No. Description Reference32 <strong>Physician</strong> assistants (PAs) practice medicine with physician supervision, which allows physicians to see more patients andconcentrate their efforts on the needs of those with complex medical conditions. <strong>Physician</strong> assistants have been practicing inMinnesota since 1970. They work in a variety of settings and specialties, although most are in primary care practices. This articleprofiles the PA profession and describes the type of work PAs do, the training and credentialing required to become a PA, and therelationship between physicians and PAs. The authors note that the role of the PA is highly individualized, depending on thephysician’s needs and preferences, the type of practice, the setting, and the PA’s training and experience. In some practices, thePA’s role will closely resemble that of the physician’s. For example, PAs will often serve as the primary care provider for some of thepatients in a panel. In a primary care setting, these will be patients who need routine health maintenance or well-child care, as well asthose with acute complaints. The PA also may help patients manage chronic health conditions such as hypertension, diabetes,dyslipidemia, asthma, obesity, and depression. Having PAs care for patients with these conditions allows the physician to devotemore time and attention to patients who have more complex conditions. In other settings, the PA may function at the periphery of thephysician’s work, implementing medical decisions, performing procedures, and instructing and educating patients and caregivers; onthe other hand, those with extensive training or experience may provide high-level consultations. In an inpatient, emergency room, orprocedural practice, the PA and physician may practice side-by-side and confer on an ongoing basis throughout the day. Supervisingphysicians assume all responsibility for the care given by the PA. Although the physician does not have to be present when the PAprovides care, he or she (or an alternate physician) must be available by phone or electronically. In most cases, the PA andphysicians work closely and have regular opportunities to discuss cases and practice standards. Clinical postgraduate specialtytraining for PAs is available in a variety of fields including dermatology, rheumatology, psychiatry, sleep medicine, emergencymedicine, occupational medicine, hospital medicine, critical care, general surgery, neurosurgery, orthopedic surgery, and urology.Advanced training or extended experience does not change the fact that a PA works under a supervising physician and that theclinical tasks delegated to the PA still must fall within the physician’s scope of practice.33 Objective. To assess applicability of national health survey data for generalizable research on outpatient care by physician assistants(PAs) and nurse practitioners (NPs). Data Sources. Methodology descriptions and 2003 data files from the National AmbulatoryMedical Care Survey, the National Hospital Ambulatory Medical Care Survey, the Medical Expenditure Panel Survey, and theCommunity Tracking Study. Study Design. Surveys were assessed for utility for research on PA and NP patient care, with respect tosurvey coverage, structure, content, generalizability to the U.S. population, and validity. National estimates of patient encounters,statistically adjusted for survey design and nonresponse, were compared across surveys. Data Collection/Extraction Methods.Surveys were identified through literature review, selected according to inclusion criteria, and analyzed based on methodologydescriptions. Quantitative analyses used publicly available data downloaded from survey websites. Principal Findings. Surveys variedwith respect to applicability to PA and NP care. Features limiting applicability included (1) sampling schemes that inconsistentlycapture nonphysician practice, (2) inaccurate identification of provider type, and (3) data structure that does not support analysis ofteam practice. Because the majority of PAs work in group practices and because independent NP practices are not sampled, theNational Ambulatory Medical Care Survey [NAMCS] probably underestimates visits to NPs and PAs. Conclusions. Researchers usingnational health care surveys to analyze PA and NP patient interactions should account for design features that may differentiallyaffect nonphysician data. Workforce research that includes NPs and PAs is needed for national planning efforts, and this research willrequire improved survey methodologies.Kimball, B. A., Rothwell, W. S.(2008). <strong>Physician</strong> assistantpractice in Minnesota:Providing care as part of aphysician-directed team.Minnesota Medicine, 91(5), 45-48.Morgan, P. A., Strand, J.,Østbye, T., & Albanese, M. A.(2007). Missing in action: Careby physician assistants andnurse practitioners in nationalhealth surveys. <strong>Health</strong> ServicesResearch, 42(5), 2022-2037.Page 45 of 74
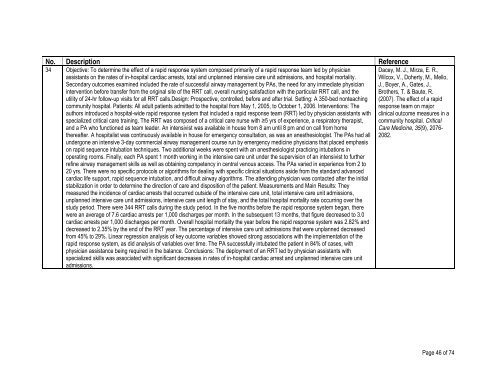
No. Description Reference34 Objective: To determine the effect of a rapid response system composed primarily of a rapid response team led by physicianassistants on the rates of in-hospital cardiac arrests, total and unplanned intensive care unit admissions, and hospital mortality.Secondary outcomes examined included the rate of successful airway management by PAs, the need for any immediate physicianintervention before transfer from the original site of the RRT call, overall nursing satisfaction with the particular RRT call, and theutility of 24-hr follow-up visits for all RRT calls.Design: Prospective, controlled, before and after trial. Setting: A 350-bed nonteachingcommunity hospital. Patients: All adult patients admitted to the hospital from May 1, 2005, to October 1, 2006. Interventions: Theauthors introduced a hospital-wide rapid response system that included a rapid response team (RRT) led by physician assistants withspecialized critical care training. The RRT was composed of a critical care nurse with ≥5 yrs of experience, a respiratory therapist,and a PA who functioned as team leader. An intensivist was available in house from 8 am until 8 pm and on call from homethereafter. A hospitalist was continuously available in house for emergency consultation, as was an anesthesiologist. The PAs had allundergone an intensive 3-day commercial airway management course run by emergency medicine physicians that placed emphasison rapid sequence intubation techniques. Two additional weeks were spent with an anesthesiologist practicing intubations inoperating rooms. Finally, each PA spent 1 month working in the intensive care unit under the supervision of an intensivist to furtherrefine airway management skills as well as obtaining competency in central venous access. The PAs varied in experience from 2 to20 yrs. There were no specific protocols or algorithms for dealing with specific clinical situations aside from the standard advancedcardiac life support, rapid sequence intubation, and difficult airway algorithms. The attending physician was contacted after the initialstabilization in order to determine the direction of care and disposition of the patient. Measurements and Main Results: Theymeasured the incidence of cardiac arrests that occurred outside of the intensive care unit, total intensive care unit admissions,unplanned intensive care unit admissions, intensive care unit length of stay, and the total hospital mortality rate occurring over thestudy period. There were 344 RRT calls during the study period. In the five months before the rapid response system began, therewere an average of 7.6 cardiac arrests per 1,000 discharges per month. In the subsequent 13 months, that figure decreased to 3.0cardiac arrests per 1,000 discharges per month. Overall hospital mortality the year before the rapid response system was 2.82% anddecreased to 2.35% by the end of the RRT year. The percentage of intensive care unit admissions that were unplanned decreasedfrom 45% to 29%. Linear regression analysis of key outcome variables showed strong associations with the implementation of therapid response system, as did analysis of variables over time. The PA successfully intubated the patient in 84% of cases, withphysician assistance being required in the balance. Conclusions: The deployment of an RRT led by physician assistants withspecialized skills was associated with significant decreases in rates of in-hospital cardiac arrest and unplanned intensive care unitadmissions.Dacey, M. J., Mirza, E. R.,Wilcox, V., Doherty, M., Mello,J., Boyer, A., Gates, J.,Brothers, T. & Baute, R.(2007). The effect of a rapidresponse team on majorclinical outcome measures in acommunity hospital. CriticalCare Medicine, 35(9), 2076-2082.Page 46 of 74