Willowbrook Lodge, 302, nursing home inspection report 8 - hiqa.ie
Willowbrook Lodge, 302, nursing home inspection report 8 - hiqa.ie
Willowbrook Lodge, 302, nursing home inspection report 8 - hiqa.ie
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
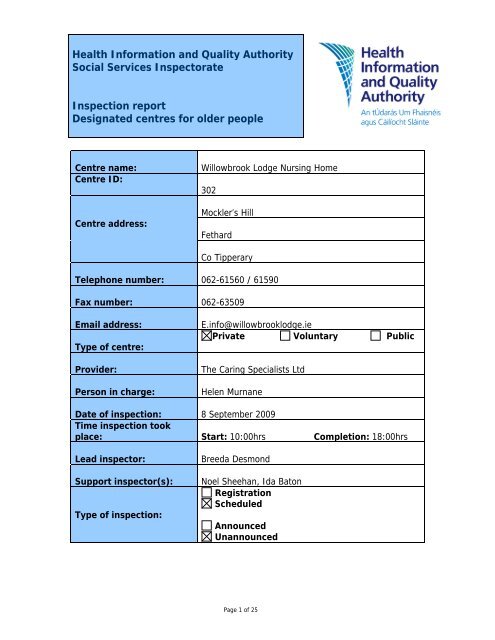
About the centreDescription of services and premises<strong>Willowbrook</strong> <strong>Lodge</strong> Nursing Home comprises a two-storey building with lift and stairaccess to the upper floor. Residents who reside on the first floor are mainly lowdependencywhile residents with higher dependency levels reside on the groundfloor. There are single, two-bedded, three-bedded, and one four-bedded room. Allrooms are en suite.Location<strong>Willowbrook</strong> is located at Mockler’s Hill, three miles from Cashel on the Fethard road,and 15 miles from Clonmel, Tipperary and Thurles. It is situated on an elevated siteoverlooking the countryside. Adjacent to the <strong>nursing</strong> <strong>home</strong> is a purpose-builtretirement village, which complements the surroundings.Date centre was first established: 1994Number of residents on the date of<strong>inspection</strong>25Dependency level of Max High Medium Lowcurrent residentsNumber of residents 0 14 9 2Management structureThe Person in Charge, Helen Murnane, <strong>report</strong>s to the Provider, Noelle Killeen, at<strong>Willowbrook</strong>. There are four nurses on the duty-roster. When the Person in Chargeis on leave, one of the four duty nurses rotate to the role of person in charge,covering these duty hours. Additional rel<strong>ie</strong>f staff are employed to complete the staffnurse quota as required.Page 3 of 25
Overall findings1. Governance: how well the centre is organisedOutcome: The centre is well organised and managed and compl<strong>ie</strong>s with therequirements of the Health Act 2007, the regulations and standards.Good governance involves the effective and effic<strong>ie</strong>nt deployment ofresources in accordance with the stated purpose and function of thecentre. Governance includes setting clear direction for the service, acommitment to continual improvement, and having a system in place toeffectively assess and manage risk.Evidence of good practiceThe provider demonstrated her knowledge of the National Quality Standards forResidential Care Settings for Older People in Ireland and the Health Act 2007 (Careand Welfare of Residents in Designated Centres for Older People) Regulations 2009and all polic<strong>ie</strong>s and required documentation were in the process of being revised inaccordance with legislative requirements.All relevant certifications including insurance, fire, and training were visible on themain hallway for public v<strong>ie</strong>wing.The complaints procedure was open, transparent and practical. Incidents andaccidents were documented and staff identif<strong>ie</strong>d the process adopted as havingpotential for learning and improvement. This was further enabled through theprovider’s leadership style of openness, transparency, and clear communication ofthe mission and vision of the centre.Planning permission has been obtained for an extension to enlarge the dining room.This has gone to tender and one of two quotes was returned at the time of the<strong>inspection</strong>.There were excellent polic<strong>ie</strong>s in relation to risk assessment and risk management.Some improvements requiredThe provider was currently revising the statement of purpose and function, contractsof care, complaints procedure, staff files and centre’s register documentation in linewith legislative requirements and there was evidence that relevant polic<strong>ie</strong>s werebeing prepared by the provider for all aspects of resident care as per the Authority’sNational Quality Standards for Residential Care Settings for Older People in Ireland.Documentation for resident care was evident on the bedroom wall of one residentwhich did not demonstrate respect for the privacy and dignity of the individual.Page 5 of 25
Significant improvements requiredThe person in charge did not have a copy of the Health Act 2007 (Care and Welfareof Residents in Designated Centres for Older People) Regulations 2009 and wasunaware that she should have a copy of them. In order to comply with requirements,a copy of the regulations must be obtained.Page 6 of 25
2. Quality of the serviceOutcome: Residents receive a good standard of service, appropriatetreatment and are treated with courtesy and respect.A quality service is one where residents are protected from harm or abuse,where practice is person centred, where rights are protected, whereresidents are enabled to play an active part in the centre, and wheremanagement, staff and residents work together towards continuousimprovement.Evidence of good practiceThere was no restriction on visiting times for family and visitors and the majority ofvisitors attended in the evenings because of work / family commitments.Inspectors noted that the providers had initiated a residents’ / relatives’ committeeand were in the process of compiling a list of advocacy groups for information.Staff questioned by inspectors had a good understanding and comprehension ofelder abuse. Care attendants said they had received training on the issue as part oftheir Further Education and Training Awards Council (FETAC) level 5 qualification. AHealth Service Executive (HSE) DVD on elder abuse prevention and detection wasalso shown to all staff.Residents had access to all parts of the centre including a designated smoking areasituated outside. There was a sheltered seating area for residents to enjoy andduring the <strong>inspection</strong>, several residents were observed to be using this area.Mass was available once a month and a minister of the Eucharist visited the centretwice a week.Activit<strong>ie</strong>s were held daily depending on what residents wanted. On the day of<strong>inspection</strong>, residents played bingo and did art in the conservatory.Some improvements requiredThe provider said she was revising the location and format for displaying menus forresidents. At the time of <strong>inspection</strong>, menus were not displayed and many residents<strong>report</strong>ed a poor menu choice.Both staff and residents said residents were given a choice of menu for their dinnerand supper the night before, and fortnightly menus were displayed on the fridge inthe kitchen for catering staff, however, no menus were on display for residents.There was a list of specialist d<strong>ie</strong>tary requirements on the fridge door in the kitchenbut these were very difficult to read.Page 7 of 25
One resident, who was unable to mobilise independently, was visited in her room bythe inspector where it was observed that the remote control for her television wasnot within reach.There were only two daily newspapers in the living room and there was no evidenceof magazines or books for residents to read.Page 8 of 25
3. Healthcare needsOutcome: Residents’ healthcare needs are met.Healthcare is integral to meeting individual’s needs. It requires thatresidents’ health, personal and social care needs are assessed andrev<strong>ie</strong>wed on an ongoing basis within a care planning process that is personcentred. Emphasis is firmly placed on health promotion, independence andmeaningful activity.Evidence of good practiceThe admissions policy and procedure showed that the resident and their family wereinvolved in the care-planning process on admission. Many residents had maintainedtheir own general practitioner (GP) services and were able to attend physiotherapy,speech and language therapy, and chiropody if required. Residents were able toaccess physiotherapy at the GP’s request. One resident remained under the care ofthe National Rehabilitation Centre, and there was documented evidence of care fromthis centre, including exercises, duration and application of splints and guidance onthe positioning of a specialist chair.A nutrition scale assessment tool was used and the providers and kitchen staff wereaware of the necessity for well-balanced, wholesome, food incorporating all elementsof the food pyramid.Some improvements requiredThe centre’s policy and approach to residents’ care plans, in terms of their healthcareneeds, was not rev<strong>ie</strong>wed and completed in line with the regulations.The rubber protectors on some Zimmer frames were perished and residents were notassessed regarding the appropriate height of Zimmer frames required to meet theirneeds.Wheelchairs had no foot-rests. Residents were transported in wheelchairs with theirfeet trailing on the ground. This has the potential to cause harm to residents.Significant improvements requiredMedications were not dispensed in proper rotation and were not stored as per AnBord Altranais 2007 guidelines. Medications are rev<strong>ie</strong>wed six-monthly by attendingGPs even though guidance indicates that a rev<strong>ie</strong>w of residents’ medication shouldtake place no less than every three months, or more frequently if indicated.Page 9 of 25
There was no photographic identification present on the medication chart eventhough there was an area for it to be attached.There was little evidence to suggest that there was a comprehensive, in-depth,rev<strong>ie</strong>w of care planning in terms of residents’ healthcare needs. For example, oneresident with a percutaneous gastrostomy tube had not been rev<strong>ie</strong>wed by a relevantclinician regarding her feeding regime since admission, and there was nodocumentation to indicate otherwise.Page 10 of 25
4. Premises and equipment: appropriateness and adequacyOutcome: The residential care setting provides premises and equipmentthat are safe, secure and suitable.A good physical environment is one that enhances the quality of life forresidents and is a pleasant place to live. It meets residents’ individual andcollective needs in a comfortable and <strong>home</strong>ly way, and is accessible, safe,clean, and well maintained. Equipment is provided in response to theassessed needs of each of the residents and maintained appropriately.Evidence of good practiceThe centre was clean with a cleaning and laundry regime in place.Pressure-rel<strong>ie</strong>ving mattresses were available for residents who required them andstaff were aware of the assessment tools required for the appropriate use of thesemattresses.Equipment was serviced as per requirements. There was evidence that fireequipment, hoists, and pressure rel<strong>ie</strong>ving mattresses had been recently serviced. Firetraining was carr<strong>ie</strong>d out in February 2009 and a fire management company wascurrently involved with the centre regarding risk assessment and risk management.The fire hose was centrally located and fire extinguishers were available throughoutthe centre.The provider outlined plans for an extension, to enlarge the dining room, which hasgone to tender. The provider was cognisant of the limited storage space availableand has identif<strong>ie</strong>d this as a necessary component of the proposed extension.One resident requested a shower curtain be placed in his en suite rather than a door.This request was seen to have been facilitated and was documented in his care plan.Health and safety statements and risk management polic<strong>ie</strong>s were present and alcoholgel was available and strategically placed about the <strong>nursing</strong> <strong>home</strong>.There was a separate kitchen sluice.Some improvements requiredThe availability of hot water was inconsistent throughout the building. In some areaswater did not reach amb<strong>ie</strong>nt temperature.Page 11 of 25
Clothes for the laundry were not segregated at source and some residents’ clotheswere not marked with names. Plastic draw-sheets were on some beds and thispractice is not in keeping with best practice.Poor lighting was noted on a corridor adjacent to one of the bedrooms and the lightwas not working in the assisted bathroom upstairs. Storage space for personalbelongings appeared limited for some residents.One resident with high dependency needs was accommodated upstairs despite fireand safety issues. Although this was at the request of her family and wasdocumented in the resident’s notes it remains an area for improvement, as this is notideal.Two staff members were questioned regarding fire evacuation and they were unsureof the protocol.Inspectors saw seating for residents was not appropriate as some residents were atrisk of falling over and were seen to be uncomfortable. Pressure-rel<strong>ie</strong>ving cushionswere available but not utilised even though many residents had high dependencylevels.Page 12 of 25
5. Communication: information provided to residents, relativesand staffOutcome: Information is relevant, clear and up to date for residents.Information is accessible, accurate, and appropriate to residents’ and staffneeds. Feedback is actively sought from residents and relatives and thisinforms future planning and service provision. Information is recorded andmaintained in accordance with legal requirements and best practice, and iscommunicated to staff on a need to know basis to ensure residents’privacy is respected.Evidence of good practiceA brochure was available which outlined the mission of the centre and the facilit<strong>ie</strong>savailable.Staff meetings were held and minutes were documented. Formal meetings occurredquarterly, and a record of attendees was kept. Previously, minutes of meetings heldwere photocop<strong>ie</strong>d and sent to staff who were unable to attend. This practice hasnow ceased and instead a second meeting is held within a week to discuss the sameissues. Informal meetings occur frequently which allows for dissemination ofinformation.The provider was in the process of setting up a residents’ / relatives’ group and wasalso accessing information to compile a listing of advocacy groups forresident/relative information.Some improvements requiredA staff communication book was evident but it had very few entr<strong>ie</strong>s.Page 13 of 25
6. Staff: the recruitment, supervision and competence of staffOutcome: Staff are competent and recruited in suffic<strong>ie</strong>nt numbers to meetresidents’ needsStaff numbers and skill-mix are determined by the size and complexity ofthe service and there should be suffic<strong>ie</strong>nt competent staff on duty, bothday and night, to meet the needs of residents. Robust recruitment andselection procedures ensure the appointment of suitably qualif<strong>ie</strong>d andexper<strong>ie</strong>nced staff. Staff are supported in their work by ongoing trainingand supervision.Evidence of good practiceThere was a planned approach to staff training and development by the providerboth in-house and externally. Many of the care attendants have ach<strong>ie</strong>ved FETAClevel 5, and others were attending this training which was facilitated in-house.Hazard Analysis Critical Control Points (HACCP) training has been completed by allkitchen staff. All staff spoken to were seen to have a good comprehension of elderabuse.Staff and residents spoken with said there was adequate staff to cater for residents’needs and inspectors’ observations supported this v<strong>ie</strong>w. Support for staff wasapparent and it was evident that staff had pride in their work and in the centre. Allstaff had clean uniforms and were neat and tidy in their appearance.Minor issued to be addressedProviders were aware of the necessity for the continuous audit of services and theongoing appraisal of staff, yet appraisal systems for staff were not currently inoperation.There was no record that the centre’s polic<strong>ie</strong>s had been read by staff. Polic<strong>ie</strong>senhance quality and safety of care and quality of life while reducing risk in the careenvironment.Report compiled byBreeda DesmondInspector of Social ServicesSocial Services InspectorateHealth Information and Quality Authority14 September 2009Page 14 of 25
Health Information and Quality AuthoritySocial Services InspectorateAction PlanProvider’s response to <strong>inspection</strong> <strong>report</strong>Centre:<strong>Willowbrook</strong> <strong>Lodge</strong> Nursing HomeCentre ID:<strong>302</strong>Date of <strong>inspection</strong>: 8 September 2009Date of response: 23 November 2009RequirementsThese requirements set out what the provider must do to meet the Health Act 2007,the Health Act 2007 (Care and Welfare of Residents in Designated Centres for OlderPeople) Regulations 2009 and the National Quality Standards for Residential CareSettings for Older People in Ireland.1. The provider is failing to comply with a regulatory requirement in thefollowing respect:The person in charge did not have a copy of the Health Act 2007 (Care and Welfare ofResidents in Designated Centres for Older People) Regulations 2009.Action required:Immediate acquisition by the person in charge of the Health Act 2007 (Care and Welfareof Residents in Designated Centres for Older People) Regulations 2009 anddissemination to all staff.Reference:Health Act 2007Regulation 17: Training and Staff DevelopmentStandard 24: Training and SupervisionPage 15 of 25
Please state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:The person in charge has acquired a copy of the Regulations.Further cop<strong>ie</strong>s have been made available to all staff.Completed2. The provider has failed to comply with a regulatory requirement in thefollowing respect:Statement of Purpose and Function was not formalised as per the Health Act 2007 (Careand Welfare of Residents in Designated Centres for Older People) Regulations 2009.Action required:Devise Statement of Purpose and Function in line with the Health Act 2007 (Care andWelfare of Residents in Designated Centres for Older People) Regulations 2009 andmake available to all staff and residents.Reference:Health Act 2007Regulation 5: Statement of PurposeStandard 28: Purpose and FunctionPlease state the actions you have taken or are planning totake following the <strong>inspection</strong> with timescales:Timescale:Provider’s response:A statement of purpose and function has been devised and iscurrently with the printers. We have received a proof copy and weexpect to finalise the document in the short term.Two weeks3. The provider has failed to comply with a regulatory requirement in thefollowing respect:Socialisation and resident activit<strong>ie</strong>s are not comprehensively addressed and evidence ofactivit<strong>ie</strong>s undertaken was not displayed. There was no notice board available to highlightissues like local events.Action required:Ensure that the residents are provided with facilit<strong>ie</strong>s for the occupation and recreation ofPage 16 of 25
esidents and provide information concerning current affairs, local matters, voluntarygroups, community resources and events.Reference: :Health Act 2007Regulation 10: Residents’ Rights, Dignity and ConsultationStandard 18: Routines and ExpectationsPlease state the actions you have taken or are planning totake following the <strong>inspection</strong> with timescales:Timescale:Provider’s response:A notice board has been placed in a suitable location in the mainday room and items of local interest to residents are displayed.CompletedWe do provide our residents with a wide var<strong>ie</strong>ty of recreation /activit<strong>ie</strong>s and we allow the residents to choose the particular activityon the day. We do accept that heretofore we did not display aspecific activit<strong>ie</strong>s programme, but such a programme is now ondisplay.We also have displayed information on advocacy groups.4. The provider has failed to comply with a regulatory requirement in thefollowing respect:There was evidence that some Zimmer frames were not maintained as rubber protectorswere perished. Wheelchairs had no foot-rests and residents were transported inwheelchairs with feet trailing on the ground.Action required:Ensure that equipment provided should be maintained in good working order.Reference:Health Act 2007Regulation 19: PremisesStandard 25: Physical EnvironmentPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:All Zimmer frames have been inspected and any faulty rubberprotection has been replaced.CompletedFoot rests have been fitted to all wheelchairs.Page 17 of 25
5. The provider is failing to comply with a regulatory requirement in thefollowing respect:Management of medication in the designated centre was not in keeping withprofessional guidelines or best practice.Action required:The person in charge immediately acquires and adapts An Bord Altranais guidelinesincluding Code of Professional Conduct (2000), Medication Management (2007), Scopeof Practice (2000), and any other guidelines appropriate to the enhancement of the roleand responsibility of the person in charge.Reference:Health Act 2007Regulation 33: Ordering, Prescribing, Storing and Administration of MedicinesStandard 14: Medication ManagementPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:Immediately following the <strong>inspection</strong> the person in charge and staffnurses undertook a complete rev<strong>ie</strong>w of An Bord Altranais guidelinesregarding the management of medication. The person in chargehas attended a medication management study day and has br<strong>ie</strong>fedall staff nurses to ensure all guidelines are being adhered to.A drug trolley has been purchased and is now in use.Photographic identification has been attached to each resident’smedication chart.Completed6. The provider is failing to comply with a regulatory requirement in thefollowing respect:The availability of hot water was inconsistent throughout the building.Action required:The provider should make a hot and cold water supply available which incorporatesthermostatic control valves or other suitable anti-scalding protection.Please state the actions you have taken or are planning totake with timescales:Timescale:Page 18 of 25
Provider’s response:Immediately following the <strong>inspection</strong>, hot water boilers were fittedto service the sink / basin in the laundry, and the sluice sinks in thecleaning stores and the sink / basin in the general sluice room.Completed7. The provider is failing to comply with a regulatory requirement in thefollowing respect:The provider failed to complete staff files in line with the requirements of the Health Act2007 (Care and Welfare of Residents in Designated Centres for Older People)Regulations 2009.Action required:Revise all staff files to include the information required under the Health Act 2007 (Careand Welfare of Residents in Designated Centres for Older People) Regulations 2009.Reference:Health Act 2007Regulations 18: RecruitmentStandard 22: RecruitmentPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:All staff members have been requested to submit all necessarydocuments to complete their files in accordance with statutoryrequirements.One month8. The provider is failing to comply with a regulatory requirement in thefollowing respect:The designated centre’s complaints procedure was not formalised as per the Health Act2007 (Care and Welfare of Residents in Designated Centres for Older People)Regulations 2009.Action required:Ensure that the centre’s complaints procedure contains all the required elements asoutlined in the Health Act 2007 (Care and Welfare of Residents in Designated Centresfor Older People) Regulations 2009.Page 19 of 25
Reference:Health Act 2007Regulation 39: Complaints ProceduresStandard 6: ComplaintsPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:A complaints procedure has been formalised which we trust willensure compliance.One month9. The provider is failing to comply with a regulatory requirement in thefollowing respect:The provider failed to ensure that the register/ directory of residents was completed asper the Health Act 2007 (Care and Welfare of Residents in Designated Centres for OlderPeople) Regulations 2009.Action required:Revise the register / directory of residents with the required information as outlined inthe Health Act 2007 (Care and Welfare of Residents in Designated Centres for OlderPeople) Regulations 2009.Reference:Health Act 2007Regulation 23: Directory of ResidentsStandard 32: Register and Residents’ RecordsPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:A rev<strong>ie</strong>w of the register / directory of residents is being undertakenand all information required as per legislation / regulation /standards will be provided.Two weeksPage 20 of 25
10.The provider is failing to comply with a regulatory requirement in thefollowing respect:The provider failed to provide evidence to suggest that there was comprehensive indepthongoing rev<strong>ie</strong>w of care planning in terms of healthcare needs for residents.Action required:Undertake ongoing assessment and care planning of all residents, subject to regularrev<strong>ie</strong>w.Reference:Health Act 2007Regulation 8: Assessment and Care PlanStandard 11: The Resident’s Care PlanPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:It is our policy to prepare an in-depth care plan for each of ourresidents on admission. The care plan is discussed, agreed andformalised with the involvement of the resident or his / herrepresentative. Care plans are rev<strong>ie</strong>wed at three-monthly intervalsor in advance of the rev<strong>ie</strong>w date if required.CompletedAll rev<strong>ie</strong>ws are completed by the staff nurses on a rotational basisthus ensuring that each staff nurse has the opportunity, over time,to rev<strong>ie</strong>w each and every residents’ care plan.11. The provider is failing to comply with a regulatory requirement in thefollowing respect:The provider failed to ensure that menus, with choice, were displayed for the residents’information.Action required:Ensure that the daily menu is displayed in a suitable format and in an appropriatelocation so that the resident or his / her representative knows what is available at eachmealtime.Reference:Health Act 2007Regulation 21: Provision of Information to ResidentsStandard 19: Meals and MealtimesPage 21 of 25
Please state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:A menu board has been placed in the dining room, and displays themeal choices of the dayCompleted12. The provider is failing to comply with a regulatory requirement in thefollowing respect:The provider failed to ensure that dirty clothes were segregated at source.Action required:Ensure that adequate facilit<strong>ie</strong>s are provided and arrangements made for residents’clothing to be sorted and kept separately.Reference:Health Act 2007Regulation 13: ClothingStandard 25: Physical EnvironmentPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:We have introduced a colour-coded laundry bag system to addressthe issue of segregation of dirty clothes at source.Completed.We endeavour at all times to ensure that residents’ clothing issorted and kept separately.13. The provider is failing to comply with a regulatory requirement in thefollowing respect:Three residents occupy room 18. The provider shall have regard for suitable storagefacilit<strong>ie</strong>s for present residents’ needs and future residents.Action required:Rev<strong>ie</strong>w storage for residents’ use and needs.Page 22 of 25
Reference:Health Act 2007Regulation 19: PremisesStandard 25: The Physical EnvironmentPlease state the actions you have taken or are planning totake with timescales:Timescale:Provider’s response:We are in the process of discussing with each individualresident/representative the subject of storage of personalbelongings. Where a resident is satisf<strong>ie</strong>d with the available storagewe will take no action, and where a request for further storage ismade, we will comply.One monthPage 23 of 25
RecommendationsThese recommendations are taken from the best practice described in theNational Quality Standards for Residential Care settings for Older People inIreland and the registered provider should consider them as a way ofimproving the service.StandardStandard 24:Training andSupervisionBest practice recommendationsStaff appraisals would ensure staff have the skills and exper<strong>ie</strong>ncenecessary.A record of all staff development is maintained.Page 24 of 25
Any comments the provider may wish to make:Provider’s response:This was our first <strong>inspection</strong> by HIQA and overall we found that the <strong>inspection</strong> teamcarr<strong>ie</strong>d out their dut<strong>ie</strong>s in a most professional and courteous manner. We wereafforded ample opportunity to discuss and clarify all matters raised by the <strong>inspection</strong>team.Discussions with residents following the <strong>inspection</strong> indicated that the residentsspoken to by the <strong>inspection</strong> team found the process to be non-invasive and enjoyedengaging with the inspectors.We would also like to add that at a staff meeting following the <strong>inspection</strong> the feedbackfrom the staff present on the day of the <strong>inspection</strong> was that they felt that theHIQA <strong>inspection</strong> system was far more positive and engaging than previous systems,and they felt that their opinions and inputs were valued and in some way reflectedtheir daily commitment to the residents and their efforts to further develop theircaring skills through ongoing training.Provider’s name: The Caring Specialists LtdDate: 23 November 2009Page 25 of 25