical pregnancy/miscarriage, especially afterART. We hope that manyclinicians in ART who normallydo not consider early pregnancyas their main interest area willfind this course attractive.On 29-30th November ourregular winter Campus coursein Amsterdam will be organisedby Mariette Goddijn onEvidence based early pregnancycare. The course will focus onthe management of ectopicpregnancy and recurrentmiscarriage, with a session onthe organisation of earlypregnancy care units anddebates on RCTs in earlypregnancy disorders.For 2013 we have alreadymade plans for a jointASRM/ESHRE precongress course before the annualmeeting in London on risk factors for recurrentpregnancy loss. An early pregnancy session during thescientific programme has already been planned onGathering evidence in early pregnancy research –Making trials happen.During the next months procedures will begin fornominating and electing a new Deputy Co-ordinatorand Junior Co-ordinator to take up their posts inIstanbul. We hope you will be t<strong>here</strong> at the precongresscourse to meet them.Ole B. ChristiansenCo-ordinator SIG Early PregnancyFuture activitiesThe title of our precongress course in London in 2013 willbe Ovarian stimulation for ART: how to achieve efficacyand safety? We are also asking for applications for ESHRECampus workshops for 2013. Please send any proposals tome at griesing@uni-luebeck.de. We will need to pick thebest applications in terms of originality, meeting structure,venue and accessibility.In 2012 we have the following events:• Anti-Mullerian hormone: An update, Lille, 10-12thMay, a Campus workshop designed to provide anevidence-based update on the role of AMH incontemporary reproductive medicine. All aspects of AMH,from its function within the ovary, its relationship withfollicle number throughout life, and to its use for assessingovarian reserve, defining PCOS and predicting themenopause will be featured.• GnRH-antagonists in ovarian stimulation, Frankfurt,28th September, a one-day workshop which will cover allclinical aspects of ovarian stimulation with GnRHantagonists.The aim of the workshop is to provideparticipants with a comprehensive and detailedunderstanding of the evidence basis of ovarian stimulationwith antagonists, and how to utilise them for a safer andsimpler IVF treatment. Areas of debate and directions forfuture research will be highligted.Georg GriesingerCo-ordinator SIG Reproductive EndocrinologyFocus on Reproduction January 2012 21
SPECIAL INTEREST GROUPS// ENDOMETRIOSIS & ENDOMETRIUM //Activities focus on the impact of endometriosis onpatients’ symptoms - pain, fertility and quality of lifeOur Campus meeting onEndometriosis and IVF heldin a sunny and warm Romein October was wellattended and fully bookedwith some 100 participants.The event was organised bythe SIGEE in collaborationwith local IVF specialistFilippo Ubaldi (a past member of the ESHRE’s ExecutiveCommittee) and Marco Sbracia. Excellent lecture contentwas accompanied by stimulating discussions. The first dayfocused on novel aspects of basic research in endometriosis,followed by extensive sessions on ovarian reserve inpatients with endometriosis, ovarian hyperstimulationregimes and outcomes of IVF. The last lectures of the firstday considered the risk of ovarian cancer in patients withendometriosis in relation to IVF - and timely observationshave emerged. The second morning considered thesurgeon’s perspective in relation to reproductive outcomesand fertility preservation. The final lectures addressedobstetric morbidity in IVF-derived pregnancies of womenwith endometriosis. First feedback from the meeting hasindicated a general appreciation of the high qualitypresentations and the opportunity for discussion ofcontroversial topics, such as the best surgical technique forovarian endometriomas.Precongress coursesWe will revisit the impact of endometriosis in our 2012precongress course in Istanbul, Pain and endometriosis.Here we propose to address clinical issues as well asmechanistic insights and best available evidence for clinicalmanagement of this highly distressing symptom. Our targetaudience is all providers of care for women withendometriosis, including clinicians, nurses and scientists(and neuroscientists) with an interest in endometriosis andpain mechanisms. We also encourage attendance of thosewho provide multi-/ cross-discipline care.Looking further ahead to London in 2013 we willbroaden the agenda with a programme which examines theimpact of pelvic pain and uterine bleeding on quality of life.Steering committeeHilary Critchley (GB), Co-ordinatorAnneli Stavreus-Evers (SE), Deputy Co-ordinator EndometriumGerard Dunselman (NL), Deputy Co-ordinator EndometriosisAnnemiek Nap (NL), Junior DeputyPaola Vigano (I) Basic Science representativeThomas D’Hooghe (BE), Past Co-ordinatorIt has been rewarding tohave received so muchsupport from SIGmembers for this PCCproposal and we willendeavour to do justice toyour enthusiasm for thistopic.Junior membershipOur SIGEE Junior faculty has been active and thanks aredue to Annemiek Nap for driving forward this initiative.In an update from Annemiek she informs us that ‘thejunior faculty of the SIGEE is an enthusiastic internationalteam of young clinicians and basic investigators from fivedifferent European countries who are active in the field ofendometrial research and endometriosis’.The goal of the junior faculty is to ensure we have apipeline of enthusiasm with a mission to improve the careof those suffering from endometriosis and fromendometrial diseases. International consensus on optimaltreatment strategies may help to achieve this importantgoal. As a result, the junior faculty team is active in theESHRE Endometriosis Guideline Group, which iscurrently updating the ESHRE Endometriosis Guidelines.Looking ahead, t<strong>here</strong> is a need for the development ofmore multidisciplinary treatment teams for endometriosis,consisting of gynaecologists, surgeons, urologists,gastroenterologists, nurses, pain specialists, andpsychologists/counsellors. Preferably, thesemultidisciplinary teams would be active in networks ofexpertise for endometriosis. Making young doctors inthese professions aware of the problem of endometriosiswould be a first step towards an increase in the number ofexperts treating the disease.But for the moment it is terrific to have such enthusiasmfrom amongst the members of the SIG Endometriosis andEndometriumHilary CritchleyCo-ordinator SIG Endometriosis & Endometrium22 Focus on Reproduction January 2012
PSYCHOLOGY AND COUNSELLING //New guidelines anticipated by London 2013New guidelinesThe new Psychology and CounsellingGuidelines now in development willprovide best practice advice on howpsychosocial care can be incorporatedinto daily practice to the benefit ofpatients and healthcare providers inthe field of infertility and ART. Weaim to create a framework that takes into considerationthe different ways in which healthcare is managedthroughout Europe. Thus, despite socio-cultural and legaldifferences in Europe, the Guidelines are intended to beapplicable to all countries.Several meetings for the development of the guidelineshave already taken place. The last was held during theannual meeting in Stockholm, w<strong>here</strong> the scope of theguidelines was discussed. The group is now working ondefining key questions, which will lead to the collection ofevidence for evaluation. ESHRE’s research specialist,Nathalie Vermeuelen, is assisting us in this process and willconduct the evidence search. She will also train the teamon how to systematise and evaluate the quality of theevidence gat<strong>here</strong>d; it is from this evidence thatrecommendations on how to incorporate psychosocial careinto daily practice will be made. We are expecting topresent the guidelines at the 2013 annual meeting inLondon.Steering committeeChris Verhaak (NL), Co-ordinatorJan Norré (BE), DeputyUschi Van den Broeck (BE), DeputyPetra Thorn (DE) ,Past Co-ordinatorSofia Gameiro (PT), Junior DeputyBudapest Campus workshopIn March we will visit Eastern Europe to deliver aworkshop in Budapest, Hungary. The workshop will focuson developing competence in psychosocial care andcounselling. This 1.5 day course will introduce participantsto psychosocial issues present at different times andsettings of the infertility experience and will provide indepthcase-discussions to deepen understanding andincrease skills for providing psychosocial care.The course has two target audiences: professionalsinvolved in the general care of people with infertility, suchas physicians, nurses and administration staff; andpsychologists and counsellors, who will be offered trainingin specific areas, such as couplestherapy or in loss and bereavement.The goal is for fertility professionalsto acquire skills for improvingpsychosocial care and/or counsellingin various settings and for variousspecific situations.IstanbulAt this year’s annual meeting in Istanbul our precongresscourse will focus on the burden of fertility treatment. Thecourse is directed at medical doctors, nurses andparamedical staff and counsellors and others involved inpsychosocial care. The aim of the course is to promotereflexion on how fertility healthcare professionals can helpmanage the burden of treatment, which will be addressedfrom different perspectives. Topics will include treatmentdrop-out, implications of different treatment protocols,impact on sex life, dealing with unsuccessful treatment, theuse of online resources to manage the burden, patient andhealthcare provider communication and quality of care.The course will end with a round-table discussion.Following the precongress course, our SIG businessmeeting welcomes all members. This year we will discussprevious and upcoming Campus events and an update ofthe progress of the guidelines will be provided. The daywill finish with our annual dinner in the city centre, held inconjunction with the International Infertility CounsellorsOrganization (IICO). Everyone interested in joining thedinner may contact Uschi Van den Broeck(uschi.vandenbroeck@uzleuven.be) for more information.This is a very promising year for the SIG Psychology andCounselling and we hope to see many of you in Budapestand Istanbul.Don’t forget for your 2012 diaries:- ESHRE Campus, Developing competence in psychosocialcare and counselling, Budapest, 23-34 March 2012- ESHRE annual meeting, Istanbul, 1-4 July 2012Sofia GameiroJunior Deputy Co-ordinatorSIG Psychology and CounsellingFocus on Reproduction January 2012 23
TASK FORCES// EU TISSUE AND CELLS DIRECTIVE //End-of-year report:short-term targets met,and hopes high forresolution on repeatserological testingAims of the EUTCD Task Force• Ascertain the impact of the EUTCD in Europe• Encourage best collaboration with the regulators(SANCO, SOHO (V&S))• Provide the evidence to help ESHRE lobby for aseparate ART Directive• Establish the highest professional standards in ART• Provide ESHRE with the documentation to helpcollaboration with the competent authorities.Impact of the EUTCD in EuropeA questionnaire sent to all members of ESHRE’sCommittee of National Representatives in spring 2010found that most (15/19) had by then fully implemented thethree directives, but found variance in nationalrequirements for serological testing, and even inconsistencyin the definition of what a ‘treatment cycle’ was. Ten of the19 member states defined ‘treatment’ as a single oocyterecovery procedure, but one also included subsequentfrozen cycles, and two made no definition at all. One inthree considered a ‘chain’ of egg collections as a cycle.Collaboration with the regulators (SANCO, SOHO-V&S)SANCO (Directorate General for Health and Consumers)• The collaboration between the Task Force, competentauthorities and the European Commission has resulted inmultiple meetings in Brussels. The meetings took placeunder the auspices of the DG SANCO and focused ontesting requirements for partner donation.• These meetings aimed to address the risk of crosscontaminationduring cryopreservation and otherprocessing and storage steps, the mix-up of gametes, thetransmission of communicable diseases from the embryo tothe mother and vice versa, and the reporting of seriousadverse reactions and events (SARE). A final document hasbeen produced for the attention of the competentauthorities and the Commission, with the final decisionstill awaited. The evidence in favour of less frequentscreening is overwhelming.SOHO-V&S (Substances of Human Origin - Vigilance andSurveillance)Task Force representatives took part in the three SOHOV&S meetings of 2010 and 2011.• The project itself aims to identify specific issues relatedto vigilance and surveillance, adapt the EUSTITE V&Stools to assisted reproduction, and make recommendationsfor the reporting of serious adverse reactions and events.To this end, the Task Force developed a paper on triggeringconditions for rapid alerts and contributed to all otherART-related topics addressed.• A final document entitled ‘Guidance on Vigilance &Surveillance in Assisted Reproductive Technologies in theEuropean Union’ has now been submitted to the EuropeanCommission. It covers the following areas: ART specificterminology, equipment and practices, safety in ART,reporting of SARE, triggering conditions for rapid alertsand ART-specific reporting tools.Evidence for a separate ART DirectiveRisk of seroconversion in the ART populationData from a single centre and three European centres hasbeen collected and submitted to SANCO as evidence thatthe risk of seroconversion in ART couples is negligible.• One paper on the risk of seroconversion in ART from asingle centre has just been published (Hughes C, Grundy K,Emerson G, Mocanu E. Viral screening at the time of eachdonation in ARTpatients: is itjustified? HumReprod 2011; 26:3169-3172).Another paperon risk ofseroconversionat Europeanlevel (threeEuropean countries)is in advancedpreparation.Feedback to ESHRE membersThe Task Force has taken part in the member’s informationsession at the annual meetings in Rome and Stockholm,and reported its activities in Focus on Reproduction.Future tasksThe Task Force has had a significant impact in promoting abetter understanding of the specific circumstances of theDirective relevant to ART. A clearer message for ARTpractitioners, centres, competent authorities and theEuropean Commission has emerged based on the 24 Focus on Reproduction January 2012
BASIC REPRODUCTIVE SCIENCE //ESHRE Campus at newreproductive biologyworld congressThe Task Force took part in the second Word Congress onReproductive Biology, held in Cairns, Australia, inOctober, with the organisation of a full day’s Campussatellite course on Human reproductive tissues, gametesand embryos: innovations by science-driven culture andpreservation systems. The event was greatly appreciated byparticipants, as reproductive biologists extend theirunderstanding of the potential applications of theirresearch in clinical medicine.It is also one of ESHRE's stated priorities to enhancerelationships with basic scientists in the area ofreproductive biology. In the long run, this strategy aims toboost scientific research and education in our field, notonly to raise practice and research standards in clinicalembryology, andrology and cryopreservation labs, but alsoto increasingly attracting both established and youngresearchers to the ESHRE meetings.The WCRB attracted more than 500 scientists fromthroughout the world and had the official representation ofthe Society for the Study of Reproduction, (USA), Societyfor Reproduction and Fertility (UK), Society forReproductive Biology (AUS), and the Japanese, Chineseand Korean societies of reproductive biology. The meetingParticipants in the ESHRE workshop, including ESHRErepresentatives Ursula Eichenlaub-Ritter and Carlos Plancha inthe near foreground.was held in the very modern Congress Palace in Cairns andthe local organisers under the leadership of Daryll Russellhad prepared excellent intermezzos and social events, sothat participants from all parts of the world couldintermingle. The scientific programme was top quality,with participating societies delegating some of their leadingperformers. Speakers included Ursula Eichenlaub-Ritter,Carlos Plancha and Johan Smitz from ESHRE, and DebraGook and Rob Gilchrist from Australia.The next WCRB will take place in Edinburgh inSeptember 2014 (with satellite meetings organised for 1-2nd September), hopefully with an even strongerrepresentation of ESHRE as a world player inreproduction science.Johan SmitzCo-ordinator TF Basic Reproductive Sciencepublished literature and as a consequence of the evidencecollected. The EC continues to base its decisions onpublished evidence only, and articles that address ARTpractice covered by the Directive should receive priority inESHRE peer-reviewed journals.While the issue of repeat serological screening is expectedto be favourably resolved in spring 2012, pending finalapproval of the competent authorities and EuropeanCommission, the Directive has numerous areas that stillrequire immediate attention, notably:- identifying areas that require further definition andamendment from an ART perspective- the Task Force’s own proposal for the establishment of aEU-ESHRE ART inspector training programme. Thiswould provide training for inspectors in the field of ARTby bringing the expertise of ESHRE and the competentauthorities together. It is now opportune to use thegoodwill and trust built up between the Task Force, thecompetent authorities and the Commission to consolidateESHRE’s leadership position in the regulation andeducation of ART inspectors.To date, the short-term goals of the Task Force have allbeen reached. The medium-term goals - to develop aninspection curriculum with wide applicability at theEuropean level and to organise an ESHRE workshop forcompetent authorities - can be achieved through pursuingthe future tasks noted above. An excellent opportunity forthis should be the ESHRE Campus meeting to be organisedby the Task Force and SIG Safety and Quality in ART inDublin in September this year.Edgar MocanuEUTCD TF Co-ordinatorFocus on Reproduction January 2012 25
TASK FORCES// DEVELOPING COUNTRIES AND INFERTILITY //An expert workshop on the socio-cultural and ethicalaspects of infertility care in poor-resource countriesIn November the Social Science Study Group of the SpecialTask Force held an expert workshop in co-operation withthe Walking Egg Foundation, the University of Amsterdam,Amsterdam Institute for Social Science Research and theWHO. During the two-day meeting, which took place inGenk, specialists from different parts of the worldreviewed the various socio-cultural and ethical aspects ofbiomedical infertility care in poor resource areas. Theseincluded:• Socio-cultural, political and economic barriers to access• Counselling, patient-staff interaction, privacy and otheraspects of care• Ethical concerns at policy and clinical level• Infertility care in times of HIV/AIDSSheryl Vanderpoel from the WHO explained how accessto infertility care would not only help countries reachMillennium Development Goal 5b (‘universal access toreproductive health care’) but would also contribute toMDG 3 (‘gender equality’), MDG 4 (‘neonatal health’),MDG 5 (‘maternal health’), MDG 6 (‘HIV/AIDs’) andMDG 8 (‘new technologies’). Guido Pennings summarisedthe ethical arguments pro and contra infertility treatmentin developing countries.The first session was dedicated to sub-Saharan Africa,and S Dyer and M Patel examined how current out-ofpocketfunding for ART deepens household poverty inSouth Africa. V Horbst and E Mariano explored howpatients in Mali, Togo and Southern Mozambique copewith the barriers to infertility care. And finally, ClausJanisch talked about his own experiences and challenges inoutput-based financing for maternal care in Kenya. The useof vouchers, which are strictly speaking conditional cashtransfers with defined benefits, could be a promisingpayment model for infertility services in poor countries.In the following session D Khalifa (Sudan), H Sallam(Egypt) and S Tremayne (Iran) reviewed socio-cultural,policy and ethical aspects of infertility care in the contextof the Eastern Mediterranean region, defined somewhat byIslamic laws and culture.The next day we turned our attention to the Asianregion. P Nahar concluded after interviewing policymakers,NGOs and donors in Bangladesh that infertility is excludedfrom the public health discourse because of its emphasis onthe epidemiological index, ie, morbidity and mortalityrates. M Pashigian examined the growth of biomedicalservices in Vietnam and the issue of illegal trade intransnational surrogates in Asia.In the next session, we travelled to Bulgaria w<strong>here</strong>,according to Y Panyotova, resource distribution givespriority to expensive treatment for only a minority. Asimilar situation was found by M Makuch in the publichealth sector of Brazil, w<strong>here</strong> the IVF centres do notprovide a service for the most under privileged. Finally, in atalk on cross-border reproductive care, Z Gurtin stressedthe importance of keeping an eye on the broader context oftransnational flows and raised questions on how theprovision of ART in low-resource countries could interact.The final session focused on infertility care in sub-Saharan Africa in times of HIV/AIDs. N Dhont and ABachow explored challenges in the double burden of HIVand infertility for the provision ofinfertility care in developing countries.The final round-table discussionrecognised the multiplicity of barriersto infertility care access and w<strong>here</strong>further research is needed. The nextstep for the group will be thefinalisation of a protocol for theassessment of newly introducedaccessible infertility care in poorresource countries from a socioculturalpoint of view.The Task Force’s workshop on socio-cultural and ethical aspects of biomedical infertilitycare was attended by 27 experts.Nathalie DhontWillem Ombelet, Co-ordinatorTF Developing countries and infertility26 Focus on Reproduction January 2012
COVER STORYThe urgent needfor new spermbiomarkersConventional semen analysis remains the gold standardfor the initial investigation of male infertility. However,semen analysis is today considered of only limited valuein predicting a couple’s chance of pregnancy with ART.Certainly, the uptake and success of ICSI have reduced thesignificance and perceived need for sperm quality tests; ICSIrequires only one sperm - even if morphologically abnormal andimmotile - for the procedure to be around 25% successful inmost European clinics. ICSI is now our most widely used meansof fertilisation in ART, but can we be satisfied with this modestlevel of success? Will a better test than semen analysis improveour results?Sperm DNA quality as a diagnostic testAs a diagnostic tool, sperm DNA damage has been shown to bemore reproducible than conventional semen parameters andmore predictive at numerous fertility check-points. 1 Forexample, men with sperm DNA fragmentation above adiagnostic threshold of 25% using the Comet assay or 30%using the Sperm Chromatin Structure assay (SCSA) have a highrisk of infertility. 2,3 So sperm DNA damage appears to exhibitbetter credentials as a novel biomarker for male infertility than asemen analysis.Semen analysis is of limitedvalue but remains the goldstandard of initial testing formale fertility. Will betterassays improve the outcomeof ICSI and IVF, asksandrologist Sheena Lewis.Sperm DNA quality as a prognostic test for ART outcomeSperm DNA damage is associated with longer times topregnancy than in fertile couples, with impaired embryocleavage and reduced implantation after IVF, and most closelywith increased risk of pregnancy loss after both IVF and ICSI.However, the lasting implications of sperm DNA damage maybe of even greater significance. As sperm have few repairmechanisms and oocytes can only repair a limited amount ofsperm DNA damage, such damage may remain in the germ linefor generations. Nature does not prevent a sperm with oxidativeDNA damage from reaching the oocyte, achieving fertilisationand thus contributing to mutations during embryonicdevelopment or even causing loss of the fetus. Damaged spermDNA may be incorporated into the embryonic genome, thusleading to errors in DNA replication, transcription andtranslation during embryogenesis, and t<strong>here</strong>by contributing to arange of human diseases in subsequent future generations. 4 Inparticular, sperm DNA may have an impact on both the shortand long-term health of children born by ART, with someFocus on Reproduction January 2012 27
studies (though not all) showing that children conceived byICSI have a higher incidence of disease than childrenspontaneously conceived. 5 Continuing into childhood, t<strong>here</strong>are associations between poor sperm DNA integrity and arange of diseases, from childhood cancers to autism.Currently available tests for sperm DNA damageFor a sperm DNA test to be clinically useful it must havestrong predictive capacity for pregnancy with little overlapbetween fertile and infertile samples. The tests most oftenused today are the Comet assay, SCSA, the terminaltransferase dUTP nick end labelling (TUNEL) assay, andthe Sperm Chromatin Dispersion (SCD or Halo) test.• The Comet assayThe Comet assay isa single cell gelelectrophoretic testwhich quantifiesbroken strands ofDNA in individualsperm cells. As themass of DNAfragments streamout from the headof unbroken DNA,they resemble a‘comet’ tail, hencethe name of theassay. One majoradvantage of thisassay is that it usesonly 5000 sperm, so is suitable for the assessment of smallsamples left over from clinical use, or for samples w<strong>here</strong>only a few sperm are available. The Comet assay canmeasure both single and double strand breaks, and, with anadditional step, even altered bases. This is useful, becausewe don’t yet know which types of DNA damage are mostdeleterious to male fertility. The Comet is sensitive,repeatable and capable of detecting both high and lowlevels of damage in sperm. 6 Since 2010, clinical thresholdsfor the diagnosis of male infertility and the prediction ofIVF outcome have been established.• The Sperm Chromatin Structure assayThe SCSA is afluorescence cell sortertest which measuresthe susceptibility ofsperm DNA todenaturation afterexposure to heat oracid conditions. Onebenefit of the SCSA isits ability to rapidlymeasure largenumbers of cells byflow cytometry. This gives it robust statistical power, butdoes make it unsuitable for samples with low counts. Inaddition, it measures only single strand fragments, and hasdemonstrated associations between native, not DGC,sperm and ART outcomes. However, the SCSA has beentested over many years and its founder, Don Evenson, hasalways wisely insisted on a standardised protocol for allusers. This has reduced inter-laboratory variation andallowed comparison of studies from different groups. 7• The Sperm Chromatin Dispersion (Halo) testThe Halo test is asimple andinexpensive assay,available to fertilitylabs in kit form.Unlike all the othertests, it measures theabsence of damagerather than thedamaged DNA insperm. The test isconvenient in that itdoes not rely oneither colour orfluorescence intensity, and is simple to analyse in a routinelaboratory with light microscopy. One limitation of theassay is that its low-density nucleoids are relatively faint,with less contrasting images. To date, correlations havebeen observed between DNA and other sperm parameters,although few correlations between sperm DNA damageand ART outcomes have been established with the Halotest, even in large (n = 600) studies. 8 Meseguer et al in2009 reported that sperm DNA damage as measured byHalo had a negative impact on pregnancy. 9• The TUNEL assayThe TUNEL assaydetects ‘nicks’ (freeends of DNA) byincorporatingfluorescentlystained nucleotides.This allows thedetection of singleand doublestranded damage.The cells can beassesed eithermicroscopically or by flow cytometric (FCM) analysis.This gives the assay the flexibility to be used for smallnumbers with microscopic analysis and in smalllaboratories without dedicated and expensive FCMfacilities. However, the TUNEL asssay can also be analysedby FCM, giving it the advantage of robust numbers withreduced time and labour. A disadvantage of the assay is itsmany protocols, which makes comparison between28 Focus on Reproduction January 2012
laboratories almost impossible and explains its manyclinical thresholds. Recently, Aitken’s group has improvedthe TUNEL assay by including a preliminary step of DDTto relax the whole chromatin structure and allow access toall ‘nicks’. They have also added a viability stain so thatDNA damage is measured only in live sperm. This haseliminated a previous inaccuracy of measuring damage(often at high levels) in dead cells. 10 Robust clinicalthresholds have yet to be established.Novel tests for oxidised basesOxidative stress has long been implicated as the majoretiological factor in sperm DNA damage. Thus, a lowphysiological level of reactive oxygen species (ROS) isconsidered necessary to maintain normal sperm function,but ROS levels above physiological norms may causedeteriorating function or reduced survival. As a result, themeasurement of oxidised bases combined withfragmentation assays may indicate the potential as well asthe actual DNA damage - and t<strong>here</strong>by enhance theprognostic value of our current tests. To this end, thedetermination of 7, 8-dihydro-8-oxo-2’-deoxoguanosine(8OhdG) has been used as a marker of oxidative DNAbases damaged by oxidation and has been shown to be auseful adjunct to sperm DNA strand breaks, especially inmen with chronic disease (eg, diabetes mellitus).Sperm DNA in the clinical settingTwo systematic reviews from the USA in 2009 (whichincluded only TUNEL and SCSA but not the Comet orHalo assays) have reported that the impact of sperm DNAdamage on ART outcomes decreases from IUI to IVF and isleast evident in ICSI. 11 T<strong>here</strong> are currently few datarelating sperm DNA damage to late fetal development orpostnatal health in humans. However, although poor spermDNA does not appear to impair early fertility outcomesfollowing ICSI, it does seem to have an impact at a laterstage, and associations between poor sperm DNA and earlypregnancy loss following ICSI (and IVF) are now beginningto emerge. 12In the light of such results, the question I find mostdifficult to answer is not whether sperm DNA damageimpairs the outcome of IUI and IVF, but rather, why spermDNA damage does not seem to affect the early stages ofICSI. At first glance, this appears to support the belief -although counterintuitive - that ICSI appears to bypassgenetic as well as functional defects.My response to the question is speculative but I havefour suggestions:* Up to 30% of women having ICSI have no detectableproblems. They are often fertile and their oocytes may havemore capacity to repair DNA damage, even if the injectedsperm cell is of poor quality. This is supported by t<strong>here</strong>cent findings of Meseguer et al who showed that highquality oocytes from donors could offset the negativeimpact of sperm DNA damage on pregnancy. 13* In ICSI the gametes are not exposed to prolonged culture,so the sperm may incur less damage than those culturedovernight, as happens in IVF procedures. The recent studyfrom Dumoulin et al shows that even the birthweight ofIVF babies can be markedly influenced by minordifferences in culture conditions over that very short butinfluential time of early embryo development. 14 Incontrast, ICSI sperm are injected into the optimalenvironment of the oolemma within a few hours ofejaculation. This may protect them from laboratoryinduceddamage.* Evidence is emerging that embryos with high spermDNA damage are associated with early pregnancy loss, soICSI success rates may indeed be sometimes affectedadversely, but at a later stage. 12* Since we choose only one sperm for ICSI - and thatchoice is arbitrary except that the sperm is usually motile -we cannot assess a cohort of similar sperm. It may be thatthe sperm we favour is unlike the rest in its characteristics.But given that our ICSI success rates are still relativelymodest, our choice appears to be still ‘hit or miss’.However, on the broader question of the clinicalusefulness of sperm DNA tests, I do believe that ourexpectations tend to be excessive. How can we expect thissingle parameter (from only one of the two gametes) toprovide an absolute criterion for fertility or infertility? Asuccessful ART outcome will depend on many other traitsof sperm quality and function, as well as the influences ofthe oocyte, uterine receptivity and maternal immunesystem competence.Limitations of sperm DNA testingThe major limitation of testing for sperm DNA damage isthat the assay renders the tested sperm unsuitable forclinical purpose. In an effort to overcome this problem, anumber of non-invasive tests have been developed andtheir correlation with DNA damage assessed. If these testscan help embryologists choose sperm with low DNAdamage for ART, a major step forward in sperm selectionwill have been achieved - but so far this is not the case.• BirefringenceOne novel tool for sperm selection has been developedusing birefringence, or double refraction. This is t<strong>here</strong>fraction of a ray of light into two rays, which travel atdifferent speeds when passing through certain anisotropicmaterials. Sperm have natural anisotropy, so birefringenceprovides a non-invasive and rapid method of selectingsperm with particular properties.Gianaroli’s group in Bologna has reported a higherproportion of sperm with birefringence innormozoospermic samples, and associations betweenbirefringence and acrosome reacted sperm. 15,16 Furtherassociations have been found between sperm displayinglow DNA damage measured by the TUNEL assay andtotal although not partial birefringence. Clinical andongoing pregnancies were also higher in sperm selected forICSI by birefringence. 15Focus on Reproduction January 2012 29
• Intracytoplasmic morphologically selected sperm injectionA method of selecting sperm for ICSI by real-time highmagnification - usng a technique originally called ‘motilesperm organelle morphology examination’ (MSOME) - hasbeen developed by Bartoov’s group in Israel and is nowmore widely known as intracytoplasmic morphologicallyselected sperm injection, or IMSI. 17 With enhanced digitalimaging, magnification can be increased to x6000 such thatthe morphology of six sub-cellular organelles - nucleus,acrosome, post-acrosomal lamina, neck, mitochondria andtail - can be assessed. In trials, implantation rates andpregnancies were higher and miscarriage rates lower withIMSI-selected sperm than with controls. 18 Investigatorshave again suggested that a single morphologicalabnormality may indicate an anomaly in nuclear DNA,though the evidence for this is circumstantial and numbersare small. ICSI based on MSOME is a very time-consumingprocess (taking up to five hours) and further studies areneeded to assure us that this does not compromise the DNAof the sperm destined for clinical use.• Hyaluronic acid-selected sperm for ICSIHyaluronic acid (HA) is present in the extracellular matrixof the cumulus oophorus of the oocyte, and in vivo maturephysiologically competent sperm bind to HA receptors priorto fertilisation. The HA assay uses media supplementedwith HA to select sperm that bind to HA for ICSI. Acorrelation between HA-selected sperm and sperm withlower levels of DNA fragmentation (using the spermchromatin dispersion test, Halo) has also been observed intwo studies. Comparisons of ICSI outcomes with HAselectedsperm and standard PVP-ICSI sperm have shownthat the former are associated with better embryo quality,higher implantation rates, increased pregnancy rates andreduced miscarriage rates.In summary, the growing interest in novel biomarkers formale infertility is a very exciting and rapidly moving area ofresearch in reproduction. A mass of new data indicates theusefulness of many of these new tests (particularly spermDNA testing), both in a more acccurate diagnosis of maleinfertility and in the prediction of ART outcomes.Alas, although some of these novel biomarkers(particularly sperm DNA testing) have increasingly robustdata to support them, t<strong>here</strong> is still a reluctance toincorporate them into routine clinical care. Whilst thisinertia continues and our traditional tests prevail, it seemsunlikely that success rates in male infertility will improve.With the wider introduction of the new tests, patients willbe better informed and clinics have additional informationon which to base their choice of treatment.Sheena E M Lewis is Professor of Reproductive Medicine, QueensUniversity Belfast, UK, and Co-ordinator of ESHRE's SIGAndrology. She is also a founding Director of Lewis Fertility TestingLtd, a spin-off development company of her university (www.www.lewisfertilitytesting.com).References1. Simon L, Brunborg G, Stevenson M, et al. Clinical significanceof sperm DNA damage in assisted reproductive outcome. HumReprod 2010; 25: 1594-1608.2. Simon L, Lutton D, McManus J, Lewis SE. Sperm DNAdamage measured by the alkaline Comet assay as anindependent predictor of male infertility and IVF success. FertilSteril 2010; 95: 652-657.3. Evenson DP, Jost LK, Marshall D, et al. Utility of the spermchromatin structure assay as a diagnostic and prognostic tool inthe human fertility clinic. Hum Reprod 1999; 14: 1039–1049.4. Aitken RJ, de Iuliis GN, McLachlan RI. Biological and clinicalsignificance of DNA damage in the male germ line. Int J Androl2009; 32: 46–56.5. Katari S, Turan N, Bibikova M, et al. DNA methylation andgene expression differences in children conceived in vitro or invivo. Human Molecular Genetics 2009; 18: 3769-3778.6. Aitken R, de Iuliis GN. Origins and consequences of DNAdamage in male germ cells. Reprod BioMed Online 2007; 14:727-733.7. Bungum M, Humaidan P, Spano M, et al. The predictive valueof sperm chromatin structure assay (SCSA) parameters for theoutcome of intrauterine insemination, IVF and ICSI. Hum Reprod2004; 19: 1401-1408.8. Nasr-Esfahani MH, Razavi S, Vahdati AA, et al. Evaluation ofsperm selection procedure based on hyaluronic acid bindingability on ICSI outcome. J Assist Reprod Genet 2008; 25: 197-203.9. Meseguer M, Santiso R, Garrido N, et al. Sperm DNAfragmentation levels in testicular sperm samples from azoospermicmales as assessed by the sperm chromatin dispersion (SCD) test.Fertil Steril 2009; 92: 1638-45.10. Mitchell LA, De Iuliis GN, Aitken RJ. The TUNEL assayconsistently underestimates DNA damage in human spermatozoaand is influenced by DNA compaction and cell vitality. Int JAndrol 2011; 34: 2-13.11. Zini A, Sigman M. Are tests of sperm DNA damage clinicallyuseful? Pros and cons. J Androl 2009; 30: 219-229.12. Zini A, Boman JM, Belzile E, Ciampi A. Sperm DNA damageis associated with an increased risk of pregnancy loss after IVFand ICSI: systematic review and meta-analysis. Hum Reprod2008; 23: 2663–2668.13. Meseguer M, Santiso R, Garrido N, et al. Effect of spermDNA fragmentation on pregnancy outcome depends on oocytequality. Fertil Steril 2011; 95: 124-128.14. Dumoulin JC, Land JA, Van Montfoort AP, et al. Effect of invitro culture of human embryos on birthweight of newborns.Hum Reprod 2010; 25: 605-12.15. Gianaroli L, Magli MC, Collodel G, et al. Sperm head'sbirefringence: a new criterion for sperm selection. Fertil Steril2008; 90: 104-112.16. Gianaroli L, Magli MC, Ferraretti AP, et al. Birefringencecharacteristics in sperm heads allow for the selection of reactedspermatozoa for intracytoplasmic sperm injection. Fertil Steril2010; 93: 807-813.17. Bartoov B, Berkovitz A, Eltes F, et al. Pregnancy rates arehigher with intracytoplasmic morphologically selected sperminjection than with conventional intracytoplasmic injection. FertilSteril 2003; 80: 1413-1419.18. Antinori M, Licata E, Dani G, et al. Intracytoplasmicmorphologically selected sperm injection: a prospectiverandomized trial. Reprod Biomed Online 2008; 16: 835-841.30 Focus on Reproduction January 2012
GETTY IMAGESFEATUREAntiretroviral therapy haschanged the outlook for mostHIV-infected couples indeveloped countries such thatconception is now a realisticoption. Augusto Semprini andSimona Fiore on behalf of theCREAThE network and ESHRE’sTask Force on Fertility and ViralDiseases review the risks oftransmission and the mostappropriate fertility techniques.Conceptionin HIV-infectedcouplesT<strong>here</strong> are no clinical guidelines for the care of fertilityin those infected with HIV, and the question of howbest to promote conception in HIV-infected coupleson highly active antiretroviral therapy is still opento discussion. Moreover, although many fertility clinics inEurope do screen patients for HIV infection, only a few areprepared to treat them if one or the other partner ispositively diagnosed - because of perceived ethical dilemmasor other concerns.Assisting couples to conceive does not solely require aconsideration of the welfare of any child born as a result oftreatment. Additional concerns are the life expectancy of anFocus on Reproduction January 2012 31
When only the female is HIV+ve:the issues for consideration• Protection for the man against sexuallytransmitted infection, and to the infant fromvertical transmission• Antiretrovirals during pregnancy• Measures to reduce the risk of verticaltransmission• Frequency of unprotected intercourse• Self-insemination in the ovulation windowshould be explained• Re-evaluate after six months of unsuccessfulattemptsinfected parent and the risk of viral transmission to boththe uninfected partner or offspring.However, despite such concerns, the fact is that indeveloped countries HIV infection has now become achronic but manageable disease; highly active antiretroviraltherapy (HAART) has substantially increased lifeexpectancy and quality of life for both children and adultsinfected with HIV. 1 Thus, in the context of mother-to-childtransmission (MTCT), a combination of prophylacticantiretroviral therapy during pregnancy and labour, deliveryby elective Caesarean section and avoidance of breastfeedingcan reduce the risk of MTCT to less than 2%. 2 Thebalance in fertility treatment decisions in HIV infection hasthus shifted considerably, such that treatment has nowbecome both feasible and appropriate.Reproductive counselling for HIV-infected couplesReproductive assistance to HIV discordant couples can havea significant impact on the prevention of viral, sexual andMTC transmission. Most HIV-infected people are youngand fertile, and both men and women are willing to have achild at sometime in their lives. 3 The marked increase in lifeexpectancy as a result of antiretroviral therapy has removedmost of the ethical difficulties in helping people with HIVbecome parents, and specific information and assistance cannow be offered to protect the uninfected partner or childfrom infection.4,5,6When only the woman is infected, self-insemination withthe partner’s semen completely eliminates the risk of sexualinfection. Semen analysis to evaluate semen quality and torule out genital infection might be indicated, and completeinfertility screening should be provided if pregnancy doesnot occur within six months - preliminary observationsindicate that HIV-positive women might have an added riskof subfertility. 7When only the man is HIV-positive, the possibility ofspontaneous conception carries a risk of sexuallytransmitted HIV to the uninfected female through infectedsemen. This risk is difficult to quantify, but might besignificantly higher than a theoretical 1/1000 risk per singleact of penetrative intercourse; a small trial on naturalconception reported four cases of seroconversion in the 94healthy women enrolled and advised to have unprotectedintercourse at the time of ovulation with their HIV-positivepartners. 8Different reports have discussed the ‘efficiency’ of sexualtransmission from male to female and a mathematicalmodel has been proposed. 9,10,11 Wilson et al put thecumulative annual risk of female-to-male HIV transmissionat 0.0022 and male-to-female at 0.0043 with an average of100 acts of sexual intercourse per year. 12 A recent review of11 cohorts reporting on 5021 heterosexual couples and 461HIV transmissions found no transmission in patientstreated with antiretrovirals and with a viral load below 400copies/ml. 13The very low risk of HIV transmission to the negativepartner and to the baby if HIV-positive individuals haveundetectable viraemia with HAART now lies behind anincreasing interest in natural conception. 14 Naturalconception has also been chosen by some couples followingassisted reproduction programmes. Indeed, in one Italianstudy up to one-third of couples did not start theirinsemination procedures and a further third withdrew fromthe programme after a number of failed attempts; half ofthese couples tried natural conception with unprotected sexand without medical control. 15Although some expert advice has claimed that the risk ofsexual transmission is negligible when the HIV-infectedpartner is receiving antiretroviral therapy (with excellentad<strong>here</strong>nce, undetectable viral load and no STDs), 16 themathematical model noted above would suggest thatabandoning condom use could quadruple the number ofcontaminations and t<strong>here</strong>by have a significant effect interms of public health. The general perception of HIVtransmission by sexual intercourse is extremely low in thispopulation, and protected sexual intercourse remains themost important means of prevention.Anecdotal reports also suggest that periconceptional preexposureprophylaxis with oral antiretroviral therapy isalready in limited use; if effective in reducing heterosexualHIV transmission, this too might be an option fordiscordant couples wanting to conceive spontaneously. 17Long-term treatment with antiretrovirals can reduce viralAUGUSTO SEMPRINI:‘COUPLES IN WHOM ONEOR BOTH PARTNERSARE HIV INFECTEDSHOULD HAVE ACCESSTO THE SAME FERTILITYADVICE AND TREATMENTAS NON-INFECTEDCOUPLES.’32 Focus on Reproduction January 2012
eplication in blood and semen, butsome infected men maintain substantialviral concentrations in their semen, evenin the presence of undetectable bloodplasma viral load with antiretroviraltreatment. 18 Certain studies have shownthat HIV-RNA may be amplified insemen when undetectable in plasma in2–8% of patients on HAART,suggesting that the genital tract mayrepresent a separate reservoir for viralreplication. 19,20 Genital tract infectionsaccount for a significant number ofepisodes of HIV genital shedding andtheir eradication is followed by areduction in the HIV concentration ingenital fluids. 21Screening for genital tract infection,for semen and ovulatory quality and fortubal patency should be performedbefore treatment to select the mostappropriate reproductive technologyand to minimise the number oftreatment cycles. Some observationshave suggested an increased prevalenceof infertility factors in couples with HIV, which canprolong the time (and number of attempts) to achievefertilisation; this may increase the risk of sexualtransmission, or make conception impossible, as in the caseof severe dyspermia or tubal disease. In the latter cases,such couples are exposed to a risk of infection without thechance of conception.Reproductive techniques in HIV-infected couplesSpermatozoa tested for the absence of HIV contaminationcan be used for fertilisation by IUI or IVF/ICSI in HIVdiscordantcouples with male infection. The technology,used in conjunction with semen washing, should minimisepotential damage to the healthy female while providing agood fertility rate.Semen washing was developed more than 15 years agoand consists of a three-step method to remove infectedseminal leukocytes and wash the spermatozoa free ofseminal plasma. 22 Other pioneering centres in Europe havestarted their own sperm washing programmes, which hasnow culminated in a European network of units providingassisted conception to HIV-discordant couples. These andother centres are now linked in CREAThE, a network ofclinics covering Italy, Spain, UK, Germany, Russia,Switzerland, France, Belgium and Israel to optimisetreatment and monitor outcomes.A systematic review of 658 abstracts (of which only 41were selected for analysis) and 17 full articles has just beenpublished. 23 The review included 3900 IUI cycles in 1184couples in 11 studies, and 738 ICSI/IVF cycles in 579couples across ten studies. The IUI and ICSI results were,respectively: pregnancy rates per cycle 18% and 38.1%;The risk of viral transmission from an HIV +ve male to his uninfected partner and futurechild can be virtually removed by ART with washed sperm. Sperm washing is based onthe observation that the HIV virus cannot attach itself to spermatozoa, but can be foundin the fluid and cells surrounding spermatozoa. Sperm washing allows the separation oflive sperm from the surrounding fluid and cells in a three-step process: 1, a spermatozoamigration on density gradient; 2, repeated washing of the migrated pellet; and 3, aspermatozoa swim up.cumulative pregnancy 50% and 52.9%; and abortion rate15.6% and 20.6%. No seroconversions in women ornewborns were detectable at birth or after 3-6 months.HIV-infected women have additional special needs insexual and reproductive health, including information andservices to protect their own health as well as to reduce therisk of mother-to-child HIV transmission. The number ofspecialists ready to offer these services to HIV-positivewomen with fertility problems has been increasing since1993. 24 And today t<strong>here</strong> is a general willingness to treatHIV-infected women with ART, given the low risk of HIVvertical transmission.A reduced pregnancy rate after IVF has been observed inHIV-infected women when the patient’s own oocytes wereused. However, no significant reduction in pregnancy ratewas found when donated oocytes were used. It has beensuggested that subclinical hypogonadism mediated byimmunosuppression may explain these observations. It isalways important to optimise the woman’s HIVimmunological status before considering ART. The mostrecent studies report clinical pregnancy rates per cyclevarying from 11-21% in HIV-1-infected women after IVFor ICSI, compared with 26% in matched controls. Thepaucity of data reported on IVF and ICSI cycles in HIV-1-infected women do not allow any further conclusion. 25It is now well accepted that couples in whom one or bothpartners are HIV infected should have access to the samefertility advice and treatment as non-infected individuals toallow them to conceive, and to do so with the minimum ofrisk to their partners or children.Reproductive counselling to individuals with HIV mightFocus on Reproduction January 2012 33
motivate them to ask specifically for reproductivetreatment in order to limit the risk of infection touninfected partners. The offer of reproductive care to menwith HIV strengthens the message that protecting thefemale partner from infection makes possible a healthymother of an uninfected child.Reproductive options are available to HIV-infectedwomen who positively choose to become pregnant becausetheir own disease is well managed and interventions canminimise the risk of vertical transmission.Dr Augusto Enrico Semprini works in clinical research at theUniveristy of Milan, Italy; he is President of the Centres forREproductive Assistance Techniques in hiv in Europe (CREAThE),and Chairman of ESHRE’s Task Force on Fertility and ViralDiseases. Dr Simona Fiore is Scientific Coordinator of CREAthE.References1. Gallant JE. Strategies for long term success in the treatment ofHIV infection. JAMA 2000; 283: 1329–1334.2. U.S. Department of Health and Human Services. Public healthservice task force recommendations for use of antiretroviral drugsin pregnant HIV-1-infected women for maternal health andinterventions to reduceperinatal HIV-1 transmission in the UnitedStates. 2006. www.aidsinfo.nih.gov/Guidelines.3. Klein J, Pena JE, Thornton MH, Sauer MV. Understanding themotivations, concerns, and desires of human immunodeficiencyvirus1-serodiscordant couples wishing to have children throughassisted reproduction. Obstet Gynecol 2003; 101: 987-994.4. Mocroft A, Ledergerber B, Katlama C, et al. EuroSIDA studygroup. Decline in the AIDS and death rates in the EuroSIDA study:an observational study. Lancet 2003; 362: 22-29.5. Heard I, Sitta R, Lert F. Reproductive choice in men and womenliving with HIV:evidence from a large representative sample ofoutpatients attending Frenchh hospitals. AIDS 2007; 21 (Suppl 1):77–82.6. Gilling-Smith C, Smith JR, Semprini AE. HIV and infertility:time to treat. T<strong>here</strong>’s no justification for denying treatment toparents who are HIV positive. BMJ 2001; 322: 566-567.7. Coll O, Suy A, Hernandez S, et al. Prenatal diagnosis in humanimmunodeficiency virus-infected women: a new screeningprogram for chromosomal anomalies. Am J Obstet Gynecol 2006:194: 192–198.8. Mandelbrot L, Heard I, Henrion-Geant E, Henrion R. Naturalconception in HIV-negative women with HIV-infected partners.Lancet 1997; 349: 850-851.9. De Vincenzi I. A longitudinal study of humanimmunodeficiency virus transmission by heterosexual partners.European Study Group on Heterosexual Transmission of HIV. NEngl J Med 1994; 331: 341–346.10. Quinn TC, Wawer MJ, Sewankambo N, et al. Viral load andheterosexual transmission of human immunodeficiency virus type1. Rakai Project Study Group. N Engl J Med 2000; 342: 921-929.11. Baeten JM, Overbaugh J. Measuring the infectiousness ofpersons with HIV-1: opportunities for preventing sexual HIV-1transmission. Curr HIV Res 2003; 1: 69-86.12. Wilson DP, Law MG, Grulich AE, et al. Relation between HIVviral load and infectiousness: a model-based analysis. Lancet2008; 372: 314-320.13. Attia S, Egger M, Müller M, et al. Sexual transmission of HIVaccording to viral load and antiretroviral therapy: systematicreview and meta-analysis. AIDS 2009; 23: 1397-1404.14. Barreiro P, Castilla JA, Labarga P, Soriano V. Is naturalconception a valid option for HIV-serodiscordant couples? HumReprod 2007; 22: 2353-2358.15. Vernazza PL, Hollander L, Semprini AE, et al. HIV-discordantcouples and parenthood: how are we dealing with the risk oftransmission? AIDS 2006; 20: 635-636.16. Vernazza P, Hirschel B, Bernasconi E, Flepp M. HIVtransmission under highly active antiretroviral therapy. Lancet2008; 372: 1806-1807.17. Lampe MA, Smith DK, Anderson GJ, et al. Achieving safeconception in HIV discordant couples: the potential role of oralpreexposure prophylaxis in the United States. Am J ObstetGynecol 2011; 204: 488.e1-8.18. Vernazza PL, Troiani L, Flepp MJ, etal. Potent antiretroviraltreatment of HIV-infection results in suppression of the seminalshedding of HIV. The Swiss HIV Cohort Study. AIDS 2000; 14:117-121.19. Bujan L, Daudin M, Alvarez M, et al. Intermittent HIV type-1shedding in semen and efficiency of sperm processing despite highseminal HIV-RNA levels. Fertil Steril 2002; 78: 1321–1323.20. Nunnari G, Otero M, Dornadula G, et al. Residual HIV-1disease in seminal cells of HIV-1 infected men on suppressiveHAART: latency without on-going cellular infections. AIDS 2002;16: 39–45.21. Rotchford K, Strum A, Wilkinson D. Effect of coinfectionwith STDs and of STD treatment on HIV shedding in genital tractsecretions: systematic review and data synthesis. Sex Transm Dis2000; 27:243–248.22. Semprini AE, Levi-Setti PE, Bozzo M, et al. Insemination ofHIV-negative women with processed semen of HIV-positivepartners. Lancet 1992; 340: 1317-1319.23. Vitorino RL. Grizstejn BG. De Andreade CA, et al. Systematicreview of the safety of assisted reproduction tecniques in couplesserodiscordant for HIV virus w<strong>here</strong> the man is positive. FertilSteril 2011; 95: 1684-1690.24. Englert Y, Van Vooren JP, Liesnard C, et al. Medically assistedreproduction and the desire for a child by HIV infected couples:has the time for a change in attitude come? Gynecol Obstet Fertil2001; 29: 339-348.25. Van der leuwen, JM Prins, S Jurrians, et al. Reproduction andfertility in human immunodeficiency virus type 1 infection.Human Reprod Update 2007; 13: 197-206.34 Focus on Reproduction January 2012
The European Society of Human Reproduction and EmbryologyMeerstraat 60Grimbergen, Belgiuminfo@<strong>eshre</strong>.euwww.<strong>eshre</strong>.eu