Caring Headlines - Let's talk safety "A look at the ... - Mghpcs.org
Caring Headlines - Let's talk safety "A look at the ... - Mghpcs.org
Caring Headlines - Let's talk safety "A look at the ... - Mghpcs.org
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
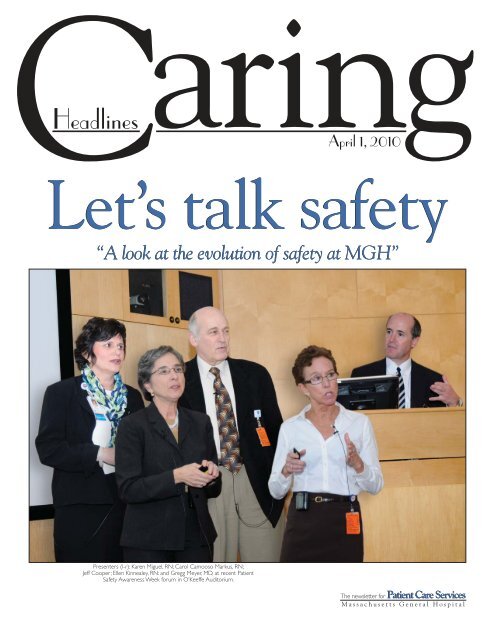
<strong>Caring</strong><strong>Headlines</strong>April 1, 2010Let’s <strong>talk</strong> <strong>safety</strong>“A <strong>look</strong> <strong>at</strong> <strong>the</strong> evolution of <strong>safety</strong> <strong>at</strong> MGH”Presenters (l-r): Karen Miguel, RN; Carol Camooso Markus, RN;Jeff Cooper; Ellen Kinnealey, RN: and Gregg Meyer, MD, <strong>at</strong> recent P<strong>at</strong>ientSafety Awareness Week forum in O’Keeffe Auditorium.The newsletter for P<strong>at</strong>ient Care ServicesMassachusetts General Hospital
Jeanette Ives EricksonLicensure, credentialing,and certific<strong>at</strong>ionWh<strong>at</strong> do <strong>the</strong>y mean, and why are<strong>the</strong>y important?Licensure,credentialing, andcertifi c<strong>at</strong>ion — allhave to do withletting p<strong>at</strong>ients and<strong>the</strong> public knowth<strong>at</strong> clinicians arequalifi ed to practicein a particularfi eld or discipline,but <strong>the</strong>re aresubtle differencesbetween <strong>the</strong>three.Even among some healthcare professionals,<strong>the</strong> distinction between licensure,credentialing, and certific<strong>at</strong>ion isnot easily understood. All have to dowith letting p<strong>at</strong>ients and <strong>the</strong> publicknow th<strong>at</strong> clinicians are qualified topractice in a particular field or discipline,but <strong>the</strong>re are subtle differencesbetween <strong>the</strong> three. Licensure in a particular discipline,such as nursing or social work, signifies th<strong>at</strong> aclinician possesses entry-level knowledge in th<strong>at</strong> discipline— it is <strong>the</strong> minimum requirement necessary topractice in a health profession, and it in no way indic<strong>at</strong>eswhe<strong>the</strong>r a clinician has knowledge or expertisebeyond th<strong>at</strong> minimum. In most st<strong>at</strong>es, including Massachusetts,continuing educ<strong>at</strong>ion is required for licenserenewal.Certific<strong>at</strong>ion is a voluntary process. It signifies th<strong>at</strong>a clinician has acquired knowledge, training, and experienceover and above wh<strong>at</strong> is minimally required in acertain specialty within his or her discipline. Becomingcertified involves successfully completing a writtenexam and demonstr<strong>at</strong>ing competency in certain preestablishedstandards. Each certifying body or agencysets <strong>the</strong> standards for certific<strong>at</strong>ion within its own specialty.In nursing, for example, some of <strong>the</strong> many certific<strong>at</strong>ionsavailable include:• neuroscience nursing• medical nursing• cardiovascular nursingJeanette Ives Erickson, RN, senior vice presidentfor P<strong>at</strong>ient Care and chief nurse• oncology nursing• critical care nursingPhysical Therapy offers certific<strong>at</strong>ion in:• geri<strong>at</strong>rics• pedi<strong>at</strong>rics• women’s health• neurology• orthopedicsOccup<strong>at</strong>ional Therapy offers certific<strong>at</strong>ion in• gerontology• hand and upper extremity rehabilit<strong>at</strong>ion• mental health• pedi<strong>at</strong>rics• physical rehabilit<strong>at</strong>ionMany disciplines offer specialty certific<strong>at</strong>ion. Studiesshow th<strong>at</strong> certific<strong>at</strong>ion increases job s<strong>at</strong>isfaction, contributesto a sense of personal empowerment, and givesp<strong>at</strong>ients a heightened sense of confidence in <strong>the</strong>ir caregivers.Public awareness about certific<strong>at</strong>ion is growing— more and more p<strong>at</strong>ients are requesting clinicianswith specialized knowledge about <strong>the</strong>ir disease or progcontinuedon next pagePage 2 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010
Jeanette Ives Erickson (continued)The body ofknowledge <strong>at</strong><strong>the</strong> core ofall healthcareprofessionsis constantlychanging andexpanding.Specialtycertifi c<strong>at</strong>ion isone way toensure th<strong>at</strong> ourpractice keepspace with <strong>the</strong>nosis. Institutions th<strong>at</strong> employ a large number of certifiedstaff are highly sought after in a competitive marketplace.At MGH, a growing number of clinicians are becomingcertified every year. The Knight NursingCenter for Clinical & Professional Development offersprepar<strong>at</strong>ion courses in some specialty areas, and financialsupport for certific<strong>at</strong>ion and re-certific<strong>at</strong>ion isavailable to nurses through <strong>the</strong> Demetri Souretis Fund.In addition to formal classes offered by <strong>the</strong> KnightCenter, several unit-based certific<strong>at</strong>ion programs havebeen initi<strong>at</strong>ed by staff in <strong>the</strong> Post Anes<strong>the</strong>sia CareUnit, <strong>the</strong> Endo scopy Unit, medical and oncologyunits, and elsewhere. Our 65Plus program has developeda robust gerontology certific<strong>at</strong>ion program to increase<strong>the</strong> number of nurses hospital-wide who arespecially trained to care for our growing popul<strong>at</strong>ion ofolder adult p<strong>at</strong>ients.The body of knowledge <strong>at</strong> <strong>the</strong> core of all healthcareprofessions is constantly changing and expanding.Specialty certifi c<strong>at</strong>ion is one way to ensure th<strong>at</strong>our practice keeps pace with <strong>the</strong> complex demands ofp<strong>at</strong>ient care in a fast-paced teaching hospital likeMGH.Unlike certifi c<strong>at</strong>ion, which is voluntary, credentialingis required by law and regul<strong>at</strong>ory agencies toensure th<strong>at</strong> healthcare professionals are qualified toperform within <strong>the</strong> scope of practice of <strong>the</strong>ir givenprofession or discipline. Credentialing is an administr<strong>at</strong>iveprocess by which a practitioner’s educ<strong>at</strong>ion,certifi c<strong>at</strong>ion, training, experience, and record with<strong>the</strong> Board of Registr<strong>at</strong>ion are examined as evidenceth<strong>at</strong> he or she is qualified to practice in aspecific role.At MGH, we’re implementing some changes in<strong>the</strong> credentialing process for nurses in <strong>the</strong> expandedrole (nurse practitioner, nurse midwife, nurseanes<strong>the</strong>tists, and psychi<strong>at</strong>ric clinical nurse specialist)and physician assistants. Currently, credentialingapplicants go through an approval process th<strong>at</strong>involves <strong>the</strong> supervising physician, <strong>the</strong> chief of service,<strong>the</strong> credentialing coordin<strong>at</strong>or, and <strong>the</strong> HealthProfes sions Staff Committee, with final approvalby <strong>the</strong> Nursing Executive Committee and me inmy role as senior vice president for P<strong>at</strong>ient Careand chief nurse.Effective May 24, 2010, <strong>the</strong> final stages of <strong>the</strong>approval process will change: <strong>the</strong> P<strong>at</strong>ient CareServices Executive Committee (not <strong>the</strong> Nurs ingExecutive Committee) and I will review applic<strong>at</strong>ions.If approved, <strong>the</strong>y’ll be sent to <strong>the</strong> Board ofTrustees for final approval. (Some conditions applyfor candid<strong>at</strong>es requesting fi rst assist and access tooper<strong>at</strong>ing rooms.) If/when final approval is granted,candid<strong>at</strong>es will receive a letter deline<strong>at</strong>ing<strong>the</strong>ir type of appointment and specific clinicalprivileges.I hope this helps clarify some of <strong>the</strong> questionsaround licensure, credentialing, and certific<strong>at</strong>ion.For more inform<strong>at</strong>ion, consult your nursing directoror supervisor, or call Julie Goldman, RN,profession al development manager, <strong>at</strong> 4-2295.complex demandsof p<strong>at</strong>ient carein a fast-pacedteaching hospitallike MGH.In this IssueP<strong>at</strong>ient Safety Awareness Week ................................1 Fielding <strong>the</strong> Issues ..............................................................8• Key WordsJeanette Ives Erickson ......................................................2• On Licensure, Credentialing, and Certifi c<strong>at</strong>ion Key Word ‘Wordle”.....................................................9New Gradu<strong>at</strong>e in Critical Care NursingAnnouncements .............................................................14Program .............................................................................4Best PracticesP<strong>at</strong>ient Safety Awareness Week ................................5 • Preventing UTIs .........................................................15Clinical Narr<strong>at</strong>ive ...............................................................6 Be Fit Lunchtime Sessions.........................................16• Darren LeBlanc, RNApril 1, 2010 — <strong>Caring</strong> <strong>Headlines</strong> — Page 3
Educ<strong>at</strong>ion/SupportNew Gradu<strong>at</strong>e in Critical CareNursing Program— by Gail Alexander, RN, professional development specialistStanding (l-r): Fred Tarazi,RN; Darren LeBlanc, RN;Jennifer Roy, RN; Jenny Rusin,RN; Rebekah Bitar, RN;Christie McKee, RN; andHannah Owens-Pike, RN.Se<strong>at</strong>ed: Christine Dunlap,RN; Jill Pallotta, RN; K<strong>at</strong>lynBreton, RN; Jeff Silvia, RN;and program coordin<strong>at</strong>or,Gail Alexander, RN.On March 4, 2010, <strong>the</strong> 16thclass of <strong>the</strong> New Gradu<strong>at</strong>e inCritical Care Nursing Programwas recognized for successfullycompleting <strong>the</strong> six-monthprogram, bringing <strong>the</strong> totalnumber of gradu<strong>at</strong>es to 146.Executive director of <strong>the</strong>Institute for P<strong>at</strong>ient Care, Gaurdia Banister, RN, comparedparticipants to Olympic <strong>at</strong>hletes. “Olympians exudea professionalism th<strong>at</strong> reflects pride in wh<strong>at</strong> <strong>the</strong>ydo. Nothing requires more professionalism than caringfor critically ill p<strong>at</strong>ients and <strong>the</strong>ir families. Olympiansare committed; <strong>the</strong>y’re highly motiv<strong>at</strong>ed; <strong>the</strong>y believein <strong>the</strong>mselves; and <strong>the</strong>y work as a team.”(Photo provided by staff)New gradu<strong>at</strong>e, K<strong>at</strong>lyn Breton, RN, and her preceptor,K<strong>at</strong>e Roche, RN, read narr<strong>at</strong>ives recounting <strong>the</strong>care <strong>the</strong>y provided transitioning a p<strong>at</strong>ient from aggressivetre<strong>at</strong>ment to comfort care. Said Breton, “The p<strong>at</strong>ient’sdaughter turned to me with tears in her eyes andsaid, ‘Can you close <strong>the</strong> curtain. I want to listen to mydad’s favorite song with him.’ As I closed <strong>the</strong> shade,she put one headphone in her f<strong>at</strong>her’s ear and one inher own. I realized <strong>the</strong>n <strong>the</strong> unique n<strong>at</strong>ure of my profession.I was witnessing <strong>the</strong> purest form of love betweena child and her f<strong>at</strong>her. No words could describehow I felt <strong>at</strong> th<strong>at</strong> moment.”Roche recognized in Breton <strong>the</strong> qualities of an exemplarynurse: someone who is, “willing to embracenot only <strong>the</strong> complex and challenging clinical tasks,but <strong>the</strong> personal, human connections th<strong>at</strong> make dayslike this <strong>at</strong> once heart-breaking and awe-inspiring.”Under Roche’s tutelage, Breton is developing her professionalidentity as a nurse.Certific<strong>at</strong>es of completion were given to:• Rebekah Bitar, RN, Cardiac ICU• Jenny Rusin, RN, Cardiac ICU• Christie McKee, RN, Cardiac Surgical ICU• Jeff Silvia, RN, Cardiac Surgical ICU• Christine Dunlap, RN, Knight Center for InterventionalCardiovascular Therapy• Fred Tarazi, RN, Medical ICU• Jill Pallotta, RN, Medical ICU• K<strong>at</strong>lyn Breton, RN, Medical ICU• Jennifer Roy, RN, Neuroscience ICU• Hannah Owens-Pike, RN, Neuroscience ICU• Darren LeBlanc, RN, Post Anes<strong>the</strong>sia Care UnitFor more inform<strong>at</strong>ion about <strong>the</strong> New Gradu<strong>at</strong>e inCritical Care Nursing Program, visit: www.mghnursing.<strong>org</strong>, or call Gail Alexander, RN, <strong>at</strong> 6-0359.Page 4 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010
SafetyP<strong>at</strong>ient Safety Awareness Weeka lot has happened since e<strong>the</strong>r— by Lela Holden, p<strong>at</strong>ient <strong>safety</strong> offi cerPresenters <strong>at</strong> <strong>the</strong>N<strong>at</strong>ional P<strong>at</strong>ient SafetyAwareness Week forum(l-r): Ellen Kinnealey, RN:Carol Camooso Markus,RN; Karen Miguel, RN;and Jeff Cooper,On Thursday, March 11, 2010,a distinguished group of MGHclinicians came toge<strong>the</strong>r inO’Keeffe Auditorium to share<strong>the</strong>ir recollections of advancesin p<strong>at</strong>ient <strong>safety</strong> over <strong>the</strong> pastfour decades. Presenters,N<strong>at</strong>haniel Sims, MD; EllenKinnealey, RN: Karen Miguel, RN; Carol CamoosoMarkus, RN; and Jeff Cooper, shared stories of <strong>the</strong>irpersonal involvement with various <strong>safety</strong> improvementsand innov<strong>at</strong>ions over <strong>the</strong> years.Sims, who presented via pre-recorded video, recounted<strong>the</strong> advances in medic<strong>at</strong>ions for cardiac-surgeryp<strong>at</strong>ients th<strong>at</strong> came in <strong>the</strong> early 1980s, but pumps<strong>at</strong> th<strong>at</strong> time were ‘heavy and dumb.’ Sims helped designsmaller pumps th<strong>at</strong> came with calcul<strong>at</strong>ors to helpdetermine safe drug doses. Kinnealey, a nurse inBiomedical Engineering, was a key player in <strong>the</strong> developmentof <strong>the</strong> first clinician-based drug library th<strong>at</strong>contained high and low limits for high-risk medic<strong>at</strong>ions.She worked closely with staff of <strong>the</strong> SurgicalIntensive Care Unit to trial <strong>the</strong>se ‘smart’ pumps.Miguel, p<strong>at</strong>ient <strong>safety</strong> officer in <strong>the</strong> Imaging Department,noted th<strong>at</strong> progress is made by ‘ordinary’people doing extraordinary things. She recalled staffbeing concerned about needle sticks in <strong>the</strong> early 90s.Miguel co-chaired <strong>the</strong> Products Review Subcommitteeas <strong>the</strong>y helped design and test a new protected needle.MGH was <strong>the</strong> first hospital to use <strong>the</strong> Sims PortextNeedle Pro, now standard-issue across <strong>the</strong> country.Markus, staff specialist in <strong>the</strong> Office of Quality &Safety, described <strong>the</strong> development of <strong>the</strong> professionalpractice model th<strong>at</strong> produced collabor<strong>at</strong>ive governancein 2003 and <strong>the</strong> champion model th<strong>at</strong> was so successfullyemployed in securing Magnet design<strong>at</strong>ion, handhygienecompliance, and most recently, ExcellenceEvery Day Joint Commission preparedness.Cooper, executive director of <strong>the</strong> Center for MedicalSimul<strong>at</strong>ion, <strong>talk</strong>ed about errors in oper<strong>at</strong>ing roomsin <strong>the</strong> early 70s. He and colleagues wrote one of <strong>the</strong>first papers on <strong>the</strong> topic in 1978. Cooper was part of<strong>the</strong> team th<strong>at</strong> brought major <strong>safety</strong> improvements toequipment used by anes<strong>the</strong>siologists. He encouragedclinicians to speak up when th<strong>at</strong> ‘inner voice’ tells yousomething’s wrong. Errors happen when people don’tbring those concerns forward.Individual present<strong>at</strong>ions were followed by a paneldiscussion, led by Gregg Meyer, MD, senior vice presidentfor The Center of Quality & Safety. Panelistsagreed th<strong>at</strong> <strong>safety</strong> challenges continue, but MGH has ahistory of listening when clinicians speak to advoc<strong>at</strong>efor safe p<strong>at</strong>ient care.For more inform<strong>at</strong>ion about <strong>safety</strong> initi<strong>at</strong>ives <strong>at</strong>MGH, call <strong>the</strong> PCS Office of Quality & Safety <strong>at</strong>3-0140.April 1, 2010 — <strong>Caring</strong> <strong>Headlines</strong> — Page 5
Clinical Narr<strong>at</strong>iveNew nurse learnsth<strong>at</strong> every day in <strong>the</strong> PACUis an opportunity to learnI’d heard storiesof p<strong>at</strong>ients wakingup in a violentst<strong>at</strong>e, but I hadnever experiencedit fi rst hand... Iquickly realizedth<strong>at</strong> given his levelof agit<strong>at</strong>ion, it wasprobably best toleave him alone for<strong>the</strong> moment.My name is Darren LeBlanc,and I am a recent gradu<strong>at</strong>eof <strong>the</strong> New Gradu<strong>at</strong>e inCritical Care NursingProgram. I’ve worked in<strong>the</strong> new Post-Anes<strong>the</strong>siaCare Unit (PACU) for <strong>the</strong>past four months. Oneday recently, when my preceptor was out sick, I was assignedto work with ano<strong>the</strong>r experienced nurse, Diane.Diane told me th<strong>at</strong> our first p<strong>at</strong>ient was a 45-year-old,Italian man named, ‘Marco,’ who was a husband andf<strong>at</strong>her of three. Marco was scheduled to arrive in <strong>the</strong>PACU following surgery for rectal adenocarcinomaand a liver biopsy to determine if his cancer hadspread.Marco arrived on <strong>the</strong> unit in <strong>the</strong> early afternoon,accompanied by members of <strong>the</strong> surgical and anes<strong>the</strong>si<strong>at</strong>eams. Like most post-oper<strong>at</strong>ive p<strong>at</strong>ients, he wasasleep. The anes<strong>the</strong>sia resident gave Diane and mesome background about Marco and asked if ei<strong>the</strong>r of usspoke French or Italian because Marco spoke boththose languages; she didn’t know if he spoke English. Ido speak a little French. The resident explained th<strong>at</strong>Marco had never had surgery before and had been veryanxious in <strong>the</strong> weeks leading up to <strong>the</strong> oper<strong>at</strong>ion.Though his surgery had been uneventful, it became apparentas we <strong>at</strong>tached him to <strong>the</strong> monitors th<strong>at</strong> hispost-oper<strong>at</strong>ive course might not be so smooth.Darren LeBlanc, RN, Cullen PostAnes<strong>the</strong>sia Care UnitMarco was on his side in a semi-fetal position, hisoxygen mask was down around his chin, and he was lyingon his IV line. Attaching his heart-monitor leadswhile he was in this position was a challenge. He beganto moan. I tried to replace his oxygen mask, butMarco became agit<strong>at</strong>ed and pushed my hand away. Itried again, but he became more agit<strong>at</strong>ed and aggressivelywaved his arms while shouting in an Italian accent,“Leave me alone! Let me sleep!” The team caringfor Marco understood th<strong>at</strong> this situ<strong>at</strong>ion could turnvol<strong>at</strong>ile; we needed to tread lightly and not exacerb<strong>at</strong>e<strong>the</strong> situ<strong>at</strong>ion. I’d heard stories of p<strong>at</strong>ients waking up ina violent st<strong>at</strong>e, but I had never experienced it firsthand. I wanted to get his oxygen mask back on, butquickly realized th<strong>at</strong> given his level of agit<strong>at</strong>ion and<strong>the</strong> fact th<strong>at</strong> his oxygen s<strong>at</strong>ur<strong>at</strong>ion was stable <strong>at</strong> 99-100%, it was probably best to leave him alone for <strong>the</strong>moment.continued on next pagePage 6 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010
Clinical Narr<strong>at</strong>ive (continued)When it wastime for Marcoto be transferredto his room onEllison 7, he askedif I was coming to<strong>the</strong> unit with him.When I told him Ihad to stay in <strong>the</strong>PACU, he seemeddisappointed...He thanked merepe<strong>at</strong>edly, and itfelt good.After getting report from <strong>the</strong> anes<strong>the</strong>sia resident, Ijoined <strong>the</strong> o<strong>the</strong>r nurses who were discussing how bestto handle Marco’s behavior. Trying to interject somehumor into <strong>the</strong> situ<strong>at</strong>ion, I told <strong>the</strong>m not to worry; Iwas <strong>the</strong> ‘p<strong>at</strong>ient whisperer.’ I went back to Marco’sroom hoping I could calm him down. Marco wasmoaning. I went to <strong>the</strong> head of <strong>the</strong> stretcher and askedif he was in pain. He was. I asked him to open his eyesand <strong>look</strong> <strong>at</strong> me. When I got his <strong>at</strong>tention, I asked himto r<strong>at</strong>e his pain on a scale of 0-10. He said it was 10and told me to leave him alone. I asked Diane to getsome dilaudid from <strong>the</strong> Omnicell so I could try to managehis pain. I took ano<strong>the</strong>r set of vital signs whileDiane was gone.When she returned, I tried to access Marco’s IVline, but he was lying on it so I couldn’t reach <strong>the</strong> port.I tried to gently move his arm as I explained wh<strong>at</strong> I wasdoing, but he yelled, “No! Leave me alone!” Not knowingwh<strong>at</strong> Marco was capable of, I was concerned th<strong>at</strong> ifI continued to prod him, he might become even moreagit<strong>at</strong>ed. I needed him to understand th<strong>at</strong> I was tryingto help control his pain, so I carefully continued my efforts.I told him in a soothing voice th<strong>at</strong> I could onlyhelp if he worked with me. I told him I had medic<strong>at</strong>ionth<strong>at</strong> would help his pain but I needed to move his armto get to <strong>the</strong> IV. Still moaning, he rolled over, and Iwas able to give him his first dose of dilaudid. Finally, Ifelt as if I’d gotten through to him.Despite <strong>the</strong> dilaudid, Marco still reported pain. Iput my hand on his shoulder and told him it wouldtake a little while for <strong>the</strong> medic<strong>at</strong>ion to work. I stayedclose by and continued to check his stoma and abdominaldressings, and monitor his vital signs and respir<strong>at</strong>oryr<strong>at</strong>e. When I checked <strong>the</strong> orders again, I saw th<strong>at</strong><strong>the</strong> doctor had ordered 15mg of Toradol. I wasn’t sureif it was safe to give Toradol with dilaudid, so I checkedwith Diane, and she assured me it was safe. One thing Irealize as a new nurse is th<strong>at</strong> you don’t know wh<strong>at</strong> youdon’t know, so if I’m not sure about something, I alwaysask.For <strong>the</strong> rest of his stay in <strong>the</strong> PACU, I cared forMarco, continued to monitor his pain, gave him moistswabs to moisten his mouth, and re-positioned himwhen he slid down on <strong>the</strong> stretcher. Marco altern<strong>at</strong>edbetween sleeping and waking with some periods ofsleep apnea. He still reported some pain, but I explainedth<strong>at</strong> <strong>the</strong> medic<strong>at</strong>ion was slowing down hisbre<strong>at</strong>hing so I had to be careful not to give him toomuch. He understood. I used o<strong>the</strong>r interventions tohelp manage his pain, such as changing his blankets,and re-positioning him. I was happy th<strong>at</strong> despite hiscontinued pain, he was clearly much more comfortablethan when he first arrived. I was also happy th<strong>at</strong>I had gained his trust and made him realize th<strong>at</strong> mygoal was to make him comfortable and keep him safe.As soon as I explained th<strong>at</strong> I wanted to help him, hehad become more cooper<strong>at</strong>ive. He began to apologizefor ‘bo<strong>the</strong>ring’ me when he asked for assistance withre-positioning or for a mouth swab. I assured him Iwas happy to help.When it was time for Marco to be transferred tohis room on Ellison 7, he asked if I was coming to <strong>the</strong>unit with him. When I told him I had to stay in <strong>the</strong>PACU, he seemed disappointed. I told him it hadbeen nice meeting him and taking care of him. I toldhim to take care of himself and I hoped he had acomfortable night. He thanked me repe<strong>at</strong>edly, and itfelt good.Experiences like this are why I love nursing, and<strong>the</strong>y happen every day in <strong>the</strong> PACU. I find it so rewardingto meet p<strong>at</strong>ients who are frightened, worried,or in pain, and spend a little time with <strong>the</strong>m, let<strong>the</strong>m know I genuinely care, and see <strong>the</strong>ir conditionschange before my eyes. It makes a big difference tome, but wh<strong>at</strong>’s more rewarding, is th<strong>at</strong> it makes a bigdifference to <strong>the</strong>m.Although I am rel<strong>at</strong>ively inexperienced in providingnursing care and administering medic<strong>at</strong>ions, Ifeel my gre<strong>at</strong>est strength lies in my genuine desire togive <strong>the</strong> best possible care and comfort to p<strong>at</strong>ients— a desire I believe is quickly communic<strong>at</strong>edin my actions and manner. I <strong>look</strong> forward to gainingmore experience in <strong>the</strong> technical aspects of nursing— experience th<strong>at</strong> when combined with my desireto heal and comfort, will lead to a successfulnursing career.Comments by Jeanette Ives Erickson, RN,senior vice president for P<strong>at</strong>ient Care and chief nursePerhaps <strong>the</strong> wisest thing Darren said in this narr<strong>at</strong>ivewas th<strong>at</strong> as a new nurse, you don’t know wh<strong>at</strong> youdon’t know. Always seek <strong>the</strong> expertise of a more experiencedclinician. Which is exactly wh<strong>at</strong> Darrendid as he cared for Marco in wh<strong>at</strong> could have been avol<strong>at</strong>ile situ<strong>at</strong>ion. With his compassion, honesty,steadfast vigilance, and personal ease, Darren earnedMarco’s trust. Who knows — with his persistent yetgentle bedside manner, maybe Darren really is <strong>the</strong>‘p<strong>at</strong>ient whisper er.’Thank-you, Darren.April 1, 2010 — <strong>Caring</strong> <strong>Headlines</strong> — Page 7
Fielding <strong>the</strong> IssuesThe healing powerof wordsQuestion: I’ve heard people <strong>talk</strong> about ‘key words’ and ‘scripting.’Wh<strong>at</strong> does th<strong>at</strong> mean?Jeanette: As clinicians, <strong>the</strong> words we use can have a profound affecton p<strong>at</strong>ients and families. In stressful times, using <strong>the</strong> right wordscan mean <strong>the</strong> difference between a positive or neg<strong>at</strong>ive experience.In <strong>the</strong> complex setting of p<strong>at</strong>ient care, sometimes a few kind wordscan go a long way toward helping and healing.Scripting is when you’re given a written text with <strong>the</strong> exactwords to say in a particular situ<strong>at</strong>ion. Scripting leaves nothing to <strong>the</strong>imagin<strong>at</strong>ion, doesn’t allow for n<strong>at</strong>ural convers<strong>at</strong>ion, and can comeacross as forced or insincere.Key words, on <strong>the</strong> o<strong>the</strong>r hand, are reminders of <strong>the</strong> topics youwant to discuss, but in your own words, <strong>at</strong> <strong>the</strong> appropri<strong>at</strong>e time, andin <strong>the</strong> appropri<strong>at</strong>e way. Using key words allows you to show emp<strong>at</strong>hyand respect while <strong>at</strong> <strong>the</strong> same time ensuring you remember <strong>the</strong>key topics you want to cover.Key words also help make our concern for <strong>the</strong> p<strong>at</strong>ient’s comfortand <strong>safety</strong> more visible.Question: Can you give me an example of key words?Jeanette: If you’re rounding, and you enter a p<strong>at</strong>ient’s room,some key words might be: privacy, <strong>safety</strong>, hand hygiene, or comfort.With those key words in mind, you might say something like, “I’mclosing your curtain in case you’d like some privacy.”“I’m just going to double-check your wrist-band. We take <strong>safety</strong>very seriously.”“It’s important th<strong>at</strong> caregivers disinfect <strong>the</strong>ir hands before cominginto contact with you or <strong>the</strong> things in your room. This helpsprevent <strong>the</strong> spread of infection.”“Are you comfortable? Can I help re-position you while I’mhere?”“Is <strong>the</strong>re anything else I can help you with?”Question: Why are key words important?Jeanette: In addition to reminding you of <strong>the</strong>tasks you want to perform, key words reinforce in<strong>the</strong> p<strong>at</strong>ient’s mind our commitment to <strong>safety</strong> and apositive p<strong>at</strong>ient experience. Eye contact, a smile, ora gentle touch can make a big difference for a p<strong>at</strong>ientwho’s scared, uncertain, or lonely.Question: Should we use key words every timewe enter a p<strong>at</strong>ient’s room?Jeanette: As I mentioned, you never want yourinteractions with p<strong>at</strong>ients to sound rehearsed or insincere.As you start to use key words, <strong>the</strong>y’ll becomea n<strong>at</strong>ural part of your convers<strong>at</strong>ions. It neverhurts to remind p<strong>at</strong>ients of <strong>the</strong> truly remarkablecare we deliver every day. We’re proud of <strong>the</strong> carewe provide; we want our interactions with p<strong>at</strong>ientsto reflect th<strong>at</strong>.Question: Is <strong>the</strong>re a list of key words we shouldbe using?Jeanette: Certainly <strong>the</strong> 7-Ps are a good place tostart (Person, Plan, Priorities, Personal hygiene,Pain-management, Position, and Pre sence). Butyou should feel free to come up with your own listof key words th<strong>at</strong> would be helpful to you on yourunit, in your specialty, with your p<strong>at</strong>ients. See <strong>the</strong>‘Wordle’ on <strong>the</strong> opposite page for ideas, or call <strong>the</strong>Office of Service Improvement <strong>at</strong> 4-2838.Page 8 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010
A WordleA Wordle is avisual represent<strong>at</strong>ionof frequently-usedwords and phrasesth<strong>at</strong> allows <strong>the</strong> viewerto appreci<strong>at</strong>e <strong>the</strong>rel<strong>at</strong>ionship betweenwords and <strong>the</strong> unity ofthoughts and ideas.A Wordle is <strong>at</strong> oncean artistic renderingand a reminder of<strong>the</strong> power of words.The Wordle <strong>at</strong>right is a collection ofwords staff might fi nduseful as <strong>the</strong>y provideexcellent careevery day.April 1, 2010 — <strong>Caring</strong> <strong>Headlines</strong> — Page 9
AnnouncementsBe FitLunchtime SeminarsJoin advanced personal trainer,Mike Bento of The Clubs <strong>at</strong>Charles River Park, for a one-hour,lunchtime Be Fit seminar.Topics varyNext session:April 15, 201012:00–1:00pmBigelow 4 Amphi<strong>the</strong><strong>at</strong>erFor more inform<strong>at</strong>ion,call 6-2900.MGH College FairEmployees are invited to <strong>the</strong>2010 MGH College FairApril 28, 201012:00pm – 3:00pmunder <strong>the</strong> Bulfi nch TentExplore careers in health care,healthcare administr<strong>at</strong>ion,healthcare policy, and businessmanagement. The fair is anopportunity to compareundergradu<strong>at</strong>e, gradu<strong>at</strong>e, andcertifi c<strong>at</strong>e programs.Some of <strong>the</strong> colleges anduniversities scheduled to <strong>at</strong>tendinclude:Boston UniversityBunker Hill Community CollegeCambridge CollegeCurry CollegeHarvard Extension SchoolMass Bay Community CollegeMassasoit CommunityMass College of PharmacyMGH Institute of HealthProfessionsNor<strong>the</strong>astern UniversityNorth Shore Community CollegeRegis CollegeRoxbury Community CollegeSuffolk UniversityUMass, LowellUniversity of PhoenixNo registr<strong>at</strong>ion required.Sponsored by Training andWorkforce Development.For more inform<strong>at</strong>ion,call John Coco <strong>at</strong> 4-3368.Holy Week 2010and Passover 5770Roman C<strong>at</strong>holic, Ecumenical, andPassover services will be offeredthroughout <strong>the</strong> week.All services will be held in <strong>the</strong>MGH Chapel on Ellison 1All are welcomeFor a complete listing of timesand services, call <strong>the</strong> MGHChaplaincy <strong>at</strong> 6-2220.Make yourpractice visible: submita clinical narr<strong>at</strong>ive<strong>Caring</strong> <strong>Headlines</strong> is alwaysinterested in receiving clinicalnarr<strong>at</strong>ives th<strong>at</strong> highlight <strong>the</strong>exceptional care provided byclinicians throughoutP<strong>at</strong>ient Care Services.Make your practice visible.Submit your narr<strong>at</strong>ive forpublic<strong>at</strong>ion in <strong>Caring</strong> <strong>Headlines</strong>.All submissions should be sent viae-mail to: ssabia@partners.<strong>org</strong>.For more inform<strong>at</strong>ion,call 4-1746.Eldercaremonthly discussion groupJoin facilit<strong>at</strong>ors, Janet T. Loughlin,LICSW, Partners EAP, and BarbaraMoscowitz, LICSW, geri<strong>at</strong>ric socialworker for <strong>the</strong> Eldercare monthlydiscussion group, sponsored by<strong>the</strong> Employee Assistance Program.Come and discuss subjectsrelevant to eldercare.Next session:April 6, 201012:00–1:00pmDoerr Conference RoomYawkey 10-650Old friends and new membersare welcomeFeel free to bring your lunchFor more inform<strong>at</strong>ion, call 6-6976or visit www.eap.partners.<strong>org</strong>.Ethics Forum:a discussion series for <strong>the</strong>MGH communityFriday, April 9, 201012:00–1:00pmSweet Conference RoomGray-Bigelow 432Brown Bag Lunch“Improving <strong>the</strong> Quality of Care <strong>at</strong><strong>the</strong> End of Life: <strong>the</strong> Case for VideoDecision Aids”keynote speaker:Angelo Volandes, MDmoder<strong>at</strong>or: Dr. Alex Cist,Optimal Care CommitteeSponsored by <strong>the</strong> MGH EthicsTaskforce. For more inform<strong>at</strong>ione-mail Jennifer HoodThe MGH BloodDonor CenterThe MGH Blood DonorCenter is loc<strong>at</strong>ed in <strong>the</strong> lobbyof <strong>the</strong> Gray-Jackson Building.The center is open for wholeblooddon<strong>at</strong>ions:Tuesday, Wednesday, Thursday,7:30am – 5:30pmFriday, 8:30am – 4:30pm(closed Monday)Pl<strong>at</strong>elet don<strong>at</strong>ions:Monday, Tuesday, Wednesday,Thursday,7:30am – 5:00pmFriday, 8:30am – 3:00pmAppointments are availableCall <strong>the</strong> MGH Blood DonorCenter <strong>at</strong> 6-8177 to schedulean appointment.Published by<strong>Caring</strong> <strong>Headlines</strong> is published twiceeach month by <strong>the</strong> departmentof P<strong>at</strong>ient Care Services <strong>at</strong>MassachusettsGeneral HospitalPublisherJeanette Ives Erickson, RNsenior vice presidentfor P<strong>at</strong>ient CareManaging EditorSusan SabiaEditorial Advisory BoardChaplaincyMichael McElhinny, MDivEditorial SupportMarianne Ditomassi, RNMary Ellin Smith, RNM<strong>at</strong>erials ManagementEdward RaekeNutrition & Food ServicesBridget Lynch, RDSusan Doyle, RDOffice of P<strong>at</strong>ient AdvocacySally Millar, RNOffice of Quality & SafetyKeith Perleberg, RNOrthotics & Pros<strong>the</strong>ticsMark TlumackiPCS DiversityDeborah Washington, RNPhysical TherapyOccup<strong>at</strong>ional TherapyMichael Sullivan, PTPolice, Security & Outside ServicesJoe CrowleyPublic AffairsSuzanne KimRespir<strong>at</strong>ory CareEd Burns, RRTSocial ServicesEllen Forman, LICSWSpeech, Language & SwallowingDisorders and Reading DisabilitiesCarmen Vega-Barachowitz, SLPTraining and Support StaffStephanie CooperTom DrakeThe Institute for P<strong>at</strong>ient CareGaurdia Banister, RNVolunteer Services, MedicalInterpreters, Ambassadors,and LVC Retail ServicesPaul BartushDistributionUrsula Hoehl, 617-726-9057SubmissionsAll stories should be submittedto: ssabia@partners.<strong>org</strong>For more inform<strong>at</strong>ion, call:617-724-1746Next Public<strong>at</strong>ionApril 15, 2010Page 10 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010
Best Practice“We pity <strong>the</strong> Foley”Sharing best practices to improve p<strong>at</strong>ient care(L-r): Warren Sandberg,MD, anes<strong>the</strong>siologist; BritNicholson, MD, senior vicepresident for Medicine;Dawn Tenney, RN, associ<strong>at</strong>echief nurse; and staff nurses,Michele Allen, RN; andStacy Strezsak, RN.Urinary tract infections are oneof <strong>the</strong> most common hospitalacquiredinfections, accountingfor approxim<strong>at</strong>ely 40% ofhealth-care-rel<strong>at</strong>ed infectionsn<strong>at</strong>ionwide. Of those, 80% are<strong>at</strong>tributable to in-dwellingurethral Foley c<strong>at</strong>heters.In December, a clinical challenge was issued to finda way to reduce <strong>the</strong> number of urinary tract infectionsrel<strong>at</strong>ed to Foley c<strong>at</strong>heter use. As part of <strong>the</strong> SandboxInnov<strong>at</strong>ion Challenge, 12 teams comprised of nurses,physicians, and o<strong>the</strong>rs, brainstormed ways to safely reduce<strong>the</strong> use of in-dwelling Foleys as a means to preventurinary tract infections. On March 11, 2010, in<strong>the</strong> East Garden Dining Room, teams presented <strong>the</strong>irproposed solutions along with an explan<strong>at</strong>ion of how<strong>the</strong>ir solutions could be implemented successfullythroughout <strong>the</strong> hospital.With <strong>the</strong>ir winning solution, affection<strong>at</strong>ely called,“We Pity <strong>the</strong> Foley,” White 11 nurses,Susan Wood, RN; Michele Allen, RN;Stacy Strezsak, RN; and SusanMorash, RN, reported a 49% reductionin Foley usage on <strong>the</strong>ir unit.Said Christiana Iyasere, MD, associ<strong>at</strong>edirector of <strong>the</strong> Innov<strong>at</strong>ionSupport Center. “By celebr<strong>at</strong>ing andacknowledging every proposed solution,<strong>the</strong> hospital community gained abetter understanding of Foley utiliz<strong>at</strong>ionand ways to prevent urinary tractinfections.”Congr<strong>at</strong>ul<strong>at</strong>ions to <strong>the</strong> team onWhite 11 and to all <strong>the</strong> Sandboxteams who shared <strong>the</strong>ir thoughts andideas to improve p<strong>at</strong>ient care.For more inform<strong>at</strong>ion about <strong>the</strong>Sandbox UTI Challenge, go to http://hub.partners.<strong>org</strong>/sandbox, or contactChristiana Iyasere <strong>at</strong> ciyasere@partners.<strong>org</strong>.(Photo provided by staff)Educ<strong>at</strong>ional offerings can now be found on <strong>the</strong>Knight Nursing Center for Clincial & Professional Development websitehttp://www2.massgeneral.<strong>org</strong>/PCS/ccpd/cpd_sum.aspFor more inform<strong>at</strong>ion, call 6-3111.April 1, 2010 — <strong>Caring</strong> <strong>Headlines</strong> — Page 11
Be FitLunchtime seminars offerhealth and fitness tipsBentoendorsesan altern<strong>at</strong>ivemethod forimproving healthand fi tness calledhigh-intensityintervaltraining.On Tuesday, March 23,2010, as part of <strong>the</strong>MGH Be Fit program,advanced personaltrainer, Mike Bento ofThe Clubs <strong>at</strong> CharlesRiver Park, presented aone-hour, lunchtimeseminar entitled, “High-intensity exercise forhealth and body-f<strong>at</strong> reduction.” The session, held inYawkey 10-650, provided an overview of a trainingregimen for runners th<strong>at</strong> focuses on brief, high-intensitysprinting punctu<strong>at</strong>ed by intervals of rest and recovery.Varying <strong>the</strong> length and dur<strong>at</strong>ion of <strong>the</strong> sprintand recovery periods can have a noticeable impact onyour fitness level and ability to reduce body f<strong>at</strong>.Bento endorses this altern<strong>at</strong>ive method, which hecalls high-intensity interval training. According toBento, some rel<strong>at</strong>ively minor changes in your workoutcan lead to speedier progress and less time <strong>at</strong> <strong>the</strong> gym.The seminar was part of a new series sponsored by<strong>the</strong> Clubs <strong>at</strong> Charles River Park designed to help educ<strong>at</strong>eemployees about health and fitness. Due to populardemand, <strong>the</strong> first session, “Are you getting <strong>the</strong>most out of your workouts?” will be repe<strong>at</strong>ed April15th in <strong>the</strong> Bigelow 4 Amphi<strong>the</strong><strong>at</strong>er <strong>at</strong> noon.For more inform<strong>at</strong>ion about monthly, lunchtimeBe Fit sessions, e-mail Mike Bento <strong>at</strong> mbento@partners.<strong>org</strong>.At left, advanced personal trainer, Mike Bentoof The Clubs <strong>at</strong> Charles River Park, presentslunchtime Be Fit seminar.C aring<strong>Headlines</strong>April 1, 2010Returns only to:Bigelow 10 Nursing Offi ce,MGH, 55 Fruit StreetBoston, MA 02114-2696First ClassUS Postage PaidPermit #57416Boston, MAPage 12 — <strong>Caring</strong> <strong>Headlines</strong> — April 1, 2010