Coverage Decisions, Appeals and Complaints - Aetna Medicare
Coverage Decisions, Appeals and Complaints - Aetna Medicare
Coverage Decisions, Appeals and Complaints - Aetna Medicare
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
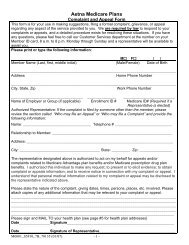
the forms on our website at:http://www.aetnamedicare.com/help_<strong>and</strong>_resources/downloadable_forms.jsp?tab=4 or bycontacting Member Services at the toll free number on your ID card for copies. Writtencomplaints should be mailed to the address indicated below or you may fax them to thefollowing toll-free fax number:<strong>Aetna</strong> <strong>Medicare</strong> Grievance <strong>and</strong> <strong>Appeals</strong> UnitP.O. Box 14067Lexington, KY 40512Fax Number all States: 1-866-604-7092<strong>Medicare</strong> Advantage <strong>Coverage</strong> DeterminationsYou have the right to request a coverage determination if you want us to provide or pay for anitem or service that you believe should be covered. We are making a coverage determinationfor you whenever we decide what is covered for you <strong>and</strong> how much we pay. In some cases wemight decide a service is not covered or is no longer covered by <strong>Medicare</strong> for you. If youdisagree with this coverage determination, you can make an appeal.St<strong>and</strong>ard <strong>Coverage</strong> Determination ProcessIf you request a coverage determination for an item or service you believe should be covered<strong>and</strong> we process your request as a st<strong>and</strong>ard coverage determination, we must give you adetermination within 14 days of receiving your request. However, we can take up to 14 morecalendar days if you ask for more time, or if we need information (such as medical records)that may benefit you. If we decide to take extra days to make the determination, we will tell youin writing. If you believe we should not take extra days, you can file a “fast complaint” alsoknown as an expedited grievance about our determination to take extra days. When you file anexpedited grievance, we will give you an answer to your grievance within 24 hours.If we do not give you our answer within 14 days (or if there is an extended time period, by theend of that period), you have the right to appeal. If our answer is yes to part or all of what yourequested, we must authorize or provide the coverage we have agreed to provide within 14days after we received your request. If we extended the time needed to make ourdetermination, we will provide the coverage by the end of that extended period. If our answer isno to part or all of what you requested, we will send you a written statement that explains whywe said no <strong>and</strong> you will have the right to appeal.“Fast” <strong>Coverage</strong> Determination ProcessIf your health requires it we will give you a fast determination <strong>and</strong> will give you an answerwithin 72 hours of receipt of your request. However, we can take up to 14 more calendar daysif we find that some information that may benefit you is missing, or if you need time to getY0001_M_OT_WB_10925 CMS Approved 10/04/2011




![[PDF] Directory - Aetna Medicare](https://img.yumpu.com/50361210/1/190x247/pdf-directory-aetna-medicare.jpg?quality=85)