Physician Assistants: A Literature Review - Health Professions ...
Physician Assistants: A Literature Review - Health Professions ...
Physician Assistants: A Literature Review - Health Professions ...
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
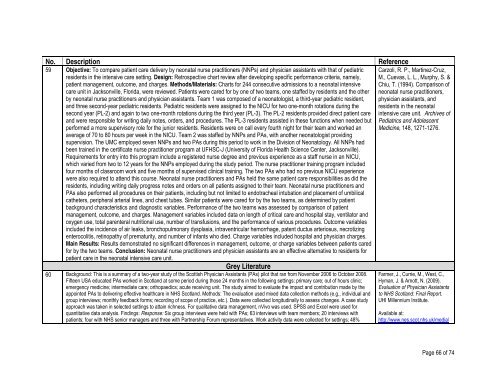
No. Description Reference59 Objective: To compare patient care delivery by neonatal nurse practitioners (NNPs) and physician assistants with that of pediatricresidents in the intensive care setting. Design: Retrospective chart review after developing specific performance criteria, namely,patient management, outcome, and charges. Methods/Materials: Charts for 244 consecutive admissions to a neonatal intensivecare unit in Jacksonville, Florida, were reviewed. Patients were cared for by one of two teams, one staffed by residents and the otherby neonatal nurse practitioners and physician assistants. Team 1 was composed of a neonatologist, a third-year pediatric resident,and three second-year pediatric residents. Pediatric residents were assigned to the NICU for two one-month rotations during thesecond year (PL-2) and again to two one-month rotations during the third year (PL-3). The PL-2 residents provided direct patient careand were responsible for writing daily notes, orders, and procedures. The PL-3 residents assisted in these functions when needed butperformed a more supervisory role for the junior residents. Residents were on call every fourth night for their team and worked anaverage of 70 to 80 hours per week in the NICU. Team 2 was staffed by NNPs and PAs, with another neonatologist providingsupervision. The UMC employed seven NNPs and two PAs during this period to work in the Division of Neonatology. All NNPs hadbeen trained in the certificate nurse practitioner program at UFHSC-J (University of Florida <strong>Health</strong> Science Center, Jacksonville).Requirements for entry into this program include a registered nurse degree and previous experience as a staff nurse in an NICU,which varied from two to 12 years for the NNPs employed during the study period. The nurse practitioner training program includedfour months of classroom work and five months of supervised clinical training. The two PAs who had no previous NICU experiencewere also required to attend this course. Neonatal nurse practitioners and PAs held the same patient care responsibilities as did theresidents, including writing daily progress notes and orders on all patients assigned to their team. Neonatal nurse practitioners andPAs also performed all procedures on their patients, including but not limited to endotracheal intubation and placement of umbilicalcatheters, peripheral arterial lines, and chest tubes. Similar patients were cared for by the two teams, as determined by patientbackground characteristics and diagnostic variables. Performance of the two teams was assessed by comparison of patientmanagement, outcome, and charges. Management variables included data on length of critical care and hospital stay, ventilator andoxygen use, total parenteral nutritional use, number of transfusions, and the performance of various procedures. Outcome variablesincluded the incidence of air leaks, bronchopulmonary dysplasia, intraventricular hemorrhage, patent ductus arteriosus, necrotizingenterocolitis, retinopathy of prematurity, and number of infants who died. Charge variables included hospital and physician charges.Main Results: Results demonstrated no significant differences in management, outcome, or charge variables between patients caredfor by the two teams. Conclusion: Neonatal nurse practitioners and physician assistants are an effective alternative to residents forpatient care in the neonatal intensive care unit.Grey <strong>Literature</strong>60 Background: This is a summary of a two-year study of the Scottish <strong>Physician</strong> <strong>Assistants</strong> (PAs) pilot that ran from November 2006 to October 2008.Fifteen USA educated PAs worked in Scotland at some period during those 24 months in the following settings: primary care; out of hours clinic;emergency medicine; intermediate care; orthopaedics; acute receiving unit. The study aimed to evaluate the impact and contribution made by theappointed PAs to delivering effective healthcare in NHS Scotland. Methods: The evaluation used mixed data collection methods (e.g., individual andgroup interviews; monthly feedback forms; recording of scope of practice, etc.). Data were collected longitudinally to assess changes. A case studyapproach was taken in selected settings to attain richness. For qualitative data management, nVivo was used. SPSS and Excel were used forquantitative data analysis. Findings: Response: Six group interviews were held with PAs; 63 interviews with team members; 20 interviews withpatients; four with NHS senior managers and three with Partnership Forum representatives. Work activity data were collected for settings; 48%Carzoli, R. P., Martinez-Cruz,M., Cuevas, L. L., Murphy, S. &Chiu, T. (1994). Comparison ofneonatal nurse practitioners,physician assistants, andresidents in the neonatalintensive care unit. Archives ofPediatrics and AdolescentMedicine, 148, 1271-1276.Farmer, J., Currie, M., West, C.,Hyman, J. & Arnott, N. (2009).Evaluation of <strong>Physician</strong> <strong>Assistants</strong>to NHS Scotland: Final Report.UHI Millennium Institute.Available at:http://www.nes.scot.nhs.uk/media/Page 66 of 74