Coverage Decisions, Appeals and Complaints - Aetna Medicare
Coverage Decisions, Appeals and Complaints - Aetna Medicare
Coverage Decisions, Appeals and Complaints - Aetna Medicare
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
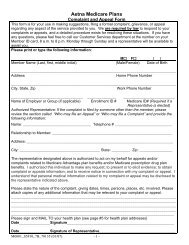
process could seriously jeopardize your life, health or ability to regain maximumfunction.3. <strong>Aetna</strong> will notify you <strong>and</strong>/or the physician of our determination as expeditiously as yourhealth condition requires but no later than 72 hours after receiving the request. We mayextend this timeframe by up to fourteen (14) calendar days if you request the extensionor if we need additional information <strong>and</strong> the extension of time benefits you.4. If you disagree with our determination to extend the time frame, you have the right torequest a “fast complaint”, also known as an expedited grievance. <strong>Aetna</strong>'s writtennotification will provide instructions <strong>and</strong> the timeframes associated with the expeditedgrievance process. When you file an expedited grievance, we will give you an answer toyour grievance within 24 hours.5. To request an expedited appeal, you may call 1-800-932-2159. You may fax, mail orh<strong>and</strong> deliver your written request to <strong>Aetna</strong>. If you write, the 72-hour review timeframewill not begin until your request is received.<strong>Aetna</strong> <strong>Medicare</strong> Grievance <strong>and</strong> <strong>Appeals</strong> UnitP.O. Box 14067Lexington, KY 40512Fax Number all states: 1-866-604-70926. If <strong>Aetna</strong> determines that your request is not time-sensitive, where your health is notseriously jeopardized, <strong>Aetna</strong> will notify you verbally <strong>and</strong> in writing <strong>and</strong> will automaticallybegin processing your request under the st<strong>and</strong>ard appeal process.7. If you disagree <strong>and</strong> believe the review should be expedited, you may file a “fastcomplaint”, also known as an expedited grievance, with <strong>Aetna</strong>. The written notice willinclude instructions on how to file an expedited grievance. When you file an expeditedgrievance, we will give you an answer to your grievance within 24 hours.8. We must give you our answer within 72 hours after we receive your appeal. We will giveyou our answer sooner if your health requires it. If we do not give you an answer within72 hours, we are required to send your request on to Level 2 of the appeals process,where it will be reviewed by an Independent Review Organization.If our answer is yes to part or all of what you requested, we must provide the coveragewe have agreed to provide within 72 hours after we receive your appeal.If our answer is no to part or all of what you requested, we will automatically forwardthe entire file to an Independent Review Organization designated by CMS for a new <strong>and</strong>impartial review.9. For cases submitted for review, the Independent Review Organization will make areconsidered determination within 72 hours <strong>and</strong> notify you in writing of the reasons forthe determination. If the Independent Review Organization upholds our determination,their notice will inform you of your right to a hearing before an Administrative Law Judgeas described in Step 7 under the st<strong>and</strong>ard appeals process.10. If the Independent Review Organization decides in your favor, we must authorize theY0001_M_OT_WB_10925 CMS Approved 10/04/2011




![[PDF] Directory - Aetna Medicare](https://img.yumpu.com/50361210/1/190x247/pdf-directory-aetna-medicare.jpg?quality=85)